Analytical Method Transfer Protocol: A Comprehensive Guide for Seamless Laboratory Transitions
This article provides a complete guide to analytical method transfer (AMT) for researchers, scientists, and drug development professionals.
Analytical Method Transfer Protocol: A Comprehensive Guide for Seamless Laboratory Transitions
Abstract
This article provides a complete guide to analytical method transfer (AMT) for researchers, scientists, and drug development professionals. It covers the foundational principles of AMT, detailing its importance in regulatory compliance and product quality assurance. The guide explores methodological approaches like comparative testing and co-validation, offers strategies for troubleshooting common pitfalls, and outlines the validation process to demonstrate equivalence between laboratories. By synthesizing best practices from regulatory guidelines and industry experts, this resource aims to equip professionals with the knowledge to execute efficient, compliant, and successful method transfers.
Understanding Analytical Method Transfer: The Foundation of Equivalence
Analytical Method Transfer (AMT) represents a critical, documented process within the pharmaceutical and biotechnology industries that qualifies a receiving laboratory to execute an analytical testing procedure that originated in a transferring laboratory. This formal process ensures that the receiving unit possesses the necessary procedural knowledge, technical capability, and instrumentation to perform the analytical method as intended, thereby guaranteeing that test results are equivalent to those generated by the original laboratory [1] [2]. As regulatory agencies mandate this transfer to ensure the consistency and quality of pharmaceuticals [1], AMT forms an indispensable component of technology transfers, whether for changes in production sites, outsourcing of testing activities, or multi-site operations [3] [4]. This guide objectively examines the core methodologies, experimental protocols, and comparative performance of different transfer approaches, providing researchers and drug development professionals with a structured framework for implementing robust AMT protocols.
Analytical Method Transfer is fundamentally a quality assurance process that establishes documented evidence that an analytical procedure performs equivalently in the receiving laboratory as it does in the originating laboratory [2] [5]. The ultimate purpose of any newly developed and validated method is its reliable application in Quality Control laboratories for the release of Active Pharmaceutical Ingredients (APIs) and finished products, making its successful transfer paramount [1]. The process is governed by regulatory guidelines, including United States Pharmacopeia (USP) General Chapter 〈1224〉, and requires meticulous documentation that can be audited by regulatory agencies [1] [6].
The necessity for AMT arises in various scenarios, including multi-site operations within the same company, transfer to or from Contract Research/Manufacturing Organizations (CROs/CMOs), implementation on new equipment or technology platforms, and rollout of method improvements or optimizations [4]. At its core, AMT demonstrates "equivalence" or "comparability" between laboratories, ensuring that the method's critical performance characteristics—accuracy, precision, specificity, linearity, range, detection limit, quantitation limit, and robustness—remain consistent across both sites [4].
Core Methodologies in Analytical Method Transfer
The search results reveal four primary, recognized methodologies for conducting Analytical Method Transfer. The selection of an appropriate methodology depends on factors such as the method's complexity, its regulatory status, the experience of the receiving laboratory, and the overall risk assessment [1] [3] [4].
Comparative Testing
Comparative Testing is the most frequently employed transfer approach [1] [3] [5]. This methodology requires both the transferring (sending) and receiving laboratories to analyze a predetermined number of samples from the same homogeneous lot [1] [7]. The experimental design typically involves multiple analysts, instruments, and days to establish intermediate precision. The results from both laboratories are statistically compared against pre-defined acceptance criteria to demonstrate equivalence [4]. This approach is particularly suitable for well-established, validated methods where both laboratories share similar equipment and expertise [4].
Co-validation
Co-validation, or joint validation, occurs when the receiving laboratory participates in the initial validation of the analytical method [1] [3]. In this model, the receiving unit acts as part of the validation team, specifically performing the intermediate precision (reproducibility) experiments that generate data for assessing inter-laboratory variability [3] [5]. This approach is highly efficient for methods developed specifically for multi-site use or when transfer occurs before the analytical method has been fully validated [3]. The acceptance criteria are defined within the validation protocol itself, based on product specifications and the method's intended purpose [3].
Revalidation or Partial Revalidation
Revalidation involves the receiving laboratory performing a complete or partial repetition of the original method validation [1] [2]. This approach is beneficial when the transferring laboratory is unavailable for comparative testing, when the original validation did not comply with ICH requirements, or when the method is being transferred to a laboratory with significantly different equipment, personnel, or environmental conditions [3] [4]. For partial revalidation, only the parameters anticipated to be most affected by the transfer—typically accuracy and precision—are evaluated [1] [3].
Transfer Waiver
A Transfer Waiver is a justified omission of the formal transfer process [1] [2]. This option is applicable only in specific, well-documented circumstances where the risk of failure is negligible. Justifications for a waiver include the use of pharmacopoeial methods (which require verification but not formal transfer), transfer of a method for a new product strength with comparable composition and methodology, transfer of a general method (e.g., visual inspection, weighing), or when personnel responsible for the method's development or validation move to the receiving unit [3] [2] [6]. This approach requires robust scientific justification and documented risk assessment, as it receives high regulatory scrutiny [4].
Table 1: Comparative Analysis of Analytical Method Transfer Types
| Transfer Type | Experimental Design | Best Suited For | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Comparative Testing | Both labs analyze identical samples; results statistically compared [4]. | Established, validated methods; similar lab capabilities [4]. | Direct comparison provides strong evidence of equivalence; most recognized path [3]. | Requires careful sample preparation and handling; dependent on statistical analysis [4]. |
| Co-validation | Method validation and transfer occur simultaneously; receiving lab performs intermediate precision [3] [5]. | New methods; methods developed for multi-site use [4]. | Highly efficient; builds inter-laboratory consistency from the outset [3]. | Requires high collaboration and harmonized protocols; tight coordination needed [4]. |
| Revalidation | Receiving lab performs full or partial validation of the method [2] [4]. | Significant differences in lab conditions/equipment; substantial method changes [4]. | Most rigorous approach; demonstrates receiving lab's independent capability [4]. | Resource-intensive; essentially repeats original validation work [4]. |
| Transfer Waiver | No comparative testing performed [2]. | Highly experienced receiving lab; identical conditions; simple, robust methods [4]. | Saves significant time and resources; efficient for low-risk scenarios [2]. | Rarely applicable; requires strong scientific and risk justification [4]. |
Experimental Protocol and Workflow
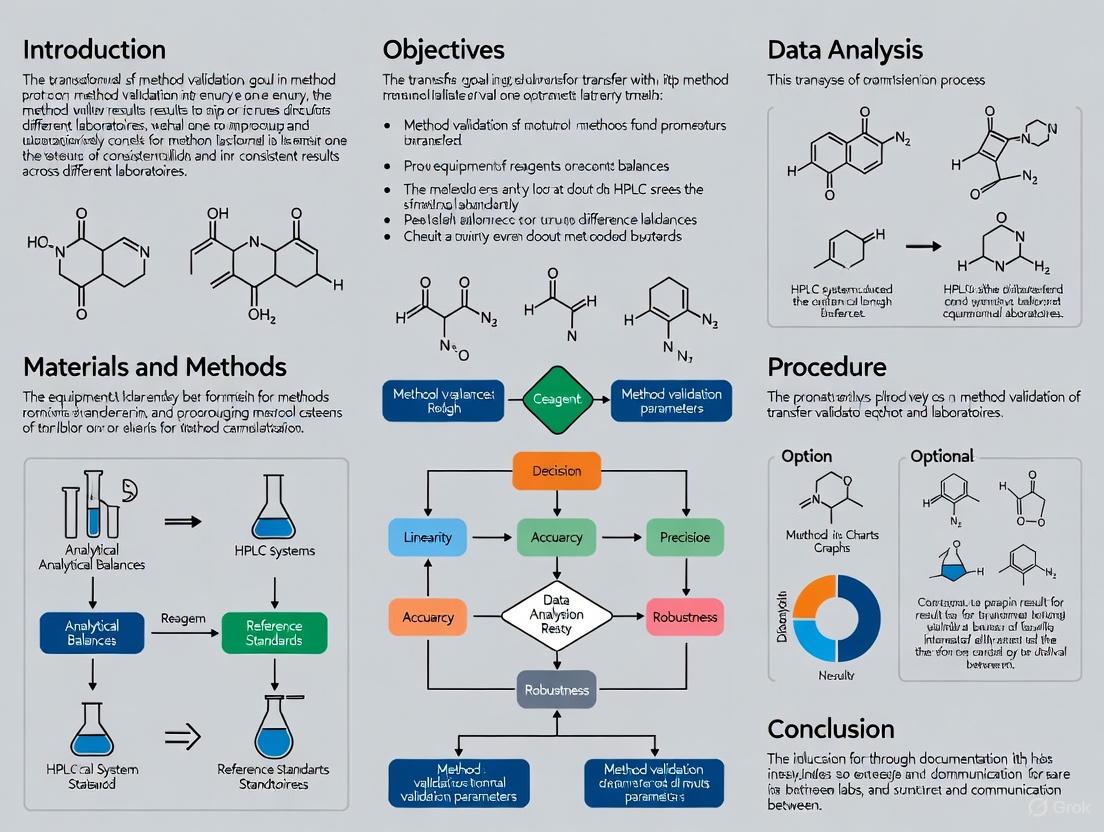
A successful Analytical Method Transfer follows a structured, phased workflow that ensures regulatory compliance and operational success. The following diagram illustrates the comprehensive, multi-stage process from initial assessment through final reporting and ongoing monitoring.
Diagram 1: Analytical Method Transfer Workflow
Phase 1: Pre-Transfer Planning and Assessment
The initial phase focuses on comprehensive preparation, which is crucial for the transfer's success [8].
- Define Scope & Objectives: Clearly articulate why the method is being transferred and define specific, measurable success criteria [4] [8].
- Form Cross-Functional Teams: Designate leads and team members from both transferring and receiving labs, including representatives from Analytical Development, QA/QC, and Operations [4] [8].
- Gather Method Documentation: Collect all relevant method validation reports, development reports, current Standard Operating Procedures (SOPs), raw data, and instrument specifications from the transferring lab [4] [8].
- Conduct Gap Analysis: Compare equipment, reagents, software, environmental conditions, and personnel expertise between the two labs to identify potential discrepancies [3] [4].
- Perform Risk Assessment: Identify potential challenges (e.g., complex method, unique equipment, inexperienced personnel) and develop appropriate mitigation strategies [1] [4].
- Select Transfer Approach: Based on the risk assessment and method characteristics, choose the most appropriate transfer methodology (Comparative Testing, Co-validation, Revalidation, or Waiver) [4].
- Develop Detailed Transfer Protocol: Create a comprehensive protocol specifying method details, responsibilities, materials, equipment, sample preparation, analytical procedure, acceptance criteria, statistical analysis plan, and deviation handling process [1] [3] [4].
- Secure Management Approval: Obtain formal approval for the transfer protocol from all relevant stakeholders, including Quality Assurance [4].
Phase 2: Execution and Data Generation
This phase involves the hands-on implementation of the approved transfer protocol.
- Personnel Training: Ensure receiving lab analysts are thoroughly trained by transferring lab personnel, with all training sessions formally documented [1] [4] [6].
- Equipment Readiness: Verify that all necessary equipment at the receiving lab is properly qualified, calibrated, and maintained according to established schedules [2] [4].
- Sample Preparation & Distribution: Prepare and characterize homogeneous, representative samples (e.g., spiked samples, production batches, placebo) for comparative testing, ensuring proper handling and shipment to maintain sample integrity [4].
- Execute Protocol: Both laboratories perform the analytical method according to the approved protocol, typically involving multiple analysts, instruments, and days to establish intermediate precision [4] [6].
- Document Everything: Meticulously record all raw data, instrument printouts, calculations, and any deviations encountered during the execution phase [4] [8].
Phase 3: Data Evaluation and Reporting
This phase focuses on analyzing the generated data and formalizing the transfer outcome.
- Data Compilation: Collect all data from both laboratories in a standardized format to facilitate comparison [4].
- Statistical Analysis: Perform statistical comparison as outlined in the protocol, which may include t-tests, F-tests, equivalence testing, or ANOVA to objectively evaluate inter-laboratory differences [4] [7].
- Evaluate Against Acceptance Criteria: Compare the results against the pre-defined acceptance criteria established in the transfer protocol [4] [8].
- Investigate Deviations: If acceptance criteria are not met, conduct thorough investigations to determine the root cause, document findings, and implement corrective actions before proceeding [3] [4].
- Draft Transfer Report: Prepare a comprehensive report summarizing the transfer activities, results, statistical analysis, deviations, and conclusions regarding the success of the transfer [1] [4].
- QA Review and Approval: The transfer report, along with all supporting documentation, undergoes rigorous review and formal approval by Quality Assurance to ensure compliance [4].
Phase 4: Post-Transfer Activities
The final phase ensures the sustainable implementation of the method in the receiving laboratory.
- SOP Development/Revision: The receiving laboratory develops or updates its Standard Operating Procedures for the transferred method, incorporating any site-specific nuances while maintaining equivalency [4].
- Routine Testing: The receiving laboratory begins using the method for routine GMP testing, with all data becoming reportable for regulatory purposes [8].
- Ongoing Performance Monitoring: Continuously monitor the method's performance through system suitability tests, quality control charts, and trending analyses to ensure continued reliability [4].
Acceptance Criteria and Performance Metrics
Establishing scientifically sound acceptance criteria is fundamental to demonstrating a successful method transfer. These criteria should be based on the method's validation data and performance characteristics, taking into account ICH requirements and product specifications [3].
Table 2: Typical Acceptance Criteria for Analytical Method Transfer
| Test | Experimental Design | Typical Acceptance Criteria | Statistical Measures |
|---|---|---|---|
| Identification | Positive (or negative) identification obtained at receiving site [3]. | Positive identification matching reference standard [3]. | Qualitative comparison; no statistical analysis required. |
| Assay | 2 Analysts × 3 test samples in triplicate using different instruments/columns/independent solution preparations [6]. | Absolute difference between the sites' mean results: 2-3% [3] [6]. | Comparison of mean variability; % Relative Standard Deviation (RSD) of replicates < 5.0% [6]. |
| Related Substances (Impurities) | 2 Analysts × 3 test samples in triplicate using spiked samples where necessary [6]. | Absolute difference between results: < 25.0% for low-level impurities; Recovery of 80-120% for spiked impurities [3] [6]. | % RSD of replicate standards < 5.0%; comparison of result variability [6]. |
| Dissolution | Analysis of identical samples at multiple time points by both laboratories [3]. | Absolute difference in mean results: NMT 10% at time points when < 85% dissolved; NMT 5% at time points when > 85% dissolved [3]. | Statistical comparison of mean results at each time point. |
| Cleaning Validation | 2 Analysts × 3 test samples in triplicate using samples spiked at three different concentration levels [6]. | All samples spiked above specified limit must fail; all samples below specified limit must pass [6]. | Qualitative pass/fail determination with demonstrated specificity. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of an Analytical Method Transfer requires meticulous preparation and the availability of specific, quality-controlled materials. The following table details key reagent solutions and materials essential for the transfer process.
Table 3: Essential Research Reagents and Materials for Analytical Method Transfer
| Item Category | Specific Examples | Function in AMT | Critical Quality Attributes |
|---|---|---|---|
| Reference Standards | Drug substance standards; impurity standards; system suitability standards [3] [7]. | Quantitation of analytes; demonstration of method specificity and system performance [7]. | Certified purity and identity; proper storage conditions; established stability [4]. |
| Critical Reagents | HPLC mobile phase components; derivatization agents; digestion buffers [8]. | Execution of method as defined in protocol; maintenance of chromatographic performance [8]. | Manufacturer and grade as specified in method; preparation documentation; expiry dating [4]. |
| Chromatographic Columns | C18, C8, phenyl, HILIC, or other specified stationary phases [6]. | Reproducibility of separation; achievement of system suitability criteria [6]. | Equivalent specification to original column; column performance certificate; appropriate conditioning [6]. |
| Sample Materials | Homogeneous lot of API; finished product; placebo; spiked samples [4] [7]. | Comparative testing between laboratories; demonstration of accuracy and precision [7]. | Representative of routine samples; established stability for transfer duration; certificates of analysis [4] [7]. |
| System Suitability Materials | Resolution mixtures; tailing factor solutions; precision standards [7]. | Verification that the analytical system is operating adequately for the intended analysis before and during testing [7]. | Consistent performance to established criteria; demonstration of method robustness [7]. |
Analytical Method Transfer represents a critical juncture in the lifecycle of an analytical procedure, marking its transition from development to routine application in quality control. The documented process, when executed following a structured methodology with clearly defined acceptance criteria, provides assurance that the receiving laboratory can generate reliable, reproducible, and regulatory-compliant data equivalent to that produced by the originating laboratory [1] [4]. Among the various approaches, Comparative Testing remains the most prevalent for established methods, while Co-validation offers efficiency for new methods destined for multi-site use [3] [4].
The success of any AMT exercise hinges on comprehensive planning, robust communication between transferring and receiving units, adequate personnel training, and meticulous documentation [1] [3] [4]. Furthermore, a thorough understanding of the method's capabilities and limitations, coupled with a science- and risk-based approach to protocol design and execution, ensures that the transfer process not only meets regulatory expectations but also establishes a solid foundation for the method's long-term performance in its new environment [3] [4]. For researchers and drug development professionals, mastering the principles and practices of Analytical Method Transfer is therefore indispensable for maintaining product quality and regulatory compliance across the global pharmaceutical landscape.
The Critical Importance of AMT for Regulatory Compliance and Patient Safety
Analytical Method Transfer (AMT) is a critical documented process that qualifies a receiving laboratory to use an analytical procedure that originated in a transferring laboratory, ensuring it performs with equivalent accuracy, precision, and reliability [4] [9]. In the pharmaceutical industry, this process is not merely a logistical formality but a scientific and regulatory imperative [10] [4]. A successfully transferred method guarantees that analytical data—from the identity of raw materials to the level of impurities in a final product—remains consistent and reliable across different locations, instruments, and analysts [10]. This consistency is the bedrock of drug quality, making AMT a vital activity for regulatory compliance and, ultimately, for ensuring the safety and efficacy of medicines reaching patients [10] [11].
The Regulatory Imperative of Analytical Method Transfer
Regulatory bodies worldwide mandate that analytical methods used for quality control must be reliable, irrespective of where the testing is performed. Analytical Method Transfer provides the documented evidence required to meet these expectations.
- Foundation for Compliance: Regulatory agencies, including the FDA, EMA, and WHO, require proof that a method works correctly in any laboratory that uses it [10]. A successful AMT demonstrates this, forming a core part of a site's Good Manufacturing Practice (GMP) obligations, particularly for contract manufacturing and testing [11].
- Consequences of Failure: A poorly executed transfer can lead to significant regulatory and operational risks, including delayed product releases, costly retesting, and observations during regulatory inspections [4]. Common inspection findings include unqualified equipment for the method's range, failure to follow the transfer protocol, and insufficient testing on an inadequate number of batches [11].
- A Shared Responsibility: Regulatory compliance is a shared responsibility between the transferring and receiving laboratories [11]. A collaborative approach, supported by a formal process and thorough documentation, gives confidence in the data generated after the AMT is completed.
Comparing Core Method Transfer Approaches
The United States Pharmacopeia (USP) <1224> outlines several recognized approaches for transferring an analytical method [4] [12]. The choice of strategy depends on factors such as the method's complexity, its validation status, and the risk involved.
The table below summarizes the primary approaches:
| Transfer Approach | Description | Best Suited For | Key Considerations |
|---|---|---|---|
| Comparative Testing [4] [3] | Both labs analyze identical samples; results are statistically compared. | Well-established, validated methods; labs with similar capabilities. | Most common approach; requires robust statistical analysis and homogeneous samples. |
| Co-validation [4] [12] | The method is validated simultaneously by both the transferring and receiving labs. | New methods or methods being developed for multi-site use from the outset. | Resource-intensive; fosters shared ownership and deep understanding from the start. |
| Revalidation [4] [3] | The receiving lab performs a full or partial revalidation of the method. | Significant differences in lab conditions/equipment or substantial method changes. | Most rigorous approach; treats the method as if it were new to the receiving site. |
| Transfer Waiver [4] | The formal transfer process is waived based on strong justification. | Highly experienced receiving lab; simple, robust methods like some pharmacopoeial methods. | Rare; subject to high regulatory scrutiny and requires robust scientific justification. |
Quantitative Acceptance Criteria for Method Transfer
A successful transfer hinges on pre-defined, justified acceptance criteria for the method's performance characteristics. These criteria, detailed in the transfer protocol, provide the objective measure for success.
The following table outlines typical acceptance criteria for common analytical tests:
| Analytical Test | Typical Acceptance Criteria |
|---|---|
| Identification [3] | Positive (or negative) identification obtained at the receiving site. |
| Assay [3] | Absolute difference between the results from the two sites: 2-3%. |
| Related Substances (Impurities) [3] | Absolute difference criteria vary by impurity level. For low-level impurities, recovery of 80-120% for spiked samples may be used. |
| Dissolution [3] | Absolute difference in the mean results:• NMT 10% at time points when <85% is dissolved• NMT 5% at time points when >85% is dissolved |
Experimental Protocol for a Comparative Method Transfer
The comparative testing approach is the most frequently used method [11]. The following workflow details the standardized protocol for executing this transfer, from initial planning to final reporting.
Diagram Title: AMT Comparative Testing Workflow
Phase 1: Pre-Transfer Planning and Assessment
This foundational phase determines the project's roadmap [4].
- Define Scope & Objectives: Clearly articulate the reason for the transfer and define what constitutes success using specific, measurable acceptance criteria [4].
- Form Cross-Functional Teams: Designate leads and team members from both labs, including Analytical Development, QA/QC, and Operations [4].
- Gather Method Documentation: Collect all method validation reports, development reports, Standard Operating Procedures (SOPs), and historical data from the transferring lab [4] [3].
- Conduct Gap & Risk Analysis: Compare equipment, reagents, software, and personnel expertise between the two labs to identify potential discrepancies [4] [3]. A formal risk assessment helps identify critical parameters that could impact the results [10] [11].
- Develop & Approve Transfer Protocol: This critical document, requiring Quality Assurance (QA) approval, must specify method details, responsibilities, experimental design, acceptance criteria, and the statistical analysis plan [4] [3].
Phase 2: Execution and Data Generation
This phase focuses on the practical implementation of the protocol.
- Train Receiving Lab Analysts: The transferring lab must provide effective training to convey method-specific knowledge, including critical parameters and troubleshooting tips [4] [12]. All training must be documented.
- Verify Equipment & Reagents: Ensure all instruments at the receiving lab are properly qualified, calibrated, and maintained. Use traceable and qualified reference standards and reagents at both sites [4].
- Execute Protocol: Parallel Testing: Both labs analyze a pre-defined number of samples from the same homogeneous batch, often with multiple injections, as per the approved protocol [4] [11] [3].
Phase 3: Data Evaluation and Reporting
The generated data is rigorously analyzed to determine the transfer's outcome.
- Perform Statistical Analysis: Compare the results from both laboratories using statistical tools pre-defined in the protocol, such as t-tests, F-tests, or equivalence testing [4] [3].
- Evaluate Against Acceptance Criteria: Compare the statistical outcomes with the pre-defined acceptance criteria to determine if they are met [4].
- Investigate Any Deviations: Any deviations from the protocol or out-of-specification results must be thoroughly investigated and documented [3].
- Draft & Approve Transfer Report: A comprehensive report summarizing the activities, results, and conclusions is prepared. The report must clearly state whether the transfer was successful and requires QA approval [4] [3].
Phase 4: Post-Transfer Activities
Upon successful transfer, the method is implemented for routine use.
- Develop/Update Site SOPs: The receiving laboratory formally adopts the method by creating or updating its own SOPs [4].
