How to Select a Comparative Method for Method Validation: A Strategic Guide for Scientists
This article provides a comprehensive, step-by-step framework for researchers and drug development professionals to strategically select a comparative method for analytical method validation.
How to Select a Comparative Method for Method Validation: A Strategic Guide for Scientists
Abstract
This article provides a comprehensive, step-by-step framework for researchers and drug development professionals to strategically select a comparative method for analytical method validation. Covering foundational principles, regulatory requirements, and practical experimental design, it addresses common challenges and advanced optimization strategies. The guide synthesizes current regulatory expectations from FDA, EMA, and ICH guidelines with proven scientific approaches to ensure robust, defensible, and audit-ready validation outcomes that safeguard data integrity and product quality.
Understanding the Critical Role of a Comparative Method
Within the rigorous framework of analytical method validation, the process of method comparison serves a critical function: it estimates the inaccuracy or systematic error of a new (test) method by comparing its results to those from an established procedure [1]. The fundamental purpose of this experiment is to determine the agreement between methods measuring the same analyte, ensuring that patient results remain reliable and comparable when a new technique is introduced [2]. The selection of an appropriate method for this comparison—whether a reference method or a comparative method—is a pivotal decision that directly influences the interpretation of the data and the conclusions drawn about the test method's performance. This guide provides a detailed examination of these two cornerstone concepts, arming researchers and scientists with the knowledge needed to make informed choices in their method validation research.
Core Definitions and Hierarchical Relationship
The terms "reference method" and "comparative method" are not interchangeable; they occupy different tiers of a quality hierarchy based on their documented accuracy.
- Reference Method: A reference method carries a specific meaning, inferring a high-quality method whose results are known to be correct. This correctness is established through comparative studies with an accurate "definitive method" and/or through the traceability of standard reference materials [1]. In practice, when a test method is compared to a reference method, any observed differences are assigned to the test method. The documented correctness of the reference method provides a strong foundation for attributing error [1].
- Comparative Method: This is a more general term used for a method whose correctness has not been rigorously documented to the same standard. Most routine laboratory methods fall into this category. When large and medically unacceptable differences are found between a test method and a routine comparative method, it becomes necessary to conduct additional experiments, such as recovery and interference studies, to identify which method is inaccurate [1].
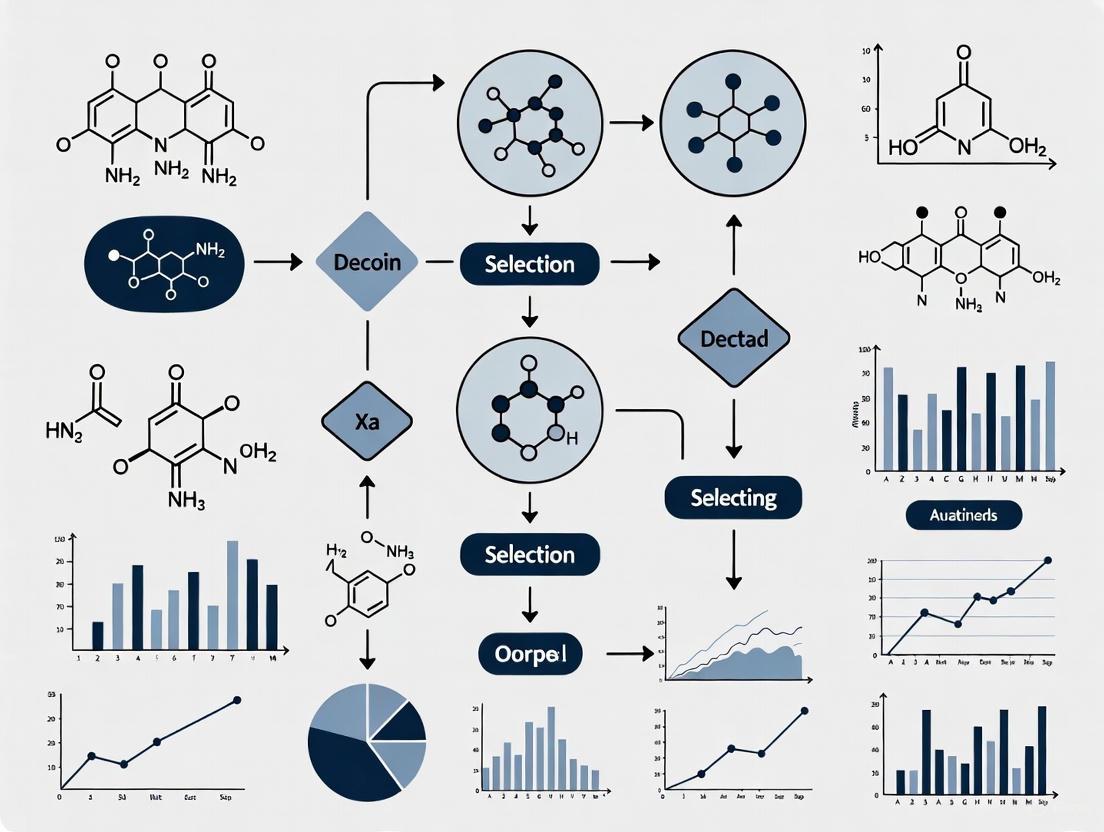
The relationship between these concepts, along with the associated level of confidence for error attribution, is illustrated in the following diagram.
Key Characteristics in a Comparative Table
The distinctions between a reference method and a comparative method extend beyond their basic definitions to encompass their foundational basis, the interpretation of results, and their typical applications. The table below provides a structured comparison of these key characteristics.
Table 1: Comparative Analysis of Reference and Comparative Methods
| Characteristic | Reference Method | Comparative Method |
|---|---|---|
| Basis of Definition | Well-documented correctness via definitive methods or traceable materials [1]. | General term for a method used in comparison; correctness not assumed [1]. |
| Primary Function | To provide an unquestioned benchmark for assessing a test method's inaccuracy [1]. | To assess the relative agreement between the new test method and a current, established method [3]. |
| Interpretation of Differences | Differences are conclusively attributed to the test method [1]. | Differences must be carefully interpreted; source of error (test or comparative method) is not known a priori [1]. |
| Typical Applications | Found in standardized, compendial settings (e.g., USP); used for definitive method validation [4]. | Used in routine laboratory practice for internal verifications, lot-to-lot reagent comparisons, and analyzer comparisons [2] [5]. |
| Regulatory & Quality Status | Often linked to a "gold standard" or a method that has undergone rigorous FDA review or collaborative trials [3]. | Represents the laboratory's current standard of practice, which may itself have been previously validated against a higher standard [1]. |
A Framework for Selecting a Comparison Method
Choosing between a reference method and a comparative method is not merely a technicality; it is a strategic decision that dictates the experimental design, data analysis, and ultimate conclusions of your validation study. The following workflow outlines the critical decision points and their consequences.
Guidance for Navigating the Selection Framework
Opt for a Reference Method When Possible: If a validated reference method is accessible and feasible for your laboratory to implement, it is the optimal choice. Its use provides the highest level of confidence in your systematic error estimates because the benchmark itself is unimpeachable. This path is strongly recommended for the initial validation of a novel method or when applying for regulatory approvals, as it offers the most defensible data [1] [3].
Using a Comparative Method Requires Rigor: When using a routine method for comparison, the focus shifts to demonstrating relative accuracy. A successful comparison shows that the new method agrees with the old one well enough for clinical purposes. However, the framework highlights a critical juncture: if differences are large, you must investigate further. You can no longer assume the new method is at fault; the discrepancy could originate from the comparative method itself [1]. Techniques like spiking studies (recovery) and interference testing are essential here to isolate the source of the error.
Essential Experimental Protocols for Method Comparison
A well-defined experimental protocol is vital to ensure that the observed differences truly reflect analytical performance and are not artifacts of poor design. The following protocols and considerations are central to a robust comparison, whether you are using a reference or a comparative method.
Quantitative Method Comparison Protocol
For quantitative assays, such as those measuring an active pharmaceutical ingredient or a clinical metabolite, the comparison relies on analyzing a set of patient samples by both the test and comparative methods.
Table 2: Key Experimental Parameters for a Quantitative Comparison
| Parameter | Recommendation & Purpose | Key Considerations |
|---|---|---|
| Sample Number | Minimum of 40 patient specimens [1] [2]. To ensure a reliable estimate of systematic error. | Sample quality (covering the entire working range) is more important than a very large number. 20 carefully selected specimens can be better than 100 random ones [1]. |
| Sample Type & Range | Patient samples should cover the entire working range and represent the expected spectrum of diseases [1]. | At least 50% of samples should be outside the reference interval to validate performance at clinically decision-making concentrations [2]. |
| Time Period | A minimum of 5 different days is recommended [1]. | This minimizes bias from a single analytical run and incorporates normal day-to-day variation into the study [1]. |
| Measurements | Analyze each specimen in singlicate by both methods as common practice; duplicate measurements are advantageous [1]. | Duplicates act as a check for sample mix-ups, transposition errors, and other mistakes. Without duplicates, discrepant results should be reanalyzed immediately [1]. |
| Data Analysis | Graph the data (difference or comparison plots) and calculate appropriate statistics [1]. | Visual inspection identifies outliers. For wide analytical ranges, use linear regression to estimate systematic error (SE) at medical decision concentrations: ( Yc = a + bXc ), ( SE = Yc - Xc ) [1]. |
Qualitative Method Comparison Protocol
For qualitative tests (positive/negative results), the comparison is analyzed using a 2x2 contingency table to assess agreement relative to the comparative method [3].
Table 3: 2x2 Contingency Table for Qualitative Method Comparison
| Comparative Method: Positive | Comparative Method: Negative | Total | |
|---|---|---|---|
| Candidate Method: Positive | a (True Positive, TP) | b (False Positive, FP) | a + b |
| Candidate Method: Negative | c (False Negative, FN) | d (True Negative, TN) | c + d |
| Total | a + c | b + d | n (Total N) |
From this table, two primary metrics of agreement are calculated [3]:
- Positive Percent Agreement (PPA): = 100% × [a / (a + c)] - Indicates how well the candidate method detects positive samples relative to the comparator.
- Negative Percent Agreement (NPA): = 100% × [d / (b + d)] - Indicates how well the candidate method detects negative samples relative to the comparator.
It is critical to understand that PPA and NPA are estimates of sensitivity and specificity, respectively. These can only be reported as true sensitivity/specificity if the comparative method is a highly accurate "gold standard" or reference method. Otherwise, they remain measures of agreement [3].
The Scientist's Toolkit: Key Reagents and Materials
The reliability of a method comparison is contingent on the quality and stability of the materials used. Below is a list of essential items and their functions in a typical comparison study.
Table 4: Essential Research Reagent Solutions and Materials
| Item | Function & Importance in Comparison Studies |
|---|---|
| Certified Reference Material (CRM) | A substance with one or more property values that are certified by a validated procedure, providing a metrological traceability link to a primary standard. Serves as the foundation for a reference method comparison [1]. |
| Patient Specimens | Naturally occurring matrices that account for real-world interferences and the spectrum of sample types. They are the preferred sample type for assessing systematic error with real clinical material [1] [2]. |
| Quality Control (QC) Materials | Stable materials with known expected values used to ensure that both the test and comparative methods are operating within acceptable performance limits before and during the comparison study [2]. |
| Appropriate Anticoagulants & Preservatives | Used in sample collection tubes to maintain specimen stability (e.g., prevent coagulation, slow metabolite degradation). Ensures that differences are analytical, not pre-analytical [1] [2]. |
| Fresh Mobile Phases / Reagents | Critical for chromatographic and enzymatic methods. Aged mobile phases must perform equivalently to fresh ones (e.g., within ±2% for response, resolution) to avoid introducing bias [4]. |
| Guibourtinidol | Guibourtinidol |
| Ethyl thiazol-2-ylglycinate | Ethyl thiazol-2-ylglycinate, MF:C7H10N2O2S, MW:186.23 g/mol |
The distinction between a reference method and a comparative method is fundamental to designing, executing, and interpreting a method validation study. A reference method provides an authoritative benchmark, allowing for definitive attribution of systematic error to the test method. In contrast, a comparative method serves as a practical standard for assessing relative agreement, but requires careful interpretation and potentially further investigation when discrepancies arise. The choice between them should be guided by availability, regulatory requirements, and the intended use of the test. By adhering to robust experimental protocols—including appropriate sample selection, replication, and statistical analysis—researchers can generate defensible data that ensures the reliability and fitness-for-purpose of new analytical methods in both drug development and clinical practice.
In pharmaceutical research and development, the choice of a comparative method is a foundational scientific and strategic decision that directly influences data integrity, product quality, and ultimately, regulatory success. A comparative method in method validation serves as a benchmark against which the performance, accuracy, and reliability of a new analytical procedure are measured. Within the current regulatory landscape, where data integrity is a paramount focus for agencies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), the selection and execution of this method are more critical than ever [6]. Regulatory bodies have explicitly stated that data integrity issues are a primary reason for delays in application approvals, such as Abbreviated New Drug Applications (ANDAs) [7].
The principles of ALCOA+, which mandate that data be Attributable, Legible, Contemporaneous, Original, and Accurate, along with being Complete, Consistent, Enduring, and Available, form the bedrock of regulatory expectations [8] [9]. The choice of an inappropriate, unvalidated, or poorly documented comparative method can directly undermine these principles, leading to data that is not trustworthy. Recent enforcement trends, including an increase in warning letters and the rejection of studies from contract research organizations (CROs) due to data integrity concerns, highlight the tangible risks of inadequate practices [10] [9]. This guide provides a detailed framework for researchers and scientists to select, validate, and document comparative methods that ensure data integrity and facilitate regulatory acceptance.
The Regulatory Landscape and Data Integrity Fundamentals
Regulatory agencies worldwide are intensifying their scrutiny of data governance practices. The FDA's 2025 focus areas include systemic quality culture, robust audit trails, and oversight of contract manufacturing organizations (CMOs) [6]. Similarly, the EU's 2025 updates to EudraLex Volume 4, specifically the revised Annex 11 and Chapter 4, formally mandate ALCOA+ principles and emphasize data lifecycle management [6]. These updates represent a significant shift from viewing ALCOA+ as best practice to treating it as a mandatory requirement for compliance.
The consequences of data integrity failures are severe and multifaceted. A recent analysis of FDA Warning Letters revealed that violations related to data "Endurance" and "Availability" have been increasing post-pandemic [9]. Furthermore, the FDA has taken public action against CROs where data integrity concerns were identified, requiring sponsors to repeat essential studies and leading to changes in the therapeutic equivalence ratings of approved generic drugs [10]. This not only results in significant financial losses and delays but also damages an organization's credibility with regulators.
Table: Recent Regulatory Actions Stemming from Data Integrity Concerns
| Event | Regulatory Impact | Consequence for Sponsor |
|---|---|---|
| FDA Declaration on Raptim Research [10] | Certain bioequivalence studies deemed unacceptable due to data integrity concerns. | Must repeat essential in vitro studies; marketed products may receive a "BX" rating, indicating they are not recommended for automatic substitution. |
| Analysis of 1766 FDA Warning Letters (2016-2023) [9] | Increase in citations for "Endurance" (data remains available) and "Availability." | Regulatory actions (e.g., Warning Letters, Import Alerts), increased inspectional scrutiny, and application delays. |
| EU's 2025 Annex 11 Update [6] | Mandatory audit trails, identity & access management controls, and explicit management responsibility for data integrity. | Requires potentially expensive upgrades to older computerized systems and implementation of strengthened data governance frameworks. |
The selection of a comparative method is deeply intertwined with these data integrity requirements. The method must be fully validated itself, its operational lifecycle must be documented within a robust quality system, and the resulting data must be secured within a tamper-evident audit trail to meet contemporary regulatory standards [8] [6].
A Framework for Selecting a Comparative Method
Selecting a fit-for-purpose comparative method requires a structured, risk-based approach that aligns with the analytical procedure's intended use and regulatory context.
Core Principles for Selection
The following principles should guide the selection process:
- Scientific Justification: The chosen method must be scientifically sound and appropriate for the analyte and matrix. This requires a thorough understanding of the chemical, biological, and physical properties involved.
- Regulatory Precedence and Harmonization: Where possible, leverage methods described in recognized pharmacopoeias (USP, EP) or ICH guidelines. Be aware of potential variations in validation requirements across different regulatory bodies (ICH, EMA, WHO, ASEAN) as identified in comparative studies [11].
- ALCOA+ by Design: The method's workflow should be designed to inherently produce data that meets ALCOA+ principles. This includes using validated, access-controlled computerized systems that generate secure audit trails from the point of data creation [8] [6].
- Practical Feasibility: The method must be operable within the constraints of the laboratory's equipment, personnel expertise, and timeline, without compromising quality.
The Method Selection Workflow
The following diagram illustrates a systematic workflow for selecting a comparative method, integrating both scientific and data integrity considerations.
Key Selection Criteria
When evaluating candidate methods, a comparative assessment against defined criteria is essential. The table below outlines critical factors.
Table: Key Criteria for Comparative Method Selection
| Criterion | Description | Considerations for Data Integrity |
|---|---|---|
| Scientific Robustness | The inherent reliability, accuracy, and precision of the method. | A robust method minimizes variability and the potential for "data cherry-picking" or manipulation to achieve desired results. |
| Regulatory Standing | The method's acceptance and history of use in regulatory submissions. | Well-established methods reduce regulatory uncertainty. Any deviation must be thoroughly justified and validated. |
| System Suitability | The ability to demonstrate that the system is operating as intended at the time of analysis. | Clear, predefined system suitability criteria are essential for ensuring the Original and Accurate nature of the data generated in a specific run [11]. |
| Automation & Control | The degree of automation and built-in electronic controls. | Automated systems with locked methods and integrated audit trails significantly enhance data Attributability and reduce transcription errors [6] [12]. |
| Validation Complexity | The extent and complexity of validation required. | The validation process for the comparative method itself must be meticulously documented to demonstrate the method is fit-for-purpose. |
Experimental Protocols for Comparative Method Validation
Once a comparative method is selected, its rigorous validation is imperative. The following protocols provide a detailed methodology for key experiments.
Protocol for a Comparative Accuracy Study
Objective: To demonstrate that the new method provides results that are statistically equivalent or superior to those obtained by the validated comparative method.
Materials and Reagents:
- Certified Reference Standards (with known purity and concentration)
- Placebo/formulation matrix (excluding the active ingredient)
- Test samples (e.g., drug product batches)
- All solvents and reagents as per the analytical procedures for both methods
Procedure:
- Preparation of Solutions: Prepare a minimum of nine determinations over a specified range (e.g., 80%, 100%, 120% of target concentration) using the placebo matrix spiked with the reference standard. This should include three concentration levels, each analyzed in triplicate.
- Sample Analysis: Analyze these prepared solutions using both the new method and the comparative method in a randomized sequence to avoid bias.
- Data Collection: Record the raw data (e.g., peak areas, absorbance) directly into a compliant computerized system, ensuring all data is attributable and contemporaneous [8].
- Calculation and Comparison: For each level, calculate the recovery percentage and compare the results from both methods using appropriate statistical tests (e.g., student's t-test, equivalence testing).
Data Integrity Considerations:
- The sequence of analysis should be pre-defined in the protocol to ensure objectivity.
- All electronic data should be saved with associated audit trails; any manual data entries must be justified and witnessed per SOP [6].
Protocol for an Intermediate Precision Study
Objective: To evaluate the impact of random variations within the laboratory (different analysts, different days, different equipment) on the results of the comparative method itself.
Procedure:
- Experimental Design: Two analysts (Analyst A and B) will perform the analysis on two different days (Day 1 and Day 2) using the same calibrated instrument where possible, or two different instruments of the same model.
- Sample Preparation: A homogeneous sample batch (e.g., at 100% concentration) is prepared and subdivided.
- Analysis: Each analyst prepares and analyzes six sample replicates on their respective days, following the same standardized method.
- Data Analysis: Calculate the %Relative Standard Deviation (%RSD) for the results from all analysts and all days combined.
Data Integrity Considerations:
- The system suitability tests must be met before each analytical run begins.
- The audit trail for the computerized system must be reviewed to confirm there were no unauthorized changes to the method or processing parameters between runs [8] [6].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are critical for executing robust comparative method validation studies.
Table: Essential Reagents and Materials for Comparative Validation Studies
| Item | Function | Critical Quality Attribute |
|---|---|---|
| Certified Reference Standard | Serves as the primary benchmark for quantifying the analyte and establishing method accuracy. | Certified identity, purity, and stability; sourced from a qualified and reputable supplier (e.g., USP, EDQM). |
| Placebo/Blank Matrix | Allows for assessment of specificity and accuracy without interference from the active ingredient. | Must be truly representative of the final product formulation, excluding only the analyte of interest. |
| System Suitability Test (SST) Solutions | Verifies that the chromatographic or analytical system is performing adequately at the time of the test. | Well-characterized mixture that provides consistent, predefined performance parameters (e.g., resolution, tailing factor). |
| Stable Isotope-Labeled Internal Standard | Used in mass spectrometric methods to correct for analyte loss during preparation and instrument variability. | High isotopic purity and chemical stability; must behave identically to the analyte but be distinguishable by the mass spectrometer. |
| Cinnolin-6-ylmethanol | Cinnolin-6-ylmethanol | Cinnolin-6-ylmethanol is For Research Use Only. Explore its applications in medicinal chemistry for developing antimicrobial and anti-inflammatory agents. Not for human use. |
| 1,6-Dimethyl-9H-carbazole | 1,6-Dimethyl-9H-carbazole|CAS 78787-77-6 | High-purity 1,6-Dimethyl-9H-carbazole for research. Explore its applications in anticancer studies and material science. For Research Use Only. Not for human use. |
Visualizing the Data Lifecycle in a Regulated Environment
Ensuring data integrity requires control over the entire data lifecycle, from generation through to archival and destruction. The following diagram maps this lifecycle and its critical control points.
In the current regulatory climate, the choice of a comparative method is a critical decision with far-reaching implications for data integrity and regulatory acceptance. It is not merely a technical formality but a core component of a company's quality culture and data governance framework. By adopting a systematic, principle-based approach to selection, following rigorous and well-documented experimental protocols, and implementing robust controls throughout the data lifecycle, pharmaceutical researchers can generate data that is not only scientifically valid but also inherently trustworthy. This commitment to excellence in comparative method practices builds a solid foundation for regulatory confidence, smooths the path to approval, and, most importantly, ensures the quality, safety, and efficacy of medicines for patients.
In pharmaceutical development and healthcare research, demonstrating that an analytical method is reliable and fit for its intended purpose is a fundamental regulatory and scientific requirement. Method validation provides documented evidence that a process consistently produces a result meeting its predetermined specifications and quality attributes. Within a broader thesis on selecting a comparative method for validation research, this guide establishes that the core objectives are intrinsically linked: proving method reliability is a direct prerequisite for ensuring patient safety [13]. A method that is not reliable cannot accurately quantify product quality or detect potential patient risks, leading to inadequate safety diagnoses and the implementation of ineffective interventions [13]. This guide details the experimental protocols, data analysis frameworks, and essential tools required to achieve these twin objectives through a comparative method validation approach.
Foundational Principles and Experimental Design
Defining the Validation Framework
A robust method validation study begins with a clear experimental plan. The overarching goal is to demonstrate that the method's performance characteristics are acceptable for the intended application, thereby ensuring the safety and efficacy of the resulting data [14] [15]. The process involves a logical sequence of steps, from defining quality requirements to judging the acceptability of the method's performance [14]. The following workflow outlines the critical stages of method validation.
Implementing Design of Experiments (DOE)
A systematic approach using Design of Experiments (DOE) is a powerful tool for method characterization and validation [15]. DOE moves beyond traditional one-factor-at-a-time studies, enabling a more efficient and accurate quantification of how factors influence method performance. The key steps in applying DOE are:
- Define the Purpose: Clearly state the goal of the study, such as assessing repeatability, intermediate precision, accuracy, linearity, or resolution [15].
- Define the Range: Establish the range of concentrations and the solution matrix the method will be used to measure. This defines the characterized "design space" [15].
- Perform a Risk Assessment: Identify all materials, equipment, analyst techniques, and method steps that may influence precision, accuracy, or other key responses. This risk assessment pinpoints where characterization is most needed [15].
- Design the Experimental Matrix: For a small number of factors (e.g., 2-3), a full factorial design may be suitable. For more factors, a D-optimal design can more efficiently explore the design space [15].
- Identify an Error Control Plan: Measure and record uncontrolled factors (e.g., analyst name, ambient temperature, hold times) during the study to account for their potential influence [15].
This structured approach ensures that the method is thoroughly understood and validated across a range of conditions, contributing directly to its reliability and, by extension, patient safety.
Key Performance Characteristics and Experimental Protocols
The following performance characteristics are typically assessed during method validation. The experiments must be designed to generate quantitative data that statistically proves the method's reliability.
Precision
Precision, the closeness of agreement between a series of measurements, is often broken down into repeatability and intermediate precision.
- Experimental Protocol: To determine repeatability, a minimum of 6 to 10 replicate measurements of a homogeneous sample at 100% of the test concentration should be performed. For intermediate precision, the same procedure is repeated on a different day, with a different analyst, or using different equipment [15]. The standard deviation (SD) and relative standard deviation (RSD) are calculated from the results.
Accuracy
Accuracy expresses the closeness of agreement between the value found and a reference value, which is accepted as either a conventional true value or an accepted reference value.
- Experimental Protocol: Accuracy is typically established using a minimum of 9 determinations over a minimum of 3 concentration levels covering the specified range (e.g., 3 concentrations, 3 replicates each). The sample matrix is spiked with a known quantity of the analyte, and the recovery is calculated as a percentage of the known added amount [15].
