A Practical Framework for Systematic Error Estimation in Method Comparison Experiments
This article provides a comprehensive guide for researchers and drug development professionals on estimating and correcting systematic error (bias) in method comparison studies.
A Practical Framework for Systematic Error Estimation in Method Comparison Experiments
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on estimating and correcting systematic error (bias) in method comparison studies. It covers foundational concepts distinguishing systematic from random error, details methodological approaches for study design and statistical analysis using techniques like Bland-Altman plots and regression, offers strategies for troubleshooting and bias mitigation, and outlines validation protocols and comparative frameworks. The content is designed to equip scientists with practical knowledge to ensure measurement accuracy, enhance data reliability, and maintain regulatory compliance in biomedical research and clinical settings.
Understanding Systematic Error: Definitions, Sources, and Impact on Measurement Validity
Defining Systematic Error (Bias) and Distinguishing it from Random Error
Fundamental Definitions and Core Concepts
In scientific research, measurement error is the difference between an observed value and the true value of a quantity. These errors are broadly categorized into two distinct types: systematic error (bias) and random error. Understanding their fundamental differences is crucial for assessing the quality of experimental data [1].
Systematic error, often termed bias, is a consistent or proportional difference between the observed and true values of something [1]. It is a fixed deviation that is inherent in each and every measurement, causing measurements to consistently skew in one direction—either always higher or always lower than the true value [2]. This type of error cannot be eliminated by repeated measurements alone, as it affects all measurements in the same way [2]. For example, a miscalibrated scale that consistently registers weights as 1 kilogram heavier than they are produces a systematic error [3].
Random error, by contrast, is a chance difference between the observed and true values that varies in an unpredictable manner when a large number of measurements of the same quantity are made under essentially identical conditions [2] [1]. Unlike systematic error, random error affects measurements equally in both directions (too high and too low) relative to the correct value and arises from natural variability in the measurement process [3]. An example includes a researcher misreading a weighing scale and recording an incorrect measurement due to fluctuating environmental conditions [1].
The table below summarizes the key characteristics that distinguish these two types of error.
Table 1: Core Characteristics of Systematic and Random Error
| Characteristic | Systematic Error (Bias) | Random Error |
|---|---|---|
| Direction of Error | Consistent direction (always high or always low) [1] | Unpredictable direction (equally likely high or low) [3] |
| Impact on Results | Affects accuracy [1] | Affects precision [1] |
| Source | Problems with instrument calibration, measurement procedure, or external influences [4] | Unknown or unpredictable changes in the experiment, instrument, or environment [4] |
| Reduce via Repetition | No, it remains constant [2] | Yes, errors cancel out when averaged [1] |
| Quantification | Bias statistics in method comparison [5] | Standard deviation of measurements [3] |
The Impact on Measurement: Accuracy vs. Precision
The concepts of accuracy and precision are visually and functionally tied to the types of measurement error. Accuracy refers to how close a measurement is to the true value, while precision refers to how reproducible the same measurement is under equivalent circumstances, indicating how close repeated measurements are to each other [1].
Systematic error primarily affects accuracy. Because it shifts all measurements in a consistent direction, the average of repeated measurements will be biased away from the true value [3]. Random error, on the other hand, primarily affects precision. It introduces variability or "scatter" between different measurements of the same thing, meaning repeated observations will not cluster tightly [1]. The following diagram illustrates the relationship between these concepts.
Experimental Protocols for Estimating Systematic Error
The primary experimental design for estimating systematic error in analytical sciences and drug development is the method-comparison study. Its purpose is to determine if a new (test) method can be used interchangeably with an established (comparative) method without affecting patient results or clinical decisions [5] [6]. The core question is one of substitution: can one measure the same analyte with either method and obtain equivalent results? [5]
Key Design Considerations
A robust method-comparison study requires careful planning across several dimensions [7] [5] [6]:
- Selection of Comparative Method: An ideal comparative method is a reference method whose correctness is well-documented through definitive methods or traceable standards. This allows any observed differences to be attributed to the test method. In practice, many studies use a routine method already in clinical use, but large, medically unacceptable differences then require further investigation to identify which method is inaccurate [7].
- Sample Selection and Size: A minimum of 40 different patient specimens is recommended, though 100 or more is preferable to identify unexpected errors from interferences or sample matrix effects. The samples must cover the entire clinically meaningful measurement range, not just the analytical range. The quality of the experiment depends more on obtaining a wide range of values than simply a large number of results [7] [6].
- Timing and Replication: Specimens should be analyzed by both methods within a short time frame, ideally within two hours, to ensure specimen stability. The experiment should be conducted over multiple days (at least 5) and multiple analytical runs to capture real-world variability. While single measurements are common, performing duplicate measurements for both methods helps minimize the effects of random variation and identifies sample mix-ups or transposition errors [7] [6].
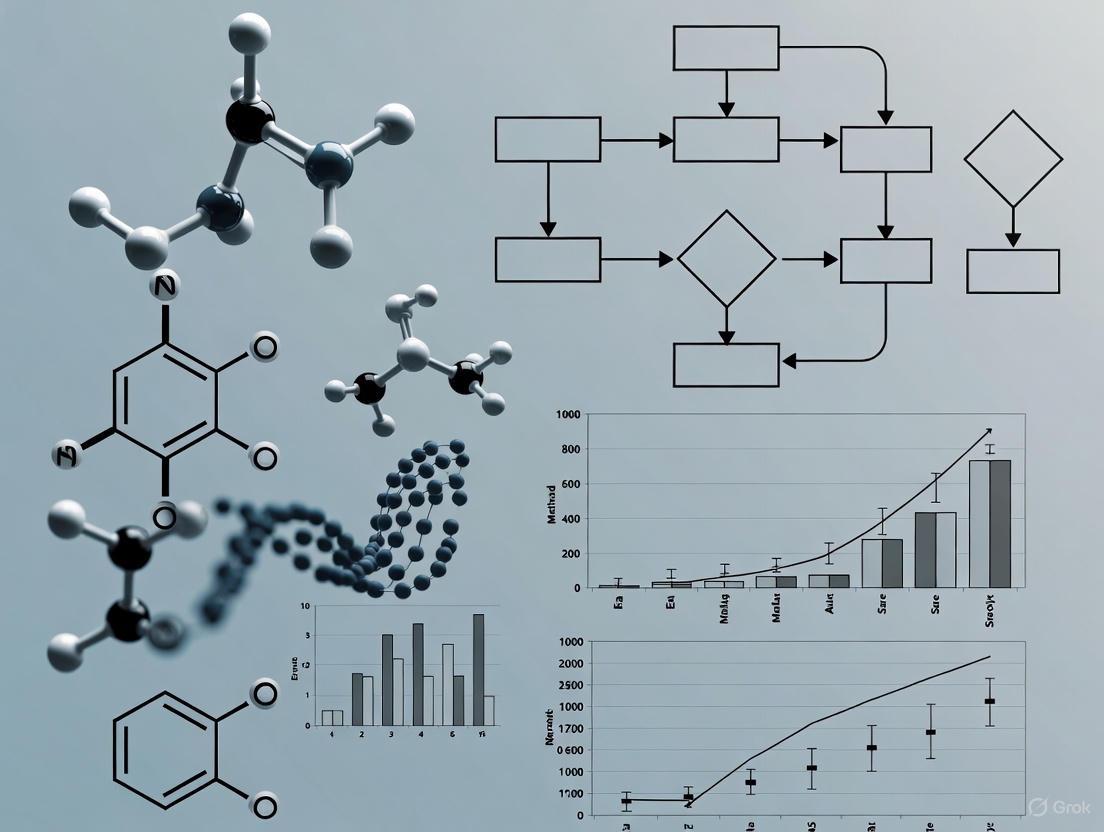
The workflow for a typical method-comparison experiment is outlined below.
Data Analysis and Visualization
The analysis of method-comparison data involves both graphical inspection and statistical quantification, moving beyond inadequate methods like correlation coefficients and t-tests, which cannot reliably assess agreement [6].
Graphical Inspection: The first and most fundamental step is to graph the data.
- Scatter Plots: A scatter diagram displays the test method results (y-axis) against the comparative method results (x-axis). This helps visualize the variability and linear relationship between methods across the measurement range [6].
- Difference Plots (Bland-Altman Plots): This is the recommended graphical method for assessing agreement. The plot displays the average of the two methods [(Test + Comparative)/2] on the x-axis and the difference between them (Test - Comparative) on the y-axis. This plot allows for visual inspection of the bias (the average difference) and how the differences vary across the measurement range [5].
Statistical Quantification:
- For a Wide Analytical Range: Use linear regression analysis (e.g., Deming or Passing-Bablok regression) to obtain the slope and y-intercept of the line of best fit. The systematic error (SE) at a critical medical decision concentration (Xc) is calculated as:
Yc = a + b*Xc, thenSE = Yc - Xc[7]. This helps identify proportional (slope) and constant (intercept) errors. - For a Narrow Analytical Range: Calculate the bias (mean difference) and the limits of agreement. The bias is the average of all individual differences (test method - comparative method). The limits of agreement are defined as
Bias ± 1.96 * Standard Deviation of the differences, representing the range within which 95% of the differences between the two methods are expected to lie [5].
- For a Wide Analytical Range: Use linear regression analysis (e.g., Deming or Passing-Bablok regression) to obtain the slope and y-intercept of the line of best fit. The systematic error (SE) at a critical medical decision concentration (Xc) is calculated as:
Table 2: Key Statistical Outputs in Method-Comparison Studies
| Statistical Metric | Description | Interpretation |
|---|---|---|
| Regression Slope (b) | The change in the test method per unit change in the comparative method [7]. | b = 1: No proportional error.b > 1: Positive proportional error.b < 1: Negative proportional error. |
| Regression Intercept (a) | The constant difference between the methods [7]. | a = 0: No constant error.a > 0: Positive constant error.a < 0: Negative constant error. |
| Bias (Mean Difference) | The overall average difference between the two methods [5]. | Quantifies how much higher (positive) or lower (negative) the test method is compared to the comparative method. |
| Limits of Agreement (LOA) | Bias ± 1.96 SD of differences [5]. | The range where 95% of differences between the two methods are expected to fall. Used to judge clinical acceptability. |
Table 3: Key Reagents and Materials for Method-Comparison Experiments
| Item | Function in the Experiment |
|---|---|
| Certified Reference Materials | Substances with one or more properties that are sufficiently homogeneous and well-established to be used for instrument calibration or method validation. Serves as an anchor for trueness [2]. |
| Patient-Derived Specimens | A panel of well-characterized clinical samples (serum, plasma, etc.) that cover the pathological and analytical range of interest. Essential for assessing performance with real-world matrix effects [7]. |
| Quality Control Materials | Stable materials with known assigned values, used to monitor the precision and stability of the measurement procedure during the comparison study over multiple days [7]. |
| Statistical Software Packages | Software (e.g., MedCalc, R, specialized CLSI tools) capable of performing Deming regression, Bland-Altman analysis, and calculating bias and limits of agreement, which are essential for proper data interpretation [5]. |
In research, systematic errors are generally considered a more significant problem than random errors [1] [3]. Random error introduces noise, but with a large sample size, the errors in different directions tend to cancel each other out when averaged, leaving an unbiased estimate of the true value [1]. Systematic error, however, introduces a consistent bias that is not reduced by repetition or larger sample sizes. It can therefore lead to false conclusions about the relationship between variables (Type I or II errors) and skew data in a way that compromises the validity of the entire study [1]. Consequently, the control of systematic error is a significant element in discussing a study's report and a key criterion for assessing its scientific value [8].
In the context of method comparison experiments, systematic error, often referred to as bias, represents a consistent, reproducible deviation of test results from the true value or from an established reference method's results [9]. Unlike random error, which scatters measurements unpredictably, systematic error skews all measurements in a specific direction, thus compromising the trueness of an analytical method [10]. The accurate estimation and management of these errors are foundational to method validation, ensuring that laboratory results are clinically reliable and that patient care decisions are based on sound data.
Systematic errors are particularly problematic in research and drug development because they can lead to false positive or false negative conclusions about the relationship between variables or the efficacy of a treatment [1]. In a method comparison experiment, the primary goal is to identify and quantify the systematic differences between a new (test) method and a comparative method. Any observed differences are critically interpreted based on the known quality of the comparative method; if a high-quality reference method is used, errors are attributed to the test method [7].
Systematic errors in laboratory and clinical measurements can originate from numerous aspects of the analytical process. Understanding their nature is the first step toward implementing effective detection and correction strategies.
Fundamental Classifications: Constant and Proportional Bias
Systematic errors manifest in two primary, quantifiable forms, which are often investigated during method comparison studies using linear regression analysis [9]:
- Constant Error (Offset Error): This is a consistent difference between the test and comparative methods that remains the same across the concentration range of the analyte. It is represented by the y-intercept (
a) in a linear regression equation (Y = a + bX). For example, a miscalibrated zero point on an instrument would introduce a constant error [1] [9]. - Proportional Error (Scale Factor Error): This error changes in proportion to the analyte's concentration. It is represented by the slope (
b) in the linear regression equation. A miscalibration in the scale factor of an instrument, such as a faulty calibration curve, is a typical cause [1] [9].
Table 1: Classification of Systematic Errors (Bias)
| Type of Bias | Description | Common Causes | Representation in Regression |
|---|---|---|---|
| Constant Bias | A fixed difference that is consistent across the measurement range. | Improper instrument zeroing, sample matrix effects, or specific interferents. | Y-Intercept (a) |
| Proportional Bias | A difference that increases or decreases proportionally with the analyte concentration. | Errors in calibration slope, incorrect reagent concentration, or instrument drift. | Slope (b) |
The following diagram illustrates how these biases affect measurement results in a method comparison context.
The sources of systematic error span the entire testing pathway, from specimen collection to data analysis.
- Specimen-Related Issues: The sample matrix itself can be a significant source of error. Sample matrix effects occur when components of the specimen interfere with the assay, leading to erroneous results that may not occur with control materials [10]. Improper sample handling, such as prolonged storage at room temperature for unstable analytes (e.g., ammonia), can also introduce bias [7].
- Calibration and Instrumentation: Uncalibrated or miscalibrated instruments are a classic source of both constant and proportional bias [1] [10]. A failure in the traceability chain, where the calibration of a routine method cannot be traced back to a higher-order reference method or material, guarantees a systematic error in patient results [10].
- Reagents and Assay Specificity: Deteriorated or improperly prepared reagents can lead to consistently biased results. Furthermore, an assay may lack perfect specificity, meaning it partially measures substances other than the intended analyte, such as metabolites or structurally similar drugs, leading to a positive bias [10].
- Environmental and Operator Factors: Experimenter drift is a phenomenon where an operator's technique slowly changes over time due to fatigue or loss of motivation, leading to a gradual introduction of bias [1]. Consistent misinterpretation of protocols or data entry errors by a specific individual are also forms of operator-induced systematic error.
Experimental Protocols for Detecting Systematic Error
A well-designed method comparison experiment is the cornerstone for detecting and quantifying systematic error. The following protocol outlines the key steps.
Protocol: The Comparison of Methods Experiment
Purpose: To estimate the inaccuracy or systematic error of a new test method by comparing it to a comparative method using real patient specimens [7].
Experimental Design:
- Selection of Comparative Method: Whenever possible, a reference method with documented correctness through traceability to definitive methods or reference materials should be used. If a routine method is used, differences must be interpreted with caution, as it may not be possible to determine which method is at fault [7].
- Specimen Selection and Number:
- A minimum of 40 different patient specimens is recommended, selected to cover the entire working range of the method [7].
- Specimens should represent the spectrum of diseases and conditions expected in routine practice. Twenty carefully selected specimens covering a wide range may provide better information than 100 random specimens [7].
- For highly specific assessments, 100-200 specimens may be needed to evaluate whether the new method's specificity matches the comparative method [7].
- Measurement Process:
- Specimens should be analyzed by both methods within a short time frame (e.g., two hours) to minimize changes in the specimen [7].
- The experiment should be conducted over a minimum of 5 different days to account for run-to-run variability and to detect long-term systematic errors. Integrating the comparison with a long-term replication study over 20 days is preferable [7].
- While single measurements are common, performing duplicate measurements on different samples or in different analytical orders helps identify sample mix-ups or transposition errors and confirms the validity of discrepant results [7].
Data Analysis:
- Graphical Inspection: The first step is to graph the data. A difference plot (Bland-Altman-type plot) showing the difference between methods (test minus comparative) versus the comparative method's result is ideal for visualizing one-to-one agreement. This helps identify outliers and patterns of constant or proportional error [7].
- Statistical Calculations:
- For data covering a wide analytical range, linear regression analysis (e.g., ordinary least squares) is used to calculate the slope (
b), y-intercept (a), and the standard error of the estimate (sy/x) [7] [9]. - The systematic error (SE) at a critical medical decision concentration (
Xc) is calculated as:Yc = a + b*Xc, thenSE = Yc - Xc[7]. - The correlation coefficient (r) is useful for assessing whether the data range is wide enough for reliable regression estimates; an
r < 0.99suggests the need for more data or alternative statistical approaches [7]. - For a narrow analytical range, calculating the average difference (bias) between the two methods via a paired t-test is often more appropriate [7].
- For data covering a wide analytical range, linear regression analysis (e.g., ordinary least squares) is used to calculate the slope (
Alternative Protocol: Quality Control for Systematic Error Detection
Purpose: To continuously monitor for the presence of systematic error using control samples with known values [9].
Experimental Design:
- Use of Certified Reference Materials: Control samples with certified concentrations are analyzed with each analytical run [9].
- Levey-Jennings Plots: The control values are plotted on a Levey-Jennings chart over time, with control lines indicating the mean and standard deviations (e.g., ±1SD, ±2SD, ±3SD) established through a prior replication study [9].
- Application of Westgard Rules: Systematic control rules are applied to identify bias. These include [9]:
- 2
2sRule: Bias is indicated if two consecutive control values exceed the 2SD limit on the same side of the mean. - 4
1sRule: Bias is indicated if four consecutive control values exceed the 1SD limit on the same side of the mean. - 10
xRule: Bias is indicated if ten consecutive control values fall on the same side of the mean.
- 2
The workflow for this quality control process is depicted below.
Comparison of Detection and Quantification Methods
Different techniques offer varying strengths in detecting and quantifying systematic error. The choice of method depends on the stage of method validation (initial vs. ongoing) and the nature of the data.
Table 2: Comparison of Systematic Error Detection Methodologies
| Methodology | Primary Application | Key Advantages | Key Limitations | Quantitative Output |
|---|---|---|---|---|
| Method Comparison Experiment | Initial method validation and verification. | Uses real patient samples; estimates error at medical decision levels; characterizes constant/proportional error. | Labor-intensive; requires a carefully selected comparative method. | Slope, Intercept, Systematic Error (SE) at Xc |
| Levey-Jennings / Westgard Rules | Ongoing internal quality control. | Real-time monitoring; easy to implement and interpret; rules are tailored for specific error types. | Relies on stability of control materials; may not detect all matrix-related errors. | Qualitative (Accept/Reject Run) or violation patterns |
| Average of Normals / Moving Averages | Continuous monitoring using patient data. | Uses real patient samples; can detect long-term, subtle shifts; no additional cost for controls. | Requires sophisticated software; assumes a stable patient population. | Moving average value and control limits |
The Scientist's Toolkit: Essential Reagents and Materials
The following materials are critical for conducting robust method comparison studies and controlling for systematic error.
Table 3: Essential Research Reagent Solutions for Systematic Error Estimation
| Item | Function in Experiment |
|---|---|
| Certified Reference Materials (CRMs) | Higher-order materials with values assigned by a definitive method. Used to establish traceability and assess the trueness of the test method [10]. |
| Commercial Control Samples | Stable, pooled specimens with assigned target values. Used for daily quality control to monitor the stability of the analytical process and detect systematic shifts [10]. |
| Panel of Patient Specimens | A carefully selected set of 40-100 fresh patient samples covering the clinical reportable range. Essential for the comparison of methods experiment to assess performance across real-world matrices [7]. |
| Calibrators | Materials of known concentration used to adjust the instrument's response to establish a calibration curve. Their traceability is paramount to minimizing systematic error [10]. |
| Interference Check Samples | Solutions containing potential interferents (e.g., bilirubin, hemoglobin, lipids). Used to test the specificity of the method and identify positive bias caused by interference [10]. |
Strategies for Mitigation and Correction
Once a systematic error is identified and quantified, several strategies can be employed to mitigate or correct it.
- Calibration and Traceability: The most direct correction for a quantified bias is to apply a correction factor derived from the method comparison or recovery experiment. Ensuring that all calibrators are traceable to higher-order reference methods and materials, as per the ISO 17511 standard, is a fundamental preventative strategy [10].
- Method Improvement: If the source of error is identified, such as a specific interferent, the method protocol can be modified to eliminate it, for example, by introducing a purification step or using a more specific antibody [10].
- Triangulation: Using multiple techniques or instruments to measure the same analyte can help identify and correct for biases inherent in any single method [1].
- Regular Training and Standardization: Comprehensive training and calibration of all personnel involved in data collection and analysis reduces operator-dependent systematic errors. Standardizing protocols across all operators and sites is crucial [1] [11].
- Process Control: Implementing robust systems for specimen handling, storage, and processing can minimize pre-analytical sources of systematic error [7] [12].
The Impact of Uncorrected Bias on Data Integrity and Clinical Decision-Making
In laboratory medicine and clinical research, every measurement possesses a degree of uncertainty termed "error," which represents the difference between a measured value and the true value [9]. Systematic error, also known as bias, is a particularly challenging form of measurement error because it is reproducible and consistently skews results in the same direction, unlike random errors which follow a Gaussian distribution and can be reduced through repeated measurements [9]. Uncorrected systematic bias directly compromises data integrity by creating reproducible inaccuracies that cannot be eliminated through averaging or increased sample sizes, ultimately leading to flawed clinical decisions based on distorted evidence.
The growing integration of artificial intelligence (AI) in healthcare introduces new dimensions to the challenge of systematic bias. AI systems trained on biased datasets risk exacerbating health disparities, particularly when these systems demonstrate differential performance across patient demographics [13] [14]. In high-stakes clinical environments, opaque "black box" AI algorithms can compound these issues by making it difficult for healthcare professionals to interpret diagnostic recommendations or identify underlying biases [14]. These challenges necessitate robust methodological approaches for detecting, quantifying, and correcting systematic errors across both traditional laboratory medicine and emerging AI-assisted clinical decision-making.
Fundamental Classification of Biases
Table 1: Categories and Characteristics of Systematic Bias
| Bias Category | Definition | Common Sources | Impact on Data |
|---|---|---|---|
| Constant Bias | Fixed difference between observed and expected values throughout measurement range | Instrument calibration errors, background interference | Consistent offset across all measurements |
| Proportional Bias | Difference between observed and expected values that changes proportionally with analyte concentration | Sample matrix effects, reagent degradation | Error magnitude increases with concentration |
| Algorithmic Bias | Systematic errors in AI/ML models leading to unfair outcomes for specific groups | Non-representative training data, flawed feature selection | Exacerbated health disparities, inaccurate predictions for minorities [13] [14] |
| Data Integrity Bias | Errors introduced through flawed data collection or processing | EHR inconsistencies, problematic data harmonization [13] | Compromised dataset quality affecting all downstream analyses |
In traditional laboratory settings, systematic errors frequently originate from instrument calibration issues, reagent degradation, or sample matrix effects that create either constant or proportional biases in measurements [9]. These technical biases can often be detected through method comparison studies using certified reference materials with known analyte concentrations.
The integration of artificial intelligence in healthcare introduces novel bias sources. AI systems fundamentally depend on their training data, and when this data originates from de-identified electronic health records (EHR) riddled with inconsistencies, the resulting models inherit and potentially amplify these flaws [13]. Additionally, algorithmic design choices and feature selection biases can create systems that perform unequally across patient demographics, particularly for underrepresented populations who may be inadequately represented in training datasets [14]. Healthcare professionals have reported instances where AI algorithms underperformed for minority patient groups or when identifying atypical presentations, raising serious concerns about fairness and reliability [14].
Detection Methodologies for Systematic Bias
Traditional Laboratory Detection Methods
Table 2: Experimental Protocols for Bias Detection
| Methodology | Protocol Description | Key Statistical Measures | Application Context |
|---|---|---|---|
| Comparison of Methods Experiment | Analyze ≥40 patient specimens by both test and comparative methods across multiple runs [7] | Linear regression (slope, y-intercept), systematic error estimation at medical decision points [7] | Laboratory method validation, instrument comparison |
| Levey-Jennings Plotting with Westgard Rules | Plot quality control measurements over time with control limits based on replication studies [9] | 2₂S rule, 4₁S rule, 10ₓ rule for systematic error detection [9] | Daily quality control monitoring |
| Statistical Process Control | Analyze patient results as "Average of Normals" or "Moving Patient Averages" [9] | Mean, standard deviation, trend analysis | Continuous bias monitoring using patient data |
Advanced and AI-Focused Detection Approaches
For AI-assisted healthcare tools, detection methodologies must address unique challenges. Bias audits using established open-source tools like IBM's AI Fairness 360 provide structured approaches to identify algorithmic disparities [13]. These tools can help quantify differential performance across patient demographics and identify potential fairness issues before clinical deployment.
The establishment of AI Ethics Boards modeled after Northeastern University's approach, which incorporates 40 ethicists and community members to review AI initiatives, represents an organizational approach to bias detection [13]. Similar to Institutional Review Boards (IRBs), these multidisciplinary committees can evaluate AI-based tools before implementation and incorporate diverse community perspectives to ensure adequate representation in care decisions [13]. Additionally, privacy-preserving techniques such as federated learning, implemented in projects like Europe's FeatureCloud, enable multi-institutional collaboration on model development without compromising patient privacy, potentially expanding dataset diversity [13].
Figure 1: Systematic Bias Detection Workflow. This diagram illustrates complementary approaches for identifying systematic errors in both traditional laboratory settings and AI-assisted healthcare tools.
Impact on Data Integrity and Clinical Outcomes
Data Integrity Compromises
Uncorrected systematic bias fundamentally undermines data integrity through several mechanisms. In laboratory medicine, both constant and proportional biases create reproducible inaccuracies that distort the relationship between measured values and true biological states [9]. When these biased measurements inform clinical decisions, the integrity of the entire decision-making process becomes compromised.
