Comparative Method in Analytical Validation: A Guide for Researchers and Scientists
This article provides a comprehensive guide to the comparative method, a critical experiment in analytical method validation used to estimate systematic error or inaccuracy.
Comparative Method in Analytical Validation: A Guide for Researchers and Scientists
Abstract
This article provides a comprehensive guide to the comparative method, a critical experiment in analytical method validation used to estimate systematic error or inaccuracy. Aimed at researchers, scientists, and drug development professionals, it covers foundational concepts from defining the comparative method's purpose in assessing systematic error against a reference to the strategic selection of a comparator. The scope extends to methodological execution, including experimental design, data analysis techniques like difference plots and linear regression, and troubleshooting common pitfalls. Finally, it explores validation within a regulatory framework, discussing risk-based approaches for method changes and the distinctions between comparability and equivalency, synthesizing best practices for ensuring data reliability and regulatory compliance.
Comparative Method Fundamentals: Defining Purpose and Key Concepts
In analytical method validation, the comparison of methods experiment is a critical study designed to estimate the inaccuracy or systematic error of a new (test) analytical method relative to a established comparative method [1]. This process is foundational for ensuring the reliability of data in pharmaceutical development, clinical diagnostics, and quality control laboratories. Systematic error, also known as bias, represents a consistent or proportional difference between observed values and the true value [2]. Unlike random error, which affects precision and varies unpredictably, systematic error skews measurements in a specific direction, potentially leading to false conclusions and decisions if left unquantified [2]. Determining this bias is therefore not merely a regulatory formality but a fundamental requirement for demonstrating that a method is fit for its intended purpose and that future measurements in routine analysis will be sufficiently close to the true value [3].
The core principle of this comparison is to analyze a set of patient specimens or test samples using both the new method and a comparative method, then estimate systematic errors based on the observed differences [1]. The results are used to judge the acceptability of the test method, often against predefined medical or quality-based decision limits [4]. This process fits within a broader method validation plan, which typically also includes experiments for precision (replication) and specific investigations into potential interferences [1] [4].
Theoretical Foundations of Analytical Error
Distinguishing Random and Systematic Error
Understanding the distinction between random and systematic error is crucial for interpreting comparison of methods data.
Random Error: This is a chance difference between an observed value and the true value. It affects the precision of a measurement, meaning it causes variability when the same quantity is measured repeatedly under equivalent conditions [2]. In a dataset, random error causes observations to scatter randomly around the true value. In highly controlled settings, it can often be reduced by taking repeated measurements and using their average [2]. Sources of random error can include electronic noise in instruments, natural variations in experimental contexts, and slight fluctuations in how measurements are read [2] [5].
Systematic Error: This is a consistent or proportional difference between the observed values and the true value. It affects the accuracy (or trueness) of a measurement, meaning it consistently skews all measurements in a specific direction away from the true value [2]. Systematic error is also referred to as bias and is generally a more significant problem in research and analysis because it can lead to false conclusions about the relationship between variables [2]. It cannot be reduced by simply repeating measurements [6].
Table: Comparison of Random and Systematic Error
| Feature | Random Error | Systematic Error |
|---|---|---|
| Definition | Unpredictable, chance differences | Consistent or proportional differences |
| Impact on Data | Affects precision (reproducibility) | Affects accuracy (trueness) |
| Direction of Effect | Equally likely to be higher or lower than true value | Consistently higher or lower than true value |
| Elimination | Cannot be eliminated, but can be reduced | Can potentially be eliminated by identifying the cause |
| Common Sources | Natural variations, imprecise instruments, procedural fluctuations | Miscalibrated instruments, flawed procedures, incorrect assumptions |
Systematic errors can be categorized based on their behavior, which helps in diagnosing their root cause [2] [5]:
- Constant Error (Offset Error): This error remains the same absolute amount across the entire analytical range. It occurs when a scale is not calibrated to a correct zero point and is also called an additive or zero-setting error [2] [5]. For example, a balance that always reads 0.5 grams over the true mass introduces a constant error.
- Proportional Error (Scale Factor Error): This error changes in proportion to the concentration of the analyte. It occurs when measurements consistently differ from the true value by a constant percentage (e.g., by 10%) and is also known as a multiplier error [2] [5]. An example would be an instrument where the response factor is incorrectly calculated.
These errors can originate from various aspects of the analytical process [6]:
- Instrumental Error: Caused by inaccurate instruments, such as a miscalibrated pH meter or a balance that does not function properly [6].
- Procedural Error: Arises from flaws in the experimental protocol or inconsistent application of procedures [6].
- Human Error: Includes transcriptional errors (e.g., recording data incorrectly) and estimation errors (e.g., misreading a scale) [6].
- Specimen-Based Error: In clinical chemistry, interferences from substances in a patient sample or instability of the analyte during storage can introduce systematic error specific to that specimen [1].
Designing the Comparison of Methods Experiment
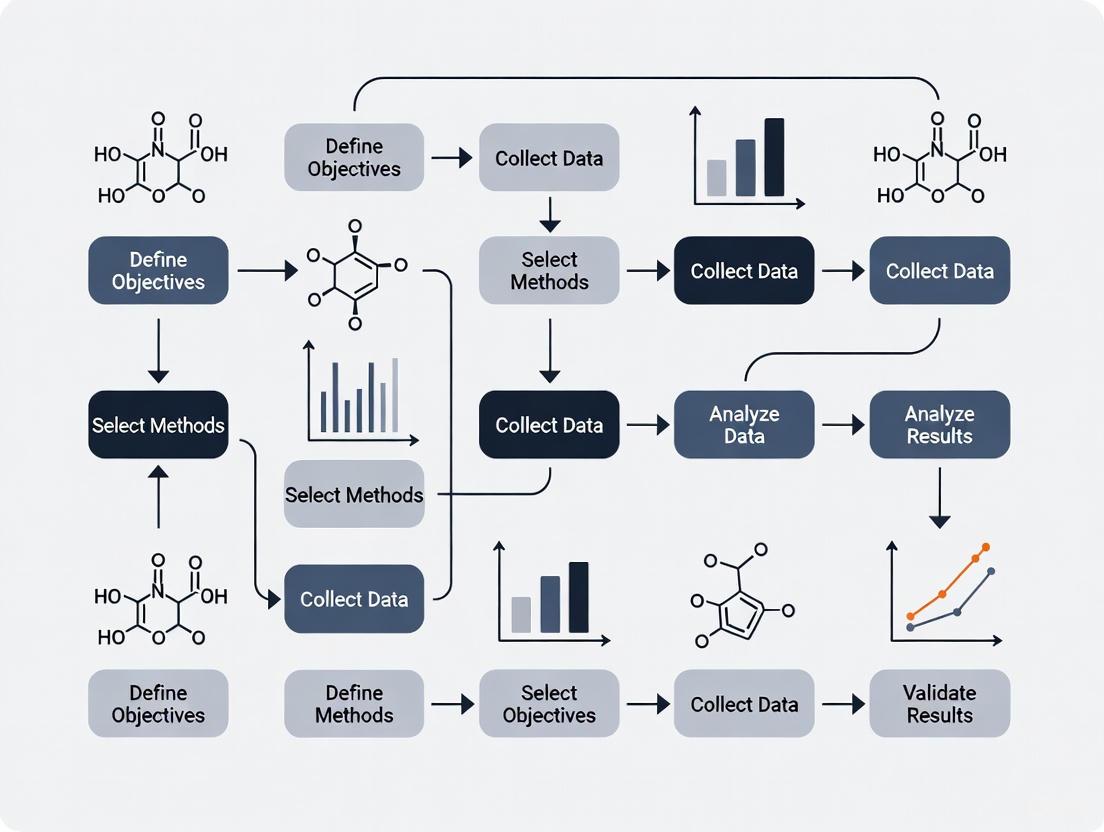
A well-designed experiment is essential for obtaining reliable estimates of systematic error. Key factors to consider are detailed below, and the overall workflow is summarized in the following diagram.
Selection of the Comparative Method
The choice of comparative method is paramount, as the interpretation of the experimental results hinges on the assumptions made about its correctness [1].
- Reference Method: The ideal comparative method is a reference method, a high-quality method whose correctness is well-documented through comparison with definitive methods and traceable reference materials [1]. When such a method is used, any observed differences are attributed to the test method.
- Routine Method: In many cases, a routine laboratory method serves as the comparative method. Its correctness may not be as rigorously documented [1]. If large and medically unacceptable differences are found, it becomes necessary to conduct additional experiments (e.g., recovery or interference studies) to identify which method is inaccurate.
Selection and Handling of Specimens
The quality of specimens used directly impacts the quality of the error estimates [1].
- Number of Specimens: A minimum of 40 different patient specimens is recommended [1]. The primary goal is to cover the entire working range of the method. Twenty carefully selected specimens covering a wide concentration range often provide better information than a hundred random specimens.
- Concentration Range: Specimens should be selected to provide results across the entire analytical range, from low to high values [1]. This is critical for reliably estimating proportional error using regression statistics.
- Stability and Handling: Specimens should generally be analyzed by both methods within two hours of each other to prevent degradation from causing observed differences [1]. Stability can be improved by refrigeration, freezing, or adding preservatives. A standardized handling procedure is essential prior to beginning the study.
Measurement Protocol and Timeline
The protocol must be designed to minimize the impact of extraneous variables.
- Replication: Common practice is single measurement by each method, but duplicate measurements are advantageous [1]. Duplicates act as a check for sample mix-ups, transcription errors, or other mistakes that could invalidate individual data points.
- Time Period: The experiment should be conducted over several days to minimize bias from a single analytical run. A minimum of 5 days is recommended, and the study can be extended over a longer period (e.g., 20 days) with only 2-5 specimens analyzed per day [1].
Data Analysis and Estimation of Systematic Error
Graphical Inspection of Data
The first step in data analysis is always to graph the results for visual inspection. This should be done while data is being collected to identify and immediately rectify any discrepant results.
- Difference Plot: When the two methods are expected to show one-to-one agreement, a difference plot (Bland-Altman-type plot) is used. The difference between the test and comparative method results (test - comparative) is plotted on the y-axis against the comparative method result on the x-axis [1]. The points should scatter randomly around the zero line. This plot readily reveals constant bias and can highlight concentrations where bias changes.
- Comparison Plot (Scatter Plot): For methods not expected to agree one-to-one, a scatter plot is used. The test method result (Y) is plotted against the comparative method result (X) [1]. A visual line of best fit can be drawn to show the relationship, helping to identify outliers and visualize proportional and constant error.
Statistical Calculation of Systematic Error
Statistical calculations provide numerical estimates of the systematic error. The appropriate statistical approach depends on the concentration range of the data.
For a Wide Analytical Range (e.g., glucose, cholesterol) - Linear Regression: Linear regression (least squares analysis) is used to calculate the slope (b) and y-intercept (a) of the line of best fit, along with the standard deviation of the points about the line (s~y/x~) [1]. The systematic error (SE) at a specific medical decision concentration (X~c~) is calculated as:
Y~c~ = a + bX~c~SE = Y~c~ - X~c~- Y-intercept (a): Estimates the constant systematic error.
- Slope (b): Estimates the proportional systematic error. A slope of 1.0 indicates no proportional error.
- Correlation coefficient (r): Is mainly useful for verifying that the data range is wide enough to provide reliable estimates of the slope and intercept. A value ≥ 0.99 is desirable [1].
For a Narrow Analytical Range (e.g., sodium, calcium) - Average Difference (Bias): When the concentration range is narrow, it is often best to calculate the average difference (bias) between the two methods [1]. This is typically derived from a paired t-test calculation, which also provides the standard deviation of the differences and a t-value to assess the statistical significance of the bias.
Table: Key Statistical Measures in Comparison of Methods
| Statistical Measure | Interpretation | Role in Estimating Systematic Error |
|---|---|---|
| Y-Intercept (a) | The value of Y when X is zero. | Estimates the constant systematic error. |
| Slope (b) | The change in Y for a one-unit change in X. | Estimates the proportional systematic error. |
| Standard Error of the Estimate (s~y/x~) | The standard deviation of the points around the regression line. | Quantifies the random scatter, which includes random error and any non-linear bias. |
| Average Difference (Bias) | The mean of (Test Result - Comparative Result). | Provides a single estimate of the average systematic error across the narrow range studied. |
Essential Reagents and Materials for a Comparison Study
The following table details key materials required for a robust comparison of methods experiment, particularly in a pharmaceutical or clinical chemistry context.
Table: Key Research Reagent Solutions and Materials
| Item | Function in the Experiment |
|---|---|
| Characterized Patient Specimens | Serve as the core test material, providing a matrix-matched and clinically relevant sample for comparison across the analytical range [1]. |
| Reference Method Materials | Include calibrators and reagents for a well-defined comparative method to which the test method is benchmarked [1]. |
| Test Method Calibrators | Materials used to calibrate the new method under evaluation, ensuring it is operating according to its specified protocol. |
| Quality Control (QC) Pools | Samples with known (or assigned) values analyzed at intervals throughout the study to monitor the stability and performance of both the test and comparative methods over time. |
| Stabilizing Reagents | Preservatives or additives used to ensure analyte stability in specimens during the testing period, preventing degradation from being misinterpreted as systematic error [1]. |
Advanced Applications and Regulatory Context
The principles of method comparison extend beyond initial validation. In the pharmaceutical industry, analytical method comparability studies are critical for managing changes to analytical methods after a drug product has been approved [7]. This is a key part of Chemistry, Manufacturing, and Controls (CMC) changes. A risk-based approach is recommended, where the extent of the comparability study (e.g., side-by-side comparison of results vs. a full statistical equivalency study) depends on the significance of the method change [7]. For instance, changing a high-performance liquid chromatography (HPLC) method to ultra-high pressure liquid chromatography (UHPLC) for speed and efficiency would require demonstrating that the new method provides equivalent performance for critical attributes like assay and impurity profiles [7].
Furthermore, a holistic approach to validation integrates the concept of measurement uncertainty [3]. This is a parameter that characterizes the dispersion of values that could reasonably be attributed to the measurand, and it incorporates both random and systematic error components [8] [3]. The data generated from a carefully designed comparison of methods experiment is fundamental to quantifying the measurement uncertainty of the test method, ultimately ensuring that it is fit for its intended purpose.
In analytical method validation research, demonstrating that a new or altered method produces reliable and accurate results is paramount. This process fundamentally relies on comparing the candidate method against a benchmark. The choice of this benchmark—specifically, whether it is a Reference Method or a Comparative Method—critically influences the design, interpretation, and regulatory acceptance of the validation study. A Reference Method provides a definitive anchor with established accuracy, whereas a Comparative Method serves as a practical benchmark whose own correctness may not be fully documented [1]. Within the framework of a broader thesis on analytical method validation, understanding this distinction is not merely academic; it dictates the experimental protocol, the statistical analysis, and the justifiability of conclusions regarding a method's suitability for its intended purpose, such as ensuring drug safety and efficacy [7].
This guide provides an in-depth technical exploration of the critical differences between Comparative and Reference Methods. It is structured to equip researchers, scientists, and drug development professionals with the knowledge to select the appropriate benchmark, design rigorous comparison experiments, and apply correct data analysis techniques to draw defensible conclusions about their analytical methods.
Defining the Core Concepts
Reference Method
A Reference Method is an analytical procedure that has been rigorously validated and whose results are known to be correct through established traceability. The key characteristic of a reference method is its documented correctness, often established through comparison with an authoritative "definitive method" or via certified Standard Reference Materials (SRMs) [1]. Results from a reference method are considered to be the "true value" for the purpose of the comparison study. Consequently, any observed differences between the test method and the reference method are attributed to errors in the test method. These methods are typically characterized by high specificity, accuracy, and precision, and are often developed and maintained by national or international standards organizations [9].
Comparative Method
A Comparative Method is a more general term for any method used as a benchmark in a comparison study. It does not inherently carry the implication of documented, definitive accuracy. In most routine laboratory settings, the benchmark is a comparative method—often the existing routine method in use [1]. The interpretation of results is less straightforward than with a reference method. If differences between the test and comparative methods are small and medically or analytically acceptable, the two methods are considered to have comparable performance. However, if differences are large, additional experimentation is required to determine which method is producing the inaccurate results, as the error cannot be automatically assigned to the test method [1].
The following table summarizes the key distinctions between these two benchmarks:
| Feature | Reference Method | Comparative Method (Routine Method) |
|---|---|---|
| Definition | A method with rigorously documented correctness and traceability [1]. | A general term for any method used for comparison; its correctness is not necessarily documented [1]. |
| Assumption | Results are the "true value." [1] | Results are a "practical benchmark." |
| Interpretation of Differences | Differences are attributed to error in the test method [1]. | Differences must be interpreted carefully; large discrepancies require investigation to identify the source of error [1]. |
| Common Use Cases | Definitive validation studies; establishing traceability; certifying reference materials [9]. | Most routine method change studies in laboratories (e.g., HPLC to UHPLC transitions) [7]. |
| Regulatory Burden | Typically higher, as the reference method itself must be justified. | Can be lower, but requires robust statistical demonstration of equivalence. |
Experimental Design for Method Comparison
A well-designed experiment is the foundation of a reliable method comparison. Key factors must be considered to ensure the results are meaningful and representative of real-world performance.
Sample Selection and Size
The quality of patient specimens or samples is more critical than sheer quantity. However, a sufficient number is needed to ensure statistical power and to identify potential interferences.
- Number of Specimens: A minimum of 40 different patient specimens is widely recommended, with 100-200 being preferable to fully assess specificity and identify matrix-related interferences [1] [10].
- Concentration Range: Specimens should be carefully selected to cover the entire working range of the method, including critical medical decision concentrations [1] [10].
- Sample Quality: Specimens should represent the expected spectrum of diseases and conditions encountered in routine practice. They should be analyzed within a stable period, ideally within two hours of each other by both methods, to avoid degradation [1].
Data Collection Protocol
The protocol should mimic routine conditions while controlling for variables that could confound results.
- Replication: While single measurements are common, performing duplicate measurements in different analytical runs or in a randomized order is highly advantageous. Duplicates act as a validity check for individual methods and help identify sample mix-ups or transcription errors [1].
- Timeframe: The experiment should be conducted over several different analytical runs and a minimum of 5 days. Extending the study over a longer period, such as 20 days, helps minimize systematic errors that might occur in a single run and provides a more realistic estimate of long-term performance [1].
- Randomization: The sample sequence should be randomized to avoid carry-over effects and systematic bias [10].
Data Analysis and Statistical Approaches
The goal of data analysis is to identify, quantify, and judge the acceptability of systematic error (bias). A combination of graphical and statistical methods is essential.
Graphical Analysis: The First Step
Graphical inspection of the data should be performed as the data is collected to identify discrepant results for immediate re-analysis [1] [10].
- Scatter Plot: This plot displays the test method results (y-axis) against the comparative/reference method results (x-axis). It is excellent for showing the analytical range, linearity, and the general relationship between the methods. A line of identity (y=x) is often drawn; deviations from this line suggest bias [1] [10].
- Difference Plot (Bland-Altman Plot): This is a powerful tool for assessing agreement. The difference between the test and comparative method (y-axis) is plotted against the average of the two methods or the value of the comparative method (x-axis). This plot readily reveals the magnitude of differences, any systematic bias (the average difference), and whether the variability of differences is constant across the measuring range [1] [10] [11].
Statistical Calculations for Quantifying Error
While graphs provide a visual impression, statistical calculations put exact numbers on the observed errors.
- Linear Regression Analysis: For data covering a wide analytical range (e.g., glucose, cholesterol), linear regression is preferred. It provides statistics for the slope (b) and y-intercept (a) of the line of best fit, and the standard deviation of the points about that line (s~y/x~) [1].
- The slope indicates a proportional error.
- The y-intercept indicates a constant error.
- The systematic error (SE) at any critical decision concentration (X~c~) is calculated as: SE = Y~c~ - X~c~, where Y~c~ = a + bX~c~ [1].
- Correlation Coefficient (r): The correlation coefficient is mainly useful for assessing whether the range of data is wide enough to provide reliable estimates of the slope and intercept. A value of r ≥ 0.99 is generally considered acceptable for this purpose. It should not be used to judge the acceptability of the method, as high correlation can exist even with significant bias [1] [10].
- Paired t-test / Average Difference (Bias): For analytes with a narrow analytical range (e.g., sodium, calcium), it is often best to simply calculate the average difference between the two methods, also known as the bias. This is typically derived from a paired t-test, which also provides a standard deviation of the differences [1].
The following table outlines the core statistical measures used and their interpretation:
| Statistical Measure | What It Estimates | Interpretation in Method Comparison |
|---|---|---|
| Slope (b) | Proportional difference between methods. | A slope of 1.00 indicates no proportional error. A slope of 1.05 indicates a 5% proportional error. |
| Y-Intercept (a) | Constant difference between methods. | An intercept of 0.0 indicates no constant error. A positive intercept indicates the test method consistently reads higher by that amount. |
| Standard Error of the Estimate (s~y/x~) | Random variation around the regression line. | A measure of the average scatter of the data points around the line of best fit. |
| Average Difference (Bias) | Systematic error averaged over all samples. | A positive value indicates the test method, on average, reads higher than the comparative method. |
| Standard Deviation of Differences | Dispersion of the individual differences. | Used to calculate the Limits of Agreement in a Bland-Altman plot (Mean Difference ± 1.96 SD) [11]. |
Essential Tools and Reagents for a Method Comparison Study
A successful method comparison study relies on more than just a protocol. The following toolkit is essential for execution.
The Scientist's Toolkit: Key Research Reagents and Materials
| Item | Function in Method Comparison |
|---|---|
| Well-Characterized Patient Samples | The core of the study, providing a real-world matrix to assess method performance across a wide concentration range and disease spectrum [1] [10]. |
| Certified Reference Materials (CRMs) | Used to verify the accuracy of a Reference Method or to help troubleshoot large biases identified with a Comparative Method. Provides a traceable link to a standard [1]. |
| Stable Quality Control Materials | Used to monitor the precision and stability of both the test and comparative methods throughout the data collection period, ensuring both systems are in control. |
| Calibrators for Both Methods | Essential for ensuring that each instrument is properly calibrated according to its own specific procedure, a prerequisite for a valid comparison. |
| Appropriated Specimen Collection Tubes | To ensure specimen integrity. The type of anticoagulant or preservative must be appropriate for both analytical methods. |
| Data Analysis Software | Software capable of performing advanced statistical analyses (e.g., linear regression, Bland-Altman plots, Deming/Passing-Bablok regression) and generating high-quality graphs is indispensable [10] [11] [12]. |
| Ki16425 | Ki16425, CAS:355025-24-0, MF:C23H23ClN2O5S, MW:475.0 g/mol |
| L-167307 | L-167307, CAS:188352-45-6, MF:C22H17FN2OS, MW:376.4 g/mol |
Regulatory and Practical Considerations in the Pharmaceutical Industry
In regulated environments like drug development, method changes are common, and demonstrating comparability is a key requirement.
- Risk-Based Approach: Regulatory guidance on method comparability is not always explicit, leading to a risk-based approach in the pharmaceutical industry. The extent of the comparability study depends on the impact of the method change [7]. A minor change (e.g., within robustness parameters of an HPLC method) may not require a full equivalency study, whereas a major change (e.g., a different separation mechanism) typically will [7].
- Equivalency vs. Comparability: The terms are sometimes differentiated. Analytical method equivalency may refer specifically to a formal statistical study to demonstrate that two methods generate equivalent results for the same sample, while analytical method comparability is a broader term that includes the evaluation of all method performance characteristics (accuracy, precision, specificity, etc.) [7].
- Documentation: A successful regulatory submission for a method change typically includes the reason for the change, complete validation data for the new method, and a side-by-side comparability/equivalency study data package [7].
The distinction between a Reference Method and a Comparative Method is a critical conceptual foundation in analytical method validation. A Reference Method acts as a definitive anchor, allowing for unambiguous assignment of error to the test method. In contrast, a Comparative Method provides a practical benchmark, requiring careful interpretation of differences and potentially further investigation to identify the source of error. The choice between them dictates the experimental design, from sample selection and replication to the statistical analysis of systematic error using regression or bias calculations.
