Advanced UV-Visible Spectrophotometric Method Development and Validation for Paracetamol Tablet Analysis
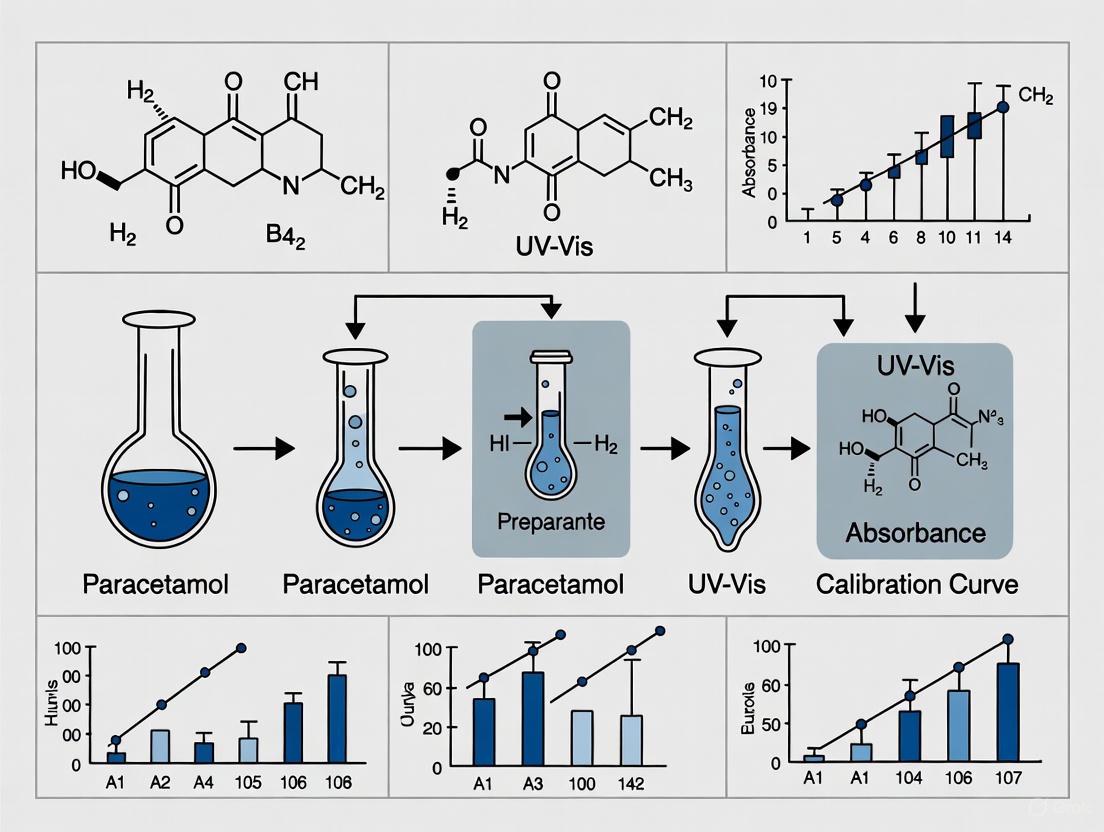
This article provides a comprehensive guide for researchers and pharmaceutical scientists on developing and validating robust UV-Visible spectrophotometric methods for paracetamol analysis in tablet formulations.
Advanced UV-Visible Spectrophotometric Method Development and Validation for Paracetamol Tablet Analysis
Abstract
This article provides a comprehensive guide for researchers and pharmaceutical scientists on developing and validating robust UV-Visible spectrophotometric methods for paracetamol analysis in tablet formulations. It covers foundational principles of UV-Vis spectroscopy and paracetamol's spectral characteristics, explores advanced methodologies including chemometric techniques and signal processing for complex mixtures, addresses critical troubleshooting and optimization strategies for common analytical challenges, and outlines rigorous validation protocols per ICH guidelines with comparative analysis against reference methods like HPLC. The content synthesizes current research to deliver a practical framework for implementing accurate, precise, and cost-effective spectrophotometric methods in pharmaceutical quality control and drug development settings.
Fundamental Principles and Spectral Characteristics of Paracetamol
Core Principles of UV-Visible Spectrophotometry and Beer-Lambert Law
UV-Visible spectrophotometry is a fundamental analytical technique in pharmaceutical research, enabling the identification and quantification of compounds based on their interaction with ultraviolet and visible light. For researchers focused on method development, such as for paracetamol tablet analysis, a deep understanding of the Beer-Lambert Law is indispensable for ensuring accurate, precise, and valid results. This document outlines the core principles, detailed protocols, and practical applications of UV-Vis spectrophotometry within the context of pharmaceutical method development, providing a structured framework for scientists and drug development professionals.
Core Theoretical Principles
The Beer-Lambert Law
The Beer-Lambert Law (also referred to as Beer's Law) is the central quantitative relationship governing absorption spectroscopy [1] [2]. It states that the absorbance of light by a solution is directly proportional to the concentration of the absorbing species and the path length the light takes through the solution. The mathematical expression of the law is:
A = ε × l × c
Where:
- A is the Absorbance (a dimensionless quantity) [2].
- ε is the Molar Absorptivity (or molar extinction coefficient), with units of L·mol⁻¹·cm⁻¹ [1].
- l is the Path Length of the cuvette, typically 1 cm [2].
- c is the Molar Concentration of the analyte in mol·L⁻¹ [1].
The law derives from the relationship between the incident light intensity ((I0)) and the transmitted light intensity ((I)) [1] [2]: [ A = \log{10} \left( \dfrac{I_o}{I} \right) ]
This relationship means that for a given path length and compound, absorbance increases linearly with concentration, forming the basis for quantitative analysis.
Transmittance and Absorbance
Transmittance (T) and Absorbance (A) are two key parameters for describing light attenuation [2].
- Transmittance is defined as the fraction of incident light that passes through a sample: ( T = I / I_0 ). It is often expressed as a percentage (%T).
- Absorbance has a logarithmic relationship to transmittance: ( A = \log{10} (1/T) = -\log{10} T ).
The table below shows the inverse logarithmic relationship between transmittance and absorbance [2].
Table 1: Relationship Between Absorbance and Transmittance
| Absorbance (A) | Transmittance (%T) |
|---|---|
| 0 | 100% |
| 1 | 10% |
| 2 | 1% |
| 3 | 0.1% |
| 4 | 0.01% |
A UV-Vis spectrophotometer consists of several key components [3]:
- Light Source: Typically a deuterium lamp (UV) and a tungsten or halogen lamp (Visible).
- Monochromator: Contains a diffraction grating or prism to select a specific wavelength of light.
- Cuvette Holder: Holds the sample and reference cuvettes. Standard path length is 1 cm.
- Detector: Measures the intensity of the transmitted light and converts it into an electrical signal.
The fundamental relationship between these components and the measurement process can be visualized as follows:
Quantitative Analysis and Method Validation
Calibration and Quantitative Determination
The primary application of the Beer-Lambert law in pharmaceutical analysis is the determination of unknown concentrations via a calibration curve [2]. A series of standard solutions with known concentrations are prepared, and their absorbance is measured at a specific wavelength. A plot of absorbance versus concentration yields a calibration curve, which should be linear within the working range. The concentration of an unknown sample is then determined from its absorbance using the equation of the calibration line.
Table 2: Exemplary Calibration Data for Paracetamol and Ibuprofen
| Concentration (µg/mL) | Paracetamol Absorbance (at 243 nm) | Ibuprofen Absorbance (at 221 nm) |
|---|---|---|
| 5 | 0.172 | - |
| 10 | 0.343 | - |
| 15 | 0.515 | - |
| 20 | 0.686 | 0.210 |
| 25 | 0.858 | - |
| 30 | 1.029 | - |
| 12 | - | 0.126 |
| 20 | - | 0.210 |
| 32 | - | 0.336 |
Note: Data is simulated based on typical linear relationships from research examples [4].
Analytical Method Validation
For a method to be suitable for drug analysis, it must be validated according to international guidelines (e.g., ICH). Key parameters and typical acceptance criteria for a UV-Vis method, as demonstrated in studies on paracetamol and other drugs, are summarized below [5].
Table 3: Key Validation Parameters for a UV-Vis Spectrophotometric Method
| Validation Parameter | Target Value / Outcome | Example from Literature |
|---|---|---|
| Linearity | Correlation coefficient (R²) > 0.999 | Terbinafine HCl: R² = 0.999 [5] |
| Range | e.g., 5-30 µg/mL | Paracetamol (via reaction): up to 6 µg/mL [6] |
| Accuracy (% Recovery) | 98-102% | Terbinafine HCl: 98.54-99.98% [5] |
| Precision (% RSD) | < 2% | Terbinafine HCl: Intraday & Interday RSD < 2% [5] |
| LOD (Limit of Detection) | e.g., 0.10 µg/mL | Paracetamol (via reaction): 0.10 µg/mL [6] |
| LOQ (Limit of Quantification) | e.g., 0.42 µg/mL | Terbinafine HCl: 0.42 µg [5] |
Experimental Protocols for Paracetamol Analysis
Protocol 1: Standard Solution Preparation and λ_max Determination
This protocol is the first step in method development, aimed at identifying the optimal wavelength for analysis.
Workflow: Wavelength Selection and Calibration
Materials and Reagents:
- Active Pharmaceutical Ingredient (API): Paracetamol reference standard.
- Solvent: Distilled water, ethanol, or phosphate buffer (pH 7.2) [5] [4].
- Volumetric flasks (e.g., 100 mL, 10 mL).
- Pipettes and micropipettes.
- UV-Vis spectrophotometer with 1 cm quartz cuvettes.
Procedure:
- Stock Solution (1000 µg/mL): Accurately weigh 100 mg of paracetamol reference standard. Transfer quantitatively to a 100 mL volumetric flask, dissolve, and make up to volume with the chosen solvent [5].
- Working Solution (10 µg/mL): Pipette 1.0 mL of the stock solution into a 100 mL volumetric flask and dilute to volume with solvent.
- Spectral Scanning: Fill a 1 cm quartz cuvette with the working solution. Place the solvent blank in the reference holder. Scan the absorption spectrum over the wavelength range of 200-400 nm.
- λmax Determination: Identify the wavelength of maximum absorption (λmax) from the resulting spectrum. For paracetamol, this is typically observed at 243 nm in ethanol-NaOH solvent systems and around 283 nm in aqueous systems [5] [4].
Protocol 2: Tablet Assay and Recovery Study
This protocol is for quantifying the drug content in a formulated tablet and validating the method's accuracy.
Materials and Reagents:
- Paracetamol tablets (commercially available).
- Paracetamol reference standard.
- Same solvents and glassware as in Protocol 1.
- Ultrasonic bath.
Procedure:
- Sample Preparation:
- Weigh and finely powder 20 tablets [7].
- Accurately weigh a portion of the powder equivalent to about 100 mg of paracetamol into a 100 mL volumetric flask.
- Add approximately 70 mL of solvent, sonicate for 20-30 minutes with intermittent shaking to ensure complete dissolution, and cool to room temperature [5].
- Dilute to volume with solvent and mix well. Filter the solution, discarding the first few mL of the filtrate.
- Dilution:
- Pipette an appropriate volume of the filtrate (e.g., 1-5 mL, depending on expected concentration) into a 100 mL volumetric flask and dilute to volume with solvent to achieve a concentration within the linear range of the calibration curve.
- Absorbance Measurement:
- Measure the absorbance of the final sample solution at the predetermined λ_max against the solvent blank.
- Concentration Calculation:
- Calculate the concentration of the sample using the linear regression equation from the calibration curve.
- Determine the weight of paracetamol in the tablet and the percentage of the label claim using standard calculations.
- Accuracy (Recovery) Study:
- To pre-analyzed tablet powder, add known amounts of the paracetamol reference standard at three different levels (e.g., 80%, 100%, 120% of the label claim) [5].
- Process and analyze these samples as described above.
- Calculate the percentage recovery of the added standard.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions and Materials
| Item | Function / Purpose | Example & Notes |
|---|---|---|
| Reference Standard | Provides a highly pure substance for calibration; essential for accurate quantification. | Paracetamol BP/USP reference standard. |
| Phosphate Buffer (pH 7.2) | Acts as a spectrophotometric solvent; maintains pH to ensure consistent analyte form and absorbance. | 250 mL 0.2M KH₂PO₄ + 175 mL 0.2M NaOH, diluted to 1L [8]. |
| Ethanol-NaOH Mixture | Solvent system for drugs with poor water solubility; can enhance solubility and stabilize the analyte. | 3:1 ratio of Ethanol to NaOH solution [4]. |
| Ammonium Molybdate | Reagent for derivatization; reacts with specific functional groups to form a colored complex (Molybdenum Blue). | Used for spectrophotometric determination of paracetamol [6]. |
| Quartz Cuvettes (1 cm) | Holds the sample solution for analysis; quartz is transparent to UV light. | Ensure clean, scratch-free surfaces for accurate readings. |
| Volumetric Glassware | For precise preparation and dilution of standard and sample solutions. | Use Class A flasks and pipettes for highest accuracy. |
| Membrane Filters (0.45 µm) | Clarifies sample solutions by removing particulate matter from tablet extracts. | Prevents light scattering and ensures a clear path for the beam. |
Critical Considerations and Limitations
While the Beer-Lambert law is foundational, several factors can cause deviations from ideal behavior and must be considered during method development [9] [3].
- Chemical Deviations: Occur at high concentrations (>0.01 M) due to molecular interactions or changes in the refractive index of the solution [9] [3]. The linear relationship between A and c may break down.
- Spectral Limitations: Stray light within the instrument or a bandwidth that is too wide can lead to inaccurate absorbance measurements, particularly at high absorbance values [3].
- Instrumental Factors: Dirty cuvettes, misalignment, and detector non-linearity can introduce errors [3].
- Electromagnetic Effects: The BBL law is a simplification of light-matter interactions. Effects such as band shifts and intensity changes can arise from the wave nature of light, especially in non-liquid samples or at interfaces [9].
Spectral Properties and Absorbance Maxima of Paracetamol
This application note details the critical spectral properties and experimental protocols for the analysis of paracetamol (also known as acetaminophen) using UV-Visible spectrophotometry. Framed within a broader thesis on method development for paracetamol in solid dosage forms, this document provides researchers and pharmaceutical scientists with validated methodologies and key parameters essential for accurate quantitative determination in bulk drug substances and formulated tablets. The fundamental principle underpinning these methods is the Beer-Lambert Law, which establishes a linear relationship between the absorbance of a solution and the concentration of the analyte, enabling precise quantification [10]. Understanding the absorbance characteristics of paracetamol, including its maximum absorbance wavelength (λmax) and how it is influenced by solvent systems, is a cornerstone of robust analytical method development for quality control in drug development.
Quantitative Spectral Data
The absorbance maximum of paracetamol is not fixed and can exhibit bathochromic or hypsochromic shifts depending on the solvent's polarity, pH, and chemical composition. The following table consolidates key spectral data for paracetamol from various validated solvent systems.
Table 1: Absorbance Maxima and Validation Parameters of Paracetamol in Different Solvent Systems
| Solvent System | Reported λmax (nm) | Linear Range (μg/mL) | Correlation Coefficient (R²) | LOD (μg/mL) | LOQ (μg/mL) | Reference |
|---|---|---|---|---|---|---|
| Methanol | 243, 200 | 2 - 44 | 0.998 | 0.432 | 1.440 | [11] [12] |
| Phosphate Buffer (pH 6.8) & Methanol (3:1) | 246 | 2 - 24 | 0.999 | 0.328 | 0.984 | [11] |
| Ethanol & 0.1M NaOH (3:1) | 243, 257 | 2 - 10 | Adheres to Beer's Law | 0.198 | 0.538 | [13] |
| 0.1N NaOH | 257 | 10 (for calibration) | Adheres to Beer's Law | - | - | [13] |
| Water (as function of pH) | Varies with pH | - | - | - | - | [14] |
Key Observations on Spectral Behavior
- Solvent-Dependent Shifts: Paracetamol consistently exhibits two primary absorbance bands in the UV region. The specific λmax can shift; for instance, a notable shift from 243 nm in pure methanol to 246 nm in a methanol-phosphate buffer mixture is observed [11].
- Effect of Alkaline Medium: In alkaline solvents like sodium hydroxide, the deprotonation of the phenolic hydroxyl group in paracetamol can cause a significant bathochromic shift, moving the λmax to a longer wavelength around 257 nm [13] [14].
- Method Suitability: The choice of solvent system directly impacts the sensitivity and selectivity of the method. The mixture of ethanol and sodium hydroxide (3:1), for example, is particularly effective for the simultaneous analysis of paracetamol and ibuprofen in combined dosage forms, as it ensures good solubility for both drugs with minimal spectral interference [13].
Experimental Protocols
Protocol 1: Standard Method for Paracetamol in Methanol or Phosphate Buffer-Methanol Mixture
This is a general and robust method suitable for the analysis of paracetamol in bulk powder and tablet formulations [11].
Workflow Overview
Materials and Procedure
Step 1: Standard Stock Solution Preparation
- Accurately weigh 100 mg of paracetamol reference standard and transfer it to a 100 mL volumetric flask.
- Add approximately 70 mL of your chosen solvent—either pure methanol or a mixture of methanol and phosphate buffer pH 6.8 in a 1:3 ratio. Vortex mix and sonicate for 10 minutes to ensure complete dissolution.
- Dilute to volume with the same solvent to obtain a primary stock solution of 1000 µg/mL.
- Filter this solution through Whatman filter paper No. 41 to remove any particulate matter.
Step 2: Working Standard Solution Preparation
- Pipette 10 mL of the filtered primary stock solution into another 100 mL volumetric flask.
- Dilute to volume with phosphate buffer pH 6.8 to obtain a secondary stock solution of 100 µg/mL.
Step 3: Calibration Curve Construction
- From the 100 µg/mL secondary stock, prepare a series of standard solutions with concentrations covering the range of 2–24 µg/mL (e.g., 2, 4, 8, 12, 16, 20, 24 µg/mL) using phosphate buffer pH 6.8 as the diluent.
- Measure the absorbance of each standard solution at the predetermined λmax (243 nm for pure methanol or 246 nm for the mixed solvent system) against a solvent blank.
- Plot the average absorbance (y-axis) against the corresponding concentration (x-axis) and determine the regression equation.
Method Validation Notes: This method has been validated showing a correlation coefficient (R²) > 0.999. Intra-day and inter-day precision (RSD) were reported to be less than 0.3% and 0.6%, respectively, with accuracy ranging from 99.92% to 100.94% [11] [12].
Protocol 2: Simultaneous Analysis of Paracetamol and Ibuprofen in an Ethanol-NaOH Solvent System
This method is optimized for fixed-dose combination products containing both paracetamol and ibuprofen [13].
Workflow Overview
Materials and Procedure
Step 1: Mixed Solvent System Preparation
- Prepare the solvent mixture by combining 75 mL of absolute ethanol with 25 mL of 0.1 M sodium hydroxide solution (a 3:1 ratio). This mixture enhances the solubility of ibuprofen, which may not dissolve adequately in ethanol alone.
Step 2: Standard Stock Solutions Preparation
- Separately weigh 25 mg of paracetamol and 25 mg of ibuprofen.
- Transfer each drug to separate 100 mL volumetric flasks. Dissolve and dilute to volume with the ethanol-NaOH solvent mixture to obtain stock solutions of 250 µg/mL for each drug.
Step 3: Dilution and Spectral Acquisition
- Make further dilutions of the individual stock solutions with distilled water to create a calibration series in the range of 10–50 µg/mL for each drug.
- Using a UV-Vis spectrophotometer, scan the solutions of pure paracetamol and pure ibuprofen across the 200–400 nm range to identify their respective absorbance maxima. Paracetamol typically shows a maximum at 243 nm, while ibuprofen shows a maximum at 221 nm [13].
- Measure the absorbance of the standard solutions at both wavelengths.
Step 4: Data Analysis using Simultaneous Equations
- The concentrations of paracetamol (CP) and ibuprofen (CI) in a mixture can be calculated using the following simultaneous equations, based on the absorptivity values of each drug at the two wavelengths:
A1 = (ax1 * C_P) + (ay1 * C_I)(Equation for λ1, 243 nm)A2 = (ax2 * C_P) + (ay2 * C_I)(Equation for λ2, 221 nm)
- Where A1 and A2 are the absorbances of the mixture at the two wavelengths, ax1 and ax2 are the absorptivities of paracetamol at λ1 and λ2, and ay1 and ay2 are the absorptivities of ibuprofen at λ1 and λ2.
- The concentrations of paracetamol (CP) and ibuprofen (CI) in a mixture can be calculated using the following simultaneous equations, based on the absorptivity values of each drug at the two wavelengths:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Paracetamol UV Spectrophotometric Analysis
| Reagent/Material | Specification/Function | Application Example |
|---|---|---|
| Paracetamol Reference Standard | High-purity compound for preparing calibration standards; essential for accurate quantification. | Used in all protocols to create primary stock solutions. |
| UV-Grade Methanol | High-purity solvent to minimize UV background interference; commonly used for dissolving paracetamol. | Main solvent in Protocol 1 [11]. |
| Phosphate Buffer (pH 6.8) | Mimics physiological pH; used as a diluent to create a stable and reproducible analytical environment. | Diluent in mixed solvent system and for calibration curves [11]. |
| Sodium Hydroxide (0.1 M) | Alkaline medium that ionizes paracetamol, causing a spectral shift; improves solubility in combination drugs. | Component of ethanol-NaOH solvent system for simultaneous analysis (Protocol 2) [13]. |
| UV-Grade Ethanol | Solvent for dissolving active ingredients, particularly useful in combination drug analysis. | Component of ethanol-NaOH solvent system (Protocol 2) [13]. |
| Volumetric Flasks | For precise preparation and dilution of standard and sample solutions. | Used in all solution preparation steps. |
| Quartz Cuvettes | For holding samples in the spectrophotometer; transparent to UV light. | Required for all absorbance measurements. |
| Whatman Filter Paper (No. 41) | For clarification of sample solutions to remove insoluble excipients or particulates. | Filtration of tablet sample solutions prior to analysis [11]. |
Advanced Considerations: The Role of pH and Chemometrics
For complex matrices where excipients cause significant spectral interference, advanced strategies beyond direct spectrophotometry are required.
- pH-Dependent Spectral Analysis: The UV spectrum of paracetamol is highly sensitive to pH due to the ionization of its hydroxyl group. The acid dissociation constant (pKa) of paracetamol is a critical parameter, and spectral shifts across a pH gradient (e.g., from 4 to 12) can be exploited for analysis [14].
- Multiway Chemometric Models: Techniques such as PARAFAC (Parallel Factor Analysis) can be applied to a three-way dataset (absorbance vs. wavelength vs. pH). This advanced mathematical approach can successfully resolve the paracetamol spectrum even in the presence of overlapping excipient signals, enabling accurate quantification without physical separation steps [14]. This is particularly valuable for analyzing syrup formulations or other complex dosage forms.
