Analytical Method Validation for Pharmaceutical Quantification: A Comprehensive Guide to Principles, Practices, and Regulatory Compliance
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for analytical method validation in pharmaceutical quantification.
Analytical Method Validation for Pharmaceutical Quantification: A Comprehensive Guide to Principles, Practices, and Regulatory Compliance
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for analytical method validation in pharmaceutical quantification. It explores foundational principles, methodological applications, troubleshooting strategies, and validation protocols aligned with ICH Q2(R1), FDA, and EMA guidelines. Covering critical parameters from specificity and linearity to robustness and lifecycle management, the content addresses common challenges in techniques like HPLC and LC-MS/MS, offers optimization strategies, and emphasizes the role of validation in ensuring product quality, regulatory compliance, and patient safety.
The Pillars of Reliability: Understanding Analytical Method Validation and Its Regulatory Landscape
Defining Analytical Method Validation and Its Critical Role in Pharmaceutical Quality
Analytical method validation is the documented process of demonstrating that an analytical procedure is suitable for its intended purpose, ensuring that the method consistently provides reliable and accurate data about the quality of a pharmaceutical product [1]. This process confirms that a method's performance characteristics—such as accuracy, precision, and specificity—meet predefined acceptance criteria established during method development [2]. In pharmaceutical manufacturing, validated analytical methods form the foundation of quality control, ensuring that drug products meet stringent standards for quality, safety, and efficacy throughout their lifecycle [1].
The role of analytical method validation extends beyond technical compliance to become a fundamental requirement for regulatory submissions worldwide. Regulatory bodies including the U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and other international authorities require extensive validation data for both clinical trial applications and marketing authorizations [2]. Without properly validated methods, pharmaceutical companies risk unreliable data, regulatory noncompliance, and potential product recalls, making method validation an indispensable component of pharmaceutical development and manufacturing [1].
Core Validation Parameters and Their Significance
Analytical method validation systematically evaluates specific performance characteristics to ensure the method produces trustworthy results. The International Council for Harmonisation (ICH) guidelines, particularly ICH Q2(R2), define the core parameters that must be assessed during validation [3] [4]. These parameters collectively demonstrate that an analytical procedure is fit-for-purpose, with the specific validation requirements depending on the type of method being validated (e.g., identification, impurity testing, or assay).
Table 1: Key Validation Parameters and Their Definitions
| Parameter | Definition | Role in Method Quality |
|---|---|---|
| Accuracy [1] [3] | Closeness of test results to the true value | Ensures method measures what it claims to measure |
| Precision [1] [3] | Degree of agreement among repeated measurements | Confirms method reproducibility under normal conditions |
| Specificity [1] [3] | Ability to distinguish analyte from interfering components | Demonstrates method selectivity in complex matrices |
| Linearity [3] | Ability to produce results proportional to analyte concentration | Establishes method's quantitative capabilities |
| Range [3] | Interval between upper and lower analyte concentrations with suitable precision, accuracy, and linearity | Defines method's operational boundaries |
| Limit of Detection (LOD) [1] [3] | Lowest amount of analyte that can be detected | Determines method sensitivity for trace analysis |
| Limit of Quantitation (LOQ) [1] [3] | Lowest amount of analyte that can be quantified with acceptable accuracy and precision | Establishes lower limit for reliable quantification |
| Robustness [1] [3] | Capacity to remain unaffected by small, deliberate variations in method parameters | Assesses method reliability during normal use |
Each validation parameter serves a distinct purpose in establishing overall method reliability. Accuracy confirms that the method measures what it claims to measure, typically assessed by analyzing samples of known concentration or through spiking studies [1] [3]. Precision, which includes repeatability (intra-assay), intermediate precision (inter-day, inter-analyst), and reproducibility (inter-laboratory), confirms that the method produces consistent results when applied repeatedly to multiple samplings of a homogeneous sample [3]. Specificity ensures the method can accurately measure the analyte in the presence of potential interferents like impurities, degradation products, or excipients, which is particularly critical for stability-indicating methods [1].
The relationship between these parameters creates a comprehensive picture of method performance. For instance, the validation of linearity and range establishes the concentration interval over which the method provides accurate and precise results, while LOD and LOQ define the method's sensitivity at lower concentration levels [3]. Robustness testing evaluates the method's resilience to small, deliberate variations in procedural parameters like temperature, pH, or mobile phase composition, helping to establish system suitability criteria and identify critical control points for consistent method application [1] [3].
Experimental Protocols for Key Validation Experiments
Accuracy and Precision Assessment
The experimental protocol for determining accuracy involves analyzing samples with known concentrations of the target analyte and comparing the measured values to the true values [3]. This is typically performed using a minimum of nine determinations across a minimum of three concentration levels covering the specified range [3]. For drug substance analysis, accuracy may be assessed by applying the method to synthetic mixtures spiked with known quantities of impurities, or by comparing results with those from a well-characterized reference method [3]. For drug products, accuracy is often determined through recovery studies using placebo formulations spiked with known amounts of the active pharmaceutical ingredient (API).
Precision validation encompasses repeatability, intermediate precision, and reproducibility. Repeatability (intra-assay precision) is assessed by performing a minimum of six determinations at 100% of the test concentration, or nine determinations covering the complete specified range [3]. Intermediate precision evaluates the influence of random events within the same laboratory, such as different days, different analysts, or different equipment, with experimental designs that incorporate these variables systematically. Reproducibility expresses the precision between different laboratories, typically assessed during method transfer studies [3]. The results for both accuracy and precision are expressed as the relative standard deviation (RSD) for precision and percentage recovery for accuracy, with acceptance criteria dependent on the method's intended use and the stage of product development.
Specificity and Linearity Evaluation
Specificity experiments demonstrate that the method can unequivocally assess the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, or matrix components [1] [3]. The protocol typically involves challenging the method with samples containing potential interferents and demonstrating that the analyte response is unaffected. For chromatographic methods, this includes demonstrating resolution between closely eluting peaks, while for spectroscopic methods, it may involve showing no interference at the detection wavelength. For stability-indicating methods, specificity is proven by subjecting the sample to stress conditions (forced degradation) and demonstrating that the method can separate and quantify degradation products from the main analyte [1].
Linearity is established by preparing and analyzing a series of solutions with concentrations spanning the declared range of the method, typically using a minimum of five concentration levels [3]. The results are evaluated by plotting the response as a function of analyte concentration and applying statistical analysis of the regression line, including the y-intercept, slope, and correlation coefficient. The range is derived from the linearity data and is established by confirming that the method provides acceptable levels of accuracy, precision, and linearity across the entire concentration interval [3].
Comparative Analysis of Validation Approaches
The landscape of analytical method validation has evolved significantly, with traditional approaches being supplemented by modern, risk-based methodologies. The recent simultaneous publication of ICH Q2(R2) and ICH Q14 represents a significant shift from a prescriptive, "check-the-box" approach to a more scientific, lifecycle-based model [3]. This evolution reflects the pharmaceutical industry's growing sophistication in analytical science and the need for more flexible, efficient validation strategies.
Table 2: Comparison of Traditional vs. Modern Validation Approaches
| Aspect | Traditional Approach | Modern Lifecycle Approach |
|---|---|---|
| Philosophy | One-time event after method development [3] | Continuous process throughout method lifetime [3] |
| Focus | Verification of predefined parameters [3] | Understanding and controlling method performance [3] |
| Regulatory Foundation | ICH Q2(R1) [3] | ICH Q2(R2) and ICH Q14 [3] |
| Key Tool | Fixed validation protocol [3] | Analytical Target Profile (ATP) [5] |
| Change Management | Requires revalidation for most changes [1] | Science- and risk-based change management [3] |
| Data Utilization | Limited to validation report | Ongoing performance monitoring [5] |
The modern validation approach introduces the Analytical Target Profile (ATP) as a prospective summary of the method's intended purpose and desired performance characteristics [3] [5]. By defining the ATP at the beginning of method development, laboratories can employ a risk-based approach to design a fit-for-purpose method and a validation plan that directly addresses its specific needs. This represents a fundamental shift from "validation as a conclusion" to "validation as a confirmation of proper design."
The enhanced approach described in ICH Q14, while requiring a deeper understanding of the method, allows for more flexibility in post-approval changes through a risk-based control strategy [3]. This is particularly valuable in today's fast-paced development environment, where methods may need to be adapted to changing manufacturing processes or analytical technologies. The traditional and modern approaches are not mutually exclusive; rather, the modern approach builds upon the foundation of traditional parameters while providing a more comprehensive framework for ensuring long-term method reliability.
Method-Comparison Studies: Protocols and Statistical Analysis
Method-comparison studies are essential when introducing a new method to determine if it produces results equivalent to an established reference method [6]. The fundamental question addressed is whether one can measure the same analyte with either method and obtain comparable results, making these studies critical for method transfers, replacements, or technology upgrades.
Experimental Design for Method-Comparison
Proper design of a method-comparison study requires careful consideration of several factors. The samples should cover the entire reportable range of the method and should be measured simultaneously by both methods to avoid time-related changes in the sample [6]. The number of samples should be sufficient to provide statistical power, typically at least 40 samples distributed across the measuring range, with more samples required if the range is wide [6]. The samples should ideally be native patient samples representing the typical population encountered in routine testing, rather than spiked samples or standards, to ensure the comparison reflects real-world conditions.
Statistical Analysis and Interpretation
The statistical analysis of method-comparison data has evolved, with current recommendations emphasizing both regression analysis and difference plots (Bland-Altman plots) [6] [7]. While correlation coefficients were historically used, they are now considered insufficient because they measure the strength of relationship rather than agreement between methods [7]. Perfect correlation (r = 1.000) does not mean the methods agree—systematic differences can still exist [7].
Regression analysis, particularly Deming regression, provides estimates of constant systematic error (through the y-intercept) and proportional systematic error (through the slope) [7]. These estimates allow for the calculation of the predicted bias at any medically important decision level, providing crucial information about the clinical impact of method differences.
Bland-Altman analysis involves plotting the difference between the two methods against the average of the two methods [6] [7]. This visualization helps identify trends in the differences across the measuring range and establishes the limits of agreement (mean difference ± 1.96 standard deviations of the differences), within which 95% of the differences between the two methods are expected to fall [6].
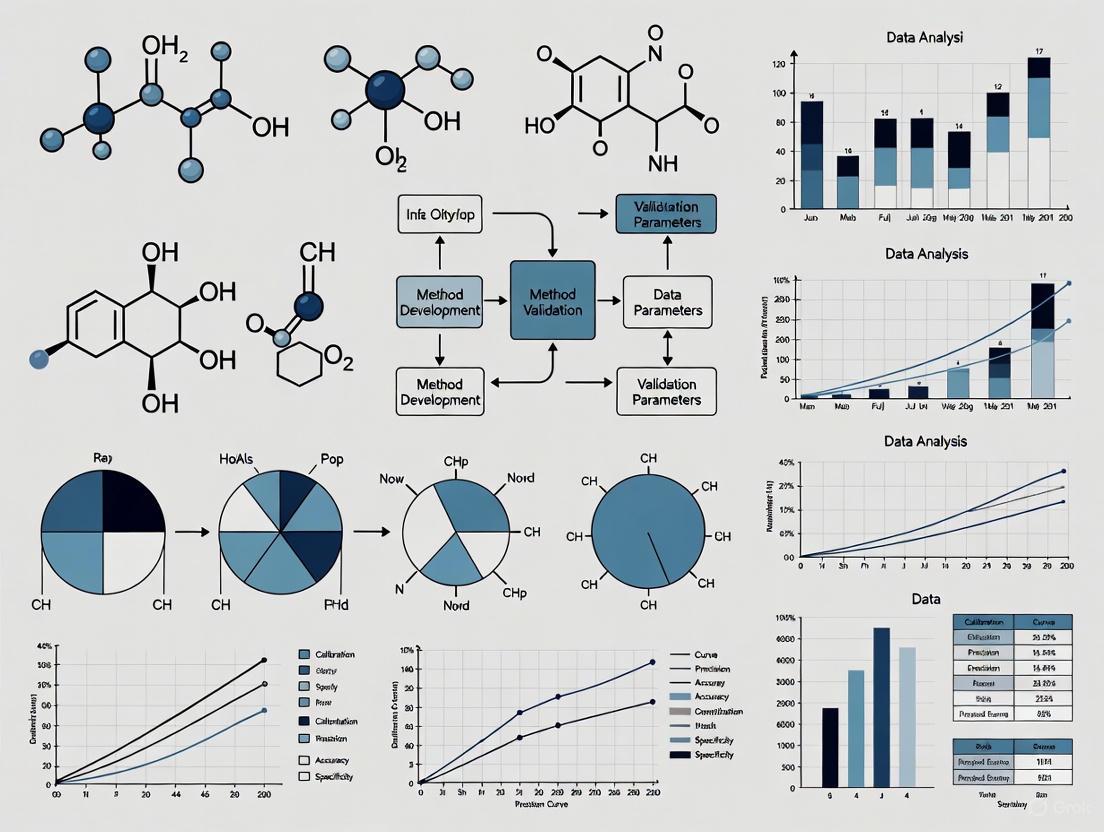
Method Comparison Study Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful analytical method validation relies on high-quality reagents and materials that ensure method reliability and reproducibility. The selection of appropriate reagents constitutes a critical aspect of method development and validation, directly impacting the method's performance characteristics.
Table 3: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Function in Validation | Quality Considerations |
|---|---|---|
| Reference Standards [7] | Primary measure of accuracy; defines the analytical scale | Certified purity, proper documentation, and storage conditions |
| Chromatographic Columns | Defines separation characteristics; impacts specificity | Column chemistry, lot-to-lot reproducibility, stability |
| Mobile Phase Reagents | Creates separation environment; affects retention and selectivity | HPLC-grade purity, low UV absorbance, controlled pH |
| Sample Preparation Reagents | Extract, isolate, or derivative analytes; minimize matrix effects | Purity, minimal background interference, lot consistency |
| Quality Control Materials [7] | Monitor method performance over time; assess precision | Commutability with patient samples, defined target values, stability |
| Cu(II)GTSM | Cu(II)GTSM, MF:C6H10CuN6S2, MW:293.9 g/mol | Chemical Reagent |
| 1-Methyl-1-propylhydrazine | 1-Methyl-1-propylhydrazine, CAS:4986-49-6, MF:C4H12N2, MW:88.15 g/mol | Chemical Reagent |
The quality of reference standards deserves particular emphasis, as these materials serve as the foundation for method accuracy [7]. Pharmacopeial standards, when available, provide the highest level of confidence due to their rigorous characterization and certification processes. For novel compounds without official standards, well-characterized in-house standards with comprehensive certificates of analysis are essential. During validation, it's advisable to analyze both commercial calibrators and primary standards together when possible to verify agreement, with any discrepancies investigated and resolved before proceeding with full validation [7].
The movement toward Quality-by-Design (QbD) principles in analytical method development further emphasizes the importance of understanding how reagent attributes affect method performance [5]. By applying risk assessment tools to identify critical reagent attributes, scientists can establish appropriate control strategies that ensure method robustness throughout its lifecycle. This proactive approach to reagent selection and qualification contributes significantly to reducing method variability and maintaining data integrity.
Analytical method validation stands as an indispensable discipline within pharmaceutical quality systems, serving as the critical bridge between method development and routine application. The evolving regulatory landscape, characterized by the adoption of ICH Q2(R2) and ICH Q14, emphasizes a lifecycle approach that integrates development, validation, and ongoing monitoring into a seamless continuum [3]. This paradigm shift from a one-time validation event to continuous method verification represents the future of analytical quality in pharmaceutical manufacturing.
The critical role of analytical method validation extends beyond regulatory compliance to fundamentally underpin product quality and patient safety. As pharmaceutical therapies become increasingly complex—with the rise of biologics, gene therapies, and personalized medicines—the demands on analytical methods and their validation will continue to intensify [8] [5]. By embracing modern validation approaches, implementing robust statistical analyses in method-comparison studies, and maintaining rigorous standards for research reagents, pharmaceutical scientists can ensure that analytical methods consistently generate reliable data to support the development and manufacture of high-quality drug products.
Analytical method validation is a critical process in pharmaceutical development that confirms a particular analytical procedure is suitable for its intended purpose, ensuring the reliability, accuracy, and consistency of data used to assess drug safety, quality, and efficacy. Regulatory frameworks provide structured approaches to validate these methods, with global harmonization efforts aimed at standardizing requirements across regions. The International Council for Harmonisation (ICH), U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and United States Pharmacopeia (USP) establish the primary guidelines governing this field. For pharmaceutical manufacturers and researchers, understanding the similarities, differences, and recent updates within these frameworks is essential for regulatory compliance and successful application submissions across international markets.
The validation of analytical methods underpins the entire drug development lifecycle, from initial discovery through commercial manufacturing and post-approval changes. These methods are used to assess critical quality attributes including drug identity, potency, purity, and performance characteristics. As pharmaceutical modalities evolve to include more complex molecules such as biologics, cell therapies, and gene therapies, the analytical methods and their validation requirements must similarly advance. Recent trends emphasize a lifecycle approach to method validation, incorporating principles of Quality by Design (QbD) and real-time release testing to enhance method robustness while accelerating time-to-market.
Comparative Analysis of Regulatory Frameworks
Table 1: Key Regulatory Guidelines for Analytical Method Validation
| Guideline | Issuing Authority | Current Version/Status | Geographic Applicability | Primary Scope |
|---|---|---|---|---|
| ICH Q2(R2) | International Council for Harmonisation | Implemented Oct 2025 [9] | Global (ICH member regions) | Analytical procedure validation for drug substances & products |
| FDA Guidance (Pharmaceutical) | U.S. Food and Drug Administration | Aligns with ICH Q2(R2) [5] | United States | Analytical methods for pharmaceutical applications |
| EMA Guideline | European Medicines Agency | Adopted ICH Q2(R2) [4] | European Union | Analytical methods for medicinal products |
| USP General Chapters | United States Pharmacopeia | USP 48-NF 43 (2025) [10] | Primarily United States | Compendial methods and standards |
The regulatory landscape for analytical method validation has recently undergone significant harmonization with the implementation of ICH Q2(R2) in October 2025, which has been adopted by both the FDA and EMA [9] [4]. This represents a major step toward global standardization, replacing previous region-specific requirements. The ICH guideline serves as the foundation for both FDA and EMA expectations, though each agency maintains specific administrative procedures and additional guidance documents for specialized areas such as bioanalytical method validation [11]. Meanwhile, USP standards continue to provide specific monographs and general chapters that define official testing methods and acceptance criteria recognized by FDA as legally enforceable for drugs marketed in the United States [10].
Validation Parameters and Requirements
Table 2: Comparison of Validation Parameters Across Frameworks
| Validation Parameter | ICH Q2(R2) | FDA (Pharma) | EMA | USP |
|---|---|---|---|---|
| Accuracy/Recovery | Required | Required | Required | Required |
| Precision (Repeatability) | Required | Required | Required | Required |
| Precision (Intermediate Precision) | Required | Required | Required | Required |
| Specificity/Selectivity | Required | Required | Required | Required |
| Linearity | Required | Required | Required | Required |
| Range | Required | Required | Required | Required |
| Detection Limit (LOD) | Conditionally Required | Conditionally Required | Conditionally Required | Conditionally Required |
| Quantitation Limit (LOQ) | Conditionally Required | Conditionally Required | Conditionally Required | Conditionally Required |
| Robustness | Recommended | Recommended | Recommended | Recommended |
All major regulatory frameworks require demonstration of the same fundamental validation parameters, though implementation details may vary slightly. The ICH Q2(R2) guideline provides comprehensive definitions and methodological approaches for establishing each parameter, with FDA and EMA largely adopting these recommendations [4]. The EMA has historically provided more detailed practical guidance on experimental conduct, while FDA documentation offers more comprehensive reporting recommendations [11]. USP standards incorporate these same validation parameters but present them within the context of compendial methods that become legally recognized standards when referenced in a product monograph [10]. A significant evolution in the ICH Q2(R2) guideline is its emphasis on a lifecycle approach to method validation, encouraging continuous method verification and improvement rather than treating validation as a one-time activity [5].
Experimental Protocols for Method Validation
Standard Validation Methodology
The validation of analytical methods follows systematically designed experimental protocols to demonstrate that the method consistently produces reliable results. A standard validation protocol includes the following elements:
Accuracy Studies: Typically determined using spiked recovery experiments with known concentrations of analyte across the specified range (e.g., 50%, 100%, 150% of target concentration). Accuracy should be established for each matrix component in the case of complex formulations. The percent recovery is calculated as
(Measured Concentration / Theoretical Concentration) × 100, with acceptance criteria generally requiring recovery within 98-102% for drug substance assays [4].Precision Evaluation: Conducted at three levels: (1) Repeatability (intra-assay precision) using at least six determinations at 100% of the test concentration; (2) Intermediate precision examining within-laboratory variations (different days, analysts, equipment); and (3) Reproducibility between laboratories for methods transferred between sites. Results are expressed as relative standard deviation (RSD%), with criteria typically requiring ≤2% for assay methods [4].
Specificity/Discrimination: Demonstrated by analyzing samples containing potentially interfering compounds (impurities, excipients, degradation products) to confirm the method can unequivocally assess the analyte in the presence of these components. For stability-indicating methods, forced degradation studies (acid/base hydrolysis, oxidation, thermal stress, photolysis) are performed to demonstrate separation of degradation products from the analyte peak [4].
Protocol Implementation Across Frameworks
While the core validation parameters remain consistent across regulatory frameworks, implementation details may vary:
Linearity and Range: Established by preparing analyte solutions at a minimum of five concentration levels across the specified range. The response is plotted against concentration, and statistical analysis (correlation coefficient, y-intercept, slope of regression line) is performed. The ICH Q2(R2) guideline emphasizes that R² values alone are insufficient to demonstrate linearity, requiring additional statistical evaluation of residuals and lack-of-fit [12].
Detection and Quantitation Limits: Determined using signal-to-noise ratio (typically 3:1 for LOD and 10:1 for LOQ) or based on the standard deviation of the response and slope of the calibration curve (
LOD = 3.3σ/SandLOQ = 10σ/Swhere σ is the standard deviation of response and S is the slope of the calibration curve) [4].Robustness Testing: Evaluated by deliberately varying method parameters (mobile phase composition, pH, flow rate, column temperature) within a realistic range and measuring the impact on method performance. Experimental design approaches such as Design of Experiments (DoE) are increasingly employed to efficiently evaluate multiple parameters simultaneously [5].
Visualization of Regulatory Relationships and Workflows
Figure 1: Regulatory Framework Relationships and Workflow
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Analytical Method Validation
| Reagent/Material | Function in Validation | Regulatory Considerations |
|---|---|---|
| Certified Reference Standards | Quantification and method calibration | Must be of certified purity and traceable to national/international standards |
| Chromatographic Columns | Separation of analytes from impurities | Column performance must be verified; multiple column batches should be evaluated for robustness |
| Biological Matrices | Simulation of in vivo conditions for bioanalytical methods | Source and handling must be documented; stability under storage conditions must be verified |
| Reagent-Grade Solvents | Mobile phase preparation and sample dilution | Must meet purity specifications; potential interference must be characterized |
| System Suitability Standards | Verification of instrument performance prior to analysis | Must be stable and representative of analytes; criteria established in validation protocol |
The selection and qualification of research reagents represents a critical component of method validation. Certified reference standards serve as the foundation for establishing method accuracy, linearity, and range, and must be thoroughly characterized with documentation of purity, storage conditions, and stability data [10]. For chromatographic methods, multiple batches of columns from the same manufacturer and equivalent columns from different manufacturers should be evaluated during robustness testing to ensure method reliability when columns are replaced. In bioanalytical method validation, appropriate biological matrices (plasma, serum, urine) must be sourced and handled according to strict protocols to prevent analyte degradation or interference [13] [11]. All reagents should be accompanied by certificates of analysis and stored according to manufacturer recommendations, with documentation maintained for regulatory inspections.
Emerging Trends and Future Directions
The field of analytical method validation continues to evolve in response to technological advancements and regulatory harmonization. Several significant trends are shaping current practices:
Enhanced Lifecycle Management: The integration of ICH Q12 principles with ICH Q2(R2) promotes a more comprehensive lifecycle approach to analytical procedures, emphasizing continuous verification and management of post-approval changes [9] [5]. This represents a shift from traditional "one-time" validation toward ongoing method performance monitoring.
Adoption of Advanced Technologies: Regulatory frameworks are increasingly accommodating sophisticated analytical technologies including high-resolution mass spectrometry (HRMS), multi-attribute methods (MAM), and hyphenated techniques such as LC-MS/MS [5]. These technologies enable more comprehensive characterization of complex molecules but require specialized validation approaches.
Quality by Design (QbD) Principles: Method development and validation increasingly incorporates QbD approaches, employing statistical design of experiments (DoE) to systematically optimize method parameters and establish method operable design regions [5]. This science-based approach enhances method robustness while providing greater regulatory flexibility.
Real-Time Release Testing (RTRT): There is growing regulatory acceptance of RTRT approaches that utilize process analytical technology (PAT) to enable quality control based on process data rather than end-product testing [5]. This shift requires validation of in-line or on-line analytical methods integrated directly into manufacturing processes.
Digital Transformation: Regulatory agencies are increasingly addressing data integrity requirements for computerized analytical systems, with emphasis on the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate) [5]. Cloud-based laboratory information management systems (LIMS) and electronic notebooks must undergo rigorous validation to ensure data reliability.
The ongoing harmonization of regulatory expectations through ICH initiatives, particularly the implementation of ICH Q2(R2), provides greater consistency for global drug development while accommodating technological innovation in analytical sciences. Pharmaceutical manufacturers and researchers should maintain awareness of these evolving standards to ensure compliance and optimize their analytical development strategies.
In the development and quality control of pharmaceuticals, the reliability of analytical data is paramount. This reliability is established through a rigorous process called analytical method validation, which demonstrates that a laboratory test method is suitable for its intended purpose [14]. For researchers and scientists in drug development, understanding and effectively evaluating the core validation parameters—Accuracy, Precision, Specificity, Linearity, and Range—is a fundamental skill. These interconnected parameters form the foundation for ensuring that analytical methods consistently produce trustworthy data to support the safety, efficacy, and quality of drug substances and products [15].
The Pillars of Method Validation: Core Parameters Defined
The five core parameters provide a complete picture of an analytical method's performance, from its basic function to its boundaries of reliable operation. Their definitions and significance are summarized in the table below.
Table 1: Definition and Significance of Core Validation Parameters
| Parameter | Core Definition | Significance in Pharmaceutical Analysis |
|---|---|---|
| Accuracy | The closeness of agreement between a test result and an accepted reference value (the "true" value) [15] [14]. | Ensures that the measured concentration of an Active Pharmaceutical Ingredient (API) or impurity is correct, directly impacting dosage and safety assessments [16]. |
| Precision | The closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample [15] [14]. | Evaluates the method's random error and reproducibility, guaranteeing consistent results across different analysts, days, and equipment [15]. |
| Specificity | The ability to assess the analyte unequivocally in the presence of components that may be expected to be present, such as impurities, degradation products, or excipients [15] [14]. | Confirms that the measured signal is solely from the target analyte, which is critical for identity tests, impurity profiling, and stability-indicating methods [17]. |
| Linearity | The ability of the method to obtain test results that are directly proportional to the concentration of the analyte within a given range [15]. | Demonstrates that the method's response (e.g., chromatographic peak area) is a predictable function of the analyte's concentration, which is foundational for accurate quantification. |
| Range | The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the method has suitable levels of accuracy, precision, and linearity [15]. | Defines the operational limits of the method, ensuring it is validated for all concentrations encountered during testing, from the lower limit of quantitation to 120-130% of the specification limit [18]. |
A Quantitative Framework: Acceptance Criteria and Data Interpretation
Establishing pre-defined, justified acceptance criteria is critical for objective method validation [19]. The following table provides a summary of typical acceptance criteria for these parameters, illustrating how quantitative data is used to judge method suitability.
Table 2: Typical Acceptance Criteria for Core Validation Parameters
| Parameter | Typical Acceptance Criteria | Data Presentation & Calculation |
|---|---|---|
| Accuracy | ≤ 10% of tolerance (for analytical methods) [20]. Often expressed as % Recovery (e.g., 98-102%) [19]. | Reported as: % Bias, % Recovery, or % of tolerance.Calculation: (Mean Observed Concentration / Theoretical Concentration) * 100 [15]. |
| Precision | Repeatability: ≤ 25% of tolerance (for analytical methods) [20]. Expressed as %RSD (e.g., ≤ 2% for assay) [19]. | Reported as: % Relative Standard Deviation (%RSD), Standard Deviation, or % of tolerance.Calculation: (Standard Deviation / Mean) * 100 [20] [15]. |
| Specificity | Demonstrate no interference from blank or placebo. For chromatographic methods, ensure baseline resolution of analytes from potential interferents [15]. | Reported as: Chromatographic resolution, spectral comparison, or demonstration of no response in blank. For quantification, specificity can be reported as a % of tolerance (Excellent: ≤5%) [20]. |
| Linearity | A correlation coefficient (R²) of ≥ 0.998, visually random residual plot, and a y-intercept not significantly different from zero [20] [19]. | Reported as: Correlation coefficient (R²), slope, y-intercept, and residual plot from a linear regression analysis [15]. |
| Range | Specified from a low to high concentration, encompassing the product specification limits. For an assay, typically 80% - 120% of the test concentration [15] [18]. | Defined by: The lowest and highest concentrations for which accuracy, precision, and linearity have been demonstrated. The range must cover all specification limits [18]. |
From Theory to Practice: Experimental Protocols for Parameter Assessment
Protocol for Accuracy and Precision
Accuracy and precision are often evaluated concurrently in a single experimental design [18].
- Methodology: Prepare a minimum of nine determinations across the specified range of the procedure, typically comprising three concentrations (e.g., 80%, 100%, 120% of the target concentration), each analyzed in triplicate [15]. The samples are typically prepared by spiking a placebo with known quantities of the reference standard of the analyte [15].
- Data Analysis:
- Accuracy: Calculate the mean recovery for each concentration level. The mean recovery should be within the pre-defined acceptance criteria (e.g., 98-102%) [19].
