A Practical Guide to Minimizing Systematic Error in Method Comparison Studies for Robust Biomedical Research
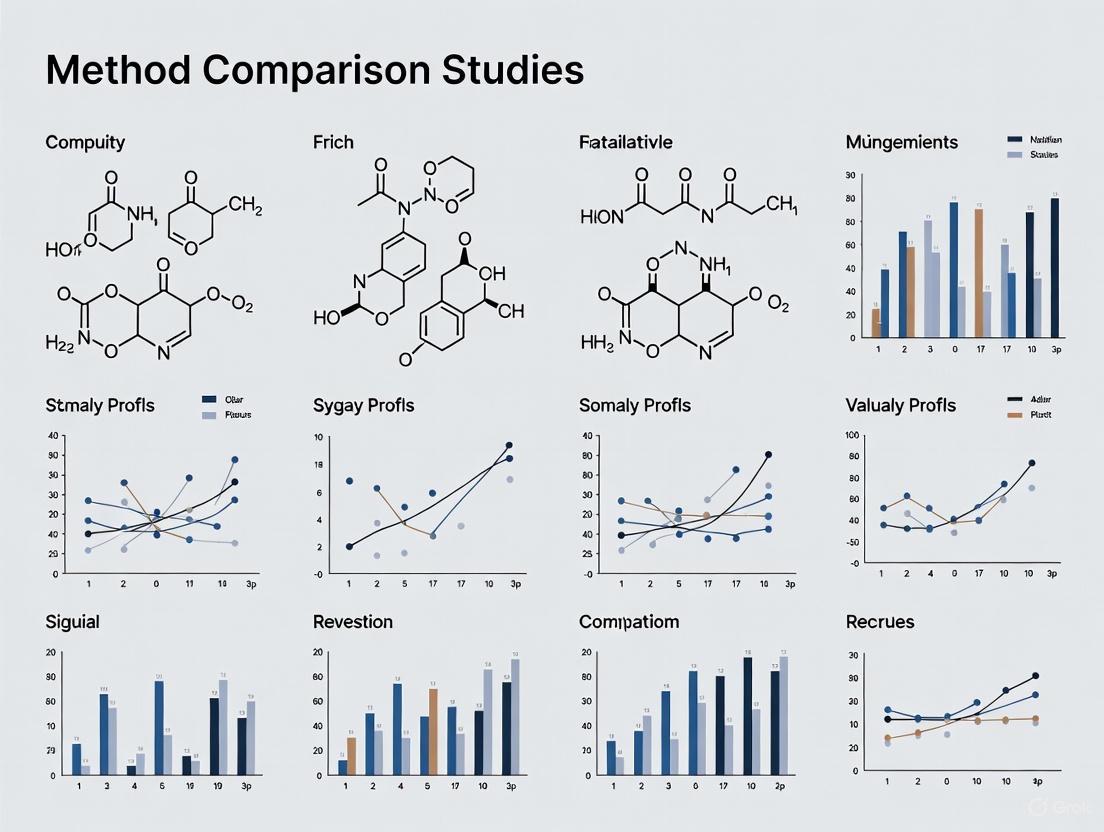
This article provides a comprehensive framework for researchers and drug development professionals to understand, identify, and minimize systematic error (bias) in method comparison studies.
A Practical Guide to Minimizing Systematic Error in Method Comparison Studies for Robust Biomedical Research
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to understand, identify, and minimize systematic error (bias) in method comparison studies. Covering foundational concepts to advanced troubleshooting, it details rigorous experimental designs for detecting constant and proportional bias, strategies for handling method failure, and robust statistical techniques for validation. By synthesizing current best practices, this guide aims to enhance the reliability and accuracy of analytical data, which is fundamental for valid scientific conclusions and sound clinical decision-making.
Understanding Systematic Error: Definitions, Sources, and Impact on Data Integrity
Troubleshooting Guides
Guide 1: Identifying and Diagnosing Systematic Error in Your Data
Problem: Your experimental results are consistently skewed away from the known true value or results from a standard method, even after repeating the experiment.
Solution: Follow this diagnostic pathway to confirm the presence and identify the source of systematic error.
Diagnostic Steps:
- Calibrate Your Instrument: Use a traceable standard reference material (SRM) with a known concentration. If your measurements consistently read higher or lower than the standard's value by a fixed amount, a constant systematic error (offset error) is likely present [1] [2]. If the difference changes proportionally with the value, you may have a proportional systematic error (scale factor error) [3] [1].
- Method Comparison Analysis: Analyze a minimum of 40 patient specimens covering the entire analytical range using both your test method and a validated comparative method (e.g., a reference method) [4]. The data analysis should involve more than just a correlation coefficient.
- Create a Difference Plot: Plot the differences between the test and comparative method (test - comparative) on the y-axis against the average of the two values or the comparative method value on the x-axis [4]. Visual inspection of this plot is a fundamental diagnostic tool.
- Interpret the Pattern:
- If the data points on the difference plot are scattered randomly around the zero line, systematic error is minimal.
- If all data points are consistently above or below the zero line, a constant systematic error is present [4] [5].
- If the data points show a trend (e.g., positive differences at low concentrations and negative differences at high concentrations), a proportional systematic error is present [4].
Guide 2: Resolving a High Systematic Error in a Method Comparison Study
Problem: A method comparison experiment has revealed a medically significant systematic error that makes your new method unacceptable for use.
Solution: Systematically investigate and correct the primary sources of bias.
Resolution Steps:
- Inspect and Calibrate Equipment: Recalibrate all instruments, including balances, pipettes, and volumetric flasks, against certified standards before the experiment and at regular intervals [6]. Check for instrument drift over time.
- Review Analytical Method: Scrutinize your method for inherent flaws, such as incomplete chemical reactions, incorrect sampling procedures, or unaccounted-for interferences from the sample matrix or reagents [6]. Perform a recovery experiment to check for specific interferences.
- Verify Reagents: Ensure all chemicals and reagents are pure, not decomposed, and correctly labeled [6]. Contaminated reagents are a common source of error.
- Standardize Analyst Technique: Implement detailed Standard Operating Procedures (SOPs) for both the method and instrument operation [6]. Provide training to eliminate analyst-specific errors, such as misreading menisci or improper instrument setup [7].
- Control the Environment: Document and control environmental factors like temperature, humidity, and electrical line voltage, as fluctuations can introduce systematic bias, especially in sensitive instrumental analyses [6] [7].
Frequently Asked Questions (FAQs)
Q1: Why can't we just use a larger sample size to eliminate systematic error, like we can with random error?
A: Systematic error (bias) cannot be reduced by increasing the sample size because it consistently pushes measurements in the same direction [5]. Every data point is skewed equally, so averaging a larger number only gives a more precise, but still inaccurate, result. In contrast, random error causes variations both above and below the true value. These variations tend to cancel each other out when averaged over a large sample, bringing the average closer to the true value [3] [5].
Q2: In a method comparison study, what is a more reliable statistic than the correlation coefficient (r) for assessing agreement?
A: While a high correlation coefficient (e.g., r > 0.99) indicates a strong linear relationship, it does not prove the methods agree. A test method could consistently show results 20% higher than the reference method and still have a perfect correlation. For assessing agreement, it is preferable to use linear regression analysis to calculate the slope and y-intercept [4]. The slope indicates a proportional error, and the y-intercept indicates a constant error. You can then use these values to calculate the systematic error at critical medical decision concentrations [4].
Q3: What is the single most effective action to minimize systematic error in my experiments?
A: There is no single solution, but the most robust strategy is triangulation—using multiple, independent techniques or instruments to measure the same thing [3] [1] [5]. If different methods and instruments all yield convergent results, you can be more confident that systematic error is minimal. This should be complemented by regular calibration of equipment against certified standards and the use of randomization in sampling and assignment to balance out unknown biases [3].
Q4: How can an experimenter's behavior introduce systematic error, and how can we prevent it?
A: Experimenters can unintentionally influence results through their spoken language, body language, or facial expressions, which can shape participant responses or performance (a form of response bias) [7]. To prevent this:
- Use masking (blinding) so neither the participant nor the experimenter knows which treatment group or condition is being tested [3].
- Provide experimenters with strict, written Standard Operating Procedures (SOPs) to ensure consistency [6] [7].
- Use pre-recorded instructions for all participants to guarantee identical delivery [7].
Data Presentation
Table 1: Characterizing Random and Systematic Error
This table summarizes the core differences between the two error types, which is fundamental for troubleshooting.
| Feature | Random Error | Systematic Error |
|---|---|---|
| Definition | Unpredictable fluctuations causing variation around the true value [3] [5] | Consistent, reproducible deviation from the true value [3] [7] |
| Effect on Data | Introduces variability or "noise"; affects precision [3] [5] | Introduces inaccuracy or "bias"; affects accuracy [3] [5] |
| Direction | Occurs equally in both directions (high and low) [5] | Always in the same direction (consistently high or low) [7] |
| Reduced by | Taking repeated measurements, increasing sample size [3] [5] | Improving calibration, triangulation, blinding, randomization [3] [1] |
| Eliminated by Averaging? | Yes, errors cancel out over many measurements [3] [5] | No, averaging does not remove consistent bias [2] [5] |
Table 2: Essential Materials for a Method Comparison Study
This toolkit lists critical reagents and materials needed to conduct a robust comparison of methods experiment.
| Item | Function & Importance |
|---|---|
| Certified Reference Material (CRM) | A substance with a known, traceable quantity of analyte. Serves as the gold standard for calibrating instruments and assessing method accuracy [4] [6]. |
| Well-Characterized Patient Specimens | At least 40 specimens covering the entire analytical range of the method. They should represent the expected pathological spectrum to properly evaluate performance across all clinically relevant levels [4]. |
| Reference/Comparative Method | A method (preferably a recognized reference method) whose correctness is well-documented. Differences from this method are attributed to the test method's error [4]. |
| Calibrated Pipettes & Volumetric Flasks | Precisely calibrated glassware and pipettes are essential for accurate sample and reagent preparation. Uncalibrated tools are a primary source of systematic error [6]. |
| Statistical Software | Required for calculating linear regression statistics (slope, intercept) and creating difference plots, which are necessary for quantifying systematic error [4]. |
Experimental Protocol: The Comparison of Methods Experiment
Purpose: To estimate the inaccuracy or systematic error of a new test method by comparing it to a comparative method using real patient specimens [4].
Methodology:
Specimen Selection:
- Collect a minimum of 40 different patient specimens.
- Select specimens to cover the entire working range of the method.
- Ensure the specimens represent the spectrum of diseases and conditions expected in routine practice [4].
Experimental Procedure:
- Analyze each specimen using both the test method (new method under evaluation) and the comparative method (established method) [4].
- Analyze specimens in a single run or, preferably, over multiple days (minimum of 5 days is recommended) to account for day-to-day variability [4].
- Analyze specimens within a short time frame (e.g., 2 hours) of each other to ensure specimen stability, unless specific handling procedures (e.g., freezing) are validated [4].
- Ideally, perform duplicate measurements on different aliquots of the sample to identify and prevent errors from sample mix-ups or transcription mistakes [4].
Data Analysis:
- Graphical Analysis: Create a difference plot (test result - comparative result vs. comparative result) to visually inspect for constant or proportional trends and identify outliers [4].
- Statistical Calculation:
- Interpretation: The calculated systematic error (SE) should be compared to pre-defined, medically acceptable limits to judge the acceptability of the new method.
Systematic errors are consistent, reproducible inaccuracies that can compromise the validity of biomedical assay results. Unlike random errors, which vary unpredictably, systematic errors introduce bias in the same direction across measurements, potentially leading to false conclusions in method comparison studies and drug development research. This technical support guide identifies common sources of systematic error in biomedical testing and provides detailed troubleshooting methodologies to help researchers minimize these errors, thereby enhancing data quality and research outcomes.
Troubleshooting Guide: Identifying and Rectifying Systematic Errors
How do sample matrix effects cause systematic error in LC-MS/MS analyses?
Issue: Matrix effects represent a significant source of systematic error in liquid chromatography-tandem mass spectrometry (LC-MS/MS), particularly causing ion suppression or enhancement that compromises quantitative accuracy.
Background: Matrix effects occur when co-eluting components from biological samples alter the ionization efficiency of target analytes. In biomonitoring studies assessing exposure to environmental toxicants, these effects can lead to inaccurate measurements of target compounds if not properly characterized and controlled [8].
Primary Mechanisms:
- Electrospray Ionization (ESI) Vulnerability: ESI is particularly susceptible to ion suppression because matrix components can interfere with charge addition to analytes in the liquid phase or inhibit transfer of ions to the gas phase [8].
- Competition for Charge: Matrix components compete with target analytes for available charges in the liquid phase [8].
- Altered Droplet Properties: Interfering compounds increase viscosity and surface tension of ESI droplets, reducing analyte transfer efficiency to the gas phase [8].
Troubleshooting Protocol:
- Sample Preparation Assessment: Compare protein precipitation (PPT), liquid-liquid extraction (LLE), and solid-phase extraction (SPE) methods. Mixed-mode SPE sorbents combining reversed-phase and ion exchange mechanisms provide the cleanest extracts [9].
- Chromatographic Optimization: Manipulate mobile phase pH to alter retention of basic compounds relative to phospholipids. Implement UPLC technology instead of HPLC for significant improvement in reducing matrix effects [9].
- Ionization Technique Evaluation: Consider atmospheric pressure chemical ionization (APCI) as it is generally less susceptible to matrix effects compared to ESI [8].
- Matrix Effect Quantification: Use post-column infusion to monitor suppression/enhancement regions or prepare calibration standards in biological matrix to assess quantification accuracy [8].
What systematic errors arise from improper calibration practices?
Issue: Inaccurate calibration introduces systematic errors that propagate through all subsequent measurements, affecting method comparison studies.
Background: Calibration errors can occur from using improper standards, unstable reference materials, or incorrect calibration procedures. For example, in amino acid assay by ion-exchange chromatography, using different commercial standards led to systematic errors during sample calibration [10].
Troubleshooting Protocol:
- Reference Standard Verification: Use certified reference materials with documented purity. Verify any commercial standards against certified reference materials before use [10].
- Calibration Curve Validation: Establish multiple calibration points covering the entire analytical measurement range. Verify linearity through statistical analysis [11].
- Regular Recalibration: Implement a calibration schedule based on instrument severity of use, environmental conditions, and required accuracy. Frequently used devices should be checked and recalibrated regularly [11].
- Cross-Validation: Compare results with reference methods when possible. In method comparison studies, analyze at least 40 patient specimens covering the entire working range of the method [4].
How does sample preparation introduce systematic errors?
Issue: Sample preparation techniques can introduce systematic errors through analyte loss, contamination, or incomplete processing.
Background: Deproteinization of plasma for amino acid assays clearly enlarges the coefficient of variation in the determination of cystine, aspartic acid, and tryptophan. Losses of hydrophobic amino acids occur during this process, particularly when the supernatant volume is small [10].
Troubleshooting Protocol:
- Deproteinization Optimization: For plasma amino acid assays, remove supernatant promptly after deproteinization. Delaying removal for 1 hour decreases tryptophan concentration [10].
- Internal Standard Selection: Use stable isotope-labeled internal standards that closely mimic analyte behavior. Note that correction for hydrophobic amino acid losses using internal standards may not be possible [10].
- Extraction Efficiency Determination: Calculate recovery percentages for each sample preparation method. Pure cation exchange SPE and mixed-mode SPE provide cleaner extracts with reduced matrix effects compared to protein precipitation [9].
- Process Standardization: Strictly control timing, temperature, and handling procedures across all samples to minimize variation.
What environmental and storage conditions cause systematic errors?
Issue: Improper sample storage and environmental control during analysis introduce systematic errors through analyte degradation or altered instrument performance.
Background: Systematic errors due to storage of plasma for amino acid assay include degradation of glutamine and asparagine at temperatures above -40°C. The concentration of cystine decreases considerably during storage of non-deproteinized plasma [10].
Troubleshooting Protocol:
- Temperature Control: Store deproteinized plasma at -40°C or lower to maintain amino acid concentrations for at least one year. For non-depproteinized plasma, neutralize samples before storage to minimize degradation [10].
- Environmental Monitoring: For multiparameter patient simulators, maintain operating temperature between 10°C and 40°C with humidity between 10% and 90% [11].
- Stability Testing: Conduct stability studies under various storage conditions. Avoid correction for changes due to storage as it is often impossible [10].
- Equipment Acclimation: Allow calibrators to stabilize at room temperature before use. Turn on multiparameter patient simulators 10 minutes before calibration [11].
How do instrument-related factors contribute to systematic errors?
Issue: Instrument characteristics and settings can introduce systematic errors through measurement limitations or inappropriate configuration.
Background: In biomedical testing, load cell measurement errors are common, especially in low-force measurements. The accuracy may be presented as a percentage of reading (relative accuracy) or percentage of full scale (fixed accuracy) [12].
Troubleshooting Protocol:
- Load Cell Specification: Verify load cell operating range matches experimental needs. For low-force measurements, ensure relative accuracy covers the expected measurement range [12].
- Bandwidth Configuration: Set appropriate system bandwidth based on event duration. For events lasting 0.2 seconds, ensure rise time is sufficiently fast to capture peak forces [12].
- Data Rate Optimization: Adjust sampling rate to capture critical events without creating excessively large files. Higher data rates do not necessarily yield additional information [12].
- Regular Performance Verification: Implement scheduled calibration checks for all instruments. For centrifuges, calibrate every six months using tachometers to verify RPM accuracy [11].
Systematic Error Comparison Tables
Table 1: Common Systematic Errors in Biomedical Testing and Their Characteristics
| Error Source | Impact on Results | Detection Method | Common Affected Techniques |
|---|---|---|---|
| Matrix Effects | Ion suppression/enhancement | Post-column infusion | LC-ESI-MS/MS |
| Improper Calibration | Constant or proportional bias | Method comparison | All quantitative techniques |
| Sample Preparation | Analyte loss/contamination | Recovery experiments | Sample extraction methods |
| Storage Conditions | Analyte degradation | Stability studies | Biobank samples, labile analytes |
| Instrument Configuration | Measurement inaccuracy | Reference materials | Mechanical testing, centrifugation |
Table 2: Systematic Error Management Strategies Across Experimental Phases
| Experimental Phase | Preventive Strategy | Corrective Action | Validation Approach |
|---|---|---|---|
| Pre-Analytical | Standardized SOPs | Sample re-preparation | Process validation |
| Calibration | Certified reference materials | Curve re-fitting | Accuracy verification |
| Analysis | Internal standards | Data normalization | Quality controls |
| Post-Analytical | Statistical review | Data transformation | Method comparison |
Experimental Workflows for Systematic Error Minimization
Sample Preparation and Analysis Workflow
Method Comparison Study Design
Research Reagent Solutions for Error Reduction
Table 3: Essential Research Reagents and Materials for Systematic Error Management
| Reagent/Material | Function | Application Example | Error Mitigated |
|---|---|---|---|
| Certified Reference Standards | Calibration and accuracy verification | Preparing calibration curves | Calibration bias |
| Stable Isotope-Labeled Internal Standards | Compensation for sample preparation losses | LC-MS/MS quantification | Matrix effects, recovery variations |
| Mixed-Mode SPE Sorbents | Comprehensive sample cleanup | Biological sample preparation | Phospholipid matrix effects |
| Quality Control Materials | Monitoring analytical performance | Process verification | Instrument drift, reagent degradation |
| Matrix-Matched Calibrators | Accounting for matrix effects | Quantitative bioanalysis | Ion suppression/enhancement |
Frequently Asked Questions
How can I determine if systematic error is affecting my assay results?
Systematic error should be suspected when consistent bias is observed across multiple measurements. Detection methods include: (1) analyzing certified reference materials with known concentrations; (2) performing method comparison studies with reference methods; (3) evaluating recovery of spiked standards; and (4) analyzing quality control samples over time. A minimum of 40 patient specimens should be tested in method comparison studies, selected to cover the entire working range and representing the spectrum of expected sample types [4].
What is the most effective approach to minimize matrix effects in LC-MS/MS?
A systematic, comprehensive strategy provides the most effective approach: (1) utilize mixed-mode solid-phase extraction (combining reversed-phase and ion exchange mechanisms) for cleaner extracts; (2) optimize mobile phase pH to separate analytes from phospholipids; (3) implement UPLC technology for improved resolution; and (4) consider atmospheric pressure chemical ionization (APCI) as an alternative to electrospray ionization for less susceptible compounds. Protein precipitation alone is the least effective sample preparation technique and often results in significant matrix effects [9].
