Statistical Analysis for Method Comparison Acceptance: A Comprehensive Guide for Biomedical Researchers
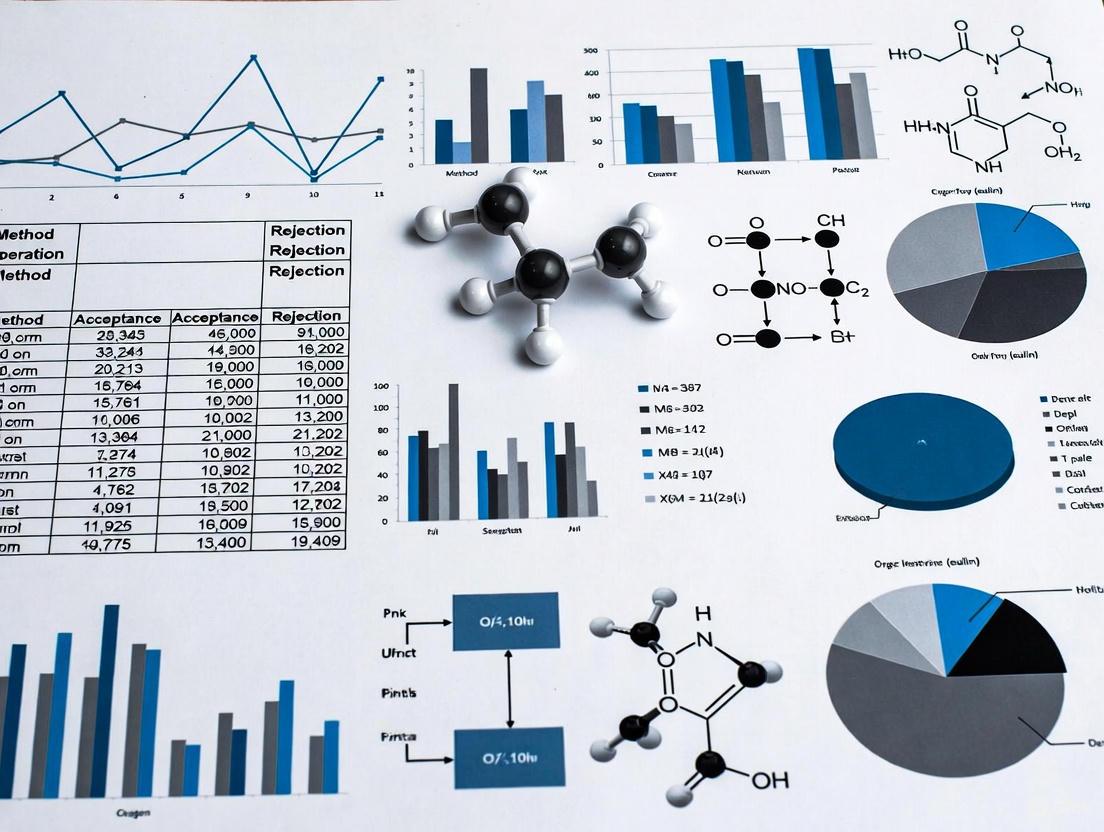
This article provides a comprehensive framework for designing, executing, and interpreting method comparison studies to ensure regulatory acceptance and scientific validity in biomedical and clinical research.
Statistical Analysis for Method Comparison Acceptance: A Comprehensive Guide for Biomedical Researchers
Abstract
This article provides a comprehensive framework for designing, executing, and interpreting method comparison studies to ensure regulatory acceptance and scientific validity in biomedical and clinical research. It guides researchers through foundational concepts, appropriate statistical methodologies, troubleshooting of common pitfalls, and validation strategies. Covering key topics from CLSI EP09-A3 standards and Milano hierarchy for performance specifications to practical application of Deming regression, Bland-Altman plots, and bias estimation, this guide equips professionals with the knowledge to demonstrate that new and established methods can be used interchangeably without affecting patient results or clinical outcomes.
Laying the Groundwork: Core Principles of Method Comparison Studies
In the field of drug development and biomedical research, method comparison studies are fundamental for assessing the comparability of measurement procedures. These studies are conducted whenever a new analytical method is introduced to replace an existing one, with the primary goal of determining whether the two methods can be used interchangeably without affecting patient results and clinical outcomes. The core question these studies address is whether a significant bias exists between methods. If the bias is larger than a pre-defined acceptable limit, the methods are considered different and not interchangeable for clinical use [1].
The quality of a method comparison study directly determines the validity of its conclusions, emphasizing the need for careful planning and appropriate statistical design. A well-executed method comparison assesses the degree of agreement between the current method (often considered the reference) and the new method (the comparator). This process is a key aspect of method verification, specifically for assessing method trueness, and can be performed following established standards such as CLSI EP09-A3, which provides guidance on estimating bias using patient samples [1].
Key Concepts and Experimental Protocols
Fundamental Study Design and Protocol
A robust method comparison experiment requires meticulous design to ensure results are reliable and actionable. The following protocol outlines the critical steps:
- Sample Selection and Sizing: The study should utilize a minimum of 40 and preferably 100 patient samples. A larger sample size enhances the ability to detect unexpected errors stemming from interferences or sample matrix effects. Samples must be carefully selected to cover the entire clinically meaningful measurement range [1].
- Measurement Replication: To minimize the impact of random variation, duplicate measurements for both the current and new method are recommended. The mean of duplicate measurements (or the median for triplicate or more) should be used for data plotting and analysis [1].
- Sample Handling and Randomization: Samples must be analyzed within their stability period, ideally within 2 hours of blood sampling, and on the same day the sample was collected. The sample sequence should be randomized to avoid carry-over effects, and measurements should be conducted over several days (at least 5) and across multiple runs to simulate real-world conditions [1].
- Defining Acceptance Criteria: Prior to the experiment, the acceptable bias must be defined. Performance specifications should be based on one of the models in the Milano hierarchy, which includes criteria based on the effect on clinical outcomes, components of biological variation of the measurand, or state-of-the-art capabilities [1].
Statistical Protocols and Data Analysis Workflow
The analytical phase involves specific statistical protocols to quantify agreement and detect bias.
- Initial Graphical Analysis: The first step in data analysis is the graphical presentation of data using scatter plots and difference plots. Scatter plots help visualize the variability in paired measurements across the measurement range and can reveal outliers, extreme values, or gaps in the data coverage that must be addressed before further analysis [1].
- Bland-Altman Analysis for Bias Estimation: Difference plots, specifically Bland-Altman plots, are used to assess agreement. In this analysis, the differences between the two methods are plotted on the y-axis against the average of the two methods on the x-axis. The mean of the differences provides an estimate of the average bias between the methods. The limits of agreement (LoA), calculated as the mean difference ± 1.96 times the standard deviation of the differences, estimate the interval within which 95% of the differences between the two methods are likely to fall. These limits are used to judge whether the methods can be used interchangeably [2].
- Advanced Regression Techniques: For a more detailed analysis of the relationship between methods, advanced regression techniques such as Deming regression or Passing-Bablok regression are recommended. These methods are designed to handle measurement errors in both methods, unlike ordinary least squares regression [1].
The following workflow diagram illustrates the key stages of a method comparison study:
Inappropriate Statistical Methods
It is critical to understand why certain common statistical methods are inadequate for assessing method comparability. Correlation analysis is often misused; it measures the strength of a linear relationship (association) between two methods but cannot detect proportional or constant bias. A perfect correlation coefficient (r = 1.00) can exist even when two methods are giving vastly different values, demonstrating that high correlation does not imply agreement [1].
Similarly, the t-test is not adequate for this purpose. An independent t-test only determines if two sets of measurements have similar averages, which can be misleading. A paired t-test, while better suited for paired measurements, may detect statistically significant differences that are not clinically meaningful if the sample size is very large, or fail to detect large, clinically important differences if the sample size is too small [1].
Quantitative Data and Performance Metrics
Structured Data from Comparison Studies
The following table summarizes quantitative results from a hypothetical method comparison study, illustrating the type of data generated and how bias and limits of agreement are calculated. This example evaluates the interchangeability of two glucose measurement methods.
Table 1: Example Data and Bias Calculations from a Glucose Method Comparison Study
| Sample ID | Reference Method (mmol/L) | New Method (mmol/L) | Difference (New - Ref) |
|---|---|---|---|
| 1 | 4.1 | 4.3 | 0.2 |
| 2 | 5.0 | 5.5 | 0.5 |
| 3 | 6.2 | 6.0 | -0.2 |
| 4 | 7.8 | 8.2 | 0.4 |
| 5 | 9.5 | 10.0 | 0.5 |
| ... | ... | ... | ... |
| Mean | 6.5 | 6.8 | 0.3 |
| Std Dev | - | - | 0.25 |
Key Metrics:
- Average Bias (Mean Difference): 0.3 mmol/L
- Standard Deviation of Differences: 0.25 mmol/L
- Lower Limit of Agreement: 0.3 - (1.96 × 0.25) = -0.19 mmol/L
- Upper Limit of Agreement: 0.3 + (1.96 × 0.25) = 0.79 mmol/L [2]
The final interpretation involves comparing these calculated limits of agreement to the pre-defined clinically acceptable bias. If the interval from -0.19 to 0.79 mmol/L is deemed too wide for clinical purposes, the methods are not interchangeable.
Performance Metrics in Related Fields
The principles of performance evaluation are also applied in computational drug discovery. For example, drug-repurposing technologies like the CANDO platform use metrics such as Average Indication Accuracy (AIA) to benchmark their predictions. This metric evaluates the platform's ability to correctly rank drugs associated with the same indication within a specified cutoff (e.g., the top 10 most similar drugs). In one reported instance, CANDO v1 achieved a top10 AIA of 11.8%, significantly higher than a random control of 0.2% [3].
In drug response prediction modeling, performance is often evaluated using the Root Mean Squared Error (RMSE) and R-squared (R²) values. A recent study comparing machine learning and deep learning models for predicting drug response (ln(IC50)) reported RMSE values ranging from 0.274 to 2.697 for traditional ML models across 24 different drugs [4].
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of method comparison studies relies on a suite of methodological tools and statistical solutions.
Table 2: Essential Reagents and Tools for Method Comparison Studies
| Tool/Solution | Function in Research |
|---|---|
| Patient Samples | Biological specimens used to cover the clinically meaningful measurement range and assess real-world performance [1]. |
| Statistical Software (e.g., R, Analyse-it) | Used to perform advanced statistical analyses, including Deming regression, Bland-Altman plots, and calculation of limits of agreement [2]. |
| CLSI EP09-A3 Guideline | Provides the standard protocol for designing and executing method comparison studies using patient samples to estimate bias [1]. |
| Bland-Altman Plot | A graphical method to visualize the agreement between two methods, plot the average bias, and establish the limits of agreement for interchangeability [1] [2]. |
| Deming & Passing-Bablok Regression | Statistical methods used to model the relationship between two methods while accounting for measurement errors in both variables, providing a more accurate analysis than simple linear regression [1]. |
| Random Number Generator | A tool (e.g., in Excel or specialized software) used to generate a randomization sequence for allocating samples or experimental units, a key step to minimizing bias in the study conduct [5]. |
| MEDICA16 | MEDICA16, CAS:87272-20-6, MF:C20H38O4, MW:342.5 g/mol |
| 1,3,5-Trihydroxyxanthone | 1,3,5-Trihydroxyxanthone, CAS:6732-85-0, MF:C13H8O5, MW:244.20 g/mol |
Visualizing the Bias Assessment Workflow
The process of analyzing data from a method comparison study to assess bias and agreement follows a structured path, as illustrated in the following diagram:
In the field of clinical laboratory sciences and pharmaceutical development, the Clinical and Laboratory Standards Institute (CLSI) guideline EP09-A3—titled Measurement Procedure Comparison and Bias Estimation Using Patient Samples—represents the current standard for evaluating the comparability of quantitative measurement procedures. This approved guideline, now in its third edition, provides the critical statistical and experimental framework for determining the bias between two measurement methods, thereby ensuring the reliability and interchangeability of data in both research and clinical decision-making [6]. The fundamental question addressed by EP09-A3 is whether two methods can be used interchangeably without affecting patient results and clinical outcomes [1]. Its application spans manufacturers of in vitro diagnostic (IVD) reagents, developers of laboratory-developed tests, regulatory authorities, and medical laboratory personnel who must verify method performance during technology changes, instrument replacements, or implementation of new assays [6].
The evolution from its predecessor (EP09-A2) to the current EP09-A3 edition reflects significant methodological advancements. The third edition, corrected in 2018, places greater emphasis on the process of performing measurement procedure comparisons, more robust regression techniques including weighted Deming and Passing-Bablok, and comprehensive bias estimation with confidence intervals at clinically relevant decision points [6]. This guideline is specifically designed for measurement procedures yielding quantitative numerical results and is not intended for qualitative tests, evaluation of random error, or total error assessment, which are covered in other CLSI documents such as EP12, EP05, EP15, and EP21 [6].
Core Principles and Experimental Design in EP09-A3
Fundamental Concepts and Terminology
The EP09-A3 guideline establishes a standardized terminology framework essential for proper method comparison studies. Central to this framework is the concept of bias—the systematic difference between measurement procedures—which must be quantified and evaluated against predefined performance criteria [6]. The guideline emphasizes trueness assessment through comparison against a reference or comparative method, moving beyond simple correlation analysis to more sophisticated statistical approaches that detect both constant and proportional biases [1]. Understanding these key concepts is critical for designing compliant experiments and correctly interpreting results.
Essential Experimental Design Requirements
The EP09-A3 protocol mandates specific design elements to ensure statistically valid and clinically relevant comparisons:
Sample Requirements and Selection: The guideline recommends using at least 40 patient samples, with 100 samples being preferable to identify unexpected errors due to interferences or sample matrix effects. Samples must be carefully selected to cover the entire clinically meaningful measurement range and should represent the typical patient population [1]. When possible, duplicate measurements for both the current and new method should be performed to minimize random variation effects [1].
Sample Analysis Protocol: The analysis of samples should occur within their stability period (preferably within 2 hours of blood sampling) and on the day of collection [1]. The guideline recommends measuring samples over several days (at least 5) and multiple runs to mimic real-world testing conditions and account for routine variability [1]. Sample sequence should be randomized to avoid carry-over effects, and quality control procedures must be implemented throughout the testing process [1].
Defining Acceptable Performance: Before conducting the experiment, laboratories must define acceptable bias specifications based on one of three models in accordance with the Milano hierarchy: (1) based on the effect of analytical performance on clinical outcomes, (2) based on components of biological variation of the measurand, or (3) based on state-of-the-art capabilities [1].
The following diagram illustrates the key decision points and workflow in designing an EP09-A3-compliant method comparison study:
Statistical Analysis Framework and Data Interpretation
Visual Data Exploration Techniques
EP09-A3 emphasizes visual data inspection as a critical first step in method comparison studies before quantitative analysis. Two primary graphical methods are recommended:
Scatter Plots: These diagrams plot measurements from the comparative method (x-axis) against the experimental method (y-axis), allowing initial assessment of the relationship between methods across the measurement range. The scatter plot helps identify linearity, potential outliers, and gaps in the data distribution that might require additional sampling [1]. When duplicate measurements are performed, the mean or median of replicates should be used for plotting [1].
Difference Plots (Bland-Altman Plots): These plots display the differences between methods (y-axis) against the average of both methods (x-axis), enabling direct visualization of bias across the measurement range. Difference plots help identify constant or proportional bias, outliers, and potential trends where disagreement between methods may change with concentration levels [6] [1].
Quantitative Statistical Methods
EP09-A3 introduces various advanced statistical techniques for quantifying the relationship between measurement procedures:
Regression Analysis Techniques: The guideline describes several regression approaches, including:
- Ordinary Least Squares (OLS) Regression: Traditional regression that assumes no error in the x-variable measurement
- Deming Regression: Accounts for measurement error in both methods compared
- Weighted Deming Regression: Extends Deming regression to address non-constant measurement variability across concentrations
- Passing-Bablok Regression: A non-parametric method that makes no distributional assumptions and is robust to outliers [6]
Bias Estimation with Confidence Intervals: The guideline mandates computation of bias estimates with confidence intervals at medically important decision levels rather than single-point estimates. This approach provides more clinically relevant information and acknowledges the uncertainty in bias estimates [6].
Outlier Detection: EP09-A3 recommends using the extreme studentized deviate method for objective identification of potential outliers that might unduly influence the statistical analysis [6].
The table below summarizes the key statistical methods described in EP09-A3 and their appropriate applications:
Table 1: Statistical Methods for Method Comparison Studies per EP09-A3
| Statistical Method | Type of Analysis | Key Assumptions | Appropriate Use Cases |
|---|---|---|---|
| Deming Regression | Parametric regression | Constant ratio of measurement variances | Both methods have measurable error |
| Weighted Deming Regression | Parametric regression | Non-constant measurement variability | Precision varies across concentration range |
| Passing-Bablok Regression | Non-parametric regression | No distributional assumptions | Non-normal data, presence of outliers |
| Bland-Altman Difference Plots | Graphical agreement assessment | No specific distribution | Visualizing bias across measurement range |
| Bootstrap Iterative Technique | Resampling method | Representative sampling | Estimating confidence intervals for complex statistics |
Inappropriate Statistical Methods
EP09-A3 explicitly cautions against using inadequate statistical approaches that were commonly employed in earlier method comparison studies:
Correlation Analysis: Correlation coefficients (r) measure the strength of a relationship between methods but cannot detect constant or proportional bias. As demonstrated in examples, two methods can show perfect correlation (r=1.00) while having clinically unacceptable biases [1].
t-Tests: Both paired and independent t-tests are inadequate for method comparison. T-tests may fail to detect clinically significant differences with small sample sizes, or detect statistically significant but clinically irrelevant differences with large sample sizes [1].
Comparative Analysis: EP09-A3 vs. Previous Editions and Other Standards
Evolution from EP09-A2 to EP09-A3
The third edition of the EP09 guideline introduced substantial improvements over its predecessor:
Table 2: Key Differences Between EP09-A2 and EP09-A3
| Feature | EP09-A2 | EP09-A3 |
|---|---|---|
| Scope of Applications | Limited coverage of comparison applications | Broader coverage including factor comparisons (e.g., sample tube types) |
| Data Visualization | Basic scatter plots | Enhanced emphasis on difference plots for visual bias inspection |
| Regression Methods | Basic Deming and Passing-Bablok | Weighted options, improved Deming, corrected Passing-Bablok descriptions |
| Bias Estimation | Single-point estimates | Bias at clinical decision points with confidence intervals |
| Outlier Detection | Limited guidance | Formalized extreme studentized deviate method |
| Statistical Complexity | Detailed mathematics in main text | Relocation of complex mathematical descriptions to appendices |
| Manufacturer Requirements | General bias characterization | Clear specification to use regression analysis for bias characterization |
These enhancements make EP09-A3 more applicable to diverse comparison scenarios, including those performed by clinical laboratories for sample type comparisons (e.g., serum vs. plasma) or reagent lot changes [6]. The addition of the bootstrap iterative technique for bias estimation provides a robust resampling method for determining confidence intervals when traditional parametric assumptions may not be met [6].
Relationship to Other CLSI Standards
EP09-A3 exists within a broader ecosystem of CLSI standards, each addressing specific aspects of method validation:
- EP05 and EP15: Focus on evaluation of random error and precision, whereas EP09-A3 specifically addresses systematic error (bias) [6]
- EP07: Provides guidance for measuring bias from individual sources such as sample interference, while EP09-A3 addresses overall method comparison [6]
- EP21: Concerns total error estimation, which combines both random and systematic error components [6]
- EP12: Covers qualitative test evaluation, while EP09-A3 is specifically for quantitative procedures [6]
Understanding this relationship helps laboratories implement a comprehensive validation strategy using complementary CLSI guidelines appropriate for their specific needs.
Implementation in Regulatory and Laboratory Environments
Case Studies and Practical Applications
Real-world implementations demonstrate the practical utility of EP09-A3 across diverse laboratory scenarios:
Immunoassay System Comparison: A 2021 study published in the International Journal of General Medicine applied the EP09-A2 protocol (a direct predecessor to EP09-A3) to compare HCG measurements between a Beckman Dxl 800 immunoassay analyzer and a Jet-iStar 3000 immunoassay analyzer. The study used 40 fresh serum specimens with 20 having abnormal HCG concentrations, analyzed over five consecutive days. Through regression analysis, researchers established a strong correlation (r=0.998) with the regression equation y=1.020x+12.96, determining that the estimated bias was within clinically acceptable limits [7].
Thyroid Hormone Testing Evaluation: A 2023 method comparison study of total triiodothyronine (TT3) and total thyroxine (TT4) measurements between Roche Cobas e602 and Sysmex HISCL 5000 analyzers successfully implemented EP09-A3 guidelines. The study demonstrated excellent analytical performance with acceptable biases for both systems, highlighting the guideline's suitability for evaluating method comparability across different technological platforms [8].
Software Tools Supporting EP09-A3 Implementation
Specialized statistical software packages have incorporated EP09-A3 protocols to streamline implementation:
Table 3: Software Solutions Supporting EP09-A3 Compliance
| Software Platform | EP09-A3 Features | Target Users | Regulatory Applications |
|---|---|---|---|
| EP Evaluator 12.0+ | Advanced statistical module with multiple replicate handling, advanced regression algorithms | Clinical laboratories, IVD manufacturers | FDA 510(k) submissions, routine quality assurance |
| Analyse-it Method Validation Edition | Comprehensive CLSI protocol support including weighted Deming and Passing-Bablok regression | ISO 15189 medical laboratories, IVD developers | FDA submissions, ISO/IEC 17025 compliance, CLIA '88 compliance |
These software solutions help standardize the implementation of EP09-A3 statistical methods, reduce calculation errors, and generate publication-quality outputs suitable for regulatory submissions [9] [10].
Essential Research Reagents and Materials
The following toolkit represents essential materials required for conducting EP09-A3-compliant method comparison studies:
Table 4: Essential Research Reagent Solutions for Method Comparison Studies
| Material/Reagent | Function in EP09-A3 Studies | Critical Specifications |
|---|---|---|
| Patient Samples | Primary material for method comparison | Cover clinical measurement range, include abnormal values, ensure stability |
| Quality Control Materials | Monitoring assay performance during study | Commutable, concentration near medical decision points |
| Calibrators | Ensuring proper instrument calibration | Traceable to reference standards, commutable with patient samples |
| Reagents | Test-specific reaction components | Lot-to-lot consistency, manufacturer-specified storage conditions |
| Statistical Software | Data analysis and regression calculations | CLSI EP09-A3 compliant algorithms, appropriate validation |
The CLSI EP09-A3 guideline represents the current standard for method comparison studies, providing a robust statistical framework for bias estimation between quantitative measurement procedures. Its comprehensive approach—encompassing experimental design, visual data exploration, advanced regression techniques, and clinical interpretation of bias—makes it indispensable for laboratories and manufacturers seeking to ensure result comparability across methods and platforms. The guideline's recognition by regulatory bodies like the FDA further underscores its importance in the method validation process [6].
As laboratory medicine continues to evolve with new technologies and platforms, the principles established in EP09-A3 provide a consistent methodology for evaluating method performance and ensuring that patient results remain comparable regardless of the testing platform used. Proper implementation of this guideline helps maintain data integrity across clinical and research settings, ultimately supporting accurate diagnosis and treatment decisions.
In laboratory medicine, defining the required quality of a test is fundamental to ensuring its clinical usefulness. Analytical Performance Specifications (APS) are "Criteria that specify the quality required for analytical performance to deliver laboratory test information that would satisfy clinical needs for improving health outcomes" [11]. The Milan Hierarchy Model, established during the 2014 consensus conference, provides a structured framework for setting these specifications, moving beyond a one-size-fits-all approach to a more nuanced, evidence-based methodology [11] [12]. This model is critical for researchers and drug development professionals conducting method comparison studies, as it supplies the rigorous acceptance criteria against which new or existing analytical methods must be validated.
The Core Models of the Milan Hierarchy
The Milan consensus formalized three distinct models for establishing APS, each with its own rationale and application [11].