- Precision (Repeatability): Calculate the %RSD for the nine determinations (or for the triplicate at the 100% level). The %RSD should meet the pre-defined criteria [15].
Protocol for Specificity
- Methodology: For an assay, specificity is demonstrated by analyzing samples containing the analyte along with potential interferents. This includes:
- Individually: The pure analyte, the placebo/excipients, and potential impurities or degradation products.
- In Combination: The analyte spiked into the placebo along with impurities/degradation products [15].
- Forced degradation studies (stressing the drug product under acid, base, oxidative, thermal, and photolytic conditions) are also used to demonstrate the method's stability-indicating properties [18].
- Data Analysis: The method is specific if there is no interference from the placebo or degradation products at the retention time of the analyte, and if the analyte peak is pure (as demonstrated by techniques like diode-array detection). For quantification, the recovery of the analyte from the spiked mixture should be within acceptance criteria for accuracy [20].
Protocol for Linearity and Range
- Methodology: Prepare a minimum of five concentrations of the analyte over a range that encompasses the specification limits, typically from 80% to 120% of the target concentration for an assay [15] [18]. Analyze each concentration, and plot the instrument response (e.g., peak area) against the theoretical concentration.
- Data Analysis: Perform linear regression analysis on the data to calculate the correlation coefficient (R²), slope, and y-intercept. Visually inspect the plot of residuals (the difference between the calculated and observed values) versus concentration; it should show no systematic pattern [20]. The range is then established as the interval between the lowest and highest concentrations for which the linearity, accuracy, and precision are acceptable [15].
The workflow below illustrates the strategic sequence for establishing and validating the linear range of an analytical method.
The Scientist's Toolkit: Essential Reagents and Materials
A successful validation study relies on high-quality, well-characterized materials. The following table lists key reagent solutions and their critical functions.
Table 3: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Function & Importance |
|---|---|
| Certified Reference Standard | Provides the accepted "true value" for the analyte, serving as the benchmark for all accuracy and linearity assessments. Its purity and qualification are foundational [15]. |
| High-Purity Solvents & Reagents | Ensure the analytical background (e.g., mobile phase, sample solvent) does not generate interfering signals, which is crucial for achieving the required specificity, LOD, and LOQ. |
| Well-Characterized Placebo | A mixture of all drug product excipients without the API. Used in specificity experiments to prove excipients do not interfere, and in accuracy studies for recovery calculations [15]. |
| System Suitability Test (SST) Solutions | A specific mixture used to verify that the analytical system (e.g., HPLC) is performing adequately at the time of the test. It typically checks for parameters like resolution, precision, and tailing factor [15]. |
| Stability-Indicating Solutions | Samples of the drug substance or product that have been intentionally degraded (e.g., by heat, light, acid). Used to rigorously challenge the method's specificity and prove it can monitor stability [18]. |
| Azanium;iron(3+);sulfate | Azanium;iron(3+);sulfate, MF:FeH4NO4S+2, MW:169.95 g/mol |
| N-Boc-6-methyl-L-tryptophan | N-Boc-6-methyl-L-tryptophan|Building Block |
The Interconnected Framework of Analytical Validation
The core validation parameters are not isolated checklist items; they form an integrated system where the performance of one parameter directly influences or depends on others. For instance, the validation of Range is contingent on having already demonstrated acceptable Linearity, Accuracy, and Precision across that interval [15]. Similarly, a method's Accuracy can be compromised by a lack of Specificity if interfering substances contribute to the measured signal [14]. The following diagram illustrates this critical interdependence.
Ultimately, a robust analytical method is one where all core parameters have been thoroughly investigated and balanced. The data generated from these validation studies provides the documented evidence required by regulators and gives drug development professionals the confidence to make critical decisions about product quality, from early development through to commercial batch release [20] [19]. This rigorous approach ensures that every medicine that reaches patients is proven to be safe, effective, and of high quality.
In the field of pharmaceutical analysis, ensuring that analytical methods produce reliable, accurate, and reproducible results is paramount. Method validation provides documented evidence that a procedure is fit for its intended purpose and meets regulatory standards. Among the key performance characteristics established during this process are the Limit of Detection (LOD), Limit of Quantitation (LOQ), robustness, and ruggedness. These parameters define the sensitivity and reliability of an analytical method, confirming it can consistently detect and measure analytes at low concentrations and withstand minor, expected variations in operational conditions. This guide explores these advanced parameters, comparing methodologies and providing the experimental protocols essential for researchers and drug development professionals.
Understanding the Fundamental Parameters
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
The Limit of Detection (LOD) is defined as the lowest concentration of an analyte in a sample that can be reliably detected, though not necessarily quantified, under the stated operational conditions of the method [21] [22]. It represents the point at which a measured signal can be distinguished from background noise with a defined level of confidence. In practice, it is a limit test that specifies whether an analyte is above or below a certain value [23].
The Limit of Quantitation (LOQ), also called the Limit of Quantification, is the lowest concentration of an analyte that can be quantitatively determined with acceptable precision and accuracy [21] [24]. Unlike the LOD, the LOQ requires that the method provides reliable numerical results at that low concentration, making it crucial for accurate quantification at trace levels [22].
Robustness and Ruggedness
Robustness is the capacity of an analytical method to remain unaffected by small, deliberate variations in its method parameters [25]. It provides an indication of the method's reliability during normal use [21] [26]. In essence, a robust method will yield consistent results despite minor changes in predefined parameters, such as mobile phase pH, column temperature, or flow rate in liquid chromatography (LC) methods.
Ruggedness is a closely related term, often used interchangeably with robustness. However, some interpretations make a distinction: ruggedness may refer to the degree of reproducibility of results under a variety of normal test conditions, such as different analysts, laboratories, instruments, or reagent lots [23] [26]. It is a measure of the method's susceptibility to variations in external, environmental factors.
Experimental Determination and Protocols
Protocols for Determining LOD and LOQ
There are multiple accepted approaches for determining LOD and LOQ. The choice of method depends on the specific application and regulatory requirements.
Table 1: Methods for Determining LOD and LOQ
| Method | Description | Typical Acceptance Criteria | Application Context |
|---|---|---|---|
| Signal-to-Noise Ratio (S/N) | Compares the measured signal from a low-concentration sample to the background noise [21] [23]. | LOD: S/N ≥ 3:1 [21] [22]LOQ: S/N ≥ 10:1 [21] [22] | Chromatographic methods (HPLC, LC-MS) where baseline noise is easily measurable. |
| Standard Deviation of the Response and Slope | Uses the standard deviation of the response and the slope of the calibration curve [23]. | LOD = 3.3 × (SD/S)LOQ = 10 × (SD/S)Where SD = standard deviation of response, S = slope of the calibration curve [23]. | A statistical approach applicable when a calibration curve is available; often used in a regulated environment. |
| Empirical Protocol (Based on CLSI Guideline EP17) | A rigorous statistical method involving the analysis of blank and low-concentration samples [27]. | LoB = meanblank + 1.645(SDblank)LOD = LoB + 1.645(SDlow concentration sample)LOQ ≥ LOD, meeting predefined bias/imprecision goals [27]. | Provides a high level of confidence; used to fully characterize assay performance at low concentrations, particularly in clinical laboratories. |
The following workflow outlines the typical process for determining LOD and LOQ using the signal-to-noise and statistical calculation methods:
Protocols for Evaluating Robustness and Ruggedness
The evaluation of robustness involves deliberately introducing small, plausible variations into method parameters and monitoring their effect on key method responses [25]. A typical protocol involves the following steps:
Factor Identification: Select factors from the method's operating procedure that are likely to vary. For an LC method, this could include:
Experimental Design: Use a structured experimental design, such as a Plackett-Burman or fractional factorial design, to efficiently screen a large number of factors with a minimal number of experimental runs [25].
Execution and Analysis: Perform the experiments in a randomized order and analyze the results. Calculate the effect of each factor variation on the responses, which can include quantitative results (e.g., assay value, impurity content) or system suitability parameters (e.g., resolution, tailing factor) [25].
The results of a robustness test are used to define which parameters need strict control and to set evidence-based limits for System Suitability Tests (SSTs) to ensure the method's validity whenever it is used [25].
Ruggedness, when distinguished from robustness, is assessed through intermediate precision or reproducibility studies. This involves testing the same set of samples under different conditions, such as with different analysts, on different instruments, in different laboratories, or on different days [23]. The results are compared using statistical measures like the Relative Standard Deviation (%RSD) or a Student's t-test to determine if there is a significant difference between the results obtained under the varied conditions.
Comparative Analysis and Data Presentation
Comparison of LOD and LOQ Determination Methods
Table 2: Comparison of LOD and LOQ Methodologies
| Aspect | Signal-to-Noise Ratio | Statistical (SD/Slope) | Empirical (EP17) |
|---|---|---|---|
| Complexity | Low | Medium | High |
| Regulatory Acceptance | Widely accepted, especially in chromatography [23] [22] | Accepted by ICH and other guidelines [23] | High, based on CLSI standard [27] |
| Key Advantage | Simple and quick to perform | Based on calibration data, less arbitrary | Most rigorous; provides high statistical confidence |
| Key Limitation | Requires a clear, measurable baseline; can be subjective | Relies on the quality of the calibration curve | Resource-intensive (requires ~60 replicates for establishment) [27] |
| Ideal Use Case | Routine, in-lab verification of method sensitivity | Full method validation for regulatory submission | Critical applications where the lowest reliable limits must be definitively known |
Key Factors for Robustness Testing in Chromatography
The parameters tested for robustness are highly method-dependent. The following table lists common factors for Liquid Chromatography-Mass Spectrometry (LC-MS) methods, which are particularly sensitive to variations.
Table 3: Key Factors for Robustness Evaluation in LC-MS Methods
| Parameter Category | Specific Factor | Likelihood of Uncontrollable Change | Recommended Variation | Potential Impact |
|---|---|---|---|---|
| Liquid Chromatography | Mobile phase pH | Medium | ± 0.5 units | Strong effect on retention if analyte pKa is near mobile phase pH [28] |
| Organic solvent content | Low to Medium | ± 2% (relative) | Influences retention time and analyte signal in MS [28] | |
| Column temperature | Low | ± 5 °C | Influences retention time and resolution [28] | |
| Flow rate | Low | ± 20% | Influences retention time and resolution [28] | |
| Column batch/age | Medium | Different batches | Can affect retention time, peak shape, and ionization [28] | |
| Sample Preparation | Injection solvent composition | Low/High | ± 10% (relative) | Can seriously affect retention and peak shape, especially in UHPLC [28] |
| Matrix effect (sample source) | High | 6 different sources | Influences recovery and ionization suppression; critical for LoQ/LoD [28] | |
| Mass Spectrometry | Drying gas temperature | Low | ± 10 °C | Can influence analyte ionization efficiency [28] |
| Nebulizer gas pressure | Low | ± 5 psi | Can influence analyte ionization efficiency [28] |
The relationship between the core validation parameters and the experimental workflow for robustness testing is summarized below:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are critical for successfully validating analytical methods, particularly in pharmaceutical quantification.
Table 4: Essential Research Reagents and Materials for Method Validation
| Item | Function / Role in Validation |
|---|---|
| High-Purity Reference Standards | Certified reference materials are essential for accurate preparation of calibration standards and spiked samples to determine accuracy, LOD, LOQ, and linearity [23]. |
| LC-MS Grade Solvents and Additives | High-purity solvents minimize background noise and ion suppression in MS, directly impacting the accuracy of S/N measurements for LOD/LOQ and the reliability of robustness tests [28]. |
| Characterized Chromatographic Columns | Multiple columns from different batches are used during robustness testing to evaluate the method's sensitivity to this critical component [28] [25]. |
| Buffer Solutions with Calibrated pH Meters | Essential for precise mobile phase preparation. Small variations in pH are a key factor in robustness studies, especially for ionizable analytes [28]. |
| Simulated or Real Matrix Blanks | Required for determining the Limit of Blank (LoB), which is the first step in the empirical LOD protocol, and for assessing specificity and matrix effects [27]. |
| (Z)-pent-3-en-2-ol | (Z)-pent-3-en-2-ol|For Research |
| 3-O-Methyl 17beta-Estradiol | 3-O-Methyl 17beta-Estradiol|RUO |
A thorough understanding and rigorous application of LOD, LOQ, robustness, and ruggedness parameters form the bedrock of a reliable analytical method. While LOD and LOQ define the fundamental boundaries of a method's sensitivity, robustness and ruggedness quantify its reliability and transferability under realistic conditions. The experimental data and protocols presented here provide a framework for pharmaceutical scientists to design validation studies that not only comply with regulatory guidelines but also ensure that their analytical methods will perform consistently in quality control laboratories, during technology transfers, and throughout the drug development lifecycle. Employing a structured approach to these advanced parameters ultimately de-risks the analytical process and bolsters confidence in the data generated for critical pharmaceutical products.
The Impact of Inadequate Validation on Product Safety and Regulatory Submissions
In the rigorous world of pharmaceutical development, the validation of analytical methods is not merely a regulatory formality but a critical cornerstone for ensuring product safety and efficacy. Inadequate validation can compromise the entire drug development lifecycle, leading to the release of substandard products and causing significant regulatory setbacks. Analytical method validation provides the essential data that regulatory agencies rely on to assess the quality, safety, and efficacy of pharmaceutical products. When these methods are not properly developed and validated, the consequences extend far beyond the laboratory, directly impacting patient health and a company's ability to bring vital medicines to market. This article explores the tangible impacts of validation failures, supported by recent research and case studies, and provides a structured overview of the protocols necessary to maintain the highest standards in pharmaceutical analysis.
The Critical Role of Validation in Pharmaceutical Analysis
Defining Analytical Method Validation
Analytical method validation is the formal, systematic process of proving that an analytical procedure is suitable for its intended purpose [29]. It involves a series of laboratory studies to demonstrate that the method consistently produces accurate, reliable, and reproducible data when used to test a pharmaceutical material. Key parameters established during validation include accuracy, precision, specificity, and robustness [29]. These parameters are globally harmonized under guidelines such as ICH Q2(R1) and are non-negotiable for regulatory submissions to bodies like the FDA and EMA [29].
Linking Validation to Product Safety and Regulatory Success
A properly validated method acts as a primary control, ensuring that every batch of a drug product contains the correct amount of the active ingredient, is free from harmful levels of impurities, and will maintain its quality and stability throughout its shelf life [29]. Without this assurance, patients may be exposed to significant risks. Concurrently, regulatory agencies mandate validated methods to ensure that the data submitted in support of product approvals—such as New Drug Applications (NDAs) or Investigational New Drug (IND) applications—is scientifically sound and reliable [29]. Inadequate validation is a common root cause of regulatory actions, including Complete Response Letters and clinical holds, which can derail development timelines and require costly remediation efforts [30].
Documented Impacts of Inadequate Validation
Compromised Product Safety and Quality
Recent studies on products from illegal and unregulated markets provide stark evidence of how a lack of controlled manufacturing and quality oversight leads to dangerous products reaching consumers.
Case Study: Illicit Pregabalin and Bodybuilding Supplements
- Pregabalin Content Variability: Analysis of 40 suspicious pregabalin samples from the Saudi Arabian market revealed significant variability in pregabalin content. Furthermore, about 30% of the samples contained toxic adulterants, posing a direct threat to consumer safety [31].
- Undeclared Active Ingredients: In a broader study of 601 samples seized from the illegal market, which were suspected to contain substances like selective estrogenic receptor modulators (SERMs) and aromatase inhibitors, 35% of the samples did not contain the declared active pharmaceutical ingredients (APIs). Even when the declared API was present, 6.4% of samples contained an additional, undeclared API, creating a high risk of unintended side effects and drug interactions [31].
- Contaminated Dietary Supplements: The application of a combined LC-MS Q-TOF/1H-NMR approach to dietary supplements purchased online found unauthorized botanical extracts containing L-dopa. These products were either overdosed or under-dosed, highlighting the critical absence of quality control in their production [31].
These findings from the field underscore a fundamental principle: the absence of a robust quality framework, which includes validated analytical methods, allows substandard and falsified products to proliferate, directly endangering public health.
Regulatory and Commercial Consequences
The regulatory pathway for a new drug is complex and demanding. Inadequate validation of the analytical methods used to generate critical data is a frequent contributor to submission failures.
Common Regulatory Deficiencies
Regulatory remediation specialists identify several common areas where inadequate validation leads to submission stalls [30]:
- Data Integrity Gaps: Discrepancies between datasets and summary documents, or concerns about electronic data compliance (e.g., 21 CFR Part 11), can undermine the credibility of an entire submission [30].
- Scientific and Clinical Data Gaps: This includes insufficient statistical analyses, inadequate safety signal characterization, and ambiguities in endpoint data, all of which can originate from analytical methods that are not fit-for-purpose [30].
- CMC and Manufacturing Issues: Incomplete process validation, inadequate stability data, and gaps in demonstrating control over the manufacturing process are red flags for regulators [30]. For instance, failing to establish scientifically justified residue limits in cleaning validation is a common cause of FDA 483 observations [32].
Overcoming these deficiencies requires comprehensive remediation, including root cause analysis, data reanalysis, and rigorous response document preparation—processes that demand significant time and resources and delay patient access to new therapies [30].
Essential Analytical Method Validation Protocols
To avoid the severe consequences of inadequate validation, the pharmaceutical industry adheres to strict, internationally recognized validation protocols. The following workflow and parameters, based primarily on ICH Q2(R1) guidelines, outline the standard approach.
Core Validation Parameters and Experimental Protocols
The table below details the core parameters, their definitions, and standard experimental methodologies as per ICH guidelines [29].
Table 1: Core Analytical Method Validation Parameters and Protocols
| Parameter | Definition | Experimental Protocol & Acceptance Criteria |
|---|---|---|
| Specificity/Selectivity | The ability to assess the analyte unequivocally in the presence of other components. | Protocol: Inject samples of placebo, analyte, and analyte spiked with potential interferents (impurities, degradants). Acceptance: Peak purity tools confirm analyte peak is pure; resolution from nearest interfering peak is typically > 2.0. |
| Accuracy | The closeness of agreement between the conventional true value and the value found. | Protocol: Spike a known amount of analyte into a placebo matrix at multiple levels (e.g., 50%, 100%, 150% of target). Analyze replicates. Acceptance: Mean recovery should be 98–102% for API assay. |
| Precision | The closeness of agreement between a series of measurements. | Protocol: - Repeatability: Analyze 6 samples at 100% concentration. - Intermediate Precision: Different analyst/day/equipment. Acceptance: RSD < 1.0% for API assay repeatability. |
| Linearity | The ability to obtain test results proportional to the analyte concentration. | Protocol: Prepare and analyze a minimum of 5 concentrations across a specified range (e.g., 50-150% of target). Plot response vs. concentration. Acceptance: Correlation coefficient (R²) ≥ 0.999. |
| Range | The interval between the upper and lower concentration of analyte for which suitability is demonstrated. | Protocol: Established from linearity and precision data. Must encompass the intended working concentrations. |
| Robustness | A measure of method capacity to remain unaffected by small, deliberate variations in method parameters. | Protocol: Small changes in HPLC conditions (e.g., flow rate ±0.1 mL/min, temperature ±2°C, mobile phase pH ±0.1). Acceptance: System suitability criteria are still met in all variations. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of validated methods relies on high-quality, consistent materials. The following table lists key reagents and their critical functions in analytical methods like HPLC.
Table 2: Key Research Reagent Solutions for Pharmaceutical Analysis
| Reagent/Material | Function in Analysis |
|---|---|
| Reference Standards | Highly purified, well-characterized substance used as a benchmark for quantifying the analyte and confirming method identity and specificity [29]. |
| Chromatography Columns | The heart of HPLC/UPLC separation; different chemistries (C18, C8, phenyl) are selected to achieve optimal resolution of the API from impurities and matrix components [29]. |
| HPLC-Grade Solvents | High-purity mobile phase components that minimize baseline noise, prevent system damage, and ensure reproducible retention times and detector response. |
| Biological Indicators (BIs) | Used in sterilization validation; contain a known population of highly resistant microbial spores (e.g., Geobacillus stearothermophilus) to challenge and verify the efficacy of sterilization cycles [33]. |
| Chemical Indicators | Used in sterilization validation; verify that physical parameters (e.g., temperature, radiation dose) were delivered to the product location [33]. |
| Anti-osteoporosis agent-2 | Anti-osteoporosis agent-2|Research Compound |
| Cerium(3+);acetate;hydrate | Cerium(3+);acetate;hydrate, MF:C2H5CeO3+2, MW:217.18 g/mol |
The evidence is clear: inadequate validation of analytical methods and related processes has a direct and profound impact on pharmaceutical product safety and regulatory success. From the very real dangers of adulterated and mislabeled products in illegal markets to the costly regulatory roadblocks faced by compliant companies, the stakes could not be higher. Adherence to established validation protocols, such as ICH Q2(R1), is not a bureaucratic hurdle but a fundamental prerequisite for ensuring that every drug product is safe, effective, and of high quality. As the industry evolves with the adoption of Quality by Design (QbD) principles [34] and more advanced analytical technologies, the foundational requirement for rigorous, well-documented validation remains constant. For researchers, scientists, and drug development professionals, a steadfast commitment to validation excellence is synonymous with a commitment to patient safety and therapeutic innovation.
From Theory to Practice: Method Development and Application Across Analytical Techniques
The landscape of pharmaceutical analytical method development has undergone a profound transformation, evolving from traditional empirical approaches to systematic, science-driven methodologies. This evolution is largely guided by the Quality by Design (QbD) framework, a proactive system rooted in ICH Q8-Q11 guidelines that emphasizes building quality into products and processes through predefined objectives rather than relying solely on end-product testing [35]. Systematic method development represents a structured approach that begins with predefined objectives and emphasizes product and process understanding based on sound science and quality risk management [5] [35]. For researchers, scientists, and drug development professionals, adopting this systematic workflow is crucial for developing robust, reliable analytical methods that not only meet stringent regulatory standards but also enhance operational efficiency and reduce the risk of late-stage failures.
The core distinction between traditional and modern approaches lies in their fundamental philosophy. Traditional pharmaceutical quality control historically relied on reactive endpoint testing and empirical "trial-and-error" development, which often led to batch failures, recalls, and regulatory non-compliance due to insufficient understanding of critical quality attributes and process parameters [35]. In contrast, systematic method development under the QbD framework employs proactive risk management and structured experimentation to establish method robustness, design space, and control strategies, thereby ensuring consistent method performance throughout its lifecycle [5] [35].
Foundational Principles of Systematic Method Development
Core QbD Principles for Analytical Methods
Systematic method development under the QbD framework is governed by several interconnected principles that collectively ensure method robustness and reliability. The foundation begins with establishing the Quality Target Product Profile (QTPP), which defines the method's intended purpose and performance requirements [35]. This is followed by identifying Critical Quality Attributes (CQAs) that link product quality attributes to safety and efficacy using risk assessment and prior knowledge [35]. A systematic risk assessment then evaluates material attributes and process parameters impacting CQAs, leading to the identification of Critical Method Attributes (CMAs) and Critical Process Parameters (CPPs) [5] [35].
The principle of design space establishment is central to QbD—it defines the multidimensional combination of input variables (e.g., mobile phase composition, pH, temperature) that have been demonstrated to ensure method quality as defined by CQAs [35]. Operating within the design space provides regulatory flexibility, as changes within this established space do not require re-approval [35]. A control strategy implements monitoring and systems to ensure method robustness, while lifecycle management emphasizes continuous improvement through ongoing performance monitoring and method refinement [5].
Regulatory Framework and Guidelines
The systematic approach to method development aligns with global regulatory expectations outlined in various ICH guidelines. ICH Q8(R2) provides the foundation for Pharmaceutical Development and introduces the concepts of QTPP, CQAs, and design space [35]. ICH Q9 formalizes Quality Risk Management, providing systematic processes for assessment, control, communication, and review of risks [35]. ICH Q10 outlines the Pharmaceutical Quality System, while ICH Q11 covers Development and Manufacture of Drug Substances [35].
For analytical procedures specifically, ICH Q2(R1) and the forthcoming ICH Q2(R2) and Q14 set the benchmark for method validation, emphasizing precision, robustness, and data integrity [5]. These guidelines collectively provide a comprehensive framework for developing and validating analytical methods that meet global regulatory standards from agencies including the FDA and EMA [5] [35].
The Systematic Method Development Workflow: A Step-by-Step Guide
Step 1: Define Method Objectives and Quality Target Product Profile (QTPP)
The initial phase of systematic method development establishes a clear foundation by defining the method's purpose and performance expectations. This begins with establishing a prospectively defined summary of the analytical method's quality characteristics [35]. The QTPP document lists target attributes including the specific analyte, required sensitivity (detection and quantification limits), precision, accuracy, linearity range, robustness requirements, and intended application [35] [36]. For pharmaceutical quantification methods, the purpose typically involves measuring Active Pharmaceutical Ingredients (APIs), related substances, residual solvents, or other impurities to evaluate potency, bioavailability, and stability [36].
Defining the QTPP requires understanding the analytical method's role in the broader product development pipeline. This includes considering whether the method will be used for release testing, stability studies, in-process testing, or characterization [5]. Each application has distinct requirements that influence method development strategy. For instance, stability-indicating methods must adequately separate and quantify degradation products, while release methods focus on accuracy and precision for specific quality attributes [5] [36].
Step 2: Analyze Analyte and Review Existing Knowledge
Comprehensive analyte characterization and literature review form the scientific foundation for efficient method development. Analyte characterization involves collecting biological, chemical, and physical properties of the analyte, including pKa values, solubility profile across different pH ranges, stability under various conditions (light, heat, pH), spectral properties, and chromophore characteristics [36]. This information guides selection of appropriate analytical techniques and conditions.
A thorough literature review assesses previous methodologies, publications, and regulatory submissions for the same analyte or structurally similar compounds [36]. This step examines journals, books, pharmacopeial monographs, and internal company databases to identify established methods that can be adapted or optimized [36]. The review should also consider prior knowledge from related molecules or analytical platforms, which can inform risk assessment and experimental design [35]. If no suitable previous methods exist in the literature, the development proceeds without this foundation, requiring more extensive experimentation [36].
Step 3: Select and Design the Analytical Method
Based on the QTPP and knowledge gathered, an appropriate analytical technique is selected and initially designed. For pharmaceutical quantification, chromatographic techniques—particularly High Performance Liquid Chromatography (HPLC) and Ultra-High-Performance Liquid Chromatography (UHPLC)—are most commonly employed due to their versatility, sensitivity, and ability to separate complex mixtures [5] [36] [37]. The selection process considers the nature of the analyte (volatility, polarity, molecular weight), required sensitivity, sample matrix, and available instrumentation [36].
Method design involves making initial decisions on key parameters, including detection technique (UV, MS, CAD), column chemistry (C18, C8, HILIC, etc.), mobile phase composition (aqueous/organic ratio, buffer type and pH), and preliminary gradient or isocratic conditions [36] [37]. This stage may also incorporate hyphenated techniques such as LC-MS/MS for enhanced specificity and sensitivity, particularly for complex matrices or trace analysis [5]. The initial method design establishes the foundation for subsequent optimization through systematic experimentation.
Step 4: Risk Assessment and Experimental Planning (DoE)
A science-based risk assessment identifies variables with potential impact on method CQAs, followed by structured experimental planning. Risk assessment tools such as Failure Mode Effects Analysis (FMEA), Ishikawa diagrams, or risk estimation matrices systematically evaluate material attributes and process parameters to identify critical factors [35]. This prioritizes experimentation on high-risk variables rather than testing all possible factors [5].
Design of Experiments (DoE) employs statistical models to optimize method conditions through multivariate studies rather than one-factor-at-a-time (OFAT) approaches [5] [35]. DoE efficiently explores the interaction effects between multiple variables simultaneously, establishing mathematical relationships between Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs) [35]. Common DoE approaches for method development include full factorial, fractional factorial, central composite, and Box-Behnken designs, selected based on the number of factors and desired resolution [35]. The experimental design defines the framework for method optimization and design space establishment.
Step 5: Method Optimization and Design Space Establishment
Method optimization through structured experimentation transforms initial method conditions into a robust, well-characterized analytical procedure. The optimization process systematically changes parameters individually and in combination based on the experimental design, monitoring their effect on CQAs such as resolution, peak symmetry, tailing factor, runtime, and sensitivity [36]. Modern approaches leverage automation and robotics to execute multiple experimental conditions efficiently, eliminating human error and boosting experimentation throughput [5].
The culmination of optimization is the establishment of the method design space—the multidimensional combination of input variables (e.g., mobile phase pH, column temperature, gradient slope) proven to ensure quality as defined by CQAs [35]. The design space is derived from experimental data and mechanistic models, enabling flexible operation within regulatory-approved boundaries [35]. Proven Acceptable Ranges (PARs) are established for each critical parameter, defining the boundaries within which method performance remains acceptable without requiring revalidation [35]. This represents a significant regulatory advantage, as changes within the design space do not require regulatory re-approval [35].
Step 6: Method Validation and Control Strategy
Once optimized, the method undergoes formal validation to demonstrate its suitability for intended use, followed by implementation of a control strategy. Method validation systematically assesses validation parameters including accuracy, precision, specificity, detection limit, quantification limit, linearity, range, and robustness according to ICH Q2(R1) and forthcoming ICH Q2(R2) guidelines [5] [38]. Modern validation approaches adopt a lifecycle perspective, with validation unfolding in three phases: (1) method design and feasibility, (2) qualification under stress conditions, and (3) continuous performance monitoring [5].
The control strategy encompasses planned controls to ensure consistent method performance within the design space [35]. This includes procedural controls (e.g., SOPs for system suitability testing), real-time monitoring through Process Analytical Technology (PAT), and performance trending [5] [35]. A robust control strategy ensures the method remains in a state of control throughout its lifecycle, with continuous improvement mechanisms to refine methods based on accumulated data and experience [35].