How often should calibration be performed to minimize systematic error?
Calibration frequency depends on the severity of instrument use, environmental conditions, and required accuracy. Frequently used devices should be checked and recalibrated regularly. Specific intervals vary by instrument - for example, centrifuges should be calibrated every six months and documented on a Maintenance Log [11]. The schedule should be established based on stability data and quality control performance.
Can statistical methods correct for systematic errors after data collection?
While some statistical approaches can help identify and partially adjust for systematic errors, prevention during experimental design is far more effective. Empirical calibration using negative controls (outcomes not affected by treatment) and positive controls (outcomes with known effects) can calibrate p-values and confidence intervals in observational studies [13]. However, statistical correction cannot completely eliminate systematic errors, particularly when their sources are not fully understood.
Commonly overlooked sources include: (1) environmental conditions during testing, such as temperature variations affecting material properties; (2) sample storage conditions leading to analyte degradation; (3) instrument bandwidth and data rate settings inappropriate for measurement speed; and (4) load cell characteristics mismatched to force measurement requirements. For example, testing medical consumables at room temperature rather than physiological temperature (37°C) can drastically affect results for catheters, gloves, and tubing [12].
Troubleshooting Guides
Problem: My experimental results are consistently skewed away from the known true value.
Diagnosis: This is a classic symptom of systematic error, a fixed deviation inherent in each measurement due to flaws in the instrument, procedure, or study design [14] [15]. Unlike random error, it cannot be reduced by simply repeating measurements [16].
Solution: Execute the following troubleshooting workflow to identify and correct the error.
Detailed Corrective Actions:
- Step 1: Verify Instrument Calibration: Systematic error often stems from poorly calibrated instruments [17] [14]. Use standard weights or certified reference materials to check your equipment. If found, apply a correction factor to all future measurements and include the uncertainty of this correction in your overall uncertainty budget [14].
- Step 2: Control Environmental Errors: External factors like temperature fluctuations, humidity, or vibration can introduce systematic bias [17] [15]. Monitor the environment and implement controls to maintain stable conditions throughout the experiment.
- Step 3: Standardize Experimental Procedure: Procedural errors from inconsistent methods are a common source of bias [15]. Develop and document a Standard Operating Procedure (SOP). Train all personnel to ensure the procedure is applied uniformly, eliminating variations in how measurements are taken or data is recorded (transcriptional error) [15].
- Step 4: Implement Blinding Techniques: Observer bias occurs when the researcher's expectations influence measurements [17] [16]. Use blinding (or masking) so that personnel measuring outcomes are unaware of the sample's group assignment or the expected results [16].
- Step 5: Use Certified Reference Materials (CRMs): The most robust way to detect systematic error is to measure a CRM with a known property value [14]. A significant difference between your result and the certified value confirms a systematic error, allowing for quantification and correction.
Guide 2: Mitigating Systematic Error in Clinical and Diagnostic Decisions
Problem: Diagnostic tests or clinical decisions are consistently inaccurate, leading to missed or delayed diagnoses.
Diagnosis: This indicates systematic error in a clinical context, often manifesting as cognitive bias in decision-making or information bias from flawed diagnostic systems [18] [19].
Solution: Implement strategies targeting cognitive processes and system-level checks.
Detailed Corrective Actions:
- Strategy: Deploy Clinical Decision Support Systems (CDSS): These technology-based systems provide alerts for potential issues like drug-drug interactions or reminders for necessary follow-up care [20] [21]. Evidence shows CDSS can reduce medication errors and prevent adverse drug events by providing a systematic check against human oversight [20].
- Strategy: Implement Cognitive Forcing: This involves teaching clinicians to recognize their own cognitive biases (e.g., anchoring, confirmation bias) and using metacognition (thinking about one's thinking) to challenge initial diagnoses [19]. Employing checklists for differential diagnosis is a practical cognitive forcing strategy.
- Strategy: Establish Diagnostic Audit Systems: Implement systems that provide feedback on diagnostic performance [18]. Trigger algorithms, for example, can automatically review records to identify patients with potential delayed diagnoses (e.g., those returning to the emergency department within days), allowing for review and correction of diagnostic processes [18].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between systematic error and random error?
| Aspect | Systematic Error (Bias) | Random Error |
|---|---|---|
| Cause | Flaw in instrument, method, or observer [14] [15] | Unpredictable, chance variations [17] [14] |
| Impact | Consistent offset from true value; affects accuracy [14] | Scatter in repeated measurements; affects precision [17] [14] |
| Reduction | Improved design, calibration, blinding [16] | More measurements or replication [15] |
| Quantification | Difficult to detect statistically; requires comparison to a standard [14] | Quantified by standard deviation or confidence intervals [14] |
Q2: How can I quantify the impact of a systematic error on my results? Systematic error can be represented mathematically. For instance, in epidemiological studies, the observed risk ratio ((RR{obs})) can be expressed as: [ RR{obs} = RR_{true} \times Bias ] where (Bias) represents the systematic error. If (Bias = 1), there is no error; if (Bias > 1), the observed risk is overestimated; and if (Bias < 1), it is underestimated [16]. In engineering, the maximum systematic error ((\Delta M)) for a measurement that is a function of multiple variables ((x, y, z...)) can be estimated by summing the individual systematic errors in quadrature: (\Delta M = \sqrt{\delta x^2 + \delta y^2 + \delta z^2}) [14].
Q3: What are the real-world consequences of systematic error in drug development? Systematic error in drug development can lead to incorrect conclusions about a drug's safety or efficacy, potentially resulting in the pursuit of ineffective compounds or the failure to identify toxic effects. This wastes immense resources. Conversely, using Model-Informed Drug Development (MIDD) approaches, which systematically integrate data to quantify benefit/risk, has been shown to yield significant savings, reducing cycle times by approximately 10 months and cutting costs by about $5 million per program by improving trial efficiency and decision-making [22].
Q4: What are the main types of systematic error (bias) in research on human subjects? The three primary types are:
- Selection Bias: Occurs when there is a systematic difference between the characteristics of those selected for the study and those who are not [16].
- Information Bias: Arises from inaccurate measurement of exposure or outcome variables, which can include observer bias or recall bias [16].
- Confounding: Occurs when a third variable is related to both the exposure and the outcome, distorting their apparent relationship [16].
Q5: Can digital health technology effectively reduce systematic errors in healthcare? Yes. Digital Health Technology (DHT), particularly Clinical Decision Support Systems (CDSS), has been proven effective. A 2025 systematic review found that DHT interventions reduced adverse drug events (ADEs) by 37.12% and medication errors by 54.38% on average. These systems work by providing automated, systematic checks against human cognitive biases and procedural oversights, making them a cost-effective strategy for improving medication safety [21].
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Reagent | Function / Explanation |
|---|---|
| Certified Reference Materials (CRMs) | A substance with one or more property values that are certified by a validated procedure, providing a traceable standard to detect and correct for systematic error in analytical measurements [14]. |
| Clinical Decision Support System (CDSS) | A health information technology system that provides clinicians with patient-specific assessments and recommendations to aid decision-making, systematically reducing diagnostic and medication errors [20] [21]. |
| Savitzky-Golay (S-G) Filter | A digital filter that can be used to smooth data and is integral to advanced algorithms (like the Recovery method in DIC) for mitigating undermatched systematic errors in deformation measurements [23]. |
| Cognitive Forcing Strategies | A set of cognitive tools designed to force a clinician to step back and consider alternative possibilities, thereby counteracting inherent cognitive biases like anchoring and confirmation bias [19]. |
| Trigger Algorithms | Automated audit systems that use predefined criteria (e.g., a patient returning to the ER within 10 days) to identify cases with a high probability of a diagnostic error for further review [18]. |
Key Concepts FAQ
What is the difference between accuracy, precision, and bias in method-comparison studies?
In method-comparison studies, bias is the central term describing the systematic difference between a new method and an established one [24]. It is the mean overall difference in values obtained with the two different methods [24]. Accuracy, in contrast, is the degree to which an instrument measures the true value of a variable, typically assessed by comparison with a calibrated gold standard [24]. Precision refers to the degree to which the same method produces the same results on repeated measurements (repeatability) or how closely values cluster around the mean [24]. Precision is a necessary condition for assessing agreement between methods [24].
How do constant and proportional bias differ from each other?
Constant and proportional bias are two distinct types of systematic error [25].
- Constant Bias (or Fixed Bias): One method gives values that are consistently higher (or lower) than the other by a constant amount, regardless of the measurement level [25]. For example, a scale that always reads 5 grams heavier than the true weight.
- Proportional Bias: One method gives values that are higher (or lower) than the other by an amount that is proportional to the level of the measured variable [25]. The absolute difference between methods increases as the magnitude of the measurement increases.
What is Total Error, and why is it important?
Total Error is a crucial concept for judging the overall acceptability of a method. It accounts for both the systematic error (bias) and the random error (imprecision) of the testing process [26]. The components of error are important for managing quality in the laboratory, as the total error can be calculated from these components [26]. A method is judged acceptable when the observed total error is smaller than a pre-defined allowable error for the test's medical application [26].
What statistical analysis should I use to detect constant and proportional bias?
The Pearson correlation coefficient (r) is ineffective for detecting systematic biases, as it only measures random error [25]. While difference plots (Bland-Altman plots) are popular, they do not distinguish between fixed and proportional bias [25]. Least products regression (a type of Model II regression) is a sensitive technique preferred for detecting and distinguishing between fixed and proportional bias because it accounts for random error in both measurement methods [25]. Ordinary least squares (Model I) regression is invalid for this purpose [25].
How can I minimize systematic errors in my experiments?
Systematic errors can be minimized through careful experimental design and procedure:
- Calibration: Perform the procedure on a known reference quantity and adjust the process until the known result is obtained [2].
- Apparatus Calibration: Corrects for instrumental errors by ensuring all equipment is properly calibrated [27].
- Control Determination: Running the experiment with a standard substance under identical conditions helps minimize errors [27].
- Blank Determination: Conducting a test without the sample identifies errors caused by reagent impurities [27].
- Standardization: Create a consistent, repeatable process for all experiments to prevent on-the-fly changes based on expectations [28].
Troubleshooting Guides
Issue 1: Detecting and Quantifying Bias in a New Glucose Meter
Problem: A new point-of-care blood glucose meter needs to be validated against the standard laboratory analyzer to determine if it can be used interchangeably.
Solution:
- Experimental Design:
- Collect a sufficient number of patient specimens (perform an a priori sample size calculation) [24].
- Ensure paired measurements are taken simultaneously (or as close as possible) with both methods to avoid time-based changes in the analyte [24].
- The specimens should cover the entire physiological range of glucose values for which the meter will be used [24].
- Data Analysis:
- Construct a Bland-Altman Plot: Plot the difference between the new meter and the lab method (y-axis) against the average of the two measurements (x-axis) [24] [26].
- Calculate Bias and Limits of Agreement: The overall bias is the mean of all the differences. The limits of agreement are calculated as bias ± 1.96 standard deviations of the differences, defining the range where 95% of differences between the two methods are expected to fall [24].
- Interpretation: Visually inspect the plot for patterns. A spread of points that is consistent across the average values suggests only constant bias. A pattern that fans out or forms a trend suggests proportional bias, indicating that a regression approach may be more appropriate [25].
Issue 2: Addressing High Background in a High-Throughput Screening Assay
Problem: A quantitative high-throughput screening (qHTS) for a new drug candidate shows systematic row, column, and edge effects, making it difficult to distinguish true signals from noise.
Solution: Apply normalization techniques to remove spatial systematic errors [29].
- Linear Normalization (LN):
- Standardization: For each plate, transform the raw data using the formula:
x_i,j' = (x_i,j - μ) / σ, wherex_i,jis the raw value, μ is the plate mean, and σ is the plate standard deviation [29]. - Background Subtraction: Create a background value for each well position by averaging its normalized value across all plates. Subtract this background surface from each plate [29].
- Standardization: For each plate, transform the raw data using the formula:
Non-Parametric Regression (LOESS):
- Apply a LOESS (Locally Weighted Scatterplot Smoothing) smoothing technique to the data to correct for local cluster effects. The optimal smoothing parameter (span) can be determined using criteria like the Akaike Information Criterion (AIC) [29].
Combined Approach (LNLO):
- For the most effective removal of multiple types of systematic error, first apply Linear Normalization (LN), then apply the LOESS smoothing (LO) to the result [29].
Issue 3: Unexplained Discrepancies in Method-Comparison Data
Problem: A method-comparison study shows poor agreement, but the standard correlation analysis shows a high correlation coefficient (r).
Solution: A high correlation does not indicate agreement, only that the methods are related [25]. Follow this diagnostic flowchart to identify potential causes.
Essential Materials and Reagents
Table 1: Key Research Reagent Solutions for Method-Comparison Studies
| Item | Function/Brief Explanation |
|---|---|
| Reference Standard | A substance with a known, high-purity value used to calibrate the established method and ensure its accuracy [27]. |
| Control Materials | Stable materials with known concentrations (e.g., high, normal, low) analyzed alongside patient samples to monitor the precision and stability of both methods [27]. |
| Blank Reagent | The reagent or solvent without the analyte, used in a "blank determination" to identify and correct for signals caused by the reagent itself [27]. |
| Calibrators | A set of standards used to construct a calibration curve, which defines the relationship between the instrument's response and the analyte concentration [2]. |
Experimental Protocol: Conducting a Method-Comparison Study
Objective: To estimate the systematic error (bias) between a new method and an established comparative method and determine if the new method is acceptable for clinical use [26].
Step-by-Step Methodology:
- Define Medical Requirements: Identify the critical medical decision concentrations for the analyte. This determines the required analytical range and where error estimates are most important [26].
- Sample Selection and Collection: Collect a sufficient number of patient specimens (e.g., via a priori power calculation) that cover the entire analytical range of interest, including the medical decision levels [24].
- Paired Measurements: Analyze each specimen with both the new and the established method in a randomized order, ensuring measurements are made as simultaneously as possible to avoid biological variation [24].
- Data Collection and Integrity: Record all paired results. Immediately plot the data on a comparison graph (scatter plot) to visually identify any outliers or non-linearity while specimens are still available for re-testing if needed [26].
- Statistical Analysis:
- For a Single Decision Level: If focused on one medical decision concentration, a Bland-Altman difference plot with calculation of bias and limits of agreement is often sufficient [26].
- For Multiple Decision Levels: If assessing error across a wide range, use regression analysis. If the correlation coefficient (r) is ≥ 0.99, ordinary linear regression may be suitable. If r < 0.975, use more robust techniques like Deming or Passing-Bablok regression [26].
- Interpretation and Decision: Compare the estimated systematic error (bias) and total error to the predefined allowable error. The method is acceptable if the observed error is smaller than the allowable error [26].
In method comparison studies, a core challenge is distinguishing true methodological bias from spurious associations caused by confounding factors. Directed Acyclic Graphs (DAGs) provide a powerful framework for this task by visually representing causal assumptions and clarifying the underlying data-generating processes [30]. A DAG is a directed graph with no cycles, meaning you cannot start at a node, follow a sequence of directed edges, and return to the same node [31] [32]. Within the context of minimizing systematic error, DAGs allow researchers to move beyond mere statistical correlation and reason explicitly about the mechanisms through which errors might be introduced, transmitted, or confounded [30]. This structured approach is vital for identifying which variables must be measured and controlled to obtain an unbiased estimate of the true method difference, thereby addressing the "fundamental problem of causal inference" – that we can never simultaneously observe the same unit under both test and comparative methods [30]. By framing the problem causally, DAGs help ensure that the subsequent statistical analysis targets the correct estimand for the target population.
Core Concepts of Causal DAGs
The "What" and "Why" of Directed Acyclic Graphs
A Directed Acyclic Graph (DAG) is defined by two key characteristics [31] [32]:
- Directed Edges: Each edge (or arrow) has a direction, signifying a one-way relationship or dependency from one node (vertex) to another.
- Acyclic: The graph contains no cycles or closed loops; it is impossible to start at any node, follow the directed arrows, and return to the starting node.
In causal inference, DAGs are used to represent causal assumptions, where nodes represent variables, and directed arrows (X → Y) represent the causal effect of X on Y [30]. The acyclic property reflects the logical constraint that a variable cannot be a cause of itself, either directly or through a chain of other causes.
Key Terminology and Properties
To effectively use DAGs, understanding their fundamental properties is essential:
- Reachability/Paths: A node A is reachable from node B if a directed path exists from B to A. The set of all such relationships defines the reachability relation of the DAG [31] [32].
- Topological Ordering: A DAG can be linearly ordered such that for every directed edge (U → V), node U comes before node V in the ordering. This is crucial for understanding dependency and the sequence of events [31] [32].
- Transitive Closure & Reduction: The transitive closure is a graph with the most edges that has the same reachability relation. Conversely, the transitive reduction is the graph with the fewest edges that preserves the same reachability, simplifying the diagram to only essential relationships [32].
Foundational Graphical Structures
All complex causal diagrams are built from a few elementary structures that describe the basic relationships between variables. The table below summarizes these core structures.
Table 1: Elementary Structures in Causal Directed Acyclic Graphs
| Structure Name | Graphical Representation | Causal Interpretation | Role in Error Mechanisms |
|---|---|---|---|
| Chain (Cause → Mediator → Outcome) | A → M → Y | A affects M, which in turn affects Y. | Represents a mediating pathway; controlling for M can block the path of causal influence from A to Y. |
| Fork (Common Cause) | A ← C → Y | A common cause C affects both A and Y. | Represents confounding; failing to control for C creates a spurious, non-causal association between A and Y. |
| Immoralities / Colliders (Common Effect) | A → C ← Y | Both A and Y are causes of C. | Conditioning on the collider C (or its descendant) induces a spurious association between A and Y. |
These structures form the building blocks for identifying confounding, selection bias, and other sources of systematic error.
Building Your DAG: A Step-by-Step Guide
Constructing a DAG is an iterative process that requires deep subject-matter knowledge. The following steps provide a systematic guide.
- Define the Causal Question: Precisely specify the exposure (e.g., the new test method) and the outcome (e.g., the result from a reference method) [30]. The entire DAG is built to investigate the causal effect of this exposure on this outcome.
- Identify the Target Population: Clarify the population for whom the causal knowledge is meant to generalize, as this influences the relevant variables and relationships [30].
- List Relevant Variables: Enumerate all known or plausible variables related to the exposure and outcome. This includes predictors of the outcome, causes of the exposure, and common causes of both.
- Draw Causal Relationships: Based on subject-matter expertise, draw directed arrows from causes to their effects. This step encodes your explicit assumptions about the data-generating mechanism.
- Simplify the Diagram: Apply the rules of d-separation (see Section 4.1) to check for redundant paths and consider using the transitive reduction to present the most parsimonious graph that retains all necessary causal relationships [32].
- Validate and Revise: Review the DAG with other experts and revise it as needed. Where ambiguity exists, it is good practice to report multiple plausible DAGs and conduct analyses for each [30].
Using DAGs for Error Identification and Control
The d-separation Criterion
d-separation is a fundamental graphical rule for determining, from a DAG, whether a set of variables Z blocks all paths between two other variables, X and Y. A path is blocked by Z if:
- The path contains a chain (X → M → Y) or a fork (X ← C → Y) and the middle variable M or C is in Z, or
- The path contains a collider (X → C ← Y) and neither C nor any descendant of C is in Z.
If all paths between X and Y are blocked by Z, then X and Y are conditionally independent given Z. This rule is the graphical counterpart to statistical conditioning and is essential for identifying confounding and selection bias.
Identifying Confounding Bias
Confounding is a major source of systematic error in method comparisons. A confounder is a variable that is a common cause of both the exposure and the outcome. In a DAG, confounding is present if an unblocked non-causal "back-door path" exists between exposure and outcome [30].
Diagram 1: Identifying a Confounder
To block this back-door path and obtain an unbiased estimate of the causal effect of A on Y, you must condition on the confounder, "Specimen Age". The DAG makes this adjustment strategy explicit.
Identifying Selection Bias (Collider Bias)
Selection bias, often arising from conditioning on a collider, is another pernicious source of systematic error.
Diagram 2: Inducing Selection Bias
In this DAG, "Study Inclusion" is a collider. While "True Analytic Concentration" and "Instrument Sensitivity" are independent in the full population, conditioning on "Study Inclusion" (e.g., by only analyzing specimens that produced a detectable signal) creates a spurious association between them, biasing the analysis.
Troubleshooting Guides and FAQs
FAQ 1: My DAG is Complex. How Do I Know What to Control For?
Question: My DAG has many variables and paths. I'm unsure which variables to include as covariates in my model to minimize confounding without introducing bias.
