Overcoming Specificity and Selectivity Challenges in Pharmaceutical Analytical Methods
This article provides a comprehensive framework for pharmaceutical researchers and drug development professionals to address critical challenges in analytical method specificity and selectivity.
Overcoming Specificity and Selectivity Challenges in Pharmaceutical Analytical Methods
Abstract
This article provides a comprehensive framework for pharmaceutical researchers and drug development professionals to address critical challenges in analytical method specificity and selectivity. It explores foundational principles distinguishing these concepts, outlines advanced methodological approaches for complex modalities like biologics, offers practical troubleshooting strategies for common failure modes, and details validation protocols aligned with ICH Q2(R2) and evolving regulatory standards. By integrating Quality-by-Design principles, lifecycle management, and emerging assessment tools, the content delivers actionable insights for developing robust, reliable analytical procedures that ensure product quality and patient safety.
Demystifying Specificity and Selectivity: Core Principles and Regulatory Expectations
Official IUPAC Definitions
The International Union of Pure and Applied Chemistry (IUPAC) provides precise, distinct definitions for specificity and selectivity in analytical chemistry.
Specificity
IUPAC defines specificity as a term that "expresses qualitatively the extent to which other substances interfere with the determination of a substance according to a given procedure." Specific is considered to be the ultimate of selective, meaning that no interferences are supposed to occur [1]. Specificity is the ideal state for an analytical method, representing absolute freedom from interference.
Selectivity
IUPAC provides both qualitative and quantitative definitions for selectivity:
- (Qualitative): "The extent to which other substances interfere with the determination of a substance according to a given procedure" [2].
- (Quantitative): "A term used in conjunction with another substantive (e.g. constant, coefficient, index, factor, number) for the quantitative characterization of interferences" [2].
Key Conceptual Relationship
The fundamental relationship between these concepts is that specificity represents the ultimate degree of selectivity [1] [3]. While selectivity can be graded (a method can be more or less selective), specificity is an absolute characteristic - few methods truly achieve it [3].
Table 1: IUPAC Definitions and Key Characteristics
| Term | Definition | Gradable? | Quantifiable? | Practical Meaning |
|---|---|---|---|---|
| Specificity | Ultimate freedom from interference by other substances | No | No | Absolute characteristic; ideal state |
| Selectivity | Extent to which other substances interfere with analyte determination | Yes | Yes (with coefficients, factors, etc.) | Can be graded and characterized quantitatively |
Troubleshooting Guides
FAQ: Common Issues and Solutions
Q1: Our method shows good recovery in pure standard solutions but fails with real samples. What could be causing this?
A: This typically indicates inadequate selectivity due to matrix effects. The method may be susceptible to interference from sample matrix components that weren't present in your pure standard solutions [3].
- Solution: Conduct comprehensive matrix matching during validation. Use standard addition methods to identify and compensate for matrix effects. Consider implementing additional clean-up steps or chromatographic separation to improve selectivity [4].
Q2: During method transfer between laboratories, we're getting different results for the same samples. Where should we focus our investigation?
A: This often stems from differences in method robustness rather than fundamental issues with specificity or selectivity [4].
- Solution:
- First, verify that both labs are using identical system suitability test parameters
- Conduct a ruggedness test examining the impact of small, deliberate variations in method parameters (pH, temperature, flow rate, etc.)
- Ensure both instruments are properly calibrated and maintained
- Document all procedural details to identify any subtle differences in execution [4] [5]
Q3: How can we demonstrate our method is truly specific for a degradation product that co-elutes with the main peak?
A: Achieving true specificity for co-eluting compounds requires orthogonal techniques [3].
- Solution: Implement hyphenated techniques like LC-MS/MS or LC-DAD to confirm peak purity. Use spectral comparison or mass spectral confirmation to demonstrate that the method can distinguish between the analyte and closely eluting impurities [6] [3]. Forced degradation studies can help validate the method's ability to separate and quantify degradation products from the active compound [4].
Q4: Our immunoassay was described as "specific" but we're seeing cross-reactivity with metabolites. Was this claim inaccurate?
A: Yes, this represents a common misuse of terminology. Immunological methods relying on antigen-antibody interactions are often described as specific, but they frequently show cross-reactivity and should more accurately be defined as selective rather than specific [3].
- Solution: Characterize the degree of cross-reactivity with known structurally similar compounds and report the method as selective with defined cross-reactivity percentages. Update method documentation to accurately reflect the selective nature of the assay [3].
Advanced Troubleshooting Scenarios
Q5: We need to adapt a selective method for a new matrix. What's the systematic approach?
A: Matrix adaptation requires re-evaluation of key validation parameters:
- Specificity: Test for new potential interferences in the novel matrix
- Selectivity: Evaluate whether the same degree of discrimination is maintained
- Accuracy and Precision: Conduct spike-recovery experiments in the new matrix
- Limit of Detection/Quantification: Determine if method sensitivity is affected by matrix components [4] [5]
Systematically document all experiments to demonstrate the method remains fit-for-purpose in the new context.
Experimental Protocols
Protocol 1: Establishing Method Selectivity
Objective: To experimentally demonstrate the selectivity of an analytical method against potentially interfering substances.
Materials:
- Analytical instrument (HPLC, GC, LC-MS, etc.)
- Analyte standard
- Potential interfering substances (related compounds, metabolites, matrix components)
- Appropriate solvents and reagents
Procedure:
Prepare individual solutions of the analyte and each potential interfering substance at concentrations expected in actual samples.
Analyze each solution separately to determine retention times/positions and detection characteristics.
Prepare mixture solutions containing the analyte and each potential interferent in combination.
Analyze the mixtures using the same method parameters.
Compare chromatograms/spectra to ensure:
Acceptance Criteria:
- Analyte peak purity meets established thresholds (e.g., >99%)
- Interference from any individual substance is <5% of analyte response
- Method can clearly distinguish analyte from closely related compounds
Protocol 2: Challenge Test for Specificity
Objective: To rigorously challenge a method's specificity using stressed samples.
Materials:
- Drug substance or product samples
- Equipment for stress conditions (heating, UV light, acid/base, oxidizing agents)
- Analytical instrumentation
- Reference standards
Procedure:
Subject samples to stress conditions:
- Acidic hydrolysis (e.g., 0.1N HCl, room temperature or elevated temperature)
- Basic hydrolysis (e.g., 0.1N NaOH, room temperature or elevated temperature)
- Oxidative degradation (e.g., 3% Hâ‚‚Oâ‚‚, room temperature)
- Thermal degradation (e.g., 70°C for 2 weeks)
- Photolytic degradation (e.g., UV light per ICH Q1B) [4]
Analyze stressed samples alongside unstressed controls and placebo formulations (if applicable).
Evaluate chromatographic separation between:
- Analyte peak and degradation products
- Analyte peak and placebo components
- All peaks of interest from each other
Use orthogonal detection (e.g., DAD or MS) to confirm peak purity and identity.
Data Interpretation:
- The method demonstrates specificity if it can accurately quantify the analyte despite the presence of degradation products and matrix components
- All degradation products are satisfactorily resolved from the analyte peak
- Peak purity tests confirm homogeneous analyte peaks [4]
Table 2: Validation Parameters for Specificity and Selectivity Assessment
| Parameter | Assessment Method | Acceptance Criteria | Relevance to Specificity/Selectivity |
|---|---|---|---|
| Peak Purity | Photodiode array or mass spectrometric detection | Peak homogeneity >99% | Direct measure of specificity |
| Resolution | Chromatographic separation of critical pairs | R ≥ 1.5 between analyte and closest eluting interference | Quantitative expression of selectivity |
| Forced Degradation | Stress testing under various conditions | Analyte stability-indicating; degradation products resolved | Demonstrates specificity against known and unknown impurities |
| Matrix Interference | Comparison of standards in solvent vs. matrix | Signal difference <5% | Measures selectivity against sample matrix |
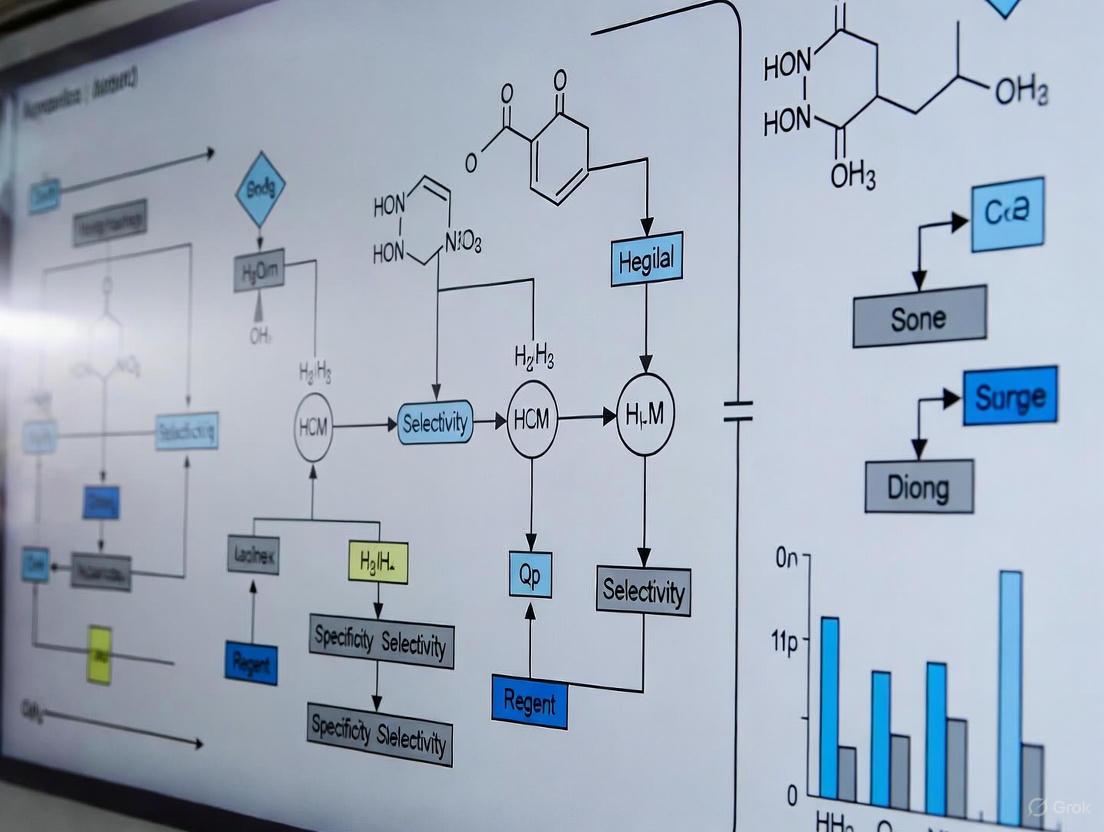
Visualization Diagrams
Achieving Specificity Through Selectivity Enhancement
The Scientist's Toolkit
Research Reagent Solutions for Specificity/Selectivity Enhancement
Table 3: Essential Materials for Method Development
| Material/Technique | Function in Specificity/Selectivity | Common Applications |
|---|---|---|
| Hyphenated Techniques (LC-MS/MS) | Provides orthogonal separation and identification; confirms peak purity through spectral data | Distinguishing closely eluting compounds; confirming analyte identity in complex matrices [6] [3] |
| Chromatography Columns (various phases) | Enhances separation selectivity through different interaction mechanisms | Method development for resolving complex mixtures; optimizing separation of critical pairs |
| Immunoaffinity Sorbents | Provides high biological selectivity for specific analytes | Sample clean-up for complex biological matrices; extracting target analytes from interfering substances [3] |
| Molecularly Imprinted Polymers | Synthetic materials with predetermined selectivity for target molecules | Selective extraction and pre-concentration of specific analytes; reducing matrix effects |
| Chemical Derivatization Reagents | Modifies analyte properties to enhance detection selectivity | Improving chromatographic separation; enhancing detection characteristics for specific compound classes |
| Design of Experiments (DoE) Software | Systematically optimizes multiple method parameters for maximum selectivity | Robustness testing; establishing method operable design regions [6] |
| Pentylcyclohexyl acetate | Pentylcyclohexyl Acetate|CAS 85665-91-4|For Research | Pentylcyclohexyl acetate is a chemical reagent for research applications. This product is For Research Use Only (RUO), not for human or veterinary use. |
| Copper nickel formate | Copper Nickel Formate | CAS 68134-59-8 | Copper nickel formate is a chemical compound for research use only (RUO). It serves as a precursor for synthesizing Cu-Ni bimetallic nanoparticles and catalysts. Not for personal or human use. |
Advanced Tools for Challenging Separations
- High-Resolution Mass Spectrometry (HRMS): Provides exact mass measurements for confident compound identification and distinguishing isobaric compounds [6]
- Multi-Attribute Methods (MAM): Consolidates analysis of multiple quality attributes into single assays, particularly valuable for biologics characterization [6]
- Process Analytical Technology (PAT): Enables real-time monitoring and control, supporting quality assurance through continuous verification of method performance [6]
The Critical Role in Patient Safety and Product Quality Assurance
Welcome to the Analytical Method Support Center
This resource provides troubleshooting guides and FAQs to help researchers and scientists address common challenges in analytical method development and validation, directly supporting specificity and selectivity research.
Frequently Asked Questions (FAQs)
Q1: What are the most critical parameters to ensure method specificity and selectivity? Specificity and selectivity are validated by demonstrating that the method can accurately measure the analyte in the presence of potential interferences like impurities, degradants, or matrix components [4]. Key parameters include assessing resolution from known interferents and demonstrating the absence of false positives or negatives through forced degradation studies [4].
Q2: How can a Quality-by-Design (QbD) approach improve my analytical methods? A QbD approach involves defining an Analytical Target Profile (ATP) early on and using risk-based design and statistical tools like Design of Experiments (DoE) to understand the method's operational range [6]. This creates a more robust and reliable method by systematically evaluating the impact of method parameters on performance characteristics [7].
Q3: What should I do if my method's performance changes after transfer to a quality control (QC) lab? This indicates a potential ruggedness issue. First, verify that the method was adequately validated and that all critical parameters were documented. Ensure comprehensive training and knowledge transfer has occurred between teams. The receiving lab should perform a robustness study to identify sensitive parameters and establish a control strategy for consistent performance [6].
Q4: When is it acceptable to modify an already-validated method? Methods can be changed to improve reliability or efficiency. If changes are necessary—due to process changes, obsolete reagents, or technological improvements—a revalidation is required [7]. The extent of revalidation (from partial verification to full validation) depends on the significance of the change. Regulatory submissions must be amended accordingly [7].
Troubleshooting Guides
Guide: Resolving Chromatographic Peak Issues
Common Symptoms and Solutions:
| Symptom | Possible Cause | Investigative Action & Solution |
|---|---|---|
| Peak Tailing [8] | Active sites on column [8], prolonged analyte retention [8] | - Use a different column chemistry (e.g., end-capped).- Modify mobile phase (e.g., use buffers or competing amines). |
| Split Peaks [8] | Contamination at inlet [9], blocked frit [9] | - Check and replace guard column.- Flush system with strong solvent.- Inspect and clean injector needle. |
| Extra / Ghost Peaks [8] | Sample carryover [8] [9], mobile phase contamination [8] | - Increase flush time in gradient.- Prepare fresh mobile phase.- Ensure thorough cleaning of auto-sampler. |
| Broad Peaks [8] | Column overloading [8], low column temperature [8], excessive tubing volume [8] | - Reduce injection volume.- Increase column temperature.- Use tubing with narrower internal diameter. |
Guide: Addressing Baseline Problems
Common Symptoms and Solutions:
| Symptom | Possible Cause | Investigative Action & Solution |
|---|---|---|
| Baseline Noise [8] | Air bubbles in system [8], contaminated detector cell [8], leaking pump seal [8] | - Degas mobile phase and purge system.- Clean or replace detector flow cell.- Check and replace pump seals if worn. |
| Baseline Drift [8] | Column temperature fluctuation [8], mobile phase composition change [8], contaminated flow cell [8] | - Use a thermostat-controlled column oven.- Prepare fresh mobile phase.- Flush flow cell with strong organic solvent. |
| High Backpressure [8] | Column blockage [8], flow rate too high [8], mobile phase precipitation [8] | - Reverse-flush column if possible, or replace.- Lower the flow rate.- Flush system with compatible solvent and prepare fresh mobile phase. |
| Low or No Pressure [8] | Major leak in system [8], air bubbles [8], faulty check valves [8] | - Identify and tighten leaking fittings.- Prime and purge the pump.- Inspect and replace check valves. |
Guide: Managing Sensitivity and Signal Problems
Common Symptoms and Solutions:
| Symptom | Possible Cause | Investigative Action & Solution |
|---|---|---|
| Loss of Sensitivity [8] | Contaminated column or guard column [8], blocked injector needle [8] [9], incorrect mobile phase [8] | - Replace guard column.- Flush or replace the injector needle.- Prepare new mobile phase with correct composition. |
| Irreproducible Response [9] | Analyte Adsorption onto active surfaces in flow path (e.g., stainless steel) [9] | - Coat the entire flow path (tubing, valves, fittings) with an inert material like Dursan or SilcoNert to prevent adsorption of sticky compounds [9]. |
| Carryover [9] | Analyte Adsorption/Desorption from active flow path surfaces [9] | - Implement the same solution: ensure all flow path components are inert-coated to prevent analyte sticking and subsequent release [9]. |
| Retention Time Shifts [9] | Small changes in flow rate or solvent composition (HPLC) [4]; temperature fluctuations (GC) [4] | - Strictly control mobile phase preparation and use a column oven for HPLC.- Ensure temperature stability for GC [4]. |
Experimental Protocols for Key Investigations
Protocol 1: Forced Degradation Study for Specificity
Objective: To demonstrate the method's ability to measure the analyte without interference from degradation products.
Materials:
- Acid/Base: 0.1M HCl, 0.1M NaOH
- Oxidizing Agent: 3% Hydrogen Peroxide
- Thermal Chamber: For solid and solution state stress
- Light Cabinet: For photostability testing (e.g., as per ICH Q1B)
Methodology:
- Stress Conditions: Expose the drug substance to various stress conditions.
- Acidic/Basic Hydrolysis: Treat with 0.1M HCl and 0.1M NaOH at room temperature for several hours.
- Oxidative Degradation: Treat with 3% Hâ‚‚Oâ‚‚ at room temperature.
- Thermal Degradation: Heat solid and solution samples at 60°C for a defined period.
- Photolytic Degradation: Expose to specified light conditions.
- Sample Analysis: After stress, neutralize, dilute, or prepare samples as appropriate and analyze using the method under validation.
- Data Analysis: Assess chromatograms for the appearance of new peaks (degradants). Confirm that the analyte peak is pure and resolved from all degradant peaks, and that mass balance is achieved (approximately 98-102%).
Protocol 2: Design of Experiments (DoE) for Robustness Testing
Objective: To systematically evaluate the method's capacity to remain unaffected by small, deliberate variations in method parameters.
Materials:
- Statistical software (e.g., JMP, Design-Expert)
- HPLC/UHPLC system capable of precise parameter control
Methodology:
- Identify Critical Parameters: Select key variables (e.g., pH of mobile phase, column temperature, flow rate, gradient time) based on prior knowledge.
- Design the Experiment: Use a fractional factorial or response surface design to define the high and low levels for each parameter.
- Execute Runs: Perform the chromatographic runs in the randomized order specified by the DoE.
- Evaluate Responses: For each run, measure critical responses like resolution, tailing factor, and retention time.
- Statistical Analysis: Use the software to build models and identify which parameters have a statistically significant effect on the responses. Establish a Method Operational Design Range (MODR) where the method performs satisfactorily [6].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function / Explanation |
|---|---|
| SilcoNert / Dursan Coatings [9] | Inert coatings applied to flow path components (tubing, fittings) to prevent adsorption of reactive analytes like Hâ‚‚S, amines, and proteins, thereby reducing carryover and peak tailing. |
| UHPLC Columns [6] | Columns packed with sub-2-micron particles that provide higher efficiency, better resolution, and faster analysis compared to traditional HPLC columns. |
| LC-MS/MS Grade Solvents | High-purity solvents with minimal impurities to reduce background noise and ion suppression in mass spectrometry, ensuring sensitivity and accurate quantification. |
| Stable Isotope Labeled Internal Standards | Used in bioanalytical methods (e.g., LC-MS/MS) to correct for analyte loss during sample preparation and for matrix effects, improving accuracy and precision. |
| qPCR Assays | Essential for biologics and cell & gene therapy analysis, used to quantify and validate specific DNA sequences, such as detecting residual host cell DNA or viral vector copy numbers [6]. |
| Arsine, dichlorohexyl- | Arsine, dichlorohexyl-, CAS:64049-22-5, MF:C6H13AsCl2, MW:230.99 g/mol |
| 2-Octyldodecyl acetate | 2-Octyldodecyl Acetate|CAS 74051-84-6|Supplier |
Method Development and Troubleshooting Workflows
Troubleshooting Logic Flow
Analytical Method Lifecycle Management
Frequently Asked Questions (FAQs)
Q1: What is the main difference between FDA and EMA in their approach to method validation?
While both agencies follow ICH guidelines, their emphasis can differ. The FDA explicitly requires system suitability tests to be an integral part of the validation protocol and expects robustness to be thoroughly described in validation reports. The EMA also expects system suitability but may be less explicit in its requirement and often considers robustness evaluation as important but not always strictly mandatory for all methods. Global submissions should address both expectations [10].
Q2: At what stage during drug development should analytical methods be validated?
For GMP activities, methods should be properly validated, even for Phase I studies, following a phase-appropriate validation approach [7]. Method validation is typically executed against commercial specifications prior to process validation, which usually occurs during the pivotal clinical phase. Full validation is generally completed 1-2 years prior to commercial license application to ensure sufficient real-time stability data [7].
Q3: Can an analytical method be changed after it has been validated?
Yes, methods can be changed when necessary due to process changes, reagent availability, or technology improvements [7]. However, the extent of changes determines the revalidation requirements, ranging from simple verification to full validation. Method comparability results should be provided, and in some cases, product specifications may need re-evaluation. Regulatory submissions must be amended to reflect these changes [7].
Q4: How does ICH Q2(R2) differ from previous versions?
ICH Q2(R2) emphasizes a lifecycle approach to analytical procedures, integrating development and validation with a stronger focus on science-based and data-driven robustness assessments. It provides updated guidance on deriving and evaluating various validation tests for both chemical and biological/biotechnological drug substances and products [11] [6].
Q5: What are the key challenges in analytical method validation for biopharmaceuticals?
Biopharmaceuticals present unique challenges, especially for novel modalities like cell and gene therapies or patient-specific cancer vaccines. These include developing surrogate potency methods when direct assays don't exist, managing extended development timelines, and addressing product-specific suitability even when using established platform technologies [7].
Troubleshooting Guides
Specificity and Selectivity Challenges
Problem: Interference from sample matrix components in complex biologics.
- Root Cause: Matrix effects from biological components can cause ion suppression in LC-MS/MS or non-specific binding in ligand-binding assays [7] [12].
- Solution:
- Implement extensive sample preparation techniques (protein precipitation, solid-phase extraction)
- Use alternative sample dilution methods to minimize matrix effects
- Employ the standard addition method or surrogate matrix approaches for endogenous compounds [12]
- Conduct parallelism assessments to ensure accurate quantification [12]
Problem: Inconsistent specificity for degradation products in stability-indicating methods.
- Root Cause: Inadequate chromatographic separation or insufficient detection specificity [4].
- Solution:
- Apply Quality by Design (QbD) principles with Design of Experiments (DoE) to optimize separation parameters [7] [6]
- Utilize multi-dimensional analytical techniques (LC-MS/MS, LC-UV-DAD) for enhanced specificity confirmation [6]
- Perform forced degradation studies under various stress conditions to validate method specificity for degradation products [4]
Problem: Method lacks robustness when transferred between laboratories.
- Root Cause: Incomplete understanding of critical method parameters and their acceptable ranges [7].
- Solution:
- Conduct comprehensive robustness studies using statistical experimental design (DoE) during method development [7] [6]
- Establish Method Operational Design Ranges (MODRs) that define acceptable parameter variations [6]
- Implement a method transfer protocol with predefined acceptance criteria and parallel testing [4]
Regulatory Compliance Issues
Problem: Regulatory submissions rejected due to insufficient validation data.
- Root Cause: Incomplete validation parameters or inadequate statistical evaluation [4].
- Solution:
- Ensure all validation parameters specified in ICH Q2(R2) are addressed based on the method's purpose (identification, testing for impurities, assay) [11]
- Provide sufficient data points for each validation parameter to ensure statistical significance [4]
- Include system suitability tests as part of the validation protocol, particularly for FDA submissions [10]
Problem: Inconsistencies in global submissions due to differing FDA and EMA expectations.
- Root Cause: Regional variations in regulatory emphasis and documentation requirements [10].
- Solution:
- Develop validation protocols that satisfy both FDA's explicit system suitability requirements and EMA's harmonization expectations [10]
- Maintain comprehensive documentation that demonstrates method robustness, even when not strictly required [10]
- Implement ALCOA+ principles for data integrity to meet both agencies' expectations [6]
Experimental Protocols
Protocol 1: Specificity and Selectivity Assessment for Chromatographic Methods
Purpose: To demonstrate the method's ability to measure the analyte unequivocally in the presence of potential interferents.