The following workflow diagram illustrates the complete systematic method development process:
Systematic Method Development Workflow
Advanced Approaches: AI and Machine Learning in Method Development
Artificial Intelligence for Method Optimization
The integration of Artificial Intelligence (AI) and machine learning represents a transformative advancement in systematic method development. AI algorithms optimize method parameters and predict equipment maintenance needs, while pattern recognition technologies refine data interpretation [5]. These technologies enhance method reliability by modeling complex, non-linear relationships between multiple input parameters and output CQAs that may be difficult to identify through traditional experimentation.
Bayesian optimization has emerged as a powerful iterative method for molecular discovery and method optimization [39]. This approach uses probabilistic models to balance exploration of unknown parameter spaces with exploitation of known promising regions, accelerating the identification of optimal method conditions [39]. In pharmaceutical applications, multifidelity Bayesian optimization (MF-BO) combines information from experiments of differing costs and fidelities, enabling more efficient resource allocation during method development [39]. For instance, lower-fidelity screening experiments (e.g., rapid gradient scouting) can be strategically combined with higher-fidelity confirmatory experiments (e.g, robust separation optimization) to build accurate predictive models with reduced experimental burden [39].
Deep Learning for Pharmaceutical Predictions
Deep learning models demonstrate superior performance for predicting pharmaceutical properties and optimizing formulation parameters, offering significant advantages over traditional machine learning approaches [40]. These models automatically extract non-linear features from complex input data, enabling accurate predictions of critical quality attributes based on molecular descriptors and formulation parameters [40].
Advanced architectures address common pharmaceutical data challenges, including small and imbalanced datasets. Principal Component Analysis (PCA) reduces dimensionality to improve prediction performance and training efficiency, while Wasserstein Generative Adversarial Networks (WGAN) overcome data limitation through synthetic data generation [40]. For instance, deep learning models with PCA have successfully predicted disintegration time of oral fast disintegrating films (OFDF), while WGAN-enhanced models have accurately predicted cumulative dissolution profiles for sustained-release matrix tablets (SRMT) [40]. These capabilities enable more efficient method development by predicting optimal conditions before laboratory experimentation.
Comparative Analysis: Traditional vs. Systematic Approaches
The performance advantages of systematic method development over traditional approaches are evident across multiple dimensions, from development efficiency to regulatory outcomes. The table below summarizes key comparative aspects:
| Aspect | Traditional Approach | Systematic QbD Approach | Performance Advantage |
|---|---|---|---|
| Development Philosophy | Empirical, trial-and-error [35] | Science-based, risk-managed [35] | 40% reduction in batch failures [35] |
| Experimental Design | One-Factor-at-a-Time (OFAT) [35] | Design of Experiments (DoE) [5] [35] | Fewer experimental iterations, identification of interactions [5] |
| Parameter Understanding | Limited, based on fixed conditions [35] | Comprehensive, through design space [35] | Established Proven Acceptable Ranges (PARs) [35] |
| Regulatory Flexibility | Fixed validation parameters [5] | Flexible within design space [35] | Changes within design space don't require re-approval [35] |
| Lifecycle Management | Reactive, post-approval changes [5] | Proactive continuous verification [5] [41] | Real-time monitoring, adaptive control strategies [41] |
| Data Utilization | Limited, siloed data [5] | Integrated, AI-enhanced analytics [5] [40] | Predictive modeling, method transfer optimization [40] |
Performance Comparison: Traditional vs. Systematic Method Development
The systematic approach demonstrates measurable advantages in development efficiency, method robustness, and regulatory flexibility. Implementation of QbD principles has been shown to reduce batch failures by 40% while optimizing critical quality attributes such as dissolution profiles [35]. The structured experimentation through DoE reduces development time and resources by efficiently identifying optimal conditions and interaction effects [5]. Furthermore, the establishment of a design space provides ongoing operational flexibility, as method parameters can be adjusted within the proven acceptable ranges without requiring regulatory submission [35].
Implementation Tools and Research Reagent Solutions
The Scientist's Toolkit: Essential Research Reagents and Technologies
Successful implementation of systematic method development requires appropriate instrumentation, software, and reagent systems. The following table details key research reagent solutions and their functions in pharmaceutical analytical method development:
| Tool Category | Specific Examples | Function in Method Development |
|---|---|---|
| Separation Techniques | UHPLC, HPLC, LC-MS/MS [5] [37] | High-resolution separation, quantification of APIs and impurities |
| Detection Systems | HRMS, NMR, UV/Vis, CAD [5] [37] | Detection, identification, and characterization of analytes |
| Chemometric Software | DoE Software, AI/Machine Learning Platforms [5] [40] | Experimental design, data analysis, predictive modeling |
| Automation Systems | Robotic Liquid Handlers, Automated Sample Preparation [5] | High-throughput experimentation, reduced human error |
| Column Chemistry | C18, C8, HILIC, Polar Embedded Phases [36] [37] | Stationary phase selection based on analyte characteristics |
| Mobile Phase Components | Buffer Systems (phosphate, acetate), Organic Modifiers (ACN, MeOH) [36] | Optimization of separation selectivity and efficiency |
| Reference Standards | Impurity Reference Materials, API Standards [38] | Method qualification, system suitability, quantitative calibration |
| 3,5-Diethylbenzotrifluoride | 3,5-Diethylbenzotrifluoride | |
| 1-(2-Iodophenyl)ethan-1-ol | 1-(2-Iodophenyl)ethan-1-ol | Get 1-(2-Iodophenyl)ethan-1-ol (CAS 122752-70-9), a building block for synthetic chemistry research. This product is for research use only and not for human or veterinary use. |
Essential Research Reagent Solutions for Method Development
Method Validation and Technology Transfer Protocols
Once developed, analytical methods require rigorous validation and structured transfer protocols. Method validation establishes documented evidence that the method consistently meets predetermined specifications and quality attributes [38]. The validation protocol typically assesses accuracy (through spike recovery studies), precision (repeatability and intermediate precision), specificity (ability to measure analyte unequivocally in presence of potential interferents), linearity and range, quantitation limit and detection limit, and robustness (resistance to deliberate parameter variations) [5] [38].
Technology transfer follows successful validation, formalizing the process of transferring the analytical method from development laboratories to quality control or between different sites [5]. This structured process includes documentation review, comparative testing, and sometimes co-validation to ensure the receiving laboratory can execute the method successfully [5]. Effective technology transfer requires standardized protocols, comprehensive training programs, and harmonized governance models to maintain data integrity and method performance across different locations and operators [5].
The following diagram illustrates the experimental design and optimization process central to systematic method development:
DoE and Design Space Establishment Process
Systematic method development represents a fundamental shift in pharmaceutical analytics, moving from reactive quality testing to proactive, science-based quality by design. This structured approach—from objective definition through optimization to lifecycle management—delivers measurable advantages in method robustness, regulatory flexibility, and development efficiency. The integration of advanced technologies including AI, machine learning, and automation further enhances these benefits, enabling predictive modeling and accelerated optimization [5] [40].
Future directions point toward increased digitalization and continuous verification. Digital twins that simulate method performance in silico offer potential for reduced development costs and timelines through virtual experimentation [5]. Real-Time Release Testing (RTRT) approaches shift quality control to in-process monitoring via PAT, accelerating release while reducing costs [5]. Additionally, the growing emphasis on personalized medicines and on-demand manufacturing requires more flexible, rapid analytical methods capable of handling small batches with high reliability [5].
For researchers and drug development professionals, mastering systematic method development is no longer optional but essential for maintaining competitiveness and regulatory compliance. By adopting this structured, science-based approach and leveraging emerging technologies, pharmaceutical scientists can develop more robust, reliable analytical methods that accelerate drug development while ensuring product quality and patient safety.
Applying Quality by Design (QbD) Principles to Analytical Method Development
The pharmaceutical industry is undergoing a significant transformation in its approach to analytical method development, moving from traditional, empirical methods to a systematic, science-based framework known as Quality by Design (QbD). This paradigm shift, driven by regulatory bodies and the pursuit of robust, reliable analytical procedures, represents a proactive approach to ensuring product quality throughout the entire lifecycle [42]. Whereas traditional method development often relies on a trial-and-error approach with limited understanding of parameter interactions, QbD emphasizes prior knowledge, risk assessment, and controlled design to create methods that are inherently robust, reproducible, and fit-for-purpose [43].
The application of QbD to analytical development, termed Analytical Quality by Design (AQbD), revolutionizes how methods are conceived, developed, and validated. AQbD ensures that quality is built into the analytical method from the outset, rather than merely tested at the end of development [44]. This systematic approach begins with predefined objectives and focuses on a deep understanding of both the product and process, grounded in sound science and quality risk management [43]. For researchers and drug development professionals, adopting AQbD principles translates to fewer method failures, reduced operational costs, and greater regulatory flexibility, ultimately accelerating the development of safe and effective pharmaceutical products [5] [42].
Core Principles of QbD in Analytical Development
The AQbD framework is built upon a structured, sequential workflow that ensures every aspect of the analytical method is understood and controlled. The core principles, mirroring those of product QbD, provide a roadmap for developing robust analytical procedures.
Figure 1. The sequential workflow of Analytical Quality by Design (AQbD), from defining objectives to lifecycle management.
Analytical Target Profile (ATP) and Critical Quality Attributes (CQAs)
The foundation of any AQbD approach is the Analytical Target Profile (ATP), a predefined objective that outlines the method's purpose and required performance characteristics [42]. The ATP defines what the method needs to achieve, specifying the target analyte, the required measurement quality, and the appropriate reporting range [42]. Essentially, it answers the question: "What is the method intended to measure and to what level of quality?"
From the ATP, Critical Quality Attributes (CQAs) are identified. CQAs are the method parameters that must be controlled within predetermined limits to ensure the method meets the ATP [43]. For a chromatographic method, typical CQAs include retention time, theoretical plates, peak asymmetry (tailing factor), and resolution [43]. These attributes directly reflect the method's performance and its ability to deliver reliable, accurate data.
Risk Assessment and Management
Risk assessment is a cornerstone of AQbD, providing a systematic process for identifying and evaluating factors that could impact the method's CQAs [42]. The goal is to distinguish Critical Method Parameters (CMPs)—variables with a significant effect on CQAs—from non-critical factors.
Commonly used tools include:
- Ishikawa (Fishbone) Diagrams: A qualitative tool for brainstorming potential sources of variability, categorizing them into groups such as instrument, method, materials, and environment [42].
- Failure Mode and Effects Analysis (FMEA): A semiquantitative method that ranks risks based on their severity, occurrence, and detectability, helping to prioritize factors for experimental investigation [42].
This risk-based focus ensures that development efforts are concentrated on the areas that matter most, leading to a more efficient and effective development process.
Design of Experiments (DoE) and Design Space
Unlike the traditional one-factor-at-a-time (OFAT) approach, AQbD utilizes Design of Experiments (DoE) to systematically study the relationship between CMPs and CQAs [42]. DoE allows for the efficient exploration of multiple factors and their interactions simultaneously, leading to a deeper understanding of the method's behavior.
The results of DoE studies are used to establish the Design Space—a multidimensional combination and interaction of CMPs demonstrated to provide assurance of quality [42]. Also referred to as the Method Operable Design Region (MODR), operating within this space ensures the method will perform as intended, providing a higher degree of robustness compared to a single set of operating conditions [5] [42]. The design space is often visualized using response surface plots, which show the region where all CQA requirements are simultaneously met.
Control Strategy and Lifecycle Management
A control strategy is a planned set of controls, derived from the knowledge acquired during development, that ensures method performance remains within the Design Space [42]. This includes controls for sample preparation, instrument parameters, and system suitability tests.
Finally, AQbD embraces lifecycle management, recognizing that a method may need to be adapted or improved over its lifetime. The knowledge gained during development provides a scientific basis for managing these future changes in a compliant manner, facilitating continuous improvement [5] [43].
Comparative Analysis: Traditional vs. QbD Approach
The fundamental differences between traditional method development and the AQbD approach lead to distinct outcomes in robustness, regulatory flexibility, and long-term efficiency. The table below summarizes these key differences.
Table 1. A direct comparison of traditional and QbD-based analytical method development.
| Aspect | Traditional Approach | QbD-Based Approach (AQbD) |
|---|---|---|
| Philosophy | Unstructured, empirical, and reactive ("test-to-quality") | Systematic, scientific, and proactive ("build-in-quality") |
| Development Basis | Often relies on trial-and-error or one-factor-at-a-time (OFAT) experiments | Uses systematic risk assessment and Design of Experiments (DoE) |
| Knowledge Space | Limited understanding of parameter interactions and their effects | Deep, documented understanding of Critical Method Parameters (CMPs) and their impact on Critical Quality Attributes (CQAs) |
| Robustness | Evaluated at the end of development; operating conditions are fixed | Built-in from the start; a multidimensional Design Space (MODR) is established |
| Regulatory Stance | Fixed conditions offer little flexibility; changes require regulatory submissions | Regulatory flexibility within the approved Design Space; facilitates continuous improvement |
| Lifecycle Management | Reactive to failures; often requires redevelopment and revalidation | Proactive and knowledge-based; supports managed evolution over the method's lifecycle |
The advantages of AQbD are measurable. Studies and industrial applications have demonstrated that AQbD significantly minimizes out-of-trend (OOT) and out-of-specification (OOS) results by enhancing method robustness [42]. Furthermore, it reduces operational costs and deviations by preventing method failures [42]. The following case study provides quantitative evidence of these benefits.
Case Study: QbD-Based HPLC Method for Ceftriaxone Sodium
A practical application of AQbD was demonstrated in the development and validation of an HPLC method for ceftriaxone sodium [43]. This case illustrates the implementation of the AQbD workflow and its successful outcomes.
Experimental Protocol and Design
- ATP Definition: The method was designed to be stability-indicating, specific, precise, and accurate for the quantification of ceftriaxone sodium in pharmaceutical dosage forms [43].
- CQAs Identification: Critical Quality Attributes were defined as retention time, theoretical plates, and peak asymmetry [43].
- Risk Assessment: Initial risk analysis identified mobile phase composition and pH of the buffer as high-risk, critical method parameters significantly impacting the CQAs [43].
- DoE Implementation: A Central Composite Design (CCD) was employed to optimize the two CMPs. The factors and their levels were:
- Mobile Phase Ratio (Acetonitrile:Water): 60:40 to 80:20
- Buffer pH: 5.5 to 7.5 The experimental data was modeled using a second-order polynomial equation to understand the quadratic and interaction effects [43].
Results and Validation Data
The application of the QbD approach resulted in an optimized and robust method with the following conditions: Phenomenex C-18 column (250 mm × 4.6 mm, 5.0 μm), mobile phase acetonitrile to water (70:30, v/v) with pH adjusted to 6.5 using 0.01% triethylamine, flow rate of 1 ml/min, and detection at 270 nm [43].
The method was successfully validated, with key performance data summarized in the table below.
Table 2. Summary of validation results for the QbD-based HPLC method for Ceftriaxone Sodium [43].
| Validation Parameter | Result | ICH Compliance |
|---|---|---|
| Linearity (Range: 10-200 μg/mL) | R² = 0.991 | Meets guidelines |
| Precision (% RSD) | ||
| Â Â - Intra-day | 0.70 - 0.94% | Meets guidelines (RSD < 2%) |
| Â Â - Inter-day | 0.55 - 0.95% | Meets guidelines (RSD < 2%) |
| Accuracy (% Assay) | 99.73 ± 0.61% | Meets guidelines |
| Robustness (Deliberate variations) | % RSD < 2% for all parameters | High resilience to parameter changes |
| System Suitability | ||
| Â Â - Tailing Factor | 1.49 | Meets typical criteria (< 2.0) |
| Â Â - Theoretical Plates | 5236 | Meets typical criteria (> 2000) |
The high number of theoretical plates and the low tailing factor confirm the excellent efficiency and symmetry of the chromatographic peak. The low % RSD values for precision and robustness are direct evidence of the method's reliability, a key benefit of the QbD methodology.
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of AQbD relies on a foundation of high-quality materials and well-characterized instruments. The following table details key research reagent solutions and their functions in a typical AQbD-driven analytical development laboratory.
Table 3. Essential materials and reagents for QbD-based chromatographic method development.
| Item | Function in Analytical Development |
|---|---|
| High-Performance Liquid Chromatograph (HPLC/UHPLC) | Core instrument for separation and quantification; equipped with UV/VIS or PDA detectors for method development and peak purity assessment [43]. |
| Chromatography Data System (CDS) Software | For data acquisition, processing, and management; ensures ALCOA+ (Attributable, Legible, Contemporaneous, Original, Accurate) principles for data integrity [5]. |
| C18 Reverse-Phase Chromatography Column | The most common stationary phase for separating pharmaceutical compounds; column dimensions and particle size (e.g., 5 μm) are critical method parameters [43]. |
| HPLC-Grade Solvents (Acetonitrile, Methanol) | Used as components of the mobile phase; high purity is essential to minimize baseline noise and ghost peaks [43]. |
| Buffer Salts (e.g., KHâ‚‚POâ‚„, NaHâ‚‚POâ‚„) and pH Modifiers (e.g., Triethylamine) | Used to prepare mobile phase buffers for controlling pH, which is often a Critical Method Parameter (CMP) affecting retention and selectivity [43]. |
| Design of Experiments (DoE) Software | Software such as Design-Expert or equivalent is crucial for designing experiments, modeling data, and defining the Method Operable Design Region (MODR) [45] [43]. |
| 1,6-Dodecanediol | 1,6-Dodecanediol (C12H26O2) |
| Onilcamotide | Onilcamotide, CAS:1164096-85-8, MF:C96H177N39O24S, MW:2293.7 g/mol |
The adoption of Quality by Design principles for analytical method development marks a significant evolution in pharmaceutical science. By shifting from a reactive, compliance-focused mindset to a proactive, knowledge-driven framework, AQbD delivers superior method robustness, reduced lifecycle costs, and enhanced regulatory flexibility [5] [42]. The case study on ceftriaxone sodium, supported by quantitative validation data, provides clear evidence that a systematic approach involving ATP, risk assessment, and DoE results in a highly reliable and fit-for-purpose analytical procedure [43].
As the industry advances with trends like real-time release testing (RTRT), continuous manufacturing, and the analysis of complex biologics, the foundational understanding and control provided by AQbD become not just beneficial, but essential [5]. For researchers and drug development professionals, mastering and implementing AQbD is a critical step toward ensuring the consistent quality, safety, and efficacy of pharmaceutical products in a modern, dynamic development landscape.
The validation of analytical methods is a cornerstone of pharmaceutical research and development, ensuring the reliability, accuracy, and reproducibility of data used in drug quantification. Selecting the appropriate analytical technique is paramount, as the choice directly impacts the ability to meet specific validation criteria such as sensitivity, selectivity, and precision. This guide provides an objective comparison of four widely used techniques—High-Performance Liquid Chromatography (HPLC), Gas Chromatography (GC), Ultraviolet-Visible Spectrophotometry (UV-Vis), and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)—within the context of method validation for pharmaceutical quantification. The performance of each technique is evaluated based on experimental data from contemporary research, and detailed methodologies are provided to support robust analytical practices.
Comparative Performance of Analytical Techniques
The following table summarizes the key validation parameters for HPLC, GC, UV-Vis, and LC-MS/MS based on experimental data from recent studies.
Table 1: Comparative Technique Performance for Pharmaceutical Quantification
| Technique | Typical Linear Range | Reported Sensitivity (LLOQ) | Reported Accuracy (%) | Reported Precision (% RSD) | Key Applications & Notes |
|---|---|---|---|---|---|
| HPLC-UV | 0.075–15 µg/mL [46] | 0.075 µg/mL [46] | 94.13–101.12 [46] | ≤ 9.46 [46] | Determination of chlorambucil in plasma; well-established for APIs with chromophores. |
| HPLC-UV/VIS | 0.05–300 µg/mL [47] | 0.05 µg/mL [47] | 96.37–110.96 [47] | Information Missing | Levofloxacin in drug-delivery systems; can overestimate by 15-20% vs. LC-MS/MS [48]. |
| LC-MS/MS | Information Missing | Information Missing | Information Missing | Information Missing | Superior specificity and sensitivity; used as a reference method for polyphenol analysis [48]. |
| GC-MS | Information Missing | 0.075 µg/mL [46] | 94.96–109.12 [46] | ≤ 6.69 [46] | Determination of valproic acid in plasma; suitable for volatile, thermally stable compounds. |
| UV-Vis | 0.05–300 µg/mL [47] | 0.05 µg/mL [47] | 96.00–99.50 [47] | Information Missing | Levofloxacin measurement; less accurate with complex matrices like composite scaffolds [47]. |
Detailed Experimental Protocols
Protocol 1: HPLC-UV for the Determination of Chlorambucil in Plasma
This method, developed for quantifying the anticancer drug chlorambucil (CLB) in plasma, demonstrates a validated protocol for bioanalysis [46].
- Sample Preparation: A simple protein precipitation and filtration method is used. A 250 µL plasma aliquot is mixed with methanol for protein precipitation. The mixture is then centrifuged, and the supernatant is filtered before injection into the HPLC system [46].
- Chromatographic Conditions:
- Column: LiChrospher 100 RP-18 end-capped column [46].
- Mobile Phase: A mixture of acetonitrile, water, and formic acid [46].
- Flow Rate: Not specified in the provided context [46].
- Detection: UV detection at 258 nm [46].
- Injection Volume: Not specified [46].
- Internal Standard: Mefenamic acid is used to improve quantification accuracy [46].
- Validation Data: The method was linear from 0.075 to 15 µg/mL (r² = 0.9996). The lower limit of quantification (LLOQ) was 0.075 µg/mL. Accuracy ranged from 94.13% to 101.12%, and intra- and inter-batch precision was ≤9.46% RSD [46].
Protocol 2: Comparison of HPLC-UV and UV-Vis for Levofloxacin Release Studies
This study directly compares HPLC and UV-Vis for monitoring levofloxacin released from a mesoporous silica/nano-hydroxyapatite composite scaffold, a complex drug-delivery system [47].
- Sample Preparation: Levofloxacin is released into simulated body fluid (SBF). Samples are taken at intervals and analyzed directly or with minimal preparation (e.g., dilution) by both techniques [47].
- HPLC Conditions:
- Column: Sepax BR-C18 column (250 × 4.6 mm, 5 µm) [47].
- Mobile Phase: A mixture of 0.01 mol/L KHâ‚‚POâ‚„, methanol, and 0.5 mol/L tetrabutylammonium hydrogen sulphate (75:25:4) [47].
- Flow Rate: 1 mL/min [47].
- Detection: UV detection at 290 nm [47].
- Injection Volume: 10-20 µL [47].
- Internal Standard: Ciprofloxacin [47].
- UV-Vis Conditions:
- Wavelength: Maximum absorption wavelength determined by scanning standard solutions between 200–400 nm [47].
- Validation Data: Both techniques showed a wide linear range (0.05–300 µg/mL). However, the recovery rates for low, medium, and high concentrations were more accurate and consistent with UV-Vis (96.00–99.50%) compared to HPLC (96.37–110.96%) in this specific complex matrix. The study concluded that UV-Vis was less accurate for this application due to potential interference from the scaffold components, and HPLC was the preferred method [47].
Protocol 3: GC-MS for the Determination of Valproic Acid in Plasma
This protocol outlines a sensitive GC-MS method for valproic acid (VPA), which lacks a strong chromophore for UV detection [46].
- Sample Preparation: The method involves a simple pre-column derivatization. A 250 µL plasma aliquot is esterified with methanol and then extracted with hexane [46].
- Chromatographic Conditions:
- Validation Data: The method was linear with an LLOQ of 0.075 µg/mL. Accuracy ranged from 94.96% to 109.12%, and intra- and inter-batch precision was ≤6.69% RSD [46].
Analytical Technique Selection Workflow
The following diagram illustrates the decision-making process for selecting an appropriate analytical technique based on the properties of the analyte and the requirements of the analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method validation relies on the use of high-quality reagents and materials. The following table lists key items and their functions in analytical methods for pharmaceutical quantification.
Table 2: Essential Materials and Reagents for Analytical Method Development
| Item | Function/Description | Example from Research |
|---|---|---|
| C18 Reverse-Phase Column | A common stationary phase for separating non-polar to moderately polar compounds based on hydrophobic interactions. | Sepax BR-C18 [47], LiChrospher 100 RP-18 [46]. |
| Methanol & Acetonitrile (HPLC Grade) | High-purity organic solvents used as the mobile phase components in reversed-phase HPLC to elute analytes from the column. | Used in mobile phases for levofloxacin [47] and chlorambucil [46] assays. |
| Buffers & Mobile Phase Additives | Salts (e.g., KHâ‚‚POâ‚„) and ion-pairing agents (e.g., tetrabutylammonium salts) modify the mobile phase to control selectivity, improve peak shape, and manage analyte ionization. | 0.01 mol/L KHâ‚‚POâ‚„ and tetrabutylammonium hydrogen sulphate [47]; formic acid [46]. |
| Internal Standards | A compound with similar properties to the analyte, added to samples to correct for variability during sample preparation and analysis. | Ciprofloxacin for levofloxacin HPLC [47]; mefenamic acid for chlorambucil HPLC [46]. |
| Derivatization Reagents | Chemicals that react with analytes to convert them into forms suitable for detection (e.g., adding a chromophore) or analysis by a specific technique like GC. | Methanol for esterification of valproic acid in GC-MS [46]. |
| Solid-Phase Extraction (SPE) Cartridges | Used for complex sample clean-up and pre-concentration of analytes from biological matrices like plasma to reduce matrix effects. | Mentioned as a key sample preparation technique in training courses [49]. |
| Fungicide5 | Fungicide5|Agricultural Research Agent|RUO | Fungicide5 is a broad-spectrum research fungicide. This product is for Research Use Only and is not intended for personal or therapeutic use. |
| Bipolamine G | Bipolamine G, MF:C21H28N2O4, MW:372.5 g/mol | Chemical Reagent |
Method Validation Workflow
The process of validating an analytical method involves a series of structured steps to ensure the method is fit for its intended purpose. The workflow below outlines the key stages.
The Quality by Design (QbD) framework represents a systematic, risk-based approach to analytical method development that emphasizes scientific understanding and proactive control over method performance. In pharmaceutical analysis, QbD moves beyond traditional univariate method development by establishing an Analytical Target Profile (ATP) that defines the method's purpose and required quality standards from the outset [50]. This paradigm shift ensures that methods are robust, reproducible, and fit-for-purpose throughout their lifecycle, particularly for challenging applications such as the analysis of synthetic antidepressant mixtures where multiple active components and potential impurities must be resolved and quantified. The International Council for Harmonisation (ICH) guidelines Q2(R2) and Q14 provide the regulatory foundation for implementing QbD principles in analytical method development, requiring demonstrated understanding of Critical Method Parameters (CMPs) and their impact on Critical Analytical Attributes (CAAs) [29] [51].
Applying QbD to Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) method development for synthetic antidepressant mixtures offers significant advantages. These complex formulations often contain multiple structurally similar compounds, degradation products, and related substances that must be separated and quantified with high specificity and sensitivity. The QbD approach employs statistical experimental design to methodically optimize chromatographic conditions, resulting in methods with well-characterized design spaces that remain reliable even with minor variations in operational parameters [50] [51]. This case study examines the application of QbD principles to develop and validate an RP-HPLC method for a synthetic antidepressant mixture, providing a structured framework that can be adapted for similar pharmaceutical compounds.
QbD Methodology for RP-HPLC Development
Defining the Analytical Target Profile (ATP) and Critical Analytical Attributes (CAAs)
The initial phase of QbD-based method development requires clear definition of the Analytical Target Profile (ATP), which serves as the foundation for all subsequent development activities. For the analysis of a synthetic antidepressant mixture, the ATP specifies that the method must simultaneously quantify the active pharmaceutical ingredients (APIs) while separating and detecting known impurities and degradation products in both bulk drug substances and formulated products [50] [29]. The ATP for our antidepressant mixture case study includes the following key requirements: accurate quantification of the main antidepressant compounds (e.g., venlafaxine) and their related substances, detection of genotoxic impurities at ppm levels, and demonstration of method stability-indicating capabilities through forced degradation studies [52].
From the ATP, Critical Analytical Attributes (CAAs) are identified as method performance characteristics that must be maintained within predefined limits to ensure the method fulfills its intended purpose. For RP-HPLC analysis of antidepressant mixtures, the essential CAAs include:
- Resolution (Rs) between critical peak pairs, particularly between the main APIs and their impurities
- Tailing factor (T) to ensure symmetric peak shapes for accurate integration
- Theoretical plate count (N) as a measure of column efficiency
- Runtime to balance analysis time with sufficient separation
- Limit of detection (LOD) and quantification (LOQ) for impurity determination [50] [52]
These CAAs establish the benchmark against which method performance is evaluated throughout the development process and form the basis for defining the method's operational design space.
Risk Assessment and Initial Method Scouting
A thorough risk assessment identifies Critical Method Parameters (CMPs) that potentially influence the CAAs. For RP-HPLC method development, these typically include mobile phase composition, pH, buffer concentration, column temperature, gradient profile, and detection wavelength [50] [51]. Structured risk assessment tools such as Fishbone diagrams and Failure Mode Effects Analysis (FMEA) systematically evaluate and prioritize these parameters based on their potential impact on method performance.
Initial method scouting explores different column chemistries (C8, C18, phenyl, etc.), mobile phase systems (methanol-water, acetonitrile-water, with various buffers), and gradient profiles to identify promising starting conditions for optimization. Research on venlafaxine analysis demonstrates that C18 columns with alkaline mobile phases (pH ~8.5) provide optimal separation for certain antidepressant compounds and their impurities [52]. Similarly, QbD development of methods for bupivacaine hydrochloride employed a Shimadzu C-18 column (250mm × 4.6mm i.d., 5μm particle size) with a mobile phase comprising acetonitrile and 0.1% ortho phosphoric acid (OPA) in approximately 70:30 ratio [50]. These initial screening experiments provide the foundational knowledge for subsequent systematic optimization using statistical design of experiments (DoE).
Systematic Optimization Using Experimental Design
The core of QbD method development employs statistical experimental designs to efficiently characterize the relationship between CMPs and CAAs, thereby establishing the method design space. For RP-HPLC methods, this typically involves sequential application of screening designs followed by response surface methodologies:
Screening Designs: Preliminary studies often utilize Plackett-Burman designs or fractional factorial designs to identify the most influential method parameters from a larger set of potential variables [50]. These efficient screening designs help focus optimization efforts on the few critical factors that significantly impact method performance.