Answer: Use the back-door criterion. To estimate the causal effect of exposure A on outcome Y, a set of variables Z is sufficient to control for confounding if:
- Z blocks every back-door path (i.e., any path starting with an arrow into A) between A and Y.
- No variable in Z is a descendant of A (i.e., not affected by A).
Troubleshooting Steps:
- List all non-causal paths between your exposure (A) and outcome (Y).
- For each path, check if it is already blocked by a collider. If not, identify a variable on that path that is not a collider which you can condition on to block it.
- The minimal sufficient set is often a set of variables that blocks all unblocked back-door paths without conditioning on colliders or their descendants.
Diagram 3: Applying the Back-Door Criterion
In this DAG, the set Z = {C1, C2} is sufficient to control for confounding. It blocks the back-door paths A ← C1 → Y and A ← C2 → Y. Controlling for "Lab Temperature" is unnecessary as it is not a common cause.
FAQ 2: Why Did My Bias Get Worse After Adjusting for a Variable?
Question: I adjusted for a variable I thought was a confounder, but the association between my exposure and outcome became stronger and more biased. What happened?
Answer: This is a classic symptom of having adjusted for a collider or a descendant of a collider. Conditioning on a collider opens a spurious path between its causes, which can create or amplify bias.
Troubleshooting Steps:
- Revisit your DAG and identify all colliders (variables with two or more arrows pointing into them).
- Check if you have conditioned (e.g., matched, stratified, or included as a covariate) on any of these colliders or variables caused by them (their descendants).
- If you find one, re-run your analysis without conditioning on that variable. Alternatively, use more advanced methods like inverse probability weighting to handle the selection without conditioning.
FAQ 3: How Do I Handle Unmeasured Confounding?
Question: My DAG suggests a crucial confounder exists, but I did not collect data on it. Is my causal inference doomed?
Answer: While an unmeasured confounder poses a serious threat to validity, your DAG still provides valuable insights and options.
Troubleshooting Steps:
- Sensitivity Analysis: Use the structure of your DAG to inform a quantitative sensitivity analysis. This analysis estimates how strong the unmeasured confounder would need to be to explain away the observed effect.
- Instrumental Variables (IV): Sometimes, a DAG can help identify a valid instrumental variable (Z), which affects Y only through its effect on A and is not affected by the unmeasured confounder. IV methods can provide unbiased effect estimates under these conditions.
- Proxy Controls: If you have a measured variable that is a proxy (an imperfect measure) of the unmeasured confounder, it may be possible to use it to partially control for confounding.
DAGs in Action: Experimental Protocol for a Method Comparison Study
The following protocol integrates DAGs into the design and analysis of a method comparison study, a key activity for minimizing systematic error in analytical research [4].
Protocol: Method Comparison with Causal Reasoning
Purpose: To estimate the systematic error (inaccuracy) between a new test method and a comparative method, using causal diagrams to guide the experimental design and statistical analysis, thereby minimizing confounding and other biases [4].
Pre-Experimental Steps:
- Define Causal Question: "What is the systematic error of the new method compared to the reference method for measuring analyte X in human serum?"
- Define Target Population: The general adult population with suspected disorders of X.
- Construct DAG: Before collecting data, assemble a team of experts to draft a DAG. Include variables such as: Test Method, Reference Method Result, Specimen Matrix, Hemolysis, Lipemia, Icterus, Patient Age, Disease Status, Laboratory Technician, and Batch Effect.
Experimental Execution [4]:
- Specimen Selection: A minimum of 40 patient specimens should be tested, selected to cover the entire working range of the method. The quality and range of specimens are more critical than a large number.
- Measurement: Analyze each specimen using both the test and comparative methods. Ideally, perform measurements in duplicate, with the duplicates analyzed in different runs or in a different order to identify sample mix-ups or transposition errors.
- Time Period: Conduct the experiment over a minimum of 5 days, and ideally up to 20 days, to capture and average out day-to-day systematic variations.
- Specimen Handling: Analyze specimens by both methods within two hours of each other to minimize differences due to specimen instability. Define and systematize specimen handling procedures (e.g., centrifugation, storage temperature) prior to the study.
Data Analysis Guided by DAG [4]:
- Graphical Inspection: Create a difference plot (test result minus reference result vs. reference result) or a scatterplot (test result vs. reference result). Visually inspect for outliers and patterns.
- Statistical Modeling: Based on the pre-specified DAG, identify the minimal sufficient set of covariates for adjustment. If the DAG indicates no confounding, a simple linear regression of the test result on the reference result may be appropriate.
- Estimate Systematic Error: For a wide analytical range, use linear regression (Y = a + bX) to estimate the slope (b) and intercept (a). Calculate the systematic error (SE) at a critical medical decision concentration (Xc) as: SE = (a + b*Xc) - Xc [4].
- Sensitivity Analysis: Perform sensitivity analyses to assess the potential impact of any unmeasured confounders identified in the DAG.
Research Reagent Solutions
Table 2: Essential Materials for Method Comparison Studies
| Item | Function / Rationale |
|---|---|
| Calibrated Reference Material | Provides a traceable standard to ensure the correctness of the comparative method, serving as a benchmark for accuracy [4]. |
| Unadulterated Patient Specimens | The primary matrix for testing; carefully selected to cover the analytical range and represent the spectrum of expected disease states and interferences [4]. |
| Stable Control Materials | Used for quality control (QC) during the multi-day experiment to monitor and ensure the stability of both methods over time [33] [27]. |
| Interference Stock Solutions | (e.g., Hemolysate, Lipid Emulsions, Bilirubin) Used in separate recovery and interference experiments to characterize the specificity of the new method and identify potential sources of systematic error suggested by the DAG [4] [27]. |
| Appropriate Preservatives & Stabilizers | (e.g., Sodium Azide, Protease Inhibitors) Ensures specimen stability between analyses by the two methods, preventing pre-analytical error from being misattributed as methodological error [4]. |
Advanced Topics: DAGs for Complex Error Mechanisms
Time-Varying Confounding and Causal Pathways
In longitudinal studies, a variable may confound the exposure-outcome relationship at one time point but also lie on the causal pathway between a prior exposure and the outcome at a later time point. Standard regression adjustment for such time-varying confounders can block part of the causal effect of interest. DAGs are exceptionally useful for visualizing these complex scenarios, and methods like g-computation or structural nested models are needed for unbiased estimation.
Integrating DAGs with Other Error-Minimization Techniques
DAGs provide a theoretical framework that complements traditional, practical error-minimization techniques. For example:
- Blank Determination: In a DAG, this practice can be framed as an intervention to set the "Sample Analyte" to zero, allowing the isolation of the effect of "Reagent Impurities" on the "Measured Signal" [33] [27].
- Standard Addition: This method can be represented as a series of interventions at different dose levels, helping to isolate the effect of the "Sample Matrix" on the "Analytical Recovery" [33].
By formally representing these practices in a DAG, researchers can better understand their underlying causal logic and how they contribute to a comprehensive error-control strategy.
Designing Rigorous Method Comparison Experiments: A Step-by-Step Protocol
Frequently Asked Questions (FAQs)
1. What is the core difference between a reference method and a routine comparative method in terms of error attribution?
The core difference lies in the established "correctness" of the method and, consequently, how differences from a new test method are interpreted. A reference method is a high-quality method whose results are known to be correct through comparison with definitive methods or traceable reference materials. Any difference between the test method and a reference method is assigned as error in the test method. In contrast, a routine comparative method does not have this documented correctness. If a large, medically unacceptable difference is found between the test method and a routine method, further investigation is needed to identify which of the two methods is inaccurate [4].
2. Why is a large sample size (e.g., 40-200 specimens) recommended for a method comparison study?
The sample size serves different purposes. A minimum of 40 patient specimens is generally recommended to cover the entire working range of the method and provide a reasonable estimate of systematic error [4] [34]. However, larger sample sizes of 100 to 200 specimens are recommended to thoroughly investigate the methods' specificity, particularly to identify if individual patient samples show discrepancies due to interferences in the sample matrix. The quality and range of the specimens are often more important than the absolute number [4].
3. My data shows a high correlation coefficient (r = 0.99). Does this mean the two methods agree?
Not necessarily. A high correlation coefficient mainly indicates a strong linear relationship between the two sets of results but does not prove agreement [34]. Correlation can be high even when there are consistent, clinically significant differences between the methods. It is more informative to use statistical techniques like regression analysis (e.g., Passing-Bablok, Deming) or Bland-Altman plots, which are designed to reveal constant and proportional biases that the correlation coefficient overlooks [34].
4. What are the key strategies to minimize systematic error in a method comparison study?
Several strategies can be employed to minimize systematic error:
- Calibration: Regularly calibrate instruments against known, traceable standards [3] [35] [2].
- Methodology: Use a reference method for comparison if possible [4].
- Experimental Design: Analyze specimens over multiple days (at least 5 recommended) to minimize systematic errors from a single run [4].
- Sample Handling: Define and systematize specimen handling to prevent stability issues from causing differences [4].
- Triangulation: Use multiple techniques or instruments to measure the same analyte to cross-verify results [3].
5. When should I use ordinary linear regression versus more advanced methods like Passing-Bablok or Deming regression?
Ordinary linear regression assumes that the comparative (reference) method has no measurement error and is best suited when this assumption is largely true, or when the data range is wide (e.g., correlation coefficient >0.975) [36]. In contrast, Passing-Bablok regression is a robust, non-parametric method that does not require normal distribution of errors, is insensitive to outliers, and accounts for imprecision in both methods. It is particularly useful when the errors between the two methods are of a similar magnitude [34]. The choice depends on the known error characteristics of your comparative method.
Troubleshooting Guides
Problem 1: Discrepant Results Between New and Routine Method
Symptoms: You observe a consistent, significant difference between your new test method and the established routine method.
Resolution Steps:
- Verify Specimen Integrity: Confirm that samples were analyzed within a stable timeframe (e.g., within 2 hours for unstable analytes) and handled identically to avoid pre-analytical errors [4].
- Check Calibration: Re-calibrate both instruments using traceable calibrators to rule out simple offset or scale factor errors [35] [2].
- Run a Control Sample: Analyze a control sample with a known target value. This helps determine which of the two methods is deviating from the expected result [35].
- Investigate Specificity: Use recovery and interference experiments to check if the new method is affected by substances in the sample matrix that the routine method is not. A blank determination can help identify reagent impurities [4] [27].
- Use a Third Method: If the discrepancy persists, employ a definitive or reference method, if available, to act as an arbiter and identify which of the two routine methods is inaccurate [4] [27].
Problem 2: Detecting and Interpreting Constant vs. Proportional Error
Symptoms: The regression analysis from your method comparison shows a non-zero intercept and/or a slope that is not 1.
Resolution Steps:
- Perform Regression Analysis: Use an appropriate regression model (e.g., Passing-Bablok) to calculate the regression line equation (y = a + bx) [34].
- Interpret the Intercept (a): A confidence interval for the intercept that does not include zero suggests a constant systematic error. This is an offset that affects all measurements by the same absolute amount, regardless of concentration [34].
- Interpret the Slope (b): A confidence interval for the slope that does not include one suggests a proportional systematic error. This error increases or decreases in proportion to the analyte concentration [34].
- Assess Clinical Impact: Calculate the systematic error at medically important decision levels. For a decision level ( Xc ), the error is ( SE = (a + bXc) - X_c ). Compare this error to your allowable total error (TEa) specifications to determine if it is clinically acceptable [4] [36].
Experimental Protocols
Detailed Protocol: Method Comparison Experiment
Purpose: To estimate the systematic error (inaccuracy) between a new test method and a comparative method using real patient samples [4].
Research Reagent Solutions & Materials
| Item | Function |
|---|---|
| Patient Samples | At least 40 different specimens, covering the entire analytical range and expected disease spectrum [4]. |
| Reference Material | A certified material with a known value, used for calibration and trueness checks [35]. |
| Control Samples | Stable materials with assigned target values, used to monitor the precision and trueness of each analytical run [35]. |
| Calibrators | Solutions used to adjust the response of an instrument to known standard values [35]. |
Procedure:
- Sample Selection: Collect a minimum of 40 patient specimens that span the full reportable range of the assay [4] [34].
- Experimental Schedule: Analyze samples over multiple days (at least 5, ideally up to 20) to incorporate routine sources of variation. Analyze 2-5 patient specimens per day [4].
- Measurement: Analyze each patient specimen using both the test method and the comparative method. Ideally, perform measurements in duplicate and in a randomized order to avoid systematic bias [4].
- Data Collection: Record all results for statistical analysis.
Data Analysis Workflow: The following diagram illustrates the logical process for analyzing method comparison data and making a decision on method acceptability.
Protocol: Calculating and Interpreting Systematic Error
Purpose: To quantify the systematic error at critical medical decision concentrations and determine its acceptability [4] [36].
Procedure:
- Perform Regression: Using your comparison data, calculate the slope (b) and y-intercept (a) of the regression line using an appropriate model (e.g., Passing-Bablok).
- Define Decision Levels: Identify one to three critical medical decision concentrations (( X_c )) for the analyte.
- Calculate Systematic Error: For each decision level (( Xc )), calculate the corresponding value from the test method (( Yc )) and the systematic error (SE).
- ( Yc = a + b \times Xc )
- ( SE = Yc - Xc )
Example Calculation Table: The table below demonstrates how systematic error is calculated and evaluated against a performance goal.
| Medical Decision Level (( X_c )) | Calculated Test Method Value (( Y_c )) | Systematic Error (SE) | Allowable Error (TEa) | Is SE acceptable? |
|---|---|---|---|---|
| 100 mg/dL | ( 2.0 + (1.03 \times 100) = 105.0 ) mg/dL | +5.0 mg/dL | ±6 mg/dL | Yes |
| 200 mg/dL | ( 2.0 + (1.03 \times 200) = 208.0 ) mg/dL | +8.0 mg/dL | ±10 mg/dL | Yes |
| 300 mg/dL | ( 2.0 + (1.03 \times 300) = 311.0 ) mg/dL | +11.0 mg/dL | ±12 mg/dL | Yes |
Example based on a regression line of Y = 2.0 + 1.03X [4].
A technical support center for robust method comparison studies
This resource provides troubleshooting guides and FAQs to help researchers, scientists, and drug development professionals effectively determine sample size and select samples for method comparison studies, with a specific focus on minimizing systematic error.
FAQs: Fundamentals of Sample Size
FAQ 1: Why is sample size critical in method comparison studies? An adequately sized sample is fundamental for two primary reasons [37]:
- To Detect the Effect of Interest: A sample must be large enough to detect the "effect" or difference of clinical importance (e.g., the systematic error between two methods). A sample that is too small can easily fail to detect a clinically important effect (Type II error). Conversely, an excessively large sample may be wasteful and can detect differences that are statistically significant but clinically unimportant [37] [38].
- To Represent the Target Population: The sample must be large enough to effectively represent the target patient population. Heterogeneous populations generally require larger sample sizes to ensure the results are accurate and generalizable [37].
FAQ 2: What are the four essential pieces of information I need to estimate sample size? Before consulting a statistician or software, you should have preliminary estimates for the following four parameters [37] [38] [39]:
- Significance Level (α): The probability of rejecting a true null hypothesis (Type I error), often set at 0.05. This is the risk you are willing to take of concluding a difference exists when it does not [38].
- Power (1-β): The probability of correctly rejecting a false null hypothesis. A common standard is 80% or 90%, meaning you have an 80% or 90% chance of detecting an effect if it truly exists [37] [39].
- Magnitude of Effect (Effect Size): The difference you are trying to detect. For method comparison, this is often the systematic error (bias) that is considered clinically significant. Smaller, more subtle biases require larger samples to detect [37].
- Variability: The standard deviation of your variable of interest. Greater variability in your data requires a larger sample size to distinguish the signal (the effect) from the noise (the variability) [37].
FAQ 3: What is a practical minimum sample size for a method comparison experiment? A minimum of 40 different patient specimens is a common recommendation [4]. The quality and range of these specimens are often more important than a very large number. Specimens should be carefully selected to cover the entire working range of the method [4]. Some scenarios, such as assessing method specificity with different measurement principles, may require 100 to 200 specimens to identify sample-specific interferences [4].
FAQs: Advanced Planning & Troubleshooting
FAQ 4: How do I select patient specimens to ensure they cover the clinical range?
- Strategy: Do not use random patient specimens received by the laboratory. Instead, purposively select specimens based on their known concentrations to ensure coverage from low to high medical decision levels [4].
- Justification: The quality of the experiment depends more on obtaining a wide range of results than on a large number of results. A wide range is crucial for reliably estimating the slope and intercept in regression analysis, which helps characterize the nature of systematic error (constant or proportional) [4] [26].
FAQ 5: My correlation coefficient (r) is low in regression analysis. What does this mean for my sample? A low correlation coefficient (e.g., below 0.975 or 0.99) primarily indicates that the range of your data is too narrow to provide reliable estimates of the slope and intercept using ordinary linear regression [26]. It does not, by itself, indicate the acceptability of method performance.
- Corrective Action: The solution is not to collect more samples at the same concentrations, but to expand the concentration range of your specimens. If expanding the range is impossible, consider using statistical techniques like Deming or Passing-Bablok regression, which are better suited for data with a narrow range or with errors in both methods [26].
FAQ 6: How can I minimize the impact of systematic error from the very beginning?
- Calibration: Calibrate your equipment or entire procedure using a known reference quantity. This is the most reliable way to reduce systematic errors [2].
- Experimental Design: Analyze patient specimens over several different analytical runs (a minimum of 5 days is recommended) to minimize systematic errors that might occur in a single run [4].
- Normalization: In high-throughput studies (e.g., using 1536-well plates), systematic errors like row, column, or edge effects can be minimized post-hoc using normalization techniques that combine linear normalization and non-parametric regression (LOESS) [29].
Data Presentation: Key Parameters & Calculations
Table 1: Fundamental Parameters for Sample Size Estimation [37] [38] [39]
| Parameter | Symbol | Common Standard(s) | Role in Sample Size |
|---|---|---|---|
| Significance Level | α | 0.05 (5%) | A stricter level (e.g., 0.01) reduces Type I error risk but requires a larger sample. |
| Statistical Power | 1-β | 0.80 (80%) | Higher power (e.g., 0.90) increases the chance of detecting a true effect but requires a larger sample. |
| Effect Size | Δ | Minimal Clinically Important Difference | A smaller, harder-to-detect effect requires a larger sample. |
| Variability | σ | Standard Deviation from prior data | Greater variability requires a larger sample to distinguish the effect from background noise. |
Table 2: Common Sample Size Formulas for Different Study Types [38]
| Study Type | Formula | Variable Explanations |
|---|---|---|
| Comparing Two Means | n = (2 * (Zα/2 + Z1-β)² * σ²) / d² |
σ = pooled standard deviation; d = difference between means; Zα/2 = 1.96 for α=0.05; Z1-β = 0.84 for 80% power. |
| Comparing Two Proportions | n = (Zα/2 + Z1-β)² * (p1(1-p1) + p2(1-p2)) / (p1 - p2)² |
p1 & p2 = event proportions in each group; p = (p1+p2)/2. |
| Diagnostic Studies (Sensitivity/Specificity) | n = (Zα/2)² * P(1-P) / D² |
P = expected sensitivity or specificity; D = allowable error. |
Experimental Protocols
Protocol 1: Conducting a Basic Method Comparison Study
Purpose: To estimate the systematic error (bias) between a new test method and a comparative method [4].
- Specimen Selection: Select a minimum of 40 patient specimens to cover the entire analytical range of the method [4].
- Analysis: Analyze each specimen using both the test and comparative methods. Ideally, analyze specimens over multiple days (at least 5) to capture day-to-day variability [4].
- Immediate Data Review: Graph the data as it is collected using a comparison plot (test method vs. comparative method) or a difference plot (difference vs. average). Investigate any large discrepancies immediately while specimens are still available [4] [26].
- Statistical Analysis:
- For a wide analytical range, use linear regression to obtain the slope and intercept, which help identify proportional and constant systematic error, respectively [4] [40].
- For a narrow range, calculate the average difference (bias) and standard deviation of the differences using a paired t-test [26].