A rigorous method comparison study, employing both graphical techniques and appropriate statistics, is not merely a regulatory checkbox. It is a scientific exercise that ensures the continued quality, safety, and efficacy of pharmaceutical products by guaranteeing that analytical methods—the tools used to make critical decisions—are providing trustworthy and reliable results.
In analytical method validation, accurate identification and quantification of systematic error is fundamental to establishing method suitability and ensuring data integrity in drug development. Systematic errors, which consistently alter results from true values, manifest primarily as constant or proportional errors. This guide provides a technical framework for differentiating between these error types within Comparison of Methods (COM) experiments, a critical component of analytical method validation. We detail experimental protocols for error detection, statistical methodologies for quantification, and practical strategies for error mitigation, providing researchers and scientists with the tools necessary to enhance the reliability of analytical measurements in pharmaceutical development.
In the context of analytical method validation, a comparative method is used to estimate the inaccuracy or systematic error of a new test method [1]. Systematic error is defined as the difference between a measured value and the unknown true value of a quantity that occurs consistently in the same direction [13] [14]. Unlike random errors, which vary unpredictably and can be reduced by averaging repeated measurements, systematic errors affect all measurements predictably and are not eliminated through replication [5] [14]. This consistent bias makes systematic error particularly problematic in analytical chemistry and drug development, where it can compromise method validity and lead to incorrect conclusions about drug quality, safety, and efficacy.
The Comparison of Methods (COM) experiment serves as the primary approach for assessing systematic error using real patient specimens [1]. In this framework, differences between a test method and a carefully selected comparative method are attributed to the test method, especially when a reference method with documented correctness is used [1]. Systematic errors are clinically significant when they exceed acceptable limits at critical medical decision concentrations, potentially impacting patient diagnosis, treatment monitoring, and therapeutic drug monitoring [1].
Systematic errors are primarily categorized as constant or proportional, a distinction crucial for diagnosing their source and implementing appropriate corrections [1] [13]. A constant error persists as a fixed value regardless of the analyte concentration, while a proportional error changes in magnitude proportionally to the analyte concentration [13]. Understanding this distinction enables researchers to determine whether a method requires recalibration at the zero point (to address constant error) or across the analytical range (to address proportional error), ultimately ensuring the method's fitness for its intended purpose in pharmaceutical analysis.
Theoretical Foundations of Error Types
Characterization of Systematic vs. Random Error
Measurement error is an inherent aspect of all analytical procedures and can be classified into two primary categories: systematic error and random error [14]. The table below summarizes their fundamental characteristics:
Table 1: Characteristics of Systematic and Random Error
| Characteristic | Systematic Error | Random Error |
|---|---|---|
| Definition | Consistent, directional bias in measurements [5] | Unpredictable fluctuations in measurements [5] |
| Cause | Imperfect calibration, instrumental faults, flawed methods [5] [13] | Electronic noise, environmental fluctuations, procedural variations [5] [14] |
| Directional Effect | Always alters results in the same direction [15] [14] | Affects results in both positive and negative directions equally [14] |
| Impact on Results | Affects accuracy (closeness to true value) [14] | Affects precision (reproducibility of measurements) [5] [14] |
| Statistical Mitigation | Not reduced by averaging multiple measurements [14] | Reduced by averaging multiple measurements [14] |
| Detectability | Can be difficult to detect without reference materials [13] | Revealed by variability in repeated measurements [13] |
Differentiating Constant and Proportional Systematic Errors
Systematic errors are further differentiated based on their relationship with the concentration of the analyte being measured.
Constant Error (Offset Error): This error remains fixed in magnitude across the analytical measurement range [13] [14]. It represents a consistent offset or displacement from the true value. A common example is a zero setting error, where an instrument does not read zero when the quantity to be measured is zero [5] [13]. For instance, a balance that consistently reads 1.5 mg when nothing is placed on it introduces a constant error of +1.5 mg to every measurement.
Proportional Error (Scale Factor Error): This error's magnitude changes in proportion to the true value of the analyte concentration [13] [14]. It arises from a multiplicative factor rather than an additive one. An example is a multiplier error in which the instrument consistently reads changes in the quantity greater or less than the actual changes [5]. For example, if a method has a 2% proportional error and the true value is 200 mg/dL, the measured value will be 204 mg/dL (error of +4 mg/dL); if the true value is 100 mg/dL, the measured value will be 102 mg/dL (error of +2 mg/dL) [13].
Complex Errors: In practice, methods often exhibit a combination of both constant and proportional errors. The total systematic error at any given concentration is the sum of the constant error and the proportional error at that concentration [1].
Experimental Design for Error Differentiation
The Comparison of Methods Experiment
The Comparison of Methods (COM) experiment is the cornerstone for estimating systematic error in method validation [1]. The purpose is to analyze patient samples by both a new test method and a comparative method, then estimate systematic errors based on the observed differences [1].
Key Experimental Factors:
Comparative Method Selection: Ideally, a reference method with documented correctness through definitive method comparison or traceable standard materials should be used. Differences are then attributed to the test method [1]. When using a routine comparative method, large, medically unacceptable differences require additional experiments to identify the inaccurate method [1].
Specimen Requirements: A minimum of 40 different patient specimens is recommended, selected to cover the entire working range of the method and represent the expected disease spectrum [1]. Specimen quality and concentration range are more critical than sheer quantity, though 100-200 specimens may be needed to assess method specificity [1].
Replication and Timing: Analysis should be performed in duplicate across multiple runs over at least 5 days to minimize systematic errors from a single run and identify sample-specific issues [1].
Specimen Stability: Specimens should be analyzed within two hours of each other by both methods unless stability data supports other handling conditions. Proper handling is critical to prevent differences due to specimen degradation rather than analytical error [1].
Data Analysis and Graphical Interpretation
Initial Graphical Inspection: Graphing data as it is collected allows for visual error assessment and identification of discrepant results needing confirmation [1].
Difference Plot: For methods expected to show 1:1 agreement, a difference plot (test result minus comparative result on the y-axis versus comparative result on the x-axis) is ideal. Differences should scatter randomly around the zero line. Consistent deviations above or below zero at certain concentrations suggest systematic error [1].
Comparison Plot (Scatter Plot): For methods not expected to show 1:1 agreement, a scatter plot (test result on y-axis versus comparative result on x-axis) is used. A visual line of best fit reveals the general relationship, helping identify outliers and the nature of systematic error [1].
Statistical Analysis for Error Quantification: For data covering a wide analytical range, linear regression analysis (least squares) is preferred to estimate systematic error at medically important decision concentrations and determine the constant and proportional components [1].
The regression line is defined as: ( Yc = a + bXc ), where:
- ( Yc ) = Value estimated by the test method at decision concentration ( Xc )
- ( a ) = Y-intercept (estimates constant error)
- ( b ) = Slope (estimates proportional error)
- ( X_c ) = Medical decision concentration
The systematic error (SE) at the decision concentration is calculated as: ( SE = Yc - Xc ) [1].
Table 2: Interpretation of Linear Regression Parameters in Error Analysis
| Regression Parameter | Mathematical Representation | Interpretation in Error Analysis |
|---|---|---|
| Slope (b) | ( b = \frac{\sum{i=1}^{n}(Xi - \bar{X})(Yi - \bar{Y})}{\sum{i=1}^{n}(X_i - \bar{X})^2} ) | Deviation from 1.0 indicates proportional error. |
| Y-Intercept (a) | ( a = \bar{Y} - b\bar{X} ) | Deviation from 0 indicates constant error. |
| Standard Error of Estimate (sâ‚/â‚“â‚Ž) | ( s{y/x} = \sqrt{\frac{\sum{i=1}^{n}(Yi - \hat{Y}i)^2}{n-2}} ) | Measures random dispersion around the regression line. |
The correlation coefficient (r) is primarily useful for assessing whether the data range is sufficiently wide to provide reliable slope and intercept estimates, not for judging method acceptability. An r value ≥ 0.99 suggests reliable regression estimates [1].
For narrow concentration ranges, calculating the average difference (bias) between methods using a paired t-test is often more appropriate than regression analysis [1].
Visualization of Experimental Workflow
The following diagram illustrates the logical workflow for designing a COM experiment, analyzing data, and differentiating error types using the statistical approaches described.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents, materials, and instrumental solutions essential for conducting robust Comparison of Methods experiments and systematic error analysis in pharmaceutical method validation.
Table 3: Essential Research Reagent Solutions for COM Studies
| Item / Reagent | Function / Purpose | Technical Specification Considerations |
|---|---|---|
| Certified Reference Materials | Provides traceable standards for calibration and accuracy assessment; crucial for identifying systematic error. | Purity certification, metrological traceability, stability documentation. |
| Patient-Derived Specimens | Matrix-matched samples for realistic method comparison across clinical decision levels. | Cover pathological range, appropriate stability, informed consent. |
| Ultra-Pure Water & Solvents | Sample preparation, dilution, and mobile phase preparation for chromatographic methods. | Specified grade (e.g., HPLC, LC-MS), low organic/particulate content. |
| Stable Isotope-Labeled Internal Standards | Normalizes variation in sample preparation and analysis; improves precision and accuracy in LC-MS. | High isotopic purity, co-elution with analyte, minimal matrix effects. |
| Calibration Verification Materials | Independent materials not used in calibration to verify method accuracy post-calibration. | Commutability with patient samples, target values with uncertainty. |
| UFLC-DAD System | High-separation efficiency analysis for specificity/selectivity assessment in complex matrices. | Detector linearity, pressure limits, injection precision, DAD spectral resolution. |
| UV-Vis Spectrophotometer | Economical quantitative analysis; used for accuracy and linearity assessment where applicable. | Wavelength accuracy, photometric linearity, stray light specification. |
| Statistical Analysis Software | Performs linear regression, t-tests, ANOVA, and calculates measurement uncertainty. | Validated algorithms, GMP/GLP compliance features, audit trail capability. |
| Kopsinine | Kopsinine, CAS:559-51-3, MF:C21H26N2O2, MW:338.4 g/mol | Chemical Reagent |
| KPT-6566 | RORγ Inverse Agonist|2-[[4-[[[4-(tert-Butyl)phenyl]sulfonyl]imino]-1-oxo-1,4-dihydro-2-naphthyl]thio]acetic Acid | 2-[[4-[[[4-(tert-Butyl)phenyl]sulfonyl]imino]-1-oxo-1,4-dihydro-2-naphthyl]thio]acetic Acid is a potent RORγ inverse agonist for autoimmune disease research. For Research Use Only. Not for human or veterinary use. |
Statistical Analysis and Error Quantification
Advanced Regression Analysis
While simple linear regression is commonly used in COM studies, advanced regression techniques may be necessary when certain assumptions are violated. Deming regression and Passing-Bablok regression account for measurement error in both methods, providing more reliable estimates of constant and proportional error when the comparative method is not a definitive reference method. These methods are particularly valuable when the correlation coefficient (r) is less than 0.99, indicating a narrow data range relative to method imprecision [1].
Total Error Approach
Modern method validation emphasizes a total error approach, which combines both systematic error (bias) and random error (imprecision) to assess overall method suitability [16]. This approach acknowledges that both error types impact the usefulness of analytical results. Statistical tolerance intervals that cover a specified proportion (beta) of future measurements with a defined confidence level are used to ensure the total error remains within acceptable limits at critical decision concentrations [16]. This framework formally controls the risk of accepting unsuitable analytical methods, unlike traditional ad-hoc acceptance criteria [16].
Error Propagation in Calculations
Understanding how constant and proportional errors propagate through calculations is essential. The rules of error propagation demonstrate that:
- For addition/subtraction, absolute errors (characteristic of constant error) are added [15].
- For multiplication/division, relative or percentage errors (characteristic of proportional error) are added [15].
- For powers, the relative error is multiplied by the power [15].
These principles allow researchers to predict how errors in raw measurements will affect final calculated results in pharmaceutical analysis.
Case Study: Error Analysis in Pharmaceutical Validation
A recent study comparing Ultra-Fast Liquid Chromatography-Diode Array Detector (UFLC−DAD) and spectrophotometric methods for quantifying metoprolol tartrate (MET) in tablets provides a practical example of systematic error assessment in pharmaceutical method validation [17].
Experimental Protocol:
- Methods Compared: UFLC−DAD (test method) and UV spectrophotometry (comparative method).
- Analyte: Metoprolol tartrate extracted from commercial 50 mg and 100 mg tablets.
- Validation Parameters: Specificity/selectivity, sensitivity, linearity, range, accuracy, precision, and robustness were assessed for both methods [17].
- Statistical Analysis: ANOVA and Student's t-test at 95% confidence level were used to compare results from both methods [17].
Results and Error Interpretation: The UFLC−DAD method demonstrated superior specificity and could analyze both 50 mg and 100 mg tablets, while the spectrophotometric method was limited to 50 mg tablets due to concentration limitations [17]. Statistical analysis revealed no significant difference between the methods for the 50 mg tablets, indicating that systematic error between the methods was not statistically or medically significant for this formulation [17]. This finding validates the use of the simpler, more economical spectrophotometric method for quality control of the 50 mg tablets, demonstrating how COM studies can guide resource-efficient analytical practices without compromising data quality.
Mitigation Strategies for Systematic Errors
Reducing Constant Error
- Regular Calibration: Frequently compare instrument readings with known standard quantities, particularly at zero concentration, to identify and correct offset errors [13] [14].
- Method of Standard Additions: This technique accounts for constant matrix effects that may cause interference by adding known amounts of analyte to the sample [13].
- Blank Correction: Consistently measure and subtract the blank signal from all sample measurements to eliminate constant background interference [13].
Reducing Proportional Error
- Calibration Across Working Range: Use multiple calibration standards across the entire analytical measurement range to establish a proper response curve and correct for proportional effects [13].
- Internal Standardization: Use internal standards that closely mimic the analyte's behavior to correct for proportional losses during sample preparation or analysis [17].
- Instrument Linearity Verification: Regularly verify that instrument response is proportional to analyte concentration throughout the claimed working range [17].
General Approaches for Both Error Types
- Method Triangulation: Use multiple analytical techniques or instruments to measure the same samples; consistent differences suggest systematic error in one method [14].
- Participate in Proficiency Testing: Analyze external quality control samples with values assigned by reference methods to identify unrecognized systematic error [1].
- Robustness Testing: Deliberately vary key method parameters (e.g., temperature, pH, mobile phase composition) during validation to identify sources of systematic error before routine use [17].
Differentiating between constant and proportional systematic error is not merely an academic exercise but a practical necessity in analytical method validation for drug development. Through carefully designed Comparison of Methods experiments, appropriate statistical analysis, and informed interpretation of regression parameters, researchers can accurately characterize the nature and magnitude of systematic error. This understanding directly informs effective mitigation strategies, ensuring that analytical methods produce reliable, accurate data suitable for regulatory submission and quality control. As the pharmaceutical industry advances with increasingly complex therapeutics, robust error analysis remains fundamental to demonstrating method suitability, ultimately protecting patient safety and ensuring drug efficacy.
In the tightly regulated pharmaceutical environment, the comparative method is a critical, structured process for evaluating the performance of a new or modified analytical procedure against an established one. This methodology is foundational to ensuring that data generated for product quality attributes remains reliable, consistent, and defensible when analytical methods evolve. Framed within a broader thesis on analytical method validation research, the comparative method is not a standalone validation activity but an integral component of a holistic Analytical Procedure Lifecycle Management strategy [18]. Its core function is to provide a scientific and statistical basis for concluding whether a new method can successfully replace an existing one without compromising the quality, safety, or efficacy assessment of the drug product.
The need for comparative studies arises from the dynamic nature of drug development and manufacturing. Changes are inevitable, whether driven by technology upgrades (e.g., transitioning from HPLC to UHPLC), process improvements, or regulatory updates [18]. In such cases, simply validating the new method according to regulatory guidelines like ICH Q2 is necessary but insufficient. Validation demonstrates that a method is capable of performing as intended for its new, isolated application. In contrast, a comparative study demonstrates that the new method performs equivalently to, or better than, the legacy method that was used to generate the original stability and specification data [7]. This direct comparison is what underpins the continuity of data packages submitted to regulatory agencies and ensures that patient safety is protected through consistent product quality monitoring.
Conceptual Framework: Comparability vs. Equivalency
Within the sphere of the comparative method, a crucial distinction exists between "comparability" and "equivalency." These terms are often used interchangeably, but they represent distinct concepts with different regulatory implications, as highlighted in industry discussions and regulatory guidance [18] [7].
Analytical Method Comparability: This is a broader evaluation to determine if a modified method yields results that are sufficiently similar to the original method to ensure consistent product quality. It is typically employed for lower-risk procedural changes where the fundamental methodology remains largely unchanged. A successful comparability study confirms that the modified procedure produces the expected results and that product quality decisions remain unaffected. These changes often fall under internal change control and may not require immediate regulatory filings [18].
Analytical Method Equivalency: This is a more rigorous, formal subset of comparability. It involves a comprehensive assessment, often requiring full validation of the new method, to demonstrate that a replacement method performs equal to or better than the original. Equivalency studies are necessary for high-risk changes, such as replacing a method with one based on a completely different separation mechanism or detection technique. Such changes require regulatory approval prior to implementation [18] [7].
The International Consortium for Innovation and Quality in Pharmaceutical Development (IQ) working group further refined this distinction, noting that "equivalency" may be restricted to a formal statistical study to evaluate similarities in method performance characteristics or the results generated for the same samples [7].
Table 1: Distinguishing Between Comparability and Equivalency
| Feature | Comparability | Equivalency |
|---|---|---|
| Scope | Broader evaluation of method performance | Formal, statistical demonstration of equivalence |
| Risk Level | Low to Moderate | High |
| Typical Triggers | Minor modifications within the method's design space | Replacement of a method; major changes to methodology |
| Regulatory Impact | Often managed via internal change control; may not require a immediate filing | Requires prior regulatory approval |
| Study Rigor | May leverage prior knowledge and robustness data | Requires a comprehensive side-by-side study, often with full validation of the new method |
Visualizing the Decision Workflow
The following diagram illustrates the logical decision process for determining when and how to implement a comparative method study within a risk-based framework.
Regulatory Landscape and Current Industry Practice
Despite its critical importance, the regulatory landscape for analytical method comparability is less clearly defined than for initial method validation. While clear guidelines like ICH Q2(R2) exist for validation, specific guidance on how or when to perform comparability or equivalency studies is sparse [7]. Regulatory documents, such as the FDA's 2003 draft guidance on Comparability Protocols, indicate that the need for and extent of an equivalency study depends on the proposed change, product type, and the test itself [7]. This lack of prescriptive detail has led to a wide range of practices across the pharmaceutical industry.
A survey conducted by the IQ Consortium revealed several key insights into current industry practices concerning HPLC assay and impurities methods [7]:
- 68% of participants viewed "comparability" and "equivalency" as two different concepts.
- 79% of companies lacked specific standard operating procedures (SOPs) dedicated to analytical method comparability, though over half addressed it within general change control policies.
- 47% of participants had received questions from health authorities on comparability packages, indicating regulatory scrutiny in this area.
- 100% of participants evaluated the need for a comparability or equivalency study when a method change was made, with 63% using a risk-based approach to determine its necessity.
Table 2: Industry Practices for Method Comparability (Based on IQ Survey)
| Practice Area | Survey Finding | Implication |
|---|---|---|
| Terminology Understanding | 68% distinguish between comparability and equivalency | Industry recognizes a nuanced, risk-based approach. |
| Internal Governance | 79% lack specific SOPs for comparability | Practices are often decentralized or embedded in other procedures. |
| Regulatory Scrutiny | 47% have received regulatory questions | Agencies are actively reviewing comparability justifications. |
| Risk-Based Application | 63% do not require studies for all changes | A risk-based approach is widely adopted for efficiency. |
The introduction of ICH Q14: Analytical Procedure Development formalizes a more structured, lifecycle approach. It encourages a science- and risk-based framework for developing, validating, and managing analytical procedures, which inherently includes managing changes through comparability and equivalency studies [18]. A harmonized industry approach, as championed by groups like the IQ Consortium, can reduce regulatory filing burdens and encourage the adoption of innovative analytical technologies.
Designing a Method-Comparison Study: Detailed Experimental Protocols
A well-designed method-comparison study is paramount for generating defensible data. The core principle is that the two methods must measure the same underlying quality attribute (e.g., assay potency or impurity content) [19]. The following protocols detail the key experiments for a robust comparability/equivalency study.
Protocol for Sample Analysis and Data Collection
The foundation of any comparison is the direct, side-by-side testing of samples using both the original and new methods [18].
1. Objective: To generate paired data sets from both methods that represent the expected range of the product's quality attributes.
2. Materials and Reagents:
- Representative Drug Substance/Product Samples: A minimum of three independent batches is recommended to capture product and process variability [7]. These should include lots that span the expected manufacturing range (e.g., from low to high potency if possible).
- Reference Standards: Qualified and traceable reference standards for the analyte of interest.
- Mobile Phases/Reagents: Prepared according to both the old and new analytical procedures.
3. Procedure:
- Prepare samples and standards according to both methods' procedures.
- Analyze all selected sample batches using both the original method and the new method.
- The order of analysis should be randomized to avoid systematic bias (e.g., time-based degradation of samples or reagents) [19].
- For each sample, the two analyses should be performed as closely in time as possible ("simultaneous sampling") to ensure the analyte has not changed [19].
- A sufficient number of replicate injections per sample should be performed to allow for a meaningful assessment of precision.
Protocol for Statistical Evaluation and Data Interpretation
Once paired data is generated, statistical tools are used to quantify the agreement between the two methods.
1. Objective: To statistically determine the bias and the limits of agreement between the original and new methods.
2. Methodology:
- Data Pairing: For each sample, record the result from the original method (Method A) and the new method (Method B). The unit of analysis is the difference between the paired results.
- Bland-Altman Analysis: This is a recommended statistical approach for method-comparison [19].
- Calculate the difference between the two methods for each pair (e.g., New Method - Original Method).
- Calculate the average of the two methods for each pair ([Method A + Method B]/2).
- Plot the differences (y-axis) against the averages (x-axis) to create a Bland-Altman plot.
- Calculate the bias (the mean of all the differences).
- Calculate the standard deviation (SD) of the differences.
- Determine the Limits of Agreement (LOA) as Bias ± 1.96 SD.
3. Interpretation:
- The bias indicates the systematic difference between the methods. A bias of zero means no average difference.
- The LOA defines the range within which 95% of the differences between the two methods are expected to lie.
- The clinical or quality impact is assessed by comparing the LOA to pre-defined acceptance criteria. These criteria should be based on the method's performance requirements and the product's Critical Quality Attributes (CQAs) [18] [19]. If the LOA falls entirely within a clinically or quality-acceptable range, the two methods can be considered equivalent.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key research reagent solutions and materials essential for conducting a method-comparison study for a chromatographic method.
Table 3: Essential Materials for a Method-Comparison Study
| Item | Function & Importance in Comparative Studies |
|---|---|
| Representative Sample Batches | Provides a matrix that captures real-world variability. Using multiple, independent batches is critical to demonstrate that equivalency holds across the product manufacturing range. |
| Qualified Reference Standards | Serves as the benchmark for quantifying the analyte in both methods. Ensures that any observed differences are due to the method and not the standard. |
| Method-Specific Mobile Phases & Buffers | Prepared exactly as specified in each procedure. Differences in pH, ionic strength, or organic composition can significantly impact chromatographic separation and results. |
| System Suitability Test (SST) Solutions | Verifies that the chromatographic system (for each method) is performing adequately before the comparative analysis is initiated, ensuring data integrity. |
| Stability-Indicating Solutions | (e.g., stressed samples) May be used to demonstrate that the new method has equivalent or better ability to separate degradants from the main peak, a key aspect for stability-indicating methods. |
| L-669083 | L-669083, CAS:130007-52-2, MF:C29H29IN4O5S, MW:672.5 g/mol |
| KT5823 | KT5823, CAS:126643-37-6, MF:C29H25N3O5, MW:495.5 g/mol |
Integrating the comparative method into the overall validation plan requires a proactive, risk-based strategy. The principles of Quality by Design (QbD) should be applied from the method development stage. This involves defining an Analytical Target Profile (ATP) which outlines the required performance characteristics of the method [18]. A well-developed method, with a understood design space established through robustness testing, is inherently more manageable when changes become necessary. A change within the method's design space might only require a comparability assessment, while a change outside the design space would likely trigger a full equivalency study [18] [7].