In AI-assisted healthcare, biased algorithms can systematically underperform for minority populations when trained on non-representative datasets, creating a form of digital discrimination that healthcare professionals find particularly concerning [14]. The "black box" nature of many complex AI models exacerbates these issues by making it difficult to identify the root causes of biased outcomes, creating transparency challenges that further erode data integrity [14]. When biased algorithms influence clinical workflows, the resulting decisions may reflect systemic inequities rather than objective clinical assessments.
Consequences for Clinical Decision-Making
The downstream effects of uncorrected bias on clinical decision-making can be profound. Healthcare professionals report reduced trust in AI-assisted decisions when they perceive potential biases, particularly for complex cases or rare conditions where algorithmic performance may be uncertain [14]. This trust erosion becomes especially problematic when biased triage recommendations during resource scarcity, such as that experienced during the COVID-19 pandemic, potentially disadvantage vulnerable patient populations [13].
Perhaps most concerning are situations where statistical errors in published literature remain uncorrected despite reader requests, as this prevents clinicians from basing their decisions on accurate evidence [15]. When such errors affect practice guidelines, they can influence care standards for numerous patients before the inaccuracies are identified and addressed.
Mitigation Strategies and Regulatory Considerations
Technical and Operational Mitigations
Several strategic approaches can mitigate the impact of systematic bias on data integrity and clinical decision-making:
Enhanced Dataset Development: Initiatives like the National Clinical Cohort Collaborative (N3C), which harmonizes data from over 75 institutions, provide templates for creating more inclusive datasets that better represent diverse patient populations [13]. Similarly, the All of Us Research Program aims to develop a nationwide database reflecting broader demographic diversity, though challenges of scale and speed remain [13].
Privacy-Preserving Collaboration: Techniques such as federated learning enable multi-institutional model development without centralizing sensitive patient data, as demonstrated by Google's Android, Apple's iOS, and Europe's FeatureCloud project [13]. These approaches facilitate broader data representation while maintaining privacy protections.
Continuous Monitoring Systems: Implementing post-deployment monitoring with continuous audit mechanisms, inspired by the Federal Aviation Administration's black boxes or the FDA's Adverse Event Reporting System (FAERS), can help detect and address failures in real-time [13]. Without such systems, troubleshooting biased AI systems in high-stakes clinical settings becomes extremely difficult.
Regulatory Frameworks and Future Directions
Regulatory agencies are increasingly focusing on bias mitigation in healthcare technologies. The FDA's draft regulatory pathway for Artificial Intelligence and Machine Learning Software as a Medical Device (SaMD) Action Plan provides a starting point for regulatory oversight, though agencies like HHS and CMS have yet to adopt similar comprehensive regulations [13]. The upcoming ICH E6(R3) guidelines, expected in 2025, will emphasize data integrity and traceability with greater scrutiny on data management practices throughout the research lifecycle [16].
Future regulatory innovation should address accountability gaps in AI-assisted decision-making, where healthcare professionals feel ultimately liable for patient outcomes while simultaneously relying on opaque algorithmic insights [14]. Clearer regulatory frameworks that define responsibility across developers, clinicians, and institutions will be essential for building trust in increasingly automated healthcare systems.
Figure 2: Clinical Impact Pathway of Uncorrected Bias. This diagram illustrates how systematic errors propagate through data systems to ultimately affect patient outcomes.
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Bias Evaluation
| Reagent/Material | Function in Bias Research | Application Context |
|---|---|---|
| Certified Reference Materials | Provide known values for method comparison studies to quantify systematic error [9] | Laboratory method validation, instrument calibration |
| Quality Control Samples | Monitor analytical performance over time using Levey-Jennings plots and Westgard rules [9] | Daily quality control, bias trend detection |
| AI Fairness 360 Toolkit | Open-source library containing metrics to test for biases in AI models and datasets [13] | Algorithmic bias detection in healthcare AI |
| Diverse Biobank Specimens | Provide representative samples across demographics to test for population-specific biases | Bias assessment in diagnostic assays and AI models |
| Standardized EHR Data Templates | Facilitate interoperable, consistent data collection to reduce structural biases [13] | Healthcare dataset creation and harmonization |
Uncorrected systematic bias represents a fundamental challenge to data integrity and clinical decision-making across both traditional laboratory medicine and emerging AI-assisted healthcare. The consistent, reproducible nature of systematic errors means they cannot be eliminated through statistical averaging alone, requiring instead targeted detection methodologies and proactive mitigation strategies. As healthcare becomes increasingly dependent on complex algorithms and large-scale data analysis, maintaining vigilance against systematic bias becomes ever more critical for ensuring equitable, evidence-based patient care.
The path forward requires collaborative effort across multiple stakeholders—clinicians, laboratory professionals, AI developers, regulators, and patients—to develop comprehensive approaches to bias detection and mitigation. Through enhanced dataset diversity, robust methodological frameworks, continuous monitoring systems, and thoughtful regulatory oversight, the healthcare community can work toward minimizing the impact of systematic errors on both data integrity and the clinical decisions that shape patient outcomes.
In scientific research and drug development, the validity of quantitative data hinges on a clear understanding of core measurement concepts. Accuracy, precision, trueness, and measurement uncertainty are distinct but interrelated properties that characterize the quality and reliability of measurement results. Within the context of method comparison experiments, these concepts provide the framework for estimating systematic errors and determining whether a new analytical method is fit for its intended purpose. The International Organization for Standardization (ISO) and the Guide to the Expression of Uncertainty in Measurement (GUM) provide standardized definitions and methodologies for evaluating these parameters, ensuring consistency and comparability across laboratories and scientific studies [17].
This guide objectively compares these fundamental concepts, delineating their roles in systematic error estimation. We present structured experimental data, detailed protocols for method comparison studies, and visualizations of their logical relationships, providing researchers and drug development professionals with the tools to critically assess measurement performance.
Defining the Concepts
Precision: The Measure of Dispersion
Precision describes the closeness of agreement between independent measurement results obtained under stipulated conditions [18] [19]. It is a measure of dispersion or scatter and is typically quantified by measures such as standard deviation or variance. High precision indicates low random error and high repeatability, meaning repeated measurements cluster tightly together. However, precision alone says nothing about a measurement's closeness to a true value; a method can be highly precise yet consistently wrong [18] [20].
- Factors Affecting Precision: Random errors, which are unpredictable fluctuations, influence precision. These can arise from environmental variations (e.g., temperature, humidity), electronic noise in instruments, or operator technique [18] [17] [19].
- Quantification: In a series of repeated measurements, precision is often expressed as the standard deviation. A smaller standard deviation indicates higher precision.
Trueness: The Proximity to a True Value
Trueness refers to the closeness of agreement between the average value of a large series of measurement results and a true or accepted reference value [18]. Unlike precision, which concerns scatter, trueness concerns the central tendency of the data. It provides information about how far the average of your measurements is from the real value and is a qualitative expression of systematic error, or bias [18] [17].
- Systematic Errors: The cause of low trueness is systematic error. These errors are consistent, predictable, and often stem from the measuring device itself or a biased procedure [18] [17]. For example, a scale that consistently reads 1 gram too high has a systematic error.
- Reference Value: Determining trueness requires a reference value, which is often established through calibration using a traceable standard [18].
Accuracy: The Combination of Trueness and Precision
Accuracy describes the closeness of a single measurement result to the true value [18] [21] [20]. It is the overarching goal in most measurements. A measurement is considered accurate only if it is both true (has low systematic error) and precise (has low random error). In other words, accuracy incorporates the effects of both trueness and precision [18].
To have high accuracy, a series of measurements must be both precise and true. Therefore, high accuracy means that each measurement value, not just the average of the measurements, is close to the real value [18]. The accuracy of a measuring device is often given as a percentage, indicating the maximum expected deviation from the true value under specified conditions [18].
Measurement Uncertainty: A Quantitative Statement of Doubt
Measurement uncertainty is a non-negative parameter characterizing the dispersion of the quantity values being attributed to a measurand [17]. In simpler terms, it is a quantitative statement about the doubt associated with a measurement result. Every measurement is subject to error, and uncertainty provides an interval around the measured value within which the true value is believed to lie with a certain level of confidence [17] [22] [23].
Uncertainty does not represent error itself but quantifies the reliability of the result. It is typically expressed as a combined standard uncertainty or an expanded uncertainty (e.g., ±0.03%) and encompasses contributions from both random effects (precision) and imperfect corrections for systematic effects (trueness) [18] [17]. As stated in the GUM, a measurement result is complete only when accompanied by a quantitative statement of its uncertainty [17].
Visualizing the Relationships
The following diagram illustrates the logical relationships between a true value, systematic error (influencing trueness), random error (influencing precision), and their combined effect on accuracy and measurement uncertainty.
Diagram 1: Relationship between measurement concepts. Systematic and random errors influence the measured value. Trueness and Precision are inversely related to these errors, respectively. Both are components of Accuracy, which itself is inversely related to Measurement Uncertainty.
Quantitative Comparison of Concepts
The table below provides a structured comparison of the four key concepts, summarizing their definitions, what they are influenced by, and how they are typically quantified.
Table 1: Quantitative Comparison of Key Metrological Concepts
| Concept | Definition | Influenced By | Quantified By | ||
|---|---|---|---|---|---|
| Precision | Closeness of agreement between repeated measurements [18] [19]. | Random errors [17]. | Standard Deviation (SD), Variance, Coefficient of Variation (CV) [17]. | ||
| Trueness | Closeness of the mean of measurement results to a true/reference value [18]. | Systematic errors (bias) [18] [17]. | Bias (mean - reference value) [18] [7]. | ||
| Accuracy | Closeness of a single measurement result to the true value [18] [21]. | Combined effect of both systematic and random errors [18]. | Total Error (often estimated as | Bias | + 2*SD) [24]. |
| Measurement Uncertainty | Parameter characterizing the dispersion of values attributable to a measurand [17]. | All sources of error (random and systematic) [17]. | Combined Standard Uncertainty, Expanded Uncertainty (e.g., ±0.03%) [18] [17]. |
Experimental Protocols for Systematic Error Estimation
The comparison of methods experiment is a critical study designed to estimate the systematic error (bias) between a new test method and a established comparative method using real patient specimens [7]. The following provides a detailed protocol for executing this experiment.
Experimental Design and Workflow
The diagram below outlines the key stages in a method comparison experiment, from planning and specimen preparation to data analysis and estimation of systematic error.
Diagram 2: Method comparison experiment workflow.
Detailed Methodologies
- Comparative Method Selection: The choice of comparative method is crucial. A reference method with documented correctness is ideal, as any differences can be attributed to the test method. When using a routine method as a comparative method, differences must be interpreted carefully, and additional experiments (e.g., recovery, interference) may be needed to identify which method is inaccurate [7].
- Specimen Selection and Handling: A minimum of 40 different patient specimens is recommended. These should be carefully selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine use [7]. Specimens should be analyzed by both methods within two hours of each other to avoid stability issues, unless specific preservatives or handling procedures (e.g., freezing) are validated [7].
- Measurement Protocol: Specimens should be analyzed over a minimum of 5 days, and ideally over a longer period (e.g., 20 days) to capture long-term sources of variation. While single measurements are common practice, performing duplicate measurements on different sample cups or in different analytical runs is advantageous as it helps identify sample mix-ups or transposition errors [7].
- Data Analysis and Systematic Error Estimation:
- Graphical Analysis: The data should first be graphed for visual inspection. A difference plot (test result minus comparative result vs. comparative result) is used when methods are expected to agree one-to-one. A comparison plot (test result vs. comparative result) is used otherwise. This helps identify outliers and the general relationship between methods [7].
- Statistical Calculations:
- For a wide analytical range (e.g., glucose, cholesterol), linear regression (Y = a + bX) is used. The systematic error (SE) at a critical medical decision concentration (Xc) is calculated as: Yc = a + bXc, then SE = Yc - Xc [7].
- For a narrow analytical range (e.g., sodium, calcium), the average difference (bias) between the two methods is calculated using a paired t-test. The standard deviation of the differences describes the distribution of these differences [7].
- Correlation Coefficient: The correlation coefficient (r) is more useful for assessing whether the data range is wide enough to provide reliable regression estimates (r ≥ 0.99 is desirable) than for judging method acceptability [7].
Advanced Considerations in Systematic Error
Decomposing Systematic Error: Constant and Variable Bias
Traditional models often treat systematic error (bias) as a single, fixed value. However, recent research proposes decomposing bias into two components [24]:
- Constant Component of Systematic Error (CCSE): A stable, correctable offset.
- Variable Component of Systematic Error (VCSE(t)): A time-dependent function that behaves unpredictably over an extended period and cannot be efficiently corrected.
This distinction is critical because the standard deviation (s~RW~) derived from long-term quality control (QC) data includes contributions from both random error and the variable bias component. Using s~RW~ as a sole estimator of random error can lead to an overestimation of method precision and miscalculations of total error [24]. This refined model challenges the assumption that long-term QC data are normally distributed and has significant implications for accurately estimating measurement uncertainty.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Method Comparison Studies
| Item | Function |
|---|---|
| Certified Reference Materials (CRMs) | Provides a traceable, true value for establishing trueness and calibrating instruments [17] [7]. |
| Stable Quality Control (QC) Pools | Monitors the stability and precision of the measurement method over time, helping to identify drift [7] [24]. |
| Patient Specimens | Serves as the core test material for comparison experiments, ensuring the evaluation covers realistic biological matrices and concentration ranges [7]. |
| Calibrators | Used to adjust the analytical output of the instrument to match the reference scale, directly addressing systematic error [7] [19]. |
In systematic error estimation for method comparison experiments, a clear demarcation between precision, trueness, accuracy, and measurement uncertainty is non-negotiable. Precision assesses random variation, trueness quantifies systematic bias, and accuracy encompasses both. Measurement uncertainty then provides a quantitative boundary for the doubt associated with any result, integrating all error components.
Advanced understanding, such as decomposing systematic error into constant and variable parts, allows for more sophisticated quality control models and accurate uncertainty budgets. For researchers and drug development professionals, rigorously applying these concepts and the associated experimental protocols ensures that analytical methods are fit for purpose, supporting the generation of reliable and defensible data critical for scientific discovery and patient safety.
Systematic error, or bias, is defined as the systematic deviation of measured results from the actual value of the quantity being measured [25]. In the context of method comparison experiments, understanding bias is crucial because it directly impacts the interpretation of laboratory results and can lead to misdiagnosis or misestimation of disease prognosis when significant [25]. Bias represents one of the most important metrological characteristics of a measurement procedure, and its accurate estimation is fundamental for ensuring reliability in scientific research and drug development.
Systematic error can be categorized into different types based on its behavior across concentration levels. The two primary forms discussed in this guide are constant bias and proportional bias, which differ in how they manifest across the analytical measurement range [26] [25]. Proper identification of which type of bias is present, or whether both exist simultaneously, is essential for determining the appropriate correction strategy and assessing method acceptability [7]. This guide provides researchers with the experimental frameworks and statistical tools necessary to distinguish between these bias types accurately, supported by practical data analysis and visualization techniques.
Theoretical Foundations of Bias Types
Constant Bias
Constant bias occurs when one measurement method consistently yields values that are higher or lower than those from another method by a fixed amount, regardless of the analyte concentration [26] [27]. This type of bias manifests as a consistent offset between methods across the entire measurement range. In statistical terms, when comparing two methods using regression analysis, constant bias is represented by the intercept (b) in the regression equation y = ax + b [25]. If the confidence interval for this intercept does not include zero, a statistically significant constant bias is present [26].
Visual inspection of method comparison data reveals constant bias as a parallel shift between the line of best fit and the line of identity [26]. For example, if a new method consistently produces results that are 5 units higher than the reference method across all concentration levels—from very low to very high values—this represents a positive constant bias. The difference between methods remains approximately the same absolute value regardless of the concentration being measured.
Proportional Bias
Proportional bias exists when the difference between methods changes in proportion to the analyte concentration [26] [25]. Unlike constant bias, the magnitude of proportional bias increases or decreases as the level of the measured variable changes. This type of bias indicates that the discrepancy between methods is concentration-dependent [27].
In regression analysis, proportional bias is detected through the slope (a) in the equation y = ax + b [25]. If the confidence interval for the slope does not include 1, a statistically significant proportional bias is present [25]. Proportional bias can be either positive (the difference between methods increases with concentration) or negative (the difference decreases with concentration) [26]. Visual evidence of proportional bias appears as a gradual divergence between the line of best fit and the line of identity as concentration increases, creating a fan-like pattern in the difference plot.
Combined Bias Effects
In practice, methods can exhibit both constant and proportional bias simultaneously [26]. This combined effect occurs when there is both a fixed offset between methods and a concentration-dependent discrepancy. The regression equation would in this case show both an intercept significantly different from zero and a slope significantly different from 1 [26] [25].
Identifying these combined effects is particularly important for method validation, as each type of bias may have different sources and require different corrective approaches [7]. For instance, constant bias might stem from calibration issues, while proportional bias could indicate problems with analytical specificity or nonlinearity in the measurement response [28].
Table 1: Characteristics of Bias Types in Method Comparison
| Bias Type | Mathematical Representation | Visual Pattern | Common Sources |
|---|---|---|---|
| Constant Bias | y = x + b (b ≠ 0) | Parallel shift from identity line | Calibration errors, matrix effects |
| Proportional Bias | y = ax + b (a ≠ 1) | Divergence from identity line | Improper slope, instrument sensitivity |
| Combined Bias | y = ax + b (a ≠ 1, b ≠ 0) | Both shift and divergence | Multiple error sources |
Experimental Design for Bias Detection
Sample Selection and Preparation
Proper sample selection is critical for comprehensive bias assessment. A minimum of 40 patient specimens is recommended, carefully selected to cover the entire working range of the method [7]. These specimens should represent the spectrum of diseases and conditions expected in routine application of the method. The quality of specimens is more important than quantity alone; 20 well-selected specimens covering the analytical range may provide better information than 100 randomly selected specimens [7].
Sample stability must be carefully controlled throughout the experiment. Specimens should generally be analyzed within two hours of each other by the test and comparative methods, unless specific analytes require shorter timeframes [7]. For unstable analytes, appropriate preservation techniques such as serum separation, refrigeration, or additive preservation should be implemented using standardized protocols to prevent handling-related discrepancies from being misinterpreted as analytical bias.
Measurement Protocol
The comparison experiment should be conducted over a minimum of 5 different days to account for daily variations in analytical performance [7]. Extending the study to 20 days with fewer specimens per day often provides more robust bias estimates by incorporating long-term reproducibility components [25]. This approach helps distinguish consistent systematic errors from random variations that occur under intermediate precision conditions.
When possible, duplicate measurements should be performed rather than single measurements [7]. Ideally, duplicates should represent different sample aliquots analyzed in different runs or at least in different order—not back-to-back replicates of the same cup. This duplicate analysis provides a check for measurement validity and helps identify discrepancies arising from sample mix-ups or transcription errors that could otherwise be misinterpreted as bias.
Reference Method Selection
The choice of comparison method significantly impacts bias interpretation. A reference method with documented accuracy through definitive methods or traceable reference materials is ideal, as any discrepancies can be attributed to the test method [7]. When using a routine method for comparison (termed a "comparative method"), differences must be carefully interpreted, as it may be unclear which method is responsible for observed discrepancies [7].
For materials used in bias estimation, reference values can be established through certified reference materials (CRMs), reference measurement procedures, or consensus values from external quality assessment schemes [28] [25]. However, research indicates that consensus values may not always approximate true values well, particularly for certain analytes like lipids and apolipoproteins, making reference method values preferable when available [28].
Statistical Analysis Methods
Regression Analysis
Regression analysis provides the primary statistical approach for identifying and quantifying both constant and proportional bias [7]. The fundamental regression equation for method comparison is:
y = ax + b
Where 'y' represents test method results, 'x' represents comparative method results, 'a' is the slope (indicating proportional bias), and 'b' is the intercept (indicating constant bias) [25]. The standard deviation of points about the regression line (s~y/x~) quantifies random error around the systematic error relationship.
For medical decision-making, systematic error at critical decision concentrations (X~c~) should be calculated as:
Y~c~ = a + bX~c~ SE = Y~c~ - X~c~
This calculation provides the clinically relevant bias at important medical decision levels [7]. When the correlation coefficient (r) is below 0.99, additional data collection or alternative regression approaches may be necessary, as simple linear regression may provide unreliable estimates of slope and intercept [7].
Difference Analysis (Bland-Altman)
The Bland-Altman method provides an alternative approach for assessing agreement between methods by plotting differences between measurements against their averages [29]. This method is particularly valuable for visualizing the magnitude and pattern of bias across the measurement range and for identifying individual outliers or concentration-dependent effects [28].
While Bland-Altman analysis effectively detects the presence of bias, it does not inherently distinguish between constant and proportional components without additional modifications [27] [29]. For this reason, many methodologies recommend combining Bland-Altman visualization with regression analysis to fully characterize the nature of systematic error [28].
Hypothesis Testing for Bias
Statistical hypothesis testing provides a framework for determining whether observed biases are statistically significant. Two common approaches include:
- Equality test: The null hypothesis states that bias equals zero against the alternative that it does not. A small p-value indicates statistically significant bias [30].
- Equivalence test: The null hypothesis states that bias falls outside a predefined interval of practical equivalence. A small p-value supports that bias is within acceptable limits [30].
These tests are complementary to point estimates of bias and should be interpreted in conjunction with confidence intervals and medical relevance considerations [30].
Table 2: Statistical Methods for Bias Detection and Characterization
| Method | Primary Function | Bias Detection Capability | Key Outputs |
|---|---|---|---|
| Linear Regression | Models relationship between methods | Constant (intercept) and proportional (slope) | Regression equation, s~y/x~ |
| Bland-Altman Analysis | Visualizes agreement and differences | Overall bias pattern and range | Mean difference, limits of agreement |
| Least Products Regression | Handles error in both variables | Constant and proportional bias with error in both methods | Unbiased slope and intercept estimates |
| Hypothesis Testing | Determines statistical significance | Whether bias is statistically different from zero | p-values, confidence intervals |
Visualization Approaches
Regression Plots
Regression Analysis Workflow
Regression plots provide the most direct visualization for identifying constant and proportional bias. The graph displays test method results on the Y-axis versus comparative method results on the X-axis [7]. The line of identity (y = x) represents perfect agreement, while the regression line (y = ax + b) shows the actual relationship.
Visual interpretation focuses on the relationship between these two lines. A constant bias appears as a parallel vertical shift between the lines, while proportional bias manifests as differing slopes causing the lines to converge or diverge across the concentration range [26]. The dispersion of points around the regression line indicates random error, which should be considered when interpreting the practical significance of systematic error [26].
Difference Plots
Difference Plot Creation Process
Difference plots (Bland-Altman plots) display the difference between methods against the average of the two methods [28] [29]. This visualization excels at showing the magnitude and pattern of disagreement across the measurement range.
A horizontal distribution of points around zero indicates no systematic bias. A horizontal distribution offset from zero suggests constant bias. A sloping pattern or fan-shaped distribution indicates proportional bias, where differences increase or decrease with concentration [26]. The mean difference represents the average bias, while the limits of agreement (mean ± 1.96 SD) show the expected range for most differences between methods [29].
Research Reagent Solutions
Table 3: Essential Materials for Method Comparison Studies
| Reagent/Material | Function | Critical Specifications |
|---|---|---|
| Certified Reference Materials (CRMs) | Provide reference quantity values for bias estimation | Commutability, traceability, uncertainty documentation |
| Commutable Control Materials | Mimic fresh patient sample properties | Matrix similarity, stability, homogeneity |
| Calibrators | Establish measurement traceability | Value assignment by reference method, stability |
| Quality Control Materials | Monitor measurement performance | Well-characterized values, appropriate concentrations |
| Patient Sample Pool | Assess real-world performance | Diverse pathologies, concentration ranges, stability |
Data Interpretation and Clinical Implications
Assessing Statistical vs. Practical Significance
A statistically significant bias does not necessarily imply medically relevant consequences [30]. For large sample sizes, even trivial biases may achieve statistical significance, while clinically important biases in small studies may lack statistical significance [30]. Therefore, bias evaluation must consider both statistical testing and clinical context.
Researchers should compare estimated biases at medically important decision concentrations to established analytical performance specifications (APSs) [25]. These specifications define the quality required for analytical performance to deliver clinically useful results without causing harm to patients [25]. The systematic error at critical decision levels should be small enough not to affect clinical interpretation or patient management decisions.
Corrective Strategies Based on Bias Type
The type of bias identified dictates the appropriate corrective approach:
- Constant bias: Often correctable through calibration adjustment or blank correction. This may involve re-calibrating instruments or applying a fixed correction factor to all results [31].
- Proportional bias: Typically requires slope correction or method-specific calibration. This may involve using different calibrators or mathematical correction based on the established proportional relationship.
- Combined bias: Needs a comprehensive approach addressing both constant and proportional components, potentially involving method optimization or replacement if corrections are complex [26].
After implementing corrections, verification studies should confirm that biases have been effectively reduced to clinically acceptable levels across the measurement range.
Impact on Reference Intervals and Clinical Decision Limits
When changing measurement methods, significant biases may necessitate reference interval verification or establishment [26]. If a new method shows consistent positive constant bias compared to the previous method, reference intervals may need corresponding adjustment to maintain consistent clinical interpretation [26].
For proportional bias, the impact on patient classification depends on where medical decision limits fall relative to the convergence point of method comparisons. If decision limits are below the convergence point for negative proportional bias, reference intervals might not need adjustment, as the bias would only affect high values [26]. Understanding these relationships is essential for maintaining consistent clinical interpretation across method changes.
Conducting Robust Method Comparison Studies: From Design to Statistical Analysis
In method comparison studies, accurate and reliable results depend on controlling key pre-analytical and biological variables. The integrity of research on diagnostic platforms, biomarker assays, or pharmacokinetic parameters hinges on a rigorous experimental design that minimizes systematic error. This guide objectively compares methodological approaches by focusing on three foundational pillars: sample selection, timing, and accounting for physiological range. Failure to adequately control these factors introduces systematic errors (biases) that compromise the validity of a method's reported performance against its alternatives. This analysis provides a structured comparison of design protocols, supported by experimental data and clear visual workflows, to guide researchers in drug development and related fields toward more robust and generalizable method comparison experiments.
Core Concepts and Definitions
Understanding the following concepts is essential for designing method comparison experiments that accurately estimate and minimize systematic error.