Linearity and Range
Linearity is the ability of the method to obtain test results proportional to the concentration of the analyte. The range is the interval between the upper and lower concentrations for which linearity has been demonstrated.
- Experimental Protocol: A minimum of 5 concentrations are prepared and analyzed in duplicate [15]. The response is plotted against the concentration, and a linear regression model is fitted. The correlation coefficient (r), y-intercept, and slope are calculated.
The data from validation experiments should be summarized clearly for evaluation and comparison against acceptance criteria. The following table provides a template for presenting key validation parameters.
Table 1: Example Summary of Method Validation Results
| Performance Characteristic | Protocol Summary | Result | Acceptance Criterion | Status |
|---|---|---|---|---|
| Accuracy (Recovery %) | 9 determinations at 3 levels (80%, 100%, 120%) | Mean Recovery = 99.5% | 98.0% - 102.0% | Pass |
| Repeatability (RSD %) | 10 replicates of 100% test concentration | RSD = 0.8% | NMT* 2.0% | Pass |
| Intermediate Precision (RSD %) | 10 replicates, different analyst & day | RSD = 1.2% | NMT 2.0% | Pass |
| Linearity (Correlation Coefficient) | 5 concentrations (50%-150%), duplicate | r = 0.999 | NLT* 0.998 | Pass |
NMT: No More Than; NLT: No Less Than
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of a method is dependent on the quality of the materials used. The following table details key reagents and materials essential for conducting a robust method validation.
Table 2: Key Research Reagent Solutions for Method Validation
| Item | Function / Purpose | Critical Quality Attributes |
|---|---|---|
| Reference Standards | Serves as the benchmark for determining accuracy and bias; used to calibrate the analytical procedure [15]. | High purity, well-characterized, and documented stability. |
| Certified Reference Materials (CRMs) | Used for method validation and quality control to verify accuracy; provides a known and traceable analyte concentration in a representative matrix. | Certified purity and concentration, supplied with a certificate of analysis, traceability to SI units. |
| High-Purity Solvents & Reagents | Form the mobile phase, sample diluent, and reaction media; essential for achieving desired chromatography and detector response. | Appropriate grade (e.g., HPLC, GC), low UV absorbance, minimal particulate matter. |
| Stable, Well-Characterized Test Samples | The material on which the validated method will be performed; used for precision and robustness studies. | Representative of future test samples, homogeneous, and stable for the duration of the testing. |
| Cyclononanamine | Cyclononanamine, CAS:59577-26-3, MF:C9H19N, MW:141.25 g/mol | Chemical Reagent |
| 2,6-Dimethyl-9H-carbazole | 2,6-Dimethyl-9H-carbazole|High-Purity Reference Standard | High-purity 2,6-Dimethyl-9H-carbazole for research. Explore its applications in medicinal chemistry and materials science. This product is for Research Use Only (RUO). Not for human or veterinary use. |
Case Study: Validation of a Comparative In Vitro Test Method
A 2025 study on the calcification of bioprosthetic heart valves provides a robust example of a comparative method validation. The researchers developed an accelerated dynamic in vitro calcification test to replace expensive and time-consuming large animal studies for evaluating anti-calcification treatments [16].
- Objective: To validate a novel in vitro test method by comparing the calcification tendency of two differently pretreated groups of porcine heart valve bioprostheses.
- Experimental Protocol: Two groups (N=4 each) of aortic bioprostheses were subjected to accelerated dynamic in vitro calcification testing. Calcification was monitored using high-speed video documentation and microscopy [16].
- Comparative Analysis: The extent of calcification was quantified using multiple techniques: μ-CT for semi-destructive quantification and colorimetry/complexometry for destructive chemical quantification. The structural identity of the deposits was confirmed as "biological apatite" using X-ray powder diffraction (XRD), and the location within the valve structure was identified via von Kossa staining [16].
- Outcome and Reliability Link: The quantitative results showed a "distinctly stronger calcification tendency" for the non-pretreated group compared to the anti-calcifying pretreated group. The study confirmed the method's reliability by demonstrating that its quantitative results and structural findings were comparable with, and in line with, published in vivo observations [16]. This validated in vitro method provides a cost-effective and animal-saving tool, contributing to the safer development of more durable heart valves.
Proving method reliability through a structured, comparative validation strategy is not merely a regulatory formality; it is a critical component of patient safety. A method that has been rigorously tested for its precision, accuracy, and robustness under a range of conditions, as demonstrated through DOE and statistical analysis, generates trustworthy data. This reliable data forms the foundation for making correct decisions about drug product quality, clinical diagnostics, and medical device performance, ultimately ensuring that the products reaching patients are safe and effective. The frameworks, protocols, and tools outlined in this guide provide a pathway for researchers to achieve these core objectives, embedding reliability and safety into the very fabric of their analytical methods.
In the global pharmaceutical landscape, the validation of analytical methods is not merely a regulatory checkbox but a fundamental pillar of drug quality, safety, and efficacy. For researchers selecting a comparative method for validation studies, navigating the harmonized yet complex framework of international guidelines is paramount. The core of this framework is built upon the International Council for Harmonisation (ICH) Q2(R2) guideline, which provides the foundational validation parameters. This is operationalized in the United States via FDA regulations (21 CFR Part 211) and USP General Chapter <1225>, and in the European Union via European Medicines Agency (EMA) adoption of ICH standards. A modernized, lifecycle approach to analytical procedures, reinforced by the simultaneous issuance of ICH Q2(R2) and ICH Q14, moves beyond a one-time validation event to an integrated process of development, validation, and continuous improvement [17]. This guide provides a detailed roadmap for scientists to understand these requirements and strategically select a robust comparative method for their validation research.
The Regulatory Landscape and Key Guidelines
The integrity of analytical data is the bedrock of pharmaceutical quality control and regulatory submissions. A clear understanding of the roles and interrelationships of the major regulatory bodies and their guidelines is the first step in selecting an appropriate method.
International Council for Harmonisation (ICH): The ICH provides a harmonized framework to ensure global consistency in drug development and manufacturing. Its guidelines, once adopted by member regions, become the global gold standard, ensuring a method validated in one region is recognized worldwide. The primary guidelines for analytical procedures are ICH Q2(R2) on validation and ICH Q14 on procedure development [17].
U.S. Food and Drug Administration (FDA): As a key member of ICH, the FDA adopts and implements ICH guidelines. Compliance with ICH Q2(R2) is a direct path to meeting FDA requirements for submissions like New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs). The FDA's own regulations, codified in 21 CFR Part 211, stipulate the Current Good Manufacturing Practice (CGMP) requirements for finished pharmaceuticals, which mandate that laboratory controls include the establishment of scientifically sound test methods [17] [18] [19].
European Medicines Agency (EMA): The EMA, representing the European Union, is another key regulatory member of ICH. It adopts ICH guidelines as scientific standards, meaning ICH Q2(R2) forms the basis for analytical procedure validation for marketing authorizations in the EU [20].
United States Pharmacopeia (USP): The USP publishes legally recognized standards for drugs and dietary supplements in the United States. USP General Chapter <1225> "Validation of Compendial Methods" provides detailed guidance on validating analytical procedures, harmonizing to the extent possible with ICH principles. Per CGMP regulations, users of USP methods are not required to fully validate them but must verify their suitability under actual conditions of use [21].
The diagram below illustrates the relationship between these key guidelines and the analytical procedure lifecycle:
Figure 1: The Interplay of Global Guidelines in the Analytical Lifecycle
Core Validation Parameters According to ICH Q2(R2) and USP
The selection of a comparative method must be justified by demonstrating that the method meets predefined performance characteristics. ICH Q2(R2) and USP <1225> define these core validation parameters, which form the critical criteria for your evaluation.
The table below summarizes the definitions and methodological approaches for establishing these key parameters, providing a clear framework for your validation studies.
Table 1: Core Analytical Procedure Validation Parameters and Their Determination
| Parameter | Definition | Common Methodological Approaches for Determination |
|---|---|---|
| Accuracy [21] | The closeness of agreement between the measured value and the true value. | For drug substances: Analyze a standard of known purity (e.g., USP Reference Standard). For drug products: Analyze synthetic mixtures or spike the placebo with known amounts of analyte. Assess using a minimum of 9 determinations over 3 concentration levels. |
| Precision [21] | The degree of scatter among repeated measurements from a homogeneous sample. | Repeatability: Multiple analyses by the same analyst, same equipment, short time. Intermediate Precision: Different days, different analysts, different equipment within the same lab. Reproducibility: Between different laboratories (collaborative studies). |
| Specificity [21] | The ability to assess the analyte unequivocally in the presence of other components. | For assays: Spike with impurities/excipients and demonstrate the assay is unaffected. For impurity tests: Spike with impurities and demonstrate they are determined with accuracy and precision. Use chromatographic peak purity tests (e.g., diode array, mass spectrometry). |
| Linearity [17] | The ability of a method to obtain results directly proportional to analyte concentration. | Analyze a series of samples with analyte concentrations across a specified range. Plot response vs. concentration and evaluate using statistical methods for linearity (e.g., correlation coefficient, y-intercept, slope). |
| Range [17] | The interval between the upper and lower concentrations of analyte for which linearity, accuracy, and precision have been demonstrated. | Established based on the intended use of the method, confirmed by the linearity and accuracy/precision data across the interval. |
| Limit of Detection (LOD) [21] | The lowest amount of analyte that can be detected, but not necessarily quantitated. | Visual evaluation: Analyze samples with known low concentrations. Signal-to-noise: Compare measured signals from low concentration samples with blank samples (typically 2:1 or 3:1 ratio). |
| Limit of Quantitation (LOQ) [21] | The lowest amount of analyte that can be quantitated with acceptable accuracy and precision. | Visual evaluation. Signal-to-noise (typically 10:1 ratio). Based on the standard deviation of the response and the slope of the calibration curve. |
| Robustness [17] | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters. | Deliberately vary parameters (e.g., pH, mobile phase composition, temperature, flow rate) and evaluate the impact on the analytical results. |
The Modernized Lifecycle Approach: ICH Q2(R2) and ICH Q14
The recent simultaneous issuance of ICH Q2(R2) and the new ICH Q14 guideline marks a significant evolution from a prescriptive, "check-the-box" validation model to a more scientific, lifecycle-based approach [17]. This shift is critical for researchers planning a long-term strategy for their analytical procedures.
From Validation to Lifecycle Management: Analytical procedure validation is no longer a one-time event conducted at the end of development. It is a continuous process that begins with method development and continues throughout the method's entire lifecycle, including post-approval changes [17].
The Analytical Target Profile (ATP): ICH Q14 introduces the ATP as a prospective summary of the method's intended purpose and its required performance characteristics [17]. The ATP is the foundational document that should guide the selection and development of your comparative method. It proactively defines what the method needs to achieve, ensuring it is "fit-for-purpose" from the very beginning.
Enhanced vs. Minimal Approach: ICH Q14 describes two pathways for method development. The traditional, minimal approach is based on univariate experimentation. The enhanced approach encourages a more systematic, science- and risk-based development, often involving multivariate studies to understand the method's operational range thoroughly. While requiring more initial investment, the enhanced approach allows for more flexible and streamlined post-approval change management [17].
Inclusion of New Technologies: ICH Q2(R2) has been expanded to explicitly include guidance for modern techniques, such as multivariate analytical procedures, ensuring the guidelines remain relevant in an era of rapid technological advancement [17].
A Strategic Roadmap for Selecting and Validating a Comparative Method
For the researcher, the following step-by-step roadmap integrates the regulatory requirements into a practical workflow for selecting and validating a comparative method.
Define the Analytical Target Profile (ATP)
Before any laboratory work begins, define the ATP. This is a crisp, quantitative statement of the method's requirements. What analyte is being measured? What is the expected concentration range? What level of accuracy and precision is required? The ATP sets the target for all subsequent activities [17].
Conduct a Risk Assessment
Employ quality risk management principles (ICH Q9) to identify potential variables that could impact method performance. Consider factors related to the sample (matrix effects, stability), the method (critical operational parameters), and the instrumentation. This risk assessment will directly inform the robustness studies in your validation plan and help define the method's control strategy [17].
Develop a Validation Protocol
Based on the ATP and risk assessment, create a detailed, prospective validation protocol. This protocol is the blueprint for your study and should explicitly define:
- The objective of the validation.
- The validation parameters to be tested (referencing Table 1).
- The detailed experimental design for each parameter.
- The predefined acceptance criteria for each parameter, derived from the ATP.
Execute Validation and Document Results
Execute the studies as outlined in the validation protocol. Meticulously document all raw data, results, and calculations. The results should be summarized and compared against the acceptance criteria. Any deviation must be investigated and justified.
Establish a Lifecycle Management Plan
Once the method is validated, maintain it under a state of control. Implement a system for change management to manage any future modifications in a structured manner. The enhanced knowledge from an ICH Q14-based development can facilitate a more science-based assessment of changes, potentially reducing regulatory reporting burdens [17].
The following workflow diagram encapsulates this strategic roadmap:
Figure 2: Strategic Roadmap for Method Validation
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental to conducting the experiments described in the validation protocols. Sourcing high-quality materials from reputable suppliers is critical to generating reliable and defensible data.
Table 2: Key Research Reagents and Materials for Method Validation
| Reagent/Material | Critical Function in Validation | Application Examples |
|---|---|---|
| Drug Substance Reference Standard [22] [21] | Serves as the primary benchmark for establishing accuracy, linearity, and precision. Its certified purity and identity are essential for all quantitative measurements. | Preparation of calibration standards for assay and impurity methods. Used in accuracy/recovery studies. |
| Impurity and Degradation Product Standards [22] [21] | Used to validate specificity, LOD, LOQ, and accuracy for impurity tests. Demonstrates the method can separate and quantify known impurities. | Forced degradation studies (stress testing). Specificity and selectivity experiments. Establishing the range for impurity quantitation. |
| Placebo/Matrix Components | Essential for validating specificity and accuracy in drug product methods. Ensures that excipients or matrix components do not interfere with the analyte signal. | Accuracy studies by spiking the placebo with known amounts of analyte. Specificity chromatograms to show no interfering peaks. |
| High-Purity Solvents and Reagents | Form the basis of mobile phases, sample solutions, and buffer preparations. Their quality directly impacts baseline noise, detection sensitivity, and reproducibility. | Preparation of mobile phases for chromatography. Sample and standard preparation. Robustness testing of method parameters. |
| 2-Bromobenzo[h]quinazoline | 2-Bromobenzo[h]quinazoline | 2-Bromobenzo[h]quinazoline is a versatile nitrogen heterocycle building block for anticancer and antimicrobial research. For Research Use Only. Not for human use. |
| 2-Cyclopentylpyridine | 2-Cyclopentylpyridine (CAS 56657-02-4) - For Research Use | Get high-purity 2-Cyclopentylpyridine (CAS 56657-02-4). This C10H13N compound is for research applications only. Not for human or veterinary use. |
Navigating the global regulatory guidelines for analytical method validation requires a deep understanding of the harmonized principles in ICH Q2(R2) and their regional implementations by the FDA and EMA. The strategic selection of a comparative method is no longer just about meeting a fixed set of validation parameters. It is about adopting a modernized, science- and risk-based lifecycle approach, as championed by ICH Q14. By starting with a well-defined Analytical Target Profile, conducting thorough risk assessments, and executing a detailed validation plan, researchers can develop robust, reliable, and defensible analytical methods. This rigorous approach not only ensures compliance with global regulatory standards from the FDA, EMA, and USP but also ultimately guarantees the quality, safety, and efficacy of pharmaceutical products reaching patients.
A Step-by-Step Strategy for Selecting Your Comparative Method
The selection of an appropriate comparative method is the foundational step in method validation research. This process determines the reference point against which a new or alternative measurement procedure (the "test method") will be evaluated. The intended use of the test method dictates the performance requirements that the comparative method must help verify, establishing the criteria for selecting a scientifically sound reference [23]. An improperly selected comparative method compromises the entire validation study, potentially leading to inaccurate conclusions about the test method's performance and inappropriate implementation in research or clinical practice.
This technical guide provides researchers, scientists, and drug development professionals with a structured framework for establishing robust method selection criteria, detailed experimental protocols for comparison, and the statistical tools required for data interpretation, all framed within a rigorous method validation context.
Core Principles and Terminology
Defining Key Performance Characteristics
A clear understanding of key metrological terms is essential for establishing meaningful selection criteria. These definitions form the vocabulary for setting performance benchmarks.
- Accuracy vs. Bias: In method-comparison studies, accuracy typically refers to the closeness of agreement between a test method's results and an accepted reference value. When comparing two clinical methods, the difference in values is more precisely termed bias, which represents the systematic difference of the test method relative to the comparative method [23].
- Precision: This term has two contextual definitions: 1) the closeness of agreement between independent results obtained under stipulated conditions (repeatability), and 2) the degree to which values cluster around the mean of their distribution. Repeatability is a necessary precondition for assessing agreement between methods [23].
- Linearity: The ability of a method to obtain results that are directly proportional to the concentration of the analyte within a given range [24].
- Limits of Agreement: A statistical range within which a specified percentage of differences between two measurement methods are expected to fall. Typically, the 95% limits of agreement are calculated as the mean difference (bias) ± 1.96 times the standard deviation of the differences [23].
Hierarchical Criteria for Method Selection
The ideal comparative method is one whose correctness is well-documented. The following hierarchy should guide the selection process, with Category 1 representing the gold standard.
Table: Hierarchy of Comparative Methods for Validation Studies
| Category | Method Type | Key Characteristics | Implication for Bias Interpretation |
|---|---|---|---|
| Category 1 | Definitive or Reference Method | A method of highest accuracy in a hierarchy of methods, confirmed through rigorous interlaboratory testing and traceability to reference materials [1]. | Any observed bias is confidently attributed to the test method. |
| Category 2 | Established Routine Method | A method in widespread use and accepted as providing clinically reliable results, but without the formal documentation of a reference method. | Differences must be interpreted with caution. Small differences indicate relative accuracy; large differences require investigation to identify the inaccurate method [1]. |
| Category 3 | Previous Generation Method | The method currently being used, which the new test method is intended to replace. | The goal is to demonstrate equivalent performance to avoid disruptive clinical impacts. |
Experimental Design and Protocols
A robust experimental design is critical for generating reliable data on method comparability. The following protocols outline the key considerations.
Specimen Selection and Handling
The quality of the specimen panel used for comparison directly influences the validity of the results.
- Number of Specimens: A minimum of 40 different patient specimens is recommended to provide a reasonable basis for statistical analysis [1] [23]. The primary goal is to cover the entire working range of the method; 20 well-selected specimens covering a wide concentration range can be more informative than 100 random specimens [1].
- Concentration Range: Specimens must be selected to cover the entire physiological and pathological range for which the test method will be used. For example, a thermometer must be validated across hypothermic, normothermic, and febrile ranges to be clinically useful [23].
- Specimen Stability and Timing: For dynamic physiological parameters, measurements must be taken simultaneously or within a time frame where the analyte is stable. The order of measurement should be randomized to avoid systematic bias from time-dependent changes [23]. Stability can be managed through preservatives, refrigeration, or prompt analysis [1].
Data Collection Protocol
The protocol for running specimens and collecting data must minimize introduced variability.
- Measurement Replication: While single measurements per specimen are common, duplicate measurements are strongly recommended. Duplicates should be performed on different aliquots, ideally in different analytical runs, to help identify sample mix-ups, transposition errors, and other mistakes that could invalidate individual data points [1].
- Study Duration: The comparison experiment should be conducted over a minimum of 5 days, and preferably extended over a longer period (e.g., 20 days) to capture inter-day analytical variation and make the study more representative of routine practice [1].
Figure 1: High-level workflow for a method comparison study.
Data Analysis and Interpretation
Graphical Analysis of Data
Visual inspection of data is a fundamental first step in analysis, allowing researchers to identify patterns, outliers, and potential problems.
- Bland-Altman Plot: This is the recommended graph for assessing agreement between two methods. The difference between the paired measurements (Test - Comparative) is plotted on the Y-axis against the average of the two measurements on the X-axis. This plot visually reveals the bias (mean difference) and the spread of the differences (limits of agreement), and can help identify concentration-dependent bias [23].
- Comparison/Scatter Plot: The test method result is plotted on the Y-axis against the comparative method result on the X-axis. A line of identity (y=x) is drawn; if the methods agree perfectly, all points will lie on this line. This plot is useful for visualizing the analytical range and the general relationship between methods [1].
Figure 2: The three-phase analytical workflow for comparison data.
Statistical Methods and Interpretation
Statistical calculations provide numerical estimates of the errors between methods.
Table: Statistical Methods for Analyzing Method Comparison Data
| Statistical Method | Calculation | Application Context | Interpretation |
|---|---|---|---|
| Bias & Limits of Agreement | Bias = Mean of differencesLOA = Bias ± 1.96*SDdiff | Preferred for narrow analytical ranges or when a single estimate of agreement is needed across the range [23]. | The bias is the estimated systematic error. The LOA define the range where 95% of differences between the two methods are expected to lie. |
| Linear Regression | Y = a + bXwhere Y = Test method, X = Comparative method | Used for data covering a wide analytical range. Provides estimates of constant error (y-intercept, a) and proportional error (slope, b) [1]. | A perfect agreement would have a slope of 1 and an intercept of 0. The systematic error at any decision level Xc is SE = (a + b*Xc) - Xc. |
| Correlation Coefficient (r) | Measures the strength of the linear relationship between two methods. | Mainly useful for verifying that the data range is wide enough to give reliable regression estimates. An r ≥ 0.99 is desirable for this purpose [1]. | Not a measure of agreement. High correlation can exist even when there is consistent bias between methods. |
The Scientist's Toolkit
Successful execution of a method-comparison study requires both conceptual knowledge and practical tools. The following table details essential resources.
Table: Essential Toolkit for Method-Comparison Studies
| Tool or Resource | Function | Example Use in Validation |
|---|---|---|
| CLSI Guidelines (e.g., EP09-A3) | Provide standardized, internationally recognized protocols for designing and evaluating method-comparison studies [24]. | Ensures the study design, sample size, and statistical analysis meet regulatory and accreditation standards (e.g., FDA, CAP). |
| Specialized Software (e.g., Analyse-it, MedCalc) | Performs complex statistical analyses (Deming regression, Passing-Bablok, Bland-Altman plots) that are not standard in general statistical packages [23] [24]. | Automates the creation of Bland-Altman plots and calculation of bias, limits of agreement, and regression statistics with confidence intervals. |
| Reference Materials | Substances with one or more sufficiently homogeneous and well-established property values used for calibration or assignment of a value [1]. | Used to verify the calibration and traceability of the comparative method, especially if it is a candidate reference method. |
| Power Analysis Tools | Used during the design phase to calculate the necessary sample size based on desired power, alpha, and the smallest clinically important difference [23]. | Prevents a underpowered study that might fail to detect a clinically significant bias between the methods. |
| 3-Methoxypyrrolidin-2-one | 3-Methoxypyrrolidin-2-one, MF:C5H9NO2, MW:115.13 g/mol | Chemical Reagent |
| Pyridazino[1,2-a]cinnoline | Pyridazino[1,2-a]cinnoline|High-Qurity|RUO |
Selecting an appropriate analytical procedure is a critical foundational step in method validation research. This decision directly influences the complexity, cost, and timeline of your validation studies and ultimately determines the reliability of the quality control data generated for your drug substance or product. The process involves identifying and evaluating existing methods before committing to laboratory experiments. There are three primary sources for these methods: compendial (officially published in pharmacopeias), reference (from scientific literature or a previously validated source), and routine (in-house developed or modified methods). A systematic evaluation at this stage ensures the selected procedure is fit-for-purpose, aligns with the Analytical Target Profile (ATP), and complies with relevant regulatory guidelines [25] [26]. This guide provides a detailed framework for sourcing and evaluating these potential methods within a comparative method validation strategy.
Categories of Analytical Methods
Compendial Methods
Compendial methods are standardized procedures published in official compendia such as the United States Pharmacopeia (USP), European Pharmacopoeia (EP), or Japanese Pharmacopoeia (JP). They are legally recognized by regulatory authorities and are validated for their intended use.
- Advantages: They are readily available, universally accepted, and do not require full validation, significantly reducing development time and resources. Their use facilitates global market access [26].
- Considerations: While they do not require full validation, their implementation is not without obligation. A compendial verification is required to demonstrate that the method works as expected under the actual conditions of use in your laboratory, with your specific instrument operator, and for your specific drug product [26].
- Typical Applications: Ideal for well-established, simple drug molecules with known and controlled properties. They are commonly used for assays, identification tests, and related substance tests for drugs that have been on the market for some time.
Reference Methods
Reference methods are well-characterized procedures that have been previously validated. They can be sourced from scientific literature, collaborators, or contract research organizations (CROs).
- Advantages: Provides a strong, data-backed starting point, which can be particularly valuable for novel drug modalities or complex analytical techniques. Using a reference method can help in bridging knowledge gaps [27].
- Considerations: The extent of the available validation data can vary. A thorough assessment is needed to determine if the existing validation meets current regulatory standards (e.g., ICH Q2(R1)) and is suitable for your product's specific Critical Quality Attributes (CQAs). The process of method transfer from the source laboratory must be meticulously planned and documented [26] [27].
- Typical Applications: Highly valuable in early product development, for biologics, and when a platform method from a similar product can be adapted [26].
Routine Methods
Routine methods are typically in-house developed procedures or modifications of existing methods. They are developed when no suitable compendial or reference method exists.
- Advantages: Can be perfectly tailored to control the specific CQAs of a unique product or to overcome specific challenges related to the sample matrix. They offer maximum flexibility.
- Considerations: This path is the most resource-intensive, requiring full method development and validation from scratch. It demands a deep understanding of the molecule's chemical properties and the analytical technique. The entire lifecycle management, from development to ongoing performance verification, falls on the developing laboratory [25] [27].
