Analytical Method Validation: A Complete Guide to Principles, Parameters, and Regulatory Compliance
This comprehensive guide explores analytical method validation, a critical process ensuring reliability and compliance in pharmaceutical and biopharmaceutical development.
Analytical Method Validation: A Complete Guide to Principles, Parameters, and Regulatory Compliance
Abstract
This comprehensive guide explores analytical method validation, a critical process ensuring reliability and compliance in pharmaceutical and biopharmaceutical development. It covers foundational principles, key validation parameters (accuracy, precision, specificity), regulatory guidelines (ICH Q2(R2), Q14), and practical strategies for troubleshooting and lifecycle management. Designed for researchers and drug development professionals, this article provides actionable insights for developing robust, compliant analytical methods that guarantee data integrity and patient safety.
Understanding Analytical Method Validation: Building Your Regulatory Foundation
Analytical Method Validation (AMV) is a critical scientific and regulatory process within pharmaceutical quality control, defined as the process of providing documented evidence that an analytical method does what it is intended to do [1] [2]. In a regulated environment, it establishes through laboratory studies that the performance characteristics of the method meet the requirements for the intended analytical application, providing assurance of reliability during normal use [2]. For any medical laboratory or pharmaceutical manufacturer seeking accreditation, demonstrating that quality standards have been implemented to generate correct results is a cornerstone of the accreditation process [3]. The process is fundamentally concerned with error assessment—determining the scope of possible errors within laboratory assay results and the extent to which this degree of error could affect clinical interpretations and, consequently, patient care [3]. Within the broader context of analytical method validation research, AMV provides the objective, quantifiable framework that bridges drug development, manufacturing, and post-market surveillance, ensuring that every measured value used to make a decision about drug quality, safety, or efficacy is itself trustworthy.
The Critical Importance of Analytical Method Validation
The importance of Analytical Method Validation extends far beyond a mere regulatory checkbox; it is a fundamental pillar of pharmaceutical quality control that directly impacts patient safety, product quality, and regulatory compliance.
Ensuring Patient Safety and Product Efficacy: Well-developed and validated methods are essential for ensuring product quality and safety [4]. They accurately detect contaminants, degradation products, and variations in active ingredient concentrations, ensuring that pharmaceuticals meet stringent quality specifications. Failure to detect a harmful impurity due to an inadequate method could pose a significant public health risk [4]. Validation provides the assurance that a method can reliably measure critical quality attributes (CQAs), such as the identity, strength, and purity of a drug product, which are vital for its therapeutic performance [5].
Regulatory Compliance and Commercial Distribution: Analytical Method Validation is not optional but a mandatory requirement for regulatory submissions and commercial distribution of pharmaceuticals [4] [5]. Regulatory agencies such as the U.S. Food and Drug Administration (FDA) and the International Council for Harmonisation (ICH) require comprehensive validation data to support drug approval applications like New Drug Applications (NDAs) [4]. The FDA considers successful Process Performance Qualification (PPQ) batches, which rely on validated methods, as the final step before commercial distribution is permitted [5]. Compliance with guidelines like ICH Q2(R1) is therefore legally enforceable, and pharmaceuticals can be deemed "adulterated" if not manufactured according to these validation guidelines [5].
Foundation for Manufacturing Process Control: In pharmaceutical manufacturing, the quality of every unit cannot always be directly verified. Instead, the industry relies on a thorough understanding, documentation, and control of the manufacturing process to ensure consistent quality [5]. Validated analytical methods are the tools that generate the data to establish this understanding. They are used to map the design space of manufacturing equipment, define process control strategies, and verify that the process is running within established parameters, thereby protecting the product revenue stream by maximizing yield and reducing troubleshooting shutdowns [5].
Core Performance Characteristics and Validation Protocols
The validation of an analytical method involves the systematic evaluation of several key performance characteristics. These parameters are investigated based on the type of method and its intended use, as defined by international guidelines [1] [4]. The following section details these characteristics, their definitions, and the standard experimental protocols used to assess them.
Table 1: Key Performance Characteristics for Analytical Method Validation
| Characteristic | Definition | Standard Experimental Protocol & Acceptance Criteria |
|---|---|---|
| Accuracy | The closeness of agreement between an accepted reference value and the value found [2]. It reflects the degree to which a measurement conforms to the actual amount of analyte [4]. | - Protocol: Comparison of results to a standard reference material or by analysis of synthetic mixtures (placebos) spiked with known quantities of analyte (spike recovery) [1] [2]. - Data: Minimum of 9 determinations over at least 3 concentration levels covering the specified range [1] [2]. - Reporting: Percent recovery (e.g., 98–102%) or the difference between the mean and true value with confidence intervals [1] [4]. |