Solvent Selection and Optimization for Paracetamol Analysis
Within the framework of method development for paracetamol tablet analysis using UV-Vis spectrophotometry, the selection and optimization of the solvent system is a critical foundational step. The choice of solvent directly influences key analytical parameters including solubility, spectral characteristics, chemical stability, and the ultimate accuracy and precision of the quantification method. This document provides detailed application notes and protocols to guide researchers and drug development professionals in selecting and optimizing solvent systems for the UV-Vis spectrophotometric analysis of paracetamol, with particular emphasis on addressing challenges in multi-component formulations.
Solvent Systems and Spectral Characteristics
The optimal solvent system must ensure complete dissolution of the analyte, provide a stable spectral profile, and minimize interference with excipients or other active ingredients. The following table summarizes validated solvent systems for paracetamol analysis, including systems suitable for challenging combination products.
Table 1: Solvent Systems and Spectral Properties for Paracetamol Analysis
| Analytical Context | Recommended Solvent System | Paracetamol λmax (nm) | Linearity Range (µg/mL) | Key Advantages | Citations |
|---|---|---|---|---|---|
| General Analysis | Methanol | 243-257 | 2.5 - 30 | Good solubility, minimal interference, common solvent. | [15] [10] |
| Paracetamol & Ibuprofen | Ethanol + 0.1 M NaOH (3:1) | 243 | 2 - 10 | Enhances ibuprofen solubility; distinct, stable peaks for both drugs. | [13] [16] |
| Paracetamol & Meloxicam | Methanol (with minimal DMF for MEL) | 262 (1D trough) | 2.5 - 30 | Resolves severe spectral overlap via 1D derivative. | [15] |
| Paracetamol & Domperidone | Methanol | N/A (Ratio Difference) | 3 - 70 | Effective for analyzing drugs with a 25:1 ratio (PAR:DOM). | [15] |
| Paracetamol & Caffeine | Acetate Buffer : Methanol (30:70) | 258 | Meeting pharmacopoeial specs | Zero-crossing derivative method resolves overlapping spectra. | [17] |
For the analysis of paracetamol with ibuprofen, a mixed solvent system of ethanol and 0.1 M sodium hydroxide (NaOH) in a 3:1 ratio has been demonstrated as particularly effective [13] [16]. This system enhances the solubility of ibuprofen, which may not dissolve well in ethanol alone, while maintaining the chemical stability of both compounds. In this solvent, paracetamol and ibuprofen exhibit distinct absorbance maxima at 243 nm and 221 nm, respectively, with minimal spectral interference and no significant alteration of peak positions or intensities due to the alkaline component [13].
Detailed Experimental Protocols
Protocol for Simultaneous Analysis of Paracetamol and Ibuprofen
This protocol details the use of an ethanol-NaOH solvent system for the simultaneous estimation of paracetamol and ibuprofen in combined dosage forms [13].
Materials and Equipment
- UV-Vis Spectrophotometer equipped with 1 cm quartz cells [13].
- Analytical balance [13].
- Paracetamol and Ibuprofen reference standards.
- Ethanol (absolute) and 0.1 M Sodium Hydroxide (NaOH) solution.
- Volumetric flasks (10 mL, 100 mL), pipettes, and other standard laboratory glassware.
Preparation of Standard Stock Solutions
- Paracetamol Stock Solution (1000 µg/mL): Accurately weigh 25 mg of paracetamol reference standard and transfer to a 25 mL volumetric flask. Dissolve and make up to volume with the ethanol-NaOH (3:1) solvent mixture [13].
- Ibuprofen Stock Solution (1000 µg/mL): Accurately weigh 25 mg of ibuprofen reference standard and transfer to a separate 25 mL volumetric flask. Dissolve and make up to volume with the same ethanol-NaOH (3:1) solvent mixture [13].
Construction of Calibration Curves
- Prepare Working Solutions: From the stock solutions, prepare a series of working standard solutions for each drug. For paracetamol and ibuprofen, dilute appropriate volumes to obtain concentrations within the range of 2–10 µg/mL using the ethanol-NaOH solvent [13].
- Spectral Acquisition: Scan the absorbance of each working solution across the 200–400 nm range against a blank of the ethanol-NaOH (3:1) solvent [13].
- Measurement and Plotting: Record the absorbance of paracetamol at 243 nm and ibuprofen at 221 nm. Plot the absorbance values against the corresponding concentrations for each drug to construct the calibration curves [13].
- Validation: Ensure the calibration curves demonstrate linearity adhering to Beer-Lambert's law. The correlation coefficient (R²) should typically be ≥0.999 for a robust method.
Protocol for Analysis of Paracetamol with Severely Overlapping Spectra
This protocol employs derivative and ratio spectrophotometry to resolve paracetamol from drugs with significant spectral overlap, such as meloxicam or domperidone [15].
For Paracetamol and Meloxicam (Mixture I)
- Stock Solutions: Prepare a 1000 µg/mL paracetamol standard solution in methanol. Prepare meloxicam stock solution (1000 µg/mL) by first dissolving in a minimal volume of dimethylformamide (DMF) and then diluting to volume with methanol. Protect from light [15].
- First-Order Derivative (1D) Spectrophotometry:
- Generate the first-derivative spectra of the standard and sample solutions.
- For paracetamol, measure the amplitude from the zero line to the trough at 262 nm. At this wavelength, the derivative spectrum of meloxicam shows zero crossing, thus causing no interference [15].
- Construct the calibration curve by plotting the 1D amplitude at 262 nm against the paracetamol concentration.
For Paracetamol and Domperidone (Mixture II)
- Stock Solutions: Prepare standard solutions of paracetamol and domperidone (1000 µg/mL each) in methanol [15].
- Ratio Difference Method:
- Obtain the absorption spectra of the sample and standard solutions.
- To analyze paracetamol, divide the stored absorption spectra by the spectrum of a standard 50 µg/mL domperidone solution (the "divisor") to obtain the ratio spectra [15].
- For the quantitation of paracetamol, record the difference between the amplitudes of the ratio spectrum at 256 nm and 288 nm.
- Plot this difference against the corresponding paracetamol concentrations to build the calibration curve [15].
Workflow and Decision Pathway
The following diagram illustrates the logical workflow for selecting and optimizing a solvent and method based on the analytical goal.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Materials for Method Development
| Reagent/Material | Function in Analysis | Application Notes |
|---|---|---|
| Methanol | Primary solvent for dissolution and dilution. | Provides good solubility for paracetamol; suitable for direct and derivative UV methods [15]. |
| Ethanol-NaOH Mixture | Mixed solvent for analyzing paracetamol-ibuprofen combinations. | The alkaline component (NaOH) enhances solubility of acidic drugs like ibuprofen and ensures distinct spectral peaks [13] [16]. |
| Dimethylformamide (DMF) | Co-solvent for poorly water-soluble drugs. | Used in minimal quantities to dissolve drugs like meloxicam before final dilution with methanol [15]. |
| Paracetamol Reference Standard | Primary standard for calibration. | Essential for constructing accurate and validated calibration curves. Purity must be certified. |
| Quartz Cuvettes | Holder for sample solution in spectrophotometer. | Required for UV range measurements; must be matched for double-beam instruments [15]. |
Instrumentation Parameters and Optimal Measurement Conditions
Within the framework of method development for paracetamol tablet analysis, the selection of appropriate instrumentation parameters and measurement conditions is a critical determinant of success in UV-Vis spectrophotometry. This technique remains a cornerstone in pharmaceutical analysis due to its simplicity, cost-effectiveness, and reliability for routine quality control [10] [18]. The fundamental principle governing quantitative analysis is the Beer-Lambert law, which establishes a linear relationship between absorbance and concentration, expressed as A = abc, where A is absorbance, a is absorptivity, b is the path length, and c is the concentration of the analyte [10] [18]. For researchers and drug development professionals, optimizing these parameters ensures the generation of accurate, precise, and validatable data for pharmaceutical formulations.
Key Instrumentation Parameters
The core parameters of a UV-Vis spectrophotometer directly influence the sensitivity, accuracy, and overall performance of the analytical method for paracetamol.
Wavelength Selection
Identifying the wavelength of maximum absorption (λmax) is paramount for achieving optimal sensitivity. For paracetamol, this parameter can vary depending on the solvent system employed.
- In 0.1N HCl and Phosphate Buffer (pH 6.8): Paracetamol exhibits a consistent absorbance maximum at 243 nm [19].
- In Methanol: The λmax has been reported at 248.8 nm [20].
- In an Ethanol-Sodium Hydroxide Solvent System: A shift in the absorption maximum to 257 nm can be observed [13].
This solvent-dependent shift underscores the necessity of establishing the exact λmax for paracetamol within the specific solvent system chosen for the analysis.
Spectral Bandwidth and Path Length
The use of a standard 1 cm path length quartz cuvette is nearly universal in these analyses [5] [20] [21]. The spectral bandwidth, a function of the spectrophotometer's monochromator, should be specified to ensure minimal stray light and adherence to the Beer-Lambert law. While a bandwidth of 1-2 nm is typical for modern instruments, the specific setting should be confirmed and held constant throughout the analysis to maintain consistency.
Optimal Solvent and Sample Conditions
The choice of solvent system is a critical methodological decision that affects solubility, stability, and the resulting spectral characteristics of paracetamol.
Solvent Systems for Paracetamol
| Solvent System | Composition | Reported λmax (nm) | Key Considerations |
|---|---|---|---|
| Aqueous Acidic | 0.1N Hydrochloric Acid (HCl) | 243 [19] | Provides a stable acidic environment; suitable for dissolution studies in simulated gastric fluid. |
| Buffered Solution | Phosphate Buffer pH 6.8 | 243 [19] | Biorelevant medium for dissolution studies simulating intestinal conditions. |
| Alkaline Solvent Mixture | Ethanol & 0.1M NaOH (3:1 or 75:25) | 257 [13] | Enhances solubility; ionization of paracetamol's phenolic group can cause a bathochromic (red) shift. |
| Organic Solvent | Methanol | 248.8 [20] | Good solubility for paracetamol; commonly used for stock solution preparation. |
Sample Preparation Protocol
A typical sample preparation workflow for the analysis of paracetamol in tablet formulations is as follows:
- Stock Solution Preparation: Accurately weigh a quantity of powdered tablets equivalent to about 100 mg of paracetamol. Transfer this powder to a 100 mL volumetric flask. Add approximately 50-70 mL of the chosen solvent (e.g., 0.1N HCl, methanol) and sonicate for 10-15 minutes to ensure complete dissolution of the active ingredient. Dilute to volume with the same solvent to obtain a stock solution of known concentration (e.g., 1000 µg/mL) [19].
- Filtration: Filter the solution using a membrane filter (e.g., 0.45 µm) to remove insoluble excipients and ensure a particulate-free solution [19].
- Dilution to Linear Range: Make an appropriate dilution of the filtrate with the solvent to bring the concentration within the validated linear range of the method, typically between 5-25 µg/mL [20] [19]. For instance, a 1 mL aliquot of the 1000 µg/mL stock can be diluted to 100 mL to yield a 10 µg/mL working standard.
Method Validation Parameters
For any analytical method to be suitable for drug development and quality control, it must be validated as per International Council for Harmonisation (ICH) guidelines. The following table summarizes typical validation parameters and their target values for a paracetamol UV-Vis method, as evidenced by research on similar drugs.
| Validation Parameter | Experimental Procedure | Target Acceptance Criteria |
|---|---|---|
| Linearity & Range | Prepare and analyze standard solutions at multiple concentrations (e.g., 5-30 µg/mL) [5] [20]. | Correlation coefficient (r²) ≥ 0.998 [5] [20]. |
| Accuracy (Recovery) | Spike pre-analyzed samples with standard at 80%, 100%, and 120% of the label claim and re-analyze [5]. | % Recovery between 98% - 102% [5] [20]. |
| Precision | Analyze multiple replicates (n=3-6) of the same sample concentration intra-day and inter-day [5]. | % RSD (Relative Standard Deviation) < 2.0% [5]. |
| LOD & LOQ | Calculate based on standard deviation of the response and the slope of the calibration curve (LOD=3.3σ/S, LOQ=10σ/S) [5]. | Signal-to-noise ratio ~3:1 for LOD and ~10:1 for LOQ [13]. |
| Specificity | Demonstrate that excipients in the tablet formulation do not interfere with the analyte's measurement at the λmax [19]. | No interference from blank or placebo at the analytical wavelength. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details the key materials required for the development and application of a UV-Vis spectrophotometric method for paracetamol tablets.
| Item | Function / Application |
|---|---|
| Double-beam UV-Vis Spectrophotometer | Primary instrument for measuring light absorption by the sample solution; double-beam design compensates for source fluctuations [20] [19]. |
| Quartz Cuvettes (1 cm path length) | Holds the sample and reference solutions; quartz is transparent across the UV-Vis range [13] [21]. |
| Analytical Balance | Used for the accurate weighing of standard drugs and tablet powder [13] [21]. |
| Paracetamol Reference Standard | Highly purified material used to prepare calibration standards for quantitative analysis. |
| Volumetric Flasks | For precise preparation of standard and sample solutions [5] [19]. |
| Membrane Filters (0.45 µm) | Clarification of sample solutions by removing insoluble particulate matter from tablet excipients [19]. |
| Sonicator / Ultrasonic Bath | Aids in the complete dissolution and degassing of samples in volumetric flasks [20]. |
| pH Meter | Essential for the preparation of buffered dissolution media, such as 0.1N HCl and Phosphate Buffer pH 6.8 [19] [21]. |
Advanced Applications: Analysis in Multi-Component Formulations
A significant challenge in pharmaceutical analysis is the quantification of paracetamol in fixed-dose combinations (FDCs), where spectral overlap with other active ingredients occurs. UV-Vis spectrophotometry, accounting for approximately 37.9% of analytical methods for ibuprofen and paracetamol FDCs, remains a viable and economical technique [10]. Strategies to resolve overlapping spectra include:
- Simultaneous Equation Method: This method utilizes the absorptivity values of each drug at two different wavelengths (e.g., λmax of paracetamol and λmax of the second drug) to set up and solve a pair of equations for their respective concentrations [13] [10].
- Area Under Curve (AUC) Method: Instead of absorbance at a single point, the area under the curve for a selected wavelength range is used for calculation, which can offer better accuracy for overlapping spectra [20].
Advanced Spectrophotometric Techniques and Practical Applications
Direct Spectrophotometric Assay for Single-Component Formulations
Within the framework of method development for paracetamol (PAR) tablet analysis, UV-Visible spectrophotometry remains a cornerstone technique in pharmaceutical quality control. Its enduring popularity stems from its inherent simplicity, cost-effectiveness, and robustness for the analysis of single-component formulations [10]. This Application Note provides a detailed protocol for the development and validation of a direct UV-Visible spectrophotometric method for the assay of paracetamol in its tablet dosage form, adhering to fundamental spectrophotometric principles and regulatory guidelines [18].
The technique is governed by the Beer-Lambert law, which establishes a linear relationship between the absorbance (A) of a solution and the concentration (c) of the analyte. The law is mathematically expressed as A = a b c, where 'a' is the absorptivity, and 'b' is the path length of the radiation through the sample [18]. For routine quantitative analysis, the selection of the wavelength of maximum absorption (λmax) is critical, as it ensures maximum sensitivity and minimizes errors due to slight instrumental wavelength shifts [18].
Principle and Theory
In a direct spectrophotometric assay for a single-component formulation, the active pharmaceutical ingredient (API) is dissolved in a suitable solvent and its absorbance is measured at a predetermined wavelength of maximum absorption [18]. The fundamental requirement is that the API's spectrum is sufficiently resolved from the spectra of excipients and other formulation components, ensuring no significant interference at the analytical wavelength.
The quantification can be performed using one of three principal procedures [18]:
- Use of Standard Absorptivity Value: The concentration is calculated directly using a known standard absorptivity value (A1%, 1 cm).
- Calibration Graph: The absorbance of a series of standard solutions is measured, and a calibration graph is constructed. The concentration of the analyte in the sample is determined by interpolating its absorbance from this graph.
- Single-Point Standardization: The concentration of the analyte is calculated by directly comparing the absorbance of the sample solution with that of a standard solution of known concentration, using the formula: Ctest = (Atest × Cstd) / Astd [18].
For paracetamol, a well-defined λmax in the UV region allows for straightforward and accurate quantification using these principles.
Materials and Experimental Requirements
The Scientist's Toolkit: Research Reagent Solutions
The following table details the essential materials and reagents required for the successful execution of this analytical method.
Table 1: Essential Research Reagents and Materials
| Item | Specification / Function |
|---|---|
| Active Pharmaceutical Ingredient (API) | Paracetamol reference standard of known purity, for preparation of calibration standards. |
| Tablet Formulation | Paracetamol tablet formulation, for sample preparation. |
| Solvent | UV-grade Methanol, Water, or other transparent solvent for dissolving the analyte. |
| Volumetric Flasks | Class A volumetric flasks of various capacities (e.g., 10 mL, 100 mL) for precise solution preparation. |
| Micropipettes | For accurate and precise transfer of liquid volumes. |
| UV-Vis Spectrophotometer | Instrument capable of measuring absorbance in the 200-400 nm range. |
| Quartz Cuvettes | High-transparency quartz cells with a standard 1 cm path length. |
| Analytical Balance | For accurate weighing of standard and sample powders. |
| Sonicator / Bath | To aid in the dissolution and extraction of the API from the tablet matrix. |
Instrumental Conditions
- Analytical Technique: UV-Visible Spectrophotometry [18]
- Wavelength (λmax): Determined experimentally for the standard solution (typically ~249 nm for Paracetamol in methanol, though this must be verified) [22]
- Path Length: 1 cm
- Solvent: Methanol [22] [18]
- Baseline Correction: A baseline correction wavelength should be empirically determined. A general recommendation is 340 nm for UV-only wavelength ranges to account for instrument noise and light-scattering particulates [23].
Experimental Protocol
The following diagram illustrates the logical workflow for the direct spectrophotometric assay of a single-component formulation.
Step-by-Step Procedure
Step 1: Preparation of Stock Standard Solution
Accurately weigh and transfer 10 mg of paracetamol reference standard into a 100 mL volumetric flask. Add approximately 60 mL of methanol, shake manually or sonicate to dissolve the powder completely, and then dilute to volume with methanol to obtain a primary stock solution with a concentration of 100 µg/mL [22].
Step 2: Spectral Scanning and Determination of λmax
Dilute an aliquot of the primary stock solution appropriately with methanol to obtain a working standard solution (e.g., 10 µg/mL). Scan this solution over the UV range (e.g., 200-400 nm) against a methanol blank. Identify the wavelength of maximum absorption (λmax), which will be used for all subsequent quantitative measurements [22] [18].
Step 3: Construction of Calibration Curve
Prepare a series of standard solutions by transferring accurate aliquots (e.g., 0.5, 1.0, 1.5, 2.0, 2.5 mL) of the primary stock solution into a set of 10 mL volumetric flasks. Dilute each to the mark with methanol to create concentrations spanning a suitable range (e.g., 5–25 µg/mL) [22]. Measure the absorbance of each solution at the predetermined λmax against a solvent blank. Plot a graph of absorbance versus concentration and determine the regression equation.
Step 4: Sample Preparation (Tablet Formulation)
Accurately weigh and finely powder not less than 20 tablets. Transfer a portion of the powder, equivalent to about 5 mg of paracetamol, into a 100 mL volumetric flask. Add about 60 mL of methanol, shake or sonicate for 20-30 minutes to ensure complete extraction of the API [22] [15]. Dilute to volume with methanol, mix well, and filter (e.g., using Whatmann filter paper no. 41). Further dilute the filtrate appropriately with methanol to yield a final concentration within the linear range of the calibration curve.
Step 5: Absorbance Measurement and Calculation
Measure the absorbance of the final prepared sample solution at the analytical wavelength. Calculate the concentration of paracetamol in the sample solution using the regression equation from the calibration curve. Alternatively, use a single-point standardization method with a concurrently analyzed standard [18]. The amount of paracetamol per tablet can then be back-calculated, considering all dilution factors.
Method Validation
The developed spectrophotometric method must be validated as per ICH guidelines to ensure it is suitable for its intended purpose [22] [18]. Key validation parameters and their typical acceptance criteria, as demonstrated in published methods for paracetamol, are summarized below.
Table 2: Validation Parameters and Typical Results for Paracetamol Assay
| Validation Parameter | Protocol Description | Typical Results for Paracetamol |
|---|---|---|
| Linearity & Range | Prepare and analyze standard solutions at multiple concentrations (e.g., 5 levels). | 5–25 µg/mL [22]. Correlation coefficient (r) of at least 0.9991 [15]. |
| Accuracy (Recovery) | Perform recovery study by spiking pre-analyzed sample with standard at three levels (e.g., 80%, 100%, 120%). | Recovery results close to 100% [22]. |
| Precision | 1. Repeatability: Analyze multiple preparations (n=5) of the same sample.2. Intermediate Precision: Perform analysis on different days or by different analysts. | Relative Standard Deviation (RSD) < 2% for both intra-day and inter-day analysis [22]. |
| Specificity | Demonstrate that the absorbance measured in the sample is due to the API alone, with no interference from excipients or impurities. | No interference from other excipients observed in the analysis of marketed tablet formulations [22]. |
| LOD (Limit of Detection) | LOD = 3.3 × N/S, where N is the standard deviation of the response and S is the slope of the calibration curve. | Can be as low as 0.10 µg/mL [22]. |
| LOQ (Limit of Quantification) | LOQ = 10 × N/S, where N is the standard deviation of the response and S is the slope of the calibration curve. | Can be as low as 0.32 µg/mL [22]. |
Troubleshooting and Best Practices
- Baseline Offset: An incorrect baseline can lead to significant errors in concentration calculations. Always apply a baseline correction at a wavelength where neither the sample nor the solvent absorbs, such as 340 nm [23].
- Adherence to Beer-Lambert Law: Ensure that the absorbance readings for both standard and sample solutions fall within the linear range of the calibration curve, ideally below an absorbance of 2.0 for optimal accuracy [18].
- Solvent Compatibility: The solvent used must be transparent at the analytical wavelength and should not react with the analyte. Methanol has been successfully used as a solvent for paracetamol analysis [22] [18].
- Complete Extraction: Ensure sufficient sonication time during sample preparation to guarantee complete extraction of the active ingredient from the tablet matrix [15].
The simultaneous quantification of active pharmaceutical ingredients (APIs) in fixed-dose combination products, such as those containing paracetamol (acetaminophen) and ibuprofen, presents a significant challenge in pharmaceutical analysis due to extensive spectral overlap in the UV region [7] [8]. Traditional ultraviolet-visible (UV-Vis) spectrophotometry cannot resolve these overlapping absorption bands, historically necessitating separation-based techniques like high-performance liquid chromatography (HPLC) [10]. However, mathematical signal transformation methods now enable accurate multicomponent analysis without prior physical separation, offering cost-effective, rapid, and eco-friendly alternatives for quality control in drug development and manufacturing [7] [8] [24]. This document details the application of derivative and wavelet transform techniques for the simultaneous determination of paracetamol and ibuprofen, framed within method development for UV-Vis spectrophotometry research.