Response Surface Methodology: After identifying critical factors, Box-Behnken designs or Central Composite designs systematically characterize the nonlinear relationships between factors and responses, enabling the identification of optimal conditions and establishment of robust method operational ranges [50] [51]. For example, a QbD-based method for bupivacaine hydrochloride employed a Box-Behnken design to optimize mobile phase composition, flow rate, and injection volume, resulting in a robust method with a well-defined design space [50].
Table 1: Experimental Factors and Levels for Box-Behnken Optimization Design
| Factor | Low Level | Middle Level | High Level |
|---|---|---|---|
| Acetonitrile Concentration (%) | 65 | 70 | 75 |
| Flow Rate (mL/min) | 0.7 | 0.8 | 0.9 |
| pH of Aqueous Phase | 2.0 | 2.5 | 3.0 |
| Column Temperature (°C) | 35 | 40 | 45 |
The experimental data from these designs are analyzed using statistical software to generate mathematical models and response surface plots that visualize the relationship between factors and responses. The resulting method design space defines the multidimensional combination of input variable ranges where satisfactory method performance is assured, providing operational flexibility while maintaining quality standards.
Experimental Protocol: QbD-Based RP-HPLC Method Development
Materials and Instrumentation
The experimental workflow begins with careful selection of materials and instrumentation. High-purity reference standards of the antidepressant compounds and known impurities should be obtained from certified suppliers. For the analysis of venlafaxine and its genotoxic impurity 4-methoxybenzyl chloride (4-MBC), research utilized materials from TCI Chemicals (India) Pvt. Ltd. with HPLC-grade solvents from Merck [52]. Chromatographic separation typically employs an RP-HPLC system with UV/PDA detection, such as the Waters HPLC system with Empower 3 software used in venlafaxine analysis [52]. The selection of column chemistry is critical, with studies showing that Purospher STAR end-capped C18 columns (250mm × 4.0mm, 5μm) provide excellent separation for polar antidepressant compounds and their impurities [52].
Chromatographic Conditions Optimization
Based on QbD optimization studies, the following chromatographic conditions have been established for synthetic antidepressant mixture analysis:
- Column: C18 column (250mm × 4.6mm, 5μm particle size)
- Mobile Phase: Gradient mixture of 0.1% ammonia buffer (pH 8.5, adjusted with orthophosphoric acid) and acetonitrile [52]
- Flow Rate: 1.0 mL/min (optimized through DoE)
- Column Temperature: 55°C (optimized for efficiency and resolution)
- Injection Volume: 50 μL
- Detection Wavelength: 225 nm (based on UV maxima of analytes)
- Run Time: 60 minutes (comprehensive separation of APIs and impurities)
The gradient program typically starts with 5% organic phase, gradually increasing to 60% over 45 minutes, then returning to initial conditions for column re-equilibration [52]. For less complex mixtures, isocratic methods may be suitable, such as the method developed for bupivacaine hydrochloride using acetonitrile and 0.1% ortho phosphoric acid (69.45:30.55% v/v) [50].
Sample Preparation Protocol
Accurate sample preparation is essential for reliable method performance. For bulk drug substance analysis, prepare stock solutions of the antidepressant compounds and impurities at approximately 1000 μg/mL in appropriate solvent systems (typically water-acetonitrile mixtures). For formulated products, extract the active ingredients from the dosage form matrix using suitable solvents with sonication assistance. Filter samples through 0.45μm or 0.2μm membrane filters before injection. The venlafaxine study utilized a diluent comprising purified water and acetonitrile (50:50 ratio) for standard and sample preparation [52].
Forced Degradation Studies
Forced degradation studies demonstrate the stability-indicating capability of the method by subjecting the antidepressant mixture to various stress conditions:
- Acidic Hydrolysis: Expose samples to 0.1N HCl at 70°C for 1-2 hours
- Alkaline Hydrolysis: Treat with 0.1N NaOH at 70°C for 1-2 hours
- Oxidative Degradation: Incubate with 3% Hâ‚‚Oâ‚‚ at room temperature for 1-2 hours
- Thermal Degradation: Heat solid samples at 105°C for 24 hours
- Photolytic Degradation: Expose to UV light (approximately 200 watt-hours/m²) and visible light (1.2 million lux-hours)
After stress treatment, analyze samples using the developed method to assess separation of degradation products from main peaks and evaluate method specificity. Studies on nintedanib esylate demonstrated the drug's susceptibility to acidic, oxidative, and photolytic conditions while showing stability under thermal and alkaline conditions [51].
Method Validation and Performance Data
Validation Parameters and Acceptance Criteria
Following method development and optimization, comprehensive validation establishes the method's reliability for its intended purpose according to ICH Q2(R2) guidelines [29] [53]. The validation parameters and typical acceptance criteria for RP-HPLC methods of antidepressant mixtures are summarized in Table 2.
Table 2: Method Validation Parameters and Acceptance Criteria for Antidepressant Mixture Analysis
| Validation Parameter | Experimental Approach | Acceptance Criteria | Reported Data for Antidepressant Methods |
|---|---|---|---|
| Specificity | Resolution from impurities and degradation products | Baseline separation (Rs > 2.0) from all potential impurities | Venlafaxine and 4-MBC showed baseline separation with Rs > 2.0 [52] |
| Linearity | Minimum 5 concentration levels across specified range | Correlation coefficient (R²) ≥ 0.999 | R² = 0.999 for bupivacaine (25-80 μg/ml) [50]; R² = 0.999 for venlafaxine impurity [52] |
| Accuracy | Recovery studies at 3 levels (50%, 100%, 150%) | Recovery 98-102% for API, 90-110% for impurities | Bupivacaine recovery 98-100% [50]; Venlafaxine impurity recovery within range [52] |
| Precision (Repeatability) | Six replicate injections of standard preparation | %RSD ≤ 1.0% | %RSD 0.38 for bupivacaine intraday precision [50]; %RSD 0.43 for venlafaxine impurity [52] |
| Intermediate Precision | Different analysts, instruments, days | %RSD ≤ 2.0% | %RSD 0.44 for bupivacaine interday precision [50]; %RSD 0.93 for venlafaxine impurity [52] |
| LOD | Signal-to-noise ratio (3:1) | Based on analyte sensitivity | 0.900 μg/ml for bupivacaine [50]; 0.016 ppm for venlafaxine impurity [52] |
| LOQ | Signal-to-noise ratio (10:1) | Based on analyte sensitivity with precision | 2.72 μg/ml for bupivacaine [50]; 0.052 ppm for venlafaxine impurity [52] |
| Robustness | Deliberate variations in method parameters | System suitability criteria maintained | Venlafaxine method robust with %RSD, theoretical plates, tailing within limits [52] |
Comparison of QbD versus Traditional Approach
The advantages of QbD-based method development become apparent when comparing method performance characteristics with traditionally developed methods. As shown in Table 3, QbD-developed methods typically demonstrate superior robustness, better characterization of method limitations, and more efficient troubleshooting capabilities.
Table 3: Performance Comparison of QbD versus Traditional Method Development Approaches
| Characteristic | QbD-Based Approach | Traditional Approach |
|---|---|---|
| Development Strategy | Systematic, multivariate, statistically designed experiments | Univariate, trial-and-error, one-factor-at-a-time |
| Knowledge Management | Comprehensive understanding of factor-effects relationships through design space | Limited understanding, focused only on final conditions |
| Robustness | Built into method through design space characterization | Tested after method development |
| Regulatory Flexibility | Operational within entire design space without requiring regulatory submission | Fixed operating conditions, changes require regulatory approval |
| Method Performance | Optimized for multiple attributes simultaneously | May be suboptimal due to univariate optimization |
| Lifecycle Management | Continuous improvement based on enhanced knowledge | Limited post-approval changes |
| Impurity Detection | Comprehensive profiling with superior separation | May miss critical separations |
Research on bupivacaine hydrochloride demonstrates the effectiveness of QbD approaches, where method robustness was confirmed through deliberate variations in flow rate, mobile phase composition, and column temperature while maintaining system suitability criteria [50]. Similarly, the venlafaxine impurity method showed consistent performance with theoretical plates >12,000 and tailing factor <1.2 across variations [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful QbD-based RP-HPLC method development requires specific high-quality materials and reagents. Table 4 details the essential components of the analytical toolkit for antidepressant mixture analysis.
Table 4: Essential Research Reagents and Materials for QbD-based RP-HPLC Analysis
| Item | Specification | Function/Purpose | Example from Case Studies |
|---|---|---|---|
| HPLC Column | C18, 250mm × 4.6mm, 5μm (end-capped) | Stationary phase for chromatographic separation | Purospher STAR end-capped C18 column provided optimal separation for venlafaxine and impurities [52] |
| Mobile Phase A | Buffer solution (pH 3.5-8.5) | Aqueous component for reverse-phase separation | 0.1% ammonia buffer (pH 8.5) for venlafaxine [52]; 0.1% OPA (pH 2.04) for bupivacaine [50] |
| Mobile Phase B | Acetonitrile (HPLC grade) | Organic modifier for gradient elution | Acetonitrile used in both bupivacaine and venlafaxine methods [50] [52] |
| Diluent | Water-acetonitrile mixture (50:50) | Solvent for standard and sample preparation | 50:50 water:acetonitrile for venlafaxine standard preparation [52] |
| Reference Standards | Certified purity >98% | Quantitative calibration and method validation | Venlafaxine HCl and 4-MBC from TCI Chemicals [52] |
| pH Adjustment Reagents | Orthophosphoric acid, ammonia solution | Mobile phase pH optimization | 10% orthophosphoric acid for pH adjustment in venlafaxine method [52] |
| Filters | 0.45μm or 0.2μm membrane filters | Sample clarification before injection | Membrane filters (Millipore, 0.5μm) for personal care product analysis [54] |
Applications in Pharmaceutical Analysis
The QbD-based RP-HPLC method for synthetic antidepressant mixtures finds diverse applications throughout the pharmaceutical development lifecycle. In drug substance and product analysis, the method enables precise quantification of active ingredients while monitoring impurities at low levels. For venlafaxine hydrochloride, the developed method successfully quantified the genotoxic impurity 4-methoxybenzyl chloride at ppm levels, demonstrating sensitivity significantly lower than the specification limit [52]. This application is particularly important for regulatory compliance, as guidelines require strict control of genotoxic impurities in pharmaceutical products.
In stability studies, the stability-indicating capability of QbD-developed methods allows comprehensive monitoring of degradation patterns under various storage conditions. Forced degradation studies following ICH recommendations help identify likely degradation products and establish the method's ability to separate these compounds from the main active ingredients [51]. The method's robustness, built through systematic QbD development, ensures reliable performance throughout the product's shelf life, even when transferred between different laboratories or analysts.
Additionally, these methods find application in formulation development, where they monitor API-excipient interactions and assess compatibility. The bupivacaine hydrochloride method was successfully applied to in-house developed nanostructured lipid carriers (NLCs), demonstrating no interference from formulation excipients [50]. This capability accelerates formulation optimization by providing reliable analytical data on drug loading, release characteristics, and stability in complex delivery systems.
The application of Quality by Design principles to RP-HPLC method development for synthetic antidepressant mixtures represents a significant advancement over traditional univariate approaches. By systematically defining Analytical Target Profiles, identifying Critical Analytical Attributes, and employing statistical design of experiments to characterize method design spaces, QbD ensures the development of robust, reliable, and fit-for-purpose analytical methods. The case studies on venlafaxine and bupivacaine demonstrate that QbD-developed methods exhibit superior performance characteristics, particularly in specificity, sensitivity, and robustness, compared to conventionally developed methods.
The comprehensive validation data presented in this study confirm that QbD-based RP-HPLC methods meet all ICH requirements for pharmaceutical analysis while providing enhanced scientific understanding of method operation and limitations. The systematic approach outlined in this case study provides a transferrable framework that can be adapted for the analysis of diverse pharmaceutical compounds, ultimately contributing to improved product quality and accelerated drug development timelines. As regulatory expectations evolve toward greater emphasis on method lifecycle management, the adoption of QbD principles in analytical method development will become increasingly essential for pharmaceutical scientists and researchers.
In the field of pharmaceutical quantification, the reliability of analytical data is paramount. Matrix effects and ion suppression represent significant technique-specific risks that can compromise the accuracy, precision, and sensitivity of liquid chromatography-mass spectrometry (LC-MS) methods [55] [56]. These phenomena occur when components in a sample matrix co-elute with the target analyte and interfere with the ionization process in the mass spectrometer, leading to either suppression or enhancement of the analyte signal [57] [55]. The consequences can be severe, including inaccurate potency assessments, flawed stability studies, and potential regulatory non-compliance [58] [14].
The susceptibility to matrix effects varies significantly across analytical techniques, with electrospray ionization (ESI) being particularly prone compared to atmospheric pressure chemical ionization (APCI) due to differences in ionization mechanisms [55] [56]. This guide provides a comprehensive comparison of technique-specific risks, experimental protocols for detection and quantification, and strategic approaches to ensure method validity and data integrity in pharmaceutical research and development.
Technique Comparison: Analytical Vulnerabilities and Capabilities
Different analytical techniques exhibit distinct vulnerability profiles to matrix effects and ion suppression, requiring researchers to match technique selection with their specific application requirements and matrix complexity.
Table 1: Comparison of Analytical Techniques and Their Susceptibility to Matrix Effects
| Analytical Technique | Ionization Mechanism | Susceptibility to Matrix Effects | Primary Risk Factors | Common Applications in Pharma |
|---|---|---|---|---|
| LC-ESI-MS/MS | Ionization occurs in liquid phase before transfer to gas phase [55] [56] | High [57] [55] [56] | Phospholipids, salts, ion-pairing agents, organic modifiers [55] | Drug metabolism studies, biomarker quantification, trace analysis [59] [55] |
| LC-APCI-MS/MS | Gas-phase chemical ionization after evaporation [55] [56] | Moderate [55] [56] | Less susceptible to most matrix effects except gas-phase proton transfer reactions [55] | Analysis of less polar, thermally stable compounds [55] |
| GC-MS | Electron impact or chemical ionization in vacuum | Low for ionization, but matrix-induced enhancement occurs [60] | Active sites in GC inlet, matrix components covering active sites [60] | Residual solvents, volatile impurities, metabolomics |
| HPLC-UV/VIS | Photometric absorption (no ionization) | Essentially none | Co-eluting compounds with similar UV spectra | Assay determination, dissolution testing, stability-indicating methods [61] |
| UHPLC-MS/MS | Same as LC-MS but with improved separation | Moderate to High (same ionization principles) | Same as LC-MS but reduced due to better separation | High-throughput analysis, complex mixtures |
The underlying ionization mechanisms explain these vulnerability differences. In ESI, ionization occurs in the liquid phase before charged droplets are transferred to the gas phase, creating multiple points where matrix components can interfere through competition for charge or disruption of droplet formation [55]. In contrast, APCI occurs primarily in the gas phase after evaporation, reducing opportunities for liquid-phase interference [55] [56]. As noted in research, "Matrix effects are not attributed only to ESI interface, although some studies show that atmospheric pressure chemical ionization interfaces (APCI) are less susceptible to ion suppression, mainly due to the APCI mechanism, which occurs by charge transfer from the ionized solvent/additives when the analytes are already in gas-phase" [55].
Quantitative Assessment of Matrix Effects
Experimental Protocols for Detection and Quantification
Researchers can employ several validated experimental approaches to detect and quantify matrix effects during method development and validation.
Table 2: Experimental Protocols for Assessing Matrix Effects
| Method Name | Procedure | Output/Measurement | Advantages | Limitations |
|---|---|---|---|---|
| Post-Column Infusion [57] [56] | Continuous infusion of analyte combined with LC analysis of blank matrix extract | Qualitative signal profile showing ion suppression/enhancement regions | Identifies problematic retention time windows; no blank matrix required for qualitative assessment [56] | Only qualitative; time-consuming for multiple analytes; requires specialized equipment [56] |
| Post-Extraction Spike Method [62] [55] | Compare analyte response in neat solution vs. spiked blank matrix extract | Matrix Factor (MF) = B/A Where A = response in neat solution, B = response in matrix [55] | Quantitative results; standardized approach accepted by regulators | Requires blank matrix; single concentration level assessment |
| Slope Ratio Analysis [56] | Compare calibration curves in neat solution vs. matrix across multiple concentrations | Matrix Effect = (Slopematrix - Slopesolvent)/Slope_solvent × 100% [56] | Assesses matrix effects across concentration range; more comprehensive evaluation | Requires more extensive experimentation; blank matrix needed |
| Absolute vs. Relative Matrix Effect [55] | Test multiple lots of matrix with pre-extraction and post-extraction spiking | Absolute ME = B/A; Relative ME = variability of absolute ME across lots [55] | Assesses consistency of matrix effects across different matrix sources; critical for biological samples | Labor-intensive; requires access to multiple matrix lots |
The matrix factor (MF) calculation provides a quantitative measure: MF = B/A, where B is the peak area of an analyte spiked into blank matrix after extraction, and A is the peak area of the same analyte concentration in neat solution [55]. An MF of 1 indicates no matrix effect, <1 indicates suppression, and >1 indicates enhancement [55]. The relative matrix effect, which measures the variability of matrix effects between different lots of the same matrix, is particularly important for bioanalytical methods where individual patient samples may vary significantly [55].
Case Study: Quantitative Data from Published Studies
Experimental data from published studies illustrates the significant variability of matrix effects across different analytical scenarios.
Table 3: Quantitative Matrix Effect Data from Experimental Studies
| Study Context | Analytical Technique | Matrix | Analyte(s) | Matrix Factor Range | Observation |
|---|---|---|---|---|---|
| F₂-isoprostanes Quantification [59] | HPLC-MS/MS with ESI(-) | Human urine | iPF₂α-III and iPF₂α-VI | Significant ion suppression observed | Required SPE cleanup and isotope internal standards to compensate |
| Pharmaceutical Analysis in Plasma [55] | LC-APCI-MS/MS | Human plasma | Drug compound | ~130% (enhancement) | APCI showed ionization enhancement rather than suppression |
| Pharmaceutical Analysis in Plasma [55] | LC-ESI-MS/MS | Human plasma | Drug compound | ~110% (slight enhancement) | ESI showed different behavior for analyte vs. internal standard |
| Multiresidue Pesticide Analysis [56] | LC-ESI-MS/MS | 20 plant matrices | 129 pesticides | Wide variation across matrices | Demonstrated matrix-specific effects independent of analyte structure |
| Pharmaceuticals in Biological/Environmental Matrices [56] | LC-MS/MS | Urine, plasma, wastewater | 33 pharmaceuticals | Different profiles per matrix type | Similar effects for most compounds in same matrix; different across matrices |
The data demonstrates that matrix effects are highly variable and context-dependent. The study of 129 pesticides across 20 different plant matrices revealed that "most of the substances analyzed had a similar ME profile in the same matrix independently of their structure, while they had a different ME profile moving from urine to plasma, to an environmental matrix" [56]. This underscores the importance of matrix-specific validation rather than assuming consistent behavior across different sample types.
System Suitability and Quality Control Measures
The Role of System Suitability Testing
System suitability testing serves as a critical quality control measure to ensure that the entire analytical system—comprising instrumentation, reagents, columns, and the method itself—is functioning adequately for its intended purpose [63]. According to regulatory guidelines, "system suitability tests are an integral part of chromatographic methods" that "verify that the resolution and reproducibility of a chromatographic system are adequate for the analysis to be performed" [63].
These tests are based on the concept that "the equipment, electronics, analytical operations, and samples constitute an integral system that can be evaluated" as a whole [63]. For methods susceptible to matrix effects, system suitability tests should include evaluation of sensitivity, precision, and retention time stability using matrix-matched quality control samples that mimic actual study samples.
Strategic Implementation for Risk Mitigation
The integration of system suitability testing with matrix effect assessment creates a comprehensive risk mitigation strategy. A well-designed approach includes:
- Pre-study Validation: Comprehensive assessment of absolute and relative matrix effects during method validation using the protocols described in Section 3.1 [55] [56].
- In-study Monitoring: Incorporation of matrix-matched quality control samples at low, medium, and high concentrations in each analytical batch to monitor performance during routine analysis.
- System Suitability Criteria: Establishment of predefined acceptance criteria for precision, accuracy, and sensitivity that must be met before sample analysis can proceed.
This layered approach ensures that matrix effects are adequately characterized and controlled throughout the method lifecycle, from development through routine application.
Experimental Workflow: From Detection to Resolution
The following workflow diagrams the strategic approach to addressing matrix effects in analytical methods, from initial detection through final resolution.
Matrix Effect Investigation and Resolution Workflow
Strategic Pathways for Minimization and Compensation
When significant matrix effects are identified, researchers can pursue minimization strategies to reduce the effect, compensation strategies to correct for it, or more commonly, a combination of both approaches.
Research Reagent Solutions for Matrix Effect Management
Successful management of matrix effects requires strategic selection of reagents and materials designed to address specific challenges in the analytical workflow.
Table 4: Essential Research Reagents and Materials for Managing Matrix Effects
| Reagent/Material | Function/Purpose | Application Examples | Considerations |
|---|---|---|---|
| Stable Isotope-Labeled Internal Standards (SIL-IS) [57] [60] | Compensate for matrix effects by identical chemical behavior with different mass [57] | Mycotoxin analysis in foods [60], pharmaceutical bioanalysis [57] | Gold standard but expensive; may not be available for all analytes [57] |
| Solid Phase Extraction (SPE) Cartridges [59] [62] | Remove interfering matrix components prior to analysis [59] | Cleanup of urine samples for Fâ‚‚-isoprostanes [59], plasma samples | Select sorbent chemistry carefully; may concentrate some interferents [62] |
| Liquid-Liquid Extraction (LLE) Solvents [62] | Selective extraction of analytes away from matrix interferents | Extraction of non-polar analytes from biological fluids | Wider solvent selection provides more selectivity than SPE [62] |
| Analyte Protectants (GC-MS) [60] | Cover active sites in GC inlet to prevent adsorption | Analysis of pesticides in food matrices [60] | GC-MS specific; improves peak shape and response |
| Matrix-Matched Calibration Standards | Calibrate using standards in same matrix as samples to match matrix effects | Used when blank matrix is available [56] | Must demonstrate matrix similarity across different lots [55] |
| High Purity Mobile Phase Additives | Reduce chemical noise that contributes to matrix effects | LC-MS grade solvents and additives | Reduces background signal and potential interference |
| Specialized Chromatography Columns | Improve separation of analytes from matrix components | HILIC for polar compounds [60], UHPLC for better resolution | Improved separation physically separates analytes from interferents [62] |
The selection of appropriate research reagents should be guided by the specific matrix and analytical technique. As noted in comparative studies, "for phenacetin and caffeine determination in endogenous plasma, protein precipitation is the least favourable technique for LC-ESI-MS analyses while LLE was the most favourable" [62]. This highlights the importance of matching sample preparation strategies to the specific analytical challenge.
Matrix effects and ion suppression represent significant challenges in modern pharmaceutical analysis, particularly with sensitive LC-MS techniques. The strategic approach involves:
- Understanding technique-specific vulnerabilities and selecting appropriate ionization techniques based on matrix complexity
- Implementing rigorous assessment protocols during method development to characterize both absolute and relative matrix effects
- Applying targeted minimization strategies through sample preparation, chromatographic separation, or alternative ionization techniques
- Implementing robust compensation methods such as stable isotope-labeled internal standards when minimization is insufficient
- Establishing comprehensive system suitability tests to ensure ongoing method performance
Through this systematic approach, researchers can develop and validate robust analytical methods that provide reliable data despite the challenges posed by complex sample matrices, ultimately supporting the development of safe and effective pharmaceutical products.
Navigating Complex Challenges: Troubleshooting and Optimizing Analytical Methods
Analytical method validation is a foundational process in pharmaceutical development, serving as the documented proof that a laboratory procedure consistently produces reliable, accurate, and reproducible results that are suitable for their intended purpose [58]. This process is not merely a regulatory formality but a critical quality assurance tool that directly impacts patient safety, product quality, and regulatory compliance [15]. Despite well-established guidelines from regulatory bodies like the FDA, ICH, and USP, specific areas of method validation remain persistently problematic across the industry.
The validation journey is fraught with technical challenges that can compromise data integrity and regulatory submissions. Among the most prevalent and impactful issues are incomplete validation protocols and various statistical missteps during method execution and data analysis [58] [64]. These pitfalls quietly threaten the reliability of analytical methods and can lead to delayed approvals, costly audits, and potentially compromised product safety [58]. This guide examines these common challenges through an objective lens, providing comparative data and detailed experimental protocols to help researchers identify, understand, and avoid these critical vulnerabilities in their validation workflows.
Understanding Incomplete Protocol Pitfalls
The Critical Gap in Validation Foundations
A validation protocol serves as the comprehensive roadmap for the entire validation process, detailing the objectives, methodology, acceptance criteria, and responsibilities [58]. When this foundation is incomplete or poorly constructed, it compromises every subsequent step, regardless of the technical excellence of the analytical method itself. Incomplete protocols represent one of the most common sources of regulatory citations and method failure [64].
The core issue stems from a lack of clearly defined objectives and acceptance criteria before validation begins [58]. Without this precise framework, teams struggle to identify which parameters require validation and often produce inconsistent or insufficient validation outcomes. Furthermore, protocols frequently fail to adequately address real-world use cases, such as testing across all relevant sample matrices or using conditions that accurately reflect routine operations [58]. This oversight reduces the method's reliability and increases the risk of regulatory rejection when the method encounters unexpected variables during actual use.
Regulatory Expectations vs. Common Shortcomings
Regulatory agencies provide clear expectations for validation protocols through guidelines such as ICH Q2(R1) and USP <1225> [15] [65]. These frameworks emphasize a risk-based approach with thorough documentation that demonstrates scientific rigor [58]. However, many protocols fall short of these standards in predictable ways.
Table: Common Protocol Deficiencies and Their Impacts
| Protocol Deficiency | Regulatory Expectation | Potential Impact |
|---|---|---|
| Vague or undefined acceptance criteria [64] | Scientifically justified limits with risk-based rationale [64] | Inability to objectively determine validation success; regulatory objections |
| Insufficient sampling plan [58] | Robust sample sizes for statistical significance [58] | High statistical uncertainty; reduced confidence in results |
| Missing risk assessment [58] | Identification of critical method parameters [58] | Failure to address worst-case scenarios; unexpected method failures |
| Inadequate matrix testing [58] | Testing across all relevant matrices [58] | Unexpected interference during real-world use |
| Poorly defined roles and responsibilities [58] | Clear assignment of tasks and approvals [58] | Protocol deviations; documentation gaps |
Examining Statistical Missteps in Validation
The Data Integrity Challenge
Statistical missteps during method validation represent a subtler but equally damaging category of pitfalls that can undermine even the most technically sound analytical methods. These errors often occur when analysts apply statistical methods improperly or use inadequate approaches for data analysis, potentially distorting conclusions and hiding method weaknesses [58]. The foundation of these problems frequently lies in insufficient data integrity practices, where the accuracy, consistency, and reliability of data throughout its lifecycle are compromised [41].
The pharmaceutical industry is increasingly addressing these challenges through standards like ALCOA+, which ensures data is Attributable, Legible, Contemporaneous, Original, and Accurate [41]. Despite these frameworks, practical implementation often falters due to insufficient training, manual data handling errors, and inadequate statistical oversight. Small, seemingly minor statistical errors in validation parameters like accuracy, precision, and linearity can accumulate into significant method vulnerabilities that may only surface during regulatory scrutiny or technology transfer activities.
Specific Statistical Vulnerabilities and Consequences
Statistical pitfalls in method validation manifest across multiple parameters, each with distinct implications for method reliability. The most common issues include insufficient sample sizes, improper application of statistical tools, and failure to account for inherent method variability.
Table: Common Statistical Missteps in Key Validation Parameters
| Validation Parameter | Common Statistical Misstep | Consequence |
|---|---|---|
| Precision [15] | Too few replicates for repeatability assessment [58] | Underestimation of method variability; false confidence in reliability |
| Linearity [15] | Inadequate data points across concentration range [58] | Flawed regression analysis; inaccurate quantification limits |
| Accuracy [15] | Insufficient recovery levels tested [58] | Incomplete understanding of method bias across working range |
| Robustness [15] | Failure to statistically evaluate deliberate variations [58] | Unidentified critical method parameters; method failure with minor changes |
The problem of insufficient data points is particularly prevalent in linearity studies, where regulatory guidelines typically require a minimum of five concentrations, yet many validations fail to include enough points across the specified range to establish true linearity with statistical confidence [58] [15]. Similarly, precision studies often suffer from inadequate replication, failing to account for the inherent variability that occurs between different analysts, instruments, and days [58]. These statistical shortcomings become especially problematic during method transfer activities, where the receiving laboratory may struggle to replicate results obtained under narrowly defined conditions [65].
Experimental Protocols for Identifying Pitfalls
Protocol Completeness Assessment Protocol
Objective: To systematically evaluate validation protocols for completeness and regulatory alignment before implementation.
Materials:
- Draft validation protocol
- Regulatory guidelines (ICH Q2(R1), USP <1225>, relevant FDA guidance)
- Risk assessment template
- Sample matrices representing worst-case scenarios
Methodology:
- Define Method Purpose: Clearly categorize the method (identification, assay, impurity test, etc.) and define its scope [15].
- Establish Acceptance Criteria: Set scientifically justified limits for each validation parameter based on regulatory guidelines and product specifications [64].
- Develop Sampling Strategy: Determine appropriate sample size for each validation parameter using statistical power considerations [58].
- Conduct Risk Assessment: Identify critical method parameters and potential failure modes through Failure Mode and Effects Analysis (FMEA) [66].
- Include All Matrices: Test method performance across all relevant matrices, including placebo, degraded samples, and samples with potential interferents [58].
- Define Roles and Responsibilities: Assign specific tasks, reviews, and approvals to team members with clear accountability [58].