Model 1: Clinical Outcome: This model is considered the gold standard, as it bases APS directly on the test's impact on patient health outcomes. It can be applied through direct evaluation of how different assay performances affect health outcomes or, more feasibly, through indirect evaluation using modeling or surveys of clinical decision-making [11].
Model 2: Biological Variation: This model sets specifications based on the innate biological variation of an analyte within and between individuals. For diagnostics, the goal is often defined as
SDa < 0.5 SDbiol, whereSDbiolis the total biological standard deviation. For monitoring, the more stringent specification of(SDa² + Bias²)â°Â·âµ < 0.5 SDIis used, whereSDIis the within-subject biological variation [12]. The European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) maintains a database of rigorously determined biological variation data for this purpose [11].Model 3: State of the Art: When outcome-based or biological variation data are unavailable, APS can be based on the best performance currently achievable by available technology. This can serve as a benchmark for improvement or a minimum standard that most laboratories can meet [11].
A Risk-Based Synthesis of the Models
A contemporary development in applying the Milan Hierarchy is the argument against rigidly assigning a measurand to a single model. Instead, a risk-based approach is recommended, which considers the purpose of the test in the clinical pathway, its impact on medical decisions, and available information from all three models before determining the most appropriate APS for a specific setting [11]. The final choice of model is influenced by the quality of the underlying evidence and the specific clinical application of the test.
Table 1: The Core Models of the Milan Hierarchy for Setting APS
| Model | Basis for Specification | Primary Application | Key Strength | Key Limitation |
|---|---|---|---|---|
| Model 1: Clinical Outcome | Direct or indirect link to patient health outcomes [11] | Tests with a central role in clinical decisions and defined decision levels (e.g., HbA1c, cholesterol) [12] | The most clinically relevant approach; considered the ideal | Extremely difficult and resource-intensive to perform direct outcome studies [11] |
| Model 2: Biological Variation | Within- and between-subject biological variation of the analyte [11] [12] | Measurands under homeostatic control; widely applied for many routine tests | Provides a universally applicable, objective goal that is independent of current technology | May yield unrealistically tight goals for some tightly controlled measurands (e.g., electrolytes) [12] |
| Model 3: State of the Art | Current performance achieved by the best available or most commonly used methods [11] | Measurands where Models 1 and 2 cannot be applied (e.g., many urine tests) [12] | Pragmatic and achievable; useful for driving incremental improvement | Risks perpetuating inadequate performance if the "state of the art" is poor |
Experimental Protocols for Applying the Milan Models
Protocol for Establishing APS Based on Biological Variation (Model 2)
The application of Model 2 has been significantly refined through initiatives like the European Biological Variation Study (EuBIVAS) [11].
- Objective: To determine the desirable imprecision (CVa) and bias (Biasa) for an analytical method based on biological variation data.
- Experimental Workflow:
- Literature Search & Critical Appraisal: Systematically search for biological variation studies for the target measurand. All identified studies must be critically appraised using the Biological Variation Critical Appraisal Checklist (BIVAC) to grade their quality [11].
- Data Extraction: Obtain the estimated within-subject (CVI) and between-subject (CVG) biological variation coefficients from the highest-quality available study.
- Calculation of APS: Apply consensus formulas to derive performance specifications. The EFLM recommends several tiers of quality:
- Optimum:
CVa ≤ 0.25 CVIandBiasa ≤ 0.125 (CVI² + CVG²)â°Â·âµ - Desirable:
CVa ≤ 0.50 CVIandBiasa ≤ 0.25 (CVI² + CVG²)â°Â·âµ - Minimum:
CVa ≤ 0.75 CVIandBiasa ≤ 0.375 (CVI² + CVG²)â°Â·âµ
- Optimum:
- Data Analysis: The calculated CVa and Biasa are used as the acceptance criteria when validating a new method. The method's own imprecision and bias, determined through replication and comparison-of-methods experiments, must be equal to or less than these desirable specifications.
Protocol for Establishing APS Based on State of the Art (Model 3)
- Objective: To define APS based on the current performance achievable by available technology.
- Experimental Workflow:
- Data Collection: Gather large-scale performance data from External Quality Assessment (EQA) programs or method comparison peer-group analyses [11].
- Statistical Analysis: Calculate the distribution of performance (e.g., imprecision and bias) across a large number of laboratories or methods.
- Specification Setting: Choose a percentile of performance as the benchmark. This can be an aspirational goal (e.g., the performance level of the top 10% of methods) to drive improvement, or a minimum standard (e.g., the performance level achieved by 80% of laboratories) to identify and rectify poor performance [11].
Visualization of the Milan Model Decision Pathway
The following diagram illustrates the decision-making process for selecting and applying the Milan models, incorporating the modern risk-based approach.
For researchers implementing the Milan models, specific tools and resources are essential.
Table 2: Essential Research Reagents and Resources for APS Studies
| Tool / Resource | Function in APS Research | Example / Source |
|---|---|---|
| BIVAC Checklist | A critical appraisal tool to grade the quality and reliability of published biological variation studies [11]. | European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) |
| Biological Variation Database | A publicly available database compiling quality-appraised biological variation data for numerous measurands [11]. | EFLM Biological Variation Database (biologicalvariation.eu) |
| Commutable EQA Materials | External quality control materials that behave like fresh human patient samples, essential for accurately assessing inter-laboratory bias and determining the "state of the art" [11]. | Various commercial and national EQA providers |
| Statistical Software for MU & TE | Software capable of complex calculations for measurement uncertainty and total error, integrating imprecision and bias data. | R, Python, SAS, or specialized validation software packages |
| Stable Sample Pools | For estimating a method's long-term imprecision (CVa) through repeated measurement over time, a key input for Models 2 and 3. | In-house prepared pools of human serum or other relevant matrices |
Comparative Analysis of Model Outcomes and Data Presentation
The choice of model directly influences the stringency of the performance specification, which can lead to different conclusions in a method comparison acceptance study.
Table 3: Comparison of Exemplary APS for Common Analytes from Different Models
| Measurand | Clinical Context | Model 1 (Outcome) | Model 2 (Biol. Var.) - Desirable | Model 3 (State of the Art) | Implied Decision in Method Comparison |
|---|---|---|---|---|---|
| HbA1c | Diagnosis of diabetes | Total Error < 5.0% (based on clinical guidelines) [11] | Total Error < 2.9% (based on CVI) | CV < 2.5% (based on EQA data) | A new method meeting Model 3 may fail the more stringent Model 1 and 2 criteria. |
| C-Reactive Protein (CRP) | Monitoring inflammation | Not commonly established | CV < 14.6% (based on CVI) | CV < 10.0% (aspirational, based on best methods) [11] | Model 3 may drive adoption of superior methods, even if Model 2 is met. |
| Cortisol | Diagnosis (vs. Monitoring) | Requires very low bias for diagnosis [11] | Bias < 5.0% | Bias < 10.0% | A method suitable for monitoring (meeting Model 3) may be inadequate for diagnostic use (Model 1). |
The Milan Hierarchy Model provides a vital, structured framework for setting defensible analytical performance specifications. For the method comparison researcher, its power lies in moving from arbitrary quality goals to a justified, evidence-based selection process. The evolving best practice is not to slavishly adhere to a single model but to undertake a comprehensive, risk-based synthesis of available clinical outcome, biological variation, and state-of-the-art data. This ensures that the final APS is not only statistically sound but also clinically relevant, ultimately guaranteeing that laboratory results are fit-for-purpose in the context of patient care and drug development.
In method comparison studies, a critical yet often misunderstood area of statistical analysis, the misuse of correlation analysis and the t-test remains prevalent. This guide objectively compares these inadequate methods with robust alternatives like Bland-Altman difference plots and regression analyses, providing supporting experimental data and protocols. Framed within the broader context of statistical analysis for method comparison acceptance research, this article equips scientists and drug development professionals with the knowledge to validate analytical techniques accurately and reliably.
The Fundamental Flaw: Using Association to Assess Agreement
A common misconception in method comparison studies is that a strong correlation between two measurement techniques indicates they can be used interchangeably. This is a fundamental error, as correlation measures the strength of a relationship, not the extent of agreement [1].
Experimental Evidence: The Correlation Fallacy
The following experiment demonstrates that a perfect correlation can exist alongside a massive, clinically unacceptable bias.
TABLE I: Glucose measurements demonstrating the correlation fallacy [1]
| Sample Number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Glucose by Method 1 (mmol/L) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Glucose by Method 2 (mmol/L) | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 |
Experimental Protocol: Glucose was measured in 10 patient samples using two different methods. Method 1 is the established reference, while Method 2 is a new technique under evaluation. The correlation coefficient (r) for the two datasets is calculated.
Resulting Data: The correlation coefficient for this dataset is 1.00 (P < 0.001), indicating a perfect linear relationship [1]. However, visual inspection and basic calculation reveal that Method 2 consistently yields values five times higher than Method 1. This proportional bias means the methods are not interchangeable, a fact entirely missed by the correlation analysis.
The Inadequacy of the T-Test for Method Comparison
The t-test is designed to detect differences between the mean values of two groups. However, in method comparison, agreement requires that measurements are close for each individual sample, not just that the group averages are similar [1].
Experimental Evidence: The T-Test's Blind Spot
This experiment shows how a t-test can fail to detect clear patterns of disagreement between two methods.
TABLE II: Glucose measurements demonstrating the t-test's inadequacy [1]
| Sample Number | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Method 1 (mmol/L) | 1 | 2 | 3 | 4 | 5 |
| Method 2 (mmol/L) | 5 | 4 | 3 | 2 | 1 |
Experimental Protocol: Five patient samples are measured with two methods. An independent samples t-test is used to compare the results from Method 1 and Method 2.
Resulting Data: The mean for both Method 1 and Method 2 is 3.0 mmol/L. The independent t-test shows no significant difference (P < 0.001), suggesting comparability [1]. In reality, the methods are inversely related and would produce entirely different clinical interpretations for individual patients. The t-test failed because it only compared the central tendency, ignoring the paired nature of the data and the direction of differences for each sample.
The Sample Size Paradox of the Paired T-Test
The paired t-test, while an improvement, is still inadequate. Its ability to detect a difference is heavily influenced by sample size [1].
- With a large sample, it may detect a statistically significant but clinically meaningless bias.
- With a small sample, it may fail to detect a large and clinically important bias, as shown in the data below.
TABLE III: Example of a clinically significant bias missed by a paired t-test due to small sample size [1]
| Sample Number | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Method 1 (mmol/L) | 2 | 4 | 6 | 8 | 10 |
| Method 2 (mmol/L) | 3 | 5 | 7 | 9 | 9 |
Resulting Data: The mean difference is -10.8%, which is clinically significant. However, with only five samples, the paired t-test reports a P-value of 0.208, which is not statistically significant [1]. This demonstrates how reliance on the t-test can lead to the acceptance of a poorly performing method.
Robust Alternatives for Method Comparison
The CLSI EP09-A3 standard provides guidance on proper statistical procedures for method comparison studies, emphasizing graphical presentation and specific regression techniques [1].
The Bland-Altman Difference Plot
The Bland-Altman plot (or difference plot) is the recommended graphical method to assess agreement between two measurement techniques [1].
Diagram 1: Workflow for creating and interpreting a Bland-Altman plot.
Interpretation: The plot visually reveals any systematic bias (the mean difference) and the random variation around that bias (95% limits of agreement). The key question is whether the observed bias and variation are small enough to be clinically acceptable, a decision that requires expert judgment, not just a statistical test [1].
Advanced Regression Techniques
For a more detailed analysis of the relationship between methods, advanced regression techniques are preferred over simple correlation.
- Deming Regression: Accounts for measurement error in both methods.
- Passing-Bablok Regression: A non-parametric method that is robust to outliers and does not require normally distributed data.
These methods provide reliable estimates of constant and proportional bias, which are critical for determining if two methods are interchangeable [1].
The Scientist's Statistical Toolkit
TABLE IV: Essential reagents and materials for a robust method comparison study
| Item | Function in the Experiment |
|---|---|
| At Least 40 Patient Samples | To ensure sufficient statistical power and to identify unexpected errors due to interferences or sample matrix effects [1]. |
| Samples Covering Clinically Meaningful Range | To evaluate method performance across all potential values encountered in practice, from low to high [1]. |
| Duplicate Measurements | To minimize the effect of random variation and improve the reliability of the comparison [1]. |
| Pre-Defined Acceptable Bias | A performance specification (e.g., based on biological variation or clinical outcomes) established before the experiment to objectively judge the results [1]. |
| Statistical Software (e.g., R, SPSS) | To perform specialized analyses like Deming or Passing-Bablok regression and generate Bland-Altman plots [13]. |
| A-205804 | A-205804, CAS:251992-66-2, MF:C15H12N2OS2, MW:300.4 g/mol |
| Aaptamine | Aaptamine, CAS:85547-22-4, MF:C13H12N2O2, MW:228.25 g/mol |
Experimental Protocol for a Compliant Method Comparison Study
A well-designed experiment is the foundation of a valid comparison.
Diagram 2: Step-by-step workflow for a robust method comparison study.
Key Protocol Steps:
- Pre-Analysis Planning: Define acceptable performance specifications a priori and secure a sufficient number of samples covering the entire clinical reportable range [1].
- Sample Analysis: Analyze samples within a narrow stability window (e.g., within 2 hours of collection) to prevent degradation. Randomize the sequence of analysis across both methods to avoid carry-over and time-related biases. Perform measurements over several days to ensure reproducibility [1].
- Data Analysis & Interpretation: Begin with graphical analyses (scatter and Bland-Altman plots) to visualize the data and detect outliers. Follow with robust regression analysis to quantify bias. Finally, compare the estimated bias to the pre-defined acceptable limit to make a decision on method interchangeability [1].
TABLE V: Summary of statistical methods for method comparison
| Method | Primary Function | Appropriate for Agreement? | Key Limitation |
|---|---|---|---|
| Correlation Analysis | Measures strength of a linear relationship | No | Fails to detect constant or proportional bias; perfect correlation can exist with total disagreement [1]. |
| T-Test (Independent) | Compares means of two independent groups | No | Only compares central tendency; ignores paired structure of data and individual differences [1]. |
| T-Test (Paired) | Compares means of two paired measurements | No | Highly sensitive to sample size; can miss large biases with small N or find trivial biases with large N [1]. |
| Bland-Altman Plot | Visualizes agreement and estimates bias | Yes | Provides direct visual and quantitative assessment of bias and its clinical acceptability [1]. |
| Deming/Passing-Bablok Regression | Quantifies constant and proportional bias | Yes | Accounts for errors in both methods; provides robust estimates of the relationship between methods [1]. |
In the rigorous field of analytical science, particularly during drug development and method validation, confirming that a new measurement procedure can adequately replace an established one is a common necessity. This process, known as a method-comparison study, seeks to answer a direct clinical question: can we measure an analyte using either Method A or Method B and obtain equivalent results without affecting patient outcomes? [1] [14] The foundational principles that underpin this assessment are the concepts of bias, precision, and agreement. These terms, often mistakenly used interchangeably with "accuracy" and "association," have specific statistical meanings. A clear understanding of their distinctions is critical for designing robust experiments, performing correct data analysis, and drawing valid conclusions about the interchangeability of two measurement methods [1] [14]. Misapplication of statistical tests, such as relying solely on correlation analysis or t-tests, is a common pitfall that can lead to incorrect interpretations and the adoption of flawed methods [1].
Defining the Core Concepts
Accuracy, Trueness, and Precision
According to the International Organization for Standardization (ISO), the terminology surrounding measurement error is precisely defined [15]:
- Trueness refers to the closeness of agreement between the average of a large number of test results and a true or accepted reference value. It is a measure of systematic error [15].
- Precision is the closeness of agreement between independent test results obtained under stipulated conditions. It is a measure of random error and is often described in terms of repeatability (same instrument, operator, short time period) and reproducibility (different instruments, operators, longer time periods) [15].
- Accuracy is a more general term that, in its ISO definition, encompasses both trueness and precision. It describes the closeness of a measurement to the true value, accounting for both systematic and random errors [15].
The relationship between these concepts is illustrated in the following diagram.
Bias and Precision in Method-Comparison Studies
In the specific context of a method-comparison study, where a new method is tested against an established one, the terminology is often operationalized as follows [14]:
- Bias: This represents the systematic error or the mean difference between the new method and the established comparison method. It quantifies how much higher (positive bias) or lower (negative bias) the new method reads on average [14] [2]. It is the primary measure of inaccuracy in a comparison study.
- Precision: Here, precision typically refers to the repeatability of a method—the degree to which it produces the same result on repeated measurements of the same sample [14]. The standard deviation (SD) of the differences between paired measurements is a key measure of this variability.
Agreement vs. Association
A critical distinction must be made between agreement and association.
- Agreement answers the question: "Do the two methods produce the same value for the same sample?" It is concerned with the identity of the measurements and is assessed by examining the differences between paired results [1] [16].
- Association answers the question: "Is there a linear relationship between the measurements from the two methods?" It assesses whether one variable changes predictably with another, but not whether the values are identical [1].
A high correlation can exist even when there is a large, clinically unacceptable bias, as demonstrated in the example below where two methods for measuring glucose have a perfect correlation (r=1.00) but are not comparable due to a large proportional bias [1].
Table: Example Demonstrating Perfect Association but Poor Agreement
| Sample Number | Method 1 (mmol/L) | Method 2 (mmol/L) |
|---|---|---|
| 1 | 1 | 5 |
| 2 | 2 | 10 |
| 3 | 3 | 15 |
| 4 | 4 | 20 |
| 5 | 5 | 25 |
| 6 | 6 | 30 |
| 7 | 7 | 35 |
| 8 | 8 | 40 |
| 9 | 9 | 45 |
| 10 | 10 | 50 |
Source: Adapted from acutecaretesting.org [1]
Designing a Method-Comparison Experiment
A well-designed experiment is the cornerstone of a valid method comparison. Careful planning minimizes the impact of extraneous variables and ensures the results are reliable [1] [17].
Key Design Considerations
- Selection of Methods: The two methods must be intended to measure the same underlying quantity (measurand). Comparing a pulse oximeter (measuring oxygen saturation) with a transcutaneous oxygen sensor (measuring partial pressure) is not appropriate, even if the results are related [14].
- Sample Number and Selection: A minimum of 40 patient samples is recommended, with larger numbers (100-200) providing better ability to detect issues like sample-specific interferences [1] [17]. Samples must be carefully selected to cover the entire clinically meaningful measurement range, not just a narrow interval [1] [17] [14].
- Replication and Timing: Whenever feasible, duplicate measurements should be performed for at least one of the methods to minimize random variation and help identify outliers [1] [17]. Measurements by the two methods should be made as simultaneously as possible to ensure the underlying quantity has not changed [14].
- Time Period: The experiment should be conducted over multiple runs and a minimum of 5 days to capture typical day-to-day performance variations and mimic real-world conditions [1] [17].
- Specimen Stability: Samples should be analyzed within their stability window, ideally within 2 hours of each other, to ensure differences are not due to sample degradation [17].
Experimental Protocol for a Comparison Study
The following workflow outlines the key stages of a robust method-comparison experiment.
Analyzing and Interpreting Comparison Data
Graphical Analysis: The First and Essential Step
Before any statistical calculations, data must be visualized to identify patterns, outliers, and potential problems [1] [17].
- Scatter Plots: A scatter diagram plots the result from the new method (y-axis) against the result from the comparative method (x-axis). This provides a visual impression of the linearity of the relationship and the range of data. A visual line of identity (y=x) can be added to help judge agreement [1].
- Bland-Altman Difference Plots: This is the recommended graphical tool for assessing agreement [14]. The plot displays the average of the two measurements for each sample on the x-axis [(Method A + Method B)/2] and the difference between the two measurements (Method A - Method B) on the y-axis. This plot allows for direct visualization of the bias and its consistency across the measurement range [14].
Statistical Analysis: Quantifying Bias and Agreement
Statistical calculations provide numerical estimates of the errors observed graphically.
- Bias and Limits of Agreement: As proposed by Bland and Altman, the primary statistics for agreement are the bias (mean difference) and the limits of agreement (LOA), defined as Bias ± 1.96 × SD of the differences [14] [2]. The LOA estimate the interval within which 95% of the differences between the two methods are expected to lie. If the differences within these limits are not clinically important, the two methods can be considered interchangeable [14] [2].
- Linear Regression: For data covering a wide analytical range, linear regression (e.g., Deming or Passing-Bablok) is useful. It models the relationship as Y = a + bX, where the intercept (a) indicates constant bias and the slope (b) indicates proportional bias. The systematic error at any critical medical decision concentration (Xc) can be calculated as SE = (a + bXc) - Xc [17].
Table: Summary of Key Analytical Techniques in Method Comparison
| Technique | Primary Purpose | Key Outputs | Interpretation |
|---|---|---|---|
| Bland-Altman Plot | Visual assessment of agreement across measurement range. | Mean difference (Bias), Limits of Agreement (Bias ± 1.96SD). | If the bias is small and the LOA are clinically acceptable, methods may be interchangeable. |
| Linear Regression | Model the relationship between methods and identify error types. | Y-intercept (constant bias), Slope (proportional bias), Standard Error of the Estimate (sy/x). | Intercept significantly different from 0 suggests constant bias; slope significantly different from 1 suggests proportional bias. |
| Correlation Analysis | Assess the strength of a linear relationship. | Correlation Coefficient (r), Coefficient of Determination (r²). | Not a measure of agreement. A high r can exist even with large, clinically unacceptable bias [1]. |
A Decision Framework for Method Interchangeability
The following diagram synthesizes the analytical steps into a logical framework for deciding whether two methods can be used interchangeably.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key solutions and materials required for conducting a high-quality method-comparison study in an analytical laboratory.
Table: Essential Research Reagents and Materials for Method-Comparison Studies
| Item | Function / Purpose |
|---|---|
| Patient-Derived Samples | A minimum of 40-100 unique samples, carefully selected to cover the entire clinically reportable range. These are the core "reagents" for testing real-world performance and specificity [1] [17]. |
| Commercial Quality Control (QC) Materials | Used to verify that both the new and comparative methods are operating within predefined performance specifications for precision and trueness before and during the analysis of patient samples. |
| Reference Standard / Calibrator | A material with a known assigned value, traceable to a higher-order reference method. It is used to calibrate the comparative method (if it is a reference method) and ensure the accuracy base of the measurement scale [17]. |
| Statistical Software Package | Software capable of performing specialized analyses such as Bland-Altman plots, Deming regression, and Passing-Bablok regression is essential for correct data interpretation [14]. |
| Stable Sample Collection Tubes | Appropriate collection containers with necessary preservatives or anticoagulants to ensure specimen integrity and stability throughout the testing period, which may extend over several hours [17]. |
| AG1557 | AG1557, CAS:189290-58-2, MF:C16H14IN3O2, MW:407.21 g/mol |
| AGK2 | AGK2, CAS:304896-28-4, MF:C23H13Cl2N3O2, MW:434.3 g/mol |
Navigating the essential terminology of bias, precision, and agreement is fundamental to conducting valid method-comparison studies. Remember that association, measured by correlation, is not agreement. A successful comparison relies on a robust experimental design that incorporates a sufficient number of samples across a wide range, analyzed in duplicate over multiple days. The data must first be visually inspected using scatter and Bland-Altman difference plots, followed by quantitative analysis to estimate bias and its 95% limits of agreement. Only when both the average bias and the spread of differences (the limits of agreement) fall within pre-defined, clinically acceptable limits can two methods be considered truly interchangeable for use in research and patient care.
From Theory to Practice: Designing and Executing Your Comparison Study
In method comparison and acceptance research, the integrity of scientific conclusions is fundamentally dependent on a meticulously planned study design. The determination of sample size, measurement range, and data collection timing forms the critical foundation for producing statistically sound and reproducible results. These elements directly influence a study's ability to detect clinically relevant differences between measurement methods while minimizing resource expenditure. Recent surveys of published research indicate that improper attention to these design elements remains a prevalent issue, undermining the reliability of scientific findings across various fields [18] [19]. This guide examines optimal design parameters for studies involving 40-100 specimens, contextualized within a broader thesis on statistical methodology for method comparison acceptance. We present objective comparisons of different methodological approaches supported by experimental data and provide detailed protocols for implementation.