Signal Transformation Fundamentals
Derivative Transform Approach
Derivative spectrophotometry transforms zero-order absorption spectra into first- or higher-order derivative spectra, which enhances spectral resolution by converting shoulder peaks into distinct, measurable signals [7] [25]. The Savitzky-Golay algorithm is the most common method for differentiation and simultaneous smoothing of spectral data. This algorithm applies a polynomial fit across a moving window of 2n+1 measurement points on the absorbance spectrum [7]. The derivative at the window center is calculated from the polynomial coefficients. The first-order derivative spectrum is obtained by measuring the amplitude at zero-crossing points, where one component's derivative signal is zero, allowing for the selective quantification of the other component [25].
Wavelet Transform Approach
Wavelet transform (WT) is a powerful signal processing tool that decomposes a complex signal, such as a severely overlapping UV spectrum, into simpler components across different frequency (scale) and time (wavelength) domains [24] [26]. This dual localization capability makes it superior to Fourier transforms for analyzing non-stationary signals like UV absorption spectra [26]. The continuous wavelet transform (CWT) is particularly useful for detailed resolution of overlapping spectral bands and is defined mathematically by:
[Wf(a,b) = \int{-\infty}^{\infty} f(t) \psi_{a,b}(t) dt]
where ( \psi_{a,b}(t) ) represents a scaled and translated version of the mother wavelet function [7] [24]. The discrete wavelet transform (DWT) and fractional wavelet transform (FWT) are also employed for specific applications involving digitized signals and optimized spectral recovery [7]. Unlike derivative methods, WT can effectively manage high noise levels and baseline drifts without significant signal deterioration [24] [26].
Application Notes: Paracetamol and Ibuprofen Analysis
Quantitative Analytical Data
The following table summarizes validated parameters for the simultaneous determination of paracetamol and ibuprofen using signal transformation methods.
Table 1: Quantitative Method Parameters for Paracetamol and Ibuprofen Analysis
| Parameter | Derivative Method | Wavelet Transform Method | HPLC (Reference) |
|---|---|---|---|
| Linear Range (Paracetamol) | 20–40 mg/L [8] | 20–40 mg/L [8] | Not Specified |
| Linear Range (Ibuprofen) | 12–32 mg/L [7] | 12–32 mg/L [7] | Not Specified |
| Wavelength (Paracetamol) | Measured at IBU's zero-crossing point [25] | Transformed signal amplitude [7] | 225 nm [8] |
| Wavelength (Ibuprofen) | Measured at PAR's zero-crossing point [25] | Transformed signal amplitude [7] | 225 nm [8] |
| Accuracy (% Recovery) | 99.1–101.5% [8] | Comparable to HPLC [7] | 100% (Reference) |
| Precision (% RSD) | < 2% [8] | Comparable to HPLC [7] | Not Specified |
| Key Advantage | Simplicity, wide availability of algorithms [25] | Superior resolution of severely overlapping spectra [7] [24] | Official pharmacopeial method [8] |
Experimental Protocol: Simultaneous Determination in Tablets
Equipment and Software
- Spectrophotometer: Double-beam UV-Vis spectrophotometer (e.g., UNICAM UV 300) with 1 cm quartz cells [7] [8].
- Software: Spectral data acquisition software (e.g., VISION32) and computational tools for signal processing (e.g., MATLAB with Wavelet Toolbox) [7] [8].
Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Reagent/Material | Specification | Primary Function |
|---|---|---|
| Paracetamol Reference Standard | High Purity (e.g., 99.5%) [7] | Primary calibration standard for accurate quantification |
| Ibuprofen Reference Standard | High Purity (e.g., 100.0%) [7] | Primary calibration standard for accurate quantification |
| Phosphate Buffer (pH 7.2) | 0.01 M - 0.2 M [7] [8] | Spectrophotometric solvent; suitable for dissolution tests |
| Methanol / Ethanol | Analytical Grade [10] | Alternative solvent or mobile phase component for HPLC |
| NaOH Solution | 0.1 N [27] | Alternative solvent for simple, economical methods |
| Membrane Filter | 0.45 μm porosity [7] [8] | Clarification of sample solutions before analysis |
Sample Preparation Procedure
- Stock Solutions: Accurately weigh and dissolve paracetamol and ibuprofen reference standards in phosphate buffer pH 7.2 to prepare individual stock solutions of 500 mg/L [7].
- Calibration Standards: From the stock solutions, prepare a series of mixed standard solutions in 25 mL or 100 mL volumetric flasks to span the linear concentration ranges of 20–40 mg/L for paracetamol and 12–32 mg/L for ibuprofen [7] [8].
- Tablet Sample Solution:
- Finely powder twenty tablets [7] [8].
- Accurately weigh a portion equivalent to one tablet and transfer to a 100 mL volumetric flask.
- Add approximately 50 mL of phosphate buffer pH 7.2 and sonicate for 20 minutes to dissolve the APIs.
- Dilute to volume with the same solvent and mix well.
- Perform an appropriate dilution to obtain a test solution with nominal concentrations of approximately 32.5 mg/L paracetamol and 20 mg/L ibuprofen [7]. Filter through a 0.45 μm membrane before analysis.
Spectral Acquisition and Data Transformation
- Zero-Order Spectra: Record the absorption spectra of all calibration standards and the sample solution against a blank (phosphate buffer pH 7.2) over the wavelength range of 200–300 nm with a data interval of 0.1–0.2 nm [7] [8].
- Derivative Method:
- Process the saved spectra using the Savitzky-Golay algorithm (e.g., 3rd-order polynomial, 125 convolution coefficients) to obtain the first-derivative spectra [8].
- For paracetamol quantification, measure the derivative amplitude at the wavelength where ibuprofen's derivative spectrum crosses zero (its zero-crossing point).
- For ibuprofen quantification, measure the derivative amplitude at paracetamol's zero-crossing point [25].
- Wavelet Transform Method:
- Export the zero-order spectral data (wavelength vs. absorbance) to MATLAB.
- Apply a continuous wavelet transform (CWT) using a suitable mother wavelet (e.g.,
sym6,haar,coif1,mexh) and optimize the scale parameter for highest spectral recovery [7] [24]. - Construct calibration graphs by measuring the amplitudes of the transformed signals for paracetamol and ibuprofen at specified wavelengths and use these to determine the concentrations in the sample solution [7].
Workflow Visualization
The following diagram illustrates the logical workflow for the simultaneous analysis of paracetamol and ibuprofen in tablets using signal transformation methods.
Derivative and wavelet transform methods provide robust, accurate, and precise alternatives to HPLC for the routine analysis and quality control of combined paracetamol and ibuprofen dosage forms [7] [8]. The protocols outlined herein enable researchers and drug development professionals to resolve severely overlapping UV spectra efficiently. The wavelet transform approach, in particular, offers enhanced signal processing capabilities that effectively manage spectral noise and complexity, ensuring reliable results without the need for costly and time-consuming separation procedures [24] [26]. These methods adhere to the principles of green analytical chemistry by minimizing solvent use and waste generation [25].
Chemometric Modeling with PCR and PLS for Multicomponent Analysis
Ultraviolet-Visible (UV-Vis) spectrophotometry is a fundamental technique in pharmaceutical analysis, prized for its simplicity, cost-effectiveness, and rapid results. However, its application to complex multi-component formulations is often hindered by significant spectral overlap, which makes quantifying individual analytes with ordinary spectrophotometry challenging. Chemometric modeling has emerged as a powerful solution, enabling the resolution of such complex mixtures through mathematical and statistical techniques. Among these, Principal Component Regression (PCR) and Partial Least Squares (PLS) regression represent two of the most robust and widely adopted multivariate calibration methods.
Framed within broader thesis research on method development for paracetamol tablet analysis, this document provides detailed application notes and protocols for implementing PCR and PLS. These techniques facilitate the simultaneous quantification of active pharmaceutical ingredients (APIs) in multi-component tablets without prior physical separation, streamlining the analytical process for drug development and quality control.
Theoretical Background
Principal Component Regression (PCR)
PCR is a two-step multivariate calibration method. The first step involves Principal Component Analysis (PCA), which decomposes the spectral data matrix (X) into a set of orthogonal, latent variables called Principal Components (PCs). These PCs are linear combinations of the original variables (wavelengths) and are calculated to capture the maximum possible variance in the spectral data itself, without considering the concentration data. The second step is a regression step, where the selected PCs are used as independent variables to build a model predicting the analyte concentrations (Y). By discarding minor PCs associated with noise, PCR can often yield more stable and robust models than classical univariate regression [28] [29].
Partial Least Squares (PLS) Regression
Unlike PCR, PLS is a one-step algorithm that simultaneously decomposes both the spectral matrix (X) and the concentration matrix (Y). PLS seeks to find latent variables (called PLS components) that not only explain the variance in the spectral data but also have maximum covariance with the concentration data of the analyte(s) of interest. This direct consideration of the response variable during dimension reduction often allows PLS to model the relationship between spectra and concentrations with fewer components than PCR, though this does not necessarily translate to superior predictive performance in all cases [30] [29]. PLS can be implemented for a single analyte (PLS1) or multiple analytes simultaneously (PLS2).
Relationship Between PCR and PLS
The choice between PCR and PLS has been a subject of extensive comparative studies in chemometrics. Theoretical and practical investigations have shown that while PLS often requires fewer latent variables to achieve an optimal model, there is generally no significant difference in the predictive ability between the two methods when the optimal number of components is used for PCR [30] [29]. The equivalence of PCR and PLS has been demonstrated within the sufficient dimension reduction framework, indicating no inherent theoretical advantage of one over the other in terms of prediction performance [29]. The selection often depends on the specific data set and the nature of the spectral interferences.
The following diagram illustrates the logical relationship and comparative workflow between PCR and PLS modeling:
Experimental Protocols
Reagent Solutions and Instrumentation
The success of chemometric methods relies on the preparation of accurate standard solutions and the use of properly calibrated instrumentation. The following table lists essential materials and their functions.
Table 1: Key Research Reagent Solutions and Instrumentation
| Item | Specification | Function/Role in Analysis |
|---|---|---|
| Paracetamol Standard | High Purity (e.g., 99.99%) [11] | Primary reference standard for calibration and validation. |
| Methanol | Analytical Reagent Grade [31] [32] | Solvent for preparing stock and working standard solutions. |
| Phosphate Buffer (pH 6.8) | Analytical Reagent Grade [11] | Aqueous solvent component for eco-friendly dilution. |
| UV-Vis Spectrophotometer | Double-beam, 1 nm bandwidth [22] [11] | Measures absorbance across the selected wavelength range. |
| Quartz Cuvettes | 10 mm path length, matched pair [22] [11] | Holds sample solutions for spectrophotometric measurement. |
| Analytical Balance | Precision 0.1 mg [22] | Accurately weighs standard compounds and tablet powder. |
Protocol 1: Calibration Set Design and Spectral Acquisition
This protocol outlines the creation of a robust calibration set, which is the foundation of a reliable chemometric model.
- Stock Solution Preparation: Accurately weigh 100 mg of each pure API (e.g., paracetamol, chlorpheniramine maleate, caffeine, ascorbic acid). Transfer each to a separate 100 mL volumetric flask, dissolve in and dilute to volume with methanol to obtain 1000 µg/mL stock solutions [32].
- Working Solution Preparation: Pipette 10 mL from each stock solution into separate 100 mL volumetric flasks and dilute to volume with methanol to obtain 100 µg/mL working standard solutions [32].
- Calibration Set Design: Prepare a series of mixtures containing varying concentrations of all analytes. A five-level, four-factor calibration design is effective for a quaternary mixture [32]. For a ternary mixture of Paracetamol (PAR), Sodium Ascorbate (ASC), and Chlorpheniramine (CHL) with a high ratio (150:140:1), an 18-mixture set with concentrations in the ranges of 5.05–30.3 mg/L for PAR, 2.04–30.60 mg/mL for ASC, and 0.20–5.05 mg/mL for CHL has been successfully applied [28].
- Spectral Acquisition: Scan the absorbance of each calibration mixture across an appropriate wavelength range (e.g., 200–350 nm [28] or 220–300 nm [32]) using a 1 nm interval. A finer data interval (e.g., 0.5 points/nm) can improve the quantification of minor components [28]. Export the spectral data (wavelengths and corresponding absorbance values) for chemometric processing.
Protocol 2: Data Preprocessing and Wavelength Selection
Raw spectral data often requires preprocessing to enhance the signal-to-noise ratio and improve model performance.
- Data Formatting: Compile the spectral data into a single matrix X (samples × wavelengths) and the known concentrations into a matrix Y (samples × analytes).
- Mean Centering: Subtract the average spectrum of the calibration set from each individual spectrum. This is a common preprocessing step that enhances the stability and interpretability of PCR and PLS models [32].
- Wavelength Selection (Optional but Recommended): Instead of using the entire spectrum, select informative wavelength regions to avoid uninformative or highly noisy regions. Techniques like Moving Window (MW) or Changeable Size Moving Window (CSMW) strategy can be employed. This reduces model complexity, removes collinear variables, and often leads to more precise predictions [30] [28].
Protocol 3: Model Development, Validation, and Application
This protocol covers the core steps of building, validating, and deploying the PCR and PLS models.
- Software and Computation: Import the preprocessed data matrices (X, Y) into chemometric software (e.g., MATLAB with PLS Toolbox, The Unscrambler X, or similar) [28] [32].
- Model Training:
- Split the data into a calibration/training set and a validation/test set.
- For PCR, perform PCA on the calibration spectral data and retain the significant principal components that capture spectral variance while excluding noise-related components.
- For PLS, specify the algorithm (PLS1 for single analyte or PLS2 for multiple analytes). The software will perform the simultaneous decomposition.
- Optimal Component Selection: Use cross-validation (e.g., leave-one-out cross-validation) on the calibration set to determine the optimal number of latent variables (LVs) for PLS or PCs for PCR. The optimal number is the one that minimizes the Root Mean Square Error of Cross-Validation (RMSECV) [28] [32].
- Model Validation: Use the external validation set, which was not used in model building, to assess the model's predictive power. Calculate the Root Mean Square Error of Prediction (RMSEP) and the Relative Error (RE%) to quantify accuracy [28].
- Application to Pharmaceutical Formulation:
- Prepare a sample solution from powdered tablets using the same solvent and dilution procedure as the standards [11].
- Record the spectrum of the sample solution.
- Use the developed PCR or PLS model to predict the concentration of each API in the sample.
The entire experimental workflow, from sample preparation to result interpretation, is summarized below:
Data Presentation and Analysis
Performance Metrics and Comparative Analysis
The following table summarizes typical validation results for chemometric models applied to multi-component pharmaceutical mixtures, including paracetamol-based formulations.
Table 2: Comparative Performance of Chemometric Models in Multicomponent Analysis
| Analytical Challenge / Mixture | Chemometric Method | Wavelength Range (nm) | Linear Range (μg/mL) | RMSEP / RMSECV | Reference |
|---|---|---|---|---|---|
| Paracetamol, CPM, Caffeine, Ascorbic Acid (Quaternary Mixture) | PLS1 | 220–300 | PARA: 4–20 | Low RMSECV values | [32] |
| PCR | 220–300 | PARA: 4–20 | reported, with PLS1 | [32] | |
| MCR-ALS | 220–300 | PARA: 4–20 | often showing slightly better accuracy. | [32] | |
| ANN | 220–300 | PARA: 4–20 | [32] | ||
| Paracetamol, Sodium Ascorbate, Chlorpheniramine (150:140:1 Ratio) | PLS1 (0.5 pt/nm) | 200–320 | CHL: 0.20–5.05 | Significantly improved accuracy for minor component (CHL) | [28] |
| Diphenylamine, Aniline, Phenol (Degradation Products) | PLS (with MW selection) | Selected Windows | 0.1–6.0 | Improved results with wavelength selection | [30] |
| PCR (with MW selection) | Selected Windows | 0.1–6.0 | Improved results with wavelength selection | [30] | |
| Paracetamol, Eperisone HCl (Binary Mixture) | Q-Absorbance Ratio | 249 & 260 (Iso-point) | PARA: 2–10 | % Recovery: 99.89% (PARA) | [22] |
Application to Tablet Formulation
The developed PCR and PLS models have been successfully applied to commercial tablet formulations. For instance, in the analysis of Grippostad C capsules, all four models (PCR, PLS, MCR-ALS, and ANN) provided satisfactory results with no significant difference in accuracy compared to official methods, demonstrating their suitability for routine quality control [32]. Another study on a paracetamol tablet (Paracip 500) using a univariate UV method reported a percent purity of 99.09%, with recovery rates at 80%, 100%, and 120% levels ranging from 100.00% to 102.10%, confirming the accuracy of spectrophotometric methods for paracetamol assay [11].
This application note has detailed the theoretical foundation and practical protocols for employing PCR and PLS regression in the spectrophotometric analysis of complex multi-component pharmaceutical formulations. Both methods have proven to be powerful, green, and viable alternatives to chromatographic techniques for the simultaneous quantification of APIs, such as paracetamol in combination with other drugs, without the need for prior separation.
The comparative studies indicate that while PLS may achieve optimal performance with fewer latent variables, both PCR and PLS offer comparable and excellent predictive accuracy when properly optimized. Key steps for success include a well-designed calibration set, appropriate wavelength selection, and rigorous validation. Integration of these chemometric models into pharmaceutical quality control laboratories can significantly enhance efficiency, reduce solvent consumption, and provide a robust framework for standard analysis.
Simultaneous Equation and Q-Absorbance Ratio Methods for Combination Products
The pharmaceutical industry increasingly relies on fixed-dose combination (FDC) products to achieve enhanced therapeutic effects through synergistic actions. Ibuprofen (IBU) and paracetamol (PAR) represents one such combination, gaining prominence in pain management due to its complementary mechanisms of action and favorable safety profile [10]. Ensuring the quality, safety, and efficacy of these combination products necessitates robust analytical methods for their simultaneous quantification in bulk and formulated dosages.
UV-Visible spectrophotometry remains a foundational technique in pharmaceutical analysis due to its simplicity, cost-effectiveness, and rapid implementation [18]. However, the simultaneous analysis of multiple active ingredients presents a significant challenge when their absorption spectra overlap. This application note, situated within a broader thesis on method development for paracetamol tablet analysis, details two well-established spectrophotometric techniques—the Simultaneous Equation (Vierodt's) method and the Q-Absorbance Ratio method. These methods effectively resolve overlapping spectra, enabling the precise and accurate quantification of individual components in a mixture without prior physical separation [33] [34]. Their utility is particularly valuable in routine quality control environments where high-throughput analysis is essential.
Theoretical Foundations
The Beer-Lambert Law
The quantitative basis of UV-Visible spectrophotometry is the Beer-Lambert law, which states that the absorbance (A) of a solution is directly proportional to the concentration (c) of the absorbing species and the path length (b) of the radiation through the sample [18]. Mathematically, this is expressed as: A = a b c where 'a' is the absorptivity coefficient. This direct relationship is fundamental to all quantitative spectrophotometric analysis.
- Simultaneous Equation Method: This approach is applicable when the absorption spectra of two components, X and Y, overlap, but each shows a distinct absorption maximum where the other exhibits significant absorption [34]. The concentration of each component is determined by solving a pair of simultaneous equations based on absorbance measurements at two different wavelengths and the respective absorptivity values.
- Q-Absorbance Ratio Method: This method requires the identification of an iso-absorptive point—a wavelength where the absorptivities of the two components are equal—in addition to the wavelength of maximum absorption of one component [33] [34]. The "Q" value is the ratio of absorbances at these two wavelengths and is used to calculate the concentrations.
Research Reagent Solutions
The following table catalogues essential materials and reagents required for the successful implementation of these analytical methods.
Table 1: Essential Research Reagents and Materials
| Reagent/Material | Specification | Primary Function |
|---|---|---|
| Paracetamol Reference Standard | Pharmaceutical grade (>99% purity) | Primary standard for calibration and method validation [7]. |
| Ibuprofen Reference Standard | Pharmaceutical grade (>99% purity) | Primary standard for calibration and method validation [7]. |
| Ethanol (Absolute) | HPLC/UV-Vis Grade | Primary solvent; ensures drug solubility and minimizes UV interference [13]. |
| Sodium Hydroxide (NaOH) | Analytical Grade | Enhances solubility of acidic drugs (e.g., ibuprofen) and can influence λmax [13]. |
| Phosphate Buffer (pH 7.2) | Analytical Grade | Provides a stable solvent medium for drugs stable at neutral pH [7]. |
| Methanol | HPLC Grade | Alternative solvent for drug dissolution and dilution [10]. |
| Volumetric Flasks | Class A, 10-100 mL | Precise preparation and dilution of standard and sample solutions. |
| Quartz Cuvettes | 1 cm path length | Holds sample solution for absorbance measurement in UV range. |
Application Notes & Protocols
Protocol 1: Simultaneous Equation Method for Paracetamol and Ibuprofen
Principle
This method relies on measuring the absorbance of a sample solution at two wavelengths: the λmax of paracetamol and the λmax of ibuprofen. The concentrations are calculated using a pair of simultaneous equations that incorporate the absorptivity values of each drug at both selected wavelengths [34].
Experimental Procedure
- Solvent System Preparation: Prepare a mixture of ethanol and 0.1 M sodium hydroxide in a 3:1 ratio (75 mL ethanol + 25 mL 0.1 M NaOH) [13].
- Standard Stock Solutions:
- Accurately weigh 25 mg of paracetamol and transfer to a 100 mL volumetric flask. Dissolve and make up to volume with the ethanol-NaOH solvent to obtain a 250 μg/mL stock solution.
- Repeat the process for ibuprofen to obtain a 250 μg/mL stock solution [13].
- Selection of Wavelengths: Scan the individual drug solutions in the range of 200-400 nm. Determine the absorbance maxima for each drug. For the paracetamol-ibuprofen combination, these are typically found at ~243 nm (λmax of PAR) and ~221 nm (λmax of IBU) [13].
- Calibration and Determination of Absorptivity:
- Dilute the stock solutions to prepare a series of standard solutions (e.g., 5-30 μg/mL for both drugs).
- Measure the absorbance of each paracetamol standard at both 243 nm (A₁) and 221 nm (A₂).
- Similarly, measure the absorbance of each ibuprofen standard at both 243 nm (A₃) and 221 nm (A₄).
- Calculate the mean absorptivity (A1%, 1cm) for each drug at both wavelengths. The absorptivity (a) is given by a = A / (c * b), where c is concentration in g/100mL.
- Sample Solution Preparation:
- Finely powder and accurately weigh tablet powder equivalent to one tablet.
- Transfer to a volumetric flask, add about 50 mL of solvent, sonicate for 20 minutes, and dilute to volume.
- Filter and further dilute to obtain a sample solution within the linear range of the calibration curve [7].
- Calculation:
- Measure the absorbance of the sample solution (A_sample) at 243 nm (λ₁) and 221 nm (λ₂).
- Use the following simultaneous equations to calculate the concentrations CPAR and CIBU (in μg/mL) in the sample solution:
- Aatλ₁ = aPARλ₁ * CPAR + aIBUλ₁ * CIBU
- Aatλ₂ = aPARλ₂ * CPAR + aIBUλ₂ * CIBU
Analytical Performance Data
The following table summarizes typical validation parameters for this method.