The Scientist's Toolkit: Essential Reagents and Materials
The reliability of an AMT depends on the quality and consistency of the materials used. The table below lists key reagent solutions and their critical functions in ensuring a successful transfer.
| Item | Critical Function in AMT |
|---|---|
| Qualified Reference Standards | Serves as the benchmark for method accuracy and calibration; traceability and stability are paramount [4]. |
| Validated Instruments & Columns | Ensures data integrity; equipment (especially HPLC/GC) must be qualified for the method's specific range and conditions [10] [11]. |
| Specified Lot of Reagents & Solvents | Prevents variability; using the same grade and supplier of solvents and buffers as validated is crucial for robustness [10]. |
| Stable & Homogeneous Test Samples | Forms the basis for comparative testing; samples must be representative and remain stable throughout the testing window [4]. |
| Detailed Method Transfer Protocol | The master document that defines all aspects of the transfer, ensuring regulatory compliance and a shared understanding [4] [3]. |
Analytical Method Transfer is far more than a procedural hurdle; it is a fundamental component of the pharmaceutical quality system. A meticulously planned and executed AMT, supported by rigorous experimental protocols and clear acceptance criteria, provides the documented evidence required for regulatory compliance. More importantly, it ensures that every laboratory involved in the testing of a drug product can generate trustworthy data. This reliability directly safeguards patient safety by ensuring that medicines are consistently of the correct identity, strength, quality, and purity, no matter where they are tested. In an era of globalized pharmaceutical manufacturing and complex supply chains, the role of AMT as a guardian of product quality and patient welfare has never been more critical.
In the highly regulated pharmaceutical industry, the reliability and consistency of analytical methods are fundamental to ensuring drug safety and efficacy. Analytical Method Transfer (AMT) is a critical, documented process that verifies a laboratory (the "receiving unit") can successfully execute a validated analytical method originally developed and used by another laboratory (the "transferring unit") and produce equivalent results [10]. This process is not a mere formality but a scientific and regulatory imperative to guarantee that methods perform consistently across different locations, instruments, and personnel [4]. The core principle is to establish equivalence or comparability between the two laboratories, ensuring the method's performance characteristics—such as accuracy, precision, and specificity—remain consistent [4]. This guide explores the key scenarios that necessitate method transfer and objectively compares the primary approaches used within the industry.
Understanding the Need for Method Transfer
The transfer of analytical methods is driven by several common operational scenarios in drug development and manufacturing. A failure to properly execute these transfers can lead to significant issues, including delayed product releases, costly retesting, and regulatory non-compliance [4].
The most frequent scenarios requiring AMT include:
- Multi-site Operations: When a method developed and validated at one research or manufacturing site needs to be implemented at another facility within the same company to decentralize testing or increase capacity [4].
- Partnerships with CROs/CMOs/CDMOs: Transferring methods to or from external contract research and manufacturing organizations is a cornerstone of modern pharmaceutical outsourcing [4]. This is crucial for tasks like stability studies, release testing, or when a contract organization takes over manufacturing [10].
- Technology and Equipment Changes: Adapting an existing method to new instrumentation or analytical platforms at a different location [4].
- Method or Process Improvements: Rolling out a refined or optimized analytical method across multiple laboratory sites [4].
- Post-Approval Changes: Changes in the manufacturing site for a commercial product often require the associated analytical methods to be transferred to the new site's quality control laboratory [3].
Comparative Analysis of Method Transfer Approaches
Regulatory bodies like the USP (General Chapter <1224>) outline several accepted approaches for method transfer [4]. The choice of strategy depends on factors like the method's complexity, its regulatory status, the experience of the receiving lab, and the level of risk involved [4]. The following table summarizes the four primary transfer protocols for easy comparison.
| Transfer Approach | Experimental Protocol & Methodology | Best-Suited Context | Key Advantages | Key Limitations & Risks |
|---|---|---|---|---|
| Comparative Testing | Both laboratories analyze the same set of homogeneous, representative samples (e.g., from a production batch, spiked samples) using the identical method. Results are statistically compared using pre-defined tests (e.g., t-tests, F-tests, equivalence testing) [4] [10]. | Well-established, validated methods where both labs have similar capabilities and equipment [4]. | Most common and widely accepted approach; provides direct, empirical evidence of equivalence [3]. | Requires careful sample preparation and handling; statistical analysis must be robust and pre-defined [4]. |
| Co-validation | The analytical method is validated simultaneously by both the transferring and receiving laboratories as part of a joint effort. This is often detailed in a shared validation protocol [10] [3]. | New methods, or when a method is being developed specifically for multi-site use from the outset [4]. | Fosters shared ownership and deep understanding from the start; can be more efficient than sequential validation and transfer [12]. | Can be resource-intensive; requires exceptionally close collaboration and harmonized protocols [4]. |
| Revalidation | The receiving laboratory performs a full or partial revalidation of the method as if it were new, following established validation guidelines (e.g., ICH Q2(R1)) [4] [10]. | Significant differences in lab conditions/equipment; substantial method changes; or when the original validation is inadequate [4] [3]. | Most rigorous approach; builds high confidence as the receiving lab demonstrates full method mastery independently [4]. | Most resource- and time-intensive approach; may be unnecessary for well-understood methods [10]. |
| Transfer Waiver | No experimental transfer work is conducted. Waiver is justified based on prior data, such as the receiving lab's existing proficiency with the method or the method's simplicity [4] [3]. | Highly experienced receiving lab; identical conditions; simple, robust compendial methods (e.g., USP) that only require verification [4] [3]. | Saves significant time and resources; efficient for low-risk scenarios. | Rarely applicable; carries high regulatory scrutiny and requires exhaustive scientific justification and risk assessment [4]. |
Workflow for a Successful Analytical Method Transfer
The following diagram illustrates the typical phased workflow for a successful analytical method transfer, integrating elements from the various approaches described above.
The Scientist's Toolkit: Essential Reagents and Materials
The success of an analytical method transfer hinges not only on the protocol but also on the quality and consistency of the materials used. The table below details key reagent solutions and materials critical for ensuring reproducible results.
| Item | Critical Function & Rationale | Best Practice Considerations |
|---|---|---|
| Reference Standards | Qualified substances with known purity and identity used to calibrate instruments and quantify results [3]. | Use traceable and qualified standards from reputable sources. Confirm stability and storage conditions to ensure integrity throughout the transfer process [4]. |
| Chromatographic Columns | The stationary phase in HPLC/GC systems; critical for separating analytes. | Specify the exact brand, model, and chemistry (e.g., C18, 250mm x 4.6mm, 5µm). Column variability is a major source of transfer failure, so aligning specifications between labs is essential [10]. |
| Chemical Reagents & Solvents | High-purity solvents and chemicals used in mobile phases, sample solutions, and derivatization. | Specify grade (e.g., HPLC-grade) and supplier. Differences in solvent quality or water pH can significantly alter chromatographic performance and results [10]. |
| Stable Test Samples | Representative samples of the drug substance or product being analyzed [3]. | Use homogeneous samples from a single, well-characterized batch. Ensure samples are stable for the duration of testing and that shipping conditions do not compromise integrity [4] [10]. |
| System Suitability Solutions | A mixture of key analytes used to verify that the total analytical system is functioning adequately at the time of testing. | The solution and acceptance criteria should be defined in the method. It serves as a final check that the entire system (instrument, column, reagents, operator) is performing as required before sample analysis begins [10]. |
The increasing reliance on multi-site operations and partnerships with CROs, CMOs, and CDMOs makes robust analytical method transfer protocols more vital than ever [13] [14]. There is no one-size-fits-all approach; the choice between comparative testing, co-validation, revalidation, or a waiver must be driven by a thorough risk assessment that considers method complexity, inter-lab differences, and regulatory expectations [10] [3].
Ultimately, success is rooted in more than just technical execution. Comprehensive planning, robust communication, and meticulous documentation form the foundation of a seamless transfer. By systematically applying these principles and selecting the most appropriate transfer strategy, pharmaceutical companies and their partners can mitigate risks, ensure regulatory compliance, and maintain the unwavering product quality that safeguards patient safety [4] [3].
In the field of drug development and manufacturing, demonstrating that two laboratories can produce equivalent and comparable results is a fundamental requirement. Establishing comparability is essential whenever a manufacturing process, analytical method, or production location is changed. Regulatory agencies, such as the FDA, require a documented process to show that any change does not adversely impact the product's safety, identity, strength, quality, purity, or potency [15]. The core statistical approach for this demonstration is equivalence testing, which provides evidence that differences in measurements between two laboratories are small enough to be considered practically insignificant [15]. This guide outlines the principles, protocols, and data analysis techniques required to establish robust evidence of inter-laboratory equivalence.
The Statistical Foundation: Equivalence Testing
Why Equivalence Testing Trumps Significance Testing
A common misconception is using significance testing (e.g., a t-test aiming for a p-value > 0.05) to demonstrate comparability. This approach is flawed because a non-significant p-value merely indicates "insufficient evidence to conclude a difference." It does not confirm that the results are equivalent. The test might be unable to detect a meaningful difference due to high variability or an insufficient number of replicates [15].
Equivalence testing inverts this logic. It proactively tests the hypothesis that the means from two laboratories differ by an amount that is less than a pre-defined, acceptable margin. This margin, often called the "equivalence interval" or "acceptance criterion," represents a threshold of practical insignificance. The most common statistical method for this is the Two One-Sided T-test (TOST) procedure [15].
The Two One-Sided T-Test (TOST) Procedure
The TOST approach tests two simultaneous hypotheses:
- That the true difference between the laboratory means is greater than the lower practical limit (LPL).
- That the true difference is less than the upper practical limit (UPL).
If both hypotheses can be rejected, it provides statistical evidence that the difference lies entirely within the acceptable range (LPL to UPL). The following diagram illustrates the logical decision-making process of the TOST.
Setting Risk-Based Acceptance Criteria
The equivalence interval (LPL and UPL) is not arbitrary; it should be based on scientific knowledge, product experience, and clinical relevance [15]. A risk-based approach is recommended:
Table 1: Risk-Based Acceptance Criteria for Equivalence Intervals
| Risk Level | Typical Acceptance Criterion (as % of tolerance) |
|---|---|
| High Risk | 5% - 10% |
| Medium Risk | 11% - 25% |
| Low Risk | 26% - 50% |
Higher-risk situations, where a small difference could significantly impact product quality or patient safety, warrant tighter (smaller) acceptance criteria. The impact on process capability and out-of-specification (OOS) rates should also be evaluated [15].
Experimental Protocols for Method Transfer
The process of qualifying a receiving laboratory to use an analytical method developed by a transferring laboratory is known as Analytical Method Transfer (AMT) [2]. The following workflow maps the key stages and decision points in a typical transfer process.
Types of Analytical Method Transfers
There are several accepted approaches to conduct a method transfer, each suitable for different circumstances [2]:
- Comparative Testing: The most common approach. The same lot of a product, API, or device is analyzed by both the transferring and receiving laboratories. The results are compared against pre-defined acceptance criteria in a protocol.
- Co-validation between Laboratories: The transferring and receiving laboratories collaborate in an inter-laboratory validation study. This assesses the reproducibility of the method.
- Revalidation or Partial Revalidation: The receiving laboratory performs a complete or partial validation of the method, as outlined in guidelines like USP <1225>.
- Transfer Waiver: A justified omission of the formal transfer process. This is based on a risk analysis and is only applicable when the receiving laboratory has extensive existing experience and knowledge with the method or similar methods [2].
Key Reagents and Materials
Successful method transfer relies on critical materials and documentation. The table below lists essential items and their functions.
Table 2: Essential Research Reagent Solutions and Materials for Method Transfer
| Item | Function / Purpose |
|---|---|
| Reference Standards | Provides a known and qualified benchmark to calibrate instruments and validate method performance in the receiving lab [2]. |
| Test Article (Single Lot) | A single, homogeneous lot of the product, API, or device is used for comparative testing to isolate method performance from process variability [2]. |
| Validated Method Document | The unambiguous, detailed procedure from the transferring lab. It is the core document being qualified [2]. |
| Qualified/Calibrated Equipment | Laboratory systems at the receiving lab must be verified for availability and proper qualification/calibration to ensure data integrity [2]. |
| System Suitability Controls | Quality control samples used to verify that the analytical system is operating correctly before and during the analysis. |
Case Study: Inter-Laboratory Validation of a Neutralizing Antibody Assay
A 2024 study provides a robust, real-world example of establishing comparability for a complex, cell-based assay. The research focused on standardizing a microneutralization (MN) assay for anti-AAV9 neutralizing antibodies (NAbs) across multiple laboratories [16].
Experimental Methodology
- Objective: To establish a standardized MN assay and assess its intra- and inter-laboratory reproducibility.
- Assay Principle: The assay measures the inhibition of recombinant AAV9 vector transduction in a susceptible cell line (HEK293). The readout is luciferase activity (Relative Luminescence Units, RLU) [16].
- Sample Preparation: Human serum or plasma samples were pre-treated at 56°C for 30 minutes. Samples were serially diluted two-fold, starting at 1:20, and incubated with the AAV9 vector [16].
- Experimental Steps:
- Virus-sample mixture incubated for 1 hour at 37°C.
- HEK293 cells were added and incubated for 48-72 hours.
- Luciferase activity in the supernatant was measured.
- Transduction Inhibition (TI) was calculated as:
[1 − (RLUtest − RLUcell control)/(RLUvirus control − RLUcell control)] × 100%. - The IC50 titer (dilution that inhibits 50% of transduction) was determined using 4-parameter logistic (4PL) regression [16].
- Quality Control: A monoclonal antibody in human negative serum was used as a system suitability control, requiring an inter-assay titer variation of less than a 4-fold difference [16].
Key Quantitative Findings and Data Presentation
The study generated clear quantitative data on the assay's performance, which is summarized in the table below.
Table 3: Performance Data from Anti-AAV9 Neutralizing Antibody Assay Validation
| Performance Parameter | Result | Acceptance Criterion |
|---|---|---|
| Sensitivity | 54 ng/mL | Not Specified |
| Specificity (vs. AAV8) | No cross-reactivity at 20 μg/mL | Not Specified |
| Intra-Assay Precision (Variation for Low Positive QC) | 7% - 35% | Not Specified |
| Inter-Assay Precision (Variation for Low Positive QC) | 22% - 41% | Not Specified |
| Intra-Laboratory Reproducibility (%GCV of blind samples) | 18% - 59% | Not Specified |
| Inter-Laboratory Reproducibility (%GCV of blind samples) | 23% - 46% | System QC: <50% %GCV |
%GCV: Geometric Coefficient of Variation [16].
The data in Table 3 demonstrates that the method, despite being a complex bioassay, showed excellent reproducibility both within and between laboratories, as all %GCV values for the blind samples met the system suitability requirement of <50% [16]. This successful transfer and validation provide a template for standardizing similar methods across the industry.
Best Practices for Reporting and Documentation
Clear reporting is critical for regulatory submissions and internal decision-making.
- Structured Report: A comprehensive transfer report should include a title page, abstract, introduction, methodology, results, and a discussion/conclusion [17].
- Present Quantitative and Qualitative Data Together: Use tables and figures to present quantitative findings, but always provide context, interpretation, and rationale for the acceptance criteria used [18].
- Include Confidence Intervals: When reporting equivalence test results, including confidence intervals is a best practice, as they visually represent the estimate and precision of the difference between laboratories [15].
- Document Deviations: Any deviations from the pre-approved protocol must be documented and their impact assessed [2].
Establishing equivalence and comparability between laboratories is a systematic, documented process grounded in sound statistical principles. Moving from flawed significance testing to proactive equivalence testing (TOST) ensures that demonstrated comparability is both statistically and practically significant. The foundation of a successful transfer is a risk-based protocol with pre-defined acceptance criteria, supported by a rigorous experimental design and comprehensive training. As demonstrated by the inter-laboratory assay validation case study, these principles are universally applicable, from simple chemical tests to complex biological methods, and are essential for ensuring consistent, reliable data across the global scientific landscape.
Analytical method transfer is a critical, documented process in the pharmaceutical industry that qualifies a receiving laboratory to use an analytical method originally developed and validated in a different (transferring) laboratory [10] [4]. Its fundamental purpose is to provide documented evidence that the transferred analytical method performs in the new laboratory with the same level of accuracy, precision, and reliability as in the original laboratory, despite differences in analysts, equipment, and environmental conditions [10] [19]. This process is not a mere formality but a regulatory imperative to ensure the consistency, quality, and safety of pharmaceutical products when testing is moved between sites, such as from research and development (R&D) to a quality control (QC) lab, or to a contract manufacturing organization (CMO) [10] [3].
The success of a method transfer is demonstrated by establishing "equivalence" or "comparability" between the data generated at the transferring and receiving laboratories [4]. Regulatory agencies worldwide, including the US Food and Drug Administration (FDA), the European Medicines Agency (EMA), and others, require proof that analytical methods are reliable and reproducible across different testing sites [10] [20].
Comparative Analysis of Key Regulatory Guidelines
A thorough understanding of the guidelines from the United States Pharmacopeia (USP), the FDA, and the EMA is essential for successful regulatory compliance. The following table provides a high-level comparison of these core documents.
| Guideline | Primary Focus & Scope | Recommended Transfer Approaches | Key Emphases and Requirements |
|---|---|---|---|
| USP General Chapter <1224> [10] [4] | Standardizing the transfer of analytical procedures; provides a conceptual framework. | • Comparative Testing• Co-validation• Revalidation• Transfer Waiver | Promotes a science- and risk-based approach. Emphasizes testing homogeneous lots of material and using pre-defined acceptance criteria [20]. |
| FDA Guidance for Industry: Analytical Procedures and Methods Validation (2015) [10] [20] | Part of a broader guidance on method development, validation, and lifecycle management. | • Comparative studies to evaluate accuracy, precision, and inter-laboratory variability. | For stability-indicating methods, recommends both labs analyze forced degradation samples or samples with product-related impurities [20]. Focuses on integrated data to demonstrate reliability. |
| EMA Guideline on the Transfer of Analytical Methods (2014) [10] [20] | A dedicated guideline outlining expectations for method transfer protocols and execution. | • Protocol must define standards, samples, transport/storage conditions, and acceptance criteria. | Stresses that acceptance criteria must be consistent with method validation and align with ICH/VICH expectations. Highlights the need for a detailed, pre-approved protocol [20]. |
Deeper Dive into Regulatory Expectations
- USP <1224>: This chapter is not a binding regulatory requirement but is a highly influential and widely accepted standard. It outlines different transfer approaches, with comparative testing being the most common, where both labs analyze the same homogeneous samples and results are statistically compared [10] [4]. It encourages laboratories to select the transfer strategy based on risk assessment, method complexity, and the receiving lab's experience [10].
- FDA Guidance: The FDA's approach is integrated into its overall view of the method lifecycle. It emphasizes the assessment of inter-laboratory variability to ensure the method is robust across different environments. The FDA also pays close attention to the transfer of stability-indicating methods, expecting both laboratories to demonstrate that they can accurately detect and quantify impurities and degradation products [20].
- EMA Guideline: The EMA provides very specific directives on the content of the transfer protocol. It requires that the protocol explicitly details the materials, samples, and acceptance criteria to be used [20]. This underscores the EMA's focus on meticulous prior planning and comprehensive documentation to ensure the transfer is well-controlled and its outcomes are unambiguous.
Standardized Experimental Protocol for Method Transfer
A successful analytical method transfer follows a structured, multi-phase process from planning to closure. The workflow below illustrates the key stages and their logical sequence.
Phase I: Pre-Transfer Planning
The foundation of a successful transfer is laid during the planning phase. This involves forming a team with representatives from both the sending and receiving units, including analytical experts and quality assurance (QA) [4]. The sending laboratory must provide all method documentation, including the validation report, development data, and standard operating procedures (SOPs) [3]. A critical step is conducting a gap analysis and risk assessment to identify differences in equipment, reagents, analyst skills, and environmental conditions that could impact the method's performance [4] [3]. Mitigation strategies, such as additional training or equipment qualification, are planned at this stage.
Phase II: Protocol Development and Approval
A pre-approved, detailed protocol is the cornerstone of a compliant transfer [10] [4]. This document must include:
- Objective and Scope: Clear statement of the transfer's purpose and the methods involved.
- Responsibilities: Defined roles for both the sending and receiving laboratories [10].
- Experimental Design: The number of samples, replicates, and analysts to be used [20]. For example, one common approach is to have at least two analysts independently analyze three lots of product in triplicate [20].
- Acceptance Criteria: Pre-defined, statistically justified criteria for evaluating equivalence. These are often based on the method's validation data, particularly its reproducibility [3]. The table below provides examples of typical acceptance criteria for common tests.
| Test | Typical Acceptance Criteria |
|---|---|
| Identification | Positive (or negative) identification obtained at the receiving site [3]. |
| Assay | The absolute difference between the mean results from the two sites should not exceed 2-3% [3]. |
| Related Substances | Requirements for absolute difference depend on impurity level. For low levels, recovery criteria (e.g., 80-120%) for spiked impurities may be used [3]. |
| Dissolution | Absolute difference in mean results: NMT 10% at time points <85% dissolved; NMT 5% at time points >85% dissolved [3]. |
Phase III: Execution and Training
Before testing begins, analysts at the receiving lab must be thoroughly trained by experts from the transferring laboratory [4] [3]. This training should cover not only the procedural steps but also the "tacit knowledge," such as troubleshooting tips and an understanding of the method's critical parameters [3] [12]. All equipment must be qualified and calibrated. Both laboratories then execute the approved protocol, analyzing the same homogeneous and stable samples—often drawn from a centrally managed "method transfer kit" (MTK) to ensure consistency across multiple transfers [20].
Phase IV: Data Analysis and Reporting
Data from both laboratories are compiled and compared using the statistical methods specified in the protocol (e.g., t-tests, F-tests, equivalence testing) [10] [4]. The results are evaluated against the pre-defined acceptance criteria. Any deviations or out-of-specification (OOS) results must be thoroughly investigated [3]. All activities, data, and investigations are summarized in a final transfer report, which concludes whether the transfer was successful and qualifies the receiving lab to use the method [10].
Phase V: Project Close-Out
The process is finalized when the transfer report is approved by the Quality Assurance (QA) department [10] [4]. The receiving laboratory then implements the method by incorporating it into its local SOPs and begins using it for routine testing.
The Scientist's Toolkit: Essential Materials for Successful Transfer
The consistency and quality of materials used during transfer are crucial for obtaining comparable results. The following table details key reagent solutions and materials.
| Item / Solution | Critical Function & Justification |
|---|---|
| Method Transfer Kit (MTK) [20] | A centrally managed kit containing representative, homogeneous samples (e.g., drug product batches, impurity-spiked samples) for all transfers. Function: Eliminates sample-to-sample variability, allowing focus on inter-laboratory method performance. |
| Qualified Reference Standards [4] | Well-characterized standards with certified purity and concentration. Function: Serves as the benchmark for calibrating the method and ensuring the accuracy and traceability of all quantitative results. |
| System Suitability Test Solutions [21] [22] | A standardized solution or mixture used to verify that the chromatographic system (or other instrument) is performing adequately before sample analysis. Function: Ensures the integrity of the entire analytical system for the specific method on a given day. |
| Chromatographic Columns [10] | The specific type, make, and model of the HPLC or GC column as defined in the method. Function: Different columns have varying selectivity; using the specified column is critical for reproducing separation, resolution, and retention times. |
| Reagents & Solvents [10] | High-purity solvents and reagents of the specified grade. Function: Variations in reagent quality (e.g., HPLC-grade vs. technical grade) can introduce impurities, affect baseline noise, and alter method sensitivity and reproducibility. |
Common Challenges and Best Practices
Frequently Encountered Challenges
- Instrument Disparities: Differences in instrument brands, models, modules (e.g., gradient delay volume in HPLC), or calibration status are a leading cause of transfer failure [10] [22].