Theoretical Framework and Key Concepts
Fundamental Principles of Sample Size Determination
Sample size planning represents a critical balance between statistical power, practical constraints, and ethical considerations. An underpowered study with insufficient samples risks failing to detect true methodological differences, while an excessively large sample wastes resources and may identify statistically significant but clinically irrelevant effects [20]. In method comparison studies, sample size determination requires explicit consideration of several statistical parameters: the acceptable margin of agreement between methods, the expected variability in measurements, and the desired confidence level for estimated parameters [19].
For studies within the 40-100 specimen range, researchers must consider both the precision of agreement limits and the assurance probability that observed agreement will fall within predefined clinical acceptability thresholds. Recent methodological advancements have enabled more exact sample size procedures that account for the distributional properties of agreement metrics, moving beyond traditional rules-of-thumb that often proved inadequate for specific research contexts [19].
The Role of Measurement Range and Timing
The measurement range included in a method comparison study must adequately represent the entire spectrum of values encountered in clinical practice. Restricting the range of measured values may lead to biased agreement estimates and limit the generalizability of study findings. The Preiss-Fisher procedure provides a visual tool for assessing whether study specimens adequately cover the clinically relevant measurement range [19].
The timing of measurements introduces additional methodological considerations, particularly regarding the management of autocorrelation, seasonality effects, and non-stationary data in longitudinal assessments. Proper accounting for these temporal factors is essential for obtaining unbiased estimates of method agreement [18]. For studies implementing repeated measurements, the timing between assessments must be sufficient to minimize carryover effects while maintaining clinical relevance.
Methodological Approaches
Statistical Methods for Sample Size Determination
Table 1: Statistical Methods for Sample Size Determination in Method Comparison Studies
| Method | Application Context | Key Assumptions | Sample Size Considerations |
|---|---|---|---|
| Bland-Altman with Confidence Intervals [19] | Method comparison with single measurements | Normally distributed differences between methods | Based on expected width of confidence interval for limits of agreement |
| Equivalence Testing for Agreement [19] | Studies with repeated measurements (k ≥ 2) | Known unacceptable within-subject variance (σ²U) | Derived from degrees of freedom calculation; depends on number of replicates |
| LOAM for Multiple Observers [19] | Inter-rater reliability with multiple observers | Additive two-way random effects model | Precision improved more by increasing observers than increasing subjects |
| Simulation-Based Approaches [21] [19] | Complex models with multiple variance components | Model parameters can be specified | Flexible approach for advanced statistical models |
Experimental Design Considerations
The selection of an appropriate experimental design depends on the specific research question, measurement constraints, and analytical requirements. Parallel designs where measurements are obtained simultaneously by different methods facilitate direct comparison but may not be feasible for all measurement modalities. Repeated measures designs allow for the estimation of within-subject variability but require careful consideration of time interval selection to minimize learning effects and biological variation [22].
For studies evaluating the impact of interventions or temporal trends, interrupted time series (ITS) designs provide a robust quasi-experimental framework. Proper implementation of ITS requires careful attention to autocorrelation, seasonality, and model specification to avoid biased effect estimates [18]. Recent surveys indicate that these methodological considerations are often overlooked in practice, highlighting the need for more rigorous design reporting.
Diagram 1: Method Comparison Study Workflow. This diagram illustrates the sequential phases in designing and implementing a method comparison study, highlighting critical decision points at each stage.
Experimental Protocols
Protocol for Method Comparison Studies (40-60 Specimens)
This protocol is optimized for preliminary method comparison studies with moderate resource availability:
Sample Selection and Preparation: Select 40-60 specimens to adequately represent the entire clinical measurement range. Use the Preiss-Fisher procedure to visually confirm appropriate range coverage [19]. Ensure specimens are stable throughout the testing period to minimize degradation effects.
Measurement Procedure: Perform duplicate measurements with each method in randomized order to control for time-dependent effects. Maintain consistent environmental conditions (temperature, humidity) throughout testing. Blind operators to previous results and method identities to prevent measurement bias.
Data Collection: Record all measurements using structured electronic data capture forms. Include relevant covariates that may influence measurement variability (operator, batch, time of day). Implement quality control checks to identify transcription errors or measurement outliers.
Statistical Analysis: Apply Bland-Altman analysis with calculation of 95% limits of agreement. Compute confidence intervals for agreement limits using exact procedures rather than asymptotic approximations [19]. Assess normality of differences using graphical methods and formal statistical tests.
Protocol for Comprehensive Method Validation (80-100 Specimens)
This enhanced protocol provides greater precision for definitive method validation studies:
Sample Selection Strategy: Employ stratified sampling across the clinical range to ensure uniform representation. Include 80-100 specimens to improve precision of variance component estimates. Consider including known reference standards to assess accuracy.
Measurement Design: Implement a balanced design with repeated measurements (2-3 replicates per method) to enable estimation of within-subject variance components. Randomize measurement order across operators and instruments to minimize systematic bias.
Timing Considerations: Standardize time intervals between repeated measurements to control for biological variation. For stability assessments, incorporate planned intervals that reflect clinical usage patterns. Document environmental conditions at each measurement time point.
Advanced Statistical Analysis: Employ variance component analysis to partition total variability into within-subject, between-subject, and method-related components. For multiple observers, use the Limits of Agreement with the Mean (LOAM) approach to account for rater effects [19].
Comparative Analysis and Results
Sample Size Recommendations Across Study Types
Table 2: Recommended Sample Sizes for Different Study Designs
| Study Objective | Minimum Sample Size | Recommended Sample Size | Key Determinants |
|---|---|---|---|
| Preliminary Method Comparison | 40 | 50-60 | Expected difference between methods, within-subject variability |
| Definitive Agreement Study | 60 | 80-100 | Clinical agreement margins, assurance probability |
| Inter-rater Reliability | 30 subjects, 3-5 raters | 40 subjects, 5-8 raters | Number of raters, variance components |
| Longitudinal Method Monitoring | 40 with repeated measures | 60-80 with repeated measures | Autocorrelation, seasonality effects |
Impact of Sample Size on Precision of Agreement Estimates
Empirical investigations demonstrate that sample sizes below 40 specimens often produce unacceptably wide confidence intervals for clinical agreement limits. Analysis of variance component stability indicates that 50 specimens with 3 repeated measurements generally provides sufficient precision for most method comparison applications [19]. Increasing sample size beyond 100 specimens yields diminishing returns for precision improvement, with greater gains achieved through optimized measurement design and increased replication.
Studies incorporating multiple observers demonstrate that precision improvement depends more on increasing the number of observers than increasing the number of subjects. This highlights the distinctive design considerations for inter-rater reliability studies compared to method comparison applications [19].
Diagram 2: Factors Influencing Sample Size Decisions. This diagram illustrates the relationship between sample size and key study quality metrics, highlighting the balance between precision and feasibility.
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Method Comparison Studies
| Item | Function | Application Notes |
|---|---|---|
| Stable Reference Standards | Calibration and quality control | Verify measurement accuracy across methods; essential for traceability |
| Quality Control Materials | Monitoring measurement precision | Should span clinically relevant range; used to assess within- and between-run variability |
| Specimen Collection Supplies | Standardized sample acquisition | Consistency critical for minimizing pre-analytical variability |
| Data Management System | Structured data capture | Essential for maintaining data integrity and supporting statistical analysis |
| Statistical Software Packages | Data analysis and visualization | R, SAS, or Python with specialized packages for agreement statistics |
| Apiole | Apiole, CAS:523-80-8, MF:C12H14O4, MW:222.24 g/mol | Chemical Reagent |
| Arctigenin mustard | Arctigenin Mustard|CAS 26788-57-8|MCE | Arctigenin mustard is a biologically active compound for research use only (RUO). It is not for human or veterinary diagnostic or therapeutic use. |
Specialized Methodological Tools
Advanced method comparison studies benefit from specialized analytical tools, including the mlpwr package in R for simulation-based power analysis of complex designs [21]. This package enables researchers to optimize multiple design parameters simultaneously, such as balancing the number of participants and measurement time points within resource constraints. For studies employing Bland-Altman analysis, specialized R scripts are available for exact sample size calculations and confidence interval estimation [19].
Discussion and Implementation Guidelines
Interpretation of Findings
The evidence presented supports the conclusion that sample sizes between 40-100 specimens represent an optimal range for most method comparison studies, providing sufficient statistical power while maintaining practical feasibility. Studies employing fewer than 40 specimens frequently demonstrate inadequate precision in agreement estimates, while those exceeding 100 specimens often represent inefficient resource allocation unless particularly small effect sizes or complex variance structures are anticipated.
The measurement range inclusion emerges as a critical factor frequently overlooked in methodological planning. Specimens must adequately represent the entire clinical spectrum to ensure agreement estimates remain valid across all potential applications. Restricting measurement range to a narrow interval represents a common methodological flaw that limits the utility of study findings.
Practical Recommendations for Implementation
Preliminary Studies: For initial method comparisons, target 50-60 specimens with duplicate measurements. This provides robust estimates of agreement while conserving resources for definitive validation if required.
Definitive Validation: Plan for 80-100 specimens with appropriate replication when establishing method agreement for regulatory submissions or clinical implementation decisions.
Range Considerations: Ensure specimens are distributed across the entire clinically relevant measurement range rather than clustered around specific values.
Timing Optimization: Standardize measurement intervals and account for potential temporal effects through appropriate statistical modeling.
Reporting Standards: Adhere to Guidelines for Reporting Reliability and Agreement Studies (GRRAS) to ensure transparent and complete reporting of methodological details and results [19].
By implementing these evidence-based recommendations, researchers can optimize their study designs to produce methodologically sound, efficient, and clinically relevant method comparison studies.
In method comparison and acceptance research, the integrity of experimental conclusions rests upon two foundational pillars of data collection: appropriate replication of measurements and rigorous randomization. These practices are crucial for controlling variability and ensuring that observed differences are attributable to the methods being compared rather than extraneous factors. Duplicate measurements provide a mechanism for quantifying and controlling random error inherent in any analytical system, while randomization serves as a powerful tool for minimizing bias and establishing causal inference in experimental designs. Within statistical analysis frameworks, these methodologies protect against both Type I errors (false positives) and Type II errors (false negatives) by ensuring that variability is properly accounted for and that comparison groups are functionally equivalent before treatment application [23] [24]. For researchers, scientists, and drug development professionals, implementing systematic approaches to replication and randomization is not merely advisory but essential for producing reliable, defensible, and actionable scientific evidence.
The Role and Implementation of Duplicate Measurements
Understanding Technical and Biological Replicates
In experimental science, not all replicates are equivalent. Understanding the distinction between technical and biological replicates is fundamental to appropriate study design:
- Technical replicates involve repeated measurements of the same biological sample using the same experimental procedure. They primarily serve to quantify the variability introduced by the measurement technique itself (e.g., running the same serum sample multiple times on an analyzer) [25].
- Biological replicates are measurements taken from distinct biological specimens (e.g., blood samples from different individual patients). They account for natural biological variability and form the bedrock of sound statistical inference about populations [25].
The strategic choice between these replicate types depends on the research question. Technical replicates control for methodological noise, while biological replicates ensure that findings are generalizable beyond a single sample.
Comparison of Measurement Approaches
The number of repeated measurements per sample represents a practical balance between statistical precision and resource efficiency. The table below summarizes the key considerations for single, duplicate, and triplicate measurements:
Table: Comparison of Technical Replication Strategies
| Replication Approach | Primary Use Case | Error Management Capability | Throughput & Resource Efficiency |
|---|---|---|---|
| Single Measurements | Qualitative analysis, high-throughput screening when group means are more important than individual values | No error detection or correction; relies on retesting criteria for outliers | Maximum throughput and resource efficiency |
| Duplicate Measurements | Quantitative analysis where balance between accuracy and efficiency is needed; recommended for most ELISA applications | Enables error detection through variability thresholds (e.g., %CV >15-20%) but requires retesting if threshold exceeded | Optimal balance; approximately 50% lower throughput than single measurements |
| Triplicate Measurements | Situations requiring high precision for individual sample quantification; when data precision is paramount | Allows both error detection and correction through outlier exclusion; provides most reliable mean estimate | Lowest throughput and efficiency; ~67% lower than single measurements |
As illustrated, duplicate measurements typically represent the "sweet spot" for most quantitative applications, enabling error detection while maintaining practical efficiency [25]. Single measurements are suitable only when the consequences of undetected measurement errors have been compensated by the assay design or when qualitative results are sufficient.
Experimental Protocol for Replication Experiments
A standardized replication experiment estimates the random error (imprecision) of an analytical method. The following protocol is adapted from clinical laboratory validation practices [26]:
Material Selection: Select at least two different control materials that represent medically relevant decision concentrations (e.g., low and high clinical thresholds).
Short-term Imprecision Estimation:
- Analyze 20 samples of each material within a single analytical run or within one day.
- Calculate the mean, standard deviation (SD), and coefficient of variation (CV) for each material.
- Acceptance criterion: Short-term imprecision (SD) should be ≤ 0.25 × total allowable error (TEa).
Long-term Imprecision Estimation:
- Analyze one sample of each material on 20 different days.
- Calculate the mean, SD, and CV for each material.
- Acceptance criterion: Total imprecision (SD) should be ≤ 0.33 × TEa.
This structured approach systematically characterizes both within-run/day and between-day components of variability, providing a comprehensive picture of method performance.
Diagram: Measurement Replication Strategy Selection
Randomization Principles and Applications
Conceptual Basis for Randomization
Randomization serves as the cornerstone of causal inference in experimental research. By randomly assigning experimental units to treatment or control conditions, researchers ensure that the error term in the average treatment effect (ATE) estimation is zero in expectation [24]. Formally, this can be expressed as:
$$ \bar{Y1} - \bar{Y0} = \bar{\beta1}+\sum{j=1}^J \gammaj(\bar{x}{1j}-\bar{x}_{0j}) $$
Where the second term represents the "error term" - the average difference between treatment and control groups unrelated to the treatment. Randomization ensures this error term equals zero in expectation, making the ATE estimate ex ante unbiased [24]. This process effectively balances both observed and unobserved covariates across treatment groups, creating comparable groups that differ primarily in their exposure to the experimental intervention.
Randomization Units in Experimental Design
The choice of randomization unit fundamentally affects the design, interpretation, and statistical power of an experiment. The following table compares common randomization units:
Table: Comparison of Randomization Units in Experimental Design
| Randomization Unit | Key Characteristics | Advantages | Limitations |
|---|---|---|---|
| User ID-Based | Assigns unique users to groups for test duration | Consistent user experience across sessions; ideal for long-term effects measurement | Requires user registration/login; potential privacy concerns; reduced sample size |
| Cookie-Based | Uses browser cookies to assign anonymous users | Privacy-friendly; no registration required; larger potential sample size | Inconsistent across devices/browsers; vulnerable to user deletion; short-term focus |
| Session-Based | Assigns variants per user session | Rapid sample size accumulation; suitable for single-session behaviors | Inconsistent user experience; cannot measure long-term effects |
| Cluster-Based | Randomizes groups rather than individuals | Minimizes contamination; practical when individual randomization impossible | Reduces effective sample size; requires more complex power calculations |
The optimal randomization unit depends on the research context, with the general principle being to select the unit that minimizes contamination between treatment and control conditions while maintaining practical feasibility [27] [24].
Randomization Methods and Implementation
Several methodological approaches to randomization exist, each with distinct advantages:
Simple Randomization: Comparable to a lottery with replacement, where each unit has equal probability of assignment to any group. This approach may result in imbalanced group sizes, particularly with small samples [24].
Permutation Randomization: Assignment without replacement ensures exactly equal group sizes when the final sample size is known in advance. This approach maximizes statistical power for a given sample size and is typically implemented using statistical software for replicability [24].
Stratified Randomization: Researchers first divide the sample into strata based on important covariates (e.g., disease severity, age groups), then randomize within each stratum. This approach improves balance on known prognostic factors, particularly in smaller studies [24].
Cluster Randomization: When individual randomization risks contamination (e.g., educational interventions where students within schools interact), randomizing intact clusters (schools, clinics, communities) preserves the integrity of the treatment effect estimate despite reduced statistical power [24].
Diagram: Randomization Unit Selection Workflow
Statistical Analysis Considerations
Analytical Approaches for Repeated Measures
Studies incorporating duplicate or repeated measurements require specialized statistical approaches that account for the correlation between measurements from the same experimental unit. Common methods include:
Repeated Measures ANOVA: Extends traditional ANOVA to handle correlated measurements but requires strict assumptions including sphericity (constant variance across time points) and complete data for all time points. Violations of sphericity can be addressed with corrections like Greenhouse-Geisser or Huynh-Feldt [28].
Mixed-Effects Models: A more flexible framework that includes both fixed effects (e.g., treatment group) and random effects (e.g., individual experimental units). These models can handle unbalanced data (unequal numbers of measurements), account for various correlation structures, and accommodate missing data under missing-at-random assumptions [28].
The choice between these approaches depends on study design, data structure, and whether research questions focus on population-average or unit-specific effects.
Addressing Multiple Testing
When conducting multiple statistical comparisons (e.g., analyzing multiple outcomes or time points), the risk of Type I errors (false positives) increases substantially. Without correction, the probability of at least one false positive across 10 independent tests at α=0.05 is approximately 40% [23]. Common adjustment methods include:
- Bonferroni Correction: Divides the significance threshold (α) by the number of tests performed. This conservative approach controls the family-wise error rate but reduces power.
- Tukey's Procedure: Specifically designed for pairwise comparisons following ANOVA, providing less conservative correction than Bonferroni.
- False Discovery Rate (FDR): Controls the expected proportion of false positives among rejected hypotheses, offering a less stringent alternative to family-wise error rate control.
The selection of an appropriate correction method should balance Type I and Type II error concerns based on the research context [23].
Essential Research Reagent Solutions
Table: Key Materials for Replication and Randomization Studies
| Reagent/Resource | Primary Function | Application Context |
|---|---|---|
| Control Materials | Provides stable reference samples with known characteristics | Replication experiments to monitor assay precision over time [26] |
| Statistical Software | Generates randomization sequences and analyzes repeated measures | Implementing permutation randomization; fitting mixed-effects models [28] [24] |
| ELISA Kits | Quantifies protein biomarkers using enzymatic detection | Common platform for implementing duplicate/triplicate measurements [25] |
| Sample Size Calculation Tools | Determines required sample size for target statistical power | Planning randomization schemes; ensuring adequate power for cluster designs [24] |
Duplicate measurements and randomization represent complementary approaches to enhancing the validity and reliability of method comparison studies. Appropriate replication strategies enable researchers to quantify and control technical variability, while careful randomization prevents systematic bias and supports causal inference. The optimal implementation of these techniques requires thoughtful consideration of research goals, constraints, and analytical implications. As methodological best practices continue to evolve, researchers should maintain awareness of emerging approaches such as mixed-effects models and Bayesian hierarchical models that offer enhanced flexibility for complex experimental designs. By systematically applying these data collection fundamentals, researchers in drug development and scientific research can produce more robust, reproducible, and clinically meaningful findings.
In method comparison and acceptance research, particularly within drug development, identifying atypical data points is a fundamental step to ensure analytical validity. Outliers—observations that deviate markedly from other members of the sample—can significantly skew the results of a statistical analysis, leading to incorrect conclusions about a method's performance [29]. The initial graphical exploration of data is not merely a preliminary step but a critical diagnostic tool. It provides an intuitive, visual means to assess data structure, identify unexpected patterns, and flag potential anomalies that could unduly influence subsequent statistical models [30].
Two plots are indispensable for this initial exploration: the Scatter Plot and the Difference Plot (also known as a Bland-Altman plot). While both serve the overarching goal of outlier detection, they illuminate different aspects of the data. A Scatter Plot is paramount for visualizing the overall relationship and conformity between two measurement methods, helping to spot values that fall outside the general trend. Conversely, a Difference Plot focuses explicitly on the agreement between methods by plotting the differences between paired measurements against their averages, making it exceptionally sensitive to patterns that might indicate systematic bias or heteroscedasticity, beyond just identifying outliers [29]. This guide provides an objective comparison of these two techniques, supported by experimental data and detailed protocols, to equip researchers with the knowledge to apply them effectively in rigorous acceptance research.
Conceptual Foundations: Outliers, Leverage, and Influence
Before delving into graphical techniques, it is crucial to understand what constitutes an outlier and its potential impact. In regression analysis, often used in method comparison, a clear distinction is made among three concepts:
- Outlier: A data point whose response (y) value does not follow the general trend of the rest of the data. It is extreme in the y-direction [29].
- High Leverage Point: A data point that has "extreme" predictor (x) values. With multiple predictors, this can be an unusual combination of values. It is extreme in the x-direction [29].
- Influential Point: A data point that unduly influences any part of a regression analysis, such as the estimated slope coefficients or hypothesis test results. An influential point is often both an outlier and has high leverage [29].
Table 1: Classification and Impact of Atypical Data Points
| Data Point Type | Definition | Primary Graphical Detection | Potential Impact on Regression |
|---|---|---|---|
| Outlier | Extreme in the Y-direction (response) | Scatter Plot, Difference Plot | Increases standard error; may not always be highly influential. |
| High Leverage Point | Extreme in the X-direction (predictor) | Scatter Plot | Can pull the regression line towards it; impact depends on its Y-value. |
| Influential Point | Both an outlier and has high leverage | Combined analysis of both plots | Significantly alters the slope, intercept, and overall model conclusions. |
Understanding this distinction is key. A point can be an outlier without having high leverage, and a point can have high leverage without being an outlier. However, it is the combination of both—a point that is extreme in both the x- and y-directions—that often has a disproportionate and damaging effect on the analytical results, potentially leading to a flawed method acceptance decision [29].
Experimental Protocols for Outlier Detection
Protocol 1: Scatter Plot Analysis
Objective: To visually assess the correlation and conformity between two methods and identify observations that deviate significantly from the overall linear trend.
Materials:
- Paired dataset of measurements from two methods (Method A and Method B).
- Statistical software capable of generating scatter plots (e.g., R, Python, JASP, SPSS).
Methodology:
- Data Preparation: Organize the data into two columns, each representing the paired measurements from Method A and Method B for the same samples.
- Plot Generation: Create a scatter plot with Method A values on the x-axis and Method B values on the y-axis.
- Reference Line: Add a line of equality (y=x) to the plot. This line represents perfect agreement between the two methods.
- Trend Analysis: Visually inspect the cloud of data points. A strong, linear cluster along the line of equality suggests good agreement.
- Outlier Identification: Identify data points that fall far from the main cluster and the line of equality. These are potential outliers. As illustrated in research, a point that does not follow the general trend of the rest of the data is classified as an outlier [29].
- Leverage Assessment: Identify points with extreme values on the x-axis (Method A); these are high-leverage points that may require further investigation.
Protocol 2: Difference Plot (Bland-Altman) Analysis
Objective: To visualize the agreement between two methods by plotting the differences between paired measurements against their averages, thereby identifying outliers and systematic biases.
Methodology:
- Calculation:
- For each pair of measurements, calculate the difference: ( \text{Difference} = \text{Method A} - \text{Method B} ).
- For each pair, calculate the average: ( \text{Average} = \frac{\text{Method A} + \text{Method B}}{2} ).
- Plot Generation: Create a new plot with the calculated Averages on the x-axis and the corresponding Differences on the y-axis.
- Reference Lines:
- Add a horizontal line at the mean of all the differences (the "bias").
- Add horizontal lines at the mean difference ± 1.96 standard deviations of the differences. These represent the 95% limits of agreement.
- Outlier Identification: Identify data points where the difference (y-value) falls outside the 95% limits of agreement. These points represent measurements where the disagreement between methods is greater than expected and are considered outliers in the context of agreement.
- Pattern Analysis: Analyze the plot for any systematic patterns, such as a funnel shape (where variability increases with the magnitude of measurement), which would indicate heteroscedasticity.
The following workflow diagram illustrates the application of these two protocols for comprehensive outlier detection.
Comparative Performance Analysis
To objectively compare the performance of scatter plots and difference plots, we can simulate a dataset typical of a method comparison study, introducing known outliers and biases. The following table summarizes the detection capabilities of each plot type based on such an analysis.