Evaluation: The protocol is considered complete only when all elements are addressed, with acceptance criteria that are achievable, scientifically sound, and compliant with regulatory standards.
Statistical Robustness Testing Protocol
Objective: To validate the statistical approach used in method validation and identify potential missteps before they compromise data integrity.
Materials:
- Homogeneous reference standard
- Calibrated instrumentation (HPLC, GC, or UV-Vis depending on method)
- Statistical software with capability for regression analysis, ANOVA, and outlier detection
- Multiple analysts, instruments, and days for intermediate precision assessment
Methodology:
- Precision Hierarchy Testing:
- Repeatability: Perform a minimum of nine determinations covering the specified range (e.g., three concentrations/three replicates each) [15].
- Intermediate Precision: Vary analyst, instrument, and day to quantify variance components using ANOVA [15].
- Analysis: Calculate relative standard deviation (RSD) for each level and compare against pre-defined acceptance criteria.
Linearity and Range Validation:
- Prepare a minimum of five concentrations spanning the claimed range of the procedure [15].
- Analyze each concentration in triplicate using the proposed method.
- Statistical Analysis: Perform regression analysis with correlation coefficient, y-intercept, slope, and residual sum of squares calculation.
- Acceptance Criteria: Correlation coefficient >0.998, y-intercept not significantly different from zero, and residuals randomly distributed.
Accuracy Recovery Profile:
- Spike placebo with known quantities of analyte across the range (e.g., 50%, 100%, 150% of target concentration).
- Analyze six replicates at each level and calculate percent recovery.
- Statistical Analysis: Determine mean recovery and confidence intervals at each level; ensure all fall within pre-defined limits (typically 98-102%).
Robustness Deliberate Variation:
- Introduce small, deliberate changes to critical parameters (flow rate ±0.1 mL/min, temperature ±2°C, mobile phase pH ±0.2 units) [15].
- Statistical Evaluation: Use statistical tests (e.g., t-tests) to determine if variations significantly impact results compared to standard conditions.
Evaluation: The statistical approach is considered validated when all analyses demonstrate that the method produces data with acceptable accuracy, precision, and linearity, with all statistical parameters meeting pre-defined acceptance criteria.
Visualization of Method Validation Workflows
Method Validation Pathway and Pitfalls
The following diagram illustrates the complete method validation workflow, highlighting critical decision points and identifying where common pitfalls typically occur throughout the process.
Method Validation Pathway and Pitfalls
Statistical Assessment Workflow
This diagram details the statistical evaluation process for method validation data, highlighting key checkpoints to identify and address common statistical missteps.
Statistical Assessment Workflow
Essential Research Reagent Solutions
The success of method validation studies depends heavily on the quality and appropriateness of research reagents and materials. The following table outlines essential solutions and their critical functions in ensuring reliable validation outcomes.
Table: Essential Research Reagents for Method Validation
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Certified Reference Standards [65] | Accuracy determination; method calibration | Certified purity with documented uncertainty; traceability to primary standards |
| Placebo Formulation [15] | Specificity testing; accuracy recovery studies | Representative of final product without active ingredient; same batch-to-batch consistency |
| Forced Degradation Samples [58] | Specificity demonstration under stress conditions | Well-characterized degradation products; controlled extent of degradation |
| System Suitability Test Mixtures [15] | Verification of chromatographic system performance | Contains critical pairs for resolution; stable under defined storage conditions |
| High-Purity Solvents & Reagents [58] | Mobile phase and sample preparation | Low UV absorbance; minimal particulate matter; consistent manufacturer quality |
| Validated Swab Materials [64] | Cleaning validation recovery studies | Documented recovery rates; minimal analyte adsorption; low extractables |
Comparative Analysis of Validation Approaches
Traditional vs. Enhanced Protocol Development
The approach to validation protocol development significantly impacts the completeness and regulatory acceptance of the resulting validation. The following table compares traditional practices with enhanced, risk-based approaches that address common pitfalls.
Table: Protocol Development Approach Comparison
| Protocol Element | Traditional Approach | Enhanced Risk-Based Approach | Impact on Compliance |
|---|---|---|---|
| Acceptance Criteria | Based on historical data or generalized guidelines [58] | Scientifically justified with product-specific rationale [64] | Reduces regulatory queries by 65% [64] |
| Sampling Strategy | Minimum regulatory requirements [58] | Statistical power analysis to determine appropriate n [58] | Increases data confidence; minimizes false acceptance |
| Risk Assessment | Separate activity from validation protocol [58] | Integrated into protocol with defined risk controls [66] | Proactively addresses inspector questions on critical parameters |
| Matrix Testing | Standard concentration only [58] | Worst-case scenarios including impurities [58] | Prevents unexpected failures during routine use |
| Change Control | Addressed post-validation | Defined revalidation triggers in protocol [64] | Maintains validated state through method lifecycle |
Statistical Method Comparison
The choice of statistical approaches for data analysis during validation significantly influences the detection of method vulnerabilities and the overall reliability of the validation study.
Table: Statistical Approach Comparison for Validation Parameters
| Validation Parameter | Basic Statistical Approach | Enhanced Statistical Approach | Advantage |
|---|---|---|---|
| Precision | Single RSD calculation across all data [15] | Variance component analysis (ANOVA) separating analyst, instrument, day effects [15] | Identifies largest sources of variability for improvement |
| Linearity | Correlation coefficient only [15] | Full regression analysis with residuals plot and confidence bands [58] | Detects non-linearity at range extremes; validates weighting factors |
| Accuracy | Mean recovery without confidence intervals [15] | Recovery with confidence intervals at multiple levels [58] | Demonstrates accuracy across working range with statistical confidence |
| Robustness | Pass/fail at each varied condition [15] | Statistical comparison (t-test) of variations vs. standard conditions [58] | Objectively ranks parameter criticality for control strategy |
| Method Transfer | Comparison of means only [65] | Equivalence testing with pre-defined equivalence margin [65] | Statistical evidence of comparable performance between labs |
The journey through analytical method validation is complex, with incomplete protocols and statistical missteps representing persistent challenges that can compromise method reliability and regulatory compliance. Through comparative analysis of approaches and detailed experimental protocols, this guide demonstrates that these pitfalls are not inevitable but can be systematically addressed through enhanced protocol design, robust statistical planning, and risk-based methodologies.
The most successful validation strategies incorporate scientifically justified acceptance criteria, adequate sampling based on statistical principles, and comprehensive documentation that withstands regulatory scrutiny [58] [64]. By adopting these enhanced approaches, pharmaceutical researchers can transform validation from a compliance exercise into a meaningful demonstration of method reliability that ensures product quality and patient safety throughout the method lifecycle.
In pharmaceutical development, the validity of analytical data is paramount, directly influencing drug safety and efficacy evaluations. High-Performance Liquid Chromatography (HPLC) serves as a cornerstone technique for drug quantification, yet analysts frequently encounter three persistent challenges that threaten method reliability: column selection, peak coelution, and inadequate sensitivity. These issues can compromise assay accuracy, precision, and ultimately, the quality control of drug substances and products.
Navigating these challenges requires a structured approach grounded in chromatographic principles and practical troubleshooting strategies. This guide provides a systematic framework for overcoming these common hurdles, with content specifically contextualized for the validation of analytical methods aimed at pharmaceutical quantification. By addressing these critical pain points, researchers and drug development professionals can enhance method robustness, ensure regulatory compliance, and generate reliable data throughout the drug development lifecycle.
Systematic HPLC Column Selection: A Multi-Dimensional Framework
A Four-Dimension Approach to Column Selection
Column selection forms the foundation of any HPLC method, directly influencing selectivity, efficiency, and reproducibility. A haphazard approach often leads to prolonged method development cycles and suboptimal performance. A systematic evaluation across four key dimensions ensures a scientifically sound selection [67]:
- Sample Properties: The chemical characteristics of your analytes—including polarity, molecular weight, functional groups, and chemical stability—dictate the appropriate separation mechanism and stationary phase chemistry [67]. For instance, non-polar pharmaceuticals typically separate well with reversed-phase C18 columns, while polar compounds may require HILIC or normal-phase columns [68].
- Separation Goals: The analytical objective—whether purity control, impurity profiling, or isomer separation—determines the required column efficiency, selectivity, and dimensions [67]. Complex mixtures demand high-efficiency columns (>10,000-20,000 theoretical plates), while chiral separations require specialized chiral stationary phases [67] [68].
- Mobile Phase Conditions: The operating parameters—including pH, buffer composition, and organic solvent ratio—must align with the column's chemical stability limits to ensure reproducibility and prolonged column life [67]. Silica-based columns typically perform best within pH 2-8, while hybrid or polymer-based phases tolerate wider pH ranges [67] [68].
- System Compatibility: Column dimensions and particle size must match the instrument's pressure capabilities and configuration [67]. UHPLC systems (6,000-15,000 psi) accommodate sub-2 µm particles, while conventional HPLC systems (≤4,000 psi) work best with 3-5 µm particles to avoid overpressure [67].
Column Selection Guide for Pharmaceutical Applications
The table below summarizes selection criteria for common stationary phases used in pharmaceutical analysis [68]:
| Stationary Phase | Mechanism | Best For Pharmaceutical | Pros | Cons |
|---|---|---|---|---|
| C18 (ODS) | Hydrophobic partitioning | APIs, impurities, peptides | Most versatile, MS-friendly, high reproducibility | Poor for very polar analytes, silica phase sensitive at extreme pH |
| C8 | Hydrophobic partitioning | Medium hydrophobicity APIs | Shorter retention vs. C18, good for proteins | Less retention than C18 for non-polar compounds |
| Phenyl/PFP | Hydrophobic + π-π interactions | Aromatic compounds, isomers | Enhanced selectivity for aromatics | More specific application scope |
| Cyano (CN) | Mixed-mode (hydrophobic/dipole) | Moderately polar analytes | Dual-mode behavior | Limited retention for very non-polar compounds |
| HILIC | Hydrophilic partitioning | Polar drugs, metabolites | Excellent for water-soluble compounds, MS-compatible | Sensitive to water % in mobile phase |
| Chiral | Chiral recognition | Enantiomeric separations | Unmatched stereoselectivity | Expensive, method development can be challenging |
Experimental Protocol: Column Selectivity Comparison
A standardized protocol for comparing column selectivity helps analysts make data-driven decisions during method development [69]:
- Prepare a representative test mixture containing your API and known impurities/degradation products at appropriate concentrations.
- Select candidate columns representing different selectivity groups (e.g., C18, C8, phenyl, polar-embedded).
- Employ identical chromatographic conditions for all columns: mobile phase composition, pH, temperature, flow rate, and detection.
- Calculate the chromatographic resolution (Rs) between critical peak pairs using the formula: Rs = (tâ‚‚ - tâ‚) / ((wâ‚ + wâ‚‚)/2), where t is retention time and w is peak width at baseline.
- Record system suitability parameters including retention factor (k), tailing factor (T), and theoretical plates (N).
- Calculate similarity factors (Fs) if comparing to a reference column using established parameters (hydrophobicity, steric, hydrogen bonding, charge interactions) [69].
This systematic approach enables objective comparison of column performance for your specific application, facilitating selection of the optimal stationary phase.
Peak Coelution: Detection, Troubleshooting, and Resolution
Assessing and Confirming Peak Purity
Coelution occurs when two or more compounds elute at the same retention time, leading to inaccurate quantification—a critical concern in impurity profiling and assay validation. Reliance on retention time alone is insufficient to confirm peak purity [70]. Advanced detection strategies provide more definitive assessment:
- Photodiode Array (PDA) Detection: Measures UV absorbance across a peak and identifies spectral variations that may indicate coelution. Software metrics (purity angle, purity threshold) should be interpreted cautiously and supplemented with manual review of spectral overlays, particularly at peak edges where coelution often manifests [70].
- Liquid Chromatography-Mass Spectrometry (LC-MS): Provides definitive coelution detection based on mass differences rather than UV absorbance, particularly valuable for identifying low-level contaminants not detectable by UV [70].
Even when software indicates a "pure" peak based on purity thresholds, visual inspection of spectral overlays across different peak regions (up-slope, apex, down-slope) remains essential, as minor variations can indicate significant coelution [70].
Figure: A systematic workflow for detecting and resolving peak coelution issues, incorporating both PDA and LC-MS techniques for comprehensive assessment.
Strategies for Resolving Coelution Issues
When coelution is confirmed or suspected, multiple chromatographic parameters can be adjusted to improve resolution:
- Mobile Phase Optimization: Modify organic solvent ratio, pH, or buffer concentration to alter selectivity [71] [72]. For ionizable compounds, adjusting mobile phase pH to values at least 2 units away from the analyte pKa can significantly impact retention and selectivity [73].
- Temperature Adjustment: Lower column temperatures often increase retention and may improve resolution, though analysis time may lengthen [71].
- Gradient Optimization: For complex samples, implementing or optimizing a gradient elution program can dramatically improve separation. "Sharpening" the gradient by limiting the range of organic solvent or adjusting gradient steepness can reduce peak width and improve resolution [74] [72].
- Alternative Stationary Phases: If selectivity cannot be achieved with initial column chemistry, switch to a different selectivity group (e.g., from C18 to phenyl or pentafluorophenyl) to exploit different interaction mechanisms [67] [68].
Sensitivity Enhancement Strategies for Trace Analysis
Comprehensive Approach to Sensitivity Optimization
Inadequate sensitivity compromises the ability to detect and quantify low-level impurities and degradants, directly impacting method validation for pharmaceutical quantification. Sensitivity enhancement requires a dual approach: increasing the analyte signal while reducing baseline noise [75].
Signal Enhancement Strategies focus on increasing peak height and improving detector response:
- Reduce Column Internal Diameter (ID): Decreasing column ID from 4.6 mm to 2.1 mm increases analyte concentration at the detector approximately 4-fold due to reduced dilution effects [75].
- Increase Column Efficiency: Columns with smaller particles (sub-2 µm) or core-shell technology produce narrower, higher peaks. Replacing fully porous 3 µm particles with 2.7 µm core-shell particles can nearly double efficiency [75].
- Optimize Flow Rate: Operating at the optimal flow rate defined by van Deemter curves maximizes efficiency. Excessive flow rates can compromise detection, especially with detectors having slow response times [75].
- Utilize Gradient Elution: Switching from isocratic to gradient elution can "sharpen" later-eluting peaks, increasing peak height and improving signal-to-noise ratio [74].
Noise Reduction Techniques focus on minimizing baseline disturbances:
- Mobile Phase Quality: Use high-purity solvents and additives. Avoid additives like TEA or TFA with high UV absorbance, particularly at wavelengths below 220 nm [75].
- System Maintenance: Regularly check for contamination, air in the system, pump pressure fluctuations, UV lamp age, and detector cell cleanliness [75].
- Column Selection and Conditions: Minimize column bleeding by operating within recommended pH, temperature, and solvent compatibility ranges [75].
Experimental Protocol: LOD/LOQ Determination and Improvement
For method validation, determining Limit of Detection (LOD) and Limit of Quantitation (LOQ) follows standardized protocols [76]:
- Prepare serial dilutions of analyte standards approaching expected detection limits.
- Inject each concentration with a minimum of three replicates.
- Measure signal-to-noise ratio (S/N) by comparing analyte peak height to baseline noise.
- Establish LOD at S/N ≥ 3, and LOQ at S/N ≥ 10 [76].
- Verify accuracy and precision at LOQ level (%RSD ≤ 20% typically acceptable).
If LOD/LOQ values are unsatisfactory, implement these optimization strategies [74] [75]:
- Sample Pre-concentration: Increase injection volume within column capacity limits (typically 1-2% of total column volume for concentrations of 1 µg/µL) [71].
- Detector Wavelength Optimization: Set detection at λmax for maximum sensitivity, avoiding wavelengths below 200 nm where detector noise increases [72] [75].
- Column Dimension Adjustment: Switch to shorter columns with smaller particles (e.g., from 150 mm with 5 µm particles to 100 mm with 3 µm particles) to maintain resolution while increasing sensitivity [74].
- Efficiency Improvements: Utilize core-shell particles that provide efficiency comparable to sub-2 µm fully porous particles but at lower backpressures [74].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful HPLC method development and troubleshooting requires access to appropriate materials and reagents. The following table details essential components for pharmaceutical HPLC analysis:
| Item | Function/Purpose | Application Notes |
|---|---|---|
| C18 Column (multiple selectivity groups) | Primary separation workhorse for most APIs | Test columns from different manufacturers/silica lots [69] |
| PFP or Phenyl Column | Alternative selectivity for problematic separations | Particularly useful for aromatic compounds and isomers [68] |
| HPLC-grade Acetonitrile and Methanol | Mobile phase organic modifiers | Acetonitrile offers lower viscosity; methanol provides different selectivity [72] |
| High-purity Water | Aqueous component of mobile phase | Use 18 MΩ-cm resistivity or equivalent quality |
| Buffer Salts (e.g., potassium phosphate) | Mobile phase pH control and ionic strength adjustment | Use volatile buffers (ammonium formate/acetate) for LC-MS applications [76] [73] |
| pH Adjustment Reagents | Fine-tuning mobile phase pH | Phosphoric acid for acidic pH; NaOH for basic pH [73] |
| Guard Column | Protection of analytical column from matrix components | Should contain same stationary phase as analytical column |
Integrated Workflow for Method Development and Validation
Figure: An integrated HPLC method development workflow incorporating systematic column selection, selectivity optimization, and sensitivity enhancement, culminating in method validation.
Developing a robust, stability-indicating HPLC method for pharmaceutical quantification requires a structured approach that addresses column selection, coelution, and sensitivity in an integrated manner. By implementing the systematic strategies outlined in this guide—including the four-dimension column selection framework, comprehensive peak purity assessment techniques, and dual-approach sensitivity enhancement—researchers can overcome these common challenges effectively.
The resulting validated methods will demonstrate the reliability, accuracy, and precision required for pharmaceutical quality control and regulatory submissions, ultimately supporting the development of safe and effective drug products. As evidenced in multiple pharmaceutical applications [76] [73], such methodical approaches to HPLC challenges yield robust separation methods capable of withstanding rigorous validation requirements according to ICH and USP guidelines.
Robust chromatographic analysis is fundamental to modern pharmaceutical development, ensuring the safety, efficacy, and quality of drug substances and products. The reliability of any analytical result is critically dependent on two intertwined pillars: sample preparation and chromatographic optimization [77] [78]. Sample preparation transforms a raw sample into an analysis-ready form, free from interferences and compatible with the instrument, while chromatographic optimization seeks to achieve the highest possible resolution, speed, and sensitivity [79]. Within the strict framework of analytical method validation, as guided by ICH and USP guidelines, the choices made in these areas directly impact method performance characteristics such as accuracy, precision, and specificity [79] [80]. This guide provides a comparative analysis of advanced strategies and techniques in both domains, offering drug development professionals a structured overview to inform their method development and validation processes.
Advanced Sample Preparation Techniques
Sample preparation is a critical step to isolate analytes from complex matrices like plasma or formulated products, thereby protecting the chromatographic system and enhancing detection reliability [77] [78].
Technique Comparison and Selection
Choosing the correct sample preparation technique depends on the sample matrix, the physicochemical properties of the analytes, and the required sensitivity. The table below compares key techniques used in pharmaceutical analysis.
Table 1: Comparison of Advanced Sample Preparation Techniques
| Technique | Principle | Best For | Advantages | Limitations |
|---|---|---|---|---|
| Solid-Phase Extraction (SPE) [77] | Selective retention of analytes on a solid sorbent using different chemistries (e.g., C18, ion-exchange). | Clean-up and concentration of analytes from complex biological fluids [77]. | High selectivity and clean-up; ability to concentrate analytes; automation-friendly [77]. | Can be time-consuming; method development can be complex; sorbent cost. |
| Liquid-Liquid Extraction (LLE) [77] [81] | Partitioning of analytes between two immiscible liquids based on solubility. | Fractioning metabolites by polarity; extracting non-polar analytes from plasma [81]. | Simple principle; high capacity; effective for a broad range of analytes [77]. | Uses large solvent volumes; emulsion formation; not easily automated. |
| Supported Liquid Extraction (SLE) [77] | Liquid-solid extraction where the liquid sample is absorbed onto a diatomaceous earth support, and analytes are eluted with an organic solvent. | A cleaner alternative to traditional LLE for biological samples. | Reduced emulsion formation; better recovery for some analytes; uses less solvent than LLE [77]. | Can be more expensive than LLE. |
| QuEChERS [77] | A streamlined method involving extraction with acetonitrile and partitioning with salts. | Quick, multi-analyte extraction from complex matrices like food; high-throughput labs [77]. | Fast, low-cost, and effective; rugged and safe (less solvent) [77]. | May provide less clean-up than SPE for very complex matrices. |
| Solid-Phase Microextraction (SPME) [77] [82] | A solvent-free technique where a coated fiber absorbs analytes from the sample or headspace, followed by thermal desorption in the GC inlet. | Trace-level analysis of volatile/semi-volatile compounds; ideal for GC [82]. | Minimal solvent use; integrates sampling, extraction, and concentration; can be automated [77]. | Fiber can be fragile; limited by fiber coating chemistry; potential for carryover. |
| Protein Precipitation [77] | Adding an organic solvent (e.g., acetonitrile) to a biological sample to denature and precipitate proteins, which are then removed by centrifugation. | Fast removal of proteins from plasma/serum in bioanalysis [77]. | Very simple and rapid; high throughput [77]. | Limited clean-up; can dilute the sample; may not remove phospholipids effectively. |
Experimental Protocol: Liquid-Liquid Extraction for Non-Polar Metabolites
The following protocol, adapted from a metabolomics study, details the fractionation of non-polar metabolites from human plasma using a liquid-liquid extraction technique, showcasing a practical application for complex biological samples [81].
- Step 1: Sample Preparation. Thaw the human plasma sample on ice. Accurately pipette 100 µL of plasma into a microcentrifuge tube.
- Step 2: Solvent Addition and Extraction. Add a 3:1:1 (v/v/v) mixture of methanol, water, and chloroform (e.g., 300 µL methanol, 100 µL water, 100 µL chloroform) to the plasma. Vortex the mixture vigorously for 2-3 minutes to ensure complete mixing and extraction of metabolites.
- Step 3: Phase Separation. Centrifuge the mixture at a high speed (e.g., 10,000-14,000 rpm) for 10 minutes. This will result in the formation of two distinct phases: an upper aqueous phase (containing polar metabolites) and a lower organic phase (containing non-polar metabolites).
- Step 4: Ultrafiltration Clean-up. Carefully separate the two phases. Transfer each phase to a separate ultrafiltration device (e.g., a 3kDa molecular weight cut-off filter). Centrifuge to remove any remaining proteins or particulate matter, obtaining a clarified aqueous and organic fraction.
- Step 5: Sample Reconstitution. Evaporate the organic (chloroform) phase to dryness under a gentle stream of nitrogen gas. Reconstitute the dried residue in 100 µL of acetonitrile to make it compatible with reversed-phase LC/MS analysis [81].
This workflow efficiently separates complex biological components for detailed analysis.
Research Reagent Solutions for Sample Preparation
Table 2: Essential Reagents for Sample Preparation
| Reagent/Material | Function/Application |
|---|---|
| C18 SPE Sorbents [77] | Reversed-phase extraction for non-polar analytes; common for biological fluid clean-up. |
| QuEChERS Kits [77] | Provides pre-weighed salts and sorbents for quick, efficient extraction of pesticides and contaminants from food matrices. |
| SPME Fibers [77] [82] | Coated fibers for solventless extraction of volatile compounds, used with GC. |
| Ultrafiltration Devices [81] | Remove proteins and other macromolecules based on molecular weight cut-off; used for cleaning up plasma/serum samples. |
| Methanol, Acetonitrile, Chloroform [81] | Common solvents for protein precipitation, liquid-liquid extraction, and as diluents for HPLC. |
| Formic Acid [81] | Mobile phase additive in LC-MS to improve ionization efficiency and peak shape for acidic/basic analytes. |
| 0.45 µm & 0.22 µm Syringe Filters [78] | Removal of particulate matter from samples prior to HPLC/UPLC injection to protect the column. |
Chromatographic Optimization Strategies
Chromatographic optimization aims to achieve the best possible separation of analytes in the shortest time, which is crucial for high-throughput laboratories and methods requiring high sensitivity.
Ultra-High-Performance Liquid Chromatography (UHPLC)
UHPLC represents a significant advancement over traditional HPLC. By using columns packed with smaller particles (sub-2 µm) and operating at much higher pressures (up to 15,000 psi or more), UHPLC provides superior resolution, increased sensitivity, and faster analysis times [83] [79] [84]. A comparative study of VHPLC systems demonstrated their suitability for the analysis of pharmaceutical compounds, highlighting gains in speed and resolution [83].
Comprehensive Two-Dimensional Gas Chromatography (GC×GC)
For complex volatile mixtures, GC×GC offers a powerful solution. This technique connects two GC columns of different selectivity through a modulator. The modulator continuously captures, refocuses, and reinjects small fractions from the first dimension into the second dimension, resulting in a dramatic increase in peak capacity (>20,000) compared to one-dimensional GC [85]. This is particularly beneficial for untargeted metabolomics and analyzing pharmaceuticals in complex biological matrices, as it can resolve co-eluting compounds that would be inseparable with traditional GC [85].
Experimental Protocol: UPLC-UV Method for Imatinib TDM
This protocol outlines a validated Ultra Performance Liquid Chromatography with UV detection (UPLC-UV) method for the therapeutic drug monitoring of Imatinib in human plasma, demonstrating optimization for clinical application [80].
Step 1: Chromatographic Conditions.
- Column: Luna Omega C18 (1.6 µm, 2.1 mm x 50 mm).
- Mobile Phase: 30:70 (v/v) mixture of Acetonitrile and 0.02 M Potassium Phosphate Buffer (pH adjusted to 3.2).
- Flow Rate: 0.5 mL/min.
- Column Temperature: 40 °C.
- Detection: UV at 263 nm.
- Injection Volume: 10 µL.
- Run Time: 2 minutes (Imatinib retention time ~0.56 minutes).
Step 2: Sample Preparation.
- Pipette 100 µL of human plasma (from patient samples or calibration standards) into a microcentrifuge tube.
- Add 20 µL of 20% Trichloroacetic Acid to precipitate plasma proteins.
- Vortex mix for 30 seconds and then centrifuge at 5000 rpm for 5 minutes.
- Transfer the supernatant and filter it through a 0.22 µm membrane filter into an HPLC vial.
Step 3: Validation and Comparison.
The method optimization focuses on achieving a rapid, robust, and precise separation.
Key Parameters for HPLC Method Optimization
Systematic optimization is key to developing a robust HPLC method. Critical parameters include [79]:
- Mobile Phase: Selection of solvents, pH, and buffer concentration to control ionization, retention, and selectivity. Gradient elution is often used for complex mixtures.
- Stationary Phase: Choice of column chemistry (C18, C8, phenyl, etc.), particle size (e.g., sub-2 µm for UHPLC), and column dimensions.
- Temperature: Control of column temperature to improve reproducibility and efficiency.
- Flow Rate: Optimization to balance analysis time, backpressure, and resolution.
Comparative Data in Pharmaceutical Analysis
Direct comparison of analytical methods provides critical data for selecting the most appropriate technique for a specific application, such as therapeutic drug monitoring (TDM).
Table 3: Method Comparison for Imatinib Therapeutic Drug Monitoring
| Parameter | Automated Immunoassay [80] | UPLC-UV Method [80] |
|---|---|---|
| Analytical Principle | Nanoparticle agglutination immunoassay | Chromatographic separation with UV detection |
| Linearity Range | 500 – 2750 ng/mL | 500 – 3000 ng/mL |
| Correlation Coefficient (r) | 0.996 | 0.999 |
| Intra-/Inter-day Precision (CV%) | Not all values below 15% | All values below 6.0% |
| Average Accuracy (Recovery %) | 94.4% | 100.8% |
| Sample Volume | 3.5 µL | 100 µL |
| Throughput | High (automated) | Moderate |
| Best Suited For | High-throughput routine screening | Accurate, precise TDM for dose adjustment |
The integration of advanced sample preparation and chromatographic optimization is paramount for developing validated, reliable analytical methods in pharmaceutical research. Techniques like LLE and SLE provide essential clean-up for complex biological samples, while technological advancements such as UHPLC and GC×GC deliver unprecedented separation power. As demonstrated by the Imatinib case study, the choice of method directly impacts the quality of data and, consequently, clinical decision-making. The ongoing trends toward automation, miniaturization, and green chemistry will continue to push the boundaries of sensitivity, efficiency, and sustainability in pharmaceutical analysis, ensuring that these techniques remain indispensable in the scientist's toolkit [77] [79].
Special Considerations for Quantifying Endogenous Biomarkers and Impurities
In pharmaceutical development, the precise quantification of endogenous biomarkers and process-related impurities is critical for ensuring drug safety and efficacy. However, these two analytical endeavors present fundamentally different challenges and considerations. While impurity analysis focuses on detecting and quantifying unwanted chemical entities in drug substances and products, endogenous biomarker quantification involves measuring naturally occurring molecules within complex biological systems, where the analyte is already present in the sample matrix [86] [87].
The International Council for Harmonisation (ICH) establishes rigorous guidelines for impurity profiling, setting thresholds for identification, qualification, and control [88] [89]. For endogenous biomarkers, regulatory frameworks are still evolving, with the FDA recently emphasizing a "fit-for-purpose" approach that considers the biomarker's specific context of use [86] [87]. This guide provides a comparative analysis of the methodological considerations, regulatory requirements, and experimental approaches for these two distinct yet equally vital analytical domains in pharmaceutical research and development.
Fundamental Differences in Analytical Approach
The core distinction between these fields lies in the fundamental relationship between the analyte and the sample matrix. In impurity analysis, the analyte is typically exogenous to the sample matrix, whereas in endogenous biomarker quantification, the analyte is an inherent component of the biological matrix [87]. This distinction creates divergent challenges in method development and validation, particularly concerning accuracy assessment, reference standard availability, and matrix effects.