| Precision | The closeness of agreement among individual test results from repeated analyses of a homogeneous sample [2]. It is commonly expressed as the relative standard deviation (RSD) [1]. | - Repeatability (Intra-assay): Same analyst, equipment, short time interval; minimum of 9 determinations or 6 at 100% test concentration [1] [2]. - Intermediate Precision: Different analysts, equipment, days; experimental design to monitor effects of variables [1] [4]. - Acceptance: % RSD; often <2% is recommended, but <5% can be acceptable for minor components [1]. |
| Specificity | The ability to measure the analyte of interest accurately and specifically in the presence of other components that may be expected to be present [2]. | - Protocol: Demonstrate that the analyte peak is well-resolved from interfering peaks (e.g., impurities, excipients, degradants) [4]. - Techniques: Chromatographic resolution, peak purity assessment using photodiode-array (PDA) detection or mass spectrometry (MS) [1] [2]. |
| Linearity & Range | Linearity: The ability of the method to obtain test results directly proportional to analyte concentration [2]. Range: The interval between upper and lower concentrations demonstrated to be determined with precision, accuracy, and linearity [2]. | - Protocol: A minimum of 5 concentration levels across the specified range [1] [2]. - Reporting: Equation for the calibration curve, coefficient of determination (R²), and residuals [1] [2]. - Acceptance: R² typically ≥ 0.999 [4]. |
| Limit of Detection (LOD) & Quantitation (LOQ) | LOD: The lowest concentration that can be detected, but not necessarily quantified [2]. LOQ: The lowest concentration that can be quantified with acceptable precision and accuracy [2]. | - Protocol: Based on signal-to-noise ratio (S/N): 3:1 for LOD, 10:1 for LOQ [1] [2]. Alternatively, LOD=3.3σ/Slope and LOQ=10σ/Slope, where σ is the standard deviation of the response [3]. - Validation: Analyze an appropriate number of samples at the calculated limit to validate performance [2]. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in procedural parameters [1]. | - Protocol: Intentional variation of parameters (e.g., mobile phase pH, flow rate, column temperature) [1]. - Measurement: Monitor effects on critical performance criteria (e.g., resolution, tailing factor) [1]. - Purpose: Indicates the method's reliability during normal use and its suitability for transfer between labs [1]. |
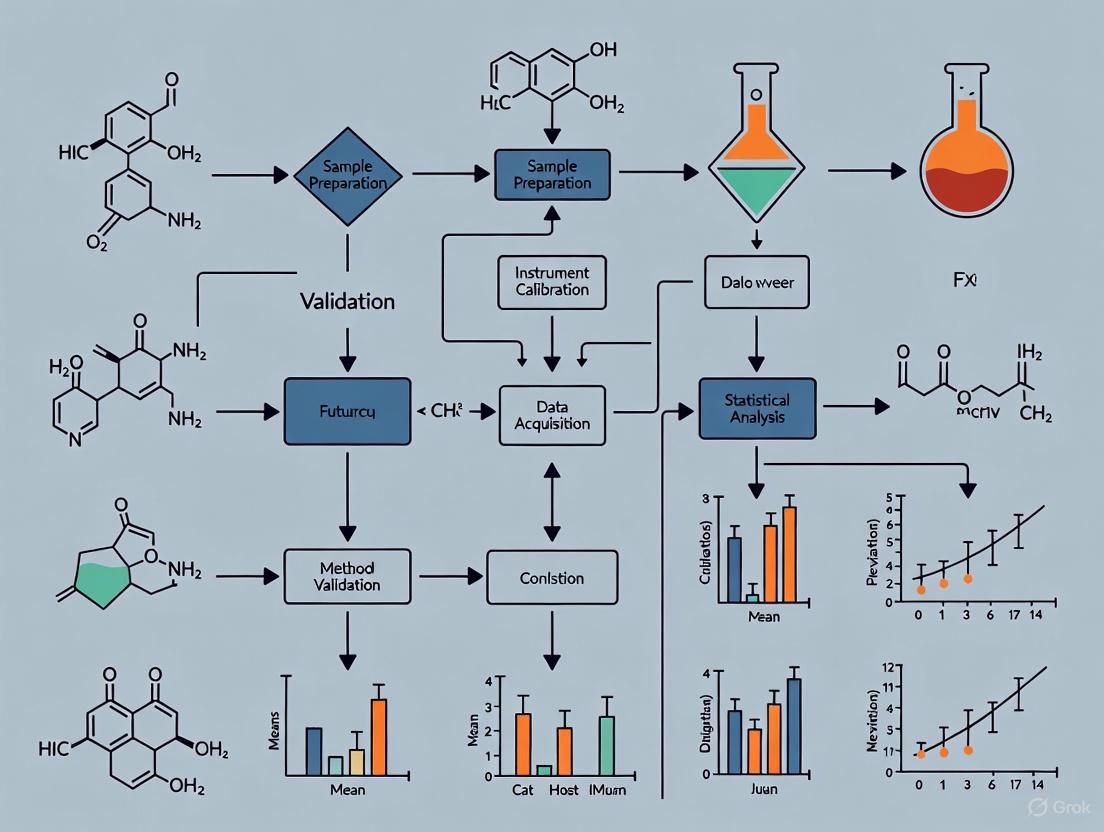
The following workflow diagram illustrates the logical sequence and relationships between the key stages of the analytical method validation lifecycle.
The Scientist's Toolkit: Essential Reagents and Materials
The execution of a robust analytical method validation relies on a suite of high-quality, well-characterized reagents and materials. The following table details key research reagent solutions and their critical functions in the validation process.
Table 2: Essential Materials and Reagents for Analytical Method Validation
| Item | Function in Validation |
|---|---|
| Standard Reference Material | A substance with one or more properties that are sufficiently homogeneous and well-established to be used for the assessment of method accuracy [1] [2]. Serves as an accepted reference value. |
| High-Purity Analytes | The authentic target substance (e.g., Active Pharmaceutical Ingredient - API) of known high purity, used for preparing calibration standards and spike solutions for accuracy and linearity studies [4]. |
| Placebo/Blank Matrix | A mixture containing all excipient materials in the correct proportions but without the active analyte [1]. Used to assess specificity and to prepare spiked samples for accuracy and LOQ/LOD studies. |
| Known Impurities and Degradants | Authentic samples of potential process-related impurities and forced-degradation products [2]. Critical for experimentally demonstrating the specificity of the method. |
| Qualified Chromatographic Columns | Columns with demonstrated performance (e.g., efficiency, selectivity) for the specific method. Robustness testing often involves evaluating columns from different lots or manufacturers [1] [4]. |
| Calibrated Instrumentation | Analytical instruments (e.g., HPLC, GC) that have undergone Installation, Operational, and Performance Qualification (IQ/OQ/PQ) to ensure they are fit for purpose and generate reliable data [2] [5]. |
Analytical Method Validation stands as a non-negotiable discipline within pharmaceutical quality control and the broader research landscape. It is the definitive process that transforms a developed analytical procedure into a scientifically sound and legally defensible tool. By rigorously characterizing the method's performance against predefined criteria such as accuracy, precision, and specificity, validation provides the documented evidence required to trust the data generated. This trust is the foundation for ensuring that every pharmaceutical product released to the market possesses the required identity, strength, quality, and purity, thereby safeguarding patient health and upholding the integrity of the global drug supply. As analytical technologies advance and regulatory frameworks evolve, the principles of AMV will continue to serve as the critical link between innovative drug development and consistent, reliable manufacturing.
Analytical method validation serves as a fundamental pillar in the pharmaceutical industry, providing documented evidence that a specific analytical procedure is fit for its intended purpose. This process guarantees the reliability, accuracy, and consistency of test results used to assess the identity, strength, quality, purity, and potency of drug substances and products. The precision of these methods directly influences the safety and efficacy of pharmaceutical products reaching patients [6]. A harmonized regulatory framework for this validation is crucial for streamlining global drug development and approval processes.