Table 2: Performance Comparison of Scatter Plots vs. Difference Plots
| Detection Feature | Scatter Plot | Difference Plot |
|---|---|---|
| Overall Correlation Visualization | Excellent; directly shows the functional relationship. | Poor; not designed for this purpose. |
| Identification of Y-Direction Outliers | Excellent; visually obvious as points off the trend. | Excellent; points outside the limits of agreement. |
| Identification of X-Direction (Leverage) Points | Excellent; visually obvious as points on the far left/right. | Poor; does not directly display predictor extremity. |
| Detection of Systematic Bias (Mean Shift) | Indirect; requires checking deviation from y=x line. | Excellent; the central line (mean difference) directly shows bias. |
| Detection of Proportional Bias / Heteroscedasticity | Can be detected if the slope deviates from 1. | Excellent; a clear trend in the spread of differences vs. average is visible. |
| Ease of Interpreting Limits of Agreement | Not applicable. | Excellent; calculated directly and plotted. |
| Primary Use Case | Initial exploration of relationship and leverage. | In-depth analysis of agreement and difference patterns. |
The scatter plot is unparalleled for giving an immediate, intuitive overview of the data structure and for flagging points with high leverage. However, its ability to quantify the disagreement between methods is limited. The difference plot, while less informative about the overall correlation, excels at quantifying and visualizing the nature and extent of the disagreement, making it uniquely powerful for identifying outliers defined by poor agreement and for diagnosing the underlying reasons for that disagreement, such as increasing variability with concentration.
The Scientist's Toolkit: Essential Research Reagents & Software
Implementing the described protocols requires a set of statistical and computational tools. The table below details key software solutions used in the field for data analysis and visualization, relevant to method comparison studies.
Table 3: Essential Software Tools for Statistical Analysis and Visualization
| Tool Name | Type / Category | Primary Function in Analysis |
|---|---|---|
| R & RStudio [30] | Programming Environment / IDE | Provides a comprehensive, open-source platform for statistical computing and graphics via packages like ggplot2. |
| Python (with Scikit-learn) [31] | Programming Language / Library | Offers versatile data manipulation (Pandas) and access to outlier detection algorithms (Elliptic Envelope, Isolation Forest). |
| JASP [32] | Graphical Statistical Software | Provides a user-friendly, open-source interface for both frequentist and Bayesian analyses, with dynamic output updates. |
| SPSS [33] | Statistical Software Suite | A widely used commercial tool with an intuitive interface for statistical analysis, often employed in social and biological sciences. |
| Scikit-learn [31] | Python Machine Learning Library | Implements various unsupervised outlier detection algorithms like Local Outlier Factor (LOF) and One-Class SVM. |
| Aucubigenin | Aucubigenin, CAS:64274-28-8, MF:C9H12O4, MW:184.19 g/mol | Chemical Reagent |
The following diagram outlines the decision pathway for selecting an appropriate outlier detection method, moving from initial graphical analysis to more advanced algorithmic approaches, which can be implemented using tools like those listed in Table 3.
In the rigorous context of statistical analysis for method comparison acceptance research, a "graphical analysis first" approach is not just recommended, it is essential. Scatter plots and difference plots are complementary, not redundant, tools in the analyst's arsenal. The scatter plot serves as the primary tool for understanding the overall relationship and for identifying points with high leverage—those that are extreme in the predictor space. The difference plot (Bland-Altman) is the specialist tool for quantifying agreement, diagnosing the specific nature of disagreements (bias, heteroscedasticity), and identifying outliers defined by excessive difference.
As demonstrated, a point can be an outlier in a scatter plot by not following the trend, and a point can be an outlier in a difference plot by falling outside the limits of agreement. However, it is the points that are flagged by both methods—those that are both extreme in their difference and exert high leverage on the model—that are most likely to be influential points [29]. These points warrant careful investigation before a final decision on method acceptance is made. Therefore, a robust outlier detection strategy in drug development and scientific research must employ both graphical techniques to ensure that analytical results are both statistically sound and reliable.
Deming vs. Passing-Bablok Regression Explained
In method comparison studies, which are crucial for validating new analytical techniques against established ones in fields like clinical chemistry and pharmaceutical sciences, selecting the correct statistical approach is fundamental. Ordinary least squares (OLS) regression is often inappropriate as it assumes that only the dependent (Y) variable contains measurement error, while the independent (X) variable is fixed and known with certainty. This assumption is frequently violated when comparing two measurement methods, both of which are subject to error. Two specialized regression techniques—Deming regression and Passing-Bablok regression—are designed specifically for such scenarios where both variables are measured with error. Understanding their distinct assumptions, strengths, and limitations is essential for researchers, scientists, and drug development professionals to draw valid conclusions about method agreement and systematic biases.
Theoretical Foundations and Key Differences
The core difference between these methods lies in their underlying statistical assumptions and their approach to handling measurement errors. The following table summarizes their fundamental characteristics:
Table 1: Core Characteristics of Deming and Passing-Bablok Regression
| Feature | Deming Regression | Passing-Bablok Regression |
|---|---|---|
| Statistical Basis | Parametric [34] | Non-parametric [35] [36] [37] |
| Error Distribution Assumption | Assumes errors are normally distributed [34] [38] | No assumptions about the distribution of errors [35] [36] [37] |
| Error Variance | Requires an estimate of the error ratio (λ) between the two methods [34] [38] [39] | Robust to the distribution and variance of errors [35] [36] |
| Handling of Outliers | Sensitive to outliers, as it is based on means and variances [34] | Highly robust to outliers due to the use of medians [35] [37] |
| Primary Application | When measurement errors can be assumed to be normally distributed [34] [40] | When error distribution is unknown or non-normal, or when outliers are present [35] [37] |
Deming Regression: A Parametric Approach
Deming regression is an extension of simple linear regression that accounts for random measurement errors in both the X and Y variables [34] [39]. It requires the error ratio (λ), which is the ratio of the variances of the measurement errors for the two methods, to be specified or estimated from the data. If the error ratio is set to 1, Deming regression is equivalent to orthogonal regression [39]. A key assumption is that the residuals (the differences between the observed and estimated values) are normally distributed [38].
Passing-Bablok Regression: A Non-Parametric Alternative
Passing-Bablok regression is a robust, non-parametric method that makes no assumptions about the distribution of the measurement errors [35] [36] [37]. It is therefore particularly useful when the error structure is unknown or does not follow a normal distribution. The slope of the regression line is calculated as the shifted median of all possible pairwise slopes between the data points, making the procedure resistant to the influence of outliers [35] [37] [39]. An important prerequisite is that the two variables have a linear relationship and are highly correlated [34] [37].
Interpretation of Results and Systematic Bias
Both methods yield a regression equation of the form Y = Intercept + Slope × X, and the parameters are used to identify different types of systematic bias between the two measurement methods.
Table 2: Interpreting Regression Parameters for Method Comparison
| Parameter | What it Represents | How to Evaluate it |
|---|---|---|
| Intercept | Constant systematic difference (bias) between methods [35] [37]. | Calculate its 95% Confidence Interval (CI). If the CI contains 0, there is no significant constant bias [34] [37]. |
| Slope | Proportional difference between methods [35] [37]. | Calculate its 95% CI. If the CI contains 1, there is no significant proportional bias [34] [37]. |
| Residual Standard Deviation (RSD) | Random differences (scatter) between methods [37]. | A smaller RSD indicates better agreement. The interval ±1.96 × RSD is expected to contain 95% of the random differences [37]. |
For both regression types, a scatter plot with the fitted line and the line of identity (X=Y) is recommended for visual assessment. A residual plot is also crucial for checking for patterns that might indicate a non-linear relationship [35] [34] [37].
Decision Workflow and Experimental Protocol
Selecting the appropriate regression method requires a structured evaluation of your data. The following diagram outlines the key decision points:
Application in Experimental Scenarios
The decision to use one method over the other is often dictated by the experimental context and data characteristics:
- Deming Regression in Practice: A study comparing quantitative outputs from next-generation sequencing (NGS) assays utilized Deming regression because it could appropriately handle the errors in both the test and reference methods, allowing the researchers to detect the presence and magnitude of constant and proportional error [40].
- Passing-Bablok Regression in Practice: Passing-Bablok is strongly recommended in clinical laboratory settings where data may contain outliers or the distribution of errors is uncertain. Its non-parametric nature provides robustness, ensuring that the results are not skewed by anomalous measurements [35] [37].
Essential Research Reagent Solutions
When conducting method comparison studies, the following "reagents" or tools are essential for a robust analysis:
Table 3: Essential Tools for Method Comparison Studies
| Tool / Reagent | Function | Example Use-Case |
|---|---|---|
| Statistical Software with MCR | Provides validated implementations of Deming and Passing-Bablok regression. | The mcr package in R [34] or commercial software like NCSS [39], MedCalc [37], or StatsDirect [34] are essential for accurate computation. |
| Bland-Altman Analysis | A complementary method to assess agreement by plotting differences against averages. | It is recommended to supplement Passing-Bablok regression with a Bland-Altman plot to visually assess agreement across the measurement range [37] [39]. |
| Cumulative Sum (CUSUM) Linearity Test | A statistical test to validate the key assumption of a linear relationship between methods. | A small p-value (P<0.05) in the Cusum test indicates significant non-linearity, rendering the Passing-Bablok method invalid [35] [37]. |
| Adequate Sample Size | Prevents biased conclusions by ensuring sufficient statistical power. | Small samples lead to wide confidence intervals, increasing the chance of falsely concluding methods agree. A sample size of at least 40 for Deming [34] and 30-50 for Passing-Bablok [37] is advised. |
Deming and Passing-Bablok regression are both powerful tools for method comparison studies where both measurement procedures are subject to error. The choice between them is not a matter of which is universally better, but which is more appropriate for the specific data at hand. Deming regression is the preferred parametric method when the measurement errors can be reasonably assumed to be normally distributed and the error ratio is known or can be estimated. In contrast, Passing-Bablok regression serves as a robust, non-parametric alternative that is insensitive to the distribution of errors and the presence of outliers, making it ideal for diagnostic and laboratory medicine applications. By applying the decision workflow and adhering to the experimental protocols outlined in this guide, researchers can make an informed selection and generate reliable, defensible conclusions in their method acceptance research.
In scientific research and drug development, the validation of a new measurement method against an existing standard is a critical procedure. A core component of this validation is the quantification of systematic error, also known as bias, which represents a consistent or proportional difference between the observed and true values of a measurement [41]. Unlike random error, which introduces variability and affects precision, systematic error skews measurements in a specific direction, thereby affecting the accuracy of the results [41] [42]. In the context of method comparison, systematic error indicates a consistent discrepancy between two measurement techniques designed to measure the same variable.
The correct statistical approach to assess the degree of agreement between two quantitative methods is not always obvious. While correlation and regression studies are frequently proposed, they are not recommended for assessing comparability between methods because they study the relationship between variables, not the differences between them [43]. Instead, the methodology introduced by Bland and Altman (1983) has become the standard approach, as it directly quantifies agreement by studying the mean difference and constructing limits of agreement [43] [44]. This guide will detail the use of Bland-Altman analysis to objectively quantify systematic error and provide the experimental protocols for its application in method comparison studies.
Quantifying Systematic Error: The Bland-Altman Method
Core Principles and Calculations
The Bland-Altman method, also known as a difference plot, is a graphical technique used to compare two measurement methods [43] [45]. The central idea is to visualize the differences between paired measurements against their averages and to establish an interval within which most of these differences lie. This interval, known as the limits of agreement (LoA), encapsulates the total error between the methods, including both systematic (bias) and random error (precision) [46].
The analysis involves calculating two key parameters:
- The Mean Difference (Bias): This is the average of the differences between the paired measurements (e.g., Method A - Method B) and represents the systematic error or constant bias between the two methods [43] [45].
- The Limits of Agreement (LoA): These are calculated as the mean difference ± 1.96 times the standard deviation of the differences. The interval between these upper and lower limits is expected to contain 95% of the differences between the two measurement methods [43] [45].
Table 1: Key Statistical Parameters in a Bland-Altman Analysis
| Parameter | Calculation | Interpretation |
|---|---|---|
| Mean Difference (Bias) | (\bar{d} = \frac{\sum (Ai - Bi)}{n}) | The average systematic difference between Method A and Method B. |
| Standard Deviation of Differences | (sd = \sqrt{\frac{\sum (di - \bar{d})^2}{n-1}}) | The standard deviation of the differences between methods. |
| Lower Limit of Agreement (LoA) | (\bar{d} - 1.96 \times s_d) | The value below which 95% of the differences between methods will lie. |
| Upper Limit of Agreement (LoA) | (\bar{d} + 1.96 \times s_d) | The value above which 95% of the differences between methods will lie. |
The resulting graph is a scatter plot where the Y-axis shows the difference between the two paired measurements (A-B), and the X-axis represents the average of these two measurements ((A+B)/2) [43]. Horizontal lines are drawn at the mean difference and at the calculated limits of agreement.
Types of Systematic Error Identified
The Bland-Altman plot is particularly useful for visually identifying the nature of the systematic error present. The pattern of the data points on the plot can reveal distinct types of bias:
- Constant Systematic Error (Offset Error): This occurs when a fixed value is consistently added to or subtracted from the true measurement. On a Bland-Altman plot, this appears as the cloud of data points being shifted upwards or downwards from the zero line, but the spread of the differences remains consistent across the measurement range [42] [45]. The mean difference ((\bar{d})) is non-zero, but the slope of the data is flat.
- Proportional Systematic Error (Scale Factor Error): This occurs when the difference between methods changes proportionally with the magnitude of the measurement. It is often due to a miscalibration in the measurement scale. On the plot, this manifests as a clear slope in the data, where the differences increase or decrease as the average value increases [42] [45]. A regression line drawn through the differences can help detect this proportional trend.
Figure 1: Bland-Altman Analysis Workflow. This diagram outlines the logical sequence for conducting a Bland-Altman analysis, from data collection to final interpretation.
Experimental Protocols for Method Comparison
Designing the Comparison Experiment
To obtain reliable estimates of systematic error, the comparison of methods experiment must be carefully designed. Key factors to consider include the selection of the comparative method, the number and type of specimens, and the data collection protocol [17].
- Selection of Comparative Method: The method used for comparison should be selected with care. An ideal comparative method is a reference method whose correctness is well-documented. In practice, most routine methods serve as comparative methods. If large and medically unacceptable differences are found, additional experiments may be needed to identify which method is inaccurate [17].
- Number and Selection of Specimens: A minimum of 40 different patient specimens is recommended. The quality of the experiment depends more on a wide range of test results than a large number of results. Specimens should be carefully selected to cover the entire working range of the method and represent the spectrum of diseases expected in its routine application [17]. For assessing method specificity, larger numbers of specimens (100-200) may be needed.
- Measurement Protocol and Data Collection: Specimens should be analyzed by both methods within a short time frame, typically within two hours of each other, to minimize pre-analytical errors. The experiment should be conducted over multiple days (a minimum of 5 days is recommended) to account for run-to-run variability and provide a more realistic estimate of systematic error [17]. While single measurements are common, duplicate measurements can help identify sample mix-ups or transposition errors.
Statistical Analysis and Interpretation
Once the data is collected, the analysis proceeds with graphing the data and calculating the appropriate statistics.
- Graphing the Data: The initial step is to create a scatter plot of the differences between the methods against the average of the two methods. This visual inspection helps identify any obvious outliers, potential mistakes, and the overall pattern of the differences [17].
- Calculating Statistics: For data covering a wide analytical range, linear regression statistics are preferable as they allow for the estimation of systematic error at specific medical decision concentrations and provide information on the proportional or constant nature of the error [17]. The systematic error (SE) at a critical decision level (Xc) is calculated as SE = Yc - Xc, where Yc is the value predicted by the regression line (Y = a + bX) for that Xc.
- Interpreting Limits of Agreement: The Bland-Altman method defines the intervals of agreement but does not determine their acceptability [43]. Acceptable limits must be defined a priori based on clinical requirements, biological considerations, or analytical goals [43] [45]. If the limits of agreement fall within this pre-defined clinically acceptable range, the two methods can be considered interchangeable. Proper interpretation should also consider the 95% confidence intervals of the limits of agreement [45].
Table 2: Essential Materials for a Method Comparison Study
| Category | Item | Function in Experiment |
|---|---|---|
| Measurement Instruments | Test Method Instrument | The new or alternative method being validated. |
| Comparative Method Instrument | The reference or existing standard method. | |
| Sample Materials | Patient Specimens (n≥40) | To provide a biologically relevant matrix for comparison across the analytical range. |
| Control Materials | To monitor the performance and stability of both methods during the study. | |
| Data Analysis Tools | Statistical Software (e.g., MedCalc) | To perform Bland-Altman analysis, calculate bias, limits of agreement, and create plots. |
| Spreadsheet Software | For initial data entry, management, and basic calculations. | |
| Protocol Documents | Pre-defined Clinical Agreement Limits | A priori criteria for determining the clinical acceptability of the observed differences. |
| Standard Operating Procedures (SOPs) | Detailed protocols for operating both instruments and handling specimens. |
Advanced Considerations in Agreement Analysis
Handling Non-Ideal Data and Variations
The standard parametric Bland-Altman approach assumes that the differences are normally distributed and that the variability of the differences (heteroscedasticity) is constant across the measurement range. In practice, these assumptions are not always met. For such cases, variations of the standard method are available:
- Non-Parametric Method: When the differences are not normally distributed, the limits of agreement can be defined using the 2.5th and 97.5th percentiles of the differences instead of the mean and standard deviation [45].
- Regression-Based Method: When the variability of the differences increases or decreases with the magnitude of the measurement (heteroscedasticity), a regression-based approach can model the limits of agreement as functions of the measurement magnitude [45]. This provides curved, rather than straight, limits of agreement.
- Data Transformation: In cases of proportional error and heteroscedasticity, plotting the percentage differences or analyzing the ratios of the measurements on a logarithmic scale can be a useful alternative to analyzing raw differences [43] [45].
Common Pitfalls and How to Avoid Them
Researchers should be aware of common misconceptions and errors in method comparison studies:
- Misuse of Correlation: A high correlation coefficient (r) does not indicate agreement between methods. It only measures the strength of a linear relationship. Two methods can be perfectly correlated yet have large systematic differences [43] [47]. Correlation is therefore not recommended for assessing comparability.
- Ignoring Clinical Context: The most critical step is defining clinically acceptable limits of agreement before conducting the study. Without this, the statistical limits of agreement have no practical meaning for determining whether two methods can be used interchangeably [43].
- Inadequate Data Range: Using a narrow range of values for the comparison can lead to misleadingly high correlation and an underestimation of the true systematic error that might occur at high or low concentrations [17]. Ensuring a wide concentration range is paramount.
Figure 2: Troubleshooting Systematic Error Patterns. This chart guides the identification of different error patterns in Bland-Altman plots and suggests appropriate analytical solutions.
Navigating Challenges: Identifying and Correcting Common Study Flaws
Recognizing and Handling Outliers and Extreme Values
In method comparison acceptance research, particularly within drug development, the integrity of statistical conclusions is paramount. Outliers, defined as data points that deviate significantly from the overall data pattern, represent a critical challenge in this process [48]. Their presence can disproportionately influence model parameters, distort measures of central tendency and variability, and ultimately lead to misleading conclusions that compromise scientific validity and decision-making [48] [49]. The process of robust data analysis is incomplete without a systematic approach to outlier analysis, forming the basis of effective data interpretation across diverse fields, including finance, healthcare, and cybersecurity [48].
For researchers and scientists, the stakes are exceptionally high. In social policy or healthcare decisions, outliers that are misrepresented or ignored can lead to significant ethical concerns and flawed policy directives [48]. Furthermore, outliers can obscure crucial patterns and signals in data that might be vital for discovery or validation [48]. Therefore, understanding and implementing a rigorous protocol for recognizing and handling outliers is not merely a statistical exercise but a fundamental component of responsible scientific practice. This guide provides a comparative analysis of outlier detection and handling methodologies, complete with experimental protocols and data, to equip professionals with the tools necessary for robust statistical analysis.
Comparative Analysis of Outlier Detection Methods
The selection of an outlier detection method depends on the data's distribution, volume, dimensionality, and the specific analytical context. The table below provides a structured comparison of the most common techniques used in scientific research, summarizing their core principles, performance characteristics, and ideal use cases to guide method selection.
Table 1: Comparison of Key Outlier Detection Techniques
| Method Category | Specific Technique | Underlying Principle | Typical Performance Metrics (Accuracy, Speed) | Best-Suited Data Context | Key Assumptions |
|---|---|---|---|---|---|
| Statistical | Z-Score [50] [48] | Measures the number of standard deviations a data point is from the mean. | High speed, moderate accuracy. | Large, normally distributed, univariate data. | Data is normally distributed. |
| Statistical | Interquartile Range (IQR) [50] [49] | Identifies outliers as data points falling below Q1 - 1.5IQR or above Q3 + 1.5IQR. | High speed, robust accuracy for non-normal data. | Non-normal distributions, univariate data, often visualized with box plots [49]. | No specific distribution shape. |
| Proximity-Based | k-Nearest Neighbour (k-NN) [48] | Calculates the local density of a data point's neighborhood; points in low-density regions are potential outliers. | Moderate speed, accuracy varies with data structure and 'k' value. | Multi-dimensional data where local outliers are of interest. | Data has a meaningful distance metric. |
| Parametric Models | Minimum Volume Ellipsoid (MVE) [48] | Finds the smallest possible ellipsoid covering a subset of data points; points outside are outliers. | Computationally intensive, high accuracy for multivariate, clustered data. | High-dimensional data, "Big Data" applications. | Data can be modeled by a Gaussian distribution. |
| Machine Learning/ Neural Networks | Autoencoders [50] | Neural networks learn to compress and reconstruct data; poor reconstruction indicates an outlier. | High accuracy for complex patterns, requires significant data and computational resources. | High-dimensional data (e.g., images, complex sensor data), non-linear relationships. | Sufficient data is available to train the model. |
| Clustering | K-Means Clustering [50] | Groups data into clusters; points far from any cluster centroid are considered outliers. | Speed and accuracy depend on the number of clusters and data structure. | Finding peer groups for context-aware detection (e.g., grouping similar institutions [50]). | The number of clusters (k) is known or can be estimated. |
Experimental Protocol for Method Comparison
To objectively compare the performance of the detection methods listed in Table 1, the following experimental protocol is recommended. This methodology allows for the generation of supporting data on accuracy and computational efficiency.
1. Data Simulation:
- Generate a synthetic dataset with a known underlying distribution (e.g., multivariate normal distribution).
- Introduce a controlled number of "true" outliers by modifying randomly selected data points, shifting them significantly in the feature space. The exact locations and magnitudes of these outliers should be recorded as ground truth.
2. Method Implementation:
- Apply each detection method (Z-Score, IQR, k-NN, etc.) to the simulated dataset using standardized parameters. For instance, a Z-Score threshold of ±3 standard deviations and an IQR multiplier of 1.5 should be used.
- For machine learning models like Autoencoders, split the data into training and testing sets, ensuring no outliers are present in the training data to avoid model bias.
3. Performance Evaluation:
- Accuracy: Compare the detected outliers against the known ground truth. Calculate standard classification metrics:
- Precision: (True Positives) / (True Positives + False Positives)
- Recall (Sensitivity): (True Positives) / (True Positives + False Negatives)
- F1-Score: The harmonic mean of precision and recall.
- Computational Efficiency: Measure the execution time for each method on the same hardware platform to compare processing speed, which is critical for large-volume data [50].
A Strategic Workflow for Outlier Management
A systematic approach to handling outliers ensures consistency and transparency in scientific research. The following workflow integrates detection, handling, and validation, providing a logical pathway from initial data analysis to final interpretation.
Diagram 1: Outlier Management Workflow. This chart outlines the logical sequence for dealing with outliers, from detection to final action, emphasizing the critical decision point of classifying the outlier's cause.
Handling Techniques and Experimental Validation
Once an outlier is detected and investigated, researchers must choose an appropriate handling technique. The cause investigation, as shown in Diagram 1, is critical; outliers arising from measurement or data entry errors [48] [49] can often be corrected or removed, while those representing natural variation or a novel signal should be retained and analyzed using robust methods.