Protocol 2: A Workflow for Systematic Error Assessment and Sample Size
The following diagram illustrates a logical workflow for integrating systematic error assessment with sample size planning in method comparison studies.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Method Comparison
| Item | Function in Experiment |
|---|---|
| Certified Reference Material | A sample with a known, traceable analyte concentration. Serves as the highest standard for assessing accuracy and identifying systematic error (bias) [40]. |
| Quality Control (QC) Samples | Stable materials with known expected values used in every run (e.g., on Levey-Jennings charts) to monitor ongoing precision and accuracy, and to detect shifts indicative of systematic error [40]. |
| Patient Specimens | Real-world samples that represent the biological matrix and spectrum of diseases. They are essential for assessing method performance under actual clinical conditions [4]. |
| Calibrators | Materials used to adjust the analytical instrument's response to establish a correct relationship between the signal and the analyte concentration. Incorrect calibration is a common source of proportional bias [40]. |
FAQs on Core Concepts
Q1: What is the difference between reproducibility and replicability in the context of experimental science?
In metascientific literature, these terms have specific meanings. Reproducibility refers to taking the same data, performing the same analysis, and achieving the same result. Replicability involves collecting new data using the same methods, performing the same analysis, and achieving the same result. A third concept, robustness, is when a different analysis is performed on the same data and yields a similar result [41].
Q2: Why is the stability of patient specimens a critical factor in method comparison studies?
Specimen stability directly impacts the validity of your results. Specimens should generally be analyzed by both the test and comparative methods within two hours of each other to prevent degradation, unless the specific analyte is known to have shorter stability (e.g., ammonia, lactate). Differences observed between methods may be due to variables in specimen handling rather than actual systematic analytical errors. Stability can often be improved by adding preservatives, separating serum or plasma from cells, refrigeration, or freezing [4].
Q3: What is the recommended timeframe for conducting a comparison of methods experiment?
The experiment should be conducted over several different analytical runs on different days to minimize systematic errors that might occur in a single run. A minimum of 5 days is recommended. Extending the experiment over a longer period, such as 20 days, and analyzing only 2 to 5 patient specimens per day, can provide even more robust data that aligns with long-term replication studies [4].
Q4: How can I minimize systematic errors introduced by my equipment or apparatus?
The primary method is calibration. All instruments should be calibrated, and original measurements should be corrected accordingly. This process involves performing your experimental procedure on a known reference quantity. By adjusting your apparatus or calculations until the known result is achieved, you create a calibration curve to correct measurements of unknown quantities. Using equipment with linear responses simplifies this process [27] [2].
Troubleshooting Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Large, inconsistent differences between methods on a few specimens | Sample mix-ups, transposition errors, or specific interferences in an individual sample matrix [4]. | Perform duplicate measurements on different samples or re-analyze discrepant results immediately while specimens are still available [4]. |
| Consistent over- or under-estimation across all measurements | Systematic error (bias), potentially from uncalibrated apparatus, reagent impurities, or flaws in the methodology itself [27] [42]. | Calibrate all apparatus and perform a blank determination to identify and correct for impurities from reagents or vessels [27] [33]. |
| Findings from an experiment cannot be repeated by others | A lack of replicability, potentially due to analytical flexibility, vague methodological descriptions, or publication bias [41]. | Ensure full transparency by sharing detailed protocols, analysis scripts, and raw data where possible. Pre-register experimental plans to mitigate bias [41]. |
| High correlation but poor agreement between methods in a comparison plot | The range of data might be too narrow to reveal proportional systematic error. A high correlation coefficient (r) does not necessarily indicate method acceptability [4]. | Ensure specimens are selected to cover the entire working range of the method. Use regression statistics to estimate systematic error at medical decision levels [4]. |
Experimental Protocol: The Comparison of Methods Experiment
This protocol is designed to estimate the inaccuracy or systematic error between a new test method and a comparative method.
The goal is to estimate systematic error by analyzing patient specimens by both the test and comparative methods. The systematic differences observed at critical medical decision concentrations are of primary interest [4].
Step-by-Step Methodology
- Selection of Comparative Method: Ideally, a certified reference method should be used. If a routine method is used instead, be cautious in interpretation, as large differences may require additional experiments to identify which method is inaccurate [4].
- Selection and Handling of Specimens:
- Number: A minimum of 40 different patient specimens is recommended. Focus on quality and range over sheer quantity [4].
- Range: Specimens should cover the entire working range of the method and represent the spectrum of diseases expected in its routine application [4].
- Stability: Analyze specimens from both methods within two hours of each other. Define and systematize specimen handling procedures (e.g., refrigeration, separation) prior to the study to avoid handling-related differences [4].
- Experimental Execution:
- Timeframe: Conduct analysis over a minimum of 5 days, and ideally up to 20 days, to capture long-term variability [4].
- Replication: Analyze each specimen singly by both methods as a common practice. However, performing duplicate measurements on different sample cups in different runs is ideal for identifying mistakes [4].
- Controls: Include appropriate positive and negative controls in each run [29] [33].
- Data Analysis and Interpretation:
- Graphical Inspection: Initially, graph the data as a difference plot (test result minus comparative result vs. comparative result) or a comparison plot (test result vs. comparative result). Visually inspect for outliers and patterns suggesting constant or proportional error [4].
- Statistical Analysis:
- For a wide analytical range, use linear regression to calculate the slope (b), y-intercept (a), and standard deviation about the line (s~y/x~). Estimate systematic error (SE) at a critical decision concentration (X~c~) as: SE = Y~c~ - X~c~, where Y~c~ = a + bX~c~ [4].
- For a narrow analytical range, calculate the average difference (bias) and standard deviation of the differences using a paired t-test [4].
- The correlation coefficient (r) is more useful for assessing if the data range is wide enough for reliable regression (preferable when r ≥ 0.99) than for judging method acceptability [4].
The following table summarizes the quantitative recommendations for a robust comparison of methods study.
| Experimental Factor | Minimum Recommendation | Ideal Recommendation | Key Rationale |
|---|---|---|---|
| Number of Specimens [4] | 40 specimens | 100-200 specimens | Wider range improves error estimation; larger numbers help assess method specificity. |
| Study Timeframe [4] | 5 days | 20 days | Minimizes systematic errors from a single run; aligns with long-term performance. |
| Replication per Specimen [4] | Single measurement | Duplicate measurements | Identifies sample mix-ups and transposition errors; confirms discrepant results. |
| Specimen Stability [4] | Analyze within 2 hours | Use preservatives/separation | Prevents degradation from being misinterpreted as analytical error. |
| Data Range [4] | Cover the working range | Wide range around decision points | Ensures reliable regression statistics and error estimation across all levels. |
Research Reagent Solutions
This table details essential materials and their functions in ensuring experimental integrity.
| Item | Function in the Experiment |
|---|---|
| Calibrated Standards [27] [2] | Used for apparatus calibration and running control determinations to establish a known baseline and correct for systematic bias. |
| Reference Method Materials [4] | The reagents, calibrators, and controls specific to a high-quality reference method, providing a benchmark for assessing the test method's accuracy. |
| Preservatives & Stabilizers [4] | Added to patient specimens to improve stability (e.g., prevent evaporation, enzymatic degradation) during the testing window. |
| Blank Reagents [27] [33] | High-purity reagents used in blank determinations to identify and correct for errors caused by reagent impurities. |
| Positive & Negative Controls [29] | Substances with known responses (e.g., an agonist like beta-estradiol for a receptor assay, and an inert vehicle like DMSO) used to monitor assay performance and normalize data. |
Experimental Workflow and Error Mitigation
This diagram outlines the logical workflow for a method comparison study, highlighting key steps for minimizing systematic error.
Experimental Workflow for Method Comparison
This diagram illustrates the relationship between key procedural controls and the types of systematic error they help to mitigate.
Error Mitigation via Procedural Controls
Frequently Asked Questions (FAQs)
Q1: What is the most critical first step in data collection to minimize systematic error? The most critical first step is comprehensive planning and standardizing your data collection protocol. This involves defining all procedures, training all personnel involved, and using tools like the Time Motion Data Collector (TMDC) to standardize studies and make results comparable [43]. Consistent protocol application helps prevent introducing bias through variations in technique or observation.
Q2: How can I quickly check if my laboratory assay might be producing systematic errors? A simple and effective method is to create a dotplot of single data points in the order of the assay run [44]. This visualization can reveal patterns that summary statistics miss, such as all samples in a particular run yielding the same value (indicating a potential instrument calibration failure) or shifts in values corresponding to specific days or batches.
Q3: My team is manually collecting workflow data. How can we improve accuracy? Manual data collection is prone to human error, including computational mistakes and incomplete patient selection [45]. To improve accuracy:
- Implement a double-entry system for critical data points.
- Use standardized digital forms with built-in validation checks.
- Where possible, supplement or replace manual collection with automated data collection from electronic health records (EHR) or clinical data repositories, which can reduce errors and identify "false negative" cases missed manually [45].
Q4: What is a fundamental principle when designing a workflow monitoring tool? A core principle is goal orientation [43]. The tool should be designed with specific, clear objectives in mind. This ensures that the data collected is relevant, the analysis is focused, and the tool effectively identifies workflow patterns, bottlenecks, and opportunities for automation or improvement.
Q5: Are automated data collection methods always superior to manual methods? Automated data collection is often superior for reducing transcription errors and allowing ongoing, rapid evaluation [45]. However, it requires an initial investment and collaboration between clinicians, researchers, and IT specialists. Challenges can include integrating data from disparate sources and accounting for workflow variations that may not be captured in structured data fields [45]. A hybrid approach is sometimes necessary.
Troubleshooting Guides
Issue 1: Suspected Systematic Error in Laboratory Results
Problem: Laboratory results appear skewed, or a quality control (QC) sample shows a consistent shift from its known value.
Investigation and Resolution Steps:
- Visualize Data by Assay Run: Plot your results in a dotplot in the order they were analyzed to identify patterns like identical values in a single run or shifts between runs [44].
- Apply QC Rules: Use established rules like the Westgard rules to analyze your QC data [40].
- 2₂S Rule: Bias is likely if two consecutive QC values fall between 2 and 3 standard deviations on the same side of the mean.
- 4₁S Rule: Bias is indicated if four consecutive QC values fall on the same side of the mean and are at least 1 standard deviation away.
- 10ₓ Rule: Bias is present if ten consecutive QC values fall on the same side of the mean.
- Perform Method Comparison: If a bias is suspected, compare your method against a gold standard or certified reference material [40]. This can identify constant bias (a fixed difference) or proportional bias (a difference that changes with the concentration).
- Check Instrumentation and Reagents: Review calibration logs, check for expired reagents, and ensure environmental conditions (e.g., temperature) are within specified ranges.
Issue 2: Inefficient or Unclear Clinical Workflows
Problem: Workflow bottlenecks are suspected, leading to delays or variations in care, but the root causes are not understood.
Investigation and Resolution Steps:
- Gather Comprehensive Data: Collect data from multiple sources to build a complete picture. This can include direct observation (e.g., using a tool like TMDC), EHR event logs, and timestamp data from a real-time locating system (RTLS) [43].
- Use a Workflow Analysis Tool: Employ a tool like the Clinical Workflow Analysis Tool (CWAT) to mine the collected data and interactively visualize workflow patterns [43].
- Identify and Quantify Bottlenecks: Analyze the visualized patterns to pinpoint specific steps where delays consistently occur. Quantify the duration of these delays and their impact on the overall process.
- Synthesize Findings and Redesign: Use the analysis to inform workflow redesign, such as redistributing tasks, introducing new technology, or changing protocols. Continuously monitor the workflow after changes are implemented to assess improvement [43].
Experimental Protocols for Key Tasks
Protocol 1: Conducting a Method Comparison Study
Purpose: To identify and quantify systematic error (bias) in a new measurement method by comparing it to a reference method.
Materials:
- A set of patient samples covering the analytical range of interest.
- Reference method (gold standard).
- New method (the method under evaluation).
- Statistical software.
Methodology:
- Sample Measurement: Measure all samples using both the reference method and the new method.
- Data Analysis: Plot the results from the new method (y-axis) against the reference method (x-axis).
- Regression Analysis: Perform simple linear regression (y = a + bx) [40].
- The intercept (a) indicates the constant bias.
- The slope (b) indicates the proportional bias. A slope of 1 indicates no proportional bias.
- Interpretation: If significant bias is found, investigate its source. Corrective actions may include instrument recalibration or applying a correction factor to the new method's results.
Protocol 2: Implementing a Workflow Time-Motion Study
Purpose: To objectively record the time and sequence of activities in a clinical workflow to identify inefficiencies.
Materials:
- Standardized data collection tool (e.g., TMDC following the STAMP checklist) [43].
- Trained observers.
Methodology:
- Protocol Design: Define the workflow to be studied, the specific activities (tasks) to be recorded, and the clinical roles to be observed.
- Data Collection: Observers directly record the start and end times of each activity for the selected subjects (e.g., clinicians). The tool should support recording multitasking and interruptions [43].
- Data Integration: Combine observational data with other timestamp data from sources like EHR or RTLS for a more comprehensive view [43].
- Pattern Analysis: Use an analysis tool (e.g., CWAT) to identify common sequences, time spent on each task, frequent interruptions, and bottlenecks [43].
Workflow Visualization
The following diagram outlines a general workflow for data collection and initial inspection, designed to incorporate steps that minimize systematic error.
Data Collection and Initial Inspection Workflow
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key materials and tools essential for conducting robust data collection and error detection in a research setting.
| Item/Reagent | Function/Brief Explanation |
|---|---|
| Certified Reference Materials | Samples with known analyte concentrations used in method comparison studies to identify and quantify systematic error (bias) [40]. |
| Time Motion Data Collector (TMDC) | A standardized tool for direct observation and recording of workflow activities, helping to identify bottlenecks and inefficiencies [43]. |
| Clinical Workflow Analysis Tool (CWAT) | A data-mining tool that uses interactive visualization to help researchers identify and interpret patterns in workflow data [43]. |
| Structured Query Language (SQL) | A programming language used to create automated queries for extracting and re-using clinical data from Electronic Health Records (EHR) and data repositories, reducing manual errors [45]. |
| Statistical Software (e.g., R, Python) | Essential for performing data visualization (e.g., dotplots, heatmaps), statistical analysis, and implementing error detection rules like the Westgard rules [44] [40]. |
| Levey-Jennings Charts | A visual tool for plotting quality control data over time against mean and standard deviation lines, used to monitor assay performance and detect shifts or trends [40]. |
FAQs on Difference Plots and Scatter Plots
Q1: What is a difference plot and when should I use it in a method comparison study?
A difference plot, also known as a Bland-Altman plot, is a graphical method used to compare two measurement techniques. It displays the difference between two observations (e.g., test method minus comparative method) on the vertical (Y) axis against the average of the two observations on the horizontal (X) axis [46]. You should use it to:
- Assess the agreement between two methods.
- Identify any systematic bias (constant or proportional error) between them.
- Check if the variability of the differences is consistent across the range of measurement (homoscedasticity) [46] [4]. It is common to combine the difference plot with a histogram and a normality plot of the differences to check if the differences are normally distributed, which is an assumption of some statistical tests [46].
Q2: My scatter plot shows a cloud of points. How do I determine the relationship between the two methods?
A scatter plot shows the relationship between two variables by plotting paired observations. To interpret the relationship:
- Draw a line of best fit (or trend line) that best represents the data. This line simplifies the dataset to reveal the underlying pattern [47].
- Calculate the equation of the line. In its simplest form, the line can be expressed as ( y = mx + b ), where ( m ) is the slope and ( b ) is the y-intercept [47].
- A slope of 1 and an intercept of 0 suggest perfect agreement. A slope different from 1 indicates a proportional error, while a non-zero intercept suggests a constant systematic error [4].
Q3: What does a "systematic error" look like on these plots?
Systematic errors manifest differently on each plot:
- On a Difference Plot: A systematic error is indicated if the points are not randomly scattered around a horizontal line at zero. If all points lie above or below the zero line, it suggests a constant systematic error. If the points form an increasing or decreasing band, it suggests a proportional systematic error [46] [4].
- On a Scatter Plot: A systematic deviation from the line of identity (the line where y=x) indicates an error. The regression statistics (slope and intercept) are used to quantify this error. The systematic error (SE) at a given medical decision concentration (Xc) is calculated as ( SE = Yc - Xc ), where Yc is the value predicted by the regression line ( Yc = a + bXc ) [4].
Q4: My data points on the difference plot fan out as the average value increases. What does this mean?
This pattern, where the spread of the differences increases with the magnitude of the measurement, means that the variance is not constant. This phenomenon is called heteroscedasticity [46]. In this case, the standard deviation of the differences is not constant across the measurement range, and it may be more appropriate to express the limits of agreement as a percentage of the average [4].
Experimental Protocol for a Method Comparison Study
The following workflow outlines the key steps for executing a robust method comparison study, from experimental design to data analysis.
1. Define Study Purpose and Select Comparative Method The goal is to estimate the inaccuracy or systematic error of a new test method against a comparative method. Ideally, the comparative method should be a reference method with documented correctness. If using a routine method, differences must be interpreted with caution [4].
2. Select Patient Specimens
- Number: A minimum of 40 different patient specimens is recommended.
- Range: Specimens should cover the entire working range of the method.
- Quality: The spectrum of diseases expected in routine application should be represented. The quality and range of specimens are more critical than a very large number [4].
3. Perform Measurements
- Replication: Analyze each specimen in duplicate by both the test and comparative methods. Duplicates should be from different sample cups and analyzed in different runs or different order to identify sample mix-ups or transposition errors.
- Time Period: Conduct the experiment over a minimum of 5 different days to minimize systematic errors from a single run.
- Specimen Stability: Analyze specimens by both methods within two hours of each other to prevent differences due to specimen handling and degradation [4].
4. Visual Data Inspection & Statistical Analysis Graph the data as it is collected. Create both a difference plot and a scatter plot to visually identify discrepant results, patterns, and systematic errors. Reanalyze specimens with large discrepancies while they are still available [4]. Follow this with statistical analysis.
The table below summarizes key parameters and their interpretations for assessing method performance.
| Parameter | Description | Interpretation in Method Comparison |
|---|---|---|
| Slope (b) | The slope of the line of best fit from regression analysis [47]. | A value of 1 indicates no proportional error. A value ≠ 1 indicates a proportional systematic error [4]. |
| Y-Intercept (a) | The Y-intercept of the line of best fit from regression analysis [47]. | A value of 0 indicates no constant error. A non-zero value indicates a constant systematic error [4]. |
| Average Difference (Bias) | The mean of the differences between the two methods [4]. | Estimates the constant systematic error or average bias between the two methods. |
| Standard Deviation of Differences | The standard deviation of the differences between the two methods [4]. | Quantifies the random dispersion (scatter) of the data points around the average difference. |
| Correlation Coefficient (r) | A measure of the strength of the linear relationship [4]. | Mainly useful for assessing if the data range is wide enough for reliable regression; an r ≥ 0.99 is desirable [4]. |
| Standard Error of Estimate (s˅y/x˅ ) | The standard deviation of the points about the regression line [4]. | Measures the average distance that the observed values fall from the regression line. |
Research Reagent Solutions
This table lists essential non-instrumental components for a method comparison study.
| Item | Function / Description |
|---|---|
| Patient Specimens | The core "reagent" for the study. They should be a diverse set of clinical samples that cover the analytic range and expected pathological conditions [4]. |
| Reference Method | A well-characterized and highly accurate method to which the new test method is compared. It serves as the benchmark for assessing systematic error [4]. |
| Statistical Software | Software capable of performing linear regression, paired t-tests, and generating high-quality difference and scatter plots for data analysis [47] [4]. |
| Line of Best Fit | A statistical tool (the trend line) that models the relationship between the test and comparative method data, allowing for the quantification of systematic error [47] [4]. |
Troubleshooting Experimental Pitfalls and Handling Method Failure
In scientific research, particularly in method comparison studies, an outlier is a data point that differs significantly from other observations [48]. These anomalies can arise from technical errors, such as measurement or data entry mistakes, or represent true variation in the data, sometimes indicative of a novel finding or a legitimate methodological difference [49] [50]. Properly identifying and handling outliers is critical for minimizing systematic error and ensuring the integrity of your research conclusions. Incorrectly classifying a true methodological difference as a technical error can lead to a loss of valuable information, while failing to remove erroneous data can skew results and violate statistical assumptions [49] [51].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between an outlier caused by a technical error and one representing a true method disagreement? An outlier stemming from a technical error is an inaccuracy, often due to factors like instrument malfunction, data entry typos, or improper calibration [50] [52]. For example, an impossible value like a human height of 10.8135 meters is clearly an error [49]. In contrast, an outlier representing a true method disagreement or natural variation is a legitimate data point that accurately captures the inherent variability of the system or highlights a genuine difference in how two methods measure a particular sample or population [49] [53]. These "true outliers" should be retained as they contain valuable information about the process being studied [50].