The risk assessment should consider:
- Impact on Product Quality: The criticality of the test method to the determination of product CQAs.
- Extent of the Change: A minor change (e.g., column dimensions within defined limits) is lower risk than a major change (e.g., a different chromatographic technique).
- Stage of Product Lifecycle: Changes post-approval are typically more stringently controlled than those during clinical development.
By embedding comparability and equivalency studies as formal components within the change management system, pharmaceutical companies can ensure that method improvements and technology transfers are executed efficiently, with maintained regulatory compliance and unwavering assurance of product quality and patient safety.
Executing a Comparison of Methods Study: Experimental Design and Analysis
Within the framework of comparative analytical method validation research, the principles of experimental design are paramount for generating reliable, reproducible, and defensible scientific data. This technical guide provides an in-depth examination of three foundational pillars of robust experimentation: determining specimen number (sample size), executing proper specimen selection, and ensuring specimen stability. In comparative studies, where the goal is to objectively evaluate the performance of one analytical method against another or against a standardized benchmark, a flawed design in any of these areas can compromise the entire validation process [20] [17]. A well-considered design not only controls for variability and bias but also ensures that the study is powered to detect scientifically meaningful differences, thereby upholding the integrity of the conclusions drawn regarding method equivalence, superiority, or compliance [21].
The following sections will dissect each of these core components, providing detailed methodologies, structured data presentation, and visual workflows tailored for researchers, scientists, and professionals in drug development and related fields.
Foundational Principles of Experimental Design
The statistical design of experiments is guided by several key principles that work in concert to enhance the validity and efficiency of research. These principles are critical for managing uncertainty and ensuring that observed effects are attributable to the variables under investigation rather than to confounding factors [21] [22].
- Replication: Repeating the experiment or measurements multiple times increases the reliability of the results and provides a more precise estimate of experimental error. Natural variability is always present; replication is essential for understanding this variability and for increasing the rigor of the findings [21].
- Randomization: The random assignment of treatments or specimens to experimental units is crucial for spreading unspecified and potential confounding variables evenly across all treatment groups. This process ensures the validity of statistical inference by mitigating biases that could arise from systematic differences between groups [21] [22]. For instance, in visual science, treatments might be randomly assigned to different groups of patients or the order of treatment might be randomized [21].
- Blocking: This technique involves grouping experimental units that are similar to one another (e.g., eyes from the same subject, animals from the same litter) into blocks. By comparing treatments within these homogenous blocks, the known but irrelevant sources of variation are reduced, leading to greater precision in estimating the treatment effects [21] [22].
- Multifactorial Design: Instead of varying one factor at a time, a more efficient approach is to study multiple factors simultaneously. This design allows for the investigation of interaction effects—where the effect of one factor depends on the level of another factor—providing a more comprehensive understanding of the system [21].
- Sequential Approach: Dedicating only a portion of the overall research budget and plan to an initial experiment is a prudent strategy. The results from one experiment inform and refine the subsequent experimental steps, allowing for a more adaptive and efficient research process [21].
Specimen Number: Power and Sample Size
Determining the appropriate number of specimens, or sample size, is a critical step in the planning phase of any experiment. This process, known as a power analysis, ensures that the study has a high probability of detecting a treatment effect if one truly exists, thereby minimizing the risk of false-negative (Type II) errors [21].
The Importance of Power Analysis
A well-executed power analysis is essential for both practical and ethical reasons. An underpowered study (with too few specimens) may fail to uncover meaningful effects, wasting resources and potentially halting promising research avenues. Conversely, an overpowered study (with more specimens than necessary) can be a wasteful use of resources and may unnecessarily expose subjects to risk [21]. Furthermore, funding agencies and scientific journals now increasingly require rigorous power justifications to ensure that the proposed research is feasible and likely to yield interpretable results [21].
Key Factors Influencing Sample Size
The required sample size in an experiment is influenced by several interconnected factors, whose relationships are summarized in the table below.
Table 1: Factors Affecting Sample Size Determination in Experimental Design
| Factor | Description | Relationship to Sample Size |
|---|---|---|
| Statistical Power | The probability that a test will correctly reject a false null hypothesis (typically set at 80% or higher). | Sample size increases with higher desired power [21]. |
| Effect Size | The magnitude of the difference or effect that is considered scientifically or clinically meaningful. | Sample size increases as the detectable difference becomes smaller [21]. |
| Measurement Variability | The inherent variance or standard deviation in the measured response. | Sample size increases proportionally to the variance [21]. |
| Type I Error (α) | The probability of incorrectly rejecting a true null hypothesis (false positive), often set at 0.05. | Sample size increases with a more stringent (smaller) α value [21]. |
| Test Directionality | Whether the statistical test is one-sided or two-sided. | Two-sided tests, which do not assume the direction of the effect, require a larger sample size than one-sided tests [21]. |
Conducting a Power Analysis
The process typically involves using specialized software (e.g., G*Power, Lenth's applets) to calculate the required sample size based on the anticipated effect size, estimated variability, and chosen levels for power and significance [21]. This analysis provides perspective on whether a well-designed experiment is feasible with the available resources and helps to formally justify the number of specimens included in the study.
Specimen Selection: Randomization and Blocking
The process of selecting and assigning specimens to experimental groups is as crucial as determining the total number. Proper methodology here directly controls for selection bias and confounding variables.
Randomization Techniques
Randomization is the cornerstone for ensuring the validity of causal inference. Several designs can be employed:
- Completely Randomized Design: Every experimental subject or specimen is assigned to a treatment group entirely at random, using tools like random number generators. This is the simplest form of randomization [23].
- Randomized Block Design: Also known as stratified random design, this approach involves first grouping specimens based on a shared characteristic (e.g., age, sex, baseline severity, batch of raw material) that is expected to influence the response. Random assignment to treatments is then performed within each of these blocks. This method controls for the known variability introduced by the blocking factor, leading to more precise comparisons [21] [23].
Between-Subjects vs. Within-Subjects Designs
The unit of assignment and measurement is another critical consideration in specimen selection.
- Between-Subjects Design: Each individual specimen or subject receives only one level of the experimental treatment. This design requires a larger total sample size to achieve the same power as a within-subjects design but avoids potential carryover effects [23].
- Within-Subjects Design: Each individual specimen or subject receives all experimental treatments consecutively, with their response measured for each. This design, also known as a repeated measures design, is highly efficient as it uses each subject as its own control, thereby eliminating variability between subjects and reducing the required sample size. Counterbalancing (randomizing the order of treatments) is essential in this design to control for order effects [21] [23].
Table 2: Comparison of Experimental Assignment Designs
| Feature | Between-Subjects Design | Within-Subjects Design |
|---|---|---|
| Treatment Assignment | Each subject receives only one treatment. | Each subject receives all treatments. |
| Sample Size Requirement | Larger | Smaller |
| Key Advantage | Avoids carryover effects. | Controls for subject-to-subject variability; greater statistical power. |
| Key Consideration | Requires careful randomization to ensure group equivalence. | Requires counterbalancing to control for order effects. |
| Example | Subjects randomly assigned to either a control group or a single treatment group. | The same subject is measured for performance after receiving a placebo, a low dose, and a high dose of a drug, in a randomized order. |
Specimen Stability: Ensuring Data Integrity
In analytical chemistry and pharmaceutical development, the stability of specimens and solutions is a critical component of method validation. It ensures that the analytical results obtained are an accurate reflection of the sample at the time of collection and are not artifacts of degradation during storage or processing [24].
Leading Principles of Stability Assessment
Stability in a bioanalytical context refers not only to the chemical integrity of the molecule but also to the constancy of the analyte concentration over time. This can be affected by solvent evaporation, adsorption to containers, precipitation, or changes in immunoreactivity for large molecules [24]. The core principle is that all conditions encountered during sample collection, storage, and processing must be demonstrated to ensure stability. The storage duration assessed during validation should be at least equal to the maximum anticipated storage period for any individual study sample [24].
Key Types of Stability Assessments
A comprehensive stability assessment covers all relevant conditions, as outlined in the table below.
Table 3: Key Stability Assessments in Bioanalytical Method Validation
| Stability Type | Description | Typical Acceptance Criteria |
|---|---|---|
| Bench-Top Stability | Evaluates analyte stability in the biological matrix at ambient temperature for the expected duration of sample processing. | Deviation from reference value ≤ 15% (chromatography) or ≤ 20% (ligand-binding assays) [24]. |
| Freeze/Thaw Stability | Assesses stability after multiple (e.g., 3-5) cycles of freezing and thawing. | Deviation from reference value ≤ 15% (chromatography) or ≤ 20% (ligand-binding assays) [24]. |
| Long-Term Frozen Stability | Determines stability in the biological matrix at the intended storage temperature (e.g., -20°C or -70°C). | Deviation from reference value ≤ 15% (chromatography) or ≤ 20% (ligand-binding assays) [24]. |
| Stock Solution Stability | Assesses stability of the analyte in stock solution under storage (e.g., refrigerated) and bench-top conditions. | Deviation from reference value ≤ 10% [24]. |
| Solution Stability | For HPLC/GC, evaluates standard and sample solutions in the prepared diluent over time in an autosampler or refrigerator. | For Assay: % Difference in Response Factor ≤ 2.0% [25].For Related Substances: No new peak ≥ Quantitation Limit; % difference for known impurities within set limits (e.g., ≤ 10%) [25]. |
Detailed Protocol: Solution Stability for Assay by HPLC
The following is a standardized protocol for establishing the stability of standard and sample solutions used in an assay method, crucial for ensuring the validity of analytical runs that may span several hours or days [25].
- Preparation: Prepare the standard and sample solutions as per the analytical method procedure.
- Aliquoting: Label six vials as V0 (initial), V1, V2, V3, V4, and V5. Transfer the solution into each vial.
- Time Points: Analyze the solutions at specified intervals, for example: V0 at 0 hours, V1 at 12 hours, V2 at 24 hours, V3 at 36 hours, V4 at 48 hours, and V5 at 60 hours.
- Analysis: At each time point, prepare a fresh standard solution and inject it in six replicates. Then, inject the corresponding stability solution (e.g., V1) in duplicate.
- Calculation:
- Calculate the Response Factor (RF) for each injection: RF = Area Response / Concentration.
- Calculate the average RF for the fresh standard (RFfresh) and for the stability solution (RFstability).
- Calculate the percentage difference:
% RF Difference = ( |RF_fresh - RF_stability| / ((RF_fresh + RF_stability)/2) ) * 100
- Acceptance Criterion: The solution is considered stable at a given time point if the % RF Difference is ≤ 2.0% [25].
The Comparative Method Validation Framework
In analytical chemistry, comparative method validation research involves systematically evaluating a new method (the "test method") against an established reference method to demonstrate its suitability for the intended purpose. The experimental design principles discussed are integral to this framework, ensuring the comparison is fair, unbiased, and scientifically sound [20] [17].
Experimental Workflow for Comparative Validation
A typical workflow for a comparative analytical method validation study, integrating the core elements of specimen number, selection, and stability, is visualized below.
Diagram 1: Comparative Method Validation Workflow
Application of Principles in Comparative Studies
- Specimen Number: The sample size for the comparison must be sufficient to provide adequate power for statistical tests (e.g., Student's t-test, ANOVA) used to evaluate differences in accuracy, precision, or other key parameters between the two methods [21] [17]. Underpowered comparisons may lead to incorrect conclusions about method equivalence.
- Specimen Selection: Specimens used in the comparison should be representative of the future routine samples and should be assigned for analysis by the two methods in a randomized order to prevent systematic bias. A randomized block design might be used if specimens come from different sources or batches [21] [23].
- Specimen Stability: The integrity of the comparison relies on the analyte remaining unchanged during the analysis. If one method is slower or requires different sample preparation, stability must be demonstrated for the entire process duration for both methods. For instance, solution stability must cover the time a sample resides in the autosampler for each method [24] [25].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials commonly used in experiments for analytical method validation, along with their critical functions.
Table 4: Essential Research Reagent Solutions and Materials
| Item | Function in Experimental Context |
|---|---|
| Certified Reference Standard | Provides a highly characterized substance with known purity and identity, serving as the benchmark for quantifying the analyte in samples and for preparing calibrators [17] [24]. |
| Internal Standard (IS) | A compound added in a constant amount to all samples, calibrators, and quality controls. It corrects for variability in sample preparation, injection volume, and instrument response, improving accuracy and precision [24]. |
| Appropriate Biological Matrix | The blank biological fluid or tissue (e.g., plasma, serum, urine) used to prepare calibrators and quality control samples. It should mimic the composition of the actual study samples to ensure accurate assessment of specificity and potential matrix effects [24]. |
| Quality Control (QC) Samples | Spiked samples with known concentrations of the analyte at low, medium, and high levels within the calibration range. They are analyzed alongside unknown samples to monitor the method's accuracy, precision, and stability over time [24]. |
| Chromatographic Solvents & Mobile Phases | High-purity solvents and buffers used to prepare mobile phases and sample diluents. Their composition, pH, and purity are critical for achieving optimal separation, peak shape, and detector response in chromatographic methods [17] [25]. |
| Stabilizers | Reagents (e.g., enzyme inhibitors, antioxidants, chelating agents) added to biological samples or solutions to prevent analyte degradation, adsorption, or other changes during storage and processing [24]. |
| KU-0060648 | KU-0060648, CAS:881375-00-4, MF:C33H34N4O4S, MW:582.7 g/mol |
| L-685458 | L-685458, CAS:292632-98-5, MF:C39H52N4O6, MW:672.9 g/mol |
The rigorous application of sound experimental design principles pertaining to specimen number, selection, and stability forms the bedrock of credible comparative analytical method validation research. By systematically addressing sample size through power analysis, controlling bias via randomization and blocking, and ensuring data integrity through comprehensive stability testing, scientists can generate high-quality, reproducible data. This structured approach not only fulfills regulatory expectations but also builds a solid scientific foundation for making confident decisions about the validity and applicability of new analytical methods, ultimately contributing to the advancement of drug development and pharmaceutical quality control.
In analytical method validation, the comparison of methods experiment is a critical study designed to estimate the inaccuracy or systematic error of a new test method against a comparative method [1]. The fundamental principle of this experiment involves analyzing patient samples using both the new method and a comparative method, then estimating systematic errors based on the observed differences [1]. The reliability of this assessment hinges on two crucial design elements: the replication strategy for measurements (single vs. duplicate) and the timeframe over which data is collected. These factors directly impact the ability to distinguish true systematic error from random variability and ensure the findings are robust under typical laboratory operating conditions.
Foundational Concepts: Replicates and Repeats
Understanding the distinction between replicates and repeats is essential for proper experimental design in method validation studies.
Definitions and Key Differences
A repeat measurement is taken during the same experimental run or consecutive runs, while a replicate measurement is taken during identical but different experimental runs, which are often randomized [26]. The core difference lies in the sources of variability they capture. Repeats, being intra-run, primarily capture the narrow variability within a single analytical session. Replicates, being inter-run, include broader sources of variability such as changes in equipment settings between runs, different reagent lots, environmental fluctuations, and operator variability over time [26].
Statistical Implications for Inference
The statistical interpretation of data differs significantly based on the replication approach. True replicates (independent experimental runs) provide a valid basis for calculating confidence intervals and performing significance tests because they represent independent measurements of the experimental effect [27]. Conversely, repeat measurements (within the same run) cannot support formal statistical inference about the hypothesis because they are not independent tests; they primarily monitor the performance or precision of that specific experimental run [27]. As stated in fundamental principles of statistical design, "Science is knowledge obtained by repeated experiment or observation: if n = 1, it is not science, as it has not been shown to be reproducible. You need a random sample of independent measurements" [27].
Single vs. Duplicate Measurements: Experimental Protocols
Standard Protocol for Single Measurements
The common practice in comparison of methods experiments is to analyze each specimen singly by both the test and comparative methods [1]. This approach is resource-efficient, allowing more specimens to be analyzed within constrained budgets and timelines. However, this efficiency comes with significant risks. With single measurements, there is no internal check for measurement validity, making the data vulnerable to uncorrected errors from sample mix-ups, transcription mistakes, or transient instrument glitches [1]. A single such error can disproportionately influence the statistical conclusions, particularly in studies with smaller sample sizes.
Enhanced Protocol for Duplicate Measurements
The duplicate measurement protocol involves analyzing two different aliquots of each patient specimen by both the test and comparative methods [1]. For optimal design, these duplicates should be processed as true replicates—different samples analyzed in different runs or at least in different analytical orders—rather than as back-to-back replicates on the same cup of sample [1]. This approach provides a robust mechanism for error detection by identifying discrepancies through paired results. Duplicate analyses confirm whether observed discrepancies are reproducible errors attributable to the method rather than isolated mistakes, significantly enhancing data reliability [1].
Decision Framework and Recommendations
The choice between single and duplicate measurements involves balancing resource constraints against data quality requirements. For methods with demonstrated high precision and stability, single measurements may suffice when analyzing a larger number of well-distributed specimens. However, duplicate measurements are strongly recommended when validating methods with unknown precision characteristics, when specimen volume is limited, when the method is prone to interference, or when the experimental design involves fewer specimens [1]. If duplicates cannot be performed, the protocol must include immediate data inspection with repeat analysis of discrepant results while specimens are still available [1].
Table 1: Comparison of Single vs. Duplicate Measurement Approaches
| Feature | Single Measurements | Duplicate Measurements |
|---|---|---|
| Resource Requirement | Lower (cost and time) | Higher (approximately double) |
| Error Detection Capability | Limited | Robust |
| Impact of Outliers | High risk | Mitigated through verification |
| Data Reliability | Conditional on no procedural errors | Enhanced through internal validation |
| Recommended Scenario | High-precision methods with large N | New methods, limited specimens, or complex matrices |
Timeframe Considerations: Experimental Protocols
Minimum Timeframe Requirements
The comparison of methods experiment should be conducted over multiple analytical runs on different days to minimize the impact of systematic errors that might occur in a single run [1]. A minimum of 5 days is recommended by guidelines to adequately capture day-to-day variability [1]. Extending the study over a longer period, such as 20 days, provides a more comprehensive assessment of method performance under realistic operating conditions. This extended timeframe allows the incorporation of expected routine variations such as different reagent lots, calibration events, multiple operators, and seasonal environmental changes.
Integrated Protocol with Long-Term Studies
A strategically efficient approach involves synchronizing the comparison study with the long-term replication study, which typically extends for 20 days [1]. This integrated design requires only 2-5 patient specimens per day while providing data that reflects both between-method differences (comparison) and within-method variability over time (replication) [1]. This approach efficiently utilizes resources while generating a comprehensive dataset that reflects real-world performance.
Specimen Stability Considerations
The experimental timeframe must account for specimen stability. Specimens should generally be analyzed within two hours of each other by the test and comparative methods unless the analytes are known to have shorter stability (e.g., ammonia, lactate) [1]. For less stable analytes, appropriate preservation techniques such as adding preservatives, separating serum/plasma from cells, refrigeration, or freezing must be implemented [1]. specimen handling protocols must be rigorously defined and systematized before beginning the study to ensure that observed differences truly represent systematic analytical errors rather than artifacts of specimen deterioration [1].
Table 2: Timeframe Considerations for Method Comparison Studies
| Factor | Minimum Recommendation | Optimal Recommendation |
|---|---|---|
| Study Duration | 5 days | 20 days (aligned with precision studies) |
| Runs per Day | Multiple runs if possible | Multiple runs with different operators |
| Specimens per Day | Sufficient to complete 40+ specimens | 2-5 specimens distributed across study period |
| Specimen Stability Measure | Analyze test/comparative methods within 2 hours | Implement preservation for unstable analytes |
| Environmental Coverage | Basic day-to-day variation | Multiple operators, reagent lots, calibration events |
Data Analysis and Presentation
Graphical Data Analysis
The initial analysis should include visual inspection of graphed data as it is collected [1]. For methods expected to show one-to-one agreement, a difference plot (test result minus comparative result versus comparative result) is ideal [1]. For methods not expected to show identical results, a comparison plot (test result versus comparative result) is more appropriate [1]. This graphical approach helps identify discrepant results early, allowing for repeat analysis while specimens are still available. Difference plots readily reveal patterns suggesting constant or proportional systematic errors when points scatter non-randomly across concentrations [1].
Statistical Analysis
For data covering a wide analytical range, linear regression statistics (slope, y-intercept, standard deviation about the regression line) are preferred as they allow estimation of systematic error at multiple medical decision concentrations and provide information about the proportional or constant nature of the error [1]. The systematic error (SE) at a specific medical decision concentration (Xc) is calculated as SE = Yc - Xc, where Yc is the value obtained from the regression line equation Yc = a + bXc [1]. The correlation coefficient (r) is mainly useful for assessing whether the data range is sufficiently wide to provide reliable estimates of slope and intercept, with values ≥0.99 indicating adequate range [1]. For narrow concentration ranges, calculating the average difference (bias) between methods with the standard deviation of differences is more appropriate [1].
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Method Validation Studies
| Item | Function/Application |
|---|---|
| Certified Reference Materials | Provides traceability to definitive methods for establishing correctness of comparative method [1] |
| Patient Specimens | 40+ specimens covering entire working range and disease spectrum for real-world performance assessment [1] |
| Preservation Reagents | Stabilizes labile analytes (e.g., anticoagulants, protease inhibitors) to maintain specimen integrity [1] |
| Quality Control Materials | Monifies method performance stability throughout data collection period [1] |
| Calibrators | Ensures both test and comparative methods are properly standardized throughout study [1] |
| FPS-ZM1 | FPS-ZM1|RAGE Inhibitor|For Research Use |
| L 748780 | L 748780, CAS:168086-64-4, MF:C19H14Cl3NO4, MW:426.7 g/mol |
Workflow Visualization
The following diagram illustrates the key decision points and workflow for designing the data collection strategy in a comparison of methods experiment:
The design of data collection in comparative method validation requires careful consideration of measurement replication strategy and study timeframe. While single measurements offer efficiency, duplicate measurements provide essential error detection and data verification capabilities. Similarly, extending the study across multiple days incorporates realistic sources of variability, producing more generalizable results. The optimal design balances practical constraints with the need for reliable, actionable data that can support confident decisions about method suitability for its intended purpose. By implementing these protocols with appropriate statistical analysis, researchers can generate robust evidence of method performance that stands up to scientific and regulatory scrutiny.
In analytical method validation research, comparative methods are fundamental for establishing the reliability, accuracy, and precision of new analytical procedures against a reference or standard method. These comparisons are vital in drug development, where they underride decisions regarding drug safety, efficacy, and quality control. Graphical data analysis, particularly through difference plots and comparison plots, transforms numerical data into visual evidence, allowing researchers to intuitively assess agreement, identify biases, and detect trends or outliers that might not be apparent from statistical summaries alone [28]. This technical guide provides an in-depth examination of these core visualization techniques, detailing their methodologies, applications, and interpretation within the rigorous context of analytical validation.
These plots serve as powerful tools for communicating complex comparative findings in a format that is accessible to scientists, regulators, and other stakeholders. They make the invisible patterns in data visible, harnessing the human visual system's superior ability to detect relationships and anomalies [29]. Adherence to the principles of Clarity, Conciseness, and Correctness is paramount, ensuring that visualizations are self-explanatory, focused on key metrics, and built upon accurate, validated data [28].
Fundamental Principles of Statistical Visualization
Effective statistical visualization is not merely about making attractive graphs; it is about designing graphics that faithfully represent the underlying data and statistical concepts to facilitate scientific inference.