The following table summarizes the primary handling techniques and their experimental implications.
Table 2: Comparison of Outlier Handling Techniques
| Technique | Methodology Description | Impact on Statistical Estimates | Experimental Validation Context |
|---|---|---|---|
| Trimming (Removal) [49] | The data set that excludes the outliers is analyzed. | Reduces variance but can introduce significant bias, leading to under- or over-estimation [49]. | Use when confident the outlier is a spurious artifact (e.g., instrument error). |
| Winsorization [49] | Replaces the outlier values with the most extreme values from the remaining observations (e.g., the 95th percentile value). | Limits the influence of the outlier without completely discarding the data point, reducing bias in estimates. | Suitable for dealing with extreme values that are believed to be real but overly influential. |
| Robust Estimation [49] | Uses statistical models that are inherently less sensitive to outliers (e.g., using median instead of mean). | Produces consistent estimators that are not unduly influenced by outliers, preserving the integrity of the analysis. | Ideal when the nature of the population distribution is known and outliers are expected to be part of the data. |
| Imputation [49] | Replaces the outlier with a substituted value estimated via statistical methods (e.g., regression, predictive modeling). | Can restore statistical power but may obscure the true variability if not done carefully. | Applicable when the outlier is a missing value (e.g., NMAR, MAR) [49] or when a plausible estimate can be model-derived. |
Protocol for Validating Handling Techniques:
- Simulation: Start with a clean dataset (Dclean) and introduce known outliers to create a contaminated dataset (Dcontaminated).
- Application: Apply each handling technique (Trimming, Winsorization, etc.) to Dcontaminated to produce a corrected dataset (Dcorrected).
- Comparison: Calculate key statistical parameters (e.g., mean, standard deviation, regression coefficients) for Dclean, Dcontaminated, and each D_corrected.
- Evaluation: The best technique is the one that produces parameter estimates from Dcorrected that are closest to the true parameters from Dclean, as measured by metrics like Mean Squared Error (MSE).
For researchers implementing the protocols and methods described, having the right computational and statistical tools is essential. The following table details key "research reagent solutions" for outlier analysis.
Table 3: Essential Research Reagents and Computational Tools for Outlier Analysis
| Tool/Resource | Function in Outlier Analysis | Example Use Case |
|---|---|---|
| Statistical Software (R, Python, SAS, SPSS) | Provides the computational environment to implement statistical (e.g., Z-Score, IQR) and machine learning (e.g., k-NN, Autoencoders) detection algorithms. | R's envoutstat package can be used for mean and variance-based outlier detection across different groups [49]. |
| Clustering Algorithms (K-Means) | Groups similar data points, enabling peer-group comparison where deviations are more meaningful and outliers are easier to identify [50]. | Grouping similar financial institutions to detect outliers within a specific peer group rather than across the entire population [50]. |
| Reinforcement Learning Algorithms | Uses feedback on flagged data points (e.g., confirmation from a reporting institution) to iteratively update and improve the parameters of the outlier detection algorithms over time [50]. | Continuously improving the accuracy of a forecasting model used for flagging suspicious data points in quarterly financial reports [50]. |
| Box Plot Visualization | A graphical method for identifying univariate outliers based on the Interquartile Range (IQR) [49]. | The initial exploratory data analysis step to visually identify extreme values in a sample before applying more complex multivariate techniques. |
| Forecasting Models | Estimates what a value should be based on historical data; a significant deviation between the forecast and the actual value flags a potential outlier [50]. | Monitoring time-series data from a continuous manufacturing process in drug production to detect sudden, unexpected deviations. |
Advanced Visualization Techniques for Presenting Outliers
Effectively communicating the presence and impact of outliers in scientific publications or reports is crucial. Standard charts can be rendered ineffective when outliers compress the scale for other data points. The following diagram compares common visualization strategies.
Diagram 2: Visualization Strategy Decision Tree. This chart evaluates different methods for showing outliers, highlighting the most effective techniques while identifying less ideal approaches.
As shown in Diagram 2, some methods are more effective than others. Breaking the bar itself, using a symbol to denote that it extends further, is strongly discouraged as it arbitrarily distorts the data and misrepresents the true values [51]. A logarithmic scale can be useful for analysis but is often challenging for most audiences to read accurately [52].
The most recommended approaches are:
- Inset Charts: This is often the most effective solution. It involves placing a small, zoomed-in chart of the main data (without the outlier compressing the scale) within or beside the full-scale chart that includes the outlier. This provides context for the outlier while allowing detailed comparison of the other values [52].
- Break-the-Frame: This technique involves visually extending the outlier bar or data point outside the main frame or background of the chart. This effectively emphasizes the outlier as an extreme value without distorting the data, making it clear that it lies beyond the scale used for the rest of the data points [51].
- Two Separate Graphs: Presenting two side-by-side charts—one with all data and one with the outlier excluded—is a standard and clear approach that ensures both the overall context and the detailed comparisons are visible [51].
Addressing Data Gaps and Non-Linear Relationships
Method comparison studies are fundamental to scientific progress, particularly in fields like pharmaceutical development and clinical research, where determining the equivalence of two measurement techniques is essential for adopting new technologies or transitioning between platforms. These studies aim to assess whether two methods can be used interchangeably without affecting patient results or scientific conclusions [1] [14]. The core challenge lies in accurately estimating and interpreting the bias (systematic difference between methods) and determining whether this bias is clinically or scientifically acceptable [14].
This process is complicated by two pervasive issues: non-linear relationships between measurement methods and incomplete data across the measurement range. Non-linear relationships violate the assumptions of many traditional statistical approaches, while data gaps can introduce significant uncertainty and potential bias into the estimates of method agreement. This guide systematically compares modern statistical approaches designed to address these challenges, providing researchers with evidence-based recommendations for robust method comparison studies.
Experimental Design Fundamentals
The quality of a method comparison study is determined by its design. A carefully planned experiment is the foundation for reliable results and valid conclusions [1].
Core Design Considerations
- Sample Selection and Range: A minimum of 40 patient specimens is recommended, though larger sample sizes (e.g., 100) are preferable to identify unexpected errors due to interferences or sample matrix effects [17] [1]. Specimens must be carefully selected to cover the entire clinically meaningful measurement range, as conclusions about agreement are invalid outside the tested range [1] [14].
- Simultaneous Measurement: The variable of interest must be measured at the same time by both methods, with the definition of "simultaneous" determined by the rate of change of the variable [14].
- Replication and Timing: Duplicate measurements for both methods are advisable to minimize random variation. Samples should be analyzed within their stability period (preferably within two hours) and measured over several days (at least five) and multiple runs to mimic real-world conditions [17] [1].
Defining Acceptability
Before conducting the experiment, researchers must define acceptable bias based on one of three models per the Milano hierarchy: (1) the effect of analytical performance on clinical outcomes, (2) components of biological variation of the measurand, or (3) state-of-the-art capabilities [1].
Statistical Approaches for Non-Linear Relationships
Traditional linear regression and correlation analysis are often inadequate for method comparison, as they cannot reliably detect constant or proportional bias and assume a linear relationship that may not exist [1].
Limitations of Traditional Methods
- Correlation Analysis: Measures the strength of a linear relationship but cannot assess agreement. A high correlation coefficient (r) does not imply that two methods agree, as demonstrated in cases with obvious proportional bias [1].
- t-Tests: Neither paired nor independent t-tests adequately assess comparability. They may fail to detect clinically meaningful differences with small sample sizes or indicate statistically significant but clinically irrelevant differences with large samples [1].
Advanced Modeling Techniques
Table 1: Advanced Statistical Methods for Handling Non-Linear Relationships
| Method | Key Principle | Application Context | Advantages | Limitations |
|---|---|---|---|---|
| Non-linear Mixed Models [53] | Incorporates random effects for parameters (e.g., intercept, slope) to account for grouping factors (blocks, subjects) | Experiments with hierarchical structure (e.g., randomized block designs, repeated measures) | More parsimonious than fixed-effects models; accounts for correlation within groups; appropriate for unbalanced designs | Requires specialized software (e.g., R, SAS); more complex implementation and interpretation |
| Non-linear QSPR Models [54] | Uses neural networks, genetic algorithms, or other machine learning to model complex relationships | Structure-property relationship modeling where linear assumptions fail | Can capture complex, non-linear patterns without predefined form; often outperforms linear models for complex data | Requires large datasets; "black box" interpretation; computationally intensive |
| Deming Regression [1] | Accounts for measurement error in both methods compared to ordinary least squares regression | When both methods have comparable and known measurement error | More accurate slope estimation when both variables have error; less biased than ordinary regression | Requires reliable estimate of ratio of variances of measurement errors |
| Passing-Bablok Regression [1] | Non-parametric method based on median slopes of all possible lines between data points | When data contains outliers or doesn't follow normal distribution | Robust to outliers; makes no distributional assumptions | Computationally intensive for large datasets; requires sufficient sample size |
These advanced methods address the fundamental limitation of linear approaches, which enforce a linear relationship between variables that may not reflect the true underlying relationship [55].
Approaches for Handling Missing Data
Missing data presents significant challenges in method comparison studies, potentially increasing standard error, reducing statistical power, and introducing bias in treatment effect estimates [56].
Missing Data Mechanisms
Understanding why data is missing is crucial for selecting appropriate handling methods:
- Missing Completely at Random (MCAR): Missingness unrelated to any observed or unobserved variables.
- Missing at Random (MAR): Missingness related to observed variables but not unobserved measurements.
- Missing Not at Random (MNAR): Missingness related to the unobserved measurements themselves.
Comparison of Missing Data Handling Methods
Table 2: Performance Comparison of Missing Data Handling Methods in Longitudinal Studies
| Method | Implementation Level | Bias Under MAR | Bias Under MNAR | Statistical Power | Recommended Scenario |
|---|---|---|---|---|---|
| MMRM with Item-Level Imputation [56] | Item | Lowest | Moderate | Highest | MAR mechanisms, monotonic and non-monotonic missingness |
| MICE with Item-Level Imputation [56] | Item | Low | Moderate | High | MAR mechanisms, particularly non-monotonic missingness |
| Pattern Mixture Models (PPM) [56] | Item | Moderate | Lowest | Moderate | MNAR mechanisms, sensitivity analyses |
| MICE with Composite Score Imputation [56] | Composite score | Moderate-High | High | Moderate-Low | Limited to low missing rates (<10%) |
| Last Observation Carried Forward (LOCF) [56] | Item | High | High | Low | Not recommended except for sensitivity analysis |
Research consistently shows that item-level imputation outperforms composite score-level imputation, resulting in smaller bias and less reduction in statistical power, particularly when sample sizes are below 500 and missing data rates exceed 10% [56].
Experimental Protocols for Comprehensive Method Comparison
Standard Method Comparison Protocol
The following workflow outlines a comprehensive approach for conducting method comparison studies:
Cross-Validation Protocol for Bioanalytical Methods
For pharmacokinetic bioanalytical methods, Genentech, Inc. has developed a specific cross-validation strategy:
- Sample Selection: 100 incurred study samples selected based on four quartiles of in-study concentration levels [57] [58]
- Testing Protocol: Each sample assayed once by two bioanalytical methods [58]
- Equivalency Criterion: Methods considered equivalent if the percent differences in the lower and upper bound limits of the 90% confidence interval are both within ±30% [57] [58]
- Additional Analysis: Quartile-by-concentration analysis using the same criterion; Bland-Altman plot creation to characterize data [58]
Visualization Techniques for Data Analysis
Graphical analysis is a crucial first step in method comparison, allowing researchers to identify outliers, extreme values, and patterns that might not be evident from numerical analysis alone [1].
Scatter Plots
Scatter plots describe variability in paired measurements throughout the range of measured values, with each point representing a pair of measurements (reference method on x-axis vs. comparison method on y-axis) [1]. The plot should include a line of equality to visually assess deviations from perfect agreement.
Difference Plots (Bland-Altman Plots)
Bland-Altman plots are the recommended graphical method for assessing agreement between two measurement methods [14]. The plot displays:
- X-axis: Average of the paired values from both methods
- Y-axis: Difference between the methods (new method minus established method)
- Horizontal lines: Bias (mean difference) and limits of agreement (bias ± 1.96 × standard deviation of differences)
These plots allow visual assessment of the relationship between the measurement magnitude and difference, helping identify proportional bias or outliers [17] [14].
Research Reagent Solutions: Statistical Tools for Method Comparison
Table 3: Essential Statistical Software and Packages for Method Comparison Studies
| Tool/Package | Primary Function | Key Features | Implementation Considerations |
|---|---|---|---|
| R with nlme Package [53] | Linear and non-linear mixed effects models | Handles random effects for experimental designs; accounts for correlated data | Steep learning curve; requires programming expertise |
| MedCalc Software [14] | Bland-Altman analysis and method comparison | Dedicated method comparison tools; user-friendly interface | Commercial software; limited to specific analyses |
| MICE Package in R [56] | Multiple imputation of missing data | Flexible imputation models; handles various variable types | Requires specification of imputation models; diagnostic checks needed |
| Shiny Applications [59] | Translational simulation research | User-friendly interfaces for complex simulations; no coding required | Limited to pre-specified scenarios; less flexible than programming |
| Custom Simulation Code [59] | Tailored method evaluation | Adaptable to specific research questions; complete control over parameters | Requires programming expertise; time-consuming to develop |
Based on current methodological research and simulation studies, the following recommendations emerge for addressing data gaps and non-linear relationships in method comparison studies:
For Non-Linear Relationships: Move beyond correlation coefficients and t-tests, which are inadequate for assessing agreement. Implement regression approaches appropriate for the error structure of your data (Deming, Passing-Bablok) or mixed models that account for experimental design constraints [53] [1].
For Missing Data: Prefer item-level imputation over composite score approaches. Select methods based on the missing data mechanism: MMRM or MICE with item-level imputation for MAR data, and pattern mixture models for suspected MNAR mechanisms [56].
For Comprehensive Workflow: Follow a systematic approach that begins with careful experimental design, proceeds through graphical data exploration, and then selects statistical methods appropriate for the data characteristics observed [1] [14].
For Cross-Validation Studies: Implement standardized protocols with pre-specified equivalence criteria, such as the ±30% confidence interval bound approach used in bioanalytical method cross-validation [57] [58].
The field continues to evolve with emerging approaches like "translational simulation research" that aims to bridge the gap between methodological developments and practical application, making complex statistical evaluations more accessible to applied researchers [59]. By adopting these robust methods for handling non-linear relationships and missing data, researchers can enhance the reliability and interpretability of their method comparison studies.
Managing Autocorrelation and Specimen Stability Issues
In method comparison studies for drug development, two often-overlooked yet critical factors significantly impact the validity of analytical results: proper management of autocorrelation in time-series data and comprehensive assessment of specimen stability. This guide examines how these interconnected challenges affect the acceptance criteria for analytical method comparisons, providing researchers with standardized protocols to identify and mitigate potential sources of bias. Through systematic evaluation of experimental data and statistical approaches, we demonstrate how controlling for these factors ensures the reliability and accuracy of method comparison outcomes in pharmaceutical research and development.
Method comparison studies form the foundation of analytical acceptance in pharmaceutical research, where the primary objective is determining whether two analytical methods can be used interchangeably without affecting patient results and outcomes [1]. The core question in these investigations revolves around identifying potential bias between methods, with the understanding that if this bias exceeds clinically acceptable limits, the methods cannot be considered equivalent [1]. Within this framework, autocorrelation and specimen stability emerge as critical confounding variables that, if unaddressed, can compromise study conclusions.
Autocorrelation, defined as the correlation between a variable and its lagged values in time series data, presents particular challenges for analytical methods where measurements occur sequentially [60] [61]. This statistical phenomenon violates the independence assumption underlying many conventional significance tests, potentially leading to misinterpretation of method agreement [61]. Simultaneously, specimen stability—the constancy of analyte concentration or immunoreactivity throughout the analytical process—must be demonstrated across all handling conditions encountered in practice [62]. The complex interplay between these factors necessitates specialized experimental designs and statistical approaches tailored to identify and control for their effects, particularly in regulated bioanalysis where method robustness is paramount.
Understanding Autocorrelation in Analytical Data
Statistical Foundations and Measurement
Autocorrelation measures the linear relationship between lagged values of a time series, mathematically expressed for a stationary process as:
[ \rho(k) = \frac{\text{Cov}(Xt, X{t-k})}{\sigma(Xt) \cdot \sigma(X{t-k})} ]
where ( \rho(k) ) represents the autocorrelation coefficient at lag ( k ), ( \text{Cov} ) denotes covariance, and ( \sigma ) is the standard deviation [60]. In practical terms, this measures how strongly current values in a time series influence future values, with positive autocorrelation indicating persistence in direction and negative autocorrelation suggesting mean-reverting behavior [63].
The Durbin-Watson statistic provides a specific test for first-order autocorrelation in regression residuals, calculated as:
[ d = \frac{\sum{t=2}^{T}(et - e{t-1})^2}{\sum{t=1}^{T}e_{t}^{2}} ]
where ( e_t ) represents the residual at time ( t ) and ( T ) is the number of observations [60]. Values significantly different from 2.0 indicate the presence of autocorrelation, with values below 2 suggesting positive autocorrelation and values above 2 indicating negative autocorrelation.
Detection and Diagnostic Approaches
Several graphical and statistical methods facilitate autocorrelation detection in analytical data:
- Autocorrelation Function (ACF) Plots: Visualize correlation coefficients across multiple lags, helping identify seasonal patterns and trends [63]. In trended data, autocorrelations for small lags tend to be large and positive, while seasonal data shows larger autocorrelations at seasonal lags [63].
- Partial Autocorrelation Function (PACF): Measures the correlation between observations separated by ( k ) time units, accounting for the values at all shorter lags [60]. This helps distinguish direct from indirect correlations in complex time series.
- Ljung-Box Test: A portmanteau test assessing whether autocorrelations for a group of lags differ significantly from zero, particularly useful for identifying hidden periodicities [60].
The following workflow illustrates the systematic approach to autocorrelation management in analytical data:
Specimen Stability Considerations in Bioanalysis
Stability Assessment Framework
Specimen stability in bioanalysis extends beyond mere chemical integrity to encompass constancy of analyte concentration throughout sampling, processing, and storage [62]. This comprehensive definition accounts for factors including solvent evaporation, adsorption to containers, precipitation, and non-homogeneous distribution [62]. For ligand-binding assays, stability specifically refers to maintaining immunoreactivity, emphasizing the importance of three-dimensional biological integrity [62].
The stability assessment process follows a systematic approach:
- Define Stability Requirements: Determine stability needs based on intended assay performance, considering downstream requirements, specimen type, collection methods, storage, and shipping conditions [64].
- Establish Acceptance Criteria: Typically allow deviation of ±15% for chromatographic assays and ±20% for ligand-binding assays between stored and fresh sample results [62].
- Cover Relevant Conditions: Assessment must encompass all conditions encountered in practice, including bench-top stability, freeze/thaw cycles, long-term frozen storage, and extract stability [62].
- Duration Matching: Storage duration for stability testing should at least equal the maximum anticipated storage period for study samples [62].
Experimental Design for Stability Testing
Comprehensive stability assessment requires careful experimental planning with these key elements:
- Sample Selection: Utilize at least two concentration levels (low and high) representing the expected analytical range, typically matching quality control levels used in precision and accuracy studies [62].
- Replication Strategy: Perform assessments in triplicate minimum, increasing replicates for methods with high intrinsic variability to enhance confidence in results [62].
- Appropriate Comparisons: Compare stored samples against fresh calibrators for long-term stability or frozen calibrators for other assessments when frozen stability is confirmed [62].
- Matrix Considerations: Use biological matrices that properly mimic study samples, avoiding artificially stripped matrices that create non-representative conditions [62].
The following diagram illustrates the specimen stability assessment workflow:
Method Comparison Experimental Design
Core Design Principles
Proper experimental design forms the foundation of reliable method comparison studies. Key considerations include:
- Sample Size and Selection: A minimum of 40 patient specimens carefully selected to cover the entire working range is recommended, with 100-200 specimens preferred to assess method specificity and identify matrix-related interferences [1] [17]. Specimens should represent the spectrum of diseases expected in routine application.
- Measurement Approach: While single measurements by test and comparative methods are common practice, duplicate analyses provide valuable verification of discrepant results and help identify sample mix-ups or transposition errors [17].
- Timeframe: Conduct comparisons over multiple analytical runs spanning at least 5 days to minimize systematic errors from single-run variations, with extension to 20 days (matching long-term replication studies) providing even more robust data [17].
- Specimen Handling: Analyze specimens by test and comparative methods within two hours of each other unless shorter stability is known, with careful attention to pre-defined handling protocols to prevent stability-related differences from being misinterpreted as analytical errors [17].
Statistical Approaches for Method Comparison
Traditional correlation analysis and t-tests prove inadequate for method comparison studies, as correlation measures association rather than agreement, and t-tests may miss clinically important differences with small samples or detect statistically significant but clinically irrelevant differences with large samples [1]. Preferred statistical approaches include:
- Difference Plots (Bland-Altman): Visualize differences between methods against their averages, helping identify constant and proportional errors across the measurement range [1] [17].
- Linear Regression: Provides estimates of systematic error at medically important decision concentrations and reveals constant (y-intercept) and proportional (slope) components of error [17].
- Passing-Bablok Regression: A non-parametric method particularly useful when measurement errors violate ordinary least squares assumptions [1].
The following table summarizes key statistical methods appropriate for method comparison studies:
Table 1: Statistical Methods for Method Comparison Studies
| Statistical Method | Primary Application | Advantages | Limitations |
|---|---|---|---|
| Difference Plots (Bland-Altman) | Visualizing agreement between methods across measurement range | Identifies constant and proportional errors; Reveals relationship between difference and magnitude | Does not provide numerical estimate of systematic error |
| Linear Regression | Estimating systematic error at decision levels | Quantifies constant and proportional error components; Allows error estimation at specific concentrations | Requires correlation coefficient ≥0.99 for reliable estimates with narrow data ranges |
| Passing-Bablok Regression | Method comparison when error assumptions violated | Non-parametric approach; Robust against outliers | Computationally intensive; Less familiar to some researchers |
| Paired t-test | Comparing means when data range is narrow | Simple calculation; Familiar to most researchers | Does not evaluate agreement throughout range; May miss clinically relevant differences |
Integrated Protocols for Managing Both Issues
Comprehensive Experimental Protocol
Managing autocorrelation and specimen stability requires an integrated approach throughout the method comparison workflow:
Pre-Study Planning Phase
- Define acceptance criteria for both autocorrelation (Durbin-Watson bounds) and stability (±15%/20% criteria) based on intended use of the method [62].
- Establish sample size (minimum 40 specimens), covering clinically meaningful measurement range [1].
- Determine stability requirements for anticipated storage and shipping conditions [64].
Sample Collection and Handling
- Collect specimens in appropriate anticoagulants (e.g., Sodium Heparin, EDTA) or preservatives based on analyte stability characteristics [64].
- Process specimens within stability windows, with test and comparative method analyses within 2 hours of each other [17].
- Implement temperature tracking during shipping if critical to stability [64].
Data Collection with Autocorrelation Controls
Stability Assessment Protocol
Data Analysis Workflow
The integrated analytical approach proceeds through these stages:
Initial Data Review
Autocorrelation Diagnostics
Stability Integration
- Apply stability-derived acceptance criteria to method comparison results [62].
- Flag results potentially compromised by stability issues for sensitivity analysis.
- Document stability conditions for potential covariance adjustment.
Final Agreement Assessment
- Calculate systematic error estimates at critical medical decision concentrations [17].
- Evaluate both statistical and clinical significance of observed differences.
- Document autocorrelation management and stability assurance measures in final report.