The International Council for Harmonisation (ICH) plays a pivotal role in establishing these technical guidelines. The recently adopted ICH Q2(R2) guideline, effective from 14 June 2024, represents the most current and comprehensive standard [7] [6]. This revision, developed in parallel with ICH Q14 on Analytical Procedure Development, introduces a modernized, science-based approach to analytical validation, aligning it with the entire lifecycle of a pharmaceutical product [6] [8]. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have endorsed and implemented these harmonized guidelines, facilitating a unified standard for industry professionals and regulators alike [7] [9].
Objective and Scope
The primary objective of ICH Q2(R2) is to provide a general framework for the principles of analytical procedure validation and to offer guidance on the selection and evaluation of various validation tests [7] [9]. It aims to bridge differences in terminology and requirements that often exist between various international compendia and regulatory documents [9]. The guideline is designed to improve regulatory communication and facilitate more efficient, science-based, and risk-based approval, as well as post-approval change management of analytical procedures [6].
The scope of ICH Q2(R2) is extensive. It applies to new or revised analytical procedures used for the release and stability testing of commercial drug substances and products, covering both chemical and biological/biotechnological entities [9] [6]. Furthermore, it can be applied to other analytical procedures used as part of a control strategy following a risk-based approach [9]. A significant expansion in this revision is the inclusion of validation principles for the analytical use of spectroscopic or spectrometry data (e.g., NIR, Raman, NMR, MS), which often require multivariate statistical analyses [7] [6].
Historical Context and Evolution
The ICH Q2 guideline has evolved over three decades to keep pace with scientific and technological advancements. The following timeline illustrates its key developmental milestones:
Figure 1: The ICH Q2 guideline evolution timeline
The most notable change in Q2(R2) is its development in conjunction with ICH Q14, creating a seamless framework that connects analytical procedure development with validation [6]. This lifecycle approach acknowledges that validation is not a one-time event but an ongoing process.
Core Validation Principles in ICH Q2(R2)
Key Terminology and Definitions
ICH Q2(R2) provides a collection of terms and definitions crucial for ensuring a common understanding across the industry and regulatory bodies. Some of the key terms include:
- Reportable Range: This is the interval between the upper and lower levels of analyte that have been demonstrated to be determined with a suitable level of precision, accuracy, and linearity. It replaces the previous concept of "Linearity" to better accommodate biological and non-linear analytical procedures [6].
- Working Range: This consists of the "Suitability of calibration model" and "Lower Range Limit verification." It is the actual interval of analyte concentrations over which the analytical procedure operates effectively, derived from the reportable range based on sample preparation and analytical technique [6].
- Specificity/Selectivity: The ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [9].
- Accuracy and Precision: Accuracy expresses the closeness of agreement between the measured value and the true value, while precision expresses the closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample [9].
Validation Characteristics and Experimental Protocols
The validation of an analytical procedure requires testing for several performance characteristics based on the procedure's intended purpose. The table below summarizes these characteristics and their experimental considerations:
Table 1: Analytical Procedure Validation Characteristics & Protocols
| Validation Characteristic | Experimental Protocol & Methodology | Key Considerations |
|---|---|---|
| Specificity/Selectivity | - Compare chromatographic or spectral profiles of analyte alone vs. in presence of interfering compounds.- For stability-indicating methods, subject samples to stress conditions (heat, light, acid, base, oxidation). | - Demonstrate separation of analyte from known and potential impurities.- For biological assays, demonstrate interference from matrix components. |
| Working Range | - Prepare and analyze a minimum of 5 concentration levels across the specified range.- Evaluate suitability of the calibration model (linear vs. non-linear).- Verify Lower Range Limit. | - Range is derived from the reportable range based on sample preparation and analytical technique.- Replaces the traditional "Linearity" characteristic. |
| Accuracy | - Spike placebo with known amounts of analyte (3 levels, 3 replicates each).- Compare measured results to theoretical values.- Use a minimum of 9 determinations across the specified range. | - For drug substance, compare against a reference standard of known purity.- For drug product, perform recovery studies. |
| Precision | Repeatability:- Multiple measurements by same analyst under identical conditions.Intermediate Precision:- Different days, analysts, or equipment within the same laboratory.Reproducibility:- Collaborative studies across different laboratories. | - Express as standard deviation or relative standard deviation.- Intermediate precision studies the within-laboratory variations. |
| Detection Limit (DL) & Quantitation Limit (QL) | Visual Evaluation:- Based on signal-to-noise ratio.Standard Deviation Method:- Based on the standard deviation of the response and the slope of the calibration curve. | - DL: Lowest amount detectable but not necessarily quantifiable.- QL: Lowest amount quantifiable with acceptable precision and accuracy. |
| Robustness | - Deliberate variations in method parameters (pH, mobile phase composition, temperature, flow rate).- Use experimental design (DOE) for multivariate procedures. | - Identify critical procedural parameters that affect analytical results.- Establish a system suitability test to control these parameters. |
The experimental workflow for validating an analytical procedure follows a systematic approach, as illustrated below:
Figure 2: Analytical procedure validation workflow
The Regulatory Landscape: FDA, EMA, and USP
FDA Guidance on Analytical Procedures
The U.S. FDA has fully adopted the ICH Q2(R2) guideline, announcing its availability as a final guidance document in March 2024 [7]. This guidance provides a general framework for the principles of analytical procedure validation, including validation principles that cover the analytical use of spectroscopic data [7]. The FDA emphasizes that the guidance is intended to "facilitate regulatory evaluations and potential flexibility in postapproval change management of analytical procedures when scientifically justified" [7].
Prior to the adoption of ICH Q2(R2), the FDA maintained its own guidance document "Analytical Procedures and Methods Validation for Drugs and Biologics" from July 2015, which provided recommendations on submitting analytical procedures and methods validation data to support drug applications [10]. With the issuance of the new ICH-based guidance, the 2015 document and the 2000 draft guidance on the same topic have been effectively superseded [7] [10].
EMA's Approach to Analytical Validation
The European Medicines Agency (EMA) has similarly adopted the ICH Q2(R2) guideline as a scientific guideline for the industry [9]. The EMA states that the guideline "applies to new or revised analytical procedures used for release and stability testing of commercial drug substances and products (chemical and biological/biotechnological)" and that it "can also be applied to other analytical procedures used as part of the control strategy following a risk-based approach" [9].
The EMA's scientific guidelines on specifications, analytical procedures, and analytical validation help medicine developers prepare marketing authorization applications for human medicines [11]. The agency recognizes the importance of method transfer between laboratories and has published concept papers on transferring quality control methods validated in collaborative trials to a product/laboratory specific context [12].