Show the Design
The first principle is to create a "design plot" that visually represents the experimental design. This plot should display the key dependent variable broken down by all the primary experimental manipulations, analogous to a preregistered analysis. Conventionally, the primary independent variable (e.g., the analytical method being compared) is placed on the x-axis, and the primary measurement of interest is placed on the y-axis. Secondary variables are then assigned to other visual channels like color or shape [29].
Facilitate Comparison
The second principle is to choose graphical elements that facilitate accurate comparisons along the dimensions most relevant to the scientific question. The human visual system is more accurate at comparing the positions of elements (e.g., the locations of points along a common scale) than it is at comparing lengths, areas, or colors [29]. This principle directly informs the selection of difference plots and scatter plots, which rely on positional comparisons, over less accurate chart types like pie charts or heatmaps for many analytical tasks.
Core Comparison Plots: Methodologies and Applications
Scatter Plots
A scatter plot is a foundational technique for comparing two continuous variables by plotting one on the x-axis and the other on the y-axis [30].
- Experimental Protocol: To create a scatter plot for method comparison:
- Collect paired measurements
(X_i, Y_i)from the reference and test methods, respectively, across a range of samples that cover the expected concentration or response range. - Plot the reference method values
(X)on the horizontal axis and the test method values(Y)on the vertical axis. - A line of perfect agreement (identity line), where
Y = X, is typically added to the plot.
- Collect paired measurements
- Interpretation: The scatter of points around the line of identity provides a visual assessment of the overall agreement. A tight cluster along the line suggests good agreement, while a systematic deviation indicates a constant or proportional bias. Scatter plots are most effective with large datasets, as trends and correlations become easier to identify [30].
Bland-Altman Plots (Difference Plots)
The Bland-Altman plot, a specific and highly valuable type of difference plot, is the gold standard for assessing agreement between two analytical methods. Instead of plotting the raw values, it focuses on the differences between them [31].
- Experimental Protocol:
- For each paired measurement
(X_i, Y_i), calculate the difference:Difference_i = Y_i - X_i. - Calculate the average of the two measurements for each pair:
Average_i = (X_i + Y_i) / 2. - Plot the
Difference_ion the y-axis against theAverage_ion the x-axis. - Add the following reference lines to the plot:
- The mean difference (
μ_d), representing the average bias between the methods. - The Limits of Agreement (LoA), calculated as
μ_d ± 1.96 * SDof the differences, which show the range within which 95% of the differences between the two methods are expected to fall.
- The mean difference (
- For each paired measurement
- Interpretation: The plot reveals the relationship between the measurement error and the magnitude of the measurement. A random scatter of points within the LoA suggests good agreement. Any systematic pattern (e.g., differences increasing with the average) indicates a proportional bias. Outliers are also easily identified.
Quantile-Quantile (Q-Q) Plots
A Q-Q plot is used to compare the underlying distributions of two datasets or to compare a dataset to a theoretical distribution [31].
- Experimental Protocol:
- Calculate the quantiles for the first sample (
q_p^(1)) and the second sample (q_p^(2)) for a series of probability pointsp. - Plot the pairs of quantiles
(q_p^(1), q_p^(2))against each other.
- Calculate the quantiles for the first sample (
- Interpretation: If the two datasets come from the same distribution, the points will fall approximately along the line of identity. Deviations from this line indicate differences in the shapes of the distributions, such as differences in skewness or variance.
Box Plots (Side-by-Side)
Side-by-side box plots, or grouped box plots, are used to compare the distributions of a quantitative variable across different categories or groups [31].
- Experimental Protocol:
- For each group to be compared (e.g., results from different laboratories or under different experimental conditions), calculate the five-number summary: minimum, first quartile (25th percentile), median, third quartile (75th percentile), and maximum.
- Draw a box from the first to the third quartile, with a line at the median.
- "Whiskers" extend from the box to the minimum and maximum values, excluding outliers. A common convention is to plot the whiskers at the 25th percentile minus 1.5 times the IQR and the 75th percentile plus 1.5 times the IQR. Individual points are drawn for any values outside this range [31].
- Interpretation: Box plots allow for the visual comparison of central tendency (medians), dispersion (IQR and whiskers), and skewness across groups. For example, they can be used to compare the precision (variance) of multiple analytical methods.
The following workflow diagram illustrates the decision process for selecting and implementing these core comparative plots.
The following tables summarize key quantitative metrics and visual characteristics for the primary plots discussed.
Table 1: Summary of Key Comparative Plot Types
| Plot Type | Primary Function | Variables Compared | Key Interpretation Focus |
|---|---|---|---|
| Scatter Plot [30] | Assess correlation and overall agreement between two methods. | Two continuous variables. | Deviation of points from the line of identity. |
| Bland-Altman Plot [31] | Quantify agreement and identify systematic bias. | Paired continuous measurements. | Spread of differences around the mean and Limits of Agreement. |
| Q-Q Plot [31] | Compare shapes of distributions. | Two sets of unpaired data or data vs. theoretical distribution. | Deviation of quantile pairs from the line of identity. |
| Side-by-Side Box Plots [31] | Compare central tendency and dispersion across groups. | One continuous and one categorical variable. | Relative position and overlap of medians, boxes, and whiskers. |
Table 2: Core Statistical Metrics for Validation
| Metric | Calculation | Interpretation in Validation |
|---|---|---|
| Mean Difference (Bias) | ( \mud = \frac{\sum (Yi - X_i)}{n} ) | Average systematic error between test and reference method. |
| Limits of Agreement (LoA) | ( \mud \pm 1.96 \times SD{differences} ) | The range containing 95% of differences between methods. |
| Correlation Coefficient | Covariance(X, Y) / (SDX * SDY) | Strength and direction of the linear relationship between methods. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following reagents and materials are critical for conducting robust analytical method validation studies in a pharmaceutical context.
Table 3: Key Research Reagent Solutions for Analytical Validation
| Reagent / Material | Function in Validation |
|---|---|
| Certified Reference Material (CRM) | Provides a ground-truth standard with known purity and concentration to establish accuracy and calibration of the analytical method. |
| System Suitability Test (SST) Mixtures | A standardized mixture used to verify that the chromatographic or other analytical system is performing adequately at the time of testing. |
| MedDRA & CDISC Standards [28] | Standardized terminologies (MedDRA) and data structures (CDISC) for coding adverse events and organizing data, ensuring regulatory compliance and interoperability. |
| Quality Control (QC) Samples | Samples prepared at low, medium, and high concentrations within the calibration range to monitor the method's precision and accuracy during a run. |
| Electronic Data Capture (EDC) System [28] | A computerized system designed for the collection of clinical data in electronic format, replacing paper-based case report forms and enabling real-time data visualization. |
| Fusarochromanone | Fusarochromanone, CAS:104653-89-6, MF:C15H20N2O4, MW:292.33 g/mol |
| AG1557 | AG1557, CAS:1161002-05-6, MF:C19H16BrNO2, MW:370.2 g/mol |
Advanced Applications in Drug Development
Comparative plots are indispensable throughout the drug development lifecycle. They are central to Risk-Based Monitoring (RBM/RBQM), where dashboards surface key risk indicators (KRIs) via heatmaps and box plots to identify sites with poor enrolment, delayed data entry, or frequent protocol deviations [28]. In safety monitoring, visualizations like bar charts and heatmaps are used to compare the frequency of adverse events (AEs) across different treatment groups, enabling the faster detection of potential safety signals [28].
The future of these methods lies in greater integration and automation. Emerging trends include AI-powered insights, where machine learning algorithms constantly analyze incoming data to detect operational risks or compliance gaps, and role-based dashboards that automatically adapt visualizations—including difference and comparison plots—to the specific needs of CRAs, data managers, and medical monitors [28].
In the rigorous field of analytical method validation, demonstrating that a new analytical procedure is comparable to a well-characterized existing method is a fundamental requirement. Such comparative studies are pivotal in pharmaceutical research and drug development, where they ensure the reliability, consistency, and accuracy of analytical data. This technical guide frames linear regression analysis—specifically the estimation of the standard error (SE) and the interpretation of the correlation coefficient (r)—within this critical context. We will explore how these statistical tools are not merely mathematical abstractions but essential components for quantifying the agreement and precision between two analytical methods. The guide provides researchers and scientists with in-depth methodologies, practical protocols, and clear interpretive frameworks to robustly execute and report comparative method validation studies.
Theoretical Foundations: Regression and Correlation in Method Comparison
Distinguishing Between Regression and Correlation Analysis
In comparative method validation, it is crucial to understand the distinct roles of regression and correlation analysis, as misapplication can lead to incorrect conclusions about method equivalence [32].
Regression Analysis deals with functional relationships where the independent variable (X) is a reference or standard method with values selected by the investigator, and the dependent variable (Y) is the response from the new method under investigation [32]. The primary purpose is often calibration or estimation of parameters (slope and intercept) that describe the relationship between the two methods. The core model for simple linear regression is expressed as: ( Y = \beta{0} + \beta{1}X + \varepsilon ) where
Yis the response from the new method,Xis the value from the reference method,β₀is the intercept,βâ‚is the slope, andεis the error term [33] [34] [35].Correlation Analysis is concerned with quantifying the strength and direction of a two-way linear association between two continuous variables, neither of which is necessarily designated as independent or dependent [36] [37]. The correlation coefficient (r) only measures how closely two variables co-vary, not the agreement between them. Its popularity stems from being a dimensionless, easily communicated quantity, but it is often misused as a universal measure of goodness-of-fit in regression contexts where it is inappropriate [32].
The Correlation Coefficient (r): Calculation and Interpretation
The Pearson product-moment correlation coefficient (r) is a measure of the linear relationship between two variables. For a sample of n paired observations (xáµ¢, yáµ¢), it is calculated as [36]: [ r = \frac{\sum{i=1}^{n}(xi - \bar{x})(yi - \bar{y})}{\sqrt{\sum{i=1}^{n}(xi - \bar{x})^2 \sum{i=1}^{n}(y_i - \bar{y})^2}} ]
The coefficient r takes a value between -1 and +1. The following table provides a standard scale for interpreting its magnitude in a research context, though these guidelines can be field-specific [36].
Table 1: Interpretation of the Pearson Correlation Coefficient (r)
| Size of Correlation | Interpretation |
|---|---|
| ±0.90 to ±1.00 | Very high correlation |
| ±0.70 to ±0.90 | High correlation |
| ±0.50 to ±0.70 | Moderate correlation |
| ±0.30 to ±0.50 | Low correlation |
| ±0.00 to ±0.30 | Negligible correlation |
Several critical pitfalls must be avoided when interpreting r:
- Causation vs. Association: A significant correlation does not imply that one variable causes the other. It merely indicates association, and the relationship may be driven by unobserved confounding variables [37].
- Sensitivity to Range: Restricting the range of one or both variables can dramatically reduce the observed r.
- Attenuation by Measurement Error: Measurement error intrinsic to any analytical technique can bias (attenuate) the correlation coefficient towards zero, leading to an underestimation of the true relationship [38].
- Linearity Assumption: The Pearson correlation is only a valid measure of linear association. It can be low even for strong, non-linear relationships (e.g., U-shaped curves) [37].
For data that is skewed, ordinal, or contains outliers, Spearman's rank correlation coefficient is often more appropriate as it is a non-parametric measure based on the ranks of the data [36].
Standard Error of the Estimate in Linear Regression
Conceptual Foundation and Calculation
In a comparative method validation study, the Standard Error of the Estimate (SEE), also known as the Standard Error of the Regression (S), is a critical measure of precision. It quantifies the average distance that the observed data points fall from the regression line [39] [40]. In the context of method comparison, it represents the typical deviation of the new method's results (Y) from the values predicted by its linear relationship with the reference method (X).
The SEE is calculated from the residuals—the differences between the observed values (yᵢ) and the values predicted by the regression model (ŷᵢ). The formula is [33]: [ Se = \sqrt{\frac{\sum{i=1}^{n}(Yi - \hat{Yi})^2}{n-2}} = \sqrt{MSE} ] where MSE is the Mean Squared Error from the Analysis of Variance (ANOVA) table of the regression model [33]. Graphically, the absolute value of each residual is the vertical distance between an actual data point and the regression line, and the SEE is the standard deviation of these vertical distances [40].
Interpretation and Application in Validation
The value of Se is expressed in the same units as the dependent variable (Y), which makes its interpretation intuitive and specific to the analytical context [39] [40]. A smaller Se indicates that the data points are clustered more tightly around the regression line, implying that the new method's results are more consistently predicted by the reference method. Conversely, a larger S_e indicates greater scatter and a less precise relationship.
In practice, Se provides vital information for assessing the predictive capability of the comparative model. Approximately 95% of the observations are expected to fall within ±2*Se of the regression line, which serves as a quick approximation of a 95% prediction interval [39]. For instance, if one is comparing two methods for measuring a drug concentration in mg/mL and obtains an S_e of 0.2 mg/mL, one can state that the predicted value from the new method will typically be within ±0.4 mg/mL of the value suggested by the reference method relationship.
Experimental Protocols for Comparative Studies
Workflow for a Method Comparison Study
The following diagram outlines the key stages of a robust experimental protocol for a comparative analytical method validation study.
Detailed Methodological Considerations
Sample Selection and Preparation: The set of samples used for the comparison should be representative of the intended scope of the new method. This includes covering the full range of concentrations (e.g., from 50% to 150% of the target assay concentration) and encompassing the relevant sample matrices (e.g., plasma, serum, finished product) [32]. Samples must be homogeneous and stable for the duration of the analysis to ensure that differences are attributable to the analytical methods and not sample degradation.
Data Acquisition and Randomization: To minimize the impact of systematic bias (e.g., instrument drift, analyst fatigue), the analysis of samples by both methods should be fully randomized. If complete randomization is not feasible, a balanced block design should be employed. A sufficient number of replicates (typically a minimum of 3) per sample is necessary to obtain reliable estimates of precision and to check for homogeneity of variance.
Statistical Analysis Workflow: The core statistical analysis involves fitting a linear regression model and calculating associated statistics. The workflow for this process, and how its components interrelate, is shown below.
Data Presentation and Analysis of Variance (ANOVA)
The ANOVA Table in Regression
The Analysis of Variance (ANOVA) is a fundamental statistical procedure used to partition the total variability of the dependent variable into components attributable to different sources. In regression analysis for method comparison, it helps determine the effectiveness of the reference method (X) in explaining the variation observed in the new method (Y) [33].
The total variation, Total Sum of Squares (SST), is broken down as follows [33]:
SST = SSR + SSE
Where:
- SSR (Regression Sum of Squares): The explained variation—the portion of total variation accounted for by the linear relationship with the reference method.
- SSE (Error Sum of Squares): The unexplained (residual) variation—the portion of total variation that the model fails to capture.
These calculations are standardly presented in an ANOVA table, which is also the source for calculating the Standard Error of the Estimate (SEE).
Table 2: Typical ANOVA Table for Simple Linear Regression [33]
| Source of Variation | Degrees of Freedom (df) | Sum of Squares (SS) | Mean Sum of Squares (MS) |
|---|---|---|---|
| Regression (Explained) | 1 | SSR = Σ(ŷᵢ - ȳ)² | MSR = SSR / 1 |
| Residual (Unexplained) | n - 2 | SSE = Σ(yᵢ - ŷᵢ)² | MSE = SSE / (n - 2) |
| Total | n - 1 | SST = Σ(yᵢ - ȳ)² |
From this table, the SEE is calculated as: ( S_e = \sqrt{MSE} ) [33]. Furthermore, the coefficient of determination, R², is derived as: ( R^2 = \frac{SSR}{SST} ), which represents the proportion of total variance in the new method that is explained by the reference method [33].
F-Test for Model Significance
The ANOVA framework also provides an F-test to evaluate the overall significance of the regression model. The null hypothesis is that the slope coefficient is zero (H₀: β₠= 0), meaning the reference method has no explanatory power for the new method's variation [33]. The F-statistic is calculated as: [ F = \frac{MSR}{MSE} = \frac{\text{Average Regression Sum of Squares}}{\text{Average Sum of Squared Errors}} ] A large F-statistic (greater than the critical value from the F-distribution with 1 and n-2 degrees of freedom) leads to the rejection of the null hypothesis, providing evidence that the linear relationship is statistically significant [33]. It is worth noting that in simple linear regression with one independent variable, this F-test is equivalent to the t-test for the slope coefficient, as F = t² [33].
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials and solutions commonly required for executing the experimental protocols in a bioanalytical method comparison study, such as for quantifying an active pharmaceutical ingredient (API).
Table 3: Key Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Function / Purpose |
|---|---|
| Certified Reference Standard | Provides the known identity and purity of the analyte (API) to prepare calibration standards and quality control samples. Serves as the benchmark for quantification. |
| Blank Matrix | The biological or chemical matrix (e.g., human plasma, formulation placebo) free of the analyte. Used to prepare calibration curves and assess selectivity. |
| Internal Standard | A compound added in a constant amount to all samples and standards during sample preparation. Used to correct for variability in sample processing and instrument analysis. |
| Mobile Phase Solvents | High-purity solvents and buffers used as the carrier in chromatographic systems (e.g., HPLC, UPLC) to separate the analyte from other matrix components. |
| Stabilization Solutions | Reagents (e.g., antioxidants, enzyme inhibitors) added to samples to prevent degradation of the analyte during storage and processing, ensuring result integrity. |
| Derivatization Reagents | Chemicals used to react with the analyte to produce a derivative that has more favorable properties for detection (e.g., higher fluorescence or UV absorption). |
Advanced Considerations and Common Misinterpretations
Limitations of the Correlation Coefficient in Method Comparison
A significant and common misuse of the correlation coefficient (r) in comparative studies is its interpretation as a measure of agreement. A high r value can be misleading and does not necessarily mean the two methods agree [32]. This is because:
- r Measures Association, Not Agreement: A high r value indicates a strong linear relationship, but the two methods could be consistently different. A new method that always gives a result 20% higher than the reference method will still produce a perfect correlation of r=1.0, despite the clear lack of agreement.
- Dependence on the Data Range: The value of r is highly sensitive to the range of the data. A wider range of analyte concentrations will artificially inflate the r value, making the agreement appear better than it is over a narrower, more relevant concentration range.
For these reasons, Bland-Altman analysis (or difference plots) is the recommended statistical tool for assessing agreement between two methods, as it focuses on the differences between paired measurements rather than their correlation [36].
Impact of Measurement Error on Correlation
All analytical measurement techniques have inherent random error. The presence of such measurement error can seriously hamper the quality of estimated correlation coefficients. Under a simple additive error model, the error causes a phenomenon known as attenuation, where the expected correlation (Ï) is biased toward zero compared to the true correlation (Ïâ‚€) [38]. The relationship is given by:
[
\rho = A \rho0
]
where the attenuation factor A is:
[
A = \frac{1}{\sqrt{(1 + \frac{\sigma{aux}^2}{\sigma{x0}^2})(1 + \frac{\sigma{auy}^2}{\sigma{y_0}^2})}}
]
Here, σ²_au represents the variance of the measurement error, and σ²_0 represents the true biological or chemical variance of the analyte [38]. This underscores that correlation coefficients estimated from "noisy" analytical data are often underestimates of the true underlying relationship.
Standard Errors of Regression Parameters
Beyond the standard error of the estimate for the model, it is crucial to calculate the standard errors for the individual regression parameters (intercept and slope). These standard errors, denoted as SE(β̂₀) and SE(β̂â‚), measure the precision of these estimates—that is, how much they would vary from sample to sample [34] [35]. They are used to construct confidence intervals and perform hypothesis tests (e.g., t-tests) on the parameters.
The formulae for these standard errors are [34]: [ SE(\hat{\beta}0)^2 = \sigma^2 \left[ \frac{1}{n} + \frac{\bar{x}^2}{\sum{i=1}^n (xi - \bar{x})^2} \right] ] [ SE(\hat{\beta}1)^2 = \frac{\sigma^2}{\sum{i=1}^n (xi - \bar{x})^2} ] where σ² is the variance of the error term ε, typically estimated by the MSE from the ANOVA table [34]. In the context of method comparison, a narrow confidence interval for the slope (using SE(β̂â‚)) that contains the value 1, and for the intercept (using SE(β̂₀)) that contains 0, provides statistical evidence for the equivalence of the two methods across the tested concentration range.
Troubleshooting Comparison Studies: Identifying and Resolving Discrepancies
Handling Outliers and Discrepant Results in Data Sets
In analytical method validation research, the comparative method serves as a foundational approach for establishing method reliability, accuracy, and precision through systematic comparison against reference standards or established methodologies. The integrity of this comparative process is critically dependent on effective identification and management of outliers and discrepant results—data points that deviate markedly from other observations. This technical guide provides drug development professionals with comprehensive frameworks for detecting, evaluating, and addressing outliers within the context of analytical method validation, emphasizing statistical rigor, methodological transparency, and compliance with regulatory standards. By implementing robust outlier management protocols, researchers can enhance data quality, improve methodological comparisons, and strengthen the evidentiary basis for analytical procedures used in pharmaceutical development.
Outliers represent observations that deviate significantly from other members of the sample in which they occur, potentially distorting statistical analyses and compromising analytical conclusions [41]. In the specialized context of analytical method validation research, outliers assume particular importance as they can directly impact assessments of method accuracy, precision, and reliability during comparative studies. The comparative method framework necessitates side-by-side evaluation of new methodologies against validated reference methods, where discrepant results require careful investigation to determine whether they represent methodological deficiencies, analytical errors, or legitimate biological variability [42].
The management of outliers intersects fundamentally with quality management systems in regulated laboratory environments. According to established guidelines, laboratories seeking accreditation under ISO/IEC 17025 or ISO 15189 must implement systematic approaches for verifying method performance characteristics, including protocols for handling anomalous results [42]. Within this framework, outlier management transcends mere statistical exercise and becomes an essential component of method validation protocols, ensuring that analytical procedures generate correct, reliable results capable of supporting critical decisions in drug development.
Statistical Foundations of Outlier Detection
Characterization of Outliers
Outliers in analytical datasets may arise from multiple sources, including experimental errors, measurement system variability, sample contamination, data processing mistakes, or genuine extreme values within the population [41] [43]. The statistical definition characterizes outliers as observations that lie an abnormal distance from other values in a random sample from a population. In analytical chemistry and pharmaceutical research, the presence of outliers can significantly impact key method validation parameters, including precision, accuracy, and the determination of the measurement range [42].
The effect of outliers on statistical measures varies considerably. The mean, as a measure of central tendency, is particularly sensitive to outlier influence, while the median remains more robust in the presence of extreme values [41]. This differential impact necessitates careful consideration when selecting statistical measures for method comparison studies, particularly when outliers may be present in the data. Understanding these statistical properties forms the foundation for effective outlier detection and management in analytical method validation.
Detection Methods
Several established statistical methods exist for detecting outliers in analytical datasets, each with distinct strengths, limitations, and applicability to different data structures encountered in pharmaceutical research.
Table 1: Statistical Methods for Outlier Detection in Analytical Data
| Method | Basis | Threshold | Applicability | Advantages | Limitations |
|---|---|---|---|---|---|
| Z-score | Standard deviations from mean | ±2-3 SD | Normally distributed data | Simple calculation, easy implementation | Sensitive to outliers itself, assumes normality |
| IQR | Interquartile range | Q1 - 1.5×IQR to Q3 + 1.5×IQR | Non-normal distributions | Robust to outliers, distribution-free | Less sensitive for large datasets |
| DBSCAN | Density-based clustering | Density connectivity | Multidimensional data | Identifies arbitrary shapes, no distribution assumption | Parameter sensitivity (eps, min_samples) |
Z-Score Method
The Z-score method standardizes data by measuring how many standard deviations an observation lies from the mean. For datasets following a normal distribution, Z-scores beyond ±3 standard deviations typically indicate potential outliers [41]. The calculation follows the formula:
This method works effectively for normally distributed data but becomes less reliable with small sample sizes or substantially non-normal distributions commonly encountered in analytical method validation studies.