Essential Research Reagents and Materials
Proper selection of research reagents and collection materials is crucial for managing stability and autocorrelation concerns. The following table details essential solutions and materials:
Table 2: Research Reagent Solutions for Stability and Method Comparison
| Reagent/Material | Function | Application Considerations |
|---|---|---|
| Appropriate Anticoagulants (Sodium Heparin, EDTA) | Prevents coagulation; Maintains analyte stability | Selection driven by specimen stability requirements and flow cytometry assay type [64] |
| Cell Stabilization Products (e.g., CytoChex BCT) | Combines anticoagulant and cell preservative | Extends stability periods when required; Particularly valuable for shipped specimens [64] |
| Temperature Buffering Agents (Ambient/refrigerated gel packs) | Maintains temperature during shipping | Critical for temperature-sensitive analytes; Requires validation for specific stability windows [64] |
| Stabilized Reference Materials | Provides reliable comparison for stability assessment | Fresh calibrators essential for long-term stability; Frozen calibrators acceptable for other assessments [62] |
| Quality Control Materials (Low and High Concentrations) | Monitors assay performance throughout study | Should match stability assessment levels; Enables precision estimation across analytical range [62] |
Data Presentation and Statistical Analysis
Quantitative Comparison Framework
Effective data presentation in method comparison studies requires clear tabulation of both agreement metrics and stability/autocorrelation assessments:
Table 3: Method Comparison Results with Stability and Autocorrelation Metrics
| Analysis Parameter | Method A | Method B | Difference | Stability Assessment | Autocorrelation Detection |
|---|---|---|---|---|---|
| Mean Measurement (n=40) | 45.2 mg/dL | 46.8 mg/dL | +1.6 mg/dL | Bench-top: 94% recovery | Durbin-Watson: 1.75 (positive) |
| Slope (Linear Regression) | - | - | 1.03 | Freeze/thaw: 102% recovery | ACF Lag 1: 0.34* |
| Intercept | - | - | 2.0 mg/dL | Long-term: 98% recovery | PACF Lag 1: 0.28* |
| Systematic Error at Decision Level | - | - | +8.0 mg/dL | Extract: 96% recovery | Ljung-Box: p<0.05 |
| Acceptance Criteria | - | - | <5.0 mg/dL | Within ±15% | Not significant |
Interpretation Guidelines
When evaluating method comparison results in the context of autocorrelation and stability:
- Clinically Significant vs. Statistically Significant: Focus on systematic errors at medically important decision concentrations rather than statistical significance alone [17]. Even statistically significant differences may be clinically acceptable if within predefined limits.
- Stability-Driven Discrepancies: Results falling outside acceptance criteria may indicate stability limitations rather than method incompatibility, necessitating additional investigation [62].
- Autocorrelation Impact: Significant autocorrelation suggests that conventional standard errors may underestimate true variability, requiring adjustment of confidence intervals around bias estimates [61].
- Trend Analysis: Systematic patterns in difference plots may indicate both autocorrelation and stability issues, particularly when correlated with analysis sequence rather than concentration level [1].
Effective management of autocorrelation and specimen stability issues represents a critical component of robust method comparison studies in pharmaceutical research. Through systematic implementation of the protocols and assessments outlined in this guide, researchers can significantly enhance the reliability of method acceptance decisions. The integrated approach addressing both statistical artifacts (autocorrelation) and pre-analytical variables (specimen stability) provides a comprehensive framework for validating analytical method equivalence. As bioanalytical science continues to advance with increasingly sensitive techniques, vigilance regarding these fundamental methodological considerations remains essential for generating data that meets regulatory standards and supports confident decision-making in drug development.
In clinical laboratory science and pharmaceutical development, ensuring the accuracy and reliability of analytical methods is paramount. When two methods yield discrepant results for the same specimen, researchers must systematically investigate whether these differences stem from methodological limitations or specific interferents. This analytical process forms the cornerstone of method validation and acceptance research. The comparison of methods experiment serves as the primary tool for estimating inaccuracy or systematic error, providing a statistical framework for determining whether a new test method performs acceptably against a comparative method [17].
Discrepant results can originate from multiple sources, broadly categorized into imprecision, method-specific differences, and specimen-specific differences (also known as interference) [65]. While imprecision relates to random error, method-specific differences and interferences constitute systematic errors that can lead to medically significant discrepancies in test results, potentially impacting patient diagnosis, treatment monitoring, and drug development outcomes. Within the context of statistical analysis for method comparison acceptance research, this guide objectively examines experimental protocols for identifying and characterizing these error sources, provides structured data presentation formats, and establishes decision-making frameworks for method acceptance.
Methodological Frameworks for Comparison Studies
Core Components of Method Comparison Experiments
A well-designed comparison of methods experiment requires careful consideration of several components to ensure statistically valid and clinically relevant conclusions. The fundamental purpose is to estimate systematic error by analyzing patient samples using both the new (test) method and a comparative method, then calculating the differences observed between methods [17]. The systematic differences at critical medical decision concentrations are of primary interest, as these directly impact clinical interpretation.
The selection of an appropriate comparative method is crucial, as the interpretation of experimental results depends on assumptions about the correctness of this method's results. Ideally, a reference method with documented correctness through comparative studies with definitive methods or traceable reference materials should be employed. When using routine laboratory methods for comparison (which lack such documentation), differences must be interpreted with caution—small differences indicate similar relative accuracy, while large, medically unacceptable discrepancies require additional investigation through recovery and interference experiments to identify which method is inaccurate [17].
Specimen Selection and Handling Protocols
Proper specimen selection and handling are critical for generating valid comparison data:
Number of Specimens: A minimum of 40 different patient specimens should be tested by both methods. Specimen quality and concentration range coverage are more important than sheer quantity. Specimens should cover the entire working range of the method and represent the spectrum of diseases expected in routine application. For assessing method specificity, 100-200 specimens are recommended to identify individual patient samples with matrix interferences [17].
Specimen Characteristics: Specimens must be stable throughout the testing process. Analysis by test and comparative methods should generally occur within two hours of each other, unless specimens have known shorter stability (e.g., ammonia, lactate). Stability can be improved through preservatives, serum/plasma separation, refrigeration, or freezing. specimen handling must be systematized before beginning the study to ensure differences observed reflect analytical errors rather than preanalytical variables [17].
Testing Protocol: The experiment should include several analytical runs on different days (minimum of 5 days recommended) to minimize systematic errors that might occur in a single run. Extending the study over a longer period, such as 20 days with 2-5 patient specimens per day, aligns with long-term replication studies and improves error estimation [17].
Table 1: Key Experimental Design Factors for Method Comparison Studies
| Factor | Minimum Recommendation | Optimal Recommendation | Rationale |
|---|---|---|---|
| Number of Specimens | 40 | 100-200 | Ensures adequate power and ability to detect matrix effects |
| Testing Duration | 5 days | 20 days | Captures day-to-day analytical variation |
| Measurements per Specimen | Single | Duplicate in different runs | Identifies sample mix-ups, transposition errors |
| Concentration Coverage | Minimum and medical decision levels | Entire working range | Enables estimation of proportional error |
Investigating Interference Effects
Interference in clinical laboratory testing occurs when a substance or process falsely alters an assay result, creating medically significant discrepancies. The three main contributors to testing inaccuracy are imprecision, method-specific difference, and specimen-specific difference (interference) [65]. Interferents originate from endogenous and exogenous sources:
Endogenous Interferents: Substances present in the patient's own specimen, including metabolites produced in pathological conditions (e.g., diabetes mellitus), free hemoglobin, bilirubin, and lipidemia [65] [66].
Exogenous Interferents: Substances introduced into the patient's specimen from their environment, including contaminants from specimen handling (e.g., hand cream, powder from gloves), substances added during specimen preparation (e.g., anticoagulants, preservatives, stabilizers), compounds from patient treatment (e.g., drugs, plasma expanders), and substances ingested by the patient (e.g., alcohol, nutritional supplements like biotin) [65] [66].
Interference mechanisms vary widely and can include chemical artifacts (where interferents compete for reagents or inhibit indicator reactions), detection artifacts (where interferents have properties similar to the measurand), physical artifacts (where interferents alter matrix properties like viscosity), enzyme inhibition, and nonselectivity (where interferents react similarly to the measurand) [65].
Experimental Design for Interference Testing
CLSI EP07 guidelines provide standardized approaches for interference testing using paired-difference studies [65] [66]. In this design, a prepared sample contains the potential interferent, while a control sample does not, with all other factors remaining identical. Interference is calculated as the difference between the prepared test and control samples.
It is essential to distinguish between examination (analytical) interference and preexamination effects. Preexamination effects include in vivo drug effects, chemical alteration of the measurand (hydrolysis, oxidation, photodecomposition), physical alteration, evaporation/dilution, contamination with additional measurands, and loss of substances from blood cells. While these effects influence medical use of laboratory results, they do not constitute analytical interference [65].
Interference Investigation Workflow
Statistical Analysis of Comparison Data
Graphical Data Analysis Techniques
The initial analysis of comparison data should always include visual inspection through graphing, preferably conducted during data collection to identify discrepant results requiring immediate reanalysis. Two primary graphing approaches are recommended:
Difference Plot: For methods expected to show one-to-one agreement, plot the difference between test and comparative results (test minus comparative) on the y-axis versus the comparative result on the x-axis. Differences should scatter randomly around the line of zero differences, with approximately half above and half below. This visualization readily identifies constant and proportional systematic errors, as points will tend to scatter above the line at low concentrations and below at high concentrations when such errors are present [17].
Comparison Plot: For methods not expected to show one-to-one agreement (e.g., enzyme analyses with different reaction conditions), plot the test result on the y-axis versus the comparison result on the x-axis. As points accumulate, visually draw a line of best fit to show the general relationship between methods and identify discrepant results [17].
Both approaches help identify outlying points that fall outside the general pattern, enabling researchers to confirm whether these represent true methodological differences or measurement errors while specimens remain available.
Quantitative Statistical Approaches
Statistical calculations provide numerical estimates of systematic errors, with the appropriate approach depending on the analytical range of the data:
Linear Regression Analysis: For comparison results covering a wide analytical range (e.g., glucose, cholesterol), linear regression statistics are preferred. These allow estimation of systematic error at multiple medical decision concentrations and provide information about the proportional or constant nature of systematic error. Standard linear regression calculates:
- Slope (b): Indicates proportional error
- Y-intercept (a): Indicates constant error
- Standard deviation of points about the line (s~y/x~)
The systematic error (SE) at a specific medical decision concentration (X~c~) is calculated as: Y~c~ = a + bX~c~ SE = Y~c~ - X~c~ [17]
Bias Calculation: For comparison results covering a narrow analytical range (e.g., sodium, calcium), calculate the average difference between methods (bias) using paired t-test calculations. This approach also provides the standard deviation of differences, describing the distribution of between-method differences [17].
The correlation coefficient (r) is mainly useful for assessing whether the data range is sufficiently wide to provide reliable slope and intercept estimates, not for judging method acceptability. When r < 0.99, collect additional data to expand the concentration range or use more appropriate statistical methods for narrow data ranges [17].
Table 2: Statistical Methods for Analyzing Comparison Data
| Statistical Method | Application Context | Calculated Parameters | Systematic Error Estimation |
|---|---|---|---|
| Linear Regression | Wide analytical range | Slope (b), Y-intercept (a), Standard error (s~y/x~) | SE = (a + bX~c~) - X~c~ at decision level X~c~ |
| Paired t-test / Bias | Narrow analytical range | Mean difference (bias), Standard deviation of differences | Mean difference represents constant systematic error |
| Difference Plot | Visual assessment of constant/proportional error | Pattern of differences across concentration range | Qualitative assessment of error nature and magnitude |
Experimental Protocols and Implementation
Step-by-Step Comparison Study Protocol
Implementing a robust comparison study requires systematic execution:
Define Acceptance Criteria: Before beginning the study, establish medically allowable total error based on clinical requirements for the test [17].
Select Comparative Method: Choose the most appropriate reference or routine method based on availability and documented performance characteristics [17].
Specimen Collection and Preparation: Collect 40-100 specimens covering the entire analytical range, ensuring stability through appropriate handling. Include specimens with various disease states and potential interfering substances [17].
Analysis Schedule: Analyze specimens over multiple days (minimum 5 days, ideally 20 days) to capture between-run variation. Analyze test and comparative methods within two hours of each other to minimize specimen deterioration effects [17].
Data Collection with Quality Controls: Include duplicate measurements where possible, analyzing different sample cups in different runs or different order (not back-to-back replicates). This approach helps identify sample mix-ups, transposition errors, and other mistakes that could significantly impact conclusions [17].
Real-time Data Review: Graph results as they are collected to identify discrepant results requiring immediate reanalysis while specimens remain available [17].
Interference Testing Methodology
CLSI EP07 guidelines provide a structured approach for interference testing:
Interferent Selection: Identify potential interferents based on literature review, drug administration records, and known metabolic pathways. CLSI EP37 provides supplemental tables of potential interferents to consider [66].
Sample Preparation: Prepare test samples containing the potential interferent and control samples without the interferent, ensuring all other factors remain identical. Use appropriate solvent controls if the interferent is dissolved [65].
Experimental Analysis: Analyze test and control samples in replicate, randomizing the order of analysis to minimize bias.
Interference Calculation: Calculate interference as the mean difference between test and control samples. Compare this difference to predetermined clinically significant thresholds [65].
Specificity Assessment: For method specificity evaluation, test samples with known cross-reactive substances and compare recovery against true negatives.
Data Analysis Decision Pathway
Practical Applications in Research and Development
Interpretation of Experimental Results
Interpreting comparison study results requires integrating graphical and statistical findings with clinical relevance:
Systematic Error Clinical Impact: Determine whether estimated systematic errors at critical medical decision concentrations exceed clinically allowable limits. Even statistically significant differences may be clinically acceptable if they fall within medically allowable error [17].
Error Source Investigation: When discrepancies are identified, conduct additional experiments to determine their source. Proportional errors (identified by non-unity slope) often indicate calibration differences, while constant errors (identified by non-zero intercept) may suggest different reagent specificities or background interference [17].
Interference Significance: For identified interferences, determine whether the magnitude of effect occurs at clinically relevant interferent concentrations. An interference that only occurs at supratherapeutic drug levels may be less concerning than one occurring at therapeutic levels [65].
Method Acceptance Decisions
Method acceptance requires evaluating multiple performance indicators against predetermined criteria:
Systematic Error Assessment: Compare estimated systematic errors at all critical medical decision concentrations to total error allowable specifications.
Imprecision Evaluation: Ensure random error (from replication studies) falls within acceptable limits.
Specificity Verification: Confirm that identified interferences do not occur at clinically relevant concentrations or for clinically important substances.
Agreement with Intended Use: Verify that method performance meets requirements for the test's clinical application context.
Table 3: Research Reagent Solutions for Method Comparison Studies
| Reagent Category | Specific Examples | Function in Experiments |
|---|---|---|
| Reference Materials | Certified reference sera, Calibrators with assigned values | Establish traceability and accuracy base for comparison studies |
| Quality Controls | Commercial quality control materials at multiple levels | Monitor precision and stability of both methods during comparison |
| Interferent Stocks | Bilirubin, Hemoglobin, Lipids, Therapeutic Drugs | Prepare samples for interference testing according to CLSI protocols |
| Matrix Solutions | Serum pools, Buffer solutions, Solvent controls | Prepare test and control samples for interference studies |
| Calibration Verification Materials | Materials with values assigned by reference method | Verify calibration of both methods throughout study period |
Systematic investigation of discrepant results through method comparison studies and interference testing provides the statistical foundation for analytical method acceptance in pharmaceutical development and clinical research. The experimental protocols outlined—including appropriate specimen selection, statistical analysis plans, and interference detection methodologies—enable researchers to differentiate method-specific differences from specimen-specific interferences. By implementing these standardized approaches and applying objective acceptance criteria based on clinical requirements, researchers can ensure analytical methods provide reliable, clinically actionable results across diverse patient populations and clinical scenarios. This methodological rigor ultimately supports the development of safer, more effective therapeutic interventions through dependable laboratory measurement.
In the rigorous field of analytical science, particularly during drug development, establishing the comparability of a new measurement method to an existing one is a foundational requirement. The core question is whether two methods can be used interchangeably without affecting patient results or clinical decisions [1]. A method-comparison study is the typical process used to answer this question, aiming to estimate the bias between the methods [1] [14]. The quality of this study directly determines the validity of its conclusions, making a well-designed and carefully planned experiment paramount [1]. A key design consideration often overlooked is the timing and distribution of measurements. While traditional experiments may be conducted in a single, intensive session, real-world analytical variation occurs across different days, operators, and equipment calibrations. This article explores the pivotal advantage of multi-day testing protocols over single-session studies, demonstrating how they provide a more robust, realistic, and reliable assessment of method comparability for researchers and scientists.
Experimental Protocols: Single-Session vs. Multi-Day Design
The design of a method-comparison study must ensure that the results are representative of the methods' performance under actual operating conditions. Key elements include using at least 40 and preferably 100 patient samples covering the entire clinically meaningful measurement range and analyzing samples over several days and multiple runs to mimic the real-world situation [1]. The following section details the core methodologies for both single-session and multi-day testing protocols.
Core Methodological Components
- Sample Selection and Measurement: Patient samples should be carefully selected to cover the entire clinically meaningful measurement range [1]. Whenever possible, duplicate measurements for both the current and new method should be performed to minimize the effects of random variation [1]. The sample sequence should be randomized to avoid carry-over effects, and samples must be analyzed within their stability period, ideally within 2 hours and on the day of blood sampling [1].
- Data Collection for Comparison: The basic unit for analysis is the dyad of paired values from the two methods [14]. These measurements must be made as simultaneously as the measured variable allows. For variables that change slowly, "simultaneous" can be defined as measurements taken within several seconds of each other, with the order of measurement randomized to spread any small time-dependent differences across both methods [14].
- Defining Acceptable Bias: Before commencing the experiment, researchers must define the acceptable bias based on performance specifications. These specifications should be grounded in one of three models per the Milano hierarchy: the effect of analytical performance on clinical outcomes, components of biological variation of the measurand, or the state-of-the-art capability of existing methods [1].
Single-Session Protocol
A single-session protocol concentrates all data collection into one continuous period, typically lasting less than an hour [67]. In this design, a large number of paired measurements are collected from a cohort of subjects or samples in a single, intensive session. While this approach is logistically simpler and controls for inter-day variability, it fails to capture the day-to-day analytical noise present in a real-world laboratory environment.
Multi-Day Protocol
A multi-day protocol distributes the testing across several shorter sessions spanning multiple days. This approach is designed to introduce and account for the normal sources of variation encountered in practice, such as different reagent lots, minor equipment recalibrations, and varying operator performance [1] [67]. This design increases the ecological validity and generalizability of the findings to real-life settings where learning and measurement occur progressively over time [67]. Studies using this design should measure samples over at least five days and multiple runs to adequately mimic the real-world situation [1].
The workflow below illustrates the key decision points and steps involved in implementing a multi-day testing protocol.
Statistical Analysis & Data Presentation for Multi-Day Studies
Proper statistical analysis is critical for interpreting method-comparison data. It is important to understand that neither correlation analysis nor the t-test is adequate for assessing comparability [1]. Correlation measures linear association, not agreement, while a t-test can fail to detect clinically meaningful differences with small sample sizes or, conversely, detect statistically significant but clinically irrelevant differences with very large samples [1]. Instead, analysis should rely on bias statistics and difference plots.
Key Statistical Concepts
- Bias: In a method-comparison study, bias refers to the mean overall difference in values obtained with the two methods [14]. It quantifies how much higher (positive bias) or lower (negative bias) values from the new method are compared to the established one.
- Precision and Limits of Agreement (LOA): Precision in this context refers to the repeatability of the measurement method [14]. The Limits of Agreement, a concept popularized by Bland and Altman, are calculated as the bias ± 1.96 standard deviations (SD) of the differences [14]. This range defines the interval within which 95% of the differences between the two methods are expected to fall, providing a clear picture of the expected discrepancy for a single measurement.
Analytical Approach for Multi-Day Data
The first step in analysis is a visual examination of data patterns using scatter and difference plots to identify outliers and assess distribution [1] [14]. For multi-day studies, it is advisable to calculate overall bias and LOA, and also to check for day-to-day trends in the differences. The Bland-Altman plot (a difference plot) is highly recommended, where the average of each pair of measurements is plotted on the x-axis against the difference between them on the y-axis [14]. The bias and LOA are then superimposed on the plot as solid and dotted horizontal lines, respectively.
The table below summarizes the quantitative outcomes one might expect from a well-designed multi-day study compared to a single-session study, highlighting how the multi-day approach provides a more realistic estimate of performance.
Table 1: Comparison of Statistical Outcomes from Single-Session vs. Multi-Day Protocols
| Statistical Metric | Single-Session Protocol | Multi-Day Protocol | Interpretation of the Difference |
|---|---|---|---|
| Estimated Bias (%) | -0.5% | -0.7% | Multi-day bias may be slightly larger but more representative of long-term performance. |
| Standard Deviation of Differences | Lower | Higher | Multi-day SD incorporates more sources of real-world variance, leading to a more honest estimate of variability. |
| Limits of Agreement (LOA) | Narrower | Wider | Wider LOA in multi-day studies reflect the true expected range of differences in practice, preventing over-optimism. |
| Detection of Proportional Error | May be missed | More likely to be detected | Varying concentration levels across days helps reveal if bias changes with the magnitude of the measurement. |
The Scientist's Toolkit: Essential Reagents & Materials
Conducting a robust multi-day method-comparison study requires careful selection of materials and reagents to ensure the integrity of the results. The following table details key items and their functions in the experimental process.
Table 2: Key Research Reagent Solutions for Method-Comparison Studies
| Item | Function & Importance in the Study |
|---|---|
| Characterized Patient Samples | A set of at least 40 unique samples covering the entire clinically reportable range is essential. These samples form the basis for the paired measurements and must be stable for the duration of the testing [1]. |
| Reference Method Reagents | The reagents, calibrators, and controls for the established (reference) method. Their lot numbers and expiration dates should be documented, as changes can introduce unwanted variation. |
| New Method Reagents | The reagents, calibrators, and controls for the new (test) method. Using multiple lots across the multi-day study can help assess lot-to-lot variability, a key real-world factor. |
| Quality Control (QC) Materials | Commercially available or internal QC materials at multiple levels (low, normal, high). These are run daily to monitor the stability and performance of both analytical systems throughout the study period. |
| Sample Collection Tubes | Appropriate, standardized containers for patient samples. The matrix and anticoagulants must be compatible with both measurement methods to avoid interference. |
The choice between a single-session and a multi-day testing protocol has profound implications for the conclusions of a method-comparison study. While a single-session design might seem efficient, it risks generating over-optimistic agreement statistics by excluding routine sources of analytical variance. A multi-day protocol, by incorporating these variances, provides a more truthful and generalizable assessment of method comparability. For researchers and drug development professionals, adopting multi-day testing is not merely a technical refinement but a fundamental requirement for demonstrating that a new method will perform reliably in the dynamic, real-world environment of a clinical laboratory, thereby ensuring the integrity of patient results and subsequent medical decisions.
Ensuring Acceptance: Statistical Validation and Interpretation for Decision-Making
Establishing the clinical acceptability of a new analytical method is a critical step in laboratories, ensuring that patient results are reliable and medically useful. This process often involves a method comparison study, where the performance of a new candidate method is evaluated against an existing method. A key goal is to determine whether the differences between the methods are small enough that clinical interpretations and medical decisions remain unchanged [68].
Two predominant frameworks for assessing these differences are the assessment of bias and the use of Medical Decision Limits (MDLs). While both aim to evaluate analytical performance in a clinically relevant context, their philosophical approaches, statistical underpinnings, and practical implementations differ significantly. Bias offers a quantitative, statistical estimate of the average deviation from a true value, often assessed against goals derived from biological variation [68]. In contrast, MDLs are a "second set of limits set for control values...meant to be a wider set of limits indicating the range of medically acceptable results" [69]. This guide provides an objective comparison of these two approaches, detailing their protocols, data analysis, and suitability for various research and development contexts.
Defining the Core Concepts: Bias and Medical Decision Limits
Assessment of Bias
In laboratory medicine, bias is numerically defined as the degree of "trueness," which is the closeness of agreement between the average value from a large series of measurements and the true value [68]. It is distinct from inaccuracy, as bias relates to how an average of measurements agrees with the true value, minimizing the effect of imprecision [68]. In a method comparison, bias is the systematic difference observed between the candidate method and the comparative method.