Materials and Reagents:
- Reference standards of analyte and potential impurities/degradation products
- Blank matrix (placebo formulation for drug products or appropriate solvent for drug substances)
- Forced degradation samples (acid/base, oxidative, thermal, photolytic stress conditions)
- Mobile phase components and other chromatographic reagents
Procedure:
- Prepare individual solutions of the analyte and all known potential interferents
- Inject blank matrix to determine background interference
- Inject individual components to confirm resolution and retention times
- Inject mixture of analyte and interferents to demonstrate separation
- Perform forced degradation studies and analyze samples to demonstrate separation of degradation products
- Quantify any co-eluting peaks and calculate resolution factors
Acceptance Criteria:
- Resolution between analyte and closest eluting peak: ≥ 2.0
- Peak purity index: ≥ 0.999 for the analyte peak
- No interference at the retention time of the analyte from blank matrix
Protocol 2: Robustness Testing Using Design of Experiments (DoE)
Purpose: To identify critical method parameters and establish acceptable ranges for robust method performance.
Materials and Reagents:
- System suitability standard and test sample
- Chromatographic reagents from multiple lots (if applicable)
Procedure:
- Identify potential critical method parameters (e.g., mobile phase pH, column temperature, flow rate)
- Design a Plackett-Burman or Fractional Factorial experiment to screen parameters
- Define low, medium, and high levels for each parameter based on normal operating conditions
- Execute experimental runs in randomized order
- Measure critical responses (resolution, tailing factor, efficiency, retention time)
- Analyze data using statistical methods to identify significant effects
- Establish Method Operational Design Ranges (MODRs) for critical parameters
Acceptance Criteria:
- All system suitability criteria met throughout the MODR
- No significant trends or failures in method performance within the MODR
- Statistical significance (p < 0.05) for critical parameter effects
Regulatory Requirements Comparison
Table 1: Key Regulatory Guidelines for Analytical Method Validation
| Guideline | Scope | Key Focus Areas | Status/Timeline |
|---|---|---|---|
| ICH Q2(R2) [11] | Analytical procedures for drug substances & products (chemical & biological) | Validation tests for assay, purity, impurities, identity; lifecycle approach | Current scientific guideline |
| ICH Q14 [6] | Analytical procedure development | Enhanced approach for method development, QbD principles | Forthcoming guideline |
| FDA Bioanalytical Method Validation (M10) [13] | Bioanalytical assays for nonclinical & clinical studies | Chromatographic & ligand-binding assays for drugs & metabolites | Final (November 2022) |
| EMA Bioanalytical Method Validation [14] | Bioanalytical methods for pharmacokinetic & toxicokinetic data | Quantitative concentration data for animal & human studies | Superseded by ICH M10 (July 2022) |
Table 2: Method Validation Parameters and Regulatory Expectations
| Validation Parameter | ICH Q2(R2) Requirements [11] | FDA Emphasis [10] | EMA Emphasis [10] |
|---|---|---|---|
| Specificity | Required for identification, purity tests, and assays | Must demonstrate no interference from placebo, impurities, or matrix | Expected, particularly for stability-indicating methods |
| Accuracy | Required with defined methodology for recovery assessment | Risk-based approach with appropriate confidence intervals | Harmonized approach across EU member states |
| Precision | Repeatability, intermediate precision, and reproducibility | System suitability as integral part of validation | Expected but may allow some flexibility based on method purpose |
| Linearity | Demonstrated across specified range with statistical measures | Appropriate number of data points with correlation coefficient | Similar to ICH with focus on practical range of use |
| Range | Established from linearity, accuracy, and precision data | Must cover all intended sample concentrations | Consistent with ICH recommendations |
| Robustness | Should be considered during development phase | Should be thoroughly described in validation reports | Evaluated but not always strictly required |
Workflow Diagrams
Analytical Method Lifecycle Management
Specificity Troubleshooting Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Analytical Method Development
| Reagent/Material | Function/Purpose | Application Notes |
|---|---|---|
| Reference Standards | Primary standard for quantification and method calibration | Use well-characterized, high-purity materials; implement two-tiered approach linking working standards to primary reference standards [7] |
| Chromatographic Columns | Stationary phase for separation | Select appropriate chemistry (C18, C8, HILIC, etc.) with multiple lots for robustness testing [4] |
| Mass Spectrometry Grade Solvents | Mobile phase components for LC-MS | Low UV absorbance, high purity to minimize background noise and ion suppression [6] |
| Surrogate Matrices | Alternative matrix for standard curves for endogenous compounds | Use for biomarker assays or endogenous compound analysis when authentic matrix is not available [12] |
| Stability-Indicating Stress Reagents | For forced degradation studies (acid, base, oxidants) | Use to validate method specificity by creating degradation products [4] |
| System Suitability Standards | Verify system performance before sample analysis | Mixture of key analytes to check resolution, tailing factor, and reproducibility [10] |
| 2-Propylheptane-1,3-diamine | 2-Propylheptane-1,3-diamine|C10H24N2 Supplier | |
| Arotinolol, (R)- | Arotinolol, (R)-, CAS:92075-58-6, MF:C15H21N3O2S3, MW:371.5 g/mol | Chemical Reagent |
For researchers, scientists, and drug development professionals, achieving reliable analytical results is paramount. The accuracy of these results is consistently challenged by three major classes of interference: matrix effects, impurities, and degradants. These interference sources can significantly compromise data integrity, leading to inaccurate quantification, reduced method sensitivity, and ultimately, flawed scientific conclusions. Within the critical research on analytical method specificity and selectivity, understanding and mitigating these interferences is not merely a procedural step but a foundational requirement for ensuring that a method can unequivocally distinguish the analyte from other components. This guide provides targeted troubleshooting and methodological support to identify, quantify, and overcome these common yet challenging obstacles.
Troubleshooting Guides
FAQ: Matrix Effects
Q1: What is a matrix effect in analytical chemistry? The matrix refers to all components of a sample other than the analyte of interest. A matrix effect is the alteration of the analytical signal caused by these co-eluting matrix components. This interference can lead to either suppression or enhancement of the analyte signal, affecting the accuracy and reliability of the results [15] [16]. In techniques like LC-MS, this is often due to matrix components interfering with the ionization efficiency of the analyte [17].
Q2: How can I quantify the matrix effect in my assay? The matrix effect (ME) can be quantitated by comparing the analytical response of an analyte in a matrix extract to its response in a pure solvent. The following formula is commonly used [15]: ME = 100 × (A(extract) / A(standard))
- A(extract): Peak area of the analyte when diluted with matrix extract.
- A(standard): Peak area of the same concentration of analyte in a pure solvent.
A value of 100 indicates no matrix effect. A value below 100 indicates signal suppression, and a value above 100 indicates signal enhancement [15]. An alternative formula (ME = 100 × (A(extract)/A(standard)) - 100) sets 0 as the ideal value, with negative and positive values indicating suppression and enhancement, respectively [15].
Q3: What practical steps can I take to reduce matrix effects?
- Improve Sample Cleanup: Utilize more selective extraction or cleanup procedures (e.g., SPE, QuEChERS) to remove interfering matrix components [16].
- Use Isotope-Labeled Internal Standards: These standards experience nearly identical matrix effects as the analyte, effectively compensating for signal loss or enhancement [16] [17].
- Matrix-Matched Calibration: Prepare calibration standards in a matrix that is free of the analyte but otherwise identical to the sample (e.g., using an extract from an organically grown source for pesticide analysis) [17].
- Standard Addition Method: Add known amounts of the analyte to the sample itself. This is particularly useful for complex or unknown matrices, as it accounts for the matrix influence directly [15].
- Chromatographic Optimization: Improve the separation to ensure the analyte elutes away from the matrix interferences, thus reducing co-elution [16].
FAQ: Impurities and Degradants
Q4: Why are new, unknown peaks appearing in my chromatogram? The appearance of unknown peaks can be attributed to several factors:
- Sample Degradation: The analyte may be degrading over time due to exposure to light, heat, or the solvent itself [18]. Omeprazole, for instance, is known to be unstable in acidic environments [18].
- Mobile Phase Contamination/Decomposition: Impurities in solvents or buffers, or the formation of degradation products from the mobile phase over time, can elute as extraneous peaks [18].
- System Carryover: A contaminated autosampler needle or injector can introduce traces from a previous, high-concentration sample [18]. Running a solvent blank can help diagnose this issue.
- Reagent Interactions: Impurities in reagents can react with the analyte or other sample components to form new compounds [19].
Q5: What is forced degradation, and why is it performed? Forced degradation, or stress testing, is the intentional degradation of a drug substance or product under conditions more severe than accelerated stability conditions. Its primary objectives are [20]:
- To establish the intrinsic stability of the molecule and elucidate its degradation pathways.
- To identify and characterize likely degradation products.
- To validate the stability-indicating properties of an analytical method by demonstrating its ability to separate the analyte from its degradants.
Q6: How much degradation is sufficient for a forced degradation study? While not strictly defined by regulations, degradation of drug substances between 5% and 20% is generally accepted for method validation [20]. A common target is approximately 10% degradation [20]. It is crucial to avoid over-stressing, which may generate secondary degradants not seen in real-time stability studies.
Experimental Protocols
Protocol 1: Quantifying Matrix Effect
This protocol is adapted from guidelines for mass spectrometry-based analysis [17].
Prepare Solutions:
- Matrix-matched Sample: Extract a blank matrix (e.g., drug-free plasma, homogenized organic strawberry). Spike a known volume of a standard analyte solution (e.g., 100 µL of 50 ppb solution) into a known volume of the blank matrix extract (e.g., 900 µL) to achieve the desired concentration.
- Neat Standard: Prepare a standard at the same concentration in pure solvent (e.g., 100 µL of 50 ppb standard added to 900 µL solvent).
Analysis: Inject both solutions into the LC-MS or GC-MS system using the validated analytical method.
Calculation: Calculate the Matrix Effect (ME) using the formula provided in the FAQ section.
ME = 100 × (Peak Area of Matrix-matched Sample / Peak Area of Neat Standard)- Interpret the results as follows:
| ME Value | Interpretation |
|---|---|
| 85% - 115% | Minimal matrix effect |
| < 85% | Signal suppression |
| > 115% | Signal enhancement |
Protocol 2: Forced Degradation Study to Identify Degradants
This protocol outlines standard stress conditions to generate degradation products for method development [21] [20].
Acid and Base Hydrolysis: Prepare a solution of the drug substance (e.g., 1 mg/mL) in 0.1 M HCl and 0.1 M NaOH, respectively. Store these solutions typically at elevated temperatures (e.g., 40°C, 60°C) and sample at multiple time points (e.g., 1, 3, 5 days) [20]. Neutralize the samples before analysis.
Oxidative Degradation: Expose the drug solution to an oxidizing agent such as 3% hydrogen peroxide (H₂O₂). Studies can be performed at room temperature or elevated temperatures (e.g., 25°C, 60°C) for shorter durations (e.g., 24 hours) [20].
Photodegradation: Expose the solid drug substance and/or solution to a light source that provides combined UV and visible radiation (as per ICH Q1B guidelines), typically at 1x and 3x ICH exposure levels [20].
Thermal Degradation: Study the solid drug substance by storing it in stability chambers at elevated temperatures (e.g., 60°C, 80°C) and different relative humidity levels (e.g., 75% RH) for specified durations [20].
Analysis: Analyze the stressed samples alongside an unstressed control using the developed chromatographic method (e.g., HPLC with a PDA or MS detector) to track the formation and separation of degradation products.
The workflow for a typical forced degradation study is outlined below:
Data Presentation
The table below summarizes typical experimental conditions used in forced degradation studies to predict the stability of a drug molecule [20].
| Degradation Type | Experimental Conditions | Typical Storage Conditions | Sampling Time Points |
|---|---|---|---|
| Acid Hydrolysis | 0.1 M HCl | 40°C, 60°C | 1, 3, 5 days |
| Base Hydrolysis | 0.1 M NaOH | 40°C, 60°C | 1, 3, 5 days |
| Oxidation | 3% H₂O₂ | 25°C, 60°C | 1, 3, 5 days (often ≤24h) |
| Photolysis | ICH-compliant light source | Not Applicable (NA) | 1, 3, 5 days |
| Thermal | Heat chamber (solid state) | 60°C / 75% RH, 80°C | 1, 3, 5 days |
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for conducting experiments related to interference sources.
| Research Reagent | Function / Purpose |
|---|---|
| Isotope-Labeled Internal Standards | Compensates for matrix effects and recovery losses during sample preparation, crucial for accurate MS quantification [16] [17]. |
| High-Purity HPLC/Spectroscopy Grade Solvents | Minimizes baseline noise and ghost peaks caused by impurities in the mobile phase [22]. |
| Buffer Salts (e.g., Phosphate, Formate, Acetate) | Controls mobile phase pH, which is critical for reproducible retention times and controlling the ionization state of ionic analytes [18]. |
| Stress Agents (e.g., HCl, NaOH, Hâ‚‚Oâ‚‚) | Used in forced degradation studies to deliberately generate degradants and understand the stability profile of a drug molecule [21] [20]. |
| SPE Sorbents and Cartridges | Used for sample cleanup to remove matrix components, thereby reducing matrix effects and protecting the analytical column [16]. |
| 9-Hydroxyvelleral | 9-Hydroxyvelleral Research Compound |
| Diholmium tricarbonate | Diholmium Tricarbonate|Ho₂(CO₃)₃ |
Systematic Troubleshooting Workflow
When facing an analytical problem, follow a logical, step-by-step approach to identify the root cause. The following diagram maps out this troubleshooting logic:
Troubleshooting Guides
Guide 1: Addressing Stability and Degradation in Complex Biologics
Problem: A bispecific antibody formulation shows increased aggregation and high viscosity at high concentrations, making subcutaneous administration difficult.
Potential Cause 1: Protein-Protein Interactions and Unfavorable Excipient Profile
- Investigation Procedure: Systematically screen excipients (e.g., surfactants, sugars, amino acids) using a high-throughput platform to identify those that effectively reduce viscosity and prevent aggregation. Assess protein-protein interaction parameters using dynamic light scattering (DLS) or static light scattering (SLS) [23].
- Solution: Optimize the formulation with a careful mix of excipients, such as surfactants (e.g., polysorbate 80) and viscosity-reducing agents (e.g., histidine, arginine), to disrupt protein-protein interactions without compromising stability [23].
Potential Cause 2: Stress from Manufacturing and Administration
- Investigation Procedure: Perform in-use stability and compatibility testing. Simulate the administration process, including dilution into IV bags and passage through administration sets, filters, and closed system transfer devices (CSTDs). Monitor for subvisible particle formation and protein loss due to adsorption [24].
- Solution: Redesign the formulation to withstand interfacial stress, potentially by optimizing surfactant type and concentration. Select administration components that minimize surface interactions and particle generation [24].
Guide 2: Overcoming Analytical Method Gaps for Gene Therapy Potency
Problem: Inconsistent and unreliable potency assay results for an AAV-based gene therapy, causing delays in product release and regulatory filings.
Potential Cause 1: Late Development of Functional Potency Assays
- Investigation Procedure: Review the assay development timeline. Confirm if the functional potency assay was initiated early in development, as it often takes up to a year to fully develop and validate [25].
- Solution: Initiate potency assay development in parallel with other critical analytical methods, not after. Begin during pre-clinical or early-phase development to ensure it is ready for later-stage regulatory submissions [25].
Potential Cause 2: Misapplication of Bioanalytical Guidance
- Investigation Procedure: Review the bioanalytical method validation plan. Check if it inappropriately applies drug-centric validation criteria (e.g., from ICH M10) without considering the Context of Use (COU) for the biomarker or potency assay [12].
- Solution: Develop a COU-driven bioanalytical study plan. Tailor accuracy, precision, and other validation parameters to the specific objectives of the potency measurement and the subsequent clinical decisions it will inform, rather than applying fixed criteria [12].
Guide 3: Ensuring Specificity and Selectivity for New Modalities
Problem: Analytical methods for an Antibody-Drug Conjugate (ADC) fail to specifically quantify the intact conjugate in patient plasma, leading to inaccurate pharmacokinetic data.
Potential Cause 1: Inadequate Sample Preparation and Matrix Effects
- Investigation Procedure: Evaluate the sample preparation protocol for extracting the ADC from plasma. Use techniques like surrogate matrix, surrogate analyte, or standard addition to account for the complex biological matrix and endogenous interferences [12] [26].
- Solution: Implement robust sample preparation, such as solid-phase extraction or immunoaffinity capture, followed by LC-MS/MS analysis with a stable isotope-labeled internal standard to correct for matrix effects and improve specificity [26].
Potential Cause 2: Method Limitations in Resolving Complex Heterogeneity
- Investigation Procedure: Characterize the method's ability to resolve the intact ADC from its naked antibody, free payload, and other metabolites. Use orthogonal techniques like SEC-MS or IEX-MS to confirm separation [23] [27].
- Solution: Employ a multi-attribute method (MAM) using high-resolution LC-MS to monitor multiple critical quality attributes (CQAs) simultaneously, ensuring selective quantification of the intact product amidst its variants and impurities [27].
Frequently Asked Questions (FAQs)
Q1: How early in development should we focus on formulation stability for a novel biologic? As early as possible. Basic formulation work should begin soon after candidate selection. Early stability data guide process development and create a stronger CMC story from the start. Addressing formulation later can introduce significant risks and expensive delays [23].
Q2: What are the key regulatory expectations for stability studies supporting a Biologics License Application (BLA)? Regulators expect comprehensive, long-term stability data from at least three batches of the drug product, typically covering the proposed shelf life (e.g., 24 months). Studies must include rigorous testing of potency, degradation products (aggregates, fragments), and chemical modifications. The data must justify the expiration date and storage conditions through statistical shelf-life modeling [27].
Q3: Our gene therapy product is a novel AAV serotype. How can we develop a platform analytical method? While full platform approaches are challenging for highly diverse gene therapies, you can platform the framework. Develop product-agnostic assays for universal attributes (e.g., host cell DNA, residual impurities) and focus custom development on the few product-specific assays critical for your serotype, such as genome titer, potency, and capsid integrity [25].
Q4: What is the biggest mistake teams make with potency assays for cell and gene therapies? The most common mistake is delaying the development of the functional potency assay. While the FDA may not require it for Phase 1, developing it can take up to a year. Starting too late is a major cause of delays in later-stage regulatory filings [25].
Q5: How can we demonstrate specificity in a potency assay for a CAR-T cell product? The assay must specifically measure the product's intended biological function (e.g., tumor cell killing). This involves using relevant, well-characterized target cells and controls, including empty vector controls and non-transduced T cells, to ensure the measured response is due to the CAR and not non-specific immune activation [28].
Data Presentation
Table 1: Key Challenges and Mitigation Strategies for Novel Modalities
| Modality | Key Challenge | Proposed Mitigation Strategy | Critical Analytical Techniques |
|---|---|---|---|
| Bispecific Antibodies | Aggregation, high viscosity at high concentration [23] | Predictive stability modeling; optimized excipient screening [23] | SE-HPLC, DLS, viscosity measurement |
| Antibody-Drug Conjugates (ADCs) | Complex heterogeneity, drug-to-ratio (DAR) distribution [23] | Multi-attribute method (MAM) by LC-MS [27] | HIC, HRAM LC-MS |
| AAV Gene Therapies | Empty/full capsid ratio, potency assay relevance [29] [25] | Orthogonal methods for capsid quantification; early development of cell-based potency assays [25] | AUC, Mass Photometry, cell-based assays |
| Cell Therapies (e.g., CAR-T) | Functional potency, product variability [28] | Development of mechanism-based bioassays [28] | Flow cytometry, cytokine release assays, cytotoxicity assays |
Table 2: Essential Research Reagent Solutions for Analytical Development
| Reagent / Material | Function in Experiment |
|---|---|
| Surrogate Matrix | Used in biomarker and endogenous compound bioanalysis to create calibration standards when the natural biological matrix is unavailable or interfered [12]. |
| Stable Isotope-Labeled Internal Standard | Added to samples during LC-MS/MS analysis to correct for variability in sample preparation, matrix effects, and instrument response, improving accuracy and precision [26]. |
| Relevant Reference Standard | A well-characterized sample of the analyte used to calibrate instruments and validate method performance, ensuring data accuracy and comparability [26] [27]. |
| Platform Purification Resins | Pre-characterized chromatography resins (e.g., for AAV purification) used in platform processes to accelerate development and improve consistency, though may require customization for novel serotypes [25]. |
Experimental Protocols
Protocol 1: High-Throughput Excipient Screening for Protein Stabilization
Objective: To rapidly identify excipients that minimize aggregation and viscosity in a high-concentration protein formulation.
Methodology:
- Preparation: Prepare a master solution of the target protein at the desired concentration.
- Excipient Panel: Dispense the protein solution into a 96-well plate containing a pre-defined library of excipients (e.g., salts, sugars, surfactants, amino acids) at various concentrations.
- Incubation: Seal the plate and incubate under stressed conditions (e.g., 40°C with agitation) to accelerate degradation.
- Analysis:
- Aggregation: Quantify soluble aggregates using a plate-reader-based size-exclusion chromatography (SEC) or static light scattering (SLS).
- Viscosity: Measure viscosity in each well using a micro-viscometer.
- Stability: Monitor other CQAs like subvisible particles by microflow imaging.
- Data Analysis: Use statistical software to rank excipients based on their ability to suppress aggregation and reduce viscosity [23].
Protocol 2: Forced Degradation Studies for Method Robustness
Objective: To challenge the specificity and selectivity of an analytical method by exposing the product to stressed conditions and ensuring the method can resolve degradation products from the main peak.
Methodology:
- Stress Conditions: Aliquot the drug substance and subject it to various stress conditions:
- Thermal: Incubate at 40°C for 1-4 weeks.
- pH: Expose to low (e.g., pH 3-4) and high (e.g., pH 9-10) conditions.
- Oxidation: Treat with hydrogen peroxide (e.g., 0.1%).
- Light: Expose to UV and visible light per ICH Q1B.
- Mechanical: Subject to agitation/vortexing.
- Analysis: Analyze stressed samples and unstressed controls using the developed method (e.g., RP-HPLC, IEX, CEX).
- Evaluation: Assess the method's ability to:
- Detect new peaks (degradants) without co-elution with the main peak (demonstrating specificity).
- Accurately quantify the main peak in the presence of degradants (demonstrating selectivity) [27].
Workflow and Relationship Visualizations
Analytical Method Development Workflow
Stability and Degradation Pathway Analysis
Advanced Techniques for Achieving Robust Specificity in Complex Analyses
Troubleshooting Guides
FAQs on Common Resolution Issues
Q1: My peaks are overlapping or co-eluting. What are the most effective ways to improve resolution?
The resolution (Rs) of two closely eluting peaks is governed by the equation: Rs = (1/4)√N * [(α-1)/α] * [k2/(1+k2)], where N is column efficiency, α is selectivity, and k is retention factor [30]. The most powerful approaches target these parameters:
- Change Selectivity (α): This is the most effective strategy for drastically improving resolution [30].
- Modify the Mobile Phase pH: This is highly effective for ionizable compounds, as it alters their hydrophobicity. A pH change of 1-2 units can significantly shift retention times [31].
- Change the Organic Modifier: Switching from acetonitrile to methanol or tetrahydrofuran can alter interaction mechanisms and peak spacing. Figure 4 provides a guide for estimating equivalent solvent strengths [30].
- Adjust Buffer or Additive Concentration: Changes can impact the retention of ionic analytes [31].
- Increase Column Efficiency (N): This sharpens peaks, improving resolution for moderately overlapped peaks.
- Use a Column with Smaller Particles: Columns packed with sub-2 µm particles provide higher plate numbers and sharper peaks [30].
- Increase Column Temperature: Higher temperatures reduce mobile phase viscosity and increase diffusion rates, enhancing efficiency. A good starting point is 40–60 °C for small molecules [30].
- Use a Longer Column: Doubling column length can increase peak capacity by approximately 40%, which is valuable for complex samples like protein digests [30].
- Optimize Retention Factor (k): Ensure analyte peaks elute within the optimal k range of 2-10. This can be achieved by reducing the strength of the mobile phase (e.g., decreasing the percentage of organic solvent) [30].
Q2: My peaks are tailing. What are the primary causes and solutions?
Peak tailing (asymmetry factor >1.2) compromises resolution, quantitation, and reproducibility [32]. The common causes and solutions are summarized in the table below.
Table 1: Troubleshooting Guide for Peak Tailing
| Possible Cause | Solution |
|---|---|
| Secondary interactions with ionized residual silanol groups on the stationary phase (especially for basic compounds) [32]. | - Operate at a lower pH (e.g., pH <3) to suppress silanol ionization [32].- Use a highly deactivated (end-capped) column [32]. |
| Column bed deformation or partially blocked inlet frit [32]. | - Reverse the column and flush with strong solvent [32].- Substitute the column to confirm the problem [32]. |
| Sample overloading or viscous sample [32]. | - Dilute the sample and re-inject [32].- Use a sample clean-up procedure (e.g., Solid-Phase Extraction) [32]. |
| Inappropriate solvent for sample dissolution [32]. | - Whenever possible, dissolve and inject samples in the mobile phase [32]. |
Q3: How can I track and identify peaks when developing a new method or screening conditions?