Interquartile Range (IQR) Method
The IQR method employs a non-parametric approach based on data quartiles, making it particularly valuable for non-normally distributed data common in analytical chemistry applications [41]. The procedure involves:
This method identifies outliers as observations falling below Q1 - 1.5×IQR or above Q3 + 1.5×IQR, providing a robust approach unaffected by extreme values that might distort mean and standard deviation calculations.
DBSCAN for Multidimensional Data
For analytical methods generating multidimensional data (e.g., chromatographic peak characteristics, spectroscopic profiles), density-based spatial clustering (DBSCAN) offers advanced outlier detection capabilities [43]. This algorithm identifies outliers as points in low-density regions of the feature space:
This approach proves particularly valuable in analytical method comparison studies where multiple parameters must be evaluated simultaneously to identify discrepant results.
Experimental Protocols for Outlier Management
Systematic Workflow for Outlier Investigation
The following workflow provides a structured approach for handling outliers in analytical method validation studies, emphasizing scientific rigor and documentation:
- Initial Detection: Apply multiple statistical methods (e.g., Z-score, IQR) to identify potential outliers in the dataset [41] [43].
- Contextual Assessment: Examine the experimental context of potential outliers, including sample preparation records, instrument performance logs, and environmental conditions.
- Root Cause Analysis: Investigate potential technical, operational, or biological causes for discrepant results.
- Impact Assessment: Evaluate the effect of the potential outlier on method performance characteristics and comparative conclusions.
- Decision Protocol: Apply predefined, statistically justified criteria for determining outlier treatment.
- Documentation: Comprehensively document the outlier, investigation process, and rationale for treatment decisions.
This workflow ensures consistent, transparent handling of outliers throughout method validation studies, supporting regulatory compliance and scientific defensibility.
Statistical Validation of Outlier Decisions
When employing the comparative method in analytical validation, establishing statistically justified criteria for outlier treatment represents a critical step. Protocol development should include:
- Predefined significance levels for statistical outlier tests
- Sample size considerations for outlier detection power
- Multiple testing corrections when evaluating numerous parameters
- Procedures for maintaining statistical integrity when addressing outliers
The experimental protocol should explicitly state whether outlier exclusion decisions will be based on statistical tests alone or require corroborating evidence from experimental records [42]. This upfront clarity prevents post hoc decision-making that could introduce bias into method comparison studies.
Visualization Approaches
Workflow Diagram for Outlier Management
The following diagram illustrates the comprehensive workflow for handling outliers in analytical method validation:
Outlier Detection Methods Diagram
This diagram illustrates the statistical relationships between different outlier detection approaches:
Treatment Strategies for Outliers
Protocol Selection Framework
Selecting appropriate treatment strategies for outliers identified during analytical method comparison requires consideration of methodological impact, scientific rationale, and regulatory expectations.
Table 2: Outlier Treatment Strategies in Analytical Method Validation
| Treatment Method | Procedure | Impact on Data | When to Use | Regulatory Considerations |
|---|---|---|---|---|
| Trimming/Removal | Complete exclusion of outlier from dataset | Reduces sample size, may introduce bias | Clear evidence of analytical error | Must document rationale and maintain original data |
| Winsorization | Capping extreme values at specified percentiles | Preserves sample size, reduces skewness | Suspected measurement errors with valid directionality | Requires transparency in statistical methods |
| Imputation | Replacing outliers with statistical estimates (median, mean) | Maintains dataset structure | When exclusion would substantially reduce power | Must report imputation method and validate sensitivity |
| Transformation | Applying mathematical functions (log, square root) | Changes distribution characteristics | Non-normal distributions with extreme values | Document pre-processing and interpret transformed results |
| Segmented Analysis | Analyzing data with and without outliers | Provides comparative perspective | Uncertain outlier status or significance | Demonstrates robustness of conclusions |
Technical Implementation of Treatment Methods
Winsorization Technique
Winsorization replaces extreme values with the nearest acceptable values based on percentile thresholds, preserving sample size while reducing outlier influence:
This approach maintains data structure while minimizing the impact of extreme values on statistical analyses in method comparison studies.
Robust Statistical Measures
When outliers may represent legitimate rather than erroneous values, employing robust statistical measures provides an alternative treatment approach:
These measures are particularly valuable in preliminary method comparison studies where the distinction between true outliers and legitimate extreme values remains uncertain.
Quality Assurance and Regulatory Compliance
Integration with Quality Management Systems
Effective outlier management must be integrated within the broader quality management framework governing analytical laboratories. This integration includes:
- Establishing standardized operating procedures (SOPs) for outlier detection and treatment
- Defining roles and responsibilities for outlier investigation and decision-making
- Implementing documentation standards that ensure traceability of outlier-related decisions
- Incorporating outlier management into method validation protocols and reports
Within the comparative method context, quality assurance practices must ensure that outlier treatment does not introduce bias into method comparisons, particularly when evaluating new methods against established reference methods [42]. This requires careful attention to consistent application of outlier criteria across compared methods.
Analytical Performance Monitoring
Robust outlier management extends beyond individual studies to encompass ongoing analytical performance monitoring. This longitudinal approach includes:
- Tracking outlier frequency and patterns across multiple studies
- Correlating outlier occurrences with specific analytical conditions
- Implementing control charts for key method performance parameters
- Establishing alert limits for outlier rates that trigger method re-evaluation
By monitoring outliers systematically over time, laboratories can distinguish random analytical variations from systematic methodological issues, supporting continuous improvement of analytical methods throughout the drug development lifecycle.
Research Reagent Solutions for Analytical Quality Control
Table 3: Essential Materials for Analytical Quality Control and Outlier Investigation
| Reagent/ Material | Function in Quality Control | Application in Outlier Management |
|---|---|---|
| Certified Reference Materials | Provide traceable accuracy standards | Investigate measurement bias in outliers |
| Quality Control Materials | Monitor analytical precision over time | Identify systematic errors causing outliers |
| Stable Isotope Internal Standards | Correct for sample preparation variability | Detect preparation errors causing outliers |
| Matrix-Matched Calibrators | Account for sample matrix effects | Identify matrix-related outliers |
| Sample Preservation Reagents | Maintain analyte stability | Recognize degradation-related outliers |
| Instrument Performance Standards | Verify instrument calibration | Distinguish instrument-related outliers |
Effective management of outliers and discrepant results represents an essential component of analytical method validation research, particularly within the comparative method framework used extensively in pharmaceutical development. By implementing systematic detection protocols, statistically justified treatment strategies, and comprehensive documentation practices, researchers can enhance the reliability of method comparison studies while maintaining regulatory compliance. The approaches outlined in this technical guide provide a foundation for robust outlier management that supports data integrity throughout the drug development process. As analytical technologies evolve, continued attention to outlier management methodologies will remain critical for generating reliable evidence regarding analytical method performance.
Addressing Issues of Specificity and Sample Matrix Interferences
In analytical method validation, the comparative method serves as a benchmark against which a new test method is evaluated. The primary purpose of this comparison is to estimate inaccuracy or systematic error [1]. Within this framework, specificity and sample matrix interferences represent critical parameters that determine the reliability and accuracy of analytical results. Specificity is defined as the ability of a method to assess the analyte unequivocally in the presence of other components that may be expected to be present, such as impurities, degradants, or matrix components [44]. The sample matrix encompasses everything present in a typical sample except the analytes of interest, and its composition can profoundly influence analytical results [44].
The regulatory importance of these factors is well-established. According to ICH guidelines, specificity is a fundamental validation parameter, while the United States Pharmacopoeia (USP) Chapter 1226 emphasizes that excipients in drug products can vary widely among manufacturers and may interfere with analytical procedures [44]. For bioanalytical methods, the FDA recommends testing blank matrix from at least six sources to ensure selectivity [44]. Understanding and addressing issues related to specificity and sample matrix is therefore essential for demonstrating that a comparative method is suitable for its intended use.
Theoretical Foundations: Defining Specificity and Matrix Effects
Specificity and Selectivity in Analytical Methods
The terms specificity and selectivity are often used interchangeably, though regulatory bodies sometimes distinguish between them. The International Conference on Harmonization (ICH) defines specificity as the ability to assess the analyte unequivocally in the presence of potential interferents [44]. The FDA often uses the term selectivity to describe the ability of an analytical method to differentiate and quantify the analyte in the presence of other components in the sample [44]. In practical terms, both concepts address the method's capacity to produce accurate results for the intended analyte despite the presence of other substances.
Sample Matrix Composition and Variability
The sample matrix consists of all components in a sample other than the analyte of interest [44]. This varies significantly across different sample types:
- Environmental samples: Water or soil components
- Bioanalytical samples: Plasma, urine, or other biological fluids with endogenous components
- Pharmaceutical formulations: Excipients, antioxidants, buffers, or container extractives
Matrix effects occur when components of the sample matrix alter the analytical response, either by enhancing or suppressing it [44]. These effects can lead to inaccurate quantification of the analyte and must be carefully evaluated during method validation.
Regulatory Definitions and Requirements
Regulatory agencies provide specific guidance for addressing specificity and matrix effects:
- ICH: Requires demonstration of specificity in the presence of impurities, degradants, and matrix [44]
- USP: Suggests assessment of specificity when verifying compendial procedures, particularly for drug substances from different suppliers with different impurity profiles [44]
- FDA: Recommends testing blank matrix from at least six sources for bioanalytical methods [44]
Experimental Design for Assessing Specificity and Matrix Effects
Core Experimental Protocol for Specificity Assessment
A well-designed comparison of methods experiment is essential for assessing systematic errors that may occur with real patient specimens [1]. The following protocol provides a framework for evaluating specificity and matrix effects:
Specimen Selection and Preparation
- Select a minimum of 40 different patient specimens covering the entire working range of the method [1]
- Include specimens representing the spectrum of diseases expected in routine application
- Ensure specimen stability by analyzing test and comparative methods within two hours of each other [1]
- For unstable analytes, employ appropriate preservation methods (serum separation, refrigeration, freezing)
Experimental Timeline
- Conduct analysis over several different analytical runs on different days [1]
- Minimum recommendation: 5 days [1]
- Ideal duration: Extend over 20 days (2-5 patient specimens per day) to coincide with long-term replication studies [1]
Analysis Protocol
- Analyze each specimen by both test method and comparative method
- Consider duplicate measurements on different samples analyzed in different runs to identify sample mix-ups or transposition errors [1]
- If singles analysis performed, inspect comparison results as collected and repeat analyses with large differences while specimens remain available [1]
Assessment of Matrix Interferences
Blank Matrix Evaluation
- Test blank matrix from multiple sources (minimum six for bioanalytical methods) [44]
- Ensure no interfering peaks co-elute with the analyte
- Use placebo formulations for pharmaceutical products containing all excipients but no active ingredient [44]
Interference Testing
- Identify most likely and worst-case interferences [45]
- Spike potential interferents at clinically relevant concentrations
- Evaluate chromatographic separation in LC methods or spectral overlaps in other techniques
Table 1: Experimental Parameters for Specificity Assessment
| Parameter | Minimum Requirement | Ideal Protocol | Regulatory Reference |
|---|---|---|---|
| Number of Specimens | 40 patient specimens | 100-200 specimens for specificity assessment | [1] |
| Sample Types | Cover working range | Disease spectrum representation | [1] |
| Timeframe | 5 days | 20 days (aligned with precision studies) | [1] |
| Matrix Sources | Not specified | 6 sources for bioanalytical methods | [44] |
| Measurement Type | Single measurements | Duplicates in different runs | [1] |
Methodologies for Evaluating Specificity
Chromatographic Specificity Assessment
Liquid chromatography (LC) methods require careful assessment of specificity through retention time separation and peak purity evaluation:
Retention Time Separation
- Achieve baseline resolution (Rs ≥ 2.0) between analyte and potential interferents [44]
- Test specificity with samples containing expected interferents
- Evaluate samples from stability studies for degradation products
Peak Purity Assessment
- Use diode-array detection (DAD) for spectral purity confirmation
- Note that peak purity algorithms have limitations with closely eluting peaks or similar spectra [44]
- Consider mass spectrometry (MS) detection for unambiguous identification
Sample Matrix and Selectivity Testing
The sample matrix choice is critical for meaningful specificity assessment:
Matrix Selection Guidelines
- Drug products: Use placebo with all excipients but no active ingredient [44]
- Environmental samples: Use similar matrix from different source (e.g., untreated water) [44]
- Bioanalytical methods: Test blank matrix from at least six different sources [44]
Challenge Samples
- Prepare samples with likely interferents at maximum expected concentrations
- Include samples from special populations (different genetics, disease states, diets) when relevant [44]
- Test for interferences from metabolites, concomitant medications, or common endogenous compounds
Table 2: Specificity Assessment Methods Across Different Matrix Types
| Matrix Type | Specificity Challenge | Assessment Method | Acceptance Criteria |
|---|---|---|---|
| Pharmaceutical Formulations | Excipient interference | Placebo analysis | No interference at retention time of analyte |
| Biological Fluids | Endogenous compounds | Analysis of 6+ blank matrix sources | Response in blank < 20% of LLOQ |
| Environmental Samples | Co-extracted contaminants | Analysis of representative blank matrix | No interference peaks |
| Multi-source APIs | Different impurity profiles | Analysis of samples from different suppliers | Consistent analyte quantification |
Data Analysis and Statistical Approaches
Graphical Data Analysis Techniques
The initial assessment of comparison data should include visual inspection of graphical representations:
Difference Plots
- Plot differences between test and comparative methods (test minus comparative) on y-axis versus comparative result on x-axis [1]
- Data should scatter around zero difference line
- Visual identification of outliers or systematic patterns [1]
Comparison Plots
- Display test result on y-axis versus comparison result on x-axis for methods not expected to show 1:1 agreement [1]
- Draw visual line of best fit to show general relationship
- Identify discrepant results for repeat analysis [1]
Statistical Analysis of Specificity and Interference Data
Regression Analysis
- Use linear regression statistics for data covering wide analytical range [1]
- Calculate slope (b), y-intercept (a), and standard deviation of points about the line (sy/x)
- Estimate systematic error (SE) at medical decision concentrations: Yc = a + bXc; SE = Yc - Xc [1]
Correlation Assessment
- Calculate correlation coefficient (r) mainly to assess whether data range is wide enough for reliable slope and intercept estimates [1]
- When r < 0.99, collect additional data to expand concentration range or use more appropriate statistical methods [1]
Narrow Range Data
- For narrow analytical ranges (e.g., electrolytes), calculate average difference (bias) between methods [1]
- Use paired t-test calculations including standard deviation of differences and t-value [1]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Specificity and Matrix Studies
| Reagent/Material | Function in Specificity Assessment | Application Notes |
|---|---|---|
| Blank Matrix | Provides interference profile without analyte | Source from 6+ lots for biological samples [44] |
| Placebo Formulation | Assess excipient interference in drug products | Contain all excipients except active ingredient [44] |
| Reference Standards | Identify retention times and quantify analytes | Use certified reference materials when available |
| Potential Interferents | Challenge method specificity | Include metabolites, concomitant medications, endogenous compounds |
| Preservative Solutions | Maintain specimen stability during testing | Appropriate for unstable analytes (e.g., ammonia, lactate) [1] |
| Mobile Phase Components | Chromatographic separation | Optimized to resolve analyte from interferents |
Workflow Visualization: Specificity Assessment in Method Validation
Specificity Assessment Workflow: This diagram outlines the systematic approach to evaluating method specificity, from matrix selection through statistical analysis and final validation.
Advanced Considerations and Troubleshooting
Managing Complex Matrix Effects
Complex matrices present unique challenges that require advanced approaches:
Heterogeneous Matrices
- Account for genetic, dietary, and disease state variations in biological matrices [44]
- Source matrices from populations similar to study subjects
- Consider demographic factors that may alter matrix composition
Matrix-Method Mismatch
- Avoid using purified standards in simple solvents for methods analyzing complex matrices [44]
- Prepare calibration standards in blank matrix to account for matrix enhancement or suppression effects
- Use standard addition methods for particularly problematic matrices
Troubleshooting Specificity Issues
Common specificity problems and potential solutions:
Co-elution Problems
- Modify chromatographic conditions (mobile phase, column, gradient)
- Employ alternative detection methods (MS instead of UV)
- Use derivatization to alter analyte properties
Variable Interferences
- Implement sample cleanup procedures to remove interferents
- Increase chromatographic resolution
- Consider orthogonal method for confirmation
Signal Suppression/Enhancement
- Use stable isotope-labeled internal standards
- Optimize sample preparation to remove matrix components
- Dilute samples to minimize matrix effects
Table 4: Troubleshooting Specificity and Matrix Interference Issues
| Problem | Potential Causes | Investigation Approach | Resolution Strategies |
|---|---|---|---|
| Inconsistent Recovery | Matrix effects varying between sources | Compare recovery across different matrix lots | Use matrix-matched standards, internal standardization |
| Interference Peaks | Inadequate chromatographic separation | Analyze individual matrix components | Optimize separation conditions, alternative sample preparation |
| Signal Suppression | Ionization competition in MS | Post-column infusion experiments | Modify sample cleanup, change ionization mode |
| Degradation Interference | Analyte instability in matrix | Evaluate stability under storage conditions | Stabilize samples, reduce processing time |
Optimizing Experimental Design for a Wide Analytical Range
In the pharmaceutical industry, ensuring the quality, safety, and efficacy of medicinal products is of utmost importance [20]. Analytical method validation (AMV) stands as a critical pillar in pharmaceutical manufacturing and drug development, serving as the foundation for reliable and reproducible analytical results [46]. Within this framework, comparative method studies represent a systematic approach to evaluating analytical procedure performance across different regulatory frameworks, experimental conditions, or technological platforms. These studies are particularly crucial when developing methods intended to operate across wide analytical ranges, where factors such as specificity, linearity, precision, and robustness must be demonstrated as consistent and reliable throughout the method's operational scope [20] [46].
The recent update from ICH Q2(R1) to ICH Q2(R2) in March 2023 marks a significant evolution in regulatory thinking, shifting from a validation checklist to a scientific, lifecycle-based strategy for ensuring method performance [46]. This modernized approach emphasizes enhanced method robustness and integrates with Analytical Quality by Design (AQbD) principles, making the optimization of experimental design not merely a regulatory requirement but a fundamental scientific endeavor to ensure method reliability across the intended analytical range [46].
Core Principles of Experimental Design for Wide Analytical Ranges
Defining the Analytical Target Profile (ATP) and Method Operable Design Region (MODR)
The foundation of optimizing experimental design for wide analytical ranges begins with establishing a clear Analytical Target Profile (ATP). The ATP is a predefined objective that outlines the intended purpose of the analytical method, including the required quality criteria and performance characteristics necessary to demonstrate the method is fit for its intended use [46]. For methods operating across wide ranges, the ATP must explicitly define performance expectations throughout the entire range, not just at specific points.
Closely linked to the ATP is the Method Operable Design Region (MODR), which represents the multidimensional combination and interaction of analytical method variables that have been demonstrated to provide assurance of quality performance [46]. Establishing the MODR through systematic experimentation allows researchers to define the boundaries within which the method will perform reliably, providing flexibility during routine use while maintaining data integrity.
Key Validation Parameters for Wide-Range Methods
When validating methods for wide analytical ranges, specific parameters require particular attention beyond standard validation protocols. The following table summarizes the enhanced requirements for wide-range methods according to ICH Q2(R2):
Table 1: Key Validation Parameters for Wide Analytical Range Methods
| Parameter | Considerations for Wide Range | ICH Q2(R2) Enhancements |
|---|---|---|
| Specificity | Demonstrate interference-free performance across entire range; evaluate matrix effects at range extremes | More guidance on matrix effects and peak purity [46] |
| Linearity | Establish proportional response across wider intervals; evaluate homoscedasticity | Same parameter, but with broader application to modern techniques [46] |
| Range | Extend beyond typical therapeutic ranges to encompass potential outliers and abnormal samples | Lifecycle-focused; integrated with development and verification [46] |
| Accuracy | Demonstrate recovery consistency across the range, not just at specific points | Same parameter, but with broader application to modern techniques [46] |
| Precision | Evaluate variance consistency across range segments; include range-position-specific precision | Same parameter, but with broader application to modern techniques [46] |
| Robustness | Test method resilience to parameter variations across different range segments | Recommended; lifecycle-focused [46] |
Advanced DOE Approaches for Range Optimization
Classical Factorial Designs for Multi-Objective Optimization
Design of Experiments (DOE) provides a structured approach to understanding the relationship between multiple factors affecting analytical method performance [47]. For wide-range methods, classical factorial designs enable researchers to efficiently explore the interaction effects between critical method parameters and their impact on performance characteristics across the analytical range.
Recent investigations evaluating over 150 different factorial designs through simulation-based studies have demonstrated that central-composite designs perform best overall for optimizing complex systems with multiple objectives [47]. These designs are particularly valuable for wide-range method development because they allow for:
- Modeling curvature in response surfaces
- Estimating quadratic effects of factors
- Identifying optimal regions within the MODR
- Understanding complex factor interactions across the analytical range
The experimental workflow for implementing factorial designs in wide-range method development follows a systematic process that can be visualized as:
Screening Designs for Factor Selection in Complex Methods
When dealing with methods that have numerous potential factors influencing performance across a wide analytical range, screening designs provide an efficient strategy for identifying the most significant variables [47]. For scenarios with many continuous factors, a screening design should be used initially to eliminate insignificant factors, followed by a central composite design for final optimization [47].
The most effective screening approaches for wide-range methods include:
- Fractional factorial designs that reduce experimental burden while maintaining ability to detect main effects
- Plackett-Burman designs for investigating large numbers of factors with minimal runs
- Definitive screening designs that can detect curvature and main effects efficiently
These screening methods are particularly valuable in the early stages of method development when the analytical range is broad, and the relationship between factors and responses is not well characterized.
Handling Mixed Factor Types: Continuous and Categorical
Many analytical methods involve both continuous factors (e.g., temperature, pH, flow rate) and categorical factors (e.g., column type, instrument model, reagent supplier) that must be optimized across the analytical range. For these scenarios, a hybrid approach is recommended: first apply a Taguchi design to handle all levels of categorical factors and represent continuous factors in a two-level format, then use a central composite design for final optimization after determining the optimal levels of categorical factors [47].
While Taguchi designs are less reliable than central composite designs overall, they are effective in identifying optimal levels of categorical factors, making them valuable for initial screening of method components that cannot be varied continuously [47].
Practical Implementation and Case Studies
Research Reagent Solutions for Wide-Range Methods
The successful implementation of wide-range analytical methods requires careful selection of reagents and materials that maintain performance across the entire operational range. The following table details essential research reagent solutions and their functions in supporting robust method performance:
Table 2: Key Research Reagent Solutions for Wide-Range Analytical Methods
| Reagent/Material | Function in Wide-Range Methods | Critical Quality Attributes |
|---|---|---|
| Reference Standards | Provide calibration across extended concentration ranges | Purity, stability, traceability, suitability for intended range |
| Chromatographic Columns | Maintain separation efficiency across diverse analyte concentrations | Batch-to-batch reproducibility, pH stability, temperature tolerance |
| Mobile Phase Additives | Modulate retention and peak shape across analytical range | Purity, UV transparency, volatility, compatibility with MS detection |
| System Suitability Mixtures | Verify method performance at multiple range points [46] | Stability, representative composition, defined acceptance criteria |
| Quality Control Materials | Monitor method performance over time across range [46] | Commutability, stability, assigned values with uncertainty |
System Suitability Testing for Range Verification
ICH Q2(R2) explicitly emphasizes system suitability testing (SST) as a routine and integral part of method validation and ongoing performance verification [46]. For wide-range methods, system suitability criteria must be established at multiple points throughout the analytical range to ensure consistent performance. The implementation strategy for range-specific system suitability testing includes:
- Defining SST criteria for lower, middle, and upper range segments
- Establishing resolution requirements between critical pairs across the range
- Setting precision targets appropriate for each range segment
- Incorporating SST failure investigation protocols with specific corrective actions
This approach aligns with the lifecycle management concept introduced in ICH Q2(R2), which promotes continuous method performance verification beyond the initial validation phase [46].