- Systematic Error: A consistent, reproducible error due to the measurement method itself, as opposed to random error. In method comparison studies, it represents the bias between a new method and a reference standard.
- Sample Selection: The process and criteria by which biological specimens are chosen for a study. Biased selection can lead to a sample population that does not adequately represent the target physiological range, skewing method performance estimates [32].
- Physiological Range: The spectrum of values for a given analyte that can be observed in a healthy or diseased population. A method must be validated across this entire range to be clinically useful, as performance can vary at different concentrations [32].
- Method Comparison Experiment: A study designed to evaluate the agreement between two or more measurement methods, typically comparing a new method to an established reference.
Comparative Analysis of Methodological Approaches
The following section compares standard and optimized protocols for the three critical design considerations, summarizing key differentiators and their impact on systematic error.
Table 1: Comparison of Standard vs. Optimized Methodological Approaches
| Design Consideration | Standard Practice | Optimized Practice | Impact on Systematic Error |
|---|---|---|---|
| Sample Selection | Convenience sampling; limited demographic/health coverage [32]. | Stratified sampling to cover the full physiological range, including pathological states [32]. | Reduces spectrum bias and improves the generalizability of the bias (difference) estimate between methods. |
| Timing | Single timepoint collection; unstandardized processing delays. | Multiple timepoints to account for diurnal/biological rhythms; standardized processing protocols. | Minimizes bias introduced by biological variability and sample degradation, providing a more stable performance estimate. |
| Physiological Range | Validation primarily within "normal" range [32]. | Deliberate inclusion of values spanning the entire expected clinical range (low, normal, high) [32]. | Ensures the method's performance is characterized across all relevant conditions, revealing context-specific biases. |
Experimental Protocols for Key Studies
Protocol for a Comprehensive Method Comparison Study
This detailed protocol is designed to systematically control for sample, timing, and range-related biases.
- Define Scope and Reference: Clearly identify the new method and the reference method against which it is being compared. The reference standard should be a widely accepted "gold standard" if available.
- Ethical Approval and Informed Consent: Obtain all necessary ethical approvals and informed consent from participants before sample collection.
- Stratified Sample Recruitment: Recruit participants to ensure coverage across key demographic strata (e.g., age, sex) and health statuses (healthy, target disease, co-morbidities) to populate the full physiological range [32].
- Standardized Sample Collection:
- Timing: For analytes with known diurnal variation (e.g., cortisol), collect samples at a standardized time of day. If relevant, collect multiple samples over time from the same subject.
- Processing: Implement a standard operating procedure (SOP) for sample handling (e.g., centrifugation speed and time, aliquot volume, storage temperature) to minimize pre-analytical variation.
- Blinded Measurement: Analyze each sample using both the new and reference methods in a blinded fashion, where the operator is unaware of the result from the other method.
- Data Collection and Storage: Record all results in a structured database, including sample ID, demographic data, collection timestamp, and results from both methods.
Protocol for a Longitudinal Variability Assessment
This protocol specifically investigates the impact of timing on method performance.
- Participant Selection: Recruit a cohort of subjects representative of the target population.
- Baseline Sampling: Collect an initial sample from each participant following the standardized collection SOP.
- Follow-up Sampling: Collect subsequent samples from the same participants at predetermined intervals (e.g., 2 weeks, 1 month, 3 months).
- Parallel Analysis: Analyze all samples using both the new and reference methods within the same analytical run, where possible, to minimize inter-assay variation.
- Data Analysis: Calculate the within-subject and between-subject variability for both methods and assess the stability of the method difference (bias) over time.
The following tables summarize hypothetical experimental data that would be generated from the protocols described above, illustrating how different design choices impact the outcomes of a method comparison.
Table 2: Impact of Sample Selection on Reported Method Bias This table compares the average bias observed when a method is tested on a limited versus a comprehensive sample population.
| Sample Population | Sample Size (n) | Average Bias (Units) | 95% Limits of Agreement |
|---|---|---|---|
| Healthy Adults Only | 40 | +0.5 | -2.1 to +3.1 |
| Full Physiological Range | 120 | +1.2 | -4.8 to +7.2 |
Table 3: Effect of Timing/Processing Delays on Analyte Stability This table shows how measured concentrations of a stable and a labile analyte change with processing delays, affecting method agreement.
| Processing Delay | Measured Concentration (Stable Analyte) | Measured Concentration (Labile Analyte) |
|---|---|---|
| Immediate (Baseline) | 100.0 | 100.0 |
| After 2 hours (RT) | 99.8 | 87.5 |
| After 4 hours (RT) | 99.5 | 75.2 |
| After 24 hours (4°C) | 98.9 | 65.8 |
Visualizing the Experimental Workflow
The diagram below outlines the logical workflow for a robust method comparison experiment, incorporating the critical design considerations.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Method Comparison Studies
| Item | Function in Experiment |
|---|---|
| Certified Reference Material (CRM) | Provides a ground-truth value with known uncertainty, used to calibrate equipment and validate the accuracy of both the new and reference methods, directly impacting systematic error estimation. |
| Quality Control (QC) Samples | (e.g., high, normal, low concentration pools). Monitored across analytical runs to ensure method precision and stability over time, helping to distinguish systematic shift from random error. |
| Biobanked Samples | Well-characterized residual clinical samples stored under controlled conditions. Used for initial validation and to test method performance across a wide physiological range without the need for immediate, fresh recruitment. |
| Stabilizing Reagents | (e.g., protease inhibitors, RNA stabilizers). Added to samples immediately upon collection to preserve analyte integrity, mitigating bias introduced by pre-analytical delays and ensuring the measured value reflects the in-vivo state. |
| Automated Liquid Handler | Reduces manual pipetting error during sample preparation and reagent addition, a potential source of systematic bias, especially in high-throughput settings. |
Implementing Bland-Altman Analysis for Assessing Agreement and Bias
Bland-Altman analysis, first introduced in 1983 and further detailed in 1986, has become the standard methodological approach for assessing agreement between two measurement techniques in clinical and laboratory research [29] [33]. This analytical technique was developed specifically to address the limitations of correlation analysis in method comparison studies. While correlation measures the strength of a relationship between two variables, it fails to quantify the actual agreement between measurement methods [33]. The Bland-Altman method quantifies agreement by analyzing the differences between paired measurements, providing researchers with a straightforward means to evaluate both systematic bias (fixed or proportional) and random error between methods [34] [35].
The core output of this analysis is the limits of agreement (LoA), which define an interval within which 95% of the differences between the two measurement methods are expected to fall [33] [36]. This approach has gained widespread acceptance across numerous scientific disciplines, with the original 1986 Lancet paper ranking among the most highly cited scientific publications across all fields [29]. For researchers investigating systematic error estimation in method comparison experiments, Bland-Altman analysis provides a robust framework for determining whether two methods can be used interchangeably or whether systematic biases preclude their equivalent application in research or clinical practice.
Fundamental Principles and Analytical Approach
Core Components of Bland-Altman Analysis
The Bland-Altman method operates on a fundamentally different principle from correlation analysis, focusing specifically on the differences between methods rather than their covariation. The analysis generates several key parameters that collectively describe the agreement between two measurement techniques:
Mean Difference (Bias): The average of the differences between paired measurements (Method A - Method B) [35]. This represents the systematic bias between methods, with values significantly different from zero indicating consistent overestimation or underestimation by one method relative to the other.
Limits of Agreement: Defined as the mean difference ± 1.96 times the standard deviation of the differences [33] [36]. These limits create an interval expected to contain 95% of the differences between the two measurement methods if the differences follow a normal distribution.
Clinical Agreement Threshold: A predetermined value representing the maximum acceptable difference between methods based on clinical requirements, biological considerations, or analytical goals [33] [36]. This threshold is not determined statistically but must be established a priori based on the specific research context.
The Bland-Altman Plot
The visual representation of the analysis is the Bland-Altman plot, which displays the relationship between differences and magnitude of measurement [34]. This scatter plot is constructed with the following axes:
- X-axis: The average of the two measurements for each subject [(Method A + Method B)/2]
- Y-axis: The difference between the two measurements for each subject (Method A - Method B)
The plot typically includes three horizontal lines: one at the mean difference (bias), and two representing the upper and lower limits of agreement [37] [36]. This visualization enables researchers to detect patterns that might indicate proportional bias, heteroscedasticity (where variability changes with measurement magnitude), or outliers that warrant further investigation.
Table 1: Key Components of a Bland-Altman Plot
| Component | Description | Interpretation |
|---|---|---|
| Mean Difference (Bias) | Average of all differences between paired measurements | Systematic over/underestimation by one method |
| Limits of Agreement | Mean difference ± 1.96 × SD of differences | Range containing 95% of differences between methods |
| Data Points | Individual difference values plotted against averages | Visual assessment of agreement patterns and outliers |
| Clinical Threshold | Predetermined acceptable difference | Reference for evaluating clinical significance |
Methodological Variations and Advanced Applications
Addressing Analytical Challenges
Standard Bland-Altman analysis assumes normally distributed differences and consistent variability across measurement ranges (homoscedasticity). However, real-world data often violate these assumptions, necessitating methodological adaptations:
Non-Normal Distributions: When differences are not normally distributed, the non-parametric approach defines limits of agreement using the 2.5th and 97.5th percentiles of the differences rather than the mean ± 1.96SD [36]. This approach does not rely on distributional assumptions and provides more robust agreement intervals for non-normal data.
Proportional Bias: Occurs when the differences between methods change systematically with the magnitude of measurement [38] [36]. This is evident in Bland-Altman plots as a sloping pattern of differences rather than random scatter around the mean difference line. Regression-based Bland-Altman analysis can model this relationship by expressing both the bias and limits of agreement as functions of the measurement magnitude [36].
Heteroscedasticity: When the variability of differences changes with measurement magnitude (often appearing as a funnel-shaped pattern on the plot), the data may require transformation or ratio-based analysis [38] [36]. Common approaches include plotting percentage differences or analyzing ratio data following logarithmic transformation [36].
Study Design Considerations
Bland-Altman analysis can be applied to different experimental designs, each with specific analytical requirements:
Single Measurements per Method: The standard approach where each method measures each subject once [39]. This design provides the basic agreement assessment but cannot evaluate within-method variability.
Multiple Unpaired Measurements: Each subject is measured several times by each method, but without natural pairing between measurements [39]. This design allows estimation of both between-method and within-method variability.
Multiple Paired Measurements: Each subject is measured several times by each method in rapid succession, maintaining natural pairing [39]. This sophisticated design provides the most comprehensive assessment of measurement agreement and variability components.
Software Implementation and Tools
Comparative Analysis of Software Solutions
Various software packages implement Bland-Altman analysis with differing capabilities, particularly in handling advanced analytical scenarios. The table below summarizes key available tools and their features:
Table 2: Software Tools for Bland-Altman Analysis
| Software Tool | Accessibility | Key Features | Limitations |
|---|---|---|---|
| BA-plotteR [38] [40] | Free web-based tool | Handles heteroscedastic data, proportional bias; validates assumptions; open-source | Requires internet access for web version |
| MedCalc [36] | Commercial statistical software | Parametric, non-parametric, and regression-based methods; comprehensive confidence intervals | License fee required |
| NCSS [39] | Commercial statistical package | Supports multiple study designs; includes Deming and Passing-Bablok regression | Commercial product with cost implications |
| GraphPad Prism [35] | Commercial statistical software | User-friendly interface; bias and LoA calculation; trend detection | Limited advanced features for complex data |
| Real Statistics [37] | Excel-based package | Bland-Altman plot creation; LoA calculation with confidence intervals | Requires Excel environment |
BA-plotteR: A Specialized Tool for Comprehensive Analysis
BA-plotteR represents a significant advancement in Bland-Altman analysis implementation, specifically designed to address limitations in commonly available statistical software [38]. This free, web-based tool provides:
Automated Assumption Checking: The tool automatically assesses normality of differences, heteroscedasticity, and proportional biases, guiding users toward appropriate analytical approaches [38].
Advanced Analytical Capabilities: BA-plotteR implements the evolved Bland-Altman methodology that can handle heteroscedastic data and various bias types through regression-based limits of agreement [38].
User Guidance: The tool provides analytical guidance when data violate the assumptions of standard Bland-Altman analysis, reducing implementation errors common among researchers [38].
Validation studies comparing BA-plotteR output against manually derived results have demonstrated perfect agreement, confirming its reliability for research applications [38] [40].
Experimental Protocols for Method Comparison Studies
Standard Protocol for Basic Bland-Altman Analysis
For researchers implementing Bland-Altman analysis for method comparison studies, the following protocol ensures proper execution:
Study Design and Sample Size:
- Select an appropriate sample size that ensures precise estimates of the limits of agreement. While early recommendations suggested 100 observations, power-based approaches using methods like those proposed by Lu et al. provide more rigorous sample size determination [41].
- Ensure measurements cover the entire clinically relevant range rather than focusing on extreme values [33].
Data Collection:
- Obtain paired measurements using both methods on each subject under similar conditions [39].
- Ensure measurement pairs are collected independently to prevent carryover effects.
Data Analysis:
Plot Generation:
- Create scatter plot with averages on x-axis and differences on y-axis.
- Add horizontal lines for mean difference and limits of agreement.
- Include confidence intervals for mean difference and limits of agreement when appropriate [36].
Interpretation:
- Assess whether limits of agreement fall within predetermined clinical acceptability thresholds.
- Check for patterns in the plot that might indicate proportional bias or heteroscedasticity.
- Evaluate the clinical implications of any systematic bias.
Protocol for Handling Heteroscedastic Data
When variability between methods changes with measurement magnitude, implement this modified protocol:
Detection: Visually inspect the Bland-Altman plot for funnel-shaped patterns or conduct statistical tests for heteroscedasticity [36].
Transformation: Apply logarithmic transformation to the measurements before analysis, or analyze ratios instead of differences [36].
Analysis: Calculate limits of agreement on the transformed scale, then back-transform to the original measurement scale if necessary [36].
Presentation: Express limits of agreement as percentages when differences are proportional to the measurement magnitude [36].
The following workflow diagram illustrates the decision process for selecting the appropriate Bland-Altman analytical approach:
Research Reagent Solutions for Method Comparison Studies
Table 3: Essential Methodological Components for Bland-Altman Analysis
| Component | Function | Implementation Considerations |
|---|---|---|
| Reference Standard | Provides benchmark for method comparison | Should represent current gold standard method; acknowledge inherent measurement error [41] |
| Calibration Materials | Ensure both methods measure same quantity | Use certified reference materials traceable to international standards |
| Statistical Software | Implement Bland-Altman analysis and visualization | Select tools that handle violations of assumptions [38] [36] |
| Clinical Agreement Threshold | Define clinically acceptable differences | Establish a priori based on biological variation or clinical impact [33] [36] |
| Sample Size Calculator | Determine adequate sample size | Use power-based approaches rather than rules of thumb [41] |
Interpretation Guidelines and Clinical Application
Systematic Approach to Results Interpretation
Proper interpretation of Bland-Altman analysis requires both statistical and clinical reasoning:
Assess Systematic Bias: Determine if the mean difference significantly differs from zero using the 95% confidence interval for the bias [35] [36]. If the confidence interval does not include zero, a statistically significant systematic bias exists.
Evaluate Limits of Agreement: Compare the limits of agreement to the predetermined clinical agreement threshold [36]. For methods to be considered interchangeable, the limits of agreement should not exceed this threshold.
Check for Patterns: Examine the Bland-Altman plot for systematic patterns [35]:
- Proportional Bias: Differences increase or decrease with measurement magnitude
- Heteroscedasticity: Variability of differences changes with measurement magnitude
- Outliers: Individual points falling outside the limits of agreement
Consider Clinical Impact: Even statistically significant bias or wide limits of agreement may be clinically acceptable depending on the application context [35]. The ultimate determination of method interchangeability rests on clinical rather than purely statistical considerations.
Addressing Methodological Criticisms
Despite its widespread adoption, Bland-Altman analysis has faced criticisms that researchers should acknowledge:
Hopkins (2004) and Krouwer (2007) questioned aspects of the methodology, but subsequent analyses found these criticisms to be "scientifically delusive" [29]. Hopkins misapplied the methodology for model validation questions, while Krouwer overgeneralized from narrow, unrealistic situations [29].
The method continues to be recommended as the appropriate statistical approach when the research question involves method comparison rather than relationship assessment [29] [33].
Bland-Altman analysis provides a robust framework for assessing agreement between measurement methods in systematic error estimation research. By focusing on differences between methods rather than their correlation, this approach offers clinically interpretable parameters including systematic bias and limits of agreement. Implementation requires careful attention to analytical assumptions, with adaptations available for non-normal distributions, proportional bias, and heteroscedastic data. Modern software tools, particularly specialized applications like BA-plotteR, have made comprehensive Bland-Altman analysis more accessible while reducing implementation errors common in general statistical packages. When properly applied and interpreted in context of clinically relevant agreement thresholds, Bland-Altman analysis remains the gold standard for method comparison studies across diverse research domains.
Using Linear Regression for Characterizing Constant and Proportional Bias
In method comparison studies, ensuring the accuracy and reliability of a new measurement procedure against a comparative method is paramount. This process requires a thorough investigation of systematic errors, which can consistently skew results. Linear regression analysis serves as a fundamental statistical tool to detect, quantify, and distinguish between two primary types of systematic bias: constant and proportional. This guide provides an objective overview of linear regression protocols for bias estimation, compares its performance with alternative statistical models, and presents experimental data to inform researchers and scientists in drug development and clinical research.
In scientific measurement, systematic error is a consistent deviation inherent in each measurement that skews results in a specific direction, unlike random errors which vary unpredictably [2] [1]. In the context of comparing two analytical methods, a test method is validated against a reference or comparative method to determine its analytical accuracy [42]. The purpose of such comparisons is to uncover systematic differences, not to point to similarities [27].
Systematic errors in this context are primarily categorized as:
- Constant Bias: A fixed deviation where one method gives values that are consistently higher or lower than the other by a constant amount, independent of the analyte concentration [27] [43].
- Proportional Bias: A deviation where the difference between methods is proportional to the level of the measured variable, meaning the error increases or decreases with concentration [27] [43].
These biases are not mutually exclusive and can occur simultaneously. Failure to identify them can lead to distorted findings, invalid conclusions, and inefficient resource allocation [44]. Linear regression provides a framework to characterize these biases objectively.
Theoretical Foundation of Linear Regression for Bias Estimation
The Regression Model
In a method comparison study, results from the test method (Y) and the comparative method (X) are plotted, and a straight line is fitted using the least squares technique. The resulting linear regression equation is: [ Y = a + bX ] where:
ais the Y-intercept, representing the estimated constant bias.bis the slope, representing the estimated proportional bias [43] [45].
The ideal scenario, where no systematic error exists, is represented by a line of identity (a=0, b=1). Deviations from these ideal values indicate systematic error [42] [43].
Relating Regression Parameters to Bias
- Y-Intercept and Constant Bias: A Y-intercept (
a) significantly different from zero suggests a constant systematic error. This represents a fixed deviation that affects all measurements equally, regardless of concentration, often caused by interferences, inadequate blanking, or miscalibrated zero points [43]. - Slope and Proportional Bias: A slope (
b) significantly different from 1.00 suggests a proportional systematic error. The magnitude of this error changes with the concentration level, often due to issues with standardization, calibration, or matrix effects [43].
The overall systematic error (bias) at any given medical decision concentration, ( XC ), can be calculated using the regression equation: ( Bias = YC - XC = (bXC + a) - X_C ) [43].
Experimental Protocols for Linear Regression Analysis
Study Design and Data Collection
A robust method comparison experiment requires careful planning.
- Sample Selection: Select 40-100 patient samples that cover the entire measuring interval of the method [42] [43]. The range should be as wide as possible to reliably estimate the slope.
- Measurement Protocol: Measure each sample using both the test and comparative methods. The experiment should be conducted over several days to capture typical within-laboratory variation.
- Data Arrangement: Data should be arranged in a list dataset layout with continuous scale variables for each method. If replicates are measured, the dataset should have a repeat/replicate measures layout [42].
The diagram below illustrates the typical workflow for a method comparison study using linear regression.
Step-by-Step Analytical Protocol
- Data Plotting: Create a scatter plot with the comparative method (X) on the horizontal axis and the test method (Y) on the vertical axis [42] [45].
- Model Fitting: Perform Ordinary Linear Regression (OLR), which minimizes the vertical distances between the data points and the regression line [45].
- Statistical Calculation: Calculate the following key statistics from the regression:
- Regression Equation (Y = a + bX)
- Correlation Coefficient (r): Assesses the linearity and the range adequacy. A value of r ≥ 0.975 is often considered adequate for OLR [42] [45].
- Standard Error of the Estimate (S~y/x~): A measure of the dispersion of observations around the regression line, which includes the random error of both methods [43].
- Confidence Intervals for Slope and Intercept: Used to test the statistical significance of the observed deviations from ideal values (1 and 0, respectively) [42] [43].
- Bias Estimation: Use the regression equation to calculate the estimated bias at critical medical decision concentrations [42] [43].
Data Presentation and Performance Comparison
Key Regression Outputs for Bias Estimation
The table below summarizes the core parameters obtained from a linear regression analysis and their interpretation for bias estimation.
Table 1: Key Linear Regression Parameters for Characterizing Systematic Error
| Parameter | Symbol | Ideal Value | Indicates | Source of Error |
|---|---|---|---|---|
| Slope | b |
1.00 | Proportional Bias | Poor calibration, matrix effects [43] |
| Y-Intercept | a |
0.00 | Constant Bias | Inadequate blanking, interference [43] |
| Standard Error of Estimate | S~y/x~ |
As low as possible | Random Error around the line | Imprecision of both methods [43] |
| Correlation Coefficient | r |
> 0.975 | Adequate range for OLR | Inadequate sample range [45] |
Performance Comparison of Regression Methods
While OLR is simple and widely used, it operates under strict assumptions. Alternative regression models can be more appropriate when these assumptions are violated. The following table compares OLR with other common methods.
Table 2: Comparison of Regression Methods for Method Comparison Studies
| Method | Key Principle | Handles X-Error? | Assumption of Error Structure | Best Used When |
|---|---|---|---|---|
| Ordinary Linear Regression (OLR) | Minimizes vertical (Y) distance | No | Constant SD (Homoscedasticity) [45] | Reference method error is negligible (r ≥ 0.975) [45] |
| Weighted Least Squares (WLS) | Minimizes vertical distance with weights | No | Constant %CV (Heteroscedasticity) [45] | Error variance increases proportionally with concentration |
| Deming Regression | Minimizes both X and Y distances | Yes | Constant SD or %CV for both methods [45] | Both methods have comparable, non-negligible error |
| Passing-Bablok Regression | Non-parametric, based on medians | Yes | Makes no assumptions about distribution | Data contains outliers or is not normally distributed [45] |
The Scientist's Toolkit: Essential Reagents and Materials
A method comparison study requires both analytical reagents and statistical tools to yield reliable results.
Table 3: Research Reagent Solutions for Method Comparison Studies
| Item | Function | Example Application |
|---|---|---|
| Patient Samples | Provide a matrix-matched, commutable material covering the analytical range. | Core resource for the comparison experiment [42]. |
| Certified Reference Material | Used for calibration and to assign a "true" value to assess absolute bias. | Verifying the calibration of the comparative method. |
| Statistical Software | To perform regression calculations (OLR, Deming), generate plots, and compute confidence intervals. | Software like Analyse-it, RegressIt, or R packages [46] [42]. |
| Quality Control Materials | To monitor the stability and precision of both measurement methods during the study. | Ensuring methods remain in a state of statistical control. |
Critical Considerations and Limitations of Linear Regression
The application of OLR in method comparison studies comes with important caveats that researchers must acknowledge.
- Assumption of No Error in X: OLR assumes the comparative method (X-values) is without error. Violating this assumption, which is common, leads to a biased estimate of the slope, always attenuating it towards zero [45]. This is a fundamental weakness of OLR.
- Requirement for Linear Relationship: The model assumes the relationship between methods is linear across the entire measuring range. Non-linearity invalidates the model [43].
- Homoscedasticity: OLR assumes the random error (variance) is constant across all concentration levels. If the error increases with concentration (heteroscedasticity), OLR becomes inefficient and weighted techniques are preferable [45].
- Sensitivity to Outliers: A single outlier can disproportionately influence the slope and intercept estimates, leading to incorrect conclusions about bias [43].
The relationships between the regression line, the ideal line, and the types of bias are visualized below.
Given these limitations, Deming Regression is often recommended over OLR for most method comparison experiments, as it accounts for error in both methods and provides a more realistic and less biased estimate [45]. OLR should be reserved for cases where the comparative method is substantially more precise than the test method and the correlation is very high.
Linear regression is a powerful, accessible tool for the initial characterization of constant and proportional systematic error in method comparison studies. By carefully interpreting the slope and intercept, researchers can gain critical insights into the performance of a new test method. However, the limitations of ordinary linear regression, particularly its sensitivity to error in the comparative method, are significant. For robust and reliable results, scientists should validate the assumptions of OLR and strongly consider more advanced techniques like Deming or Passing-Bablok regression, which are better suited for the reality of laboratory data and provide a more objective comparison.
Establishing Limits of Agreement and Confidence Intervals
In method comparison studies, researchers and drug development professionals must quantitatively assess whether two measurement techniques can be used interchangeably for clinical or research purposes. The Bland-Altman analysis, introduced in 1983 and refined in subsequent publications, has become the standard methodological framework for assessing agreement between two quantitative measurement methods [33] [47]. This approach focuses on quantifying the systematic differences (bias) between methods and establishing limits within which most differences between measurements are expected to lie, providing a more clinically relevant assessment than traditional correlation coefficients alone [33]. Within the broader context of systematic error estimation research, Limits of Agreement (LoA) offer a practical framework for identifying and quantifying both fixed and proportional errors between measurement techniques, enabling researchers to make informed decisions about method interchangeability based on clinically acceptable difference thresholds [36].
The fundamental principle of Bland-Altman analysis lies in its focus on the differences between paired measurements rather than their correlation. While a high correlation coefficient might suggest a linear relationship between methods, it does not guarantee agreement, as two methods can be perfectly correlated yet consistently yield different values [33]. By estimating the range in which 95% of differences between measurement methods fall, LoA provide researchers with clinically interpretable metrics for assessing whether the disagreement between methods is sufficient to impact diagnostic or treatment decisions in practice [35] [36].