While UV spectra can be featureless, making peak tracking difficult, most modern software can create derivative spectra (dA/dλ) [33]. These 1st-order derivative spectra contain more useable maxima and minima, providing additional data points to increase confidence when identifying or tracking peaks across different method conditions [33].
Q4: I am experiencing inconsistent retention times and selectivity. What should I investigate?
Retention time instability often points to issues with method equilibration or mobile phase/sample composition.
- Insufficient Equilibration: In gradient elution, allow for at least 10 column volumes for re-equilibration after the gradient [32].
- Mobile Phase Instability: Evaporation of volatile components or buffer degradation can change composition over time. Cover solvent reservoirs and prepare fresh mobile phase frequently [32].
- Sample Solvent Effects: Injecting a sample dissolved in a solvent stronger than the mobile phase can cause peak distortion and retention time shifts. Dissolve the sample in the mobile phase or a weaker solvent whenever possible [32].
- Column Temperature Fluctuation: Use a column oven to maintain a constant temperature [32].
Advanced Strategy: Multidimensional Modeling for Robust Methods
For high-value applications like pharmaceutical development, multidimensional modeling is a powerful tool to define a Method Operable Design Region (MODR)—a set of robust method conditions where baseline separation (Rs ≥ 1.5) is consistently achieved despite minor, expected variations [31].
This approach uses a first-principles model calibrated with a minimal number of experiments (e.g., 4 runs for a 2-parameter model) to predict separation patterns across a wide range of conditions (e.g., gradient time, temperature, and pH) [31]. This strategy can be applied to:
- Column Interchangeability: Identify shared MODRs across different C18 columns, ensuring equivalent performance and mitigating supply chain issues [31].
- Batch-to-Batch Reproducibility: Compare column batches to select method conditions that are robust against minor manufacturing variations [31].
- HPLC System Comparability: Account for instrumental differences (e.g., dwell volume, thermal control) when transferring methods between systems [31].
The following workflow outlines the systematic application of this modeling approach in method development.
Systematic Workflow for Robust Method Development
Experimental Protocols
Protocol 1: Targeted Isolation of Natural Products using UHPLC-Guided Workflow
This protocol leverages advanced metabolite profiling for the targeted isolation of specific compounds from complex natural extracts, a common challenge in drug discovery from natural sources [34].
1. Metabolite Profiling and Compound Prioritization:
- Instrumentation: UHPLC system coupled to PDA and High-Resolution Mass Spectrometry (HRMS) [34].
- Analytical Column: Reversed-phase column (e.g., C18) with sub-2 µm particles [34].
- Method: Run a generic, wide-window gradient (e.g., 5-100% organic modifier over 20-60 minutes).
- Data Analysis: Use HRMS/MS data for putative annotation of metabolites (dereplication). Prioritize compounds based on desired properties (e.g., structural novelty, bioactivity from assays) [34].
2. Analytical Method Transfer to Semi-Preparative Scale:
- Objective: Replicate the selectivity of the analytical UHPLC separation at the semi-prep scale.
- Tool: Use HPLC modeling software to transfer the analytical gradient to semi-preparative conditions via chromatographic calculation, ensuring similar selectivity [34].
- Semi-Preparative Column: Use a column with the same bonded phase chemistry as the analytical column but with larger internal diameter and particle size (e.g., 5-10 µm) [34].
3. Targeted Isolation with Multi-Detection Guidance:
- Setup: Connect the semi-prep HPLC to UV, MS, and/or Evaporative Light Scattering (ELSD) detectors.
- Process: Inject the extract. Use the real-time detector signals to precisely trigger the collection of fractions containing the target ions (from MS) or chromophores (from UV), while monitoring for purity [34].
- Scale: This approach can be applied from milligram to gram amounts of extract depending on the system and column size [34].
Protocol 2: Systematic Optimization for Complex Biological Samples
This protocol is designed to achieve rapid, high-resolution separation of complex biological samples (e.g., plasma, tissue extracts) which are prone to matrix effects and co-elution [35].
1. Sample Preparation to Mitigate Matrix Effects:
- Technique: Use protein precipitation (PP) with acetonitrile, which is simple but may not fully remove phospholipids. For cleaner extracts, employ Solid-Phase Extraction (SPE) [35].
- Internal Standard: Whenever possible, use a stable isotope-labeled internal standard (SIL-IS) for each analyte to correct for matrix-induced ion suppression/enhancement in LC-MS [35].
2. Column and Mobile Phase Screening:
- Strategy: Use an automated UHPLC system with switching valves to screen different stationary phases (e.g., C18, phenyl, HILIC) and mobile phase conditions (pH, organic modifier) [36].
- Initial Conditions: Start with a fast, wide-gradient (e.g., 5-95% acetonitrile in 10 min) at a temperature of 40-60°C on a short column (e.g., 50 mm) packed with sub-2 µm particles [36].
3. Resolution Optimization via Parameter Fine-Tuning:
- If co-elution persists:
- Flatten the gradient: Decrease the rate of organic modifier increase to improve resolution [30].
- Adjust pH: For ionizable compounds, fine-tune pH in 0.2-0.5 unit increments to maximize selectivity differences [31].
- Change organic modifier: Switch from acetonitrile to methanol to alter selectivity [30].
- Increase temperature: Elevate temperature to 60-90°C for large molecules to enhance efficiency [30].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for HPLC/UHPLC Method Development
| Item | Function & Rationale |
|---|---|
| Columns with sub-2 µm Particles | Foundation of UHPLC; provide high efficiency and resolution, enabling faster separations [36]. |
| Superficially Porous Particles (Core-Shell) | Provide efficiency similar to sub-2 µm fully porous particles but with lower backpressure, compatible with a wider range of HPLC systems [30]. |
| High-Purity Buffers & Additives | Essential for controlling mobile phase pH and ionic strength; critical for reproducible retention of ionizable compounds [31]. |
| LC-MS Grade Solvents | Minimize UV absorbance background noise and MS chemical noise, improving detection sensitivity [33] [35]. |
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Gold standard for compensating matrix effects and analyte loss during sample preparation in quantitative LC-MS bioanalysis [35]. |
| In-line Filter (0.22 µm) & Guard Column | Protect the analytical column from particulate matter and strongly adsorbed matrix components, extending column life [32]. |
| Modeling & Method Development Software | Allows for predictive method development and robust optimization with minimal experimental runs, saving time and resources [31]. |
| 2,2,6-Trimethyldecane | 2,2,6-Trimethyldecane Reference Standard |
| 2,6-Dicyclohexyl-p-cresol | 2,6-Dicyclohexyl-p-cresol, CAS:7226-88-2, MF:C19H28O, MW:272.4 g/mol |
Peak purity assessment is a critical analytical procedure within pharmaceutical development, directly supporting a broader thesis on enhancing analytical method specificity and selectivity. It ensures that a chromatographic peak for a primary analyte, such as a drug substance, is not attributable to more than one component, like a co-eluting degradant or impurity. This evaluation is foundational for validating stability-indicating methods, which are mandated for regulatory submissions. Within the pharmaceutical industry, two predominant techniques facilitate this assessment: Photodiode Array (PDA or DAD) detection and Mass Spectrometry (MS) detection [37] [38]. This technical support center provides troubleshooting guides, FAQs, and detailed protocols to address the specific challenges researchers face in implementing these techniques.
Understanding Peak Purity Assessment
Core Concepts and Definitions
What is peak purity assessment? Peak purity assessment is a set of analytical procedures used to demonstrate that a chromatographic peak is spectrally homogeneous, meaning it originates from a single compound. This is a direct measure of an analytical method's selectivity and is a crucial component of forced degradation studies for regulatory filings [37].
Why is it crucial for method specificity and selectivity research? A method's ability to accurately measure the analyte of interest without interference from other components is its specificity. Peak purity assessment is the experimental proof that the method can distinguish the main analyte from impurities, even under stressful conditions that generate degradants. Without this confirmation, stability studies risk being compromised by undetected co-elutions, leading to inaccurate stability conclusions [37].
Key Techniques at a Glance
The following table summarizes the two primary techniques used for peak purity assessment.
Table 1: Comparison of Primary Peak Purity Assessment Techniques
| Feature | Diode Array Detector (DAD/PDA) | Mass Spectrometry (MS) |
|---|---|---|
| Fundamental Principle | Compares UV-Vis absorption spectra across a chromatographic peak [37] [39]. | Monitors mass-to-charge ratios (m/z) across a chromatographic peak [37] [38]. |
| Primary Output | Purity angle and purity threshold (or spectral similarity factor) [37]. | Extracted Ion Chromatograms (XICs), comparison of mass spectra [37] [38]. |
| Key Strength | Efficient, non-destructive, and well-understood for detecting co-elutions with different UV spectra [37]. | Highly selective and sensitive; can detect co-elutions with minimal spectral difference if they have different masses [37] [38]. |
| Key Limitation | Cannot distinguish co-eluting compounds with nearly identical UV spectra; prone to false negatives/positives under certain conditions [37]. | Higher cost and complexity; not universal (e.g., for isomers with identical mass); destructive technique [37] [40]. |
Diagram 1: Peak Purity Assessment Workflow
Diode Array Detection (DAD/PDA) Deep Dive
How It Works
A Diode Array Detector uses a broad-spectrum light source (e.g., Deuterium and Tungsten lamps). The light passes through the sample flow cell, and after dispersion by a holographic grating, the full spectrum of light is projected onto an array of diodes. This allows for the simultaneous detection of absorbance across a wide UV-Vis range (typically 190-900 nm) for each data point collected during the chromatographic run [39]. For peak purity, the key is to compare the UV spectra obtained at different points across the peak—typically the upslope, apex, and downslope [37].
Commercial software algorithms calculate spectral contrast. For example, in Waters' Empower software, spectra are treated as vectors, and the "purity angle" (a weighted average of the angles between all spectra in the peak and the apex spectrum) is compared to a "purity threshold" (which accounts for spectral noise). A peak is considered pure if the purity angle is less than the purity threshold [37]. Agilent's OpenLab uses a similar approach, calculating a similarity factor [37].
Troubleshooting Guide for PDA-based PPA
Table 2: Common PDA PPA Issues and Solutions
| Problem | Potential Causes | Troubleshooting Steps |
|---|---|---|
| False Negative (PPA passes, but impurity is co-eluting) | 1. Impurity has a nearly identical UV spectrum to the parent compound.2. Impurity concentration is too low.3. Impurity elutes very close to the peak apex [37]. | 1. Employ an orthogonal technique like MS.2. Increase sample load or stress conditions to generate higher impurity levels.3. Optimize the chromatographic method to improve separation. |
| False Positive (PPA fails for a pure peak) | 1. Significant baseline shift due to mobile phase gradients.2. Suboptimal integration or background noise.3. UV measurement at extreme wavelengths (<210 nm) [37]. | 1. Use a mobile phase blank for background subtraction.2. Re-integrate the chromatogram and adjust PPA processing parameters (e.g., baseline points).3. If possible, select a wavelength with higher analyte absorbance and lower noise. |
| High Spectral Noise | 1. Low analyte concentration.2. Detector lamp failure or aging.3. Contaminated flow cell [37] [41]. | 1. Concentrate the sample or use a path length flow cell.2. Check lamp hours and replace if necessary.3. Flush the flow cell thoroughly with appropriate solvents. |
Experimental Protocol: PDA-based Peak Purity
Objective: To demonstrate the spectral homogeneity of the main analyte peak in a stressed sample using a PDA detector.
Materials and Reagents:
- HPLC System: Equipped with a Diode Array Detector (e.g., Agilent 1260 Infinity II DAD, Waters Alliance with 2998 PDA, or Scion 6430 DAD) [37] [39].
- Software: CDS with PPA algorithm (e.g., Waters Empower, Agilent OpenLab CDS, Shimadzu LabSolutions) [37].
- Analytical Column: As per the validated method (e.g., C18, 150 x 4.6 mm, 5 µm).
- Mobile Phase: Prepared as per the validated method.
- Samples: Stressed sample (e.g., acid/base/oxidative degraded) and a reference standard of the pure analyte.
Procedure:
- System Suitability: Ensure the LC system meets all suitability criteria (e.g., retention time reproducibility, plate count, tailing factor) before analysis.
- Data Acquisition: Inject the stressed sample and acquire chromatographic data with PDA detection. Set the PDA to acquire a full spectrum (e.g., 210-400 nm) at a sufficiently high rate (e.g., 1 spectrum/second) to obtain multiple spectra across the peak of interest.
- Data Processing:
- Integrate the chromatogram at the appropriate wavelength.
- Select the main analyte peak for PPA.
- In the CDS software, initiate the peak purity algorithm. The software will typically automatically select spectra from the peak start, apex, and end for comparison.
- Review the overlaid normalized spectra and the calculated purity result (e.g., Purity Angle and Purity Threshold in Empower, or Similarity in OpenLab).
- Interpretation: A peak is considered spectrally pure if the software-specific criterion is met (e.g., Purity Angle < Purity Threshold). Visually confirm that the overlaid normalized spectra from different parts of the peak are identical.
Mass Spectrometry Detection Deep Dive
How It Works
LC-MS separates ions by their mass-to-charge (m/z) ratio. For peak purity assessment, the goal is to demonstrate that the same precursor ions, product ions, and/or adducts attributed to the parent compound are present consistently across the entire chromatographic peak [37] [38]. This is typically assessed by examining the Extracted Ion Chromatograms (EICs or XICs) for key ions and comparing mass spectra taken at the peak front, apex, and tail [37] [38].
If an impurity with a different molecular weight is co-eluting, its distinct m/z signal will cause the EIC for that ion to peak at a different retention time or show a distorted shape. Furthermore, the mass spectrum will change across the peak as the relative proportions of the analyte and impurity change [38]. Chemometric techniques like Principal Component Analysis (PCA) can also be applied to the full MS data set to detect subtle spectral changes indicating impurity presence [38].
Troubleshooting Guide for MS-based PPA
Table 3: Common MS PPA Issues and Solutions
| Problem | Potential Causes | Troubleshooting Steps |
|---|---|---|
| No Peaks / Low Signal | 1. Ion source contamination or improper ionization.2. Gas leaks or incorrect gas pressures.3. Incorrect MS tuning or calibration [41] [40]. | 1. Clean the ion source and check ionization mode (positive/negative).2. Use a leak detector to check for gas leaks, especially at column connectors and valves [41].3. Re-tune and re-calibrate the mass spectrometer according to manufacturer protocols. |
| Poor Mass Accuracy/Resolution | 1. Instrument calibration drift.2. Contaminated analyzer.3. Signal saturation [40]. | 1. Re-calibrate using the appropriate standard.2. Schedule routine instrument maintenance.3. Dilute the sample or reduce the injection volume. |
| Cannot Distinguish Isomers | 1. Fundamental limitation: Isomers have identical m/z ratios [40]. | 1. Optimize the chromatographic method to achieve baseline separation.2. Use tandem MS (MS/MS) to compare fragment ion patterns if the isomers fragment differently. |
| Signal Drift/Instability | 1. Contaminated API interface.2. Fluctuations in mobile phase delivery or gas flow. | 1. Clean the interface components (e.g., orifice, skimmer).2. Check LC pump performance and ensure gas supplies are stable and sufficient. |
Experimental Protocol: MS-based Peak Purity
Objective: To demonstrate the mass spectral homogeneity of the main analyte peak in a stressed sample using an LC-MS system.
Materials and Reagents:
- LC-MS System: Single quadrupole or higher-end MS system (e.g., Waters QDa, Agilent MSD, Sciex API systems) [37] [38] [40].
- Software: Instrument control and data processing software.
- Analytical Column: As per the validated method.
- Mobile Phase: Volatile buffers compatible with MS (e.g., ammonium formate, ammonium acetate) and MS-grade organic solvents.
- Samples: Stressed sample and a reference standard of the pure analyte.
Procedure:
- MS Tuning: Tune and calibrate the mass spectrometer for optimal sensitivity and mass accuracy for the analyte of interest.
- Method Setup: Configure the LC-MS method. Set the mass spectrometer to scan a relevant m/z range that includes the [M+H]+ (or other relevant adducts) of the analyte and its potential degradants.
- Data Acquisition: Inject the stressed sample and acquire data in full-scan mode.
- Data Processing:
- Examine the Total Ion Chromatogram (TIC).
- Generate Extracted Ion Chromatograms (XICs) for the primary ion of the analyte (e.g., [M+H]+) and for any potential or known impurity ions.
- Extract and overlay mass spectra from at least three points across the analyte peak: the leading edge, the apex, and the trailing edge.
- Interpretation: The peak is considered pure by MS if:
- The EIC for the analyte ion is symmetrical and overlaps perfectly with the TIC peak.
- The overlaid mass spectra from across the peak are identical, showing the same ions with the same relative abundances.
- There are no detectable, consistently evolving EICs for other ions within the retention time window of the main peak.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Materials for Peak Purity Assessment Experiments
| Item | Function / Explanation |
|---|---|
| Volatile Buffers (e.g., Ammonium Formate, Ammonium Acetate) | Essential for LC-MS mobile phases to prevent ion suppression and source contamination. Non-volatile salts can clog the MS interface [38]. |
| MS-Grade Solvents (e.g., Acetonitrile, Methanol) | High-purity solvents minimize background noise and chemical noise in mass spectrometry, ensuring high-quality spectra [40]. |
| Forced Degradation Samples | Stressed samples (e.g., via heat, light, acid, base, oxidation) are required to generate potential degradants against which the method's selectivity and peak purity must be demonstrated [37]. |
| Reference Standards | Highly pure analyte standards are critical for system suitability testing and as a spectral reference for comparison during PDA and MS analysis [37]. |
| PDA Calibration Solution | A solution like holmium oxide is used to validate the wavelength accuracy of the PDA detector, ensuring spectral data is reliable [37]. |
| MS Calibration Solution | A standard containing compounds of known mass (e.g., sodium formate for TOF, manufacturer-specific mix for quadrupoles) is used to calibrate the m/z scale for accurate mass measurement [40]. |
| Chloroac-met-OH | Chloroac-met-OH, MF:C7H12ClNO3S, MW:225.69 g/mol |
| 1,3-Benzodioxole-4,5-diol | 1,3-Benzodioxole-4,5-diol|CAS 23780-63-4 |
Frequently Asked Questions (FAQs)
Q1: My PDA peak purity passes, but I still suspect a co-elution. What should I do? This is a common scenario, often due to the limitations of PDA. A passing PDA result only confirms that no impurities with different UV spectra were detected. You should:
- Spike with Markers: Spike the sample with available impurity standards and see if the peak shape or purity result changes.
- Employ Orthogonal Detection: The most powerful approach is to analyze the sample using LC-MS. MS can often separate and detect co-eluting species based on mass, even if their UV spectra are identical [37].
- Use Orthogonal Chromatography: Re-analyze the sample using a different chromatographic mechanism (e.g., HILIC instead of RP-LC) to see if the separation improves [37].
Q2: Can peak purity assessment ever definitively prove a peak is 100% pure? No. Peak purity assessment can only conclude that no co-eluting compounds were detected given the limitations of the technique used. PDA cannot detect impurities with identical UV spectra, and MS cannot distinguish isomers with identical masses. Therefore, PPA increases confidence in the method's selectivity but does not provide absolute proof of purity. It is one part of a comprehensive method validation strategy [37].
Q3: When developing a new method, which technique should I use first for peak purity? PDA is typically the first-line tool. It is non-destructive, less expensive to operate, and provides valuable spectral information during method development. If the PDA results are ambiguous, or if the molecule/impurities are known to have poor chromophores or very similar structures, then MS should be incorporated as a complementary, more selective technique [37].
Q4: What are the key software settings to check if I get a failing purity result with PDA? First, verify the spectral acquisition and processing parameters:
- Signal-to-Noise: Ensure the peak has a sufficiently high S/N. Low S/N can artificially inflate the purity angle.
- Baseline Points: Manually review and adjust the peak start and stop points for integration to ensure the algorithm is only comparing spectra from within the peak.
- Spectral Range: Narrow the spectral range used for the calculation to a region where the analyte has strong, characteristic absorbance and avoid regions of high noise (e.g., below 220 nm where mobile phase absorption can be high) [37].
Diagram 2: Suspected Co-elution Troubleshooting Path
Forced Degradation Studies to Establish Stability-Indicating Capabilities
Troubleshooting Guides
Inadequate Degradation Under Stress Conditions
Problem: Insufficient degradation (typically less than 5-10%) is observed after subjecting the drug substance to standard stress conditions, making it difficult to evaluate the method's stability-indicating capability [20].
Solutions:
- Increase stress intensity gradually: For thermal stress, increase temperature in increments (e.g., from 40°C to 60°C or 80°C). For hydrolysis, consider higher acid/base concentrations (e.g., 0.1M to 0.5M HCl/NaOH) or extended exposure times [20].
- Evaluate multiple time points: Sample at 24-hour intervals for up to 7-14 days to monitor degradation progression and avoid under-stressing or over-stressing [20].
- Explore alternative stress conditions: If standard conditions fail, investigate photolytic stress (1× and 3× ICH conditions) or oxidation with different oxidizing agents (3% H₂O₂, azobisisobutyronitrile) [20].
Preventive Measures:
- Conduct preliminary scouting studies with small drug quantities to determine optimal stress conditions.
- Refer to established degradation protocols for similar chemical entities.
- Terminate studies if no degradation occurs after exceeding accelerated condition severity [20].
Poor Chromatographic Separation of Degradants
Problem: Inadequate separation between the active pharmaceutical ingredient (API) and its degradation products, compromising accurate quantification and method specificity [42] [43].
Solutions:
- Optimize selectivity: Adjust mobile phase composition, pH, or gradient profile. Incorporating selectivity as a primary optimization parameter can significantly improve separation without sacrificing analysis time [44] [45].
- Modify column temperature: Elevated temperatures can improve separation kinetics and reduce analysis time. Increasing temperature from 40°C to 80°C can decrease mobile phase viscosity, potentially cutting analysis time in half [44].
- Consider alternative columns: Different stationary phases (C8, phenyl, polar-embedded) may provide different selectivity for challenging separations [44].
Preventive Measures:
- During method development, screen multiple column chemistries and mobile phase conditions.
- Utilize chromatographic modeling software to predict separation conditions.
- Implement quality by design (QbD) principles to define method operable design regions [43].
Low Sensitivity in Detecting Minor Degradants
Problem: Inability to detect low-concentration degradation products, potentially missing critical quality attributes [46].
Solutions:
- Increase injection volume or sample concentration: Ensure minor degradants are above the detection limit, while considering potential column overloading for the main compound [20].
- Optimize detection parameters: For UV detection, select wavelength that maximizes degradant detection. Verify the data acquisition rate is sufficient to prevent peak broadening and apparent sensitivity loss [46].
- Address adsorption issues: "Prime" the system with multiple injections of the analyte to saturate adsorption sites on new components, particularly important for biomolecules like proteins and peptides [46].
- Verify column performance: Monitor column efficiency (plate number), as decreased performance reduces peak height and apparent sensitivity [46].
Preventive Measures:
- Characterize detector response for known degradants during method development.
- Validate method sensitivity according to ICH guidelines, establishing detection and quantitation limits [43].
Inconsistent Peak Purity Assessment Results
Problem: Inconclusive or variable results from photodiode array (PDA) peak purity assessments, creating uncertainty about method selectivity [37].
Solutions:
- Optimize PDA settings: Ensure proper baseline correction and avoid extreme wavelengths (<210 nm or >800 nm) where noise interference increases [37].
- Verify integration: Suboptimal integration can lead to false positive purity failures due to interference from background noise or neighboring peaks [37].
- Employ orthogonal techniques: When PDA results are inconclusive, utilize mass spectrometry (MS) for peak purity assessment, which detects co-eluting compounds based on mass differences rather than spectral contrast [37].
- Spike with known impurities: Confirm separation by spacing stressed samples with available impurity standards [37].
Preventive Measures:
- Establish scientifically justified acceptance criteria for peak purity tests during method validation [43].
- Understand limitations of PDA-based peak purity assessment, particularly for compounds with similar UV spectra or low concentration degradants [37].
Frequently Asked Questions (FAQs)
Q1: How much degradation should be targeted during forced degradation studies?
A: A degradation level between 5% and 20% is generally accepted, with 10% often considered optimal for small molecule pharmaceuticals. This provides sufficient degradant levels for detection and characterization without promoting secondary degradation products that might not form under normal storage conditions [20].
Q2: When should forced degradation studies be performed in the drug development process?
A: Although regulatory guidance suggests stress testing during Phase III, conducting these studies earlier (preclinical or Phase I) is highly encouraged. Early studies provide critical information for formulation development, manufacturing process improvement, and stability-indicating method optimization, potentially avoiding stability-related issues later in development [20].
Q3: What are the essential stress conditions to include in a forced degradation study protocol?
A: A minimal forced degradation study should include:
- Acid and base hydrolysis (e.g., 0.1M HCl and NaOH at elevated temperatures)
- Oxidative degradation (e.g., 3% Hâ‚‚Oâ‚‚)
- Thermal degradation (solid and solution state at elevated temperatures)
- Photolytic degradation (per ICH Q1B conditions)
- Humidity studies (e.g., 75% RH) [20]
Q4: How can I demonstrate my analytical method is truly stability-indicating?