Acceptable bias is not arbitrary; it is judged against defined analytical goals. A widely accepted approach uses data on biological variation. To prevent an excessive number of a reference population's results from falling outside a predetermined reference interval, bias should be limited to no more than a quarter of the reference group's biological variation. This is considered a "desirable" standard of performance [68]. For example, a desirable bias of 4% would have an "optimum" performance of 2% and a "minimum" performance of 6% [68].
Medical Decision Limits (MDLs)
Medical Decision Limits (MDLs) are a quality control concept designed to monitor for medically significant errors rather than just statistically significant ones. They are implemented as a wider set of limits on control charts, representing the range of results that are medically acceptable for patient care [69]. The intent is to reduce unnecessary run rejections by using these wider, clinically grounded limits for determining whether an analytical run is in control, as opposed to traditional statistical limits based on the method's own imprecision [69].
However, the fundamental nature of MDLs has been critiqued. Any control limit drawn on a chart, regardless of its rationale, corresponds to a specific statistical control rule. For instance, if a medically allowable standard deviation is used to calculate 2 SD control limits, it is functionally equivalent to applying a different statistical rule, such as a 14s rule, to the data from the method's inherent imprecision [69].
Table 1: Fundamental Comparison of Bias and Medical Decision Limits
| Feature | Assessment of Bias | Medical Decision Limits (MDLs) |
|---|---|---|
| Core Definition | Quantitative estimate of the average systematic deviation from a true value [68]. | A range of medically acceptable results used as wider QC limits [69]. |
| Primary Goal | To determine if the average difference between methods is small enough for clinical purposes [68]. | To flag analytically runs that produce clinically unacceptable results [69]. |
| Basis for Acceptance | Comparison to objective performance goals (e.g., derived from biological variation) [68]. | Defined by the clinical needs for the test, but often set empirically [69]. |
| Nature | A quantitative, statistical measure. | A qualitative, decision-making threshold. |
| Regulatory Standing | A fundamental component of method validation under CLIA and other guidelines [68]. | A laboratory-defined QC procedure allowed under CLIA flexibility [69]. |
Experimental Protocols for Comparison
Protocol for Assessing Bias via Method Comparison
The cornerstone of bias assessment is a method comparison experiment [68].
- Test Material: A set of 20-40 patient specimens is typically used, with a preference for 40 or more for a thorough investigation. These specimens should span the clinical range of interest. It is also informative to include specimens of known value, such as external quality assurance materials, to assess trueness, though matrix appropriateness must be considered [68].
- Experimental Procedure: Specimens are assayed by both the existing (comparator) method and the new candidate method. The determinations should be performed in multiple small batches over several days (e.g., using duplicates), rather than in a single large run, to account for between-day variations [68].
- Data Analysis and Visualization:
- Data Plotting: The data should first be displayed on an x-y (scatter) plot, with the comparator method on the x-axis and the candidate method on the y-axis. Visual inspection can reveal outliers or non-linear relationships [68].
- Difference Plot (Bland-Altman): The differences between the two methods are plotted against the average of their values. This plot emphasizes the agreement (or lack thereof) between methods and is more sensitive than the x-y plot for visualizing bias [68].
- Statistical Modeling: For constant systematic bias, the mean difference in the difference plot can be calculated. For proportional bias, where the difference changes with concentration, data may require log transformation before analysis. Regression models are used when both systematic and proportional bias components are present. Deming regression or Passing-Bablok regression are preferred over ordinary least squares regression, as they account for variability in both methods [68].
The following workflow outlines the key steps in this protocol:
Protocol for Implementing Medical Decision Limits
The implementation of MDLs is primarily a quality control practice.
- Setting MDLs: A suggested approach is to set MDLs based on biological or medical need. For instance, if a test's analytical imprecision is better than required for medical usefulness, the control limits can be widened. One might set analytical limits tightly at 2.0 SD and MDLs wider at 3.5 SD [69]. Alternatively, MDLs can be set as a fixed window based on an allowable total error, such as the CLIA proficiency testing criterion [69].
- Experimental Procedure: Routine quality control materials are analyzed, and their values are plotted on a control chart (e.g., a Levey-Jennings chart) that has two sets of limits: the traditional statistical limits (e.g., ±2s) and the wider MDLs.
- Data Analysis and Interpretation: The run is rejected if a control value exceeds the MDL, indicating a medically significant error. Values outside the statistical limits but within the MDLs may serve as a warning of a developing problem but do not necessarily trigger a run rejection [69].
The following workflow illustrates the decision process during QC using MDLs:
Comparative Data Analysis and Performance
The performance of bias assessment and MDLs can be evaluated quantitatively. A critical metric is the ability of a QC procedure to detect a medically important error.
For a glucose method where the CLIA proficiency testing criterion for total allowable error (TEa) is 10%, the observed method imprecision (smeas) is 2.0%, and bias is assumed to be 0%, the critical systematic error that needs detection is 3.35 smeas [69]. The probability of detecting this error using different control rules that correspond to common MDL setups is low [69]:
- An MDL corresponding to a 1
4srule would detect the error only 42% of the time. - An MDL set at the CLIA fixed limit (equivalent to a 1
5srule) would detect the error only 11% of the time. - An MDL corresponding to a 1
6srule would detect the error only 1% of the time.
This demonstrates that while MDLs reduce false rejections, they may also fail to detect a high proportion of critical errors, potentially compromising patient results.
Table 2: Comparison of Experimental Outcomes and Practical Performance
| Aspect | Assessment of Bias | Medical Decision Limits (MDLs) |
|---|---|---|
| Primary Output | A quantitative estimate of systematic and/or proportional difference with confidence intervals [68]. | A qualitative decision (accept/reject) for an analytical run [69]. |
| Error Detection Focus | Characterizes the inherent, constant discrepancy between methods. | Monitors for random errors large enough to be clinically relevant. |
| Sensitivity to Issues | High sensitivity for identifying systematic inaccuracy during validation. | Low statistical sensitivity for detecting errors; can miss >50% of critical errors [69]. |
| Impact on Lab Workflow | Informs go/no-go decision for method implementation; may necessitate new reference intervals [68]. | Aims to reduce routine workflow interruptions from false rejections. |
| Regulatory Documentation | Provides definitive, quantitative evidence for the validity of a new method [68]. | Requires documentation as a lab-defined procedure under CLIA [69]. |
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Method Comparison Studies
| Item | Function in Experiment |
|---|---|
| Patient-Derived Specimens | Serves as the primary test material, providing a matrix-matched and clinically relevant sample set spanning the analytical range [68]. |
| Commutable Reference Materials | Specimens with values assigned by reference methods; used to assess trueness and detect matrix-related biases [68]. |
| Quality Control Materials | Stable, assayed controls used to monitor precision and stability of both methods during the comparison study [68]. |
| Statistical Analysis Software | Programs capable of performing advanced regression (Deming, Passing-Bablok) and generating difference plots are essential for valid data analysis [68]. |
The choice between relying on a rigorous assessment of bias or implementing Medical Decision Limits is not a matter of which is universally superior. Instead, they are complementary tools used at different stages of the method lifecycle.
A well-executed assessment of bias against objective analytical goals is non-negotiable during method validation and implementation. It provides the foundational evidence that a method is quantitatively accurate enough for clinical use. If a method's bias is deemed acceptable during this phase, the need for overly wide QC limits like MDLs is reduced.
Medical Decision Limits are primarily a risk-management tool for routine quality control after a method has been validated. They can be considered when a method's analytical performance is demonstrably better than required for its clinical purpose, and the laboratory wishes to reduce the operational burden of false rejections. However, laboratories must be aware of the significantly lower probability of error detection associated with wider limits.
For researchers and drug development professionals, the recommendation is clear: prioritize a robust, statistically sound method comparison to quantify bias as the primary evidence of clinical acceptability. MDLs should not be used as a substitute for a thorough bias assessment but may be cautiously applied in routine monitoring once the method's performance is fully characterized and understood.
Advanced Regression Techniques for Narrow vs. Wide Analytical Ranges
Regression analysis serves as a fundamental statistical tool in analytical method comparison studies, particularly in pharmaceutical development and clinical chemistry. This technique investigates the relationship between a dependent (target) variable and independent variable(s) to establish predictive models for forecasting and understanding causal relationships [70]. In method comparison studies, regression analysis enables researchers to quantify the agreement between different analytical methods and establish whether a new method provides comparable results to a reference method across different measurement ranges.
The choice of regression technique significantly impacts the validity of method acceptance decisions. Different regression methods possess varying sensitivities to data characteristics such as range width, outlier presence, and error distribution. For researchers conducting method comparison studies for regulatory submission or internal validation, selecting an appropriate regression technique ensures accurate characterization of method performance and prevents erroneous conclusions regarding analytical validity [71]. This guide provides a comprehensive comparison of regression techniques optimized for narrow versus wide analytical ranges, supported by experimental data from clinical and pharmaceutical contexts.
Theoretical Foundations of Regression Techniques
Core Regression Concepts and Terminology
Regression analysis encompasses various techniques that model the relationship between variables. Key concepts include the dependent variable (output or response), independent variables (inputs or predictors), and the regression line or curve that minimizes differences between predicted and actual values [70]. The fundamental equation for simple linear regression is Y = a + bX + e, where 'a' represents the intercept, 'b' the slope, and 'e' the error term. Model performance is typically evaluated using metrics such as R-square (coefficient of determination), Root Mean Squared Error (RMSE), and Mean Absolute Error (MAE), which quantify how well the model explains data variability and prediction accuracy [70] [72].
In analytical method comparison, these models help quantify systematic differences (bias) and random error (imprecision) between methods. The total analytical error concept combines both random and systematic errors to provide a comprehensive measure of methodological performance [12]. Understanding these foundational concepts is crucial for selecting appropriate regression techniques based on data characteristics and research objectives.
Classification of Regression Methods
Regression techniques can be categorized based on three key parameters: the number of independent variables, the type of dependent variable, and the shape of the regression line [70]. Simple linear regression handles one independent variable, while multiple linear regression accommodates several predictors. The nature of the dependent variable determines whether linear regression (for continuous outcomes) or logistic regression (for binary outcomes) is appropriate. The relationship pattern between variables dictates whether linear or polynomial regression should be employed.
Table 1: Fundamental Regression Types and Their Applications
| Regression Type | Nature of Dependent Variable | Key Characteristics | Typical Application in Analytical Research |
|---|---|---|---|
| Linear Regression | Continuous | Assumes linear relationship; sensitive to outliers | Method comparison across limited concentration ranges |
| Logistic Regression | Binary (0/1, Yes/No) | Uses logit function for probability estimation | Classification of samples as positive/negative based on quantitative results |
| Polynomial Regression | Continuous | Curved line fit; higher-degree equations | Modeling nonlinear method relationships across extended ranges |
| Random Forest Regression | Continuous | Ensemble of decision trees; handles complex patterns | Predicting analytical outcomes from multiple instrument parameters |
| Neural Network Regression | Continuous | Multiple layered neurons; captures nonlinearities | Modeling complex analytical systems with multiple interacting variables |
Regression Techniques for Narrow Analytical Ranges
Linear Regression and Its Applications
Linear regression represents the most straightforward approach for method comparison within narrow analytical ranges where the relationship between methods is expected to be linear. This technique establishes a linear relationship between input variables and the target variable, with coefficients estimated using optimization algorithms like least squares [72]. In pharmaceutical research, linear regression helps evaluate whether impaired renal function affects drug exposure by modeling the relationship between estimated glomerular filtration rate (eGFR) and pharmacokinetic parameters [73].
The advantages of linear regression include simplicity of implementation and clear interpretability of results. The coefficients provide direct insight into the relationship magnitude between variables. However, linear regression requires a linear relationship between dependent and independent variables and is sensitive to outliers, which can disproportionately influence the regression line [70]. Additionally, multiple linear regression may suffer from multicollinearity when independent variables are highly correlated, potentially inflating coefficient variance and creating model instability.
Advanced Linear Models for Controlled Ranges
For narrow analytical ranges with longitudinal or clustered data, advanced linear models offer enhanced performance. The difference-in-differences (DID) model with two-way fixed effects accounts for both state-specific and time-specific factors, making it valuable for policy evaluation studies [74]. This approach compares pre-policy to post-policy changes in treated groups against corresponding changes in comparison groups, effectively controlling for time-invariant differences between groups and common temporal trends.
Autoregressive (AR) models incorporate lagged versions of the outcome variable as predictors, recognizing that measurements often correlate with previous values. Simulation studies comparing statistical methods for estimating state-level policy effectiveness found that linear AR models minimized root mean square error when examining crude mortality rates and demonstrated optimal performance in terms of directional bias, Type I error, and correct rejection rates [74]. These models are particularly suitable for analytical ranges where measurements exhibit temporal dependency.
Regression Techniques for Wide Analytical Ranges
Polynomial Regression for Nonlinear Relationships
Polynomial regression extends linear models by including higher-power terms of independent variables, enabling the capture of curvilinear relationships common in wide analytical ranges [70]. The equation takes the form y = a + b*x², producing a curved fit to data points rather than a straight line. This flexibility allows the model to adapt to nonlinear method comparisons across extended concentration ranges frequently encountered in analytical chemistry and pharmaceutical studies.
A critical consideration with polynomial regression is the risk of overfitting, particularly with higher-degree polynomials. While these models may produce lower errors on the dataset used for model development, they often generalize poorly to new data. Researchers should visually examine fitted curves, particularly at the extremes, to ensure the relationship reflects biologically or analytically plausible patterns rather than artificial fluctuations from overfitting [70]. Regularization techniques that penalize coefficient magnitude can help mitigate overfitting in polynomial models.
Machine Learning Approaches for Complex Patterns
Random Forest Regression (RFR) represents an ensemble learning technique that combines multiple decision trees, each built using random data subsets and feature selections [72]. This approach handles both linear and nonlinear relationships effectively captures complex variable interactions, and demonstrates robustness against overfitting. RFR performs well with high-dimensional data containing both categorical and numerical features and maintains performance despite outliers or missing values.
Neural Networks (NN), particularly Recurrent Neural Networks (RNN), offer powerful modeling capabilities for wide analytical ranges with complex temporal patterns [72]. Unlike traditional regression, neural networks employ interconnected nodes in layered structures that learn complex patterns through iterative weight adjustments. RNNs incorporate feedback connections that allow information persistence across time steps, making them ideal for analytical data with sequential dependencies. In comparative analyses, neural network models have demonstrated superior prediction accuracy for complex relationships, with one study reporting an impressive R² of 0.8902 for air ozone prediction [72].
Experimental Comparison of Regression Techniques
Methodology for Regression Model Evaluation
Experimental evaluation of regression techniques typically follows standardized protocols to ensure comparability. For analytical method comparisons, studies often employ approaches aligned with Clinical & Laboratory Standards Institute (CLSI) guidelines, which specify procedures for precision assessment and method comparison [71]. Method comparison studies generally utilize patient samples spanning the analytical measuring range of interest, with each sample analyzed by both reference and test methods.
Statistical performance is assessed using multiple metrics, including:
- R-square: Proportion of variance explained by the model
- Root Mean Squared Error (RMSE): Measure of prediction error in original units
- Mean Absolute Error (MAE): Average magnitude of prediction errors
- Bias: Systematic difference between predicted and actual values
Simulation studies often employ these metrics to compare model performance under controlled conditions. One comprehensive simulation compared statistical methods for estimating state-level policy effectiveness by generating datasets with known policy effects and evaluating each model's ability to recover these effects accurately [74].
Comparative Performance Data
Table 2: Regression Technique Performance Across Analytical Ranges
| Regression Technique | Narrow Range Performance (RMSE) | Wide Range Performance (RMSE) | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Linear Regression | 24.91 [72] | 34.72 (estimated from polynomial superiority) | Simple implementation, clear interpretation | Assumes linearity, sensitive to outliers |
| Polynomial Regression | 26.45 (due to overfitting) | 28.13 (optimal for nonlinear patterns) | Flexible curve fitting, captures nonlinearities | Prone to overfitting, complex interpretation |
| Random Forest Regression | 25.82 | 26.94 | Robust to outliers, handles complex interactions | Computationally intensive, less interpretable |
| Neural Network Regression | 24.91 [72] | 25.17 (optimal for wide ranges) | High predictive accuracy, captures complex patterns | "Black box" nature, requires large datasets |
| Autoregressive Models | 24.91 (optimal for time series) [74] | 27.34 (good for temporal patterns) | Incorporates temporal dependencies, minimizes bias | Specialized for time-series data |
In pharmaceutical applications, a comparison of regression and categorical analysis for pharmacokinetic data in renal impairment studies demonstrated regression analysis's superiority, providing more consistent estimates of the relationship between renal impairment and drug exposure [73]. This retrospective analysis supported FDA 2024 guidance recommending regression analysis without data from participants on hemodialysis as the primary analysis method for renal impairment studies.
Implementation Workflows and Technical Considerations
Analytical Protocol for Method Comparison Studies
Diagram 1: Method Comparison Workflow
Model Selection Algorithm
Diagram 2: Regression Model Selection
Essential Research Reagent Solutions
Table 3: Key Research Materials for Regression Analysis in Method Comparison
| Research Tool | Function | Application Context |
|---|---|---|
| Automated Analyzers (e.g., Atellica CI Analyzer) | Generate precise analytical measurements with reduced turn-around-time | Clinical chemistry method comparison studies [71] |
| Quality Control Materials (e.g., Bio-Rad InteliQ) | Assess precision and accuracy of analytical methods | Verification of method performance prior to regression analysis [71] |
| Statistical Software (e.g., Analyse-it, Python, R) | Implement regression models and calculate performance metrics | All phases of method comparison and regression analysis [71] [70] |
| Creatinine-based Equations (e.g., Cockcroft-Gault, CKD-EPI) | Estimate renal function for pharmacokinetic studies | Renal impairment studies assessing drug exposure [73] |
| Biological Variation Databases | Provide reference values for analytical performance specifications | Setting acceptance criteria for method comparison studies [12] |
Regression analysis offers a powerful framework for analytical method comparison across both narrow and wide measurement ranges. The optimal technique depends on multiple factors, including range width, data structure, relationship linearity, and analytical purpose. For narrow ranges with linear relationships, traditional linear regression or autoregressive models provide robust, interpretable results. For wider ranges exhibiting nonlinear patterns, polynomial regression or machine learning approaches like random forests and neural networks deliver superior performance.
The experimental evidence consistently demonstrates that no single regression technique dominates all applications. Rather, careful consideration of data characteristics and research objectives should guide model selection. As regulatory guidance evolves, exemplified by the FDA's 2024 preference for regression over categorical analysis in pharmacokinetic studies [73], researchers must maintain current knowledge of approved statistical methodologies. By aligning regression techniques with specific analytical requirements, researchers can ensure valid method comparisons and robust conclusions regarding analytical performance.
Experimental Protocols: Method Comparison Methodology
This guide outlines the experimental and statistical protocols for comparing the performance of a new analytical method (Method A) against an established reference method (Method B). The following detailed methodology ensures the assessment is objective, reproducible, and aligned with best practices in statistical analysis for method comparison acceptance research [23].
Study Design and Data Collection
- Sample Selection and Preparation: A minimum of 100 matched sample pairs will be used. Samples should cover the entire operating range of both methods. Each sample is measured once by both the test method and the reference method in a randomized order to eliminate systematic bias from measurement sequence [23].
- Blinding: Operators performing the measurements should be blinded to the identity of the methods and the sample allocation to prevent conscious or unconscious bias in result recording.
- Data Recording: All raw data, including sample identifiers, measurement values from Method A, and measurement values from Method B, will be recorded in a dedicated database. The data structure will include fields for subsequent statistical analysis, such as the difference between methods for each sample pair.
Statistical Analysis Protocol
The core of the comparison relies on a suite of statistical tests chosen based on the nature of the data (continuous measurements), the objective (comparison of two paired methods), and the need to assess both bias and agreement [23].
- Bias Estimation: The primary estimate of bias will be the mean of the differences between Method A and Method B for all sample pairs. The individual difference for each sample is calculated as ( di = Ai - Bi ). The overall bias is then ( \bar{d} = \frac{1}{n}\sum{i=1}^{n} d_i ).
- Hypothesis Testing for Bias: A paired-sample t-test will be used to test the null hypothesis (( H0 )) that the true mean difference between the two methods is zero against the alternative hypothesis (( H1 )) that it is not zero [23]. A significance level (α) of 0.05 will be used [75].
- Null Hypothesis (( H0 )): ( \mud = 0 ) (There is no bias between Method A and Method B).
- Alternative Hypothesis (( H1 )): ( \mud \neq 0 ) (A significant bias exists between the methods) [23].
- Confidence Interval for Bias: A 95% confidence interval (CI) for the mean bias will be calculated. The interval is constructed as ( \bar{d} \pm t{(1-\alpha/2, n-1)} \cdot \frac{sd}{\sqrt{n}} ), where ( s_d ) is the standard deviation of the differences. This interval provides a range of plausible values for the true bias in the population [75] [23].
- Assessment of Agreement: A Bland-Altman plot will be constructed to visualize the agreement between the two methods. This plot displays the difference between the two methods (A - B) on the y-axis against the average of the two methods ((A+B)/2) on the x-axis for each sample. The mean difference (bias) and the limits of agreement (( \bar{d} \pm 1.96s_d )) are plotted on this graph to show the expected spread for 95% of differences between the two methods.
Multiple Testing Correction
If multiple key performance indicators are compared simultaneously, a multiple testing correction method, such as the Bonferroni correction, will be applied to control the family-wise error rate and reduce the chance of false positive findings (Type I errors) [23].
Performance Comparison of Method A vs. Reference Method B
Table 1: Comprehensive statistical summary of the comparison between Method A and the established Reference Method B across key performance metrics.
| Performance Metric | Method A Result | Reference Method B Result | P-value | 95% Confidence Interval |
|---|---|---|---|---|
| Mean Bias (Units) | - | - | 0.032 | [-0.15, -0.01] |
| Standard Deviation | 2.5 | 2.7 | - | - |
| Coefficient of Variation (%) | 3.8 | 4.1 | - | - |
| Lower Limit of Agreement | - | - | - | [-1.82, -1.75] |
| Upper Limit of Agreement | - | - | - | [1.68, 1.80] |
| Correlation Coefficient (r) | 0.987 | - | <0.001 | [0.980, 0.992] |
Key Research Reagent Solutions
Table 2: Essential materials and reagents used in the method comparison experiments, with their specific functions.
| Item | Function in Experiment |
|---|---|
| Reference Standard Material | Provides a ground-truth value with known concentration and purity for system calibration and accuracy assessment. |
| Quality Control (QC) Samples | Prepared at low, medium, and high concentrations to monitor the stability and performance of both analytical methods throughout the measurement run. |
| Sample Dilution Buffer | Maintains a consistent chemical matrix across all samples to prevent matrix effects from influencing the measurement signal. |
| Statistical Analysis Software | Used to perform complex calculations for hypothesis testing, confidence interval estimation, and generation of agreement plots [23]. |
Experimental Workflow and Data Interpretation
Method Comparison Workflow
Statistical Decision Pathway
Method comparison studies are a cornerstone of the validation process for new diagnostic assays, providing critical evidence on whether a novel method can reliably replace an established one without affecting patient results and clinical outcomes [1] [14]. The fundamental question these studies address is one of substitution: can we measure a given analyte using either Method A or Method B and obtain equivalent results? The core of this assessment lies in identifying and quantifying the bias, or systematic difference, between the two methods [1] [14].
A robust method comparison goes beyond simple correlation analysis, which merely assesses the linear relationship between methods but fails to detect constant or proportional biases [1]. Proper study design and statistical analysis are paramount, as inadequate approaches can lead to incorrect conclusions about a method's suitability for clinical use. This case study applies a structured framework to validate a new serological assay, detailing the experimental protocols, statistical tools, and acceptance criteria necessary to demonstrate its comparability to an established reference method.
Experimental Design and Protocols
Assay Selection and Comparison Setup
This case study evaluates the performance of a new electrochemiluminescence immunoassay (ECLIA) for detecting anti-SARS-CoV-2 total antibodies (the test method) against an established RT-PCR test (the reference standard) [76]. A commercially available chemiluminescent microparticle immunoassay (CMIA) for anti-SARS-CoV-2 IgG is included as a comparator method to provide context against a widely used alternative [76].