Q2: Why is it considered bad practice to remove an outlier simply to improve the fit of my model? Removing outliers solely to improve statistical significance or model fit (e.g., R-squared) is controversial and frowned upon because it invalidates statistical results and presents an unrealistic view of the process's predictability [49] [48]. This practice can lead to a biased dataset and inaccurate conclusions, making your research appear more robust and predictable than it actually is [49] [50]. Decisions to remove data points must be based on justifiable causes, not desired outcomes.
Q3: How can I distinguish between a legitimate scientific disagreement over methods and a potential research misconduct issue? The key distinction often lies in intent [53]. An honest error or scientific disagreement involves unintentional mistakes or divergent interpretations of methods and data within the bounds of disciplinary norms. Research misconduct (fabrication, falsification, or plagiarism) involves a deliberate intent to deceive [53]. For instance, a dispute over whether to use an intent-to-treat versus on-treatment analysis in a clinical trial is a scientific disagreement, whereas systematically excluding data that undermines a hypothesis without a justifiable, pre-specified reason may constitute falsification [53]. Collegial discussion and dialogue are the preferred ways to resolve such disagreements.
Q4: My dataset is small. What are my options if I suspect outliers but cannot remove them without losing statistical power? When dealing with small samples, removal of data points is risky. Instead, consider using statistical analyses that are robust to outliers [49]. Non-parametric hypothesis tests do not rely on distributional assumptions that outliers often violate. Alternatively, you can use data transformation (e.g., log transformation) to reduce the impact of extreme values, or employ bootstrapping techniques which do not make strong assumptions about the underlying data distribution [49].
Troubleshooting Guides
Guide 1: A Protocol for Identifying Outliers
Objective: To provide a step-by-step methodology for detecting potential outliers in a dataset.
- Step 1: Visual Inspection Create a box plot of your data. Most statistical software packages will automatically plot outliers as individual points outside the whiskers of the box [50]. This provides an immediate, intuitive view of potential anomalies.
- Step 2: Calculate Descriptive Statistics Compute the following statistics for your dataset: mean, median, standard deviation, and quartiles (Q1 at the 25th percentile and Q3 at the 75th percentile). Compare the mean and median; a large difference can indicate the influence of outliers [48].
- Step 3: Apply Quantitative Detection Methods Use one or more of the following objective techniques to flag potential outliers. The results from these methods are summarized in the table below.
| Method | Calculation Steps | Best Used For | Assumptions | ||
|---|---|---|---|---|---|
| IQR Method [50] [51] | 1. Calculate IQR = Q3 - Q12. Lower Bound = Q1 - (1.5 × IQR)3. Upper Bound = Q3 + (1.5 × IQR)4. Data points outside [Lower Bound, Upper Bound] are potential outliers. | Datasets with skewed or non-normal distributions. A robust method as it does not depend on the mean. | None. Robust to non-normal data. | ||
| Z-Score Method [50] [51] | 1. Calculate mean (μ) and standard deviation (σ)2. Compute Z-score for each point: ( Z = (x - μ) / σ )3. Data points with ( | Z | > 3 ) are often considered outliers. | Large sample sizes where the data is approximately normally distributed. | Data is normally distributed. Sensitive to outliers in small datasets. |
| Standard Deviation Method [51] | 1. Calculate mean (μ) and standard deviation (σ)2. Data points outside of μ ± 3σ are considered outliers. | Univariate data with an assumed normal distribution. | Data follows a normal distribution. |
The following workflow diagram illustrates the logical process for investigating a suspected outlier.
Guide 2: A Framework for Addressing Detected Outliers
Objective: To establish a justified course of action for a confirmed outlier based on its root cause.
Scenario A: The Outlier is a Technical Error
- Action: If the outlier is confirmed to be a measurement or data entry error, your first priority is to correct the value if possible (e.g., by referring to original records or re-measuring) [49]. If correction is impossible, you may remove the data point because it is a known incorrect value [49].
- Documentation: You must document the specific error and the reason for removal in your research records [50].
Scenario B: The Outlier is Not from the Target Population
- Action: If you can establish that the outlier comes from a different population than the one you are studying (e.g., a manufacturing anomaly, a subject with a confounding health condition), it is generally legitimate to remove it [49].
- Documentation: Clearly state the specific reason why the data point does not fit your target population definition [49].
Scenario C: The Outlier is a Result of Natural Variation
- Action: If the outlier is a legitimate, albeit extreme, observation from the population you are studying, you should not remove it [49] [48]. Deleting it would misrepresent the true variability of the data.
- Alternative Approaches: In this case, you should:
- Use robust statistical methods that are less sensitive to outliers (e.g., non-parametric tests, robust regression) [49].
- Perform a sensitivity analysis by running your analysis both with and without the outlier and reporting the differences [49]. This is considered a best practice and demonstrates the stability of your findings.
- Consider data transformation (e.g., log, square root) to reduce the influence of the extreme value on your analysis [54].
The following diagram maps these scenarios to the appropriate decision pathway.
The Scientist's Toolkit: Essential Reagents for Reliable Data Analysis
This table details key methodological "reagents"—the core statistical techniques and protocols—essential for handling outliers responsibly in method comparison studies.
| Tool | Category | Function & Explanation |
|---|---|---|
| IQR Detection [50] [51] | Identification | A robust method for flagging outliers based on data spread, using quartiles instead of the mean. Ideal for non-normal data. |
| Box Plot [50] | Visualization | Provides an immediate graphical summary of data distribution and visually highlights potential outliers for further investigation. |
| Sensitivity Analysis [49] | Protocol | The practice of running statistical analyses with and without suspected outliers to assess their impact on the conclusions. |
| Robust Statistical Tests [49] | Analysis | Non-parametric tests (e.g., Mann-Whitney U) used when outliers cannot be removed, as they do not rely on distributional assumptions easily violated by outliers. |
| Data Transformation [54] | Preprocessing | Applying mathematical functions (e.g., log, square root) to the entire dataset to reduce the skewing effect of outliers and make the data more symmetrical. |
| Detailed Lab Notebook | Documentation | Critical for recording the identity of any removed data point, the objective reason for its removal, and the statistical justification. This ensures transparency and reproducibility [49] [50]. |
Effectively managing outliers is a critical skill in minimizing systematic error in research. The process extends beyond mere detection to a careful investigation of the root cause. Always remember the core principle: remove only what you can justify as erroneous or irrelevant to your research question, and retain and manage what is legitimate, even if it is inconvenient. By following the structured protocols, utilizing the appropriate statistical tools, and maintaining rigorous documentation outlined in this guide, researchers can ensure their methodological choices are defensible, transparent, and scientifically sound.
Troubleshooting Guides
Guide 1: Diagnosing and Resolving Multiple Imputation Failures
Q: My multiple imputation procedure fails to run or produce results. What are the most common causes and solutions?
A: Multiple imputation failures commonly occur due to two primary issues: perfect prediction and collinearity within your imputation model [55].
Perfect Prediction occurs when a covariate or combination of covariates completely separates outcome categories, preventing maximum likelihood estimates from being calculated. This frequently happens with categorical data where certain predictor values perfectly correspond to specific outcomes [55].
Immediate Solutions:
- Simplify your imputation model by reducing the number of variables
- Use Bayesian priors to stabilize estimation
- Combine categorical variable categories to eliminate perfect separation
- Consider imputing composite variables instead of individual components [55]
Collinearity arises when highly correlated variables in the imputation model create numerical instability in the estimation algorithms [55].
Immediate Solutions:
- Remove redundant variables from the imputation model
- Create composite scores from highly correlated items
- Use principal components instead of original variables
- Apply regularization techniques to stabilize estimation [55]
For complex cases, consider these advanced strategies:
Algorithmic Adjustments:
- Modify the visit sequence in MICE algorithms to improve convergence [56]
- Break feedback loops by carefully setting predictor matrices [56]
- Use different imputation methods for different variable types [55]
Monitoring Convergence:
- Plot key parameters across iterations to visually assess convergence [56]
- Ensure different imputation streams are freely intermingling without definite trends [56]
- Monitor scientifically relevant statistics (correlations, proportions) rather than just means and variances [56]
Guide 2: Handling Non-Convergence in Simulation Studies
Q: How should I handle simulation iterations that fail to converge when comparing statistical methods?
A: Non-convergence in simulation studies presents significant challenges for valid method comparison. Current research indicates only 23% of simulation studies mention missingness, with even fewer reporting frequency (19%) or handling methods (14%) [57].
Systematic Documentation Approach:
- Quantify and report missingness for all methods and conditions, even if none occurs [57]
- Pre-specify handling methods in your analysis plan [57]
- Differentiate between convergence rates as a performance measure versus a nuisance [57]
Handling Strategies Based on Missingness Type:
Table: Classification of Missingness Types in Simulation Studies
| Type | Description | Recommended Handling |
|---|---|---|
| Systematic Missingness | Non-convergence patterns differ systematically between methods | Analyze missingness mechanisms before proceeding with comparison |
| Sporadic Missingness | Isolated non-convergence with no apparent pattern | Consider resampling or multiple imputation of performance measures |
| Catastrophic Missingness | Complete method failure under certain conditions | Report as a key finding about method limitations |
Best Practices for Minimizing Bias:
- Avoid complete case analysis (using only convergent iterations) as this can severely bias results [57]
- Consider simulating additional data until all methods converge if missingness is minimal [57]
- Implement sensitivity analyses to assess how handling methods affect conclusions [57]
- Document all decisions transparently to enable critical evaluation [57]
Frequently Asked Questions
Q: What's the fundamental difference between non-convergence as a performance measure versus a nuisance in method comparison studies?
A: When non-convergence itself is a performance measure (e.g., comparing algorithm robustness), convergence rates should be analyzed and reported as a key outcome. When non-convergence is a nuisance (interfering with comparing other performance measures), the focus should be on minimizing its impact on fair method comparison while transparently reporting handling approaches [57].
Q: How can I adjust my imputation model when facing numerical problems with large numbers of variables?
A: Several proven strategies exist for large imputation models:
- Use composite variables instead of multiple individual items [55]
- Implement a two-stage imputation approach [55]
- Incorporate prior information to stabilize estimates [55]
- Change the form of the imputation model (e.g., using linear instead of nonlinear models for initial imputation) [55]
- Carefully select auxiliary variables based on their correlation with missingness patterns [55]
Q: What are the most reliable methods for monitoring MICE algorithm convergence?
A: Effective convergence monitoring includes:
- Visual inspection of parameter streams across iterations [56]
- Ensuring free intermingling of different imputation chains without definite trends [56]
- Monitoring multiple parameters of interest, including scientifically relevant statistics [56]
- Using a combination of diagnostics rather than relying on a single method [56]
- Being particularly vigilant when imputing derived variables that feed back into predictors [56]
Experimental Protocols
Protocol: Systematic Handling of Non-convergence in Method Comparison Studies
Objective: To minimize systematic error when comparing statistical methods in the presence of non-convergence.
Materials: Statistical software (R, Python, or Stata), simulation framework, documentation system.
Procedure:
Pre-specification Phase
- Define convergence criteria for all methods
- Specify primary handling method for non-convergent cases
- Plan sensitivity analyses for alternative handling methods
Execution Phase
- Run simulations with comprehensive monitoring
- Document all non-convergent cases with relevant conditions
- Record convergence rates for each method-condition combination
Analysis Phase
- Implement pre-specified handling approach
- Conduct sensitivity analyses with alternative approaches
- Compare convergence rates as a performance measure when relevant
Reporting Phase
- Quantify and report all missingness [57]
- Justify handling methods with reference to study goals
- Acknowledge limitations introduced by missingness
Workflow Visualization
Systematic Error Minimization Framework: This workflow ensures consistent handling of non-convergence issues while documenting decisions to minimize introduction of systematic error through ad-hoc problem-solving.
The Scientist's Toolkit
Table: Essential Resources for Handling Non-Convergence
| Tool/Resource | Application Context | Key Function |
|---|---|---|
| MICE Algorithm (R/Python/Stata) | Multiple imputation with complex data | Flexible imputation by chained equations with customizable models [55] [58] |
| Visit Sequence Control | Improving MICE convergence | Reordering imputation sequence to enhance stability [56] |
| Predictor Matrix Tuning | Breaking feedback loops | Carefully setting which variables predict others in MICE [56] |
| Convergence Diagnostics | Monitoring MCMC/MICE convergence | Visual and statistical assessment of algorithm convergence [56] |
| Multiple Imputation Packages (R: mice, missForest; Python: fancyimpute, scikit-learn) | Implementing advanced imputation | Software implementations of various imputation methods [58] |
| Simulation Frameworks | Method comparison studies | Structured environments for conducting and monitoring simulation studies [57] |
Current Reporting Practices
Table: Prevalence of Missingness Reporting in Methodological Literature (Based on 482 Simulation Studies) [57]
| Reporting Practice | Prevalence | Implication for Systematic Error |
|---|---|---|
| Any mention of missingness | 23% (111/482) | Majority of studies potentially biased by unaccounted missingness |
| Report frequency of missingness | 19% (92/482) | Limited transparency in assessing potential impact |
| Report handling methods | 14% (67/482) | Inability to evaluate appropriateness of handling approaches |
| Complete documentation | <14% | Significant room for improvement in methodological practice |
The consistent implementation of these strategies, combined with transparent reporting, will significantly enhance the reliability of your method comparison studies and minimize systematic errors introduced by non-convergence and algorithmic failures.
Why is handling method failure critical in research?
In methodological research, method failure occurs when a method under investigation fails to produce a result for a given data set. This is a common challenge in both simulation and benchmark studies, manifesting as errors, non-convergence, system crashes, or excessively long run times [59] [60].
Handling these failures inadequately can introduce systematic error into your comparison studies. Popular approaches like discarding failing data sets or imputing values are often inappropriate because they can bias results and ignore the underlying reasons for the failure [59]. A more robust perspective views method failure not as simple missing data, but as the result of a complex interplay of factors, which should be addressed with realistic fallback strategies that reflect what a real-world user would do [59] [60].
Troubleshooting Guides
Guide 1: Diagnosing the Root Cause of Method Failure
Problem: A method fails to produce a result during a comparison study. Objective: Systematically identify the source of the failure to select the correct fallback strategy.
Experimental Protocol & Diagnosis:
- Check for Logged Errors: Review all error messages and warnings from the software output. Common indicators include
NA,NaN, or explicit error messages [59]. - Verify Data Integrity: Check for data set characteristics known to cause failures, such as:
- Profile Resource Usage: Determine if the failure is due to:
- Review Method Assumptions: Confirm that the data meets the core assumptions of the statistical or machine learning method used (e.g., linearity, independence, homoscedasticity).
Fallback Decision Pathway: The following workflow outlines a systematic response to method failure, helping you choose an appropriate fallback strategy.
Guide 2: Managing Failures in Multi-Study Comparisons
Problem: How to aggregate performance measures (e.g., average accuracy, bias) across multiple data sets or simulation repetitions when one or more methods fail for some data sets. Objective: Ensure a fair and unbiased comparison that accounts for method failure without discarding valuable information.
Experimental Protocol:
- Record All Failures: For every data set and method combination, log whether the method succeeded or failed, and the reason for the failure if known [59].
- Apply a Fallback Strategy: For each instance of failure, implement a pre-specified fallback method. This should be a simple, robust method that can provide a result where the primary method fails [59] [60].
- Calculate Two Performance Tables: To understand the impact of failures, calculate performance metrics in two ways [59]:
- Performance with Fallbacks: Use the primary method's result when available, and the fallback method's result in case of failure.
- Performance on Successful Subset: Calculate performance using only the data sets where all methods succeeded.
Data Presentation: The tables below illustrate how to compare method performance while transparently accounting for failures.
Table 1: Performance with Fallback Strategy Applied
| Benchmark Data Set | Method 1 Accuracy | Method 2 Accuracy | Method 3 Accuracy (with Fallback) |
|---|---|---|---|
| Data Set 1 | 0.85 | 0.88 | 0.87 |
| Data Set 2 | 0.90 | 0.91 | 0.86 |
| Data Set 3 | 0.82 (Fallback) | 0.80 | 0.82 |
| Data Set 4 | 0.78 | 0.76 | 0.79 (Fallback) |
| Average Accuracy | 0.84 | 0.84 | 0.84 |
Table 2: Performance on the Subset of Data Sets Where All Methods Succeeded
| Benchmark Data Set | Method 1 Accuracy | Method 2 Accuracy | Method 3 Accuracy |
|---|---|---|---|
| Data Set 1 | 0.85 | 0.88 | 0.87 |
| Data Set 2 | 0.90 | 0.91 | 0.86 |
| Average Accuracy | 0.88 | 0.90 | 0.87 |
Comparing these two tables provides a more complete picture than a single aggregated number and helps quantify the bias introduced by only analyzing the "easy" data sets.
Frequently Asked Questions (FAQs)
Q1: What is the most common mistake in handling method failure? The most common mistake is to silently discard data sets where a method fails and only report results on the remaining data. This introduces systematic error because the failures are often correlated with specific, challenging data characteristics (e.g., separability, small sample size). It creates a biased comparison that overestimates the performance of fragile methods on "easy" data [59].
Q2: When is it acceptable to impute a value for a failed method? Imputation is rarely the best strategy. As noted in research, imputing a value (e.g., the performance of a constant predictor) treats the failure as simple "missing data," which ignores the informational value of the failure itself. A fallback strategy is almost always preferable to simple imputation because it uses a legitimate, albeit simpler, methodological result [59].
Q3: How do fallback strategies minimize systematic error? Fallback strategies minimize systematic error by preserving the intent of the comparison across the entire scope of the study. Discarding data sets where methods fail systematically removes a specific type of "hard" case, making the experimental conditions unlike the real world. Using a fallback method allows you to include these difficult cases in your aggregate performance measures, leading to a more realistic and generalizable estimate of a method's overall utility [59] [2].
Q4: Should fallback strategies be decided before starting the study? Yes, whenever possible. Pre-specifying fallback strategies in the study design is a key practice to minimize bias. If researchers choose a fallback strategy after seeing the results, it can introduce a form of p-hacking or "researcher degrees of freedom," where the handling of failures is unconsciously influenced to make the results look more favorable [59].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Solutions for Robust Method Comparison Studies
| Research Reagent Solution | Function in Handling Method Failure |
|---|---|
| Pre-specified Fallback Method | A simple, robust method (e.g., linear model, mean predictor) used to generate a result when a sophisticated primary method fails, preventing data exclusion [59] [60]. |
| Comprehensive Error Logging | Systematic recording of all errors, warnings, and resource usage data to enable root cause analysis of failures [59]. |
| Resource Monitoring Scripts | Code that tracks memory and computation time in real-time, helping to diagnose failures due to resource exhaustion [59]. |
| Standardized Performance Metrics | Pre-defined metrics that include calculations both with fallbacks and on the successful subset, allowing for transparent assessment of failure impact [59]. |
Core Concepts: Systematic Error and Calibration
What are constant and proportional biases?
In method comparison studies, systematic error (or bias) is a reproducible inaccuracy that skews results consistently in the same direction. Unlike random error, it cannot be eliminated by repeating measurements and requires corrective action such as calibration [40]. Systematic bias manifests in two primary forms:
- Constant Bias: A consistent difference between observed and expected measurements that remains the same throughout the concentration range. It is described by the equation: ( \text{Observed} = \text{Expected} + \text{B}0 ), where ( \text{B}0 ) represents the constant bias [40].
- Proportional Bias: A difference that changes proportionally with the analyte concentration. It follows the equation: ( \text{Observed} = \text{B}1 \times \text{Expected} ), where ( \text{B}1 ) represents the proportional bias coefficient [40].
How does calibration correct for these biases?
Calibration establishes a mathematical relationship between instrument signal response and known analyte concentrations using regression modeling [61]. This relationship creates a correction factor that adjusts future measurements to minimize both constant and proportional biases. For mass spectrometry, using matrix-matched calibrators and stable isotope-labeled internal standards (SIL-IS) is critical to mitigate matrix effects that cause bias [61].
Table: Types of Systematic Error and Their Characteristics
| Bias Type | Mathematical Representation | Common Causes | Impact on Results |
|---|---|---|---|
| Constant Bias | Observed = Expected + B₀ |
Insufficient blank correction, calibration offset [40] | Shifts all results equally, regardless of concentration |
| Proportional Bias | Observed = B₁ × Expected |
Differences in calibrator vs. sample matrix, instrument response drift [40] | Error increases or decreases proportionally with the concentration of the analyte |
Troubleshooting Guides
How do I detect systematic error in my dataset?
Problem: Suspected systematic error is skewing experimental results. Solution: Employ statistical tests and visual tools to identify non-random patterns.