A: A stability-indicating method must demonstrate specificity by resolving the API from all potential degradation products. This is typically established through forced degradation studies followed by:
- Chromotographic peak purity assessment (PDA or MS)
- Mass balance calculations (ensuring total accounted material ≈ 100%)
- Resolution of all known degradants from the API and from each other [37]
Q5: What are common mistakes in validating the specificity of stability-indicating methods?
A: Common mistakes include:
- Not investigating all potential interferences (degradants, excipients, related compounds)
- Using generic, non-specific acceptance criteria without scientific justification
- Failing to consider sample changes over time (e.g., in stability studies)
- Not performing forced degradation studies under sufficiently diverse conditions to generate relevant degradants [43]
Experimental Protocols
Standard Forced Degradation Protocol for Small Molecules
This protocol provides a systematic approach for forced degradation studies on drug substances [20].
Materials and Reagents:
- Drug substance (API)
- 0.1M Hydrochloric acid (HCl)
- 0.1M Sodium hydroxide (NaOH)
- 3% Hydrogen peroxide (Hâ‚‚Oâ‚‚)
- pH buffers (2, 4, 6, 8)
- Appropriate solvents for drug substance
Procedure:
- Sample Preparation: Prepare drug solution at approximately 1 mg/mL in appropriate solvent [20].
- Acid Hydrolysis:
- Mix 1 mL drug solution with 1 mL 0.1M HCl
- Heat at 40°C and 60°C
- Withdraw samples at 1, 3, and 5 days
- Neutralize with equivalent base before analysis
- Base Hydrolysis:
- Mix 1 mL drug solution with 1 mL 0.1M NaOH
- Heat at 40°C and 60°C
- Withdraw samples at 1, 3, and 5 days
- Neutralize with equivalent acid before analysis
- Oxidative Degradation:
- Mix 1 mL drug solution with 1 mL 3% Hâ‚‚Oâ‚‚
- Store at 25°C and 60°C
- Withdraw samples at 1, 3, and 5 days
- Thermal Degradation:
- Expose solid drug substance to 60°C and 80°C
- For solution state, heat drug solution at same temperatures
- Include humidity control (75% RH) where appropriate
- Withdraw samples at 1, 3, and 5 days
- Photolytic Degradation:
- Expose solid and solution samples to 1× and 3× ICH light conditions
- Include dark controls
- Analyze after 1, 3, and 5 days of exposure [20]
Analysis:
- Analyze all samples using the developed chromatographic method
- Compare with unstressed controls
- Calculate percentage degradation
- Perform peak purity assessment
Peak Purity Assessment Using Photodiode Array Detection
This protocol details the assessment of chromatographic peak purity using PDA detection [37].
Materials and Equipment:
- HPLC system with photodiode array detector
- Suitable chromatographic data system (e.g., Waters Empower, Agilent OpenLab, Shimadzu LabSolutions)
- Stressed samples and controls
- Reference standards (if available)
Procedure:
- Chromatographic Analysis:
- Inject stressed samples using validated method
- Acquire UV spectra across the peak (typically 210-400 nm)
- Ensure adequate signal-to-noise ratio (>10:1 for minor peaks)
- Spectral Acquisition:
- Set data acquisition rate to collect sufficient spectra across each peak (minimum 10-12 spectra per peak)
- Ensure proper baseline correction by collecting baseline spectra at peak onset and offset
- Purity Assessment (Empower Software Example):
- Baseline-correct spectra by subtracting interpolated baseline
- Convert spectra to vectors in n-dimensional space
- Normalize vector lengths using least-squares regression
- Calculate purity angle (weighted average of spectral angles) and purity threshold (angle accounting for solvent and noise contributions)
- Compare purity angle to purity threshold: peak is considered pure if purity angle < purity threshold [37]
- Data Interpretation:
- Evaluate spectral homogeneity across entire peak
- Investigate any regions where spectral contrast suggests potential co-elution
- For borderline results, confirm with orthogonal techniques
Troubleshooting:
- If false positives occur (pure peak fails purity test), check for baseline shifts, integration errors, or noise interference
- If false negatives occur (impure peak passes purity test), consider low impurity concentration, similar UV spectra, or impurity eluting near peak apex [37]
Data Presentation
Typical Stress Conditions and Outcomes
Table 1: Standard forced degradation conditions and expected degradation ranges for small molecule pharmaceuticals [20]
| Stress Condition | Typical Parameters | Target Degradation | Common Degradants | Sampling Time Points |
|---|---|---|---|---|
| Acid Hydrolysis | 0.1M HCl, 40-60°C | 5-20% | Dealkylation products, hydrolysis products | 1, 3, 5 days |
| Base Hydrolysis | 0.1M NaOH, 40-60°C | 5-20% | Hydrolysis products, decarboxylation products | 1, 3, 5 days |
| Oxidation | 3% H₂O₂, 25-60°C | 5-20% | N-oxides, sulfoxides, hydroxylated products | 1, 3, 5 days |
| Thermal (Solid) | 60-80°C, ±75% RH | 5-20% | Dehydration products, dimers, degradation products | 1, 3, 5 days |
| Photolysis | 1× & 3× ICH options | 5-20% | Photodegradation products, dimers | 1, 3, 5 days |
Kinetic Modeling Parameters for Biologics Aggregation
Table 2: First-order kinetic model parameters for predicting aggregation in various protein therapeutics [47]
| Protein Modality | Formulation Concentration (mg/mL) | Temperatures Studied (°C) | Study Duration (Months) | Dominant Degradation Process | Activation Energy (Ea) Range |
|---|---|---|---|---|---|
| IgG1 | 50-80 | 5, 25, 30, 33, 40 | 12-36 | Aggregation | Molecule-dependent |
| IgG2 | 150 | 5, 25, 30 | 36 | Aggregation | Molecule-dependent |
| Bispecific IgG | 150 | 5, 25, 40 | 18 | Aggregation | Molecule-dependent |
| Fc-fusion Protein | 50 | 5, 25, 35, 40, 45, 50 | 36 | Aggregation | Molecule-dependent |
| scFv | 120 | 5, 25, 30 | 18 | Aggregation | Molecule-dependent |
| Bivalent Nanobody | 150 | 5, 25, 30, 35 | 36 | Aggregation | Molecule-dependent |
| DARPin | 110 | 5, 15, 25, 30 | 36 | Aggregation | Molecule-dependent |
Workflow Visualization
Forced Degradation Study Workflow
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key reagents and materials for forced degradation studies [20] [47]
| Reagent/Material | Function in Forced Degradation | Typical Concentrations/ Conditions | Application Notes |
|---|---|---|---|
| Hydrochloric Acid (HCl) | Acid hydrolysis stress | 0.1M - 1.0M, 40-60°C | Neutralize before analysis to prevent continued degradation and column damage |
| Sodium Hydroxide (NaOH) | Base hydrolysis stress | 0.1M - 1.0M, 40-60°C | Neutralize before analysis to prevent continued degradation and column damage |
| Hydrogen Peroxide (H₂O₂) | Oxidative stress | 1-3%, 25-60°C | Typically shorter exposure times (24h maximum) to avoid over-degradation |
| Buffer Solutions | pH-specific degradation studies | pH 2, 4, 6, 8 buffers | Helps identify pH-specific degradation pathways |
| Azobisisobutyronitrile (AIBN) | Free radical oxidation studies | Variable concentrations, 40-60°C | Alternative oxidative stressor for specific degradation pathways |
| Size Exclusion Chromatography Column | Aggregate quantification in biologics | UHPLC compatible, 450Ã… pore size | Critical for monitoring high molecular weight species in protein therapeutics |
| Photodiode Array Detector | Peak purity assessment | Spectral range: 210-400 nm | Essential for spectral contrast analysis and peak homogeneity assessment |
| Einecs 260-048-5 | Einecs 260-048-5, CAS:56195-26-7, MF:C26H22N6O4, MW:482.5 g/mol | Chemical Reagent | Bench Chemicals |
| 3-Methylthiacyclohexane | 3-Methylthiacyclohexane, CAS:5258-50-4, MF:C6H12S, MW:116.23 g/mol | Chemical Reagent | Bench Chemicals |
Quality-by-Design (QbD) Approaches for Method Operational Design Ranges
Frequently Asked Questions (FAQs) on QbD Fundamentals
Q1: What is the core difference between a Traditional approach and a QbD approach to analytical method development?
A1: The core difference lies in being reactive versus proactive. A traditional, quality-by-testing (QbT) approach relies on univariate, one-factor-at-a-time (OFAT) experimentation and fixed parameters, often leading to methods that are not fully understood and may fail when variations occur [48] [49]. In contrast, Quality by Design (QbD) is a systematic, proactive approach that begins with predefined objectives. It uses risk assessment and multivariate experiments to build scientific understanding and control variability, ensuring method robustness throughout its lifecycle [50] [51] [49].
Q2: What are the key elements of an Analytical QbD (AQbD) framework?
A2: The AQbD framework consists of several interconnected elements, as outlined in ICH guidelines [50] [49]:
- Analytical Target Profile (ATP): A predefined summary of the method's requirements, defining what the method is intended to measure (e.g., accuracy, precision, specificity) [51] [49].
- Critical Quality Attributes (CQAs): Performance characteristics (e.g., resolution, tailing factor, analysis time) that must be within appropriate limits to ensure the method fulfills its ATP [50] [49].
- Risk Assessment: A systematic process (using tools like Ishikawa diagrams and FMEA) to identify and rank Critical Method Parameters (CMPs) whose variability can impact the CQAs [51] [49].
- Design Space (Method Operable Design Region - MODR): The multidimensional combination of CMPs demonstrated to provide assurance of quality. Operating within the MODR is not considered a change [52] [48].
- Control Strategy: Ongoing procedures to ensure the method performs as expected, such as system suitability tests (SSTs) and continuous monitoring [50] [51].
Q3: How is "Design Space" specifically defined and what is its regulatory significance?
A3: Per ICH Q8(R2), a Design Space is "The multidimensional combination and interaction of input variables (e.g., material attributes) and process parameters that have been demonstrated to provide assurance of quality" [52]. For an analytical method, this is often called the Method Operable Design Region (MODR) [48].
Its regulatory significance is substantial: working within the approved design space is not considered a change. Movement outside the design space is considered a change and would normally initiate a regulatory post-approval change process [52]. This provides operational flexibility.
Q4: What is the relationship between "Specificity" and "Selectivity" in the context of QbD?
A4: While sometimes used interchangeably, these concepts have distinct meanings crucial for method robustness:
- Specificity is the ideal, representing the ability of a method to assess the analyte unequivocally in the presence of other components, without any ambiguity [53]. A highly specific sensor (e.g., an antibody) binds to a single target and no other.
- Selectivity refers to the ability of a method to distinguish and quantify the analyte in the presence of other components, which may include impurities, degradants, or matrix. A selective method can resolve the analyte from these other entities, even if they are structurally similar [53]. In practice, most methods are selective rather than perfectly specific.
Q5: Why is multivariate experimentation (DoE) preferred over the OFAT approach in QbD?
A5: The traditional OFAT approach varies one factor while holding others constant. This fails to capture interactions between factors, which are common in complex analytical systems like HPLC [51] [49]. For example, the effect of changing pH might depend on the buffer concentration.
Design of Experiments (DoE) is a statistical tool that systematically varies all relevant factors simultaneously. This allows for the efficient identification of interactions and the modeling of the relationship between CMPs and CQAs, which is essential for defining a robust design space [50] [51].
Troubleshooting Guides for Common QbD Challenges
Challenge 1: Poor Method Robustness and Frequent System Suitability Test (SST) Failures
Symptoms: Method performance is highly sensitive to minor, unavoidable variations in parameters like mobile phase pH, column temperature, or buffer concentration, leading to out-of-specification (OOS) results and failed SSTs.
| Potential Root Cause | Investigation Protocol | Corrective & Preventive Actions (CAPA) |
|---|---|---|
| Inadequate Design Space [48] | 1. Audit the Development Data: Review the DoE used to establish the method's operating range. Was the range too narrow? Were key parameter interactions missed? 2. Conduct a Robustness Test: Using a fractional factorial DoE, deliberately vary CMPs (e.g., flow rate ±0.1 mL/min, temperature ±2°C, pH ±0.1 units) around the set points and measure the impact on CQAs (e.g., resolution of a critical pair). | 1. Redefine the Design Space: Use the new DoE data to establish a wider, more robust MODR where all CQAs are met. 2. Implement a Control Strategy: Tighten control on the most sensitive parameters (e.g., use a water bath for precise temperature control) and update SST criteria to better monitor method health [51]. |
| Uncontrolled Critical Material Attributes (CMAs) [50] | 1. Supplier/Column Variability: Test the method using batches of reagents from different suppliers or different columns of the same type (e.g., different lot numbers, same C18 chemistry). 2. Analyze Impact: Check for shifts in retention time, peak shape, or resolution. | 1. Strengthen CMA Definitions: In the method, explicitly specify the required material attributes (e.g., column endcapping type, silica purity, buffer salt grade). 2. Qualify Sources: Qualify specific suppliers and column lots during method validation to ensure consistency. |
Challenge 2: Inadequate Specificity/Selectivity for Complex Mixtures
Symptoms: Inability to resolve the analyte peak from impurities, degradants, or matrix components, leading to inaccurate quantification.
| Potential Root Cause | Investigation Protocol | Corrective & Preventive Actions (CAPA) |
|---|---|---|
| Insufficient Method Scouting & Screening [49] | 1. Re-evaluate the ATP: Was the complexity of the sample (e.g., related substances with closely related structures) fully considered when selecting the technique? 2. Technique Scouting: Test alternative separation modes (e.g., HILIC vs. Reversed-Phase) or different selective detectors (e.g., MS vs. UV). | 1. Apply AQbD from the Start: Use a structured screening DoE to evaluate different columns, mobile phase pH, and organic modifiers to find the most selective starting conditions [49]. 2. Leverage Alternative Selectivity: Consider using an array of selective but not perfectly specific sensors (e.g., lectins for glycan analysis) to build a discriminatory "fingerprint" for complex samples [53]. |
| Sub-Optimal Critical Process Parameters | 1. Model Verification: If a method model was developed, verify if the predicted "optimal" point truly provides the best separation for all critical peak pairs. 2. Forced Degradation Studies: Stress the sample (e.g., with heat, acid, base) to generate degradants and verify if the method can still resolve the analyte. | 1. Response Surface Modeling: Use a DoE to create a response surface model for resolution of the most critical peak pair. Use this model to find a new, more selective operating region. 2. Adjust CMPs: Fine-tune parameters known to impact selectivity, such as mobile phase pH in HPLC, which can dramatically alter the ionization state of analytes. |
Challenge 3: Managing the Transition from Research to Regulated Laboratory
Symptoms: A method developed in a research environment performs inconsistently or fails validation when transferred to a Quality Control (QC) laboratory due to differences in equipment, operators, or environmental conditions.
| Potential Root Cause | Investigation Protocol | Corrective & Preventive Actions (CAPA) |
|---|---|---|
| Lack of Ruggedness Testing [54] | 1. Gap Analysis: Compare all equipment, reagents, and environmental conditions (e.g., room temperature/humidity) between the development and receiving labs. 2. Intermediate Precision Study: Have multiple analysts in the receiving lab run the method on different days using different instruments. | 1. Incorporate Ruggedness into DoE: During method development, include factors like "analyst" and "instrument" as experimental variables in the DoE study to build ruggedness directly into the design space [55]. 2. Formal Method Transfer Protocol: Execute a formal method transfer protocol that includes a pre-defined acceptance criteria for the comparative testing. |
| Overly Restrictive Set Points [52] | Review the method documentation. Are only single set points specified for parameters (e.g., "pH 3.0") without any allowable operating range? | Define the MODR: Instead of a single set point, define and validate the method's MODR. This provides the QC lab with operational flexibility to make minor adjustments within the approved space to maintain performance without requiring a regulatory post-approval change [52] [48]. |
Essential Research Reagent Solutions and Materials
The following table details key materials and their functions in developing robust analytical methods using QbD principles.
| Item / Reagent | Function in QbD Method Development |
|---|---|
| Chromatography Columns (Various Chemistries) | The stationary phase is a primary CMA. Screening different chemistries (C18, C8, phenyl, HILIC) is crucial in the initial scouting phase to achieve the fundamental selectivity required for separation [49]. |
| Buffer Salts & pH Modifiers | These are CMPs that critically impact selectivity, particularly for ionizable compounds. Controlling buffer pH, concentration, and type (e.g., phosphate vs. acetate) is essential for robustness [51]. |
| Chemical Standards (Analytes, Impurities, Degradants) | High-purity reference standards are necessary to accurately define the ATP, identify critical peak pairs, and validate that CQAs like resolution and specificity are met throughout the design space. |
| Design of Experiments (DoE) Software | A critical non-reagent tool. Software platforms (e.g., JMP, Design-Expert) are used to create multivariate experiments, model the data, and visually define the design space and MODR [55]. |
| System Suitability Test (SST) Reference Mixture | A standardized mixture of the analyte and key impurities used to verify that the analytical system is performing adequately at the start of each run, forming a key part of the life cycle control strategy [51] [48]. |
Experimental Protocol: Defining an HPLC Design Space Using DoE
This protocol provides a detailed methodology for establishing a robust Design Space for a stability-indicating HPLC method for an Active Pharmaceutical Ingredient (API) and its related substances [49].
Objective: To develop a robust HPLC method capable of separating an API from its known impurities and degradants, and to define the MODR where the method consistently meets all CQAs.
Step 1: Define the Analytical Target Profile (ATP) The ATP states: "The method must be able to quantify the API and its five known related substances in a drug product with an accuracy of 95-105%, a precision of RSD <2.0%, and must demonstrate specificity against placebo components."
Step 2: Identify Critical Quality Attributes (CQAs) From the ATP, the following CQAs are defined for the chromatographic output:
- CQA 1: Resolution (Rs) between the critical pair (API and closest eluting impurity) ≥ 2.0.
- CQA 2: Tailing factor (Tf) for the API peak ≤ 1.5.
- CQA 3: Total run time ≤ 15 minutes.
Step 3: Risk Assessment to Identify Critical Method Parameters (CMPs)
- Tool: Fishbone (Ishikawa) Diagram and FMEA.
- Process: Brainstorm all potential factors (Mobile Phase, Column, Temperature, etc.). A risk filter is applied to score factors based on their potential impact on CQAs.
- Output: High-risk CMPs selected for DoE study:
- CMP 1: pH of aqueous buffer (e.g., range 2.5 - 4.5)
- CMP 2: Percentage of organic modifier at start of gradient (e.g., range 5 - 15%)
- CMP 3: Gradient time (e.g., range 20 - 40 minutes)
- CMP 4: Column temperature (e.g., range 25 - 45°C)
Step 4: Experimental Design (DoE) and Execution
- Design Selection: A Central Composite Design (CCD) is suitable for this number of factors, as it efficiently models curvature and interaction effects.
- Execution: Prepare mobile phases and samples according to the experimental matrix generated by the DoE software. Run all experiments in a randomized order to avoid bias.
Step 5: Data Analysis and Model Building
- Process: Input the experimental data (CMP values and the resulting CQA values) into the DoE software.
- Output: The software generates a mathematical model (transfer function) for each CQA. For example:
Resolution (Rs) = 5.2 + 0.8*(pH) - 0.5*(%Organic) + 0.3*(pH*%Organic)... - Validation: Check model validity using statistical parameters (e.g., R², p-value, lack-of-fit).
Step 6: Defining and Visualizing the Design Space (MODR)
- Process: Using the models and the software's optimization function, define the region of CMPs where all CQAs are simultaneously met (Rs ≥ 2.0, Tf ≤ 1.5, Time ≤ 15 min).
- Visualization: The MODR is visualized as an overlay of contour plots or a 3D surface plot. The green region in the diagram below represents the MODR for two CMPs, where all CQAs are fulfilled.
The following diagram illustrates the logical workflow for this AQbD process, from defining objectives to establishing a control strategy.
Troubleshooting Guides
Guide 1: Addressing Poor or Inconsistent Analyte Recoveries
- Problem: Recoveries of your target analyte are unacceptably low or show high variability between samples.
- Description: This is a common issue when matrix components interfere with the analyte's ability to bind to antibodies or the stationary phase during analysis, leading to inaccurate quantitative results [56].
- Diagnosis & Solutions:
- Check 1: Assess Matrix Effects. Perform a post-column infusion test to identify regions of ion suppression or enhancement in your chromatogram. Infuse a dilute solution of the analyte into the effluent from the LC column and monitor the signal; a dip or rise indicates co-eluting matrix components affecting detection [57].
- Check 2: Evaluate Sample Preparation. Inconsistent recoveries often stem from variable sample preparation. Ensure thorough mixing of samples after any freeze-thaw cycle to prevent protein aggregation or phase separation, which can lead to heterogeneous sampling [57].
- Solution: Implement Internal Standardization. Use a stable isotope-labeled analog of your analyte as an internal standard. This standard is added to every sample and calibrator, correcting for losses during sample preparation and variations in detector response due to matrix effects [57].
Guide 2: Managing High Background Contamination
- Problem: Samples show unacceptably high levels of interfering contaminants, complicating separation and quantification.
- Description: Complex sample matrices can introduce contaminants that co-elute with the analyte or cause high background noise, reducing method robustness [58].
- Diagnosis & Solutions:
- Check 1: Review Sample Cleanup. Inadequate cleanup is a primary cause. Re-evaluate your Solid-Phase Extraction (SPE) protocol, including the selection of sorbent, conditioning, washing, and elution steps [58].
- Check 2: Inspect Reagents and Vials. Ensure all solvents and reagents are of high purity. Check that vial septa are not leaking, as evaporation or contamination from the environment can occur if vials are not properly sealed [57].
- Solution: Optimize Solid-Phase Extraction (SPE). Use SPE as a routine cleanup step. Select a sorbent chemistry that selectively retains your analyte while allowing contaminants to pass through in the wash step. A well-optimized SPE method can significantly reduce background interference and improve method robustness [58].
Guide 3: Mitigating Matrix Effects in Detection
- Problem: The detector response for your analyte is suppressed or enhanced by the sample matrix, leading to inaccurate quantitation.
- Description: The "matrix effect" occurs when components in the sample matrix alter the detector's response to the analyte. This is a well-known challenge in techniques like Mass Spectrometry (MS), Fluorescence, and Evaporative Light Scattering Detection (ELSD) [57].
- Diagnosis & Solutions:
- Check 1: Compare Calibration Slopes. Prepare calibration curves in a pure solvent and in the sample matrix. A significant difference in the slopes indicates a matrix effect is influencing the detector response [57].
- Check 2: Identify the Source. Matrix effects can originate from the sample itself or from mobile phase components and their impurities [57].
- Solution: Employ Matrix-Matched Calibration. Prepare your calibration standards in the same matrix as your experimental samples. This accounts for the matrix effect during calibration, leading to more accurate results. Alternatively, sample dilution or buffer exchange can be used to reduce the concentration of interfering components [56].
Frequently Asked Questions (FAQs)
FAQ 1: What exactly is meant by "matrix effect" in quantitative LC-MS analysis? The matrix effect refers to the suppression or enhancement of the ionization of your target analyte in the mass spectrometer source due to the presence of co-eluting components from the sample matrix. These components compete for the available charge during the electrospray process, leading to inaccurate quantification [57].
FAQ 2: How can I experimentally prove my method is selective for my analyte in a complex matrix? Selectivity is demonstrated by showing that the analytical method can differentiate the analyte from other substances like impurities or excipients. According to ICH guidelines, this is typically achieved when the chromatographic resolution between the analyte peak and the closest potential interfering peak is greater than 2.0. This shows the method can practically distinguish the analyte from others, even if it is not 100% specific [59].
FAQ 3: What is the crucial difference between specificity and selectivity in method validation? Specificity is the ideal ability of a method to confirm the identity of an analyte unequivocally in the presence of other components. Selectivity refers to the method's ability to differentiate the analyte from other substances. A key distinction is that a method can be proven selective without being completely specific. However, if a method is specific, it is inherently also selective [59].
FAQ 4: My sample has a very different pH from the assay buffer. What is a quick fix? A practical solution is pH neutralization. You can neutralize your sample by adding a small volume of a concentrated buffering solution. This brings the sample into the ideal pH range for the assay, improving reliability and performance [56].