- Typical Applications: Essential for new chemical entities, complex formulations like combination products, or when a new analytical technique offers superior specificity or sensitivity.
Table 1: Comparison of Analytical Method Sources
| Characteristic | Compendial Method | Reference Method | Routine/In-House Method |
|---|---|---|---|
| Development Effort | Low | Moderate | High |
| Regulatory Acceptance | High (Pre-established) | Requires Assessment | Must be Demonstrated |
| Validation Requirement | Verification | Transfer/Partial Validation | Full Validation |
| Cost & Timeline | Low/Fast | Moderate/Medium | High/Slow |
| Flexibility | Low | Moderate | High |
| Ideal Use Case | Standardized, simple drugs | Novel drugs with existing models | Unique CQAs, no existing method |
A Framework for Method Evaluation
Once potential methods are sourced, a systematic, risk-based evaluation must be conducted to select the most suitable candidate for validation.
Defining the Analytical Target Profile (ATP) and Fit-for-Purpose
The evaluation begins with a clear definition of the ATP. The ATP is a predefined objective that outlines the required performance characteristics of the method [25] [26]. It states what the method needs to achieve (e.g., "quantify impurity X at a level of 0.1% with an accuracy of 90-110%") rather than how to achieve it. The fit-for-purpose concept is central to this, meaning the validation scope should be appropriate for the product's development stage—simpler approaches for early stages and full validation for commercial filing [26].
The principles of Quality by Design (QbD) can be applied during method development to build robustness into the procedure by understanding the impact of critical method parameters [25].
Key Parameters for Evaluation
The following performance characteristics, as defined in guidelines like ICH Q2(R1), should be evaluated against the ATP to determine a method's suitability [28].
- Accuracy: The closeness of agreement between the accepted reference value and the value found. For drug products, it is typically assessed by spiking known amounts of analyte and measuring percent recovery [28].
- Precision: The closeness of agreement between a series of measurements. This includes repeatability (intra-assay), intermediate precision (inter-day, inter-analyst, inter-equipment), and reproducibility (inter-laboratory) [28].
- Specificity: The ability to assess the analyte unequivocally in the presence of other components like impurities, degradants, or matrix. This is demonstrated by resolving the analyte peak from the closest eluting potential interferent [28].
- Linearity and Range: The ability to obtain test results proportional to analyte concentration within a given range. Linearity is demonstrated across a minimum of five concentration levels [28].
- Limit of Detection (LOD) & Quantitation (LOQ): The lowest concentration that can be detected or quantitated with acceptable accuracy and precision. These are often determined based on signal-to-noise ratios (3:1 for LOD, 10:1 for LOQ) or statistical approaches [28].
- Robustness: A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., pH, temperature, flow rate), indicating its reliability during normal usage [28].
Table 2: Experimental Protocols for Key Evaluation Parameters
| Parameter | Experimental Protocol Summary | Typical Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a minimum of 9 determinations across 3 concentration levels covering the specified range. For drug products, use synthetic mixtures spiked with known quantities [28]. | Report as % recovery of the known, added amount (e.g., 98-102%). |
| Precision (Repeatability) | Analyze a minimum of 9 determinations covering the specified range (e.g., 3 concentrations, 3 replicates each) or 6 determinations at 100% of test concentration [28]. | Report as % Relative Standard Deviation (% RSD). |
| Linearity | Prepare and analyze a minimum of 5 concentrations spanning the declared range of the method [28]. | Correlation coefficient (r²), slope, and y-intercept of the calibration curve. Residuals should be random. |
| Specificity | For chromatographic methods, inject samples containing potential interferents (impurities, degradants, matrix). Use peak purity tools (e.g., photodiode-array or mass spectrometry) to demonstrate the analyte peak is pure [28]. | Resolution between the analyte and closest eluting peak; Peak purity index match. |
| Robustness | Deliberately vary method parameters (e.g., ± 0.1 pH units, ± 2°C column temperature) using an experimental design (e.g., Design of Experiments) and monitor the effect on system suitability criteria [28] [27]. | Method meets system suitability requirements despite variations. |
The following workflow diagram outlines the logical decision process for sourcing and evaluating analytical methods.
Method Sourcing and Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful evaluation and validation of an analytical method depend on the quality and consistency of the materials used. The following table details key reagents and their critical functions.
Table 3: Essential Research Reagents and Materials for Method Evaluation
| Reagent / Material | Function in Evaluation & Validation |
|---|---|
| Certified Reference Standards | Serves as the benchmark for quantifying the analyte and establishing method accuracy, linearity, and precision. Their purity and traceability are paramount [27]. |
| Forced Degradation Samples | Artificially degraded samples (via heat, light, acid, base, oxidation) are used to demonstrate method specificity by proving the method can separate the analyte from its degradation products [26]. |
| System Suitability Standards | A reference preparation used to verify that the chromatographic system (or other instrument) is performing adequately at the time of testing. Parameters like retention time, tailing factor, and plate count are monitored [28]. |
| High-Purity Reagents & Solvents | Essential for preparing mobile phases, buffers, and sample solutions. Impurities can cause baseline noise, ghost peaks, and interference, adversely affecting LOD/LOQ and specificity. |
| Spiking Materials (Impurities) | Isolated or synthesized impurities, aggregates, or related substances are used in spiking studies to prove method accuracy and specificity for impurity tests, as demonstrated in the SEC case study [26]. |
| 5-Fluoro-2-methylpiperidine | 5-Fluoro-2-methylpiperidine HCl |
| 3-Vinylpiperidine | 3-Vinylpiperidine|High-Purity Research Chemical |
Regulatory and Lifecycle Considerations
Under the ICH Q14 guideline, analytical procedures are now viewed through a lifecycle management lens [25]. This means that the initial selection of a method should consider its long-term suitability and the potential for future changes.
When changes to a method are necessary, a risk-based assessment is required to determine the level of study needed. Two key concepts are:
- Comparability: Demonstrating that a modified method yields results sufficiently similar to the original. This is often sufficient for low-risk changes [25].
- Equivalency: A more rigorous assessment, often requiring a full validation, to demonstrate a replacement method performs equal to or better than the original. This is required for high-risk changes and needs regulatory approval [25].
For methods used at multiple sites, a formal analytical transfer process is mandatory to confirm the method performs consistently in the receiving laboratory. Approaches include comparative testing, covalidation, or validation at the receiving site [26].
Sourcing and evaluating potential analytical methods is a strategic process that sets the trajectory for successful method validation. By systematically assessing compendial, reference, and routine methods against a predefined Analytical Target Profile, scientists can select the most efficient and robust path forward. Adopting a lifecycle mindset, as encouraged by ICH Q14, and employing a fit-for-purpose approach ensures that the chosen method is not only validated for today's needs but remains suitable and compliant throughout the product's lifetime. A rigorous evaluation at this stage is an investment that pays dividends in robust data, regulatory success, and the assurance of product quality and patient safety.
The comparison of methods experiment is a critical component of method validation, serving to estimate the systematic error, or inaccuracy, of a new test method relative to a comparative method [29]. When framed within the broader thesis of selecting a comparative method, the design of this experiment is paramount. The fundamental assumption is that the comparative method provides correct results; the interpretation of the experimental outcomes hinges on this premise [29]. This guide provides researchers and drug development professionals with a detailed protocol for designing and executing this definitive experiment, ensuring that the selected comparator provides a robust benchmark for assessing the new method's performance.
Key Factors in Experimental Design
The integrity of the comparison study depends on several key design factors, summarized in the table below.
Table 1: Key Experimental Design Factors for Method Comparison
| Factor | Consideration & Recommendation | Rationale |
|---|---|---|
| Comparative Method | Preferably a reference method; otherwise, a routine method with documented correctness [29]. | Errors are attributed to the test method if the comparator's correctness is known. Discrepancies with a routine method require careful interpretation [29]. |
| Number of Specimens | Minimum of 40 patient specimens, carefully selected to cover the entire working range [29]. For specificity assessment, 100-200 specimens are recommended [29]. | Quality and range of concentrations are more critical than a large number of random specimens. A wide range ensures reliable statistical estimates [29]. |
| Measurements | Common practice: single measurement. Advantageous: duplicate measurements on different samples or in different runs [29]. | Duplicates act as a check for sample mix-ups, transposition errors, and other mistakes, validating discrepant results [29]. |
| Time Period | A minimum of 5 days, ideally extended over a longer period (e.g., 20 days) with 2-5 specimens per day [29]. | Minimizes systematic errors that could occur in a single analytical run and incorporates routine day-to-day variation [29]. |
| Specimen Stability | Analyze test and comparative methods within two hours of each other, unless stability data indicates otherwise [29]. | Prevents specimen degradation from being a source of observed difference between the methods [29]. |
Statistical Analysis and Data Interpretation
Graphical Analysis
The first step in data analysis is to graph the results for visual inspection, ideally as data is collected [29].
- Difference Plot: Used when methods are expected to show one-to-one agreement. This plot displays the difference between the test and comparative results (test minus comparative) on the y-axis against the comparative result on the x-axis. Data should scatter around the zero line, allowing for immediate identification of large discrepancies and potential constant or proportional errors [29].
- Comparison Plot: Used when methods are not expected to agree one-to-one (e.g., different enzyme reaction conditions). This plot displays the test result on the y-axis against the comparative result on the x-axis. A visual line of best fit shows the general relationship [29].
Statistical Calculations
Statistical calculations provide numerical estimates of systematic error. The appropriate method depends on the analytical range of the data [29].
For a Wide Analytical Range (e.g., glucose, cholesterol): Linear Regression Analysis Linear regression (least squares analysis) is used to calculate the slope (b) and y-intercept (a) of the line of best fit, and the standard deviation of the points about that line (s~y/x~) [29]. The systematic error (SE) at a specific medical decision concentration (X~c~) is calculated as follows:
Y~c~ = a + bX~c~SE = Y~c~ - X~c~Example: Given a regression line Y = 2.0 + 1.03X, the systematic error at X~c~ = 200 is calculated as Y~c~ = 2.0 + 1.03200 = 208, thus SE = 208 - 200 = 8 mg/dL* [29]. The correlation coefficient, r, is also calculated. A value ≥ 0.99 indicates a sufficiently wide data range for reliable regression estimates [29].For a Narrow Analytical Range (e.g., sodium, calcium): Average Difference (Bias) The average difference (bias) between the two methods is calculated, typically using a paired t-test, which also provides the standard deviation of the differences [29].
Table 2: Summary of Statistical Methods for Data Analysis
| Analysis Method | Application | Key Outputs | Estimation of Systematic Error |
|---|---|---|---|
| Linear Regression | Wide analytical range | Slope (b), Y-intercept (a), Standard Error of Estimate (s~y/x~) | SE = (a + bX~c~) - X~c~ at critical decision concentration X~c~ [29] |
| Paired t-test / Average Difference | Narrow analytical range | Mean difference (Bias), Standard deviation of differences | The mean difference itself is the estimate of constant systematic error [29] |
Experimental Workflow and Data Analysis Pathway
The following diagram illustrates the end-to-end workflow for designing and executing a comparison of methods experiment, from planning to final interpretation.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful comparison experiment relies on carefully selected materials and reagents.
Table 3: Essential Research Reagent Solutions for the Comparison Experiment
| Item | Function / Purpose |
|---|---|
| Characterized Patient Specimens | The core of the experiment. These should cover the clinical range and represent the expected spectrum of diseases to challenge the method's real-world performance [29]. |
| Reference Materials / Controls | Used to verify the correct calibration and ongoing performance of both the test and comparative methods throughout the study period. |
| Calibrators for Test Method | Essential for establishing the correct calibration curve for the new method prior to and during the analysis of patient specimens. |
| Reagents for Test Method | The specific chemical reagents, antibodies, or other detection molecules required for the analytical reaction of the candidate method. |
| Reagents for Comparative Method | The specific reagents required for the established comparative or reference method. |
| Preservatives / Stabilizers | Used to ensure specimen integrity, especially if analysis cannot be completed within the recommended two-hour window [29]. |
| 4-Methylazocan-4-ol | 4-Methylazocan-4-ol, MF:C8H17NO, MW:143.23 g/mol |
| (E)-5-Oxoundec-2-enenitrile | (E)-5-Oxoundec-2-enenitrile|High-Purity Reference Standard |
Data Analysis and Interpretation Logic
Once data is collected, a clear logic path guides the choice of statistical analysis and the final interpretation of the method's performance.
In the process of method-comparison research, determining an appropriate sample size, selecting representative specimens, and ensuring their stability are critical steps that directly impact the validity and reliability of the study's findings. A well-designed sampling plan ensures that the estimated bias and precision of the new method, relative to the comparative method, are sufficiently accurate to support a decision on their interchangeability [23]. This section provides a technical guide for researchers and drug development professionals on executing these foundational steps.
Core Concepts and Parameters for Sample Size Determination
Sample size calculation is a statistical exercise that balances cost, practicality, and the desired precision of the final estimates [30]. The goal is to select a number of samples and observations that will yield a reliable estimate of the systematic error (bias) between the test method and the comparative method.
Key Statistical Parameters
The following parameters are essential inputs for any sample size calculation [31]:
- Statistical Analysis to be Used: The choice of statistical test (e.g., paired t-test, linear regression) is a primary driver of the sample size calculation [31].
- Acceptable Precision Level (δ): The margin of error (MoE) or the maximum acceptable difference between the sample estimate and the true population parameter. A smaller δ requires a larger sample size [31] [30].
- Study Power (1-β): The probability of correctly rejecting the null hypothesis when it is false. Typically set at 80% or 90%. Higher power demands a larger sample size [31].
- Confidence Level (1-α): The probability that the confidence interval contains the true population parameter. Commonly set at 95% [31].
- Effect Size (ES): The magnitude of the difference or relationship that the study is designed to detect. In method-comparison studies, this is the clinically meaningful bias or difference between methods. A smaller effect size requires a larger sample size to detect [31] [23].
- Population Variability (σ): The inherent variance of the analyte being measured. Higher variability necessitates a larger sample size to achieve a precise estimate [30].
Quantitative Specifications for Sample Size
The table below summarizes the general recommendations and quantitative specifications for a method-comparison study.
Table 1: Sample Size and Selection Specifications for Method-Comparison Studies
| Aspect | Minimum Specification | Ideal Specification | Rationale & Considerations |
|---|---|---|---|
| Number of Specimens | 40 patient specimens [1] [23] | 100-200 specimens [1] | A minimum of 40 covers basic statistical needs. 100-200 helps assess method-specific interference and specificity [1]. |
| Number of Measurements | Single measurement per specimen by each method [1] | Duplicate measurements per specimen in different runs [1] | Duplicates provide a check for measurement validity and help identify sample mix-ups or transposition errors [1]. |
| Time Period | 5 different days [1] | 20 days or longer [1] [23] | Multiple days help minimize systematic errors from a single run and provide a more realistic estimate of long-term performance. |
| Physiological Range | Cover the clinical reporting range [23] | Cover the entire working range of the method [1] | Ensures the method is validated across all conditions in which it will be used clinically, from low to high values [1] [23]. |
| Data Analysis | Bias and Limits of Agreement (Bland-Altman) [23] | Linear Regression [1] | Linear regression is preferable for a wide analytical range as it allows error estimation at multiple medical decision levels [1]. |
Experimental Protocol for Sample Collection and Handling
A detailed methodology is crucial for the integrity of the method-comparison study.
Specimen Selection and Justification
- Source: Patient specimens are preferred as they represent the full spectrum of diseases and matrices encountered in routine practice [1].
- Concentration Range: Specimens should be carefully selected to cover the entire working range of the method. This is more critical than a large number of specimens with a narrow concentration range [1].
- Selection Method: Purposeful selection based on observed concentrations is recommended over simple random selection from received specimens to ensure a wide analytical range is achieved [1].
Stability and Handling Requirements
- Temporal Stability: Specimens should generally be analyzed by both the test and comparative methods within two hours of each other to prevent analyte degradation from causing observed differences [1].
- Stability Procedures: For less stable analytes, preservation techniques such as adding preservatives, separating serum/plasma from cells, refrigeration, or freezing must be defined and systematized prior to the study [1].
- Measurement Order: The order of analysis (test method first vs. comparative method first) should be randomized to distribute any potential time-dependent effects across both methods [23].
Workflow and Logical Relationships
The following diagram illustrates the integrated workflow for establishing sample size, selection, and stability requirements.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Method-Comparison Studies
| Item | Function in the Experiment |
|---|---|
| Patient-Derived Specimens | Serves as the primary test material, providing a real-world matrix for evaluating method performance across a biological range of the analyte [1] [23]. |
| Reference Method | An established, high-quality method with documented correctness used as a benchmark for comparison. Differences are attributed to the test method [1]. |
| Comparative Method | A general term for the established method in clinical use. Its correctness may not be as rigorously documented as a reference method, requiring careful interpretation of large differences [1]. |
| Statistical Software (e.g., R, MedCalc) | Used for sample size calculation a priori and for subsequent data analysis, including Bland-Altman plots and linear regression to quantify bias and precision [31] [23]. |
| Sample Size Calculation Tools (e.g., G*Power) | Free-of-charge software that assists researchers in calculating the required sample size based on the defined statistical parameters, eliminating the need for manual calculation [31]. |
| Specimen Preservation Materials (e.g., preservatives, separators) | Critical for maintaining analyte stability between the paired measurements on the test and comparative methods, especially for labile analytes [1]. |
| 2-Azaspiro[4.4]nonan-7-ol | 2-Azaspiro[4.4]nonan-7-ol|Research Chemical |
| 4-Nicotinoylbenzonitrile | 4-Nicotinoylbenzonitrile|High-Purity Research Chemical |
A rigorously planned approach to sample size, selection, and stability is non-negotiable for a definitive method-comparison study. By justifying the number of specimens based on statistical principles, ensuring they are representative of the intended clinical use, and controlling pre-analytical variables through strict stability protocols, researchers can generate evidence that reliably informs the decision to implement a new method in a drug development or clinical setting.
Within the framework of selecting a comparative method for method validation research, the data analysis phase is critical for assessing systematic error, or inaccuracy. This assessment determines whether a new method and a comparative method can be used interchangeably without affecting patient results [32]. A meticulously planned analysis strategy progresses from graphical inspection to identify data structure and potential issues, to statistical calculations that quantify the systematic error at medically important decision concentrations [1]. This step ensures that the conclusions drawn about method comparability are valid, reliable, and clinically relevant.
Graphical Inspection: The First Line of Analysis
Graphical inspection is the most fundamental data analysis technique, providing an immediate visual impression of the relationship between methods and the presence of potential errors. It should be performed as data is collected to identify discrepant results that need confirmation while specimens are still available [1].
Scatter Plots
Purpose and Protocol: A scatter plot describes the variability in paired measurements across the measurement range. Each point on the graph represents a single patient sample, with the value from the comparative (or reference) method plotted on the x-axis and the value from the new (test) method plotted on the y-axis [32]. To minimize random variation, duplicate measurements should be performed for both methods, and the mean (or median for three or more measurements) of these replicates should be used for plotting [32].
Interpretation and Pitfalls: A scatter plot reveals the degree of association between the methods. However, a strong linear relationship (high correlation) does not imply comparability, as it may mask a significant constant or proportional bias [32]. Visually, the data points should be assessed for coverage of the entire clinically meaningful measurement range; gaps in coverage, as shown in Figure 2b of the search results, necessitate additional measurements to ensure a valid comparison [32]. The graph should also be inspected for outliers and the general pattern of the data relative to the line of equality.
Difference Plots
Purpose and Protocol: Difference plots, such as Bland-Altman plots, are specifically designed to assess agreement between two methods. The difference between the test and comparative method results (test minus comparative) is plotted on the y-axis against the average of the two methods (or the comparative method result) on the x-axis [32] [1].
Interpretation: In a method comparison with expected one-to-one agreement, the differences should scatter randomly around the horizontal line of zero difference [1]. Systematic patterns, such as points lying predominantly above or below the line at certain concentrations, indicate constant or proportional systematic errors. This plot makes it easy to identify any individual results with large differences that may be outliers [1].
Table 1: Summary of Graphical Analysis Methods
| Graph Type | Primary Purpose | Axes | What to Look For |
|---|---|---|---|
| Scatter Plot | Visualize association and variability across the measurement range. | X: Comparative MethodY: Test Method | Linearity of relationship, gaps in data coverage, potential outliers. |
| Difference Plot | Assess agreement and identify systematic error. | X: Average of Methods or Comparative MethodY: Difference (Test - Comparative) | Scatter around zero, constant/proportional bias, outliers. |
The following diagram illustrates the recommended workflow for the graphical inspection of data in a method comparison study:
Statistical Calculations: Quantifying Systematic Error
After a thorough graphical inspection, statistical calculations provide numerical estimates of the systematic error. The choice of statistics depends on whether the data covers a wide or narrow analytical range.
Linear Regression Analysis
Application: Linear regression (least squares analysis) is preferred for data covering a wide analytical range (e.g., glucose, cholesterol) as it allows for the estimation of systematic error at multiple medical decision concentrations and provides information on the constant or proportional nature of the error [1].
Key Statistics and Interpretation: The regression line is defined by the formula Y = a + bX, where Y is the test method result, X is the comparative method result, a is the y-intercept, and b is the slope.
- Y-intercept (a): Estimates the constant systematic error. A value significantly different from zero suggests a constant bias.
- Slope (b): Estimates the proportional systematic error. A value significantly different from 1.0 suggests a proportional bias.
- Systematic Error at Decision Level (SE): The systematic error at a critical medical decision concentration (
Xc) is calculated asSE = Yc - Xc, whereYc = a + b*Xc[1]. - Standard Error of the Estimate (s~y/x~): Describes the random scatter of the data points around the regression line.
- Correlation Coefficient (r): Primarily useful for verifying that the data range is sufficiently wide to provide reliable estimates of the slope and intercept. An
rvalue ≥ 0.99 is generally desirable for this purpose [1].
Paired t-test Analysis (Bias)
Application: For comparisons with a narrow analytical range (e.g., sodium, calcium), it is often best to calculate the average difference, or bias, between the methods [1].
Key Statistics and Interpretation:
- Mean Difference (Bias): The average of the differences between the test and comparative method results. This is the estimate of the constant systematic error across the measured samples.
- Standard Deviation of the Differences: Describes the distribution of the individual differences between the methods.
- t-value: Used to determine if the calculated bias is statistically significant.
Table 2: Summary of Key Statistical Methods for Method Comparison
| Statistical Method | Application Context | Key Outputs | Interpretation of Systematic Error |
|---|---|---|---|
| Linear Regression | Wide analytical range. | Slope (b), Y-intercept (a), s~y/x~, Systematic Error (SE) at X~c~. | Y-intercept (a): Constant error.Slope (b): Proportional error.SE at X~c~: Total error at decision level. |
| Paired t-test / Bias | Narrow analytical range. | Mean Difference (Bias), Standard Deviation of Differences. | Mean Bias: Average constant systematic error across the measured range. |
Essential Experimental Protocols for Reliable Analysis
The validity of the data analysis is entirely dependent on the quality of the underlying experimental data. Adherence to a rigorous protocol is non-negotiable.
Sample Selection and Handling
- Number of Samples: A minimum of 40 different patient specimens should be tested, with 100-200 being preferable to identify issues related to sample-specific interferences [32] [1].
- Concentration Range: Specimens must be carefully selected to cover the entire clinically meaningful measurement range rather than being chosen at random [32] [1].
- Stability and Timing: Specimens should generally be analyzed by both methods within two hours of each other to prevent stability issues from being misinterpreted as analytical error. Stability can be improved by appropriate specimen processing (e.g., serum separation, refrigeration) [1].
Measurement and Data Collection
- Replication: While single measurements are common, performing duplicate measurements for both methods is highly advantageous. Duplicates act as a check for sample mix-ups, transposition errors, and other mistakes that could invalidate individual data points [1].
- Timeframe: The experiment should be conducted over a minimum of 5 different days and multiple analytical runs to capture typical between-run variation and provide a more realistic estimate of method performance [32] [1].
- Randomization: The sample sequence should be randomized to avoid carry-over effects [32].
The Researcher's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for Method Comparison Studies
| Item | Function and Specification |
|---|---|
| Patient-Derived Specimens | Serve as the core test material; must cover the full clinical range and represent the spectrum of expected diseases and matrices [1]. |
| Reference Method Materials | The benchmark for comparison; ideally a well-documented, high-quality method with traceability to reference standards [1]. |
| Quality Control (QC) Materials | Used to monitor the stability and performance of both the test and comparative methods throughout the data collection period. |
| Preservatives / Stabilizers | Ensure specimen integrity (e.g., prevent analyte degradation) during the window between measurements on the two instruments [1]. |
| 3-(3-Fluorophenyl)pyridine | 3-(3-Fluorophenyl)pyridine, CAS:79412-32-1, MF:C11H8FN, MW:173.19 g/mol |
| 2-Ethoxy-3-methoxybenzamide | 2-Ethoxy-3-methoxybenzamide |
The following workflow summarizes the key experimental and analytical steps in a method comparison study, from planning to final interpretation:
A disciplined approach to planning data analysis, moving from graphical inspection to statistical calculations, is fundamental to a robust method comparison. This process, when supported by a sound experimental design with appropriate sample selection and handling, allows researchers to accurately quantify systematic error. This quantitative estimate of bias, framed against pre-defined acceptability criteria, provides the objective evidence base required to make a definitive decision on the suitability of a comparative method for method validation.
Overcoming Common Challenges and Pitfalls in Method Comparison
Identifying and Managing Outliers and Discrepant Results
Outliers and discrepant results refer to observations in a dataset that deviate markedly from other members of the sample, potentially due to variability in measurement or experimental error [33]. In method validation research, particularly in pharmaceutical development, the identification and management of these data points is not merely a statistical exercise but a fundamental requirement for ensuring analytical method reliability, regulatory compliance, and patient safety [34]. The selection of an appropriate comparative method for validation hinges on understanding how different techniques handle anomalous data that could otherwise compromise method equivalence studies, transferability, and ultimately, drug product quality assessments.