- For High-Throughput Screening (HTS) Data: Use a t-test on hit distribution surfaces to confirm the presence of systematic error before applying any correction method [62]. An uneven distribution of hits across well locations indicates location-specific bias.
- For Clinical Laboratory Data: Apply Westgard rules to quality control data for systematic error detection [40]:
- 22S Rule: Bias is present if two consecutive quality control values fall between 2 and 3 standard deviations on the same side of the mean.
- 41S Rule: Bias is present if four consecutive control values fall on the same side of the mean and are at least 1 standard deviation away.
- 10x Rule: Bias is present if ten consecutive control values fall on the same side of the mean.
- For General Method Comparison: Perform a method comparison against a gold standard or certified reference material. Plot the results and use ordinary least squares (OLS) regression to fit a line (( y = mx + c )). The intercept (( c )) indicates constant bias, while the slope (( m )) indicates proportional bias [40].
My calibrated method still shows bias. How do I correct it?
Problem: A calibrated method continues to exhibit constant or proportional bias. Solution: Apply advanced correction techniques based on the error type.
- For Proportional Bias in Mass Spectrometry:
- Investigate Heteroscedasticity: Check if the variance of your calibration data changes with concentration [61].
- Apply Weighting Factors: If heteroscedasticity is present, use weighted regression (e.g., ( 1/x ) or ( 1/x² )) during calibration curve fitting instead of ordinary least squares to ensure all concentration levels are accurately modeled [61].
- For Bias in Log-Linear Calibrations:
- For Complex Datasets with Multiple Biases:
- In high-throughput screening, use the B-score normalization method. This robust technique applies a two-way median polish to account for row and column effects on assay plates, followed by normalization using the median absolute deviation (MAD) [62].
- The Well correction technique can remove systematic biases affecting specific well locations across all plates in an assay [62].
How do I handle bias in survey or panel data?
Problem: Overlapping panel surveys suffer from non-response and coverage biases. Solution: Implement a two-step reweighting process [64]:
- Model Non-Response: Use machine learning techniques like XGBoost to model the propensity for non-response in the longitudinal sample based on data from previous measurements. This creates adjusted weights that account for dropout patterns.
- Calibrate to Population Totals: Further adjust the weights from step one using calibration to match known population totals for auxiliary variables (e.g., age, sex, geographic location). This corrects for coverage bias and improves representativeness [64].
Flowchart: Two-Step Reweighting for Panel Data
Experimental Protocols
Protocol: Method comparison for bias estimation
Purpose: To quantify constant and proportional bias between a new method and a reference method [40].
Materials:
- Certified reference materials or samples analyzed by a gold standard method
- Appropriate matrix-matched calibrators
- Stable isotope-labeled internal standards (if applicable)
Procedure:
- Analyze a series of samples covering the analytical measurement range using both the test method and the reference method.
- Plot the results from the test method (y-axis) against the reference method (x-axis).
- Perform ordinary least squares (OLS) linear regression on the data to obtain the line of best fit: ( y = mx + c ).
- Interpretation:
- The intercept (( c )) estimates the constant bias.
- The slope (( m )) estimates the proportional bias.
- An ideal method would have ( c = 0 ) and ( m = 1 ).
Protocol: B-score normalization for HTS data
Purpose: To correct for systematic row and column effects within microtiter plates in high-throughput screening [62].
Procedure:
- For each plate ( p ), apply a two-way median polish procedure. This robustly estimates the plate mean (( \hat{\mu}p )), row effects (( \hat{R}{ip} )), and column effects (( \hat{C}_{jp} )).
- Calculate the residual ( r{ijp} ) for each well (in row ( i ), column ( j ), plate ( p )) using the formula: ( r{ijp} = x{ijp} - \hat{x}{ijp} = x{ijp} - (\hat{\mu}p + \hat{R}{ip} + \hat{C}{jp}) ) [62].
- Compute the Median Absolute Deviation (MAD) for the residuals of each plate ( p ).
- Calculate the final B-score for each measurement: ( \text{B-score} = \frac{r{ijp}}{\text{MAD}p} ) [62].
This process removes systematic spatial biases, allowing for more accurate hit selection.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Bias Correction and Calibration
| Reagent/Material | Function | Application Context |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides a known concentration with high accuracy for method comparison and bias estimation [40]. | General laboratory medicine, analytical chemistry |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Compensates for matrix effects and losses during sample preparation; ensures accurate quantification by mass spectrometry [61]. | LC-MS/MS clinical methods |
| Matrix-Matched Calibrators | Calibrators prepared in a matrix similar to the patient sample to conserve the signal-to-concentration relationship and avoid bias [61]. | Mass spectrometry, clinical chemistry |
| Positive & Negative Controls | Used to normalize data and detect plate-to-plate variability in HTS assays [62]. | High-throughput screening, drug discovery |
Frequently Asked Questions (FAQs)
What is the difference between accuracy and precision in the context of bias?
Accuracy (or trueness) refers to the proximity of a test result to the true value and is directly affected by systematic error (bias). Precision refers to the reliability and reproducibility of measurements and is affected by random error. A method can be precise but inaccurate if a large bias is present [40].
When should I use weighted versus unweighted regression for my calibration curve?
Use weighted regression when your calibration data exhibits heteroscedasticity—that is, when the variability (standard deviation) of the instrument response changes with the concentration of the analyte. Using ordinary least squares (unweighted) regression on heteroscedastic data can lead to significant inaccuracies, especially at the lower end of the calibration curve. The choice of weighting factor (e.g., ( 1/x ), ( 1/x² )) should be based on the nature of the data [61].
Can calibration completely eliminate systematic error?
While calibration is the primary tool for correcting systematic error, it may not eliminate it. The effectiveness depends on using appropriate calibration materials (e.g., matrix-matched calibrators), correct regression models, and stable analytical conditions. Residual bias should be monitored and quantified using quality control materials and method comparison studies [40] [61].
How do I know if my bias is clinically or scientifically significant?
Statistical significance does not always equate to practical significance. Evaluate the impact of the observed bias by comparing it to pre-defined acceptance criteria. These criteria are often based on the intended use of the data. For example, in a clinical laboratory, bias may be compared to allowable total error limits based on biological variation or clinical guidelines [65] [40]. In pharmaceutical screening, the effect on hit selection rates (false positives/negatives) determines significance [62].
In method comparison studies, a primary goal is to identify and minimize systematic error, also known as bias. Westgard Rules provide a statistical framework for ongoing quality control (QC), enabling researchers to detect significant shifts in analytical method performance. Originally developed by Dr. James O. Westgard for clinical laboratories, these multi-rule QC procedures are a powerful tool for any scientific field requiring high data fidelity, such as drug development. By applying a combination of control rules, researchers can achieve a high rate of error detection while maintaining a low rate of false rejections, ensuring that systematic biases are identified and addressed promptly [66].
Troubleshooting Guides
Guide 1: Investigating a Persistent Systematic Bias
A systematic bias, indicated by rules such as 2:2s or 10X, suggests a consistent shift in results away from the established mean.
- Problem: The control data shows a persistent shift in one direction.
- Detection Rules: This pattern is typically flagged by the 2:2s, 10X, or 4:1s rules [67] [68].
- Corrective Actions:
- Inspect Reagents: Check for expired reagents, improper preparation, or contamination. Replace with a new lot if necessary [67].
- Review Calibration: Verify the calibration status of the instrument. Recalibrate using traceable standards.
- Check Instrument Function: Look for signs of instrument malfunction, such as drifts in temperature, deteriorating light sources, or pump failures [67] [69].
- Verify Control Material: Ensure the control specimen is not old, compromised, or prepared improperly [67].
Guide 2: Addressing a Spike in Random Error
A random error, indicated by the 1:3s or R4s rule, suggests unpredictable variability in the measurement process.
- Problem: The control data shows high variability or a single, extreme outlier.
- Detection Rules: This is most commonly identified by the 1:3s or R4s rules [67] [68].
- Corrective Actions:
- Check Pipetting Technique: Ensure consistent and accurate pipetting; check for pipette calibration.
- Inspect Sample Integrity: Look for bubbles, particulates, or incomplete mixing in samples or reagents.
- Review Environmental Conditions: Check for fluctuations in ambient temperature or humidity that could affect the assay.
- Identify Transient Instrument Issues: Investigate for unstable power supplies, intermittent fluidic blockages, or electrical faults [69].
Guide 3: Resolving a Shift Detected Across Multiple Runs
Some errors become apparent only when reviewing data over time, across several analytical runs.
- Problem: A gradual trend or shift is observed when evaluating control data from consecutive runs.
- Detection Rules: This is identified by rules applied across runs, such as 10X (10 consecutive results on one side of the mean) or the 2:2s rule applied to the same control material in consecutive runs [67] [69].
- Corrective Actions:
- Perform Preventive Maintenance: Conduct scheduled maintenance for the instrument, including cleaning optics, replacing worn parts, and verifying critical functions.
- Analyze Reagent Degradation: Monitor reagent performance over time, especially after opening or reconstitution.
- Re-evaluate Control Mean and SD: If the method's performance has permanently changed, it may be necessary to re-establish the mean and standard deviation for the control material after the underlying issue is fixed [70].
Frequently Asked Questions (FAQs)
Q1: What is the difference between a warning rule and a rejection rule? The 1:2s rule is typically used as a warning rule. A single control measurement exceeding the ±2 standard deviation (SD) limit triggers a careful inspection of the control data using other, stricter rules. In contrast, rejection rules (like 1:3s, 2:2s, R4s) mandate that the analytical run be rejected and patient/research results withheld until the problem is resolved [66] [69].
Q2: Can I use Westgard Rules if I only run one level of control? The full power of multi-rule QC is realized with at least two control measurements. If only one level of control is used, the 1:2s rule must serve as a rejection rule, not just a warning, as the other rules cannot be applied. However, it is strongly recommended to use at least two levels of control to effectively detect errors across the assay's range [67] [66].
Q3: One of my three control levels is outside 3SD, but the other two are fine. Should I accept the run? No. According to the 1:3s rule, a single control measurement exceeding the ±3SD limit is a rejection rule and the run should be rejected. This indicates a significant problem, which could be random error or an issue specific to that control level (e.g., deteriorated control material) [70].
Q4: How do I know which Westgard Rules to use for my specific assay? The choice of QC rules should be based on the analytical performance of your method. A best practice is to calculate the Sigma-metric of your assay: Sigma = (Allowable Total Error % - Bias %) / CV %.
- High Sigma (≥6): Use simple rules (e.g., 1:3s) with fewer controls.
- Moderate Sigma (4-5.5): Use multi-rule procedures (e.g., 1:3s/2:2s/R4s).
- Low Sigma (<4): Requires more powerful multi-rule procedures with more control measurements [71] [72].
Q5: What does it mean if one control is above +2SD and another is below -2SD in the same run? This violates the R4s rule, which indicates excessive random error or imprecision in the analytical run. The run should be rejected, and the process should be investigated for sources of random variability [67] [68].
Westgard Rules Reference Table
The table below summarizes the key Westgard Rules, their criteria, and the type of error they typically detect [67] [66] [68].
| Rule | Criteria | Interpretation | Error Type |
|---|---|---|---|
| 1:2s | One measurement exceeds ±2SD | Warning to check other rules. If N=1, it is a rejection rule. | Random or Systematic |
| 1:3s | One measurement exceeds ±3SD | Reject the run. | Random Error |
| 2:2s | Two consecutive measurements exceed the same ±2SD limit (within a run or across runs for the same material) | Reject the run. | Systematic Error |
| R4s | One measurement exceeds +2SD and another exceeds -2SD in the same run | Reject the run. | Random Error |
| 4:1s | Four consecutive measurements exceed the same ±1SD limit | Reject the run. | Systematic Error |
| 10X | Ten consecutive measurements fall on the same side of the mean | Reject the run. | Systematic Error |
The Scientist's Toolkit: Essential Materials for QC Implementation
| Item | Function in Quality Control |
|---|---|
| Control Materials | Stable, assayed materials with known values that mimic patient samples; used to monitor precision and accuracy over time. |
| Levey-Jennings Chart | A graphical tool for plotting control values against time, with lines indicating the mean and ±1, 2, and 3 standard deviations. |
| Sigma-Metric Calculation | A quantitative measure (Sigma = (TEa - Bias)/CV) to assess the performance of a method and guide the selection of appropriate QC rules. |
| Total Allowable Error (TEa) | A defined quality requirement that specifies the maximum error that is clinically or analytically acceptable for a test. |
Westgard Rules Logic and Workflow
The following diagram illustrates the logical workflow for applying Westgard Rules in a sequential manner, starting with the 1:2s warning rule.
Statistical Validation and Assessing Method Acceptability
A technical support guide for researchers navigating method comparison studies.
In method comparison studies, a fundamental step in minimizing systematic error is selecting the appropriate statistical tool for analysis. Two commonly used yet distinct methods are Linear Regression and the Bland-Altman analysis. Choosing incorrectly can lead to biased conclusions, hindering research validity. This guide provides clear, actionable protocols to help you select and apply the right tool for your experimental data.
Understanding the Core Methods
What is Linear Regression Analysis?
Linear regression models the relationship between a dependent variable (e.g., a new measurement method) and an independent variable (e.g., a reference method) by fitting a straight line through the data points. Its key output, the coefficient of determination (R²), indicates the proportion of variance in the dependent variable that is predictable from the independent variable [73] [74].
- R² Interpretation: A value of 100% means the model explains all the variation, while 0% means it explains none. However, a high R² does not automatically mean good agreement between methods; it only indicates the strength of a linear relationship [75] [74].
What is Bland-Altman Analysis?
The Bland-Altman plot (or difference plot) is a graphical method used to assess the agreement between two quantitative measurement techniques [76] [77]. It involves plotting the differences between two methods against their averages for each subject [78].
- Key Components:
- Mean Difference (Bias): The average of all differences between the two methods, indicating a systematic error or constant bias [78].
- Limits of Agreement (LoA): Defined as the mean difference ± 1.96 times the standard deviation of the differences. This interval is expected to contain 95% of the differences between the two measurement methods [75] [78].
The plot helps visualize patterns, such as whether the differences are consistent across all magnitudes of measurement or if the variability changes (heteroscedasticity) [78] [77].
Direct Comparison: Key Differences
The table below summarizes the core distinctions between the two methods.
| Feature | Linear Regression | Bland-Altman Analysis |
|---|---|---|
| Primary Goal | To model a predictive relationship and quantify correlation [75] [74]. | To assess the agreement and interchangeability of two methods [76] [78]. |
| What it Quantifies | Strength of linear relationship (R²) and regression equation (slope, intercept) [79] [73]. | Mean bias (systematic error) and limits of agreement (random error) [75] [78]. |
| Handling of Errors | Does not directly quantify the scale of measurement error between methods [75]. | Directly visualizes and quantifies systematic and random errors via bias and LoA [76]. |
| Best Use Case | When trying to predict the value of one method from another, or to calibrate a new method [75]. | When determining if two methods can be used interchangeably in clinical or laboratory practice [76] [78]. |
Decision Workflow & Experimental Protocol
Follow this structured workflow to choose the correct analytical path for your data.
Step-by-Step Experimental Protocol
1. Study Design & Data Collection
- Paired Measurements: Collect measurements from the same set of subjects or samples using both Method A and Method B.
- Sample Size: Ensure an adequate sample size. A minimum of 40-50 subjects is often recommended for Bland-Altman analysis to obtain reliable estimates of the limits of agreement [77].
- Cover the Range: Select samples that cover the entire range of values expected in clinical or research practice [75].
2. Data Preparation
- For each pair of measurements, calculate:
- The Average:
(Method_A + Method_B) / 2 - The Difference:
Method_A - Method_B(The choice of which method to subtract is important; note it for bias interpretation) [78].
- The Average:
3. Conducting Bland-Altman Analysis [75] [78]
- Create the Plot: On a scatter plot, set the X-axis as the Average of the two measurements and the Y-axis as the Difference.
- Calculate and Plot Key Lines:
- Mean Difference (Bias): Calculate the average of all differences. Plot this as a solid horizontal line.
- Limits of Agreement (LoA): Calculate
Mean Difference ± 1.96 * Standard Deviation of Differences. Plot these as dashed horizontal lines.
- Check for Patterns: Examine the scatter for:
- Constant Bias: Most points are clustered around a horizontal line away from zero.
- Proportional Bias: A trend where differences increase or decrease as the average increases. A regression line of differences on averages can help detect this [78].
- Heteroscedasticity: The spread (scatter) of the differences noticeably widens or narrows with increasing average values.
4. Conducting Linear Regression Analysis [79] [74]
- Perform Regression: Regress the results of the new method (Y) on the reference method (X).
- Examine Outputs:
- Regression Equation:
Y = Intercept + Slope * X - R-squared (R²): The percentage of variance explained.
- Regression Equation:
- Interpret Parameters:
- An Intercept significantly different from zero suggests a constant systematic error.
- A Slope significantly different from 1.0 suggests a proportional systematic error.
5. Interpretation & Reporting
- For Bland-Altman, the final step is clinical judgment: Are the Limits of Agreement narrow enough to be clinically acceptable? This must be defined a priori based on biological or clinical requirements [75] [78].
Troubleshooting Common Problems (FAQs)
FAQ 1: My Bland-Altman plot shows that the spread of differences gets larger as the average gets larger (Heteroscedasticity). What should I do?
This is a common issue where the measurement error is proportional to the magnitude.
- Solution A: Plot Ratios or Percentage Differences [78]. Instead of raw differences, plot
(Difference / Average) * 100on the Y-axis. This normalizes the differences relative to the size of the measurement. - Solution B: Use a Regression-Based Bland-Altman Approach [78]. This method models the bias and limits of agreement as functions of the measurement magnitude, rather than assuming they are constant. The limits of agreement will appear as curved lines on the plot.
FAQ 2: I have a high R² value from my regression analysis. Can I conclude the two methods agree well?
No, this is a common and dangerous misconception [75] [74]. A high R² only indicates a strong linear relationship, not agreement.
- Example: A new method might consistently give values that are 20 units higher than the reference method. The correlation can be perfect (R² = 1.0), but the methods do not agree due to the constant bias. Bland-Altman analysis would clearly reveal this 20-unit bias.
FAQ 3: When should I avoid using the standard Bland-Altman method?
Recent research highlights a key limitation: avoid standard Bland-Altman when one of the two methods is a reference "gold standard" with negligible measurement error [80].
- The Problem: The standard method's underlying assumptions are violated in this scenario, leading to biased estimates of the limits of agreement.
- The Solution: In such cases, a simple linear regression of the differences (or the new method's results) on the reference method's values is a more robust approach [80].
FAQ 4: How do I define what "good agreement" is for my study?
The Bland-Altman method gives you the limits of agreement, but it does not tell you if they are acceptable. This is a clinical or practical decision [75] [78].
- Approach 1: Based on Analytical Goals. Use quality specifications (e.g., from CLIA guidelines) or calculate based on the combined inherent imprecision of both methods.
- Approach 2: Based on Clinical Relevance. Ask: "Would the observed random differences between methods be too small to influence patient diagnosis or treatment?" If yes, the agreement is acceptable.
Essential Research Reagent Solutions
The table below lists key statistical "reagents" for your method comparison study.
| Tool / Concept | Function / Explanation |
|---|---|
| Bland-Altman Plot | The primary graphical tool for visualizing agreement and quantifying bias and limits of agreement [78] [77]. |
| Limits of Agreement (LoA) | An interval (Mean Bias ± 1.96 SD) that defines the range where 95% of differences between two methods are expected to lie [75]. |
| Mean Difference (Bias) | The estimate of average systematic error between the two methods [78]. |
| Coefficient of Determination (R²) | A statistic from regression that quantifies the proportion of variance explained by a linear model; indicates correlation, not agreement [79] [73]. |
| Heteroscedasticity | A situation where the variability of the differences changes with the magnitude of the measurement; violates an assumption of the standard Bland-Altman method [78] [77]. |
| Clinical Agreement Limit (Δ) | A pre-defined, clinically acceptable difference between methods. Used to judge the Limits of Agreement [78]. |
Frequently Asked Questions
1. What is the practical significance of the slope and intercept in a method comparison study? The slope and intercept are critical for identifying systematic error. The slope (b₁) represents the proportional systematic error (PE); a value different from 1 indicates that the error between methods increases proportionally with the analyte concentration, often due to issues with calibration or standardization. The intercept (b₀) represents the constant systematic error (CE); a value different from 0 suggests a constant bias, potentially caused by assay interference or an incorrect blanking procedure [81].