Relationship with USP Guidelines
While the search results do not explicitly mention USP (United States Pharmacopeia) guidelines, it is important to note that USP general chapters on validation of compendial procedures have historically been aligned with ICH guidelines. With the adoption of ICH Q2(R2), it is expected that USP will update its relevant chapters to maintain alignment with these international standards.
The harmonized approach between ICH, FDA, EMA, and USP reduces the regulatory burden on pharmaceutical companies operating in multiple regions, allowing them to develop a single validation package that meets the requirements of all these regulatory bodies.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful analytical method validation requires carefully selected reagents and materials. The following table details key research reagent solutions and their functions in validation experiments:
Table 2: Essential Research Reagents and Materials for Analytical Validation
| Reagent/Material | Function in Validation | Application Examples |
|---|---|---|
| Reference Standards | - Certified materials with known purity and identity used to calibrate instruments and prepare known concentration samples for accuracy, precision, and linearity studies. | - Drug substance and drug product reference standards from USP, EP, or certified suppliers. |
| Placebo Formulation | - A mixture of all inactive components of the drug product used to demonstrate specificity and assess potential interference in accuracy and LOD/LOQ studies. | - Prepared according to the drug product composition without the active ingredient. |
| Forced Degradation Materials | - Chemicals and conditions used to intentionally degrade the drug substance or product to demonstrate the stability-indicating capability of the method. | - Acid (e.g., HCl), Base (e.g., NaOH), Oxidizing agents (e.g., H₂O₂), Thermal chambers, UV light chambers. |
| High-Purity Solvents & Reagents | - Used for preparation of mobile phases, sample solutions, and standard solutions to minimize background interference and ensure reproducibility. | - HPLC-grade solvents, ultrapure water, analytical-grade salts and buffers. |
| System Suitability Test Materials | - Reference preparations used to verify that the analytical system is operating properly before and during the analysis of validation samples. | - Typically a reference standard solution at a specific concentration that provides key parameters (e.g., retention time, peak area, resolution). |
Advanced Topics: Q2(R2) and Multivariate Methods
Integration with ICH Q14: A Lifecycle Approach
A fundamental advancement in the revised guideline is its intrinsic connection with ICH Q14 "Analytical Procedure Development." These two documents were developed in parallel and are intended to be implemented together, creating a comprehensive framework for the entire analytical procedure lifecycle [6] [8]. This integrated approach offers several significant benefits:
- Knowledge-Driven Validation: Suitable data derived from development studies (per ICH Q14) can be used as part of the validation data package, reducing redundant testing and leveraging existing knowledge [6].
- Risk-Based Approaches: The enhanced understanding gained during method development facilitates a more scientific, risk-based validation strategy, focusing resources on critical method aspects [8].
- Efficient Change Management: Knowledge gained from applying an enhanced approach to analytical procedure development provides better assurance of procedure performance and enables more efficient regulatory approaches to postapproval changes [8].
Validation of Multivariate and Non-Linear Methods
ICH Q2(R2) explicitly addresses the validation of modern analytical techniques, including multivariate methods such as Near-Infrared (NIR) and Raman spectroscopy, which often employ complex statistical models like Principal Component Analysis (PCA) or Partial Least Squares (PLS) regression [6]. The guideline recognizes that these methods may not follow traditional linear relationships and provides adapted validation principles.
For these advanced techniques, the concept of "Reportable Range" replaces the traditional "Linearity" characteristic, acknowledging that some analytical procedures, particularly biological assays, may exhibit non-linear response functions [6]. The validation focuses on the "Working Range," which consists of verifying the suitability of the calibration model and the lower range limit [6]. This approach ensures that these powerful analytical tools can be appropriately validated and gain regulatory acceptance.
The regulatory framework for analytical method validation, centered on ICH Q2(R2) with adoption by FDA and EMA, represents a significant evolution in pharmaceutical quality systems. This modernized approach embraces scientific understanding, risk-based principles, and lifecycle management of analytical procedures. The integration of Q2(R2) with ICH Q14 creates a cohesive system that connects development with validation, facilitating more robust analytical procedures and efficient post-approval changes.
For researchers, scientists, and drug development professionals, understanding and implementing this harmonized framework is crucial for successful regulatory submissions across international markets. The guidelines provide the flexibility to incorporate advanced analytical technologies while maintaining rigorous standards for demonstrating that analytical procedures remain fit for their intended purpose throughout their lifecycle. As analytical technologies continue to evolve, this science- and risk-based framework will continue to support innovation while ensuring product quality, safety, and efficacy.
Analytical method validation provides documented evidence that an analytical procedure is suitable for its intended purpose, ensuring the reliability, accuracy, and reproducibility of data in pharmaceutical research and drug development. This in-depth technical guide examines the three core scenarios mandating validation activities: prior to routine use, following method changes, and when introducing new biological matrices. Framed within broader analytical method validation research, this whitepaper details specific experimental protocols and provides structured tables of validation parameters, serving as a critical resource for researchers and development professionals in maintaining data integrity and regulatory compliance.
Method validation is a required process in any regulated environment, providing objective evidence that a method consistently fulfills the requirements for its specific intended use [13] [2]. In pharmaceutical development and bioanalysis, the "fit-for-purpose" paradigm governs validation activities, with the extent of validation directly determined by the application of the data generated [14]. Validation establishes performance characteristics such as accuracy, precision, specificity, and robustness through structured laboratory studies, offering assurance of reliability during normal use [2]. The fundamental requirement stems from the need to ensure the scientific validity of results produced during routine sample analysis, which forms the basis for critical decisions in drug exploration, development, and manufacture [14].
Within a comprehensive validation framework, three primary triggers necessitate validation activities: initial validation before routine application (full validation), re-validation following method modifications (partial validation), and validation when applying existing methods to new matrices (cross-validation or partial validation) [13] [15] [14]. Understanding these requirements is essential for maintaining quality standards throughout the drug development lifecycle.
Core Scenarios Requiring Validation
Pre-Routine Use (Full Validation)
Full validation is comprehensively required for newly developed methods before their implementation in routine testing [13] [14]. This extensive validation provides the foundational documentation of all relevant performance characteristics when no prior validation data exists. According to international guidelines, full validation applies to methods used to produce data supporting regulatory filings or pharmaceutical manufacture for human use [14]. This includes bioanalytical methods for bioavailability (BA), bioequivalence (BE), pharmacokinetic (PK), toxicokinetic (TK), and clinical studies, alongside analytical testing of manufactured drug substances and products [14].