This technical guide provides research scientists and drug development professionals with a comprehensive framework for outlier management specifically contextualized within method validation research. We present advanced detection methodologies, detailed treatment protocols, and practical implementation strategies to strengthen comparative method selection and validation protocols.
Understanding Outliers in Method Validation
Theoretical Framework and Definitions
In regulated pharmaceutical environments, an outlier represents an observation that appears inconsistent with the remainder of the dataset, potentially indicating measurement error, execution variability, or genuine biological deviation [35]. Unlike simple data anomalies, discrepant results in validation studies carry direct implications for acceptance criteria, method performance claims, and regulatory submissions.
Classification of Outliers:
- Global Outliers: Extreme values diverging drastically from the entire dataset's fundamental characteristics, challenging foundational assumptions of method precision and accuracy [36].
- Contextual Outliers: Observations anomalous within specific experimental parameters (e.g., chromatography conditions, sample matrices) that may represent method robustness limitations [36].
- Collective Outliers: Subgroups exhibiting deviant behavior that may indicate systematic error introduction during method execution [36].
Impact on Validation Parameters
Outliers disproportionately influence key validation parameters including precision (repeatability, intermediate precision), accuracy, and linearity assessments [35]. Their undetected presence can lead to underestimation of method variability, false confirmation of specificity, and incorrect determination of quantification limits—potentially compromising the entire validation study [33].
Detection Methods: A Comparative Framework
Statistical Detection Protocols
Statistical methods provide objective, rule-based approaches for outlier identification with defined statistical confidence levels appropriate for regulatory scrutiny.
Grubbs' Test for Single Outliers (Recommended for Small Validation Datasets)
Experimental Protocol:
- Formulate hypotheses: Hâ‚€ (No outliers) vs. Hâ‚ (Presence of outlier)
- Calculate the G statistic: G = |suspect value - sample mean| / sample standard deviation
- Compare against critical values from Grubbs' distribution table at α=0.05 significance level
- If G > critical value, reject Hâ‚€ and classify the suspect value as an outlier [34]
Interquartile Range (IQR) Method (Robust for Non-Normal Distributions)
Experimental Protocol:
- Arrange data in ascending order, calculate Q₠(25th percentile) and Q₃ (75th percentile)
- Compute IQR = Q₃ - Qâ‚
- Establish lower and upper fences: [Q₠- 1.5×IQR, Q₃ + 1.5×IQR]
- Flag any observations outside these boundaries as potential outliers [33] [37]
Z-Score Method (Appropriate for Large, Normally Distributed Data)
Experimental Protocol:
- Calculate sample mean (x̄) and standard deviation (s)
- Compute Z-score for each observation: Zᵢ = |xᵢ - x̄| / s
- Flag observations with |Z| > 3 as potential outliers [33] [38]
Machine Learning Detection Protocols
Machine learning approaches offer advantages for high-dimensional method validation data (e.g., dissolution profiles, stability-indicating methods).
Isolation Forest Algorithm Protocol
Experimental Implementation:
- Prepare normalized dataset of method validation parameters
- Set contamination parameter based on expected outlier rate (typically 0.01-0.1)
- Generate random partitioning trees (typically 100 trees)
- Calculate anomaly score based on path length to isolation
- Flag observations with scores > 0.5 as potential outliers [37] [38]
Local Outlier Factor (LOF) Protocol
Experimental Implementation:
- Standardize all method performance metrics (e.g., peak area, retention time, resolution)
- Compute k-distance (distance to k-th nearest neighbor) for each point
- Calculate reachability distance and local reachability density
- Derive LOF score (ratio of local densities)
- Flag observations with LOF significantly greater than 1 as outliers [37]
DBSCAN (Density-Based Spatial Clustering) Protocol
Experimental Implementation:
- Standardize multidimensional method data (e.g., chromatographic parameters)
- Set epsilon (neighborhood distance) and min_samples parameters
- Identify core points, border points, and noise points
- Classify noise points as outliers [33]
Visual Detection Methods
Visualization techniques provide intuitive outlier assessment complementary to statistical tests.
Box Plot Implementation:
- Plot method performance data as quartiles with whiskers extending to 1.5×IQR
- Identify points beyond whiskers as potential outliers [33] [34]
Scatter Plot Implementation:
- Plot relationship between two method variables (e.g., concentration vs. response)
- Visually identify points deviating from the overall pattern [33]
Table 1: Comparative Analysis of Outlier Detection Methods
| Method | Data Type | Sample Size | Key Assumptions | Regulatory Acceptance |
|---|---|---|---|---|
| Grubbs' Test | Univariate, Normal | n < 25 | Normal distribution | High (established statistical test) |
| IQR Method | Univariate, Non-normal | n > 10 | None | Moderate to High |
| Z-Score | Univariate, Normal | n > 30 | Normal distribution | Moderate |
| Isolation Forest | Multivariate | n > 50 | None | Emerging |
| Local Outlier Factor | Multivariate with clusters | n > 100 | Similar density clusters | Emerging |
| DBSCAN | Multivariate, spatial | n > 50 | Density-based clusters | Limited |
Table 2: Performance Metrics of Detection Methods (Based on Empirical Studies)
| Method | Sensitivity | Specificity | Computational Complexity | Implementation in Python |
|---|---|---|---|---|
| IQR | Moderate | High | Low | scipy.stats.iqr |
| Z-Score | High (normal data) | Low (non-normal) | Low | scipy.stats.zscore |
| Isolation Forest | High | Moderate | Moderate | sklearn.ensemble.IsolationForest |
| Local Outlier Factor | High | High | High | sklearn.neighbors.LocalOutlierFactor |
| DBSCAN | Variable | Moderate | Moderate | sklearn.cluster.DBSCAN |
Management Strategies for Discrepant Results
Decision Framework for Outlier Treatment
A systematic approach to outlier management ensures scientific rigor and regulatory defensibility.
Decision Framework for Outlier Management in Validation Studies
Technical Protocols for Outlier Treatment
Winsorization Technique Protocol
Experimental Implementation:
- Identify outliers using IQR or similar robust method
- Set Winsorization limits (typically 5th and 95th percentiles)
- Cap extreme values at the specified percentile thresholds
- Document original values and adjustment rationale in validation records [33] [35]
Python Implementation:
Trimming/Pruning Protocol
Experimental Implementation:
- Apply statistical test (e.g., Grubbs') to confirm outliers
- Remove confirmed outliers from dataset
- Recalculate method performance metrics
- Compare results with and without outliers for sensitivity analysis [35]
Robust Statistical Estimation Protocol
Experimental Implementation:
- Replace mean with median for central tendency
- Use median absolute deviation (MAD) instead of standard deviation
- Apply Huber or Tukey bisquare M-estimators for regression-based validation parameters [39] [35]
Documentation and Regulatory Considerations
Comprehensive documentation of outlier management decisions is critical for regulatory compliance.
Documentation Requirements:
- Original and modified datasets with clear annotation
- Statistical test results with acceptance criteria
- Investigational findings regarding root cause analysis
- Impact assessment on validation conclusions [34] [35]
Implementation in Method Validation Research
Integration with Validation Lifecycle
Table 3: Outlier Management Across Validation Stages
| Validation Stage | Primary Detection Methods | Treatment Approach | Documentation Emphasis |
|---|---|---|---|
| Method Development | Exploratory, Visual | Removal or Transformation | Hypothesis generation |
| Pre-validation | IQR, Z-score | Winsorization | Method robustness assessment |
| Formal Validation | Grubbs', Statistical tests | Protocol-defined removal | Regulatory defensibility |
| Transfer Studies | Comparative statistical tests | Consensus-based decision | Comparative analysis |
| Routine Monitoring | Control charts, ML algorithms | Investigation-driven | Trend analysis |
Case Study: Chromatographic Method Validation
Experimental Context:
- Method: HPLC-UV for drug product assay
- Validation Parameters: Accuracy, precision, linearity, specificity
- Dataset: 6 concentrations, 3 replicates each (n=18 per validation parameter)
Detected Anomaly:
- One accuracy recovery at 80% concentration: 98.5% (vs. expected 100.5±2%)
Investigation Protocol:
- Sample preparation records review: No deviations noted
- Instrument integration: Acceptable peak symmetry and baseline resolution
- Standard preparation: Within acceptable weighing variability
- Statistical testing: Grubbs' test significant at α=0.05
Resolution:
- Outlier retained based on biological plausibility (potential formulation heterogeneity)
- Additional replicates incorporated to maintain statistical power
- Method precision calculated with and without outlier for sensitivity analysis [34]
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Computational Tools
| Item | Function | Application Context | Implementation Considerations |
|---|---|---|---|
| Statistical Software (e.g., R, Python with SciPy) | Outlier detection and statistical analysis | All validation stages | Version control, script validation |
| Robust Regression Libraries (e.g., HuberRegressor) | Resistant linear modeling | Linearity assessment | Algorithm selection justification |
| Machine Learning Frameworks (e.g., Scikit-learn) | Multivariate outlier detection | Method robustness studies | Training/validation data separation |
| Electronic Lab Notebook (ELN) | Documentation and audit trail | Regulatory compliance | 21 CFR Part 11 compliance |
| Reference Standards | Analytical method calibration | System suitability | Traceability and certification |
| Quality Control Materials | Method performance verification | Ongoing validation monitoring | Stability and homogeneity testing |
| 5-Aminopyridazine 1-oxide | 5-Aminopyridazine 1-oxide, MF:C4H5N3O, MW:111.10 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Methodologies and Emerging Trends
Hybrid Approaches for Complex Data
Combining multiple detection methods significantly improves outlier identification reliability in method validation studies. A 2025 study demonstrated that a hybrid rule-based and statistical approach improved detection accuracy by 23% compared to individual methods [37]. The integration of domain knowledge (e.g., analytical method characteristics) with statistical tests creates a more robust framework for legitimate outlier identification versus false positives.
AI and Machine Learning Innovations
Artificial intelligence technologies are transforming outlier management in method validation through adaptive algorithms that learn from historical validation data. Current research focuses on:
- Autoencoders for unsupervised anomaly detection in high-dimensional analytical data [34]
- One-Class SVM for establishing normal method performance boundaries [34] [38]
- Ensemble Methods that combine multiple detectors to improve consensus detection [36]
These approaches are particularly valuable for continuous method verification and lifecycle management as required by modern quality paradigms.
Advanced Hybrid Outlier Detection Workflow
Effective identification and management of outliers and discrepant results represents a critical competency in method validation research. This guide has presented a comprehensive technical framework integrating traditional statistical methods with emerging machine learning approaches, all contextualized within the pharmaceutical development paradigm. The selection of an appropriate comparative method for validation must incorporate principled outlier management strategies that are scientifically defensible, regulatory compliant, and pragmatically implementable.
As analytical technologies evolve and regulatory expectations advance, the outlier management landscape will continue to sophisticate. Research organizations that institutionalize these robust practices position themselves for successful method validation, regulatory submission, and ultimately, delivery of quality medicines to patients.
Addressing Matrix Effects and Specificity Concerns in Complex Samples
Matrix effects represent a significant challenge in analytical chemistry, particularly when developing and validating methods for complex samples in drug development and bioanalysis. These effects occur when components in the sample matrix interfere with the detection or quantification of target analytes, leading to compromised data quality and potentially erroneous results. Within the context of method validation research, understanding and addressing matrix effects is paramount for selecting appropriate comparative methods that ensure reliability, accuracy, and regulatory compliance.
Matrix effects manifest as suppression or enhancement of the analyte signal, primarily due to co-eluting components that alter ionization efficiency in mass spectrometry-based methods [40] [41]. In complex biological samples such as plasma, serum, urine, and tissues, these interfering components may include salts, lipids, proteins, phospholipids, metabolites, and dosing vehicle excipients [42] [41]. The impact varies depending on the sample origin, preparation techniques, and analytical instrumentation, but consistently affects key method validation parameters including accuracy, precision, sensitivity, and specificity.
For researchers and drug development professionals, the systematic evaluation and mitigation of matrix effects provides a critical framework for selecting and validating robust analytical methods. This technical guide comprehensively addresses the theoretical foundations, detection methodologies, and practical strategies for managing matrix effects, with specific emphasis on their implications for method validation decision-making.
Understanding Matrix Effects: Mechanisms and Impacts
Fundamental Mechanisms
Matrix effects arise through multiple physicochemical mechanisms that interfere with the analytical process. In liquid chromatography-mass spectrometry (LC-MS), the predominant mechanism involves competition for charge and disruption of droplet formation during electrospray ionization (ESI). Co-eluting matrix components compete with target analytes for available charges, thereby reducing ionization efficiency through ion suppression or, less commonly, enhancing ionization through ion enhancement [43] [41]. The extent of these effects depends on the relative concentration, surface activity, and ionization efficiency of both target analytes and matrix interferents.
Another significant mechanism involves physical interference with droplet desolvation and gas-phase ion chemistry. Less-volatile compounds such as phospholipids and proteins can increase the viscosity and surface tension of charged droplets, reducing the efficiency of droplet evaporation and subsequent ion release [43]. In inductively coupled plasma mass spectrometry (ICP-MS), matrix effects manifest differently, including polyatomic interference from ions formed by the sample matrix that overlap with analyte signals, ionization efficiency variations due to matrix composition, and chemical interference where matrix components form compounds with analytes, altering their ionization characteristics [44].
Consequences for Analytical Data Quality
The practical impacts of unaddressed matrix effects significantly compromise analytical data quality and method validation parameters:
Accuracy and Precision Degradation: Matrix effects introduce systematic errors that lead to underreporting (signal suppression) or overreporting (signal enhancement) of analyte concentrations [40] [42]. This directly impacts method accuracy, while the variable nature of matrix effects across different sample sources undermines precision [43].
Reduced Sensitivity and Higher Detection Limits: Signal suppression diminishes method sensitivity, effectively raising the lower limits of detection and quantification. This is particularly problematic for trace-level analytes in bioanalysis [42].
Impaired Specificity: Co-eluting interferents may produce indistinguishable signals from target analytes, especially when using single-reaction monitoring in MS, leading to false positives or negatives [45].
Non-linear Response: Matrix components can cause non-linear instrument response at different analyte concentrations, violating key assumptions of quantitative analysis [41].
The variability of matrix effects across different sample lots and sources presents a particular challenge for method validation, as effects observed during validation with controlled samples may not fully represent those encountered with actual study samples [42].
Detection and Assessment Methods
Qualitative Assessment Techniques
Post-Column Infusion
The post-column infusion method provides a qualitative assessment of matrix effects across the chromatographic run. In this approach, a constant flow of analyte solution is introduced into the HPLC eluent post-column via a syringe pump, while a blank matrix extract is injected [43] [42]. The monitored ion chromatogram reveals regions of ion suppression or enhancement as deviations from the stable baseline signal.
Experimental Protocol:
- Prepare a neat solution of the analyte at a concentration that produces a consistent signal.
- Set up the syringe pump to deliver a constant flow of the analyte solution (typical flow rates: 10-20 μL/min) that merges with the column effluent before the mass spectrometer interface.
- Inject a processed blank matrix sample (without analyte) onto the chromatography system.
- Monitor the analyte signal throughout the chromatographic run.
- Note regions where significant signal suppression (>20% deviation) or enhancement occurs, as these indicate potential matrix effect zones [42].
This method is particularly valuable during method development for identifying problematic retention time windows where analytes should not elute, thereby guiding chromatographic optimization [42].
Post-Extraction Spiking
The post-extraction spiking approach, introduced by Matuszewski et al., quantitatively assesses matrix effects by comparing analyte responses in matrix versus neat solutions [42]. This method calculates the Matrix Factor (MF), a numerical indicator of matrix effects magnitude.
Experimental Protocol:
- Prepare at least six lots of blank matrix from different sources.
- Process these blank matrices through the entire sample preparation procedure.
- Spike the analyte into the processed blank matrices at low and high concentrations (representing the calibration curve range).
- Prepare equivalent concentration neat solutions in mobile phase or reconstitution solvent.
- Analyze all samples and calculate the absolute MF for each matrix lot and concentration: $MF = \frac{Peak Area{matrix}}{Peak Area{neat solution}}$
- Calculate the internal standard-normalized MF: $IS-normalized MF = \frac{MF{analyte}}{MF{IS}}$ [42]
An absolute MF <1 indicates signal suppression, while >1 indicates enhancement. The IS-normalized MF should be close to 1.0 for adequate compensation [42].
Quantitative Assessment Methods
Pre-extraction Spiking
The pre-extraction spiking method, referenced in ICH M10 guidance, evaluates the consistency of matrix effects across different matrix lots by assessing accuracy and precision of quality control samples [42].
Experimental Protocol:
- Prepare quality control samples (low and high concentrations) in at least six different lots of blank matrix, including any special matrices (hemolyzed, lipemic).
- Process these samples through the entire sample preparation and analysis procedure.
- Calculate the measured concentration for each sample against a calibration curve prepared in a different matrix lot.
- Determine accuracy (% bias) and precision (% CV) for each matrix lot.
- Acceptance criteria: Bias within ±15% and CV ≤15% for each individual matrix source demonstrates consistent matrix effect [42].
Table 1: Comparison of Matrix Effect Assessment Methods
| Method | Type of Data | Key Parameters | Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| Post-Column Infusion | Qualitative | Signal deviation regions | Method development | Identifies problematic RT windows | Does not provide quantitative data |
| Post-Extraction Spiking | Quantitative | Matrix Factor (MF) | Method development/validation | Provides numerical matrix effect magnitude | Requires multiple matrix lots |
| Pre-Extraction Spiking | Quantitative | Accuracy and precision | Method validation | Confirms method robustness | Does not quantify effect magnitude |
Strategic Approaches for Mitigating Matrix Effects
Sample Preparation Techniques
Effective sample preparation represents the first line of defense against matrix effects by physically removing interfering components before analysis.
Solid-Phase Extraction (SPE): SPE utilizes cartridges with various sorbent chemistries to selectively retain either the analyte or interfering matrix components. Reversed-phase, ion-exchange, and mixed-mode sorbents can effectively remove phospholipids, proteins, and salts [45]. The technique is particularly valuable for aqueous environmental matrices where analytes are present at low concentrations, enabling both preconcentration and matrix cleanup [45].
Liquid-Liquid Extraction (LLE): LLE exploits differential solubility of analytes and matrix components in immiscible solvents. By selecting appropriate organic solvents, hydrophilic interferents can be effectively separated from hydrophobic analytes [40]. Although somewhat cumbersome, LLE provides excellent cleanup for many biological matrices.
Protein Precipitation: While simple and rapid, protein precipitation often provides insufficient removal of phospholipids and other interferents, potentially exacerbating matrix effects in certain cases [45]. It is often combined with further cleanup techniques for challenging matrices.
Dilution: Simple sample dilution reduces the concentration of matrix components, thereby minimizing their influence on the ionization process [40] [44]. This approach is particularly effective when the analytical method has sufficient sensitivity to accommodate dilution. The dilution factor should be optimized to balance matrix effect reduction with maintained detection capability [44].
Chromatographic Optimization
Chromatographic separation represents a powerful approach for mitigating matrix effects by temporally separating analytes from interfering matrix components.
Gradient Elution Optimization: Adjusting the mobile phase composition gradient can effectively separate analytes from early-eluting salts and late-eluting phospholipids [45] [41]. Method development should focus on achieving retention times that avoid regions of significant suppression identified through post-column infusion.
Column Chemistry Selection: Different stationary phases (C18, phenyl, pentafluorophenyl, HILIC) provide distinct selectivity that can be exploited to resolve analytes from matrix interferents [43]. The use of longer columns (150mm vs. 50mm) or smaller particle sizes can enhance separation efficiency [43].
Mobile Phase Modification: Adjustment of pH, buffer concentration, or organic modifier can subtly alter retention times and ionization characteristics to minimize co-elution [43]. However, mobile phase additives may themselves cause signal suppression and require careful evaluation [43].
Instrumental Approaches
Modern instrumentation provides several technological solutions for addressing matrix effects.
Ionization Source Selection: Alternative ionization techniques such as atmospheric pressure chemical ionization (APCI) or atmospheric pressure photoionization (APPI) are generally less susceptible to matrix effects than electrospray ionization (ESI) for certain compound classes [42] [41]. Switching from ESI to APCI has proven effective in cases where significant signal enhancement was observed despite using stable isotope-labeled internal standards [42].
High-Resolution Mass Spectrometry: High-resolution instruments (Q-TOF, Orbitrap) provide accurate mass measurements that enable mathematical resolution of isobaric interferences, significantly enhancing specificity in complex matrices [46].
Collision/Reaction Cell Technology: In ICP-MS, collision and reaction cells using gases like helium or hydrogen effectively remove polyatomic interferences through energy discrimination or chemical reactions [44]. Similar technology in LC-MS/MS can reduce chemical noise.
Table 2: Matrix Effect Mitigation Strategies Across Analytical Techniques
| Strategy | LC-MS/MS | ICP-MS | GC-MS | Key Considerations |
|---|---|---|---|---|
| Sample Dilution | Highly effective | Highly effective | Limited application | Balance with sensitivity requirements |
| Internal Standards | SIL-IS preferred | Elemental analogues | Deuterated standards | Structural similarity crucial |
| Chromatographic Optimization | Primary approach | Not applicable | Primary approach | Retention time shifting |
| Reaction/Collision Cells | Limited use | Primary approach | Not applicable | Gas selection optimization |
| Ionization Source Switching | ESI to APCI/APPI | Not applicable | Not applicable | Compound-dependent efficacy |
| Matrix-Matching Calibration | Limited use | Highly effective | Limited use | Requires blank matrix |
Advanced Correction Methods
Internal Standardization
Internal standards represent the most widely employed approach for compensating matrix effects in quantitative bioanalysis.
Stable Isotope-Labeled Internal Standards (SIL-IS): SIL-IS containing deuterium (2H), carbon-13 (13C), or nitrogen-15 (15N) are the gold standard for compensation, as they exhibit nearly identical chemical properties and retention times as the native analyte, while being distinguishable mass spectrometrically [45] [42]. This co-elution ensures the SIL-IS experiences virtually identical matrix effects as the analyte, providing optimal compensation [43]. Notably, 13C- and 15N-labeled standards are often preferred over deuterated standards to eliminate chromatographic isotope effects that can occur with deuterium [45].
Structural Analogues as Internal Standards: When SIL-IS are unavailable or cost-prohibitive, structurally similar compounds can serve as internal standards, though they provide less reliable compensation due to potential differences in retention behavior and ionization characteristics [43]. The structural analogue should be carefully selected to match the physicochemical properties of the analyte as closely as possible.
Individual Sample-Matched Internal Standard (IS-MIS): A novel approach for non-target screening involves matching internal standards to individual samples rather than using a pooled sample reference. This strategy has demonstrated superior performance in heterogeneous samples like urban runoff, achieving <20% RSD for 80% of features compared to 70% with conventional approaches, despite requiring approximately 59% more analysis time [46].
Calibration Strategies
Alternative calibration approaches can effectively compensate for matrix effects when standard addition is impractical.
Standard Addition Method: This technique involves spiking known quantities of the analyte into aliquots of the sample [43] [44]. The measured response is plotted against the spiked concentration, and the absolute value of the x-intercept represents the original analyte concentration. Standard addition inherently accounts for matrix effects as they are present in all measured solutions [43]. Although highly accurate, this approach is time-consuming and requires sufficient sample volume [44].
Matrix-Matched Calibration: Preparation of calibration standards in the same matrix as the sample ensures that both experience similar matrix effects [44]. This approach is particularly valuable in ICP-MS applications and when analyzing relatively clean matrices where blank matrix is obtainable [44]. The major limitation is the requirement for analyte-free matrix, which is often unavailable for endogenous compounds [43].
The following workflow diagram illustrates a systematic approach to addressing matrix effects in analytical method development:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Addressing Matrix Effects
| Reagent/Material | Function | Application Notes | Key Considerations |
|---|---|---|---|
| Stable Isotope-Labeled Standards | Internal standardization for compensation | 13C, 15N preferred over deuterated | Co-elution with analyte critical |
| Solid-Phase Extraction Cartridges | Sample clean-up | Various chemistries available (C18, ion-exchange, mixed-mode) | Select based on analyte and interferent properties |
| Phospholipid Removal Plates | Specific removal of phospholipids | Specialized sorbents for phospholipid capture | Particularly valuable for plasma/serum |
| Quality Control Matrices | Method assessment | Include hemolyzed, lipemic, and lot-to-lot variations | Minimum 6 different lots recommended |
| Matrix-Matched Calibration Standards | Calibration compensation | Prepared in blank matrix | Requires analyte-free matrix |
| Post-Column Infusion System | Matrix effect mapping | Syringe pump and T-connector | Qualitative but highly informative |
Method Validation Considerations
Incorporating Matrix Effect Assessment into Validation Protocols
Regulatory guidelines including ICH M10 mandate rigorous assessment of matrix effects during bioanalytical method validation [42]. The following approaches should be incorporated:
Multi-lot Matrix Evaluation: Analyze quality control samples prepared in at least six different lots of matrix, including any potentially problematic matrices (hemolyzed, lipemic) [42]. Acceptance criteria typically require accuracy within ±15% and CV ≤15% for each individual matrix source [42].
Internal Standard Tracking: Monitor internal standard responses during sample analysis to identify abnormal matrix effects in individual samples [42]. Samples with aberrant IS responses should be reanalyzed with dilution to confirm result reliability [42].
Matrix Factor Determination: For LC-MS/MS methods, calculate both absolute and IS-normalized matrix factors across the calibration range to quantify matrix effects and verify adequate compensation [42].