Methodological Approaches for Limits of Agreement
Core Mathematical Framework
The standard Bland-Altman model represents measurements using the framework $y{mi} = αm + μi + e{mi}$, where $y{mi}$ denotes the measurement by method $m$ on subject $i$, $αm$ represents the method-specific bias, $μi$ is the true subject value, and $e{mi}$ represents random error terms assumed to follow a normal distribution $N(0, σ_m^2)$ [48]. From this foundation, the Limits of Agreement are derived as:
LoA = Mean Difference ± 1.96 × Standard Deviation of Differences [33] [36]
The mean difference ($\bar{d}$) estimates the average bias between methods, while the standard deviation of differences ($s_d$) quantifies the random variation around this bias. The multiplication factor of 1.96 assumes that differences follow a normal distribution, encompassing 95% of expected differences between the two measurement methods [36]. For smaller sample sizes, some practitioners recommend replacing the 1.96 multiplier with the appropriate t-distribution value to account for additional uncertainty in estimating the standard deviation [48].
Comparative Analysis of LoA Methodologies
Table 1: Comparison of Limits of Agreement Methodological Approaches
| Method Type | Key Assumptions | Calculation Approach | Best Use Cases |
|---|---|---|---|
| Parametric (Conventional) | Differences are normally distributed; constant bias and variance across measurement range [36] | LoA = Mean difference ± 1.96 × SD of differences [36] | Ideal when normality and homoscedasticity assumptions are met |
| Nonparametric | No distributional assumptions; appropriate for non-normal data or outliers [49] [36] | LoA based on 2.5th and 97.5th percentiles of differences [36] | Small samples, non-normal differences, or presence of outliers |
| Regression-Based | Bias and/or variance change with measurement magnitude [36] | Separate regression models for mean differences and variability [36] | When heteroscedasticity is present (variance changes with magnitude) |
| Transformation-Based | Measurements require transformation to achieve additivity or constant variance [48] | Apply transformation (log, cube root), calculate LoA, then back-transform [48] | Percentage measurements, volume data, or when variance depends on mean |
The parametric approach remains the most widely implemented method but depends critically on the assumptions of normality and homoscedasticity (constant variance across the measurement range) [36]. The nonparametric alternative offers robustness when these assumptions are violated, defining LoA using the empirical 2.5th and 97.5th percentiles of the observed differences rather than parametric estimates [49] [36]. When variability between methods changes systematically with the magnitude of measurement (heteroscedasticity), the regression-based approach developed by Bland and Altman models both the mean difference and variability as functions of the measurement magnitude, producing LoA that vary appropriately across the measurement range [36]. For specific data types such as percentages, volumes, or concentrations, transformation-based methods can stabilize variance and produce more accurate agreement limits [48].
Confidence Interval Estimation for Limits of Agreement
Conceptual Foundation and Calculation Methods
While Limits of Agreement estimate the range containing 95% of differences between measurement methods, confidence intervals (CIs) quantify the precision of these estimates based on sample size and variability [50]. As with any statistical estimate derived from sample data, LoA are subject to sampling variability, and their CIs become particularly important when making inferences about population agreement based on limited data [50] [47].
The standard error for the Limits of Agreement is calculated as:
SE = $s_d \times \sqrt{1/n + 1.96^2/(2n-2)}$ [50] [48]
where $s_d$ represents the standard deviation of differences and $n$ is the sample size. For the 95% confidence level, the interval for each limit (upper and lower) is calculated as:
LoA ± t_{0.975, n-1} × SE
where $t_{0.975, n-1}$ is the 97.5th percentile of the t-distribution with $n-1$ degrees of freedom [50]. This calculation acknowledges that both the mean difference and standard deviation of differences are estimates with associated uncertainty that decreases with increasing sample size.
Advanced Approaches for Confidence Intervals
Several advanced methods have been developed to improve the accuracy of confidence intervals for Limits of Agreement:
MOVER (Method of Variance Estimates Recovery): This approach, recommended by recent methodological research, provides more accurate coverage probabilities for LoA CIs, particularly with smaller sample sizes [51] [47].
Exact methods based on non-central t-distribution: For situations where measurements can be considered exchangeable (mean difference equals zero), exact confidence limits can be derived from the χ²-distribution [48].
Bootstrap procedures: Nonparametric bootstrap methods can estimate CIs without distributional assumptions, making them particularly valuable for nonparametric LoA or when dealing with complex data structures [47].
Proper interpretation of LoA with their CIs requires that the maximum clinically acceptable difference (Δ) must lie outside the CI of the LoA to conclude agreement between methods [52] [36]. This conservative approach ensures that even considering estimation uncertainty, the methods demonstrate sufficient agreement for practical use.
Experimental Protocols and Implementation Guidelines
Sample Size Determination
Adequate sample size is crucial for precise estimation of Limits of Agreement and their confidence intervals. Method comparison studies typically require larger sample sizes than many other statistical comparisons due to the need to estimate both central tendency and variability parameters with sufficient precision [52].
The sample size calculation for a Bland-Altman study depends on several factors:
- Type I error (α): Typically set at 0.05 for a two-sided test
- Type II error (β): Commonly set at 0.20 or 0.10 (power of 80% or 90%)
- Expected mean of differences: Based on preliminary data or literature
- Expected standard deviation of differences: Based on preliminary data
- Maximum allowed difference between methods (Δ): The clinically acceptable difference [52]
For example, with an expected mean difference of 0.001167, standard deviation of differences of 0.001129, and maximum allowed difference of 0.004, a sample size of 83 achieves 80% power with a 5% α-level [52]. Software packages such as MedCalc implement the method by Lu et al. (2016) for sample size calculations specific to Bland-Altman analysis [52].
Protocol for Method Comparison Studies
Table 2: Key Methodological Steps in Bland-Altman Analysis
| Step | Procedure | Purpose | Common Pitfalls |
|---|---|---|---|
| Study Design | Collect paired measurements from subjects covering expected measurement range | Ensure representative sampling of population and measurement conditions | Limited range leads to poor generalizability |
| Data Collection | Measure each subject with both methods in random order or simultaneously | Minimize order effects and biological variation | Systematic measurement order introducing bias |
| Assumption Checking | Create Bland-Altman plot; assess normality (Q-Q plot) and homoscedasticity | Validate statistical assumptions underlying analysis | Proceeding with analysis when assumptions are violated |
| LoA Calculation | Compute mean difference and standard deviation of differences | Quantify bias and agreement limits | Using parametric methods when transformations are needed |
| CI Estimation | Calculate confidence intervals for bias and LoA | Quantify precision of agreement estimates | Ignoring CIs, especially with small sample sizes |
| Interpretation | Compare LoA and their CIs to clinically acceptable difference | Make decision about method interchangeability | Confusing statistical significance with clinical relevance |
A critical methodological consideration involves handling multiple measurements per subject. When study designs include repeated measurements from the same subjects, standard Bland-Altman approaches that ignore this clustering will underestimate variances and produce inappropriately narrow LoA and confidence intervals [53] [47]. Appropriate analytical methods for repeated measures include:
- Mixed-effects models: Account for within-subject correlation through random effects [53]
- Modified variance calculations: Incorporate between-subject and within-subject variance components [47]
- Generalized least squares: Accommodate correlated errors and unequal variances [51]
Visualization and Interpretation of Results
The Bland-Altman Plot
The Bland-Altman plot serves as the primary visualization tool for method comparison studies, providing a comprehensive graphical representation of agreement between two measurement methods [33] [35]. This scatterplot displays:
- X-axis: The average of the two measurements for each subject $(A+B)/2$
- Y-axis: The difference between the two measurements for each subject $(A-B)$
- Central line: The mean difference (bias) between methods
- Upper and lower lines: The Limits of Agreement (bias ± 1.96 × SD of differences)
- Optional additional lines: Confidence intervals for the mean difference and LoA [36]
Visual inspection of the Bland-Altman plot allows researchers to identify potential trends in the data, such as increasing variability with higher measurements (heteroscedasticity), systematic patterns in differences across the measurement range, or the presence of outliers that might unduly influence the agreement statistics [35] [36]. Some implementations also include a regression line of differences against averages to help detect proportional bias [36].
Interpretation Guidelines
Proper interpretation of Bland-Altman analysis requires both statistical and clinical reasoning:
- Assessing bias: The mean difference should be examined for statistical significance (whether its CI excludes zero) and clinical relevance (whether the magnitude would affect clinical decisions) [35]
- Evaluating LoA width: The range between upper and lower LoA should be compared to predefined clinically acceptable difference thresholds [36]
- Considering uncertainty: The confidence intervals for LoA should be examined, particularly in relation to the clinically acceptable difference [50] [47]
- Contextualizing findings: The practical implications of the observed agreement should be considered within the specific application context
For a method comparison to demonstrate sufficient agreement for interchangeable use, the predefined clinical agreement limit (Δ) should be larger than the upper confidence limit of the higher LoA, and -Δ should be smaller than the lower confidence limit of the lower LoA [52] [36]. This conservative approach ensures that even considering estimation uncertainty, the methods demonstrate acceptable agreement.
Advanced Applications and Alternative Approaches
Repeated Measures and Complex Designs
Traditional Bland-Altman methods assume independent paired measurements, but many study designs incorporate multiple measurements per subject across different conditions or time points [53] [47]. Ignoring this clustering leads to variance underestimation and inappropriately narrow LoA and confidence intervals [47]. Appropriate analytical approaches for repeated measures include:
- Mixed-effects models: Incorporate random subject effects to account for within-subject correlation [53]
- Variance component methods: Explicitly model between-subject and within-subject variance components [47]
- Generalized least squares: Accommodate various correlation structures and variance patterns [51]
Research indicates that failing to account for repeated measures can substantially underestimate the LoA and their confidence intervals, particularly when between-subject variability is high relative to within-subject variability [47].
Alternative Agreement Indices
While Limits of Agreement represent the most established method for assessing agreement, several alternative indices provide complementary information:
- Concordance Correlation Coefficient (CCC): Combasures both precision and accuracy relative to the line of identity [53]
- Total Deviation Index (TDI): Estimates a boundary that captures a specified proportion of differences between methods [53]
- Coverage Probability (CP): Calculates the probability that the absolute difference between methods falls within a pre-specified boundary [53]
- Coefficient of Individual Agreement (CIA): Accounts for both between-method and within-method variability when replicate measurements are available [53]
These alternative approaches can be implemented within the linear mixed model framework, allowing comprehensive assessment of agreement across different dimensions [53].
Transformation-Based Approaches
For specific measurement types, transformation-based LoA may provide more appropriate agreement assessments:
- Logarithmic transformations: Appropriate for ratio-based measurements, concentrations, or when variability increases with magnitude [48]
- Cube root transformations: Recommended for volume measurements or counts per unit volume based on dimensionality arguments [48]
- Logit transformations: Suitable for percentage measurements or proportional data bounded by 0 and 1 [48]
After calculating LoA on the transformed scale, results are back-transformed to the original measurement scale, producing agreement limits that may vary appropriately with the measurement magnitude [48].
The Researcher's Toolkit
Table 3: Essential Resources for Method Comparison Studies
| Tool Category | Specific Solutions | Key Functionality | Implementation Considerations |
|---|---|---|---|
| Statistical Software | MedCalc [52] [36] | Comprehensive Bland-Altman analysis with sample size calculation | Implements parametric, nonparametric, and regression-based methods |
| R Packages | SimplyAgree [51] | Tolerance limits, agreement analysis with correlated data | Flexible correlation structures, tolerance intervals |
| BivRegBLS [51] | Tolerance limits using bivariate least squares | Alternative to standard Bland-Altman approaches | |
| Methodological Approaches | MOVER CIs [51] [47] | Improved confidence interval calculation | More accurate coverage for LoA confidence intervals |
| Nonparametric bootstrap [47] | Confidence intervals without distributional assumptions | Useful for small samples or non-normal data | |
| Experimental Design | Repeated measures protocols [53] [47] | Accounting for within-subject correlation | Prevents underestimation of variances |
The researcher's toolkit for agreement studies continues to evolve, with recent methodological developments emphasizing tolerance intervals as an alternative to traditional Limits of Agreement [51]. Tolerance intervals incorporate both the uncertainty in the location and variance parameters, providing a more comprehensive assessment of where future observations are likely to fall [51]. From a practical implementation perspective, researchers should consider reporting the mean difference (bias) with its CI, the Limits of Agreement with their CIs, the standard deviation of differences, variance components when relevant, and clinical interpretation of the findings in relation to predefined acceptable difference thresholds [47].
Best Practices for Data Collection and Handling Paired Measurements
In method comparison experiments, paired measurements are a fundamental design where two measurements are collected from the same experimental unit or subject under different conditions [54] [55]. This approach is crucial for controlling for variability between subjects and providing more precise estimates of the difference between methods. The core principle involves treating the differences between paired observations as a single dataset for analysis [55]. Proper handling of these measurements is essential for accurate systematic error estimation, which quantifies consistent, predictable deviations from true values that can skew research conclusions [1] [28].
Systematic error, or bias, represents a consistent deviation from the true value and is a critical metrological characteristic in measurement procedures [28]. Unlike random error, which creates unpredictable variability, systematic error affects accuracy in a consistent direction, potentially leading to false conclusions about relationships between variables [1]. In pharmaceutical and clinical research, understanding and controlling systematic error is particularly important when comparing new measurement methods against established ones to determine if they can be used interchangeably [56].
Fundamentals of Paired Experimental Designs
Types of Paired Measurements
Paired measurements can be structured in several ways, each with specific applications in research settings:
Repeated Measures from Same Subject: The same subject is measured under two different conditions or time points (e.g., pre-test/post-test designs, before-and-after interventions) [54] [55]. This is common in clinical trials where patients serve as their own controls.
Matched Pairs: Different subjects are paired based on shared characteristics (e.g., age, gender, disease severity) to control for confounding variables [55]. This approach is valuable when repeated measures from the same subject are not feasible.
Natural Pairs: Inherently linked pairs (e.g., twins, paired organs, husband-wife pairs) where the natural relationship forms the basis for pairing [55].
Paired Comparisons: Used in preference testing or ranking studies where respondents compare pairs of options to determine overall preferences [57]. This method is particularly useful for subjective assessments where absolute measurements are not possible.
Key Assumptions for Valid Paired Analyses
For paired analyses to yield valid results, several assumptions must be met:
Independence of Subjects: Subjects must be independent, meaning measurements for one subject do not affect measurements for others [54].
Consistent Pairing: Each pair of measurements must be obtained from the same matched unit under the two conditions being compared [54].
Normality of Differences: The distribution of differences between paired measurements should be approximately normally distributed, particularly important for small sample sizes [54].
Table: Overview of Paired Measurement Types and Their Applications
| Pairing Type | Description | Common Research Applications |
|---|---|---|
| Repeated Measures | Same subject measured under two conditions | Clinical trials, intervention studies, method comparison |
| Matched Pairs | Different subjects paired by characteristics | Observational studies, case-control designs |
| Natural Pairs | Inherently linked subjects | Twin studies, paired organ research |
| Paired Comparisons | Forced-choice preference assessment | Product testing, preference ranking, survey research |
Systematic Error in Method Comparison Studies
Defining Systematic Error
Systematic error represents a consistent or proportional difference between observed values and the true values of what is being measured [1]. In contrast to random error, which creates unpredictable variability, systematic error skews measurements in a specific direction, affecting accuracy rather than precision [1] [4]. Systematic errors are generally more problematic than random errors in research because they can lead to false conclusions about relationships between variables, potentially resulting in Type I or II errors [1].
Systematic errors can be categorized into several types with distinct characteristics:
Offset Error: Also called additive or zero-setting error, this occurs when a measurement scale is not properly calibrated to zero, resulting in all measurements being shifted by a consistent amount [58] [4]. For example, a scale that consistently adds 15 pounds to each measurement demonstrates offset error [58].
Scale Factor Error: Known as multiplicative error, this involves measurements consistently differing from true values proportionally (e.g., by 10%) [58] [4]. A scale that repeatedly adds an extra 5% to all measurements would demonstrate scale factor error [58].
Source-Based Classification: Systematic errors can originate from various aspects of research:
- Instrument Error: Faulty equipment or imperfect measurement devices [58]
- Researcher Error: Physical limitations, carelessness, or improper use of instruments by researchers [58]
- Analysis Method Error: Flaws in experimental planning or analytical techniques [58]
- Response Bias: Research materials that prompt inauthentic responses through leading questions [1]
- Experimenter Drift: Deviations from standardized procedures due to fatigue or boredom over long periods [1]
- Sampling Bias: When some population members are more likely to be included in the study than others [1]
Estimating Systematic Error in Practice
In practical terms, systematic error is estimated as the mean of replicate results from a control or reference material minus the conventional true value of the quantity being measured [28]. Since the true value is generally unobtainable, researchers use conventional true values derived from:
- Assigned Values: Obtained with primary or reference measurement procedures [28]
- Consensus Values: Derived from external quality assessment schemes, calculated as the mean or median after outlier removal [28]
- Procedure-Defined Values: Specific to particular measurement protocols
Research comparing consensus values with reference measurement values has shown that consensus values may not always be appropriate for estimating systematic error, particularly for certain clinical measurements like cholesterol, triglycerides, and HDL-cholesterol [28]. This highlights the importance of using appropriate reference standards in method comparison studies.
Experimental Protocols for Paired Comparison Studies
Protocol Design Considerations
Well-designed protocols are essential for generating reliable paired comparison data. Key considerations include:
Sample Size Determination: Adequate sample size is crucial for detecting meaningful differences. For paired t-tests, sample size depends on the expected effect size, variability of differences, and desired statistical power [54].
Randomization Sequence: When order of treatment administration may influence results, randomizing the sequence of measurements helps control for order effects [1].
Blinding Procedures: Implementing single or double-blinding where possible prevents conscious or unconscious bias in measurement collection or interpretation [1].
Standardization of Procedures: Developing detailed, standardized protocols for measurement techniques, timing, and environmental conditions minimizes introduced variability [1].
Paired Testing Methodology
Paired testing, also known as auditing, provides an effective methodology for detecting systematic differences in treatment between groups [59]. This approach involves:
Matched Testers: Two testers are assigned comparable identities and qualifications, differing only in the characteristic being tested (e.g., race, disability status) [59].
Standardized Interactions: Testers undergo rigorous training to conduct themselves similarly during interactions, maintaining the same level of pursuit, questioning, and responsiveness [59].
Comprehensive Documentation: Testers systematically document each stage of their experience to capture subtle forms of differential treatment that might not be immediately apparent [59].
Appropriate Sampling: Tests should be conducted on a representative sample of units (jobs, rental housing) in the study area, with sufficient sample size to ensure conclusions are not attributable to chance [59].
Table: Key Elements of Paired Testing Protocol
| Protocol Element | Description | Purpose |
|---|---|---|
| Tester Matching | Creating comparable identities differing only in tested characteristic | Isolate effect of variable of interest |
| Standardized Training | Rigorous training to ensure consistent behavior | Minimize introduced variability |
| Blinded Interactions | Testers unaware of their paired counterpart | Prevent biased documentation |
| Systematic Documentation | Detailed recording of all interaction aspects | Capture subtle differential treatment |
| Representative Sampling | Tests conducted across representative sample | Ensure generalizable results |
Data Collection Best Practices
Pre-Collection Planning
Effective data collection begins with comprehensive planning:
Equipment Calibration: Regularly calibrate instruments using known standards to identify offset or scale factor errors [1] [58]. Document calibration procedures and results.
Pilot Testing: Conduct preliminary studies to identify potential sources of error and refine measurement protocols before full-scale data collection [1].
Staff Training: Standardize training for all personnel involved in data collection to minimize researcher-introduced variability [1] [59].
Environmental Control: Identify and control environmental factors that may influence measurements (e.g., temperature, time of day) [1].
During Collection Procedures
Implement these practices during active data collection:
Repeated Measurements: Take multiple measurements of the same quantity and use their average to increase precision and identify inconsistencies [1].
Real-Time Data Checking: Implement procedures to identify and address data quality issues as they occur, rather than after collection is complete.
Blinding Maintenance: Ensure that blinding procedures are maintained throughout data collection to prevent introduction of bias [1].
Documentation of Deviations: Record any deviations from planned protocols, along with possible implications for data quality.
Handling Paired Data Structure
Consistent Pair Identification: Maintain clear identifiers that link paired measurements throughout data collection and analysis [54] [55].
Simultaneous Recording: Record paired measurements in close temporal proximity when possible to minimize the effect of time-dependent confounding factors.
Difference Calculation: Compute differences between paired measurements consistently (e.g., always Measurement A - Measurement B) [54].
Statistical Analysis of Paired Measurements
The Paired t-Test Framework
The paired t-test is the primary statistical method for analyzing paired continuous measurements, testing whether the mean difference between pairs is zero [54]. The procedure involves:
Calculating Differences: For each pair, compute the difference between measurements ((di = x{i1} - x_{i2})) [54].
Computing Mean Difference: Calculate the average difference ((\overline{x_d})) across all pairs [54].
Standard Error of Differences: Determine the standard error of the differences: (SE = \frac{sd}{\sqrt{n}}), where (sd) is the standard deviation of differences and n is the sample size [54].
Test Statistic: Compute the t-statistic: (t = \frac{\overline{x_d}}{SE}) [54].
Comparison to Critical Value: Compare the calculated t-value to the critical value from the t-distribution with (n-1) degrees of freedom [54].
Assessing Agreement Between Methods
Beyond testing for significant differences, it's important to assess the agreement between measurement methods:
Bland-Altman Plots: Visualize differences between paired measurements against their means, displaying limits of agreement ((\pm 1.96 \times) standard deviation of differences) [56]. For repeated binary measurements, Bland-Altman diagrams can be adapted based on latent variables in generalized linear mixed models [56].
Intraclass Correlation Coefficient (ICC): Measures reliability or agreement for continuous data, useful for assessing consistency between methods [56].
Cohen's Kappa: For categorical data, assesses agreement between methods beyond what would be expected by chance [56]. For repeated measurements, this can be calculated based on latent variables in GLMMs [56].
Concordance Correlation Coefficient (CCC): Evaluates both precision and accuracy relative to the line of perfect concordance [56].
Handling Non-Normal Data
When the assumption of normally distributed differences is violated:
Nonparametric Alternatives: Use Wilcoxon signed-rank test for paired data when differences are not normally distributed, particularly with small sample sizes [54].
Data Transformation: Apply appropriate transformations (e.g., logarithmic) to achieve normality when possible.
Bootstrap Methods: Implement resampling techniques to generate confidence intervals without distributional assumptions.
Table: Statistical Methods for Analyzing Paired Measurements
| Method | Data Type | Purpose | Key Assumptions |
|---|---|---|---|
| Paired t-test | Continuous | Test if mean difference equals zero | Normality of differences |
| Wilcoxon Signed-Rank | Continuous/Ordinal | Nonparametric alternative to paired t-test | Symmetric distribution of differences |
| Bland-Altman Plot | Continuous | Visualize agreement between methods | No relationship between difference and mean |
| Cohen's Kappa | Categorical | Chance-corrected agreement | Independence of ratings |
| Intraclass Correlation | Continuous | Reliability assessment | Normally distributed components |
The Researcher's Toolkit: Essential Materials and Solutions
Statistical Software and Tools
JMP Statistical Software: Provides comprehensive functionality for paired t-tests and visualization of paired data, including assumption checking and descriptive statistics [54].
R Statistical Environment: Offers extensive packages for analyzing paired data, including ggplot2 for Bland-Altman plots, irr for agreement statistics, and lme4 for mixed models appropriate for repeated paired measurements [56].
OpinionX: Specialized tool for paired comparison studies, particularly useful for preference ranking and survey-based paired data, featuring win rate calculations and segmentation analysis [57].
Generalized Linear Mixed Models (GLMM) Frameworks: Essential for analyzing paired repeated binary measurements impacted by both measuring methods and raters, allowing incorporation of multiple sources of fixed and random effects [56].
Reference Materials and Controls
Certified Reference Materials: Substances with one or more properties that are sufficiently homogeneous and well-established to be used for instrument calibration or method validation [28].
Control Materials with Assigned Values: Materials with values assigned by reference measurement procedures, essential for accurate estimation of systematic error [28].
Quality Control Samples: Materials used to monitor the stability of measurement procedures over time, helping to detect shifts in systematic error.
Documentation and Reporting Tools
Standardized Data Collection Forms: Pre-designed forms that ensure consistent recording of paired measurements and relevant covariates.
Electronic Laboratory Notebooks: Digital systems for recording experimental details, protocols, and results in a searchable, secure format.
Data Validation Scripts: Automated checks for data quality, including identification of outliers, missing data patterns, and violations of statistical assumptions.
Proper data collection and handling of paired measurements requires meticulous attention to both theoretical principles and practical implementation. By understanding the sources and types of systematic error, implementing robust experimental protocols, applying appropriate statistical analyses, and utilizing essential research tools, scientists can generate reliable evidence from method comparison studies. The practices outlined in this guide provide a framework for producing valid, reproducible results in pharmaceutical research and development, ultimately supporting the development of accurate measurement methods and informed decision-making in drug development.
Troubleshooting Systematic Error: Detection, Correction, and Quality Control
Procedures for Detecting Bias Using Control Samples and Method Comparison
Systematic error, or bias, is a fundamental metrological characteristic of any measurement procedure, with a direct impact on the interpretation of clinical laboratory results and drug development data [28]. In method comparison experiments, bias represents a consistent deviation between a test method and a comparative or reference method, potentially leading to inaccurate medical decisions or flawed research conclusions. Estimating systematic error typically involves calculating the mean of replicate results from a control or reference material minus the material's true value [28]. Since a true value is inherently unobtainable, practitioners rely on conventional true values derived from primary reference methods, assigned values, or consensus values from external quality assessment schemes.
This guide objectively compares established procedures for detecting bias across laboratory medicine and analytical science, providing researchers with structured methodologies for evaluating measurement system performance. The comparative analysis focuses on practical implementation, statistical rigor, and applicability to various research contexts, from traditional clinical chemistry to modern computational approaches.