The International Conference on Harmonization (ICH) specifies four primary method types requiring validation, each with distinct requirements [14]:
- Identification tests ensuring analyte identity through comparison to reference standards
- Quantitative tests for impurities content accurately reflecting purity characteristics
- Limit tests controlling impurities
- Quantitative assays measuring the analyte present in drug substance or product
For full validation, all relevant performance parameters must be established, typically including specificity, linearity, accuracy, precision, detection limit, quantitation limit, robustness, and system suitability [2] [16]. The standard operating procedures (SOPs) with step-by-step instructions should be developed specifically for immunochemical methods and multicenter evaluations, though most remain generic enough for other technologies [13].
Method Changes (Partial Validation or Re-validation)
Partial validation is performed when a previously-validated method undergoes modifications that do not constitute fundamental changes to the method's core principles but may still impact performance [13] [14]. This limited validation scope confirms that the method remains suitable for its intended use following specific, defined changes.
Common triggers for partial validation include [14] [2]:
- Transfer of a validated method to another laboratory to be run on different instrumentation by different personnel
- Changes in equipment or instrumentation platforms
- Modifications to solution composition or reagent suppliers
- Adjustments to quantitation range to accommodate different sample concentrations
- Revisions to sample preparation procedures that do not alter the fundamental extraction principle
- Updates to software controlling analytical instrumentation
The extent of partial validation depends directly on the nature and significance of the changes implemented. As stated in validation guidelines, "if a validated in vitro diagnostic (IVD) method is transferred to another laboratory to be run on a different instrument by a different technician it might be sufficient to revalidate the precision and the limits of quantification since these variables are most sensitive to the changes, while more intrinsic properties for a method, e.g., dilution linearity and recovery, are not likely to be affected" [13]. The specific parameters requiring re-validation should be determined through risk assessment evaluating the potential impact of each change on method performance [14].
New Matrices (Partial Validation)
Introducing a new biological matrix from the same species into a previously validated method necessitates partial validation to address matrix-specific effects [15]. This requirement recognizes that biological matrices differ significantly in composition, potentially affecting analytical method performance through matrix effects, interference, or differential analyte recovery.
International guidance specifically recommends partial validation when introducing new matrices, with particular attention to matrix protein content as a critical variable [15]. Transitioning a method validated for serum or plasma to analysis of low-protein matrices such as urine, cerebral spinal fluid (CSF), or oral fluid frequently results in inconsistent analyte recovery due to several factors:
- Increased non-specific binding in low-protein matrices leading to reduced recovery
- Exacerbated adsorption and absorption interactions with container materials
- Differences in endogenous compounds that may cause interference
- Variations in pH and ionic strength affecting analyte stability and detection
The matrix protein content significantly influences method performance, as higher protein levels typically facilitate better analyte stability and reduce surface interactions [15]. When validating methods for low-protein matrices, mitigation strategies may include adding surfactants, bovine serum albumin (BSA), or β-cyclodextrin to minimize non-specific binding and improve recovery rates [15].
Validation Parameters and Experimental Protocols
Key Validation Parameters
Analytical method validation systematically evaluates multiple performance characteristics to ensure method suitability. The specific parameters assessed depend on the method type and its intended application, with full validation requiring comprehensive evaluation.
Table 1: Essential Validation Parameters and Definitions
| Parameter | Definition | Experimental Approach |
|---|---|---|
| Accuracy | Closeness of agreement between accepted reference value and value found | Analysis of samples spiked with known quantities of analyte; comparison to reference material [2] |
| Precision | Closeness of agreement between independent test results under stipulated conditions | Repeated analyses of homogeneous samples; measured as repeatability, intermediate precision, reproducibility [13] [2] |
| Specificity | Ability to measure analyte accurately in presence of components that may be expected to be present | Resolution of analyte from closely eluting compounds; peak purity tests using PDA or MS detection [2] |
| Linearity | Ability to obtain test results proportional to analyte concentration within given range | Minimum of 5 concentration levels across specified range; statistical analysis of calibration curve [2] |
| Range | Interval between upper and lower concentrations with demonstrated precision, accuracy, linearity | Established from linearity studies; confirms acceptable performance across specified concentration levels [2] |
| LOD/LOQ | Lowest concentration of analyte that can be detected (LOD) or quantitated (LOQ) with acceptable precision | Signal-to-noise ratios (3:1 for LOD, 10:1 for LOQ) or based on standard deviation of response and slope [2] |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters | Systematic changes to critical parameters (e.g., incubation times, temperatures) while analyzing same samples [13] |
| Recovery | Detector response from analyte added to and extracted from matrix compared to true concentration | Comparison of extracted samples to non-extracted standards; demonstrates extraction efficiency [13] |
Experimental Design and Protocols
Precision Evaluation
Precision validation encompasses three distinct measurements requiring specific experimental designs [13] [2]:
Repeatability (intra-assay precision): Assessed by analyzing a minimum of nine determinations covering the specified range (three concentrations, three repetitions each) or a minimum of six determinations at 100% of the test concentration under identical conditions over a short time interval. Results reported as %RSD.
Intermediate precision: Evaluates within-laboratory variations due to random events using experimental design where factors are deliberately varied (different days, analysts, equipment). Typically generated by two analysts preparing and analyzing replicate sample preparations independently, using different HPLC systems. Results subjected to statistical testing (e.g., Student's t-test) to examine differences in mean values.
Reproducibility: Assesses collaborative studies between different laboratories, requiring a minimum of eight sets of acceptable results after outlier removal. Documentation includes standard deviation, relative standard deviation, and confidence intervals.
Robustness Testing
Robustness validation follows a structured protocol [13]:
- Identify critical parameters in the procedure (e.g., incubation times, temperatures, pH, mobile phase composition)
- Perform assays with systematic variations in these parameters, one at a time, using identical test samples
- If measured concentrations remain unaffected by variations, adjust protocol to incorporate appropriate tolerances (e.g., 30 ± 3 minutes)
- If changes systematically alter results, reduce magnitude of variations until no dependence is observed
- Incorporate established tolerances into the final method protocol
For methods with multiple critical parameters, specialized software (e.g., MODDE) or published experimental design methods can reduce the number of required experiments [13].