Table 2: Analytical Performance of the Simultaneous Equation Method for PAR and IBU
| Parameter | Paracetamol | Ibuprofen | Reference |
|---|---|---|---|
| Linear Range (μg/mL) | 1 – 15 / 5 – 30 | 2 – 20 / 5 – 30 | [10] |
| Wavelengths Used (nm) | 240 / 256 | 220 / 222.4 | [10] |
| Limit of Detection (LOD) (μg/mL) | 0.214 | 0.600 | [10] |
| Accuracy (% Recovery) | 100.02 ± 0.47* | 99.87 ± 0.53* | [34] |
| Precision (% RSD) | < 2% | < 2% | [13] |
| Remarks | *Reported for a different drug combination (Paracetamol & Zaltoprofen), demonstrating typical method performance. |
Protocol 2: Q-Absorbance Ratio Method for Paracetamol and Ibuprofen
Principle
This method involves measuring the absorbance of a sample solution at two wavelengths: the iso-absorptive point of the two drugs (where their absorptivities are equal) and the λmax of one component [33]. The ratio of these absorbances (the Q-value) is used to determine the concentration of each component in the mixture.
Experimental Procedure
- Solvent and Stock Solutions: Prepare as described in Protocol 4.1.2.
- Identification of Iso-absorptive Point:
- Prepare standard solutions of paracetamol and ibuprofen at the same concentration.
- Scan their absorbance spectra and overlay them. The point where the two spectra cross is the iso-absorptive point (λiso). For some PAR-IBU methods, this has been reported at 226.4 nm [10].
- Selection of λmax: Identify the λmax of one component, for example, ibuprofen at 222.4 nm (λIBU) [10].
- Calibration and Determination of Absorptivity:
- Prepare calibration curves for both pure drugs at both λiso and λIBU.
- Confirm that the absorptivities (A1%, 1cm) for both drugs are identical at λiso (aiso).
- Determine the absorptivity of ibuprofen at its λmax (aIBUλIBU) and at the iso-absorptive point (aIBUλiso). Note that aIBUλiso = aiso.
- Similarly, determine the absorptivity of paracetamol at the iso-point (aPARλiso = aiso) and at λIBU (aPAR_λIBU).
- Sample Analysis and Calculation:
- Measure the absorbance of the sample solution at the iso-absorptive point (Aiso) and at λIBU (AIBU).
- Calculate the Q-value: QM = AIBU / Aiso
- Calculate the concentration of ibuprofen (CIBU) and paracetamol (CPAR) in the sample using the following equations, where aIBUλIBU and aPARλIBU are the absorptivities of the pure drugs at λIBU, and aiso is the absorptivity at the iso-point:
- CIBU = (QM - QIBU) * (Aiso) / ( (QPAR - QIBU) * aiso )
- CPAR = (QPAR - QM) * (Aiso) / ( (QPAR - QIBU) * aiso )
- (Where QIBU = aIBUλIBU / aiso and QPAR = aPARλIBU / aiso)
Analytical Performance Data
The following table summarizes key performance metrics for the Q-Absorbance Ratio method.
Table 3: Analytical Performance of the Q-Absorbance Ratio Method for PAR and IBU
| Parameter | Details | Reference |
|---|---|---|
| Wavelengths Used | Iso-absorptive point: 226.4 nm; λmax (IBU): 256 nm | [10] |
| Linear Range (μg/mL) | 5–30 for both PAR and IBU | [10] |
| Accuracy (% Recovery) | 99.82 ± 0.48 (PAR), 99.84 ± 0.51 (IBU) | [34] |
| Precision (% RSD) | < 2% | [13] |
| Key Advantage | Simplifies calculation; less sensitive to minor errors in wavelength selection compared to the simultaneous equation method. | [33] |
| Remarks | *Reported for a different drug combination (Paracetamol & Zaltoprofen), demonstrating typical method performance. |
Method Validation and Comparative Analysis
Both the Simultaneous Equation and Q-Absorbance Ratio methods must be validated according to ICH guidelines to ensure reliability, accuracy, and precision for their intended use in pharmaceutical analysis [13] [18]. Key validation parameters include linearity, precision, accuracy, limit of detection (LOD), and limit of quantification (LOQ).
Table 4: Summary of Validation Parameters for UV-Spectrophotometric Methods
| Validation Parameter | Protocol & Acceptance Criteria |
|---|---|
| Linearity | Prepare standard solutions at 5-6 concentration levels across the specified range. The correlation coefficient (r²) should be >0.995 [13]. |
| Precision | Assessed by repeatability (intra-day) and intermediate precision (inter-day). Express results as % Relative Standard Deviation (% RSD), with <2% being acceptable [13]. |
| Accuracy (Recovery) | Perform by spiking a pre-analyzed sample with known quantities of standard drugs at three different levels (e.g., 80%, 100%, 120%). The mean recovery should be 98-102% [13] [34]. |
| LOD & LOQ | Calculate based on the standard deviation of the response and the slope of the calibration curve (LOD = 3.3σ/S; LOQ = 10σ/S). For PAR and IBU, LOD values can be as low as 0.198 μg/mL and 0.8 μg/mL, respectively [13]. |
| Specificity | Demonstrated by the absence of interference from excipients at the selected wavelengths, confirmed by analyzing placebo solutions [13]. |
Advanced Techniques and Future Perspectives
While the classical methods described are robust for routine analysis, advanced mathematical techniques are employed for more complex scenarios. The application of derivative spectroscopy and wavelet transforms to the original or ratio spectra can further enhance resolution and accuracy [7]. These advanced signal processing techniques help to correct baseline drift, suppress noise, and resolve severely overlapping peaks, thereby improving the sensitivity and specificity of UV spectrophotometric methods for combination products [7].
Practical Application to Tablet Formulation Analysis
Within the broader context of method development for paracetamol (acetaminophen) research, the analysis of tablet formulations presents distinct practical challenges. UV-Visible (UV-Vis) spectrophotometry remains a cornerstone technique for this purpose, prized for its cost-effectiveness, rapid analysis time, and operational simplicity, making it exceptionally suitable for routine quality control in pharmaceutical settings [8] [10]. This application note provides detailed protocols for the accurate quantification of paracetamol in both single-component and complex multi-component tablet formulations, leveraging the principles of spectrophotometric analysis.
The fundamental advantage of UV-Vis spectrophotometry lies in the direct relationship between analyte concentration and light absorption, as described by the Beer-Lambert law [10]. However, a significant challenge arises in fixed-dose combination (FDC) products, where the spectral profiles of active ingredients frequently overlap [8] [10]. This document details robust methodologies to overcome this hurdle, ensuring precise and reliable determination of paracetamol.
Research Reagent Solutions and Essential Materials
The following table catalogs the key reagents, materials, and instruments required to execute the analytical protocols described herein.
Table 1: Essential Research Reagents and Materials for Tablet Analysis
| Item Name | Function/Application | Specifications/Notes |
|---|---|---|
| Paracetamol Reference Standard | Primary standard for calibration curve construction | Certified high purity (e.g., 99.88%) for accurate quantification [35]. |
| Ibuprofen Reference Standard | Primary standard for combination product analysis | Required for analysis of paracetamol-ibuprofen FDCs [8]. |
| Ethanol | Solvent for drug extraction and dissolution | HPLC grade recommended; often used in mixture with NaOH [13]. |
| Sodium Hydroxide (NaOH) | Alkaline solvent component | Enhances solubility of paracetamol and ibuprofen; used as 0.1M solution [13]. |
| Methanol | Alternative solvent for extraction and mobile phase | HPLC grade for optimal performance [35] [8]. |
| Phosphate Buffer (pH 7.2) | Spectrophotometric solvent & dissolution medium | Mimics physiological conditions; suitable for dissolution testing [8]. |
| UV-Vis Spectrophotometer | Primary analytical instrument | Equipped with 1 cm quartz cells for measurement [8] [13]. |
| Analytical Balance | Precise weighing of standards and samples | High precision (e.g., 0.01 mg) is critical [13]. |
| Ultrasonic Bath | Aid in sample dissolution and extraction | Ensures complete and efficient extraction of active ingredients from tablets [8]. |
Analytical Methodologies and Experimental Protocols
Protocol 1: Analysis of Single-Ingredient Paracetamol Tablets
This protocol is designed for the straightforward quantification of paracetamol in single-active ingredient tablets using a direct spectrophotometric method [13].
Workflow Overview:
Detailed Procedure:
- Standard Stock Solution (1000 µg/mL): Accurately weigh 25 mg of paracetamol reference standard and transfer it to a 25 mL volumetric flask. Dissolve and make up to volume with a solvent mixture of ethanol and 0.1 M sodium hydroxide (3:1 v/v) [13].
- Calibration Standards: Dilute the stock solution with distilled water or the same solvent mixture to prepare a series of standard solutions covering a concentration range of 2–10 µg/mL.
- Sample Preparation:
- Weigh and finely powder not less than 20 tablets.
- Accurately weigh a portion of the powder equivalent to about 25 mg of paracetamol and transfer to a 25 mL volumetric flask.
- Add approximately 15 mL of the ethanol-NaOH solvent, sonicate for 10–15 minutes to ensure complete extraction, and dilute to volume with the same solvent.
- Filter the solution, then further dilute a portion of the filtrate to obtain a final concentration within the linear range of the calibration curve (e.g., 5–8 µg/mL).
- Spectrophotometric Measurement:
- Using the solvent mixture as a blank, measure the absorbance of each calibration standard and the prepared sample solution at the maximum absorbance wavelength (λ_max) of paracetamol, approximately 243 nm [13].
- Calculation:
- Construct a calibration curve by plotting the absorbance of the standards against their concentrations.
- Determine the concentration of paracetamol in the sample solution from the linear regression equation of the calibration curve.
- Calculate the paracetamol content per tablet using the dilution factors and the average tablet weight.
Protocol 2: Simultaneous Analysis of Paracetamol and Ibuprofen in Fixed-Dose Combination Tablets
This protocol addresses the challenge of analyzing paracetamol in the presence of ibuprofen, where their UV spectra significantly overlap. The method employs a simultaneous equation (Vierordt's) method based on absorbance measurement at two wavelengths [10].
Workflow Overview:
Detailed Procedure:
- Selection of Wavelengths: The two wavelengths selected are typically the λmax of one drug and an iso-absorptive point or the λmax of the second drug. Common pairs are 256 nm and 222.4 nm, or 220 nm and 240 nm [10].
- Standard Solutions and Calibration:
- Prepare individual stock solutions (1000 µg/mL) of paracetamol and ibuprofen in methanol or ethanol-NaOH solvent [8] [13].
- From these, prepare a series of five or more standard solutions for each drug within their linear ranges (e.g., 5–30 µg/mL for both) [10].
- Measure the absorbance of each paracetamol standard at both selected wavelengths (λ1 and λ2) and construct a calibration curve at each wavelength. Repeat this process for ibuprofen standards.
- Determine the molar absorptivity (a) or specific absorptivity (A1%, 1cm) for paracetamol (a1,P, a2,P) and ibuprofen (a1,I, a2,I) at both wavelengths from the slopes of the respective calibration curves.
- Sample Solution Preparation:
- Weigh and powder not less than 20 tablets.
- Accurately weigh a portion equivalent to one tablet's average weight and transfer to a volumetric flask (e.g., 100 mL).
- Add solvent (methanol or ethanol-NaOH), sonicate for 15–20 minutes, and dilute to volume.
- Filter and further dilute appropriately to bring the concentration within the working range of the calibration curves.
- Measurement and Calculation:
- Measure the absorbance of the sample solution (Aλ1 and Aλ2) at the two selected wavelengths, λ1 and λ2.
- The concentrations of Paracetamol (CP) and Ibuprofen (CI) in the sample solution are calculated by solving the following simultaneous equations:
- Aλ1 = a1,PCP + a1,ICI
- Aλ2 = a2,PCP + a2,ICI
- These equations can be solved using Cramer's rule or matrix inversion to obtain the individual concentrations.
Data Presentation and Method Validation
The following table consolidates key parameters from validated methods for the simultaneous analysis of paracetamol and ibuprofen, providing a reference for method development and validation.
Table 2: Reported UV-Vis Spectrophotometric Methods for Paracetamol and Ibuprofen Analysis
| Technique Used | Wavelengths (nm) | Solvent System | Linear Range (µg/mL) | LOD/LOQ (µg/mL) | Reference |
|---|---|---|---|---|---|
| Simultaneous Equation & Q-Absorbance Ratio | 256.0 & 222.4 | Methanol | 5–30 (for both) | Not Available | [10] |
| Simultaneous Equation | 220.0 & 240.0 | Ethanol | 1–15 (PAR)2–20 (IBU) | LOD: 0.214 (PAR)LOD: 0.600 (IBU) | [10] |
| Simultaneous Equation | 257.0 & 222.0 | 0.1N NaOH | 10 (PAR)12 (IBU) * | LOD: 0.198 (PAR)LOQ: 0.538 (PAR)LOD: 0.800 (IBU)LOQ: 0.930 (IBU) | [13] |
| Signal Transforms (Derivative, Fourier, Wavelet) | 200–300 (range) | Phosphate Buffer pH 7.2 | 20–40 (PAR)12–32 (IBU)1–3.5 (Caffeine) | R² > 0.990 | [8] |
Note: The values 10 and 12 µg/mL for PAR and IBU, respectively, in [13] likely represent the upper limits of the linear range or specific concentrations tested for Beer's law adherence. PAR: Paracetamol; IBU: Ibuprofen; LOD: Limit of Detection; LOQ: Limit of Quantification.
Advanced Spectral Resolution Techniques
For formulations with severe spectral overlap, advanced chemometric techniques can be applied. These methods use mathematical algorithms to resolve the individual contributions of each drug in a mixture without physical separation [8].
- Derivative Transform: Applying first or second derivatives to the ratio spectra can minimize the effect of overlapping absorption bands.
- Fourier Transform (FT): This technique convolutes the ratio spectrum using a trigonometric Fourier series to isolate the signal of the target analyte.
- Wavelet Transform: This method uses mother wavelet functions (e.g., sym6, haar) to deconvolute the overlapping signals in the ratio spectra, offering high resolution for quantification [8].
The development and validation of these spectrophotometric methods should be performed in accordance with the ICH guidelines to ensure reliability, accuracy, precision, and specificity for their intended use in pharmaceutical analysis [35] [13].
Resolving Analytical Challenges and Method Optimization Strategies
Addressing Spectral Overlap in Multicomponent Formulations
Ultraviolet-visible (UV-Vis) spectroscopy serves as a cornerstone technique in pharmaceutical analysis due to its rapid, cost-effective, and efficient nature. A significant challenge arises, however, when quantifying individual components in multicomponent formulations whose UV spectra extensively overlap. Conventional single-wavelength (zero-order) absorbance measurement becomes impossible without prior separation. This application note details practical strategies and advanced spectrophotometric protocols for resolving such overlapping spectra, with a specific focus on formulations containing paracetamol, a widely used analgesic and antipyretic drug.
The fundamental principle enabling the simultaneous analysis of multiple components without physical separation is the additivity of absorbances. According to the Beer-Lambert Law, in a mixture containing multiple absorbing species, the total absorbance at any given wavelength is the sum of the absorbances of all individual components. This principle, expressed mathematically, forms the basis for all subsequent resolution techniques: Atotal,λ = ε1,λbc1 + ε2,λbc2 + ... + εn,λbcn [36].
Key Spectrophotometric Methods for Resolution of Spectral Overlap
The following core methodologies have been developed and validated to address the challenge of spectral overlap in pharmaceutical analysis.
Simultaneous Equation Method (Vierordt's Method)
This classical approach is applicable when the absorption spectra of the individual components are known and the total signal is the sum of the contributions from each component [36].
- Principle: The method requires measuring the absorbance of the sample mixture at multiple wavelengths (equal to or greater than the number of components, n). The analytical sensitivity (ε) of each pure component is determined at these selected wavelengths from calibration curves of standard solutions [36].
- Mathematical Foundation: A set of n linear equations is constructed and solved using matrix algebra. The concentration vector C is calculated from the absorbance vector A and the matrix of molar absorptivities Ɛ using the equation: C = (ƐTƐ)-1ƐTA [36].
- Requirements: Accurate prior knowledge of the ε values for all pure components at the selected wavelengths is essential. The method demands high wavelength reproducibility, making it ideally suited for diode-array or Fourier transform spectrometers [36].
Derivative Spectroscopy
Derivative spectroscopy transforms zero-order spectra into first- or higher-order derivative spectra, which can reveal subtle spectral features and provide points for measurement free from interference.
- Principle: This technique converts a normal UV spectrum (absorbance vs. wavelength) into its first, second, or higher derivative (dA/dλ, d²A/dλ², etc.). The derivative spectrum often shows increased resolution of overlapping bands [15].
- Application Example: For a mixture of paracetamol and meloxicam, the first-order derivative (1D) spectrum allows for the quantification of paracetamol by measuring the trough (negative peak) at 262 nm, where meloxicam shows zero crossing and thus no contribution. Conversely, meloxicam can be determined from a peak in the 1D spectrum at 342 nm, where paracetamol does not interfere [15].
Ratio Subtraction and Ratio Difference Methods
These methods leverage the manipulation of ratio spectra to isolate the signal of one component from another.
- Principle: The absorption spectrum of the mixture is divided by the spectrum of a standard solution of one of the components (the "divisor"). This generates a ratio spectrum that is subsequently manipulated [15].
- Application Example: In a paracetamol-domperidone mixture, the ratio difference method can be applied. The recorded spectra are divided by the spectrum of a standard domperidone solution. The difference between the amplitudes of the resulting ratio spectrum at two carefully selected wavelengths (e.g., 256 nm and 288 nm) is then proportional to the concentration of paracetamol [15].
Chemometric Multivariate Calibration
For highly complex mixtures, chemometric models coupled with full-spectrum data offer a powerful solution.
- Principle: Methods like Classical Least Squares (CLS) and Partial Least Squares (PLS) use the entire spectral data set rather than a few discrete wavelengths. They build a mathematical model that correlates spectral changes with component concentrations [36] [37].
- Advanced Techniques: Variable selection techniques such as Interval-PLS (i-PLS) and Genetic Algorithm-PLS (GA-PLS) can significantly enhance model performance and predictive ability by focusing on the most informative spectral regions [37].
Table 1: Summary of Key Methods for Resolving Spectral Overlap
| Method | Underlying Principle | Key Advantage | Typical Application |
|---|---|---|---|
| Simultaneous Equation [36] | Solving linear equations based on absorptivity | Conceptually simple, good for 2-3 component mixtures | Paracetamol & Lornoxicam in tablets [19] |
| Derivative Spectroscopy [15] | Using peaks/troughs in derivative spectra | Eliminates interference from turbidity or unwanted background | Paracetamol in presence of Meloxicam (measured at 262 nm trough) [15] |
| Ratio Difference [15] | Dividing spectra by a divisor and measuring amplitude differences | Effective for analyzing minor components in a mixture | Domperidone as a minor component with Paracetamol [15] |
| Multivariate Calibration [36] [37] | Full-spectrum analysis using statistical models | Handles very complex mixtures; robust against noise | Ternary antihypertensive drug mixtures [37] |
Experimental Protocols
This section provides a detailed, step-by-step protocol for the simultaneous determination of two drugs using the simultaneous equation method, applicable for quality control of tablet formulations.
Protocol: Simultaneous Determination of Paracetamol and Lornoxicam in Tablet Dosage Form
This protocol is adapted from a validated method for analyzing drugs in dissolution media [19].
Research Reagent Solutions
Table 2: Essential Materials and Reagents
| Item | Specification / Function |
|---|---|
| UV-Vis Spectrophotometer | Double-beam instrument with 1 cm matched quartz cells [19] |
| Analytical Balance | Accurate to 0.01 mg (e.g., digital analytical balance) [13] |
| Paracetamol Standard | Certified pure reference standard for calibration |
| Lornoxicam Standard | Certified pure reference standard for calibration |
| Solvent: 0.1N HCl | Serves as the dissolution medium and solvent for analysis [19] |
| N,N-Dimethylformamide (DMF) | Aids in the dissolution of Lornoxicam [19] |
| Volumetric Flasks, Pipettes | For precise preparation and dilution of standard and sample solutions |
Step-by-Step Procedure
Preparation of Standard Stock Solutions
- Paracetamol Stock Solution (100 µg/mL): Accurately weigh 100 mg of pure paracetamol and transfer it to a 100 mL volumetric flask. Dissolve and make up to volume with 0.1N HCl [19].
- Lornoxicam Stock Solution (100 µg/mL): Accurately weigh 10 mg of pure lornoxicam into a 100 mL volumetric flask. Dissolve it in approximately 20 mL of N,N-dimethylformamide first, then dilute to volume with 0.1N HCl [19].
Construction of Calibration Curves
- From the stock solutions, prepare a series of working standard solutions for each drug within the validated linearity range (e.g., 4-12 µg/mL for paracetamol and 4-16 µg/mL for lornoxicam) using 0.1N HCl as the diluent [19].
- Scan the absorbance of each standard solution across the UV range (e.g., 200-400 nm).
- Determine the absorptivity values for each drug at the selected analytical wavelengths (typically λmax of each component). For a paracetamol-lornoxicam mixture, these are 243 nm (λmax of paracetamol) and 374 nm (λmax of lornoxicam) [19]. At 374 nm, paracetamol shows no significant absorbance.
Sample Preparation (Tablet Extraction)
- Weigh and finely powder not less than 20 tablets.
- Accurately weigh a portion of the powder equivalent to the average weight of one tablet and transfer it to a 100 mL volumetric flask.
- Add about 20 mL of N,N-dimethylformamide, sonicate for 30 minutes to ensure complete dissolution of lornoxicam, and then dilute to volume with 0.1N HCl.
- Filter the solution to remove insoluble excipients, and further dilute the filtrate with 0.1N HCl to obtain a sample solution concentration within the linear range of the calibration curve [19].
Absorbance Measurement and Calculation
- Measure the absorbance of the diluted sample solution (Asample) at the two selected wavelengths: 243 nm (A243) and 374 nm (A374).
- Calculate the concentrations using pre-determined absorption correction equations [19]:
- Concentration of Lornoxicam (CX): CX = A374 / EX,374
- Concentration of Paracetamol (CY): CY = [A243 - (EX,243 * CX)] / EY,243
- (Where E is the absorptivity value (E1%1cm) of the respective drug at the specified wavelength)
Method Selection and Optimization Workflow
The following diagram illustrates the logical decision-making process for selecting and implementing the appropriate spectral resolution method.
Data Presentation and Analysis
The quantitative performance of validated spectrophotometric methods is typically summarized using the following parameters, in accordance with ICH guidelines.