Comparative Analysis of Bias Detection Procedures
Table 1: Comparison of Major Bias Detection Procedures
| Procedure | Primary Application Context | Key Strengths | Statistical Foundation | Sample Requirements |
|---|---|---|---|---|
| TEAMM (Trend Exponentially Adjusted Moving Mean) | Continuous monitoring of analytic bias using patient samples [60] | Superior sensitivity for all bias levels; quantifies medical damage via ULMU [60] | Generalized algorithm unifying Bull's algorithm and average of normals [60] | Patient samples; optimized N and P parameters [60] |
| Comparison of Methods Experiment | Method validation for systematic error estimation [7] | Estimates constant and proportional error; uses real patient specimens [7] | Linear regression; difference plots; Bland-Altman analysis [7] [29] | 40+ patient specimens covering working range [7] |
| Control Material with Assigned Values | Estimating systematic error of measurement procedures [28] | Direct metrological traceability; eliminates consensus value limitations [28] | Mean difference from conventional true value; Bland-Altman plots [28] | Control materials with reference measurement procedure values [28] |
| Bland-Altman Method | Assessing agreement between two measurement methods [29] | Standard approach for method comparison; visualizes differences across measurements [29] | Difference plots with limits of agreement; response to criticisms addressed [29] | Paired measurements from two methods [29] |
| Unsupervised Bias Detection (HBAC) | AI system fairness auditing without protected attributes [61] | Detects complex, intersectional bias; model-agnostic; privacy-preserving [61] | Hierarchical Bias-Aware Clustering; statistical hypothesis testing [61] | Tabular data with user-defined bias variable [61] |
Table 2: Performance Indicators and Implementation Requirements
| Procedure | Optimal Bias Detection Capability | Implementation Complexity | Data Analysis Requirements | Regulatory Compliance Support |
|---|---|---|---|---|
| TEAMM | Optimized for all bias levels [60] | Moderate (parameter optimization needed) [60] | Computer simulation; ULMU calculation [60] | Not specified |
| Comparison of Methods | Constant and proportional systematic errors [7] | Moderate (experimental design critical) [7] | Linear regression; difference plots; correlation analysis [7] | Method validation guidelines [7] |
| Control Material with Assigned Values | Metrological traceability to reference standards [28] | Low to moderate (depends on material availability) [28] | Difference analysis; linear regression against reference values [28] | Proficiency testing standards [28] |
| Bland-Altman Method | Agreement assessment with clinical relevance [29] | Low (standard statistical software) [29] | Difference calculations; agreement limits [29] | Widely accepted in medical literature [29] |
| Unsupervised Bias Detection (HBAC) | Complex bias patterns without predefined groups [61] | High (computational clustering algorithms) [61] | Cluster analysis; statistical hypothesis testing with Bonferroni correction [61] | Emerging AI auditing frameworks [61] |
Detailed Experimental Protocols
Comparison of Methods Experiment Protocol
The comparison of methods experiment represents a cornerstone procedure for estimating systematic error between a new test method and an established comparative method [7]. This protocol requires meticulous execution across multiple phases:
Experimental Design Phase: Select a minimum of 40 different patient specimens carefully chosen to cover the entire working range of the method and represent the spectrum of diseases expected in routine application [7]. Specimens should be analyzed within two hours of each other by both methods to prevent stability issues from affecting results. The experiment should extend across multiple runs on different days, with a minimum of 5 days recommended to minimize systematic errors that might occur in a single run [7].
Data Collection Phase: Analyze each specimen by both test and comparative methods. While common practice uses single measurements, duplicate measurements provide advantages for identifying sample mix-ups, transposition errors, and other mistakes [7]. If duplicates are not performed, immediately inspect comparison results as they are collected, identify specimens with large differences, and repeat analyses while specimens remain available.
Statistical Analysis Phase:
- Graph the data using difference plots (test minus comparative results versus comparative result) for methods expected to show one-to-one agreement, or comparison plots (test result versus comparative result) for methods with different measurement principles [7].
- Calculate linear regression statistics (slope, y-intercept, standard deviation about the regression line sy/x) for data covering a wide analytical range.
- Estimate systematic error (SE) at medical decision concentrations (Xc) using: Yc = a + bXc, then SE = Yc - Xc [7].
- For narrow analytical ranges, calculate the average difference (bias) between methods using paired t-test calculations [7].
Method Comparison Experimental Workflow
Control Material with Assigned Values Protocol
This procedure estimates systematic error using control materials with conventional true values, providing a fundamental approach for quantifying measurement procedure bias [28]:
Material Selection: Obtain control materials with values assigned through reference measurement procedures rather than consensus values. Studies demonstrate that consensus values from external quality assessment schemes may show significant constant and proportional differences compared to reference measurement values, particularly for lipid quantities including cholesterol, triglycerides, and HDL-cholesterol [28].
Experimental Execution: Perform replicate measurements of the control material using the test measurement procedure under validation. The number of replicates should provide sufficient statistical power to detect clinically significant bias, typically 20 measurements across multiple runs [28].
Systematic Error Calculation: Calculate the mean of replicate results and subtract the conventional true value of the control material: Systematic Error = Meanreplicates - Conventional True Value [28]. This estimate can be further validated through comparison with peer group means from proficiency testing programs, though results indicate that consensus values may not adequately substitute for reference measurement procedure values [28].
Statistical Analysis: Utilize Bland-Altman plots to visualize differences between method results and assess agreement [28]. For materials with multiple assigned values, apply linear regression analysis to evaluate constant and proportional differences between conventional true value types [28].
Unsupervised Bias Detection Protocol
For AI systems and complex computational models, the Hierarchical Bias-Aware Clustering (HBAC) algorithm provides a sophisticated approach for detecting bias without predefined protected attributes [61]:
Data Preparation: Prepare tabular data with uniform data types across all columns except the bias variable. Define a bias variable column representing the performance metric of interest (e.g., error rate, accuracy, selection rate) [61].
Parameter Configuration: Set hyperparameters including iterations (how often data can be split into smaller clusters, default=3) and minimal cluster size (default=1% of dataset rows) [61]. Define bias variable interpretation direction (whether higher or lower values indicate better performance).
Algorithm Execution:
- Split dataset into training and test subsets (80-20 ratio) [61].
- Apply HBAC to training data: iteratively split clusters using k-means (numerical data) or k-modes (categorical data), selecting clusters with highest standard deviation in bias variable [61].
- Save cluster centroids and assign cluster labels to test dataset.
- Perform statistical hypothesis testing using one-sided Z-test to compare bias variable means between the most deviating cluster and remainder of dataset [61].
- If significant difference detected, examine feature differences using t-tests (numerical) or χ² tests (categorical) with Bonferroni correction for multiple comparisons [61].
Result Interpretation: The tool generates a bias analysis report highlighting clusters with statistically significant deviations in the bias variable, serving as starting points for expert investigation of potentially unfair treatment patterns [61].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Bias Detection Experiments
| Tool/Reagent | Function in Bias Detection | Application Context | Implementation Considerations |
|---|---|---|---|
| Reference Control Materials | Provides conventional true value for systematic error estimation [28] | Control material-based bias estimation | Prefer materials with values assigned by reference measurement procedures [28] |
| Patient Specimens | Enables method comparison using real clinical samples [7] | Comparison of methods experiments | Select 40+ specimens covering analytical range and disease spectrum [7] |
| Hierarchical Bias-Aware Clustering (HBAC) | Identifies biased performance clusters without protected attributes [61] | AI system fairness auditing | Open-source Python package: unsupervised-bias-detection [61] |
| Bland-Altman Analysis | Assesses agreement between two measurement methods [29] | Method comparison studies | Widely accepted standard approach with available statistical implementations [29] |
| Linear Regression Statistics | Quantifies constant and proportional systematic errors [7] | Data analysis for method comparisons | Calculate slope, intercept, sy/x; estimate SE at decision levels [7] |
| TEAMM Algorithm | Continuous monitoring of analytic bias using patient data [60] | Quality control in clinical laboratories | Optimized parameters (N and P) for different bias levels [60] |
Method Selection Framework
Bias Detection Method Selection Guide
Systematic error detection remains a critical component of method validation across diverse scientific disciplines, from traditional clinical chemistry to emerging AI technologies. The procedures detailed in this guide provide researchers with validated methodologies for quantifying bias, each with distinct strengths and appropriate application contexts. Control material approaches offer metrological traceability, comparison of methods experiments reflect real-world performance with patient samples, and unsupervised detection methods identify complex bias patterns in computational systems. By selecting the appropriate procedure based on measurement context, available resources, and performance requirements, researchers can ensure the reliability and fairness of their analytical systems, ultimately supporting accurate scientific conclusions and equitable technological applications.
Applying Westgard Rules and Levey-Jennings Plots for Ongoing Quality Control
In the realm of clinical laboratory science and analytical research, ensuring the accuracy and reliability of measurement systems is paramount. The framework of statistical quality control (SQC), primarily implemented through Levey-Jennings plots and Westgard Rules, provides a systematic approach for monitoring analytical performance and detecting systematic errors during routine operation. These tools serve as the frontline defense against the release of erroneous results, forming a critical component of a broader quality management system. Within the context of method comparison experiments, SQC provides the necessary ongoing verification that the analytical process remains stable and that the performance characteristics estimated during initial method validation persist over time. This article objectively compares the application of these SQC tools, supported by experimental data, to guide researchers and scientists in selecting appropriate error-detection strategies for their specific analytical processes.
Core Concepts: Levey-Jennings Plots and Westgard Rules
The Levey-Jennings Plot: Visualizing Process Behavior
The Levey-Jennings plot is a visual graph that plots quality control data over time, showing how results deviate from the established mean [62]. It is an adaptation of Shewhart control charts for the clinical laboratory setting. Control limits, typically set at the mean ±1s, ±2s, and ±3s (where "s" is the standard deviation of the control measurements), are drawn on the chart [63]. The plot provides a running record of method performance, allowing for visual inspection of trends, shifts, and the scatter of control data.
Westgard Rules: A Multi-Rule Decision Framework
Westgard Rules are a set of statistical decision criteria used to determine whether an analytical run is in-control or out-of-control [63]. They are designed to be used together in a multi-rule procedure that maximizes error detection (the ability to identify problematic runs) while minimizing false rejections (unnecessarily rejecting good runs) [63]. The rules are defined using a shorthand notation:
- 1
2s(Warning Rule): A single control measurement exceeds the mean ±2s. This triggers inspection by the rejection rules but does not, by itself, reject the run [63]. - 1
3s(Rejection Rule): A single control measurement exceeds the mean ±3s. This indicates a high probability of error and rejects the run [63]. - 2
2s(Rejection Rule): Two consecutive control measurements exceed the same mean ±2s limit. This detects systematic error [63]. - R
4s(Rejection Rule): One control measurement exceeds the mean +2s and another exceeds the mean -2s within the same run. This detects random error [63]. - 4
1s(Rejection Rule): Four consecutive control measurements exceed the same mean ±1s limit. This detects systematic error and is typically applied across runs and materials [63]. - 10
x(Rejection Rule): Ten consecutive control measurements fall on one side of the mean. This detects systematic error [63].
The following workflow diagram illustrates how these rules are typically applied in practice to evaluate a quality control run.
Experimental Comparison of QC Rule Performance
Methodology for Assessing QC Rule Performance
The performance of different QC rule sets can be evaluated experimentally by implementing them in a laboratory setting and monitoring outcomes over time. A typical study design involves:
- Instrumentation and Analytes: Studies are performed on specific analytical platforms (e.g., a nephelometer for immunological parameters) [64].
- Phased Implementation: The study is divided into distinct phases (e.g., A, B, C, D), each utilizing a different set of QC rules for the same tests [64].
- Performance Metrics: Key metrics are tracked throughout the study, including the coefficient of variation (CV%) for imprecision, bias (%) for inaccuracy, and the analytical Sigma-metric, which combines both to give a holistic view of method performance [64].
- Error Detection Capability: The effectiveness of a QC procedure is quantified by its probability of error detection (Pᵉᵈ), or the likelihood that it will detect a clinically significant error. This is often balanced against its probability of false rejection (Pᶠʳ), which is the chance of rejecting an in-control run [65].
Comparative Experimental Data
A 2024 study by Cristelli et al. provides direct experimental data comparing the performance of different Westgard rule combinations for five immunological parameters [64]. The study implemented rule changes in phases, as detailed in the table below.
Table 1: Experimental Phases and QC Rule Configurations from Cristelli et al. (2024)
| Test | Phase A (Old Rules) | Phase B (New Rules) | Phase C (Adjusted Rules) | Phase D (Final Rules) |
|---|---|---|---|---|
| IgA | 13s/R4s/22s |
13s/22s |
13s/22s/R4s/41s |
13s |
| AAT | 13s/R4s/22s |
13s/22s/R4s/41s/10x |
13s/22s/R4s/41s/10x |
13s/23s/R4s/31s/12x |
| Prealbumin | 13s/R4s/22s |
13s/22s/R4s/41s/10x |
13s/22s/R4s/41s/8x |
13s/22s/R4s/41s/8x |
| Lp(a) | 13s/R4s/22s |
13s/22s/R4s/41s/10x |
13s/22s/R4s/41s |
13s/22s/R4s/41s/10x |
| Ceruloplasmin | 13s/R4s/22s |
13s/22s/R4s/41s/10x |
13s/22s/R4s/41s/8x |
13s/23s/R4s/31s/12x |
Source: Adapted from Cristelli et al. [64]
The analytical performance of the methods, measured by the Sigma-metric, was tracked across these phases. The results are summarized below.
Table 2: Analytical Performance Metrics (Phase D) from Cristelli et al. (2024)
| Test | CV (%) | Bias (%) | Sigma Metric |
|---|---|---|---|
| IgA | 2.55 | -1.09 | 5.33 |
| AAT | 3.88 | -2.21 | 3.25 |
| Prealbumin | 3.99 | -0.14 | 2.95 |
| Lp(a) | 8.02 | -0.34 | 3.81 |
| Ceruloplasmin | 2.48 | -3.65 | 3.49 |
Source: Adapted from Cristelli et al. [64]
A critical finding of the study was that implementing more complex, "newly suggested rejection rules... did not observe an improvement in monitoring of analytical performance" when viewed through the lens of the Sigma metric [64]. The authors noted inhomogeneous changes in Sigma values, with some parameters improving and others declining, suggesting that changing QC rules alone does not directly improve the inherent stability of the analytical method.
Analysis of Error Detection Performance
A follow-up commentary on the Cristelli et al. study provided a crucial clarification and different perspective on evaluating QC performance. The authors argued that the purpose of QC rules is not to improve method precision or accuracy (the Sigma metric), but to improve the detection of errors when the method becomes unstable [65].
The commentary provided a quantitative analysis of error detection, demonstrating that for the AAT test, the Westgard Advisor's recommendation to change rules from Phase A (13s/22s/R4s) to Phase B (13s/22s/R4s/41s/10x) increased the probability of error detection (Pᵉᵈ) from 15% to 69% [65]. This change came with a minor trade-off, increasing the probability of false rejection (Pᶠʳ) from 1% to 3%. This data highlights the primary function of more complex multi-rule procedures: to significantly enhance the ability to detect out-of-control conditions, thereby preventing the release of unreliable patient results.
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of a QC strategy requires specific materials and tools. The following table details key components of a robust QC system.
Table 3: Essential Research Reagent Solutions for Quality Control
| Item | Function in QC |
|---|---|
| Third-Party Control Materials | Commercially available control materials independent of instrument manufacturers. Used to monitor performance without potential conflicts of interest and to validate manufacturer claims [66]. |
| Stable Control Products | Liquid or lyophilized materials with a known and stable analyte concentration and a long expiration date. They are used to establish a stable baseline (mean and SD) for the Levey-Jennings chart [67]. |
| Statistical QC Software / LIS | A Laboratory Information System (LIS) or dedicated software that automates data capture, plots Levey-Jennings charts, applies Westgard Rules, and provides real-time alerts for rule violations [62]. |
| Proficiency Testing (PT) Samples | Samples provided by an external program for external quality assessment (EQA). Labs analyze PT samples to compare their performance against peers and reference methods, providing an external check on accuracy [62]. |
| Calibrators and Reference Materials | Materials used to standardize the analytical instrument. Their traceability to higher-order standards is critical for minimizing systematic error (bias) in the measurement process [66]. |
Protocol for Implementing a Multi-Rule QC Procedure
For researchers aiming to implement a Westgard Rules-based QC system, the following step-by-step protocol is recommended.
- Establish a Baseline: For a new control material, analyze it over a minimum of 20 days to establish a robust mean and standard deviation (s). Assay the new lot in parallel with the old lot if possible [67].
- Construct the Levey-Jennings Chart: Create a control chart with the concentration on the y-axis and time/run number on the x-axis. Draw lines at the mean, mean ±1s, mean ±2s, and mean ±3s [63].
- Define the QC Procedure: Select the appropriate Westgard Rules based on the quality required for the test and the method's Sigma performance. For a method with a Sigma ≥6, a simple 1
3srule may suffice, while a method with a Sigma of 3-4 will likely require a full multi-rule procedure [66]. - Execute the QC Workflow: For each run, after analyzing the control materials and plotting the data, follow the logical workflow as shown in the diagram above: use the 1
2sas a warning to trigger the application of the stricter rejection rules (13s, 22s, R4s, etc.) [63]. - Respond to Violations: If a rejection rule is violated, reject the analytical run. Do not report patient results. Troubleshoot the process, identify and correct the root cause, document all actions, and then re-analyze the patient samples [67].
- Maintain the System: Exclude all control data from rejected runs when updating the mean and SD statistics. Regularly review QC data for trends and participate in EQA programs to ensure ongoing accuracy [67].
Levey-Jennings plots and Westgard Rules constitute a powerful, synergistic system for ongoing quality control. The experimental data demonstrates that while the choice of specific rules does not directly improve a method's inherent Sigma performance, it has a profound impact on the system's ability to detect errors. Simpler rule sets offer ease of use but may allow a significant number of erroneous runs to go undetected. In contrast, more complex multi-rule procedures, while slightly increasing the false rejection rate, dramatically enhance error detection, thereby safeguarding the integrity of reported results. The optimal configuration is not universal; it must be tailored to the analytical performance of each method and the clinical requirements of each test. For researchers engaged in method comparison, this SQC framework provides the essential ongoing data needed to confirm that the systematic errors estimated during validation remain controlled, ensuring the long-term reliability of the analytical process.
In scientific research and method comparison experiments, measurement error is an unavoidable reality. This error consists of two primary components: random error, which is unpredictable and follows a Gaussian distribution, and systematic error (bias), which consistently skews results in one direction [9]. Unlike random error, which can be reduced through repeated measurements, systematic error is reproducible and cannot be eliminated by replication alone [9]. This persistent nature makes bias particularly dangerous for clinical decision-making and research validity, necessitating robust correction strategies [9].
Calibration and recovery experiments represent two fundamental approaches for identifying, quantifying, and correcting systematic errors. These methodologies are essential components of a comprehensive validity argument in scientific measurement, enabling researchers to distinguish between more and less valid measurement methods [68]. Within the broader thesis of systematic error estimation, these strategies provide frameworks for validating measurements of latent variables that can be externally manipulated, moving beyond traditional multi-trait multi-matrix (MTMM) approaches that require unrelated latent variables and conceptually different methods [68] [69].
Theoretical Foundations of Calibration Experiments
Conceptual Framework
Experiment-based calibration is a validation strategy wherein researchers generate well-defined values of a latent variable through standardized experimental manipulations, then evaluate measurement methods by how accurately they reproduce these known values [69]. This approach is formalized through the concept of retrodictive validity: the correlation between intended standard scores of a latent variable (S) and actually measured scores (Y) [69]. The theoretical model accounts for both experimental aberration (ω), representing deviations between intended and truly achieved latent variable scores, and measurement error (ε), representing noise in the measurement process itself [69].
The calibration framework can be represented through the following logical relationships:
Figure 1: Theoretical model of experiment-based calibration showing relationships between standard scores, true scores, measured scores, experimental aberration, and measurement error.
Retrodictive Validity
The core metric in calibration experiments, retrodictive validity (ρSY), quantifies how well measured scores correlate with standard scores generated through experimental manipulation [69]. This correlation serves as a complementary validity index that avoids limitations of classical psychometric indices, particularly in experimental contexts where between-person variability is minimized by design [69]. From a statistical estimation perspective, the accuracy of retrodictive validity estimators depends critically on design features, particularly the distribution of standard values (S) and the nature of experimental aberration (ω) [69].
Recovery Experiments: Methodology and Applications
Fundamental Principles
Recovery experiments represent a classical technique for validating analytical method performance by estimating proportional systematic error - error whose magnitude increases as the concentration of the analyte increases [70]. This type of error often occurs when a substance in the sample matrix reacts with the target analyte, competing with the analytical reagent [70]. The experimental workflow involves preparing paired test samples and calculating the percentage of a known added amount of analyte that the method can recover [70].
The following diagram illustrates the standardized workflow for conducting recovery experiments:
Figure 2: Experimental workflow for recovery experiments showing preparation of test and control samples followed by analysis and recovery calculation.
Experimental Protocol
The recovery experiment protocol requires careful execution with attention to critical factors [70]:
Sample Preparation: Prepare paired test samples using patient specimens containing the native analyte. Add a small volume of standard solution containing known analyte concentration to the first test sample (Test Sample A). Add an equivalent volume of pure solvent to the second test sample (Control Sample B) to maintain identical dilution effects.
Volume Considerations: The volume of standard added should be small relative to the original patient specimen (recommended ≤10% dilution) to minimize dilution of the original specimen matrix, which could alter error characteristics.
Pipetting Accuracy: Use high-quality pipettes with careful attention to cleaning, filling, and delivery time, as pipetting accuracy is critical for calculating the exact concentration of analyte added.
Analyte Concentration: The amount of analyte added should reach clinically relevant decision levels. For example, with glucose reference values of 70-110 mg/dL, adding 50 mg/dL raises concentrations to 120-160 mg/dL, covering medically critical interpretation ranges.
Replication: Perform duplicate or triplicate measurements to account for random error, with the systematic error estimated from differences in average values.
Data Calculation and Interpretation
The data analysis follows a systematic procedure [70]:
- Tabulate results for all pairs of test and control samples
- Calculate average values for replicates
- Determine the difference between test and control samples
- Compute the average difference across all specimens tested
- Calculate percent recovery using the formula:
The observed recovery percentage indicates method performance, with comparisons made against predefined acceptability criteria based on clinical requirements or regulatory standards.
Interference Experiments for Constant Systematic Error
Conceptual Basis
Interference experiments estimate constant systematic error caused by substances other than the analyte that may be present in the specimen being analyzed [70]. Unlike proportional error, constant systematic error remains relatively consistent regardless of analyte concentration, though it may change with varying concentrations of the interfering material [70]. These experiments are particularly valuable when comparison methods are unavailable and supplement error estimates from method comparison studies [70].
Experimental Protocol
The interference experiment methodology shares similarities with recovery experiments but differs in critical aspects [70]:
Sample Preparation: Prepare paired test samples using patient specimens. Add a solution containing the suspected interfering material to the first test sample. Add an equivalent volume of pure solvent or diluting solution to the second test sample.
Interferer Selection: Test substances selected based on manufacturer's claims, literature reports, and common interferers including bilirubin, hemolysis, lipemia, preservatives, and anticoagulants used in specimen collection.
Interferer Concentration: The amount of interferer added should achieve distinctly elevated levels, preferably near the maximum concentration expected in the patient population.
Specific Testing Methods:
- Bilirubin: Add standard bilirubin solution
- Hemolysis: Compare aliquots before and after mechanical hemolysis or freeze-thaw cycles
- Lipemia: Add commercial fat emulsions or compare lipemic specimens before and after ultracentrifugation
- Additives: Compare samples collected in tubes with different additives
Data Analysis
The interference data analysis follows this procedure [70]:
- Tabulate replicate results for all pairs of samples
- Calculate average values for replicates
- Determine differences between samples with and without interferent
- Compute the average difference across all specimens
The judgment on acceptability compares the observed systematic error with clinically allowable error based on proficiency testing criteria or clinical requirements.
Comparative Analysis: Calibration vs. Recovery Approaches
The table below provides a structured comparison of calibration and recovery experiments for bias correction:
Table 1: Comprehensive comparison of calibration and recovery experiments for systematic error correction
| Feature | Calibration Experiments | Recovery Experiments |
|---|---|---|
| Primary Objective | Establish retrodictive validity through correlation of standard and measured scores [69] | Estimate proportional systematic error by measuring recovery of known analyte additions [70] |
| Error Type Addressed | General measurement inaccuracy, experimental aberration [69] | Proportional systematic error (magnitude increases with analyte concentration) [70] |
| Experimental Design | Generation of standard scores through controlled manipulation of latent variables [69] | Paired samples: test specimens with analyte additions and controls with solvent additions [70] |
| Key Metrics | Retrodictive validity (ρSY), estimator variance [69] | Percent recovery, difference between test and control measurements [70] |
| Data Analysis Approach | Correlation analysis, variance estimation of retrodictive validity estimators [69] | Difference testing, paired t-test statistics [70] |
| Sample Requirements | Multiple standard values with optimal distribution properties [69] | Patient specimens or pools with native analyte [70] |
| Advantages | Does not require unrelated latent variables; enables optimization of measurement evaluation [68] | Can be performed quickly for specific error sources; applicable when comparison methods unavailable [70] |
| Limitations | Requires experimental manipulation of latent variable; domain-specific implementation challenges [69] | Requires careful pipetting; limited to analy |
Addressing Differential and Non-Classical Measurement Error Scenarios
In method comparison experiments, the accurate estimation of systematic error is fundamental to ensuring the reliability of scientific data. Measurement error, the difference between a measured value and its true value, is an unavoidable aspect of all empirical research [71]. These errors are broadly categorized as either random error, which are statistical fluctuations that occur in any measurement system, or systematic error (bias), which are reproducible inaccuracies that consistently skew results in the same direction [71] [9]. While random error can be reduced by averaging repeated measurements, systematic error cannot be eliminated through repetition and often requires corrective action such as calibration [9]. This guide focuses on the more complex and problematic scenarios of differential and non-classical measurement error, providing researchers with protocols for their detection, quantification, and adjustment within method comparison studies.
The impact of unaddressed measurement error is profound. It can introduce bias into estimated associations, reduce statistical power, and coarsen observed relationships, potentially leading to incorrect conclusions in everything from clinical diagnostics to epidemiological studies [72]. In laboratory medicine, for instance, systematic error can jeopardize patient health by skewing test results in a manner that affects clinical decision-making [9]. Understanding and correcting for these errors is therefore not merely a statistical exercise but a core component of research integrity and validity.