2. How is the Standard Error of the Estimate (SEE) interpreted? The Standard Error of the Estimate (sᵧ/ₓ or SEE) estimates the standard deviation of the random errors around the regression line. In a method comparison context, it quantifies the random analytical error (RE) between the two methods. It incorporates the random error of both methods plus any unsystematic, sample-specific error (e.g., varying interferences). A smaller SEE indicates better agreement and precision between the methods [82] [81].
3. My slope is not equal to 1. How do I determine if this is a significant problem? A slope different from 1 may or may not be practically important. To test its significance, calculate the confidence interval for the slope using its standard error (sb). If the interval (e.g., b₁ ± t*sb) does not contain the value 1, the observed proportional systematic error is statistically significant. You should then assess whether the magnitude of this error is clinically or analytically acceptable for your intended use [83] [81].
4. What are the key assumptions I must check when performing linear regression for method comparison? The key assumptions are [81]:
- Linearity: The relationship between the two methods is linear.
- No Error in X-values: The reference method (X) is error-free (this is often violated in practice, but a high correlation coefficient (r > 0.99) minimizes the impact).
- Gaussian Distribution: The Y-values are normally distributed at each X.
- Homoscedasticity: The variance of the errors is constant across the concentration range.
5. How can I estimate the total systematic error at a specific medical decision level? The overall systematic error (bias) at a critical concentration Xc is not simply the overall average bias. Use your regression equation to calculate it [81]:
- Predict the value from the new method: Ŷc = b₁ * Xc + b₀
- The systematic error at Xc is: Bias = Ŷc - Xc This allows you to evaluate the method's performance at clinically relevant decision points (e.g., hypoglycemic, normal, and hyperglycemic glucose levels).
Troubleshooting Guides
Problem: Significant Proportional Systematic Error (Slope ≠ 1)
Description The new method demonstrates a proportional bias relative to the comparative method. The difference between methods increases as the analyte concentration increases.
Diagnostic Steps
- Check the Scatterplot: Visually inspect the plot of data. The points will show a fanning pattern if the error is proportional.
- Calculate Slope and its Confidence Interval: Fit the regression model and compute the 95% confidence interval for the slope. If the interval does not include 1.00, the proportional error is statistically significant [83] [81].
- Investigate Calibration: Review the calibration process of the new method. Incorrect calibration is a common cause.
Solution Recalibrate the new method using appropriate and fresh calibration standards. Ensure the calibration curve covers the entire analytical measurement range of interest [81].
Experimental Workflow for Diagnosing Proportional Error
Problem: Significant Constant Systematic Error (Intercept ≠ 0)
Description The new method shows a constant bias, meaning the difference between methods is the same across all concentration levels.
Diagnostic Steps
- Check the Scatterplot: The data points will be consistently shifted upward or downward from the line of identity (Y=X).
- Calculate Intercept and its Confidence Interval: Determine the 95% confidence interval for the intercept. If the interval does not include 0.0, the constant error is statistically significant [83] [81].
- Review Reagent Blanks and Specificity: Examine the method's blanking procedure and check for non-specific interference.
Solution Check and correct the method's blank value. Investigate potential chemical interferences in the sample matrix and adjust the procedure to mitigate them [81].
Problem: High Random Error (Large Standard Error of the Estimate)
Description The scatter of data points around the fitted regression line is large, indicating poor precision and agreement between the methods for individual samples.
Diagnostic Steps
- Calculate the Standard Error of the Estimate (SEE): A larger SEE indicates greater random dispersion [82].
- Check for Heteroscedasticity: See if the spread of residuals changes with concentration. A funnel-shaped pattern in a residual plot confirms this.
- Review Replication Data: Check the inherent imprecision of both methods from a separate replication experiment.
Solution Identify and minimize sources of random variation. This may include improving the precision of the new method, using more stable reagents, or controlling environmental factors like temperature [81].
The following table summarizes the core statistics used to evaluate a linear regression model in method comparison studies [84] [82] [83].
| Statistic | Symbol | Formula | Interpretation in Method Comparison |
|---|---|---|---|
| Slope | ( b_1 ) | ( b1 = r \frac{sy}{sx} ) or ( \frac{\sum{(Xi - \bar{X})(Yi - \bar{Y})}}{\sum{(Xi - \bar{X})^2}} ) | Proportional Error. Ideal value = 1. |
| Intercept | ( b_0 ) | ( b0 = \bar{Y} - b1\bar{X} ) | Constant Error. Ideal value = 0. |
| Standard Error of the Estimate (SEE) | ( s_{y/x} ) | ( \sqrt{\frac{\sum{(Yi - \hat{Y}i)^2}}{n-2}} ) | Random Error (RE). Measures data scatter around the line. |
| Standard Error of the Slope | ( se(b1) ) or ( sb ) | ( \frac{s{y/x}}{\sqrt{\sum{(Xi - \bar{X})^2}}} ) | Uncertainty in the slope estimate. Used for its CI and significance test. |
| Standard Error of the Intercept | ( se(b0) ) or ( sa ) | ( s{y/x} \sqrt{ \frac{1}{n} + \frac{\bar{X}^2}{\sum{(Xi - \bar{X})^2}} } ) | Uncertainty in the intercept estimate. Used for its CI and significance test. |
Where ( \hat{Y}_i ) is the predicted value of Y for a given X, and ( r ) is the correlation coefficient.
The Scientist's Toolkit: Essential Materials for Method Comparison
| Item | Function in Experiment |
|---|---|
| Stable Reference Material | Provides a "true value" for calibration and serves as a quality control check for both methods. |
| Matrix-Matched Calibrators | Calibration standards in the same biological matrix as the sample (e.g., serum, plasma) to account for matrix effects. |
| Clinical Samples with Broad Concentration Range | A set of patient samples covering the low, middle, and high end of the analytical measurement range is crucial for evaluating proportional error. |
| Statistical Software (e.g., R, Python, LINEST in Excel) | Used to perform regression calculations, compute standard errors, confidence intervals, and generate diagnostic plots. |
Computational Protocol for Key Statistics
The Python code below provides a practical example of calculating the slope, intercept, and their standard errors from experimental data [85] [86].
Diagnostic Logic for Systematic Error
Estimating Systematic Error at Critical Medical Decision Concentrations
Key Concepts: Systematic Error in the Laboratory
What is systematic error and how does it differ from random error?
Systematic error, often referred to as bias, is a consistent or reproducible deviation from the true value that affects all measurements in the same direction. Unlike random error, which causes unpredictable fluctuations, systematic error skews results consistently and cannot be eliminated by repeated measurements [40] [3].
Random error affects precision and causes variability around the true value, while systematic error affects accuracy by shifting measurements away from the true value in a specific direction [3]. In research, systematic errors are generally more problematic than random errors because they can lead to false conclusions about relationships between variables [3].
Why is estimating systematic error at medical decision concentrations critical?
Medical decision concentrations are specific analyte values at critical clinical thresholds used for diagnosis, treatment initiation, or therapy modification. Systematic error at these concentrations is particularly dangerous because it can lead to misdiagnosis or inappropriate treatment [4] [81].
For example, a glucose method might have different systematic errors at hypoglycemic (50 mg/dL), fasting (110 mg/dL), and glucose tolerance test (150 mg/dL) decision levels [81]. A method comparison showing no overall bias at mean values might still have clinically significant systematic errors at these critical decision points [81].
Experimental Protocols
Comparison of Methods Experiment: Core Protocol
The comparison of methods experiment is the primary approach for estimating systematic error using patient specimens [4].
Table: Comparison of Methods Experiment Specifications
| Parameter | Specification | Rationale |
|---|---|---|
| Number of Specimens | Minimum of 40 | Ensure statistical reliability [4] |
| Specimen Selection | Cover entire working range; represent spectrum of diseases | Assess performance across clinical conditions [4] |
| Measurement Approach | Single or duplicate measurements per specimen | Duplicates help identify sample mix-ups or transposition errors [4] |
| Time Period | Minimum of 5 days, ideally 20 days | Minimize systematic errors from single runs [4] |
| Specimen Stability | Analyze within 2 hours of each method unless preservatives used | Prevent handling-induced differences [4] |
| Comparative Method | Reference method preferred; routine method acceptable | Establish basis for accuracy assessment [4] |
Method Comparison Workflow
Data Analysis & Interpretation
Statistical Analysis of Comparison Data
Regression analysis is the preferred statistical approach for estimating systematic error across a range of concentrations [4] [81]. The regression equation (Y = a + bX) allows calculation of:
- Constant systematic error from the y-intercept (a) [81]
- Proportional systematic error from the slope (b) [81]
- Overall systematic error at any medical decision concentration (Xc) using: Yc = a + bXc, then SE = Yc - Xc [81]
Correlation coefficient (r) should be 0.99 or greater to ensure reliable estimates of slope and intercept from ordinary linear regression [4].
Table: Systematic Error Components and Their Interpretation
| Component | Statistical Measure | Indicates | Potential Causes |
|---|---|---|---|
| Constant Error | Y-intercept (a) | Consistent difference across all concentrations | Inadequate blank correction, mis-set zero calibration [81] |
| Proportional Error | Slope (b) | Difference proportional to analyte concentration | Poor calibration, matrix effects [81] |
| Random Error Between Methods | Standard error of estimate (S_y/x) | Unpredictable variation between methods | Varying interferences, method imprecision [81] |
Graphical Analysis Techniques
Difference plots (also called Bland-Altman plots) display the difference between test and comparative method results (y-axis) versus the comparative result (x-axis) [4]. This helps visualize whether differences scatter randomly around zero or show patterns indicating systematic error [4].
Comparison plots display test method results (y-axis) versus comparative method results (x-axis), with a line of identity showing where points would fall for perfect agreement [4].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Why can't the correlation coefficient alone judge method agreement? Perfect correlation (r = 1.000) only indicates that values increase proportionally, not that they're identical. Systematic differences can still exist even with high correlation coefficients [87]. Correlation coefficients mainly help determine if the data range is wide enough for reliable regression estimates [4].
What should we do when large differences are found between methods? Identify specimens with large differences and reanalyze them while still fresh [4]. If differences persist, perform interference and recovery experiments to determine which method is at fault [4] [87].
How do we handle non-linear relationships in comparison data? Examine the data plot carefully, particularly at high and low ends [81]. If necessary, restrict statistical analysis to the range that shows linear relationship [81].
Troubleshooting Systematic Error Detection
Problem: Inconsistent results between quality control and method comparison
- Potential cause: QC materials may have different matrix effects than patient samples [40]
- Solution: Use patient samples for method comparison and investigate specificity differences between methods [4]
Problem: Discrepant results at medical decision levels despite acceptable overall performance
- Potential cause: Proportional systematic error that becomes clinically significant only at certain concentrations [81]
- Solution: Calculate systematic errors specifically at critical decision concentrations using regression statistics [81]
Problem: Unacceptable systematic error identified
- Potential causes: Calibration issues, reagent problems, instrumental drift [1] [2]
- Solutions: Calibrate against primary standards, implement correction factors based on regression equation, or method modification [40]
Research Reagent Solutions & Essential Materials
Table: Essential Materials for Systematic Error Estimation
| Material/Reagent | Function | Specifications |
|---|---|---|
| Certified Reference Materials | Calibration and accuracy assessment | Certified values with established traceability [40] |
| Quality Control Materials | Monitoring assay performance | Multiple concentration levels covering medical decision points [40] |
| Patient Specimens | Method comparison studies | 40+ specimens covering analytical range and disease states [4] |
| Primary Standards | Calibration verification | Highest purity materials for independent calibration [87] |
| Commercial Calibrators | Routine calibration | Lot-to-lot consistency verification required [87] |
Advanced Detection Methods
Quality Control-Based Detection
Levey-Jennings plots visually display control material measurements over time with reference lines showing mean and standard deviation limits [40]. Systematic error is suspected when consecutive values drift to one side of the mean [40].
Westgard rules provide specific criteria for identifying systematic error:
- 2₂S rule: Two consecutive controls >2SD but <3SD on same side of mean [40]
- 4₁S rule: Four consecutive controls >1SD on same side of mean [40]
- 10ₓ rule: Ten consecutive controls on same side of mean [40]
Patient-Based Detection Methods
Average of Normals: Statistical analysis of results from healthy patients to detect shifts in the population mean [40].
Moving Patient Averages: Tracking average results across patient populations to identify systematic changes over time [40].
This technical support guide provides troubleshooting and best practices for determining the acceptability of a new analytical method by comparing its total error to predefined quality specifications.
Core Concepts: Understanding Error and Quality Specifications
What is the relationship between systematic error, random error, and total error?
In method validation, total error represents the combined effect of both random error (imprecision) and systematic error (inaccuracy) in your analytical measurement [88]. Systematic error, or bias, refers to consistent, reproducible deviations from the true value, while random error refers to unpredictable variations in measurements [89]. The total error (TE) is calculated using the formula: TE = Bias + Z × CV, where Bias is the inaccuracy, CV is the coefficient of variation representing imprecision, and Z is a multiplier setting the confidence level (typically Z=2 for ~95% confidence) [88].
How do I establish predefined quality specifications for my assay?
Quality specifications, also known as total allowable error (TEa), define the maximum error that is clinically or analytically acceptable for an assay. These specifications can be derived from several sources [88]:
- Regulatory guidelines from bodies such as the European Working Group or CLIA [88].
- Biological variation data, which sets goals based on the natural variation of an analyte in healthy individuals.
- State-of-the-art performance, based on the best performance achievable by current technologies.
You should establish these specifications before conducting validation studies to provide objective acceptance criteria for your method.
Troubleshooting Guides
No Assay Window or Poor Signal
| Possible Cause | Investigation Steps | Corrective Action |
|---|---|---|
| Incorrect instrument setup [90] | Verify instrument parameters, including excitation/emission wavelengths, filters, and gain settings. | Consult manufacturer's instrument setup guides; ensure proper filter selection for TR-FRET assays. [90] |
| Reagent issues | Check reagent expiration, preparation, and storage conditions. | Prepare fresh reagents; ensure correct reconstitution and handling. |
| Improper assay development | Test development reaction with controls (e.g., 100% phosphopeptide control and substrate). [90] | Titrate development reagent to achieve optimal signal differentiation (e.g., a 10-fold ratio difference). [90] |
Inconsistent Performance (High Imprecision)
| Possible Cause | Investigation Steps | Corrective Action |
|---|---|---|
| Pipetting inaccuracies | Check pipette calibration; use same pipette for same steps. | Regularly calibrate pipettes; use multi-channel pipettes for high-throughput steps. |
| Unstable environmental conditions | Monitor laboratory temperature and humidity. | Allow instruments and reagents to acclimate to room temperature; control laboratory conditions. |
| Reagent lot variability | Test new reagent lots alongside current lots before full implementation. | Use duplicate measurements and ratio-based data analysis to account for lot-to-lot variability. [90] |
Unacceptable Total Error
| Possible Cause | Investigation Steps | Corrective Action |
|---|---|---|
| Significant systematic error (Bias) | Perform method comparison with 40+ patient samples across reportable range. [4] | Investigate source of bias (calibration, interference); apply correction factor if justified and validated. |
| High imprecision (CV) | Review replication study data; identify steps with highest variation. | Optimize incubation times; ensure consistent technique; use quality reagents. |
| Inappropriate quality specifications | Verify that the selected TEa is realistic and appropriate for the clinical/analytical use of the assay. | Consult published guidelines from sources like the European Working Group or CLIA. [88] |
Experimental Protocols for Assessment
Protocol 1: Method Comparison Experiment to Estimate Systematic Error
Purpose: To estimate inaccuracy or systematic error by comparing a new method to a comparative method. [4]
- Sample Requirements: A minimum of 40 different patient specimens, selected to cover the entire working range of the method. [4]
- Sample Analysis: Analyze each specimen by both the test and comparative methods. Ideally, perform analyses within 2 hours of each other to ensure specimen stability. [4]
- Time Period: Conduct the experiment over a minimum of 5 days, using 2-5 patient specimens per day, to account for run-to-run variability. [4]
- Data Analysis:
- Graphical Inspection: Create a difference plot (test result minus comparative result vs. comparative result) or a comparison plot (test result vs. comparative result) to visually identify discrepant results and patterns of error. [4]
- Statistical Analysis:
- For wide analytical ranges, use linear regression to obtain the slope (b) and y-intercept (a) of the line of best fit. Calculate the systematic error (SE) at a medical decision concentration (Xc) as: SE = Yc - Xc, where Yc = a + bXc. [4]
- For narrow analytical ranges, calculate the average difference (bias) between the two methods using a paired t-test. [4]
- Passing and Bablok regression is also commonly used to account for measurement variability in both methods. Methods are considered harmonized if the 95% confidence interval for the intercept includes zero and for the slope includes one. [88]
Protocol 2: Estimating Total Error from Imprecision and Inaccuracy Studies
Purpose: To calculate the total error of a method by combining estimates of its random error (imprecision) and systematic error (inaccuracy). [88]
- Within-Day Imprecision (CV_wd): Measure two patient samples (with different concentrations) 20 times each in a single run. Calculate the mean, standard deviation (SD), and coefficient of variation (CV) for each level. The average of these two CVs is the final within-day imprecision. [88]
- Between-Day Imprecision (CV_bd): Analyze commercial control materials (at normal and pathological levels) once daily for 30 days. Calculate the mean, SD, and CV for each level over the 30 days. The average of these two CVs is the final between-day imprecision, representing the random analytical error. [88]
- Inaccuracy (Bias): Use the data from the between-day imprecision study. Calculate the percentage bias for each control level as: Bias (%) = [(Mean Value - Target Value) / Target Value] × 100%. The measure of inaccuracy is the systematic analytical error. [88]
- Total Error (TE) Calculation: Use the formula TE = Bias + 2 × CV_bd (using Z=2) to calculate the total error. Compare the calculated TE to the predefined total allowable error (TEa) for your assay. [88]
Workflow Visualization
Method Comparison and Acceptance Workflow
Essential Research Reagent Solutions
| Reagent / Material | Function in Validation |
|---|---|
| Commercial Control Materials | Used for determining between-day imprecision and inaccuracy (bias). They provide a stable, matrix-matched material with assigned target values. [88] |
| Calibrators | Used to standardize the analyzer and establish the calibration curve. Essential for minimizing systematic error. [88] |
| Patient Samples | Used for method comparison and within-day imprecision studies. Should cover the entire analytical measurement range and represent the expected sample matrix. [4] [88] |
| Reference Method Reagents | If available, reagents for a reference method provide the highest standard for comparison to assess the relative systematic error of the new method. [4] |
| TR-FRET Donor/Acceptor Reagents | For binding assays (e.g., LanthaScreen), these reagents enable ratiometric data analysis, which helps correct for pipetting variances and reagent lot-to-lot variability. [90] |
Frequently Asked Questions (FAQs)
My method has a large assay window but the Z'-factor is low. Is it acceptable for screening?
No. A large assay window alone is not a good measure of robustness. The Z'-factor incorporates both the assay window and the variability (standard deviation) of the data. An assay with a large window but high noise can have a low Z'-factor. Assays with Z'-factor > 0.5 are generally considered suitable for screening. [90]
What is the advantage of using ratio-based data analysis in TR-FRET assays?
Taking a ratio of the acceptor signal to the donor signal (e.g., 520 nm/495 nm for Tb) accounts for small variances in pipetting and lot-to-lot variability of the reagents. The donor signal serves as an internal reference, making the ratio more robust than raw RFU values. [90]
In a method comparison, my correlation coefficient (r) is 0.98. Does this mean the methods agree?
Not necessarily. A high correlation coefficient mainly indicates a strong linear relationship, not agreement. It is more useful for verifying that the data range is wide enough to provide reliable estimates of slope and intercept. You must examine the regression statistics (slope and intercept) to evaluate systematic differences. [4] [88]
How many samples are needed for a reliable method comparison study?
A minimum of 40 patient specimens is recommended. However, the quality and concentration distribution of the samples are more important than the absolute number. Select 40 carefully chosen samples covering the entire reportable range rather than 100 random samples. [4]
Method comparison studies are fundamental experiments designed to estimate the systematic error, or bias, between a new test method and a comparative method [4]. The primary purpose is to determine whether the analytical errors of the new method are acceptable for their intended clinical or research use, ensuring that results are reliable and fit-for-purpose [4] [91]. This process is a cornerstone of method validation in laboratory medicine, pharmaceutical development, and any field reliant on precise quantitative measurements.