Matrix-Related Partial Validation
When introducing a new matrix, a targeted partial validation protocol should include [15]:
- Comparison of matrix properties: Evaluate analyte chemistry, sample container materials, and biological matrix characteristics between original and new matrices
- Assessment of matrix effects: Analyze multiple lots of the new matrix (at least 6) to account for natural variability, comparing precision and accuracy to original validation
- Recovery experiments: Determine analyte recovery in the new matrix across the validated concentration range, identifying potential non-specific binding issues
- Stability assessment: Evaluate analyte stability in the new matrix under various storage conditions
- Selectivity verification: Confirm absence of interfering substances specific to the new matrix
Decision Framework for Validation Requirements
The flowchart below outlines the decision process for determining the appropriate validation level based on specific scenarios and changes to the analytical method:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful method validation requires specific, high-quality materials and reagents to ensure accurate and reproducible results. The following table details essential components for validation experiments:
Table 2: Essential Research Reagents and Materials for Method Validation
| Material/Reagent | Function in Validation | Critical Considerations |
|---|---|---|
| Certified Reference Standards | Provides accepted reference value for accuracy determination; establishes calibration curve | Purity certification; proper storage conditions; stability documentation [2] |
| Matrix Blank Samples | Evaluates specificity and selectivity; establishes baseline interference | Multiple lots required to account for natural variability; appropriate storage [15] [17] |
| Quality Control Samples | Assesses precision and accuracy across validation range | Prepared at low, medium, high concentrations; should mimic actual study samples [17] |
| Internal Standards | Compensates for variability in sample preparation and analysis | Stable isotope-labeled analogs preferred; should not interfere with analyte [2] |
| System Suitability Solutions | Verifies chromatographic system performance before validation experiments | Evaluates resolution, tailing factor, plate count, repeatability [2] |
| Protein Additives (BSA) | Mitigates non-specific binding in low-protein matrices | Critical for urine, CSF, oral fluid validations; concentration optimization required [15] |
| Surfactants & Stabilizers | Improves recovery in challenging matrices; enhances solubility | Compatibility with detection method; minimal background interference [15] |
Method validation represents a fundamental requirement in pharmaceutical research and drug development, providing documented evidence of analytical procedure suitability for its intended use. The three primary scenarios demanding validation activities—pre-routine implementation, method modifications, and new matrix introduction—form the cornerstone of quality assurance in analytical data generation. Understanding the distinction between full, partial, and cross-validation approaches enables scientists to allocate resources efficiently while maintaining regulatory compliance. As analytical technologies advance and regulatory expectations evolve, the principles of method validation remain essential for ensuring the reliability, accuracy, and reproducibility of data supporting critical decisions in the drug development lifecycle. Through systematic application of the protocols and decision frameworks outlined in this technical guide, researchers and development professionals can effectively establish method suitability while advancing the broader objectives of analytical method validation research.
Analytical method validation is a cornerstone of pharmaceutical development, providing the foundation for data integrity and regulatory compliance. This in-depth technical guide examines the three essential prerequisites for successful method validation: robust instrument qualification, well-characterized reference standards, and comprehensive analyst training. Framed within the broader context of analytical method validation research, this whitepaper provides researchers, scientists, and drug development professionals with detailed methodologies, technical specifications, and practical frameworks for establishing these foundational elements. The objective of validation is to demonstrate that an analytical procedure is suitable for its intended purpose, requiring meticulous attention to these prerequisites before validation activities can commence [18].
Within the pharmaceutical development lifecycle, analytical method validation research generates evidence that test methods are capable of producing reliable results that support product quality assessments. According to regulatory guidelines, "Methods validation is the process of demonstrating that analytical procedures are suitable for their intended use" [18]. This process depends entirely on three fundamental pillars: properly qualified instruments that generate accurate data, characterized reference standards that provide points of comparison, and competent analysts who execute procedures correctly. Without establishing these prerequisites, any subsequent validation data remains questionable.
The requirement for validated methods extends throughout the drug development continuum. While early-phase studies may employ "qualified" methods with limited validation data, late-stage trials and commercial products require fully validated methods per current regulations [18]. The US Food and Drug Administration states that "the suitability of all testing methods used shall be verified under actual conditions of use" [18], making these prerequisites non-negotiable for laboratories operating under Good Manufacturing Practice (GMP), Good Laboratory Practice (GLP), and Good Clinical Practice (GCP) regulations.
Instrument Qualification
Definition and Regulatory Framework
Instrument qualification is the process of documenting that equipment is properly installed, functions correctly, and performs according to predefined specifications, thus ensuring it is fit for its intended analytical purpose. Qualification establishes evidence that instruments produce reliable and consistent results, forming the foundational layer for all subsequent analytical measurements. The International Organization for Standardization outlines competency and operational requirements for testing laboratories in ISO/IEC 17025, which emphasizes the need for properly maintained equipment to ensure valid results [19].
The Four-Phase Qualification Framework
Instrument qualification follows a structured approach across four distinct phases:
- Design Qualification (DQ): The documented verification that the proposed instrument design and specifications meet the analytical requirements and intended application. This phase establishes the foundation for all subsequent qualification activities.
- Installation Qualification (IQ): The documented verification that the instrument has been delivered, installed, and configured according to the manufacturer's specifications and the laboratory's requirements. This includes verification of components, documentation, and installation environment.
- Operational Qualification (OQ): The documented verification that the installed instrument operates according to predefined specifications throughout its anticipated operating ranges. This phase tests instrument functionality and performance under standardized conditions.
- Performance Qualification (PQ): The documented verification that the instrument consistently performs according to predefined specifications for the specific analytical methods and applications under actual conditions of use. This ongoing verification occurs during routine analysis.
Performance Parameters and Acceptance Criteria
The table below summarizes key performance parameters and typical acceptance criteria for liquid chromatography instrumentation, though specific requirements vary by instrument type and application.
Table 1: Performance Parameters for Liquid Chromatography Instrument Qualification
| Parameter | Test Method | Acceptance Criteria | Frequency |
|---|---|---|---|
| Pump Flow Accuracy | Measure volumetric flow at multiple set points | ± 1-2% of set flow rate | OQ / Periodic PQ |
| Pump Composition Accuracy | Measure ratio of mobile phases | ± 0.5-1.0% absolute | OQ / Periodic PQ |
| Injector Precision | Multiple injections of standard | RSD ≤ 0.5-1.0% | OQ / Periodic PQ |
| Injector Carryover | Inject blank after high concentration | ≤ 0.1-0.5% of target concentration | OQ / Periodic PQ |
| Detector Wavelength Accuracy | Scan holmium oxide filter | ± 1-2 nm from certified values | OQ / Annual PQ |
| Detector Noise and Drift | Monitor baseline signal | Specification per manufacturer | OQ / Periodic PQ |
| Column Oven Temperature | Measure with independent probe | ± 1-3°C of set temperature | OQ / Annual PQ |
Experimental Protocol for Pump Flow Accuracy
Purpose: To verify that the delivered flow rate matches the set flow rate across the instrument's operational range.