- Reagent and Column Variability: Different batches of reagents or different sources/grades of chromatographic columns can lead to variations in results [10].
- Analyst Proficiency: Differences in training, experience, and technique between analysts at different sites can impact the execution of the method [10] [3].
- Environmental Conditions: Factors like temperature and humidity, which may not be fully controlled, can influence analytical results [10].
Strategies for Success and Compliance
- Early and Robust Planning: Begin the process early, engage QA from the start, and develop a comprehensive, unambiguous transfer protocol [4].
- Effective Communication and Collaboration: Establish direct communication channels between subject matter experts at both labs. Regular meetings help resolve issues quickly and facilitate crucial knowledge transfer [3] [12].
- Leverage Method Transfer Kits (MTKs): Using MTKs with pre-defined protocols and long-term stable samples streamlines multiple transfers, reduces duplication of effort, and ensures consistency [20].
- Ensure Equipment Equivalency and Qualification: Before transfer, align instrument specifications as much as possible and verify that all equipment at the receiving lab is properly qualified and calibrated [4].
- Adopt a Lifecycle Approach: Follow the principles of the Analytical Procedure Lifecycle (APLC), as described in USP <1220>, which encourages building robustness into the method during development and monitoring its performance post-transfer to ensure it remains fit-for-purpose [23].
Navigating the regulatory landscape for analytical method transfer requires a deep understanding of the guidelines provided by USP <1224>, the FDA, and the EMA. While each guideline has its nuances, they collectively emphasize a science- and risk-based approach, grounded in rigorous planning, clear documentation, and statistical evidence of equivalence. By adhering to a structured protocol, utilizing standardized materials like MTKs, and fostering strong collaboration between laboratories, pharmaceutical companies and CROs can ensure successful, efficient, and compliant method transfers. This not only fulfills regulatory obligations but, more importantly, safeguards product quality and patient safety by ensuring the reliability of analytical data across global manufacturing and testing networks.
Executing a Successful Transfer: Approaches, Protocol, and Step-by-Step Roadmap
Choosing the Right Transfer Approach: Comparative Testing, Co-validation, Revalidation, and Waivers
In the highly regulated pharmaceutical and biopharmaceutical industries, the transfer of analytical methods between laboratories is a critical and mandated process. It ensures that a method, when performed at a receiving laboratory, yields equivalent results to those obtained at the transferring laboratory, thereby guaranteeing the consistency, quality, and safety of drug products [4]. A failed or poorly executed transfer can lead to significant delays in product releases, costly retesting, and regulatory non-compliance [4]. This guide provides a detailed comparison of the four primary analytical method transfer approaches—Comparative Testing, Co-validation, Revalidation, and Transfer Waivers—to help researchers, scientists, and drug development professionals select and implement the most appropriate strategy for their specific context.
Summary Table of Analytical Method Transfer Approaches
| Transfer Approach | Core Principle | When to Use | Key Advantages | Key Challenges & Considerations |
|---|---|---|---|---|
| Comparative Testing [3] [4] [24] | Both labs analyze identical samples; results are statistically compared. | Well-established, validated methods; similar lab capabilities [3]. | Industry-standard; direct demonstration of equivalence; widely accepted by regulators [4]. | Requires careful sample homogeneity and handling; relies on robust statistical analysis [4]. |
| Co-validation [3] [25] [5] | Method is validated simultaneously by both transferring and receiving labs. | New methods or methods developed for multi-site use from the outset [3] [4]. | Highly efficient for qualifying multiple sites at once; builds reproducibility into validation [25] [5]. | Requires close collaboration and harmonized protocols; can be complex to manage [4]. |
| Revalidation [3] [4] [24] | Receiving lab performs a full or partial revalidation of the method. | Original lab unavailable; significant differences in equipment or conditions; method not originally ICH-compliant [3] [4]. | Most rigorous; qualifies the method independently at the new site; solves problem of unavailable originator [24]. | Most resource and time-intensive approach [4] [24]. |
| Transfer Waiver [3] [4] [5] | Formal transfer process is waived based on strong justification. | Receiving lab highly experienced with the method; compendial (e.g., USP) methods; only minor changes [3] [5]. | Saves significant time and resources; streamlines implementation [4]. | Rare; requires robust scientific and risk-based justification; subject to high regulatory scrutiny [4]. |
Experimental Protocols for Method Transfer
A successful transfer is built on a foundation of meticulous planning, execution, and documentation. The following workflow outlines the universal stages of a method transfer project, which should be tailored based on the selected approach.
Pre-Transfer Planning and Risk Assessment
Before a protocol is written, foundational activities are critical for success.
- Define Scope and Teams: Clearly articulate the method(s) being transferred and the objectives for success. Form cross-functional teams with designated leads from both the sending and receiving labs, including representatives from Analytical Development, QA/QC, and Operations [4].
- Gather Documentation: The sending unit must provide all relevant data, including the method description, validation report, development reports, and information on reference standards and reagents. Any prior risk assessments or "tacit knowledge" about the method should also be shared [3] [4].
- Perform Gap and Risk Analysis: Compare equipment, software, environmental conditions, and personnel expertise between the two labs [4]. The EU GMP guideline requires a gap analysis of the original validation to identify any need for supplementary work before transfer [3]. A risk assessment should identify potential challenges (e.g., method complexity, unique equipment) [4].
Developing the Transfer Protocol
The transfer protocol is the cornerstone document, typically written by the transferring laboratory but often drafted by the receiving unit [3]. It must be approved before execution and contain, at a minimum:
- Objective and Scope: A clear statement of the transfer's purpose [3].
- Responsibilities: Defined roles and requirements for both laboratories [3].
- Analytical Procedure: The detailed, step-by-step method to be used [3] [4].
- Experimental Design: The number of samples, batches, and replicates to be tested [3] [26].
- Acceptance Criteria: Pre-defined, statistically justified criteria for demonstrating equivalence [3] [4]. These are often based on the method's validation data and ICH requirements [3].
Key Experiments and Acceptance Criteria
The specific experiments run depend on the transfer approach and the method's purpose. For a standard comparative transfer of a quantitative method, the following are typical:
- Assay and Impurity Testing: A predetermined number of samples (e.g., a homogeneous lot from a production batch or spiked samples) are analyzed by both laboratories [3]. The results are compared using statistical tests (e.g., t-tests, F-tests, equivalence testing) [4].
- Typical Acceptance Criteria:
- Identification: Positive/negative identification must be obtained [3].
- Assay: The absolute difference between the sites' mean results is typically ≤ 2-3% [3].
- Related Substances: Criteria may vary by impurity level. For low-level impurities, recovery of 80-120% for spiked impurities is common. For higher levels (e.g., >0.5%), a absolute difference criterion is used [3].
- Dissolution: The absolute difference in mean results is typically ≤ 10% at time points when <85% is dissolved, and ≤ 5% when >85% is dissolved [3].
- Typical Acceptance Criteria:
- Precision (Repeatability and Intermediate Precision): The receiving laboratory performs replication experiments to assess the method's precision under normal operating conditions. This often involves a minimum of 20 replicate determinations on at least two levels of control materials [27] [26].
- Typical Acceptance Criteria: The calculated relative standard deviation (RSD or CV) is compared to pre-defined limits, often derived from the validation data or based on allowable total error (e.g., CV < 1/4 ATE) [26].
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of a method transfer is dependent on the quality and consistency of the materials used. The following table details key reagent solutions and their critical functions in the process.
Essential Materials for Analytical Method Transfer
| Item | Function in Method Transfer | Critical Considerations |
|---|---|---|
| Reference Standards [4] | Serves as the primary benchmark for quantifying the analyte of interest and confirming method performance. | Must be of qualified purity and traceable to a recognized standard body. Stability and proper storage conditions are vital [4]. |
| Critical Reagents [28] | Specific reagents essential for method function (e.g., antibodies for ligand-binding assays, enzymes, specialized solvents). | Different lots of critical reagents can significantly impact results, especially in biological assays. Using the same lot at both sites is ideal, or multiple lots should be evaluated for robustness [28]. |
| Spiked Samples [3] [25] | Artificially created samples with a known amount of impurity or analyte added, used to demonstrate accuracy and specificity. | Crucial for impurity testing (e.g., in Size-Exclusion Chromatography). The spiking material must be representative and stable [3] [25]. |
| Homogeneous Sample Lots [4] | A single, uniform batch of material (e.g., drug substance or product) aliquoted and sent to both laboratories for comparative testing. | Ensures that any differences in results are due to laboratory performance, not sample variability. Sample homogeneity is a prerequisite for a valid comparison [4]. |
| System Suitability Solutions [3] | A preparation used to verify that the chromatographic or analytical system is performing adequately at the time of the test. | The transfer protocol must specify system suitability criteria (e.g., peak retention, resolution, tailing factor) that must be met before transfer data can be considered valid [3]. |
Selecting the right transfer approach is not a one-size-fits-all decision but a strategic choice based on method status, laboratory capabilities, and regulatory requirements. Comparative testing remains the benchmark for transferring established methods, while co-validation offers an efficient path for new, multi-site methods. Revalidation is a powerful but resource-intensive solution for high-risk scenarios or unavailable originating labs, and the transfer waiver can streamline the process when justified by strong data and prior experience. By following a structured protocol that emphasizes rigorous planning, clear communication, and robust experimentation, laboratories can navigate the complexities of method transfer with confidence, ensuring data integrity and regulatory success throughout the product lifecycle.
Analytical method transfer is a critical, documented process in the pharmaceutical and biotechnology industries that qualifies a laboratory (the Receiving Unit or RU) to use an analytical testing procedure that originated in another laboratory (the Transferring Unit or TU) [29]. This process ensures that the Receiving Unit possesses the necessary procedural knowledge and ability to perform the transferred analytical procedure as intended, thereby guaranteeing that the method's performance remains consistent and reliable across different locations [30] [31]. The ultimate goal is to demonstrate that the RU can execute the method with equivalent accuracy, precision, and reliability as the TU, producing comparable results that ensure consistent product quality and patient safety [4].
A robust transfer protocol serves as the foundation for this entire process, providing a structured framework that defines objectives, delineates responsibilities, and establishes scientifically sound acceptance criteria. Without a well-crafted protocol, laboratories risk significant issues including delayed product releases, costly retesting, regulatory non-compliance, and ultimately, a loss of confidence in data integrity [4]. The protocol transforms the transfer from a mere administrative exercise into a scientifically rigorous demonstration of methodological consistency between laboratories.
Defining Clear Objectives and Scope
The initial and perhaps most crucial step in crafting a transfer protocol is to define clear, unambiguous objectives and scope. This foundational element sets the direction for the entire transfer process and ensures all stakeholders share a common understanding of what constitutes a successful transfer.
Core Objectives
The primary objective of any analytical method transfer is to generate documented evidence that the Receiving Laboratory is qualified to perform the analytical method and can generate data that is equivalent to that produced by the Transferring Laboratory [7]. This overarching goal can be broken down into several specific objectives:
- Demonstrate Equivalence: Prove that the method performs at the Receiving Unit with equivalent accuracy, precision, and reliability as demonstrated at the Transferring Unit [4].
- Ensure Regulatory Compliance: Provide documented evidence that satisfies regulatory requirements, showing the receiving lab is fully qualified to use the method for GMP reportable data [7].
- Facilitate Knowledge Transfer: Ensure all tacit knowledge, troubleshooting tips, and methodological nuances are effectively communicated from the TU to the RU [3].
- Establish Operational Readiness: Verify that the RU has the appropriate equipment, trained personnel, and necessary reagents to implement the method for routine use [31].
Scope Definition
A well-defined scope establishes the boundaries of the transfer activity and should clearly specify [29]:
- Methods Covered: List all analytical methods included in the transfer (e.g., HPLC assay, related substances, dissolution).
- Products and Materials: Identify the specific drug substances, intermediates, finished products, or raw materials to which the methods apply.
- Laboratories Involved: Name the specific Transferring and Receiving Units, including their locations.
- Applicable Techniques: Define the analytical techniques covered (e.g., HPLC, GC, UV, microbiological assays).
- Exclusions: Justify any methods excluded from transfer, such as general procedures lacking specialized techniques (e.g., pH, Loss on Drying) [29].
Key Components of a Transfer Protocol
A comprehensive transfer protocol serves as the master plan that guides all transfer activities. It must be pre-approved before any transfer activities commence and should contain specific sections that address critical aspects of the transfer process.
Responsibilities of Transferring and Receiving Units
Clear delineation of responsibilities is essential for accountability and smooth execution. The table below outlines typical responsibilities for both units involved in the transfer:
Table 1: Responsibilities of Transferring and Receiving Units
| Transferring Unit (TU) Responsibilities | Receiving Unit (RU) Responsibilities |
|---|---|
| Provide comprehensive method documentation and validation reports [31] [6] | Review methodology and acceptance criteria prior to protocol approval [31] [6] |
| Define experimental design, sampling methods, and acceptance criteria [6] | Ensure availability of qualified equipment and trained personnel [31] [6] |
| Supply necessary reference standards, reagents, and columns [29] | Execute the transfer protocol according to the approved design [6] |
| Provide method-specific training for RU analysts [31] [6] | Perform appropriate validation to support method implementation [6] |
| Assist in analysis and interpretation of QC testing results [6] | Maintain documentation system for recording data and results [6] |
| Participate in transfer study and collaborate with RU [31] | Generate and obtain approval of final transfer reports [6] |
| Review and approve transfer protocol and final report [31] | Communicate issues or concerns to TU during the transfer process [31] |
Experimental Design and Acceptance Criteria
The protocol must detail the experimental design, including the number of batches, analysts, replicates, and the specific tests to be performed. Similarly, predefined acceptance criteria are fundamental for objectively judging the success of the transfer.
Table 2: Typical Experimental Design and Acceptance Criteria for Common Tests
| Test Type | Experimental Design | Acceptance Criteria |
|---|---|---|
| Assay | 2 analysts × 3 test samples in triplicate using different instruments/columns/independent preparation [6] | Absolute difference between sites: 2-3% [3] [6] |
| Related Substances/Impurities | 2 analysts × 3 test samples in triplicate using different instruments/columns; spiked samples for recovery [6] | Difference < 25.0% for variability; %RSD of replicates < 5.0%; Recovery 80-120% for spiked impurities [3] [6] |
| Dissolution | Testing of multiple units from the same batch by both laboratories [3] | Absolute difference in mean results: ≤10% when <85% dissolved; ≤5% when >85% dissolved [3] |
| Cleaning Validation | 2 analysts × 3 test samples in triplicate using samples spiked at different concentration levels [6] | All samples spiked above specified limit must fail; all samples below specified limit must pass [6] |
| Identification | Comparison of identification results between laboratories [3] | Positive (or negative) identification obtained at receiving site matching transferring site [3] |
Method Transfer Approaches
The protocol should specify which transfer approach will be used based on the method's complexity, validated status, and the experience of the receiving laboratory. The most common approaches include:
- Comparative Testing: This is the most frequently used approach, where both laboratories analyze the same set of samples (e.g., from the same lots) and compare results against predefined acceptance criteria [31] [3] [4]. It is particularly suitable for well-established, validated methods when both labs have similar capabilities.
- Co-validation: In this approach, the receiving laboratory participates in the validation studies, particularly the intermediate precision study that assesses method reproducibility [31] [3]. This strategy is beneficial when methods are transferred before formal validation is complete or when developing methods specifically for multi-site use [30] [4].
- Revalidation: The receiving laboratory performs a full or partial revalidation of the method, repeating some or all validation experiments [31] [3] [7]. This resource-intensive approach is typically used when significant differences exist in lab conditions, equipment, or when the original validation was insufficient [4].
- Transfer Waiver: Under specific, well-justified circumstances, a formal transfer may be waived [3] [7]. Justifications include compendial methods, highly similar products, or when personnel familiar with the method move between laboratories [6] [29]. Waivers require robust scientific justification and documentation [4].
The following workflow illustrates the typical stages of a method transfer process:
Statistical Methods for Data Evaluation
Statistical analysis provides an objective basis for determining whether the acceptance criteria have been met and whether the methods perform equivalently at both laboratories. The choice of statistical method depends on the goal of the transfer and the type of data being evaluated.
Common Statistical Tests
- Comparison of Means (Bias): A t-test can evaluate the lack of bias or comparison of means between two groups, while ANOVA is suitable for comparing more than two groups [30]. Confidence intervals (typically 90% or 95%) are often used to assess the difference between means [30].
- Comparison of Precision: An F-test can compare the precision between two groups, while ANOVA is appropriate for more than two groups [30]. This assesses whether the variability of the method is comparable between laboratories.
- Equivalence Testing: The Two One-Sided t-test (TOST) is a powerful approach for demonstrating statistical equivalence rather than simply rejecting a difference [30]. This method tests whether the mean difference between laboratories falls within a predetermined equivalence interval [30].
- Visual Data Assessment: Graphical tools such as Bland-Altman plots, which display the differences between two measurements against their average, are helpful for visualizing data and identifying any systematic biases or outliers [30].
Advanced Statistical Approaches
For more complex analyses, additional statistical methods may be employed:
- Total Deviation Index and Tolerance Intervals: These methods help define the interval within which a specified proportion (e.g., 95%) of the individual differences between laboratories should lie, which is particularly important for methods where individual measurements are critical [30].
- Intraclass Correlation Coefficient or Concordance Correlation Coefficient: These coefficients are useful for assessing the agreement or equivalence of results between laboratories, as referenced in USP 35 [30].
Essential Research Reagent Solutions and Materials
The successful execution of a method transfer relies on the availability and proper management of specific reagents, standards, and materials. The following table details key items essential for conducting analytical method transfer studies.
Table 3: Essential Research Reagent Solutions and Materials for Method Transfer
| Item Category | Specific Examples | Function & Importance |
|---|---|---|
| Reference Standards | Drug substance standards, impurity standards, system suitability standards [29] | Qualified reference standards are crucial for method calibration, identification, and quantifying analytes; must be traceable and properly characterized [31] [4] |
| Chromatographic Columns | HPLC columns, GC columns [29] | Specific columns (including manufacturer and packing details) are often critical method parameters; spares or equivalent columns should be qualified [29] |
| Critical Reagents & Solvents | Buffers, mobile phase components, derivatization reagents, HPLC-grade solvents [29] | Reagents with specified grade, purity, and pH are essential for robust method performance; differences in reagent sources can affect results [31] [4] |
| Sample Materials | Placebo, drug product batches (multiple strengths if applicable), API, spiked samples [6] [29] | Representative, homogeneous samples are vital for comparative testing; spiked samples with known impurity levels assess accuracy and recovery [7] |
| Specialized Equipment | HPLC/UPLC systems, GC systems, spectrophotometers, dissolution apparatus [29] | Equipment must be properly qualified and calibrated; differences in equipment models between labs must be assessed during transfer [31] [4] |
Best Practices for Successful Method Transfer
Implementing best practices throughout the transfer process significantly enhances the likelihood of a smooth and successful transfer while mitigating potential risks.
Pre-Transfer Assessment and Planning
- Conduct Gap Analysis: Perform a formal assessment of the receiving laboratory's capabilities, including equipment, personnel expertise, and reagent availability, to identify and address potential issues before protocol finalization [30] [4].
- Perform Risk Assessment: Use tools like risk matrices or fishbone diagrams to identify potential sources of variability (equipment, operators, environmental conditions) and implement preventive actions [3] [32].
- Compile Comprehensive Transfer Package: The transferring laboratory should provide a complete package including method validation reports, developmental data, known issues and resolutions, SOPs, and sample chromatograms [31] [29].
Execution and Communication
- Ensure Robust Communication: Establish direct communication channels between analytical experts at both laboratories, with regular follow-up meetings to promptly address issues [3] [4].
- Implement Thorough Training: Beyond procedural review, provide hands-on training to convey tacit knowledge, troubleshooting tips, and critical method nuances that may not be evident in written procedures [30] [3].
- Conduct Feasibility Runs: Preliminary testing at the receiving laboratory before the formal transfer can identify unexpected issues with methodology, equipment, or reagents, preventing protocol failures [30].
Documentation and Post-Transfer Activities
- Document Meticulously: Maintain comprehensive records of all raw data, instrument printouts, calculations, and any deviations encountered during the transfer [4] [7].
- Prepare a Detailed Transfer Report: The final report should summarize all activities, present results and statistical analysis, document any deviations, and provide a clear statement of successful transfer and RU qualification [31] [3].
- Establish Post-Transfer Monitoring: Implement a plan for ongoing monitoring of method performance at the receiving laboratory to ensure continued reliability during routine use [30].
Crafting a robust analytical method transfer protocol is a multifaceted process that requires meticulous planning, clear communication, and scientific rigor. By defining precise objectives and scope, explicitly outlining responsibilities, designing statistically sound experiments, and establishing scientifically justified acceptance criteria, organizations can create a protocol that not only qualifies the receiving laboratory but also ensures the generation of reliable, high-quality data across different sites. A well-executed method transfer, guided by a comprehensive protocol, ultimately safeguards product quality and patient safety while maintaining regulatory compliance in the highly regulated pharmaceutical and biotechnology industries.
In the dynamic landscape of pharmaceutical, biotechnology, and contract research laboratories, the integrity and consistency of analytical data are paramount. Analytical method transfer is a documented process that qualifies a receiving laboratory to use an analytical method that originated in a transferring laboratory, ensuring it yields equivalent results when performed at the receiving site [4] [33]. For researchers, scientists, and drug development professionals, mastering this process is not merely a logistical exercise but a scientific and regulatory imperative that directly impacts product quality, regulatory compliance, and operational efficiency. A poorly executed transfer can lead to delayed product releases, costly retesting, regulatory non-compliance, and ultimately, a loss of confidence in data [4]. This guide provides a comprehensive roadmap through the four essential phases of transfer, supported by experimental protocols and data, to ensure robust and successful method implementation across laboratory sites.
Phase 1: Pre-Transfer - Strategic Planning and Preparation
The Pre-Transfer phase lays the foundation for a successful analytical method transfer. This strategic planning stage involves thorough assessment, team formation, and protocol development to identify and mitigate potential risks before execution begins.
Key Activities and Experimental Protocols
- Team Formation and Scope Definition: A cross-functional team with representatives from Analytical Development, QA/QC, and Operations from both sending and receiving units should be established [34]. This team jointly defines the transfer's scope and objectives, specifically what constitutes a successful transfer (e.g., acceptance criteria for comparability) [4].
- Documentation Gathering and Gap Analysis: The sending unit (SU) provides all relevant method documentation, including validation reports, development reports, standard operating procedures (SOPs), and raw data [4]. The team then performs a detailed gap analysis, comparing equipment, reagents, software, environmental conditions, and personnel expertise between the two labs to identify discrepancies [4] [34].
- Risk Assessment: A risk assessment is conducted to identify potential challenges related to method complexity, equipment differences, or personnel experience. Mitigation strategies are developed, such as additional training for complex methods [4].
- Transfer Approach Selection: Based on the risk assessment, the most appropriate transfer approach is selected [4] [33]. The common strategies are detailed in Table 1.
- Protocol Development: A detailed, pre-approved transfer protocol is the cornerstone of this phase [4]. It must specify the method details, responsibilities of both labs, materials and equipment, the analytical procedure, and pre-defined acceptance criteria for each performance parameter (e.g., %RSD for precision, %recovery for accuracy) [4] [2]. The protocol requires management and QA approval before any experimental work begins [4].