Strategic Method Selection Framework
When selecting a comparative method for validation research, consider the following decision framework:
For regulated bioanalysis: Prioritize approaches incorporating SIL-IS with thorough matrix effect assessment across multiple lots, as mandated by regulatory guidelines [42].
For high-throughput environments: Balance mitigation effectiveness with practical considerations, potentially employing dilution with sufficient sensitivity headroom [40].
For non-targeted analysis: Implement advanced normalization strategies like Individual Sample-Matched Internal Standards (IS-MIS) for heterogeneous samples [46].
For resource-limited settings: Focus on chromatographic optimization as a cost-effective primary strategy, supplemented by structural analogue internal standards when necessary [43].
The following diagram illustrates the relationship between different mitigation strategies and their application contexts:
Matrix effects present a formidable challenge in the analysis of complex samples, directly impacting the selection and validation of robust analytical methods. A systematic approach encompassing thorough assessment, strategic mitigation, and appropriate correction is essential for generating reliable data in drug development research. The most effective strategies combine multiple complementary approaches—judicious sample preparation, chromatographic optimization, and isotope-labeled internal standardization—tailored to the specific analytical requirements and sample characteristics.
For method validation research, the comprehensive evaluation of matrix effects across multiple matrix lots provides critical data for comparative method selection. By implementing the protocols and strategies outlined in this technical guide, researchers and drug development professionals can make informed decisions that ensure methodological robustness, regulatory compliance, and ultimately, the generation of scientifically sound analytical data.
Mitigating Risks from Insufficient Sample Size or Narrow Concentration Range
Selecting a comparative method for validation research is a cornerstone of analytical science, particularly in regulated industries like pharmaceutical development. The reliability of this comparison hinges on two fundamental design parameters: sample size and the concentration range of the samples tested. Failures in either parameter introduce significant risk, leading to models that are unstable, inaccurate, or unfit for their intended purpose.
Evidence suggests that insufficient sample size is a widespread problem. A 2023 systematic review found that 73% of studies developing clinical prediction models used sample sizes lower than the minimum required to estimate overall risk and minimize overfitting [47]. Furthermore, just 8% of the included studies provided any sample size justification, indicating a critical gap in methodological rigor [47]. Similarly, in external validation studies for prognostic models, sample sizes are often clearly inadequate, leading to "exaggerated and misleading performance" [48]. These deficiencies underscore the necessity of a principled approach to study design to mitigate the risks of unreliable results and to ensure that a method is truly fit for purpose.
Risks of an Inadequate Study Design
Consequences of Insufficient Sample Size
An inadequately small sample size jeopardizes the entire validation endeavor, primarily through overfitting and imprecise estimation. Overfitting occurs when a model describes the random noise in the specific sample rather than the underlying relationship that holds in the broader population. While shrinkage methods like LASSO can mitigate overfitting, they are not a panacea; the shrinkage parameters themselves are estimated with uncertainty when the sample size is small, still leading to unreliable models [47].
The second major consequence is imprecise estimation. Small samples yield estimates of performance measures—such as the c-statistic, calibration slope, or bias—with unacceptably wide confidence intervals. This imprecision makes it impossible to draw meaningful conclusions about the model's predictive accuracy in the target population [48]. For example, a study might report a seemingly high c-index, but if this estimate is based on only a handful of outcome events, the confidence interval will be so wide that the result is practically useless and potentially highly misleading [48].
Consequences of a Narrow Concentration Range
The concentration range of the samples used in a method-comparison study must reflect the entire range of values expected in routine practice. A narrow range poses a direct threat to the assessment of the method's linearity and its ability to detect constant and proportional bias.
A method may perform well within a limited, "easy" range but fail to provide accurate results at clinically critical decision levels, such as near the lower limit of quantitation (LLOQ) or at high concentrations. Consequently, the method's reportable range—the span of concentrations between the lowest and highest results that can be reliably reported without dilution—remains unverified [49]. Using a narrow range prevents a proper evaluation of the method's robustness across the full scope of its intended use, leaving the risk of reporting erroneous results for patient samples that fall outside the validated range.
Establishing a Risk-Based Framework: AQbD Principles
A proactive, systematic approach to method development and validation, known as Analytical Quality by Design (AQbD), is the most effective strategy for mitigating the risks associated with poor study design. In contrast to the unstructured "trial-and-error" or "one-factor-at-a-time" (OFAT) approach, AQbD builds quality and robustness into the method from the very beginning [50].
The core of AQbD is a deep, science-based understanding of the method, facilitated by risk assessment and multivariate experimentation. The workflow begins by defining an Analytical Target Profile (ATP), which is a predefined objective that outlines the required quality of the analytical results. The critical method attributes (CMAs—e.g., accuracy, precision) that fulfill the ATP are identified, and the critical method parameters (CMPs—e.g., pH, temperature, flow rate) that can impact the CMAs are assessed for risk [50].
Using Design of Experiments (DoE), the relationships between CMPs and CMAs are modeled. This allows for the computation of a Method Operability Design Region (MODR), a multidimensional space of method parameters where the quality criteria are met with a known level of confidence [50]. Operating within the MODR provides flexibility and ensures method robustness, as the impact of small, deliberate variations is understood and controlled from the outset.
The following diagram illustrates this iterative, knowledge-driven lifecycle of a method developed under AQbD principles.
Quantitative Guidance for Sample Size
Sample Size for Model Development and External Validation
Rigorous, a priori sample size calculation is non-negotiable for producing reliable models. For studies developing a prediction model for a binary outcome using logistic regression, the approach by Riley et al. is recommended. This calculation ensures sufficient sample size to meet three key criteria: minimizing overfitting, ensuring precise estimate of the model's explained variation (R²), and precise estimation of the average outcome risk [47]. The required information and typical values are summarized in the table below.
Table 1: Key Parameters for Sample Size Calculation in Model Development (Riley et al. approach)
| Parameter | Description | How to Determine |
|---|---|---|
| Number of Candidate Predictor Parameters (p) | The total number of regression coefficients to be estimated in the model. | Count all predictors, including terms for categorical variables and interactions. |
| Expected Outcome Proportion (E) | The prevalence of the event of interest in the development dataset. | Based on prior literature or pilot data. |
| Anticipated Cox-Snell R² | The expected proportion of variance explained by the model. | Can be approximated from the anticipated c-statistic (C) using: R² ≈ (C/0.9)â°Â·âµ - 1 [47]. |
| Target Shrinkage | The desired degree of penalization to reduce overfitting (e.g., 0.90 or 0.95). | Typically set to 0.90 for a 10% shrinkage [47]. |
For the external validation of an existing prognostic model, the focus shifts to precise estimation of performance measures like the c-index and calibration. A resampling study recommends a minimum of 100 events and ideally 200 or more to achieve unbiased and precise estimation of these metrics [48]. It is critical to note that the outdated rule of thumb of "10 events per variable" (10 EPV) is cautioned against, as it lacks a solid rationale and fails to consider the overall performance of the prediction model [47].
Sample Size and Range for Method-Comparison Studies
The design of a method-comparison study requires careful consideration of both the number of samples and the range of concentrations they cover.
- Number of Paired Measurements: The sample size (number of paired measurements) must be sufficient to decrease the likelihood of chance findings. The number of subjects and measurements should be determined a priori using power, alpha, and the smallest difference between methods that would be considered clinically important (effect size) [23]. An adequate sample size is especially crucial when the hypothesized outcome is "no difference," as a small sample may lead to a false conclusion of equivalence.
- Concentration Range: The samples must span the entire reportable range of the method, from the lowest to the highest concentration that the method is intended to measure [49]. The range of values in the study should cover the full spectrum of physiological and pathological conditions for which the method will be used [23]. Using a narrow range can lead to a false sense of agreement between methods, as potential proportional bias may remain undetected.
Table 2: Key Design Considerations for a Method-Comparison Study
| Design Aspect | Consideration | Rationale |
|---|---|---|
| Sample Size (N) | Calculate based on power, alpha, and a clinically important difference [23]. | Ensures precision and reduces the risk of falsely concluding equivalence. |
| Concentration Range | Should cover the full reportable range, including clinically critical decision levels [49]. | Ensures the method is validated across all intended uses and allows detection of proportional bias. |
| Sample Type | Use real patient samples. | Reflects the true matrix and the variety of endogenous components that will be encountered. |
| Timing | Simultaneous or near-simultaneous measurement of the same sample by both methods [23]. | Prevents real changes in the analyte from being misinterpreted as a difference between methods. |
Experimental Protocols for Robust Comparison
Protocol for a Method-Comparison Experiment
A well-defined protocol is essential for generating reliable data from a method-comparison study.
- Sample Selection and Preparation: Select N patient samples that cover the full reportable range. The samples should be as close to the native patient material as possible. If stabilization or processing is required, it must be applied uniformly.
- Measurement Order: Analyze each sample using both the test method and the comparison method. The order of analysis should be randomized to avoid systematic bias due to instrument drift or sample degradation over time [23].
- Data Collection: For each sample, record the paired result (Test Result, Comparison Method Result). A minimum of 40 samples is often a starting point, but the final number should be justified by a proper sample size calculation.
- Data Analysis and Interpretation:
- Visual Inspection: Create a Bland-Altman plot (difference vs. average plot) to visualize the agreement and check for trends in the differences across the concentration range [23] [49].
- Statistical Analysis: Use regression analysis to quantify systematic error. Ordinary least squares regression is insufficient as it assumes no error in the x-variable. Deming regression or similar techniques that account for error in both methods are preferred [49]. The slope represents proportional bias, and the intercept represents constant bias.
The following workflow outlines the key stages of this experimental process.
Protocol for Determining Reportable Range (Linearity)
This experiment validates the range over which the method provides results that are directly proportional to the concentration of the analyte.
- Sample Preparation: Prepare a set of 5-10 samples with known concentrations by serially diluting a high-concentration stock solution with an appropriate matrix. The concentrations must bracket the expected range from the lowest to the highest reportable value [51].
- Analysis: Analyze each sample in duplicate or triplicate.
- Data Analysis: Plot the measured response against the known theoretical concentration.
- Assessment: Visually and statistically evaluate the linearity. The plot should be inspected for indications of nonlinearity. A statistical analysis of the regression line, including the correlation coefficient, y-intercept, slope, and residual sum of squares, should be performed [51]. The method's response is considered linear if the relationship is visually linear and the residuals are randomly scattered.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Method Validation Studies
| Item | Function in Validation |
|---|---|
| Primary Standard | A highly purified and characterized compound used to establish a calibration curve with known accuracy. Serves as a reference for evaluating the test method's trueness [49]. |
| Commercial Calibrators | Ready-to-use solutions with assigned values. Used to calibrate the instrument under routine service conditions. Should be compared against primary standards [49]. |
| Quality Control (QC) Materials | Stable materials with known or assigned concentrations at multiple levels (e.g., low, medium, high). Used in replication experiments to validate precision (imprecision) across the reportable range [49]. |
| Interference Kit | Solutions of common endogenous substances (e.g., bilirubin, hemoglobin) and exogenous substances (e.g., common medications). Used to systematically test and validate the method's specificity by spiking into samples [49]. |
| Appropriate Biological Matrix | The base material (e.g., human plasma, serum, urine) that matches the patient sample type. Used to prepare linearity, QC, and recovery samples to ensure the validation reflects the real-world matrix effects [49]. |
Mitigating the risks of insufficient sample size and narrow concentration range is not merely a statistical formality but a fundamental requirement for generating trustworthy analytical methods. The consequences of neglect—overfitted models, imprecise estimates, and undetected biases—severely compromise the utility and safety of a method in patient care or product quality control.
Adopting a risk-based framework like AQbD, which prioritizes deep method understanding and proactive risk management, provides a structured path to robustness. By combining this with rigorous, a priori sample size calculations and experimental protocols that stress-test the method across its entire intended operating range, researchers and drug development professionals can ensure their comparative method validation studies yield reliable, defensible, and fit-for-purpose results.
Interpreting Proportional vs. Constant Systematic Error from Regression Analysis
In the context of method validation research, the selection of a comparative method is a critical decision that directly impacts the assessment of a new method's accuracy. The core objective of a comparison of methods experiment is to estimate the inaccuracy or systematic error present in a new test method by comparing its performance against a established comparative method [1]. Systematic errors, unlike random errors, are consistent inaccuracies that can significantly skew results and lead to incorrect conclusions if not properly identified and quantified [52]. Through regression analysis—a foundational statistical technique for modeling relationships between variables—these systematic errors can be not only detected but also characterized as either constant or proportional in nature [53]. This distinction is vital for researchers, scientists, and drug development professionals, as it directly informs the troubleshooting process, guides improvements in method development, and provides a scientific basis for selecting the most accurate and reliable comparative method for validation studies. A well-characterized method ensures the integrity of data supporting drug development and patient care.
Theoretical Foundations of Systematic Error
Defining Constant and Proportional Error
Systematic errors introduce a consistent bias into measurements, and understanding their specific form is essential for accurate method validation.
Constant Systematic Error (CE): This error, also known as constant bias, represents a fixed discrepancy that does not change with the concentration of the analyte [53] [54]. It is independent of the measurement value; whether the sample concentration is high or low, the absolute amount of the error remains the same. In a regression model, this type of error is associated with the y-intercept [53]. Graphically, a constant error manifests as a vertical shift of the regression line away from the origin, meaning the line does not pass through the point (0,0) [54]. This is often due to issues such as inadequate blanking, a miscalibrated zero point, or a specific interference in the assay that adds a constant amount to the reading [53].
Proportional Systematic Error (PE): This error, in contrast, is dependent on the concentration of the analyte [53] [54]. Its magnitude increases (or decreases) in direct proportion to the analyte level. In regression analysis, proportional error is revealed by a deviation of the slope from the ideal value of 1.00 [53]. On a graph, it appears as a change in the steepness or angle of the regression line compared to the line of perfect agreement [54]. This type of error is frequently caused by problems in calibration, standardization, or a matrix effect that compromises the proportionality of the analytical response [53].
Overall Systematic Error (SE) or Bias: The total systematic error at any given medical decision concentration is the combined effect of both the constant and proportional errors. It represents the overall bias between the test method and the comparative method at a specific concentration of interest [53].
Table 1: Summary of Systematic Error Types
| Error Type | Source in Regression | Manifestation | Common Causes |
|---|---|---|---|
| Constant Error (CE) | Y-Intercept (a) |
Fixed value is added/subtracted regardless of concentration. | Inadequate blanking, matrix interference, mis-set zero calibration. |
| Proportional Error (PE) | Slope (b) |
Error increases/decreases as a percentage of the concentration. | Poor calibration, erroneous standardization, matrix effect. |
| Overall Systematic Error (SE) | Combination of a and b |
The total difference between methods at a specific concentration. | The combined effect of constant and proportional factors. |
The Role of Regression Analysis in Method Comparison
Regression analysis serves as a powerful tool to deconstruct the relationship between two methods. The simple linear regression model, Y = a + bX, is commonly used, where Y is the result from the test method, X is the result from the comparative method, b is the slope, and a is the y-intercept [55].
- Ideal Method Agreement: If two methods are in perfect agreement, the regression line should have a slope (
b) of 1.00 and a y-intercept (a) of 0.0 [53]. This represents a 1:1 relationship across the measuring range. - Estimating Error at Decision Levels: A key advantage of regression is the ability to estimate the total systematic error (
SE) at critical medical decision concentrations (X_c). The error is calculated asSE = Y_c - X_c, whereY_cis the value predicted by the regression equation (a + bX_c) [53] [1]. This is crucial because a method may show negligible bias at the mean of the data but clinically significant errors at diagnostically important thresholds [53].
Experimental Protocol for Method Comparison
A rigorously designed experiment is fundamental to obtaining reliable estimates of systematic error.
Experimental Design and Data Collection
The quality of the regression analysis is contingent on the quality of the data collected. Key design considerations include:
- Number of Specimens: A minimum of 40 different patient specimens is recommended, with the quality and range of concentrations being more critical than the sheer number. Specimens should cover the entire working range of the method [1]. Larger numbers (100-200) are beneficial for assessing method specificity [1].
- Specimen Analysis: Specimens should be analyzed over a minimum of 5 days to capture routine sources of variation, though extending the study over 20 days (aligning with a precision study) is preferable [1].
- Replication: While single measurements are common, duplicate measurements on separate aliquots are advantageous. They help identify sample mix-ups, transposition errors, and confirm the repeatability of discrepant results [1].
- Specimen Stability: Specimens should be analyzed by both methods within two hours of each other unless stability data supports a longer interval. Proper handling (e.g., refrigeration, freezing, preservatives) is essential to prevent stability-related biases [1].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions and Materials for Method Comparison
| Item | Function in Experiment |
|---|---|
| Patient-Derived Specimens | Serves as the test matrix for comparison; should cover the analytical measurement range and represent the expected pathological spectrum. |
| Comparative Method Reagents | The consumables (calibrators, controls, enzymes, antibodies, buffers) required to perform the analysis on the established comparative method. |
| Test Method Reagents | The consumables specific to the new method being validated. |
| Quality Control Materials | Used to monitor the stability and performance of both the test and comparative methods throughout the experiment. |
| Calibrators | Essential for establishing the analytical calibration curve for both methods; traceability to reference materials is critical. |
Data Analysis and Interpretation
Graphical and Statistical Analysis
A robust data analysis strategy involves both visual and numerical techniques.
- Graphical Inspection: The first step is to create a difference plot (test result minus comparative result vs. comparative result) or a comparison plot (test result vs. comparative result) [1]. These plots provide a visual impression of the data, revealing the overall agreement, the presence of outliers, and potential patterns of constant or proportional error [1].
- Statistical Calculations:
- Linear Regression: For data covering a wide analytical range, calculate the slope (
b), y-intercept (a), and the standard error of the estimate (s_y/x) [53] [1]. - Correlation Coefficient (
r): While often reported, thervalue is primarily useful for verifying that the data range is sufficiently wide to provide reliable estimates of slope and intercept. Anrvalue ≥ 0.99 is generally considered adequate for this purpose [53] [1]. - Bias from t-test: For a narrow analytical range, the average difference (bias) between paired results, often derived from a paired t-test, is a more appropriate measure of systematic error [1].
- Linear Regression: For data covering a wide analytical range, calculate the slope (
Interpreting Regression Parameters for Systematic Error
The statistical outputs from regression must be interpreted through the lens of method validation.
- Assessing the Y-Intercept for Constant Error: The observed y-intercept (
a) should be tested to see if it is statistically significantly different from zero. This is typically done by evaluating its confidence interval or performing a t-test [53] [56]. If the confidence interval for the intercept does not include zero, it provides evidence of a constant systematic error [53]. However, as noted in [57], the constant term also serves to ensure the residuals have a mean of zero, so it should almost always be included in the model even if its direct interpretation is not meaningful. - Assessing the Slope for Proportional Error: Similarly, the observed slope (
b) should be tested to see if it is statistically significantly different from 1.00. If the confidence interval for the slope does not include the ideal value of 1.00, it indicates the presence of a proportional systematic error [53]. - Quantifying Total Systematic Error: As previously mentioned, the total systematic error at a critical medical decision level
X_cis calculated asSE = Y_c - X_c, whereY_c = a + b * X_c[53] [1]. This is the most clinically relevant estimate of bias.
Implications for Comparative Method Selection
The identification and characterization of systematic errors directly inform the selection of a comparative method within a validation thesis.
- A Framework for Decision-Making: The primary goal is to select a method that demonstrates minimal and clinically acceptable systematic error. The process of interpreting regression output provides a structured framework for this decision. A method showing statistically and clinically insignificant constant and proportional error (i.e., a slope CI containing 1.0 and an intercept CI containing 0.0) is a strong candidate.
- Prioritizing Error Type for Your Context: The nature of the systematic error can guide the selection based on the clinical or analytical application. For example, a method with a small, stable constant error might be acceptable if medical decisions are made far from the zero point, whereas a proportional error could be more detrimental across the entire range. The calculated total error (
SE) at specific decision levels is the ultimate metric for acceptability. - Hierarchy of Method Quality: The highest standard for a comparative method is a reference method, whose correctness is well-documented through definitive methods and traceable standards. In this case, any observed error is confidently attributed to the test method [1]. More commonly, a routine method is used as a comparative method. When differences are large, additional experiments (e.g., recovery, interference) are needed to determine which method is at fault [1]. Therefore, selecting a method with a proven track record of accuracy (e.g., a method traceable to a higher-order standard) strengthens the validation.
In conclusion, the interpretation of proportional and constant systematic error via regression analysis is not merely a statistical exercise. It is a critical, interpretative process that provides deep insight into the performance characteristics of an analytical method. This process enables informed, defensible decisions in the selection of a comparative method, ultimately ensuring that method validation research yields accurate, reliable, and clinically relevant results.
Strategies for When a Perfect Reference Method is Unavailable
In method validation research, the ideal scenario of a perfect reference standard or "gold-standard" method is often a luxury. More frequently, researchers and drug development professionals must select a comparative method whose correctness is not definitively documented [1] [58]. This guide outlines strategic approaches for these common situations, where the objective is to validate a new (test) method against a non-reference comparative method. The core challenge lies in designing a study and interpreting results in a way that the observed differences between methods can be correctly attributed, providing a reliable estimate of the new method's inaccuracy or systematic error [1].
Selecting an Appropriate Comparative Method
The selection of the comparative method is the most critical decision, as it forms the basis for all subsequent conclusions about the test method's performance.
Defining Comparator Types
A "reference method" is a specifically defined term, implying a method of high quality whose results are known to be correct through documented traceability to definitive methods or standard reference materials [1] [59]. In the context of dietary supplements and natural products, for example, the use of matrix-based reference materials is crucial for assessing the accuracy, precision, and sensitivity of analytical measurements [59]. In contrast, a "comparative method" is a more general term for a routine method whose correctness is assumed but not fully documented [1]. Most laboratory methods fall into this category.
Strategic Selection Framework
When a perfect reference is unavailable, the goal shifts to selecting the best available comparator. The following table summarizes the key considerations for different types of comparative methods.
Table 1: Strategies for Selecting a Comparative Method in the Absence of a Perfect Reference
| Comparator Type | Description | Key Strategic Considerations |
|---|---|---|
| Established Routine Method | A well-characterized, stable method currently in use within the laboratory. | Assess its precision and long-term performance data. A method with low imprecision is preferable, as observed differences are more likely to originate from the test method [1] [5]. |
| Method of Higher Order | A method with a better-documented calibration traceability or a more specific analytical principle. | Favor a method that uses a different analytical principle than the test method. This helps ensure that any sample-specific interferences affect the methods differently, making them easier to detect [1]. |
| Composite Reference | A value derived from multiple methods or the consensus of several laboratories. | Using the average result from multiple instruments or methods as the reference value can provide a better estimation of the test method's bias by averaging out individual instrument errors [5]. |
The following diagram illustrates the logical decision process for selecting a comparative method.
Designing the Comparison of Methods Experiment
A robust experimental design is essential to minimize ambiguity when interpreting differences between the test and comparative methods.
Specimen Selection and Handling
The quality of specimens is more critical than sheer quantity. A minimum of 40 different patient specimens is recommended, selected to cover the entire working range of the method and represent the spectrum of diseases expected in its routine application [1]. Twenty carefully selected specimens covering a wide concentration range often provide better information than one hundred random specimens.
- Number of Specimens: For a wide analytical range (e.g., glucose), aim for 40-100 specimens to ensure a good distribution. To specifically assess a method's specificity against interferences, larger numbers (100-200) are recommended [1].
- Stability and Handling: Analyze specimens by both methods within two hours of each other, unless specific stability data indicate a shorter window. Define and systematize specimen handling (e.g., refrigeration, freezing, preservatives) prior to the study to prevent handling-related differences from being misattributed as analytical error [1].
Data Collection Protocol
The data collection phase should be designed to capture realistic, long-term performance of the methods.
- Replication: While analyzing each specimen singly by both methods is common practice, performing duplicate measurements on different samples or in different analytical runs provides a check for sample mix-ups, transposition errors, and other mistakes. If duplicates are not performed, inspect results as they are collected and immediately reanalyze specimens with large discrepancies [1].
- Time Period: Conduct the experiment over several different analytical runs on different days to minimize the impact of systematic errors from a single run. A minimum of 5 days is recommended, and extending the study over a longer period (e.g., 20 days) while analyzing only 2-5 specimens per day integrates long-term performance assessment [1].
The following workflow diagram maps out the key stages of the experimental protocol.
Data Analysis and Interpretation
The analysis phase must accurately quantify and attribute the observed differences between the two methods.
Graphical Analysis
Graphing the data is a fundamental first step for visual inspection. The two primary types of graphs are:
- Difference Plot: The difference between the test and comparative results (test - comparative) is plotted on the y-axis against the comparative result on the x-axis. This is ideal when the methods are expected to show one-to-one agreement. The data should scatter randomly around the zero line, allowing easy visualization of constant or proportional biases [1].
- Comparison Plot (Scatter Plot): The test result is plotted on the y-axis against the comparative result on the x-axis. This is used when methods are not expected to agree one-to-one (e.g., different enzyme assays). A visual line of best fit shows the general relationship [1].
Statistical Analysis and Quantifying Systematic Error
Statistical calculations provide numerical estimates of systematic error. The choice of statistic depends on the analytical range of the data and the nature of the methods being compared.