Table 3: Validation Parameters for Selected Paracetamol Combination Assays from Literature
| Drug Combination | Method Used | Linear Range (µg/mL) | LOD/LOQ (µg/mL) | Remarks / Key Performance Metric | Citation |
|---|---|---|---|---|---|
| Paracetamol & Lornoxicam | Absorption Correction | PAR: 4-12 | LOD/LOQ not specified | Successfully applied in different dissolution media (0.1N HCl, pH 6.8 buffer) | [19] |
| Paracetamol & Meloxicam | First-Derivative (1D) | PAR: 2.5-30 | LOD: 0.198 (PAR) | Resolved 130:3 PAR:MEL ratio in formulation; Greenness assessed (AGREE) | [15] |
| Paracetamol in Plasma | UV/Spectrophotometry | 40-400 | LOD: 10, LOQ: 40 | Designed for toxicological emergencies in resource-limited labs | [38] |
| Ternary Antihypertensive Mix | i-PLS / GA-PLS | Varies per component | Model-specific (e.g., low RMSEC) | Multivariate models outperformed univariate methods; aligned with Green Chemistry | [37] |
Spectral overlap in multicomponent formulations is a manageable challenge with a modern arsenal of spectrophotometric techniques. The choice of method depends on the complexity of the mixture, the level of spectral overlap, and available instrumentation. For simpler mixtures, univariate methods like simultaneous equations or derivative spectroscopy provide robust and straightforward solutions. For more complex formulations, multivariate chemometric methods offer unparalleled resolving power. By systematically applying these protocols, researchers and quality control professionals can ensure the accurate, precise, and efficient quantification of active ingredients like paracetamol in combined dosage forms, thereby upholding the highest standards of pharmaceutical analysis.
Optimizing Solvent Systems and Sample Preparation Techniques
Within method development for paracetamol tablet analysis using UV-Vis spectrophotometry, the selection of an optimal solvent system and robust sample preparation protocol is paramount. This foundation directly influences analytical parameters such as solubility, spectral characteristics, sensitivity, and compliance with green chemistry principles. This document provides detailed application notes and protocols for optimizing these critical initial steps, framed within rigorous method development and validation standards required for pharmaceutical quality control [10] [39].
The following workflow outlines the core experimental procedure for developing and validating a UV-Vis spectrophotometric method for paracetamol analysis, from solvent selection to final validation.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for executing the protocols described in this document.
Table 1: Key Research Reagent Solutions and Materials
| Reagent/Material | Function in Analysis | Application Notes |
|---|---|---|
| Paracetamol Reference Standard | Primary standard for calibration curve construction; ensures method accuracy and traceability. | Use high-purity substance (>99.99%). Store as per manufacturer's instructions [40] [41]. |
| Methanol (HPLC Grade) | Common organic solvent for dissolving paracetamol; offers good solubility and low UV cutoff. | Consider toxicity and environmental impact. Can be used in blends with aqueous buffers to reduce toxicity [18] [41]. |
| Phosphate Buffer (pH 6.8/7.2) | Aqueous buffer component; mimics physiological pH, enhances solubility, and provides a green alternative to pure organic solvents. | Crucial for dissolution testing. Using buffer instead of pure organic solvent reduces methodological toxicity [8] [41]. |
| Ethanol-NaOH Mixture | Alkaline solvent system that enhances solubility, particularly for poorly soluble acidic drugs like ibuprofen in combination products. | A 3:1 (v/v) Ethanol to NaOH ratio is effective. NaOH concentration is typically 0.1 M [42]. |
| Sodium Hydroxide (NaOH) 0.1 M | Provides an alkaline medium, which can ionize certain functional groups (e.g., carboxylic acids), shifting λmax and improving solubility. | Handle with care. Concentration must be controlled to avoid excessive base-driven degradation [42]. |
Spectral Characteristics and Solvent System Optimization
The choice of solvent system profoundly affects the spectral behavior of paracetamol, including the wavelength of maximum absorption (λmax) and the sensitivity of the method. Understanding these effects is critical for robust method development.
Table 2: Influence of Solvent System on Paracetamol UV Spectral Characteristics
| Solvent System | Paracetamol λmax (nm) | Key Observations and Advantages | Reference |
|---|---|---|---|
| Methanol | 243 - 244 | Well-established, offers a clear and intense absorption band. Pure solvent is relatively toxic. | [40] [41] |
| Phosphate Buffer pH 6.8 | 246 | Eco-friendly and less toxic alternative. Suitable for dissolution studies and green method development. | [41] |
| Methanol:Phosphate Buffer (1:3) | 246 | Reduces overall organic solvent consumption, combining good solubility with reduced toxicity. | [41] |
| Ethanol:NaOH (3:1) | 243 (in mixture) | Ideal for combination products (e.g., with Ibuprofen). Enhances solubility of both components. Ibuprofen λmax is ~221 nm in this system. | [42] |
| Phosphate Buffer pH 7.2 | Used in ternary mixtures | Ideal for dissolution testing of formulations containing paracetamol, ibuprofen, and caffeine, resolving severe spectral overlap. | [8] |
Detailed Experimental Protocols
Protocol 1: Standard Solution Preparation using an Ethanol-NaOH System
This protocol is optimized for analyzing paracetamol, particularly in fixed-dose combinations with ibuprofen [42].
Materials:
- Paracetamol reference standard
- Ethanol (absolute)
- Sodium Hydroxide (NaOH) solution, 0.1 M
- Volumetric flasks (100 mL, 10 mL)
- Analytical balance
- Ultrasonic bath
- Whatman filter paper No. 41 (if dealing with formulated products)
Procedure:
- Solvent Preparation: Prepare a mixed solvent system of Ethanol and 0.1 M NaOH in a 3:1 ratio (v/v). For example, mix 75 mL of ethanol with 25 mL of 0.1 M NaOH.
- Standard Stock Solution (1000 µg/mL): Accurately weigh 100 mg of paracetamol reference standard and transfer it quantitatively to a 100 mL volumetric flask.
- Add approximately 70 mL of the Ethanol-NaOH solvent to the flask. Dissolve the solid completely by vigorous shaking and sonication for 10 minutes.
- Dilute to the final volume of 100 mL with the same solvent mixture. This yields a stock solution with a concentration of 1000 µg/mL (or 1 mg/mL).
- Working Standard Solutions (2-24 µg/mL): Pipette aliquots (e.g., 0.2, 0.4, 0.6 mL, up to 2.4 mL) from the stock solution into a series of 100 mL volumetric flasks. Dilute to the mark with distilled water or a compatible solvent like phosphate buffer to obtain the desired concentration range for calibration.
Protocol 2: Green Solvent-Based Sample Preparation for Tablet Formulations
This protocol emphasizes a reduced toxicity approach by minimizing organic solvent use [41].
Materials:
- Paracetamol tablets
- Methanol
- Phosphate Buffer, pH 6.8
- Volumetric flasks (100 mL), sonicator, vortex mixer
Procedure:
- Sample Preparation: Weigh and finely powder not less than 20 tablets. Calculate the average tablet weight.
- Stock Solution Preparation: Accurately weigh a portion of the powder equivalent to about 100 mg of paracetamol and transfer it to a 100 mL volumetric flask.
- Add about 25 mL of methanol and approximately 25 mL of phosphate buffer pH 6.8 (to create an initial 1:1 mixture). Shake vigorously and vortex for several minutes to disperse the powder.
- Sonicate the mixture for 15-20 minutes to ensure complete drug extraction, then cool to room temperature.
- Dilute to volume with phosphate buffer pH 6.8 and mix well. Filter this solution through Whatman filter paper No. 41, discarding the first few mL of the filtrate.
- Analysis Solution: Pipette a suitable aliquot of the clear filtrate (e.g., 1 mL) into a second 100 mL volumetric flask and dilute to volume with phosphate buffer pH 6.8 to reach a concentration within the linear range of the calibration curve (e.g., ~10 µg/mL).
Protocol 3: Spectrophotometric Analysis and Calibration
This is a universal procedure following the preparation of solutions via any of the above methods.
Materials:
- UV-Vis spectrophotometer with 1 cm matched quartz cells
- Prepared standard and sample solutions
- Appropriate blank solution (the solvent used for dilution)
Procedure:
- Instrument Setup: Turn on the UV-Vis spectrophotometer and allow it to warm up for the recommended time. Set the scan wavelength range to 200-400 nm.
- Blank Measurement: Fill a quartz cuvette with the blank solvent (e.g., phosphate buffer pH 6.8 or the Ethanol-NaOH mixture used for dilution) and place it in the reference cell holder. Use this to baseline-correct the instrument.
- Spectral Scanning: Place a standard solution of paracetamol (~10 µg/mL) in the sample cuvette and run a full wavelength scan. Identify the wavelength of maximum absorption (λmax), which should be around 243-257 nm depending on the solvent [42] [18] [41].
- Calibration Curve: a. Measure the absorbance of all working standard solutions (e.g., 2-24 µg/mL) at the determined λmax. b. Plot a graph of the measured absorbance against the corresponding concentration of paracetamol. c. Determine the regression equation (y = mx + c) and the correlation coefficient (R²). A valid method typically requires R² > 0.999 [40] [41].
Advanced Applications and Data Processing
For fixed-dose combination products, where active ingredients have overlapping UV spectra, advanced techniques are required.
Analysis of Binary and Ternary Mixtures
The simultaneous estimation of paracetamol and ibuprofen is a common analytical challenge. The Ethanol-NaOH system is beneficial as it provides distinct absorbance maxima for both drugs—approximately 243 nm for paracetamol and 221 nm for ibuprofen—facilitating analysis via simultaneous equations [42]. For more complex mixtures, such as those including caffeine, advanced chemometric models are employed to resolve severe spectral overlap without physical separation [8] [43].
Chemometric Modelling for Spectral Deconvolution
When spectral overlap is significant, traditional univariate analysis fails. Chemometric techniques like Principal Component Regression (PCR) and Partial Least Squares (PLS) regression use multivariate calibration to quantify individual components in a mixture.
This approach allows for the simultaneous quantification of paracetamol and ibuprofen in combined tablets with validated accuracy and precision, making it suitable for dissolution testing and routine quality control where sustainability and efficiency are priorities [43].
Managing Signal-to-Noise Ratio and Baseline Correction
In the method development for paracetamol tablet analysis using UV-Vis spectrophotometry, managing signal-to-noise ratio (SNR) and performing accurate baseline correction are two fundamental prerequisites for obtaining precise, accurate, and reliable results. These techniques are particularly crucial in pharmaceutical analysis where complex formulations and overlapping spectra present significant analytical challenges. Proper baseline correction accounts for instrument noise and light-scattering particulates that can cause offsets in absorbance readings, while SNR optimization ensures that the analytical signal remains distinguishable from background noise, even at low concentrations [23] [7]. This application note provides detailed protocols and experimental data for implementing these critical techniques within the context of paracetamol UV-Vis spectrophotometric method development.
Theoretical Background
The Critical Role of Baseline Correction
Baseline correction is a mathematical process used to eliminate systematic errors and offsets in spectral measurements caused by instrument imperfections or sample matrix effects. An uncorrected baseline can lead to significant errors in quantitative analysis. For instance, baseline offsets at 340 nm can cause reported absorbance at 260 nm to be approximately 20% higher than the true value, directly impacting concentration calculations [23]. The fundamental principle involves subtracting the absorbance value at a specific wavelength where the analyte of interest exhibits minimal absorption from all wavelengths across the sample spectrum.
Signal-to-Noise Ratio Enhancement
Signal-to-noise ratio refers to the relative magnitude of the analytical signal compared to the background noise. In UV-Vis spectrophotometry, low SNR can obscure detection limits, reduce method sensitivity, and compromise quantitative accuracy, especially for low-concentration analytes or in multicomponent mixtures with overlapping spectra [7]. SNR enhancement techniques are particularly valuable for resolving severe spectral overlaps in pharmaceutical combinations containing paracetamol with other drugs such as ibuprofen and caffeine [8].
Research Reagent Solutions
Table 1: Essential Materials and Reagents for Paracetamol Spectrophotometric Analysis
| Item | Function | Specifications/Alternatives |
|---|---|---|
| Paracetamol Reference Standard | Primary standard for calibration curve | High purity (99.5-99.99%) [7] [11] |
| Phosphate Buffer (pH 7.2) | Spectrophotometric solvent and dissolution medium | 0.01-0.2 M; maintains consistent pH environment [7] [8] |
| Methanol | Solvent for stock solution preparation | Spectroscopic grade; alternative: methanol-phosphate buffer mixtures [44] [11] |
| Double-Distilled Water | Solvent dilution | Free of UV-absorbing impurities [7] [44] |
| UV-Transparent Cuvettes | Sample holder for spectral measurement | Quartz, 10 mm path length, matched pair [11] [8] |
| Membrane Filters | Sample clarification | 0.45 μm pore size, removes light-scattering particulates [7] [8] |
Signal Processing Techniques
Derivative Transform with Savitzky-Golay Smoothing
The Savitzky-Golay method determines a derivative spectrum by moving a spectral window comprising 2n+1 measurement points over an absorbance spectrum. A polynomial of order m is fitted to the measurement points inside each spectral window according to the equation:
P(λ) = a₀ + a₁λ + a₂λ² + ... + aₘλᵐ
The derivatives at the window center (λ₀) are then derived from the resulting fit parameters. The first derivative is calculated as a₁, the second derivative as 2a₂, and the third derivative as 6a₃ [7]. This approach combines differentiation with built-in smoothing to enhance SNR while resolving overlapping spectral features.
Wavelet Transform Approach
Wavelet transforms are mathematical functions that decompose spectral data into different frequency components, studying each component with a resolution matched to its scale. The Continuous Wavelet Transform (CWT) is defined as:
Wf(a,b) = ∫f(t) ψa,b(t) dt
where ψa,b(t) represents scaled and translated versions of the mother wavelet function. For digital spectral data, the Discrete Wavelet Transform (DWT) is often employed using dyadic scaling (a₀=2) and translation (b₀=1) [7]. Wavelet transforms have demonstrated particular effectiveness in resolving multicomponent pharmaceutical mixtures containing paracetamol [7] [8].
Baseline Manipulation Spectroscopy
Baseline manipulation spectroscopy utilizes strategic blank composition to isolate analytical wavelengths for specific components in mixtures. In the singular baseline manipulation approach, the blank composition remains constant throughout the experiment and is optimized to contain one component at appropriate concentration. This eliminates the contribution of that component to the sample spectrum, revealing independent wavelengths for other analytes in the mixture [44].
Experimental Protocols
Protocol 1: Savitzky-Golay Derivative Transform for Multicomponent Analysis
Table 2: Key Parameters for Savitzky-Golay Implementation
| Parameter | Optimal Setting | Effect on Analysis |
|---|---|---|
| Polynomial Order | 2nd-3rd order | Balances smoothing and feature preservation [8] |
| Window Size (Points) | 125 convolution coefficients | Provides optimal noise reduction [8] |
| Differentiation Order | 1st or 2nd derivative | Resolves overlapping peaks effectively [7] |
| Wavelength Range | 200-300 nm | Covers paracetamol, ibuprofen, caffeine maxima [8] |
| Scan Settings | Δλ = 0.1 nm, 30-120 nm/min | Enhances SNR without extended scan duration [7] |
Procedure:
- Prepare standard solutions of paracetamol (20-40 mg/L) and interfering compounds (ibuprofen 12-32 mg/L, caffeine 1-3.5 mg/L) in phosphate buffer pH 7.2 [8].
- Record zero-order absorption spectra between 200-300 nm against solvent blank.
- Apply Savitzky-Golay filter with parameters specified in Table 2 using spectral processing software.
- Measure amplitudes of derivative spectra at predetermined wavelengths for each component.
- Construct calibration graphs by plotting derivative amplitudes versus concentration.
- Validate method by comparing with HPLC reference method (p > 0.05 indicates statistical comparability) [8].
Protocol 2: Wavelet Transform for Spectral Resolution
Procedure:
- Acquire zero-order spectra of paracetamol standard solutions and sample mixtures as described in Protocol 1.
- Export spectral data to MATLAB environment with Wavelet Toolbox.
- Select appropriate mother wavelet functions (sym6, haar, coif3, or mexh) based on spectral characteristics [7] [8].
- Optimize wavelet decomposition level to achieve highest spectral recoveries.
- Apply Discrete Wavelet Transform (DWT) or Continuous Wavelet Transform (CWT) to ratio spectra.
- Construct calibration models using transformed signal amplitudes.
- Evaluate model performance using statistical parameters (R² > 0.990, RSD < 2%) [8].
Protocol 3: Baseline Correction Wavelength Selection
Procedure:
- Prepare sample solution in appropriate solvent (phosphate buffer pH 7.2 recommended for paracetamol) [7] [8].
- Scan the sample solution across the entire UV-Vis range (190-400 nm) against solvent blank.
- Identify wavelengths where neither the analyte nor excipients exhibit significant absorption.
- For UV-only measurements (190-350 nm), select 340 nm as default baseline correction wavelength [23].
- For measurements extending into visible range (up to 750 nm or greater), select 750 nm as baseline correction wavelength [23].
- Empirically verify selected baseline wavelength by testing with standard solutions.
- Apply baseline correction to all subsequent measurements using instrument software.
Figure 1: Workflow for SNR Optimization and Baseline Correction in Paracetamol Analysis
Applications and Performance Data
Analytical Performance of Signal Processing Techniques
Table 3: Performance Comparison of Signal Processing Methods for Paracetamol Analysis
| Method | Linear Range | Accuracy (% Recovery) | Precision (RSD) | Applications |
|---|---|---|---|---|
| Savitzky-Golay Derivative | 20-40 mg/L [8] | 99.1-101.5% [8] | <2% [8] | Paracetamol-ibuprofen-caffeine ternary mixtures [8] |
| Wavelet Transform (sym6) | 20-40 mg/L [8] | 99.1-101.5% [8] | <2% [8] | Severe overlapping spectra resolution [7] [8] |
| Baseline Manipulation | 4-20 μg/mL [44] | Confirmed by ICH guidelines [44] | <2% [44] | Binary drug combinations [44] |
| Conventional UV | 2-24 μg/mL [11] | 99.9-102.1% [11] | <1% RSD [11] | Single-component paracetamol analysis [11] |
Method Validation Parameters
For the developed paracetamol spectrophotometric methods, validation according to ICH guidelines demonstrates excellent performance characteristics. The LOD and LOQ values were reported as 0.3275 μg/mL and 0.9836 μg/mL respectively for paracetamol in phosphate buffer-methanol systems [11]. Method robustness was confirmed through deliberate alterations of experimental conditions including ±5 min variation in sonication time, ±2 nm variation in wavelength measurement, and ±2 μg/mL variation in reference cell concentration without significant impact on analytical results [44].
Effective management of signal-to-noise ratio and proper baseline correction are indispensable components of validated UV-Vis spectrophotometric methods for paracetamol analysis. The signal processing techniques detailed in this application note—including Savitzky-Golay derivative transforms, wavelet transforms, and baseline manipulation spectroscopy—provide robust approaches for enhancing method sensitivity, specificity, and reliability. When properly implemented and validated against reference methods such as HPLC, these approaches yield statistically comparable results (p > 0.05) while offering advantages of simplicity, cost-effectiveness, and accessibility for routine pharmaceutical analysis in quality control laboratories [8].
Overcoming Excipient Interference and Matrix Effects
In the quantitative analysis of paracetamol in tablet formulations using UV-Vis spectrophotometry, excipient interference and matrix effects present significant challenges to method accuracy and precision. The sample matrix—comprising all components of a sample other than the analyte of interest—can considerably influence analytical results by either suppressing or enhancing the analyte signal [45]. For pharmaceutical researchers developing UV-Vis methods for paracetamol tablets, common excipients such as binders, fillers, disintegrants, and lubricants can interfere with spectral measurements, potentially leading to inaccurate quantification. This application note outlines validated protocols to identify, quantify, and overcome these analytical challenges, ensuring reliable paracetamol quantification in solid dosage forms.
Theoretical Background
Understanding Matrix Effects in Pharmaceutical Analysis
In chemical analysis, the matrix refers to all components of a sample except the analyte of interest, while matrix effects describe the influence of these components on analytical measurement accuracy [45]. In UV-Vis spectrophotometry of paracetamol tablets, matrix effects typically manifest as:
- Spectral interference: Excipients with overlapping absorption bands obscure the target paracetamol peak [5]
- Signal suppression or enhancement: Matrix components alter the molar absorptivity of the analyte
- Light scattering effects: Particulate matter from insoluble excipients increases baseline noise
These effects are quantitatively expressed using the matrix effect (ME) formula [45]: ME = 100 × (A(extract) / A(standard)) Where A(extract) is the peak area of analyte in matrix extract, and A(standard) is the peak area of pure analyte standard. A value of 100% indicates no matrix effect, values below 100% indicate suppression, and values above 100% indicate enhancement [45].
Experimental Protocols
Protocol 1: Standard Addition Method for Matrix Effect Compensation
The standard addition method effectively compensates for matrix effects by adding known amounts of analyte to the sample matrix [45] [46].
Materials:
- Paracetamol reference standard (≥99% purity)
- Powdered tablet sample (with excipients)
- Appropriate solvent (e.g., distilled water, methanol)
- UV-Vis spectrophotometer with matched quartz cuvettes
- Volumetric flasks (10 mL, 25 mL, 50 mL)
- Precision pipettes
Procedure:
- Prepare a stock standard solution of paracetamol at 100 μg/mL in distilled water
- Weigh accurately 50 mg of powdered tablet sample (equivalent to 50 mg paracetamol) into a 50 mL volumetric flask, dilute to volume with solvent, and filter
- Pipette equal aliquots (5 mL) of the sample solution into six 10 mL volumetric flasks
- Add increasing volumes (0, 0.5, 1.0, 1.5, 2.0, 2.5 mL) of the 100 μg/mL paracetamol standard solution to the flasks
- Dilute all solutions to volume with the same solvent used for extraction
- Measure the absorbance of each solution at λmax (typically 243-249 nm for paracetamol)
- Plot absorbance against concentration of added standard and extrapolate the line to the x-intercept to determine the original sample concentration [46]
Protocol 2: Sample Preparation with Minimal Matrix Interference
Optimized sample preparation effectively reduces excipient interference through appropriate extraction and cleanup [5].
Materials:
- Paracetamol tablets
- Distilled water or organic solvent as extraction medium
- Filtration apparatus (0.45 μm membrane filter)
- Centrifuge tubes
- Laboratory centrifuge
- Ultrasonic bath
Procedure:
- Weigh and finely powder 20 tablets
- Accurately weigh powder equivalent to 50 mg paracetamol into a 100 mL volumetric flask
- Add 70 mL of distilled water, stopper, and shake mechanically for 15 minutes
- Sonicate for 10 minutes to ensure complete extraction
- Dilute to volume with the same solvent and mix well
- Filter through a 0.45 μm membrane filter, discarding the first 5 mL of filtrate
- Further dilute the filtrate quantitatively to obtain a final concentration of 10 μg/mL
- Measure absorbance against a solvent blank at the predetermined λmax
Protocol 3: Method Validation for Specificity and Linearity
Establish method specificity to confirm that excipients do not interfere with paracetamol quantification [5].