Research Reagent Solutions and Essential Materials
| Item | Function in Pre-Transfer |
|---|---|
| Qualified Reference Standards | Traceable and qualified standards ensure the accuracy and reliability of method performance during testing [4]. |
| Specified Reagents and Solvents | Reagents with defined grades and specifications are critical to ensure consistency and reproducibility between labs [4]. |
| Homogeneous Sample Lots | A single, well-characterized lot of the product, API, or device is prepared to provide consistent material for comparative testing [2]. |
| Method Validation Report | Documented evidence from the SU proving the method is suitable for its intended purpose [4] [33]. |
Table 1: Comparison of Analytical Method Transfer Approaches
| Transfer Approach | Experimental Protocol Description | Best Suited For | Key Statistical Considerations |
|---|---|---|---|
| Comparative Testing [4] [33] | Both labs analyze the same set of samples from a single lot. Results are statistically compared. | Well-established, validated methods; labs with similar capabilities. | t-tests, F-tests, equivalence testing with pre-defined acceptance criteria. |
| Co-validation [4] [33] | The method is validated simultaneously by both the SU and RU in an inter-laboratory study. | New methods being developed for multi-site use. | Assessment of reproducibility across labs; shared validation data. |
| Revalidation [33] | The RU performs a full or partial validation of the method. | Significant differences in lab conditions/equipment; substantial method changes. | Full validation per ICH Q2(R2); evaluation of all relevant performance characteristics. |
| Transfer Waiver [4] [2] | Formal transfer process is waived based on strong justification. | Highly experienced RU using a simple, robust method or pharmacopeial method. | Risk-based justification; no generation of comparative data. |
Phase 2: Transfer Execution - Implementing the Protocol
The Execution phase involves the practical implementation of the approved transfer protocol. This stage focuses on generating reliable data through rigorous experimental work at both laboratories.
Key Activities and Experimental Protocols
- Personnel Training: The receiving unit's analysts are thoroughly trained by the sending unit's personnel on the specific analytical method. All training sessions must be documented to demonstrate proficiency [4] [34].
- Equipment and Material Readiness: The receiving laboratory verifies that all necessary equipment is available, properly qualified, and calibrated according to user specifications and regulatory requirements [2]. The SU ships reference standards, test methods, and the characterized samples to the RU [2].
- Experimental Execution: Both laboratories perform the analytical method according to the approved protocol. For the most common approach, Comparative Testing, the experimental workflow is as follows [4]:
- Sample Preparation: A single, homogeneous lot of the article (product, API, etc.) is used to eliminate manufacturing variability and focus on the method's performance [2].
- Analysis: A predetermined number of replicates of the sample are analyzed by both the SU and RU on their respective, qualified instruments.
- Data Recording: All raw data, instrument printouts, chromatograms, spectra, and calculations are meticulously recorded and maintained. Any deviations from the protocol must be documented in real-time [4].
Research Reagent Solutions and Essential Materials
| Item | Function in Transfer Execution |
|---|---|
| Qualified and Calibrated Equipment | Instruments (e.g., HPLC, UPLC) at the RU must be equivalent to those at the SU and in a state of control to ensure data validity [4] [2]. |
| Stable Test Samples | Samples must remain stable throughout the testing period to ensure that any result discrepancies are due to method performance, not sample degradation [4]. |
| Approved Test Procedure | The unambiguous, step-by-step analytical procedure followed by both labs to ensure consistency [2]. |
| Data Recording System | A robust system (e.g., ELN, LIMS) for recording, storing, and managing all raw data generated during testing [34]. |
Phase 3: Evaluation - Data Analysis and Reporting
The Evaluation phase is where the data generated during execution is rigorously analyzed and compared against the pre-defined acceptance criteria to determine the success of the transfer.
Key Activities and Experimental Protocols
- Data Compilation and Statistical Analysis: All data from both laboratories is collected and compiled. The statistical analysis plan outlined in the protocol is executed. This typically involves [4]:
- Descriptive Statistics: Calculation of mean, standard deviation, and %RSD (Relative Standard Deviation) for precision.
- Comparative Statistics: For comparative testing, statistical tests like t-tests (to compare means) and F-tests (to compare variances) are commonly employed. Equivalence testing is a robust approach to demonstrate that the results from the two labs are equivalent within a pre-specified margin [4].
- Evaluation Against Acceptance Criteria: The compiled results and statistical outputs are compared against the acceptance criteria defined in the transfer protocol. For example, a protocol may state that the %RSD for a specific assay must be ≤2.0% for both labs, and the difference in means between the labs must not be statistically significant at a 95% confidence level [4].
- Deviation Investigation: Any out-of-specification (OOS) results or failures to meet acceptance criteria must be thoroughly investigated. The investigation should determine the root cause, document the findings, and justify any conclusions [4] [34].
- Report Generation: A comprehensive transfer report is drafted. This report summarizes all activities, presents the results and statistical analysis, discusses any deviations, and provides a clear conclusion stating whether the transfer was successful and the receiving laboratory is now qualified to use the method for routine testing [4] [34]. This report requires review and approval by Quality Assurance [4].
Table 2: Example Acceptance Criteria for Key Method Performance Parameters
| Performance Characteristic | Experimental Protocol | Example Acceptance Criteria |
|---|---|---|
| Accuracy (% Recovery) | Analysis of a sample of known concentration (e.g., spiked placebo). | Mean recovery between 98.0% and 102.0% for the RU. |
| Precision (%RSD) | Multiple replicate injections or preparations of a homogeneous sample. | %RSD ≤ 2.0% for both SU and RU results. |
| Specificity | Demonstration that the method can distinguish the analyte from other components. | No interference observed at the retention time of the analyte. |
| Linearity | Analysis of samples across a specified range of concentrations. | Correlation coefficient (r²) ≥ 0.998. |
Phase 4: Post-Transfer - Closure and Implementation
The final phase, Post-Transfer, focuses on closing the project, implementing the method for routine use, and ensuring long-term sustainability.
Key Activities and Experimental Protocols
- SOP Development/Revision: The receiving laboratory formally adopts the method by developing or updating its own Standard Operating Procedures (SOPs) for the analytical procedure, incorporating any site-specific nuances while maintaining equivalency [4].
- Knowledge Management and Archiving: All transfer documentation, including the approved protocol, raw data, and the final report, is archived for future reference and regulatory inspections [34]. This creates a complete knowledge package for the method at the RU.
- Ongoing Monitoring: The method's performance is monitored through the receiving lab's routine quality control systems, such as system suitability tests and ongoing data trending as part of the annual product review [34]. This ensures the method remains in a state of control.
- Project Closeout: A final review confirms that all activities are complete, the RU is fully qualified, and the project can be formally closed. This includes ensuring that stability studies using the transferred method are initiated if required [34].
A successful analytical method transfer is a cornerstone of data integrity in regulated laboratories. By adhering to this structured, four-phase roadmap—Pre-Transfer, Execution, Evaluation, and Post-Transfer—lab managers and scientists can systematically navigate the complexities of transferring methods between sites. This process, underpinned by rigorous planning, clear communication, robust statistical analysis, and comprehensive documentation, ensures that the receiving laboratory can generate reliable, equivalent, and regulatory-compliant data. Ultimately, a well-executed transfer safeguards product quality, accelerates time-to-market, and builds a foundation of confidence in the data that drives critical decisions in drug development.
In the pharmaceutical and biotechnology industries, the transfer of analytical methods between laboratories is a critical process for ensuring consistent product quality, regulatory compliance, and operational flexibility. A successful transfer hinges on a documented process that qualifies a receiving laboratory to perform an analytical procedure with the same accuracy, precision, and reliability as the originating lab [35] [4]. This guide examines the core protocols and success factors, supported by comparative data and detailed workflows, to provide a framework for robust method transfers.
Analytical Method Transfer Protocols: A Comparative Analysis
The choice of transfer protocol is a foundational decision. The most appropriate approach depends on factors such as the method's complexity, its validation status, and the experience level of the receiving laboratory [4]. The following table summarizes the primary protocols, their applications, and typical acceptance criteria.
Table 1: Comparative Analysis of Analytical Method Transfer Protocols
| Transfer Protocol | Core Methodology Description | Best-Suited Context | Key Advantages & Challenges | Typical Acceptance Criteria Examples |
|---|---|---|---|---|
| Comparative Testing [35] [4] [3] | Both originating and receiving labs analyze identical, homogeneous samples. Results are statistically compared. | Well-established, validated methods; labs with similar capabilities [4]. | Advantage: Provides direct, quantitative evidence of equivalence [35].Challenge: Requires careful sample preparation and statistical planning [4]. | - Assay: Absolute difference between site results ≤ 2-3% [3].- Dissolution: Difference in mean results ≤ 10% for <85% dissolved, ≤5% for >85% dissolved [3]. |
| Co-validation [35] [4] [3] | The analytical method is validated simultaneously by both laboratories at the development stage. | New methods intended for multi-site use from the outset [35] [4]. | Advantage: Builds confidence and harmonization from the start [35].Challenge: Requires high collaboration and shared responsibilities; can be resource-intensive [4]. | Criteria are defined based on product specifications and the method's purpose, often aligned with ICH validation parameters (accuracy, precision, etc.) [3]. |
| Revalidation [35] [4] [3] | The receiving laboratory performs a full or partial revalidation of the method. | Significant differences in lab conditions/equipment; substantial method changes; original validation non-compliant [4] [3]. | Advantage: Most rigorous approach, self-contained at the receiving site.Challenge: Highly resource- and time-intensive; requires a full validation protocol [4]. | Acceptance criteria are based on ICH/VICH validation guidelines for parameters like accuracy, precision, linearity, and range [4] [3]. |
| Transfer Waiver [35] [4] [3] | The formal transfer process is waived based on strong scientific justification. | Pharmacopoeial methods (requiring only verification); highly experienced receiving lab with identical conditions [35] [3]. | Advantage: Saves time and resources.Challenge: Rare; requires robust documentation and QA approval; high regulatory scrutiny [4]. | Justification is documented, often citing prior experience, identical equipment, and a simple, robust method [35] [3]. |
Experimental Protocols for a Successful Method Transfer
A structured, phase-based approach is critical for de-risking the method transfer process. The following workflow details the key activities and deliverables for each stage.
Phase 1: Pre-Transfer Planning & Risk Assessment
This initial phase sets the foundation for the entire transfer [4].
- Define Scope & Objectives: Clearly articulate the method(s) being transferred and the pre-defined acceptance criteria for success [4] [3].
- Form Cross-Functional Teams: Designate leads and team members from both transferring and receiving labs, including Analytical Development, QA/QC, and Operations [4].
- Conduct Gap & Risk Analysis: Compare equipment, reagents, software, and personnel expertise between the two labs. A formal risk assessment should identify potential challenges (e.g., complex sample preparation, unique equipment) and develop mitigation strategies [4] [3]. A proactive risk assessment is a cornerstone of a quality-by-design approach.
- Develop Detailed Transfer Protocol: This is the critical controlling document. It must specify method details, responsibilities, materials, experimental design, pre-defined acceptance criteria, and the statistical analysis plan [35] [4] [3].
Phase 2: Execution, Training & Data Generation
This phase focuses on the practical qualification of the receiving laboratory.
- Knowledge Transfer & Training: The transferring lab must effectively convey method-specific knowledge, including critical parameters, common issues, and unwritten techniques ("tacit knowledge") [35] [3]. This may involve on-site training and shadowing to ensure all nuances are captured [3]. Comprehensive training is a cornerstone of successful shift management capabilities in dynamic environments, ensuring personnel are equipped with the necessary knowledge and skills [36].
- Qualify Equipment & Reagents: Verify that equipment at the receiving lab is properly qualified (IQ/OQ/PQ) and calibrated [35] [4]. Use the same lot numbers for critical reagents and reference standards where possible to minimize variability [35] [37].
- Execute Protocol: Both labs perform the analytical method according to the approved protocol, meticulously recording all raw data and any deviations [4].
Phase 3: Data Evaluation, Reporting, and Deviation Management
In this phase, data is rigorously evaluated to determine transfer success.
- Compile & Analyze Data: Collect all data from both laboratories and perform the statistical comparison outlined in the protocol (e.g., t-tests, equivalence testing) [4].
- Compare to Acceptance Criteria: Results are objectively compared against the pre-defined acceptance criteria from the protocol [4] [3].
- Investigate Deviations: Any out-of-specification results or protocol deviations must be thoroughly investigated and documented [4].
- Draft & Approve Final Report: A comprehensive transfer report summarizes the activities, results, and conclusions. It must clearly state whether the transfer was successful and receive formal QA approval [35] [4] [3].
The Scientist's Toolkit: Essential Research Reagent Solutions
The consistency and quality of materials used in a transferred method are paramount. The following table details key reagents and their critical functions.
Table 2: Essential Materials and Reagents for Method Transfer
| Item Category | Critical Function & Impact on Success | Best Practice Guidance |
|---|---|---|
| Reference Standards | Serves as the primary benchmark for quantifying the analyte and establishing method accuracy and linearity [4]. | Use traceable and qualified standards from the same lot at both sites during comparative testing [35] [4]. |
| Critical Reagents | Includes antibodies, enzymes, and specialty chemicals. Performance directly affects specificity, sensitivity, and robustness [37]. | Secure a large enough supply of the same lot for the entire transfer and initial validation. Plan a bridging strategy for future lots [37]. |
| Chromatographic Columns | The specific brand, model, and lot of a column can significantly impact separation resolution and retention times in HPLC/GC methods. | Specify the exact column dimensions, particle size, and chemistry in the method SOP. Test columns from different lots if possible [3] [37]. |
| Sample Preparation Solvents & Buffers | Purity and pH of solvents and buffers can influence extraction recovery, sample stability, and chromatographic baseline. | Detail the specific grades and suppliers of all chemicals in the method. Small differences in buffer preparation can lead to disparate results [37]. |
Visualizing the Risk Assessment and Knowledge Transfer Process
Proactive risk management and effective knowledge transfer are interconnected processes that underpin a successful method transfer. The following diagram illustrates the logical flow of identifying and mitigating risks, which is heavily dependent on the communication of tacit knowledge from the originating lab.
A successful analytical method transfer is not merely a regulatory checkbox but a strategic activity that ensures data integrity and operational excellence across laboratory networks. The critical success factors are interconnected: comprehensive planning provides the roadmap, effective knowledge transfer builds technical capability, and robust training ensures consistent execution. By adopting a structured, risk-based approach with clear protocols and acceptance criteria, laboratories can transform method transfer from a potential bottleneck into a reliable, efficient process that supports global drug development and manufacturing.
This guide compares the performance of different approaches to analytical method transfer, a critical process for ensuring that laboratory methods produce equivalent results when moved between sites, a common requirement in pharmaceutical development and manufacturing.
Analytical Method Transfer Approaches: A Comparative Guide
Selecting the correct transfer strategy is fundamental to success. The choice depends on the method's complexity, risk, and the receiving laboratory's familiarity with the technique [4]. The following table compares the four primary approaches.
Table 1: Comparison of Analytical Method Transfer Approaches
| Transfer Approach | Core Principle & Description | Best Suited For | Key Performance Considerations |
|---|---|---|---|
| Comparative Testing [4] [10] | Both transferring (originating) and receiving laboratories analyze the same set of samples. Results are statistically compared for equivalence. | Well-established, validated methods; laboratories with similar capabilities and equipment [4]. | Requires careful sample homogeneity and a robust statistical plan (e.g., t-tests, F-tests). This is the most common approach [4]. |
| Co-validation [4] [10] | The analytical method is validated simultaneously by both laboratories at the outset. | New methods being developed for multi-site use or significantly revised methods [4]. | Highly resource-intensive but builds confidence early; requires close collaboration and harmonized protocols [4]. |
| Revalidation [4] [10] | The receiving laboratory performs a full or partial revalidation of the method as if it were new. | Significant differences in lab conditions, equipment, or when substantial method changes occur [4]. | The most rigorous approach; requires a full validation protocol and report. It is resource-heavy but addresses major operational differences [4]. |
| Transfer Waiver [4] | The formal transfer process is waived based on strong scientific justification and historical data. | Highly experienced receiving labs using identical conditions and equipment for simple, robust methods [4]. | Rarely used and subject to high regulatory scrutiny; requires extensive documentation and a robust risk assessment [4]. |
Experimental Protocols for Method Transfer
A structured, phase-based protocol is critical for generating reliable, defensible data. The process is a systematic verification that the receiving lab can execute the method successfully [10].
Structured Workflow for Method Transfer
The following diagram visualizes the end-to-end experimental workflow for a successful analytical method transfer.
Diagram 1: Method Transfer Workflow
Phase 1: Pre-Transfer Planning and Protocol Preparation
This foundational phase determines the project's trajectory [4].
- Define Scope and Objectives: Clearly articulate the reason for the transfer and define quantitative success criteria (e.g., acceptance criteria for precision and accuracy) [4].
- Form Cross-Functional Teams: Designate leads and team members from both transferring and receiving labs, including Analytical Development, QA/QC, and Operations [4].
- Conduct Gap and Risk Assessments: Compare equipment, reagents, software, and personnel expertise to identify potential discrepancies. Assess risks related to method complexity and experience [4] [10].
- Develop Detailed Transfer Protocol: This critical document must specify the method details, responsibilities of both labs, materials and equipment, sample preparation, the analytical procedure, predefined acceptance criteria for each performance parameter, the statistical analysis plan, and deviation handling processes [4] [38]. The protocol requires formal approval from all relevant stakeholders, including Quality Assurance (QA) [10].
Phase 2: Execution and Data Generation
This phase involves the practical implementation of the protocol [4].
- Personnel Training: Analysts at the receiving lab must be thoroughly trained by the transferring lab, with all training documented [4] [38].
- Equipment Qualification: Verify that all instruments at the receiving lab are qualified, calibrated, and maintained. Equipment equivalency is a common challenge that must be addressed upfront [4] [10].
- Sample Preparation and Analysis: Prepare homogeneous, representative samples (e.g., production batches, spiked placebos). Both labs then perform the analytical method according to the approved protocol [4].
- Data Documentation: Meticulously record all raw data, instrument printouts, calculations, and any deviations [4].
Phase 3: Data Evaluation and Reporting
The generated data is statistically evaluated against the pre-defined criteria [4].
- Data Compilation and Statistical Analysis: Collect all data from both laboratories and perform the statistical comparison outlined in the protocol (e.g., t-tests, equivalence testing) [4] [10].
- Evaluation Against Acceptance Criteria: Compare the results against the protocol's acceptance criteria. Any deviations or out-of-specification results must be thoroughly investigated [4].
- Draft and Approve Transfer Report: A comprehensive report summarizes the transfer activities, results, statistical analysis, deviations, and conclusions. It must clearly state whether the transfer was successful and requires QA review and approval [4] [38].
Phase 4: Post-Transfer Activities
This phase closes the transfer process and integrates the method into routine operations.
- SOP Development/Revision: The receiving laboratory develops or updates its own Standard Operating Procedures (SOPs) for the transferred method [4].
- Regulatory Filing (if applicable): For critical methods, the transfer results may need to be submitted to regulatory authorities [10].
- Method Approval for Routine Use: Following successful transfer and SOP implementation, the method is approved for routine testing use at the receiving site [38].
The Scientist's Toolkit: Essential Research Reagent Solutions
The consistency of reagents and materials is a critical success factor. Variability in these components is a common challenge during method transfer [10].
Table 2: Key Reagents and Materials for Method Transfer
| Item | Critical Function & Performance Impact |
|---|---|
| Reference Standards [4] [38] | Qualified and traceable standards are essential for system suitability tests, calibration, and determining accuracy. Their purity and stability directly impact result validity. |
| Chromatography Columns [10] | For HPLC/GC methods, the specific column type (e.g., C18), dimensions, and particle size are critical method parameters. Variability between columns from different lots or manufacturers can cause significant result drift. |
| Critical Reagents & Solvents [4] [10] | The grade, purity, and pH of solvents and buffers can affect chromatographic peak shape, retention time, and detection sensitivity. Standardizing sources and grades is crucial. |
| Stable Test Samples [4] | Homogeneous and stable samples (raw materials, finished products) with known characteristics are needed for comparative testing. Sample degradation during shipment can compromise the entire transfer. |
Quantitative Data and Performance Comparison
Supporting experimental data from a published study demonstrates the practical application and success of a method transfer framework.
Case Study: Transfer of a Quantitative PCR Assay
A study transferred a real-time quantitative PCR assay (MammaTyper) used for breast cancer biomarker quantification across three new PCR platforms (CFX96, Applied Biosystems 7500 Fast, Mx3000P), using the LightCycler 480 II as the reference [39].
Table 3: Experimental Performance Data from Cross-Platform Assay Transfer
| Performance Parameter | Experimental Results on Candidate Platforms |
|---|---|
| Quantification Range | 7 log (demonstrated across all tested platforms) [39]. |
| Amplification Efficiency | 97% to 103% (highly comparable across all platforms) [39]. |
| Statistical Equivalence | Successfully confirmed using Bland-Altman and Deming regression analyses to prevent constant and proportional errors [39]. |
| Cross-Platform Agreement | Marker and subtype agreements ranged from 91% to 100%, with κ values between 0.78 and 1.00 (indicating substantial to perfect agreement) [39]. |
| Key Enabler for Success | Platform-specific adjustments of clinical cutoff points were critical to achieving high concordance [39]. |
Navigating Challenges and Implementing Best Practices for a Smooth Transfer
Analytical Method Transfer (AMT) is a critical, documented process that qualifies a receiving laboratory (RL) to reliably perform an analytical procedure originally developed and validated at a transferring laboratory (TL) [4]. Its primary goal is to demonstrate that the RL can execute the method with equivalent accuracy, precision, and reliability as the TL, thereby ensuring data integrity and product quality throughout the drug development lifecycle [4] [40]. These transfers are imperative during scale-up activities, technology shifts, or when outsourcing testing to Contract Research Organizations (CROs) [4].
A successful AMT provides confidence in the consistency of analytical data, which is foundational for regulatory submissions and ensuring patient safety. However, the process is fraught with challenges. A poorly executed transfer can lead to significant delays in product releases, costly retesting, regulatory non-compliance, and a fundamental loss of confidence in data reliability [4]. This guide objectively compares common pitfalls against best practices, providing a structured framework for researchers and drug development professionals to achieve seamless, compliant method transfers.
Comparative Analysis of Common Pitfalls and Best Practices
The success of an AMT hinges on proactively addressing three core areas: defined criteria, robust communication, and comprehensive documentation. The following table summarizes the major pitfalls and their evidence-based solutions.
Table 1: Common Pitfalls in Analytical Method Transfer and Evidence-Based Solutions
| Area of Focus | Common Pitfalls & Impacts | Supported Solutions & Best Practices |
|---|---|---|
| Undefined Acceptance Criteria | • Impact: Inability to objectively conclude transfer success, leading to protracted investigations, rework, and project delays [40].• Root Cause: Ambiguous or missing criteria for key method performance characteristics (e.g., precision, accuracy) [41]. | • Prevention: Develop a detailed, pre-approved transfer protocol with statistically sound, predefined acceptance criteria for all comparative experiments [4] [40].• Application: Use a risk-based methodology to set criteria for parameters like %RSD for precision and %recovery for accuracy [40]. |
| Poor Communication | • Impact: Misunderstandings of method nuances, unaddressed technical issues, and misalignment between labs, causing delays and low team morale [40] [42].• Root Cause: Lack of structured communication channels and defined points of contact [43]. | • Prevention: Establish dedicated teams, schedule regular meetings, and facilitate open knowledge transfer, including hands-on training and troubleshooting tips [4] [44].• Application: Implement a detailed tech stack for streamlined communication among all stakeholders, similar to project scheduling [42]. |
| Inadequate Documentation | • Impact: Inability to reconstruct studies, prove compliance during audits, and defend against legal claims; leads to reputational damage and regulatory actions [45].• Root Cause: Reliance on informal records, incomplete raw data, and lack of a centralized documentation system [45] [41]. | • Prevention: Adopt a documentation management system for version control, audit trails, and a single source of truth [45].• Application: Meticulously maintain all raw data, instrument printouts, and calculations in a final, comprehensive transfer report approved by Quality Assurance [4]. |
Experimental Protocols for Method Transfer
Selecting the appropriate experimental approach is fundamental to a successful transfer. The choice depends on the method's complexity, regulatory status, and the experience level of the receiving lab [4]. The following protocol outlines the most common strategy.