Table 2: Statistical Methods for Quantifying Systematic Error in Method Comparison
| Statistical Method | Application Context | Calculation and Interpretation |
|---|---|---|
| Linear Regression | Preferred for data covering a wide analytical range (e.g., cholesterol). | Calculates the slope (b) and y-intercept (a) of the line of best fit (Y = a + bX). Systematic error (SE) at a medical decision concentration (Xc) is: Yc = a + b*Xc; SE = Yc - Xc. The slope indicates proportional error, and the y-intercept indicates constant error [1]. |
| Mean Difference (Bias) | Used for data with a narrow analytical range (e.g., sodium, calcium). | The average difference between the test and comparative results. It is typically calculated via a paired t-test, which also provides the standard deviation of the differences and a t-value to assess if the bias is statistically significant [1] [5]. |
| Sample-Specific Differences | Useful for small comparison studies (e.g., <10 samples) or when monitoring External Quality Assessment (EQA) samples. | Examines the difference for each sample individually. The overview report shows the smallest and largest sample-specific difference, and each sample is expected to be within pre-defined goals [5]. |
When the comparative method is not a reference method, the Bland-Altman difference (where the mean difference is plotted against the average of the two methods) is often the recommended way to estimate the bias of the candidate method, as it does not assume one method is correct [5].
Interpreting Discrepant Results
When large, medically unacceptable differences are observed, careful interpretation is required. It cannot be automatically assumed that the error lies with the test method. Additional experiments, such as recovery and interference studies, may be necessary to identify which method is inaccurate and to understand the source of the discrepancy [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials required for conducting a rigorous method comparison study.
Table 3: Essential Research Reagents and Materials for Method Validation Studies
| Item | Function and Importance |
|---|---|
| Well-Characterized Patient Specimens | The foundation of the study. Specimens must be matrix-matched to routine samples and cover the entire measuring range to properly evaluate method performance across all clinically relevant concentrations [1]. |
| Matrix-Based Reference Materials | Certified reference materials with a matrix similar to the study specimens (e.g., human serum). They are used to assess the accuracy, precision, and sensitivity of analytical measurements and to validate the performance of the comparative method [59]. |
| Quality Control (QC) Materials | Stable control materials at multiple concentration levels are analyzed concurrently throughout the study to monitor the stability and performance of both the test and comparative methods, ensuring data integrity [1]. |
| Reagent Lots | For reagent lot comparisons, distinct lots are defined as separate items in the study plan. Using the lot identifier from the instrument export file allows for automatic sorting of results in the validation software [5]. |
| Data Analysis Software | Software capable of performing statistical analyses (linear regression, paired t-tests, Bland-Altman) and generating difference and comparison plots is essential for objective, reproducible data analysis [1] [5]. |
Leveraging Modern Validation Paradigms and Lifecycle Management
Integrating Quality by Design (QbD) Principles into Method Selection
The selection of a comparative method for method validation research is a critical step that directly impacts the reliability of data and the success of pharmaceutical development. The traditional approach to analytical method development often involves a sequential, one-factor-at-a-time (OFAT) process, which can be time-consuming, resource-intensive, and may lack reproducibility and robustness [60] [61]. In contrast, Quality by Design (QbD) represents a systematic, proactive, and risk-based framework for ensuring that quality is built into analytical methods from their inception. When applied to method selection, QbD principles shift the paradigm from simply finding a "workable" method to designing a robust, fit-for-purpose analytical procedure that consistently delivers reliable results throughout its lifecycle [62] [63].
According to the International Council for Harmonisation (ICH), QbD is formally defined as "a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management" [63]. The extension of these principles to analytical methods, known as Analytical Quality by Design (AQbD), has gained significant traction in the pharmaceutical industry over the past decade, with regulatory agencies such as the FDA and EMA actively encouraging its implementation [63] [60]. For researchers selecting a comparative method for validation studies, adopting an AQbD approach ensures the chosen method will not only meet immediate analytical needs but will also remain reliable and adaptable to future changes in the product or process.
Core Principles of Analytical QbD
The Analytical Procedure Lifecycle
Analytical QbD redefines the method development and selection process as an integrated lifecycle, in contrast to the discrete, sequential stages of traditional approaches. This lifecycle perspective, now formalized in regulatory guidelines such as ICH Q14 and USP <1220>, emphasizes continuous verification and improvement, ensuring the method remains fit-for-purpose long after its initial validation [63] [25]. The traditional approach to method transfer represents a one-off evaluation that may not provide a high level of assurance of long-term method reliability, potentially leading to method failure months after transfer [62]. In contrast, the AQbD lifecycle encompasses three interconnected stages:
- Stage 1: Design and Development – This initial stage focuses on establishing the Analytical Target Profile (ATP), identifying Critical Method Attributes (CMAs), and conducting risk assessment to pinpoint Critical Method Parameters (CMPs). Method selection and optimization are performed using structured experimentation, primarily Design of Experiments (DoE), to define a Method Operable Design Region (MODR) [63].
- Stage 2: Performance Qualification – This stage demonstrates that the selected method, when operated within the MODR, consistently meets the criteria outlined in the ATP. It corresponds to the traditional method validation but with enhanced understanding of method capabilities and limitations [63].
- Stage 3: Ongoing Performance Verification – Throughout the method's routine use, its performance is continuously monitored through risk-based verification to ensure it remains in a state of control. This allows for proactive management of method changes over time [63].
This lifecycle management enables continuous improvement and facilitates regulatory flexibility for method adjustments within the established design space without requiring extensive revalidation [60] [25].
Key Terminology and Definitions
A clear understanding of AQbD-specific terminology is essential for proper implementation when selecting a comparative method:
- Analytical Target Profile (ATP): A prospective summary of the analytical procedure's requirements that defines the quality of the reportable value needed for its intended purpose. The ATP specifies the measurement quality needed (e.g., precision, accuracy) but not the specific technique to achieve it [60] [25].
- Critical Method Attributes (CMAs): These are the output performance characteristics of the method that are critical for ensuring the procedure meets the ATP. Examples include resolution, tailing factor, and theoretical plates in chromatographic methods [64] [60].
- Critical Method Parameters (CMPs): These are the input variables of the method that significantly impact the CMAs. For an HPLC method, these typically include mobile phase composition, column temperature, flow rate, and pH [65] [60].
- Method Operable Design Region (MODR): The multidimensional combination and interaction of CMPs that have been demonstrated to provide assurance that the method will meet the ATP requirements. Operating within the MODR provides built-in robustness against small, intentional variations in method parameters [60] [61].
- Risk Assessment: A systematic process for identifying, analyzing, and evaluating risks associated with method variables. Tools such as Fishbone (Ishikawa) diagrams and Failure Mode Effect Analysis (FMEA) are commonly used to prioritize factors for experimental investigation [62] [60].
The following table summarizes these key AQbD elements and their significance in method selection:
Table 1: Core Elements of Analytical QbD and Their Role in Method Selection
| AQbD Element | Definition | Role in Method Selection |
|---|---|---|
| Analytical Target Profile (ATP) | Predefined objectives for method performance | Serves as the primary reference for evaluating candidate methods against required quality standards |
| Critical Method Attributes (CMAs) | Key output performance characteristics critical for quality | Provides measurable criteria for comparing method performance during selection |
| Critical Method Parameters (CMPs) | Input variables that significantly impact CMAs | Identifies which parameters require tight control in the selected method |
| Method Operable Design Region (MODR) | Multidimensional space of CMPs where method meets ATP | Defines the operational flexibility of the selected method |
| Control Strategy | Planned set of controls derived from risk management | Ensures selected method maintains performance throughout its lifecycle |
The AQbD Workflow for Method Selection
Defining the Analytical Target Profile (ATP)
The foundation of QbD-based method selection is establishing a clear and comprehensive Analytical Target Profile. The ATP translates the analytical needs into specific, measurable performance requirements that will guide the selection and evaluation of potential methods [60] [25]. Rather than specifying a particular technique or technology at the outset, the ATP focuses on the quality of the measurement needed to support decision-making for the product or process.
When defining the ATP for selecting a comparative method, key considerations include:
- Analyte Characteristics: The chemical and physical properties of the target analyte, including stability, solubility, and chemical functionality, which influence suitable analytical techniques [63].
- Performance Requirements: Specific criteria for accuracy, precision, specificity, detection and quantification limits, and linearity range based on the intended use of the method. For instance, method variability (precision) should represent only a small proportion of the product specification range [62].
- Operational Intent: Practical requirements for the method's implementation, including analysis time, available equipment, skill requirements, and environmental considerations. These are often gathered through Voice of the Customer (VoC) analysis from quality control laboratories where the method will be routinely operated [62].
- Regulatory and Compliance Needs: Any specific regulatory requirements for the method, such as compliance with pharmacopeial standards or validation according to ICH Q2(R1) guidelines [65] [64].
A well-defined ATP provides the objective basis for evaluating and comparing potential methods, ensuring the selected approach is truly fit-for-purpose from both scientific and practical perspectives.
Risk Assessment and Factor Prioritization
Once the ATP is established, a systematic risk assessment is conducted to identify potential factors that could impact the method's ability to meet its target profile. This step is crucial for focusing method selection and development efforts on the most influential variables, thereby optimizing resource utilization [62] [60].
The risk assessment process typically involves:
- Method Mapping: Deconstructing the analytical procedure into discrete steps (e.g., sample preparation, dissolution, extraction, chromatographic separation, data analysis) to comprehensively identify potential variables at each stage [62].
- Cause-and-Effect Analysis: Using tools such as Fishbone (Ishikawa) diagrams to facilitate brainstorming of all potential factors that may influence method performance criteria. Major categories typically include instrument parameters, environmental conditions, analyst techniques, sample properties, and reagent characteristics [62] [60].
- Risk Prioritization: Employing semiquantitative tools such as Failure Mode Effects Analysis (FMEA) or a Risk Estimation Matrix (REM) to classify factors based on their potential impact, occurrence probability, and detectability [60]. Factors are typically categorized as:
- Control (C): Factors that should be fixed or controlled to eliminate variability
- Noise (N): Environmental or operational factors that cannot be practically controlled
- Experimental (X): Factors that require systematic investigation to determine their optimal ranges [62]
This risk-based approach ensures that method selection and optimization efforts focus on the high-impact factors that truly matter to method performance, rather than applying equal attention to all possible variables.
Experimental Design for Method Evaluation
At the heart of the AQbD approach to method selection is the use of Design of Experiments (DoE) to systematically evaluate candidate methods and their operating parameters. Unlike the traditional OFAT approach, which varies one factor at a time while holding others constant, DoE allows for efficient exploration of multiple factors and their interactions simultaneously [63] [60]. This provides a more comprehensive understanding of method behavior across a wide operational space.
Common experimental designs used in AQbD include:
- Screening Designs (e.g., Full Factorial, Plackett-Burman): Used in early evaluation stages to identify which of many potential factors have significant effects on method performance [66] [61].
- Response Surface Designs (e.g., Central Composite, Box-Behnken): Employed to model the relationship between critical factors and responses, enabling the definition of the Method Operable Design Region [65] [64].
For example, in developing an RP-HPLC method for Tafamidis Meglumine, researchers used a Box-Behnken design to evaluate three critical parameters (mobile phase composition, column temperature, and flow rate) and their effects on chromatographic responses (retention time, tailing factor, and theoretical plates) [65]. Similarly, in the development of a method for ceftriaxone sodium, a central composite design was applied to optimize mobile phase composition and pH while studying their effects on retention time, theoretical plates, and peak asymmetry [64].
The following workflow diagram illustrates the systematic AQbD approach to method selection and development:
Diagram 1: AQbD Method Development Workflow
Practical Implementation and Case Studies
Experimental Protocols for AQbD-Based Method Evaluation
Implementing AQbD for method selection requires structured experimental protocols that generate meaningful data for informed decision-making. The following protocols illustrate key experiments in the AQbD workflow:
Protocol 1: Risk Assessment Using Fishbone Diagram and FMEA
Purpose: To systematically identify and prioritize factors that may impact method performance.
Procedure:
- Assemble a cross-functional team including method developers, end-users, and subject matter experts [62].
- Conduct a method walk-through where all team members observe an analyst performing the method from start to finish in the intended environment [62].
- Construct a Fishbone (Ishikawa) diagram with main categories typically including Instrument/Equipment, Materials/Reagents, Analyst/Personnel, Environmental Conditions, Sample Properties, and Method Parameters [62] [60].
- Brainstorm potential factors under each category that could influence method performance criteria identified in the ATP.
- Perform Failure Mode Effects Analysis (FMEA) by rating each potential failure mode for Severity (S), Occurrence (O), and Detectability (D) on a scale of 1-10, then calculating Risk Priority Number (RPN = S × O × D) [62] [60].
- Prioritize factors based on RPN scores, with higher scores indicating greater risk and need for control or investigation.
Output: A prioritized list of factors categorized as Control (C), Noise (N), or Experimental (X) for further investigation [62].
Protocol 2: Method Operable Design Region (MODR) Definition Using DoE
Purpose: To define the multidimensional region where variations in Critical Method Parameters do not significantly affect method performance.
Procedure:
- Select critical factors identified from risk assessment for experimental investigation (X-factors).
- Choose an appropriate experimental design based on the number of factors and desired resolution. Box-Behnken or Central Composite designs are commonly used for response surface methodology [65] [64].
- Define response variables based on the ATP, such as resolution, tailing factor, theoretical plates, retention time, or accuracy [65] [66].
- Execute the experimental design with randomized run order to minimize bias.
- Analyze results using statistical methods such as multiple linear regression or partial least squares modeling to develop mathematical relationships between factors and responses.
- Generate contour plots or response surfaces for critical responses and overlay them to visualize the MODR where all responses meet acceptance criteria [61].
Output: A defined MODR with established proven acceptable ranges for Critical Method Parameters.
Case Studies in Pharmaceutical Analysis
Several recent applications demonstrate the successful implementation of AQbD for analytical method development and selection:
Case Study 1: Stability-Indicating RP-HPLC Method for Tafamidis Meglumine Researchers applied AQbD principles to develop and validate a stability-indicating RP-HPLC method for Tafamidis Meglumine in bulk drug and formulation. Using a Box-Behnken design, they systematically optimized three critical parameters: mobile phase composition, column temperature, and flow rate. The resulting method demonstrated excellent linearity (R² = 0.9998) over 2–12 µg/mL, high sensitivity (LOD 0.0236 µg/mL, LOQ 0.0717 µg/mL), and effective separation of degradation products under various stress conditions. The method achieved an AGREE score of 0.83, indicating high environmental sustainability and analytical reliability [65].
Case Study 2: HPLC Method for Ceftriaxone Sodium A QbD-based approach was employed to develop an HPLC method for ceftriaxone sodium in pharmaceutical dosage forms. A central composite design was used to optimize mobile phase composition and pH, studying their effects on retention time, theoretical plates, and peak asymmetry. The optimized method showed a retention time of 4.15 min, tailing factor of 1.49, and theoretical plates of 5236. Validation demonstrated excellent precision (%RSD < 2%) and accuracy (assay 99.73 ± 0.61%), confirming the method's robustness and suitability for its intended purpose [64].
Case Study 3: UPLC Method for Casirivimab and Imdevimab A recent study applied AQbD to develop an ultra-performance liquid chromatography method for simultaneous analysis of monoclonal antibodies casirivimab and imdevimab. Risk assessment identified critical parameters, which were then optimized using a Taguchi orthogonal array design. The method was validated showing excellent linearity (R² > 0.999), low detection limits, and good reproducibility (%RSD < 2%). The method was successfully applied to commercial formulation analysis and demonstrated minimal environmental impact through greenness assessment [66].
The Scientist's Toolkit: Essential Research Reagents and Materials
The implementation of AQbD requires specific reagents, materials, and software tools to support systematic method evaluation. The following table details key solutions used in AQbD-based method development:
Table 2: Essential Research Reagents and Materials for AQbD Implementation
| Category | Specific Examples | Function in AQbD |
|---|---|---|
| Chromatographic Columns | Qualisil BDS C18 [65], ACQUITY UPLC CSH C18 [61], Phenomenex ODS C18 [64] | Provide stationary phases with different selectivity for systematic screening of separation performance |
| Mobile Phase Modifiers | Ortho-phosphoric acid [65], formic acid [66] [61], triethylamine [64] | Adjust pH and ionic characteristics to optimize separation and peak shape |
| Organic Solvents | Acetonitrile, methanol [65] [61], ethanol [66] | Function as organic modifiers in reversed-phase chromatography; different selectivities are evaluated |
| DoE Software | Design Expert [64], Fusion AE [61] | Facilitate experimental design generation, data analysis, and visualization of design space |
| Risk Assessment Tools | FMEA templates [62], Ishikawa diagrams [60] | Systematically identify, analyze, and prioritize potential sources of method variability |
Method Comparability and Equivalency in QbD Framework
Demonstrating Method Comparability and Equivalency
In the context of AQbD, method selection often involves comparing a new or modified method against an established procedure. ICH Q14 provides a structured framework for assessing method comparability and equivalency, which is essential for making informed selection decisions and managing method changes throughout the analytical procedure lifecycle [25].
- Comparability evaluates whether a modified method yields results sufficiently similar to the original, ensuring consistent product quality. Comparability studies typically confirm that modified procedures produce expected results, and for low-risk changes with minimal impact on product quality, may not require regulatory filings [25].
- Equivalency involves a more comprehensive assessment to demonstrate that a replacement method performs equal to or better than the original. Such changes require regulatory approval prior to implementation and typically involve side-by-side testing of representative samples using both methods, statistical evaluation using tools such as paired t-tests or ANOVA, and predefined acceptance criteria based on method performance attributes and Critical Quality Attributes (CQAs) [25].
The following diagram illustrates the decision process for method changes under ICH Q14:
Diagram 2: Method Change Decision Process
Comparison of Methods Experiment
When selecting a comparative method for validation, a properly designed comparison of methods experiment is critical for assessing systematic errors that may occur with real patient specimens [1]. Key considerations for this experiment include:
- Comparative Method Selection: Ideally, a reference method with well-documented correctness should be used. When using a routine comparative method, large differences may require additional experiments to identify which method is inaccurate [1].
- Sample Selection: A minimum of 40 different patient specimens should be tested, selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application. Specimens should be analyzed within two hours of each other by both methods to minimize stability issues [1].
- Experimental Design: The comparison should include several different analytical runs on different days (minimum 5 days) to minimize systematic errors that might occur in a single run. Duplicate measurements are recommended to identify potential sample mix-ups or transposition errors [1].
- Data Analysis: Results should be graphed using difference plots or comparison plots to visually inspect for systematic errors and outliers. Statistical analysis using linear regression for wide analytical ranges or paired t-tests for narrow ranges provides numerical estimates of systematic error at medically important decision concentrations [1].
Benefits and Regulatory Implications
Advantages of AQbD in Method Selection
Adopting a QbD approach for method selection offers significant advantages over traditional approaches:
- Enhanced Method Robustness: By systematically evaluating the impact of method parameters and their interactions, AQbD identifies a Method Operable Design Region where the method remains reliable despite small, intentional variations [60] [61]. This built-in robustness reduces the incidence of out-of-trend (OOT) and out-of-specification (OOS) results during routine use [60].
- Regulatory Flexibility: Methods developed using AQbD principles provide greater understanding of method capabilities and limitations, creating opportunities for regulatory flexibility and continuous improvement throughout the method lifecycle without requiring revalidation [62] [60].
- Reduced Investigation Costs: The comprehensive understanding gained through AQbD reduces manufacturing resources involved with investigating OOS results and increases confidence in analysis testing cycle times [62].
- Knowledge Management: AQbD facilitates the capture and leverage of development data to inform future modifications and troubleshooting, creating a knowledge repository that benefits future method development efforts [25].
Regulatory Framework and Future Directions
The regulatory landscape for analytical methods has evolved significantly with the incorporation of AQbD principles. Key developments include:
- ICH Q14 Guidelines: The recent ICH Q14 guideline on Analytical Procedure Development provides a formalized framework for the creation, validation, and lifecycle management of analytical methods, encouraging a structured, risk-based approach [63] [25].
- USP <1220>: The United States Pharmacopeia general chapter <1220> on "Analytical Procedure Life Cycle" formally outlines requirements to guarantee the suitability of any analytical procedure throughout its entire lifecycle [63].
- Regulatory Acceptance: Leading regulatory bodies including the US FDA and European Medicines Agency have emphasized the importance of integrating AQbD into pharmaceutical quality systems [63]. Surveys indicate that the majority of pharmaceutical companies have incorporated AQbD to some extent, with large companies showing higher implementation ratios [63].
As the pharmaceutical industry continues to adopt AQbD, the approach is expected to become the standard for analytical method development and selection, driven by its demonstrated benefits in producing reliable, robust, and adaptable analytical procedures.
Integrating Quality by Design principles into method selection represents a fundamental shift from the traditional, empirical approach to a systematic, science- and risk-based paradigm. By beginning with a clear Analytical Target Profile, conducting thorough risk assessments, employing Design of Experiments, and defining a Method Operable Design Region, researchers can select comparative methods with greater confidence in their reliability and long-term performance. The structured framework provided by AQbD not only ensures methods are fit-for-purpose at the time of selection but also provides the flexibility to adapt to future changes throughout the analytical procedure lifecycle. As regulatory guidance continues to evolve with ICH Q14 and USP <1220>, adopting AQbD for method selection will become increasingly essential for pharmaceutical scientists committed to quality, efficiency, and innovation in analytical science.
Adopting a Risk-Based Approach to Focus on Critical Method Parameters
In the pharmaceutical quality control context, risk is formally defined as the combination of the probability of occurrence of harm and the severity of that harm [50]. The adoption of a risk-based approach for analytical method development represents a fundamental shift from traditional quality-by-testing (QbT) practices toward a more systematic, scientific framework. This paradigm, heavily influenced by ICH guidelines Q8(R2) and Q9, emphasizes building quality into methods from their inception rather than merely testing quality at the conclusion of development [50]. For researchers selecting a comparative method for validation studies, this risk-based framework provides a structured mechanism to identify and focus resources on the Critical Method Parameters (CMPs) that truly impact method performance and product quality.
The limitations of traditional QbT approaches, which typically employ one-factor-at-a-time (OFAT) investigations, are well-documented. Such unstructured approaches often require numerous experiments while providing limited information about variable interactions, potentially leading to false optimum conditions and incomplete risk understanding [50]. In contrast, Analytical Quality by Design (AQbD) incorporates prior knowledge, risk management, and structured experimental design throughout the analytical method lifecycle, delivering a comprehensive understanding of method parameters and their effects on Critical Method Attributes (CMAs) [50].
Foundational Principles of a Risk-Based Framework
Regulatory and Conceptual Basis
The risk-based approach is grounded in key regulatory documents, including the FDA's "Pharmaceutical cGMPs for the 21st Century - A Risk Based Approach" and the ICH Q9 guideline on quality risk management [50]. These documents clarify that risk management strategies are essential for ensuring quality in pharmaceutical processes, with quality control methods playing a pivotal role in overall quality assurance.
Within this framework, analytical methods are viewed as an integral part of the control strategy for drug manufacturing. They must be submitted to regulatory bodies in specific dossiers to support market authorization applications (MAA) [50]. The risk associated with method performance must be accurately assessed throughout all stages of the method lifecycle, which encompasses design, development, validation, control strategy, and continual improvement [50].
Key Terminology and Definitions
Critical Method Parameters (CMPs): Variables in the analytical procedure that have a significant impact on method performance and must be controlled within predetermined ranges to ensure the method meets its intended purpose.
Critical Method Attributes (CMAs): Key characteristics of the method that define its performance, such as accuracy, precision, specificity, and robustness.
Method Operability Design Region (MODR): A multidimensional region of method parameters where method performance meets predefined criteria with a known level of probability [50].
Analytical Target Profile (ATP): A prospective description of the required quality characteristics of the analytical method, defining its intended purpose and performance criteria.
Implementation Strategy: A Systematic Workflow
The AQbD Workflow for Comparative Method Selection
Implementing a risk-based approach follows a structured Analytical Quality by Design (AQbD) workflow that transforms method development from an empirical exercise to a systematic, knowledge-driven process. This workflow consists of six interconnected phases that guide the selection and validation of comparative methods.
Phase 1: Define the Analytical Target Profile (ATP)
The foundation of risk-based method development begins with clearly defining the Analytical Target Profile. The ATP represents a prospective description of the method's required quality characteristics, serving as the cornerstone for all subsequent development activities. When selecting a comparative method for validation studies, the ATP must explicitly state:
- The specific analytes to be measured and their expected concentration ranges
- The required accuracy and precision levels based on the method's intended use
- The necessary specificity requirements for the sample matrix
- The desired range, linearity, and robustness criteria
- Any regulatory or compliance requirements specific to the therapeutic area
The ATP should be developed through collaborative discussions among analytical scientists, quality assurance, and regulatory affairs professionals to ensure alignment with both scientific and business objectives.
Phase 2: Identify Critical Method Attributes (CMAs)
With the ATP defined, the next critical step involves identifying which method attributes are truly critical to ensuring the method fulfills its intended purpose. CMAs represent the bridge between the high-level requirements outlined in the ATP and the specific operational parameters that will be controlled during method execution.
Key CMAs typically include:
- Specificity/Selectivity: The ability to measure the analyte accurately in the presence of potential interferents
- Accuracy: The closeness of test results to the true value
- Precision: The degree of agreement among individual test results
- Detection and Quantitation Limits: The lowest amounts of analyte that can be detected or quantified
- Linearity and Range: The ability to obtain results proportional to analyte concentration
- Robustness: The capacity to remain unaffected by small, deliberate variations in method parameters
Phase 3: Risk Assessment and Parameter Ranking
The risk assessment phase represents the core of the risk-based approach, where potential sources of variability are systematically identified and evaluated. This process follows a structured methodology to distinguish Critical Method Parameters from non-critical parameters.