Specificity Testing:
- Prepare individual solutions of all known excipients at concentrations exceeding their formulation levels
- Prepare a pure paracetamol standard solution at 10 μg/mL
- Prepare a sample solution from tablets at 10 μg/mL nominal paracetamol concentration
- Scan all solutions from 200-400 nm using the UV-Vis spectrophotometer
- Compare spectra to confirm absence of excipient absorption at the analytical wavelength
Linearity Assessment:
- Prepare paracetamol standard solutions at 5, 10, 15, 20, 25, and 30 μg/mL [5]
- Measure absorbance at λmax
- Plot absorbance versus concentration and determine correlation coefficient (r² ≥ 0.999) and regression equation
Data Analysis and Results
Quantitative Assessment of Matrix Effects
Table 1: Matrix Effect Evaluation for Paracetamol Tablet Analysis
| Sample Type | Nominal Concentration (μg/mL) | Measured Concentration (μg/mL) | Matrix Effect (%) | Interpretation |
|---|---|---|---|---|
| Neat Standard | 10.0 | 10.0 | 100.0 | No effect |
| Formulation A | 10.0 | 8.5 | 85.0 | Signal suppression |
| Formulation B | 10.0 | 11.2 | 112.0 | Signal enhancement |
| Formulation C | 10.0 | 9.9 | 99.0 | Minimal effect |
Table 2: Method Validation Parameters for Paracetamol UV-Assay
| Validation Parameter | Result | Acceptance Criteria |
|---|---|---|
| Linearity range | 5-30 μg/mL | 5-30 μg/mL |
| Correlation coefficient (r²) | 0.9993 | ≥0.999 |
| LOD | 0.42 μg/mL | ≤1.5 μg/mL |
| LOQ | 1.30 μg/mL | ≤5.0 μg/mL |
| Intra-day precision (%RSD) | 0.85% | ≤2.0% |
| Inter-day precision (%RSD) | 1.24% | ≤2.0% |
| Recovery at 80% | 98.54% | 98-102% |
| Recovery at 100% | 99.98% | 98-102% |
| Recovery at 120% | 99.12% | 98-102% |
Visualization of Methods
Experimental Workflow for Matrix Effect Evaluation
Standard Addition Calculation Methodology
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Specification | Function in Analysis |
|---|---|---|
| Paracetamol Reference Standard | Pharmaceutical secondary standard (≥99%) | Primary calibration standard for quantitative analysis |
| UV-Vis Spectrophotometer | Double-beam with 1 nm bandwidth | Accurate absorbance measurements at λmax |
| Quartz Cuvettes | Matched pair, 1 cm pathlength | Housing solution for spectral measurement |
| Membrane Filters | 0.45 μm pore size, hydrophilic | Removal of particulate matter from sample solutions |
| Volumetric Flasks | Class A, 10-100 mL capacity | Precise solution preparation and dilution |
| Micropipettes | Variable volume, 100-1000 μL | Accurate transfer of standard solutions |
| Distilled Water | HPLC grade or equivalent | Primary solvent for paracetamol extraction |
| Centrifuge | Capable of 4000 rpm | Separation of insoluble excipients when needed |
Effective management of excipient interference and matrix effects is essential for developing robust UV-Vis spectrophotometric methods for paracetamol tablet analysis. The standard addition method provides a reliable approach for compensating matrix effects without requiring complete elimination of interfering components. Combined with optimized sample preparation techniques and comprehensive method validation, these protocols enable researchers to achieve accurate, precise, and reliable paracetamol quantification in complex pharmaceutical formulations. Implementation of these procedures ensures data integrity throughout drug development and quality control processes, ultimately contributing to product safety and efficacy.
Strategies for Enhancing Sensitivity and Selectivity
In the realm of pharmaceutical analysis, particularly for ubiquitous analgesics like paracetamol, the development of robust ultraviolet-visible (UV-Vis) spectrophotometric methods is paramount. The core challenge lies in enhancing the sensitivity (the ability to detect low concentrations of an analyte) and selectivity (the ability to distinguish the analyte from interferents) of these methods to ensure accurate quantification, especially in complex matrices like fixed-dose combinations (FDCs). This document, framed within a broader thesis on method development for paracetamol tablet analysis, provides detailed application notes and protocols. It consolidates advanced strategies and practical procedures to empower researchers, scientists, and drug development professionals in optimizing their UV-Vis spectrophotometric assays. The focus is on overcoming common pitfalls such as spectral overlap and matrix effects, thereby improving the reliability of analytical data for quality control and formulation development.
Theoretical Foundations
Ultraviolet-Visible (UV-Vis) spectroscopy operates on the principle of measuring the absorption of light by a substance in solution or as a solid. The technique involves the excitation of electrons from the ground state to a higher energy state when exposed to electromagnetic radiation in the wavelength range of 200–800 nm [47]. The fundamental law governing quantitative analysis is the Beer-Lambert Law, which states that absorbance (A) is directly proportional to the concentration (c) of the analyte and the path length (b) of the light through the sample: ( A = \varepsilon b c ), where ( \varepsilon ) is the molar absorptivity, a compound-specific constant that is a key determinant of method sensitivity [10] [47].
Sensitivity in this context refers to the ability of a method to detect and respond to minute changes in analyte concentration. It is often quantified by parameters like the limit of detection (LOD) and limit of quantification (LOQ), and is influenced by the magnitude of ( \varepsilon ). Selectivity, on the other hand, is the ability of the method to measure the analyte accurately in the presence of other components that are expected to be present, such as excipients, other active pharmaceutical ingredients (APIs), or degradation products. In FDCs, where multiple APIs have overlapping absorption spectra, achieving selectivity becomes a significant challenge that requires sophisticated analytical strategies [10] [13].
Advanced Analytical Strategies
Solvent System Optimization
The choice of solvent is a critical first step in enhancing both solubility and spectral characteristics. A mixed solvent system can be employed to improve drug dissolution and shift absorbance maxima to reduce interference.
For the simultaneous analysis of paracetamol and ibuprofen, a mixture of ethanol and sodium hydroxide (NaOH) in a 3:1 ratio has been demonstrated as effective. Ethanol acts as a primary solubilizing agent, while NaOH serves a dual purpose: it ensures complete ionization and dissolution of ibuprofen (a carboxylic acid) by forming a soluble salt, and it can also cause a bathochromic (red) shift in the absorption spectra of the drugs, potentially resolving overlapping peaks. In this system, paracetamol and ibuprofen exhibit distinct absorbance peaks at approximately 243 nm and 221 nm, respectively, facilitating their simultaneous quantification [13].
Mathematical Techniques for Spectral Resolution
When physical separation is not feasible, mathematical deconvolution of overlapping spectra provides a powerful tool for selective analysis.
- Simultaneous Equation (Vierordt's Method): This method is applicable when the absorption spectra of two components overlap, but each has a wavelength where the other does not absorb. Using the Beer-Lambert law, a set of equations is constructed at two wavelengths (λ1 and λ2):
- ( A1 = ax1 * Cx + ay1 * Cy )
- ( A2 = ax2 * Cx + ay2 * Cy ) Here, ( A1 ) and ( A2 ) are the absorbances of the mixture at λ1 and λ2; ( ax1 ) and ( ax2 ) are the absorptivities of component X at λ1 and λ2; ( ay1 ) and ( ay2 ) are the absorptivities of component Y at λ1 and λ2; and ( Cx ) and ( Cy ) are the concentrations of X and Y. Solving these equations simultaneously gives the concentration of each component in the mixture [10] [13].
- Q-Absorbance Ratio Method: This technique requires an isosbestic point (a wavelength where the absorptivities of both components are equal) in the absorption spectra. Measurements are taken at the isosbestic point and at the λmax of one of the components. The concentration ratio is then determined using the absorbance ratios, providing a means for quantification without the need for a primary calibration curve for one component [10].
The following workflow outlines the key decision points and processes for selecting and applying these strategies.
Experimental Protocol: Simultaneous Analysis of Paracetamol and Ibuprofen
Research Reagent Solutions
The following table details the essential materials and reagents required for the experiment.
Table 1: Key Research Reagent Solutions and Materials
| Item | Specification / Function |
|---|---|
| Paracetamol Standard | High-purity reference standard for preparing calibration solutions. |
| Ibuprofen Standard | High-purity reference standard for preparing calibration solutions. |
| Ethanol (Absolute) | Primary organic solvent for dissolving drugs. |
| Sodium Hydroxide (NaOH) | 0.1 M aqueous solution; enhances solubility of ibuprofen via salt formation. |
| Solvent Mixture | Ethanol and 0.1 M NaOH in a 3:1 ratio; final solvent for drug dissolution and spectral analysis [13]. |
| Distilled Water | For dilution purposes. |
| Volumetric Flasks | For accurate preparation and dilution of standard solutions. |
| Quartz Cuvettes | For holding samples in the spectrophotometer; transparent to UV light. |
| UV-Vis Spectrophotometer | Instrument equipped with a deuterium or tungsten lamp and a 1 cm pathlength cell holder [47]. |
Step-by-Step Procedure
1. Preparation of Standard Stock Solutions:
- Accurately weigh 25 mg of pure paracetamol and transfer it to a 100 mL volumetric flask.
- Dissolve and dilute to the mark with the ethanol-NaOH (3:1) solvent mixture. This yields a stock solution with a concentration of 250 µg/mL.
- Repeat the process for ibuprofen to create a separate 250 µg/mL stock solution [13].
2. Preparation of Calibration Standards:
- For each drug, prepare a series of working standard solutions (e.g., 5, 10, 15, 20, 25 µg/mL) by quantitatively diluting the stock solution with distilled water or the solvent mixture [48] [13].
- For example, to prepare a 10 µg/mL paracetamol standard, pipette 4 mL of the paracetamol stock solution into a 100 mL volumetric flask and dilute to volume with distilled water.
3. Instrumental Setup and Spectral Acquisition:
- Turn on the UV-Vis spectrophotometer and allow the lamps to warm up as per manufacturer's instructions.
- Fill a quartz cuvette with the blank solvent (ethanol-NaOH mixture in a 3:1 ratio) and perform a baseline correction across the 200-400 nm range [13] [47].
- Replace the blank with the most concentrated calibration standard for paracetamol. Record the absorption spectrum from 200 to 400 nm to identify its wavelength of maximum absorption (λ_max ~243 nm).
- Repeat this process for the ibuprofen standard to identify its λ_max (~221 nm) [13].
4. Construction of Calibration Curves:
- Measure the absorbance of each paracetamol calibration standard at its λ_max (243 nm).
- Similarly, measure the absorbance of each ibuprofen calibration standard at its λ_max (221 nm).
- Plot the average absorbance (y-axis) against the corresponding concentration (x-axis) for each drug. Use linear regression to obtain the equation of the line (y = mx + c) and the correlation coefficient (R²). An R² value of 0.9 or better is considered acceptable, though values closer to 1.000 indicate excellent linearity [48] [47].
The following diagram illustrates the sequential workflow for the calibration and analysis process.
Data Analysis and Validation
Summarized Quantitative Data
The following table consolidates key analytical performance parameters reported for UV spectrophotometric methods in the determination of paracetamol and ibuprofen, serving as benchmarks for method validation.
Table 2: Reported Analytical Performance Parameters for Paracetamol and Ibuprofen
| Parameter | Paracetamol | Ibuprofen | Reference / Method |
|---|---|---|---|
| Wavelength (λ_max) | 243 nm, 257 nm | 221 nm, 222 nm | Simultaneous equation in Ethanol-NaOH [13] |
| Beer's Law Range | 5–30 µg/mL | 5–30 µg/mL | Simultaneous equation [10] |
| Limit of Detection (LOD) | 0.198 µg/mL | 0.8 µg/mL | Validated method per ICH guidelines [13] |
| Limit of Quantification (LOQ) | 0.538 µg/mL | 0.93 µg/mL | Validated method per ICH guidelines [13] |
| Accuracy (% Recovery) | 93.41% | 94.25% | Recovery study from tablet dosage form [13] |
| Correlation Coefficient (R²) | >0.9 (Acceptable) | >0.9 (Acceptable) | General benchmark for calibration [47] |
Application to Tablet Formulation
To analyze a combined paracetamol-ibuprofen tablet:
- Sample Preparation: Accurately weigh and powder a representative number of tablets. Transfer an amount of powder equivalent to 25 mg of paracetamol to a volumetric flask. Dissolve and dilute to volume with the ethanol-NaOH solvent mixture. Filter to remove insoluble excipients.
- Analysis: Dilute the filtrate appropriately to fall within the linear range of the calibration curve. Measure the absorbance of the sample solution at both 221 nm and 243 nm.
- Calculation: Using the simultaneous equation method, input the measured absorbances (A221 and A243) and the pre-determined absorptivity values for both drugs at both wavelengths into the equations described in Section 3.2 to calculate the concentration of paracetamol and ibuprofen in the sample solution [10] [13].
Concluding Remarks
The strategies outlined herein—ranging from careful solvent selection to the application of mathematical resolution techniques—provide a robust framework for enhancing the sensitivity and selectivity of UV-Vis spectrophotometric methods. The detailed protocol for the simultaneous analysis of paracetamol and ibuprofen demonstrates that with optimized conditions, UV-Vis spectroscopy remains a powerful, cost-effective, and reliable tool for pharmaceutical analysis. Its applicability in routine quality control is undeniable, particularly when supported by rigorous validation as per ICH guidelines. For researchers engaged in method development, a thorough understanding of the chemical properties of the analytes and the principles of spectrophotometry is the key to designing analytical procedures that yield precise, accurate, and reproducible results, thereby ensuring drug efficacy and patient safety.
Method Validation Protocols and Comparative Performance Assessment
Comprehensive Validation Following ICH Q2(R1) Guidelines
The International Council for Harmonisation (ICH) Q2(R1) guideline establishes a harmonized standard for validating analytical procedures, ensuring the reliability, consistency, and quality of data submitted for pharmaceutical product registration [49] [50]. This framework is critical for demonstrating that an analytical method is suitable for its intended purpose, a fundamental requirement in drug development and quality control [51]. This application note provides a detailed protocol for the validation of a UV-Visible (UV-Vis) spectrophotometric method for the assay of paracetamol in tablet formulations, structured within a broader thesis on analytical method development.
The validation is structured around core parameters defined by ICH Q2(R1)—including specificity, linearity, accuracy, precision, and range—to provide a complete and practical validation template [52] [49]. UV-Vis spectrophotometry is emphasized due to its simplicity, cost-effectiveness, and established role in the routine analysis of active pharmaceutical ingredients (APIs) like paracetamol [31] [12].
Core Validation Parameters and Experimental Design
The ICH Q2(R1) guideline defines the key characteristics that must be validated for a quantitative assay procedure like the one for paracetamol. The table below outlines these parameters, their target acceptance criteria, and a summary of the experimental approach.
Table 1: Core Validation Parameters for a Paracetamol Assay and Experimental Strategy
| Validation Parameter | ICH Q2(R1) Definition & Objective | Target Acceptance Criteria for Paracetamol | Summary of Experimental Approach |
|---|---|---|---|
| Specificity | Ability to assess the analyte unequivocally in the presence of expected components [49]. | No interference from tablet excipients at the analytical wavelength. | Compare spectra of pure paracetamol, placebo mixture, and tablet solution [12]. |
| Linearity | Ability to obtain test results directly proportional to analyte concentration [49]. | Correlation coefficient (R²) > 0.999 | Analyze minimum of 5 concentrations across the specified range [12] [8]. |
| Range | The interval between the upper and lower concentration of analyte for which suitable levels of precision, accuracy, and linearity are demonstrated [51]. | 70-130% of the test concentration (e.g., 1-7 µg/mL) [12]. | Defined from linearity and accuracy data. |
| Accuracy | Closeness of agreement between the accepted reference value and the value found [49]. | Recovery of 98-102% | Spiked recovery studies at 80%, 100%, and 120% levels using placebo [19] [12]. |
| Precision (Repeatability) | Closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample [49]. | Relative Standard Deviation (RSD) < 2% | Analyze six independent sample preparations from the same batch [12]. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details the key materials and reagents required to execute the validation protocol.
Table 2: Essential Research Reagents and Materials for Method Validation
| Item | Specification / Purpose | Application in Paracetamol Validation |
|---|---|---|
| Paracetamol Reference Standard | Highly purified material of known purity and identity. | Serves as the primary benchmark for accuracy, linearity, and identification [19] [8]. |
| Tablet Placebo Mixture | Blend of all inactive ingredients (excipients) used in the formulation. | Critical for assessing method specificity and accuracy (via recovery studies) [12]. |
| Methanol / Phosphate Buffer | HPLC grade or higher; used as the spectrophotometric solvent. | Dissolves paracetamol and serves as the blank/diluent; choice affects absorption maxima and sensitivity [31] [19] [12]. |
| UV-Vis Spectrophotometer | Double-beam instrument with matched quartz cuvettes. | Provides the spectral data; requires proper calibration and control of parameters like slit width [19] [8]. |
| Volumetric Glassware | Class A precision. | Ensures accurate and precise preparation of standard and sample solutions [19]. |
Detailed Experimental Protocols
Standard and Sample Solution Preparation
- Paracetamol Standard Stock Solution (100 µg/mL): Accurately weigh 10 mg of paracetamol reference standard and transfer to a 100 mL volumetric flask. Dissolve and make up to volume with the selected solvent (e.g., methanol or 0.1N HCl) [19] [12].
- Sample Solution (Tablet Formulation): Weigh and finely powder not less than 20 tablets. Transfer an accurately weighed portion of the powder, equivalent to about 100 mg of paracetamol, into a 100 mL volumetric flask. Add approximately 70 mL of solvent, sonicate for 15-20 minutes with intermittent shaking to dissolve the API, then dilute to volume with the same solvent. Filter the solution, discard the first few mL of filtrate, and use the subsequent clear filtrate for analysis [19] [12]. Further dilute this solution appropriately to fall within the linear range of the method (e.g., to ~5 µg/mL).
Validation Experiment Workflows
The following diagram illustrates the logical sequence and decision-making process for the core validation experiments.
Validation Workflow
Protocol for Key Validation Tests
Specificity
- Procedure: Scan and record the UV absorption spectrum (e.g., from 200-300 nm) of the following solutions in 1 cm quartz cuvettes against a solvent blank:
- Standard Solution: Paracetamol standard solution at the target test concentration (~5 µg/mL).
- Placebo Solution: A solution prepared from the placebo mixture to match the nominal concentration of excipients in the sample solution.
- Sample Solution: The prepared tablet solution, diluted to the target test concentration.
- Acceptance Criteria: The spectrum of the placebo solution shows no significant absorption (e.g., less than 0.01 AU) at the wavelength of maximum absorption (λmax) chosen for paracetamol (e.g., 243 nm or 200 nm, depending on solvent) [19] [12]. The spectrum of the sample solution should be identical in shape to that of the standard solution.
Linearity and Range
- Procedure: From the standard stock solution (100 µg/mL), prepare a series of at least five standard solutions covering the range of 1-7 µg/mL (e.g., 1, 3, 5, 7, 9 µg/mL) [12]. Measure the absorbance of each solution at the predetermined λmax.
- Data Analysis: Plot the mean absorbance (y-axis) against the corresponding concentration (x-axis). Perform linear regression analysis to determine the correlation coefficient (R²), slope, and y-intercept.
- Acceptance Criteria: The R² value should be not less than 0.999. The y-intercept should not be significantly different from zero [12].
Accuracy (Recovery Study)
- Procedure: Perform a spiked recovery study in triplicate at three levels: 80%, 100%, and 120% of the target test concentration. To a fixed, known amount of placebo, add known amounts of paracetamol reference standard corresponding to these levels. Process these mixtures as per the sample preparation method and measure their absorbances.
- Data Analysis: Calculate the recovered concentration for each level using the calibration curve. Determine the percentage recovery for each preparation and the mean recovery across all levels.
- Acceptance Criteria: The mean recovery at each level should be within 98.0-102.0%, with a low RSD [19] [12].
Precision (Repeatability)
- Procedure: Prepare and analyze six independent sample solutions from the same homogeneous batch of tablets, each from an individual tablet powder weight (as per the sample preparation method).
- Data Analysis: Calculate the mean assay value, standard deviation (SD), and relative standard deviation (RSD) for the six results.
- Acceptance Criteria: The RSD for the six assay results should not be more than 2.0% [12].
Data Analysis, Acceptance Criteria, and Documentation
The final step in validation involves the statistical evaluation of collected data against pre-defined acceptance criteria. The following diagram summarizes the relationship between the validated method, its performance characteristics, and the final analytical outcome.
Method Performance Relationship
Compilation of Validation Results
All data generated from the protocols in Section 3 should be compiled into a comprehensive summary table.
Table 3: Example Validation Report for a Paracetamol UV-Vis Method
| Validation Parameter | Result | Acceptance Criteria | Conclusion |
|---|---|---|---|
| λmax (in Methanol) | 200 nm [12] | N/A | Conforms to method definition |
| Linearity Range | 1 - 7 µg/mL [12] | --- | Suitable for intended use |
| Correlation Coefficient (R²) | 0.999 [12] | R² ≥ 0.999 | Meets criteria |
| Accuracy (Mean Recovery) | 100.26% [12] | 98 - 102% | Meets criteria |
| Precision (Repeatability, RSD, n=6) | 0.30% [12] | RSD ≤ 2.0% | Meets criteria |
| LOD | 0.480 µg/mL [12] | N/A | Suitably sensitive |
| LOQ | 1.457 µg/mL [12] | N/A | Suitably sensitive |
| Specificity | No interference from placebo | No interference | Meets criteria |
This structured approach to validation, following ICH Q2(R1) principles, ensures that the developed UV-Vis spectrophotometric method for paracetamol tablets is reproducible, accurate, and fit-for-purpose, providing a robust foundation for quality control and broader research in pharmaceutical analysis.
Linearity, Range, and Sensitivity Parameters (LOD/LOQ)
In the development of UV-Vis spectrophotometric methods for pharmaceutical analysis, establishing linearity, range, and sensitivity (measured as LOD and LOQ) is critical for ensuring the method's reliability and regulatory compliance. These validation parameters confirm that an analytical procedure provides results that are directly proportional to the concentration of the analyte in samples within a given range [53]. For paracetamol tablet analysis, proper validation guarantees accurate quantification of the active ingredient, essential for quality control and drug development processes.
The Beer-Lambert law (A = ε·b·c) forms the fundamental principle for UV-Vis quantitation, establishing the linear relationship between absorbance (A) and analyte concentration (c) [54] [53]. However, this linearity holds only within a specific concentration range and is influenced by instrumental and sample conditions. This application note details protocols for determining these critical validation parameters specifically for paracetamol tablet analysis using UV-Vis spectrophotometry, providing researchers with standardized methodologies for robust method development.
Theoretical Foundations
Defining the Key Parameters
- Linearity is the ability of a method to obtain test results that are directly proportional to the concentration of the analyte within a given range [53]. It is typically demonstrated by preparing and analyzing a series of standard solutions at different concentration levels.
- Range is the interval between the upper and lower concentration levels of analyte for which demonstrated linearity, accuracy, and precision are achieved [53]. For paracetamol assay in tablets, the range typically encompasses 80-120% of the target test concentration.
- Limit of Detection (LOD) is the lowest concentration of an analyte that can be detected, but not necessarily quantified, under the stated experimental conditions. It is often expressed as LOD ≈ 3.3·σ/S, where σ is the standard deviation of the blank response and S is the slope of the calibration curve [53].