Materials: Calibrated digital thermometer, calibrated analytical balance (0.1 mg sensitivity), weighing vessel, HPLC-grade water, stopwatch, and graduated cylinder.
Procedure:
- Allow the HPLC system to equilibrate at ambient temperature.
- Set the pump to deliver 100% mobile phase (water) at 1.0 mL/min.
- Prime the system thoroughly to remove air bubbles.
- Place an empty weighing vessel on the balance and tare.
- Direct the column outlet to the weighing vessel and simultaneously start the stopwatch.
- Collect eluent for exactly 10 minutes.
- Weigh the collected eluent and record the mass.
- Calculate the actual flow rate using the density of water at the recorded temperature.
- Repeat the procedure at different flow rates (e.g., 0.5 mL/min, 1.5 mL/min, 2.0 mL/min).
- Calculate the percentage difference between set and actual flow rates.
Acceptance Criteria: The actual flow rate must be within ± 2% of the set flow rate at each tested value.
Reference Standards
Characterization and Classification
Reference standards are highly characterized substances used as comparison benchmarks in analytical procedures. They provide the critical link between measured values and true values, enabling quantification and method qualification. According to regulatory guidelines, method specificity must demonstrate the ability to assess the analyte unequivocally in the presence of potential interferents, which requires well-characterized reference standards [18].
Table 2: Classification and Characterization of Reference Standards
| Standard Type | Source | Characterization Requirements | Primary Use |
|---|---|---|---|
| Primary Reference Standard | Pharmacopeial (USP, EP) or certified reference material | Fully characterized with Certificate of Analysis (CoA); highest purity available | Method validation and qualification |
| Secondary Reference Standard | Qualified against primary standard; internally or commercially sourced | CoA with purity and qualification data | Routine testing where primary standard is unavailable or costly |
| Working Reference Standard | Qualified against primary or secondary standard; internally prepared | Documented testing for identity, purity, and strength | Daily system suitability and calibration |
| Impurity Reference Standard | Pharmacopeial, commercial, or isolated from process | Characterized with identity and purity assessment | Identification and quantification of impurities |
Experimental Protocol for Purity Determination by HPLC
Purpose: To determine the purity of a reference standard using HPLC with area normalization for use in method validation.
Materials: Reference standard sample, HPLC system with UV detector, qualified balance, appropriate solvents, and calibrated volumetric glassware.
Procedure:
- Prepare the sample solution at an appropriate concentration (typically 0.1-1.0 mg/mL) in the designated diluent.
- Inject the sample solution into the HPLC system using the validated method.
- Record the chromatogram with adequate run time to ensure all impurities are eluted and detected.
- Integrate all peaks in the chromatogram, excluding the solvent front.
- Calculate the percentage of each impurity using the area normalization method: % Impurity = (Peak Area of Impurity / Total Area of All Peaks) × 100%
- Calculate the purity of the main component: % Purity = 100% - Total % of All Impurities
- Perform minimum triplicate determinations to ensure result consistency.
Acceptance Criteria: The primary reference standard should have a purity of ≥ 99.0% unless otherwise justified. The relative standard deviation (RSD) for replicate determinations should be ≤ 2.0%.
Storage and Handling Requirements
Proper storage and handling are critical for maintaining reference standard integrity. Standards should be stored in conditions that maintain stability, typically in sealed containers protected from light, moisture, and excessive temperature. The storage conditions should be based on stability data and clearly documented. Access should be controlled to prevent contamination or mix-ups, and usage logs should track quantities and dates of use.
Trained Analysts
Competency Requirements
Analyst competency forms the human foundation of reliable analytical data. ISO/IEC 17025 emphasizes that "the laboratory shall document the competence requirements for each function influencing the results of laboratory activities" [20]. This includes specific requirements for education, qualification, training, technical knowledge, skills, and experience appropriate to each role. Competency requirements must be formally documented for all positions, including technicians, internal auditors, quality managers, and support staff involved in laboratory activities [20].
Comprehensive Training Framework
ISO/IEC 17025 requires laboratories to maintain procedures for determining competency requirements, personnel selection, training, supervision, authorization, and ongoing monitoring of competence [20]. The training process should include:
- Initial Assessment: Evaluation of education, qualifications, and experience against documented competency requirements.
- Structured Training Program: Combination of theoretical instruction and practical exercises on specific techniques, instruments, and standard operating procedures.
- Supervised Practice: Hands-on application of methods under supervision until proficiency is demonstrated.
- Authorization: Formal approval to perform specific tasks independently based on demonstrated competency.
- Continuous Monitoring: Ongoing assessment through performance reviews, proficiency testing, and periodic recertification.
Experimental Protocol for Analyst Competency Assessment
Purpose: To objectively demonstrate an analyst's competency in executing a specific analytical method.
Materials: Approved test method procedure, qualified instrument, reference standards, test samples, and data recording system.
Procedure:
- Select a validated analytical method relevant to the analyst's responsibilities.
- Provide the analyst with the method procedure, applicable SOPs, and necessary materials.
- The analyst prepares all required solutions and standards independently.
- The analyst performs the analysis according to the method, including system suitability tests.
- A qualified supervisor observes the technique and records any deviations.
- The analyst processes the data and reports the results.
- Evaluate the results against predefined criteria including:
- System suitability requirements met
- Accuracy of standard preparation (compared to theoretical values)
- Precision of replicate injections (RSD within specified limits)
- Accuracy of sample results (compared to known values or reference analyst)
- Adherence to documentation and data integrity practices
Acceptance Criteria: The analyst must meet all method validation parameters (accuracy, precision, etc.) within specified limits and demonstrate proper technique without critical errors.