Experimental Protocols & Data Presentation
Table 1: Common Matrix Interferences and Mitigation Strategies
| Interference Type | Example Sources | Impact on Analysis | Recommended Mitigation Strategy |
|---|---|---|---|
| Ionization Suppression | Phospholipids, salts in biological samples [57] | Alters MS detector response, leading to inaccurate quantitation [57] | Use internal standard (e.g., stable isotope-labeled analog); optimize chromatographic separation [57] |
| Protein Binding | Serum, plasma samples [56] | Prevents analyte binding to antibodies or columns, causing low recovery [56] | Protein precipitation; dilution with compatible buffer; use of blocking agents [56] |
| Nonspecific Binding | Polymers, lipids in samples [56] | Causes high background noise and variable results [56] | Add blocking agents (e.g., BSA) to assay buffers; optimize antibody affinity [56] |
| pH Imbalance | Urine, cell culture media [56] | Disrupts antibody-antigen binding or column retention [56] | pH neutralization with buffering concentrates [56] |
Table 2: Key Sample Preparation Techniques for Clean-up
| Technique | Primary Function | Typical Use Case | Key Parameter to Optimize |
|---|---|---|---|
| Solid-Phase Extraction (SPE) | Selective enrichment and clean-up [58] | Removing contaminants from complex biological fluids prior to HPLC [58] | Sorbent chemistry (C18, ion-exchange, mixed-mode) and elution solvent strength [58] |
| Sample Dilution | Reducing interference concentration [56] | When the analyte is at a high concentration but the matrix causes interference [56] | Dilution factor and compatibility of dilution buffer with the assay matrix [56] |
| Buffer Exchange | Replacing the sample matrix [56] | Placing a sample from an incompatible buffer (e.g., high salt) into an assay-compatible buffer [56] | Molecular weight cut-off (MWCO) of exchange columns; buffer composition [56] |
| Centrifugation / Filtration | Removing particulate matter [56] | Clarifying turbid samples like soil extracts or food homogenates [56] | Centrifuge speed/filter pore size to retain debris while allowing analyte to pass [56] |
Protocol: Post-Column Infusion for Matrix Effect Assessment
Purpose: To visually identify regions of ion suppression or enhancement in a liquid chromatography method coupled with mass spectrometry (LC-MS) [57].
Materials:
- LC system with auto-sampler and column
- Mass Spectrometer
- T-connector (for post-column infusion)
- Syringe pump
- Dilute solution of the target analyte in a compatible solvent
- Blank matrix sample (e.g., drug-free plasma) and a processed standard
Methodology:
- Setup: Connect the outlet of the LC column to one port of the T-connector. Connect the syringe pump, loaded with the dilute analyte solution, to the second port. Connect the third port to the MS inlet.
- Infusion: Start the LC flow and the syringe pump at a constant rate, so a steady signal for the analyte is observed at the MS detector.
- Injection: Inject the blank matrix sample onto the LC column and start the chromatographic method.
- Data Acquisition: Monitor the MS signal of the infused analyte throughout the LC run time. A stable signal indicates no matrix effect. A depression in the signal indicates ion suppression, while a signal increase indicates ion enhancement, both caused by matrix components eluting from the column at that time [57].
Workflow Visualization
Sample Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for Mitigating Matrix Effects
| Item | Function & Purpose |
|---|---|
| Stable Isotope-Labeled Internal Standard | Corrects for analyte loss during preparation and detector response variation; the most effective way to compensate for matrix effects in quantitation [57]. |
| SPE Cartridges (C18, Mixed-Mode) | Selectively retain analytes based on hydrophobicity or ion exchange; used for sample clean-up and concentration, removing interfering contaminants [58]. |
| Blocking Agents (e.g., BSA) | Added to assay buffers to occupy nonspecific binding sites on surfaces or proteins, reducing background noise and improving signal-to-noise ratio [56]. |
| Buffer Exchange Columns | Desalting columns or spin filters with specific MWCO used to transfer the analyte from an incompatible sample matrix into an assay-friendly buffer [56]. |
| Matrix-Matched Calibrators | Calibration standards prepared in the same biological matrix as the unknown samples; essential for accurate quantification as they account for inherent matrix effects [56]. |
| Erbium trifluoroacetate | Erbium trifluoroacetate, MF:C6H3ErF9O6, MW:509.33 g/mol |
| 4-(11-Heneicosyl)pyridine | 4-(11-Heneicosyl)pyridine|CAS 50734-69-5 |
Solving Specificity Failures: Practical Troubleshooting and Risk Mitigation
Diagnosing and Resolving Co-elution and Matrix Interference Issues
In the pursuit of robust analytical methods, specificity and selectivity are paramount. Specificity refers to the ideal ability of a method to confirm the identity of an analyte unequivocally, even in the presence of other components, while selectivity is the practical capability to differentiate the analyte from other substances like impurities, excipients, or degradation products [59]. Co-elution and matrix interference represent two significant challenges that directly compromise these attributes. Co-elution occurs when two or more analytes exit the chromatography column at the same time, preventing their proper identification and quantification [60]. Matrix interference arises when extraneous components in a sample disrupt the detection of the target analyte, leading to signal suppression or enhancement and ultimately, inaccurate results [61] [62]. This guide provides a structured approach to diagnosing and resolving these critical issues, thereby enhancing the reliability of analytical data.
FAQ: Frequently Asked Questions
Q1: What is the fundamental difference between co-elution and matrix interference?
Co-elution is a chromatographic separation failure where two or more compounds have identical or very similar retention times, making them appear as a single, unresolved peak in the chromatogram [60]. Matrix interference, on the other hand, is a detection problem. It occurs when compounds from the sample matrix co-elute with the analyte and interfere with its detection in the mass spectrometer, typically causing ionization suppression or enhancement, even if the analyte is chromatographically resolved [63] [62].
Q2: How can I quickly check if a symmetrical chromatographic peak is pure or a hidden co-elution?
A symmetrical peak can be deceptive. To check for hidden co-elution:
- Use a Diode Array Detector (DAD): Collect multiple UV spectra (e.g., ~100) across the peak. If the spectra are not identical, it indicates a potential co-elution [60].
- Use Mass Spectrometry (MS): Take mass spectra at the upslope, apex, and downslope of the peak. A shifting mass spectral profile suggests co-eluting compounds [60].
- Look for Subtle Visual Cues: A shoulder on a peak—a sudden discontinuity—can be a visual indicator of co-elution, as opposed to a gradual exponential decline seen in tailing [60].
Q3: My method is sensitive to lot-to-lot variations in a biological matrix. Is this a matrix effect?
Yes, this is a classic sign of matrix effects. Different lots of a matrix (e.g., plasma from different donors) can contain varying levels of endogenous compounds like phospholipids, salts, or proteins. If these compounds co-elute with your analyte, they can cause variable ionization suppression or enhancement, leading to inconsistent results and poor method reproducibility [62].
Q4: Are there any ethical considerations when dealing with co-elution?
Ignoring a known co-elution is a serious ethical and scientific issue. Reporting data from unresolved peaks invalidates your results and can be considered a form of laboratory fraud, especially in regulated environments like EPA- or FDA-certified labs [64]. It is an ethical obligation to diagnose, report, and resolve co-elution problems to ensure data integrity.
Troubleshooting Guide: A Step-by-Step Diagnostic Approach
Diagnosing Co-elution
Co-elution can be obvious, as with a shoulder peak, or completely hidden. The table below summarizes the diagnostic techniques.
Table 1: Techniques for Diagnosing Co-elution
| Technique | Principle of Operation | What to Look For | Advantages & Limitations |
|---|---|---|---|
| Spectral Analysis (DAD) [60] | Collects full UV-Vis spectra across the chromatographic peak. | Differences in the spectral profile between the peak's start, apex, and end. | Advantage: Direct evidence of peak purity. Limitation: Requires a DAD detector. |
| Mass Spectrometric Analysis [60] | Collects mass spectra at different points across the peak. | Changes in the mass spectral fingerprint or ion ratios across the peak. | Advantage: Highly specific and sensitive. Limitation: Requires an MS detector. |
| Change of Chromatography | Deliberately alters a method parameter (e.g., mobile phase pH, gradient). | A single peak splits into two or more distinct peaks. | Advantage: Can be performed with standard HPLC equipment. Limitation: Indirect evidence. |
The following workflow outlines the logical process for diagnosing and investigating co-elution:
Diagnosing Matrix Interference in LC-MS
Matrix effects are a predominant concern in quantitative LC-MS. The following techniques are used to assess them.
Table 2: Techniques for Assessing Matrix Effects in LC-MS
| Technique | Experimental Protocol | Interpretation of Results |
|---|---|---|
| Post-Column Infusion [63] [62] | 1. Infuse a constant concentration of the analyte post-column into the MS.2. Inject a blank, prepared sample matrix extract.3. Monitor the analyte signal. | A dip or rise in the baseline signal indicates regions of ionization suppression or enhancement caused by co-eluting matrix components. This is a qualitative assessment. |
| Post-Extraction Spiking [63] [62] | 1. Prepare a neat standard in mobile phase (A).2. Prepare a blank matrix sample, extract it, and spike the analyte back in at the same concentration (B).3. Compare the MS responses of A and B. | % Matrix Effect = (B/A) × 100%A value of 100% means no effect; <100% indicates suppression; >100% indicates enhancement. This is a quantitative assessment. |
| Slope Ratio Analysis [62] | 1. Prepare a calibration curve in a neat solution.2. Prepare a matrix-matched calibration curve in the same blank matrix.3. Compare the slopes of the two curves. | % ME = [(Slopematrix / Slopeneat) - 1] × 100%This provides a semi-quantitative assessment of ME across a concentration range. |
The logical relationship and process for dealing with matrix interference are shown below:
Resolution Strategies and Experimental Protocols
Resolving Co-elution by Optimizing Chromatographic Parameters
The resolution of two peaks is governed by three factors: efficiency (N), capacity factor (k'), and selectivity (α) [60]. The troubleshooting approach is systematic.
Table 3: Troubleshooting and Resolving Co-elution
| Symptom | Suspected Issue | Actionable Fixes & Experimental Changes |
|---|---|---|
| Peaks are too early (k' < 1) | Low Capacity Factor | Weaken the mobile phase. In Reversed-Phase HPLC, reduce the organic solvent percentage. This increases retention, aiming for a k' between 1 and 5 [60]. |
| Peaks are broad | Low Efficiency | Increase column efficiency. Use a newer column with a smaller particle size (e.g., sub-2μm) or a longer column. Ensure the system is not poorly maintained (e.g., clogged frits, excessive void volume) [60]. |
| Good k' and N, but peaks still co-elute | Poor Selectivity | Change the chemistry. This is the most powerful approach. 1. Change Mobile Phase: Alter pH, switch buffer salts, or use ion-pairing reagents [60] [65]. 2. Change Stationary Phase: Move beyond C18. Try C8, biphenyl, phenyl-hexyl, amide, or HILIC columns to exploit different chemical interactions [60]. |
Experimental Protocol: Post-Column Infusion for Matrix Effect Assessment
This protocol helps identify chromatographic regions prone to ionization suppression/enhancement [63] [62].
Materials:
- LC-MS system with a post-column T-piece.
- Syringe pump for infusion.
- Standard solution of the analyte.
- Blank matrix samples (e.g., blank plasma extract).
Methodology:
- Infusion Setup: Connect the syringe pump, loaded with the analyte standard, to a T-piece installed between the HPLC column outlet and the MS ion source.
- Begin Infusion: Start a constant flow of the analyte standard into the MS. A stable signal baseline should be observed.
- Chromatographic Run: Inject the prepared blank matrix sample and run the chromatographic method as usual.
- Data Analysis: Observe the signal of the infused analyte. Note any significant deviations (dips or rises) from the stable baseline. These deviations correspond to the retention times where co-eluting matrix components are affecting ionization.
Strategies to Minimize or Compensate for Matrix Interference
A. Minimization Strategies (When sensitivity is crucial):
- Improve Sample Clean-up: Use more selective extraction techniques like solid-phase extraction (SPE) to remove interfering phospholipids and proteins [61] [62].
- Enhance Chromatographic Separation: Adjust the method to shift the analyte's retention time away from the region of major interference identified by post-column infusion [63]. This is the most effective way to minimize matrix effects.
- Dilute the Sample: Simple sample dilution can reduce the concentration of interfering compounds below the level that causes a significant effect, provided the method sensitivity allows it [61] [63].
- Optimize MS Parameters: In some cases, adjusting source temperatures or gas flows can mitigate effects.
B. Compensation Strategies (When a blank matrix is available):
- Stable Isotope-Labeled Internal Standard (SIL-IS): This is the gold standard. The SIL-IS co-elutes with the analyte and experiences identical matrix effects, perfectly correcting for them [63] [62].
- Matrix-Matched Calibration: Prepare calibration standards in the same blank matrix as the samples. This accounts for the average matrix effect but may not correct for variability between individual samples [61] [62].
- Standard Addition: Spike known amounts of analyte into aliquots of the sample itself. This method is useful for endogenous compounds or when a blank matrix is unavailable, but it is labor-intensive [63].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Reagents and Materials for Mitigating Co-elution and Matrix Effects
| Item | Function/Benefit | Common Examples / Notes |
|---|---|---|
| Alternative HPLC Columns | Provides different selectivity to resolve co-eluting compounds. | C18, C8, Biphenyl, Phenyl-Hexyl, Cyano, Amide, HILIC [60]. |
| Ion-Pairing Reagents | Allows retention and separation of ionic compounds on reversed-phase columns. | Tetra-n-butylammonium (TBA) for anions [65]; Alkyl sulfonates for cations. |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | The most effective way to compensate for matrix effects in quantitative LC-MS. | e.g., Creatinine-d3 for creatinine analysis [63]. Ideally, the SIL-IS differs by ≥ 3 Da. |
| SPE Cartridges | Removes matrix interferences during sample preparation, cleaning up the sample. | Reverse-phase, ion-exchange, and mixed-mode sorbents target different interferences [62]. |
| Protein Precipitation Solvents | Rapidly removes proteins from biological samples to reduce interference. | Acetonitrile, Methanol. Can be combined with phospholipid removal plates. |
| Chemical Cross-linkers | Prevents antibody co-elution in immunoprecipitation protocols. | Dimethyl Pimelimidate (DMP); commercial cross-linking kits [66]. |
Troubleshooting Guides
Common HPLC Issues and Solutions
Table 1: Troubleshooting Common HPLC Performance Problems [67] [68]
| Symptom | Possible Causes | Recommended Solutions |
|---|---|---|
| Broad Peaks | System not equilibrated; Injection solvent too strong; Injection volume/mass too high; Temperature fluctuations; Old or contaminated column [67]. | Equilibrate column with 10 volumes of mobile phase; Use weaker injection solvent; Reduce injection volume/mass; Use column oven; Replace guard cartridge or column [67]. |
| Tailing Peaks | Old guard cartridge; Injection solvent too strong; Injection volume/mass too high; Voided column [67]. | Replace guard cartridge; Ensure injection solvent is same or weaker strength than mobile phase; Reduce injection volume/mass; Replace column [67]. |
| Varying Retention Times | System not equilibrated; Temperature fluctuations; Pump not mixing solvents properly; Leaking piston seals [67]. | Equilibrate column with 10 volumes of mobile phase; Use thermostatically controlled column oven; Ensure proportioning valve works correctly; Replace leaking piston seals [67]. |
| High Backpressure | Particulate clogging at inlet frit or within column bed [68]. | Flush with strong solvent (e.g., 100% acetonitrile); For severe clogs, reverse flow direction as last resort [68]. |
| Extra Peaks | Degraded sample; Contaminated solvents; Contaminated guard cartridge or column [67]. | Inject fresh sample; Use fresh HPLC-grade solvents; Replace guard cartridge; Wash or replace column [67]. |
| No Peaks | Empty sample vial; System leak; Pump not mixing solvents properly; Damaged/blocked syringe; Old detector lamp [67]. | Inject fresh sample; Check/replace leaking tubing/fittings; Check proportioning valve; Replace syringe; Replace lamp (>2000 hours) [67]. |
Common GC Temperature Programming Issues and Solutions
Table 2: Troubleshooting GC Temperature Programming [69] [70]
| Symptom | Possible Causes | Recommended Solutions |
|---|---|---|
| Poor Early Peak Resolution | Incorrect initial temperature; Unsuitable for splitless injection [69]. | For split injection: Lower initial temperature by 20°C. For splitless: Set initial oven 20°C below solvent boiling point with 30s hold [69]. |
| Poor Mid-Chromatogram Resolution | Suboptimal ramp rate; Critical pair co-elution [70]. | Estimate optimum rate as 10°C per hold-up time; Insert mid-ramp isothermal hold at 45°C below critical pair elution temperature [69] [70]. |
| Long Run Time/Peak Broadening | Use of isothermal analysis for wide elution range; Final temperature too low [70]. | Switch to temperature programming; Set final temperature 20°C above elution temperature of last analyte [69] [70]. |
| Irreproducible Retention Times | Unoptimized method; Lack of robustness [70]. | Avoid excessive "fiddling"; If >10 adjustments don't yield robust method, consider changing stationary phase [70]. |
Optimization Methodologies
Mobile Phase Optimization for HPLC
The mobile phase is a powerful tool for manipulating selectivity in reversed-phase HPLC. The most efficient way to improve resolution is by optimizing selectivity, primarily influenced by the stationary phase and mobile phase composition [71].
Experimental Protocol: Systematic Mobile Phase Screening
- Select Organic Modifier Type: Begin by screening the three most common solvents—acetonitrile, methanol, and tetrahydrofuran—as they possess different solvatochromatic properties (acidity, dipole-dipole interactions, basicity) that significantly impact selectivity [72]. Use solvents from different selectivity groups on the selectivity triangle; solvents from groups far apart on the triangle guarantee the highest difference in selectivity [71].
- Optimize Modifier Concentration: For each modifier, prepare mobile phases with varying organic percentages (e.g., 30%, 50%, 70%). A 10% change in modifier concentration typically produces a 2–3-fold change in analyte retention [72]. Aim for a retention factor (k) between 2 and 10 for all analytes of interest [72].
- Adjust pH for Ionizable Analytes: When dealing with ionizable analytes, prepare buffers at different pH values, ensuring the pH is within ±1 pH unit of the buffer pKa for optimal capacity [72]. Use volatile buffers (e.g., ammonium formate) for LC-MS applications [72].
- Critical Note: When eluent pH is within 1 unit of an analyte's pKa, carefully control eluent pH to avoid retention and selectivity changes [72].
- Evaluate Temperature Effects: Investigate temperature as a variable (e.g., 25°C, 35°C, 45°C), as retention of ionizable analytes is most affected. Variations of just 5°C can profoundly affect selectivity [72].
- Assess Solubility: Ensure the optimized mobile phase completely solubilizes the sample without compromising other parameters like UV absorption or column pressure [71].
Figure 1: Mobile phase optimization workflow for HPLC methods.
Column Conditioning and Troubleshooting
Proper column care is essential for consistent performance and longevity [68].
Experimental Protocol: Column Washing and Equilibration
- Post-Use Washing:
- Strong Solvent Flush: Flush the column with 20–30 mL (or 10–20 column volumes) of a strong organic solvent (e.g., 100% acetonitrile or methanol) to remove strongly retained compounds [68].
- Storage Solvent Flush: Transition to your storage solvent (e.g., 70% methanol in water) and flush an additional 10–20 column volumes [68].
- Monitor Baseline: Continuously monitor system pressure and detector baseline during washing; consistent pressure and a stable, low baseline indicate effective cleaning [68].
- Column Equilibration:
- Flush the column with 10 column volumes of the mobile phase before analysis. For complex methods or gradients, more may be needed [68].
- The column is equilibrated when retention times, peak areas, and peak shapes for a standard analyte become consistent over several injections [68].
- Preventing Hydrophobic Collapse: Never store or extensively flush reversed-phase columns with 100% water, as this can cause "de-wetting." Always maintain at least 5–10% organic solvent [68].
GC Temperature Program Optimization
Temperature programming is critical for affecting selectivity (α) in GC separations [70]. The following protocol outlines a systematic approach to developing a robust temperature program.
Experimental Protocol: Developing a GC Temperature Program
- Initial Sample Screening:
- Column: Use a standard 5% Phenyl dimethylpolysiloxane column (30m x 0.25mm x 0.25μm) [70].
- Injection: Use split injection (100:1 ratio) with 1μL injection volume [70].
- Oven Program: 40°C initial, then ramp at 10°C/min to 330°C, hold for 10 min [70].
- Carrier Gas: Helium at 35 cm/sec or Hydrogen at 45 cm/sec [70].
- Isothermal or Gradient?: If peaks in the screening chromatogram elute within a window of less than one quarter of the gradient time, isothermal analysis may be possible. Otherwise, proceed with temperature programming [69] [70].
- Set Initial Temperature:
- Determine Ramp Rate: A excellent approximation for the optimum ramp rate is 10°C per hold-up time (t₀) of the system. Calculate t₀ from column dimensions and flow rate [70].
- Set Final Temperature and Time: Set the final temperature at 20°C above the elution temperature of the last sample component. A hold time of 3–5 times the column dead volume is typical [69] [70].
- Resolve Critical Pairs with Mid-Ramp Holds: If specific peaks co-elute, insert a mid-ramp isothermal section. The hold temperature is calculated as T(hold) = T(elution of critical pair) - 45°C. Empirically determine the hold length, starting with a 1-minute hold [69] [70].
Figure 2: GC temperature program optimization decision workflow.
Frequently Asked Questions (FAQs)
Q1: How can I quickly improve the resolution of a problematic HPLC separation? The most efficient way to improve resolution is to optimize selectivity by changing the mobile phase composition [71]. Switch to an organic modifier from a different selectivity group (e.g., from acetonitrile to methanol) or adjust the pH if you are dealing with ionizable analytes. Even small changes in selectivity can lead to large, desirable changes in resolution [71] [72].
Q2: My reversed-phase HPLC column is producing broad peaks and shifting retention times. What should I do? This often indicates the column requires washing and equilibration [68]. First, flush the column with 20-30 mL of a strong solvent (e.g., 100% acetonitrile). Then, equilibrate it with at least 10 column volumes of your mobile phase. If performance does not improve, the column may be contaminated or voided and could require replacement [67] [68].
Q3: When should I use an isothermal GC analysis versus a temperature program? If your screening analysis shows that all peaks of interest elute within a time window of less than one quarter of the gradient run time, isothermal analysis may be suitable [69] [70]. Isothermal analysis is simpler but can lead to broad later-eluting peaks. For samples with a wide boiling point range, temperature programming provides sharper peaks throughout the chromatogram and shorter run times [70].
Q4: What is "hydrophobic collapse" in HPLC, and how can I prevent it? Hydrophobic collapse (or "de-wetting") occurs when highly hydrophobic reversed-phase columns (like C18) are exposed to 100% aqueous mobile phases, causing the stationary phase pores to collapse and become inaccessible [68]. Prevent this by always maintaining at least 5-10% organic solvent in your mobile phase or storage solution. If de-wetting occurs, flush the column with a high concentration (95-100%) of a strong organic solvent to re-wet the pores [68].
Q5: How do I know if my GC temperature program ramp rate is optimal? A reliable approximation for the optimum ramp rate is 10°C per hold-up time (t₀) [70]. If you encounter poor separation, especially in the middle of the chromatogram, try halving or doubling the ramp rate to assess selectivity changes. If that fails, consider implementing a mid-ramp isothermal hold to resolve critical pairs [69] [70].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Chromatographic Method Development [67] [71] [68]
| Item | Function / Purpose | Key Considerations |
|---|---|---|
| HPLC Solvents (Acetonitrile, Methanol, THF) | Organic modifiers for reversed-phase mobile phases. | Each has different solvatochromatic properties; switching between them is the primary way to alter selectivity [71] [72]. |
| Volatile Buffers (Ammonium formate, Ammonium acetate) | Control mobile phase pH for ionizable analytes, especially in LC-MS. | Ensure concentration is 10-50 mM and pH is within ±1 unit of buffer pKa for effective capacity [72]. |
| Strong Solvents (Isopropanol) | Washing and reconditioning reversed-phase columns. | Used to remove strongly hydrophobic contaminants and recover de-wetted columns [68]. |
| Syringe Filters (0.2 μm) | Filter samples prior to HPLC injection. | Prevents insoluble materials and particulates from clogging the column inlet frit [68]. |
| Guard Cartridges | Protect the analytical column from contaminants. | Should be replaced when peak tailing or broadening occurs; must be of similar chemistry to the analytical column [67]. |
| Standard GC Columns (e.g., 5% Phenyl dimethylpolysiloxane) | Versatile stationary phase for initial method screening and development. | A good first choice for unknown samples; dimensions typically 30m x 0.25mm x 0.25μm [70]. |
| Deactivated Liners (for GC) | Sample vaporization chamber for GC injection. | A straight, deactivated, unpacked liner is often recommended for initial screening [70]. |
Addressing Method Sensitivity Problems with LOD/LOQ Optimization
Understanding LOD and LOQ: Core Definitions and Importance
What are the fundamental definitions of LOD and LOQ?
The Limit of Detection (LOD) is the lowest concentration of an analyte that can be reliably distinguished from a blank sample (containing no analyte) but not necessarily quantified with exact precision. Conversely, the Limit of Quantification (LOQ) is the lowest concentration that can be measured with acceptable precision and accuracy under stated experimental conditions [73] [74].
These parameters are critical for validating analytical methods, especially in regulated industries like pharmaceuticals, where they ensure methods are "fit for purpose" for detecting and quantifying trace impurities, degradation products, or low-dose active ingredients [74] [75].
How are LOD and LOQ mathematically determined?