Regulatory Considerations and Lifecycle Management
ICH Q2(R2) Updates Impacting Wide-Range Methods
The transition from ICH Q2(R1) to Q2(R2) introduces several important changes that specifically impact the validation of methods with wide analytical ranges [46]. These include:
- Enhanced Robustness Requirements: While robustness was optional with limited detail in Q2(R1), it is now recommended with a lifecycle focus, requiring integration with development and verification activities [46].
- Risk Assessment Integration: The updated guideline requires risk assessment approaches to justify design and control strategies, which is particularly important for identifying and mitigating range-specific failure modes [46].
- Lifecycle Approach: Unlike Q2(R1), which lacked a lifecycle perspective, Q2(R2) makes this a central concept, promoting continuous method performance verification throughout the method's operational lifetime [46].
Analytical Method Lifecycle Approach
The analytical method lifecycle concept forms the core foundation of ICH Q2(R2) and divides an analytical procedure's life into three key stages: method development, method validation, and continued method performance verification [46]. For wide-range methods, this lifecycle approach ensures that method performance is monitored and maintained throughout the product's lifecycle, with particular attention to range-related performance characteristics.
The relationship between these lifecycle stages and their key outputs for wide-range methods can be visualized as:
Optimizing experimental design for analytical methods with wide operational ranges requires a systematic approach that integrates modern DOE methodologies with the enhanced regulatory framework of ICH Q2(R2). By implementing structured factorial designs, establishing appropriate system suitability criteria across the range, and adopting a lifecycle management perspective, researchers can develop robust methods that deliver reliable performance throughout their intended analytical scope. The comparative method framework provides the necessary structure for demonstrating method reliability across different conditions, instruments, and laboratories, ultimately supporting the development of medicines with enhanced quality assurance and patient safety.
Collaborative Models and Leveraging Published Validations for Efficiency
In analytical method validation research, a comparative study is a systematic investigation that aims to determine whether significant differences exist in predefined performance measures between two or more methods, instruments, or datasets, while controlling for variables such as sample composition, instrumentation, and operational settings [48]. The core objective is to generate quantifiable, comparable data to prove or disprove a hypothesis about method performance [48].
The traditional model of method validation, often conducted in isolation by individual laboratories, presents significant challenges. It is notoriously resource-intensive, characterized by redundancy, manual processes, and extended project timelines [49] [50]. Collaborative models and the strategic leverage of published validations represent a paradigm shift within this comparative framework. Instead of each laboratory generating its own foundational data for comparison, these approaches use existing, peer-reviewed validation studies as the benchmark for comparison. This allows an organization to conduct a more abbreviated, verification-based comparison, accepting the original published data and findings, thereby eliminating significant method development work [49]. This article provides a technical guide for implementing these efficient models, complete with protocols and tools for the pharmaceutical development professional.
Collaborative Validation Models: Theory and Design
Defining the Collaborative Approach
The collaborative method validation model is a formalized approach where multiple Forensic Science Service Providers (FSSPs) or laboratories, performing the same tasks using the same technology, work cooperatively. The goal is to standardize methodology and share common validation data to increase efficiency during both the validation and implementation phases [49]. This model transitions validation from an isolated, repetitive activity to a communal, standardized one.
A key outcome of this model is the publication of validation data in recognized peer-reviewed journals. This publication acts as a communication channel for technological improvements and allows for peer review, which supports the establishment of the method's validity. For a subsequent laboratory, adherence to the strictly defined method parameters in the publication permits a shift from a full validation to a verification exercise [49]. The second laboratory reviews, accepts, and confirms the original published findings against their own system, creating a direct comparative cross-check against benchmarks established by the originating laboratory.
Quantitative Business Case for Collaboration
The business case for collaborative validation is built on the reduction of redundant effort. The following table summarizes the core cost-saving opportunities, based on salary, sample, and opportunity cost analyses [49].
Table 1: Business Case Analysis for Collaborative Validation Models
| Cost Factor | Traditional Independent Validation | Collaborative/Verification Model | Source of Efficiency |
|---|---|---|---|
| Personnel Effort | High (100% baseline) | Significantly reduced | Eliminates redundant method development and extensive testing; focuses on verification [49] [50]. |
| Sample & Material Consumption | High (100% baseline) | Significantly reduced | Leverages existing experimental data; requires fewer samples for verification [49]. |
| Timeline | Extended project timelines | Accelerated validation cycles | Abbreviated process bypasses method development and optimization phases [49] [50]. |
| Opportunity Cost | High (resources tied up in validation) | Lower (resources freed for other tasks) | Reallocation of critical personnel to higher-value R&D tasks [50]. |
| Standardization | Varies by laboratory | High (inherently standardized) | Utilizes the same method and parameter set, enabling direct data comparison [49]. |
Protocol for Leveraging Published Validations: A Verification Framework
When a laboratory adopts a method from a peer-reviewed publication, it moves from validation to verification. The following workflow and detailed protocol outline this process.
Figure 1: Workflow for the Verification of a Published Method
Pre-verification Phase: Protocol Definition
A Validation Protocol is a forward-looking, pre-approved plan that defines the strategy, design, and acceptance criteria for the study [51]. Before any laboratory work begins, the team must prepare and approve this protocol.
- Objective and Scope: Clearly state the purpose is to verify the published method within the user's specific environment. The scope must define the method's intended use [51].
- Method Description: Provide a detailed description of the method, strictly adhering to the parameters published in the source journal article (e.g., equipment, reagents, software settings) [49] [51].
- Verification Parameters and Acceptance Criteria: Define the specific validation parameters to be tested and the acceptance criteria, which must be based directly on the data reported in the publication. Key parameters typically include [51]:
- Accuracy
- Precision (Repeatability, Intermediate Precision)
- Specificity
- Linearity and Range
- Limit of Detection (LOD) and Quantitation (LOQ)
- Experimental Design: Outline the procedure for the verification experiments, including the number of replicates, concentration levels, and sample matrices to be tested. This design should be a subset of the original validation, sufficient to confirm performance [49].
- Responsibilities and Timelines: Assign roles and set a timeline for the verification activities [51].
Execution and Analysis Phase
- Adherence to Method: Execute the verification study, strictly following the published method as detailed in the protocol. Any deviation must be documented and scientifically justified in the final report [49] [51].
- Data Collection and Analysis: Collect raw data and perform the statistical analysis as specified in the protocol. Compare the results directly against the pre-defined acceptance criteria derived from the publication [51].
Post-verification Phase: Report Generation
A Validation Report is a retrospective document that summarizes the study results and concludes whether the method is valid for its intended use [51].
- Summary of Study: Briefly describe the verification exercise and its purpose.
- Raw Data and Statistical Analysis: Present all raw data and the analysis conducted.
- Comparison with Acceptance Criteria: Provide a clear comparison between the obtained results and the acceptance criteria.
- Deviations and Investigations: Document any deviations from the protocol and the investigations performed to address them.
- Conclusion and Recommendation: Conclude whether the method verification was successful and recommend the method for implementation in routine use [51].
Advanced Applications: Integrating Vendor Data and Statistical Tools
Leveraging Vendor Testing Data
A highly efficient strategy is the formal integration of vendor-provided test data and documents into the validation lifecycle. Vendors conduct comprehensive testing with deep product knowledge, and leveraging their documents can eliminate duplication and accelerate timelines [50].
- Strategy: For Computer Systems Validation (CSV) and Equipment Validation, incorporate vendor test documents and results for Operational Qualification (OQ) and Performance Qualification (PQ). Vendor tests can often be replicated with the user's own materials and processes [50].
- Digital Integration: Use a Validation Lifecycle Management System (VLMS) to electronically execute vendor-provided PDF test documents. This maintains end-to-end digital continuity, avoids the errors and data integrity risks of paper-based hybrid processes, and ensures compliance with ALCOA+ principles [50].
- Benefits:
Statistical Methods for Validation and Comparison
Robust statistical analysis is the foundation of any comparative method study. The following tools are essential for ensuring the validity and reliability of the data.
Table 2: Essential Statistical Techniques for Method Validation and Comparison
| Statistical Technique | Function in Method Validation | Key Application Considerations |
|---|---|---|
| Exploratory Factor Analysis (EFA) | Assesses construct validity by identifying a smaller set of latent factors that explain the variability in a larger set of measured variables [52]. | Used in psychometric analysis to validate questionnaires assessing perceptions (e.g., user acceptance of a new method). Requires assessment of data factorability and decision on factor retention criteria [52]. |
| Reliability Analysis | Quantifies the extent to which variance in results is attributable to the latent variables, indicating the consistency of a measurement instrument [52]. | Measured by metrics like Cronbach's alpha. Ensures the tool (e.g., a new method for measuring a complex attribute) produces stable and consistent results [53] [52]. |
| Sample Size & Power Analysis | Determines the number of participants or samples needed to detect a true effect with a certain probability [48]. | Based on four parameters: significance level (α, often 0.05), power (1-β, often 0.8), effect size (minimal clinically relevant difference), and population variability [48]. |
| Gradient Boosting / Machine Learning | Enhances traditional efficiency analysis methods (like Data Envelopment Analysis) to handle complex, non-linear data patterns and undesirable outputs [54]. | Improves accuracy in predicting production functions and discerning subtle inefficiencies in analytical processes that deterministic methods might overlook [54]. |
The Scientist's Toolkit: Key Reagents and Research Solutions
The following table details essential "research reagent solutions" and materials critical for conducting method validation and verification studies.
Table 3: Essential Research Reagents and Materials for Method Validation
| Item / Solution | Function in Validation |
|---|---|
| Certified Reference Materials (CRMs) | Provides a standardized, traceable benchmark with known purity and concentration to establish accuracy and calibration during method development and verification. |
| Stable Isotope-Labeled Internal Standards | Accounts for variability in sample preparation and instrument response; critical for achieving precise and accurate quantitative results in LC-MS/MS methods. |
| System Suitability Test (SST) Solutions | A mixture of key analytes used to verify that the chromatographic system and instrument are performing adequately at the start of, during, and at the end of an analytical run. |
| Validation Sample Kits (Accuracy/Precision) | Pre-prepared sets of samples at specified concentrations (e.g., blank, LLOQ, low, mid, high, upper limit of quantification) to streamline the testing of key validation parameters. |
| Mobile Phase Buffers & Reagents | High-purity solvents and buffers formulated for consistent pH and ionic strength to ensure chromatographic reproducibility, which is fundamental to method robustness. |
| Data Integrity & Management Platform (e.g., VLMS) | A digital system for electronically executing test protocols, managing vendor data, and maintaining an audit trail to ensure compliance with ALCOA+ principles [50]. |
Collaborative models and the strategic leverage of published data represent a significant evolution in the comparative methodology of analytical method validation. By shifting from isolated, full validations to cooperative, verification-focused approaches, laboratories can achieve substantial gains in efficiency, cost-effectiveness, and standardization. This paradigm, supported by robust protocols, statistical rigor, and digital tools, enables drug development professionals to accelerate timelines, reallocate valuable resources, and maintain the highest standards of data quality and regulatory compliance.
Validation, Regulatory Context, and Advanced Comparability Strategies
Comparative Method within ICH Q2 and Broader Regulatory Guidelines
In the pharmaceutical and biotech sectors, the "comparative method" is a fundamental principle applied throughout the analytical procedure lifecycle to ensure continuous method suitability, reliability, and compliance. With the formal adoption of ICH Q2(R2) on validation and ICH Q14 on analytical procedure development in November 2023, regulatory expectations have evolved to emphasize a more structured, knowledge-based approach to method comparison activities [55] [56]. These guidelines recognize that drug development is inherently dynamic, and analytical methods must consequently evolve in response to new data, updated processes, and changing regulatory expectations [18].
The comparative method encompasses two distinct but related concepts: comparability and equivalency [18]. Comparability evaluates whether a modified analytical procedure yields results sufficiently similar to the original method to ensure consistent product quality assessment without affecting the control strategy. Equivalency involves a more rigorous, statistically driven assessment to demonstrate that a replacement method performs equal to or superior to the original procedure, typically requiring full validation and regulatory approval before implementation [18]. Understanding this distinction is critical for researchers, scientists, and drug development professionals navigating analytical method changes within the current regulatory framework.
Regulatory Framework and Key Guidelines
Evolution from ICH Q2(R1) to ICH Q2(R2)
The International Council for Harmonisation (ICH) officially adopted Q2(R2) as a harmonized guideline on November 1, 2023, marking a significant evolution from the previous Q2(R1) standard [55] [56]. This updated validation guideline provides expanded guidance for validating analytical procedures, with particular enhancements for biological and biotechnological products [56]. The revision incorporates informative annexes that provide additional detail on validation considerations, addressing previous gaps in the guidance [56].
Multiple regulatory authorities have officially incorporated Q2(R2) and Q14, with others in the process of adoption [55]. To support consistent global implementation, the ICH released comprehensive training materials in July 2025, developed by the Q2(R2)/Q14 Implementation Working Group (IWG) [57]. These resources aim to foster a harmonized understanding and application of the new guidelines across both ICH and non-ICH regions, illustrating both minimal and enhanced approaches to analytical development and validation [57].
ICH Q14: Analytical Procedure Development and Lifecycle Management
ICH Q14 introduces, for the first time, comprehensive guidance on the development of analytical procedures [55]. This guideline works in concert with Q2(R2) to establish a complete framework for the entire analytical procedure lifecycle, from initial development through validation and ongoing management [18]. Q14 emphasizes a structured, risk-based approach to assessing, documenting, and justifying method changes, encouraging the use of prior knowledge and data to drive decisions [18].
A foundational concept introduced in ICH Q14 is the Analytical Target Profile (ATP), which defines the required quality attributes of an analytical procedure to ensure it remains fit-for-purpose throughout its lifecycle [18]. By defining the ATP early in development, organizations can create analytical procedures with future needs in mind, thereby minimizing the impact of changes when they become necessary.
Complementary Regulatory Guidelines
While ICH guidelines provide the international standard, several complementary guidelines complete the regulatory landscape for analytical method validation:
- FDA's Analytical Procedures and Methods Validation Guidance: Expands upon the ICH framework with requirements specific to the U.S. regulatory landscape, emphasizing method robustness and comprehensive documentation of analytical accuracy [58].
- USP <1225> Validation of Compendial Procedures: Establishes validation requirements for four categories of analytical procedures used in pharmaceutical testing [58].
- ICH Q12: Provides guidance on established conditions and change management, which interfaces directly with analytical procedure lifecycle management [57].
Table 1: Key Regulatory Guidelines Governing Comparative Methods
| Guideline | Scope | Focus Areas | Status |
|---|---|---|---|
| ICH Q2(R2) | Validation of analytical procedures | Enhanced validation parameters, biological assays, annexes with examples | Adopted Nov 2023; implemented in multiple regions [55] [56] |
| ICH Q14 | Analytical procedure development | ATP, risk-based development, lifecycle management, change management | Adopted Nov 2023; implemented in multiple regions [55] [18] |
| FDA Analytical Procedures Guide | Method validation for U.S. submissions | Method robustness, life-cycle management, revalidation procedures | Current [58] |
| USP <1225> | Validation of compendial procedures | Categorization of methods, performance characteristics, acceptance criteria | Current [58] |
Method Comparability vs. Equivalency: Key Concepts
Comparability Assessments
Comparability in analytical procedures refers to the evaluation of whether a modified method yields results sufficiently similar to the original procedure, ensuring consistent assessment of product quality attributes [18]. Comparability studies typically confirm that modified procedures produce expected results while maintaining the established control strategy. These changes are generally considered lower risk and may not require regulatory filings or commitments prior to implementation [18].
Common scenarios requiring comparability assessments include:
- Minor method adjustments to improve operational efficiency
- Technology upgrades within the same methodology (e.g., HPLC instrument replacements)
- Supplier changes for critical reagents with demonstrated quality equivalence
- Updates to address continuous improvement initiatives
For low-risk procedural changes where the method's range of use has been defined through robustness studies, minimal additional experimental work may be necessary to support the comparability claim [18].
Equivalency Demonstrations
Equivalency represents a more rigorous standard than comparability, requiring comprehensive assessment to demonstrate that a replacement method performs equal to or better than the original procedure [18]. Equivalency studies typically necessitate full validation of the new method and statistical comparison to the established procedure. Such changes require regulatory approval prior to implementation [18].
Scenarios typically requiring equivalency demonstrations include:
- Complete replacement of an analytical method with a fundamentally different methodology
- Changes to methods for critical quality attributes with narrow acceptance criteria
- Transfer of methods between laboratories with significantly different operating environments
- Platform method implementation across multiple products or material types
Table 2: Comparison of Method Comparability and Equivalency Requirements
| Aspect | Comparability | Equivalency |
|---|---|---|
| Definition | Evaluation of sufficient similarity between original and modified method [18] | Demonstration of equal or superior performance of replacement method [18] |
| Regulatory Impact | Typically does not require prior regulatory approval [18] | Requires regulatory approval before implementation [18] |
| Validation Requirements | Partial validation or verification may be sufficient [18] | Full validation typically required [18] |
| Statistical Rigor | Moderate statistical assessment | Comprehensive statistical evaluation with predefined acceptance criteria [18] |
| Common Scenarios | Minor modifications, technology upgrades, supplier changes [18] | Method replacements, technology transfers, platform method implementation [18] |
Experimental Design for Comparative Studies
Method Equivalency Study Design
A robust method equivalency study incorporates multiple experimental components to generate conclusive evidence of equivalent or superior performance:
Side-by-Side Testing: Analysis of representative samples using both the original and new methods under standardized conditions [18]. This should include a sufficient number of replicates to account for normal method variation and cover the entire validated range.
Statistical Evaluation: Application of appropriate statistical tools to quantify agreement between methods [18]. Common approaches include paired t-tests, ANOVA, equivalence testing, and tolerance interval analysis [59]. The statistical methods should be predetermined in the study protocol with justified acceptance criteria.
Acceptance Criteria: Predefined thresholds based on method performance attributes and critical quality attributes (CQAs) [18]. These criteria should reflect the analytical requirement to detect meaningful differences in product quality.
Risk-Based Documentation: Tailoring of documentation and regulatory submissions to the criticality of the change and its potential impact on product quality assessment [18].
Statistical Approaches for Comparative Studies
The ICH Q2(R2) guideline acknowledges that vague terminology in previous versions necessitated effective protocol design and data analysis [59]. Appropriate statistical methods should be employed to demonstrate both precision and accuracy claims, with all relevant data and formulae documented for regulatory submission [59].
Key statistical considerations include:
Specificity Testing: Demonstration of the ability to detect the analyte of interest in the presence of interfering substances [59]. This can be shown by spiking known levels of impurities or degradants into a sample with a known amount of the analyte of interest, typically testing a neat sample and a minimum of three different levels of interfering substances [59].
Precision Analysis: Evaluation of both repeatability (intra-assay precision) and intermediate precision (different days, analysts, equipment) [59]. The suggested testing consists of a minimum of two analysts on two different days with three replicates at a minimum of three concentrations [59].
Accuracy and Linearity: Assessment through confidence intervals or tolerance intervals to set appropriate accuracy specifications [59]. Linearity is typically demonstrated via least squares regression with a minimum of five dose levels throughout the range, each tested for a minimum of three independent readings [59].
The following workflow diagram illustrates the decision process for selecting between comparability and equivalency approaches:
Implementation Toolkit for ICH Q2(R2) Compliance
Gap Analysis and Change Management
Transitioning from ICH Q2(R1) to Q2(R2) requires systematic assessment of existing methods and validation practices. Researchers have developed a comprehensive toolkit designed to streamline risk assessment and change management efforts [55] [56]. This toolkit identifies 56 specific omissions, expansions, and additions between the previous and current guidelines, providing a structured approach to compliance [55].
Key components of this implementation toolkit include:
- Gap Analysis Worksheet Template: Outlines specific changes between Q2(R1) and Q2(R2) to facilitate systematic assessment of current validation practices [56].
- Risk Assessment Framework: Enables prioritization of method revalidation activities based on product criticality and extent of change required [55].
- Change Management Protocol: Provides a structured approach to documenting and implementing necessary changes to analytical procedures [55].
- Training Materials: Comprehensive modules covering fundamental principles and practical applications of Q2(R2) and Q14 [57].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of comparative methods requires specific materials and reagents tailored to the analytical technique and product type. The following table details essential components of the scientist's toolkit for comparative method studies:
Table 3: Essential Research Reagent Solutions for Comparative Method Studies
| Reagent/Material | Function | Application in Comparative Studies |
|---|---|---|
| Reference Standards | Provides known quality analyte for method calibration and performance assessment | Qualification of both original and modified methods; demonstration of accuracy [59] |
| System Suitability Solutions | Verifies proper function of analytical system before sample analysis | Ensures both methods are operating within specified parameters during comparative testing [58] |
| Forced Degradation Samples | Contains intentionally degraded analyte to evaluate method specificity | Demonstrates equivalent specificity for stability-indicating methods [59] |
| Placebo/Matrix Blanks | Contains all components except analyte to assess interference | Evaluation of equivalent specificity between original and modified methods [59] |
| Quality Control Samples | Known concentration samples for accuracy and precision assessment | Statistical comparison of method performance using predefined acceptance criteria [18] |
Case Studies and Practical Applications
Platform Method Implementation
The concept of platform methods represents a proactive approach to comparative method challenges [18]. By developing flexible procedures that apply across multiple materials and strengths, organizations can minimize the need for extensive revalidation when changes occur. Platform methods are particularly valuable in early-phase development, where they can anticipate future manufacturing or formulation changes [18].
Case Study: A biotech company developed a platform HPLC method for related substances that was specifically designed to accommodate anticipated process improvements. By establishing specificity and accuracy across a broader range of excipients than initially required, the method retained suitability despite significant manufacturing changes, avoiding the need for complete revalidation [18].
Risk-Based Change Management
ICH Q14 encourages a structured, risk-based approach to assessing, documenting, and justifying method changes [18]. This approach tailors the level of evidence required to the potential impact on product quality and the analytical procedure's ability to monitor critical quality attributes.
Case Study: A pharmaceutical manufacturer implemented a risk-based classification system for analytical procedure changes, categorizing modifications as low, medium, or high risk based on their potential impact on the control strategy [18]. This system allowed for appropriate resource allocation, with low-risk changes requiring only comparability assessments while high-risk changes necessitated full equivalency studies [18].
Emerging Trends in Comparative Methods
The implementation of ICH Q2(R2) and Q14 continues to evolve, with regulatory authorities providing further clarification on interpretation and application. The close relationship between analytical method development and validation means that many aspects of Q14 are reflected in Q2(R2) implementation [55]. Future directions in comparative methods include:
- Increased Application of Enhanced Approaches: ICH Q14 describes both minimal and enhanced approaches to analytical development, with the enhanced approach incorporating more structured procedures and risk management [57].
- Multivariate Analytical Procedures: The ICH training materials include specific modules addressing multivariate methods, representing an expansion of the traditional univariate approach to analytical validation [57].
- Knowledge Management Systems: Effective capture and leverage of development data to inform future modifications and troubleshooting [18].
ICH Q14 and Q2(R2) collectively transform how organizations approach analytical procedures, emphasizing long-term planning from the outset [18]. The comparative method—encompassing both comparability and equivalency assessments—serves as a critical tool for maintaining analytical control throughout a product's lifecycle while accommodating necessary evolution in analytical technologies and practices.
By cultivating a forward-thinking culture and implementing the structured approaches outlined in the latest regulatory guidelines, organizations can transition their change management practices from reactive to proactive [18]. Through intelligent design, validations become more seamless, and analytical procedures can stay aligned with innovation, remaining fit-for-purpose throughout a product's commercial lifecycle [18].
In the tightly regulated pharmaceutical landscape, analytical methods cannot remain static throughout a product's lifecycle. Changes in manufacturing processes, technological advancements, and continuous improvement initiatives necessitate modifications to analytical procedures [18]. Analytical method comparability and analytical method equivalency represent two distinct, structured approaches for validating these changes, serving as the core comparative methods in analytical validation research. These methodologies ensure that altered or replacement methods provide reliable, accurate data to guarantee product quality and patient safety, forming a critical component of the analytical procedure lifecycle management [18] [7].