Risk Assessment Techniques
Several established methodologies can be employed for risk assessment in analytical method development:
- Failure Mode Effects Analysis (FMEA): A systematic approach for identifying potential failure modes, their causes, and effects
- Fishbone Diagrams: Visual tools for categorizing and exploring potential causes of method failure
- Risk Ranking and Filtering: A method for comparing risks against predefined criteria to prioritize them for control
Table: Risk Priority Number (RPN) Matrix for Method Parameter Assessment
| Parameter | Severity (1-10) | Occurrence (1-10) | Detection (1-10) | RPN | Criticality |
|---|---|---|---|---|---|
| Column Temperature | 8 | 6 | 4 | 192 | Critical |
| Mobile Phase pH | 9 | 5 | 3 | 135 | Critical |
| Flow Rate | 7 | 4 | 3 | 84 | Critical |
| Detection Wavelength | 6 | 3 | 2 | 36 | Non-Critical |
| Injection Volume | 5 | 2 | 2 | 20 | Non-Critical |
| Autosampler Temperature | 3 | 2 | 3 | 18 | Non-Critical |
Risk Assessment Tools and Templates
The risk assessment process can be facilitated through structured tools that document the relationship between method parameters and quality attributes.
Table: Risk Assessment Tool for Method Parameters
| Method Step | Parameter | CMA Impacted | Risk Level | Rationale | Mitigation Strategy |
|---|---|---|---|---|---|
| Sample Preparation | Extraction Time | Accuracy, Precision | High | Incomplete extraction affects recovery | DoE to establish proven acceptable range |
| Chromatographic Separation | Gradient Profile | Specificity, Resolution | High | Direct impact on peak separation | DoE to optimize and establish MODR |
| Detection | Wavelength | Specificity | Medium | Spectral interference possible | Verification with placebo samples |
| Data Processing | Integration Parameters | Precision | Low | Automated system with validation | System suitability controls |
Phase 4: Design of Experiments (DoE) for CMP Evaluation
Once CMPs are identified through risk assessment, Design of Experiments provides a structured, efficient approach to understanding parameter effects and interactions. Unlike OFAT approaches, DoE enables simultaneous variation of multiple parameters, revealing interaction effects while reducing the total number of experiments required.
DoE Selection Criteria
The selection of an appropriate experimental design depends on multiple factors:
- Screening Designs (e.g., Plackett-Burman, Fractional Factorial): Used when numerous potential factors require evaluation to identify the most significant ones
- Response Surface Methodology (e.g., Central Composite Design, Box-Behnken): Employed to optimize critical parameters and characterize their relationship with CMAs
- Mixture Designs: Appropriate when component proportions are the primary variables
- Full Factorial Designs: Used for comprehensive evaluation of all factor combinations when the number of factors is limited
DoE Implementation Protocol
A robust DoE implementation follows a structured protocol:
- Define Experimental Objectives: Clearly state what knowledge the experiment is intended to generate
- Select Factors and Ranges: Choose parameters and ranges based on risk assessment results and practical considerations
- Choose Experimental Design: Select the most appropriate design based on objectives, factors, and resources
- Randomize Run Order: Minimize the impact of uncontrolled variables through randomization
- Execute Experiments: Conduct experiments according to the design matrix, documenting any deviations
- Analyze Results: Use statistical methods to model relationships between parameters and responses
- Verify Model: Confirm model predictions through confirmatory experiments
Phase 5: Define the Method Operability Design Region (MODR)
The MODR represents the multidimensional combination of analytical procedure input variables and process parameters that have been demonstrated to provide assurance of quality [50]. Unlike a single setpoint approach, the MODR offers operational flexibility while maintaining method performance.
MODR Establishment Protocol
Establishing a MODR involves:
- Statistical Analysis of DoE Data: Developing mathematical models describing the relationship between CMPs and CMAs
- Response Surface Analysis: Visualizing the experimental space where CMA criteria are met
- Probability-Based Boundaries: Defining regions with an acceptable probability of meeting CMA targets
- Edge of Failure Determination: Identifying parameter boundaries where method performance becomes unacceptable
- Verification Experiments: Confirming MODR predictions through experiments at boundary conditions
Phase 6: Control Strategy and Lifecycle Management
The final phase involves implementing a control strategy to ensure the method remains in a state of control throughout its lifecycle. This includes:
- Procedural Controls: Standard operating procedures defining method execution
- System Suitability Tests: Criteria that must be met before the method can be used
- Control Charts: Monitoring method performance over time
- Change Management Procedures: Processes for evaluating and implementing method changes
Experimental Protocols for Risk-Based Method Evaluation
Comparative Method Assessment Protocol
When selecting a comparative method for validation studies, a structured assessment protocol ensures appropriate method selection based on risk principles.
Table: Method Comparison Experiment Parameters
| Parameter | Recommendation | Rationale | Regulatory Reference |
|---|---|---|---|
| Number of Samples | Minimum 40 patient specimens | Wide coverage of working range and disease spectrum | [1] |
| Sample Selection | Cover entire working range; represent disease spectrum | Quality depends more on range than number | [1] |
| Measurements | Single or duplicate measurements | Duplicates provide validity check | [1] |
| Time Period | Minimum 5 days, ideally 20 days | Minimize run-to-run variability | [1] |
| Sample Stability | Analyze within 2 hours between methods | Prevent handling-induced differences | [1] |
| Data Analysis | Graphical analysis + regression statistics | Visual identification of patterns + quantitative estimates | [1] |
Statistical Methods for Comparative Assessment
Various statistical approaches can be employed for method comparison, each with specific applications and limitations.
Table: Statistical Methods for Method Comparison
| Method | Application Context | Key Outputs | Assumptions/Limitations | |
|---|---|---|---|---|
| Linear Regression | Wide analytical range | Slope, y-intercept, sy/x | Linear relationship; constant variance | |
| Bland-Altman Plot | Agreement assessment | Mean bias, limits of agreement | Independence of differences and magnitudes | |
| Paired t-test | Narrow analytical range | Mean difference, p-value | Normally distributed differences | |
| Tolerance Interval | Comparability acceptance | 95/99 TI | Based on historical lot data | [67] |
| Correlation Coefficient | Range adequacy assessment | r-value | Mainly useful for assessing data range, not acceptability | [1] |
Protocol for Robustness Testing of Critical Parameters
Robustness testing evaluates a method's capacity to remain unaffected by small, deliberate variations in method parameters [50]. The following protocol provides a structured approach:
- Select Variations: Choose variations (±) for each CMP based on practical operating ranges
- Design Experiment: Use a structured approach (e.g., Plackett-Burman, fractional factorial)
- Execute Testing: Conduct experiments with deliberate parameter variations
- Evaluate Effects: Monitor impact on CMAs (resolution, retention time, peak area, etc.)
- Establish Ranges: Document proven acceptable ranges for each CMP
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing a risk-based approach requires specific tools and reagents designed to support robust method development and validation.
Table: Essential Research Reagent Solutions for Risk-Based Method Development
| Reagent/Tool | Function in Risk-Based Approach | Application Example | Critical Quality Attributes |
|---|---|---|---|
| Reference Standards | Definitive method comparison | Accuracy assessment | Purity, stability, traceability |
| System Suitability Test Mixtures | Verify method performance before use | MODR boundary verification | Resolution, precision, peak symmetry |
| Matrix-Matched Calibrators | Account for sample matrix effects | Specificity assessment | Commutability, stability |
| Quality Control Materials | Ongoing method performance monitoring | Control strategy implementation | Stability, homogeneity, assigned values |
| Chemometric Software | DoE design and data analysis | MODR establishment | Statistical modeling capabilities |
| Column Characterization Kits | Stationary phase performance assessment | Robustness testing | Reproducibility, selectivity |
Regulatory and Business Implications
Regulatory Flexibility Through MODR
The deep method understanding gained through AQbD allows a MODR to be defined where the method fits its purpose at each point, with quality criteria assured with a defined probability level [50]. This approach has significant regulatory implications:
- Reduced Post-Approval Submissions: Changes within the MODR typically require only notification to regulatory bodies rather than prior approval
- Established Conditions Focus: ECs focus on method-specific performance criteria rather than operational parameters
- Streamlined Lifecycle Management: Continual improvements within the MODR are facilitated without major regulatory submissions
Business Benefits and Efficiency Gains
Organizations implementing risk-based validation typically reduce unnecessary testing by 30-45% while maintaining or improving quality outcomes [68]. Additional benefits include:
- Faster Method Development: Structured approaches reduce method optimization timelines
- Reduced Investigation Costs: Better method understanding decreases out-of-specification results
- Improved Technology Transfer: Well-characterized methods transfer more successfully between sites
- Enhanced Operational Flexibility: MODR allows parameter adjustments without regulatory submission
Adopting a risk-based approach to focus on Critical Method Parameters represents a fundamental evolution in analytical science that aligns with modern quality paradigms. By systematically identifying, evaluating, and controlling the parameters that truly impact method performance, organizations can develop more robust, reliable, and regulatory-flexible methods. The structured workflow outlined in this guide—from ATP definition through MODR establishment and control strategy implementation—provides a practical roadmap for implementation. For researchers selecting comparative methods for validation studies, this risk-based framework offers a scientifically sound methodology that prioritizes resources on critical factors, ultimately enhancing method understanding, regulatory compliance, and operational efficiency throughout the analytical method lifecycle.
In pharmaceutical development and regulated research, the integrity of analytical data is paramount. This data forms the foundation for critical decisions regarding product safety, efficacy, and quality. Method validation and method verification are two essential, distinct processes that ensure analytical methods produce reliable, accurate, and reproducible results. While both aim to confirm a method's suitability for its intended purpose, they apply at different stages of the method's lifecycle and require different levels of investment [69] [70].
Understanding the distinction is more than an academic exercise; it is a practical necessity for regulatory compliance and efficient resource allocation. The U.S. Food and Drug Administration (FDA) and other regulatory bodies have shown increasing focus on documented evidence that analytical methods are properly validated or verified, as seen in recent regulatory guidance and inspections [71] [72]. This guide provides researchers and drug development professionals with a clear framework for selecting the correct path, supported by experimental protocols and data-driven comparisons.
Core Concepts and Definitions
What is Method Validation?
Method validation is the comprehensive, documented process of proving that an analytical method is acceptable for its intended purpose through extensive laboratory studies [69] [73]. It is performed when a method is newly developed or significantly modified [74]. The process establishes and documents that the method's performance characteristics—such as accuracy, precision, and specificity—are capable of producing reliable results that meet predefined acceptance criteria [75] [73].
Validation provides the foundational evidence that a method is scientifically sound and robust across its defined range. It is typically required for methods supporting new drug applications, clinical trials, and novel assay development [69].
What is Method Verification?
Method verification is the process of confirming that a previously validated method performs as expected in a specific laboratory setting, with its unique analysts, equipment, and environmental conditions [69] [70]. It is not a re-validation but a targeted assessment to demonstrate that the method, which has already been proven suitable elsewhere, retains its expected performance when implemented in a new context [74] [76].
Verification is typically employed when adopting a compendial method (e.g., from the USP, Ph. Eur.) or a method transferred from another laboratory [75] [74]. Its purpose is to generate objective evidence that the method is suitable for its intended use under actual conditions of use [73].
Decision Framework: Validation or Verification?
The choice between validation and verification depends on the method's origin and the context of its use. The following decision diagram provides a clear pathway for researchers to determine the required approach.
When is Method Validation Required?
Method validation is necessary in the following scenarios [69] [74]:
- Developing a new analytical method in-house for a novel product or analyte.
- Significantly modifying an existing method's parameters beyond allowable limits (e.g., changing detection principles, sample preparation techniques, or critical chromatographic conditions).
- Applying an existing method to a new matrix or product where potential interference is unknown.
- Supporting regulatory submissions for new drug applications (NDA, ANDA), where the method has not been previously reviewed [75].
When is Method Verification Appropriate?
Method verification is the correct approach in these situations [75] [74]:
- Implementing a compendial method (e.g., USP, Ph. Eur., AOAC) in your quality control laboratory for the first time.
- Adopting a previously validated method from a client, partner, or another site within your organization.
- Transferring a validated method from research and development to a quality control laboratory.
- Using a method from a Marketing Authorization dossier for routine testing.
Performance Characteristics: A Comparative Analysis
The scope of testing differs significantly between validation and verification. Validation requires a comprehensive assessment of all relevant performance parameters, while verification focuses on confirming critical attributes under actual use conditions.
Table 1: Performance Characteristics Assessed in Validation vs. Verification
| Performance Characteristic | Definition | Assessment in Validation | Assessment in Verification |
|---|---|---|---|
| Accuracy | Closeness of test results to the true value [73] | Required | Required |
| Precision | Degree of agreement among repeated measurements [73] | Required (Repeatability & Reproducibility) | Required (Repeatability) |
| Specificity | Ability to assess analyte unequivocally in the presence of potential interferents [73] | Required | Required |
| Linearity | Ability to obtain results proportional to analyte concentration [75] | Required | Not Required |
| Range | Interval between upper and lower analyte levels with suitable precision, accuracy, and linearity [73] | Required | Not Required |
| Detection Limit (LOD) | Lowest amount of analyte that can be detected [73] | Required for impurity methods | Confirmatory |
| Quantitation Limit (LOQ) | Lowest amount of analyte that can be quantified with acceptable precision and accuracy [75] | Required for impurity methods | Confirmatory |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters [73] | Required | Not Required |
Experimental Protocols and Methodologies
Protocol for Comprehensive Method Validation
A full method validation should follow a structured, pre-approved protocol. The International Council for Harmonisation (ICH) Q2(R1) guideline provides the standard methodology [75] [74].
Accuracy
- Experimental Methodology: Prepare a minimum of 9 determinations across the specified range (e.g., 3 concentrations/3 replicates each) [75].
- Procedure: Spike the analyte into a placebo or blank matrix at known concentrations (e.g., 80%, 100%, 120% of target). Compare measured values against true values.
- Data Analysis: Calculate percent recovery for each concentration. The mean recovery should be within established limits (e.g., 98-102% for API assay).
- Acceptance Criteria: Results should be within ±2% of the true value for drug substance assay, or as justified by the method's intended use.
Precision
- Repeatability (Intra-assay):
- Methodology: Analyze a minimum of 6 determinations at 100% of the test concentration [75].
- Data Analysis: Calculate the relative standard deviation (RSD). For API assay, RSD is typically ≤1.0%.
- Intermediate Precision (Ruggedness):
- Methodology: Conduct the analysis on different days, with different analysts, and different instruments.
- Data Analysis: Compare results from both series using statistical tests (F-test, t-test). No significant difference should be observed.
Specificity
- Methodology: For chromatographic methods, inject individually: blank (placebo), standard, sample, and forced degradation samples (acid/base, oxidative, thermal, photolytic stress) [73].
- Data Analysis: Demonstrate that the analyte peak is pure and free from interference. For assay, resolution from closest eluting peak should be >2.0.
Linearity and Range
- Methodology: Prepare a minimum of 5 concentrations spanning the claimed range (e.g., 50-150% of target concentration) [75].
- Procedure: Analyze each concentration in duplicate or triplicate. Plot response versus concentration.
- Data Analysis: Calculate correlation coefficient (typically R² > 0.999 for API assay), y-intercept, and slope of the regression line.
Robustness
- Methodology: Deliberately vary method parameters (e.g., mobile phase pH ±0.2 units, column temperature ±5°C, flow rate ±10%).
- Data Analysis: Evaluate the impact on system suitability parameters (resolution, tailing factor, efficiency). The method should remain unaffected by small variations.
Protocol for Method Verification
Method verification is a more focused assessment, typically evaluating accuracy, precision, and specificity for the specific product and laboratory conditions [74].
Verification of Accuracy and Precision
- Experimental Methodology: Prepare a minimum of 6 determinations at 100% of test concentration.
- Procedure: For drug product analysis, prepare samples by spiking API into placebo at target concentration. Analyze using the method being verified.
- Data Analysis: Calculate mean recovery (accuracy) and RSD (precision). Compare results against established acceptance criteria from the original validation.
Verification of Specificity
- Methodology: Inject blank (placebo) and spiked sample to demonstrate absence of interference at the retention time of the analyte.
- Data Analysis: Verify that any interference from excipients or impurities does not exceed specified thresholds (typically ≤0.5% for chromatographic purity methods).
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful method validation and verification require high-quality materials and reagents. The following table details essential items for these processes.
Table 2: Essential Research Reagents and Materials for Method Validation/Verification
| Item | Function/Purpose | Quality/Specification Requirements |
|---|---|---|
| Reference Standard | Serves as the benchmark for method accuracy and calibration [75] | Certified purity, preferably from official sources (USP, EP) or fully characterized in-house |
| High-Purity Reagents | Mobile phase preparation, sample extraction, and derivatization | HPLC/GC grade for chromatographic methods; ACS grade for wet chemistry |
| Placebo/Blank Matrix | Evaluates method specificity and detects potential interference [73] | Should contain all inactive components in the same ratio as the test product |
| System Suitability Standards | Verifies chromatographic system performance before sample analysis [74] | Should test critical parameters (resolution, tailing, repeatability, theoretical plates) |
| Forced Degradation Materials | Establishes method stability-indicating capability and specificity [73] | Acids, bases, oxidizing agents, heat, and light sources for stress studies |
Regulatory Landscape and Compliance Considerations
Regulatory bodies globally provide clear guidelines for method validation and verification. The ICH Q2(R1) guideline serves as the international standard for analytical procedure validation, while USP General Chapters <1225> and <1226> provide specific guidance on validation and verification of compendial procedures [75] [74].
Recent FDA inspections have shown increased scrutiny on product-specific verification, even for compendial methods [71]. The FDA has issued final guidance in January 2025 specifically addressing validation and verification for tobacco products, reflecting the agency's broader emphasis on these practices across regulated product categories [72].
For laboratories seeking ISO/IEC 17025 accreditation, method verification is generally required to demonstrate that standardized methods function correctly under local laboratory conditions [69] [77].
Choosing between method validation and verification is a critical decision that impacts both regulatory compliance and operational efficiency. The appropriate path depends entirely on the method's origin and context of use:
- Choose validation for new methods, significant modifications, or methods supporting regulatory submissions for novel products.
- Choose verification for compendial methods or previously validated methods being implemented in a new laboratory setting.
A strategic approach to method validation and verification not only ensures regulatory compliance but also enhances data integrity, reduces the risk of product failure, and builds confidence in analytical results. By implementing the frameworks and protocols outlined in this guide, researchers and drug development professionals can make informed decisions that support both scientific rigor and operational excellence in their analytical workflows.
Implementing Lifecycle Management and Continuous Performance Monitoring
The paradigm for analytical methods in pharmaceutical development and quality control has fundamentally shifted from a one-time validation event to a holistic, integrated lifecycle approach. This modern framework, formalized in guidelines such as ICH Q14, emphasizes that method validation is not an endpoint but a core component of continuous monitoring and improvement [25]. Implementing robust lifecycle management ensures that analytical procedures remain fit-for-purpose, produce reliable data, and support product quality throughout the entire drug development and commercialization process.
Within the context of selecting a comparative method for validation research, the lifecycle approach provides a structured, science-driven foundation. It moves beyond simply comparing two sets of data and instead focuses on building a deep understanding of the method's capabilities, limitations, and performance boundaries from the outset. This understanding is critical for designing a validation study that can generate meaningful comparability or equivalency data, ultimately leading to more robust and defensible regulatory submissions [26] [25].
The Analytical Procedure Lifecycle Framework
The analytical procedure lifecycle is a comprehensive model that encompasses all stages of a method's existence, from initial conception through retirement. This model is built upon the principle of Knowledge Management, where data and understanding are systematically captured and used to inform decisions [25].
Stages of the Lifecycle
The lifecycle, as advocated by USP <1220> and other regulatory stimuli, consists of three primary stages [78]:
- Stage 1: Procedure Design and Development: This initial stage is driven by the Analytical Target Profile (ATP) and involves using risk-based strategies and prior knowledge to design and develop a robust method.
- Stage 2: Procedure Performance Qualification (Method Validation): This stage demonstrates that the procedure is suitable for its intended use, providing formal proof that it meets the criteria defined in the ATP.
- Stage 3: Continued Procedure Performance Verification: This ongoing stage involves monitoring the method's performance during routine use to ensure it remains in a state of control.
A key feature of this model is the presence of feedback loops from Stage 3 back to Stage 2 and Stage 1, and even to the ATP itself, enabling continuous improvement [78]. The following diagram illustrates this interconnected flow and the core activities within each stage.
The Analytical Target Profile (ATP) as the Foundation
The Analytical Target Profile (ATP) is the cornerstone of the entire lifecycle. It is a prospective summary of the quality and performance requirements for the analytical procedure, directly linked to the product's Critical Quality Attributes (CQAs) [79]. The ATP defines the procedure's intended purpose, outlining the required measurement quality—including accuracy, precision, selectivity, and range—before any development work begins [78] [26].
In the context of comparative method validation, a clearly defined ATP provides the objective, pre-defined criteria against which any method (new, modified, or alternative) must be evaluated. It answers the question: "What constitutes an equivalent or comparable method?" Without a clear ATP, comparability assessments risk becoming subjective and statistically flawed.
Designing for the Lifecycle: Method Development and Validation
A core tenet of the lifecycle approach is that quality is built into the method during the design and development phase, not just tested for during validation. This involves adopting a Quality by Design (QbD) mindset for analytical procedures [78] [25].
Strategic Method Development
Method development should be executed with long-term suitability in mind. Key strategies include:
- Risk-Based Approach: Identifying critical method parameters (e.g., mobile phase composition, column temperature) early and understanding their impact on method performance through structured experimentation, such as Design of Experiments (DOE) [25]. This helps define the method's design space—the combination of parameters within which variations do not significantly affect performance.
- Platform Methods: For similar products (e.g., monoclonal antibodies), developing flexible platform procedures that can be applied across multiple materials with minimal revalidation. This employs a "generic validation" concept, saving time and resources [26].
- Knowledge Management: Meticulously capturing development data in reports and notebooks. This creates a "roadmap" that is invaluable for future troubleshooting, method improvement, or justifying changes to regulators [25].
Fit-for-Purpose Method Validation
The validation strategy should be aligned with the product's development stage and the method's purpose, a concept known as "fit-for-purpose" or graduated validation [26]. A method for early-phase clinical trials may require less extensive validation than one for a commercial product filing. Key validation approaches include:
- Full Validation: Conducted per ICH Q2(R1) for commercial methods, included in a Biologics License Application (BLA) [26].
- Covalidation: When a method is used at multiple sites simultaneously, validation can be designed to include studies (e.g., intermediate precision) performed at both the developing and receiving laboratories, with data combined into a single validation package [26].
- Compendial Verification: For official pharmacopeial methods (e.g., USP, EP), full validation is not required. Instead, the laboratory must verify that the method works as expected under actual conditions of use [26].
Table 1: Key Performance Metrics for Analytical Method Validation
| Performance Characteristic | Objective | Typical Acceptance Criteria | Relevance to Comparative Studies |
|---|---|---|---|
| Accuracy | Measure closeness to true value | Recovery: 90-110% for assay | Crucial for demonstrating that a new method provides an unbiased measurement compared to a reference. |
| Precision (Repeatability, Intermediate Precision) | Measure degree of scatter | RSD < 2% for assay | Used to ensure the new method's variability is comparable to or better than the original. |
| Specificity | Ability to measure analyte unequivocally | No interference from blank | Must be demonstrated for the new method's specific conditions and sample matrix. |
| Linearity & Range | Direct proportionality of response | R² > 0.998 | The working range of the new method must be suitable for its intended use. |
| Robustness | Resilience to small, deliberate parameter changes | System suitability criteria met | A robust method reduces the risk of failure during transfer and routine use. |
Continuous Performance Monitoring and Change Management
The post-validation phase is where lifecycle management proves its long-term value. The goal is to proactively ensure the procedure remains in a state of control throughout its operational life.
Ongoing Performance Verification
Continuous monitoring involves the regular collection and assessment of data generated during routine analysis of quality control samples. A primary tool for this is the use of control charts, which track key performance indicators (e.g., system suitability test results, reference standard potency) over time [78]. Statistical trends or out-of-trend (OOT) results can provide an early warning of potential method drift or degradation, triggering an investigation before the method fails.
Managing Change: Comparability and Equivalency
Change is inevitable in the drug development lifecycle. A robust lifecycle management program provides a structured, risk-based framework for handling changes to analytical procedures [25]. The two key concepts in this area are Comparability and Equivalency.
- Comparability is evaluated when a method is modified (e.g., a minor change to sample preparation). The goal is to demonstrate that the modified method yields results "sufficiently similar" to the original, ensuring no adverse impact on product quality decisions. These changes typically do not require a prior regulatory submission [25].
- Equivalency is a more rigorous assessment required when replacing a method with a completely new one (e.g., switching from HPLC to UHPLC). It must be demonstrated that the new method performs "equal to or better than" the original. This usually requires a full side-by-side validation and statistical comparison, and such changes require regulatory approval before implementation [25].
The following workflow outlines the decision-making process for managing such changes, from the initial trigger through to the necessary regulatory actions.
Experimental Protocols for Method Comparison
When selecting a comparative method for validation research, particularly for an equivalency study, the experimental design is critical. The following protocols provide detailed methodologies for key experiments.
Protocol for Side-by-Side Equivalency Testing
This is the core experiment for demonstrating method equivalency during a method replacement [25].
- Objective: To demonstrate that a new analytical procedure (Method B) is equivalent to the currently used procedure (Method A) by statistically comparing results from both methods when analyzing the same set of representative samples.
- Materials:
- Representative drug substance and drug product samples covering the expected quality range (e.g., from different manufacturing batches, including samples with known impurities).
- All reference standards, reagents, and mobile phases as specified in both Method A and Method B.
- Instrumentation for both Method A and Method B, qualified and maintained.
- Procedure: a. Sample Preparation: Prepare a single, homogeneous lot of each sample type. Split each lot and analyze portions using both Method A and Method B. The analysis should be performed by different analysts on different days to incorporate realistic variability. b. Testing Sequence: Analyze a minimum of 6 independent sample preparations for each method. The order of analysis should be randomized to avoid bias. c. Data Collection: Record the reportable result (e.g., % assay, % impurity) for each injection.