Several established mathematical models exist for calculating these limits. A common approach uses the standard deviation of the response and the slope of the calibration curve [73]. The formulas are typically:
- LOD = 3.3 × σ / S
- LOQ = 10 × σ / S
Where σ is the standard deviation of the response (often from the blank or a low-concentration sample) and S is the slope of the calibration curve [73]. An alternative, simpler approach uses the signal-to-noise ratio, defining LOD at a ratio of 3:1 and LOQ at 10:1 [73] [75]. It is crucial to note that due to the high experimental uncertainty at these low concentrations, LOD and LOQ values should generally be reported with only one significant digit [76].
Optimization Strategies: Improving Your Method's Sensitivity
How can I optimize my HPLC method to achieve a lower LOD/LOQ?
Achieving lower detection and quantification limits often involves increasing the signal from your analyte relative to the system's background noise (improving the signal-to-noise ratio) [77].
Table 1: Strategies for HPLC Method Optimization to Improve LOD/LOQ
| Optimization Target | Strategy | Key Consideration |
|---|---|---|
| Peak Sharpening | Switch from an isocratic to a gradient elution [77]. | Gradient runs often produce narrower, higher peaks, improving the signal-to-noise ratio. |
| Column Dimensions | Use a column with a smaller inner diameter (e.g., 3 mm vs. 4.6 mm) and/or smaller particle size (e.g., 3 μm vs. 5 μm) [77]. | This increases efficiency and peak height. Remember to adjust the flow rate to maintain linear velocity and avoid high backpressure. |
| Column Chemistry | Consider core-shell (fused-core) particles [77]. | These particles can provide efficiency similar to smaller fully porous particles but with lower backpressure, leading to narrower peaks. |
| Detector Parameters | Optimize detector settings like slit width and response time [78]. | A wider slit allows more light, reducing noise. A longer response time can filter high-frequency noise. Balance this with potential loss of spectral resolution or peak distortion. |
| Sample Concentration | Increase injection volume or pre-concentrate the sample [78]. | Be wary of column overloading, which can cause peak broadening or tailing, negating the benefits [8] [78]. |
The following workflow visualizes a systematic approach to optimizing your method's sensitivity:
Troubleshooting Common Problems: An FAQ Guide
During validation, I found the LOQ to be unacceptably high (e.g., 4%). What can I do?
This is a common challenge. First, confirm the analytical purpose. For a potency assay with a range of 80-120%, a 4% LOQ may be acceptable. However, for an impurity method requiring quantification at 0.2%, it is not [78]. To improve the LOQ, you can:
- Reduce Baseline Noise: Ensure mobile phases are freshly prepared and degassed. Check for detector lamp failure or a contaminated flow cell [8].
- Increase Analyte Signal: As shown in Table 1, consider using a column with a smaller internal diameter or different particle technology. Adjusting the detection wavelength to the analyte's maximum absorbance can also enhance the signal [78].
- Adjust Instrument Settings: Increasing the detector's response time can smooth high-frequency noise, and widening the slit width can increase light throughput, both improving the signal-to-noise ratio [78]. Always verify that these changes do not negatively impact peak shape or data integrity.
My peaks are broad or tailing, which hurts sensitivity. How can I fix this?
Broad peaks reduce peak height, which is critical for a good signal-to-noise ratio. Common fixes include [8]:
- Modify Mobile Phase Composition: Adjust the organic solvent ratio or pH. For reversed-phase HPLC, adding buffer to the mobile phase can improve peak shape.
- Address Column Issues: A contaminated or overloaded column can cause broadening and tailing. Try flushing the column with a strong solvent or reducing the injection volume. If the problem persists, the column may need replacement.
- Optimize Method Parameters: Ensure the column temperature is controlled and appropriate. Check for excessive tubing volume between the column and the detector.
My baseline is noisy, making it hard to identify peaks near the LOD. What are the common causes?
Baseline noise directly impacts the ability to detect low-concentration analytes. Frequent causes and solutions include [8]:
- Air Bubbles: Degas all mobile phases thoroughly and purge the system.
- Leaks: Check for loose fittings, especially before the detector, and tighten them gently.
- Contaminated Mobile Phase or System: Prepare fresh mobile phase and flush the system, including the detector flow cell, with a strong organic solvent.
- Worn-out Components: A UV lamp nearing end-of-life will produce increased noise and should be replaced.
Calculation and Validation: Ensuring Regulatory Compliance
What are the different approaches to calculating LOD and LOQ, and how do they compare?
Different guidelines recommend slightly different approaches, which can lead to varying results. A recent study comparing calculation methods for an HPLC-UV method found that the signal-to-noise ratio method yielded the lowest LOD/LOQ values, while the standard deviation of the response and slope method gave the highest values [79]. This highlights the importance of specifying and justifying the chosen calculation method in validation reports.
Table 2: Comparison of LOD/LOQ Calculation Methods
| Method | Description | Key Advantage | Common Guideline Reference |
|---|---|---|---|
| Signal-to-Noise (S/N) | LOD = 3:1 S/N, LOQ = 10:1 S/N. | Simple, intuitive, and directly measured from the chromatogram. | FDA, ICH [73] [75] |
| Standard Deviation of Blank and Slope | Uses standard deviation of blank measurements and calibration curve slope (LOD=3.3σ/S). | Based on statistical principles of the blank's response. | ICH Q2(R1) [73] |
| Calibration Curve (Statistical) | Uses the standard error of the regression and the slope of the calibration curve. | Leverages data from the entire calibration range, not just the blank. | EURACHEM, IUPAC [80] |
The diagram below illustrates the statistical relationship between the blank, LOD, and LOQ, and how they are derived from the distribution of measurements:
What is required for regulatory compliance when validating LOD and LOQ?
Regulatory bodies like the FDA and ICH have specific expectations. The ICH Q2(R1) guideline requires the parameter "specificity" for identification, impurity, and assay tests, which ensures the method can assess the analyte unequivocally in the presence of potential interferents [81]. While the guideline allows for multiple calculation approaches, the chosen method must be clearly documented [73] [79]. For bioanalytical methods, the FDA may require the Lower Limit of Quantification (LLOQ) to be defined with a signal-to-noise ratio greater than 10:1 and with precision and accuracy within ±20% [79].
Experimental Protocols: A Step-by-Step Guide
Protocol 1: Determining LOD and LOQ via Signal-to-Noise Ratio
This is a direct and commonly used method.
- Instrument Preparation: Ensure the HPLC system is equilibrated and stable. Perform system suitability tests to confirm performance.
- Baseline Recording: Inject a blank sample (e.g., the sample matrix without the analyte) and record the chromatogram for a period that covers the expected retention time of your analyte.
- Noise Measurement: On the chromatogram, select a region of the baseline near the analyte's retention time. Measure the peak-to-peak noise (N) over a defined time window.
- Low-Concentration Standard Injection: Inject a standard with a known, low concentration of the analyte.
- Signal and Noise Calculation: Measure the height of the analyte peak (S) from the low-concentration standard. Calculate the signal-to-noise ratio (S/N).
- Calculation: The concentration that yields an S/N of 3 is the LOD. The concentration that yields an S/N of 10 is the LOQ. If your standard does not give these exact ratios, use interpolation from multiple concentrations.
Protocol 2: Determining LOD and LOQ via Standard Deviation of the Blank and Calibration Curve
This method is based on ICH recommendations [73].
- Blank Analysis: Measure at least 10-20 replicate blank samples. The blank should be commutable with the actual patient or sample specimens [74].
- Low-Level Sample Analysis: Prepare and analyze at least 10-20 replicates of a sample known to contain a low concentration of the analyte (near the expected LOD) [74].
- Calibration Curve: Generate a calibration curve with a minimum of 5 concentration points across your expected range, including the low end.
- Calculation:
- Calculate the standard deviation (σ) of the responses from the blank or the low-concentration sample.
- From the calibration curve, obtain the slope (S).
- Apply the formulas: LOD = 3.3 × σ / S and LOQ = 10 × σ / S [73].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagents and Materials for Sensitivity Optimization
| Item | Function in LOD/LOQ Optimization |
|---|---|
| HPLC Grade Solvents | High-purity solvents minimize baseline noise and ghost peaks caused by UV-absorbing impurities [8]. |
| Core-Shell Chromatography Columns | Provides high efficiency and sharp peaks, improving signal height and resolution without the high backpressure of sub-2μm fully porous particles [77]. |
| Matrix-Matched Blank Samples | Critical for accurately determining the baseline signal and noise contribution from the sample itself, leading to correct LOD/LOQ calculations [80] [75]. |
| Certified Reference Materials | Used to prepare accurate calibration standards and spiked samples for validating the precision and accuracy at the LOQ level [75]. |
| Sensitive Detectors (e.g., MS, FLD) | For UV detectors, a new, high-energy lamp is essential. Mass spectrometry or fluorescence detection often provides inherently lower LOD/LOQ than UV for many compounds [78]. |
Implementing Risk-Based Approaches to Prioritize Critical Variables
Troubleshooting Guides
Challenges in Defining the Analytical Target Profile (ATP)
| Problem | Possible Root Cause | Recommended Solution | Regulatory Reference |
|---|---|---|---|
| Unclear ATP parameters | Insufficient prior knowledge of the product or method technology [82]. | Develop ATP from specific Critical Quality Attributes (CQAs) in the Quality Target Product Profile (QTPP). Define what is measured and the required performance criteria upfront [82]. | ICH Q14 [82] [83] |
| Difficulty selecting a technology to meet the ATP | Multiple technologies may satisfy the ATP, requiring extensive initial scouting [82]. | Invest in early experimentation to evaluate candidate methodologies. Leverage platform technologies for common product types (e.g., monoclonal antibodies) to reduce risk [82]. | - |
Challenges in Risk Assessment and Control Strategy
| Problem | Possible Root Cause | Recommended Solution | Regulatory Reference |
|---|---|---|---|
| Inability to identify Critical Method Parameters (CMPs) | Lack of structured experimentation to understand the relationship between method parameters and performance [82]. | Use risk assessment tools (e.g., Ishikawa diagrams, FMEA) and Design of Experiments (DoE) to identify CMPs and their impact [82]. | ICH Q9 [82] |
| Method performance is unstable during routine use | Inadequate control strategy; failure to manage Established Conditions (ECs) and monitor performance continuously [82]. | Implement system suitability tests (SST) and sample suitability tests. Establish a continuous monitoring system for method outputs to quickly detect out-of-trend (OOT) results [82]. | ICH Q12 [82] |
| Determining the risk level of a software function in an automated method | Uncertainty in applying a risk-based approach to computerized systems [84]. | For software, determine if a failure would directly cause a quality problem compromising safety. Functions controlling critical process parameters (e.g., temperature) are typically high risk [84]. | FDA CSA Guidance [84] |
Challenges Related to Method Performance and Complexity
| Problem | Possible Root Cause | Recommended Solution | Regulatory Reference |
|---|---|---|---|
| Method works for simple but not complex samples (e.g., biologics) | High sample complexity and heterogeneity (e.g., from post-translational modifications) overwhelm the method's selectivity [85]. | Employ orthogonal analytical techniques (e.g., LC-MS combined with capillary electrophoresis) to fully characterize the product and verify method specificity [85]. | - |
| Difficulty measuring polydisperse or non-spherical nanoparticles | The analytical technique is biased towards certain particle sizes or shapes [86]. | Use techniques suitable for polydisperse systems, such as Analytical Centrifugation or Nanoparticle Tracking Analysis (NTA), instead of Dynamic Light Scattering (DLS) alone [86]. | - |
| Method requires mid-stream change after validation | Process changes, obsolete reagents, or new technology may render the original method unsuitable [7]. | Execute a revalidation (from partial to full) and submit the necessary amendments to the regulatory filing. Provide method comparability data [7]. | FDA Guidance [7] |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between a traditional and a risk-based approach to analytical method development?
The traditional approach focuses on meeting immediate performance criteria with limited experimentation. In contrast, the risk-based enhanced approach, as outlined in ICH Q14, is a proactive and systematic lifecycle process. It begins with an Analytical Target Profile (ATP), uses risk assessment and Design of Experiments (DoE) to identify Critical Method Parameters (CMPs), and establishes a control strategy with Defined Ranges (e.g., Proven Acceptable Ranges (PAR)) for these parameters. This creates a more robust and well-understood method [82].
Q2: When during drug development should an analytical method be validated?
Method validation should be "phase-appropriate." For early-phase clinical trials (e.g., Phase I), a proper validation is a GMP requirement and FDA expectation. However, the full validation against commercial specifications is typically completed 1-2 years prior to the commercial license application, coinciding with process validation [7]. The concept of "phase-appropriate validation" allows for the validation rigor to align with the clinical development stage [7].
Q3: How can Quality by Design (QbD) principles be applied to analytical method development?
Applying QbD to analytical methods involves:
- Defining an ATP: Establishing the required performance of the method before development begins [82].
- Systematic Understanding: Using risk assessment and DoE to understand the relationship between method inputs (parameters) and outputs (performance) [82].
- Establishing a Design Space: Defining the multidimensional combination of method parameters that ensure quality, known as the Method Operable Design Region (MODR) [82].
- Implementing a Control Strategy: Using system suitability tests and continuous monitoring to ensure the method remains in a state of control throughout its lifecycle [82].
Q4: Our method failed after a minor instrument change. How could this have been prevented?
This is a classic symptom of a method that lacked robustness testing during development. To prevent this, a robustness study should be conducted during method optimization. This involves deliberately introducing small, plausible variations to method parameters (e.g., mobile phase pH ±0.2, flow rate ±10%, column temperature ±5°C) and confirming the method's performance remains within acceptance criteria. This helps define the method's robustness and establishes permissible ranges for system suitability tests [83].
Q5: What should we do if a more advanced analytical technology becomes available after our method is approved?
Regulators encourage method improvements. You can change to a more advanced method (e.g., one that is faster or more sensitive) after providing sufficient qualification/validation data for the new method and demonstrating comparability to the original method. In some cases, product specifications may need to be re-evaluated. This change would be managed through post-approval change regulatory procedures [7].
Experimental Protocols and Workflows
Core Workflow for Risk-Based Analytical Procedure Development
The following diagram illustrates the integrated lifecycle for developing and managing analytical procedures under a risk-based framework, aligning with regulatory guidelines like ICH Q14.
Protocol for a Robustness Study Using a Risk-Based Approach
1. Objective: To evaluate the analytical method's robustness by determining its sensitivity to small, deliberate variations in method parameters and to establish a control strategy for system suitability.
2. Pre-Study Requirements:
- A finalized, optimized method procedure.
- Identification of potential Critical Method Parameters (CMPs) via a prior risk assessment (e.g., FMEA). Typical parameters for a chromatographic method include:
- Mobile Phase pH
- Percent Organic Solvent in Mobile Phase
- Column Temperature
- Flow Rate
- Different Column Batches or Brands
3. Methodology:
- Experimental Design: Utilize a structured approach like Design of Experiments (DoE), such as a Full or Fractional Factorial design, to efficiently study the interaction effects of multiple parameters simultaneously [82].
- Parameter Ranges: Define a realistic range for each parameter (e.g., pH ±0.2 units, flow rate ±10%).
- Response Monitoring: For each experimental run, analyze a system suitability standard and a sample. Record critical responses such as:
- Resolution (Rs) between critical peak pairs.
- Tailing Factor (Tf).
- Theoretical Plates (N).
- Retention Time (tR).
- Peak Area %RSD from replicate injections.
4. Data Analysis:
- Analyze the data using statistical software to determine which parameters have a significant effect on the critical responses.
- Establish the Proven Acceptable Range (PAR) or Method Operable Design Region (MODR) for each critical parameter.
5. Output and Implementation:
- Define System Suitability Criteria: Based on the results, set justified acceptance criteria for system suitability tests to ensure the method performs as validated during routine use [82] [83].
- Document Established Conditions: Document the PARs/MODRs for critical parameters as part of the method's Established Conditions (ECs) for regulatory submissions [82].
The Scientist's Toolkit: Key Research Reagent Solutions
| Category | Item / Solution | Function / Explanation |
|---|---|---|
| Risk Management Tools | Ishikawa (Fishbone) Diagram | A visual tool used to brainstorm and categorize all potential sources of method variation (e.g., Man, Machine, Method, Material) during initial risk assessment [82]. |
| Failure Mode and Effects Analysis (FMEA) | A systematic, proactive method for evaluating a process to identify where and how it might fail and to assess the relative impact of different failures, helping to prioritize CMPs [82]. | |
| Experimental Design | Design of Experiments (DoE) Software | Software that enables the structured design and statistical analysis of experiments to efficiently optimize methods and understand parameter interactions, a core part of the QbD approach [82]. |
| Separation Techniques | Orthogonal Analytical Columns | Having columns with different chemistries (e.g., C18, Phenyl, HILIC) is crucial for scouting and demonstrating method specificity, especially for complex molecules like biopharmaceuticals [85] [83]. |
| Reference Materials | Primary and Working Reference Standards | Well-characterized standards are essential for method development, qualification, and validation. A two-tiered system (primary vs. working) is recommended by regulators to ensure traceability and consistency [7]. |
| Data Management | Laboratory Information Management System (LIMS) | Software that helps manage method data, including system suitability test (SST) results. It is vital for the continuous monitoring and trending required for lifecycle management [82]. |
Managing Method Changes and Mid-Stream Modifications
Frequently Asked Questions (FAQs)
1. When is it acceptable to change an analytical method mid-stream during product development? Methods can be changed at any time during or after product development to implement faster, more sensitive, accurate, or reliable techniques [7]. Such changes are often encouraged by regulators [7]. The key requirement is to provide sufficient qualification or validation data for the new method, alongside evidence of method comparability to demonstrate that the new method is at least equivalent to the old one [7]. In some cases, product specifications may need to be re-evaluated [7].
2. What is the regulatory expectation for validating a modified method? The extent of revalidation depends on the nature and scope of the changes [7]. It can range from a simple verification, demonstrating the method still performs as intended, to a full validation for significant changes [7]. Any modifications that impact the original regulatory submission must be documented with all appropriate amendments filed [7]. The validation should follow a "fit-for-purpose" approach, with requirements typically increasing as the product moves toward commercialization [87].
3. At what point in the drug development timeline should analytical methods be fully validated? For most biopharmaceuticals, full method validation is typically executed against the commercial specifications prior to process validation [7]. This is usually completed one to two years prior to the commercial license application to allow for sufficient real-time stability data [7]. It is a GMP requirement that methods are properly validated for any GMP activity, even to support Phase I studies, applying a "phase-appropriate validation" concept [7].
4. How can we efficiently manage method changes when working with multiple testing sites? Covalidation is an efficient approach where at least two laboratories together validate a method [87]. The primary laboratory performs a full validation and includes receiving laboratories in specific parts of the validation study, such as intermediate precision or quantitation limit verification [87]. All data is then combined into a single validation package, validating all laboratories simultaneously and avoiding a separate, lengthy transfer process [87].
Key Experimental Protocols for Method Changes
Protocol 1: Conducting a Method Comparability Study When a method is changed, demonstrating comparability between the old and new methods is critical [7].
- Objective: To prove that the new method provides results that are equivalent or superior to the original method.
- Methodology:
- Sample Selection: Select a representative set of samples that cover the expected range of the analyte, including samples from different stages of the process and samples with known impurities or degradation products.
- Testing: Analyze all selected samples using both the original and the modified method. The testing should be performed in a manner that allows for a direct comparison, ideally using the same sample preparations where possible.
- Data Analysis: Use statistical tools (e.g., linear regression, t-tests) to compare the results from both methods. The acceptance criteria for comparability should be pre-defined based on the method's purpose and the product's critical quality attributes.
- Outcome: A documented report showing that the new method is comparable to the original method, supporting the change.
Protocol 2: Specificity Testing via Spiking Study for an Impurity Method This protocol is essential for validating the specificity of a method, particularly for impurity testing, and is a common requirement when modifying methods for complex products [87] [88].
- Objective: To demonstrate that the method can accurately measure the analyte of interest in the presence of other components, such as process-related impurities or degradation products.
- Methodology (for Size-Exclusion Chromatography - SEC):
- Obtain Spiking Material: Generate stable impurities (e.g., aggregates and low-molecular-weight species) in sufficient quantities. This can be achieved through forced-degradation studies (e.g., controlled oxidation for aggregates, reduction for LMW species) or by collecting fractionated impurities from a purification process [87].
- Prepare Spiked Samples: Spike the main product sample with known amounts of the generated impurity material across a relevant concentration range (e.g., from low to high percentages) [87].
- Analysis and Calculation: Analyze the spiked samples and calculate the recovery of the impurity. For example, good accuracy is demonstrated with 90–100% recovery for aggregates and 80–100% for LMW species [87].
- Outcome: Data proving the method's specificity and accuracy in quantifying impurities, which is crucial for regulatory acceptance of the modified method [88].
Data Presentation: Core Validation Parameters
The following table summarizes the key parameters, as defined by ICH Q2(R1), that should be considered when revalidating a modified analytical method [89].
| Validation Parameter | Experimental Objective | Typical Acceptance Criteria |
|---|---|---|
| Specificity [89] [88] | Demonstrate measurement of analyte without interference from other components. | Analyte peak is well-resolved from impurities/degradants. No cross-signal contribution in LC-MS/MS [88]. |
| Accuracy [89] | Determine the closeness of results to the true value. | Recovery of 98–102% for the API. |
| Precision [89] | Assess the degree of repeatability under normal operating conditions. | Low Relative Standard Deviation (RSD) for repeatability; demonstrates consistency across analysts/days for intermediate precision. |
| Linearity [89] | Establish a proportional relationship between result and analyte concentration. | Correlation coefficient (R²) ≥ 0.999 across a specified range. |
| Robustness [89] | Measure the method's capacity to remain unaffected by small, deliberate parameter variations. | Consistent performance (e.g., retention time, resolution) with small changes in flow rate, temperature, or mobile phase pH. |
Workflow and Relationship Diagrams
Method Change Control Workflow
Analytical Method Lifecycle
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item / Reagent | Critical Function in Method Management |
|---|---|
| Forced-Degradation Samples | Used in specificity testing to generate impurities and degradation products, proving the method can resolve the analyte from its potential impurities [87]. |
| Stable Reference Standards | Provide a known and consistent baseline for comparability studies during a method change, ensuring results are traceable and accurate [7]. |
| System Suitability Test Mixtures | Verify that the modified method and the instrument system are performing as expected each day they are used, a key step after any method change [89]. |
| Platform Assay Reagents | For common product types (e.g., monoclonal antibodies), using pre-validated platform reagents can significantly speed up method modification and validation [7] [87]. |
Demonstrating Method Reliability: Validation Protocols and Comparative Assessment
Designing Comprehensive Validation Protocols for Specificity and Selectivity
FAQ 1: What is the fundamental difference between specificity and selectivity?
| Term | Definition | Key Analogy | Primary Application Context |
|---|---|---|---|
| Specificity | The ability of a method to assess the analyte unequivocally in the presence of components that may be expected to be present [81]. | Using a single key that fits only one specific lock [81]. | Official guidelines like ICH Q2(R1); often used for identification tests where the goal is to confirm a single analyte's identity [90] [81]. |
| Selectivity | The ability of the method to measure and differentiate the analytes in the presence of components that may be expected to be present, such as endogenous matrix components [81] [91]. | Identifying every single key on a keyring, not just the one that opens the door [81]. | Bioanalytical method validation; methods that quantify multiple analytes and need to distinguish them from a complex background [92] [91]. |
In many modern contexts, selectivity is the preferred term, as it is widely recognized that very few analytical methods are truly specific for a single analyte in all possible scenarios. IUPAC recommends using selectivity to avoid confusion, as it is a term that can be graded, whereas specificity is considered absolute [93] [94].
Figure 1: Specificity vs. Selectivity Conceptual Workflow
FAQ 2: How do I experimentally demonstrate specificity for a chromatographic assay?
For a chromatographic method like HPLC, demonstrating specificity involves proving that the analyte peak is pure and free from co-elution with other potential components.
Detailed Experimental Protocol:
- Generate a Stress Sample: Subject your drug substance or product to stress conditions such as strong acid, strong base, oxidation, heat, and light to force degradation [90].
- Analyze Stressed and Unstressed Samples: Inject the following samples into the chromatographic system:
- Blank Matrix: The sample matrix without the analyte (e.g., placebo formulation or biological fluid) to identify interfering peaks from the matrix itself.
- Unstressed Sample (Control): The sample containing the analyte to establish the normal chromatographic profile.
- Stressed Sample: To observe potential degradation products and demonstrate that the analyte peak is resolved from them.
- Sample Spiked with Interferents: If available, spike the sample with known impurities, excipients, or structurally similar compounds to show they do not interfere with the analyte peak [90] [81].
- Evaluate Critical Resolution: For critical separations, specificity is demonstrated by the resolution of the two components that are most challenging to separate. The resolution factor (Rs) should meet predefined acceptance criteria [90] [81].
- Perform Peak Purity Assessment: Use advanced detection methods like Photodiode-Array (PDA) detection or Mass Spectrometry (MS). The PDA detector collects UV spectra across the entire analyte peak. Software is then used to compare these spectra; a pure peak will have homogeneous spectra throughout. MS detection provides even more definitive proof of purity by confirming a single mass throughout the peak [90].