A comparative method in this context is a systematic, evidence-based process for evaluating the performance of a new or modified analytical procedure against an established one. The fundamental premise is to generate sufficient data to demonstrate that the updated method is fit-for-purpose and that the change does not adversely impact the decision-making process regarding product quality [7]. The choice between demonstrating comparability or equivalency is guided by a risk-based approach, which allocates resources based on the potential impact of the method change on product quality and patient safety [60] [61]. This strategy aligns with modern regulatory paradigms outlined in ICH Q14 (Analytical Procedure Development) and ICH Q9 (Quality Risk Management), emphasizing scientific understanding and risk control over prescriptive rules [18] [62].
Core Concepts: Distinguishing Comparability from Equivalency
Analytical Method Comparability
Analytical method comparability refers to studies that evaluate the similarities and differences in method performance characteristics between two analytical procedures [7]. It is a broader evaluation that assesses whether a modified method yields results that are sufficiently similar to the original method, ensuring consistent assessment of product quality [18]. The goal is to confirm that the modified procedure produces the expected results and remains suitable for its intended purpose without necessarily demonstrating statistical equality.
- Purpose: To demonstrate that the modified method's performance is sufficiently similar to the original method.
- Regulatory Impact: These changes typically do not require regulatory filings or commitments prior to implementation [18].
- Typical Use Cases: Minor changes, such as adjustments within the method's established design space or robustness range, equipment upgrades within the same technology platform, or supplier changes for reagents [18] [7].
Analytical Method Equivalency
Analytical method equivalency is a more rigorous, subset of comparability. It involves a comprehensive assessment, often requiring full validation, to demonstrate that a replacement method performs equal to or better than the original procedure [18]. Chatfield et al. suggest that equivalency should be restricted to a formal statistical study to evaluate similarities in method performance characteristics [7].
- Purpose: To demonstrate that the new method generates equivalent results to the original method, often through formal statistical testing [7].
- Regulatory Impact: Such changes require regulatory approval prior to implementation [18].
- Typical Use Cases: High-risk changes, such as method replacements, changes in separation mechanism (e.g., normal-phase to reversed-phase HPLC), changes in detection technique, or alterations outside the established robustness ranges [18] [7].
The following workflow outlines a risk-based decision process for determining when to perform comparability versus equivalency studies:
The Risk-Based Framework for Decision Making
Foundations of Risk-Based Approach
A risk-based approach to analytical method changes ensures that the level of effort and rigor in comparative validation is proportional to the potential impact on product quality and patient safety [60]. This framework is anchored in ICH Q9 (Quality Risk Management) principles and is further supported by ICH Q14 for analytical procedure lifecycle management [18] [62]. The fundamental question driving this approach is: "What is the potential of this method change to affect the ability of the method to accurately measure critical quality attributes (CQAs)?"
Risk assessment provides a structured framework to evaluate potential failure points during testing procedures [60]. By implementing risk assessment early, organizations can allocate resources more efficiently, focusing validation efforts where they are most needed [60]. This proactive approach typically reduces unnecessary testing by 30-45% while maintaining or improving quality outcomes [60].
Risk Classification and Strategy
The level of risk associated with an analytical method change determines the appropriate comparative strategy. The following table outlines common risk categories and the recommended approach for each:
Table 1: Risk-Based Classification for Analytical Method Changes
| Risk Level | Type of Change | Recommended Approach | Documentation & Regulatory Requirements |
|---|---|---|---|
| Low Risk | Changes within pharmacopoeial allowed ranges (e.g., USP <621>) or within established method robustness ranges [7] | Comparability often sufficient; may not require specific comparative studies [7] | Documentation within internal quality systems; typically does not require regulatory submission [18] |
| Medium Risk | Technology upgrades (HPLC to UHPLC with similar separation mechanism), software updates, column supplier changes [18] | Comparability with side-by-side testing on representative samples; may include limited statistical evaluation [18] | Internal documentation with scientific justification; may require regulatory notification depending on change criticality [7] |
| High Risk | Changes to separation mechanism, detection technique, or method replacement [7]; Methods with stability-indicating properties [7] | Equivalency requiring formal statistical demonstration [18] [7] | Comprehensive documentation with statistical analysis; requires regulatory approval prior to implementation [18] |
Risk Assessment Tools and Methodologies
Various tools facilitate systematic risk assessment for analytical methods:
Analytical Target Profile (ATP): A predefined objective that defines the required quality of measurements produced by the method [18] [62]. The ATP serves as the foundation for risk assessment, as all potential failures are evaluated against their impact on achieving the ATP.
Failure Mode Effects Analysis (FMEA): A systematic approach for identifying potential failure modes in the analytical method, their causes, and effects [60]. Each potential failure is rated for severity, occurrence, and detection, with a risk priority number (RPN) guiding mitigation efforts.
Ishikawa (Fishbone) Diagrams: Visual tools used to identify and group potential sources of variation according to categories such as the 6 Ms (Mother Nature, Measurement, humanpower, Machine, Method, and Material) [62].
Risk Assessment Matrices: Tools that combine the probability of occurrence of harm with the severity of that harm to determine risk levels and appropriate mitigation strategies [61].
Experimental Protocols for Comparability and Equivalency Studies
Protocol for Analytical Method Comparability
For lower-risk changes where a comparability study is deemed appropriate, the following methodology provides a structured approach:
Define Study Scope and Acceptance Criteria: Based on the risk assessment, define which method performance characteristics will be compared (e.g., precision, accuracy, specificity) and establish predefined acceptance criteria prior to study initiation [18].
Select Representative Samples: Choose samples that represent the variability encountered during routine analysis, typically including samples from multiple batches that cover the specification range [18].
Execute Side-by-Side Testing: Analyze the selected samples using both the original and modified methods. The testing should incorporate realistic variation, such as different analysts, instruments, or days, to demonstrate robustness [18].
Evaluate Data: Compare the results against the predefined acceptance criteria. This evaluation may include visual comparison of chromatograms, calculation of percent difference for assay values, or comparison of impurity profiles [7].
Document and Report: Document the study protocol, raw data, analysis, and conclusions. Justify that any observed differences do not impact the method's ability to accurately measure the relevant quality attributes [18].
Protocol for Analytical Method Equivalency
For high-risk changes requiring a demonstration of equivalency, a more rigorous, statistically grounded approach is necessary:
Define Equivalence Margin: Establish the upper and lower practical limits (equivalence margin) where deviations are considered practically zero [63]. This margin should be risk-based, considering:
- Product knowledge and clinical relevance
- Impact on process capability and out-of-specification (OOS) rates
- Method performance requirements and specifications [63]
Table 2: Risk-Based Acceptance Criteria for Equivalence Testing
Risk Level Typical Acceptance Criterion (% of tolerance) Statistical Confidence Level High Risk 5-10% 95% (Alpha=0.05) Medium Risk 11-25% 95% (Alpha=0.05) Low Risk 26-50% 90% (Alpha=0.10) Adapted from industry practices described in [63]
Determine Sample Size: Calculate the minimum sample size needed to achieve sufficient statistical power (typically 80-90%) using formula:
n=(tâ‚−α+tâ‚−β)²(s/δ)²for one-sided tests, where 's' is the estimated standard deviation and 'δ' is the equivalence margin [63].Execute Controlled Study: Conduct side-by-side testing using both methods on an appropriate number of samples that represent the expected range of the analytical procedure. Incorporate expected routine variation (different analysts, instruments, days) [18].
Perform Statistical Analysis - Two One-Sided Tests (TOST):
- Use the TOST approach to demonstrate that the difference between methods is significantly less than the upper practical limit AND significantly greater than the lower practical limit [63].
- Calculate confidence intervals (typically 90% for equivalence) for the difference between methods [63].
- If the entire confidence interval falls within the equivalence margin, equivalence is demonstrated [63].
Document and Report: Prepare a comprehensive report including the statistical analysis, raw data, and scientific justification for the equivalence margins. This package typically requires regulatory submission and approval [18] [7].
The following diagram illustrates the statistical concept of equivalence testing using the TOST approach:
The Scientist's Toolkit: Essential Reagents and Solutions
Successful implementation of comparability and equivalency studies requires specific materials and reagents to ensure reliable, reproducible results. The following table details key research reagent solutions and their functions in analytical method comparison studies:
Table 3: Essential Research Reagent Solutions for Comparative Method Studies
| Reagent/Solution | Function/Purpose | Critical Quality Attributes |
|---|---|---|
| System Suitability Test Solutions | Verify chromatographic system performance before comparative analysis [64] | Precise retention time, peak symmetry, resolution between key peaks; must be stable throughout study duration |
| Reference Standards | Calibrate both methods to ensure accurate quantification [63] | Certified purity, stability, well-characterized impurities; should be from qualified suppliers |
| Placebo/Blank Solutions | Demonstrate specificity and selectivity of both methods [65] | Must represent all formulation components; should show no interference with analyte peaks |
| Quality Control Samples | Monitor method performance throughout the study; typically at low, medium, and high concentrations [66] | Prepared from independent weighing; cover specification range; used to assess accuracy and precision |
| Stressed Samples | For stability-indicating methods, demonstrate that both methods can adequately separate and quantify degradation products [7] | Artificially degraded samples (heat, light, acid/base oxidation); should generate relevant degradants |
| Mobile Phase Buffers | Maintain consistent pH and ionic strength for chromatographic separations [62] | Precise pH control, filtered and degassed; prepared consistently for both methods |
Regulatory Landscape and Compliance Considerations
Global Regulatory Expectations
Regulatory expectations for analytical method comparability and equivalency vary across major markets, though all emphasize a science-based, risk-informed approach:
ICH Guidelines: ICH Q2(R2) provides guidance on validation of analytical procedures, while ICH Q14 outlines a structured approach to analytical procedure development and lifecycle management [65] [18]. These guidelines encourage a science- and risk-based approach to method changes.
US FDA: The FDA's draft guidance "Comparability Protocols - Chemistry, Manufacturing, and Controls Information" states that proper validation is required to demonstrate that a new analytical method provides similar or better performance compared with the existing method [7]. The agency recommends that whether an equivalency study is needed depends on the extent of the proposed change, type of product, and type of test [7].
European Pharmacopoeia: The new Ph. Eur. chapter 5.27 "Comparability of alternative analytical procedures" describes how comparability may be demonstrated, emphasizing that the final responsibility lies with the user and must be documented to the satisfaction of the competent authority [67].
USP: USP General Chapter <1010> "Analytical Data-Interpretation and Treatment" discusses statistical approaches to compare method precision and accuracy [7]. USP <1033> recommends equivalence testing over significance testing for biological assay validation [63].
Documentation and Submission Requirements
Proper documentation is critical for successful regulatory compliance:
- For Comparability Studies: Include method information, reason for change, risk assessment, comparative data, and justification that the method remains fit-for-purpose [7].
- For Equivalency Studies: Provide comprehensive package including protocol with predefined acceptance criteria, full validation data for the new method, side-by-side comparison data, statistical analysis (including equivalence testing), and scientific justification for equivalence margins [7] [63].
Survey results from International Consortium for Innovation and Quality in Pharmaceutical Development (IQ) member companies indicate that 68% have had successful regulatory reviews of analytical method comparability packages, while 47% have received questions from health authorities, highlighting the importance of thorough, well-documented submissions [7].
The distinction between analytical method comparability and equivalency represents a fundamental comparative method in pharmaceutical analytical science, enabling continuous improvement while ensuring product quality and patient safety. A risk-based approach provides a rational framework for determining the appropriate level of evidence needed to justify method changes, focusing resources where they have the greatest impact on quality.
As the regulatory landscape evolves with ICH Q14 and updated ICH Q2(R2), the emphasis on analytical procedure lifecycle management continues to grow [18] [65]. Implementing a robust, risk-based strategy for method changes not only facilitates regulatory compliance but also enhances operational efficiency. Companies adopting these approaches report reductions in validation timelines by up to 65% and decreases in unnecessary testing by 30-45%, while maintaining or improving quality outcomes [60].
The successful implementation of this framework requires cross-functional collaboration, thorough scientific understanding, and appropriate statistical applications. When executed properly, this approach transforms method change management from a reactive, compliance-driven activity to a proactive, science-based enabler of innovation and continuous improvement throughout the product lifecycle.
Managing Method Changes in Registration and Post-Approval Stages
In the pharmaceutical industry, managing changes to analytical methods during the registration and post-approval stages is a critical component of Chemistry, Manufacturing, and Controls (CMC). Analytical methods are integral parts of CMC, and common reasons for method changes include applying new analytical technologies and accommodating changes in chemical or formulation processes [7].
When changes are made, pharmaceutical companies must demonstrate that the new method provides equivalent or better performance than the existing method. This process is known as analytical method comparability [7]. Within this broader concept, analytical method equivalency refers specifically to studies that evaluate whether a new method can generate equivalent results to the existing method for the same samples [7].
Unlike analytical method validation, which has clear regulatory guidelines (ICH Q2), limited formal guidance exists specifically for method comparability studies. Regulatory expectations are that companies will adopt risk-based approaches to determine when and how to perform comparability studies, considering the extent of the proposed change, product type, and test type [7].
Regulatory Framework and Key Guidelines
Regulatory Landscape
Several regulatory documents provide guidance on analytical method changes:
- FDA Draft Guidance (2003): Stated that proper validation is required to demonstrate similar or better performance with method changes [7]
- USP General Chapter <1010>: Provides statistical approaches for method comparison [7]
- ICH Q2(R2): The revised guideline on validation of analytical procedures emphasizes modern technologies and risk-based approaches [68]
- ICH Q14: Provides a framework for analytical procedure development, introducing the Analytical Target Profile (ATP) concept [68]
Regulatory agencies generally expect that analytical method equivalency must be demonstrated when changes are made, though requirements vary based on the significance of the change [7].
Risk-Based Approach
A risk-based approach is recommended for analytical method comparability, particularly for HPLC assay and impurities methods [7]. The level of rigor required depends on:
- Type of change: Changes within established robustness ranges or compendial allowances may need only validation, while more significant changes (e.g., separation mechanism changes) typically require full equivalency studies [7]
- Product criticality: Tests for critical quality attributes generally require more rigorous assessment
- Stage of product lifecycle: Post-approval changes typically require more extensive data than those during development [7]
Table: Risk Assessment for Analytical Method Changes
| Change Type | Risk Level | Typical Requirement |
|---|---|---|
| Changes within USP <621> chromatography ranges | Low | Method validation only |
| Changes within established robustness ranges | Low to Moderate | Limited comparability assessment |
| Change in stationary phase chemistry | Moderate to High | Side-by-side comparison |
| Change in detection technique (e.g., UV to MS) | High | Full equivalency study |
| Change in separation mechanism (e.g., normal-phase to reversed-phase) | High | Extensive comparability package with overlapping stability data |
The Comparative Method Concept
Defining the Comparative Method
In analytical method comparability, the comparative method (or "reference method") serves as the benchmark against which the new method is evaluated. The choice of comparative method significantly impacts data interpretation [1].
A true reference method has established correctness through comparison with definitive methods or traceable reference materials. With a reference method, differences are attributed to the test method [1]. Most routine laboratory methods fall into the broader comparative method category, where differences must be carefully interpreted to identify which method is inaccurate [1].
Statistical Approaches for Method Comparison
Statistical analysis is essential for demonstrating method equivalency. The appropriate statistical approach depends on the data characteristics and study design.
Table: Statistical Methods for Analytical Method Comparison
| Statistical Method | Application | Interpretation |
|---|---|---|
| Linear Regression | Wide analytical range (e.g., glucose, cholesterol) | Provides slope (proportional error) and y-intercept (constant error) |
| Paired t-test | Narrow analytical range (e.g., sodium, calcium) | Determines average difference (bias) between methods |
| Correlation Coefficient (r) | Assess data range suitability | r ≥ 0.99 indicates sufficient range for reliable regression |
| Difference Plot | Visual assessment of agreement | Shows differences versus concentration to identify error patterns |
For regression analysis, systematic error (SE) at a critical decision concentration (Xc) is calculated as:
- Yc = a + bXc (where a = y-intercept, b = slope)
- SE = Yc - Xc [1]
Experimental Design for Method Comparability
Sample Selection and Handling
Proper experimental design is crucial for reliable comparability data:
- Number of specimens: Minimum of 40 patient specimens recommended, selected to cover the entire working range [1]
- Sample quality: Carefully selected specimens with wide concentration range are more important than large numbers of random specimens [1]
- Sample stability: Analyze specimens within two hours of each other by both methods, unless stability data supports longer intervals [1]
- Matrix representation: Samples should represent the spectrum of diseases expected in routine application [1]
Measurement Protocol
- Replication strategy: Single measurements are common, but duplicates provide better reliability by identifying sample mix-ups or transposition errors [1]
- Time period: Minimum of 5 different days recommended to minimize run-to-run variability [1]
- Experimental duration: Extending over 20 days (with 2-5 specimens daily) aligns with long-term precision studies [1]
Data Analysis and Interpretation
Graphical Data Analysis
Visual data inspection is fundamental for identifying patterns and discrepant results:
- Difference plots: Display test minus comparative results (y-axis) versus comparative results (x-axis) to visualize errors across concentrations [1]
- Comparison plots: Display test results (y-axis) versus comparative results (x-axis) for methods not expected to show 1:1 agreement [1]
- Boxplots: Show distributions of results from both methods for easy visual comparison [69]
Handling Discrepant Results
- Initial inspection: Graph data as collected to identify large differences requiring confirmation [1]
- Outlier investigation: Reanalyze specimens with discrepant results while samples are still available [1]
- Cause identification: Investigate whether differences represent true method performance issues or procedural errors [1]
Method Transfer Considerations
Transfer Protocols
When method changes involve transferring methods between laboratories, several protocol options exist:
- Comparative Testing: Both laboratories test the same samples and compare results (most common approach) [70] [71]
- Co-validation: Both laboratories collaborate on validation studies [70] [71]
- Revalidation: Receiving laboratory performs partial or full revalidation [70] [71]
- Waiver: Transfer waiver may be justified for compendial methods or identical laboratory conditions [70]
Transfer Challenges
Common challenges in method transfer include:
- Instrument variability: Differences in calibration, maintenance, or components between instruments [70] [71]
- Reagent variability: Different lots of reagents or columns affecting results, particularly in HPLC methods [70] [71]
- Analyst technique: Differences in analyst training, experience, or technique [70]
- Environmental conditions: Variations in temperature, humidity, or laboratory setup [71]
Implementation Framework
Developing a Comparability Protocol
A structured approach ensures successful method comparability studies:
- Define Objective and Scope: Clearly state the purpose and specific methods being compared [70]
- Establish Acceptance Criteria: Predefine statistically sound success criteria based on the method's original validation data and intended use [70]
- Document Responsibilities: Define roles of sending unit, receiving unit, and quality assurance [71]
- Outline Procedures: Detail sample preparation, instrument run sequences, and data analysis methods [70]
- Plan for Deviations: Establish processes for handling out-of-specification results [70]
Documentation and Reporting
Comprehensive documentation is essential for regulatory compliance:
- Protocol approval: Obtain quality assurance approval before study initiation [71]
- Data reporting: Compile all analytical data with emphasis on deviations and investigations [71]
- Final report: Include summary of results against acceptance criteria, conclusion on success, and documentation of any deviations [70]
- Regulatory filing: For critical methods, submit comparability results to regulatory authorities [71]
Workflow and Decision Framework
Method Change Assessment Workflow
The following diagram illustrates the decision process for managing analytical method changes:
Experimental Design for Comparability Testing
The following workflow details the experimental approach for method comparability studies:
Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for Method Comparability Studies
| Reagent/Material | Function | Critical Considerations |
|---|---|---|
| Reference Standards | Quantification and method calibration | Use same lot for both methods; ensure traceability and purity [70] [71] |
| Chromatography Columns | Stationary phase for separation | Match chemistry, dimensions, and lot between methods; critical for HPLC/UHPLC methods [7] [71] |
| Mobile Phase Reagents | Liquid chromatography eluent components | Standardize grade, supplier, and preparation methods [70] [71] |
| Sample Preparation Reagents | Extraction, dilution, or derivation of analytes | Control purity, pH, and composition variability [71] |
| System Suitability Standards | Verify system performance before analysis | Use validated reference materials to ensure both methods operate within specifications [71] |
| Quality Control Samples | Monitor method performance during study | Use identical samples with known concentrations for both methods [1] |
Managing method changes in registration and post-approval stages requires a systematic, risk-based approach centered on demonstrating comparability through well-designed studies. The "comparative method" serves as the scientific benchmark for these assessments, with statistical equivalence testing forming the core of the evaluation process.
Successful implementation hinges on robust experimental design, appropriate statistical analysis, and comprehensive documentation. By adopting the frameworks and best practices outlined in this guide, pharmaceutical professionals can ensure regulatory compliance while facilitating continuous improvement in analytical methodologies throughout the product lifecycle.
Phase-Appropriate Validation Strategies from Development to Commercial
Analytical method validation serves as a critical cornerstone in the drug development process, ensuring that pharmaceutical products meet stringent standards for identity, strength, quality, purity, and potency throughout their lifecycle from early development to commercial marketing [72]. The validation process provides documented evidence that analytical methods are fit for their intended purpose, delivering reliable, reproducible, and accurate results that form the basis for critical decisions regarding patient safety and drug efficacy [73] [17]. Within the broader context of analytical method validation research, comparative method studies represent a fundamental scientific approach for establishing method equivalence when introducing new technologies or transferring methodologies between laboratories [19] [1]. These comparative assessments are particularly vital during method transfers between development and quality control laboratories, where demonstrating equivalent performance is essential for maintaining data integrity across different operational environments [73].
The concept of phase-appropriate validation has emerged as a strategic framework that aligns validation activities with the specific stage of drug development, recognizing that regulatory expectations and analytical requirements naturally evolve as a compound progresses through clinical trials [72] [73] [74]. This approach acknowledges that only a small percentage of drug candidates successfully navigate the entire development pathway, with approximately 90% of compounds failing during Phase 1 trials [75]. By implementing risk-based, phase-appropriate validation strategies, pharmaceutical companies can optimize resource allocation, reduce development costs, and maintain appropriate focus on patient safety without prematurely committing to comprehensive validation activities typically reserved for late-stage development and commercial phases [75] [76] [77].
Regulatory Foundation and Key Concepts
Regulatory Framework for Analytical Validation
The regulatory landscape governing analytical method validation is established through international guidelines and standards that provide the foundation for ensuring data reliability and patient safety. The International Council for Harmonisation (ICH) guidelines, particularly ICH Q2(R1), serve as the primary international standard for analytical procedure validation, outlining key validation parameters and methodological requirements [76] [20]. These guidelines are supplemented by regional regulatory documents, including the FDA Guidance for Industry on Analytical Procedures and Method Validation, which explicitly recognizes that the extent of validation should align with the development phase of the investigational drug [76] [77]. Similarly, the European Medicines Agency (EMA), World Health Organization (WHO), and Association of Southeast Asian Nations (ASEAN) have established complementary guidelines that collectively emphasize scientific soundness and fitness for purpose while acknowledging regional nuances in implementation expectations [20].
Regulatory authorities explicitly endorse a phase-appropriate approach to method validation, particularly during early development stages. FDA's guidance for Phase 1 investigational drugs specifically states that analytical methods "should be scientifically sound (e.g., specific, sensitive, and accurate), suitable, and reliable for the specified purpose" rather than requiring full validation [77]. This regulatory position acknowledges the evolving nature of pharmaceutical processes during early development and prevents unnecessary resource expenditure on drug candidates that may not progress to later stages [76]. The ICH Q7 guideline further reinforces this concept by advocating for "scientifically sound" rather than fully validated laboratory controls for Active Pharmaceutical Ingredients (APIs) destined for clinical trials [76].
Foundational Terminology and Definitions
Understanding the specialized terminology within method validation is essential for proper implementation of phase-appropriate strategies. The following key terms form the vocabulary of analytical validation:
Method Validation: A protocol-guided activity that ensures a test procedure is accurate, reproducible, and sensitive within a specified range, demonstrating through assessment of performance characteristics that the method is suitable for its intended purpose [73].