Defining Error Scenarios: From Classical to Non-Classical
Classical and Berkson Error Models
Most standard correction methods are built upon a foundation of classical measurement error assumptions. The classical measurement error model posits that a measured value (X^) varies randomly around the true value (X) according to the equation (X^ = X + UX), where the error (UX) is normally distributed with a mean of zero and is independent of the true value (X) [72] [73]. This type of error is assumed in many laboratory and objective clinical measurements, such as serum cholesterol or blood pressure [73]. A key characteristic of classical error is that it increases the variability of the measured variable but does not introduce a systematic bias in the mean; the measurement is unbiased at the individual level.
The Berkson error model, in contrast, describes a different scenario. It is often applicable in controlled exposures, such as clinical trials or environmental studies, where the measured value (X^) is fixed (e.g., a prescribed dose or an ambient pollution level), and the true individual exposure (X) varies around this fixed value: (X = X^ + UX) [72] [73]. Here, the error (UX) is again independent of the measured value (X^*). Unlike classical error, Berkson error in an exposure does not typically bias the estimated association coefficient but instead increases the imprecision of the estimate, widening confidence intervals [72].
Differential and Non-Classical Measurement Error
The situation becomes more complex and problematic with differential and non-classical errors. Differential error exists when the measurement error in one variable is related to the value of another variable, most critically, the outcome of interest [72] [73]. In statistical terms, the error in the measured exposure (X^*) provides extra information about the outcome (Y) beyond what is provided by the true exposure (X) and other covariates. This is a common threat in case-control or cross-sectional studies where knowledge of the outcome status can influence the recall or measurement of the exposure [72]. For example, a patient with a disease might recall past exposures differently (recall bias) than a healthy control.
Non-classical measurement error is a broader term that encompasses differential error and any other error that violates the assumptions of the classical model [74]. This includes errors that are correlated with the true value (e.g., over-reporting of occupation prestige), correlated with other variables in the model, or correlated with errors in other measurements (dependent error) [72] [74]. A specific example of dependent error is "same-source bias," where two variables (e.g., opioid use and antiretroviral adherence) are both assessed via a single phone interview, and the errors in reporting are correlated due to factors like stigma or cognitive effects [72].
Table 1: Comparison of Key Measurement Error Types and Their Impacts.
| Error Type | Formal Definition | Primary Cause | Impact on Association Estimates |
|---|---|---|---|
| Classical Error | (X^* = X + UX), (UX) independent of (X) | Random fluctuations in measurement process | Attenuates effect estimates (bias towards null); increases variance. |
| Berkson Error | (X = X^* + UX), (UX) independent of (X^*) | Assigned exposure differs from true individual exposure. | Does not cause bias but increases imprecision (wider CIs). |
| Differential Error | Error in (X^*) is related to the outcome (Y) | Outcome-influenced recall or measurement (e.g., recall bias). | Unpredictable bias; can be away from or towards the null. |
| Non-Classical Error | Error in (X^*) is correlated with (X) or other errors | Systematic misreporting (e.g., over-reporting of occupation). | Unpredictable bias; direction and magnitude are situation-specific. |
The following diagram illustrates the causal structures of these error mechanisms, highlighting how differential error creates a direct path between the measurement error and the outcome.
Diagram 1: Causal diagrams illustrating classical, differential, and dependent measurement error mechanisms. Note the key difference in (B), where the outcome influences the error, and in (C), where errors in exposure and outcome are correlated.
Experimental Protocols for Error Detection and Evaluation
The Comparison of Methods Experiment
A cornerstone protocol for assessing systematic error in laboratory medicine and analytical chemistry is the Comparison of Methods (COM) experiment. The primary purpose of this experiment is to estimate the inaccuracy or systematic error between a new test method and a comparative method by analyzing multiple patient specimens with both techniques [7].
Experimental Design:
- Specimen Selection and Number: A minimum of 40 different patient specimens should be tested, carefully selected to cover the entire working range of the method. The quality and range of specimens are more critical than a large number. Using 100-200 specimens is recommended to thoroughly assess method specificity, especially if the new method uses a different chemical reaction or measurement principle [7].
- Replication and Timing: Analyze each specimen in a single measurement by both test and comparative methods, though duplicate measurements are advantageous for identifying mistakes. The experiment should be conducted over a minimum of 5 days, and ideally 20 days, to minimize systematic errors that might occur in a single run [7].
- Comparative Method: The choice of comparative method is critical. A reference method with documented correctness is ideal, as any differences can be attributed to the test method. If a routine method is used, large and medically unacceptable differences require additional experiments (e.g., recovery, interference) to identify which method is inaccurate [7].
Data Analysis Workflow:
- Graphical Inspection: The first step is to graph the data. For methods expected to show one-to-one agreement, a difference plot (test result minus comparative result vs. comparative result) should be created. For methods not expected to agree one-to-one (e.g., different enzyme analyses), a comparison plot (test result vs. comparative result) is appropriate. These graphs should be inspected for outliers and consistent patterns (e.g., points scattering above the line at low concentrations and below at high concentrations), suggesting constant or proportional systematic errors [7].
- Statistical Calculation: For data covering a wide analytical range, use linear regression to obtain the slope ((b)) and y-intercept ((a)) of the line of best fit. The systematic error ((SE)) at a critical medical decision concentration ((Xc)) is calculated as: (Yc = a + b \cdot Xc), then (SE = Yc - X_c) [7]. The correlation coefficient ((r)) is mainly useful for assessing if the data range is wide enough for reliable regression estimates [7].
Quality Control Procedures for Ongoing Detection
For the continuous monitoring of systematic error in a laboratory setting, statistical quality control (QC) procedures are essential.
- Levey-Jennings Plots: This involves plotting the measured values of a certified reference material over time on a chart that includes lines for the mean and control limits (e.g., ±1, 2, and 3 standard deviations). Visual inspection of this plot can reveal trends or shifts that indicate the presence of systematic error [9].
- Westgard Rules: These are a set of decision rules used to evaluate QC results. Specific rules are designed to detect systematic error, including [9]:
- 2₂S Rule: Bias is indicated if two consecutive control values fall between the 2 and 3 standard deviation limits on the same side of the mean.
- 4₁S Rule: Bias is indicated if four consecutive control values fall on the same side of the mean and are at least 1 standard deviation away from the mean.
- 10ₓ Rule: Bias is indicated if ten consecutive control values fall on the same side of the mean.
Method Comparison for Bias Characterization
When a systematic error is detected, a method comparison with a gold standard or reference material can be used to characterize the nature of the bias. The observed values from the test method are regressed on the expected values from the reference method. The resulting regression equation, (Y = a + b \cdot X), characterizes the bias [9]:
- Constant Bias: Represented by the y-intercept ((a)). It is a difference that remains constant across the measurement range.
- Proportional Bias: Represented by the slope ((b \neq 1)). It is a difference that changes proportionally with the concentration of the analyte.
Statistical Adjustment and Correction Methods
When validation data are available, several statistical methods can be employed to correct for the effects of measurement error.
- Regression Calibration (RC): This method replaces the unobserved true exposure value (X) in the analysis model with its expected value given the measured exposure (X^) and other covariates, (E(X|X^)), which is estimated from a validation study. This approach works well for classical error and can be adapted for some non-classical scenarios, though it may perform less optimally with substantial error [72] [73].
- Simulation-Extrapolation (SIMEX): This is a simulation-based method that first introduces additional measurement error into the data in a controlled way to observe how the parameter estimates worsen, and then extrapolates back to the scenario of no measurement error. SIMEX is particularly useful when the measurement error variance is known or can be estimated [72].
- Multiple Imputation for Measurement Error (MIME): This method treats the unknown true values (X) as missing data and uses multiple imputation to generate several plausible values for them, based on a model relating (X) to (X^*) from a validation study. The analysis is then performed on each imputed dataset, and the results are combined [72].
Table 2: Overview of Statistical Correction Methods for Measurement Error.
| Method | Key Principle | Data Requirements | Advantages | Limitations |
|---|---|---|---|---|
| Regression Calibration (RC) | Replaces true value with its expectation given measured value. | Validation data to model (E(X|X^*)). | Conceptually simple; implemented in many software packages. | Can be biased with large measurement error or non-linear models. |
| Simulation-Extrapolation (SIMEX) | Adds simulated error to model its effect and extrapolates backwards. | Knowledge/estimate of measurement error variance. | Intuitive graphical component; does not require a model for (X). | Requires correct specification of error model and extrapolation function. |
| Multiple Imputation for M.E. (MIME) | Imputes multiple plausible true values based on measurement model. | Validation data to build imputation model. | Flexible; can be combined with multiple imputation for missing data. | Computationally intensive; requires careful specification of imputation model. |
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Method Comparison and Error Evaluation.
| Item | Function in Experiment | Critical Specifications |
|---|---|---|
| Certified Reference Materials (CRMs) | Serves as an unbiased, high-quality comparative method to identify systematic error in a test method. | Value assigned with high accuracy; traceability to international standards; stated uncertainty. |
| Patient Specimens | Used as real-world samples in a comparison of methods experiment to assess method performance across a biological range. | Cover the entire analytical range; represent the spectrum of expected diseases; stable for the duration of testing. |
| Quality Control Materials | Used in Levey-Jennings plots and Westgard rules for ongoing detection of random and systematic error. | Stable, commutable, and available at multiple concentration levels (normal, pathological). |
| Calibration Standards | Used to adjust instrument response and correct for proportional systematic error identified in method comparison. | Purity and concentration verified by a reference method; prepared in a matrix matching patient samples. |
Optimizing Experimental Protocols to Minimize Introduced Biases
In the rigorous world of scientific research, particularly in drug development, the integrity of experimental data is paramount. Systematic errors, or biases, pose a significant threat to this integrity by consistently skewing data in one direction, leading to false conclusions and potentially costly erroneous decisions in the research pipeline [1] [75]. Unlike random errors, which tend to cancel each other out over repeated trials, systematic errors do not offset each other and can profoundly reduce the reliability and reproducibility of experimental results [75]. The optimization of experimental protocols is therefore not merely a procedural refinement but a fundamental necessity for ensuring the internal validity of research findings. This guide provides a structured approach to identifying, understanding, and mitigating these biases, with a focus on practical strategies for researchers and scientists engaged in method comparison experiments.
Understanding Systematic vs. Random Error
To effectively minimize bias, one must first distinguish it from random variability. Systematic error and random error are two fundamentally different types of measurement error.
- Systematic Error (Bias): This is a consistent or proportional difference between the observed value and the true value. It is reproducible and pushes measurements in a predictable direction. Examples include a miscalibrated instrument that consistently registers weights too high or an experimental procedure that consistently induces a learning effect [1]. In research, systematic errors are generally a bigger problem than random errors because they can skew data away from the true value, leading to false positive or false negative conclusions about the relationship between variables [1].
- Random Error: This is a chance difference between the observed and true values, causing measurements to vary unpredictably around the true value in both directions. It arises from natural, uncontrollable fluctuations in the environment, the measurement instrument, or the participant [1]. While random error affects the precision of measurements, it does not typically bias the mean estimate when enough measurements are taken, as the errors in different directions cancel each other out [1].
The table below summarizes the core differences:
Table: Key Differences Between Systematic and Random Error
| Feature | Systematic Error (Bias) | Random Error |
|---|---|---|
| Direction | Consistent, predictable direction | Unpredictable, both directions |
| Impact on | Accuracy (deviation from truth) | Precision (reproducibility) |
| Source | Flawed methods, instruments, or procedures | Natural variability, imprecise instruments |
| Reduction by | Improving protocol design & calibration | Increasing sample size, repeated measurements |
| Effect on Mean | Shifts the mean value | Does not affect the mean, increases variance |
Systematic biases can infiltrate an experiment from multiple sources. A comprehensive strategy to minimize bias must address each of these potential origins.
Measurement Instruments
Biases can be introduced when measurement instruments are inappropriate, inaccurate, or incorrectly configured [75]. For instance, a slow stopwatch would consistently record shorter times than the actual duration.
- Minimization Techniques:
Experimental Procedures
Inappropriate or unclear procedures are a major source of bias. This includes non-randomized order of conditions leading to learning or fatigue effects, and inconsistent wording of instructions that inadvertently influence participant performance [75].
- Minimization Techniques:
- Randomization: Randomize the order of conditions, tasks, and task scenarios in within-group or split-plot designs to counter sequence effects [75].
- Pilot Studies: Conduct multiple, serious pilot studies with participants from the target population to identify unforeseen procedural biases before the main experiment [75].
- Standardized Documentation: Prepare written documents with detailed instructions for participants and detailed procedures for experimenters to ensure consistency across all sessions [75].
Participants
The characteristics of the participant pool can systematically skew results if the pool is not representative of the target population. For example, recruiting only from a highly technical website would yield data that outperforms that of the general public [75].
- Minimization Techniques:
- Careful Recruitment: Ensure the participant pool is representative of the target user population [75].
- Random Sampling: Use probability sampling methods to ensure every member of the population has a known chance of being selected, which helps counter sampling bias [1].
- Calm Environment: Create a low-stress environment and reassure participants that the interface, not them, is being tested [75].
Experimenter Behavior
Experimenters can intentionally or unintentionally influence results through spoken language, body language, or inconsistent application of procedures across sessions or multiple experimenters [75].
- Minimization Techniques:
- Masking (Blinding): Wherever possible, hide the condition assignment from participants and researchers. This includes blinded conduct of experiments and blinded outcome assessment to prevent experimenter expectancies and demand characteristics from influencing the results [76] [1].
- Experimenter Training: Train all experimenters to be neutral, calm, and patient, and require them to strictly follow the same written procedures [75].
- Recorded Instructions: Use prerecorded instructions to guarantee all participants receive identical information [75].
Environmental Factors
Environmental conditions such as lighting, noise, and physical setup can introduce systematic biases if not controlled.
- Minimization Techniques:
- Control Variables: In controlled experiments, carefully control any extraneous environmental variables that could impact measurements for all participants [1].
Current Reporting Standards and the Reproducibility Crisis
Despite the availability of established guidelines like the ARRIVE 2.0 for animal research, the reporting of measures against bias in nonclinical research remains alarmingly low. A recent 2025 study analyzing 860 biomedical research articles published in 2020 revealed significant gaps in transparency [76].
Table: Reporting Rates of Measures Against Bias in Nonclinical Research (2020)
| Measure Against Bias | Reporting Rate (In Vivo Articles) | Reporting Rate (In Vitro Articles) |
|---|---|---|
| Randomization | 0% - 63% (between journals) | 0% - 4% (between journals) |
| Blinded Conduct of Experiments | 11% - 71% (between journals) | 0% - 86% (between journals) |
| Sample Size Calculation | Low, despite being a key statistical element | Low, despite being a key statistical element |
This poor reporting quality reflects a deeper issue in experimental conduct and is a key contributor to the irreproducibility crisis in nonclinical research, where irreproducibility rates have been estimated between 65-89% [76]. The analysis further suggested that reporting standards are generally better in articles on in vivo experiments compared to in vitro studies [76].
A Framework for Bias Minimization: A Visual Workflow
The following diagram synthesizes the major sources of systematic bias and their corresponding mitigation strategies into a single, cohesive experimental workflow.
The Scientist's Toolkit: Essential Reagents and Materials
Beyond methodological rigor, certain key reagents and materials are fundamental for implementing robust, bias-aware protocols. The following table details several of these essential tools.
Table: Key Research Reagent Solutions for Bias Minimization
| Item / Solution | Function in Bias Minimization |
|---|---|
| Random Number Generator | Generates unpredictable sequences for random allocation of subjects or samples to experimental groups, a cornerstone of randomization. |
| Blinding Kits | Materials (e.g., coded labels, opaque containers) used to conceal group assignments from participants and/or researchers to prevent conscious or subconscious influence. |
| Power Analysis Software | Enables a priori sample size calculation to ensure the experiment has a high probability of detecting a true effect, reducing the risk of false negatives. |
| Standardized Reference Materials | Calibrated substances used to verify the accuracy and performance of measurement instruments, mitigating instrument-based bias. |
| Automated Liquid Handlers | Robotics that perform repetitive pipetting tasks with high precision, reducing variability and experimenter-induced errors in sample preparation. |
| Electronic Lab Notebooks (ELN) | Software for detailed, timestamped, and standardized recording of experimental procedures and data, enhancing transparency and reproducibility. |
Optimizing experimental protocols to minimize introduced biases is an active and continuous process that is critical for the advancement of reliable science, especially in fields like drug development where the stakes are high. By understanding the distinct nature of systematic error, diligently addressing its five major sources, and adhering to rigorous reporting standards, researchers can significantly enhance the internal validity and reproducibility of their work. The integration of strategies such as randomization, blinding, careful power analysis, and thorough piloting into a standardized workflow provides a robust defense against the pervasive threat of bias, ultimately leading to more accurate, trustworthy, and impactful scientific conclusions.
Validation Frameworks and Comparative Analysis for Method Equivalence
Developing a Validation Protocol for Demonstrating Method Equivalence
In pharmaceutical development and analytical sciences, demonstrating that a new or modified analytical procedure is equivalent to an existing one is a critical requirement. Method equivalence ensures that changes in technology, suppliers, or processes do not compromise the reliability of data used for critical quality decisions regarding drug substances and products [77]. At the heart of this demonstration lies the precise estimation and control of systematic errors—differences between methods that are predictable rather than random. A robust validation protocol must effectively quantify these errors to prove that two methods would lead to the same accept/reject decision for a given material [78].
The International Council for Harmonisation (ICH) Q14 guideline on Analytical Procedure Development has formalized a framework for the lifecycle management of analytical procedures, emphasizing the importance of forward-thinking development and risk-based strategies [77]. Within this framework, distinguishing between method comparability and method equivalency becomes crucial. Comparability typically evaluates whether a modified method yields results sufficiently similar to the original, often for lower-risk changes. In contrast, equivalency involves a more comprehensive assessment, usually requiring full validation and regulatory approval, to demonstrate that a replacement method performs equal to or better than the original [77].
Theoretical Framework: Systematic Error Estimation in Method Comparison
Defining Systematic Error Components
Systematic error, or bias, represents the consistent, predictable difference between a measured value and a reference value. Recent research proposes refining the traditional understanding of systematic error by distinguishing between its constant and variable components [24].
- Constant Component of Systematic Error (CCSE): A stable, correctable bias that remains consistent across measurements under varying conditions.
- Variable Component of Systematic Error (VCSE(t)): A time-dependent bias that behaves as a function of time and cannot be efficiently corrected through standard calibration.
This distinction is critical for method equivalence studies, as long-term quality control data often include both random error and the variable component of systematic error. Treating VCSE(t) as purely random error can lead to miscalculations of total error and measurement uncertainty [24].
The Comparison of Methods Experiment
The fundamental approach for assessing systematic error between methods is the comparison of methods experiment. The primary purpose of this experiment is to estimate inaccuracy or systematic error by analyzing patient samples using both the new (test) method and a comparative method [7]. The systematic differences observed at critical medical decision concentrations represent the errors of interest, with information about the constant or proportional nature of these errors being particularly valuable for troubleshooting and improvement [7].
Table 1: Key Characteristics of Systematic Error Components
| Error Component | Nature | Correctability | Primary Impact |
|---|---|---|---|
| Constant Systematic Error | Stable, predictable | Readily correctable through calibration | Accuracy offset |
| Variable Systematic Error | Time-dependent, fluctuating | Not efficiently correctable | Measurement uncertainty |
| Random Error | Unpredictable, inconsistent | Cannot be corrected, only characterized | Precision variability |
Experimental Design for Method Comparison
Specimen Selection and Handling
Proper specimen selection is fundamental to a valid method comparison study. A minimum of 40 different patient specimens should be tested by both methods, selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application [7]. Specimen quality and range distribution are more critical than simply maximizing quantity—20 well-selected specimens covering the analytical range often provide better information than 100 randomly selected specimens [7].
Specimens should generally be analyzed within two hours of each other by the test and comparative methods to minimize stability issues, unless specific analytes require shorter timeframes. For tests with known stability concerns (e.g., ammonia, lactate), appropriate preservation techniques such as serum separation, refrigeration, or freezing should be implemented [7].
Experimental Timeline and Replication
The comparison study should extend across multiple analytical runs on different days to minimize the impact of systematic errors that might occur in a single run. A minimum of 5 days is recommended, though extending the experiment to match the 20-day duration of long-term replication studies provides more robust data [7].
Regarding replication, while common practice uses single measurements by each method, duplicate measurements provide significant advantages. Ideal duplicates consist of two different sample aliquots analyzed in different runs or at least in different order (not back-to-back replicates). Duplicates help identify sample mix-ups, transposition errors, and other mistakes that could compromise study conclusions [7].
Selection of Comparative Method
The choice of comparative method significantly influences the interpretation of results. A reference method with well-documented correctness through comparative studies with definitive methods or traceable reference materials is ideal. When a test method is compared against a reference method, any differences are attributed to the test method [7].
When using a routine method as the comparative method (without documented correctness), differences must be interpreted more carefully. Small differences indicate similar relative accuracy, while large, medically unacceptable differences require additional experiments (e.g., recovery and interference studies) to identify which method is inaccurate [7].
Statistical Analysis and Data Interpretation
Graphical Data Analysis
The initial analysis should include visual inspection of data graphs to identify patterns and potential outliers. Two primary graphing approaches are recommended [7]:
- Difference Plot: Displays the difference between test and comparative results (test minus comparative) on the y-axis versus the comparative result on the x-axis. Differences should scatter randomly around the zero line.
- Comparison Plot: Displays the test result on the y-axis versus the comparison result on the x-axis, particularly useful when methods aren't expected to show one-to-one agreement.
Visual inspection should be performed during data collection to identify discrepant results early, allowing for repeat analysis while specimens are still available [7].
Statistical Calculations for Systematic Error
For data covering a wide analytical range, linear regression statistics are preferred for estimating systematic error at multiple medical decision concentrations. The regression provides slope (b), y-intercept (a), and standard deviation of points about the line (sy/x). The systematic error (SE) at a specific medical decision concentration (Xc) is calculated as [7]:
- Yc = a + bXc
- SE = Yc - Xc
The correlation coefficient (r) is mainly useful for assessing whether the data range is sufficiently wide to provide reliable slope and intercept estimates. When r is below 0.99, collecting additional data to expand the concentration range or using more sophisticated regression techniques is recommended [7].
For narrow analytical ranges, calculating the average difference (bias) between methods using paired t-test statistics is often more appropriate. This approach provides the mean difference, standard deviation of differences, and a t-value for assessing statistical significance [7].
Table 2: Statistical Approaches for Different Method Comparison Scenarios
| Scenario | Recommended Statistical Approach | Key Outputs | Considerations |
|---|---|---|---|
| Wide Analytical Range | Linear Regression | Slope, y-intercept, s_y/x | Preferable when r ≥ 0.99 |
| Narrow Analytical Range | Paired t-test | Mean difference, SD of differences | Appropriate for limited concentration range |
| Method Equivalency Testing | Equivalence testing with predefined acceptance criteria | Confidence intervals around differences | Requires prior definition of equivalence margins |
| Proportional Systematic Error | Deming Regression or Passing-Bablok | Slope with confidence intervals | Accounts for error in both methods |
Regulatory and Compliance Considerations
ICH Q14 and Analytical Procedure Lifecycle
The introduction of ICH Q14: Analytical Procedure Development provides a formalized framework for creating, validating, and managing analytical methods throughout their lifecycle. This guideline encourages a structured, risk-based approach to assessing, documenting, and justifying method changes [77]. Under ICH Q14, method development should begin with the end state in mind, leveraging prior knowledge and risk-based strategies to define the Analytical Target Profile (ATP). This ensures the method is fit for purpose and can accommodate future changes with minimal impact [77].
Pharmacopoeial Requirements
Global pharmacopoeias permit the use of alternative methods to existing monographs, but with significant regulatory restrictions. The European Pharmacopoeia General Notices specifically require competent authority approval before implementing alternative methods for routine testing [78]. Furthermore, pharmacopoeias include the disclaimer that "in the event of doubt or dispute, the analytical procedures of the pharmacopoeia are alone authoritative," establishing the pharmacopoeial method as the referee in case of discrepant results [78].
The recently implemented Ph. Eur. chapter 5.27 on Comparability of Alternative Analytical Procedures provides guidance for demonstrating that an alternative method is comparable to a pharmacopoeial method. However, the burden of demonstration lies with the user, requiring thorough documentation and validation to the satisfaction of competent authorities [78].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Method Equivalence Studies
| Reagent/Material | Function in Equivalence Studies | Critical Quality Attributes |
|---|---|---|
| Reference Standards | Establish measurement traceability and accuracy | Purity, stability, commutability |
| Quality Control Materials | Monitor method performance over time | Stability, matrix compatibility, concentration values |
| Patient Specimens | Assess method performance across biological range | Stability, representativeness of population, concentration distribution |
| Calibrators | Establish correlation between signal and concentration | Traceability, accuracy, matrix appropriateness |
| Matrix Components | Evaluate specificity and potential interferences | Purity, relevance to sample type |
Advanced Topics in Systematic Error Management
Risk-Based Approach to Method Changes
A strategic, risk-based approach is essential for effective method lifecycle management. For low-risk procedural changes with minimal impact on product quality, a comparability evaluation may be sufficient. For high-risk changes such as complete method replacements, a comprehensive equivalency study demonstrating equal or better performance is required, typically including full validation and regulatory approval [77].
Common drivers for method changes include [77]:
- Technology upgrades (e.g., instrument changes)
- Supplier changes for critical reagents
- Manufacturing process improvements
- Continuous improvement initiatives
- Updates to regulatory requirements
Specification Equivalence Evaluation
Specification equivalence represents a practical approach for evaluating whether different analytical procedures produce equivalent results for a given substance, regardless of manufacturing site or method differences. Drawing from the Pharmacopoeial Discussion Group concept of harmonization, specification equivalence is established when testing by different methods yields the same results and the same accept/reject decision [78].
The evaluation proceeds attribute-by-attribute, assessing both analytical procedures and their associated acceptance criteria. This "in-house harmonization" enables manufacturers to scientifically justify compliance with multiple regional specifications while minimizing redundant testing [78].