Troubleshooting Guide:
| Issue | Potential Cause | Suggested Solution |
|---|---|---|
| Co-elution of peaks | Inadequate chromatographic separation. | Optimize the mobile phase (pH, composition, gradient) or change the chromatographic column. |
| Poor peak shape | Secondary interactions or column issues. | Use a different column chemistry (e.g., C18 vs. phenyl), add modifiers to the mobile phase, or ensure the column is in good condition. |
| PDA cannot confirm peak purity | Low analyte concentration, spectral similarity, or high system noise. | Concentrate the sample if possible, or use the more powerful orthogonal technique of Mass Spectrometry (MS) for confirmation [90]. |
FAQ 3: How is selectivity validated for a biomarker immunoassay?
Validating selectivity in biomarker assays is complex because the analyte is endogenous, making traditional spike-recovery experiments insufficient. The core scientific question shifts to confirming that the assay's critical reagents (like antibodies) recognize both the standard calibrator material and the endogenous analyte in the same way [92].
Detailed Experimental Protocol:
- Source Individual Matrix Samples: Collect a minimum of 10 individual samples of the biological matrix (e.g., serum, plasma, CSF) from relevant donors. These should cover the expected biological variation [92] [91].
- Prepare Spiked and Native Samples:
- For each individual matrix, prepare two sets of samples:
- Set A (Spiked): Spike the sample with a known concentration of the analyte standard.
- Set B (Native): Use the sample at its native, unspiked concentration.
- For each individual matrix, prepare two sets of samples:
- Perform Parallelism Studies: This is the cornerstone of biomarker selectivity. Create a series of dilutions for both the spiked and native samples using an appropriate diluent. Also, prepare a standard calibration curve in a substitute matrix (like buffer) [92] [91].
- Analyze and Compare: Run all diluted series and the standard curve in the same assay.
- Evaluate for Parallelism: The dilution curves of the spiked and native samples should be parallel to the standard calibration curve. This demonstrates that the assay responds to the analyte in the complex biological matrix in the same way it responds to the pure standard, confirming the method's selectivity [92].
Figure 2: Biomarker Assay Selectivity Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Material | Critical Function in Validation |
|---|---|
| Chemical Reference Standards | Provides the benchmark for identity, purity, and quantity. Used to prepare calibrators for accuracy, linearity, and range studies [90]. |
| Certified Reference Material (CRM) | An essential material with accepted reference values for establishing method trueness (accuracy) and traceability [91]. |
| Well-Characterized Impurities & Degradants | Used to spike samples and directly challenge the specificity/selectivity of the method by proving resolution from the main analyte [90]. |
| Critical Reagents (e.g., Antibodies, Enzymes) | The core biological components of immunoassays. Their quality and stability are paramount, and their performance must be validated through parallelism studies [92] [91]. |
| Appropriate Biological Matrix | The blank or individual samples of the actual sample material (e.g., plasma, urine, tissue homogenate) are required to assess matrix effects and validate selectivity [92] [91]. |
FAQ 4: What are common challenges in validating specificity/selectivity and how are they solved?
| Challenge | Root Cause | Proven Solution |
|---|---|---|
| Inability to separate critical pair | The physicochemical properties of the analyte and interferent are too similar. | Employ an orthogonal separation mechanism (e.g., switch from reversed-phase to HILIC) or use a different detection method (e.g., MS detection for unambiguous identification) [90] [93]. |
| Poor spike recovery in matrix | The complex matrix is suppressing or enhancing the analytical signal, a phenomenon known as the matrix effect. | Improve sample clean-up (e.g., solid-phase extraction), use a stable isotope-labeled internal standard (especially in MS), or demonstrate parallelism to correct for the effect [92] [91]. |
| Lack of available impurities | Synthetic impurities or degradation products are not available for spiking. | Perform forced degradation studies to generate impurities in-situ. Then, use a second, well-characterized method (orthogonal) to compare results and prove specificity [90]. |
Establishing Science-Based Acceptance Criteria for Regulatory Compliance
Troubleshooting Guides and FAQs
FAQ: Specificity and Selectivity
Q: What are the fundamental differences between specificity and selectivity in analytical methods?
Specificity is the ability of a method to measure the analyte accurately and exclusively in the presence of other components, while selectivity is the ability to distinguish and quantify multiple analytes simultaneously within a mixture. For identification tests, specificity requires 100% detection, and the reportable specificity should be calculated as (Measurement - Standard) in units, then expressed as a percentage of the tolerance. Excellent results are ≤5% of tolerance, while acceptable results are ≤10% [95]. Method developers of ligand-binding assays often face challenges establishing selectivity and specificity due to nonspecific background signal, matrix interference, and drug interference [96].
Q: How do I set science-based acceptance criteria for method precision?
Precision should be evaluated relative to the product specification tolerance, not just as a percentage coefficient of variation (%CV). The recommended calculation is:
- For two-sided specification limits: Repeatability % Tolerance = (Standard Deviation (Repeatability) × 5.15) / (USL - LSL)
- For one-sided specification limits: Repeatability % Margin = (Standard Deviation (Repeatability) × 2.575) / (USL - Mean) or (Mean - LSL)
The recommended acceptance criterion for analytical method repeatability is ≤25% of the tolerance. For bioassays, this is relaxed to ≤50% of the tolerance [95].
Q: What is the recommended approach for setting acceptance criteria for accuracy/bias?
Accuracy or bias should be evaluated once a reference standard is available. The average distance from the measurement to the theoretical reference concentration is the bias in units. This bias should be evaluated as a percentage of the tolerance or margin [95]:
- Bias % of Tolerance = (Bias / Tolerance) × 100
- Bias % of Margin = Bias / (USL - Mean or Mean - LSL) for one-sided specifications
The recommended acceptance criterion for bias in analytical methods is ≤10% of the tolerance, which also applies to bioassays [95].
Q: When should analytical methods be validated, and can they be changed post-approval?
Analytical methods need to be validated for any GMP activity, even to support Phase I studies, using a phase-appropriate approach [7]. Methods can be changed mid-stream or after approval if changes are necessary due to process updates, reagent availability, or technological improvements. However, any change requires some form of revalidation, from a simple verification to a full validation, and may impact the regulatory submission, necessitating amendments [7].
Troubleshooting Guide: Common Method Performance Issues
Problem: High background signal or nonspecific interference in ligand-binding assays (e.g., ELISA).
| Possible Cause | Diagnostic Experiments | Corrective Action & Solution |
|---|---|---|
| Matrix Effects | - Compare standard curve in buffer vs. biological matrix.- Spike recovery experiment at multiple concentrations. | - Change immunoassay platform; microfluidic systems with fast kinetics can reduce nonspecific background [96].- Use a different sample dilution or modify the matrix. |
| Nonspecific Binding | - Test assay with irrelevant antibody or protein.- Include additional blocking steps with different agents. | - Optimize blocking conditions (e.g., concentration, duration).- Include wash steps with mild detergents (e.g., Tween-20). |
| Drug Interference | Spike analyte into samples containing potential interfering substances. | - Develop a sample pre-treatment protocol (e.g., extraction, precipitation).- Use an alternative assay format with higher drug tolerance [96]. |
Problem: Failure to meet linearity or range acceptance criteria.
| Possible Cause | Diagnostic Experiments | Corrective Action & Solution |
|---|---|---|
| Incorrect Range | Evaluate a range wider than the specification limits (minimally 80-120%). | Ensure the validated range is wide enough to cover the product specification limits and is demonstrated to be linear, accurate, and repeatable [95]. |
| Non-Linear Response | - Plot studentized residuals from the regression line.- Fit a quadratic model to the residuals. | The assay is linear as long as the studentized residuals remain within ±1.96. If the curve exceeds this limit, the range must be truncated [95]. |
| Sample Degradation | Re-inject samples from the high and low end of the range after sitting. | Ensure sample stability throughout the analytical process. |
Problem: Method lacks robustness, showing high variability during transfer.
| Possible Cause | Diagnostic Experiments | Corrective Action & Solution |
|---|---|---|
| Poorly Understood Method Parameters | Use a systematic approach like Design of Experiments (DoE) to evaluate the effect of multiple method parameters (e.g., pH, temperature, flow rate). | Adopt a Quality by Design (QbD) approach during development to identify and control critical method parameters, establishing a robust "design space" [7]. |
| Insufficient System Suitability Criteria | Review validation data to identify parameters with high variability. | Establish stringent system suitability tests (SSTs) that monitor method performance in real-time before sample analysis. |
The following table summarizes key quantitative acceptance criteria recommendations for analytical method validation, based on a percentage of the product specification tolerance [95].
Table 1: Recommended Acceptance Criteria Relative to Specification Tolerance
| Validation Characteristic | Recommended Calculation | Excellent Performance | Acceptable Performance |
|---|---|---|---|
| Repeatability | (Stdev * 5.15) / (USL - LSL) | ≤ 25% of Tolerance | Varies by risk |
| Bias/Accuracy | Bias / (USL - LSL) * 100 | ≤ 10% of Tolerance | Varies by risk |
| Specificity | (Measurement - Standard) / Tolerance * 100 | ≤ 5% of Tolerance | ≤ 10% of Tolerance |
| LOD (Limit of Detection) | LOD / Tolerance * 100 | ≤ 5% of Tolerance | ≤ 10% of Tolerance |
| LOQ (Limit of Quantitation) | LOQ / Tolerance * 100 | ≤ 15% of Tolerance | ≤ 20% of Tolerance |
Experimental Protocol: Demonstrating Specificity
Objective: To demonstrate that the analytical method can accurately quantify the analyte in the presence of other potentially interfering components (e.g., impurities, degradants, matrix).
Materials:
- Analyte of Interest: High-purity reference standard.
- Interferents: Likely impurities, degradants (from forced degradation studies), and components of the sample matrix (e.g., proteins, salts).
- Placebo: Formulation matrix without the active ingredient.
Procedure:
- Preparation of Solutions:
- Solution A (Analyte alone): Prepare the analyte at the target concentration (e.g., 100% of claim) in the solvent.
- Solution B (Placebo): Prepare the placebo formulation in the solvent.
- Solution C (Specificity Challenge): Prepare the analyte at the target concentration in the presence of the placebo and potentially interfering substances at expected or exaggerated levels.
- Analysis:
- Inject each solution (A, B, and C) into the analytical system in replicate (n=3).
- Record the responses (e.g., peak area, concentration).
- Data Analysis:
- Placebo Interference: Solution B should not show any peak or response corresponding to the analyte.
- Accuracy in Presence of Interferents: Calculate the mean measured concentration for Solution A and Solution C.
- %Bias for Specificity: = [(Mean Concentration of Solution C - Mean Concentration of Solution A) / Theoretical Concentration] × 100.
- % of Tolerance: = (Bias from specificity challenge / (USL - LSL)) × 100.
Acceptance Criteria: The calculated % of Tolerance for the specificity challenge should be ≤10% [95].
Experimental Workflow and Logical Pathways
Research Reagent Solutions
Table 2: Essential Materials for Analytical Method Development and Validation
| Item | Function & Application |
|---|---|
| Reference Standard | Highly characterized substance used to calibrate the analytical method and determine accuracy/bias. Essential for all quantitative methods [95] [7]. |
| Forced Degradation Samples | Samples (API or product) subjected to stress conditions (heat, light, pH) to generate degradants. Used to demonstrate method specificity and stability-indicating properties. |
| Placebo/Blank Matrix | The formulation matrix without the active ingredient. Critical for demonstrating the absence of interference and assessing specificity [95]. |
| Platform-Specific Reagents | Kits and reagents for specific platforms (e.g., Meso Scale Discovery, microfluidic systems). Choice of platform can impact specificity, background signal, and linear range [96]. |
| System Suitability Standards | Control samples with known values used to verify that the analytical system is performing adequately at the time of analysis. |
Core Concepts: Understanding the Lifecycle Approach
What is the analytical procedure lifecycle, and why is it critical for managing specificity and selectivity?
The analytical procedure lifecycle is a holistic, knowledge-driven framework for managing an analytical method from its initial development through its routine use and eventual retirement. It moves beyond the traditional, one-time validation event to an integrated system of continuous verification and revalidation to ensure the method remains fit-for-purpose, especially for critical attributes like specificity and selectivity, throughout its operational life [6] [97].
This approach is built on three main stages:
- Stage 1: Procedure Design: This involves developing the method and defining its performance requirements, including an Analytical Target Profile (ATP). The ATP is a pre-defined objective that outlines the quality standards the method must achieve [6].
- Stage 2: Procedure Performance Qualification: This stage demonstrates that the method, as designed, is capable of meeting the ATP and is suitable for its intended use [6].
- Stage 3: Continuous Procedure Performance Verification: This is the ongoing process of ensuring the method remains in a state of control during routine use. It involves monitoring method performance to detect undesired variability and initiating revalidation when necessary [6] [98].
A lifecycle approach is critical for specificity and selectivity because these attributes are foundational to method reliability. A method that cannot consistently distinguish the analyte from interferences (specificity) or measure it accurately in the presence of other components (selectivity) will produce flawed data, risking product quality and patient safety. Continuous monitoring provides objective evidence that these attributes are maintained despite minor, inevitable changes in reagents, analysts, or equipment [99].
What is the difference between method validation, verification, and revalidation?
These are distinct but interconnected activities within the lifecycle management of an analytical method.
- Method Validation is the process of proving that a newly developed analytical procedure is suitable for its intended purpose. It is a comprehensive exercise conducted prior to the method's use in routine testing and is required for regulatory submissions. It involves characterizing a set of performance parameters as defined in ICH Q2(R1) [99] [97].
- Method Verification is the process of confirming that a compendial (e.g., USP) or previously validated method is suitable for use under the actual conditions of a specific laboratory. It involves testing a subset of validation characteristics to prove the laboratory can successfully execute the method with its specific operators, equipment, and reagents [97].
- Method Revalidation is the process of reassessing the method's validity after a defined change. It is required when changes occur that could impact the method's performance. The degree of revalidation depends on the nature and significance of the change [100] [97].
The following workflow illustrates how these activities connect within the broader method lifecycle:
Troubleshooting Guides & FAQs
How do I establish a system for continuous performance verification?
A robust system for continuous verification relies on a control strategy with defined metrics and regular monitoring.
Problem: Method performance is drifting, leading to out-of-specification (OOS) results or failed system suitability tests, but the root cause is not understood.
Solution: Implement a lifecycle approach as outlined in ICH Q12 and Q14, which emphasizes ongoing data collection and analysis to verify the method remains in a state of control [6]. This involves:
- Define Control Strategies: Identify the key performance indicators (KPIs) for your method, such as peak tailing factor, resolution, or signal-to-noise ratio, which are directly linked to specificity and selectivity [97].
- Implement Trend Programs: Use control charts to monitor these KPIs for every analysis. Process Analytical Technology (PAT) tools can be leveraged for real-time monitoring where feasible [100].
- Set Alert and Action Limits: Establish statistically derived limits that trigger investigation (alert) or corrective action (action) when trend data indicates the method is moving out of control [98].
- Conduct Periodic Reviews: Regularly review all monitored data, OOS results, and deviations to assess the method's continued suitability [100].
When is revalidation required, and what is the scope?
Knowing when and how much to revalidate is a common challenge for scientists.
Problem: Uncertainty about whether a change in a reagent, instrument, or process necessitates a full or partial revalidation.
Solution: A risk-based assessment should be conducted for any change. The scope of revalidation should be commensurate with the level of risk the change poses to the method's performance, particularly to specificity and selectivity [100] [97]. The following table summarizes common triggers and the typical scope of revalidation.
| Trigger for Revalidation | Scope / Actions Required | Key Parameters to Re-assess (Non-Exhaustive) |
|---|---|---|
| Change in drug substance synthesis | Partial to Full Revalidation | Specificity, Accuracy, Linearity, Range [97] |
| Change in formulation of the drug product | Partial to Full Revalidation | Specificity, Accuracy, Linearity [97] |
| Change in the analytical procedure | Partial Revalidation | Parameters affected by the change (e.g., Precision, Robustness) [97] |
| Transfer of methods to a new laboratory | Method Transfer & Verification | Precision (Repeatability), Intermediate Precision/Ruggedness, Specificity [97] |
| Change in major equipment or instruments | Partial Revalidation & Requalification | Specificity, Precision, Robustness [97] |
| Ongoing monitoring shows a negative trend | Investigation, then Partial Revalidation | Parameters linked to the trend (e.g., Specificity if resolution is dropping) [100] |
How can I troubleshoot declining specificity in my chromatographic method?
Declining specificity is a high-priority issue that directly compromises data integrity.
Problem: Chromatographic peaks are co-eluting, showing peak tailing, or otherwise failing to provide adequate resolution.
Solution: Follow a structured troubleshooting protocol focused on the method's critical parameters.
Experimental Protocol for Troubleshooting Specificity:
- Confirm the Issue:
- Inject a system suitability sample containing the analyte and known potential interferences (e.g., impurities, degradants, excipients). Quantify the resolution between the critical pair of peaks [97].
- Investigate the Mobile Phase:
- Experiment: Prepare a fresh batch of mobile phase using high-purity solvents and salts. Systematically vary the pH (±0.2 units) or the organic solvent ratio (±2-5%) and analyze the impact on resolution and peak shape [101] [99].
- Rationale: The pH can alter the ionization state of the analyte and impurities, affecting their retention and separation. Small changes in solvent strength can significantly impact resolution.
- Investigate the Column:
- Experiment: Replace the analytical column with a new one of the same type (from the same or a different lot) or a column with similar chemistry but different selectivity (e.g., C18 vs. C8). Repeat the system suitability test [99].
- Rationale: Column degradation over time (e.g., loss of stationary phase) or lot-to-lot variability from the manufacturer can drastically alter selectivity.
- Investigate the Temperature:
- Experiment: Vary the column oven temperature (±5°C) and observe the effect on separation. Use a Design of Experiments (DoE) approach if multiple parameters are suspect to efficiently understand interactions [6].
- Rationale: Temperature can affect retention factors and selectivity.
- Final Verification:
- Once optimal conditions are found, perform a limited revalidation (e.g., for specificity, precision, and robustness) to document that the method's performance has been restored and is now controlled under the modified conditions [99].
The logical flow for this investigative process is outlined below:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and their functions, which are critical for developing and maintaining robust analytical methods, particularly for ensuring specificity and selectivity.
| Item | Function in Specificity/Selectivity Research |
|---|---|
| Certified Reference Standards | Provides a definitive benchmark for the analyte's identity and purity; essential for accurately determining retention time, resolution, and for method validation [97]. |
| Forced Degradation Samples | Stressed samples (e.g., by heat, light, acid, base, oxidation) generate potential degradants; used to challenge the method's ability to separate the analyte from its impurities (specificity) [99]. |
| High-Purity Solvents & Reagents | Minimize baseline noise and ghost peaks that can interfere with the detection and accurate integration of the analyte and impurity peaks [101]. |
| Columns with Different Selectivities | A set of columns (e.g., C18, C8, phenyl, cyano) is used during method development and troubleshooting to find the best stationary phase for resolving the analyte from critical impurities [99]. |
| Stable Isotope-Labeled Analytes | Used as internal standards in Mass Spectrometry to compensate for matrix effects and signal suppression/enhancement, thereby improving the reliability and selectivity of quantitative results. |
Comparative Method Assessment Using Red Analytical Performance Index (RAPI)
The Red Analytical Performance Index (RAPI) is a novel, standardized tool designed to quantitatively assess the analytical performance of quantitative methods. It was developed to fill a critical gap in the White Analytical Chemistry (WAC) framework, which evaluates methods based on three pillars: environmental impact (green), practical/economic factors (blue), and analytical performance (red). RAPI provides a structured, visual, and comparable way to score the "redness" or reliability of an analytical method, ensuring it is fit-for-purpose before considering its sustainability or cost-effectiveness [102] [103].
This tool consolidates ten key analytical validation parameters into a single, easy-to-interpret score. By using open-source software, it generates a star-shaped pictogram that offers an at-a-glance overview of a method's strengths and weaknesses, making it invaluable for researchers and drug development professionals during method selection, development, and validation [102] [103].
RAPI Assessment Criteria and Scoring
RAPI's evaluation is based on ten universal analytical parameters derived from international validation guidelines (such as ICH Q2(R2) and ISO 17025). Each parameter is scored on a five-level scale (0, 2.5, 5.0, 7.5, or 10 points), contributing equally to a final aggregate score between 0 and 100 [102] [103].
Table 1: RAPI Scoring Criteria and Parameters
| Assessment Parameter | Description and Scoring Basis |
|---|---|
| Repeatability | Variation in results under the same conditions, by a single analyst, over a short timescale (assessed as RSD%) [102] [103]. |
| Intermediate Precision | Variation in results within a single laboratory under controlled but varied conditions (e.g., different days or analysts) [102] [103]. |
| Reproducibility | Variation across different laboratories, equipment, and operators [103]. |
| Trueness | Closeness of measured value to a true/reference value, expressed as relative bias (%) [103]. |
| Recovery & Matrix Effect | % Recovery of the analyte and the qualitative impact of the sample matrix [103]. |
| Limit of Quantification (LOQ) | The lowest concentration that can be reliably quantified, expressed as a percentage of the average expected analyte concentration [103]. |
| Working Range | The span between the LOQ and the method's upper quantifiable limit [103]. |
| Linearity | The proportional relationship between analyte concentration and signal response, simplified using the coefficient of determination (R²) [103]. |
| Robustness/Ruggedness | The method's capacity to remain unaffected by small, deliberate variations in operational conditions [103]. |
| Selectivity | The method’s ability to differentiate and accurately measure the analyte in the presence of interferents [103]. |
Table 2: Interpreting the Final RAPI Score
| Final RAPI Score (0-100) | Performance Interpretation |
|---|---|
| 0-25 | Poor performance; method is not validated or is unreliable. |
| 26-50 | Moderate performance; method may be suitable for some screening purposes but has significant weaknesses. |
| 51-75 | Good performance; a reliable method that is likely fit-for-purpose. |
| 76-100 | Excellent performance; a robust, thoroughly validated method [103]. |
RAPI Implementation Workflow
The following diagram illustrates the logical workflow for conducting a method assessment using the Red Analytical Performance Index.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: What should I do if my analytical method lacks data for one or more RAPI parameters, resulting in a score of 0 for that criterion? A zero score indicates incomplete validation. The RAPI tool penalizes absent data to promote thoroughness and transparency. To address this:
- Re-evaluate Validation Protocol: Design and conduct experiments to collect data for the missing parameter(s), such as performing an inter-laboratory study for reproducibility or testing against interferents for selectivity [103].
- Phase-Appropriate Approach: In early development stages (e.g., Phase I clinical trials), a "phase-appropriate validation" is acceptable. Document the rationale for omitting certain parameters and plan for full validation as the product development progresses [7].
Q2: How can RAPI help when dealing with complex samples, like in cell and gene therapies (CGTs), where selectivity is a major challenge and reference materials are scarce? RAPI highlights selectivity as a key criterion, forcing a critical assessment.
- Identify Gaps: A low selectivity score pinpoints the issue. Use RAPI's structured output to justify the need for advanced techniques or controls to regulators [104].
- Alternative Materials: When reference standards are scarce, the industry uses alternative controls. Document these clearly and use RAPI to demonstrate the method's performance despite material limitations. Early engagement with health authorities to gain buy-in on your strategy is critical [104].
Q3: My method scored high on "green" metrics but moderate on RAPI. How should I interpret this? A moderate RAPI score suggests the method may not be sufficiently reliable for its intended use, even if it is environmentally friendly.
- Prioritize Performance: According to White Analytical Chemistry principles, the red dimension (performance) is the foundational requirement. A method cannot be deemed good if it fails to produce reliable results [102] [103].
- Use RAPI for Optimization: The RAPI pictogram shows which specific parameters (e.g., precision, LOQ) need improvement. Focus method optimization efforts on these areas to enhance overall performance without significantly compromising greenness [102].
Q4: Can I use RAPI to compare two different analytical techniques (e.g., HPLC vs. SERS) for the same analyte? Yes, this is one of RAPI's primary purposes. It standardizes performance assessment across different platforms.
- Objective Comparison: By scoring both methods against the same ten criteria, RAPI provides an objective, side-by-side comparison of their analytical strengths and weaknesses [103].
- Informed Decision-Making: The composite score and visual pictogram help determine which technique offers superior performance for your specific application, aiding in evidence-based instrument or method selection [103].
Essential Research Reagent Solutions
The following reagents and tools are fundamental for developing and validating robust analytical methods, particularly when aiming for a high RAPI score.
Table 3: Key Reagents and Materials for Analytical Method Development
| Reagent/Material | Function in Method Development & Validation |
|---|---|
| Certified Reference Materials (CRMs) | Essential for establishing method trueness (accuracy) by providing a known, traceable value to measure against [103]. |
| Stable Isotope-Labeled Internal Standards | Used to correct for analyte loss during sample preparation and to account for matrix effects, directly improving the scores for trueness and recovery [105]. |
| Molecularly Imprinted Polymers (MIPs) | Synthetic antibodies used in sample clean-up to improve selectivity by specifically extracting the target analyte from a complex matrix [105]. |
| Aptamers/Antibodies | Biological recognition elements used in assays or sensors to provide high specificity and selectivity for the target molecule [105]. |
| Derivatization Reagents | Chemicals that react with the target analyte to improve detection, e.g., by increasing its Raman cross-section for SERS or adding a fluorescent tag, thereby enhancing sensitivity (LOQ) and selectivity [105]. |
FAQ: Understanding Method Transfer Fundamentals
What is an analytical method transfer and when is it required? Analytical method transfer is a formally documented process that qualifies a receiving laboratory (RL) to use an analytical testing procedure that originated in a transferring laboratory (TL). Its primary goal is to demonstrate that the RL can execute the method and generate results equivalent to those produced by the TL in terms of accuracy, precision, and reliability [106] [107]. This process is typically required when moving methods between sites for commercial manufacturing, transferring methods to or from contract research/manufacturing organizations (CROs/CMOs), or when implementing methods on new equipment or platforms at different locations [106].