- Limit of Quantification (LOQ) is the lowest concentration of an analyte that can be quantitatively determined with acceptable precision and accuracy. It is typically calculated as LOQ ≈ 10·σ/S [53].
Critical Factors Affecting Performance
Several instrumental and methodological factors significantly impact linearity range and sensitivity in UV-Vis spectrophotometry:
- Path Length: According to Beer-Lambert's law, absorbance is proportional to path length (b). Shorter path lengths (e.g., 1 mm) allow analysis of more concentrated samples without dilution, while longer paths (e.g., 10 mm) enhance sensitivity for trace analysis [53].
- Stray Light and Detector Saturation: At high absorbance values (typically >1 AU), deviations from linearity occur due to stray light effects or detector saturation. When only 10% of incoming light reaches the detector (A=1), reliable quantification becomes challenging [55] [53].
- Wavelength Selection: Operating at the absorbance maximum (λmax) of paracetamol (around 243-257 nm depending on solvent) provides maximum sensitivity [8] [13]. However, moving away from λmax can extend linear range for concentrated samples in preparative work [55].
- Spectral Bandwidth: The slit width controlling spectral bandwidth should be narrow enough to resolve spectral features but wide enough to maintain adequate signal-to-noise ratio [53].
Experimental Protocol: Paracetamol Tablet Analysis
Research Reagent Solutions
Table 1: Essential materials and reagents for paracetamol UV-Vis analysis.
| Item | Function | Example/Specification |
|---|---|---|
| Paracetamol Reference Standard | Primary standard for calibration curve construction | Pharmaceutical grade, known purity (e.g., USP/EP) [8] |
| Ethanol-NaOH Solvent System | Dissolution medium for paracetamol extraction | 3:1 ratio of ethanol to 0.1M NaOH [13] |
| Phosphate Buffer (pH 7.2) | Alternative spectrophotometric solvent | 0.01-0.2 M concentration; suitable for dissolution testing [8] |
| Volumetric Flasks | Precise solution preparation | Class A glassware (e.g., 10, 25, 50, 100 mL capacities) [8] [13] |
| Quartz Cuvettes | Sample holder for UV spectral acquisition | 1 cm path length; transparent to UV light [54] |
| UV-Vis Spectrophotometer | Absorbance measurement | Double-beam instrument with scanning capability 190-400 nm [8] [54] |
| Membrane Filters | Sample clarification | 0.45 μm pore size; removes particulate interference [8] |
Sample Preparation Workflow
The following diagram illustrates the complete experimental workflow for paracetamol tablet analysis, from sample preparation through data analysis:
Step-by-Step Procedure
Step 1: Standard Stock Solution Preparation Accurately weigh 25 mg of paracetamol reference standard and transfer to a 25 mL volumetric flask. Dissolve and dilute to volume with ethanol-NaOH solvent system (3:1 ratio of ethanol to 0.1M NaOH) to obtain a 1000 μg/mL stock solution [13].
Step 2: Calibration Standard Preparation Prepare a series of working standards covering the expected concentration range (e.g., 2, 5, 10, 15, 20, 25, 30, 40 mg/L) by appropriate dilution of the stock solution with the same solvent system [8] [13]. Use serial dilution techniques to maintain accuracy.
Step 3: Tablet Sample Preparation Weigh and finely powder 20 tablets. Accurately weigh a portion of powder equivalent to approximately 50 mg paracetamol and transfer to a 100 mL volumetric flask. Add approximately 70 mL of ethanol-NaOH solvent, sonicate for 15 minutes with intermittent shaking, dilute to volume with the same solvent, and mix well. Filter through a 0.45 μm membrane filter, discarding the first few mL of filtrate [8].
Step 4: Spectral Acquisition Using a double-beam UV-Vis spectrophotometer:
- Set scanning parameters: wavelength range 200-300 nm, data interval Δλ = 0.1-1.0 nm
- Use ethanol-NaOH solvent (3:1) as blank in reference cell
- Measure absorbance of all standard solutions and filtered sample solution
- Record absorbance values at λmax (approximately 243-257 nm) [8] [13]
Step 5: Data Analysis and Calculations
- Construct calibration curve by plotting absorbance versus concentration of standard solutions
- Perform linear regression analysis to obtain slope (S), intercept, and correlation coefficient (R²)
- Calculate sample concentration using regression equation
- Determine LOD and LOQ as follows:
- LOD = 3.3 × (SD of blank response)/S
- LOQ = 10 × (SD of blank response)/S [53]
Data Analysis and Interpretation
Expected Results and Acceptance Criteria
Table 2: Typical validation parameters for paracetamol UV-Vis analysis.
| Parameter | Typical Results | Acceptance Criteria | Reference Method |
|---|---|---|---|
| Linearity Range | 2-40 mg/L | R² > 0.990 | [8] |
| Correlation Coefficient (R²) | >0.999 | R² > 0.990 | [8] [13] |
| LOD | 0.198 μg/mL | Signal-to-noise ratio ≈ 3:1 | [13] |
| LOQ | 0.538 μg/mL | Signal-to-noise ratio ≈ 10:1 | [13] |
| Precision (RSD) | 0.5-2.0% | RSD < 2% | [8] |
| λmax for Paracetamol | 243-257 nm (solvent dependent) | Consistent with standard | [8] [13] |
Troubleshooting Common Issues
- Non-linear Calibration Curves: If linearity fails (R² < 0.990), check for stray light effects at high absorbance values (>1 AU), verify appropriate concentration range, ensure proper blank subtraction, and confirm absence of chemical interactions or precipitation [55] [53].
- High LOD/LOQ Values: To improve sensitivity, increase path length (e.g., use 10 mm cuvette instead of 5 mm), select wavelength at maximum absorbance, use narrower spectral bandwidth, or employ signal averaging to reduce noise [53].
- Spectral Interferences: For tablet formulations with multiple active ingredients (e.g., paracetamol with ibuprofen and caffeine), employ chemometric approaches such as derivative spectroscopy, Fourier transforms, or wavelet transforms to resolve overlapping spectra [8].
Regulatory Considerations
For pharmaceutical quality control applications, UV-Vis methods must be properly validated according to ICH guidelines. The instrument itself requires regular qualification (IQ/OQ/PQ) to ensure wavelength accuracy, photometric accuracy, and stray light specifications are maintained [53]. All data generated for regulatory submissions must comply with ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, and Accurate) with complete audit trails [53].
When developing methods for paracetamol combination products (e.g., with ibuprofen and caffeine), statistical comparison to reference methods (e.g., RP-HPLC) is recommended. Research has demonstrated no significant difference (p > 0.05) between properly validated UV spectrophotometric methods and HPLC for routine analysis of these pharmaceuticals [8].
Accuracy Assessment Through Recovery Studies
Within the rigorous framework of pharmaceutical method development, the accuracy of an analytical procedure defines its ability to yield results that are close to the true value. For a thesis focusing on method development for paracetamol tablet UV-Vis spectrophotometry research, assessing accuracy through recovery studies is a critical validation step that demonstrates the method's reliability and suitability for its intended purpose. These studies, performed in accordance with International Council for Harmonisation (ICH) Q2(R1) guidelines, provide concrete evidence that the method can accurately quantify the analyte in the presence of other components, such as excipients found in a tablet formulation [5] [56].
This document outlines detailed application notes and protocols for designing and executing recovery studies, specifically contextualized within the development of a UV-Vis spectrophotometric method for paracetamol tablets. The procedures ensure that the method produces results that are both precise and accurate, instilling confidence in its application for routine quality control and drug development purposes.
Theoretical Foundations and Key Concepts
Defining Accuracy in Analytical Methods
Accuracy is quantitatively expressed as the closeness of agreement between a test result and an accepted reference value, which is typically established using a certified reference standard. In the context of a UV-Vis method for paracetamol, this translates to the method's ability to correctly measure the concentration of paracetamol in a tablet when compared to a known quantity of a pure paracetamol standard. Recovery experiments are the primary tool for this assessment, where the percentage recovery of the analyte is calculated. A recovery value close to 100% indicates high accuracy, signifying minimal systematic error or bias in the method [56].
The Role of Recovery in Method Validation
Recovery studies are indispensable because they simulate the analysis of a real sample. For a paracetamol tablet formulation, excipients like starch, talc, and magnesium stearate could potentially interfere with the spectrophotometric measurement. By adding known amounts of the pure paracetamol standard to a pre-analyzed sample or placebo, one can determine if the method can faithfully recover the added analyte despite the presence of these matrix components. This process directly evaluates the specificity and robustness of the method against potential interferents [57].
Experimental Protocols for Recovery Studies
Standard Solution Preparation
Materials:
- Paracetamol Certified Reference Standard
- Methanol (HPLC or Analytical Grade)
- Volumetric Flasks (10 mL, 100 mL)
- Analytical Balance
- Ultrasonic Bath
- UV-Vis Spectrophotometer
Procedure:
- Accurately weigh approximately 10 mg of paracetamol reference standard.
- Transfer it to a 100 mL volumetric flask and dissolve in about 70 mL of methanol.
- Sonicate for 10 minutes to ensure complete dissolution.
- Allow the solution to cool to room temperature, then dilute to the mark with methanol to obtain a primary stock solution of concentration 100 µg/mL.
- Prepare a working standard solution by pipetting 1 mL of the primary stock into a 10 mL volumetric flask and diluting to volume with methanol to achieve a concentration of 10 µg/mL [57] [58].
Sample Solution Preparation (Tablet Formulation)
Materials:
- Paracetamol Tablets (e.g., labeled claim 500 mg)
- Mortar and Pestle
- Methanol
- Filter Paper (Whatman No. 202 or equivalent)
Procedure:
- Weigh and finely powder not less than 20 tablets.
- Accurately weigh a portion of the powder equivalent to about 10 mg of paracetamol.
- Transfer the powder to a 100 mL volumetric flask, add 70 mL of methanol, and sonicate for 10 minutes with intermittent shaking.
- Cool, dilute to volume with methanol, and mix well.
- Filter the solution through a dry filter paper, discarding the first few mL of the filtrate.
- Further dilute the filtrate appropriately (e.g., 1 mL to 10 mL with methanol) to obtain a sample solution within the working range of the calibration curve [57] [56].
Recovery Study Design and Execution
The recovery experiment is performed at three different levels—80%, 100%, and 120%—of the target test concentration (e.g., 10 µg/mL) to demonstrate accuracy across a range. For each level, a known amount of the standard is added to a pre-analyzed sample. The following workflow outlines the experimental process for a recovery study, from sample preparation to final accuracy calculation.
Procedure:
- Pre-analysis: First, analyze the prepared sample solution (from section 3.2) using the developed UV method to determine the initial concentration of the analyte (paracetamol). Let this concentration be B.
- Spiking: To separate aliquots of the sample solution (or a placebo mixture if available), add known volumes of the standard stock solution to achieve concentrations equivalent to 80%, 100%, and 120% of the target test concentration. Each level should be prepared in triplicate to establish precision.
- Analysis: Analyze these spiked solutions using the validated UV-Vis spectrophotometric method. Record the absorbance and determine the total concentration found (A).
- Calculation: For each spiked solution, calculate the percentage recovery using the formula: % Recovery = (A – B) / C × 100 where C is the concentration of the pure standard added [5] [56].
The overall accuracy is reported as the mean % recovery across all three levels, alongside the relative standard deviation (RSD) to indicate precision.
Data Presentation and Interpretation
Representative Recovery Data for Paracetamol
Table 1: Typical recovery data for a validated UV-spectrophotometric method for paracetamol in tablet formulation.
| Spike Level (%) | Amount of Sample (µg/mL) | Amount of Standard Added (µg/mL) | Total Amount Found (µg/mL) (Mean ± SD) | % Recovery (Mean ± SD) | % RSD |
|---|---|---|---|---|---|
| 80 | 10.0 | 8.0 | 17.98 ± 0.21 | 99.78 ± 0.26 | 0.26 |
| 100 | 10.0 | 10.0 | 19.95 ± 0.18 | 99.75 ± 0.18 | 0.18 |
| 120 | 10.0 | 12.0 | 21.91 ± 0.25 | 99.59 ± 0.21 | 0.21 |
Acceptance Criteria and Statistical Analysis
For a method to be considered accurate, the mean recovery should typically be between 98.0% and 102.0% for the drug product. The % RSD for the recovery at each level should generally be less than 2%, demonstrating excellent repeatability and precision of the measurements [5] [57]. The data presented in Table 1, with recoveries consistently near 100% and low RSD values, confirms that the hypothetical method for paracetamol is accurate and that the tablet excipients do not interfere with the quantification.
Statistical comparison using a Student's t-test can be employed to show that there is no significant difference between the results obtained by the new method and those from a reference method or the labeled claim, further validating the method's accuracy [57].
The Scientist's Toolkit
Table 2: Essential research reagents and materials for recovery studies in UV-spectrophotometric analysis of paracetamol tablets.
| Item | Function/Justification |
|---|---|
| Paracetamol Certified Reference Standard | Serves as the primary benchmark for accuracy assessment, ensuring traceability and reliability of results. |
| Methanol (HPLC Grade) | Acts as a solvent for dissolving both standard and sample; its UV transparency minimizes background interference. |
| Volumetric Flasks | Used for precise preparation and dilution of standard and sample solutions to ensure accurate concentration. |
| Microbalance | Allows for accurate weighing of small quantities of standard and sample powder, which is critical for preparing precise stock solutions. |
| Ultrasonic Bath | Aids in the complete dissolution of the drug and the liberation of the API from the tablet matrix, ensuring a homogenous solution. |
| UV-Vis Spectrophotometer | The core instrument for measuring the absorbance of paracetamol at its λmax, enabling quantitative analysis. |
Troubleshooting and Best Practices
- Low Recovery Values: This can indicate incomplete extraction of the drug from the tablet matrix, degradation of the analyte, or interference from excipients that quench the absorbance. Re-optimize the extraction procedure (e.g., longer sonication time) and verify the stability of the standard and sample solutions [56].
- High Variability in Recovery (%RSD > 2%): This often points to issues with pipetting accuracy, incomplete mixing of solutions, or inhomogeneity of the tablet powder. Ensure proper calibration of volumetric equipment, use reverse pipetting for viscous solvents, and mix solutions thoroughly after each dilution step [5].
- Systematic Bias (Recovery consistently >102% or <98%): This suggests a potential calibration error or incorrect assignment of the reference standard's purity. Re-prepare standard solutions from fresh stock and verify the purity value of the standard.
In the development and validation of an analytical method for paracetamol tablet assay using UV-Vis spectrophotometry, demonstrating the method's precision is a critical requirement for regulatory acceptance and ensuring consistent, reliable product quality. Precision, defined as the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample, is not a single attribute but is evaluated at different levels to account for various sources of variability [59]. This document provides detailed application notes and protocols for evaluating two fundamental tiers of precision—repeatability and intermediate precision—specifically within the context of a thesis on UV-Vis spectrophotometric method development for paracetamol tablets, guiding researchers and drug development professionals in conducting these essential validation studies.
Conceptual Framework: Levels of Precision
Precision evaluation characterizes the random errors associated with a measurement procedure. The terminology used in method validation distinguishes between different conditions of measurement, primarily defined by the scope and sources of variation introduced during testing [60] [61].
Repeatability
Repeatability expresses the precision under a set of conditions where the same measurement procedure is performed by the same operators using the same measuring system in the same location over a short period of time [60] [62]. These are often termed "repeatability conditions" and represent the best-case scenario for precision, yielding the smallest possible variation in results [60]. In a practical laboratory setting, this typically translates to intra-day precision, where all analyses are conducted within a single analytical run or sequence [22].
Intermediate Precision
Intermediate precision (also referred to as within-laboratory precision) assesses the variability within a single laboratory over an extended period, typically several months [60] [63]. It is a more realistic measure of a method's performance under normal operating conditions because it incorporates the effects of expected, minor variations such as different analysts, different instruments, different batches of reagents or columns, and new calibrations [60] [59] [61]. The value of intermediate precision, expressed as a standard deviation, is invariably larger than that of repeatability because it accounts for more sources of random error [60].
Relationship to Reproducibility
While not the focus of this protocol, reproducibility represents the broadest measure of precision, defined as the precision between measurement results obtained in different laboratories [60] [63]. It is assessed during collaborative inter-laboratory studies and is crucial for methods intended for standardization or use across multiple sites [60]. The informal use of terms like "internal precision" and "external precision" is discouraged in favor of the standardized, internationally recognized definitions for repeatability, intermediate precision, and reproducibility [61].
Experimental Protocols
The following protocols are designed for the precision evaluation of a UV-Vis spectrophotometric method developed for the assay of paracetamol in tablet formulation, in alignment with ICH Q2(R1) guidelines.
Protocol for Repeatability (Intra-day Precision)
1. Principle: To assess the variability of the method when the analysis is performed under identical conditions within a short timeframe [62].
2. Materials and Reagents:
- Paracetamol reference standard
- Sample tablets of paracetamol
- Solvent (e.g., methanol, water as per the developed method)
- Volumetric flasks, pipettes, and other necessary glassware
3. Instrumentation: UV-Vis Spectrophotometer
4. Procedure: 1. Prepare a homogeneous sample solution from a powdered paracetamol tablet composite, ensuring it is within the linearity range of the method (e.g., a specific concentration such as 10 μg/mL) [22]. 2. Using the same spectrophotometer, the same analyst, and the same batch of reagents and solvents, prepare six independent sample preparations from this homogeneous powder blend [59]. 3. Analyze all six preparations in a single analytical sequence or within a very short period (e.g., one day or one run). 4. Record the absorbance values at the determined λmax for paracetamol (e.g., 249 nm) and calculate the corresponding assay values for each preparation [22].
5. Data Analysis: * Calculate the mean, standard deviation (SD), and relative standard deviation (RSD %) of the six assay results. * The RSD is the primary metric for repeatability, calculated as: RSD (%) = (Standard Deviation / Mean) × 100.
Protocol for Intermediate Precision
1. Principle: To evaluate the impact of normal, within-laboratory variations on the analytical results of the paracetamol assay over an extended period [63].
2. Experimental Design: A nested design involving two analysts over two different days is recommended to effectively capture the sources of variability [59].
3. Procedure: 1. Day 1, Analyst 1: Prepare and analyze six independent sample preparations of the paracetamol tablet composite as per the method. Record the assay results. 2. Day 2, Analyst 2: A second analyst independently performs the same procedure on a different day. This analyst should use a different spectrophotometer (if available), prepare their own standard and reagent solutions, and potentially use a different lot of solvents [59]. 3. In total, twelve determinations are generated (six from each analyst/day combination).
4. Data Analysis: * Calculate the mean, SD, and RSD for the entire set of twelve results. This RSD represents the intermediate precision of the method [59]. * Statistically compare the mean values obtained by the two analysts using a Student's t-test to determine if there is a significant difference between the operators [59].
Data Presentation and Acceptance Criteria
The data generated from the precision studies should be summarized clearly. The following tables provide templates for data presentation and typical acceptance criteria as per ICH guidelines for assay validation.
Table 1: Example Data Table for Repeatability Study of Paracetamol Assay
| Replicate Number | Analyst 1 (Day 1) Assay (%) |
|---|---|
| 1 | 99.5 |
| 2 | 100.2 |
| 3 | 99.8 |
| 4 | 100.5 |
| 5 | 99.3 |
| 6 | 100.1 |
| Mean | 99.9 |
| SD | 0.45 |
| RSD (%) | 0.45 |
Table 2: Example Data Table for Intermediate Precision Study of Paracetamol Assay
| Replicate Number | Analyst 1 (Day 1) Assay (%) | Analyst 2 (Day 2) Assay (%) |
|---|---|---|
| 1 | 99.5 | 98.8 |
| 2 | 100.2 | 99.5 |
| 3 | 99.8 | 100.2 |
| 4 | 100.5 | 99.0 |
| 5 | 99.3 | 100.5 |
| 6 | 100.1 | 99.7 |
| Mean | 99.9 | 99.6 |
| Overall SD | 0.52 | |
| Overall RSD (%) | 0.52 |
Table 3: Typical Acceptance Criteria for Precision of an Assay Method
| Precision Level | Acceptance Criterion (RSD %) | Reference Guideline |
|---|---|---|
| Repeatability | Typically ≤ 1.0% | ICH Q2(R1) [22] |
| Intermediate Precision | Typically ≤ 2.0% | ICH Q2(R1) [22] |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents required for the successful execution of precision studies in UV-Vis spectrophotometric analysis of paracetamol.
Table 4: Essential Reagents and Materials for Paracetamol UV-Vis Spectrophotometry
| Item | Function / Explanation |
|---|---|
| Paracetamol Reference Standard | Highly purified material used to prepare calibration standards, providing the benchmark for accuracy and quantification. |
| Methanol (HPLC/AR Grade) | Common solvent used to dissolve paracetamol and prepare sample and standard solutions; must be UV-grade for low background noise [22]. |
| Pharmaceutical Tablet Formulation | The actual drug product (e.g., 500 mg paracetamol tablet) used to prepare the sample solution for assay determination. |
| Volumetric Flasks | For accurate preparation and dilution of standard and sample solutions to ensure precise concentration. |
| UV-Vis Cuvettes | Matched quartz cells that hold the sample solution in the light path of the spectrophotometer. |
| Analytical Balance | For accurate weighing of the reference standard and powdered tablet sample. |
| Syringe Filters (0.45 μm) | For filtration of sample solutions to remove particulate matter from the tablet excipients, ensuring clear solutions and reproducible absorbance readings [22]. |
Workflow and Logical Relationships
The entire process of precision evaluation, from conceptualization to data interpretation, can be visualized in the following workflow. This diagram outlines the logical sequence of steps and decision points for establishing method precision.
High-Performance Liquid Chromatography (HPLC) stands as a cornerstone analytical technique in pharmaceutical analysis, representing a dominant force with "mature" technologies that have been widely practiced for five decades [64]. This application note frames the role of HPLC within a broader thesis research context focused on method development for paracetamol tablet analysis using UV-Vis spectrophotometry. For researchers and drug development professionals, understanding the comparative advantages and limitations of HPLC provides essential context for selecting appropriate analytical techniques for pharmaceutical formulation analysis, particularly for common medications like paracetamol.
The versatility of HPLC is evidenced by its widespread adoption across diverse analytical scenarios. More than $4 billion of HPLC equipment, columns, and accessories were sold worldwide in 2012 alone, demonstrating its entrenched position in analytical laboratories [64]. While UV-Vis spectrophotometry offers simplicity and cost-effectiveness for certain paracetamol applications, HPLC provides a powerful complementary technique with superior separation capabilities and specificity, especially for complex matrices and multi-component formulations.
Advantages of HPLC in Pharmaceutical Analysis
Technical Superiority and Versatility
The dominance of HPLC as a premier analytical technique is no accident, deriving from several prominent advantages that render it indispensable for pharmaceutical analysis [64]. Its most significant advantage lies in its exceptional applicability to diverse analyte types, from small organic molecules like paracetamol to large biomolecules and polymers. This versatility enables method development for a wide spectrum of pharmaceutical compounds without fundamental technique limitations.