Developing a robust validation protocol for demonstrating method equivalence requires careful attention to systematic error estimation throughout the experimental process. By implementing appropriate specimen selection strategies, statistical analyses, and regulatory-aware protocols, scientists can generate defensible data to support method changes. The distinction between constant and variable components of systematic error provides a more nuanced understanding of method performance, enabling more accurate estimation of measurement uncertainty and better decision-making in analytical method lifecycle management.
As regulatory frameworks continue to evolve with guidelines such as ICH Q14, a proactive, knowledge-driven approach to method development and validation becomes increasingly important. By building quality into methods from the initial development stages and maintaining comprehensive understanding of systematic error sources, organizations can ensure ongoing method suitability while efficiently managing necessary changes throughout a product's lifecycle.
Assessing Performance Against Gold Standards and Alloyed Gold Standards
In medical diagnostics and pharmaceutical development, the "gold standard" serves as the definitive benchmark method for confirming a specific disease or condition against which new tests are evaluated [79]. This concept is fundamental to validating new diagnostic tests through independent, blinded comparisons that assess critical metrics like accuracy, sensitivity, and specificity [79]. Historically, the term was coined in 1979 by Thomas H. Rudd, who drew an explicit analogy to the monetary gold standard system that pegged currencies to fixed quantities of gold to ensure stability and predictability [79].
However, a critical understanding has emerged in modern methodology: many reference standards are not perfect, constituting what researchers term an "alloyed gold standard" [80]. This imperfection has profound implications for performance assessment, as using an imperfect reference standard can significantly bias estimates of a new test's diagnostic accuracy [80]. The limitations of traditional gold standards include their frequent invasiveness, high costs, limited availability, and ethical concerns that prevent widespread use [79]. In cancer diagnosis, for instance, the gold standard often requires surgical biopsy, while in tuberculosis diagnosis, culture-based detection of Mycobacterium tuberculosis remains definitive but time-consuming [79].
This comparison guide examines the methodological frameworks for assessing diagnostic performance against both traditional and alloyed gold standards, providing researchers with evidence-based protocols to navigate the complexities of systematic error estimation in method comparison experiments.
Quantitative Impact of Imperfect Gold Standards
Theoretical Framework and Empirical Evidence
When a gold standard is imperfect, its limitations directly impact the measured performance characteristics of new tests being evaluated. A 2025 simulation study examined this phenomenon specifically, analyzing how imperfect gold standard sensitivity affects measured test specificity across different disease prevalence levels [80].
Table 1: Impact of Imperfect Gold Standard Sensitivity on Measured Specificity
| Gold Standard Sensitivity | Death Prevalence | True Test Specificity | Measured Specificity | Underestimation |
|---|---|---|---|---|
| 99% | 98% | 100% | <67% | >33% |
| 95% | 90% | 100% | 83% | 17% |
| 90% | 80% | 100% | 87% | 13% |
| 99% | 50% | 100% | 98% | 2% |
The simulation results demonstrated that decreasing gold standard sensitivity was associated with increasing underestimation of test specificity, with the extent of underestimation magnified at higher disease prevalence [80]. This prevalence-dependent bias occurs because imperfect sensitivity in the gold standard misclassifies true positive cases as negative, thereby increasing the apparent false positive rate of the test being evaluated [80].
Case Study: Mortality Index Validation
A concrete example of this phenomenon comes from real-world oncology research validating mortality endpoints. Researchers developed an All-Source Composite Mortality Endpoint (ASCME) that combined multiple real-world data sources, then validated it against the National Death Index (NDI) database, considered the industry-recognized gold standard for death ascertainment [80].
However, the NDI itself has imperfect sensitivity due to delays in death certificate filing and processing. Analysis revealed that at 98% death prevalence (common in advanced cancer studies), even near-perfect gold standard sensitivity (99%) suppressed measured specificity from the true value of 100% to less than 67% [80]. This quantitative demonstration underscores how even minor imperfections in reference standards can dramatically alter performance assessments in high-prevalence settings.
Experimental Protocols for Method Comparison
Establishing the Comparison Framework
The comparison of methods experiment is critical for assessing systematic errors that occur with real patient specimens [7]. Proper experimental design ensures that observed differences truly reflect test performance rather than methodological artifacts.
Table 2: Key Experimental Design Parameters for Method Validation
| Parameter | Recommendation | Rationale |
|---|---|---|
| Number of Patient Specimens | Minimum of 40 | Provides reasonable statistical power while remaining practical |
| Specimen Selection | Cover entire working range | Ensures evaluation across clinically relevant concentrations |
| Measurement Replication | Duplicate measurements | Identifies sample mix-ups, transposition errors, and methodological mistakes |
| Time Period | Minimum of 5 days | Minimizes systematic errors that might occur in a single run |
| Specimen Stability | Analyze within 2 hours | Prevents degradation artifacts from affecting results |
| Blinding | Independent interpretation | Prevents differential verification bias |
The analytical method used for comparison must be carefully selected because the interpretation of experimental results depends on assumptions about the correctness of the comparative method [7]. When possible, a reference method with documented traceability to standard reference materials should serve as the comparator [7].
Statistical Analysis and Data Interpretation
Appropriate statistical analysis is fundamental to interpreting comparison data accurately. The most fundamental analysis technique involves graphing comparison results and visually inspecting the data [7]. Difference plots display the difference between test and comparative results on the y-axis versus the comparative result on the x-axis, allowing researchers to identify systematic patterns in discrepancies [7].
For data covering a wide analytical range, linear regression statistics are preferable as they allow estimation of systematic error at multiple medical decision concentrations [7]. The systematic error (SE) at a given medical decision concentration (Xc) is calculated by determining the corresponding Y-value (Yc) from the regression line (Y = a + bX), then computing the difference: SE = Yc - Xc [7].
Correlation coefficients (r) are mainly useful for assessing whether the data range is wide enough to provide good estimates of slope and intercept, with values of 0.99 or larger indicating reliable linear regression estimates [7]. For narrower analytical ranges, calculating the average difference between methods (bias) with paired t-tests is often more appropriate [7].
Advanced Error Modeling in Method Comparison
Distinguishing Error Components
Modern error modeling distinguishes between constant and variable components of systematic error (bias) in measurement systems [24]. This refined understanding challenges traditional approaches that often conflate these components, resulting in miscalculations of total error and measurement uncertainty.
The proposed model defines the constant component of systematic error (CCSE) as a correctable term, while the variable component of systematic error (VCSE(t)) behaves as a time-dependent function that cannot be efficiently corrected [24]. This distinction is crucial in clinical laboratory settings where biological materials and measuring systems exhibit inherent variability that traditional Gaussian distribution models cannot adequately capture [24].
The total measurement error (TE) comprises both systematic error (SE) and random error (RE) components, with systematic error further divisible into constant and variable elements [24]. Understanding this hierarchy enables more accurate quantification of measurement uncertainty.
Visualizing Method Validation Workflow
The following diagram illustrates the comprehensive workflow for validating a new diagnostic method against a reference standard, incorporating procedures to account for potential imperfections in the gold standard:
Method Validation Workflow with Error Assessment
This workflow emphasizes critical steps for accounting for potential imperfections in reference standards, including sensitivity analyses and bias correction methods that become essential when working with alloyed gold standards.
Essential Research Reagent Solutions
Table 3: Essential Materials for Method Validation Studies
| Reagent/Material | Function | Application Context |
|---|---|---|
| Certified Reference Materials | Establish metrological traceability and calibration verification | Quantifying constant systematic error components across measurement range |
| Quality Control Materials | Monitor assay performance stability over time | Detecting variable systematic error components in longitudinal studies |
| Biobanked Patient Specimens | Provide real-world clinical samples across disease spectrum | Assessing diagnostic performance across clinically relevant conditions |
| Standardized Infiltration Factors | Estimate outdoor pollution contribution to personal exposure | Air pollution health effects research (e.g., MELONS study) [81] |
| Statistical Correction Tools | Implement simulation extrapolation (SIMEX) and regression calibration (RCAL) | Correcting bias from exposure measurement error in epidemiological studies [81] |
These essential materials enable researchers to implement robust validation protocols that account for both constant and variable components of systematic error. The selection of appropriate reagents and statistical tools should align with the specific validation context and potential sources of imperfection in the reference standard.
Implications for Research and Development
Impact on Epidemiological Study Validity
The consequences of imperfect gold standards extend beyond laboratory medicine to epidemiological research. A 2025 air pollution study (MELONS) demonstrated that exposure measurement error between personal exposure measurements and surrogate measures can lead to substantially biased health effect estimates [81]. In simulation studies, these biases were consistently large and almost always directed toward smaller estimated health effects (toward the null) [81].
This systematic underestimation has profound implications for environmental regulations and public health policies based on such studies. The research found that when tested under theoretical measurement error scenarios, both simulation extrapolation (SIMEX) and regression calibration (RCAL) approaches performed well in correcting estimated hazard ratios [81]. This suggests that acknowledging and quantitatively addressing measurement imperfection can improve the accuracy of health effect estimation.
Methodological Recommendations
Based on the evidence presented, researchers should adopt the following practices when assessing performance against gold standards:
- Acknowledge Imperfection: Recognize that most gold standards are alloyed to some degree, and proactively assess the potential impact of their limitations on validation results [80].
- Implement Correction Methods: Apply statistical correction techniques like SIMEX and regression calibration when imperfection in the reference standard is suspected or known [81].
- Report Prevalence Context: Always consider and report the prevalence of the condition being assessed, as the impact of gold standard imperfection is highly prevalence-dependent [80].
- Validate Across Range: Ensure method validation covers the entire analytical measurement range and clinically relevant decision points [7].
- Account for Error Structure: Distinguish between constant and variable components of systematic error when estimating total measurement uncertainty [24].
These practices will enhance the reliability of diagnostic test evaluations and provide more accurate assessments of true clinical performance, ultimately supporting better healthcare decisions and more efficient drug development processes.
Statistical Approaches for Quantifying and Adjusting for Measurement Error
In scientific research, particularly in fields such as epidemiology, clinical chemistry, and drug development, the accurate measurement of variables is fundamental to drawing valid conclusions. Measurement error, defined as the discrepancy between the measured value and the true value of a variable, is a ubiquitous challenge that can substantially bias study findings and lead to incorrect interpretations [72]. All measurements contain some degree of error, and failing to account for this error can result in biased effect estimates, reduced statistical power, and distorted relationships between variables [82] [72]. The conceptual foundation for understanding measurement error begins with recognizing that virtually all epidemiologic studies suffer from some degree of bias, loss of power, or coarsening of relationships as a result of imperfect measurements [72].
Within the context of method comparison experiments, researchers systematically evaluate the performance of a new measurement method (test method) against an established one (comparative method) to identify and quantify systematic errors [7] [83]. The primary purpose of these experiments is to obtain an estimate of systematic error or bias, which is crucial for understanding the accuracy of a new method [83]. Different statistical approaches have been developed to quantify, correct, or adjust for these errors, each with specific assumptions, requirements, and applications. The choice of an appropriate method depends on the measurement error model assumed, the availability of suitable calibration study data, and the potential for bias due to violations of the classical measurement error model assumptions [82].
Fundamental Concepts and Error Models
Types of Measurement Error
Measurement errors are broadly categorized based on their statistical properties and relationship to other variables:
- Random Error: Chance fluctuations or random variations that average out to the truth over many repetitions. In the classical measurement error model, this within-person random error is independent of the true exposure with a mean of zero and constant variance [82] [73]. Its effect is typically an attenuation of the estimated effect size toward the null [82].
- Systematic Error: More serious errors that do not average out to the true value even with many repetitions. These can occur at both within-person and between-person levels [82].
- Differential Error: Occurs when the errors in one variable are related to another variable, such as the outcome. This is common when knowledge of the outcome can influence measurement of the exposure, such as in case-control studies with recall bias [72] [73].
- Non-Differential Error: Occurs when the error provides no extra information about the outcome beyond what is provided by the true exposure and other covariates in the model [73].
- Dependent Error: Occurs when errors in two or more variables are correlated with each other, such as in same-source bias where participants systematically over-report or under-report multiple behaviors due to stigma [72].
Measurement Error Models
Formal error models describe the mathematical relationship between true and measured variables:
- Classical Measurement Error Model: Describes a measurement that has no systematic bias but is subject to random error: (X^* = X + e), where (e) is a random variable with mean zero independent of (X) [72] [73]. This model assumes the error is independent of the true value and additive.
- Linear Measurement Error Model: An extension that accounts for both random error and systematic bias: (X^* = \alpha0 + \alphaX X + e), where (e) is a random variable with mean zero independent of (X) [73]. The classical model is a special case where (\alpha0 = 0) and (\alphaX = 1).
- Berkson Error Model: An "inverse" model where the true value varies around the measured value: (X = X^* + e), where (e) is a random variable with mean zero independent of (X^*) [72] [73]. This occurs when all individuals in specific subgroups are assigned the average value of their subgroup.
The following diagram illustrates the relationships between these fundamental error concepts and their manifestations in research data:
Statistical Approaches for Quantification and Adjustment
Multiple statistical approaches have been developed to quantify and correct for measurement error across different research contexts. The table below summarizes the key methods, their applications, and implementation requirements:
Table 1: Statistical Approaches for Measurement Error Quantification and Adjustment
| Method | Primary Application | Data Requirements | Key Assumptions | Advantages | Limitations |
|---|---|---|---|---|---|
| Regression Calibration | Correct exposure measurement error in nutritional epidemiology [82] | Calibration study with reference instrument [82] | Classical measurement error model; error is non-differential [82] [73] | Reduces bias in effect estimates; most common approach in nutritional epidemiology [82] | Requires assumptions to be fully met; may not be suitable for differential error [82] |
| Method of Triads | Quantify relationship between dietary assessment instruments and "true intake" [82] | Three different measures of the same exposure [82] | All measurement errors are independent [82] | Allows quantification of validity coefficients without a gold standard [82] | Requires three independent measures; may be impractical in some settings [82] |
| Multiple Imputation | Handle differential measurement error [82] | Validation subsample with both error-prone and true measures [82] | Missing at random mechanism for true values [82] | Flexible approach for various error structures; accounts for uncertainty in imputed values [82] | Computationally intensive; requires careful specification of imputation model [82] |
| Moment Reconstruction | Address differential measurement error [82] | Information on measurement error distribution [82] | Known error distribution parameters [82] | Can handle differential error without full validation data [82] | Relies on accurate specification of error distribution [82] |
| Maximum Likelihood | Adjust diagnostic performance measures (sensitivity, specificity) for biomarker measurement error [84] | Internal reliability sample with replicate measurements [84] | Normal distribution for true values and errors; specified measurement error structure [84] | Produces consistent, asymptotically normal estimators; enables confidence interval construction [84] | Requires distributional assumptions; computational complexity with complex error structures [84] |
| Survival Regression Calibration (SRC) | Correct measurement error in time-to-event outcomes in oncology real-world data [85] | Validation sample with both true and mismeasured time-to-event outcomes [85] | Weibull distribution for survival times; non-differential error structure [85] | Specifically designed for time-to-event data; handles right-censoring [85] | Limited evaluation in diverse survival distributions; requires validation data [85] |
Total Analytic Error Concept
In clinical laboratory settings, the concept of Total Analytic Error (TAE) provides a practical framework for assessing overall method performance. TAE combines estimates of both bias (from method comparison studies) and precision (from replication studies) into a single metric: TAE = bias + 2SD (for a 95% confidence interval) [86]. This approach recognizes that the analytical quality of a test result depends on the total effect of a method's precision and accuracy, which is particularly important when clinical laboratories typically make only a single measurement on each patient specimen [86].
Experimental Protocols for Method Comparison Studies
Core Experimental Design
Well-designed method comparison experiments are essential for generating reliable data on measurement error. The following protocol outlines key considerations:
- Sample Selection and Size: A minimum of 40 different patient specimens should be tested by both methods, selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application [7]. Specimens should be carefully selected based on observed concentrations rather than randomly collected, with quality of specimens being more important than quantity [7].
- Measurement Procedures: Analyze patient specimens by both the new test method and the comparative method within two hours of each other to maintain specimen stability [7]. Ideally, perform duplicate measurements on different samples analyzed in separate runs or different order rather than back-to-back replicates on the same sample [7].
- Timeframe: Conduct the experiment over several different analytical runs on different days (minimum of 5 days recommended) to minimize systematic errors that might occur in a single run [7].
Reference Instrument Selection
The choice of an appropriate reference instrument is critical for method comparison studies:
- Gold Standard: When possible, select a reference method with documented correctness through comparative studies with definitive methods or traceability of standard reference materials [7].
- Alloyed Gold Standard: In situations where a perfect gold standard is impractical (e.g., multiple week diet records in nutritional epidemiology), the best performing instrument under reasonable conditions may be used, acknowledging some residual error [82].
- Comparative Method: For routine laboratory methods without documented correctness, differences must be carefully interpreted, with additional experiments (recovery and interference) needed to identify which method is inaccurate when large, medically unacceptable differences are found [7].
The workflow for designing and executing a robust method comparison study follows this logical sequence:
Data Analysis and Visualization Techniques
Graphical Approaches for Initial Data Inspection
- Difference Plots (Bland-Altman Plots): Display the difference between test and comparative results on the y-axis versus the comparative result (or mean of both methods) on the x-axis [7] [83]. Differences should scatter around the line of zero differences, with any large differences standing out for further investigation [7].
- Comparison Plots: Display the test result on the y-axis versus the comparison result on the x-axis [7]. This shows the analytical range of data, linearity of response over the range, and the general relationship between methods as shown by the angle of the line and its intercept with the y-axis [7].
Statistical Calculations for Error Quantification
- Linear Regression Statistics: For data covering a wide analytical range, calculate slope (b), y-intercept (a), and standard deviation of points about the line (s~y/x~) [7]. Systematic error at a medical decision concentration (X~c~) is calculated as SE = Y~c~ - X~c~, where Y~c~ = a + bX~c~ [7].
- Correlation Coefficient (r): Mainly useful for assessing whether the data range is wide enough to provide good estimates of slope and intercept, with r ≥ 0.99 indicating adequate range for ordinary linear regression [7] [83].
- Paired t-test Statistics: For data covering a narrow analytical range, calculate the average difference (bias) between methods, along with the standard deviation of differences [7].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Methodological Components for Measurement Error Research
| Component | Function | Application Context |
|---|---|---|
| Calibration Study | Provides additional information on random or systematic error in the measurement instrument of interest [82] | Required for most measurement error correction methods; can be internal (nested within main study) or external (separate population) [82] [73] |
| Validation Sample | Subset of participants with both error-prone and true measurements to characterize measurement error structure [84] [85] | Enables estimation of measurement error model parameters; essential for methods like regression calibration and maximum likelihood [84] [85] |
| Reference Instrument | More accurate measurement method used as benchmark for comparing new test method [82] [7] | Serves as "gold standard" or "alloyed gold standard" in method comparison studies [82] [7] |
| Replication Data | Multiple measurements of the same variable within individuals to assess random error [84] | Used to estimate within-person variation and measurement error variance [84] |
| Statistical Software | Implementation of specialized measurement error correction methods | Required for complex methods like regression calibration, maximum likelihood, and survival regression calibration [82] [84] [85] |
Advanced Applications and Specialized Methods
Survival Regression Calibration for Time-to-Event Outcomes
In oncology research using real-world data, Survival Regression Calibration (SRC) has been developed to address measurement error in time-to-event outcomes like progression-free survival [85]. This method extends standard regression calibration approaches by:
- Fitting separate Weibull regression models using both true and mismeasured outcome measures in a validation sample
- Calibrating parameter estimates in the full study according to the estimated bias in Weibull parameters
- Effectively reducing bias in median progression-free survival estimates compared to standard regression calibration methods [85]
Adjusting Diagnostic Performance Measures
For biomarkers subject to measurement error, maximum likelihood approaches can correct estimates of diagnostic performance measures including:
- Sensitivity and Specificity: Naïve estimates converge to biased values; for sensitivity: (Se{nai} = 1 - \Phi\left(\frac{\Phi^{-1}(1-Se)}{\sqrt{1+\tau1^2/(M1\sigma1^2)}}\right)), where (\tau1^2) and (\sigma1^2) are error and true variances [84]
- Youden Index and Optimal Cut-point: Bias-corrected estimates account for measurement error in the biomarker [84]
- ROC Curve and AUC: Appropriate adjustment prevents underestimation of AUC, which could erroneously suggest a biomarker is ineffective [84]
Addressing Real-World Endpoint Measurement Error
In real-world oncology data, two specific bias types require specialized attention:
- Misclassification Bias: Arises from how endpoints are derived or ascertained, such as false positives (patients without progression falsely classified as progressed) or false negatives (true progression events not captured) [87]
- Surveillance Bias: Stems from when outcomes are observed or assessed at different and irregular intervals compared to trial settings [87]
Simulation studies show these biases can substantially impact median progression-free survival estimates, with false positive misclassification biasing estimates earlier and false negative misclassification biasing estimates later [87].
Comparative Analysis of Regression Techniques for Error Mitigation
In scientific research and drug development, the accuracy of quantitative measurements forms the bedrock of reliable data and valid conclusions. Systematic error, or bias, is a fundamental metrological characteristic of any measurement procedure, and its accurate estimation is crucial for the correct interpretation of clinical laboratory results [28]. This guide provides a comparative analysis of various regression techniques, framed within the context of systematic error estimation in method comparison experiments. We objectively evaluate the performance of multiple regression algorithms, supported by experimental data, to aid researchers and scientists in selecting appropriate error mitigation strategies for their specific applications, from clinical laboratories to predictive modeling in material science and manufacturing.
Theoretical Foundation: Systematic Error and Label Noise
The Challenge of Systematic Error
Systematic error is defined as an estimator of the mean of a set of replicate results of measurement obtained in a control or reference material minus a true value of the quantity intended to be measured [28]. In practice, since a true value is unobtainable, a conventional true value is used, which can be an assigned value (obtained with a primary or reference measurement procedure), a consensus value, or a procedure-defined value.
The presence of experimental noise associated with sample labels puts a fundamental limit on the performance metrics attainable by regression models [88]. In biological contexts, for instance, this label noise is particularly pronounced as sample labels are typically obtained through experiments. This noise creates an upper bound for metrics like the coefficient of determination (R²), meaning a model with an R² of 1 (perfect prediction) cannot be achieved in practical scenarios with inherent measurement error [88].
Upper Bounds of Model Performance
Research has shown that an expected upper bound for R² can be derived for regression models when tested on holdout datasets. This upper bound depends only on the noise associated with the response variable and its variance, providing researchers with a benchmark for assessing whether further model improvement is feasible [88]. Monte Carlo simulations have validated these upper bound estimates, demonstrating their utility for bootstrapping performance of regression models trained on various biological datasets, including protein sequence data, transcriptomic data, and genomic data [88].
Various regression techniques have been developed to address different data structures and error characteristics. The choice of technique depends on factors such as the number of independent variables, type of dependent variables, and the shape of the regression line [89].
Common Regression Types
- Linear Regression: Establishes a relationship between a dependent variable (Y) and one or more independent variables (X) using a best fit straight line. It assumes linear relationship between variables and is sensitive to outliers [89].
- Polynomial Regression: Useful when the power of the independent variable is more than 1. The best fit line is not straight but rather a curve that fits into the data points [89].
- Ridge Regression: A model tuning method that analyzes data suffering from multicollinearity. It uses regularization to prevent overfitting by penalizing large coefficients [90].
- Lasso Regression: Uses shrinkage for data values toward a central point. It is well-suited for models showing high levels of multicollinearity and can automate variable selection [90].
- Support Vector Regression (SVR): Based on the principle of support vector machines, SVR develops a hyperplane between two sets of data with a maximum margin. It is effective for both linear and non-linear models [91].
- Principal Component Regression (PCR): Combines principal component analysis and least squares regression to handle multicollinearity by transforming correlated variables into uncorrelated principal components [91].
- Random Forest Regression: An ensemble learning method that operates by constructing a multitude of decision trees at training time and outputting the mean prediction of the individual trees [90].
- XGBoost Regression: An optimized distributed gradient boosting library belonging to a family of boosting algorithms that convert weak learners into strong learners [90].
Comparative Performance Analysis
Quantitative Comparison of Regression Algorithms
Table 1: Comparative performance of regression algorithms in predicting concrete compressive strength
| Regression Algorithm | R² Score | MAE (MPa) | RMSE (MPa) | Key Characteristics |
|---|---|---|---|---|
| XGBoost | 0.9300 | Not Reported | Not Reported | Best performance, handles complex patterns [90] |
| Random Forest | 0.8995 | Not Reported | Not Reported | Robust to outliers, good for non-linear relationships [90] |
| Linear Regression | 0.6275 | 7.74 | 9.79 | Simple, interpretable, assumes linearity [90] |
| Ridge Regression | ~0.60 | Not Reported | Not Reported | Addresses multicollinearity [90] |
| Lasso Regression | ~0.62 | Not Reported | Not Reported | Performs variable selection [90] |
Table 2: Performance comparison of regression models in machining composites
| Regression Model | Performance Ranking | Key Strengths | Limitations |
|---|---|---|---|
| Support Vector Regression (SVR) | Best | Suitable for linear and non-linear models, few tuning parameters [91] | Computational complexity with large datasets |
| Polynomial Regression | Intermediate | Captures curvature in data | Can overfit with high degrees |
| Linear Regression | Intermediate | Simple, interpretable | Assumes linearity |
| Principal Component Regression | Intermediate | Handles multicollinearity | Interpretation of components can be challenging |
| Ridge, Lasso, Elastic Net | Intermediate | Addresses multicollinearity, regularization | Requires hyperparameter tuning |
| Quantile Regression | Intermediate | Robust to outliers | Computationally intensive |
| Median Regression | Worst | Simple | Limited flexibility [91] |
Analysis of Performance Results
The comparative analysis reveals that ensemble methods like XGBoost and Random Forest typically achieve superior prediction performance for complex, non-linear relationships, as demonstrated in the concrete compressive strength prediction study [90]. However, their "black box" nature can limit interpretability in contexts where understanding causal relationships is crucial.
For method comparison studies where interpretability is paramount, SVR emerges as a strong candidate, balancing performance with more transparent modeling approaches [91]. Traditional methods like Linear and Polynomial Regression, while simpler, often provide sufficient accuracy for less complex relationships and benefit from greater interpretability.
The significant performance improvement observed in Ridge and Lasso Regression after cross-validation highlights the importance of proper hyperparameter tuning, particularly for addressing multicollinearity issues [90].