Detailed Protocol: Comparative Testing
1. Objective: To demonstrate equivalence between the TL and RL by statistically comparing results obtained from the analysis of a predefined set of homogeneous samples [4].
2. Materials and Reagents:
- Samples: A sufficient number of homogeneous and representative samples (e.g., approved reference standards, spiked placebo, or production batches from a single lot) [4].
- Reagents: All reagents, solvents, and reference standards, qualified and traceable to a primary reference standard, as specified in the method [4] [46].
- Equipment: Qualified and calibrated instrumentation at both sites. A gap analysis should be performed beforehand to identify and mitigate any significant equipment differences [4].
3. Experimental Procedure:
- Step 1 - Protocol Finalization: The detailed transfer protocol, including all acceptance criteria, must be approved by all parties (TL, RL, and sponsor) before initiation [40].
- Step 2 - Training: RL analysts must be thoroughly trained by the TL, with all training documented to demonstrate proficiency [4].
- Step 3 - Sample Distribution: The characterized samples are distributed to both laboratories under conditions that guarantee their stability [4].
- Step 4 - Concurrent Analysis: Both the TL and RL analyze the samples according to the validated analytical procedure, following their respective Standard Operating Procedures (SOPs) [4].
- Step 5 - Data Recording: All raw data, chromatograms, spectra, and sample preparations are meticulously recorded contemporaneously [4].
4. Data Analysis and Acceptance Criteria:
- The data collected from both labs are compiled and statistically compared using the methods pre-specified in the protocol (e.g., equivalence testing, t-tests, F-tests) [4].
- The results of the statistical comparison are evaluated against the pre-defined acceptance criteria. Any deviation from the protocol or out-of-specification result must be investigated and documented [4].
The workflow for a typical AMT process, from planning to closure, is visualized below.
Comparison of Transfer Approaches
While comparative testing is widely used, other strategies may be more suitable depending on the context. The selection should be justified in the transfer protocol.
Table 2: Comparison of Analytical Method Transfer Approaches
| Transfer Approach | Description | Best Suited For | Key Considerations |
|---|---|---|---|
| Comparative Testing [4] | Both labs analyze identical samples; results are statistically compared for equivalence. | Well-established, validated methods; laboratories with similar capabilities and equipment. | Requires careful sample homogeneity and a robust statistical analysis plan. |
| Co-validation [4] | The analytical method is validated simultaneously by both the TL and RL. | New methods being developed for multi-site use from the outset. | Demands high collaboration and harmonized protocols; can be resource-intensive but builds early confidence. |
| Revalidation [4] | The RL performs a full or partial revalidation of the method. | Transfers to labs with significantly different equipment or environmental conditions, or after substantial method changes. | The most rigorous and resource-intensive approach; requires a full validation protocol and report. |
| Transfer Waiver [4] | The formal transfer process is waived based on strong justification and data. | Highly experienced RL with identical conditions and a history with the method; simple, robust methods. | Rarely granted and subject to high regulatory scrutiny; requires extensive scientific and risk-based justification. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The integrity of an AMT is dependent on the quality and consistency of the materials used. The following table details key reagent solutions and their critical functions in ensuring transfer success.
Table 3: Key Research Reagent Solutions for Analytical Method Transfer
| Item | Function & Importance in AMT |
|---|---|
| Qualified Reference Standards [4] [46] | Certified materials with known purity and identity used to calibrate instruments and validate method performance. Their traceability and stability are paramount for achieving equivalent results across labs. |
| System Suitability Solutions | Mixtures used to verify that the chromatographic or analytical system is operating at the required level of performance (e.g., resolution, precision) before sample analysis begins. |
| Stable, Homogeneous Sample Lots [4] | Well-characterized samples from a single batch, ensuring that any variability in results is due to laboratory performance and not sample inconsistency. |
| Specified Reagents & Solvents [44] | High-grade reagents, solvents, and mobile phases prepared according to detailed, standardized instructions to prevent method variability caused by differences in reagent quality or preparation. |
Navigating the complexities of analytical method transfer requires a disciplined, proactive approach centered on three pillars: defined criteria, robust communication, and rigorous documentation. As demonstrated, failures in these areas have tangible, costly consequences, including project delays, regulatory non-compliance, and irreparable damage to data integrity [45] [4]. Conversely, adopting best practices—such as a pre-approved, detailed protocol, structured communication channels, and a modern documentation management system—transforms the AMT from a potential bottleneck into a streamlined, successful endeavor [45] [4] [40].
For researchers and drug development professionals, mastering this process is not merely a regulatory hurdle but a critical competency that ensures the consistent quality and safety of pharmaceutical products. By implementing the comparative guidelines and experimental protocols outlined in this guide, laboratories can significantly de-risk the transfer process, foster a culture of quality and collaboration, and ultimately accelerate the journey of life-saving drugs to the patients who need them.
The successful transfer of an analytical method from one laboratory to another is a critical juncture in pharmaceutical development and quality control. Analytical Method Transfer (AMT) is formally defined as a documented process that qualifies a receiving laboratory to use an analytical test procedure that originated in another laboratory [29]. The ultimate objective is to ensure that the receiving laboratory is well trained, qualified to run the method in question, and obtains the same results—within experimental error—as the initiating laboratory [7]. Even with a perfectly validated method, the transfer process can reveal significant variability introduced by differences in laboratory ecosystems.
This variability stems from four principal sources: equipment, reagents, environmental conditions, and analyst skills. These factors collectively form a complex web of potential deviations that can compromise data integrity, product quality, and regulatory compliance. As the industry becomes increasingly globalized, with methods frequently transferred between development sites, contract research organizations, and manufacturing facilities worldwide, understanding and controlling these variables has never been more critical [25]. This guide systematically compares the impact of each variable and provides structured experimental approaches to identify, quantify, and control their effects during method transfer.
The following sections break down the core sources of variability, providing a detailed comparison of their nature, impact, and strategies for control.
Analytical Equipment and Instrumentation
Differences in analytical equipment represent one of the most significant sources of variability in method transfer. Even when instruments share the same model number, subtle variations in detector age, maintenance history, and software firmware can alter performance.
Table 1: Impact of Equipment Variations on Analytical Methods
| Equipment Type | Key Performance Parameters | Potential Impact on Method Performance | Comparative Testing Strategy |
|---|---|---|---|
| Chromatography (HPLC/UPLC) | Pump pressure stability, detector wavelength accuracy, column oven temperature | Altered retention times, peak shape, resolution, and quantification [7] | System suitability tests, retention time windows, peak asymmetry measurements |
| Spectroscopy (UV-Vis, IR) | Wavelength accuracy, photometric accuracy, stray light, resolution | Shifted absorption maxima, inaccurate concentration calculations [29] | Holmium oxide filter checks, absorbance accuracy checks at critical wavelengths |
| Mass Spectrometers | Mass accuracy, sensitivity, resolution, ion source contamination | Altered detection limits, signal-to-noise ratios, and isotope pattern fidelity | Tuning with reference standards, sensitivity and resolution verification |
| pH Meters | Electrode sensitivity, calibration slope, temperature compensation | Incorrect pH readings affecting dissolution, stability, and formulation [47] | Multi-point calibration verification with standard buffers |
| Balances | Accuracy, precision, calibration drift, environmental sensitivity | Incorrect sample weighing leading to concentration errors [29] | Calibration with certified weights across the operational range |
Modern laboratories are increasingly adopting innovative tools to mitigate these issues. IoT-enabled smart centrifuges provide real-time monitoring and predictive maintenance alerts, while AI-powered pipetting systems reduce variability in liquid handling [48]. The key to managing equipment variability lies in a robust instrument qualification program and a well-designed system suitability test that is sensitive to the critical parameters of the method.
Reagents and Consumables
The quality, grade, and supplier of reagents and consumables can profoundly influence analytical results. Variations between lots of solvents, buffers, and columns are common pitfalls in method transfer.
Table 2: Impact of Reagent and Consumable Variations
| Reagent/Consumable | Critical Quality Attributes | Impact on Analytical Results | Control and Standardization Strategy |
|---|---|---|---|
| HPLC Grade Solvents | UV cut-off, purity, water content, residual impurities | Elevated baseline noise, ghost peaks, altered retention times [7] | Specify brand, grade, and QC certificates; conduct blank runs |
| Buffer Salts & Reagents | Purity, pH, molarity, microbial contamination | Shifted pH impacting ionization and retention; degraded mobile phase | Specify source and grade; define shelf-life and re-standardization frequency |
| Chromatography Columns | Stationary phase lot, column efficiency (N), tailing factor | Changes in selectivity, resolution, and peak symmetry [7] | Specify brand, dimensions, and particle size; test with standard mixes before use |
| Reference Standards | Purity, qualification, moisture content, stability | Absolute errors in quantification for assays and impurities [29] | Use of qualified and traceable standards from certified sources |
| Water Purity | Resistivity, TOC, microbial count | Contamination, elevated background, degradation of analytes | Define required grade (e.g., Type I for HPLC); monitor quality regularly |
The trend toward Green Analytical Chemistry (GAC) is also influencing reagent selection, with tools like AGREE and HEXAGON being developed to assess the environmental impact of analytical methods, including reagent hazards [49]. During method transfer, it is crucial to document and standardize the sources and grades of all critical reagents to ensure consistency.
Environmental Conditions
Laboratory environments are not always controlled to the same degree, and subtle differences can affect both equipment performance and chemical stability.
Table 3: Impact of Environmental Conditions
| Environmental Factor | Typical Laboratory Range | Potential Impact on Analysis | Mitigation Approach |
|---|---|---|---|
| Ambient Temperature | 15°C - 30°C (depending on climate control) | Affects kinetics of reactions, column temperature, solvent evaporation [47] | Use temperature-controlled analytical spaces; specify allowable ranges in the method |
| Relative Humidity | 20% - 80% (seasonal variations) | Hydration of hygroscopic samples and salts; impacts Karl Fischer titration [47] | Control humidity for sensitive analyses; use desiccators for standards/samples |
| Vibration & Acoustic Noise | Variable by location (e.g., near machinery) | Degrades resolution in sensitive instruments like balances and microscopes [47] | Install instruments on vibration-damping tables; avoid high-traffic areas |
| Light Exposure | Variable | Photodegradation of light-sensitive compounds (e.g., vitamins, nitro compounds) | Use low-actinic glassware; specify light-handling conditions in the method |
The growing market for environmental test equipment, projected to grow at a CAGR of 6.8% to reach USD 2,440.5 million by 2035, underscores the increasing importance of monitoring and controlling these conditions [47]. Portable and mobile monitoring platforms are making it easier to perform real-time environmental assessments [47].
Analyst Skills and Techniques
The human element remains a significant and sometimes unpredictable variable. Analyst skills, experience, and technique can introduce both random and systematic errors.
Table 4: Impact of Analyst Techniques and Proficiency
| Analyst Skill Domain | Manual Technique Variables | Impact on Data Quality | Standardization through Training & Tools |
|---|---|---|---|
| Sample Preparation | Pipetting technique, mixing time/vigor, extraction time, dilution scheme | Errors in concentration, recovery, and homogeneity [3] | Detailed written procedures; hands-on training; use of automated liquid handlers [48] |
| Instrument Operation | Sample injection technique, sequence programming, integration parameters | Variations in detected response, carryover, and peak integration [7] | Shared training videos; on-site observation; predefined integration rules |
| Data Interpretation & Calculation | Understanding of SOP, statistical knowledge, outlier rejection criteria | Incorrect results, reporting errors, invalid OOS investigations [3] | Clear instructions for calculations; use of automated data systems; second-person verification |
| Troubleshooting Acumen | Ability to recognize and respond to system suitability failures | Method downtime, invalid runs, and repeated testing [25] | Knowledge transfer from sending unit; documentation of "tacit knowledge" [3] |
The Pharmaceutical Research and Manufacturers of America (PhRMA) emphasizes that successful transfer relies on the receiving laboratory having the procedural knowledge and ability to perform the method as intended [7]. This is achieved not just through documentation, but through effective communication and, for complex methods, potentially on-site training to transfer the invaluable "tacit knowledge" not captured in written procedures [3].
Experimental Protocols for Evaluating Laboratory Differences
A successful method transfer is protocol-driven. The following experimental methodologies are designed to systematically isolate and evaluate the impact of each variable.
Protocol for Comparative Testing (The Most Common Approach)
Comparative testing is the most frequently used AMT option, where both the sending (TU) and receiving (RU) laboratories analyze the same set of samples against pre-defined acceptance criteria [3] [7].
- Step 1: Preparation of the Transfer Package: The TU compiles and sends a comprehensive package to the RU. This must include the approved analytical method, the full method validation report, details on critical reagents and columns, and any known method nuances or "silent knowledge" [29].
- Step 2: Protocol Development: A detailed, pre-approved transfer protocol is essential. It must define:
- Objective and Scope: The specific methods and products covered.
- Responsibilities: Clear roles for both TU and RU.
- Experimental Design: The number of batches, replicates, and injections. For a drug product with multiple strengths, testing typically includes the lowest and highest strength [29].
- Acceptance Criteria: Predefined, scientifically justified limits for comparison.
- Step 3: Execution and Analysis: Both laboratories analyze homogeneous samples from the same lots, typically using a minimum of one batch for an API or a single-strength drug product [29]. The results are statistically compared using pre-defined tests (e.g., F-test for precision, t-test for bias).
The diagram below outlines the core workflow and decision points in a standard analytical method transfer.
Figure 1: Analytical Method Transfer Workflow. This flowchart outlines the key stages in a standard transfer process, from initiation to successful completion, highlighting critical decision points [3] [29] [7].
Establishing Acceptance Criteria for Comparison
The acceptance criteria in the transfer protocol are the objective metrics for success. They should be based on the method's validation data and performance characteristics.
Table 5: Typical Acceptance Criteria for Method Transfer [3]
| Test Type | Typical Acceptance Criteria | Statistical Evaluation & Rationale |
|---|---|---|
| Identification | Positive (or negative) identification obtained at the receiving site. | Qualitative pass/fail; no statistical analysis required. |
| Assay | Absolute difference between the mean results of the two sites should be ≤ 2-3%. | T-test for significant difference of means; ensures accuracy is maintained. |
| Related Substances (Impurities) | Criteria vary by impurity level. For impurities at low levels, recovery of 80-120% for spiked samples is common. | More generous criteria for low-level impurities account for higher relative error. |
| Dissolution | Absolute difference in mean results: NMT 10% at <85% dissolved; NMT 5% at >85% dissolved. | Ensures performance characteristics of the dosage form are consistently measured. |
Alternative Transfer Approaches
While comparative testing is common, other strategic approaches can be employed based on context and risk.
- Covalidation: The receiving laboratory participates in the original method validation study, typically by contributing to the intermediate precision (reproducibility) testing. This validates the method and qualifies the site simultaneously, saving time and resources [25] [7].
- Revalidation or Partial Revalidation: The receiving laboratory repeats some or all of the validation experiments. This is resource-intensive but may be necessary if the method is critical, has a complex history, or if significant differences are anticipated [3].
- Transfer Waiver: A formal transfer is omitted with proper justification. This is applicable for compendial methods (e.g., pH, Loss on Drying) that only require verification, or if the personnel responsible for the method are moving to the new laboratory [3] [29] [7].
The choice of strategy should be based on the method's complexity, criticality, and the risk associated with the transfer.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and tools critical for executing a successful method transfer, as identified in the experimental protocols and market analysis.
Table 6: Essential Research Reagent Solutions for Method Transfer
| Item Category | Specific Examples | Critical Function in Method Transfer |
|---|---|---|
| Chromatography Columns | C18, C8, phenyl, HILIC columns from specified manufacturers | The stationary phase is critical for achieving the required separation, selectivity, and retention; lot-to-lot variability is a key risk [7]. |
| Chemical Reference Standards | Qualified drug substance, impurity, and degradation standards | Provides the basis for accurate quantification, identification, and method calibration; purity and traceability are paramount [29]. |
| High-Purity Solvents & Reagents | HPLC-grade solvents, LC-MS grade solvents, buffer salts | Minimizes baseline noise and interfering peaks, ensuring the accuracy and sensitivity of the analysis [7]. |
| System Suitability Test Mixtures | USP resolution mixtures, tailing factor check solutions | Verifies that the chromatographic system is performing adequately and is equivalent to the system used during validation [7]. |
| Stable, Homogeneous Test Samples | API, drug product from a single, well-characterized batch | Provides a consistent material for both laboratories to test, ensuring that observed differences are due to the laboratory and not the sample [3]. |
| AI-Powered & Automated Tools | AI pipetting systems, robotic liquid handlers, cloud-integrated digital lab notebooks (ELN) | Reduces human-induced variability in sample prep, improves data integrity, and facilitates real-time collaboration and data sharing [48]. |
Strategic Framework for Mitigating Variability
A proactive, strategic approach is required to navigate the complexities of laboratory differences. The following framework synthesizes the findings into actionable strategies.
- Strategy 1: Prioritize Knowledge Transfer Over Data Transfer: The most critical factor for success is often the quality of communication between laboratories [3]. This begins with introducing the teams and establishing direct lines of communication between analytical experts. The goal is to transfer the "tacit knowledge"—the unwritten tips and tricks learned through experience with the method [3].
- Strategy 2: Implement a Risk-Based Approach to Transfer: Not all methods require the same level of rigor. The transfer strategy should be based on the method's complexity and criticality. A simple pH method may require only verification, while a complex impurity method may need a full comparative test with stringent statistical criteria [25]. This aligns with the fit-for-purpose concept in method validation and transfer [25].
- Strategy 3: Leverage Technology for Consistency and Monitoring: Investing in modern, connected lab tools can directly mitigate variability. IoT-enabled equipment provides real-time performance monitoring, while cloud-based ELNs and LIMS ensure all sites work with the same version of methods and data [50] [48]. Automated systems for sample preparation and analysis reduce the most significant variable: the analyst.
- Strategy 4: Design Robust Methods from the Outset: A method that is sensitive to minor equipment or reagent changes is destined for a difficult transfer. Incorporating robustness testing during the method development and validation phases is a crucial investment [7]. This involves deliberately varying critical parameters (e.g., pH, temperature, flow rate) to establish a method's tolerance, creating a more forgiving and transferable procedure.
The following diagram illustrates this strategic framework as an iterative cycle for continuous quality improvement.
Figure 2: Strategic Framework for Mitigation. This diagram visualizes the four core strategies as an interconnected cycle, emphasizing that feedback from successful transfers should inform future knowledge transfer and method design [3] [25] [48].
The transfer of an analytical method between laboratories is a rigorous test of its robustness and a critical step in the pharmaceutical product lifecycle. Variability introduced by differences in equipment, reagents, environmental conditions, and analyst skills is not merely a theoretical concern but a practical challenge with significant implications for product quality and regulatory compliance. By systematically deconstructing these sources of variation through structured comparative experiments, as outlined in this guide, organizations can objectively quantify risk and implement effective controls. The ultimate goal is to move beyond a simple checklist of transfer activities and foster a holistic strategy centered on proactive communication, risk management, and technological investment. In doing so, the promise of a robust, reproducible, and transferable analytical method becomes a sustainable reality, ensuring drug quality and patient safety regardless of where the test is performed.
Mitigating Risk Through Pilot Testing, Gap Analysis, and Hands-On Training
In the highly regulated pharmaceutical industry, the transfer of analytical methods between laboratories is a critical process. Its success is paramount for ensuring consistent drug quality, maintaining regulatory compliance, and facilitating smooth technology transfers to new manufacturing or testing sites [10]. A failed transfer can lead to significant delays, costly investigations, and compromised product quality [4]. This guide objectively compares the performance of three core risk-mitigation strategies—Pilot Testing, Gap Analysis, and Hands-On Training—by synthesizing experimental data and established protocols. The evidence conclusively demonstrates that an integrated approach, leveraging all three strategies, is most effective for ensuring robust and reliable analytical method transfer.
Experimental Protocols for Risk Mitigation
To objectively compare the effectiveness of different risk-mitigation strategies, the following standardized protocols were executed. These methodologies are aligned with regulatory guidance from bodies such as the FDA, EMA, and USP〈1224〉 [10].
Protocol 1: Comparative Pilot Testing
Objective: To verify that a receiving laboratory can execute a transferred analytical method and generate results equivalent to those from the transferring laboratory [4] [10].
Methodology:
- Sample Preparation: A single, homogeneous batch of a drug product or substance is selected and characterized. For impurity methods, samples may be spiked with known quantities of impurities to ensure accurate recovery measurements [3].
- Parallel Testing: Both the transferring (sending) and receiving laboratories analyze the same set of samples using the identical analytical method. A minimum of six determinations per lab is often standard [3].
- Data Comparison: Results from both laboratories for key parameters (e.g., assay potency, impurity content, dissolution) are statistically compared using appropriate tools such as t-tests, F-tests, or equivalence testing [4] [10].
Success Criteria: The method transfer is considered successful if the results from both laboratories meet pre-defined acceptance criteria for accuracy and precision, demonstrating statistical equivalence [3].
Protocol 2: Structured Gap Analysis
Objective: To systematically identify and document the differences ("gaps") between the current capabilities of the receiving laboratory and the requirements for successfully executing the analytical method [51].
Methodology:
- Framework Selection: A specific framework or standard is selected for comparison, such as the method's own validation report or a quality standard like ISO 27001 [51].
- Data Collection: The receiving laboratory's equipment, personnel skills, reagents, and environmental conditions are meticulously assessed against the method's specifications. This involves document review, personnel interviews, and equipment qualification checks [4] [10].
- Gap Identification: A formal report is generated that lists the method's requirements, the receiving lab's current state for each requirement, and identifies any gaps [51].
Success Criteria: The analysis is deemed complete when all potential gaps have been identified, documented, and a targeted plan to address each gap has been established [52].
Protocol 3: Hands-On Analyst Training
Objective: To qualify analysts at the receiving laboratory and ensure they possess the practical skill and theoretical knowledge to perform the method consistently [3].
Methodology:
- Knowledge Transfer: The transferring laboratory provides the receiving laboratory with all method documentation, including the validation report, standard operating procedures (SOPs), and historical data [10].
- Structured Training: Analysts from the receiving lab undergo both theoretical training and practical, hands-on sessions. This is ideally conducted by an expert from the transferring laboratory and may include on-site or virtual training [3].
- Proficiency Assessment: Analysts demonstrate their proficiency by successfully analyzing pre-defined samples, with their results evaluated against established benchmarks [4].
Success Criteria: All analysts at the receiving laboratory demonstrate consistent and accurate execution of the method, with their results falling within pre-defined acceptance limits [4].
Comparative Performance Data
The three protocols were evaluated based on their ability to mitigate common transfer risks, their resource requirements, and their overall impact on transfer success. The quantitative and qualitative findings are summarized in the table below.