The successful coupling of HPLC to mass spectrometry (MS) has provided an invincible edge—creating what many consider "the perfect analytical tool" that combines excellent separation capability with the unsurpassed sensitivity and specificity of MS [64]. HPLC-MS is rapidly becoming the standard platform technology for bioanalytical testing, trace analysis for residues, and life science research. For paracetamol analysis, this enables not only quantification but also structural identification of degradants and metabolites.
HPLC delivers exceptional precision and robustness, making it indispensable for quality control applications. In pharmaceutical stability studies, HPLC can quantitatively track all components (API and all related substances, including isomers) with very precise retention times and peak areas (typically <0.1% RSD for UHPLC) [64]. This precision is crucial for establishing shelf lives and storage conditions for active pharmaceutical ingredients and drug products, as demonstrated in stability studies monitoring paracetamol degradants under various storage conditions.
Application-Specific Advantages for Paracetamol Analysis
For paracetamol-specific analysis, HPLC methods demonstrate particular strengths in several domains. A simple, robust HPLC method for serum paracetamol determination demonstrated excellent precision (better than CV 5% at both micromolar and millimolar concentrations) and recovery exceeding 96% without interference from other drugs, metabolites, or dietary constituents [65]. This performance across therapeutic and overdose concentration ranges highlights the reliability of HPLC for clinical monitoring.
In complex formulations containing paracetamol combined with other active ingredients, HPLC provides simultaneous quantification capabilities. Research has demonstrated successful development of RP-HPLC methods for analyzing paracetamol in combination with caffeine and tramadol in pharmaceutical formulations, with LODs of 0.2 μg/mL, 0.1 μg/mL, and 0.3 μg/mL for paracetamol, caffeine, and tramadol hydrochloride, respectively [66]. The linear concentration ranges of 0.8–270 μg/mL for paracetamol, 0.4–250 μg/mL for caffeine, and 1.0–300 μg/mL for tramadol demonstrate the wide dynamic range achievable [66].
HPLC further excels at analyzing paracetamol in challenging dosage forms with significant ratio disparities, such as Comtrex tablets containing paracetamol, pseudoephedrine, and brompheniramine in a 250:15:1 ratio [67]. The ability to resolve and quantify components at such concentration differences underscores the power of HPLC for complex formulation analysis.
Limitations and Challenges of HPLC
Technical and Practical Limitations
Despite its numerous advantages, HPLC exhibits several limitations that researchers must consider during method development and technique selection. These "perceived limitations," as they're often termed, have been mitigated by recent advances but remain practical considerations for analytical planning [64].
The lack of a truly universal detector for HPLC is frequently mentioned, though UV-Vis detectors approach universality for chromophoric compounds [64]. While refractive index detection provides broader applicability, it suffers from low sensitivity and incompatibility with gradient elution. Mass spectrometry is evolving toward universal detection for ionic or ionizable compounds but remains cost-prohibitive for many laboratories. This limitation is particularly relevant when comparing HPLC to UV-Vis spectrophotometry, which provides direct detection for compounds with chromophores like paracetamol.
HPLC traditionally offers less separation efficiency than capillary gas chromatography, with conventional HPLC having a practical peak capacity of approximately 200 using columns with ~20,000 plates under gradient conditions [64]. This limited peak capacity can prove insufficient for very complex samples. However, the advent of UHPLC has extended peak capacity to the 400–1000 range within approximately 60 minutes, with two-dimensional LC further increasing separation power for comprehensive analysis of highly complex samples in proteomics and metabonomics [64].
The technique can be relatively difficult for novices due to the bewildering array of HPLC modules, columns, mobile phases, and operating parameters [64]. While modern systems with single-point control via data systems have simplified operation of existing methods, substantial experience and scientific judgment remain necessary to develop new methods, interpret anomalous results, or troubleshoot problems.
HPLC analysis can be arduous, particularly for regulated testing under good manufacturing practices (GMP) [64]. The multiple steps—weighing reference standards, preparing samples and mobile phases, setting up the column and modules, performing system suitability testing, injecting standards for calibration followed by sample analysis, peak integration, reporting, and review with sign-offs—create a time-intensive process. Fortunately, automation of most steps for routine testing has improved reproducibility and efficiency.
Resource and Application Limitations
From a practical implementation perspective, HPLC presents several resource-related challenges that may influence technique selection for paracetamol analysis.
The significant solvent consumption creates both economic and environmental concerns [68]. HPLC typically involves higher solvent use compared to techniques like GC, resulting in higher operational costs and waste disposal considerations. This contrasts with UV-Vis spectrophotometry, which generally requires minimal solvent consumption per analysis.
HPLC demonstrates limited suitability for volatile compounds, where gas chromatography may prove superior [68]. While HPLC excels for non-volatile, polar, and thermally unstable compounds like paracetamol, its application to volatile analytes remains challenging without derivatization.
The technique can be time-consuming for method development, requiring optimization of multiple parameters including mobile phase composition, pH, buffer concentration, flow rate, and column temperature [66]. For paracetamol analysis, researchers must optimize these parameters to achieve adequate separation from excipients, degradants, and other API components in formulations.
Comparative Technical Data
Table 1: Performance Comparison of HPLC with Alternative Techniques for Paracetamol Analysis
| Parameter | HPLC | UV-Vis Spectrophotometry | GC-MS |
|---|---|---|---|
| Precision (RSD) | <0.1-5% [64] [65] | 1-3% (typical) | 0.5-2% |
| Detection Limit for Paracetamol | 0.2 μg/mL [66] | 0.26 μg/mL [20] | 0.1 μg/mL |
| Linear Range for Paracetamol | 0.8-270 μg/mL [66] | 5-25 μg/mL [20] | 1-500 μg/mL |
| Analysis Time | 10-30 minutes | 1-5 minutes | 5-15 minutes |
| Separation Capability | Excellent | Poor | Good |
| Specificity | High | Moderate | High |
| Equipment Cost | High | Low | High |
| Solvent Consumption | High | Low | Low |
Table 2: HPLC Performance for Paracetamol in Combination Formulations
| Drug Combination | HPLC Column | Mobile Phase | LOD/LOQ | Application |
|---|---|---|---|---|
| Paracetamol, Caffeine, Tramadol [66] | C18 | Methanol/Phosphate | 0.2/0.8 μg/mL (PAR) | Pharmaceutical formulations |
| Paracetamol, Pseudoephedrine, Brompheniramine [67] | Zorbax SB-C18 | Water:Acetonitrile (75:25, v/v; pH 3.2) | Not specified | Comtrex tablets |
| Paracetamol, Nabumetone [20] | C18 | Methanol/Phosphate | 0.26/0.79 μg/mL (PAR) | Bulk and tablet dosage forms |
Experimental Protocols
Standard HPLC Protocol for Paracetamol Analysis in Tablets
Scope and Application: This protocol describes a reversed-phase HPLC method for the determination of paracetamol in tablet formulations, suitable for quality control testing and stability studies.
Materials and Equipment:
- HPLC system with UV detector
- C18 column (150 × 4.6 mm, 5 μm)
- Paracetamol reference standard
- Methanol (HPLC grade)
- Water (HPLC grade)
- Phosphoric acid
- Ultrasonic bath
- Analytical balance
Mobile Phase Preparation: Prepare a mixture of water and methanol in the ratio 75:25 (v/v). Adjust pH to 3.2 using phosphoric acid. Filter through a 0.45 μm membrane filter and degas by sonication for 10 minutes.
Standard Solution Preparation: Accurately weigh 25 mg of paracetamol reference standard and transfer to a 25 mL volumetric flask. Dissolve in and dilute to volume with mobile phase to obtain a stock solution of 1 mg/mL. Dilute further to prepare working standards in the range of 5-50 μg/mL.
Sample Solution Preparation: Weigh and powder 20 tablets. Transfer an accurately weighed portion of the powder equivalent to 50 mg of paracetamol to a 50 mL volumetric flask. Add 30 mL of mobile phase, sonicate for 15 minutes with occasional shaking, and dilute to volume with mobile phase. Filter through a 0.45 μm membrane filter, discarding the first 5 mL of filtrate.
Chromatographic Conditions:
- Column: C18 (150 × 4.6 mm, 5 μm)
- Mobile phase: Water:methanol (75:25, v/v; pH 3.2)
- Flow rate: 1.0 mL/min
- Detection wavelength: 243 nm
- Injection volume: 20 μL
- Column temperature: Ambient
System Suitability: The relative standard deviation for replicate injections of standard solution should not be more than 2.0%. The tailing factor for paracetamol peak should not be more than 2.0. The theoretical plates should not be less than 2000.
Stability-Indicating Method for Paracetamol
Purpose: This protocol describes an HPLC method for simultaneous determination of paracetamol and its degradants in stability samples.
Materials and Equipment: UHPLC system with PDA detector, C18 column (100 mm × 3.0 mm, 2-μm), ammonium formate, formic acid, acetonitrile (HPLC grade)
Mobile Phase Preparation:
- Mobile phase A: 20 mM ammonium formate (pH 3.7)
- Mobile phase B: 0.05% formic acid in acetonitrile
Chromatographic Conditions [64]:
- Column: 100 mm × 3.0 mm, 2-μm dp C18
- Flow rate: 0.8 mL/min
- Temperature: 40°C
- Gradient program:
- 5-15% B in 2 min
- 15-40% B in 10 min
- 40-90% B in 1 min
- Detection: UV absorbance at 280 nm
- Injection volume: 3 μL
Sample Preparation: Place not less than 20 tablets in a suitable volumetric flask. Add approximately 70% of the diluent (20% acetonitrile in 0.1 N HCl), sonicate for 30 minutes with occasional shaking, and dilute to volume. Centrifuge a portion of the solution and use the supernatant for analysis.
Visualization of HPLC Analysis Workflow
Diagram 1: HPLC Analysis Workflow for Paracetamol Tablets. This diagram illustrates the sequential steps involved in HPLC analysis of paracetamol tablets, from sample preparation to final reporting.
Diagram 2: Decision Framework: HPLC vs. UV-Vis for Paracetamol Analysis. This diagram compares the advantages and limitations of HPLC and UV-Vis spectrophotometry for paracetamol analysis, providing a decision framework for technique selection.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for HPLC Analysis of Paracetamol
| Reagent/Material | Specification | Function in Analysis |
|---|---|---|
| C18 Column | 150 × 4.6 mm, 5 μm particle size | Stationary phase for reverse-phase separation of paracetamol from excipients and degradants |
| Methanol | HPLC grade | Organic modifier in mobile phase to control retention and separation efficiency |
| Water | HPLC grade | Aqueous component of mobile phase; solvent for standard and sample preparation |
| Paracetamol Reference Standard | Pharmacopoeial grade (USP/BP) | Primary standard for calibration curve generation and method validation |
| Ammonium Formate | Analytical grade | Buffer component for mobile phase to control pH and improve peak shape |
| Formic Acid | HPLC grade | Mobile phase additive to improve ionization in MS detection and control pH |
| Phosphoric Acid | Analytical grade | Mobile phase pH adjustment for optimal separation and peak symmetry |
| Membrane Filters | 0.45 μm porosity | Filtration of mobile phase and sample solutions to remove particulate matter |
HPLC remains an indispensable technique in the pharmaceutical analyst's arsenal, offering distinct advantages for paracetamol analysis including exceptional specificity, precision, and the ability to simultaneously quantify multiple components in complex formulations. The technique's limitations—including solvent consumption, operational complexity, and equipment costs—must be balanced against its superior performance characteristics.
For researchers developing UV-Vis spectrophotometric methods for paracetamol tablets, HPLC provides a powerful reference methodology for method validation and comparative studies. The decision to employ HPLC versus alternative techniques like UV-Vis spectrophotometry should be guided by the specific analytical requirements, including the need for separation capability, specificity, precision, and regulatory compliance.
Understanding the comparative advantages and limitations of HPLC enables researchers to make informed decisions about technique selection and method development strategy for paracetamol analysis, ultimately supporting the development of robust, reliable analytical methods for pharmaceutical quality control.
Conclusion
UV-Visible spectrophotometry remains a vital analytical technique for paracetamol tablet analysis, offering an optimal balance of accuracy, cost-effectiveness, and operational simplicity. The development of advanced signal processing and chemometric methods has significantly enhanced its capability to resolve complex spectral overlaps in multicomponent formulations, making it statistically comparable to HPLC for routine quality control. Future directions should focus on integrating greener solvent systems, expanding chemometric applications for dissolution testing, and developing automated spectrophotometric workflows to support the growing demand for sustainable pharmaceutical analysis. The continued evolution of these methodologies will further strengthen their role in ensuring drug quality and supporting clinical research endeavors.
References
- 1. The Beer-Lambert Law [https://chem.libretexts.org/Bookshelves/Physical_and_Theoretical_Chemistry_Textbook_Maps/Supplemental_Modules_(Physical_and_Theoretical_Chemistry)/Spectroscopy/Electronic_Spectroscopy/Electronic_Spectroscopy_Basics/The_Beer-Lambert_Law]
- 2. Beer-Lambert Law | Transmittance & Absorbance [https://www.edinst.com/resource/the-beer-lambert-law/]
- 3. Shining a Light on Spectrophotometry: Principles, Practices ... [https://sperdirect.com/blogs/news/shining-a-light-on-spectrophotometry-principles-practices-and-real-world-applications?srsltid=AfmBOooHha39uKtpFqkpMsKsGSy2lVnfYySF0StCl67pGMfFpNzmrQew]
- 4. Simultaneous UV Spectrophotometric Analysis of Paracetamol ... [https://www.ijrpas.com/AbstractView.aspx?PID=2025-4-4-13]
- 5. Development and validation of the UV-spectrophotometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658052/]
- 6. Spectrophotometric determination of paracetamol in pure ... [https://pubmed.ncbi.nlm.nih.gov/2484999/]
- 7. UV Spectrophotometric Simultaneous Determination of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3950367/]
- 8. RP-HPLC and UV Spectrophotometric Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7031732/]
- 9. The Bouguer‐Beer‐Lambert Law: Shining Light on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7540309/]
- 10. Analytical Techniques for the Determination of Paracetamol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328053/]
- 11. Development and Validation of A UV Spectroscopic ... [http://www.orientjchem.org/vol29no2/development-and-validation-of-a-uv-spectroscopic-method-for-analysis-of-paracetamol-in-bulk-powder-and-tablet/]
- 12. Method development and validation of paracetamol in bulk ... [https://wjpsonline.com/index.php/wjps/article/view/paracetamol-uv-visible-spectroscopy]
- 13. Simultaneous UV Spectrophotometric Analysis of ... [https://ijrpas.com/HTMLPaper.aspx?Journal=International%20Journal%20of%20Research%20in%20Pharmacy%20and%20Allied%20Science;PID=2025-4-4-13]
- 14. Three-way analysis of pH-UV absorbance dataset for the ... [https://www.sciencedirect.com/science/article/abs/pii/S1386142520300263]
- 15. Simple spectrophotometric methods for the quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560461/]
- 16. Simultaneous UV Spectrophotometric Analysis of Paracetamol ... [https://ijrpas.com/AbstractView.aspx?PID=2025-4-4-13]
- 17. Analysis of paracetamol and caffeine contents in tablet ... [https://journal-jps.com/new/index.php/jps/article/view/489?articlesBySameAuthorPage=3]
- 18. UV-Visible Spectrophotometric Method Development and ... [https://www.omicsonline.org/uv-visible-spectrophotometric-method-development-and-validation-of-assay-of-paracetamol-tablet-formulation-2155-9872.1000151.php?aid=9714]
- 19. Development and validation of spectrophotometric method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658093/]
- 20. UV-visible spectrophotometric simultaneous estimation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658063/]
- 21. Development and validation of an ultraviolet-visible ... [https://www.frontiersin.org/journals/analytical-science/articles/10.3389/frans.2023.1066348/full]
- 22. Development and Validation of UV-Visible Spectrophotometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3848213/]
- 23. Baseline Correction | Technical Note 119 [https://www.denovix.com/tn-119-baseline-correction/]
- 24. Application of continuous wavelet transforms for ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224124021729]
- 25. First-order derivative spectrophotometric method for ... [https://www.sciencedirect.com/science/article/pii/S2772577424000077]
- 26. Wavelet Transform-Based UV Spectroscopy for ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2018.00503/full]
- 27. Development and Validation of Analytical Method for ... [https://www.semanticscholar.org/paper/Development-and-Validation-of-Analytical-Method-for/b4017d117eab2f7076a7ae7cd29133a8aec78f0b]
- 28. Optimization of wavelength range and data interval in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762457/]
- 29. The equivalence of partial least squares and principal ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743915002737]
- 30. A comparative study between PCR and PLS in ... [https://www.sciencedirect.com/science/article/pii/S1386142506005348]
- 31. UV-VISIBLE SPECTROPHOTOMETRIC METHOD ... [https://ijpsr.com/bft-article/uv-visible-spectrophotometric-method-development-and-validation-of-assay-of-paracetamol-tablet-formulation/]
- 32. Application of smart chemometric models for spectra ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-024-01148-9]
- 33. A brief Review on Q-absorption Ratio Method in UV- ... [https://ajpaonline.com/AbstractView.aspx?PID=2022-12-4-11]
- 34. DEVELOPMENT AND VALIDATION OF UV ... [https://ijpsr.com/bft-article/development-and-validation-of-uv-spectroscopic-methods-for-simultaneous-estimation-of-paracetamol-and-zaltoprofen-in-bulk-and-tablet-formulation/]
- 35. Two chromatographic methods for analyzing paracetamol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11791058/]
- 36. Curve Fitting B: Multicomponent Spectroscopy [https://terpconnect.umd.edu/~toh/spectrum/CurveFittingB.html]
- 37. Univariate and multivariate signal processing ... [https://www.nature.com/articles/s41598-025-22700-0]
- 38. Validation of a spectrophotometric method for the ... [https://www.sciencedirect.com/science/article/pii/S235200782030055X]
- 39. UV-VISIBLE SPECTROPHOTOMETRIC METHOD DEVELOPMENT AND VALIDATION OF ASSAY OF PARACETAMOL TABLET FORMULATION | INTERNATIONAL JOURNAL OF PHARMACEUTICAL SCIENCES AND RESEARCH [https://ijpsr.com/bft-article/uv-visible-spectrophotometric-method-development-and-validation-of-assay-of-paracetamol-tablet-formulation/?view=fulltext]
- 40. UV Spectrophotometric Method Development and Validation for Quantitative Estimation of Paracetamol | PDF [https://www.slideshare.net/slideshow/uv-spectrophotometric-method-development-and-validation-for-quantitative-estimation-of-paracetamol/80549904]
- 41. Development and Validation of A UV Spectroscopic Method for Analysis of Paracetamol in Bulk Powder and Tablet : Oriental Journal of Chemistry [https://www.orientjchem.org/vol29no2/development-and-validation-of-a-uv-spectroscopic-method-for-analysis-of-paracetamol-in-bulk-powder-and-tablet/]
- 42. International Journal of Research in Pharmacy and Allied Science-Simultaneous UV Spectrophotometric Analysis of Paracetamol and Ibuprofen in an Ethanol–NaoH Solvent System [https://ijrpas.com/HTMLPaper.aspx?Journal=International+Journal+of+Research+in+Pharmacy+and+Allied+Science%3BPID%3D2025-4-4-13]
- 43. Simultaneous quantification of Ibuprofen and Paracetamol in combined tablet formulations by UV–VIS spectrophotometry and chemometric modelling - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S3050475925004294]
- 44. Development and validation of UV-Visible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658078/]
- 45. Matrix (chemical analysis) [https://en.wikipedia.org/wiki/Matrix_(chemical_analysis)]
- 46. 6.4B: Accounting for Matrix Effects [https://chem.libretexts.org/Bookshelves/Analytical_Chemistry/Molecular_and_Atomic_Spectroscopy_(Wenzel)/6%3A_Atomic_Spectroscopy/6.4%3A_Other_Considerations/6.4B%3A_Accounting_for_Matrix_Effects]
- 47. 4.4: UV-Visible Spectroscopy [https://chem.libretexts.org/Bookshelves/Analytical_Chemistry/Physical_Methods_in_Chemistry_and_Nano_Science_(Barron)/04%3A_Chemical_Speciation/4.04%3A_UV-Visible_Spectroscopy]
- 48. Construction of calibration curve for uv-spectroscopic ... [https://www.slideshare.net/slideshow/construction-of-calibration-curve-for-uvspectroscopic-analysis-of-paracetamol/60290152]
- 49. Understanding the ich ( Q ) 2 R 1 guideline [https://www.linkedin.com/pulse/understanding-ich-q2r1-guideline-priyadarshana-asolkar-cipgc]
- 50. ( ICH ) Validation of Analytical Procedures: Text and Methodology... Q 2 R 1 [https://www.gmp-compliance.org/guidelines/gmp-guideline/ich-q2r1-validation-of-analytical-procedures-text-and-methodology]
- 51. Understanding ICH ( Q ): Validation of Analytical Procedures in the... 2 R 1 [https://iampharmacist.com/2025/05/31/ich-q2r1/]
- 52. ( ICH 2) Validation of analytical procedures - Scientific Q 2 R guideline [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 53. UV-Visible Spectrophotometry ( UV - Vis ) – Analytical Method [https://sgsystemsglobal.com/glossary/uv-visible-spectrophotometry-uv-vis/]
- 54. UV-Vis Spectroscopy: Principle, Strengths and Limitations ... [https://www.technologynetworks.com/analysis/articles/uv-vis-spectroscopy-principle-strengths-and-limitations-and-applications-349865]
- 55. linearity of UV detector issue [http://www.chromforum.org/viewtopic.php?t=12521]
- 56. Diacerein | UV-Spectrophotometer | Recovery | Accuracy [https://www.ijpsonline.com/articles/development-and-validation-of-a-uv-spectrophotometric-method-for-determination-of-diacerein-in-bulk-and-a-capsule-dosage-form-3594.html?view=mobile]
- 57. Simple spectrophotometric methods for the determination ... [https://e-jghs.org/DOIx.php?id=10.35500/jghs.2025.7.e4]
- 58. Spectrophotometric quantification of paracetamol and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10387862/]
- 59. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 60. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 61. Precision [https://www.geoanalyst.org/precision/]
- 62. Conditions of measurement - Precision [https://analyse-it.com/docs/user-guide/measurement-systems-analysis/precision/measurement-conditions]
- 63. Difference Between Reproducibility And Intermediate ... [https://pharmaguru.co/difference-between-reproducibility-and-intermediate-precision-in-analytical-method-validation/]
- 64. The Essence of Modern HPLC : Advantages , Limitations ... [https://www.chromatographyonline.com/view/essence-modern-hplc-advantages-limitations-fundamentals-and-opportunities]
- 65. Paracetamol (acetaminophen) analysis by high ... [https://pubmed.ncbi.nlm.nih.gov/3961897/]
- 66. Development and Validation of an RP-HPLC-PDA Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156741/]
- 67. Analytical methods for the determination of paracetamol ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-019-0595-6]
- 68. vs GC: Choosing the Right HPLC ... | Lab Manager Chromatography [https://www.labmanager.com/hplc-vs-gc-choosing-the-right-chromatography-technique-33689]