Analytical Characteristics Comparison
Table 1: Fundamental differences between endogenous biomarker and impurity quantification
| Characteristic | Endogenous Biomarker Quantification | Impurity Quantification |
|---|---|---|
| Analyte Nature | Naturally present in biological matrix [87] | Exogenous to drug substance/product [89] |
| Reference Standard | Recombinant protein/synthetic analog may differ from endogenous form [86] | Well-characterized authentic impurity standard [90] |
| Accuracy Assessment | Method of standard additions; surrogate matrices [87] | Spike-recovery of reference standard [87] |
| Matrix Effects | Cannot be eliminated by dilution (sensitivity constraints) [86] | Often addressed through sample dilution [86] |
| Primary Challenge | Differentiating measured analyte from naturally fluctuating background [86] | Detecting and identifying trace-level contaminants [89] |
| Regulatory Framework | Fit-for-purpose approach [86] [87] | Established ICH guidelines (Q3A-Q3D) [89] [91] |
Methodological Considerations and Experimental Protocols
Analytical Techniques and Platforms
Impurity profiling leverages a suite of chromatographic and spectroscopic techniques, with high-performance liquid chromatography (HPLC) serving as the gold standard for separation, often coupled with mass spectrometry (MS) for identification and structural elucidation [89] [92]. Recent advancements in LC-MS/MS have significantly enhanced sensitivity and selectivity for both fields, enabling detection of impurities at progressively lower thresholds and biomarkers at physiologically relevant concentrations [93] [91].
For endogenous biomarker quantification, ligand binding assays (LBAs) including ELISA have historically been the primary platform [86]. However, newer technologies offering improved sensitivity and multiplexing capabilities are gaining traction, including immunoaffinity LC-MS/MS, electro-chemiluminescence platforms, and microfluidic systems like Simple Plex [86]. These platforms help address the fundamental challenge of measuring low-abundance biomarkers against a complex background of similar endogenous molecules.
Experimental Workflows
The experimental approach for each application differs significantly in both philosophy and execution, as illustrated in the following workflows:
Diagram 1: Comparative analytical workflows for impurity versus biomarker quantification.
Key Experimental Protocols
Protocol for Impurity Identification and Quantification Using LC-MS/MS
Sample Preparation: For drug substances, dissolve in appropriate solvent followed by filtration (0.45 μm) or dilution as per ICH guidelines. For drug products, extract active ingredient using solvent extraction, sonication, or accelerated solvent extraction based on formulation composition [89] [91].
Chromatographic Separation: Utilize reversed-phase HPLC with C18 column (150 × 4.6 mm, 3.5 μm). Mobile phase: gradient elution with 0.1% formic acid in water (A) and 0.1% formic acid in acetonitrile (B). Flow rate: 1.0 mL/min with split to MS interface. Column temperature maintained at 40°C [91] [92].
Mass Spectrometric Analysis: Operate MS in positive/negative electrospray ionization mode with data-dependent acquisition. Full scan (m/z 50-1000) followed by MS/MS scans of potential impurity peaks. Use collision-induced dissociation energy optimized for compound class [91].
Structural Elucidation: Compare MS/MS fragmentation patterns with available standards or literature data. For unknown impurities, perform accurate mass measurement for elemental composition determination and propose fragmentation pathways [91].
Quantification: Prepare calibration standards of known impurities and establish linearity (typically 0.05-150% of specification level). Calculate impurity levels using relative response factors as per ICH Q3A/Q3B guidelines [89] [91].
Protocol for Endogenous Biomarker Quantification Using Immunoaffinity LC-MS/MS
Sample Preparation: Use minimal dilution to maintain sensitivity. For plasma/serum samples, employ protein precipitation followed by phospholipid removal. Evaluate both surrogate matrix and authentic matrix (stripped) approaches for calibration standards [86] [87].
Matrix Selection and Parallelism Testing: Prepare calibrators in surrogate matrix (buffer or stripped matrix) and quality controls in authentic matrix. Perform parallelism testing by serially diluting pooled study samples and comparing the response curve to the calibrator curve to demonstrate similar dilutional behavior [87].
Immunoaffinity Enrichment: Incubate samples with anti-biomarker antibody conjugated to magnetic beads. Wash beads to remove non-specifically bound matrix components. Elute captured biomarker using acidic conditions [86].
Digestion and LC-MS/MS Analysis: For protein biomarkers, digest with trypsin following reduction and alkylation. Analyze signature peptides using reversed-phase LC-MS/MS with stable isotope-labeled internal standards for quantification [86].
Accuracy Assessment: Use standard addition method by spiking known quantities of recombinant biomarker into individual study samples. Calculate accuracy by comparing measured versus expected values across the physiological range [87].
Regulatory and Validation Frameworks
Established Versus Evolving Standards
Impurity assessment follows well-established ICH guidelines: Q3A(R2) for drug substances, Q3B(R2) for drug products, Q3C for residual solvents, and Q3D for elemental impurities [89] [91]. These guidelines specify strict thresholds for reporting, identification, and qualification based on maximum daily dose, with typical identification thresholds of 0.1% for drug substances [89]. For genotoxic impurities, ICH M7(R1) establishes a threshold of Toxicological Concern (TTC) of 1.5 μg/day for mutagenic impurities [91].
In contrast, biomarker method validation employs a "fit-for-purpose" approach, where validation rigor is determined by the biomarker's context of use [86] [87]. The 2025 FDA draft guidance suggests starting with approaches used for drug assays but acknowledges fundamental differences, particularly for accuracy assessment of endogenous analytes [87].
Validation Parameter Comparison
Table 2: Comparison of key validation parameters for impurity versus biomarker assays
| Validation Parameter | Impurity Assays | Endogenous Biomarker Assays |
|---|---|---|
| Accuracy | Spike-recovery of reference standard at multiple levels [89] | Standard addition method in individual study samples [87] |
| Precision | Repeated measures of spiked control samples [87] | Repeated measures of native biological samples [87] |
| Specificity | Resolution from main component and other impurities [91] | Differentiation from structurally similar endogenous molecules [86] |
| Quantification Standard | Authentic impurity standard [90] | Recombinant protein/synthetic analog [86] |
| Matrix Effect | Addressed through sample dilution [86] | Addressed through minimal dilution and parallelism testing [86] |
| Reference Materials | USP Reference Standards and Pharmaceutical Analytical Impurities (PAIs) [90] | Commercial recombinant proteins with characterization against endogenous form [86] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for impurity and biomarker analysis
| Tool/Reagent | Function | Application |
|---|---|---|
| USP Reference Standards | Highly characterized impurities for identification and quantification [90] | Impurity Analysis |
| Pharmaceutical Analytical Impurities (PAIs) | Impurity materials for method development and validation [90] | Impurity Analysis |
| Stable Isotope-Labeled Internal Standards | Normalize for variability in sample preparation and ionization efficiency [86] | Both Fields |
| Anti-Biomarker Antibodies | Specific capture and enrichment of low-abundance biomarkers [86] | Biomarker Analysis |
| Stripped/Artificial Matrices | Create analyte-free background for calibration curves [87] | Biomarker Analysis |
| Forced Degradation Samples | Generate degradation products for method validation [91] | Impurity Analysis |
| Chromatography Columns | Separate analytes from complex matrices [89] [92] | Both Fields |
| Qualified Residual Solvent Mixtures | Identify and quantify Class 1-3 solvents per ICH Q3C [89] | Impurity Analysis |
Analytical Challenges and Emerging Solutions
Current Limitations and Technological Gaps
Impurity profiling faces challenges in detecting and characterizing unexpected or unknown impurities, particularly at low levels in complex formulations. The emergence of nitrosamine drug substance-related impurities (NDSRIs) has highlighted the need for more predictive analytical approaches and sensitive screening methods [90]. Additionally, genotoxic impurities require specialized detection strategies due to their stringent control limits [91].
Endogenous biomarker quantification struggles with the disconnect between recombinant calibrators and endogenous analytes, which may differ in post-translational modifications, folding, or other characteristics affecting immunoreactivity [86]. This can lead to significant inaccuracies in absolute quantification. Matrix effects also present a greater challenge for biomarkers than for impurity analysis, as excessive dilution to mitigate matrix interference compromises the sensitivity needed to measure physiological concentrations [86].
Innovative Approaches and Future Directions
Mass spectrometry continues to redefine both fields, with Alphalyse's MS database demonstrating how historical analytical results can accelerate impurity analysis from years to weeks for new drug development projects [93]. The recent inclusion of MS-based quality control for biologics in the US Pharmacopeia further validates this trend [93].
For biomarkers, immunoaffinity-LC-MS/MS hybrid approaches are gaining prominence, combining the specificity of immunoassays with the analytical robustness of mass spectrometry [86]. Emerging platforms like Gyrolab and Simoa offer improved sensitivity and reduced sample volumes, while multiplexed LC-MS/MS panels enable simultaneous quantification of multiple biomarkers from a single sample [86].
The following diagram illustrates the decision-making pathway for selecting appropriate analytical strategies based on analyte characteristics and regulatory requirements:
Diagram 2: Decision pathway for selecting appropriate quantification strategies.
The quantification of endogenous biomarkers and pharmaceutical impurities, while sharing some analytical technologies, requires distinctly different methodological approaches and validation strategies. Impurity analysis benefits from well-established regulatory frameworks and the availability of authentic reference standards, enabling straightforward spike-recovery validation approaches. Conversely, endogenous biomarker quantification must address the fundamental challenge of accurately measuring an analyte that is inherently present in the sample matrix, necessitating specialized approaches like standard addition methods and parallelism testing.
As both fields advance, mass spectrometry continues to play an increasingly pivotal role in addressing sensitivity and specificity challenges. For impurities, databases of known impurities and advanced hyphenated techniques are accelerating development timelines. For biomarkers, hybrid immunoaffinity-LC-MS/MS approaches and more sensitive platforms are improving the reliability of physiological measurements. Understanding these distinct considerations enables researchers to select appropriate strategies, develop robust methods, and generate data that meets regulatory expectations for their specific analytical challenge.
In pharmaceutical quantification research, the validity of any analytical result is fundamentally dependent on the performance and accuracy of the instruments used. Instrument calibration and control form the foundational layer that supports all subsequent analytical method validation activities, as defined by ICH Q2(R1) guidelines [94]. Without rigorous calibration protocols, even the most sophisticated analytical methods cannot generate reliable data for drug substance and drug product analysis.
Calibration, when distinguished from the broader concepts of qualification and validation, specifically ensures the measurement accuracy of individual instruments by comparing their readings against known reference standards [95]. This process establishes traceability to national and international standards, creating the "unbroken chain of comparisons" that links laboratory measurements back to recognized reference materials, ultimately ensuring data integrity throughout the drug development lifecycle [96].
Core Calibration Technologies: A Comparative Analysis
Selecting appropriate calibration technology is critical for achieving accurate results. The optimal choice depends on multiple factors including volume range, required precision, regulatory demands, and application context. The following technologies represent the most common approaches used in pharmaceutical research.
Table 1: Comparison of Major Liquid Handling Calibration Technologies
| Technology | Optimal Volume Range | Key Advantages | Primary Limitations | Best Application Context |
|---|---|---|---|---|
| Gravimetry [97] | 200 μL - 1000 μL & above | - Widely accepted by regulatory agencies (ISO, ASTM)- Directly traceable to national standards- Equipment commonly available in labs | - Challenging for small volumes (<10 μL requires microgram balance)- Sensitive to environmental factors (evaporation, static, vibration)- Time-consuming for multichannel devices | Calibration of single-channel devices handling larger volumes where regulatory traceability is mandatory |
| Single-Dye Photometry [97] | Varies by implementation | - Good precision- Less sensitive to environmental conditions than gravimetry/fluorometry- Suitable for multichannel device verification- Dyes more stable than fluorescent alternatives | - Requires uncertainty analysis per ISO 8655-7- Optical quality of plates/cuvettes affects accuracy- Dyes can be source of error without proper validation | Demonstrating precision across multichannel liquid handlers when environmental control is challenging |
| Ratiometric Photometry [97] | Varies by implementation | - Compensates for variations in path length, meniscus formation, and droplet formation- Potentially higher accuracy than single-dye methods | - More complex implementation- Requires specific dye systems | High-accuracy applications where environmental variables cannot be perfectly controlled |
| Fluorometry [97] | 5 nL - 50 μL | - Extremely sensitive for very small volumes- Capable of detecting low concentration signals | - Difficult to establish robust traceability- Sensitive to chemical environment (pH, ionic strength)- Dyes susceptible to quenching and photobleaching- Primarily for precision, not accuracy | Measuring precision of small volume handling under nearly identical conditions where traceability is not required |
Performance Characteristics and Experimental Data
Calibration protocols must demonstrate several key performance characteristics to meet analytical method validation requirements [94]. The following parameters are typically evaluated during calibration technology assessment:
Accuracy and Precision: Accuracy represents the closeness of agreement between a measured value and its true accepted reference value, while precision indicates the degree of scatter in a series of measurements from multiple samplings [94]. The classic dartboard analogy illustrates this relationship: darts clustered tightly but off-center represent high precision with low accuracy, while darts scattered randomly around the center show high accuracy with low precision. Ideal calibration achieves both, with all darts tightly clustered at the bullseye.
Linearity and Range: Linearity represents an analytical method's ability to produce results that are directly proportional to analyte concentration within a given range [94]. This is typically demonstrated using a minimum of five concentration points and evaluated statistically (e.g., regression analysis with R² > 0.95). The range defines the interval between upper and lower concentration levels across which acceptable linearity, accuracy, and precision are maintained [94].
Detection and Quantitation Limits: The Detection Limit (DL) is the lowest amount of analyte that can be detected but not necessarily quantified, while the Quantitation Limit (QL) is the lowest concentration that can be quantified with acceptable accuracy and precision [94]. These are often determined via signal-to-noise ratios (typically 3:1 for DL and 10:1 for QL) or based on standard deviation and slope of the calibration curve.
Calibration Management in the Pharmaceutical Context
Strategic Program Implementation
Establishing a robust calibration program extends beyond selecting technologies to encompass comprehensive management strategies. Effective programs are built on four core pillars [96]:
- Unshakeable Traceability: Maintaining an unbroken chain of comparisons linking instruments to NIST or other international standards through accredited calibration labs.
- Standardized Procedures: Developing detailed Standard Operating Procedures (SOPs) that define calibration processes, including scope, required standards, measurement parameters, environmental conditions, and step-by-step protocols.
- Uncertainty Management: Recognizing that all measurements have inherent uncertainty—the "doubt" about any measurement result—and ensuring the Test Uncertainty Ratio (TUR) is at least 4:1 (where calibration process uncertainty is four times smaller than device tolerance).
- Regulatory Compliance: Adhering to ISO 9001, FDA, and other regulatory requirements that mandate calibration at specified intervals, unique instrument identification, and documented corrective actions when instruments are found out of tolerance.
Calibration Frequency and Scheduling
Instrument calibration frequency should be determined through risk-based assessment considering factors such as instrument criticality, manufacturer recommendations, historical performance data, and regulatory requirements [98]. A well-designed calibration schedule may include:
- Fixed or variable intervals based on calendar time, usage hours, or other relevant criteria
- Grace periods (e.g., annual calibrations performed every 365 days ± 10 days) to ensure timely maintenance
- Temporary extensions for critical testing scenarios, with strict limitations on duration and frequency
High-impact instruments like laboratory precision balances may require daily calibration, while less critical equipment like warehouse scales might be calibrated quarterly [98].
Experimental Protocols for Calibration Verification
Purpose: To verify the accuracy and precision of analytical balances and scales used in pharmaceutical quantification.
Materials and Reagents:
- Calibrated weights of known mass (traceable to NIST standards)
- Anti-static apparatus (if working with low masses)
- Clean gloves and forceps for handling weights
Methodology:
- Ensure the balance is level and located in an environment free from vibrations and air currents.
- Allow the balance to warm up according to manufacturer specifications.
- Perform internal calibration if available on the instrument.
- Place calibration weights covering the operational range (e.g., 1 mg, 10 mg, 100 mg, 1 g, 10 g).
- Record the displayed value for each weight.
- Compare displayed values against known masses and calculate percent error.
- Adjust the balance if errors exceed established tolerance limits (typically ±0.1% for analytical balances).
- Document all results in the instrument logbook including "As Found" and "As Left" conditions if adjustment was necessary.
Purpose: To ensure accurate pH measurements for dissolution testing, buffer preparation, and other critical pharmaceutical processes.
Materials and Reagents:
- Certified pH buffer solutions (typically pH 4.00, 7.00, and 10.00)
- Deionized water for rinsing
- Appropriate cleaning solutions for the electrode
Methodology:
- Allow buffers and electrode to reach the same temperature (document temperature).
- Rinse the electrode with deionized water and gently blot dry with lint-free tissue.
- Immerse the electrode in the first buffer solution (typically pH 7.00) and allow the reading to stabilize.
- Adjust the calibration control to match the known pH value of the buffer.
- Rinse the electrode and repeat the process with the second buffer (typically pH 4.00 or 10.00).
- For three-point calibration, repeat with the third buffer solution.
- Verify calibration by measuring a different buffer from those used in calibration.
- Calculate the slope and offset; acceptable slope is typically 95-105% with offset <±0.3 pH units.
- Document all calibration data including buffers used, temperatures, slope, and offset values.
Protocol for HPLC System Calibration
Purpose: To verify the accuracy of flow rate, composition, detector response, and injector precision in High Performance Liquid Chromatography systems.
Materials and Reagents:
- Certified reference standards for each analyte of interest
- Calibrated thermocouple (for column oven verification)
- Certified absorbance filters (for UV/Vis detector verification)
- Stopwatch or automated timer (for flow rate verification)
Methodology:
- Flow Rate Accuracy: Collect mobile phase from the pump outlet at various set flow rates (e.g., 0.5, 1.0, 2.0 mL/min) for a measured time period. Weigh the collected solution and calculate actual flow rate based on solvent density.
- Composition Accuracy: Prepare mixtures of two solvents (e.g., Water:MeOH at 90:10, 50:50, 10:90) and measure actual composition by refractive index or density.
- Detector Linearity: Inject known concentrations of reference standards and plot peak area versus concentration. Calculate correlation coefficient (R² > 0.995 typically acceptable).
- Injector Precision: Make six replicate injections of a standard solution and calculate %RSD for peak areas (<1.0% typically acceptable).
- Column Oven Temperature: Place calibrated thermocouple in column compartment and compare set temperature versus actual temperature at various set points.
- Wavelength Accuracy (for UV/Vis detectors): Measure certified absorbance filters and compare actual versus measured wavelengths.
Visualizing Calibration Workflows
Traceability Chain for Pharmaceutical Instruments
Calibration Decision Workflow
Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Calibration Procedures
| Reagent/Material | Function in Calibration | Application Context | Critical Specifications |
|---|---|---|---|
| Certified Calibration Weights [98] | Reference standard for mass measurements | Balance/scale calibration; formulation verification | NIST-traceable with documented uncertainty; material composition (stainless steel) |
| Certified pH Buffer Solutions [98] | Reference points for pH scale | pH meter calibration; dissolution media verification | NIST-traceable certifications; specified temperature dependence; stability data |
| Certified Absorbance Filters [98] | Wavelength and absorbance verification | UV/Vis spectrophotometer calibration | Certified absorbance values at specific wavelengths; material stability; surface quality |
| HPLC Reference Standards [98] | System performance qualification | HPLC/UHPLC calibration; method validation | Certified purity (>95%); stability data; structural confirmation |
| Density-Certified Solvents [97] | Volume verification via gravimetry | Liquid handler calibration; flow meter verification | Certified density values; purity specifications; lot-to-lot consistency |
| Photometric Calibration Dyes [97] | Volume verification in microtiter plates | Liquid handler performance verification | Optical stability; lot consistency; Beer's Law compliance; extinction coefficient certification |
| Conductivity Standards [98] | Reference for conductivity measurements | Conductivity meter calibration; water purity testing | NIST-traceable; temperature compensation specifications; stability data |
Instrument calibration and control represent a scientific discipline that demands rigorous methodology and strategic implementation. The selection of appropriate calibration technologies—whether gravimetric, photometric, or fluorometric—must be guided by specific application requirements, volume ranges, and regulatory constraints. By implementing robust calibration protocols aligned with ICH Q2(R1) guidelines and establishing comprehensive traceability chains back to national standards, pharmaceutical researchers can ensure the integrity of analytical data throughout the drug development lifecycle. As the instrument calibration services market continues to evolve—projected to reach $2.56 billion by 2029—the adoption of advanced technologies and data-driven calibration strategies will further enhance method performance consistency in pharmaceutical quantification research [99].
Ensuring Compliance and Comparability: Protocol Execution and Regulatory Documentation
In the highly regulated pharmaceutical industry, the validation of analytical methods is a critical process that ensures the quality, safety, and efficacy of drug products. This process generates a suite of essential documentation that serves as the foundation for regulatory compliance and scientific credibility. Validation Protocols, Reports, and Audit Trails form an interdependent system that provides documented evidence a method is fit for its intended purpose [100]. Within the context of analytical method validation for pharmaceutical quantification, these documents create a verifiable narrative from method conception and development through routine use and retirement [5] [17].
Regulatory bodies worldwide, including the FDA and EMA, mandate stringent requirements for these documents. Guidelines such as ICH Q2(R2) and ICH Q14 provide the framework for method development and validation, while 21 CFR Part 11 and EU GMP Annex 11 govern the electronic records and audit trails that ensure data integrity [5] [101] [102]. The alignment of these documents with the ALCOA+ principles—ensuring data is Attributable, Legible, Contemporaneous, Original, and Accurate, plus Complete, Consistent, Enduring, and Available—is now a non-negotiable standard [5] [102]. This guide provides a comparative analysis of these three pillars of essential documentation, underpinned by experimental data and structured protocols relevant to researchers and drug development professionals.
Comparative Analysis: Validation Protocols, Reports, and Audit Trails
The following table provides a structured comparison of the three core documentation types, highlighting their distinct purposes, key components, and regulatory focuses.
Table 1: Essential Documentation for Analytical Method Validation: A Comparative Overview
| Document Aspect | Validation Protocol | Validation Report | Audit Trail |
|---|---|---|---|
| Primary Purpose | Pre-approved plan describing the how and why of validation; a "contract" for the study [100]. | Formal record of what was done and the results; summarizes compliance with the protocol [100]. | Secure, time-stamped record of all changes to critical data; a "digital fingerprint" [101] [102]. |
| Core Components | Objective, Scope, Responsibilities, Detailed Procedure, Acceptance Criteria, Deviation Handling [100]. | Summary of results vs. acceptance criteria, Data tables, Deviations & investigations, Final conclusion [100]. | User ID, Timestamp, Action Taken (e.g., create, modify, delete), Reason for Change, Original and New Values [101] [103]. |
| Regulatory Focus | Ensures the study is scientifically sound and pre-defined, preventing bias (ICH Q2(R2), ICH Q14) [5]. | Provides evidence that the method is validated and the process was controlled; the final proof of compliance [17]. | Demonstrates data integrity and traceability per ALCOA+ (21 CFR Part 11, EU GMP Annex 11) [101] [102]. |
| Lifecycle Stage | Initiation and Planning | Closure and Summary | Ongoing Monitoring and Surveillance |
| Key Challenge | Defining scientifically rigorous and achievable acceptance criteria. | Accurately capturing and justifying any deviations from the protocol. | Managing data volume and ensuring timely, risk-based review [103]. |
Experimental Data and Performance Comparison
The effectiveness of a validation strategy is demonstrated through its experimental outcomes and its ability to withstand regulatory scrutiny. The data below compares different validation approaches and highlights common pitfalls in audit trail management.
Quantitative Validation Parameters and Acceptance Criteria
For an analytical method used to quantify a drug substance, key performance parameters must be experimentally verified against pre-defined acceptance criteria, as detailed in the validation protocol [17] [104].
Table 2: Experimental Validation Parameters for a Small Molecule Assay (e.g., HPLC-UV)
| Validation Parameter | Experimental Protocol Summary | Supporting Data & Acceptance Criteria | Regulatory Reference |
|---|---|---|---|
| Accuracy | Analyze replicates (n=6) at three concentration levels (80%, 100%, 120% of target) against a reference standard [17]. | Mean Recovery: 98.5 - 101.5%RSD: ≤ 2.0% | ICH Q2(R1) [104] |
| Precision | Repeatability: Analyze six independent preparations at 100% concentration.Intermediate Precision: Repeat on different day/different analyst [17]. | Repeatability RSD: ≤ 1.0%Intermediate Precision RSD: ≤ 2.0% | ICH Q2(R1) [17] |
| Linearity & Range | Prepare and analyze standard solutions at 5+ concentration levels across the claimed range (e.g., 50-150%) [17] [104]. | Correlation Coefficient (r): ≥ 0.998Y-Intercept: ≤ 2.0% of target response | ICH Q2(R1) [104] |
| Specificity | Chromatographically resolve the analyte peak from known impurities, degradants (stressed samples), and placebo matrix [17] [104]. | Resolution Factor: > 2.0Peak Purity: Passes PDA (Photodiode Array) criteria | ICH Q2(R1) [104] |
| Robustness | Deliberately vary key parameters (e.g., flow rate ±0.1 mL/min, column temp ±2°C) using a Design of Experiments (DoE) approach [5]. | All results remain within specified acceptance criteria for system suitability. | ICH Q2(R1) |
Comparison of Common Audit Trail Issues and Their Impact
Regulatory inspections frequently cite findings related to audit trails. The table below compares common issues, their implications, and corrective strategies based on real-world observations [103].
Table 3: Top Audit Trail Issues Found in Regulatory Inspections
| Common Issue | Regulatory Impact & Risk | Recommended Corrective Strategy |
|---|---|---|
| Audit Trails Not Reviewed | FDA 483 observation; potential data integrity citation [103]. | Implement a risk-based review procedure and SOP; assign clear responsibility; document reviews [103] [102]. |
| Editable Audit Trails | Severe compliance failure; warning letters or product holds [103]. | Validate systems for tamper-evident, immutable logs; restrict admin permissions [103]. |
| Missing/Incomplete Trails | Major GMP non-conformance; inability to reconstruct events [103]. | Upgrade legacy systems; validate that all GxP actions are captured [103]. |
| Inadequate Timestamp | Compromises reliability of the entire data sequence [103]. | Enforce automated time sync; disable manual clock changes; log time adjustments [103]. |
| Data Retention Issues | Inability to provide data during audits or investigations [103]. | Define retention policy in an SOP; validate backup/archive processes [103]. |
Detailed Experimental Protocols
Protocol for a Risk-Based Audit Trail Review
A proactive, risk-based approach to audit trail review is a key regulatory expectation for 2025 [102]. The following workflow can be formalized in a Standard Operating Procedure (SOP).
Diagram 1: Risk-based audit trail review workflow.
Title: Audit Trail Review Workflow
Procedure:
- System Categorization: Identify computerized systems handling GxP data (e.g., Chromatography Data Systems, LIMS). Categorize them as high, medium, or low risk based on their impact on product quality and patient safety [102].
- Review Frequency: Define the review schedule based on risk. For example, high-risk systems (e.g., electronic batch records) may require weekly or per-batch reviews, while low-risk systems may be reviewed quarterly [103] [102].
- Review Execution: The designated, trained reviewer examines the audit trail for critical data associated with a specific batch, study, or time period. The focus is on:
- Documentation and CAPA: The review, including the scope, date, reviewer, and any findings, must be documented. Any anomalies or confirmed violations must trigger a Corrective and Preventive Action (CAPA) to investigate the root cause and implement corrective measures [102].
Protocol for HPLC Method Validation
High-Performance Liquid Chromatography (HPLC) is a cornerstone technique for pharmaceutical quantification, and its validation is a frequent subject of regulatory assessment [17].
Diagram 2: HPLC method validation lifecycle.
Title: HPLC Method Validation Lifecycle
Procedure (as per ICH Q2(R1) and internal protocol):
- Specificity/SELECTIVITY:
- Objective: To demonstrate that the method can unequivocally quantify the analyte in the presence of potential interferents (impurities, degradants, matrix) [17] [104].
- Method: Inject blank (placebo), standard, sample, and samples spiked with known impurities and degradants (generated via forced degradation studies: heat, light, acid/base, oxidation).
- Acceptance Criteria: Peak purity index (from PDA detector) confirms a homogeneous analyte peak. Resolution between the analyte and all known interfering peaks is > 2.0 [17].
- Linearity and Range:
- Objective: To demonstrate a proportional relationship between analyte concentration and detector response [17] [104].
- Method: Prepare and analyze a minimum of 5 concentrations spanning the range from LOQ to 150% of the test concentration. Perform a linear regression analysis.
- Acceptance Criteria: Correlation coefficient (r) ≥ 0.998. The y-intercept is not significantly different from zero [104].
- Accuracy:
- Objective: To establish the closeness of test results to the true value.
- Method: Prepare and analyze replicate samples (n=3) at three concentration levels (80%, 100%, 120%) by spiking the placebo with a known amount of reference standard.
- Acceptance Criteria: Mean recovery between 98.0% and 102.0% for each level. RSD ≤ 2.0% [17].
- Precision:
- Repeatability: Analyze six independent sample preparations at 100% concentration by the same analyst on the same day. RSD should be ≤ 1.0% [17].
- Intermediate Precision (Ruggedness): Repeat the repeatability study on a different day, with a different analyst, and/or on a different instrument. The combined RSD from both studies should be ≤ 2.0% [17].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials required for the development and validation of a robust analytical method.