Understanding and minimizing systematic error is crucial because, unlike random error which can be reduced by repeated measurements, systematic error consistently skews results in one direction and is not eliminated through averaging [16] [40]. Left undetected, it can lead to biased conclusions, misguided decisions, and invalid comparisons [16] [89]. This case study walks through a full statistical analysis from a method comparison, providing a practical framework for researchers.
Experimental Design and Protocol
A robust experimental design is the first and most critical step in controlling for systematic error.
Specimen Selection and Handling
- Number of Specimens: A minimum of 40 different patient specimens is recommended to provide a reliable estimate of systematic error [4]. Some experts suggest 100-200 specimens if the goal is to also assess the method's specificity across a spectrum of sample matrices [4].
- Concentration Range: Specimens should be carefully selected to cover the entire working range of the method. A wide range is more important than a large number of specimens with similar concentrations [4] [91].
- Stability and Analysis: Specimens should generally be analyzed by both the test and comparative method within two hours of each other to prevent degradation from causing observed differences. Stability can be improved by refrigeration, freezing, or other appropriate preservation techniques [4].
Analysis Protocol
- Replication: While common practice is to analyze each specimen once by each method, performing duplicate measurements in different analytical runs is advantageous. This helps identify sample mix-ups, transposition errors, and other blunders that could be misinterpreted as methodological error [4].
- Timeframe: The experiment should be conducted over a minimum of 5 days, and ideally longer (e.g., 20 days), incorporating several different analytical runs. This helps minimize the impact of systematic errors that might occur in a single run and provides a more realistic picture of long-term performance [4].
A Practical, Stepwise Analytical Workflow
We advocate a stepwise approach to data analysis, focused on identifying and characterizing different components of error [91]. The following workflow outlines this systematic process.
Step 1: Characterize Imprecision
Before comparing methods, accurately characterize the imprecision (random error) of each method across the measuring range. This can be presented as a characteristic function of standard deviation versus concentration and is crucial for understanding the baseline noise of each method [91].
Step 2: Graph the Data for Visual Inspection
The most fundamental analysis technique is to graph the data. This should be done as data is collected to identify discrepant results early [4].
- Scatter/Comparison Plot: Plot the test method results (y-axis) against the comparative method results (x-axis). Visually inspect the plot for the analytical range, linearity, and the general relationship between methods. Draw a visual line of best fit [4].
- Difference Plot: If the methods are expected to show one-to-one agreement, a difference plot (Bland-Altman-type plot) is highly informative. Plot the difference between the test and comparative results (test - comparative) on the y-axis against the comparative result on the x-axis. The points should scatter randomly around the line of zero difference [4] [91].
- Goal: Identify any obvious outliers, potential constant bias (all points shifted above or below zero), or proportional bias (differences increasing/decreasing with concentration) [4]. Any extreme discrepancies should be investigated and reanalyzed if possible.
Step 3: Calculate Statistical Estimates of Systematic Error
Statistical calculations provide numerical estimates of the errors visually identified in the graphs.
- For a Wide Analytical Range (e.g., glucose, cholesterol): Use linear regression statistics (slope
b, y-intercepta) to model the relationship [4]. The systematic error (SE) at any critical medical decision concentration (Xc) is calculated as: - For a Narrow Analytical Range (e.g., sodium, calcium): Calculate the average difference (bias) between the two methods. This is typically derived from a paired t-test analysis. The standard deviation of these differences describes the spread [4].
Step 4: Analyze Differences After Bias Correction
After identifying constant or proportional bias through regression, the data can be corrected for these systematic errors. The remaining differences then reflect the imprecision and sample-specific biases (matrix effects) of both methods [91]. The standard deviation of these differences (SDD) can be compared to the SDD predicted from the methods' imprecision data. A larger observed SDD indicates the presence of sample-method interaction bias [91].
Step 5: Decision on Method Acceptability
The final step is to compare the estimated systematic errors (from Step 3) against a priori defined acceptability limits based on clinical or analytical requirements [91]. If the errors are within these limits, the method can be considered fit-for-purpose.
Data Analysis and Statistical Output
Key Statistical Parameters Table
The following table summarizes the key statistics you will encounter and their interpretation.
Table 1: Key Statistical Parameters in Method Comparison
| Statistical Parameter | Description | Interpretation in Method Comparison |
|---|---|---|
Slope (b) |
The slope of the linear regression line. | Indicates proportional error. b = 1 means no proportional error; b > 1 or b < 1 indicates the error is concentration-dependent [4] [40]. |
Y-Intercept (a) |
The y-intercept of the linear regression line. | Indicates constant error. a = 0 means no constant error; a > 0 or a < 0 indicates a fixed bias across all concentrations [4] [40]. |
| Average Difference (Bias) | The mean of differences between test and comparative method results. | An estimate of the overall systematic error between the two methods [4]. |
| Standard Deviation of Differences (SDD) | The standard deviation of the differences. | Quantifies the dispersion of the differences around the mean difference. A larger SDD indicates greater random dispersion and/or sample-method bias [91]. |
Standard Error of the Estimate (s₍y/x₎) |
The standard deviation of the points around the regression line. | A measure of the scatter of the data around the line of best fit [4]. |
Correlation Coefficient (r) |
A measure of the strength of the linear relationship. | Primarily useful for verifying a wide enough data range for reliable regression. An r > 0.99 suggests a good range; lower values may indicate a need for more data [4]. It does not indicate agreement. |
Data Analysis Workflow Diagram
The statistical analysis follows a logical sequence from data inspection to final judgment, as illustrated below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Reagents and Materials for Method Comparison Studies
| Item | Function / Purpose |
|---|---|
| Patient Specimens | The primary sample for analysis. Should represent the full spectrum of diseases and conditions encountered in routine practice to test the method's real-world robustness [4]. |
| Certified Reference Materials | Samples with a known concentration of the analyte, used as a gold standard for assessing accuracy and systematic error in method comparison experiments [40]. |
| Quality Control (QC) Materials | Stable materials with known expected values, used to monitor the precision and stability of the measurement procedure during the study [40]. |
| Calibrators | Materials used to calibrate the instrument and establish the relationship between the instrument's response and the analyte concentration [40]. |
Troubleshooting Common Issues & FAQs
Q1: My scatter plot looks good, but the difference plot shows a clear pattern. Which one should I trust? The difference plot is often more sensitive for detecting specific bias patterns. A scatter plot can hide systematic biases, especially constant biases, because the eye is drawn to the overall linear trend. The difference plot explicitly shows the differences versus the magnitude, making patterns like proportional error much easier to see [91]. Always use both plots, but rely heavily on the difference plot for error identification.
Q2: I found an outlier. What should I do? First, check for possible errors in data recording or sample mix-ups. If duplicates were performed, check if the discrepancy is repeatable [4]. If no obvious mistake is found, statistical guidance suggests removing the outlier and investigating it separately, as it may represent a sample-specific interference (e.g., unique matrix effect) [4] [91]. The decision to exclude should be documented transparently in your report.
Q3: What is the minimum acceptable correlation coefficient (r) for my data?
There is no universal minimum r. The correlation coefficient is more useful for ensuring your data range is wide enough to give reliable estimates of the slope and intercept. If r is less than 0.99, it may indicate your data range is too narrow, and you should consider collecting additional data at the extremes of the reportable range [4]. Do not use a high r value to claim good agreement, as it measures strength of relationship, not agreement.
Q4: How do I differentiate between a constant and a proportional systematic error? This is determined from the linear regression parameters.
- Constant Error: Is indicated by a y-intercept (
a) that is significantly different from zero. This represents a fixed amount of bias that is the same at all concentrations [4] [40]. - Proportional Error: Is indicated by a slope (
b) that is significantly different from one. This represents a bias that increases or decreases as a proportion of the analyte concentration [4] [40]. Your regression output (slope and intercept) along with their confidence intervals will help you identify which type is present.
Q5: My method shows significant systematic error. What are potential sources? Systematic error typically stems from calibration issues [91] [40].
- Constant Bias: Often due to insufficient blank correction, background interference, or an offset in calibration [40].
- Proportional Bias: Often due to an error in the assigned value of a calibrator, differences in the specificity of the methods, or matrix effects between calibrators and patient samples [91] [40]. Investigating these areas can help you identify and potentially correct the root cause.
Conclusion
Minimizing systematic error is not a single step but an integral component of the entire method validation lifecycle, requiring careful planning from experimental design through to statistical analysis. By understanding error sources, implementing rigorous comparison protocols, adeptly troubleshooting failures, and applying robust statistical validation, researchers can significantly enhance data reliability. Future directions should emphasize the adoption of more sophisticated error-handling frameworks that reflect real-world usage, the development of standardized reporting guidelines for method comparison studies, and a greater focus on the traceability of measurements to reference standards. Ultimately, these practices are paramount for generating trustworthy evidence that informs clinical guidelines and accelerates the development of safe and effective therapeutics.
References
- 1. Systematic Errors in Research: Definition, Examples [https://www.formpl.us/blog/systematic-research-errors]
- 2. Minimizing Systematic Error [https://courses.cit.cornell.edu/virtual_lab/LabZero/Minimizing_Systematic_Error.shtml]
- 3. . Random | Definition & Examples vs Systematic Error [https://www.scribbr.com/methodology/random-vs-systematic-error/]
- 4. The Comparison of Methods Experiment - Westgard QC [https://westgard.com/lessons/basic-method-validation/lesson23.html]
- 5. - Statistics By Jim Random Error vs Systematic Error [https://statisticsbyjim.com/basics/random-error-vs-systematic-error/]
- 6. Errors in pharmaceutical analysis | PPTX | Chemistry | Science [https://www.slideshare.net/BiNduXtrEiy/errors-in-pharmaceutical-analysis]
- 7. Systematic Error - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/computer-science/systematic-error]
- 8. Biological Matrix Effects in Quantitative Tandem Mass Spectrometry-Based Analytical Methods: Advancing Biomonitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4695332/]
- 9. Systematic and comprehensive strategy for reducing matrix effects in LC/MS/MS analyses - PubMed [https://pubmed.ncbi.nlm.nih.gov/17236825/]
- 10. Evaluation of systematic due to deproteinization, errors ... calibration [https://pubmed.ncbi.nlm.nih.gov/8925103/]
- 11. Metrology and Biomedical | by Ali Bulut | Medium Calibration [https://medium.com/@alibulutb/metrology-and-biomedical-calibration-52e97c26393a]
- 12. Top 5 Sources of Error in Biomedical Testing | PDF [https://www.slideshare.net/slideshow/top-5-sources-of-error-in-biomedical-testing/71934516]
- 13. Assessing the effectiveness of empirical calibration under different... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-022-01687-6]
- 14. Systematic Error - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/systematic-error]
- 15. Practices of Science: Scientific Error | manoa.hawaii.edu/ExploringOurFluidEarth [https://manoa.hawaii.edu/exploringourfluidearth/physical/world-ocean/map-distortion/practices-science-scientific-error]
- 16. in Epidemiology Systematic Error [https://www.numberanalytics.com/blog/ultimate-guide-systematic-error-epidemiology]
- 17. Sources of Error in Measurement in Research Methodology: Bias and Precision - LeanScape - LeanScape [https://leanscape.io/sources-of-measurement-error-bias-and-precision/]
- 18. Strategies to reduce diagnostic errors: a systematic review | BMC Medical Informatics and Decision Making | Full Text [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-019-0901-1]
- 19. Cognitive forcing strategies in clinical decisionmaking - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0196064402849459]
- 20. Computerized Clinical Decision Support To Prevent Medication Errors and Adverse Drug Events - Making Healthcare Safer IV - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK600580/]
- 21. Journal of Medical Internet Research - Digital Health Technology... [https://www.jmir.org/2025/1/e65546]
- 22. of Model-Informed Impact on Drug ... Development Drug Development [https://pubmed.ncbi.nlm.nih.gov/40135941/]
- 23. Advanced Algorithms of Mitigating Undermatched Systematic in... Error [https://link.springer.com/article/10.1007/s11340-025-01238-2]
- 24. Design, Analysis and Interpretation of Method-Comparison Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 25. Comparing methods of measurements [https://pubmed.ncbi.nlm.nih.gov/9075596/]
- 26. Points of Care in Using Statistics in Method-Comparison Studies - Westgard QC [https://westgard.com/essays/method-validation/essay19.html]
- 27. Methods of Minimizing Errors in Analysis, Accuracy, Precision and Significant Figures | Pharmaguideline [https://www.pharmaguideline.com/2021/10/methods-of-minimizing-errors-in-analysis.html]
- 28. Understanding Experimenter Bias: Definition, Types, and How to Reduce | Amplitude [https://amplitude.com/explore/experiment/experimenter-bias]
- 29. Minimizing Systematic Errors in Quantitative High Throughput Screening Data Using Standardization, Background Subtraction, and Non-Parametric Regression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5102623/]
- 30. Methods in causal inference. Part 1: causal and... diagrams [https://pmc.ncbi.nlm.nih.gov/articles/PMC11588567/]
- 31. Introduction to Directed - GeeksforGeeks Acyclic Graph [https://www.geeksforgeeks.org/dsa/introduction-to-directed-acyclic-graph/]
- 32. - Wikipedia Directed acyclic graph [https://en.wikipedia.org/wiki/Directed_acyclic_graph]
- 33. Methods of minimizing errors | PPTX [https://www.slideshare.net/slideshow/methods-of-minimizing-errors/243267760]
- 34. of Comparison : Passing and Bablok... - Biochemia Medica methods [https://www.biochemia-medica.com/en/journal/21/1/10.11613/BM.2011.010]
- 35. Chapter 50: Standardization and quality assurance of quantitative... [https://www.clinical-laboratory-diagnostics.com/k50.html]
- 36. Linear Method ... | Analyse-it® 2.30 documentation comparison [https://analyse-it.com/docs/230/user-guide/method-evaluation/linear]
- 37. Considerations: Basics for Preparing Sample or Basic... Size Clinical [https://pmc.ncbi.nlm.nih.gov/articles/PMC10133938/]
- 38. , power and effect Sample revisited... - Biochemia Medica size size [https://www.biochemia-medica.com/en/journal/31/1/10.11613/BM.2021.010502]
- 39. Statistical Sample Calculations for Size Trials - Quantics... Clinical [https://www.quantics.co.uk/blog/statistical-calculations-of-sample-size-for-clinical-trials/]
- 40. Systematic Error Detection in Laboratory Medicine | IntechOpen [https://www.intechopen.com/chapters/58071]
- 41. 3 Replication – Experimentology [https://experimentology.io/003-replication.html]
- 42. Systematic Error - SAGE Research Methods [https://methods.sagepub.com/reference/encyclopedia-of-survey-research-methods/n568.xml]
- 43. Principles for Designing and Developing a Workflow Monitoring Tool to Enable and Enhance Clinical Workflow Automation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769810/]
- 44. Data visualizations to detect systematic errors in laboratory assay results - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723702/]
- 45. Comparison of Manual Versus Automated Data Collection Method for an Evidence-Based Nursing Practice Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3644815/]
- 46. > Compare pairs > Statistical Reference Difference plot Guide [https://analyse-it.com/docs/user-guide/compare-pairs/difference-plot]
- 47. Mastering Lines of Best Fit in Pre-Algebra [https://www.numberanalytics.com/blog/mastering-lines-best-fit-pre-algebra]
- 48. Outlier - Wikipedia [https://en.wikipedia.org/wiki/Outlier]
- 49. Guidelines for Removing and Handling Outliers in... - Statistics By Jim [https://statisticsbyjim.com/basics/remove-outliers/]
- 50. How to Find Outliers | 4 Ways with Examples & Explanation [https://www.scribbr.com/statistics/outliers/]
- 51. Outliers and Outlier Detection - GeeksforGeeks [https://www.geeksforgeeks.org/data-analysis/what-is-outlier-detection/]
- 52. Measurements and Error Analysis [https://www.webassign.net/question_assets/unccolphysmechl1/measurements/manual.html]
- 53. Misconduct versus Honest Error and Scientific Disagreement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3443861/]
- 54. Understanding Outliers : A Complete Guide to Detection and... | Medium [https://medium.com/@timothyciesha/understanding-outliers-a-complete-guide-to-detection-and-handling-in-data-science-3fa4a620ac95]
- 55. Practical strategies for handling breakdown of multiple imputation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8017730/]
- 56. Stefvanbuuren [https://stefvanbuuren.name/fimd/sec-algoptions.html]
- 57. Handling Missingness, Failures , and Non - Convergence in Simulation... [https://arxiv.org/html/2409.18527v3]
- 58. Advanced Imputation for Surveys Strategies [https://www.numberanalytics.com/blog/advanced-survey-imputation-strategies]
- 59. Rethinking the handling of method failure in comparison studies [https://arxiv.org/html/2408.11594v3]
- 60. Rethinking the Handling of Method Failure in Comparison Studies [https://pubmed.ncbi.nlm.nih.gov/41065339/]
- 61. Calibration Practices in Clinical Mass Spectrometry: Review and Recommendations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9467832/]
- 62. Systematic error detection in experimental high-throughput screening | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-12-25]
- 63. AMT - Correcting in log-linear instrument bias in the... calibrations [https://amt.copernicus.org/articles/14/6551/2021/]
- 64. and XGBoost reweighting to reduce coverage and... Calibration [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02171-z]
- 65. NonClinical Dose Formulation Analysis Method Validation and Sample Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2976985/]
- 66. | Multirules by James Westgard - Rules QC Westgard Westgard [https://westgard.com/westgard-rules.html]
- 67. 2.pptx WESTGARD RULES [https://www.slideshare.net/slideshow/westgard-rules-2pptx/261902324]
- 68. - Wikipedia Westgard rules [https://en.wikipedia.org/wiki/Westgard_rules]
- 69. QC - The Multirule Interpretation - Westgard QC [https://www.westgard.com/lesson18.htm]
- 70. Ten Ways to do the Wrong QC Wrong - Westgard QC [https://westgard.com/lessons/westgard-rules/westgard-rules/quest16.html]
- 71. Best Practices for "Westgard Rules" - Westgard QC [https://westgard.com/lessons/westgard-rules/westgard-rules/lesson74.html]
- 72. Evaluation of Sigma Metrics and Westgard Rule Selection and Implementation of Internal Quality Control in Clinical Chemistry Reference Laboratory, Ethiopian Public Health Institute - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9300779/]
- 73. Coefficient of determination - Wikipedia [https://en.wikipedia.org/wiki/Coefficient_of_determination]
- 74. How To Interpret R-squared in Regression Analysis - Statistics By Jim [https://statisticsbyjim.com/regression/interpret-r-squared-regression/]
- 75. Understanding Bland - PMC Altman analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470095/]
- 76. [ Comparison of two measurement methods: the Bland and Altman ...] [https://pubmed.ncbi.nlm.nih.gov/10730176/]
- 77. Bland–Altman plot - Wikipedia [https://en.wikipedia.org/wiki/Bland%E2%80%93Altman_plot]
- 78. - Bland plot - MedCalc Statistical Software Manual Altman [https://www.medcalc.org/en/manual/bland-altman-plot.php]
- 79. Coefficient of Determination (R²) | Calculation & Interpretation [https://www.scribbr.com/statistics/coefficient-of-determination/]
- 80. The Bland - Altman method should not be used when one... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0278915]
- 81. Z-14: Estimating Analytical Errors Using Regression Statistics - Westgard QC [https://westgard.com/lessons/z-stats-basic-statistics/lesson44.html]
- 82. Statistics in Analytical Chemistry - Regression (5) [https://sites.chem.utoronto.ca/chemistry/coursenotes/analsci/stats/ErrRegr.html]
- 83. 3.1 - Inference for the Population Intercept and Slope | STAT 462 [https://online.stat.psu.edu/stat462/node/102/]
- 84. Mathematics of simple regression [https://people.duke.edu/~rnau/mathreg.htm]
- 85. Data Science One on One — Part 9: Standard ... | Medium Errors of [https://medium.com/@polanitzer/data-science-one-on-one-part-9-standard-errors-of-coefficients-ef64079804b9]
- 86. How to Calculate and Slope ... | Saturn Cloud Blog Intercept Error of [https://saturncloud.io/blog/how-to-calculate-slope-and-intercept-error-of-linear-regression/]
- 87. Basic Method Validation, 3rd Edition, FAQs - Westgard QC [https://westgard.com/resources/resources/bmv3edfaqs.html]
- 88. Validation of methods performance for routine... - Biochemia Medica [https://www.biochemia-medica.com/en/journal/21/2/10.11613/BM.2011.028]
- 89. analysis and Error of minimization | PhysicsFlow systematic errors [https://www.physicsflow.com/g8/2.8]
- 90. Drug Discovery Assays Support—Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 91. – a practical approach based on Method identification comparison error [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2017-0842/html]