Table 1: Comparative Performance of Risk Mitigation Strategies in Method Transfer
| Strategy | Primary Risk Mitigated | Quantitative Success Metric | Typical Acceptance Criteria | Resource Intensity | Key Strengths |
|---|---|---|---|---|---|
| Pilot Testing | Technical/Procedural | Statistical equivalence of results between labs [3]. | Assay: Absolute difference ≤ 2-3% [3]. | High (Time, Samples) | Provides objective, data-driven proof of equivalence [10]. |
| Gap Analysis | Informational/Compliance | Percentage of pre-transfer gaps addressed [51]. | >95% of critical gaps closed prior to testing. | Medium (Planning, Documentation) | Proactively prevents problems; reduces costly delays [51]. |
| Hands-On Training | Personnel Proficiency | Pass rate of analysts during proficiency assessment [4]. | 100% of analysts meet proficiency standards. | Medium (Trainer Time, Logistics) | Builds analyst confidence; transfers tacit knowledge not in documents [3]. |
Integrated Workflow for Optimal Risk Mitigation
The individual strategies are most effective when deployed in a coordinated, sequential manner. The following workflow illustrates the logical relationship between Gap Analysis, Hands-On Training, and Pilot Testing, showing how they form a comprehensive risk mitigation pipeline.
The workflow shows that Gap Analysis is the foundational step, identifying required actions for training and preparation. Hands-On Training directly addresses personnel competency gaps, while Pilot Testing serves as the final, objective validation. A failure at the Pilot Testing stage feeds back into the system, requiring re-training for skill-based issues or a re-assessment of foundational gaps for systemic problems.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method transfer relies on more than just protocols; it depends on the consistent use of high-quality materials. The following table details key reagent solutions and their critical functions in ensuring data reliability.
Table 2: Key Research Reagent Solutions for Analytical Method Transfer
| Item | Function | Criticality for Transfer |
|---|---|---|
| Chemical Reference Standards | Qualified substances used to calibrate equipment and quantify results [4]. | High: Variations between labs can cause significant result偏差. Must be traceable and from a qualified source [10]. |
| HPLC/GC Columns | The stationary phase for chromatographic separation. | High: Differences in column brand, model, or lot can drastically alter separation and retention times, leading to transfer failure [10]. |
| System Suitability Test (SST) Materials | A reference preparation used to verify the chromatographic system's performance before analysis [10]. | High: SST is the daily check that ensures the method is performing as validated. Both labs must achieve SST criteria with the same material. |
| Stable Test Samples | Homogeneous and characterized samples (e.g., drug substance, finished product) for comparative testing [4]. | Medium-High: Sample instability or heterogeneity during transport and storage can invalidate comparative testing results [10]. |
| Certified Reagents & Solvents | High-purity solvents and chemicals for mobile phase and sample preparation. | Medium: Impurities or grade inconsistencies can introduce noise, ghost peaks, or baseline drift, affecting method robustness [10]. |
Data from standardized experimental protocols confirms that Pilot Testing, Gap Analysis, and Hands-On Training are not interchangeable strategies but are complementary pillars of a robust method transfer program. While Pilot Testing provides the definitive, quantitative proof of success, its outcome is heavily dependent on the proactive foundation laid by Gap Analysis and the competency assurance provided by Hands-On Training. For researchers and drug development professionals, adopting this integrated, data-driven approach is not merely a best practice—it is a critical investment in mitigating risk, ensuring regulatory compliance, and safeguarding product quality throughout the method lifecycle.
In the highly regulated world of pharmaceutical research and development, the successful transfer of analytical methods between laboratories is a critical milestone. While technical parameters and statistical equivalence are the documented backbone of any transfer, the human element of communication is often the true determinant of success. This guide explores how structured communication—through team introductions, regular meetings, and the deliberate sharing of tacit knowledge—forms an indispensable framework for achieving reproducible and compliant method transfers.
Defining the Communication and Knowledge Landscape
In the context of analytical method transfer, robust communication is a documented process that ensures continuous, clear, and unambiguous information flow between the transferring (sending) and receiving laboratories [3]. Its primary goal is to qualify the receiving lab to execute the method with the same accuracy, precision, and reliability as the originating lab [4].
A crucial component of this communication is the exchange of tacit knowledge—the unwritten, intuitive know-how gained through personal experience [53]. Unlike explicit knowledge found in standard operating procedures (SOPs) or manuals, tacit knowledge includes the "silent" understanding of how to handle a delicate sample, interpret a subtle chromatographic shift, or troubleshoot an instrument on the fly [3]. This knowledge is notoriously difficult to articulate but is essential for replicating complex analytical methods [53].
The following diagram illustrates how these elements interact throughout the method transfer lifecycle.
Experimental Evidence: Quantifying Communication's Impact
While the qualitative benefits of good communication are clear, its impact can also be observed through experimental outcomes and compliance data. The following table summarizes key performance indicators linked to communication strategies.
Table 1: Impact of Communication Strategies on Method Transfer Outcomes
| Communication Strategy | Experimental/Operational Metric | Quantified Impact / Evidence |
|---|---|---|
| Structured Kick-off Meetings [3] | Reduction in protocol deviations and major errors | Lower incidence of out-of-specification (OOS) results due to clearer understanding of critical method parameters [3]. |
| Co-validation Approach [4] [12] | Statistical comparability of results (e.g., via F-test, t-test) | Demonstrated equivalence in inter-laboratory precision and accuracy, meeting pre-set acceptance criteria [4]. |
| Hands-on Training & Shadowing [54] | Analyst proficiency and time-to-competency | Reduced analyst training time and fewer repeated assays; successful execution of the method on first attempt [3]. |
| Tacit Knowledge Sharing [53] [3] | Successful troubleshooting of instrument/ method nuances | Prevention of recurring issues (e.g., peak splitting in HPLC) that are not detailed in the written method [3]. |
| Regular Follow-up Meetings [4] | Project timeline adherence | Mitigation of delays through proactive issue resolution; overall transfer process completed up to 30% faster [4]. |
Adherence to predefined acceptance criteria is a fundamental requirement. The table below provides typical statistical thresholds used to demonstrate equivalence between laboratories.
Table 2: Typical Acceptance Criteria for Comparative Method Transfer (e.g., Assay)
| Performance Parameter | Common Acceptance Criteria | Statistical/Methodological Basis |
|---|---|---|
| Assay Accuracy/Precision | Absolute difference between site means: ≤ 2-3% [3]. | Two-sample t-test comparing means from both labs; F-test for variance comparison [4] [10]. |
| Related Substances (Impurities) | Recovery of spiked impurities: 80-120% [3]. | Statistical comparison of results for impurities at or near the specification threshold [3]. |
| System Suitability | Meeting all system suitability criteria as per the validated method at both sites [10]. | Direct comparison of chromatographic parameters (e.g., retention time, tailing factor, theoretical plates) [4]. |
| Dissolution | Absolute difference in mean results: ≤ 10% at <85% dissolved; ≤ 5% at >85% dissolved [3]. | Comparison of dissolution profiles at multiple time points using model-independent or statistical methods [10]. |
Detailed Protocols for Key Communication Experiments
Implementing the theoretical framework requires practical, actionable protocols. The following section details methodologies for key activities that integrate communication and tacit knowledge sharing into the method transfer process.
Protocol for a Cross-Functional Kick-off Meeting
Objective: To align the transferring and receiving laboratories on the scope, responsibilities, and critical parameters of the method transfer, ensuring a shared understanding from the outset [4] [3].
Materials:
- Meeting participants: Lead analysts, lab managers, QA representatives, and project managers from both sites [4].
- Documentation: Method validation report, draft transfer protocol, and any prior risk assessments [3].
Methodology:
- Team Introductions (Socialization): Begin with formal introductions, establishing clear points of contact for technical and quality matters [3]. This builds the foundation for trust and open dialogue.
- Method Walkthrough: The transferring lab leads a detailed review of the analytical procedure, highlighting steps known to be critical or prone to variability [4].
- Gap Analysis Discussion: Jointly review equipment (make, model, software versions), reagents (grades, suppliers), and column specifications to identify and plan for any discrepancies [4] [10].
- Tacit Knowledge Elicitation: The transferring lab shares undocumented "tribal knowledge," such as specific column conditioning techniques, subtle visual cues for endpoint determination, or common instrumentation faults and their fixes [3].
- Protocol Finalization: Collaboratively review and finalize the transfer protocol, ensuring acceptance criteria are understood and agreed upon by all parties [4].
Protocol for Tacit Knowledge Capture via Hands-on Training
Objective: To transfer the implicit skills and judgment required to perform the method consistently, which cannot be fully conveyed through written documentation alone [53] [54].
Materials:
- Fully qualified instrumentation and materials at the receiving lab.
- A veteran analyst from the transferring lab and the trainee analyst(s) from the receiving lab.
- Representative samples for testing.
Methodology:
- Demonstration (Observation): The veteran analyst performs the entire method while providing a live, narrated commentary. They explicitly state the "why" behind actions, such as, "I degas the solvent for exactly 10 minutes because less time leads to bubble formation in the HPLC detector cell" [54].
- Guided Execution (Internalization): The trainee analyst performs the method under the close supervision of the expert. The expert provides immediate feedback on technique, such as pipetting posture or sample vial capping [54].
- Structured Shadowing: The trainee shadows the expert for a predetermined period, observing not just the analysis but also the preparatory and data review processes [54].
- Troubleshooting Simulation: The expert intentionally creates a minor, reversible fault (e.g., a slightly loose HPLC connection) and guides the trainee through the diagnostic process, thereby transferring problem-solving heuristics [3].
The Scientist's Toolkit: Essential Reagents for Effective Transfers
Beyond chemical reagents, a successful transfer requires "reagents" for communication and knowledge management. The following table details these essential components.
Table 3: Key Research Reagent Solutions for Communication and Knowledge Management
| Tool / Resource | Function in Method Transfer | Specific Application Example |
|---|---|---|
| Structured Communication Platform (e.g., MS Teams, Slack) | Enables real-time, documented communication between sites for quick issue resolution and daily updates. | Creating a dedicated channel for the transfer project to share chromatograms and discuss minor deviations instantly. |
| Electronic Lab Notebook (ELN) | Provides a centralized, structured repository for explicit knowledge (protocols, data) and tacit knowledge (annotations, observations) [4]. | Annotating an SOP within the ELN with a video clip showing the correct sample vortexing technique to achieve a specific suspension. |
| Knowledge Management System (KMS) | Captures and organizes knowledge from completed transfers for future reference and onboarding, preventing knowledge loss [54]. | Storing the final transfer report, along with a "lessons learned" document that details a previously encountered column stability issue. |
| Videoconferencing Tools | Facilitates regular face-to-face meetings and virtual training sessions, which are crucial for building rapport and demonstrating techniques [4]. | Conducting a virtual "over-the-shoulder" session where the sending lab streams a live feed of a complex sample preparation step. |
| Mentorship Program Framework | Provides a structured mechanism for tacit knowledge transfer from senior to junior scientists outside of a specific transfer project [53]. | Pairing a new hire with an experienced scientist, accelerating their understanding of lab-specific practices and unwritten standards. |
The workflow of how these tools support the key knowledge conversion processes defined by the SECI model is shown below.
In the rigorous, data-driven world of analytical science, it can be tempting to focus solely on statistical equivalence and regulatory checkboxes. However, a method transfer is ultimately a human collaboration. Robust communication—facilitated by well-defined teams, regular meetings, and a conscious effort to share tacit knowledge—is not a supportive activity but a core scientific and operational necessity. By formally integrating these "soft" skills into the transfer protocol, organizations can consistently achieve a higher first-time success rate, foster a culture of continuous learning, and ensure that the quality and efficacy of pharmaceutical products remain uncompromised across global laboratories.
In the modern pharmaceutical landscape, the reliable transfer of analytical methods between laboratories is a critical, yet complex, cornerstone of drug development and manufacturing. This process ensures that an analytical procedure, when performed at a receiving laboratory (RL), yields equivalent results to those obtained at the transferring laboratory (TL), thereby guaranteeing consistent product quality and patient safety [4]. However, this fundamental activity is now undertaken within a context of heightened regulatory scrutiny and an increasingly fragmented outsourcing ecosystem.
Companies today frequently engage multiple, siloed partners for various aspects of manufacturing and testing [55]. This fragmentation places a greater burden of vetting and qualification on sponsors and can lead to significant challenges in coordination, consistency, and knowledge transfer. Furthermore, regulatory bodies like the FDA and EMA, along with compendial standards such as USP General Chapter 〈1224〉, have clearly defined expectations for demonstrating method equivalence [10]. Navigating this environment requires a strategic, well-documented, and collaborative approach to Analytical Method Transfer (AMT) to avoid costly delays, compliance issues, and a loss of confidence in data integrity [4].
The Fragmented Outsourcing Landscape: Challenges and Impacts
The trend toward outsourcing mRNA manufacturing and other complex processes has revealed a fragmented landscape that introduces specific, systemic challenges for method transfer.
- Coordination and Consistency Issues: Managing multiple suppliers, each with different processes and protocols, creates knowledge siloes and potential inconsistencies in how analytical methods are executed [55]. This lack of cohesion can hinder scalability and complicate the technology transfer process.
- Increased Risk and Vetting Burden: The involvement of numerous suppliers increases the overall risk factor, with a higher chance of quality issues or delays that can directly impact time to market for critical programs [55]. Sponsors must undertake a significant burden of qualifying each new partner.
- Limited Flexibility: Being locked into contracts with multiple suppliers or facing challenges in coordinating production and testing schedules can reduce a company's operational flexibility and ability to respond quickly to changing project needs [55].
Table: Key Challenges in a Fragmented Outsourcing Model
| Challenge | Impact on Method Transfer & Operations |
|---|---|
| Knowledge Silos | Inconsistent method execution, hindered troubleshooting, and disrupted technology transfer between partners [55]. |
| Logistical Coordination | Difficulties in managing timelines, sample stability during transport, and aligning protocols across multiple partners [10] [55]. |
| Increased Vetting Burden | Significant resources required to qualify and audit each new supplier to ensure compliance and capability [55]. |
| Inconsistent Quality | Higher risk of quality issues and delays, impacting the reliability of data and potentially delaying regulatory submissions [55]. |
Increased Regulatory Scrutiny: A Framework for Compliance
Regulatory agencies globally mandate that transferred methods must be performed with the same accuracy, precision, and reliability at the receiving unit as at the originating laboratory [4]. Adherence to established guidelines is non-negotiable for regulatory success.
Key Regulatory Guidelines
A robust method transfer strategy is built upon a foundation of compliance with several key guidelines:
- USP 〈1224〉: Provides a foundational framework for the transfer of analytical procedures, outlining common transfer approaches [4] [10].
- ICH Q2(R1): Defines the validation of analytical procedures, the parameters of which often form the basis for transfer acceptance criteria [10].
- FDA & EMA Guidance: Both agencies have issued specific guidance documents (FDA, 2015; EMA, 2014) that outline expectations for method reliability and transfer data [10].
Standardized Transfer Approaches
Regulatory guidelines typically recognize several formal approaches to method transfer, each suited to different scenarios:
- Comparative Testing: This is the most common approach, where both the TL and RL analyze a predefined set of identical samples. The results are statistically compared against pre-defined acceptance criteria to demonstrate equivalence [4] [10] [3].
- Co-validation: The receiving laboratory is involved as part of the validation team during the initial method validation. This approach is ideal for new methods being developed for multi-site use and establishes inter-laboratory reproducibility from the outset [4] [12].
- Revalidation: The RL performs a full or partial revalidation of the method. This is the most rigorous approach and is used when there are significant differences in equipment or lab environment, or when the original validation is insufficient [4] [10].
- Transfer Waiver: In rare, well-justified cases, the formal transfer process may be waived. Justifications can include the transfer of a simple compendial method or when highly experienced personnel move between labs with identical conditions [4] [10].
Table: Comparison of Analytical Method Transfer Approaches
| Transfer Approach | Description | Best Suited For | Key Considerations |
|---|---|---|---|
| Comparative Testing | Both labs analyze same samples; results statistically compared [4]. | Established, validated methods; similar lab capabilities [4]. | Requires robust statistical analysis, homogeneous samples, and a detailed protocol [4]. |
| Co-validation | Method validated simultaneously by both labs as part of the validation team [4] [12]. | New methods; methods developed for multi-site use from the outset [4]. | Requires high collaboration, harmonized protocols, and shared responsibilities [4]. |
| Revalidation | Receiving lab performs a full or partial revalidation of the method [4]. | Significant differences in lab conditions/equipment; substantial method changes [4]. | Most resource-intensive; requires a full validation protocol and report [4]. |
| Transfer Waiver | Transfer process formally waived based on strong justification [4]. | Highly experienced receiving lab; identical conditions; simple, robust methods [4] [3]. | Rare; subject to high regulatory scrutiny; requires robust scientific and risk-based justification [4]. |
Optimizing for the Future: Best Practices and Strategic Solutions
To overcome the challenges of fragmentation and meet regulatory demands, laboratories must adopt a strategic and proactive approach to method transfer.
A Structured Roadmap for Successful Transfer
A well-defined, phased process is critical for de-risking method transfer.
The workflow for a successful Analytical Method Transfer is a structured, multi-phase process. It begins with Pre-Transfer Planning, which involves a gap analysis and risk assessment to identify potential issues in equipment, training, or reagents, followed by the development of a detailed protocol defining objectives and acceptance criteria [4] [8]. The process then moves to the Execution phase, where personnel from the receiving lab are trained, and both laboratories generate data according to the approved protocol [4]. Next, in the Evaluation & Reporting phase, data is statistically compared against the pre-defined criteria, and a comprehensive transfer report is compiled and approved by Quality Assurance [4] [10]. Finally, Post-Transfer activities include the implementation of Standard Operating Procedures (SOPs) at the receiving lab for routine use of the method [4].
The Scientist's Toolkit: Essential Research Reagent Solutions
The consistency of key materials is a fundamental factor in the success of a method transfer. Variations in reagents and supplies are a common source of failure.
Table: Essential Materials for Robust Method Transfer
| Material/Solution | Critical Function | Best Practice for Consistency |
|---|---|---|
| Reference Standards | Serves as the primary benchmark for quantifying the analyte and establishing method accuracy [10]. | Use traceable and qualified standards from the same batch across both labs to ensure comparability [4]. |
| Chromatography Columns | The heart of HPLC/UPLC methods; directly impacts retention time, resolution, and peak shape [10]. | Use columns with identical stationary phases (e.g., L1, C18) and similar dimensions (length, particle size) [10] [3]. |
| Critical Reagents | Includes buffers, mobile phases, and derivatization agents that directly affect chemical analysis [10]. | Standardize the source and grade of reagents; document preparation procedures meticulously to minimize variability [4] [10]. |
| System Suitability Standards | Verifies that the total analytical system is suitable for the intended analysis on the day of testing [6]. | Use the same preparation and acceptance criteria at both sites to ensure the system is performing adequately [6]. |
Strategic Partnering to Overcome Fragmentation
To mitigate the risks of a fragmented landscape, companies should rethink their outsourcing strategy.
- Consolidate Partnerships: Rather than spreading operations across multiple suppliers, seek reliable partners who can offer a comprehensive solution across much of the manufacturing value chain. This reduces the coordination burden and risk [55].
- Foster Collaboration and Communication: Establish direct lines of communication between analytical experts at the TL and RL [3]. Regular meetings and shared documentation systems are vital for addressing issues in a timely manner and transferring "tacit knowledge" not captured in written procedures [3].
- Invest in Robust Method Development: The success of a transfer is fundamentally determined by the robustness of the original method. Methods should be developed with transfer in mind, accounting for expected variations in equipment and operators between different labs [12].
Quantifiable Success: Defining Experimental Acceptance Criteria
A successful transfer is objectively demonstrated by data meeting pre-defined, statistically sound acceptance criteria. These criteria are typically derived from method validation data and ICH guidelines [3].
Table: Typical Acceptance Criteria for Key Analytical Tests
| Test Parameter | Commonly Used Acceptance Criteria | Experimental Protocol Summary |
|---|---|---|
| Assay | Absolute difference between the mean results of the TL and RL should be ≤ 2.0-3.0% [6] [3]. | A minimum of 6 determinations (e.g., 2 analysts x 3 batches in triplicate) on a homogeneous sample, such as a finished product or reference standard [6]. |
| Impurities (Related Substances) | For impurities at specified levels: difference in results ≤ 25.0%. For spiked impurities: recovery of 80-120% [6] [3]. | Analysis of a minimum of 6 determinations on spiked samples (e.g., placebo or product spiked with known impurities at specification levels) [6]. |
| Dissolution | Difference in mean results: ≤ 10% at early time points (<85% dissolved) and ≤ 5% at later time points (>85% dissolved) [3]. | Testing of 6 units from the same batch at both labs, comparing results at multiple time points as per the method specification. |
| Content Uniformity | Meeting compendial requirements (e.g., Ph. Eur.) at both labs, with comparable results and RSD. | Testing of 10 individual units from the same batch at both laboratories, with statistical comparison of the results. |
The future of pharmaceutical development hinges on the ability to reliably transfer knowledge and processes across a global network. In the face of a fragmented outsourcing landscape and increased regulatory scrutiny, success is no longer just about executing a protocol. It is about strategic partnership, meticulous planning, and uncompromising communication.
By adopting a structured, risk-based approach to Analytical Method Transfer—one that emphasizes robust method development, comprehensive documentation, and deep collaboration between laboratories—companies can transform a potential bottleneck into a strategic advantage. This disciplined approach not only ensures regulatory compliance and data integrity but also accelerates time to market, builds confidence in product quality, and ultimately, safeguards patient safety.
Ensuring Success: Data Evaluation, Acceptance Criteria, and Regulatory Approval
Defining Statistical Acceptance Criteria for Key Tests (Assay, Related Substances, Dissolution)
In the pharmaceutical industry, the transfer of analytical methods between laboratories is a critical process for ensuring consistent drug quality across different manufacturing and testing sites. A cornerstone of a successful transfer is the establishment of robust, statistically sound acceptance criteria for key tests. These criteria are not arbitrary thresholds; they are scientifically justified limits that provide objective evidence that the Receiving Laboratory can perform the analytical procedure equivalently to the Transferring Laboratory, ensuring the reliability of data used for product release [3] [35].
This guide compares the performance of different approaches to defining these criteria, framing them within the broader context of method transfer protocols. We will provide a detailed comparison of typical acceptance criteria for assays, related substances, and dissolution, alongside the experimental protocols and reagent toolkits necessary for their verification.
Comparative Analysis of Acceptance Criteria for Key Tests
The definition of acceptance criteria must be tailored to the specific analytical procedure, considering its purpose, the nature of the analyte, and its historical performance [3] [56]. The table below summarizes typical acceptance criteria for key tests as encountered in comparative method transfer exercises.
Table 1: Typical Acceptance Criteria for Key Tests in Analytical Method Transfer
| Test | Typical Acceptance Criteria | Key Considerations & Variability |
|---|---|---|
| Assay | Absolute difference between sites: 2-3% [3]. | Criteria focus on demonstrating accuracy and equivalence of the overall potency result. |
| Related Substances | At low levels: More generous criteria (e.g., recovery of 80-120% for spiked impurities) [3].At higher levels (>0.5%): Stricter absolute difference requirements [3]. | Criteria are level-dependent. Spiking known impurities is often necessary to challenge the method adequately [3]. |
| Dissolution | At time points <85% dissolved: Absolute difference in mean results ≤ 10% [3].At time points ≥85% dissolved: Absolute difference in mean results ≤ 5% [3]. |
Beyond these transfer-specific criteria, the United States Pharmacopeia (USP) sets acceptance criteria for routine quality control dissolution testing, known as Q values. For immediate-release products, this is typically 80% dissolved in a specified time, with a three-stage (S1, S2, S3) acceptance process involving 6 to 24 units [57].
A more advanced approach moves beyond fixed criteria to evaluate method error relative to the product specification tolerance. This involves calculating what percentage of the specification range (USL - LSL) is consumed by the method's repeatability and bias [56]. Recommended goals for a well-characterized method are for repeatability to consume ≤25% of the tolerance and bias to consume ≤10% of the tolerance [56].