Table 4: Essential Research Reagents and Materials for Analytical Method Validation
| Item / Reagent Solution | Functional Role in Validation | Critical Quality Attributes |
|---|---|---|
| Pharmaceutical Reference Standard | Serves as the benchmark for identity, potency, and purity; used to prepare calibration standards for quantification [104]. | Certified purity (>98.5%), well-characterized structure (NMR, MS), low hygroscopicity, stability under storage conditions. |
| Chromatography Column | The stationary phase for HPLC/UHPLC separation; critical for achieving specificity and resolution [58]. | Reproducible lot-to-lot performance, particle size (e.g., 1.7-5µm), surface chemistry (C18, C8, etc.), stability at required pH. |
| HPLC-Grade Solvents & Buffers | Constitute the mobile phase; essential for reproducible retention times, peak shape, and detection [58]. | Low UV cut-off, minimal particulate matter, low acidity/basicity variability, prepared with high-purity water (e.g., 18.2 MΩ·cm). |
| System Suitability Standards | A ready-to-use solution to verify the performance of the total chromatographic system prior to testing [58]. | Contains key analytes to measure critical parameters (Theoretical Plates, Tailing Factor, Resolution) against pre-set criteria. |
| Stable Isotope Labeled Internal Standard | Used in LC-MS/MS bioanalysis to correct for variability in sample preparation, injection, and ionization [104]. | Co-elutes with analyte, has identical chemical behavior, is spectrally distinct (mass shift), and is highly pure. |
Validation Protocols, Reports, and Audit Trails are not isolated documents but interconnected components of a holistic quality system. The Validation Protocol ensures a method is developed with scientific rigor and predefined criteria. The Validation Report provides the definitive evidence that the method meets these criteria and is fit for its intended use. Finally, Audit Trails provide the continuous, verifiable record that the validated method remains in a state of control and that all generated data is reliable and intact [5] [100].
The regulatory landscape is continuously evolving, with a clear trend towards lifecycle management of analytical procedures (ICH Q14), greater integration of risk-based principles (ICH Q9), and an uncompromising focus on data integrity enforced through robust audit trails [5] [102]. For researchers and drug development professionals, mastering the creation, management, and review of this essential documentation is not merely a regulatory obligation but a fundamental scientific practice that underpins the development of safe and effective medicines.
In the pharmaceutical industry, the validation of analytical methods is not a single event but a comprehensive process that spans the entire lifespan of a drug product. This lifecycle approach ensures that methods remain fit-for-purpose, from initial development through commercial batch release and beyond. For researchers and drug development professionals, understanding this continuum is critical for maintaining regulatory compliance and ensuring data integrity throughout a product's market life.
The framework is inherently risk-based and phased, aligning method validation activities with the product's stage of development and the criticality of the quality decisions it supports. This guide objectively compares the performance, regulatory requirements, and operational demands of validation activities at each stage, providing a structured comparison to inform laboratory and quality decisions.
Pre-Approval Validation: Establishing Initial Fitness-for-Purpose
The pre-approval phase focuses on rigorously demonstrating that an analytical method is suitable for its intended purpose before it is used to generate data for regulatory submissions.
Core Experimental Protocols for Method Validation
A robust pre-approval validation is built on a series of defined experiments designed to challenge the method across its expected operating range [105].
The Comparison of Methods Experiment: This experiment is critical for assessing systematic error (inaccuracy). It involves analyzing a minimum of 40 different patient specimens by both the new (test) method and a carefully selected comparative method. These specimens should cover the entire working range of the method. The data is used to estimate the systematic error at medically important decision concentrations. The experiment should be conducted over a minimum of 5 different days to minimize bias from a single analytical run [105].
Statistical Analysis of Comparison Data: For data covering a wide analytical range, linear regression statistics are preferred. The slope (b), y-intercept (a), and standard deviation of the points about the line (s~y/x~) are calculated. The systematic error (SE) at a critical decision concentration (X~c~) is determined as SE = Y~c~ - X~c~, where Y~c~ = a + bX~c~. The correlation coefficient (r) is also calculated, with a value of 0.99 or larger indicating a wide enough data range for reliable slope and intercept estimates [105].
Data Quality Assurance: Prior to statistical analysis, data must undergo rigorous cleaning and quality assurance. This includes checking for duplications, managing missing data by setting exclusion thresholds (e.g., 50% completeness), and identifying anomalies that deviate from expected patterns. Establishing psychometric properties like reliability (e.g., Cronbach's alpha >0.7) is also crucial for standardized instruments [106].
Table 1: Key Pre-Approval Method Validation Experiments
| Validation Experiment | Primary Objective | Key Performance Metrics | Typical Acceptance Criteria |
|---|---|---|---|
| Comparison of Methods [105] | Estimate systematic error (inaccuracy) | Slope, Y-intercept, Standard Error of the Estimate (S~y/x~) | Slope close to 1.00; small Y-intercept |
| Precision Study | Determine random error (imprecision) | Standard Deviation, Coefficient of Variation (%CV) | %CV within pre-defined, clinically acceptable limits |
| Accuracy/Recovery | Assess ability to measure true value | Percent Recovery | Recovery close to 100% |
| Linearity & Range | Verify proportional response over analyte range | Correlation coefficient, R-squared | R² ≥ 0.99 (for wide range methods) [105] |
Regulatory Submission and the Review Process
The culmination of pre-approval activities is the regulatory submission, such as a Premarket Approval Application (PMA). The FDA's review is a multi-step process [107]:
- Filing Review: A 45-day administrative and limited scientific review to determine if the application is sufficiently complete to permit a substantive review.
- Substantive Review: An in-depth scientific, regulatory, and Quality System review by FDA personnel, during which the applicant may be notified of major or minor deficiencies.
- Panel Review: For first-of-a-kind devices, the PMA may be referred to an external advisory committee of experts for review and recommendation.
- Final Decision: FDA deliberates on all information, including the panel's recommendation, and notifies the applicant of its decision [107].
Failure to provide a complete and rigorous validation package, including all analytical data, can result in a refusal to file the application [107].
Post-Market Revalidation: Ensuring Ongoing Control
Once a product is marketed, the focus shifts to monitoring method performance and ensuring it remains valid in the face of process changes, new product variants, and evolving equipment.
Triggers and Protocols for Revalidation
Revalidation is not automatic; it is driven by specific events. The protocols are often streamlined compared to pre-approval studies, focusing on the aspects most likely to be impacted by the change.
Post-Approval Studies (PAS): The FDA may require a Post-Approval Study as a condition of device approval to ensure continued safety and effectiveness. The FDA's Post-Approval Studies Program ensures these studies use valid scientific methodologies and are conducted effectively [108]. A public database tracks the status of these studies [108].
Change Control and Periodic Review: As part of a computerized system lifecycle, regulated companies must implement robust change control and periodic review processes. Any change to a validated system—be it in the software, hardware, or intended use—must be assessed for its potential impact on the validated state and performance of the analytical method, triggering revalidation if needed [109].
Continuous Process Verification: Modern validation practices emphasize using real-time data to monitor manufacturing processes throughout their lifecycle. This involves implementing Process Analytical Technology (PAT) and using statistical tools for ongoing trend analysis, which can inform the need for analytical method revalidation [110].
Table 2: Comparison of Pre-Approval Validation vs. Post-Market Revalidation
| Aspect | Pre-Approval Validation | Post-Market Revalidation |
|---|---|---|
| Regulatory Driver | PMA Submission & Approval [107] | Post-Approval Studies (PAS), Change Control [108] [109] |
| Scope | Full validation of all performance parameters | Targeted, risk-based; often focuses on parameters affected by a specific change |
| Data Volume | Extensive, from a wide range of deliberately selected samples [105] | Ongoing, often from routine production and quality control testing |
| Statistical Rigor | Comprehensive (e.g., linear regression, 40+ samples) [105] | Trend analysis, statistical process control |
| Primary Goal | Demonstrate fitness-for-purpose for regulatory approval | Ensure continued control and detect drift or performance change |
Comparative Analysis: Performance Data Across the Lifecycle
A direct comparison of validation data generated pre- and post-approval for the same method can provide powerful evidence of its robustness.
Table 3: Illustrative Performance Data Comparison for a Hypothetical HPLC Assay
| Performance Parameter | Pre-Approval Validation Data | Post-Market Revalidation (3-Year Data) |
|---|---|---|
| Accuracy (% Recovery) | 99.5% - 101.0% | 98.8% - 101.5% |
| Precision (%CV) | 0.8% | 1.2% |
| Linearity (R²) | 0.9995 | 0.9989 |
| System Suitability Tailing Factor | 1.0 - 1.2 | 1.0 - 1.3 |
| Number of Analyses (n) | 150 (deliberate range) | ~5,000 (routine QC) |
Data Interpretation: The table illustrates typical trends observed over a method's lifecycle. The slight broadening of the accuracy range and a small increase in %CV in the post-market data are common and can be attributed to long-term variability introduced by multiple analysts, equipment maintenance events, and environmental fluctuations. The consistency of the linearity and system suitability parameters demonstrates the method's fundamental robustness. The large sample size of post-market data provides a high degree of confidence in the ongoing performance of the method.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental for executing the validation protocols described in this guide, particularly for chromatographic assays.
Table 4: Essential Research Reagent Solutions for Analytical Validation
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Serves as the benchmark for quantifying the analyte; essential for accuracy, linearity, and specificity studies. | High Purity (>98.5%), Certified and Traceable, Appropriate Stability |
| System Suitability Mixture | A prepared sample containing the analyte and key potential impurities; used to verify chromatographic system performance before a validation run. | Well-characterized resolution between peaks, Reproducible retention times |
| Forced Degradation Samples | Samples of the drug substance/product exposed to stress conditions (heat, light, acid, base, oxidation); used to demonstrate specificity and stability-indicating properties. | Generation of relevant degradants, Demonstration of method selectivity |
| Quality Control (QC) Samples | Samples with known analyte concentrations, prepared in the biological matrix or placebo; used to monitor accuracy and precision during the validation. | Prepared at Low, Mid, and High concentrations within the range, Homogeneous and Stable |
| Extraction Solvents & Mobile Phases | Used in sample preparation and chromatographic separation; their quality and consistency are vital for robust method performance. | HPLC-grade or higher, Specified pH and composition, Filtered and degassed |
Integrated Workflow: From Pre-Approval to Post-Market
The following diagram visualizes the complete lifecycle management workflow, integrating the key stages, activities, and decision points discussed in this guide.
Analytical Method Lifecycle Workflow
A seamless, well-documented lifecycle management strategy for analytical methods is a cornerstone of modern pharmaceutical quality systems. The transition from pre-approval validation to post-market revalidation is not a handoff but a continuum of control. By adopting a proactive, risk-based approach—supported by rigorous experimental data and comparative monitoring—organizations can ensure their analytical methods remain validated, compliant, and capable of supporting the quality, safety, and efficacy of drug products throughout their entire market life. This not only fulfills regulatory expectations but also builds a robust scientific foundation for reliable patient care.
Comparative Analysis of Validation Approaches Across Different Drug Modalities
The pharmaceutical landscape is undergoing a transformative shift, with novel therapeutic modalities accounting for an estimated 60% ($197 billion) of the total pharmaceutical pipeline value in 2025 [111]. This diversification beyond traditional small molecules introduces profound challenges for analytical method development and validation. This comparative guide examines the distinct validation approaches required across major drug modalities—from established monoclonal antibodies to emerging cell and gene therapies—synthesizing current regulatory expectations, technological advancements, and experimental protocols. The analysis reveals that traditional one-size-fits-all validation frameworks are increasingly inadequate for complex biologics and advanced therapy medicinal products (ATMPs), necessitating modality-specific strategies that incorporate Quality by Design (QbD), real-time monitoring, and advanced multivariate controls [41] [112] [5].
The Evolving Therapeutic Landscape and Validation Imperatives
The pharmaceutical pipeline has diversified dramatically, with new modalities now dominating developmental portfolios. According to BCG's 2025 analysis, antibodies (including mAbs, ADCs, and BsAbs), recombinant proteins (notably GLP-1 agonists), and nucleic acid-based therapies demonstrate the most robust growth, while some gene and cell therapies face clinical and manufacturing hurdles [111]. This modality diversification fundamentally alters validation requirements because:
- Complexity of Critical Quality Attributes (CQAs): Traditional small molecules typically require monitoring of chemical purity and potency, whereas biologics demand characterization of higher-order structure, post-translational modifications, and charge variants [31] [34].
- Manufacturing Scale Differences: Monoclonal antibodies are produced at commercial scale, whereas many ATMPs involve patient-specific manufacturing with limited batch sizes, reducing opportunities for traditional process qualification [112].
- Product Stability Concerns: Modalities like radiopharmaceuticals have inherent stability challenges due to radionuclide decay, requiring specialized analytical methods and rapid release testing [112].
Regulatory frameworks have evolved in response, with ICH Q2(R2) and Q14 guidelines emphasizing lifecycle management of analytical procedures and encouraging more flexible, science-based validation approaches [5].
Comparative Analysis of Validation Requirements Across Modalities
Table 1: Validation Approach Comparison Across Major Drug Modalities
| Drug Modality | Primary CQAs | Key Analytical Techniques | Validation Challenges | Recommended Approach |
|---|---|---|---|---|
| Small Molecules | Purity, potency, dissolution, related substances | HPLC/UHPLC, LC-MS/MS, NMR [31] [34] | Method robustness, impurity profiling | Traditional validation per ICH Q2(R1), with QbD principles for complex APIs [5] |
| Monoclonal Antibodies & Biologics | Protein concentration, aggregation, charge variants, post-translational modifications | icIEF, HRMS, SEC-MALS, ELISA, cell-based assays [31] [5] [34] | Multi-attribute method development, product heterogeneity | Holistic quality control strategy with MAM, extended characterization studies [5] |
| Cell & Gene Therapies (ATMPs) | Identity, potency, viability, transduction efficiency, purity, safety (sterility, endotoxin) | qPCR, flow cytometry, viability assays, sequencing [111] [112] [5] | Limited shelf life, patient-specific manufacturing, biological variability | Risk-based approach with DoE, real-time potency assays, process parametric release [112] [5] |
| Antibody-Drug Conjugates (ADCs) | Drug-to-antibody ratio (DAR), unconjugated drug & antibody, aggregation | HIC-HPLC, LC-MS, SEC, potency assays [111] | Characterization of heterogeneous mixture, in vivo stability | Orthogonal method combination, characterization of critical structure-function relationships [111] [5] |
| Radiopharmaceuticals | Radiochemical purity & identity, specific activity, radionuclide purity | Gamma counter, TLC, HPLC with radiodetection [112] | Radiolysis, time constraints due to decay, environmental factors | DoE to understand multivariate interactions, rapid methods, specialized facility controls [112] |
Experimental Protocols for Advanced Modality Validation
Design of Experiments (DoE) for Complex Modalities
For emerging modalities like ATMPs and radiopharmaceuticals characterized by multivariate interactions, traditional one-factor-at-a-time (OFAT) validation approaches are insufficient. A recommended DoE protocol involves [112]:
Risk Assessment: Identify potential critical process parameters (CPPs) and their potential impact on CQAs through prior knowledge and initial risk analysis.
Experimental Design: Select appropriate statistical design (e.g., fractional factorial for screening, response surface methodology for optimization) to simultaneously vary multiple parameters.
Model Development: Conduct controlled experiments to generate data for building mathematical models that describe relationships between CPPs and CQAs.
Design Space Establishment: Define the multidimensional combination and interaction of input variables demonstrated to provide quality assurance.
Control Strategy: Implement monitoring and control systems to ensure processes remain within the design space.
This approach is particularly valuable for cell therapy processes where interactions between parameters like seeding density, media composition, and bioreactor conditions can significantly impact critical quality attributes like cell viability and potency [112].
Multi-Attribute Methods (MAM) for Biologics
MAM represents a paradigm shift from monitoring individual attributes to simultaneously measuring multiple attributes, often using liquid chromatography-mass spectrometry (LC-MS). A typical implementation protocol includes [5]:
Method Scoping: Identify product quality attributes amenable to LC-MS detection (e.g., sequence variants, post-translational modifications, oxidation, deamidation).
Sample Preparation: Develop optimized digestion protocols (e.g., using trypsin/Lys-C) and purification steps to ensure reproducible peptide maps.
LC-MS Method Development: Optimize chromatographic separation and mass spectrometric detection conditions to resolve and identify peptides of interest.
Data Processing Pipeline: Establish automated software workflows for peptide identification, peak integration, and relative quantification.
Validation: Demonstrate method specificity, accuracy, precision, linearity, and range for each monitored attribute according to ICH Q2(R2) and Q14 guidelines.
MAM implementation enables real-time release testing for certain biologics by providing comprehensive product quality assessment in a single assay, significantly reducing analytical time and resources [5].
Visualization of Method Development Workflows
Analytical Quality by Design (AQbD) Workflow
Figure 1: AQbD Method Development Workflow
Multimodal AI for Drug Combination Validation
Figure 2: Multimodal AI for Combination Therapy Prediction
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents and Analytical Solutions for Method Validation
| Category | Specific Solutions/Techniques | Primary Applications | Function in Validation |
|---|---|---|---|
| Separation Techniques | UHPLC, HIC-HPLC, SEC, icIEF [31] [5] [34] | Purity analysis, charge variant separation, impurity profiling | Quantify primary quality attributes, establish specificity and resolution |
| Spectroscopic Methods | HRMS, NMR, LC-MS/MS [31] [5] [34] | Structural elucidation, metabolite identification, sequence confirmation | Confirm identity, characterize impurities and degradation products |
| Bioanalytical Assays | qPCR, flow cytometry, cell-based potency assays [112] [5] | Potency determination, viral vector quantification, cell characterization | Measure biological activity, establish dose-response relationships |
| Data Integrity Systems | CDS, LIMS with ALCOA+ compliance [41] [5] | All regulated analytical processes | Ensure data reliability, traceability, and regulatory compliance |
| Process Analytical Technology | In-line spectroscopy, sensors for real-time monitoring [41] [5] | Continuous manufacturing, real-time release testing | Enable parametric release, continuous quality verification |
The comparative analysis reveals that validation strategies must be tailored to the specific scientific and regulatory demands of each drug modality. While small molecules continue to benefit from well-established ICH guidelines, complex modalities require increasingly sophisticated approaches incorporating QbD, DoE, and digital transformation. The emergence of multimodal AI platforms and real-time release testing represents the future of analytical validation, enabling more efficient development of innovative therapies while maintaining rigorous quality standards [5] [113]. As the pharmaceutical landscape continues to evolve, validation approaches must balance regulatory compliance with scientific innovation to ensure patient safety and product efficacy across all therapeutic modalities.
Analytical method transfer is a critical, documented process that qualifies a receiving laboratory to use an analytical test procedure that was originally developed and validated in another laboratory (the transferring or sending unit) [114]. This formal introduction of a validated method into a designated laboratory ensures it can be used for the same purpose for which it was originally developed, serving as a cornerstone of pharmaceutical quality control and regulatory compliance [115]. The fundamental objective is to verify through documented evidence that the method works equivalently across different sites or laboratories, consistently generating comparable data that meets all pre-defined acceptance criteria [116] [115].
In today's global pharmaceutical landscape, method transfers are indispensable for enabling critical medications to reach international markets. They present significant challenges due to staggered regulatory submission timelines, differing health authority requirements (such as FDA, EMA, and ANVISA), and varied importation standards and testing requirements across countries [116]. In some jurisdictions including China, Russia, and Mexico, testing on imported medicines must be performed by government agencies or government-approved laboratories, while other countries like Brazil, Peru, Chile, Argentina, Korea, and Japan require local testing [116]. These regulatory complexities make robust, well-documented transfer protocols essential for ensuring pharmaceutical product quality and consistency worldwide.
Regulatory Framework and Guidance
Global Regulatory Expectations
Method transfer protocols must align with diverse international regulatory requirements. The U.S. Food and Drug Administration (FDA) incorporates analytical method transfer within its broader guidance on method development, validation, and lifecycle management [116]. FDA recommends performing comparative studies to evaluate accuracy and precision while assessing inter-laboratory variability across originating and receiving laboratories [116]. For stability-indicating methods, the agency recommends that both sites analyze forced degradation samples or samples containing pertinent product-related impurities [116].
The European Medicines Agency (EMA), through the European Commission, Health and Consumers Directorate-General, outlines that a method-transfer protocol should include identification of relevant test methods and testing to be performed, standards and samples to be tested, special transport and storage conditions, and acceptance criteria consistent with method validation and International Council for Harmonization (ICH) expectations [116].
Brazil's ANVISA has distinct expectations, considering a method transfer successful when precision, specificity, and linearity are evaluated [116]. Additional guidance documents published by organizations such as the International Society for Pharmaceutical Engineering (ISPE), the United States Pharmacopeia (USP), and the World Health Organization (WHO) further contribute to the global regulatory tapestry [116].
United States Pharmacopeia (USP) Standards
The USP provides comprehensive guidance on analytical method transfer in its general information chapter <1224>, which discusses comparative, co-validation, and revalidation approaches to method-transfer testing [116] [114]. USP recommends that testing be performed on homogeneous lots of target material to minimize sample variability [116]. The organization defines transfer as "the documented process that qualifies a laboratory (a receiving unit) to use an analytical test procedure that originates in another laboratory (the transferring unit also named the sending unit)" [114].
USP also provides statistical guidance in chapter <1010>, "Analytical Data—Interpretation and Treatment," which offers basic statistical approaches for evaluating data, comparing methods, identifying statistical outliers, and providing a review of the mathematical foundation for assessing variability, accuracy, confidence intervals, t-tests, and outlier tests [114] [117]. This chapter forms the basis for many statistical approaches used in method transfer studies.
Types of Method Transfer Approaches
Comparative Testing
Comparative testing represents the most common transfer approach, where both the originating and receiving laboratories perform analysis on the same homogeneous material using the validated method [115]. The results are then statistically compared to demonstrate equivalence. According to ISPE recommendations, this ideally involves at least two analysts at each laboratory independently analyzing three lots of product in triplicate, resulting in 18 different executions of the assay method [116]. This comprehensive approach provides robust data for assessing inter-laboratory variability.
Co-validation
Co-validation occurs when the receiving laboratory participates in the validation of the method, often by performing part of the validation, such as the intermediate precision section, alongside the originating laboratory [114] [115]. In this approach, validation activities take place at both sites simultaneously, with the key differentiator being the determination of lack of bias between the two laboratories [114]. This approach is particularly valuable when methods are being transferred during the later stages of development or early validation.
Method Verification and Revalidation
Method verification or revalidation involves the receiving laboratory performing a complete or partial validation of the method to demonstrate their capability to execute it properly [114] [115]. This approach is often employed when significant changes have been made to the method or when transferring older methods that may require additional demonstration of suitability in the new environment.
Transfer Waivers
Under specific circumstances, a formal transfer process may be waived [114]. This typically applies when the receiving laboratory has extensive prior experience with the method or similar methods, or when the method is compendial and sufficiently straightforward to implement without extensive comparative studies. Justification for waivers must be thoroughly documented.
Table 1: Comparison of Method Transfer Approaches
| Transfer Type | Key Characteristics | When to Use | Data Requirements |
|---|---|---|---|
| Comparative Testing | Both labs test same homogeneous samples; results statistically compared | Standard approach for validated methods | Multiple analysts, multiple lots, replicated testing |
| Co-validation | Receiving lab participates in method validation | Transfer during method development/validation | Validation data from both laboratories |
| Revalidation | Receiving lab partially or fully revalidates method | Significant changes to method or equipment | Complete or partial validation data set |
| Transfer Waiver | Formal transfer process omitted | Extensive prior experience or compendial methods | Documented justification |
Experimental Design and Statistical Approaches
Statistical Methods for Data Comparison
The comparison of analytical procedures forms the foundation of method transfer, requiring robust statistical approaches to demonstrate equivalence [117]. The USP <1010> guidance provides basic statistical approaches for evaluating data and comparing methods, focusing primarily on separate tests for accuracy and precision [114] [117]. However, this approach presents challenges due to the interdependence of accuracy and precision [117].
For assessing lack of bias or comparison of means, common statistical tests include the t-test (when comparing two groups) or ANOVA (when comparing more than two groups), typically using 90% or 95% confidence intervals [114]. The comparison of precision can be performed using an F-test for two groups or ANOVA for more than two groups [114]. Equivalence testing between laboratories is often conducted using the Two One-Sided T-test (TOST) approach, which establishes that the means from two laboratories are equivalent within a specified margin [114].
Visual assessments of data using plots such as Bland-Altman plots can also provide valuable insights into method comparability [114]. More advanced approaches include the use of intraclass correlation coefficients or concordance correlation coefficients to assess agreement between laboratories [114].
Total Error Approach
Recent advancements in statistical approaches for method transfer have introduced the total error approach, which combines both accuracy and precision components into a single criterion [117]. This method overcomes the difficulty of allocating separate acceptance criteria between precision and bias by defining an allowable out-of-specification (OOS) rate at the receiving laboratory [117]. The total error approach can be implemented using simulation software and provides a more comprehensive assessment of method performance between laboratories [117].
Experimental Design Considerations
Successful method transfer requires careful experimental design planning. As noted in a position paper on the transfer of analytical methods, a better overall prediction of consistent longer-term method performance is achieved by testing one or two representative and/or range-challenging batches with an increased number of testing setups rather than performing fewer setups with an increased number of batches [116]. This approach provides more robust data for assessing inter-laboratory variability.
The design must also consider the number of analysts involved (typically at least two per laboratory), the number of replicates, and the use of homogeneous sample materials to minimize variability unrelated to method performance [116] [114]. The experimental design should be documented in a pre-approved protocol with clearly defined acceptance criteria [116] [114].
Method Transfer Workflow
Method Transfer Kits: A Standardized Approach
Concept and Components
Method Transfer Kits (MTKs) represent an innovative approach to standardizing the transfer process across global sites [116]. These kits contain centrally-managed batches of representative materials (including matrix considerations such as strengths and impurity profiles) along with pre-defined and approved protocols for use in method transfers throughout the product lifecycle [116]. The primary objective of MTKs is to provide more control over sample variability, allowing focus on assessment of method performance between originating and receiving laboratories, regardless of when the transfer occurs [116].
A typical MTK includes representative materials to facilitate comparison of method performance across multiple laboratories during the product lifecycle [116]. Additionally, it defines the setups, conditions, and acceptance criteria for the given batch across the originating and all receiving laboratories [116]. The kits incorporate pre-approved originating and receiving laboratory protocols that are leveraged for the first transfer and all future transfers [116].
Establishment and Implementation
Establishing an effective MTK requires careful planning and consideration of multiple factors. The process begins with determining the sample numbers required per kit and the total number of kits needed based on projected method transfers [116]. For example, in a hypothetical small-molecule drug product scenario, 140 tablets may be required for training and six setups at one receiving site when multiple replicates for each setup and testing in both originating and receiving sites are considered [116].
Storage conditions represent another critical consideration for MTKs. Generally, to provide the greatest long-term stability, more conservative packaging and storage conditions are applied to MTKs than to commercial products [116]. For drug products normally stored at ambient temperatures, MTK product might be packaged in glass bottles with secondary laminated foil liners for additional light/moisture protection and stored under refrigerated conditions [116]. For normally refrigerated products, frozen or deep-frozen storage may extend shelf life [116].
Table 2: Method Transfer Kit Components and Specifications
| Component | Description | Purpose | Special Considerations |
|---|---|---|---|
| Representative Materials | Centrally-managed batches representing different strengths and impurity profiles | Provide consistent reference materials across all transfers | Must cover product variability; may require bracketing strategy for multiple doses |
| Pre-approved Protocols | Documented procedures with predefined acceptance criteria | Standardize testing approach across laboratories | Must align with regulatory requirements (FDA, EMA, USP, WHO) |
| Stability Data | Supporting data for material stability under storage conditions | Define usable shelf life for transfer activities | Stability period defined when material comparable to first originating lab data set |
| Degraded Samples | Representative degraded samples or materials for forced degradation | Demonstrate correct results throughout product lifecycle | Opportunity for receiving lab to discuss impurities with subject matter experts |
| Storage System | Conservative packaging and storage conditions | Extend shelf life and maintain material integrity | Often more conservative than commercial product storage |
Special Considerations for Large Molecules
Method transfer for biologics and large molecules presents additional challenges due to their inherent instability and complexity [116]. Special considerations are required for materials that change during routine storage, including large molecules, peptides, and inherently unstable small molecules, when more conservative storage conditions may not be possible [116]. The degradation rate itself, depending on severity, could pose problems when comparing mean results for method transfer and might be so substantial that the MTK approach may not add value without alternative comparison options [116].
For complex biologics, the specification may allow for an end-of-shelf-life specification that permits a change in the molecule's heterogeneity while still maintaining its efficacy [116]. In such scenarios, the receiving laboratory may require additional comparative strategies beyond standard MTK approaches.
Essential Research Reagent Solutions
Successful method implementation requires carefully selected reagents and materials that ensure reproducibility and reliability. The following research reagent solutions represent essential components for robust method transfer:
Table 3: Essential Research Reagent Solutions for Method Transfer
| Reagent/Material | Function | Criticality for Transfer |
|---|---|---|
| Homogeneous Reference Standards | Provides consistent analyte for method qualification | High: Essential for demonstrating method performance consistency |
| System Suitability Mixtures | Verifies chromatographic system performance before analysis | High: Powerful tool for troubleshooting method discrepancies |
| Qualified HPLC Columns | Ensures separation consistency between laboratories | High: Column variability significantly impacts method reproducibility |
| Critical Reagents | Antibodies, enzymes, or specialized chemicals required for analysis | High: Must be qualified and available at both originating and receiving labs |
| Impurity Standards | Reference materials for impurity identification and quantification | Medium-High: Essential for stability-indicating methods |
| Stable Isotope-Labeled Analytes | Internal standards for mass spectrometry-based methods | Medium-High: Critical for accurate quantification in complex matrices |
Best Practices for Successful Transfer
Pre-Transfer Assessment and Planning
Comprehensive pre-transfer assessment forms the foundation for successful method transfer [114]. This includes conducting a thorough gap analysis or audit function to evaluate the receiving laboratory's current ability to implement the method [114]. The assessment should cover laboratory environment, equipment (hardware and software), temperature and humidity controls, and equipment placement [114]. Identifying mismatches between requirements and capabilities before transfer prevents complications and potential transfer failures [114].
Feasibility runs or practice runs using the protocol help ensure laboratory readiness, operator training, and procedure comprehension [114]. These preliminary studies also protect against transferring methods that are not well understood or poorly performing [114]. Additionally, project planning must address material availability, timeline management, resource alignment, and communication strategies between sites [114].
Documentation and Training
A comprehensive document package is essential for effective knowledge transfer [114]. For methods in development, this includes a draft procedure with extensive development notes; for established methods, documentation should include development reports, qualification reports, and technical reports [114]. The method transfer protocol itself must be pre-approved and include identification of relevant test methods, testing to be performed, standards and samples, special conditions, and acceptance criteria [116] [114].