- Data Analysis: a. Descriptive Statistics: Calculate the mean, standard deviation, and relative standard deviation (RSD) for the results from each method. b. Statistical Comparison: Perform a statistical test to compare the means of the two methods. A paired t-test is commonly used for this purpose. If the p-value is greater than the significance level (e.g., α=0.05), there is no statistically significant difference between the two methods. c. Acceptance Criteria: Predefine equivalence margins (e.g., ±1.5% for assay) based on the method's performance and the product's CQAs. The 90% or 95% confidence interval for the difference between the two methods should fall entirely within these pre-defined margins.
Protocol for a Spiking Study for Accuracy and Specificity
This protocol is essential for impurity methods, such as Size-Exclusion Chromatography (SEC), to demonstrate the method's ability to accurately recover and quantify known impurities [26].
- Objective: To determine the accuracy and specificity of an analytical procedure by spiking the sample with known amounts of impurity and demonstrating adequate recovery.
- Materials:
- Purified drug substance (the "blank" matrix).
- Authentic samples of the target impurities (e.g., aggregate and low-molecular-weight species). These can be obtained through forced-degradation studies, fraction collection from a purification process, or controlled chemical reactions (e.g., oxidation for aggregates, reduction for LMW species) [26].
- Procedure: a. Preparation of Spiked Samples: Prepare a series of samples where the purified drug substance is spiked with known, increasing concentrations of the impurity (e.g., 0.5%, 1.0%, 2.0%, 5.0% of the main peak). b. Preparation of Unspiked Sample: Prepare a control sample of the purified drug substance without any spike. c. Analysis: Analyze the unspiked and all spiked samples in duplicate using the analytical procedure under validation.
- Data Analysis:
a. Calculate the percentage recovery for each spike level using the formula:
(Measured Concentration - Baseline Concentration) / Spiked Concentration * 100%. b. Plot the observed % impurity against the expected % impurity. The data should show good linearity with a correlation coefficient (R²) close to 1. c. Acceptance Criteria: Recovery is typically acceptable between 90-110% for impurities, demonstrating the method is accurate and specific for the analyte of interest in the presence of the sample matrix [26].
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful implementation of lifecycle management relies on high-quality materials and tools. The following table details key reagent solutions used in the development and validation of analytical methods, particularly for biologics and chromatographic analysis.
Table 2: Key Research Reagent Solutions for Analytical Lifecycle Management
| Reagent / Material | Function / Purpose | Application Example |
|---|---|---|
| Stable Reference Standards | Serves as the primary benchmark for quantifying the analyte and determining method accuracy and precision. | Used in every quantitative analysis to create a calibration curve and for system suitability testing. |
| Authentic Impurity Standards | Used to confirm method specificity and to perform accuracy/spiking studies for impurity quantification. | In an SEC method validation, used to spike the main peak to prove the method can accurately recover aggregates and fragments [26]. |
| Forced-Degradation Samples | Samples subjected to stress conditions (heat, light, acid/base) to generate impurities and demonstrate the method's stability-indicating properties. | Used in specificity studies to prove the method can separate and resolve degradation products from the main active pharmaceutical ingredient. |
| Platform Eluents & Columns | Standardized, pre-screened mobile phases and chromatography columns for platform methods to ensure consistency and facilitate method transfer. | In automated method development systems, used for extensive, automated screening of parameters to define the optimal method and its design space [79]. |
| System Suitability Test Kits | Pre-defined mixtures used to verify that the chromatographic system is performing adequately before sample analysis. | A critical component of continued performance verification (Stage 3), run at the beginning of every sequence to ensure the method is in control. |
Implementing a comprehensive lifecycle management program with continuous performance monitoring is no longer a regulatory aspiration but a scientific and operational necessity. By adopting the principles outlined in this guide—anchored by a clear ATP, executed through QbD-based development, and sustained by proactive monitoring—organizations can ensure their analytical procedures are robust, reliable, and adaptable.
For the specific task of selecting a comparative method for validation research, this lifecycle framework provides the necessary rigor. It shifts the focus from a simple statistical exercise to a thorough, knowledge-driven process that evaluates the method's foundational design and long-term performance. This leads to more meaningful comparability and equivalency conclusions, reduced regulatory risk, and ultimately, a stronger foundation for ensuring drug product quality and patient safety throughout the product's lifecycle.
In the context of method validation research, the selection of a comparative method is a foundational decision that determines the validity and regulatory acceptance of a new test procedure. Audit and inspection readiness hinges on the ability to produce comprehensive documentation that not only details the experimental work but also provides a clear, justifiable narrative for every decision made throughout the validation process. This documentation forms the essential evidence that demonstrates scientific rigor and regulatory compliance to inspectors, reviewers, and stakeholders.
The integrity of any method validation study rests upon a complete and understandable record of the work performed, evidence obtained, and conclusions reached [80]. For researchers and drug development professionals, this documentation provides the primary support for the conclusions presented in audit reports and regulatory submissions. It facilitates meaningful reviews by supervisors, quality assurance personnel, and regulatory inspectors, while simultaneously enabling the scientific community to assess the validity and reliability of the proposed method [81] [80].
Fundamental Principles of Audit Documentation
Characteristics of High-Quality Audit Evidence
Effective audit documentation serves multiple critical functions within the method validation framework. It provides tangible support for the conclusions and opinions reached during the validation process, facilitates internal and external review of the work for quality control and compliance, ensures accountability by demonstrating that proper procedures were performed, and assists future audits of the same methodology by providing reference to past practices [81].
The quality of audit evidence plays a pivotal role in the credibility of the entire validation process. Evidence must possess two essential characteristics: reliability, which ensures that it is dependable and verifiable, and relevance, meaning it should directly relate to the audit objectives and the specific methodological comparisons being evaluated [81]. High-quality evidence bolsters the credibility of the validation study, giving regulatory agencies, management, and stakeholders confidence in the findings. Conversely, low-quality or questionable evidence can cast doubt on the entire validation, potentially leading to disputes and skepticism regarding the proposed method's suitability [81].
Essential Components of Audit Documentation
Audit documentation should encompass specific particulars that create a complete record of the validation process. According to International Standards on Auditing (ISA) guidelines, this includes [81]:
- A description of the data or information being compiled
- The identity of the researcher responsible for creating the documentation
- Adherence to validation procedures in accordance with relevant standards and regulatory obligations
- Noteworthy information pertaining to the methodology's performance characteristics
- Researcher's assessments concerning sampling or testing strategies
- The timeframe for the validation study
- A comprehensive account of the evidence acquired, testing methodologies employed, and outcomes yielded
The reviewability standard is a crucial concept in audit documentation. This principle requires that documentation contain sufficient information to enable an experienced researcher who has had no previous connection with the study to understand the work that was performed, who performed it, when it was completed, and what conclusions were reached [80]. This experienced auditor should possess a reasonable understanding of audit activities and have studied the relevant technical domain and the accounting issues pertinent to the methodology [80].
Table: Essential Characteristics of Effective Audit Documentation
| Characteristic | Description | Impact on Audit Quality |
|---|---|---|
| Completeness | Contains all pertinent information including procedures, findings, and deviations | Ensures a clear and complete audit trail of the validation process |
| Timeliness | Documentation occurs promptly as work is performed | Maintains accuracy and relevance while preventing loss of critical details |
| Accuracy | Precise recording of details without errors or omissions | Prevents misunderstandings that could compromise the validation's integrity |
| Consistency | Standardized formats and procedures across documentation | Simplifies review process and promotes efficiency in audit evaluation |
| Cross-referencing | Findings linked to validation objectives and standards | Allows traceability of evidence back to its source and purpose |
Documentation Framework for Method Comparison Studies
Designing the Comparison of Methods Experiment
The comparison of methods experiment represents a critical component of method validation research, specifically designed to estimate inaccuracy or systematic error [1]. This experiment involves analyzing patient samples by both the new test method and a established comparative method, then estimating systematic errors based on observed differences. The documentation framework for this experiment must capture both the experimental design and execution details to support subsequent regulatory review.
Several factors require careful consideration and documentation when designing the comparison study. The selection of the comparative method is particularly significant, as the interpretation of experimental results depends on assumptions about the correctness of the comparative method's results [1]. When possible, a "reference method" with well-documented correctness through comparative studies with definitive methods or traceability to standard reference materials should be selected. With such reference methods, any differences are appropriately attributed to the test method. When using routine methods for comparison, differences must be interpreted more carefully, potentially requiring additional experiments to determine which method is inaccurate [1].
Specimen considerations represent another critical documentation area. A minimum of 40 different patient specimens should be tested by both methods, selected to cover the entire working range and represent the spectrum of expected sample matrices [1]. Documentation should specify the selection criteria, acceptance parameters, and handling procedures. Specimen stability requires particular attention, with analysis typically occurring within two hours between methods unless preserved appropriately [1]. The documentation must capture all handling procedures to ensure differences observed stem from analytical variation rather than preanalytical variables.
Statistical Analysis and Data Interpretation
Appropriate statistical analysis transforms raw comparison data into meaningful estimates of systematic error. The documentation should include both graphical representations and numerical statistical calculations that put exact values on visual impressions of errors [1].
Graphical analysis serves as a fundamental documentation component. For methods expected to show one-to-one agreement, a "difference plot" displaying the difference between test and comparative results versus the comparative result provides immediate visual assessment [1]. For methods not expected to show direct agreement, a "comparison plot" with test results on the y-axis and comparison results on the x-axis better illustrates the relationship [1]. Both approaches help identify discrepant results that require confirmation through repeat measurements.
Statistical calculations should provide information about systematic error at medically or analytically important decision concentrations. For comparison results covering a wide analytical range, linear regression statistics are preferable as they allow estimation of systematic error at multiple decision levels and provide information about the proportional or constant nature of the error [1]. The documentation should include:
- Slope (b) and y-intercept (a) of the line of best fit
- Standard deviation of points about the line (s_y/x)
- Calculation of systematic error (SE) at critical decision concentrations (Xc) using: Yc = a + bXc then SE = Yc - X_c
- Correlation coefficient (r) to assess whether the data range is sufficient for reliable slope and intercept estimates
For narrow analytical ranges, calculation of the average difference (bias) between methods with standard deviation of differences is typically more appropriate [1].
Table: Key Experimental Parameters for Method Comparison Studies
| Parameter | Documentation Requirement | Regulatory Significance |
|---|---|---|
| Number of Specimens | Minimum of 40 patient specimens covering entire working range | Ensures adequate evaluation across analytical measurement range |
| Specimen Quality | Documentation of selection criteria, handling, and stability procedures | Verifies that differences are analytical rather than preanalytical |
| Testing Protocol | Single vs. duplicate measurements; time between analyses | Demonstrates control of analytical variation within the experiment |
| Study Duration | Minimum of 5 different days with 2-5 specimens daily | Ensves evaluation of between-run variability in error estimation |
| Comparative Method | Rationale for selection and documented performance characteristics | Supports attribution of observed differences to test method |
Practical Implementation: Best Practices for Researchers
Documentation Strategies for Method Validation
Implementing effective documentation practices requires both systematic approaches and attention to critical details that support audit readiness. Researchers should adopt several key strategies to ensure their documentation meets regulatory standards and inspection requirements.
Document thoroughly and promptly to maintain accuracy and prevent loss of critical details [81]. Comprehensive documentation should record all pertinent information, including the validation plan, procedures performed, evidence obtained, findings, and any deviations from the planned approach. Delayed documentation can lead to inconsistencies or loss of information essential for reconstructing the validation process during audit review.
Ensure consistency and standardization across all documentation through standardized formats and procedures [81]. This uniformity simplifies the review process and promotes efficiency during both internal quality control checks and external regulatory inspections. Standardization should extend to terminology, formatting of data presentations, and structure of justification narratives to create a coherent validation story.
Maintain cross-referencing systems that link findings directly to validation objectives and applicable standards [81]. This practice helps researchers and auditors trace evidence back to its source and purpose, demonstrating how each element of the validation addresses specific methodological performance characteristics or regulatory requirements.
The Scientist's Toolkit: Essential Research Reagent Solutions
Method validation studies require specific materials and reagents that must be carefully documented to support the technical validity of the work. The following table outlines key research reagent solutions essential for robust method comparison studies:
Table: Essential Research Reagent Solutions for Method Validation
| Reagent/Material | Function in Validation | Documentation Requirements |
|---|---|---|
| Certified Reference Materials | Provide traceability to reference measurement procedures; establish accuracy base | Source, certification documentation, expiration dates, storage conditions |
| Quality Control Materials | Monitor assay performance during validation; assess precision | Concentration levels, preparation methodology, stability data |
| Calibrators | Establish analytical measurement relationship; define response curve | Source, traceability, value assignment process, stability documentation |
| Patient Specimens | Assess method performance with real-world matrices; evaluate specificity | Selection criteria, inclusion/exclusion parameters, handling procedures |
| Interference Substances | Evaluate method specificity; identify potential interferents | Substances tested, concentrations used, scientific rationale for selection |
Overcoming Common Documentation Challenges
Researchers frequently encounter specific challenges in documentation that can compromise audit readiness if not properly addressed. Recognizing and proactively managing these challenges is essential for maintaining documentation integrity.
Incomplete or inaccurate data often arises from data entry errors or missing information [81]. Researchers should implement diligent data verification processes and seek additional sources to corroborate findings when discrepancies are identified. Regular internal audits of documentation during the validation process can identify these issues early, allowing correction while source materials and institutional knowledge remain available.
Data volume and complexity can become overwhelming in comprehensive method validation studies [81]. Researchers should utilize data management tools and electronic laboratory notebooks to streamline organization and ensure all relevant data is captured in structured formats. Establishing clear data hierarchies and indexing systems facilitates efficient retrieval during audit review.
Lack of documentation standardization across different phases of validation or between team members creates confusion and inefficiency [81]. Research teams should establish standardized documentation practices before study initiation and provide training to ensure all personnel follow consistent procedures. Template documents with required elements clearly identified promote completeness and standardization.
The essential role of documentation in method validation research extends far beyond creating an audit trail. Properly executed documentation provides the foundational evidence that demonstrates scientific rigor, methodological soundness, and regulatory compliance. For researchers selecting comparative methods, the documentation must tell a coherent story that connects methodological choices to experimental outcomes and justified conclusions.
The most successful validation approaches integrate documentation as an inherent component of the scientific process rather than a separate compliance activity. By embedding documentation practices into daily research operations and maintaining a continuous state of inspection readiness, research teams can confidently respond to audit requests while simultaneously enhancing the scientific quality of their methodological work. This integrated approach ultimately strengthens the validity of research findings and accelerates the adoption of new methods into clinical and analytical practice.
Conclusion
Selecting the right comparative method is a foundational decision that determines the success and credibility of your entire method validation process. A strategic approach, grounded in a clear understanding of regulatory guidelines and scientific principles, ensures the generation of reliable, high-quality data. As the field evolves with trends like AI-driven analytics, Real-Time Release Testing (RTRT), and increased regulatory harmonization, the principles of robust comparative method selection will remain paramount. By systematically applying the frameworks outlined in this article—from foundational understanding to lifecycle management—scientists can build a defensible validation strategy that accelerates drug development, ensures compliance, and ultimately protects patient safety.
References
- 1. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 2. What to consider when performing method comparisons on ... [https://acutecaretesting.org/en/articles/what-to-consider-when-performing-method-comparisons-on-blood-gas-analyzers]
- 3. A Central Requirement for New Test Methods [https://dcndx.com/insights/method-comparison-experiment-central-requirement-new-test-methods/]
- 4. Validation of Chromatographic Methods of Analysis [https://www.sciencedirect.com/science/chapter/bookseries/pii/S0099542805320090]
- 5. A step by step guide to quantitative comparisons in ... [https://finbiosoft.com/a-step-by-step-guide-to-quantitative-comparisons-in-validation-manager/]
- 6. How Mature Are Your Data Integrity Practices? New FDA ... [https://www.propharmagroup.com/thought-leadership/how-mature-is-your-data-integrity-new-fda-and-eu-regulatory-focus-areas]
- 7. FDA official says data integrity issues are the main reason ... [https://www.raps.org/news-and-articles/news-articles/2025/4/fda-official-says-data-integrity-issues-are-the-ma]
- 8. Data Integrity in Regulatory Submissions: Best Practices for ... [https://aayutechnologies.com/blog/data-integrity-in-regulatory-submissions/]
- 9. Trends in FDA Data Integrity Enforcement Before and After ... [https://pubmed.ncbi.nlm.nih.gov/41071512/]
- 10. Certain studies conducted by Raptim Research Pvt. Ltd. ... [https://www.fda.gov/drugs/drug-safety-and-availability/fda-pharmaceutical-companies-certain-studies-conducted-raptim-research-pvt-ltd-are-unacceptable]
- 11. Comparative Study of Analytical Method Validation and ... [https://www.ijdra.com/index.php/journal/article/view/675]
- 12. Top 5 Trends in Pharmaceutical Compliance for 2025 [https://jafconsulting.com/top-5-trends-in-pharmaceutical-compliance-for-2025/]
- 13. Measurement of patient safety: a systematic review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5013509/]
- 14. The Experimental Plan for Method Validation [https://www.westgard.com/lessons/basic-method-validation/lesson21.html]
- 15. Design of Experiments for Analytical Method Development ... [https://www.biopharminternational.com/view/design-experiments-analytical-method-development-and-validation]
- 16. In Vitro Calcification of Bioprosthetic Heart Valves [https://pubmed.ncbi.nlm.nih.gov/41117258/]
- 17. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 18. 21 CFR Part 211 -- Current Good Manufacturing Practice ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-C/part-211]
- 19. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 20. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 21. VALIDATION OF COMPENDIAL METHODS [http://www.uspbpep.com/usp29/v29240/usp29nf24s0_c1225.html]
- 22. USP Reference Standards [https://www.usp.org/reference-standards]
- 23. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 24. Analyse-it® Method Validation Edition [https://analyse-it.com/products/method-validation]
- 25. A New Era for Analytical Procedure Lifecycle Management [https://synergbiopharma.com/navigating-analytical-method-comparability-and-equivalency-under-ich-q14-a-new-era-for-analytical-procedure-lifecycle-management/]
- 26. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 27. A Step-by-Step Guide to Analytical Method Development ... [https://emerypharma.com/blog/a-step-by-step-guide-to-analytical-method-development-and-validation/]
- 28. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 29. The Comparison of Methods - Westgard QC Experiment [https://westgard.com/lessons/basic-method-validation/lesson23.html]
- 30. 3.3.3.3. Selecting Sample Sizes [https://www.itl.nist.gov/div898/handbook/ppc/section3/ppc333.htm]
- 31. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 32. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 33. Why Detecting Outliers is Crucial for Accurate Data Analysis? [https://www.dasca.org/world-of-data-science/article/why-detecting-outliers-is-crucial-for-accurate-data-analysis]
- 34. Outliers and anomalies in training and testing datasets for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303909/]
- 35. Statistical data preparation: management of missing values ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548942/]
- 36. Outliers in Data: Identification and Impact Revealed [https://www.usdsi.org/data-science-insights/outliers-in-data-identification-and-impact-revealed]
- 37. Improving Time Series Data Quality: Identifying Outliers ... [https://www.mdpi.com/2624-6511/8/3/82]
- 38. Need to Perfect Data Validation Techniques? Here's Guideï¼ [https://www.fanruan.com/en/blog/data-validation-techniques]
- 39. Outlier Detection and Treatment in Research Data: 2024- ... [https://editverse.com/outlier-detection-and-treatment-in-research-data-2024-2025-best-practices/]
- 40. Understanding The Matrix Effect in Bioprocessing [https://bataviabiosciences.com/matrix-effect/]
- 41. Understanding and Mitigating Matrix Effects in Metabolomics [https://www.linkedin.com/posts/clarity-bio-systems_%F0%9D%90%81%F0%9D%90%9E%F0%9D%90%B2%F0%9D%90%A8%F0%9D%90%A7%F0%9D%90%9D-%F0%9D%90%AD%F0%9D%90%A1%F0%9D%90%9E-%F0%9D%90%8F%F0%9D%90%9E%F0%9D%90%9A%F0%9D%90%A4-%F0%9D%90%82%F0%9D%90%A8%F0%9D%90%A7%F0%9D%90%AD%F0%9D%90%9E%F0%9D%90%A7%F0%9D%90%9D%F0%9D%90%A2%F0%9D%90%A7%F0%9D%90%A0-activity-7370698501799907328-WLFq]
- 42. Assessment of matrix effect in quantitative LC-MS bioanalysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11352789/]
- 43. Strategies for the Detection and Elimination of Matrix ... [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 44. How to Mitigate Matrix Effects in ICP-MS for Complex ... [https://www.drawellanalytical.com/how-to-mitigate-matrix-effects-in-icp-ms-for-complex-sample-analysis/]
- 45. Overview of Methods and Considerations for Handling ... [https://www.chromatographyonline.com/view/overview-methods-and-considerations-handling-complex-samples]
- 46. Overcoming Matrix Effects in Non-Target Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224152/]
- 47. Sample size requirements are not being considered in studies ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02008-1]
- 48. Sample size considerations for the external validation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4738418/]
- 49. Basic Method Validation, 3rd Edition, FAQs [https://www.westgard.com/resources/resources/bmv3edfaqs.html]
- 50. Review Risk-based approach for method development in ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708518312147]
- 51. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 52. Systematic errors in Data Analysis [https://codefinity.com/blog/Systematic-errors-in-Data-Analysis]
- 53. Z-14: Estimating Analytical Errors Using Regression Statistics [https://www.westgard.com/lessons/z-stats-basic-statistics/lesson44.html]
- 54. Difference Between Constant & Proportional Error [https://www.sciencing.com/difference-between-constant-proportional-error-12185218/]
- 55. Application and interpretation of linear-regression analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11537238/]
- 56. Additional notes on regression analysis -- how to interpret ... [https://people.duke.edu/~rnau/regnotes.htm]
- 57. How to Interpret the Constant (Y Intercept) in Regression ... [https://statisticsbyjim.com/regression/interpret-constant-y-intercept-regression/]
- 58. Diagnostic test validation studies when there is a perfect reference standard - PubMed [https://pubmed.ncbi.nlm.nih.gov/34140725/]
- 59. The Importance of Reference Materials and Method Validation for Advancing Research on the Health Effects of Dietary Supplements and Other Natural Products - PubMed [https://pubmed.ncbi.nlm.nih.gov/34970578/]
- 60. AQbD-novel strategy for analytical methods [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 61. A Quality by Design (QbD) Based Method Development for ... [https://www.waters.com/nextgen/us/en/library/application-notes/2011/quality-by-design-method-development-for-determination-of-impurities-in-ziprasidone.html?srsltid=AfmBOoqXLLD06DSws94ALyvtskTJZrzrLzXVxHaykEfgo_tp3JIhdNzX]
- 62. The Application of Quality by Design to Analytical Methods [https://www.pharmtech.com/view/application-quality-design-analytical-methods]
- 63. Recent applications of analytical quality-by-design ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743924001837]
- 64. QbD approach to HPLC method development and validation ... [https://fjps.springeropen.com/articles/10.1186/s43094-021-00286-4]
- 65. QbD-based development and AGREE-guided validation of ... [https://link.springer.com/article/10.1007/s44371-025-00319-4]
- 66. Development of a quality by design-based ultra ... [https://www.sciencedirect.com/science/article/pii/S2772577425000448]
- 67. Drug Product Comparability: Developing Criteria [https://www.bioprocessintl.com/cmc-forums/emerging-strategies-for-drug-product-comparability-and-process-validation-part-1-analytical-tools-and-drug-product-comparability]
- 68. What Is Method Validation Risk Assessment and Its ... [https://altabrisagroup.com/method-validation-risk-assessment/]
- 69. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 70. Difference Between Method Verification Vs Validation in ... [https://altabrisagroup.com/method-verification-vs-validation-in-gmp-labs/]
- 71. FDA Hyper Focused on Validations and Verifications [https://certified-laboratories.com/blog/fda-hyper-focused-on-validations-and-verifications/]
- 72. Validation and Verification of Analytical Testing Methods ... [https://www.federalregister.gov/documents/2025/01/07/2024-31541/validation-and-verification-of-analytical-testing-methods-used-for-tobacco-products-guidance-for]
- 73. Method Validation Vs. Verification - A Simple Breakdown [https://cptclabs.com/method-validation-vs-verification/]
- 74. Difference Between Validation And Verification Of ... [https://gmpinsiders.com/method-validation-vs-verification/]
- 75. What Is The Difference Between Verification And Validation of ... [https://boracdmo.com/what-is-the-difference-between-verification-and-validation-of-analytical-methods-in-the-pharmaceutical-industry/]
- 76. Analytical Methodology: Validation, Verification, or ... [https://vicihealthsciences.com/analytical-methodology-validation-verification-qualification/]
- 77. To Validate or Verify, that is the Question | ANAB Webinar [https://anab.ansi.org/resource/to-validate-or-to-verify-that-is-the-question/?srsltid=AfmBOopS0xS8f_jq3VSz-8Pb7WK5NhmB2G2smjYGg5kdPMIFdY2BM4cb]
- 78. Understanding the Lifecycle Approach for Analytical ... [https://www.chromatographyonline.com/view/understanding-lifecycle-approach-analytical-procedures]
- 79. Method Life Cycle Management [https://www.thermofisher.com/us/en/home/industrial/pharma-biopharma/pharmaceutical-quality-control-testing/method-lifecycle-management.html]
- 80. AS 1215: Audit Documentation - Appendix A [https://pcaobus.org/oversight/standards/auditing-standards/details/AS1215_Appendix_A]
- 81. Audit Evidence & Documentation: Guide & Best Practices [https://www.scrut.io/post/audit-evidence-documentation-reporting]