Method Qualification: Shows that a method is suitable for use based on the evaluation of specific performance characteristics, typically applied during early-phase drug development (pre-clinical through Phase 1) to demonstrate the method is scientifically sound [73] [76].
Method Verification: A demonstration that proves a compendial method is suitable for use in a particular environment or quality system, including specific equipment, personnel, and facility considerations [73].
Method Transfer: A formal process in which an analytical method is moved from a sending laboratory to a receiving laboratory, including comparative assessments and criteria demonstrating equivalent performance between laboratories [73].
Comparative Method: An established method used as a basis for comparison when evaluating a new or modified analytical method, often employed during method transfer or when demonstrating equivalence between methodologies [19] [1].
Within the context of comparative method studies, additional specialized terminology includes bias (the mean difference in values obtained with two different methods of measurement), precision (the degree to which the same method produces the same results on repeated measurements), and limits of agreement (the range within which 95% of the differences between methods are expected to fall) [19].
Phase-Appropriate Validation Requirements
Validation Progression Through Clinical Development
The phase-appropriate validation framework strategically aligns the rigor and completeness of analytical validation activities with the stage of clinical development, regulatory requirements, and patient safety considerations. This approach recognizes that analytical methods evolve alongside the drug development process, with increasing sophistication and validation requirements as the product moves closer to commercial marketing [72] [73] [74]. The following table summarizes the progressive nature of validation activities throughout the drug development lifecycle:
Table 1: Phase-Appropriate Analytical Validation Requirements Across Clinical Development
| Development Phase | Primary Validation Goals | Key Methodological Requirements | Typical Validation Parameters Assessed |
|---|---|---|---|
| Preclinical | Assign purity to drug substances for toxicology studies; qualify impurities present in API used in animal studies [72] | Purity, TGA, Micro ROI, Alternative Techniques [72] | Limited validation; focus on scientific soundness for intended purpose [72] |
| Phase 1 | Assign purity to drug substances for First In Human (FIH) studies; evaluate impurity levels; ensure patient safety [72] | Qualified (Scientifically Sound) Test Methods; Appearance; Identification; Purity; Residual Solvents; Water Content [72] | Specificity, Accuracy, Precision, Linearity, Detection Limit, Quantitation Limit, Solution Stability [74] [77] |
| Phase 2A/2B | Assign purity for larger patient populations; evaluate impurity levels with modified processes; perform genotoxic assessment [72] | Validated Test Methods; Appearance; Identification; Purity/Assay; Related Substances; Residual Solvents [72] | Specificity, Repeatability, Linearity, Accuracy, LOD/LOQ (if applicable), Solution Stability, Intermediate Precision [74] |
| Phase 3/Registration | Well-characterized API for pivotal clinical studies; control impurities to meet commercial targets; lock commercial processes [72] | Fully Validated Methods; Comprehensive testing including all critical quality attributes [72] | All ICH Q2(R1) parameters: Specificity, Accuracy, Precision, Linearity, Range, LOD, LOQ, Robustness, Solution Stability [74] |
| Commercial | Ensure API meets all regulatory standards; well-defined control strategy; validated manufacturing process [72] | Fully Validated and Maintained Methods; Ongoing verification and monitoring [72] | Complete validation per ICH Q2(R1); continuous monitoring and trending of method performance [72] [73] |
Detailed Validation Parameters by Phase
The specific validation parameters required at each development phase reflect the evolving regulatory expectations and risk-based approach to patient safety. During Phase 1, the primary focus remains on ensuring that methods are scientifically sound and capable of accurately characterizing the critical quality attributes that impact patient safety, such as potency, impurities, and identity [72] [77]. The validation approach at this stage typically includes assessment of specificity, accuracy, precision, linearity, detection limit, quantitation limit, and solution stability, but excludes more comprehensive parameters such as intermediate precision and robustness that become necessary in later phases [74] [77].
As drug development progresses to Phase 2, the validation requirements expand to include intermediate precision, reflecting the need to demonstrate method reliability across different analysts, instruments, or days while the manufacturing process undergoes optimization and refinement [74]. By Phase 3, methods must undergo full validation encompassing all parameters identified in ICH Q2(R1), including robustness, which demonstrates that the method remains unaffected by small, deliberate variations in method parameters and provides an indication of its reliability during normal usage [74] [76]. This progressive approach to validation ensures that resources are allocated efficiently while maintaining appropriate focus on patient safety and data integrity throughout the development lifecycle [73] [75].
Comparative Method Validation: Principles and Protocols
Foundational Principles of Method Comparison
Comparative method validation represents a critical component within the broader validation landscape, serving to establish equivalence between analytical methods during technology changes, method transfers, or platform migrations [19] [1]. The fundamental principle underlying comparative method studies is the demonstration that two methods for measuring the same analyte produce equivalent results within defined acceptance criteria, addressing the clinical question of substitution: "Can one measure X with either Method A or Method B and get the same results?" [19]. These studies are particularly vital in pharmaceutical development when methods are transferred from analytical development laboratories to quality control units, or when implementing new technologies to replace established methodologies [73] [1].
The design of comparative method studies requires careful consideration of multiple factors to ensure scientifically sound conclusions. The selection of measurement methods must ensure that both techniques measure the same fundamental property or analyte, while timing of measurement must account for the stability of the analyte and potential physiological variations [19]. The number of measurements and subject/sample selection should provide sufficient statistical power to detect clinically relevant differences, with a minimum of 40 different patient specimens recommended to cover the entire working range of the method and represent the spectrum of expected sample matrices [19] [1]. Additionally, the conditions of measurement should reflect the intended use conditions across the physiological or analytical range for which the methods will be employed [19].
Experimental Design for Method Comparison Studies
The protocol for conducting comparative method validation requires meticulous planning and execution to generate meaningful data. The following experimental workflow outlines the key stages in designing and executing a robust method comparison study:
The experimental design begins with clearly defining study objectives and acceptance criteria based on the intended use of the method and clinically relevant differences [19] [1]. The selection of an appropriate comparative method is crucial, with reference methods preferred when available due to their established accuracy and traceability [1]. The sample plan should include a minimum of 40 specimens carefully selected to cover the entire analytical range rather than relying on random selection, as data distribution quality significantly impacts the reliability of statistical conclusions [19] [1].
The measurement protocol should implement simultaneous or nearly simultaneous sampling to minimize variations due to analyte instability, with duplicate measurements recommended to identify potential outliers or measurement errors [19]. The experimental execution should extend across multiple days (minimum of 5 recommended) to incorporate routine analytical variation and provide more realistic performance assessment [1]. Throughout the study, specimen stability must be maintained through appropriate handling conditions, with analysis typically conducted within two hours between methods unless stability data supports longer intervals [1].
Statistical Analysis and Data Interpretation
The analysis of comparative method data employs both graphical and statistical approaches to evaluate agreement between methods. The Bland-Altman plot serves as a primary graphical tool, displaying the difference between methods against the average of the two measurements, with horizontal lines indicating the mean difference (bias) and limits of agreement (mean difference ± 1.96 standard deviations) [19]. This visualization facilitates identification of potential proportional or constant bias and outliers that may require further investigation.
Statistical analysis typically includes linear regression for methods with wide analytical ranges, providing estimates of slope (proportional error), y-intercept (constant error), and standard deviation of points about the regression line (s_y/x) [19] [1]. For methods with narrow analytical ranges, paired t-test calculations are more appropriate, providing the mean difference (bias), standard deviation of differences, and confidence intervals for the bias [19] [1]. The correlation coefficient (r) is mainly useful for assessing whether the data range is sufficient to provide reliable estimates of slope and intercept, with values ≥0.99 indicating adequate range for linear regression analysis [1].
Table 2: Key Statistical Parameters in Comparative Method Studies
| Statistical Parameter | Calculation Method | Interpretation | Acceptance Criteria Considerations |
|---|---|---|---|
| Bias (Mean Difference) | Mean of (Test Method - Comparative Method) | Systematic difference between methods; positive values indicate test method reads higher | Should be less than clinically acceptable difference; may vary by analyte and concentration |
| Limits of Agreement | Bias ± 1.96 × SD of differences | Range containing 95% of differences between methods | Should fall within predefined clinical acceptability limits |
| Slope | Linear regression coefficient | Proportional difference between methods; values ≠1 indicate proportional error | Typically 1.00 ± 0.05 depending on analyte and concentration range |
| Intercept | Y-intercept from linear regression | Constant difference between methods; values ≠0 indicate constant error | Should approach zero; significance depends on concentration range |
| Standard Error of Estimate (s_y/x) | SD of points about regression line | Measure of random scatter around regression line | Lower values indicate better agreement; should be less than acceptable imprecision |
The interpretation of comparative study results must consider both statistical significance and clinical relevance, with focus on the estimated systematic error at medically important decision concentrations [19] [1]. The successful demonstration of method equivalence requires that both statistical criteria and predefined acceptance criteria are met, ensuring that the methods can be used interchangeably for their intended purpose without impacting patient safety or product quality [19].
Implementation Strategies and Industry Best Practices
Practical Implementation of Phase-Appropriate Validation
Successful implementation of phase-appropriate validation strategies requires a systematic approach that balances regulatory expectations, resource allocation, and risk management. Pharmaceutical companies should develop a comprehensive Validation Master Plan early in the development process that outlines the progressive validation activities aligned with clinical milestones [75]. This plan should incorporate method scalability considerations, recognizing that early-phase methods may utilize generic high-performance liquid chromatography (HPLC) approaches that suffice until more is known about the compound and its impurity profile [77]. As the drug product progresses through development and manufacturing processes become locked, methods should be refined and fully validated to support commercial specifications [72] [77].
A critical aspect of practical implementation involves method transfer from analytical development to quality control laboratories, which typically employs one of three approaches: comparative testing, co-validation between laboratories, or complete revalidation in the receiving laboratory [73]. The transfer process should be documented through a formal protocol that includes predefined acceptance criteria and side-by-side comparison studies, particularly when methods are being transferred between organizations or across different geographical locations [73] [1]. Successful method transfers demonstrate that the receiving laboratory can execute the method equivalently to the sending laboratory, ensuring continuity of data quality and integrity [73].
The Scientist's Toolkit: Essential Reagents and Materials
The execution of robust analytical method validation requires specific reagents, reference standards, and instrumentation to ensure accurate and reproducible results. The following table outlines key research reagent solutions and materials essential for conducting validation studies:
Table 3: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Specification Requirements | Primary Function in Validation | Quality Considerations |
|---|---|---|---|
| Reference Standards | Certified purity ≥98%; documentation of origin and characterization [17] | Quantification of analyte; method calibration; accuracy determinations | Should be traceable to certified reference materials; stored according to manufacturer recommendations |
| Chromatographic Solvents | HPLC or LC-MS grade; low UV absorbance; specified purity [17] | Mobile phase preparation; sample extraction and dilution | Lot-to-lot consistency; expiration date monitoring; appropriate filtration |
| Buffer Components | Analytical grade; specified pH and molarity [17] | Mobile phase modification; sample preservation | Stability monitoring; pH verification; microbial growth prevention |
| System Suitability Standards | Well-characterized mixture of key analytes and impurities [76] | Verification of chromatographic system performance before validation runs | Should challenge critical method parameters (resolution, efficiency, sensitivity) |
| Placebo/Matrix Blanks | Representative of formulation without active ingredient [76] | Specificity assessment; interference checking | Should match final composition; include all inert components |
Risk-Based Approaches and Resource Optimization
The phase-appropriate validation paradigm inherently incorporates risk-based principles that focus resources on critical quality attributes most relevant to patient safety at each development stage [75] [76]. During early-phase development, the primary risk consideration is ensuring that clinical trial materials have consistent safety profiles, particularly regarding impurity levels and potency [72] [76]. This focus allows for more flexible validation approaches that may not include full robustness testing or intermediate precision, provided the methods are scientifically sound and capable of detecting clinically relevant changes in critical quality attributes [76] [77].
Resource optimization strategies include deferring stability-indicating method development until later phases when manufacturing processes are more defined, thereby avoiding redevelopment activities when processes change [77]. Similarly, the use of method bridging studies can efficiently address method modifications without complete revalidation, particularly when new impurities emerge due to process changes [73]. Industry surveys conducted through the IQ Consortium indicate that these phased approaches can reduce method development costs by 30-50% during early development phases while maintaining appropriate quality standards and ensuring patient safety [76].
Phase-appropriate validation strategies represent a sophisticated, risk-based framework that aligns analytical validation activities with the stage of drug development, regulatory expectations, and patient safety requirements. This approach acknowledges the evolving nature of pharmaceutical processes and the high attrition rate of drug candidates, thereby optimizing resource allocation while maintaining scientific rigor [72] [73] [75]. The successful implementation of these strategies requires understanding of both regulatory guidelines and practical analytical considerations, with validation activities progressing from scientifically sound methods in early development to fully validated methods supporting commercial marketing applications [74] [76] [77].
Within this framework, comparative method validation serves as a critical tool for establishing method equivalence during technology transfers, method modifications, or platform changes [19] [1]. The design and execution of robust comparison studies require careful attention to experimental parameters, statistical analysis methods, and clinically relevant acceptance criteria to ensure that methods perform equivalently for their intended purpose [19]. As the pharmaceutical landscape continues to evolve with increasing numbers of virtual companies and milestone-driven funding models, the strategic implementation of phase-appropriate validation approaches becomes increasingly vital for efficiently advancing drug candidates through the development pipeline while maintaining the highest standards of product quality and patient safety [75] [77].
Conclusion
The comparative method experiment is a cornerstone of analytical method validation, providing an essential estimate of systematic error that is critical for ensuring the accuracy and reliability of data used in drug development and quality control. A successfully executed study hinges on a robust foundational understanding, a meticulously planned experimental methodology, proactive troubleshooting, and integration into the wider regulatory and validation strategy. Key takeaways include the necessity of selecting a well-characterized comparative method, designing an experiment with adequately selected patient specimens, using graphical and statistical tools for insightful data analysis, and adopting a risk-based approach for method changes. For future directions, the increasing adoption of collaborative validation models and green chemistry principles, as evidenced in modern studies, promises to enhance efficiency and sustainability. Ultimately, a rigorous comparative method study strengthens the scientific basis for analytical results, ensuring patient safety and supporting regulatory submissions throughout the product lifecycle.
References
- 1. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 2. Random vs. Systematic Error | Definition & Examples [https://www.scribbr.com/methodology/random-vs-systematic-error/]
- 3. A practical guide to analytical method validation, including ... [https://www.sciencedirect.com/science/article/pii/S0165993607000118]
- 4. Determining Inaccuracy - Basic Method Validation [https://www.westgard.com/lessons/basic-method-validation/methodbias.html]
- 5. Random vs. Systematic Error [https://www.physics.umd.edu/courses/Phys276/Hill/Information/Notes/ErrorAnalysis.html]
- 6. Practices of Science: Scientific Error [https://manoa.hawaii.edu/exploringourfluidearth/physical/world-ocean/map-distortion/practices-science-scientific-error]
- 7. Analytical Method Comparability in Registration and Post ... [https://www.pharmtech.com/view/analytical-method-comparability-registration-and-post-approval-stages-risk-based-approach]
- 8. Uncertainty Analysis is an Important Part of Test Method ... [https://medinstitute.com/blog/uncertainty-analysis-is-an-important-part-of-test-method-validation/]
- 9. A Central Requirement for New Test Methods [https://dcndx.com/insights/method-comparison-experiment-central-requirement-new-test-methods/]
- 10. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 11. Method comparison: Comparison of multiple methods [https://www.medcalc.org/en/manual/comparison-of-multiple-methods.php]
- 12. Method comparison / Agreement [https://analyse-it.com/docs/user-guide/method-comparison/method-comparison]
- 13. Observational error [https://en.wikipedia.org/wiki/Observational_error]
- 14. Random Error vs Systematic Error [https://statisticsbyjim.com/basics/random-error-vs-systematic-error/]
- 15. Errors in Measurement [https://www.geeksforgeeks.org/physics/errors-in-measurement/]
- 16. A total error approach for the validation of quantitative ... [https://pubmed.ncbi.nlm.nih.gov/17373576/]
- 17. Comparative analysis and validation of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452224000530]
- 18. A New Era for Analytical Procedure Lifecycle Management [https://synergbiopharma.com/navigating-analytical-method-comparability-and-equivalency-under-ich-q14-a-new-era-for-analytical-procedure-lifecycle-management/]
- 19. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 20. Comparative Study of Analytical Method Validation and ... [https://www.ijdra.com/index.php/journal/article/view/675]
- 21. Focus on Data: Statistical Design of Experiments and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7425741/]
- 22. Design of experiments [https://en.wikipedia.org/wiki/Design_of_experiments]
- 23. Guide to Experimental Design | Overview, Steps, & Examples [https://www.scribbr.com/methodology/experimental-design/]
- 24. Stability: Recommendation for Best Practices and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012051/]
- 25. Solution Stability In Analytical Method Validation: How To ... [https://pharmaguru.co/solution-stability-in-analytical-method-validation/]
- 26. Replicates and repeats in designed experiments - Minitab [https://support.minitab.com/en-us/minitab/help-and-how-to/statistical-modeling/doe/supporting-topics/basics/replicates-and-repeats-in-designed-experiments/]
- 27. Replicates and repeats—what is the difference and is it ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3321166/]
- 28. The Role of Clinical Trial Data Visualisation in Modern ... [https://www.quanticate.com/blog/clinical-trial-data-visualisation]
- 29. 15 Visualization [https://experimentology.io/015-viz.html]
- 30. 17 Important Data Visualization Techniques - HBS Online [https://online.hbs.edu/blog/post/data-visualization-techniques]
- 31. Graphical Summaries | Introduction to Data Science [https://dept.stat.lsa.umich.edu/~kshedden/introds/topics/graphical_summaries/]
- 32. On the misinterpretation of the correlation coefficient in ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517306004492]
- 33. ANOVA and Standard Error of Estimate in Simple Linear ... [https://analystprep.com/study-notes/cfa-level-2/quantitative-method/anova-and-standard-error-of-estimate-in-simple-linear-regression/]
- 34. Proof for the standard error of parameters in linear regression [https://stats.stackexchange.com/questions/289457/proof-for-the-standard-error-of-parameters-in-linear-regression]
- 35. Regression Standard Errors, Translated Into English [https://nickchk.substack.com/p/regression-standard-errors-translated]
- 36. A guide to appropriate use of Correlation coefficient in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3576830/]
- 37. Interpretation of correlations in clinical research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6130913/]
- 38. Corruption of the Pearson correlation coefficient by ... [https://www.nature.com/articles/s41598-019-57247-4]
- 39. Regression Analysis: How to Interpret S, the Standard Error ... [https://blog.minitab.com/en/blog/adventures-in-statistics-2/regression-analysis-how-to-interpret-s-the-standard-error-of-the-regression]
- 40. 12.6 Standard Error of the Estimate – Introduction to Statistics [https://ecampusontario.pressbooks.pub/introstats2ed/chapter/12-6-standard-error-of-the-estimate/]
- 41. Detecting and Treating Outliers | Treating the odd one out! [https://www.analyticsvidhya.com/blog/2021/05/detecting-and-treating-outliers-treating-the-odd-one-out/]
- 42. Verification of quantitative analytical methods in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8199534/]
- 43. Why Detecting Outliers is Crucial for Accurate Data Analysis? [https://www.dasca.org/world-of-data-science/article/why-detecting-outliers-is-crucial-for-accurate-data-analysis]
- 44. The Importance of the Sample Matrix [https://www.chromatographyonline.com/view/importance-sample-matrix-0]
- 45. A Guide to Analytical Method Validation [https://scioninstruments.com/us/blog/a-guide-to-analytical-method-validation-2/]
- 46. Recent Advances in Analytical Method Validation as per ICH Q2(R2): A Comparative Review with ICH Q2(R1) [https://www.ijpsjournal.com/article/Recent+Advances+in+Analytical+Method+Validation+as+per+ICH+Q2R2+A+Comparative+Review+with+ICH+Q2R1]
- 47. Optimization through classical design of experiments (DOE) [https://www.sciencedirect.com/science/article/pii/S2352710225001676]
- 48. Chapter 10 Methods for Comparative Studies - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK481584/]
- 49. Collaborative versus traditional method validation approach [https://www.sciencedirect.com/science/article/pii/S2589871X20300528]
- 50. Leveraging Vendor Testing: A Smarter Approach to ... [https://www.valgenesis.com/blog/leveraging-vendor-testing-a-smarter-approach-to-validation]
- 51. Analytical Method Validation Protocol And Report [https://pharmaguru.co/analytical-method-validation-protocol-and-report/]
- 52. A statistical approach to quantitative data validation focused ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3795879/]
- 53. Development and validation of a tool to measure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9107731/]
- 54. Enhanced efficiency assessment in manufacturing [https://www.sciencedirect.com/science/article/pii/S030504832500026X]
- 55. Navigating ICH Q2(R2) compliance in analytical method ... [https://pubmed.ncbi.nlm.nih.gov/40154788/]
- 56. Navigating ICH Q2(R2) compliance in analytical method ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925002072]
- 57. ICH publishes Training Materials on Q2(R2) and Q14 [https://www.gmp-compliance.org/gmp-news/ich-publishes-training-materials-on-q2r2-and-q14]
- 58. 3 Key Regulatory Guidelines for Method Validation [https://altabrisagroup.com/regulatory-guidelines-for-method-validation/]
- 59. Analytical Methods: A Statistical Perspective on the ICH ... [https://www.biopharminternational.com/view/analytical-methods-statistical-perspective-ich-q2a-and-q2b-guidelines-validation-analytical-methods]
- 60. What Is Method Validation Risk Assessment and Its ... [https://altabrisagroup.com/method-validation-risk-assessment/]
- 61. Review Risk-based approach for method development in ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708518312147]
- 62. Analytical Method Development with a Practical Risk ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/619865-Analytical-Method-Development-with-a-Practical-Risk-Assessment-Program-that-Enhances-Commercial-QC-Robustness/]
- 63. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 64. Risk-Based Strategy for Analytical Method Validation with QbD [https://institute.acs.org/risk-based-strategy-for-the-development-and-validation-of-analytical-methods-with-a-qbd-approach-2024.html]
- 65. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 66. Risk-Based Test Method Development, Validation and Life ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/517625-Risk-Based-Test-Method-Development-Validation-and-Life-Cycle/]
- 67. How to Demonstrate Comparability of Analytical Procedures [https://www.gmp-compliance.org/gmp-news/how-to-demonstrate-comparability-of-analytical-procedures]
- 68. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 69. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 70. Analytical Method Transfer Between Laboratories [https://www.labmanager.com/method-transfer-between-laboratories-challenges-and-solutions-34250]
- 71. Analytical Method Transfer in Pharmaceuticals | AMT ... [https://www.pharmaguideline.com/2025/09/analytical-method-transfer-in-pharmaceuticals.html]
- 72. Analytical Strategies from Early Development to Validation: Part One [https://registech.com/blog/analytical-strategies-from-early-development-to-validation-part-one/]
- 73. Analytical Strategies from Early Development to Validation: Part Two [https://www.registech.com/analytical-development/analytical-strategies-from-early-development-to-validation-part-two/]
- 74. Phase Appropriate Analytical Method Development and Validation – Mikart [https://www.mikart.com/phase-appropriate-analytical-method-development-and-validation/]
- 75. Phase-Appropriate Drug Development – Validation Process - pharm-int [https://www.pharm-int.com/resources/phase-appropriate-drug-development-validation-process/]
- 76. GMPs for Method Validation in Early Development: An Industry Perspective (Part II) | Pharmaceutical Technology [https://www.pharmtech.com/view/gmps-method-validation-early-development-industry-perspective-part-ii]
- 77. Designing Phase-Appropriate CMC Analytical Programs | Pharmaceutical Technology [https://www.pharmtech.com/view/designing-phase-appropriate-cmc-analytical-programs]