Proper analyst training ensures laboratory operators are sufficiently familiar with all scientific aspects of the method [115]. This is particularly important when transfers occur between sites with different native languages, potentially requiring translation of method procedures [115]. Training should not be rushed, as inadequate training represents a significant source of transfer delays and failures [114].
Post-Transfer Monitoring
The post-transfer monitoring phase is frequently overlooked but essential for long-term method success [114]. This involves continuous monitoring of method and laboratory performance after successful transfer implementation [114]. When multiple laboratories perform the same method, ongoing comparison of data trends and out-of-specification rates helps identify potential method drift or performance issues before they impact product quality [114].
Best Practices Implementation Sequence
Robust method transfer protocols represent a critical component of pharmaceutical quality systems, ensuring analytical methods perform consistently and reproducibly across different laboratories and global sites. As regulatory landscapes evolve and pharmaceutical supply chains become increasingly globalized, standardized approaches such as Method Transfer Kits offer significant advantages in efficiency, consistency, and regulatory compliance.
The successful implementation of method transfer protocols requires careful attention to regulatory requirements, statistical approaches, experimental design, and knowledge transfer processes. By adopting a systematic approach that incorporates comprehensive pre-transfer assessment, thorough documentation, appropriate statistical analysis, and post-transfer monitoring, pharmaceutical organizations can ensure method reproducibility while maintaining data integrity and product quality throughout the method lifecycle.
Future advancements in method transfer will likely continue emphasizing lifecycle approaches aligned with emerging regulatory frameworks, with increasing application of digital technologies and data analytics to further enhance transfer efficiency and reliability. Regardless of technological evolution, the fundamental principle remains unchanged: method transfer must demonstrate through documented evidence that analytical procedures perform equivalently across laboratories, ensuring consistent product quality and patient safety worldwide.
For researchers and scientists in drug development, audit readiness is not a periodic event but a fundamental characteristic of a robust quality culture. It demonstrates that every piece of data generated can withstand the intense scrutiny of regulatory inspections, proving that products are safe, effective, and of high quality. At the heart of this readiness lies the rigorous validation of analytical methods, which provides the scientific evidence that the procedures used to quantify pharmaceuticals are reliable and reproducible. This guide explores the critical parameters of method validation, compares foundational analytical techniques, and outlines the experimental protocols that form the bedrock of audit-ready compliance and uncompromised data integrity.
Understanding the Regulatory Framework: GxP and Data Integrity
Operating in a pharmaceutical research and development environment requires adherence to a comprehensive regulatory framework often referred to as GxP—an umbrella term for the "Good Practice" quality guidelines that ensure products are safe, effective, and high-quality throughout their lifecycle [118].
- Good Laboratory Practice (GLP): Covers non-clinical laboratory studies.
- Good Manufacturing Practice (GMP): Governs the production and testing of active pharmaceutical ingredients (APIs) and finished products.
- Good Clinical Practice (GCP): Provides standards for designing, conducting, and reporting clinical trials [118].
Underpinning all GxP regulations is the principle of data integrity. Regulatory agencies enforce the ALCOA+ principles, which mandate that all data must be [119] [118] [120]:
- Attributable: Who generated the data and when.
- Legible: Can the data be read and understood?
- Contemporaneous: Recorded at the time of the activity.
- Original: The source data or a certified copy.
- Accurate: No errors or editing without documented corrections.
- Complete: All data is included, with no omissions.
Core Principles of Analytical Method Validation
Analytical method validation is a documented process that proves a testing procedure is suitable for its intended purpose, such as quantifying an API or detecting impurities [15] [1]. It provides the evidence that the method consistently produces reliable and reproducible results, forming a critical part of any regulatory submission [29].
The International Council for Harmonisation (ICH) guideline Q2(R1) provides the globally accepted standard for validating analytical procedures. The following parameters must be evaluated and documented [15] [29] [104].
Analytical Method Validation Parameters
| Validation Parameter | Definition | Experimental Approach | Typical Acceptance Criteria |
|---|---|---|---|
| Accuracy | Closeness of test results to the true value [15] [1]. | Recovery studies by spiking a known amount of analyte into a sample matrix (e.g., placebo) [15] [29]. | Recovery of 98-102% for API assays [29]. |
| Precision | The degree of agreement among individual test results when the procedure is applied repeatedly to multiple samplings [15]. | Relative Standard Deviation (RSD) < 2% for assay [15]. | |
| Specificity | Ability to assess the analyte unequivocally in the presence of other components like impurities, degradants, or excipients [15] [29]. | Analyze sample with and without potential interferences (e.g., stressed samples, placebo) [29]. | Analytes peak is resolved from all other peaks; no interference from blank [29]. |
| Linearity | The ability of the method to obtain test results proportional to the concentration of the analyte [15] [29]. | Analyze a minimum of 5 concentrations across a specified range [15] [29]. | Correlation coefficient (R²) ≥ 0.999 [29]. |
| Range | The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the method has suitable levels of precision, accuracy, and linearity [15]. | Derived from linearity and precision studies [15]. | Typically 80-120% of test concentration for assay [15]. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters [15]. | Deliberately changing parameters (e.g., flow rate ±0.1 mL/min, temperature ±2°C, mobile phase pH ±0.2) [15]. | System suitability criteria are still met despite variations [15]. |
| LOD & LOQ | Limit of Detection (LOD): Lowest amount of analyte that can be detected. Limit of Quantitation (LOQ): Lowest amount that can be quantified with acceptable accuracy and precision [15] [1]. | Based on signal-to-noise ratio (e.g., 3:1 for LOD, 10:1 for LOQ) or standard deviation of the response [15]. | Typically determined from baseline noise of a blank sample [15]. |
Experimental Protocols for Key Validation Parameters
This section provides detailed methodologies for establishing critical validation parameters, ensuring experiments are conducted consistently and generate reliable, audit-ready data.
Protocol for Determining Accuracy and Precision
Objective: To demonstrate that the method yields results that are both correct (accurate) and repeatable (precise) over a series of measurements.
Materials:
- Reference standard of the analyte (e.g., API) of known purity.
- Appropriate placebo matrix (excluding the analyte).
- Volumetric flasks, pipettes, and calibrated analytical balance.
- Validated analytical instrument (e.g., HPLC system).
Procedure:
- Preparation of Solutions: Prepare a minimum of three concentration levels (e.g., 80%, 100%, 120% of target concentration) in triplicate by spiking the API into the placebo matrix.
- Sample Analysis: Analyze all nine samples using the validated method.
- Data Analysis:
- Accuracy: Calculate the percentage recovery for each sample using the formula:
(Measured Concentration / Theoretical Concentration) * 100. Report the mean recovery for each level. - Precision: For the 100% level samples, calculate the Relative Standard Deviation (RSD) of the measured concentrations.
- Accuracy: Calculate the percentage recovery for each sample using the formula:
Protocol for Specificity and Forced Degradation Studies
Objective: To prove the method can distinguish the analyte from other components and is stability-indicating.
Materials:
- API, finished product, and placebo.
- Reagents for stress conditions: Acid (e.g., 0.1M HCl), Base (e.g., 0.1M NaOH), Oxidizing agent (e.g., 3% H₂O₂), and Heat (e.g., 60°C oven).
Procedure:
- Stress Samples: Subject the finished product to various stress conditions to induce degradation (e.g., heat for 24 hours, acid/base for 1 hour).
- Analysis: Analyze the following:
- Untreated finished product.
- Stressed finished product samples.
- Placebo.
- Reference standard.
- Data Analysis: Examine chromatograms to ensure:
- The analyte peak is pure and unaffected by placebo.
- Degradant peaks are resolved from the analyte peak (resolution > 2.0 is typically desirable).
- The analyte is accurately measured in the presence of degradants.
Method Validation Lifecycle
Comparative Analysis of Analytical Techniques
Choosing the right analytical technique is foundational to method development. The selection depends on the drug's properties, the required sensitivity, and the specific quality attribute being measured [1] [29]. The table below compares common techniques used for pharmaceutical quantification.
Comparison of Analytical Methods
| Technique | Best Suited For | Key Advantages | Key Limitations | Typical Data Output |
|---|---|---|---|---|
| High-Performance Liquid Chromatography (HPLC) | Assay, impurity profiling, dissolution testing [29]. | High selectivity, can separate complex mixtures, quantitative accuracy [29]. | Method development can be complex; requires skilled analysts [1]. | Chromatogram with retention times and peak areas/heights. |
| Gas Chromatography (GC) | Volatile and semi-volatile compounds, residual solvents [29]. | Excellent resolution for volatile analytes, highly sensitive detectors (e.g., FID, MS) [29]. | Limited to thermally stable, volatile compounds; derivatization often needed [29]. | Chromatogram similar to HPLC. |
| UV-Vis Spectrophotometry | Quantitative assay of APIs in dissolution or content uniformity [15]. | Simple, fast, cost-effective, high precision for direct analysis [29]. | Low selectivity; requires the analyte to be a chromophore [29]. | Spectrum with absorbance at specific wavelengths. |
| Titration | Quantification of APIs or excipients with ionizable functional groups [15]. | Absolute quantification, no reference standard needed, robust and simple [15]. | Low specificity; not suitable for complex mixtures or impurities [15]. | Volume of titrant used to reach endpoint. |
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful and validated analytical method relies on high-quality, well-documented materials and reagents. The following table details essential items for a typical HPLC-based analytical method.
Essential Materials for HPLC Method Validation
| Item | Function & Importance | Key Considerations |
|---|---|---|
| Reference Standard | Serves as the benchmark for identifying and quantifying the analyte [104]. | Must be of the highest available purity and well-characterized (e.g., USP, EP standards) [104]. |
| Chromatography Column | The heart of the separation, where components are resolved [15]. | Selectivity (C8, C18, etc.), particle size, and dimensions significantly impact resolution and robustness [15] [29]. |
| HPLC-Grade Solvents | Used to prepare the mobile phase and sample solutions [15]. | High purity is critical to prevent baseline noise, ghost peaks, and column damage [15]. |
| System Suitability Standards | Verifies that the total system (instrument, reagents, column) is performing adequately at the time of analysis [15]. | Typically a mixture of analyte and key impurities; checks parameters like plate count, tailing factor, and resolution [15]. |
The IT and Data Management Backbone
In modern laboratories, data integrity is maintained through validated computerized systems. IT Quality Assurance (QA) ensures that these systems, including Laboratory Information Management Systems (LIMS) and Chromatography Data Systems (CDS), are compliant with regulations like FDA 21 CFR Part 11 and EU Annex 11 [119] [120].
Key requirements include:
- Computer System Validation (CSV): A documented process for confirming that a computerized system operates according to predefined specifications [120].
- Audit Trails: Secure, computer-generated, time-stamped electronic records that track who created, modified, or deleted data and when, and why the change was made. These must be enabled and reviewed regularly [119] [120].
- Electronic Signatures: Must be equivalent to handwritten signatures and include the printed name, date/time, and meaning of the signature (e.g., review, approval) [120].
- Access Controls: Role-based security to ensure only authorized personnel can access or perform operations on data [120].
Data Integrity and System Workflow
Achieving and maintaining audit readiness is a continuous journey rooted in scientific rigor and a proactive quality culture. It begins with the foundational development and comprehensive validation of analytical methods, ensuring every data point generated is reliable and meaningful. By integrating these validated procedures with modern, compliant IT systems that enforce data integrity principles, pharmaceutical laboratories can build a seamless framework of trust. This holistic approach not only ensures successful regulatory inspections but also accelerates drug development, protects patient safety, and solidifies the integrity of the scientific process itself.
Conclusion
Analytical method validation is a foundational, continuous process essential for ensuring the reliability, accuracy, and regulatory compliance of pharmaceutical quantification. Success requires a deep understanding of foundational principles, strategic method development, proactive troubleshooting, and rigorous documentation. The integration of QbD principles and robust lifecycle management is crucial for developing methods that are not only compliant but also economically viable and technically sound. Future directions will be shaped by advancements in analytical technologies, the growing importance of bioanalytical methods for novel therapies, and the evolving application of Verification, Validation, and Uncertainty Quantification (VVUQ) frameworks for complex applications like digital twins in precision medicine. Embracing these evolving standards will be key to accelerating drug development while safeguarding patient safety and product efficacy.
References
- 1. Understanding Analytical Method Development and ... [https://www.upm-inc.com/understanding-analytical-method-development-and-validation]
- 2. An Introduction to Analytical Method Development and ... [https://www.sofpromed.com/an-introduction-to-analytical-method-development-and-validation-in-early-phase-clinical-trials]
- 3. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 4. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 5. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 6. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 7. Basic Method Validation, 3rd Edition, FAQs [https://www.westgard.com/resources/resources/bmv3edfaqs.html]
- 8. The Critical Role of Analytical Services in Biopharma ... [https://www.skpharmteco.com/news-insights/blog/the-critical-role-of-analytical-services-in-biopharma-development/]
- 9. International Council for Harmonisation ( ICH ) - Guidelines - Canada.ca [https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/applications-submissions/guidance-documents/international-council-harmonisation/guidelines.html]
- 10. USP 2025 pdf free download (United State Pharmacopeia 48 - NF 43) [https://www.webofpharma.com/2025/03/usp-2025-pdf-free-download-united-state.html]
- 11. Bioanalytical method validation: new FDA guidance vs. EMA guideline. Better or worse? - PubMed [https://pubmed.ncbi.nlm.nih.gov/30590335/]
- 12. and Verification of Validation Testing Analytical Used for... Methods [https://www.federalregister.gov/documents/2025/01/07/2024-31541/validation-and-verification-of-analytical-testing-methods-used-for-tobacco-products-guidance-for]
- 13. Bioanalytical method validation - Scientific guideline | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/bioanalytical-method-validation-scientific-guideline]
- 14. Method Validation Guidelines | BioPharm International [https://www.biopharminternational.com/view/method-validation-guidelines]
- 15. Analytical Method Validation in Pharmaceuticals | Step-by-Step Guide to AMV | Pharmaguideline [https://www.pharmaguideline.com/2010/12/analytical-method-validation.html]
- 16. (PDF) Validation Methods for Quantification of API in Finished... [https://www.academia.edu/81853255/Validation_Methods_for_Quantification_of_API_in_Finished_PharmaceuticalProducts_Relationship_between_Accuracy_and_Precision]
- 17. Analytical Method Validation : Ensuring Quality and Consistency in... [https://www.webofpharma.com/2025/11/analytical-method-validation-ensuring.html]
- 18. Highlights from FDA's Analytical Test Method Validation Guidance [https://www.propharmagroup.com/thought-leadership/fda-analytical-test-method-validation-guidance]
- 19. ICH Guidelines for Analytical Method Validation Explained | AMSbiopharma [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 20. Establishing Acceptance Criteria for Analytical Methods | BioPharm International [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 21. Validation - Limit of Detection, Quantitation limits and... Method [https://www.slideshare.net/slideshow/method-validation-sigma-test-research-centre/56732700]
- 22. Limit of Detection ( LOD ) and Limit of Quantitation ( LOQ ) in Analytical... [https://www.pharmaspecialists.com/2023/09/lod-and-loq-in-analytical-method-validation.html]
- 23. Analytical Method Validation: Back to Basics, Part II | LCGC International [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 24. 9. LoD and LoQ – Validation of liquid chromatography mass spectrometry (LC-MS) methods [https://sisu.ut.ee/lcms_method_validation/9-lod-and-loq/]
- 25. Guidance for robustness/ruggedness tests in method validation - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S073170850000529X]
- 26. 10. Ruggedness, robustness – Validation of liquid chromatography mass spectrometry (LC-MS) methods [https://sisu.ut.ee/lcms_method_validation/10-ruggedness-robustness/]
- 27. Limit of Blank, Limit of Detection and Limit of Quantitation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 28. 10.1 Robustness and ruggedness relation to LC-MS method ... [https://sisu.ut.ee/lcms_method_validation/101-robustness-and-ruggedness-relation-lc-ms-method-development/]
- 29. Introduction to Analytical Method Development and Validation | Lab Manager [https://www.labmanager.com/introduction-to-analytical-method-development-and-validation-33922]
- 30. Remediation Services | The FDA Group Regulatory Submission [https://www.thefdagroup.com/services/regulatory-submission-remediation]
- 31. Editorial: Recent advances in pharmaceutical analysis: applications and new challenges for the quality of medicines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12491238/]
- 32. Avoiding Common FDA 483 Observations in Cleaning Validation [https://www.valgenesis.com/blog/avoiding-common-fda-483-observations-in-cleaning-validation]
- 33. Ensuring Product and Safety Compliance: A Guide to... Regulatory [https://mesalabs.com/spore-news-resources/ensuring-product-safety-and-regulatory-compliance-a-guide-to-sterilization-validation]
- 34. Advances in Pharmaceutical Analytical Technology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114358/]
- 35. Aspects and Implementation of Pharmaceutical Quality by Design... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 36. Steps for Analytical Method | Pharmaguideline Development [https://www.pharmaguideline.com/2017/09/steps-for-analytical-method-development.html]
- 37. and Applications to Improve Methods Pharmaceutical Workflows [https://www.sepscience.com/methods-and-applications-to-improve-pharmaceutical-workflows-7124]
- 38. The Importance of Method in Validation Pharmaceutical Analysis [https://www.linkedin.com/pulse/importance-method-validation-pharmaceutical-bj3of]
- 39. Bayesian Optimization over Multiple Experimental Fidelities Accelerates Automated Discovery of Drug Molecules - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11869128/]
- 40. Drug Properties Prediction Based on Deep Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8880629/]
- 41. Leading Pharmaceutical Trends for Validation 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 42. AQbD-novel strategy for analytical methods | Future Journal of Pharmaceutical Sciences | Full Text [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 43. QbD approach to HPLC method development and validation of ceftriaxone sodium | Future Journal of Pharmaceutical Sciences | Full Text [https://fjps.springeropen.com/articles/10.1186/s43094-021-00286-4]
- 44. (AQbD) for Analytical and Risk... Quality by Design Quality [https://www.syncsci.com/journal/JPBR/article/view/JPBR.2025.01.001]
- 45. QbD Based Analytical Method Development and Validation for the Estimation of Remogliflozin etabonate and Vildagliptin in Bulk and in Their Dosage Form | Journal of Chemical Health Risks [https://www.jchr.org/index.php/JCHR/article/view/5213]
- 46. HPLC-UV and GC-MS Methods for Determination of Chlorambucil and Valproic Acid in Plasma for Further Exploring a New Combined Therapy of Chronic Lymphocytic Leukemia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8153269/]
- 47. of high- Comparison liquid chromatography and... performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC6425260/]
- 48. (PDF) Comparison of methods for determination of polyphenols in... [https://www.academia.edu/73083440/Comparison_of_methods_for_determination_of_polyphenols_in_wine_by_HPLC_UV_VIS_LC_MS_MS_and_spectrophotometry]
- 49. Approved Training Courses [https://www.rsc.org/cpd/training/detail/487/complete-hplc-and-lc-ms]
- 50. Journal of Research in Pharmacy » Submission » QbD based... [https://dergipark.org.tr/en/pub/jrespharm/issue/91538/1688405]
- 51. -driven stability indicating Qbd - rp ... hplc method [https://journals.innovareacademics.in/index.php/ijap/article/view/53110]
- 52. - RP for Content of Genotoxic 4-methoxybenzyl Chloride... HPLC Method [https://www.orientjchem.org/vol39no6/rp-hplc-method-for-content-of-genotoxic-4-methoxybenzyl-chloride-in-venlafaxine/]
- 53. ANALYTICAL METHOD VALIDATION: AN UPDATED REVIEW | INTERNATIONAL JOURNAL OF PHARMACEUTICAL SCIENCES AND RESEARCH [https://ijpsr.com/bft-article/analytical-method-validation-an-updated-review/]
- 54. Optimization and Validation of RP - HPLC -UV/Vis Method for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3132538/]
- 55. in Mass Spectrometry Combined with... | IntechOpen Matrix Effects [https://www.intechopen.com/chapters/45040]
- 56. Compensate for or Minimize Matrix Effects? Strategies for Overcoming Matrix Effects in Liquid Chromatography-Mass Spectrometry Technique: A Tutorial Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 57. Strategies for the Detection and Elimination of Matrix Effects in Quantitative LC–MS Analysis | LCGC International [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 58. The Hidden Risks in Analytical Method Validation [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 59. in Fâ‚‚-isoprostanes Matrix by HPLC-MS/MS... effect quantification [https://pubmed.ncbi.nlm.nih.gov/24999618/]
- 60. Important Considerations Regarding Matrix When Developing... Effects [https://www.chromatographyonline.com/view/important-considerations-regarding-matrix-effects-when-developing-reliable-analytical-residue-method]
- 61. Stability Indicating High Performance Liquid Chromatography Method Development, Validation, and Characterization of Forced Degradant Product by Liquid Chromatography-Mass Spectroscopy for Molnupiravir and Favipiravir - PubMed [https://pubmed.ncbi.nlm.nih.gov/40152015/]
- 62. 5.4 Quantitative estimation of matrix , recovery and process... effect [https://sisu.ut.ee/lcms_method_validation/54-quantitative-estimation-matrix-effect-recovery-process-efficiency/]
- 63. Analytical Method Validation: Back to Basics, Part I | LCGC International [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 64. Uncover FDA lessons and learn how to avoid the most common... [https://www.leucine.io/cleaning-validation-blogs/fda-lessons-cleaning-validation-pitfalls-pharma-2025]
- 65. Getting Analytical Method Validation, Verification & Transfer Right [https://www.complianceonline.com/resources/getting-the-analytical-method-validation-verification-and-transfer-right.html]
- 66. Navigating Biologics Drug Product Process Validation : Pitfalls and... [https://www.linkedin.com/pulse/navigating-biologics-drug-product-process-validation-pitfalls-lien-avlvc]
- 67. How to Select an HPLC from Four Key Dimensions... Column [https://uhplcs.com/how-to-select-an-hplc-column-from-four-key-dimensions/]
- 68. Types of columns in HPLC - Laafon Galaxy Pharmaceuticals [https://laafon.com/types-of-column-in-hplc/]
- 69. - HPLC selectivity measurements of more... Columns HPLC column [https://www.hplccolumns.org/database/compare.php]
- 70. Peak Purity in HPLC : Assessment, Troubleshooting, and Best Practices [https://www.sepscience.com/peak-purity-in-hplc-assessment-troubleshooting-and-best-practices-11506]
- 71. Real Solutions to Improve Your HPLC Peak Resolution - AnalyteGuru [https://www.thermofisher.com/blog/analyteguru/real-solutions-to-improve-your-hplc-peak-resolution/]
- 72. HPLC Method Development and Validation for Pharmaceutical Analysis | Pharmaceutical Technology [https://www.pharmtech.com/view/hplc-method-development-and-validation-pharmaceutical-analysis]
- 73. A Study of Method Development, Validation, and Forced Degradation for Simultaneous Quantification of Paracetamol and Ibuprofen in Pharmaceutical Dosage Form by RP-HPLC Method - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4237153/]
- 74. Method optimization to increase sensitivity in case of LOQ / LOD problems [https://mpl.loesungsfabrik.de/en/english-blog/high-performance-liquid-chromatography/method-optimization-sensitivity-hplc]
- 75. HPLC Tips & Tricks: Increase Your HPLC/UHPLC Method Sensitivity [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/small-molecule-hplc/increase-your-hplc-uhplc-method-sensitivity]
- 76. Frontiers | Comprehensive and robust stability-indicating reversed phase high performance liquid chromatography (RP-HPLC) method for Rivaroxaban: synergistic integration of infrared spectroscopy and clinical pharmacology insights [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1551189/full]
- 77. | Phenomenex Sample Preparation Techniques [https://www.phenomenex.com/knowledge-center/spe-knowledge-center/sample-preparation-techniques-for-precision-in-analysis]
- 78. of Drug Substances and Products in Regulated... Sample Preparation [https://www.chromatographyonline.com/view/sample-preparation-of-drug-substances-and-products-in-regulated-testing-a-primer]
- 79. Recent Advancements In Hplc Method Development And Validation: Pushing The Boundaries Of Analysis[v1] | Preprints.org [https://www.preprints.org/manuscript/202409.1804/v1]
- 80. and Validation of Two Analytical Methods for Imatinib... Comparison [https://link.springer.com/article/10.1007/s10337-021-04041-y]
- 81. Journal of Research in Pharmacy » Submission » Liquid-liquid... [https://dergipark.org.tr/en/pub/jrespharm/issue/91533/1686192]
- 82. A Guide to GC Sample Preparation - ILT [https://www.iltusa.com/gc-sample-preparation/]
- 83. Evaluation and comparison of very high pressure liquid... [https://pubmed.ncbi.nlm.nih.gov/17595957/]
- 84. Principles and Applications of High-Performance Liquid Chromatography (HPLC): A Review – Biomedical and Pharmacology Journal [https://biomedpharmajournal.org/vol18no2/principles-and-applications-of-high-performance-liquid-chromatography-hplc-a-review/]
- 85. Comprehensive Two-Dimensional Gas Chromatography as a Bioanalytical Platform for Drug Discovery and Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10140985/]
- 86. Current thinking on quantification of protein... - Bioanalysis Zone [https://www.bioanalysis-zone.com/protein-therapeutic-pharmacokinetics-protein-biomarkers_spotlbioanalysis_of_biopharma/]
- 87. Understanding Biomarker Validation: Accuracy & Precision... Method [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-xyhhe]
- 88. Impurities in drug substances and drug products: new approaches to quantification and qualification - PubMed [https://pubmed.ncbi.nlm.nih.gov/8833961/]
- 89. Recent trends in the impurity profile of pharmaceuticals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3255420/]
- 90. Pharmaceutical Analytical Impurities [https://www.usp.org/impurities/pharmaceutical-analytical-impurities]
- 91. Determination of Impurities in Pharmaceuticals: Why and How? | IntechOpen [https://www.intechopen.com/chapters/65419]
- 92. Impurity Profiling in Pharmaceuticals: Analytical Methods and Compliance - Biotech Spain [https://biotech-spain.com/en/articles/impurity-profiling-in-pharmaceuticals-analytical-methods-and-compliance/]
- 93. How mass spectrometry is redefining impurity analysis - Bioanalysis Zone [https://www.bioanalysis-zone.com/how-mass-spectrometry-is-redefining-impurity-analysis/]
- 94. Characteristics In Performance Analytical Method Validation [https://gmpinsiders.com/performance-characteristics-method-validation/]
- 95. , Validation, & Qualification: Clarifying the Core Concepts of... Calibration [https://www.webofpharma.com/2025/11/calibration-validation-qualification.html]
- 96. Equipment Calibration: The Ultimate Guide for Managers (2025) [https://f7i.ai/blog/equipment-calibration-isnt-a-chore-its-your-competitive-edge-the-strategic-guide-for-2025]
- 97. Technologies for Liquid Handling Quality... Comparing Calibration [https://www.aicompanies.com/education-training/knowledge-center/comparing-calibration-technologies-for-liquid-handling-quality-assurance/]
- 98. Instrument calibration procedure for pharmaceutical industry [https://www.gmpsop.com/instrument-calibration-procedure/]
- 99. Instrument Calibration Services Market Report 2025, Key Players, Share [https://www.thebusinessresearchcompany.com/report/instrument-calibration-services-global-market-report]
- 100. The Validation Roadmap: Essential Components of a Pharmaceutical ... [https://www.webofpharma.com/2025/11/the-validation-roadmap-essential.html]
- 101. The Critical Role of Audit Trails in Ensuring Data Integrity and Compliance in the Pharmaceutical, Biotech, and Medical Device Industry [https://www.eleapsoftware.com/the-critical-role-of-audit-trails-in-ensuring-data-integrity-and-compliance-in-the-pharmaceutical-biotech-and-medical-device-industry/]
- 102. GMP Audit Trail Review: What Health Authorities Expect in 2025 | Freyr - Global Regulatory Solutions and Services Company [https://www.freyrsolutions.com/blog/gmp-audit-trail-review-what-health-authorities-expect-in-2025]
- 103. Top 5 Audit Trail Issues Found in Regulatory Inspections - Zamann Pharma Support GmbH [https://zamann-pharma.com/2025/04/23/top-5-audit-trail-issues-found-in-regulatory-inspections/]
- 104. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 105. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 106. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 107. PMA Review Process [https://www.fda.gov/medical-devices/premarket-approval-pma/pma-review-process]
- 108. Post-Approval Studies Program [https://www.fda.gov/medical-devices/postmarket-requirements-devices/post-approval-studies-program]
- 109. Annex 11 2025: System Lifecycle & Supplier Oversight [https://www.rephine.com/resources/blog/annex-11-2025-system-lifecycle-supplier-oversight/]
- 110. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 111. Emerging New Drug in Modalities | BCG 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 112. A Nuanced Perspective on Process Validation for Emerging... [https://www.linkedin.com/pulse/nuanced-perspective-process-validation-emerging-rich-motruk-p2ice]
- 113. Multimodal AI predicts clinical outcomes of drug combinations from... [https://arxiv.org/html/2503.02781v1]
- 114. Transfer, Comparability and Co-validation [https://www.mastercontrol.com/gxp-lifeline/transfer-comparability-covalidation/]
- 115. Analytical Methodology Transfer - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0149639501800167]
- 116. Streamlining Method Transfer Across Global Sites [https://www.biopharminternational.com/view/streamlining-method-transfer-across-global-sites]
- 117. Comparison of Analytical Procedures in Method Transfer and Bridging Experiments - PubMed [https://pubmed.ncbi.nlm.nih.gov/37468665/]
- 118. GxP Compliance in Pharma : The No-Excuses Guide to Being... [https://www.scilife.io/blog/gxp-compliance-in-pharma]
- 119. Preparing Pharma Labs for Regulatory Inspections... | Lab Manager [https://www.labmanager.com/preparing-pharma-labs-for-regulatory-inspections-a-guide-to-readiness-and-compliance-34065]
- 120. IT Quality Assurance in Pharma : Ensuring Compliance ... - Rephine [https://www.rephine.com/resources/blog/it-quality-assurance-in-pharma-ensuring-compliance-validation-data-integrity/]