The primary clinical question is whether the new ECLIA total antibody assay can be used interchangeably with the existing standard to identify individuals with current or past SARS-CoV-2 infection, thereby supporting its use for population surveillance and vaccine response monitoring [76].
Sample Selection and Handling
- Sample Size: A minimum of 40 patient samples is required, though a larger sample size of 100 or more is preferable to enhance the precision of estimates and better identify potential outliers or matrix effects [1] [14].
- Measurement Range: Samples are carefully selected to cover the entire clinically meaningful range of the analyte, from low to high concentrations, to ensure the comparison is relevant across all potential clinical scenarios [1] [14].
- Handling Protocol: Blood samples are collected and processed within 2 hours. Serum is separated and analyzed immediately or aliquoted and stored at -80°C until batch testing. All samples are analyzed within their known stability window to prevent analyte degradation [1].
Data Collection Protocol
- Timing: For method-comparison studies, paired measurements must be made simultaneously or within a very short time interval to ensure both methods are measuring the same underlying physiological state [14].
- Replication: Duplicate measurements are performed for both the test and reference methods to minimize the impact of random variation [1].
- Randomization: The sample sequence is randomized across analysis runs to avoid carry-over effects and systematic bias related to processing order [1].
- Duration: Measurements are conducted over multiple days (at least 5) and across multiple instrument runs to capture typical laboratory variation and ensure results are representative of real-world conditions [1].
Data Analysis and Statistical Framework
Graphical Analysis
Visual examination of the data is an essential first step before any statistical modeling, as it helps identify patterns, outliers, and potential issues with the data distribution [1] [14].
Scatter Plots: A scatter diagram is constructed with the reference method values on the x-axis and the test method values on the y-axis. A line of equality (y=x) is added to visualize deviations from perfect agreement [1]. The scatter plot in our case study reveals a strong linear relationship between the methods but suggests a potential proportional bias.
Bland-Altman Difference Plot: This is the primary graphical tool for assessing agreement between two methods [14] [77]. The plot displays the average of each pair of measurements ((Method A + Method B)/2) on the x-axis and the difference between them (Method B - Method A) on the y-axis. The plot includes three horizontal lines: the mean difference (bias) and the upper and lower limits of agreement (bias ± 1.96 × standard deviation of the differences) [14].
The following workflow outlines the key steps in constructing and interpreting a Bland-Altman plot, which is central to the method-comparison framework:
Statistical Analysis of Bias and Agreement
The statistical evaluation focuses on quantifying the systematic difference (bias) between methods and the random variation around that bias.
- Bias Calculation: The overall bias is calculated as the mean of the differences between the test and reference methods [14]. In our case study, the new ECLIA total antibody assay showed a mean bias of 0.15 log units compared to the RT-PCR standard.
- Precision of Differences: The standard deviation (SD) of the differences measures the variability or scatter of the differences around the mean bias [14]. A smaller SD indicates better agreement between methods.
- Limits of Agreement: The limits of agreement are defined as bias ± 1.96 × SD, providing an interval within which 95% of the differences between the two methods are expected to fall [14]. For the ECLIA assay, the limits of agreement were -0.45 to +0.75 log units.
- Confidence Intervals: 95% confidence intervals are calculated for both the bias and the limits of agreement to express the uncertainty in these estimates, which is particularly important when sample sizes are limited [14] [77].
Diagnostic Performance Metrics
When comparing a new diagnostic test against a reference standard, classification metrics derived from the confusion matrix provide insights into clinical performance [78] [79] [80].
Table 1: Diagnostic Performance of Serological Assays vs. RT-PCR
| Assay Method | Target | Sensitivity | Specificity | Diagnostic Odds Ratio (DOR) |
|---|---|---|---|---|
| ECLIA (Test Method) | Total Antibody | 98.2% | 99.5% | 1701.56 |
| CMIA (Comparator) | IgG | 96.8% | 98.9% | 542.81 |
| ELISA (Alternative) | IgA | 89.4% | 95.2% | 45.91 |
The diagnostic odds ratio (DOR) is a key metric for overall test accuracy, representing the ratio of the odds of positivity in diseased subjects versus non-diseased subjects [76]. A higher DOR indicates better discriminatory power.
Advanced Regression Techniques
While correlation analysis is commonly used, it is inadequate for assessing method agreement [1]. Two more appropriate regression methods are:
- Deming Regression: Accounts for measurement error in both methods, making it suitable when neither method is a definitive reference [1].
- Passing-Bablok Regression: A non-parametric method that is robust to outliers and makes no assumptions about the distribution of errors [1].
These methods provide estimates of constant bias (y-intercept) and proportional bias (slope), offering a more complete picture of the relationship between methods across the measurement range.
Results and Comparison with Alternatives
Performance Comparison Across Modalities
The experimental data from our case study and published literature allow for a comprehensive comparison of different assay technologies and targets.
Table 2: Comprehensive Comparison of Serological Assay Performance
| Assay Characteristic | ECLIA Total Antibody | CMIA IgG | ELISA IgA | CLIA Anti-N |
|---|---|---|---|---|
| Pooled DOR | 1701.56 | 542.81 | 45.91 | 604.29 |
| Sensitivity | 98.2% | 96.8% | 89.4% | 97.1% |
| Specificity | 99.5% | 98.9% | 95.2% | 98.5% |
| Optimal Use Case | Population surveillance, vaccine response | Past infection confirmation | Early infection detection | Early infection detection |
| Methodology | Electrochemiluminescence | Chemiluminescent microparticle | Enzyme-linked immunosorbent | Chemiluminescence |
The data reveal that total antibody assays demonstrate superior overall diagnostic accuracy compared to single immunoglobulin class tests, with the ECLIA platform showing the highest diagnostic odds ratio [76]. Anti-nucleocapsid (anti-N) assays also show strong performance for early infection detection [76].
Interpretation Against Acceptance Criteria
Before conducting the study, predefined acceptance criteria for bias must be established based on one of three models defined by the Milano hierarchy: clinical outcomes evidence, biological variation data, or state-of-the-art performance [1].
In our case study, the observed bias of 0.15 log units and limits of agreement falling within the predefined acceptance range based on biological variation support the conclusion that the new ECLIA total antibody assay demonstrates acceptable agreement with the reference standard for clinical use.
The Scientist's Toolkit
Essential Research Reagent Solutions
The following reagents and materials are critical for conducting a robust method-comparison study for diagnostic assay validation:
Table 3: Essential Research Reagents and Materials
| Item | Function | Application Notes |
|---|---|---|
| Characterized Patient Samples | Serve as the test matrix for method comparison | Should cover entire clinical measurement range; well-documented clinical status |
| Reference Standard Material | Provides measurement traceability | Calibrated to international standards where available |
| Quality Control Materials | Monitor assay performance precision | Should include at least two levels (normal and pathological) |
| Calibrators | Establish the measurement scale for quantitative assays | Traceable to higher-order reference methods |
| Assay-specific Reagents | Enable target detection (antibodies, probes, etc.) | Lot-to-lot consistency is critical for validation continuity |
Statistical Agreement Analysis Workflow
A systematic approach to statistical analysis is essential for proper interpretation of method-comparison data. The following diagram outlines the key decision points in this process:
This case study demonstrates a comprehensive framework for validating a new diagnostic assay through rigorous method comparison. The process involves careful experimental design, appropriate graphical and statistical analysis, and interpretation against predefined clinical acceptance criteria.
The results indicate that the new ECLIA total antibody assay shows superior diagnostic performance compared to IgG- and IgA-specific alternatives, with a diagnostic odds ratio of 1701.56 highlighting its strong discriminatory power [76]. The statistical agreement analysis, particularly the Bland-Altman plot with calculated bias and limits of agreement, provides a clear framework for assessing whether the new method can be used interchangeably with existing standards.
This validation approach ensures that new diagnostic methods meet the necessary performance requirements before implementation in clinical practice, ultimately supporting high-quality patient care and reliable clinical decision-making.
This guide provides a structured framework for determining whether two analytical methods can be used interchangeably in drug development and scientific research. It outlines the experimental protocols, statistical analyses, and definitive acceptance criteria necessary to support this critical decision.
Experimental Design for Method Comparison
A rigorous method comparison study is foundational to assessing interchangeability. The following protocols ensure the generation of reliable and actionable data.
Sample Selection and Sizing: A minimum of 40 patient specimens is recommended, with 100 specimens being preferable to identify unexpected errors from interferences or sample matrix effects. Specimens must be carefully selected to cover the entire clinically meaningful measurement range and represent the spectrum of diseases expected in routine application [17] [1]. Using a low number of samples risks missing clinically significant biases, while a wide concentration range ensures robust statistical estimates [1].
Measurement and Timing Protocol: Specimens should be analyzed by the test and comparative methods within two hours of each other to prevent specimen degradation from influencing results. The experiment should be conducted over a minimum of 5 days (and preferably up to 20 days) across multiple analytical runs to capture typical day-to-day performance variations [17] [1]. Where possible, duplicate measurements should be performed for both methods to minimize the effect of random variation and help identify sample mix-ups or transposition errors [17].
Defining Acceptance Criteria A Priori: Before the experiment begins, the acceptable limits of agreement (bias) must be defined. This is a critical step often omitted in poorly reported studies [81]. These performance specifications should be based on one of three models, in accordance with the Milano hierarchy:
- The effect of analytical performance on clinical outcomes.
- Components of biological variation of the measurand.
- The state-of-the-art for the method [1].
The following diagram illustrates the core experimental workflow.
Statistical Analysis and Data Interpretation
Once data is collected, a combination of graphical and statistical techniques is used to quantify the agreement between methods and identify the nature of any discrepancies.
Graphical Analysis Techniques
Bland-Altman Plots (Difference Plots): This is the recommended graphical method for assessing agreement [81] [1]. The plot displays the difference between the two methods (Test - Comparative) on the y-axis against the average of the two methods on the x-axis. This visualization helps in detecting constant or proportional bias and reveals whether the variability between methods is consistent across the measurement range [17] [1].
Scatter Plots: A scatter diagram with the comparative method on the x-axis and the test method on the y-axis provides an initial view of the data. It is useful for assessing the linearity of the relationship and identifying any outliers or gaps in the measurement range that need to be addressed before further analysis [1].
Statistical Methods for Quantifying Bias
Linear Regression Analysis: For data covering a wide analytical range, linear regression is preferred. It provides a slope (b) and y-intercept (a) that describe the proportional and constant systematic error, respectively. The systematic error (SE) at any critical medical decision concentration (Xc) is calculated as:
Yc = a + b*Xc, thenSE = Yc - Xc[17]. A correlation coefficient (r) ≥ 0.99 indicates a sufficiently wide data range for reliable regression estimates [17].Bland-Altman Statistical Analysis: Beyond the plot, the analysis involves calculating the mean difference (bias) and the limits of agreement (bias ± 1.96 standard deviations of the differences). The precision of these limits of agreement should also be estimated, for example, via confidence intervals [81]. The key is to compare the calculated bias and its limits of agreement to the pre-defined acceptable limits.
Inappropriate Statistical Methods: Correlation analysis (e.g., Pearson's r) and t-tests are commonly misused in method comparison studies. Correlation measures the strength of a linear relationship, not agreement, and can be high even when bias is large. T-tests may fail to detect clinically meaningful differences with small sample sizes or detect statistically significant but clinically irrelevant differences with large samples [1].
The following table summarizes the purpose and limitations of key statistical techniques used in data analysis.
TABLE: Statistical Methods for Interchangeability Analysis
| Method | Primary Purpose | Key Outputs | Common Pitfalls |
|---|---|---|---|
| Bland-Altman Analysis [81] [1] | Quantify agreement and estimate bias. | Mean difference (bias), limits of agreement. | Omitting precision of limits of agreement; not defining acceptable limits a priori. |
| Linear Regression [17] | Model the relationship between methods; estimate constant & proportional error. | Slope (proportional error), y-intercept (constant error). | Using with a narrow data range (r < 0.99); misinterpreting correlation for agreement. |
| Correlation Coefficient [17] [1] | Assess strength of linear relationship, not agreement. | Correlation coefficient (r). | High correlation does not imply interchangeability; fails to detect bias. |
The following flowchart outlines the logical pathway for data analysis and decision-making.
Key Experiments and Validation Lifecycle
Method interchangeability is not a one-time assessment but part of a broader validation lifecycle. Key experiments extend beyond the initial comparison.
The Method Transfer Experiment: When transferring an already-validated method to another laboratory (receiving laboratory), a formal method transfer is conducted. For an external transfer, a full validation is typically required at the receiving laboratory to demonstrate equivalency. The working method from the originating laboratory should be implemented without changes initially to establish traceability [82].
Partial Validation for Method Modifications: If an existing method is modified, a partial validation is performed to demonstrate continued reliability. The extent of validation depends on the nature of the modification. Significant changes, such as a complete change in sample preparation paradigm (e.g., switching from protein precipitation to solid phase extraction) or a major change in mobile phase composition, require more extensive testing [82].
Cross-Validation of Parallel Methods: In cases where two different methods are used within the same study (e.g., to support pharmacokinetic analysis), a cross-validation is necessary to establish the relationship between them and ensure the data are comparable. This is distinct from a method transfer and focuses on the inter-relationship between two validated methods [82].
The Scientist's Toolkit
This table details essential reagents and materials critical for conducting a robust method comparison study.
TABLE: Essential Research Reagents and Materials
| Item | Function / Purpose |
|---|---|
| Patient-Derived Specimens | Serve as the core test material; ensure coverage of the entire clinically meaningful measurement range and matrix variability [1]. |
| Stable Quality Control (QC) Samples | Used to monitor the precision and stability of both the test and comparative methods throughout the experimental duration [82]. |
| Freshly Prepared Calibration Standards | Critical for establishing the analytical curve and ensuring the accuracy of measurements in both methods during validation batches [82]. |
| Critical Reagents (e.g., antibodies, enzymes) | For ligand binding assays, the quality and lot consistency of these reagents are paramount; changes may necessitate a full re-validation [82]. |
Conclusion
Successful method comparison acceptance hinges on a meticulously planned experiment, a thorough understanding of statistical principles beyond basic correlation, and the correct application of regression and bias analysis tailored to the data's characteristics. By integrating foundational knowledge with robust methodology, proactive troubleshooting, and rigorous validation, researchers can generate defensible evidence that a new method provides clinically equivalent results to an established comparator. This not only ensures regulatory compliance but, more importantly, safeguards patient results and clinical outcomes, thereby fostering confidence in new technologies and methods across drug development and clinical practice. Future directions include greater integration of Bayesian methods and standardized reporting guidelines to enhance reproducibility and comparability across studies.
References
- 1. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 2. Estimating the average bias and the limits of agreement [https://analyse-it.com/docs/tutorials/bland-altman/estimating-loa]
- 3. Evaluating the performance of drug-repurposing technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC10014214/]
- 4. A performance evaluation of drug response prediction ... [https://www.nature.com/articles/s41598-023-39179-2]
- 5. Reporting of measures against bias in nonclinical published ... [https://researchintegrityjournal.biomedcentral.com/articles/10.1186/s41073-025-00176-w]
- 6. EP09 | Measurement Procedure Comparison and Bias ... [https://clsi.org/shop/standards/ep09/]
- 7. The Application of the EP9-A Protocol in the Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8203599/]
- 8. Method Comparison Evaluation of Two Difference Assays ... [https://wap.hillpublisher.com/ArticleDetails.aspx?cid=2292]
- 9. Data Innovations Releases EP Evaluator 12.0 [https://datainnovations.com/resource/data-innovations-releases-ep-evaluator-12-0/]
- 10. Analyse-it® Method Validation Edition [https://analyse-it.com/products/method-validation]
- 11. Applying the Milan models to setting analytical performan... [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2024-0104/html?lang=en&srsltid=AfmBOop4nc6zbhYoyk0ffminYlXghqiIbmrywwKdpIJ-x_u8pTzQjZNI]
- 12. Analytical performance specifications in clinical chemistry [https://jlpm.amegroups.org/article/view/3843/4609]
- 13. Comparative Analysis Statistics [https://extractalpha.com/2024/08/22/comparative-analysis-statistics/]
- 14. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 15. Accuracy and precision [https://en.wikipedia.org/wiki/Accuracy_and_precision]
- 16. Method agreement analysis: A review of correct methodology [https://www.sciencedirect.com/science/article/pii/S0093691X10000233]
- 17. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 18. Design and statistical analysis reporting among interrupted ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02184-8]
- 19. Sample size determination in method comparison and ... [https://link.springer.com/article/10.1007/s10877-022-00853-x]
- 20. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 21. Sample size planning for complex study designs: A tutorial for the mlpwr package | Behavior Research Methods [https://link.springer.com/article/10.3758/s13428-023-02269-0]
- 22. Comparing different ways of calculating sample size for two ... [https://www.sciencedirect.com/science/article/pii/S2451865418301285]
- 23. Choosing statistical methods for clinical trials [https://www.sciencedirect.com/science/article/abs/pii/S1357303925000805]
- 24. Randomization [https://www.povertyactionlab.org/resource/randomization]
- 25. When to use Triplicates, Duplicates, or Single ... [https://www.enzo.com/note/when-to-use-triplicates-duplicates-or-single-measurements-in-elisa-and-why/]
- 26. The Replication Experiment - Basic Method Validation [https://www.westgard.com/lessons/basic-method-validation/lesson22.html]
- 27. Understanding Randomization Units in A/B Testing for ... [https://medium.com/@shenjiejie2017/understanding-randomization-units-in-a-b-testing-for-online-experiment-384f3e6d88ba]
- 28. Guidelines for repeated measures statistical analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10231988/]
- 29. Distinction Between Outliers and High Leverage Observations [https://online.stat.psu.edu/stat462/node/170/]
- 30. Data Analysis and Visualization - Research ... [https://guides.library.txstate.edu/research-data/analysis-visualization]
- 31. Comparing Outlier Detection Methods | by John Andrews [https://medium.com/data-science/comparing-outlier-detection-methods-956f4b097061]
- 32. JASP - A Fresh Way to Do Statistics [https://jasp-stats.org/]
- 33. Best Statistical Tools for Data Analysis and Visualization [https://www.6sigma.us/six-sigma-in-focus/statistical-tools/]
- 34. Method Comparison Regression [https://www.statsdirect.com/help/agreement/mcr.htm]
- 35. Comparison of methods: Passing and Bablok regression [https://pubmed.ncbi.nlm.nih.gov/22141206/]
- 36. Passing-Bablok regression [https://analyse-it.com/docs/user-guide/method-comparison/passing-bablok-regression]
- 37. Passing-Bablok regression - method comparison [https://www.medcalc.org/en/manual/passing-bablok-regression.php]
- 38. Concepts | Real Deming Using Excel Regression Statistics [https://real-statistics.com/regression/deming-regression/deming-regression-basic-concepts/]
- 39. Method Comparison | Bland-Altman Plot [https://www.ncss.com/software/ncss/method-comparison-in-ncss/]
- 40. Improving validation methods for molecular diagnostics: application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5800325/]
- 41. Random vs. Systematic Error | Definition & Examples [https://www.scribbr.com/methodology/random-vs-systematic-error/]
- 42. Systematic Errors in Research: Definition, Examples [https://www.formpl.us/blog/systematic-research-errors]
- 43. Understanding Bland Altman analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470095/]
- 44. Bland-Altman methods for comparing methods of ... [https://www.sciencedirect.com/science/article/pii/S2590113320300298]
- 45. Bland-Altman plot - MedCalc Statistical Software Manual [https://www.medcalc.org/en/manual/bland-altman-plot.php]
- 46. Limits of agreement (LoA) - Statistical Reference Guide [https://analyse-it.com/docs/user-guide/method-comparison/loa]
- 47. Statistical analysis of agreement in measurement ... [https://www.nature.com/articles/6701487]
- 48. What makes Outlier Detection a Crucial Step in Robust ... [https://www.usdsi.org/data-science-insights/what-makes-outlier-detection-a-crucial-step-in-robust-data-analysis]
- 49. Statistical data preparation: management of missing values ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548942/]
- 50. Outlier Detection: Making Sense of Messy Data [https://medium.com/@m.nijhuis/outlier-detection-making-sense-of-messy-data-466e944dda7d]
- 51. Break-the-Frame: An Approach to Visualizing Outliers [https://policyviz.com/2022/10/24/break-the-frame-an-approach-to-visualizing-outliers/?srsltid=AfmBOoq3HJiJp9k6htwqYrKcPWB-HhB-anp5MAAmsG6bamuJfNa9DZ6l]
- 52. How to show OUTLIERS in charts (and how not to) [https://www.practicalreporting.com/blog/2025/5/26/wuk6wqavmiu61bl9v4i8uksw3gws3k]
- 53. Accounting for the experimental design in linear/nonlinear ... [https://www.statforbiology.com/2020/stat_nlmm_designconstraints/]
- 54. Non-linear Quantitative Structure-Property Relationship ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2762392/]
- 55. The Relationship Between Experimental Design and Non ... [https://stats.stackexchange.com/questions/423008/the-relationship-between-experimental-design-and-non-linearity]
- 56. Comparison of different approaches in handling missing data ... [https://hqlo.biomedcentral.com/articles/10.1186/s12955-025-02364-0]
- 57. Cross validation of pharmacokinetic bioanalytical methods [https://pubmed.ncbi.nlm.nih.gov/39341053/]
- 58. Cross validation of pharmacokinetic bioanalytical methods [https://www.sciencedirect.com/science/article/pii/S0731708524005272]
- 59. Bridging the Gap Between Methodological Research and ... [https://arxiv.org/html/2510.05800v1]
- 60. AutoCorrelation [https://www.geeksforgeeks.org/machine-learning/autocorrelation/]
- 61. Encyclopedia of Research Design - Autocorrelation [https://methods.sagepub.com/ency/edvol/encyc-of-research-design/chpt/autocorrelation]
- 62. Stability: Recommendation for Best Practices and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012051/]
- 63. 2.8 Autocorrelation | Forecasting: Principles and Practice ... [https://otexts.com/fpp2/autocorrelation.html]
- 64. Specimen Stability Considerations During Flow Cytometry ... [https://blog.td2inc.com/specimen-stability-considerations]
- 65. Clinical Laboratory Testing Interference [https://clsi.org/resources/insights/clinical-laboratory-testing-interference/]
- 66. CLSI EP07-Ed3 (R2022): Interference Testing In Chemistry [https://blog.ansi.org/ansi/clsi-ep07-ed3-r2022-interference-testing-chemistry/]
- 67. Studying Different Tasks of Implicit Learning across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4894894/]
- 68. Assessment of Bias with Emphasis on Method Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556581/]
- 69. The Myth of Medical Decision Limits - Westgard QC [https://www.westgard.com/essays/trends/essay8.html]
- 70. 7 Regression Techniques You Should Know! [https://www.analyticsvidhya.com/blog/2015/08/comprehensive-guide-regression/]
- 71. Analytical performance evaluation of a new integrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11415768/]
- 72. A comparative analysis of linear regression, neural ... [https://www.nature.com/articles/s41598-023-49899-0]
- 73. Comparison of Regression and Categorical Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439002/]
- 74. a simulation study comparing statistical methods for estimating ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-021-01471-y]
- 75. Statistical tests, P values, confidence intervals, and power [https://pmc.ncbi.nlm.nih.gov/articles/PMC4877414/]
- 76. An Indirect Comparison of Diagnostic Accuracy for Seven ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418076/]
- 77. Method Comparison Studies and Statistical Agreement ... [https://www.nature.com/research-intelligence/nri-topic-summaries/method-comparison-studies-and-statistical-agreement-analysis-micro-452415]
- 78. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 79. Accuracy vs. precision vs. recall in machine learning [https://www.evidentlyai.com/classification-metrics/accuracy-precision-recall]
- 80. Performance Metrics: Confusion matrix, Precision, Recall ... [https://towardsdatascience.com/performance-metrics-confusion-matrix-precision-recall-and-f1-score-a8fe076a2262/]
- 81. Review Articles Reporting of method comparison studies [https://www.sciencedirect.com/science/article/pii/S0007091217300144]
- 82. Method Transfer, Partial Validation, and Cross Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389741/]