Experimental Protocols for Method Comparison
Standardized Comparison Methodology
The comparison of methods experiment is critical for assessing the systematic errors that occur with real patient specimens [7]. The following protocol provides a framework for conducting such experiments:
- Comparative Method Selection: When possible, a "reference method" should be chosen, implying a high-quality method whose results are known to be correct. With routine methods, differences must be carefully interpreted, and additional experiments may be needed to identify which method is inaccurate [7].
- Sample Selection and Size: A minimum of 40 different patient specimens should be tested, selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application. The quality of specimens (wide range of values) is more important than large numbers, though 100-200 specimens help assess specificity differences [7].
- Measurement Approach: Analyze each specimen singly by both test and comparative methods, though duplicate measurements provide a validity check. Conduct the study over multiple analytical runs (minimum of 5 days) to minimize systematic errors that might occur in a single run [7].
- Specimen Handling: Analyze specimens within two hours of each other by both methods, unless stability is known to be shorter. Carefully define and systematize specimen handling to prevent differences due to handling variables rather than analytical errors [7].
Data Analysis Workflow
The following workflow outlines the standard process for comparing measurement methods and evaluating regression techniques for error mitigation:
Statistical Analysis Approaches
For data analysis in method comparison studies:
- Graphical Analysis: Create difference plots (test minus comparative results versus comparative result) or comparison plots (test result versus comparison result) to visually inspect data patterns, identify discrepant results, and observe constant or proportional errors [7].
- Statistical Calculations for Wide Analytical Range: Use linear regression statistics (slope, y-intercept, standard deviation of points about the line) to estimate systematic error at medical decision concentrations. Calculate systematic error as SE = Yc - Xc, where Yc is the value from the regression line at critical decision level Xc [7].
- Statistical Calculations for Narrow Analytical Range: Calculate the average difference between results (bias) and the standard deviation of differences. Use paired t-test calculations to determine if biases are statistically significant [7].
- Correlation Analysis: Calculate correlation coefficient (r) mainly to assess whether the data range is wide enough to provide good estimates of slope and intercept, not for judging method acceptability [7].
Advanced Regression Applications in Error Mitigation
Domain-Specific Applications
- Building Airtightness Measurements: Research comparing Ordinary Least Squares (OLS), Weighted Least Squares (WLS), and Weighted Line of Organic Correlation (WLOC) in building airtightness testing per ISO 9972 found that WLS and WLOC outperformed traditional OLS, particularly under higher wind speeds. WLS showed the highest overall coverage of 95% confidence intervals, while WLOC provided a good balance between accuracy and reliability [92].
- Wear Prediction in Mechanical Systems: A study on predicting wear damage in moving mechanical contacts employed a methodology with four key stages: feature selection, sample size determination, regression model selection, and model evaluation. The research compared Linear Regression, Support Vector Machines (SVMs), and Random Forests (RFs), using metrics including MAE, MBE, RMSE, and R² to assess predictive performance [93].
- Machining Process Optimization: In turning and drilling operations of composite materials, regression models have been successfully applied to predict response values like surface roughness and tool wear. The prediction performance of various models can be contrasted using statistical error estimators including Mean Absolute Percentage Error (MAPE), Root Mean Squared Percentage Error (RMSPE), Root Mean Squared Logarithmic Error (RMSLE), and Root Relative Squared Error (RRSE) [91].
Error Metric Selection Framework
Different error metrics provide insights into various aspects of model performance:
- Root Mean Squared Error (RMSE): Measured in the same units as the data, this statistic determines the width of confidence intervals for predictions and is minimized during parameter estimation. It gives disproportionate weight to very large errors due to the squaring process [46].
- Mean Absolute Error (MAE): Measured in the same units as the data, usually slightly smaller than RMSE. Less sensitive to occasional very large errors as it doesn't square errors [46].
- Mean Absolute Percentage Error (MAPE): Expressed in generic percentage terms, useful for reporting when the relative size of errors is more important than absolute values. Can only be computed with strictly positive data [46].
- Bias (Mean Error): A signed measure indicating whether forecasts are disproportionately positive or negative. While normally considered undesirable, it's not the sole determinant of model quality as MSE equals the variance of errors plus the square of the mean error [46].
Essential Research Reagents and Materials
Table 3: Essential research reagents and solutions for method comparison studies
| Reagent/Solution | Function/Purpose | Application Context |
|---|---|---|
| Control Materials | Provide conventional true values for estimating systematic error; may be assayed or unassayed [28] | General method validation |
| Reference Materials | Materials with values assigned by reference measurement procedures; highest quality conventional true values [7] | Critical method validation |
| Patient Specimens | Natural matrices representing real-world analysis conditions; cover clinical range of interest [7] | Clinical method comparison |
| Lyophilized Control Sera | Stable, reproducible materials for proficiency testing and inter-laboratory comparison [28] | Quality assessment programs |
| Primary/Reference Standards | Highest order reference materials for assigning values to other materials and calibrators [28] | Traceability establishment |
This comparative analysis demonstrates that no single regression technique universally outperforms others across all error mitigation scenarios. The selection of an appropriate regression method depends on multiple factors, including the data characteristics (linearity, multicollinearity, noise structure), analytical requirements (interpretability vs. predictive power), and specific application domain.
For method comparison studies focused on systematic error estimation, traditional techniques like linear regression with appropriate data transformation often provide sufficient accuracy with high interpretability. However, in complex predictive modeling scenarios with non-linear relationships and multiple interacting variables, ensemble methods like XGBoost and Random Forest, or flexible approaches like SVR, may offer superior performance despite their more complex interpretation.
The findings support incorporating alternative regression techniques such as WLS and WLOC into standardized testing procedures, offering better uncertainty estimation and more accurate predictions under varying conditions. By improving measurement and modeling standards through appropriate regression technique selection, this research contributes to the broader goals of accuracy, reliability, and validity in scientific research and drug development.
Establishing Acceptance Criteria for Bias in Regulatory Contexts
In the rigorous world of pharmaceutical development and clinical laboratory science, the validity of analytical methods hinges on the accurate estimation and control of systematic error, or bias. Method comparison experiments are the cornerstone of this process, providing the empirical evidence to quantify the agreement between a new test method and a reference or comparative method [7]. For researchers and drug development professionals, establishing robust, statistically sound acceptance criteria for this bias is not merely a technical exercise—it is a regulatory imperative. This guide provides a structured framework for designing, executing, and interpreting method comparison studies, with a focus on establishing defensible acceptance criteria for bias within a regulatory context. We will objectively compare different statistical approaches and data presentation techniques, supported by experimental data and clear protocols.
Core Principles of Method Comparison
A method comparison experiment is fundamentally designed to estimate the inaccuracy or systematic error of a test method relative to a comparative method [7]. The interpretation of the results, however, is entirely dependent on the quality of the comparative method.
- Selecting a Comparative Method: The ideal comparative method is a reference method, a designation that implies its correctness is well-documented through definitive methods and traceable reference materials. In such cases, any observed discrepancy is confidently attributed to the test method [7]. When using a routine method for comparison, differences must be interpreted with caution, as it may be unclear which method is the source of error. In these scenarios, additional experiments, such as recovery or interference studies, are necessary to resolve ambiguity [7].
- Defining Systematic Error: Systematic error can manifest as a constant shift affecting all measurements equally (constant error) or as an error that changes proportionally with the analyte concentration (proportional error) [7]. The systematic error at a specific medical decision concentration ((X_c)) is the primary metric of interest for assessing a method's clinical acceptability [7].
Experimental Design and Protocols
The validity of the acceptance criteria is a direct function of the experimental design. A poorly executed experiment will yield unreliable estimates of bias, regardless of the statistical sophistication applied later.
Key Experimental Design Factors
The following table summarizes the critical parameters for designing a robust comparison of methods experiment, based on established guidelines [7].
| Design Factor | Recommendation & Rationale |
|---|---|
| Number of Specimens | Minimum of 40 patient specimens [7]. Quality and range are more critical than sheer volume; specimens should cover the entire working range of the method and reflect the expected disease spectrum. Larger numbers (100-200) are recommended to assess method specificity [7]. |
| Specimen Measurement | Common practice is single measurement by each method, but duplicate measurements are advantageous. Duplicates act as a validity check, helping to identify sample mix-ups or transposition errors that could be misinterpreted as methodological bias [7]. |
| Time Period | Minimum of 5 days, ideally extending to 20 days. Analyzing specimens over multiple days and analytical runs minimizes the impact of systematic errors that could occur in a single run and provides a more realistic estimate of long-term performance [7]. |
| Specimen Stability | Specimens should be analyzed by both methods within a short time frame (e.g., two hours) to prevent degradation from altering results. Stability can be improved with preservatives, refrigeration, or freezing, but the handling protocol must be defined and consistent to ensure differences are analytical, not pre-analytical [7]. |
The workflow below outlines the key stages of a method comparison experiment, from design to statistical analysis and acceptance checking.
The Scientist's Toolkit: Essential Research Materials
The following reagents and materials are fundamental for executing a method comparison study in a bioanalytical or clinical chemistry setting.
| Item | Function & Importance |
|---|---|
| Characterized Patient Specimens | The core material. Must be ethically sourced and characterized to cover the analytical range and pathological conditions. Their commutability (behaving like fresh patient samples) is critical for a valid assessment [7]. |
| Reference Method or Material | Provides the anchor for accuracy. An FDA-cleared method, a method with established traceability to a higher-order standard (e.g., NIST), or a recognized reference laboratory serves as the benchmark [7]. |
| Quality Control (QC) Pools | Used to monitor the stability and precision of both the test and comparative methods throughout the experiment. They help ensure that observed differences are due to systematic bias and not random analytical instability [7]. |
| Statistical Analysis Software | Essential for calculating complex statistics (linear regression, error propagation) and generating visualizations (difference plots, scatter plots). Tools like R, Python (with SciPy/StatsModels), or specialized validation software are typical [7] [94]. |
Data Analysis and Visualization
The analytical phase transforms raw data into actionable estimates of systematic error.
Graphical Data Inspection
The first and most crucial step is visual inspection of the data [7]. Two primary plots are used:
- Difference Plot: Plots the difference between the test and comparative method results (test - comparative) on the y-axis against the comparative result on the x-axis. This is ideal when methods are expected to agree one-to-one. It allows for immediate visual assessment of bias, its consistency across the range, and the identification of outliers [7].
- Comparison Plot (Scatter Plot): Plots the test method result on the y-axis against the comparative method result on the x-axis. This is useful for all comparisons, especially when a 1:1 relationship is not expected. A visual line of best fit shows the general relationship between the methods [7].
Statistical Calculations for Systematic Error
While graphs provide a visual impression, statistics provide quantitative estimates.
- For a Wide Analytical Range (e.g., Glucose, Cholesterol): Linear regression analysis is the preferred technique. It provides the slope (b, estimating proportional error) and y-intercept (a, estimating constant error) of the line of best fit [7].
- The systematic error (SE) at any critical medical decision concentration ((X_c)) is calculated as:
- (Yc = a + b \times Xc)
- (SE = Yc - Xc) [7]
- The correlation coefficient (r) is also calculated. While an r ≥ 0.99 indicates a sufficiently wide data range for reliable regression estimates, it should not be used as a sole measure of acceptability [7].
- The systematic error (SE) at any critical medical decision concentration ((X_c)) is calculated as:
- For a Narrow Analytical Range (e.g., Sodium, Calcium): The average difference (or bias) between paired results is a more straightforward and often more appropriate measure. This is typically derived from a paired t-test analysis, which also provides a standard deviation of the differences and a t-value to assess statistical significance [7].
Advanced Error Estimation: Error Propagation
In complex experiments where a result is calculated from multiple measured parameters (e.g., flux in membrane filtration), the total experimental error must account for all contributing factors. Error propagation is a vital technique for this, where the errors from individual measurements are combined according to a specific formula to estimate the overall error of the calculated parameter [94]. This prevents the common pitfall of underestimating total experimental error. Validation of the propagated error estimate can be done by repeating a selected experiment approximately five times under identical conditions and verifying that the repeated data points fall within the estimated error range [94].
Establishing Acceptance Criteria
Acceptance criteria are pre-defined limits for bias that are grounded in the clinical or analytical requirements of the test.
- Basis in Clinical Guidelines: For many established tests, clinical practice guidelines or recommendations from bodies like the National Academy of Clinical Biochemistry (NACB) or the American Diabetes Association provide desirable specifications for total error, from which allowable bias can be derived.
- Statistical versus Clinical Significance: A statistically significant bias (e.g., a low p-value in a t-test) may be clinically irrelevant if its magnitude is small. Conversely, a bias that is not statistically significant due to a small sample size could still be clinically unacceptable. The acceptance criteria must be based on clinical, not just statistical, consequences.
- Regulatory Frameworks for Novel Data Types: The emergence of synthetic data in pharmaceutical research (e.g., for pharmacovigilance signal detection or clinical trial simulation) introduces new validation paradigms. Acceptance criteria for these datasets must rigorously assess:
- Statistical Fidelity: How well marginal and joint distributions of key variables (e.g., drug usage, adverse events) match the real-world benchmark data [95].
- Analytical Utility: Whether analyses performed on the synthetic data (e.g., training a predictive model) yield outcomes consistent with those from the original data. Performance is often measured by metrics like Area Under the Curve (AUC); for example, a model trained on synthetic hematology data achieved fidelity metrics with ≥85% agreement with real data [95].
Comparison of Data Analysis Methods
The choice of statistical method depends on the data range and the nature of the comparison. The table below provides a comparative overview.
| Analysis Method | Primary Use Case | Key Outputs | Strengths | Limitations |
|---|---|---|---|---|
| Linear Regression | Wide analytical range; to model proportional and constant error [7] | Slope (b), Intercept (a), Standard Error of Estimate (Sy/x) | Quantifies constant and proportional error; allows SE estimation at any decision level [7] | Requires wide data range (r ≥ 0.99 is ideal); sensitive to outliers [7] |
| Average Difference (Bias) | Narrow analytical range; simple assessment of overall bias [7] | Mean Bias, Standard Deviation of Differences | Simple to calculate and interpret; robust for narrow ranges [7] | Does not distinguish between constant and proportional error; less informative for wide ranges. |
| Error Propagation | Complex, calculated outcomes; overall system error estimation [94] | Total Propagated Experimental Error | Provides a more complete and realistic error estimate by incorporating all known uncertainty sources [94] | Requires identification and quantification of all individual error sources; can be mathematically complex [94]. |
The following diagram illustrates the decision-making process for selecting the appropriate statistical method based on the data characteristics.
Establishing acceptance criteria for bias is a systematic process that integrates sound experimental design, rigorous data analysis, and clinically relevant benchmarks. There is no universal statistical method; the choice between linear regression, average difference, or error propagation depends entirely on the data structure and the study's objectives. By adhering to the principles outlined in this guide—from careful specimen selection to the application of appropriate statistical models and validation techniques like error propagation—researchers and drug development professionals can generate defensible evidence of method validity. This evidence is crucial for satisfying regulatory requirements and ensuring that analytical methods produce reliable, actionable data in the critical context of pharmaceutical development and patient care.
Conclusion
Systematic error estimation is not merely a statistical exercise but a fundamental component of method validation that directly impacts the reliability of scientific conclusions and patient outcomes. A rigorous approach encompassing robust study design, appropriate statistical analysis using Bland-Altman and regression methods, proactive troubleshooting with quality control procedures, and thorough validation against standards is essential. Future directions include the development of more sophisticated error models that account for complex, real-world measurement scenarios, the integration of machine learning techniques for automated bias detection, and the establishment of standardized reporting guidelines for method comparison studies to enhance reproducibility and trust in biomedical research.
References
- 1. Random vs. Systematic Error | Definition & Examples [https://www.scribbr.com/methodology/random-vs-systematic-error/]
- 2. Systematic Error - an overview [https://www.sciencedirect.com/topics/engineering/systematic-error]
- 3. Random Error vs Systematic Error [https://statisticsbyjim.com/basics/random-error-vs-systematic-error/]
- 4. Random vs. Systematic Error [https://www.physics.umd.edu/courses/Phys276/Hill/Information/Notes/ErrorAnalysis.html]
- 5. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 6. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 7. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 8. [Systematic errors in clinical studies : A comprehensive ... [https://pubmed.ncbi.nlm.nih.gov/28236001/]
- 9. Systematic Error Detection in Laboratory Medicine [https://www.intechopen.com/chapters/58071]
- 10. 50 Standardization and quality assurance of quantitative ... [https://clinical-laboratory-diagnostics.com/k50.html]
- 11. Differentiate Precision and Accuracy in Clinical Research ... [https://www.bioaccessla.com/blog/differentiate-precision-and-accuracy-in-clinical-research-steps]
- 12. Measurement of Errors in Clinical Laboratories - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3689332/]
- 13. Regulating medical AI before midnight strikes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360511/]
- 14. Evaluating accountability, transparency, and bias in AI ... [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-025-01243-z]
- 15. Appraising Important Medical Literature Biases [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.925643/full]
- 16. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 17. Uncertainty of Measurement: A Review of the Rules for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3387884/]
- 18. The difference between precision, trueness and accuracy [https://www.dewetron.com/news/the-difference-between-precision-trueness-and-accuracy/]
- 19. Precision vs Accuracy in Metrology [https://advancedspectral.com/precision-vs-accuracy/]
- 20. Practices of Science: Precision vs. Accuracy [https://manoa.hawaii.edu/exploringourfluidearth/physical/world-ocean/map-distortion/practices-science-precision-vs-accuracy]
- 21. Precision vs. Accuracy: Why the Difference Matters in ... [https://www.simco.com/blog/precision-vs-accuracy-why-the-difference-matters-in-calibration/]
- 22. Accuracy Error Tolerance and Uncertainty in Calibration ... [https://www.tek.com/en/blog/accuracy-error-tolerance-and-uncertainty-in-calibration-results]
- 23. Measurement Uncertainty (MU), Accuracy, Precision [https://elsmar.com/elsmarqualityforum/threads/measurement-uncertainty-mu-accuracy-precision-relationship.26804/]
- 24. Distinguishing Constant and Variable Bias in Systematic ... [https://www.mdpi.com/2673-8244/5/4/67]
- 25. Bias in Laboratory Medicine: The Dark Side of the Moon [https://pmc.ncbi.nlm.nih.gov/articles/PMC10485854/]
- 26. Different types of bias [https://eclinpath.com/test-basics/quality-assurance/print-21/]
- 27. Comparing methods of measurements [https://pubmed.ncbi.nlm.nih.gov/9075596/]
- 28. Estimating Systematic Error of Measurement Procedures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5952177/]
- 29. Bland-Altman methods for comparing methods of ... [https://www.sciencedirect.com/science/article/pii/S2590113320300298]
- 30. Average bias - Method comparison / Agreement [https://analyse-it.com/docs/user-guide/method-comparison/average-bias]
- 31. Observational error [https://en.wikipedia.org/wiki/Observational_error]
- 32. Utilizing tables, figures, charts and graphs to enhance the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394528/]
- 33. Understanding Bland Altman analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470095/]
- 34. Bland-Altman Plot: Assessing Agreement [https://numiqo.com/tutorial/bland-altman-plot]
- 35. Interpreting results: Bland-Altman [https://www.graphpad.com/guides/prism/latest/statistics/bland-altman_results.htm]
- 36. Bland-Altman plot - MedCalc Statistical Software Manual [https://www.medcalc.org/en/manual/bland-altman-plot.php]
- 37. Bland-Altman Plot [https://real-statistics.com/reliability/interrater-reliability/bland-altman-analysis/bland-altman-plot/]
- 38. BA-plotteR – A web tool for generating Bland-Altman plots ... [https://www.sciencedirect.com/science/article/abs/pii/S0034528821001715]
- 39. Method Comparison | Bland-Altman Plot [https://www.ncss.com/software/ncss/method-comparison-in-ncss/]
- 40. BA-plotteR - A web tool for generating Bland-Altman plots ... [https://pubmed.ncbi.nlm.nih.gov/34058399/]
- 41. Bland–Altman plot [https://en.wikipedia.org/wiki/Bland%E2%80%93Altman_plot]
- 42. Linear Method comparison [https://analyse-it.com/docs/230/user-guide/method-evaluation/linear]
- 43. Z-14: Estimating Analytical Errors Using Regression Statistics [https://www.westgard.com/lessons/z-stats-basic-statistics/lesson44.html]
- 44. Systematic errors in Data Analysis [https://codefinity.com/blog/Systematic-errors-in-Data-Analysis]
- 45. Why your laboratory should never use ordinary linear ... [https://finbiosoft.com/linear-regression-olr-wls-deming-passing-bablok/]
- 46. How to compare regression models [https://people.duke.edu/~rnau/compare.htm]
- 47. Bland-Altman Analysis - Guide [https://sec.lumc.nl/method_agreement_analysis/guide.html]
- 48. Limits of Agreement Based on Transformed Measurements [https://www.mdpi.com/2571-905X/8/1/17]
- 49. Nonparametric Limits of Agreement in Method Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7698333/]
- 50. Confidence Interval for Bland-Altman [https://real-statistics.com/reliability/interrater-reliability/bland-altman-analysis/confidence-interval-bland-altman/]
- 51. Agreement & Tolerance Limits • SimplyAgree [https://aaroncaldwell.us/SimplyAgree/articles/agreement_analysis.html]
- 52. Sample size calculation: Bland-Altman plot [https://www.medcalc.org/en/manual/sample-size-bland-altman.php]
- 53. Using multiple agreement methods for continuous repeated ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01022-x]
- 54. Paired t-Test | Introduction to Statistics [https://www.jmp.com/en/statistics-knowledge-portal/t-test/paired-t-test]
- 55. 4.5 - Paired Samples | STAT 200 [https://online.stat.psu.edu/stat200/lesson/4/4.6]
- 56. Assessing method agreement for paired repeated binary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7233794/]
- 57. Paired Comparison (Methods, Examples, Tools) [https://www.opinionx.co/blog/paired-comparison]
- 58. Systematic Errors in Research: Definition, Examples [https://www.formpl.us/blog/systematic-research-errors]
- 59. Paired Testing [https://www.urban.org/research/data-methods/data-analysis/quantitative-data-analysis/impact-analysis/paired-testing]
- 60. Optimal Procedures for Detecting Analytic Bias Using ... [https://pubmed.ncbi.nlm.nih.gov/9291452/]
- 61. Unsupervised bias detection tool [https://algorithmaudit.eu/technical-tools/bdt/]
- 62. A Detailed Look at How Modern Laboratory Information ... [https://www.ligolab.com/post/a-detailed-look-at-how-modern-laboratory-information-systems-fully-support-quality-control]
- 63. "Westgard Rules" and Multirules [https://www.westgard.com/westgard-rules.html]
- 64. Implementation of new Westgard rules suggested by the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11654237/]
- 65. Reply to Christelli et al.: Implementation of new Westgard ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12161511/]
- 66. 2025 IFCC Recommendations for IQC [https://www.westgard.com/essays/quality-requirements-and-standards/ifcc-iqc-2025.html]
- 67. FAQ's about controls and out-of-controls - Westgard QC [https://www.westgard.com/questions/quest9.html]
- 68. Calibration experiments: An alternative to multi-method ... [https://www.sciencedirect.com/science/article/pii/S0148296325001754?dgcid=rss_sd_all]
- 69. Experiment-based calibration in psychology [https://pmc.ncbi.nlm.nih.gov/articles/PMC11158008/]
- 70. Interference and Recovery Experiments - Westgard QC [https://www.westgard.com/lessons/basic-method-validation/lesson27.html]
- 71. Measurements and Error Analysis [https://www.webassign.net/question_assets/unccolphysmechl1/measurements/manual.html]
- 72. The Measurement Error Elephant in the Room [https://pmc.ncbi.nlm.nih.gov/articles/PMC9005058/]
- 73. Impact on Nutrition Research and Adjustment for its Effects [https://prevention.cancer.gov/tools-resources/measurement-error-impact-nutrition-research-and-adjustment-its-effects]
- 74. Measurement error in occupation and the impact on ... [https://www.sciencedirect.com/science/article/abs/pii/S0276562419302458]
- 75. Systematic Error - an overview [https://www.sciencedirect.com/topics/computer-science/systematic-error]
- 76. Reporting of measures against bias in nonclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12398162/]
- 77. A New Era for Analytical Procedure Lifecycle Management [https://synergbiopharma.com/navigating-analytical-method-comparability-and-equivalency-under-ich-q14-a-new-era-for-analytical-procedure-lifecycle-management/]
- 78. Specification Equivalence—A Practical Approach [https://www.pharmtech.com/view/specification-equivalence-a-practical-approach]
- 79. Gold standard (test) [https://grokipedia.com/page/Gold_standard_(test)]
- 80. Behavior of test specificity under an imperfect gold standard [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125893/]
- 81. The London Study (MELONS) - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275175/]
- 82. Systematic review of statistical approaches to quantify, or ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0421-6]
- 83. Points of Care in Using Statistics in Method-Comparison ... [https://www.westgard.com/essays/method-validation/essay19.html]
- 84. Adjustment for Measurement Error in Evaluating Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3808490/]
- 85. mitigating bias due to measurement error in real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464481/]
- 86. Total Analytic Error [https://myadlm.org/cln/articles/2013/september/total-analytic-error]
- 87. Measurement error and bias in real-world oncology ... [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2024.1423493/full]
- 88. Performance of Regression Models as a Function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8243133/]
- 89. 7 Regression Techniques You Should Know! [https://www.analyticsvidhya.com/blog/2015/08/comprehensive-guide-regression/]
- 90. Comparison of Regression Analysis Algorithms - Gursev Pirge [https://gursev-pirge.medium.com/comparison-of-regression-analysis-algorithms-db710b6d7528]
- 91. A Comparative Analysis on Prediction Performance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8587803/]
- 92. Regression techniques under ISO 9972 – a comparative ... [https://www.aivc.org/resource/regression-techniques-under-iso-9972-comparative-analysis]
- 93. Predicting Wear Damage in Moving Mechanical Contacts ... [https://www.sciencedirect.com/science/article/abs/pii/S0019057825004562]
- 94. Tutorial review of error evaluation in experimental water ... [https://www.sciencedirect.com/science/article/pii/S0045653524007264]
- 95. Synthetic Data in Pharma: A Guide to Acceptance Criteria [https://intuitionlabs.ai/articles/synthetic-data-pharma-acceptance-criteria]