How does method transfer relate to method validation? Method validation confirms that an analytical procedure is suitable for its intended purpose, demonstrating that performance characteristics meet predefined criteria. Method transfer builds upon this foundation by verifying that these established performance characteristics can be consistently reproduced by a different laboratory [108] [109]. While validation focuses on the method's fundamental capabilities, transfer focuses on the laboratory's ability to implement it correctly.
What are the main approaches to analytical method transfer? There are four primary recognized approaches to method transfer, each with specific applications [106] [110] [111]:
| Transfer Approach | Description | Best Suited For |
|---|---|---|
| Comparative Testing | Both laboratories analyze identical samples; results are statistically compared against pre-defined acceptance criteria. | Well-established, validated methods; laboratories with similar capabilities [106]. |
| Co-validation | The receiving laboratory participates in the original method validation, often for intermediate precision assessment. | New methods being developed for multi-site use from the outset [106] [87]. |
| Revalidation | The receiving laboratory performs a full or partial revalidation of the method. | Significant differences in lab conditions/equipment or when the original TL is unavailable [106] [109]. |
| Transfer Waiver | The formal transfer process is waived based on strong scientific justification and risk assessment. | Highly experienced RLs, simple/robust methods, or compendial methods that only require verification [106] [111]. |
Can a method transfer be waived? Yes, in specific, well-justified cases, a formal transfer may be waived [108] [107]. Common justifications include the use of simple compendial methods (e.g., USP, Ph. Eur.) that only require verification, situations where the receiving laboratory is already highly familiar with the method, or when personnel responsible for the method relocate with it. The rationale for any waiver must be thoroughly documented and approved by Quality Assurance [106] [111].
FAQ: Specificity and Selectivity in Method Transfer
Why are specificity and selectivity critical in method transfer? Specificity and selectivity are fundamental analytical properties that ensure a method accurately measures the analyte of interest without interference from other sample components [112]. During transfer, even minor differences in equipment, reagents, or technician technique can alter a method's interaction with complex sample matrices. Verifying that the receiving laboratory can achieve the same level of specificity is essential for maintaining data integrity and ensuring patient safety, particularly in pharmaceutical analysis [96] [112].
What practical challenges affect specificity during transfer? Challenges often arise from differences in laboratory environments that were not fully explored during the initial method development and validation [96] [112]. These can include:
- Matrix Effects: Variances in reagent sources or water quality can cause different levels of matrix interference.
- Instrumentation: Different models or brands of HPLC/MS, GC/MS, or other platforms may have varying sensitivities to interfering substances.
- Sample Components: Degradation products, excipients, or concomitant medications may interact differently with the analytical system in the new environment.
How can we troubleshoot selectivity issues during transfer? A systematic approach is key to resolving selectivity problems [112]:
- Confirm the Root Cause: Use hyphenated techniques (like LC-MS or GC-MS) to confirm the identity of the analyte peak and check for co-eluting impurities.
- Compare Chromatograms: Perform a side-by-side comparison of system suitability or sample analysis outputs (e.g., chromatograms, spectra) from both laboratories to identify discrepancies in retention times, peak shape, or baseline resolution.
- Review Method Parameters: Re-examine critical method parameters with the transferring laboratory, such as mobile phase pH, gradient profile, or column temperature, which can profoundly impact selectivity.
- Standardize Materials: Ensure both labs use columns from the same manufacturer and identical batches of critical reagents.
Troubleshooting Guide: Common Method Transfer Challenges
Effective troubleshooting requires a structured methodology to identify and resolve discrepancies between laboratories. The following workflow provides a logical pathway for investigation.
Problem: Failing System Suitability Test (SST)
- Symptoms: Resolution, tailing factor, or precision outside acceptance criteria.
- Investigation Protocol:
- Confirm that the column (including manufacturer, model, and lot), mobile phase composition, pH, and temperature match the method exactly [106] [110].
- Check the instrument for performance issues (e.g., lamp energy, detector linearity, pump pressure fluctuations, injector precision) via diagnostic tests.
- Prepare fresh mobile phase and standards, ensuring all weighings and dilutions are correct.
- Resolution Steps: If the issue persists, perform a deliberate parameter variation (robustness testing) around the critical method parameters, in consultation with the transferring lab, to identify the most sensitive factors and establish a control strategy [106] [111].
Problem: Statistical Failure in Comparative Testing
- Symptoms: Results between labs fail pre-defined statistical equivalence criteria (e.g., t-test, F-test).
- Investigation Protocol:
- Verify that the same, homogenous batch of samples was used by both labs and that sample stability was maintained during shipping and storage [106] [107].
- Conduct a gap analysis of the entire procedure, from sample preparation to data processing, to identify subtle differences in technique [110].
- Ensure both labs are using the same version of the method and data processing algorithms (e.g., integration parameters for chromatography).
- Resolution Steps: The receiving laboratory should repeat the analysis. If the failure is confirmed, a joint investigation should be launched. It may be necessary to have an analyst from the transferring laboratory observe the process at the receiving lab to identify unrecorded "tacit knowledge" [110] [113].
Problem: Inconsistent Specificity/Selectivity
- Symptoms: Appearance of new peaks, loss of resolution, or different relative retention times.
- Investigation Protocol:
- Use orthogonal techniques (e.g., LC-MS or diode-array detection) to check peak purity and identity [112].
- Analyze placebo or blank samples to rule out interference from the sample matrix.
- Test samples spiked with known impurities to confirm the method's ability to separate and quantify them accurately.
- Resolution Steps: If the issue is column-related, sourcing a column from the same lot used by the TL may be necessary. If the method itself is found to be non-robust, a partial revalidation may be required to establish updated, more robust conditions [109].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following materials and instruments are critical for the successful execution and troubleshooting of analytical method transfers.
| Item Category | Specific Examples | Critical Function & Notes |
|---|---|---|
| Reference Standards | Drug Substance, Known Impurities, System Suitability Reference | Qualified standards with Certificates of Analysis (CoA) are essential for confirming method specificity, accuracy, and system performance [106] [109]. |
| Chromatographic Columns | HPLC/UPLC Columns (C18, C8, etc.) | The specific manufacturer, model, particle size, and dimensions are often critical method parameters. Using an identical column is highly recommended [106] [113]. |
| High-Purity Reagents | HPLC-Grade Solvents, Buffering Salts, Water | Consistent quality and grade of reagents are vital for preventing baseline noise, ghost peaks, and variable retention times [106] [107]. |
| Specialized Instrumentation | HPLC/UPLC with DAD/UV, GC-MS, LC-MS, Dissolution Apparatus | Equipment must be qualified and calibrated. While identical models are ideal, a justification and bridging data are needed if different models are used [106] [107] [109]. |
| Stable Test Samples | Active Pharmaceutical Ingredient (API), Drug Product, Placebo, Spiked Samples | Homogeneous and well-characterized samples from the same lot are required for comparative testing. Stability during shipment and storage must be verified [106] [111]. |
Experimental Protocol: Executing a Comparative Method Transfer
This protocol outlines the key steps for conducting a transfer via the comparative testing approach, which is the most common strategy [106] [109].
1. Pre-Transfer Planning and Protocol Development
- Activity: Form a cross-functional team with representatives from both the transferring and receiving laboratories, including Quality Assurance [106] [109].
- Output: A detailed, pre-approved Transfer Protocol. This document is the cornerstone of the transfer and must include [106] [110] [111]:
- Objective and Scope: Clear statement of the method(s) being transferred.
- Responsibilities: Defined roles for TL, RL, and QA.
- Experimental Design: Number of batches, replicates, injections, and analysts at the RL.
- Acceptance Criteria: Pre-defined, statistically sound criteria for equivalence.
- Materials and Methods: Detailed procedure, including equipment and column specifications.
- Deviation Handling: Process for managing any protocol deviations.
2. Execution and Data Generation
- Training and Knowledge Transfer: Analysts at the RL receive comprehensive training from the TL, including hands-on demonstration and transfer of "tacit knowledge" not captured in the written procedure [110] [113].
- Equipment and Readiness: The RL verifies all required equipment is available, qualified, and calibrated [107].
- Sample Analysis: Both laboratories analyze the pre-defined set of homogenous samples (typically a minimum of 3 replicates from one lot for a well-behaved method) following the approved method [106] [107] [111].
3. Data Evaluation and Reporting
- Statistical Analysis: Results are compiled and statistically compared as per the protocol (e.g., using t-tests for assay, F-tests for precision) [106] [111].
- Report Generation: A final Transfer Report is issued, summarizing all activities, results, raw data, and a definitive conclusion on whether the transfer was successful [106] [110]. The report must be approved by all relevant stakeholders.
Typical Acceptance Criteria for Common Tests [110] [109]
| Test | Typical Acceptance Criteria |
|---|---|
| Identification | Positive (or negative) identification obtained at the receiving site. |
| Assay | Absolute difference between the mean results of the two laboratories ≤ 2.0-3.0%. |
| Related Substances (Impurities) | Absolute difference for individual impurities may vary (e.g., ≤ 0.1% for impurities > 0.5%). For spiked impurities, recovery of 80-120% is common. |
| Dissolution | Difference in mean results ≤ 10% at time points <85% dissolved; ≤ 5% at time points >85% dissolved. |
Conclusion
Mastering specificity and selectivity challenges requires a holistic approach that integrates robust method development, systematic troubleshooting, and lifecycle validation. The convergence of QbD principles, advanced analytical technologies, and evolving regulatory frameworks provides powerful tools for ensuring method reliability. Future directions will increasingly emphasize real-time monitoring, AI-assisted method optimization, and standardized assessment metrics like RAPI for comprehensive method evaluation. By adopting these strategies, pharmaceutical scientists can develop analytically sound methods that not only meet compliance requirements but also serve as trustworthy guardians of product quality and patient safety throughout the drug development lifecycle.
References
- 1. IUPAC - specific (S05788) [https://goldbook.iupac.org/terms/view/S05788]
- 2. IUPAC - selectivity (S05564) [https://goldbook.iupac.org/terms/view/S05564]
- 3. Generating selectivity in analytical chemistry to reach the ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993697001222]
- 4. The Hidden Risks in Analytical Method Validation - [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 5. Validation of analytical methods based on accuracy profiles [https://www.sciencedirect.com/science/article/abs/pii/S0021967307002804]
- 6. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 7. Challenges in Analytical Method Development and ... [https://www.biopharminternational.com/view/challenges-analytical-method-development-and-validation]
- 8. HPLC Troubleshooting Guide [https://scioninstruments.com/us/blog/hplc-troubleshooting-guide-2/]
- 9. How To Identify & Prevent Analytical Test Problems [https://www.silcotek.com/blog/how-to-identify-prevent-analytical-test-problems]
- 10. FDA vs EMA: Method Validation Differences [https://www.linkedin.com/posts/pharcell_fda-vs-ema-key-differences-in-method-validation-activity-7355492349134749697-KnTR]
- 11. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 12. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 13. M10 Bioanalytical Method Validation and Study Sample ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m10-bioanalytical-method-validation-and-study-sample-analysis]
- 14. Bioanalytical method validation - Scientific guideline [https://www.ema.europa.eu/en/bioanalytical-method-validation-scientific-guideline]
- 15. Matrix (chemical analysis) [https://en.wikipedia.org/wiki/Matrix_(chemical_analysis)]
- 16. Matrix Effect - an overview [https://www.sciencedirect.com/topics/engineering/matrix-effect]
- 17. What is matrix effect and how is it quantified? [https://sciex.com/support/knowledge-base-articles/what-is-matrix-effect-how-to-quantify-it_en_us]
- 18. Problem with Impurity.Please help me! [http://www.chromforum.org/viewtopic.php?t=17801]
- 19. Troubleshooting Unwanted Peaks for HPLC [https://www.phenomenex.com/documents/2023/07/11/18/25/troubleshooting-unwanted-peaks-for-hplc-a-case-study-using-formic-acid?srsltid=AfmBOop8uNyTG0eHHMie9h8yoT_oTU-eC_6mcEdDrnpdFRabHrON-7Jn]
- 20. Development of forced degradation and stability indicating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5761119/]
- 21. Drug Degradation - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/drug-degradation]
- 22. and HPLC Tips: A Practical Troubleshooting for... Performance Guide [https://www.pgeneral.com/applications/hplc-troubleshooting-and-performance-tips-a-practical-guide-for-chromatographers/]
- 23. How to Improve Biologic Drug Product Stability Guide [https://www.leukocare.com/blog/how-to-improve-biologic-drug-product-stability]
- 24. In-use stability and compatibility of Biologics [https://www.lonza.com/knowledge-center/Blogs/administer-effective-medicinal-product]
- 25. Overcoming Obstacles in Gene Therapy Manufacturing [https://resilience.com/blog/overcoming-gene-therapy-obstacles]
- 26. Bioanayltical Method Development and Validation [https://ajprd.com/index.php/journal/article/view/1578]
- 27. Statistical Tools for Biologics Stability Testing [https://www.bioprocessintl.com/qa-qc/comprehensive-stability-assessment-of-biotechnological-products-degradation-mechanisms-statistical-tools-and-regulatory-compliance-part-1]
- 28. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 29. Advanced Therapies Issue 2025 - May [https://www.bioprocessintl.com/publications/bioprocess-international/may-2025]
- 30. Methods for Changing Peak Resolution in HPLC [https://www.chromatographyonline.com/view/methods-changing-peak-resolution-hplc-advantages-and-limitations]
- 31. Leveraging Multidimensional Modeling to Resolve ... [https://www.chromatographyonline.com/view/leveraging-multidimensional-modeling-to-resolve-frequent-separation-challenges-in-hplc]
- 32. Troubleshooting and Performance Improvement for HPLC [https://www.aurigeneservices.com/blogs/troubleshooting-and-performance-improvement-for-hplc]
- 33. UV Detection for HPLC – Fundamental Principle, Practical ... [https://www.chromatographyonline.com/view/lcgc-blog-uv-detection-hplc-fundamental-principle-practical-implications]
- 34. Advanced high-resolution chromatographic strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11576662/]
- 35. Optimizing Ultra-High-Performance Liquid ... [https://www.intechopen.com/chapters/1188571]
- 36. Ultra-high-pressure liquid chromatography (UHPLC) in ... [https://www.sciencedirect.com/science/article/abs/pii/S016599361400185X]
- 37. Liquid Chromatographic Peak Purity Assessments in ... [https://www.chromatographyonline.com/view/liquid-chromatographic-peak-purity-assessments-in-forced-degradation-studies---an-industry-perspective]
- 38. Peak purity assessment in liquid chromatography–mass ... [https://www.sciencedirect.com/science/article/abs/pii/S002196730100543X]
- 39. Diode Array Detector HPLC | DAD [https://scioninstruments.com/us/blog/diode-array-detector-hplc/]
- 40. A Beginner's Guide to Mass Spectrometry [https://www.acdlabs.com/blog/a-beginners-guide-to-mass-spectrometry/]
- 41. A Guide To Troubleshooting Mass Spectrometry [https://gentechscientific.com/a-guide-to-troubleshooting-mass-spectrometry/]
- 42. Common Problems in Analytical Method Validation [https://www.pharmaspecialists.com/2024/05/common-problems-in-analytical-method-validation.html]
- 43. Common Mistakes in Method Validation and How to Avoid ... [https://www.linkedin.com/pulse/common-mistakes-method-validation-how-avoid-them-part-oona-mcpolin]
- 44. What Are Options to Improve My Separation? Part 4 [https://www.chromatographyonline.com/view/what-are-options-to-improve-my-separation-part-4-solutions-to-consider-for-improving-separation-speed]
- 45. 12.3: Optimizing Chromatographic Separations [https://chem.libretexts.org/Bookshelves/Analytical_Chemistry/Analytical_Chemistry_2.1_(Harvey)/12%3A_Chromatographic_and_Electrophoretic_Methods/12.03%3A_Optimizing_Chromatographic_Separations]
- 46. Essentials of LC Troubleshooting, Part V: What Happened ... [https://www.chromatographyonline.com/view/essentials-of-lc-troubleshooting-part-v-what-happened-to-my-sensitivity-]
- 47. Simplified kinetic modeling for predicting the stability of ... [https://www.nature.com/articles/s41598-025-07037-y]
- 48. Design Space of Robust Analytical Methods in the ... - SEQENS [https://www.seqens.com/knowledge-center/design-space-of-robust-analytical-methods-in-the-pharmaceutical-environment/]
- 49. Quality by Design: A Tool for Separation Method ... [https://www.chromatographyonline.com/view/quality-design-tool-separation-method-development-pharmaceutical-laboratories]
- 50. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 51. A Beginner's Guide to Quality by Design (QbD) for HPLC ... [https://www.sepscience.com/a-beginners-guide-to-quality-by-design-qbd-for-hplc-method-development-11307]
- 52. Design Space in QbD — Definitions [https://qbdworks.com/design-space-in-qbd/]
- 53. Selectivity and Specificity: Pros and Cons in Sensing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6173322/]
- 54. 3.4: Selecting an Analytical Method [https://chem.libretexts.org/Bookshelves/Analytical_Chemistry/Analytical_Chemistry_2.1_(Harvey)/03%3A__The_Vocabulary_of_Analytical_Chemistry/3.04%3A_Selecting_an_Analytical_Method]
- 55. Essentials in Quality By Design [https://www.bioprocessintl.com/cell-line-development/essentials-in-quality-by-design]
- 56. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOopaWLGErj7RHMhbQGznUKko7VgY2QASSqY_hwivtjnW8wCzsXL3]
- 57. Matrix Effects on Quantitation in Liquid Chromatography [https://www.chromatographyonline.com/view/matrix-effects-on-quantitation-in-liquid-chromatography-sources-and-solutions]
- 58. From Sample to Separation: Best Practices in HPLC ... [https://www.chromatographyonline.com/view/from-sample-to-separation-best-practices-in-hplc-sample-preparation]
- 59. Understanding Specificity vs Selectivity in Analytical ... [https://www.linkedin.com/posts/uttam-chand-87b69926b_analyticalmethodvslidation-regulatory-activity-7393824442247802880-f4qV]
- 60. - Co : How to Detect and Fix Overlapping Peaks. Elution [https://axionlabs.com/chromatography-training/co-elution-in-chromatography/]
- 61. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOoqyqqDCCw4uF2qATWIxo8RHB9CbYEC7jCkzX3Gsn4eLrswrlwH4]
- 62. Compensate for or Minimize Matrix Effects? Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 63. Strategies for the Detection and Elimination of Matrix ... [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 64. Can you just ignore a coelution? [http://www.chromforum.org/viewtopic.php?t=111094]
- 65. Prevention of co-elution of steroid sulfates with serum ... [https://pubmed.ncbi.nlm.nih.gov/9853415/]
- 66. Six Fixes For Antibody Co - Elution In Immunoprecipitations [https://bitesizebio.com/7451/six-fixes-for-antibody-co-elution-in-immunoprecipitations/]
- 67. Chromatography Troubleshooting Guides-Liquid ... [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/chromatography-consumables-resources/chromatography-troubleshooting-guides/chromatography-troubleshooting-guides-liquid-chromatography.html]
- 68. HPLC Column Troubleshooting: Restore Performance & ... [https://www.labx.com/resources/hplc-column-troubleshooting-restore-performance-optimize-your-chromatography/26]
- 69. GC Temperature Programming—10 Things You Absolutely ... [https://www.chromatographyonline.com/view/gc-temperature-programming-10-things-you-absolutely-need-know]
- 70. GC Temperature Program Development [https://www.elementlabsolutions.com/uk/chromatography-blog/post/gc-temperature-program-development]
- 71. How to optimize your mobile phase to improve selectivity ... [https://www.buchi.com/en/blogs/colorful-researchers/how-to-optimize-your-mobile-phase-to-improve-selectivity-and-resolution-in-chromatography]
- 72. Mobile-Phase Optimization Strategies in Reversed- ... [https://www.chromatographyonline.com/view/mobile-phase-optimization-strategies-reversed-phase-hplc-0]
- 73. What Is LOD and LOQ Determination in Analytical ... [https://altabrisagroup.com/lod-and-loq-determination/]
- 74. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 75. A Guide to Analytical Method Validation [https://scioninstruments.com/us/blog/a-guide-to-analytical-method-validation-2/]
- 76. Going Low: Understanding Limit of Detection in Gas ... [https://www.chromatographyonline.com/view/going-low-understanding-limit-of-detection-in-gas-chromatography-gc-]
- 77. Method optimization to increase sensitivity in case of LOQ ... [https://mpl.loesungsfabrik.de/en/english-blog/high-performance-liquid-chromatography/method-optimization-sensitivity-hplc]
- 78. How to improve limit of quantitation? [http://www.chromforum.org/viewtopic.php?t=19785]
- 79. Comparison of Different Approaches for Calculating LOD ... [https://ps.tbzmed.ac.ir/Article/ps-40452]
- 80. A tutorial for computing limits of detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267021011685]
- 81. What is the difference between specificity and selectivity? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/specificity-selectivity]
- 82. Challenges in Developing Analytical Procedures with the ... [https://www.pharmoutsourcing.com/Featured-Articles/621016-Challenges-in-Developing-Analytical-Procedures-with-the-New-ICH-Q14-Guideline/]
- 83. Analytical Method Development and Validation in ... [https://resolvemass.ca/analytical-method-development-and-validation-in-pharmaceuticals/]
- 84. Determining the Risk Based Approach [https://medvacon.com/determining-the-risk-based-approach/]
- 85. Biopharmaceutical analysis — current analytical ... [https://link.springer.com/article/10.1007/s00216-025-06036-2]
- 86. Current Status and Challenges of Analytical Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9122548/]
- 87. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 88. Analytical Procedures and Validation_Specificity ... [https://nitrosamines.usp.org/t/analytical-procedures-and-validation-specificity-parameter-requirment/13578]
- 89. Introduction to Analytical Method Development and ... [https://www.labmanager.com/introduction-to-analytical-method-development-and-validation-33922]
- 90. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 91. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 92. Understanding Biomarker Method Validation: Specificity & ... [https://www.linkedin.com/pulse/understanding-biomarker-method-validation-dm9qe]
- 93. The use of selectivity in analytical chemistry [https://www.sciencedirect.com/science/article/abs/pii/S0165993601000930]
- 94. Selectivity or specificity? Validation of analytical methods ... [https://www.sciencedirect.com/science/article/abs/pii/0731708595016791]
- 95. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 96. case studies using a microfluidics platform [https://pubmed.ncbi.nlm.nih.gov/24830889/]
- 97. Analytical Method Validation Questions and Answers [https://www.complianceonline.com/resources/analytical-method-validation-questions-and-answers.html]
- 98. Continued Process Verification Is Critical in ... [https://www.pharmtech.com/view/continued-process-verification-is-critical-in-pharmaceutical-manufacturing]
- 99. Understanding Analytical Method Development and ... [https://www.upm-inc.com/understanding-analytical-method-development-and-validation]
- 100. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 101. Overcoming challenges in the analysis of the ubiquitous ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425008921]
- 102. Red analytical performance index (RAPI) and software [https://pubs.rsc.org/en/content/articlehtml/2025/gc/d4gc05298f]
- 103. The Red Component of Analytical Chemistry: Assessing ... [https://www.chromatographyonline.com/view/the-red-component-of-analytical-chemistry-assessing-the-performance-of-analytical-methods]
- 104. Facing challenges on CGT method validation controls ... [https://www.biophorum.com/news/facing-challenges-on-cgt-method-validation-controls-read-our-guide/]
- 105. Selectivity/Specificity Improvement Strategies in Surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5713634/]
- 106. Analytical Method Transfer: Best Practices and Guidelines | Lab Manager [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 107. Analytical Method Transfer Checklist: Ensuring Seamless Tech Transfer [https://www.propharmagroup.com/thought-leadership/how-conduct-analytical-method-transfer]
- 108. Step-by-Step Guide to Troubleshoot 'Method Transfer ... [https://inpeaks.com/2020/07/02/step-by-step-guide-to-troubleshoot-method-transfer-challenges/]
- 109. Importance of acceptance criteria in analytical method transfer [https://www.gmpsop.com/importance-of-acceptance-criteria-in-analytical-method-transfer/]
- 110. Best practices for analytical method transfers - Medfiles [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 111. Analytical Method Transfer | LCGC International [https://www.chromatographyonline.com/view/analytical-method-transfer-1]
- 112. Selectivity in analytical chemistry revisited [https://www.sciencedirect.com/science/article/abs/pii/S0165993601000929]
- 113. Analytical Method Transfer: Common Pitfalls and How to ... [https://www.qbdgroup.com/en/blog/analytical-method-transfer-common-pitfalls-and-how-to-avoid-them]