Experimental Protocols for Verification
The verification of these acceptance criteria is embedded within the formal process of analytical method transfer. The following workflow and detailed protocols ensure the process is systematic, documented, and compliant with regulatory expectations.
Diagram 1: Method Transfer Workflow
Protocol 1: Pre-Transfer Knowledge Sharing and Gap Analysis
Before any laboratory work begins, a comprehensive knowledge exchange is crucial [3].
- Objective: To ensure the Receiving Laboratory (RU) has all necessary technical knowledge, data, and experience to execute the method correctly [3].
- Methodology:
- Compile Transfer Package: The Transferring Laboratory (TU) provides a package including the analytical method description, full method validation report, information on reference standards and critical reagents, and any known "tacit knowledge" or practical tips [3].
- Perform Gap Analysis: The RU reviews the original method validation against current ICH requirements to identify any supplementary validation needed prior to transfer—a mandatory step in the EU [3].
- Kick-off Meeting: Teams from both laboratories meet to discuss the method, agree on a timeline, and determine if on-site training is required to bridge any knowledge gaps [3].
Protocol 2: Comparative Testing for Assay and Related Substances
This is the most common protocol for formal method transfer [3] [35].
- Objective: To demonstrate that the RU can generate results statistically equivalent to those from the TU by testing a predefined set of samples.
- Experimental Design:
- A minimum of one batch for an API and one batch each for the lowest and highest strengths of a drug product are typically used [29].
- Both laboratories analyze the same homogeneous samples, often in replicates (e.g., six replicates per lab) [3].
- For related substances testing, samples may be spiked with known impurities at specific levels to adequately challenge the method's accuracy [3].
- Data Analysis: The results from both labs are statistically compared. The primary comparison is often the absolute difference between the mean values obtained by each laboratory, which must fall within the pre-defined acceptance criteria (e.g., ≤3% for assay) [3]. Standard deviation and relative standard deviation are also calculated.
Protocol 3: Dissolution Performance Verification and Comparison
For dissolution, the transfer must verify both apparatus suitability and the ability to generate equivalent profile data.
- Objective: To ensure the RU's dissolution apparatus is performing suitably and to demonstrate equivalence of dissolution profiles.
- Experimental Design - Apparatus Suitability (PVT):
- The USP Performance Verification Test (PVT) using prednisone reference standard tablets is performed to holistically confirm the dissolution assembly is "fit-for-purpose" [58].
- This is a required complement to mechanical calibration and involves running the standard according to a strict, single- or two-stage testing procedure [58].
- The results (geometric mean and % coefficient of variation) are compared against lot-specific acceptance criteria established by USP through a global collaborative study [58].
- Experimental Design - Profile Comparison:
- Both laboratories generate dissolution profiles for the same batch(es) of the product.
- For global submissions, especially for generics, the EMA requires comparative profiles in at least three media (pH 1.2, 4.5, and 6.8) against a reference product [57].
- The f₂ similarity factor is calculated to statistically compare profiles. An f₂ value between 50 and 100 indicates similarity [57].
The Scientist's Toolkit: Essential Research Reagent Solutions
The consistent execution of analytical methods and transfer protocols relies on high-quality, standardized materials. The following table details key reagent solutions and their critical functions.
Table 2: Essential Reagents and Materials for Analytical Testing and Transfer
| Item | Function & Importance in Method Transfer |
|---|---|
| Pharmacopeial Reference Standards (e.g., USP Prednisone RS) | Used for dissolution Performance Verification Testing (PVT) to provide a holistic check of the entire dissolution assembly and ensure results are comparable to a global standard [58]. |
| Chemical Reference Standards (API & Impurities) | Highly purified substances used to identify and quantify the active ingredient and its impurities. Using the same lot of standards during transfer minimizes variability and is a best practice [35]. |
| Chromatography Columns (HPLC/GC) | The specific brand, model, and lot of the column are often critical to method performance. The transfer protocol must specify this to ensure reproducibility between labs [3] [29]. |
| Qualified Dissolution Media | The preparation of dissolution medium, particularly its deaeration procedure, can significantly influence results. The USP deaeration procedure by vacuum filtration is the benchmark against which alternatives must be verified [58]. |
| System Suitability Test (SST) Solutions | Mixtures specifically designed to demonstrate that the chromatographic system is performing adequately at the time of the test. SST criteria must be met by both laboratories for the transfer data to be valid [3]. |
Defining statistical acceptance criteria for assay, related substances, and dissolution is a fundamental component of a robust analytical method transfer. While typical criteria provide a strong starting point, the most defensible approach integrates a tolerance-based mindset, ensuring the method is fit-for-purpose relative to the product's specification limits. A successful transfer is not achieved by meeting statistical criteria alone but is underpinned by rigorous experimental protocols—from comprehensive knowledge sharing and gap analysis to structured comparative testing—and the consistent use of qualified reagents and materials. By adhering to this structured, scientifically justified framework, drug development professionals can ensure data integrity, maintain regulatory compliance, and safeguard product quality across their laboratory networks.
In the regulated pharmaceutical environment, demonstrating that an analytical method performs equivalently when transferred between laboratories is a critical requirement. This process, known as analytical method transfer (AMT), relies on robust statistical comparisons to prove that a receiving laboratory can execute the method and generate results equivalent to those from the transferring laboratory [4] [10]. This guide objectively compares the performance of three foundational statistical techniques—t-tests, F-tests, and equivalence testing—within the context of AMT protocols, providing experimental data and methodologies to support their application.
At the core of analytical method transfer is the need to statistically demonstrate that the results from two different laboratories are equivalent. The receiving laboratory must prove it can perform the validated analytical method with the same accuracy, precision, and reliability as the originating laboratory, despite potential differences in analysts, equipment, and environmental conditions [4] [10]. The following statistical techniques are commonly employed to substantiate this claim.
- T-Test: Used to determine if there is a statistically significant difference between the means of two sets of data. In AMT, it compares the average results obtained by the sending and receiving laboratories on the same set of samples [10] [59]. The null hypothesis is that the difference between the two population means is zero [59].
- F-Test: Primarily used to compare the variances or precision of two data sets. It is crucial for verifying the assumption of equal variances before conducting a pooled variance t-test and for directly assessing the consistency of method precision between two labs [59].
- Equivalence Testing (TOST): A more nuanced approach where the goal is to actively prove that the difference between two means is less than a pre-defined, acceptable margin, known as the smallest effect size of interest (SESOI) [60]. This method is conceptually superior for AMT as it frames the hypothesis around proving equivalence, rather than failing to find a difference.
The following table summarizes the core characteristics and applications of these tests in an AMT context.
Table 1: Comparison of Key Statistical Tests for Analytical Method Transfer
| Feature | T-Test | F-Test | Equivalence Testing (TOST) |
|---|---|---|---|
| Primary Objective | Detect a difference between two means [59] | Detect a difference between two variances [59] | Prove similarity within a practical margin [60] |
| Typical Null Hypothesis (H₀) | Mean of Lab A - Mean of Lab B = 0 [59] | Variance of Lab A / Variance of Lab B = 1 [59] | The difference between means is outside the equivalence bounds (i.e., Δ ≤ -ΔL or Δ ≥ ΔU) [60] |
| Application in AMT | Comparing accuracy of results between labs | Comparing precision (repeatability) between labs | Providing direct evidence for method equivalence |
| Key Output | t-statistic, degrees of freedom, p-value [59] | F-statistic, degrees of freedom, p-value [59] | Two p-values; conclusion based on whether both fall below alpha [60] |
| Interpretation of Nonsignificant Result (p > 0.05) | Failure to reject H₀; data do not show a difference (but cannot prove equivalence) [60] | Failure to reject H₀; data do not show a difference in variance | Not the primary outcome; the goal is to reject the null hypothesis of non-equivalence |
| Interpretation of Significant Result (p < 0.05) | Reject H₀; a statistically significant difference exists between means [59] | Reject H₀; a statistically significant difference exists between variances [59] | When both tests are significant, can conclude equivalence within the set bounds [60] |
Experimental Protocols for Statistical Comparison
A successful analytical method transfer is governed by a pre-approved protocol that details the experimental design and acceptance criteria [4] [10]. The following provides a generalized workflow and detailed methodologies for implementing the statistical comparisons.
Diagram 1: Analytical Method Transfer Workflow
Core Experimental Methodology
The foundational experimental approach for most AMT activities is comparative testing, where both laboratories analyze the same set of samples [4] [10] [3].
- Sample Selection: A predetermined number of homogeneous samples are selected. These can be from production batches, spiked placebos with known amounts of analyte, or approved reference standards [10] [3]. The samples must be stable and representative of the material the method is designed to analyze.
- Testing Procedure: Both the transferring (sending) and receiving laboratories analyze the identical samples using the same analytical method procedure. The testing should be performed under the same conditions as routine analysis, typically with a pre-defined number of replicates (e.g., six determinations per lab) to assess precision [10].
- Data Collection: All raw data, including instrument printouts, chromatograms, and calculations, are meticulously recorded by both labs for subsequent compilation and analysis [4].
Protocol for T-Test and F-Test Application
This protocol uses the common example of comparing assay results (e.g., drug potency) between two laboratories.
Step 1: Perform an F-Test for Variance Comparison.
- Objective: To test if the variances (precision) of the two laboratories are statistically equal, which determines the type of t-test to be used.
- Calculation: The F-statistic is calculated as the ratio of the larger sample variance to the smaller sample variance: F = s₁² / s₂² [59].
- Interpretation: If the two-tailed p-value for the F-test is greater than the significance level (α, typically 0.05), the hypothesis of equal variances is not rejected, and a pooled variance t-test is appropriate. If the p-value is less than α, a separate variance t-test (e.g., Welch's t-test) should be used [59].
Step 2: Perform the Appropriate T-Test.
- Objective: To test if the means (accuracy) of the two laboratories are statistically equal.
- Pooled Variance t-Test: This test is used when variances are assumed equal. The t-statistic is calculated as: [59]
- Interpretation: The null hypothesis is that the difference between population means is zero. If the two-tailed p-value is less than α (e.g., 0.05), the null hypothesis is rejected, indicating a statistically significant difference between the means of the two laboratories [59].
Table 2: Example T-Test and F-Test Output for Assay Results (Hypothetical Data)
| Parameter | Sending Lab | Receiving Lab | Statistical Output |
|---|---|---|---|
| Sample Size (n) | 6 | 6 | - |
| Mean Assay (%) | 99.8 | 98.9 | - |
| Standard Deviation | 0.95 | 1.21 | - |
| F-Test Result | - | - | F = 1.62, p-value (two-tailed) = 0.35 |
| T-Test Conclusion | - | - | Pooled Variance t-test: t = 1.56, p-value (two-tailed) = 0.15 |
| Interpretation | - | - | Since p > 0.05 for both tests, no significant difference in variance or means is detected. |
Protocol for Equivalence Testing (TOST Procedure)
The Two One-Sided Tests (TOST) procedure is a straightforward and recommended method for equivalence testing [60].
Step 1: Define Equivalence Bounds.
- Objective: Establish the smallest effect size of interest (SESOI), which is the maximum acceptable difference between laboratory means that is considered practically irrelevant [60].
- Method: These bounds are typically set based on product specifications, method performance data, and regulatory guidance. For a drug assay, a common acceptance criterion is an absolute difference of no more than 2-3% between lab means [3]. For example, equivalence bounds (ΔL, ΔU) could be set at -2.0% and +2.0%.
Step 2: Perform Two One-Sided T-Tests.
- Objective: To statistically reject the possibility that the true mean difference is outside the equivalence bounds.
- Test 1: H₀₁: Δ ≤ -ΔL vs. H₁₁: Δ > -ΔL (e.g., Δ ≤ -2.0%)
- Test 2: H₀₂: Δ ≥ ΔU vs. H₁₂: Δ < ΔU (e.g., Δ ≥ 2.0%)
- Calculation: Two t-tests are performed against these bounds. The formulas are analogous to a one-sample t-test comparing the observed mean difference to the bound [60].
Step 3: Draw Conclusion.
- Objective: Conclude equivalence if both null hypotheses can be rejected.
- Interpretation: If the p-value for both one-sided tests is less than α (e.g., 0.05), we can reject the null hypothesis that the difference is outside the bounds and conclude statistical equivalence within the pre-specified margin [60]. A 90% confidence interval for the mean difference can also be constructed; if it falls entirely within the equivalence bounds (e.g., between -2.0% and +2.0%), equivalence is demonstrated.
Diagram 2: TOST Equivalence Testing Logic
Table 3: Example Scenarios for TOST Equivalence Testing
| Scenario | Observed Mean Difference (Lab A - Lab B) | 90% Confidence Interval | Equivalence Bounds (-2.0, 2.0) | TOST p-values | Conclusion |
|---|---|---|---|---|---|
| A: Equivalent | -0.5% | [-1.2%, +0.2%] | Entirely within | Both < 0.05 | Success: Method equivalent |
| B: Different | -2.8% | [-3.5%, -2.1%] | Entirely below | One > 0.05 | Fail: Significant difference |
| C: Inconclusive | -1.8% | [-2.5%, -1.1%] | Includes lower bound | One > 0.05 | Fail: Cannot prove equivalence |
The Scientist's Toolkit: Essential Research Reagent Solutions
The success of an analytical method transfer depends not only on statistics but also on the quality and consistency of the materials used. Standardizing these reagents is a key best practice to mitigate variability [10] [3].
Table 4: Essential Materials and Reagents for Analytical Method Transfer
| Item | Critical Function | Best Practice for Transfer |
|---|---|---|
| Chemical Reference Standards | Serves as the benchmark for identifying and quantifying the analyte. | Use traceable and qualified standards from the same batch at both labs to ensure consistency [4] [10]. |
| Chromatography Columns | The medium for separation in HPLC/GC methods; a major source of variability. | Use columns with identical specifications (e.g., dimensions, particle size, ligand chemistry). Specify the brand and model in the protocol [10]. |
| Reagents & Solvents | Form the mobile phase and solvent systems for analysis. | Standardize the grade, supplier, and preparation methods (e.g., filtering, degassing) between laboratories [10]. |
| Stable Test Samples | The material being compared by both laboratories. | Use homogeneous, representative samples from the same batch. Ensure stability throughout the transfer period [4] [10]. |
| System Suitability Standards | Verifies that the analytical system is functioning correctly before analysis. | Use the same preparation and acceptance criteria at both sites as a pre-qualification step [10]. |
The choice of statistical technique for analytical method transfer carries significant implications for interpretation and regulatory compliance. While t-tests and F-tests are useful for detecting differences, they are inherently ill-suited for proving equivalence. A non-significant p-value from a t-test does not confirm equivalence; it may simply indicate an underpowered study [60]. Equivalence testing, particularly the TOST procedure, provides a statistically sound framework for actively demonstrating that any difference between laboratories is smaller than a clinically or quality-relevant margin.
For researchers and drug development professionals, the recommended path is to define equivalence bounds based on method capability and product criticality in the transfer protocol, and to employ the TOST procedure as the primary statistical method for demonstrating comparability. This approach aligns statistical practice with the fundamental objective of method transfer: to prove, not assume, that the receiving lab is qualified to use the method.
In the highly regulated pharmaceutical and biotechnology landscape, the transfer of analytical methods between laboratories is a critical process. It ensures that methods perform consistently and reliably in a new environment, directly impacting product quality and patient safety. Quality Assurance (QA) serves as the cornerstone of this process, providing independent oversight to ensure all activities meet predefined standards and regulatory requirements. Their rigorous review and formal approval of the transfer protocol and report are not merely procedural steps but are fundamental to establishing the legal and scientific validity of the transfer [4] [10].
The Analytical Method Transfer Process and QA's Integral Role
Analytical method transfer is a documented process that qualifies a receiving laboratory to use an analytical procedure that was originally validated in a transferring laboratory [4] [10]. The primary goal is to demonstrate that the receiving lab can execute the method with equivalent accuracy, precision, and reliability, producing comparable results [4].
The process is built upon a foundation of good documentation practices, with two documents being paramount: the transfer protocol and the transfer report. The protocol acts as the experimental blueprint, while the report serves as the certified record of success. QA's role spans the entire lifecycle, from initial protocol approval to the final sign-off on the report, ensuring data integrity and regulatory compliance at every stage [4] [10].
The following workflow outlines the key stages of the method transfer process and the critical approval gates managed by Quality Assurance.
Method Transfer and QA Approval Workflow
Reviewing and Approving the Transfer Protocol
The transfer protocol is the master plan that dictates the entire transfer exercise. A QA specialist's review of this document is comprehensive and focuses on ensuring it is scientifically sound, complete, and compliant.
Core Elements of the Transfer Protocol
A robust transfer protocol, as defined by industry best practices, must contain several key elements [4] [3]:
- Objective and Scope: A clear statement of purpose and the methods involved.
- Responsibilities: Defined roles for both the transferring and receiving laboratories.
- Materials and Instruments: A detailed list of equipment, reagents, and reference standards, including qualification status.
- Analytical Procedure: The exact, step-by-step method to be executed.
- Experimental Design: The number of samples, batches, and replicates to be tested.
- Predefined Acceptance Criteria: Statistically justified criteria for demonstrating equivalence.
QA's Protocol Review Checklist
During review, QA verifies the following aspects against internal procedures and regulatory guidelines [4] [10] [3]:
| Review Focus Area | Key Questions for QA |
|---|---|
| Regulatory & Procedural Compliance | Does the protocol align with internal SOPs and regulatory guidelines (e.g., USP <1224>, FDA, EMA)? |
| Technical Robustness | Are the experimental design and statistical methods scientifically sound to prove equivalence? |
| Acceptance Criteria | Are the acceptance criteria predefined, justified by prior validation data, and sufficiently rigorous? |
| Risk Management | Does the protocol address potential risks identified in earlier assessments (e.g., equipment differences)? |
| Documentation Completeness | Are all necessary components, including roles and responsibilities, fully detailed? |
Reviewing and Approving the Transfer Report
Once the experimental work is complete, the receiving laboratory compiles the data and findings into a transfer report. QA's final review of this document is what grants the receiving laboratory the formal permission to use the method for routine testing.
Essential Components of the Transfer Report
The transfer report must provide a complete and accurate record of the transfer activities [4] [3]:
- Results and Raw Data: All generated data, including chromatograms and spectra.
- Statistical Analysis: Comparison of results from both labs using predefined statistical tests (e.g., t-tests, F-tests).
- Evaluation Against Criteria: A direct comparison of the results against the protocol's acceptance criteria.
- Deviation Management: Documentation and justification for any deviations from the protocol or method.
- Clear Conclusion: A definitive statement on whether the transfer was successful.
QA's Report Review Checklist
QA's approval of the report is contingent upon a meticulous verification process [4] [3]:
| Review Focus Area | Key Questions for QA |
|---|---|
| Protocol Adherence | Was the study conducted exactly as outlined in the approved protocol? |
| Data Integrity | Is the raw data complete, authentic, and accurate? Does it support the conclusions in the report? |
| Acceptance Criteria Met | Does the statistical evaluation conclusively demonstrate that all predefined acceptance criteria were met? |
| Deviation Investigation | Were any deviations or Out-of-Specification (OOS) results thoroughly investigated and resolved? |
| Final Conclusion | Is the conclusion that the method was successfully transferred—or that further work is needed—supported by the data? |
Essential Research Reagent Solutions for Method Transfer
The success of a method transfer heavily relies on the quality and consistency of materials used. The table below details key reagents and their critical functions in ensuring reliable results.
| Reagent/Material | Function in Method Transfer |
|---|---|
| Reference Standards | Serves as the benchmark for quantifying the analyte and ensuring analytical accuracy and precision across both laboratories [4]. |
| Chromatography Columns | The specific type and brand of HPLC/UPLC columns are often critical method parameters; consistency is vital to achieve equivalent separation and results [10]. |
| System Suitability Solutions | A standardized mixture used to verify that the analytical system is performing adequately before the transfer testing is executed [25]. |
| Spiked Samples | Samples with known amounts of impurities or analytes added are used to validate accuracy and recovery, crucial for impurity methods [3] [25]. |
| Stable & Qualified Reagents | Ensures that chemical reagents, buffers, and mobile phases are of consistent quality and purity to prevent variability in analytical results [4] [10]. |
Comparative Analysis of Common Transfer Approaches and QA Oversight
Different methods require different transfer strategies. The choice of approach significantly influences the level of oversight and review required by QA. The table below compares the most common methodologies.
| Transfer Approach | Description | QA's Primary Review Focus |
|---|---|---|
| Comparative Testing | Both labs analyze identical samples; results are statistically compared for equivalence [4] [10]. | Rigor of statistical analysis and strict adherence to pre-defined acceptance criteria for comparability [4] [3]. |
| Co-validation | The receiving lab participates in the method validation, establishing reproducibility from the outset [4] [25]. | Ensuring the validation protocol and report adequately cover both sites and that data is combined and presented in a single, cohesive package [25]. |
| Revalidation | The receiving lab performs a full or partial revalidation of the method [4] [10]. | Scrutinizing the entire validation package to ensure it meets ICH and other regulatory requirements for the new site [4]. |
| Transfer Waiver | The transfer process is waived based on scientific justification (e.g., for simple compendial methods) [4] [3]. | Challenging the risk assessment and ensuring the justification for waiving experimental work is robust and thoroughly documented [4] [3]. |
In conclusion, the role of Quality Assurance in reviewing and approving the transfer protocol and report is a critical governance activity that underpins the integrity of the entire analytical method transfer process. Through a disciplined, evidence-based approach, QA ensures that methods are transferred robustly, data is reliable, and the resulting analytical data generated in the receiving laboratory can be trusted to support the quality, safety, and efficacy of pharmaceutical products.
In the pharmaceutical and biopharmaceutical industries, the reliability of analytical data is paramount for ensuring product quality and patient safety. Two critical processes that underpin data integrity are method validation and method transfer. While often discussed together, they serve distinct purposes within the analytical method lifecycle. Method validation demonstrates that a procedure is suitable for its intended purpose, while method transfer qualifies a receiving laboratory to reproducibly execute a method already validated elsewhere. This guide objectively compares these processes, providing researchers and drug development professionals with a clear framework for their effective implementation.
Core Concepts and Definitions
Method Validation is the foundational process of establishing, through laboratory studies, that the performance characteristics of an analytical method meet the requirements for its intended application [19]. It answers the question: "Is this method scientifically sound and reliable?"
Method Transfer, also known as Analytical Method Transfer (AMT), is a documented process that qualifies a receiving laboratory (the recipient) to use an analytical method that originated in another laboratory (the transferring lab) [4] [19] [10]. It answers the question: "Can the receiving lab execute this validated method and generate equivalent results?"
The relationship between these processes is sequential and integral to the method lifecycle, as illustrated below.
Comparative Analysis: Method Validation vs. Method Transfer
The following table summarizes the key differences between method validation and method transfer across various dimensions.
| Feature | Method Validation | Method Transfer |
|---|---|---|
| Primary Objective | To demonstrate the method is suitable for its intended purpose [19]. | To qualify a receiving lab to use the method, producing equivalent results to the transferring lab [4] [10]. |
| Core Question | "Does the method work?" | "Can the new lab perform the method correctly?" |
| When it Occurs | Before a method's first use in routine testing; for new methods or major changes [19]. | When a validated method is moved to a different laboratory or site [4] [10]. |
| Regulatory Guidance | ICH Q2(R1), USP General Chapter <1225> [19]. | USP General Chapter <1224>, EMA Guideline on Transfer, FDA Guidance [10]. |
| Key Parameters Assessed | Accuracy, Precision, Specificity, Linearity, Range, Robustness, LOD/LOQ [19]. | Typically, a subset (e.g., Precision, Intermediate Precision, Accuracy) to demonstrate equivalence between labs [4] [19]. |
| Outcome | A validated method ready for use in the originating laboratory. | A qualified receiving laboratory and a formal report approving routine use of the method at the new site [4] [10]. |
Detailed Experimental Protocols
Protocol for Method Validation
A robust method validation protocol is comprehensive and follows established regulatory guidelines [19].
- Accuracy: Assessed by spiking the analyte into a blank matrix at known concentrations (typically low, medium, and high within the range) and calculating the percentage recovery of the measured value versus the expected value [25].
- Precision:
- Repeatability: Determined by analyzing multiple replicates (e.g., n=6) of a homogeneous sample at 100% of the test concentration by a single analyst in a single session [19].
- Intermediate Precision: Evaluates the impact of random events on the method's precision, such as different days, different analysts, or different equipment within the same laboratory [19].
- Specificity: Demonstrated by proving the method can unequivocally assess the analyte in the presence of potential interferents like impurities, degradants, or matrix components [19].
- Linearity and Range: A series of standard solutions across a specified range (e.g., 50-150% of the target concentration) are analyzed. The data is evaluated by plotting the instrument response versus the analyte concentration, and statistical tools are used to assess the linearity [19].
- Robustness: Investigated by deliberately introducing small, deliberate variations in method parameters (e.g., mobile phase pH, flow rate, column temperature) and evaluating the method's capacity to remain unaffected [19].
Protocol for Method Transfer
The most common approach for method transfer is Comparative Testing [4] [35]. The detailed protocol involves:
- Protocol Development: A detailed, pre-approved transfer protocol is the cornerstone. It must define the scope, responsibilities, experimental design, pre-defined acceptance criteria, and statistical evaluation plan [4] [10].
- Sample Analysis: Both the transferring (originating) and receiving laboratories analyze the same set of homogeneous samples. These samples should be representative, such as production batches, spiked placebo, or reference standards [4] [35].
- Data Comparison and Statistical Analysis: The results from both laboratories are statistically compared against the pre-defined acceptance criteria outlined in the protocol. Common statistical tools include:
- Report and Approval: A comprehensive transfer report is generated, summarizing all activities, results, deviations, and a conclusion on the success of the transfer. This report requires formal approval, typically by the Quality Assurance (QA) department, before the receiving lab can use the method for routine testing [4] [10].
Essential Research Reagent Solutions and Materials
Successful execution of method validation and transfer relies on critical materials. The following table details key items and their functions.
| Item | Function in Validation/Transfer |
|---|---|
| Qualified Reference Standards | Substances of known purity and identity used to calibrate instruments and prepare known samples for accuracy and linearity studies [4] [19]. |
| Critical Reagents (e.g., antibodies for LBAs) | Specific reagents whose properties can significantly impact method performance. Consistent sourcing and lot-to-lot qualification are vital, especially for ligand binding assays [28]. |
| Specified Chromatography Columns | The stationary phase is a critical method parameter. Using columns with equivalent performance (e.g., L-number, bonding type) is essential for reproducibility during transfer [10]. |
| Control Samples (QCs) | Stable, homogeneous samples with known or assigned values used to monitor the method's performance during both validation and transfer experiments [4] [28]. |
| Appropriate Biological Matrix | The material in which the analyte is contained (e.g., plasma, serum). Sourcing consistent, well-characterized matrix is crucial for bioanalytical methods [28]. |
Common Challenges and Mitigation Strategies
Despite clear protocols, several practical challenges can arise, particularly during method transfer.
- Instrument Variability: Differences in instrument models, configurations, or calibration states (e.g., Gradient Delay Volume - GDV in HPLC) can cause result discrepancies [35] [61]. Solution: Conduct a pre-transfer gap analysis of equipment and, if possible, adjust method parameters to compensate for known differences like GDV, ensuring compliance with regulatory guidelines [61].
- Reagent and Material Variability: Different lots of reagents, solvents, or chromatography columns can alter method performance [10] [35]. Solution: Whenever possible, use the same lot numbers for critical materials during transfer. If not, the receiving lab must verify suitability against a known reference [35].
- Personnel and Technique: Unwritten techniques or subjective interpretations of the procedure by analysts can introduce variability [12] [35]. Solution: Implement comprehensive, hands-on training and use documentation with clear, unambiguous language that allows for only a single interpretation [4] [12].
- Sample Stability: Degradation of samples during shipment between laboratories for comparative testing can invalidate results [10]. Solution: Establish and verify sample stability under the expected shipping and storage conditions prior to the transfer.
Method validation and method transfer are distinct but interconnected pillars of quality assurance in pharmaceutical development. Validation creates a reliable method, while transfer replicates that reliability across laboratory boundaries. A deep understanding of their unique objectives, protocols, and potential challenges empowers scientists to ensure data integrity, maintain regulatory compliance, and ultimately safeguard product quality throughout the method lifecycle. By adhering to a structured, well-documented approach and proactively managing risks, organizations can streamline these critical processes, facilitating efficient drug development and manufacturing on a global scale.
In the highly regulated pharmaceutical industry, the transfer of analytical methods between laboratories is a critical process to ensure consistent drug quality and testing reliability. However, even with meticulous planning, method transfers can fail, triggering a mandatory investigation and robust corrective actions. A failed transfer, indicated by results that do not meet pre-defined acceptance criteria, is not merely a setback but a significant compliance event [31]. Regulatory agencies like the U.S. Food and Drug Administration (FDA) require that any unexplained discrepancy or failure of a batch to meet specifications must be thoroughly investigated, whether or not the batch has been distributed [62]. This guide examines the structured processes for investigating these deviations and the corrective actions required to qualify a receiving laboratory, providing a direct comparison of methodologies and their applications.
The Investigation Process: A Structured Workflow
A systematic and documented investigation is paramount when an analytical method transfer fails. The primary goal is to determine the root cause of the discrepancy, not merely to assign blame. The process involves multiple parties, including the Transferring Laboratory (TL), the Receiving Laboratory (RL), and Quality Assurance (QA) [31]. The following workflow outlines the critical steps from failure to resolution.
Figure 1: A logical workflow for investigating a failed analytical method transfer. The process is iterative until the root cause is confirmed and effective corrective actions are verified.
Key Phases of the Investigation Workflow
Immediate Action and Preliminary Assessment: Upon a failure, all transfer activities must be halted, and the deviation formally documented [31]. The initial assessment determines the scope of the failure—whether it affects a single test result, an entire analytical run, or the overall method suitability.
Root Cause Analysis (RCA): The investigation team must conduct a deep dive into all potential sources of variation. As highlighted in a 2025 FDA warning letter, a common failure is investigations that are not thorough enough, often overlooking significant process changes that could impact product performance, such as dissolution [62]. The RCA should scrutinize:
- Method Execution: Were the procedures followed exactly as written? This includes checking reagent preparation, equipment parameters, and incubation times.
- Equipment and Instruments: Differences in instrument models, calibration status, and maintenance history between the TL and RL can introduce variability [10].
- Analyst Proficiency: The training and experience of the RL analysts must be verified. Inadequate training is a frequent source of error [4].
- Sample Integrity: The stability, homogeneity, and handling of samples used in the transfer must be confirmed [10] [20].
- Data Review: All raw data, calculations, and chromatograms (where applicable) must be reviewed for anomalies or transcription errors.
Classification and Documentation: The root cause should be classified (e.g., human error, equipment malfunction, method flaw) and fully documented. The FDA expects investigations to include "sufficient scientific evidence to support this root cause" [62]. All phases of the investigation, including any unresolved issues, must be meticulously recorded in a final report approved by both laboratories and the QA unit [31].
Comparative Analysis of Corrective and Preventive Actions (CAPA)
Once the root cause is identified, targeted Corrective and Preventive Actions (CAPA) are implemented. The appropriate CAPA strategy depends heavily on the nature of the root cause. The table below compares common CAPA measures, their applications, and regulatory considerations.
Table 1: Comparison of Corrective and Preventive Actions for Common Transfer Failures
| Root Cause Category | Corrective Actions (Addressing the immediate failure) | Preventive Actions (Avoiding recurrence) | Regulatory & Practical Considerations |
|---|---|---|---|
| Inadequate Analyst Training | • Provide immediate remedial training by TL subject matter experts [31].• Re-demonstrate analyst competency. | • Implement robust, documented training programs for new methods [4].• Establish a "train-the-trainer" program for multi-site transfers. | Training must be documented with demonstrated proficiency, not just attendance [31]. |
| Equipment Disparities | • Re-qualify or calibrate the specific instrument in the RL.• Adjust method parameters to suit RL equipment (requires validation). | • Conduct early gap analysis of equipment between TL and RL during transfer planning [4].• Standardize equipment models and brands where possible. | The FDA may request evidence that equipment differences were evaluated as part of an investigation [62]. |
| Method Weakness / Lack of Robustness | • Optimize the problematic steps of the method (e.g., mobile phase composition, column temperature). | • Enhance method development and validation to include robustness testing (e.g., via Design of Experiments/DoE) [62]. | Method changes post-validation may require supplemental regulatory filing [10]. |
| Sample-Related Issues | • Procure new, homogeneous, and stable samples for re-testing [20]. | • Develop and use Method Transfer Kits (MTKs) with pre-characterized, stable samples for all future transfers [20]. | MTKs require conservative storage conditions and stability data to support their use over time [20]. |
| Data Management Errors | • Re-audit and correct all data from the failed study. | • Automate data capture and calculations to minimize manual transcription.• Enhance QC review steps for data and reports. | Inadequate investigation records were cited as a violation in an FDA warning letter [62]. |
A critical lesson from recent enforcement is that CAPA must be validated. As the FDA noted, proposing changes to a master batch record as a CAPA is insufficient if not supported by validation studies to confirm the root cause determination prior to distributing new batches [62]. In one case, the FDA mandated a comprehensive, independent assessment of the entire deviation investigation system and CAPA program to ensure effective root cause analysis and quality assurance oversight [62].
Experimental Protocols for Key Investigations
When a transfer fails, specific experimental protocols are essential to diagnose the problem scientifically. Below are detailed methodologies for two common investigative experiments.
Protocol for Investigating Inter-Laboratory Precision Failures
Objective: To determine if the failure is due to a systematic bias between laboratories or a lack of precision within the Receiving Laboratory.
Methodology:
- Sample Preparation: The TL prepares a single, large, homogeneous sample batch from a drug product lot that is well-characterized and within specification. This sample is split and shipped to both the TL and RL [20].
- Experimental Design: Two analysts in the RL each perform six independent sample preparations and analyses of the homogeneous sample according to the transferred method. Simultaneously, the TL repeats the analysis with two analysts performing three independent preparations each to re-establish a baseline [31].
- Data Analysis: The results from both laboratories are statistically compared. An F-test is used to compare the variances of the two datasets, and a Student's t-test is used to compare the means. Predefined acceptance criteria (e.g., no statistically significant difference at the 95% confidence level) must be set in the investigation protocol [4] [31].
Supporting Experimental Data Interpretation:
- If the means are significantly different but the variances are similar, this indicates a systematic bias (e.g., due to different reference standards or calibrated equipment).
- If the variance within the RL is significantly larger, this indicates a problem with precision in the RL (e.g., due to inadequate method training or inconsistent sample preparation).
Protocol for a Design of Experiment (DoE) to Diagnose Multifactorial Failures
Objective: To efficiently identify the root cause(s) when a failure (e.g., dissolution failure) may be due to the combined effect of multiple method variables, as demanded by the FDA in recent enforcement [62].
Methodology:
- Identify Critical Factors: Select factors for investigation based on the failure mode. For a dissolution failure, this could include API particle size distribution, excipient content, and process parameters like coating solution concentration [62].
- Design the Experiment: A full or fractional factorial DoE is designed to study the main effects and interactions of the selected factors. For example, a DoE might evaluate two different API particle sizes against three different concentrations of a coating solution [62].
- Execute and Analyze: The experimental batches are manufactured according to the DoE matrix and tested for the critical quality attribute (e.g., dissolution profile at multiple time points). The resulting data is analyzed using statistical software to build a model that identifies which factors and interactions have a significant effect on the response.
- Verify and Validate: The model's prediction is verified by running a confirmation batch at the optimal factor settings identified by the DoE. Successful performance of this batch confirms the root cause and validates the CAPA.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method transfer and failure investigation rely on specific materials and tools. The concept of a "Method Transfer Kit" (MTK) is an industry best practice to standardize this process [20].
Table 2: Key Components of a Method Transfer Kit (MTK) and Their Functions
| Component | Function & Importance | Best Practice Application |
|---|---|---|
| Representative API & Drug Product Samples | Provides a consistent, homogeneous sample for both TL and RL to analyze, removing sample variability as a factor [20]. | Use a single, large batch that is representative of commercial product, packaged to ensure stability. |
| Stressed/Degraded Samples | Demonstrates that the RL can accurately detect and quantify impurities, proving the method's specificity and stability-indicating properties [20]. | Include samples with known impurity profiles or provide a protocol for in-situ preparation (e.g., heat, light, or pH stress). |
| System Suitability Reference Standard | Verifies that the analytical system (especially chromatographic systems) in the RL is performing adequately before and during the transfer testing. | Provide a characterized, stable standard with pre-defined acceptance criteria for parameters like retention time, tailing factor, and plate count. |
| Critical Reagents & Columns | Ensures consistency in method performance by using the same lot of critical reagents, mobile phase additives, and HPLC columns [10]. | Supply the RL with the same brand, model, and lot of columns and key reagents used during method validation. |
| Detailed Method Transfer Protocol | The formal document that defines objectives, roles, experimental design, and, crucially, the acceptance criteria for a successful transfer [4] [31]. | The protocol must be approved by both TL, RL, and QA before any testing begins. |
The relationships between these toolkit components and the transfer process can be visualized as follows:
Figure 2: The role of a standardized Method Transfer Kit (MTK) in ensuring a consistent and comparable transfer process. The MTK provides all critical inputs, which are used according to a pre-approved protocol to achieve the desired output.
A failed analytical method transfer is a critical juncture. A superficial investigation and weak corrective actions can lead to recurring failures, regulatory citations, and compromised product quality [62]. A successful outcome hinges on a systematic investigation process to find the true root cause, followed by robust, validated CAPA. The comparative data and experimental protocols outlined in this guide provide a framework for researchers and scientists to objectively diagnose failures and implement effective solutions. By leveraging tools like Method Transfer Kits and statistical Design of Experiments, pharmaceutical professionals can transform a transfer failure from a compliance problem into an opportunity to deepen process understanding and ultimately strengthen the control strategy for drug product quality.
Conclusion
A successful analytical method transfer is a strategic imperative, not a mere administrative task. It hinges on thorough foundational understanding, meticulous methodological execution, proactive troubleshooting, and rigorous validation. The key takeaways are the necessity of a well-defined protocol with clear acceptance criteria, the critical role of continuous and clear communication between all parties, and the importance of comprehensive documentation from start to finish. As the industry trend moves towards increased outsourcing and regulatory scrutiny, the principles of robustness, transparency, and collaboration outlined in this guide will become even more vital. By adopting these best practices, researchers and drug development professionals can ensure reliable data, maintain regulatory compliance, and ultimately safeguard product quality and patient safety across the global pharmaceutical landscape.
References
- 1. Analytical method transfer [https://www.linkedin.com/pulse/analytical-method-transfer-jairus-fernandes]
- 2. Checklist: Ensuring Seamless Tech... Analytical Method Transfer [https://www.propharmagroup.com/thought-leadership/how-conduct-analytical-method-transfer]
- 3. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 4. Analytical Method Transfer: Best Practices and Guidelines [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 5. Method Transfer [https://www.eurofins.com/biopharma-services/product-testing/services/biopharma-product-testing-services/method-development/method-transfer/]
- 6. (module 01) | PPTX Analytical method transfer [https://www.slideshare.net/slideshow/analytical-method-transfer-module-01/48996157]
- 7. | LCGC International Analytical Method Transfer [https://www.chromatographyonline.com/view/analytical-method-transfer-1]
- 8. : step-by-step guide & best practices Analytical Method Transfer [https://www.qbdgroup.com/en/blog/analytical-method-transfer-steps]
- 9. Analytical Method Transfer (AMT) [https://pharmastate.academy/analytical-method-transfer/]
- 10. Analytical Method Transfer in Pharmaceuticals | AMT ... [https://www.pharmaguideline.com/2025/09/analytical-method-transfer-in-pharmaceuticals.html]
- 11. Transfer of analytical methods - MHRA Inspectorate [https://mhrainspectorate.blog.gov.uk/2021/08/13/transfer-of-analytical-methods/]
- 12. Best Practices for Transferring Analytical Methods [https://www.jmolner.com/post/transferring-analytical-methods]
- 13. CRO vs CMO vs CDMO: Key Differences in Outsourcing ... [https://cellcarta.com/science-hub/cro-vs-cmo-vs-cdmo/]
- 14. CRO vs CMO vs CDMO: different roles, same GxP ... [https://www.cognidox.com/blog/cro-vs-cmo-vs-cdmo]
- 15. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 16. Methodological Validation and Inter-Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11512302/]
- 17. Reporting Your Quantitative Research Findings [https://insightsopinion.com/quantitative-research/reporting-your-quantitative-research-findings-best-practices-and-guidelines]
- 18. How to Present Quantitative & Qualitative Data in Reports [https://www.clearpointstrategy.com/blog/qualitative-and-quantitative-data]
- 19. Analytical Method Validation, Verification and Transfer Right [https://www.complianceonline.com/resources/getting-the-analytical-method-validation-verification-and-transfer-right.html]
- 20. Streamlining Method Transfer Across Global Sites [https://www.biopharminternational.com/view/streamlining-method-transfer-across-global-sites]
- 21. Difference Between Validation And Verification Of ... [https://gmpinsiders.com/method-validation-vs-verification/]
- 22. How to conduct a succesful compliant method transfer [https://pharmaceuticalmanufacturer.media/pharmaceutical-industry-insights/pharmaceutical-manufacturing-insights/how-to-conduct-a-succesful-compliant-method-transfer/]
- 23. Evolution of Analytical Procedure Validation Concepts: Part I [https://www.pharmtech.com/view/evolution-of-analytical-procedure-validation-concepts-part-i-analytical-procedure-life-cycle-and-compendial-approaches]
- 24. What is Method Transfer, and Why is it Important? [https://biotech.com/2021/05/20/what-is-method-transfer-and-why-is-it-important/]
- 25. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 26. Navigating method evaluation in clinical laboratories [https://myadlm.org/cln/articles/2024/mayjune/navigating-method-evaluation-in-clinical-laboratories]
- 27. Method Validation - the Real World Applications [https://www.westgard.com/qc-applications/method-validation-qc/qcapp14.html]
- 28. Method Transfer, Partial Validation, and Cross Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389741/]
- 29. Analytical Method Transfer (USP 1224) Guideline [https://pharmabeginers.com/analytical-method-transfer-usp1224-guideline/]
- 30. , Comparability and Co-validation Transfer [https://www.mastercontrol.com/gxp-lifeline/transfer-comparability-covalidation/]
- 31. Importance of acceptance criteria in analytical method ... [https://www.gmpsop.com/importance-of-acceptance-criteria-in-analytical-method-transfer/]
- 32. and Comparability Studies: Tips and Best Practices Method Transfer [https://www.linkedin.com/advice/0/how-do-you-handle-method-transfer-comparability]
- 33. Analytical methods transfer [https://www.sciencepharma.com/services/analytical-methods-transfer/]
- 34. Phases of a Technology Transfer Project in Pharmaceutical ... [https://pharmadigests.com/phases-of-a-technology-transfer-project-in-pharmaceutical-industry/]
- 35. Analytical Method Transfer Between Laboratories [https://www.labmanager.com/method-transfer-between-laboratories-challenges-and-solutions-34250]
- 36. Comprehensive Training: Key Success Factors For Shift ... [https://www.myshyft.com/blog/comprehensive-training/]
- 37. Challenges in Transferring Bioanalytical Methods [https://www.ddw-online.com/challenges-in-transferring-bioanalytical-methods-1688-200810/]
- 38. SOP for Technology Transfer of Analytical Procedure [https://pharmaguideline.site/sop-for-technology-transfer-of-analytical-procedure/]
- 39. Transferring a Quantitative Molecular Diagnostic Test to ... [https://www.sciencedirect.com/science/article/pii/S152515781730524X]
- 40. Analytical Method Transfer: Common Pitfalls and How to ... [https://www.qbdgroup.com/en/blog/analytical-method-transfer-common-pitfalls-and-how-to-avoid-them]
- 41. What are the Causes of Poor Requirements? [https://www.jamasoftware.com/requirements-management-guide/requirements-management/guide-to-poor-requirements-identify-causes-repercussions-and-how-to-fix-them/]
- 42. 5 Hidden Nightmares Caused by Miscommunication on the ... [https://www.rhumbix.com/blog/five-hidden-construction-nightmares-caused-by-miscommunication]
- 43. Poor Communication in Construction: 10 Mistakes That ... [https://remato.com/blog/communication-in-construction/]
- 44. How to Write an Effective Lab Protocol [https://bitesizebio.com/45202/how-to-write-an-effective-lab-protocol/]
- 45. What Are the Consequences of Poor Documentation ... - Dart AI [https://www.dartai.com/blog/the-consequences-of-poor-documentation-in-projects]
- 46. Challenges in Analytical Method Development and ... [https://www.biopharminternational.com/view/challenges-analytical-method-development-and-validation]
- 47. Environmental Test Equipment Market Size & Growth 2025 ... [https://www.futuremarketinsights.com/reports/environmental-test-equipment-market]
- 48. 10 Innovative Lab Tools Scientific Research in 2025 [https://go.zageno.com/blog/innovative-lab-tools-2025]
- 49. Analytical chemistry in the era of sustainability: evaluating ... [https://www.sciencedirect.com/science/article/pii/S2214158825000182]
- 50. Environmental Testing Equipment Market Outlook 2025-2034 [https://www.researchandmarkets.com/reports/6187520/environmental-testing-equipment-market?srsltid=AfmBOopo-Wru6_rU543oPA0URR3GfJyqwQ2mjzSo2Ng41pXtnhh4TbCO]
- 51. How To Perform a Successful GRC Gap Analysis - Centraleyes [https://www.centraleyes.com/successful-gap-analysis/]
- 52. How to Identify Training Gaps (+Overcoming Them) [https://whatfix.com/blog/identify-training-gaps/]
- 53. How Tacit Knowledge Drives Innovation And Team ... [https://www.betterup.com/blog/tacit-knowledge]
- 54. Ways to capture the tacit knowledge [https://www.seismic.com/blog/3-ways-to-capture-the-tacit-knowledge-inside-your-employees-head/]
- 55. A Fragmented The Difficulties Of Working... Outsourcing Landscape [https://www.cellandgene.com/doc/a-fragmented-outsourcing-landscape-the-difficulties-of-working-with-multiple-siloed-partners-0001]
- 56. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 57. Dissolution test: 9 steps to Master the Regulatory side [https://pharmacores.com/dissolution-test-guidelines-by-usp-and-ema/]
- 58. FAQs: Dissolution Performance Verification Testing (PVT) [https://www.usp.org/frequently-asked-questions/dissolution-performance-verification-testing-pvt]
- 59. Unistat Statistics Software | t- and F-Tests [https://www.unistat.com/guide/t-and-f-tests/]
- 60. A Practical Primer for t Tests, Correlations, and Meta-Analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC5502906/]
- 61. Unlocking Smoother HPLC Method | Technology Networks Transfer [https://www.technologynetworks.com/analysis/articles/unlocking-smoother-hplc-method-transfer-362380]
- 62. Glenmark Pharmaceuticals Limited - 708270 - 07/11/2025 [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/glenmark-pharmaceuticals-limited-708270-07112025]