Integrated Workflow for Establishing Prerequisites
The following diagram illustrates the logical relationship and sequential dependencies between the three essential prerequisites in the analytical method validation framework:
Analytical Method Validation Prerequisites Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for establishing the prerequisites for analytical method validation:
Table 3: Essential Research Reagent Solutions for Method Validation Prerequisites
| Reagent/Material | Technical Function | Quality Requirements | Application Context |
|---|---|---|---|
| System Suitability Standards | Verify instrument performance and method suitability prior to analysis | Certified reference materials or highly characterized compounds | Daily instrument qualification and method performance verification |
| Primary Reference Standards | Provide ultimate traceability for quantitative measurements | Pharmacopeial standards or CRM with full characterization | Method validation, qualification of secondary standards, critical testing |
| HPLC/MS Grade Solvents | Mobile phase preparation to minimize background interference and enhance detection | Low UV absorbance, high purity, minimal particulate matter | All chromatographic methods, especially for sensitive detection techniques |
| Volumetric Glassware | Precise measurement and preparation of standard and sample solutions | Class A certification, calibration certificates | Standard preparation, sample dilution, mobile phase preparation |
| Stable Isotope Labeled Standards | Internal standards for mass spectrometric methods to correct for variability | High isotopic purity, chemical purity matching analyte | Bioanalytical method validation, complex matrix analysis |
| Filter Membranes | Sample clarification and removal of particulate matter | Low extractables, compatible with solvent systems, appropriate pore size | Sample preparation for chromatographic analysis, especially UHPLC systems |
Instrument qualification, reference standards, and trained analysts represent the fundamental triad that must be established before undertaking analytical method validation research. These prerequisites ensure the generation of reliable, accurate, and reproducible data that meets regulatory expectations. By systematically addressing these foundational elements through documented protocols, objective evidence, and continuous monitoring, laboratories establish a culture of quality and scientific rigor. This foundation supports the broader objective of analytical method validation research: to demonstrate unequivocally that analytical procedures are fit for their intended purpose throughout the drug development lifecycle.
Analytical method validation represents a critical investment in pharmaceutical development and manufacturing, serving as the primary defense against product failure, regulatory non-compliance, and patient harm. This technical guide examines the structured framework of method validation through a risk-based lens, demonstrating how rigorous experimental protocols and lifecycle management directly reduce business risks while safeguarding patient safety. By implementing modern validation approaches aligned with ICH Q2(R2) and Q14 guidelines, organizations can achieve significant cost reductions through streamlined operations while ensuring the reliability of analytical data that forms the foundation of therapeutic decision-making.
Analytical method validation is the documented process of proving that an analytical procedure is suitable for its intended purpose, ensuring the reliability, reproducibility, and compliance of data throughout the drug development lifecycle [21]. Beyond technical necessity, validation represents a strategic business function that systematically mitigates risks across multiple domains—regulatory, operational, financial, and most critically, patient safety. The fundamental business case for validation rests on its capacity to prevent costly failures, streamline product development, and maintain product quality that protects consumers.
The contemporary validation landscape has evolved from a prescriptive "check-the-box" exercise to a science- and risk-based framework emphasized in modern ICH Q2(R2) and Q14 guidelines [22]. This paradigm shift enables organizations to focus resources more efficiently, with implementations typically reducing unnecessary testing by 30-45% while maintaining or improving quality outcomes [23]. The validation process thus transforms from a compliance cost center to a value-generating activity that directly supports business objectives through enhanced efficiency and risk mitigation.
Regulatory Foundation and the Risk-Based Approach
The ICH and FDA Regulatory Framework
The International Council for Harmonisation (ICH) provides the harmonized framework that becomes the global gold standard for analytical method guidelines, with the U.S. Food and Drug Administration (FDA) adopting these guidelines for use in the United States [22]. The simultaneous release of ICH Q2(R2) on validation and ICH Q14 on analytical procedure development represents a significant modernization, shifting validation from a one-time event to a continuous lifecycle management process [22].
This regulatory evolution emphasizes a risk-based approach to validation, where resources are allocated according to the potential impact on product quality and patient safety. Method validation risk assessment provides a structured framework to evaluate potential failure points before they impact results, systematically examining critical parameters that might affect method performance from sample preparation to instrument variability and data interpretation [23].
Core Validation Parameters and Requirements
ICH Q2(R2) outlines fundamental performance characteristics that must be evaluated to demonstrate a method is fit for purpose. The selection and extent of validation testing depend on the method's intended use and the associated risks to product quality [9].
Table 1: Core Validation Parameters and Their Risk Mitigation Functions
| Validation Parameter | Technical Definition | Risk Mitigation Function | Business Impact |
|---|---|---|---|
| Accuracy | Closeness of test results to the true value [22] | Prevents incorrect potency assessments | Avoids product recall, overdose, or underdose |
| Precision | Degree of agreement among repeated measurements [22] | Controls variability in manufacturing quality control | Reduces batch rejection rates |
| Specificity | Ability to assess analyte unequivocally [22] | Ensures detection of impurities and degradation | Prevents toxic side effects from impurities |
| Linearity and Range | Interval where suitable accuracy, precision, and linearity exist [22] | Guarantees method performance across all concentrations | Prevents measurement errors at critical decision points |
| Robustness | Capacity to remain unaffected by small variations [22] | Ensures method reliability during transfer and long-term use | Reduces investigation costs and method troubleshooting |
Risk Assessment Methodologies in Validation
Structured Risk Assessment Framework
Method validation risk assessment is a structured approach to identifying potential failures in analytical methods before testing begins [23]. This proactive framework enables organizations to allocate validation resources efficiently by focusing efforts on critical aspects with the highest risk potential, typically reducing unnecessary testing by 30-45% while maintaining or improving quality outcomes [23].
An effective risk assessment framework includes three key components:
- Risk Identification Process: Systematic examination of each aspect of the analytical method to uncover vulnerabilities using assessment techniques like FMEA (Failure Mode Effects Analysis) or fishbone diagrams [23].
- Mitigation Strategy Development: Establishment of specific mitigation techniques designed to address each identified risk, focusing on prevention rather than reaction through redundant verification steps and quantitative acceptance criteria [23].
- Documentation and Communication: Comprehensive documentation standards that capture all risk assessment activities, providing evidence of due diligence and creating an audit trail for regulatory inspections [23].
Analytical Target Profile (ATP) and Lifecycle Management
ICH Q14 introduces the Analytical Target Profile (ATP) as a prospective summary of a method's intended purpose and desired performance characteristics [22]. By defining the ATP at the beginning of development, organizations can use a risk-based approach to design a fit-for-purpose method and a validation plan that directly addresses its specific needs. The ATP serves as the foundation for the entire method lifecycle, facilitating science-based change management without extensive regulatory filings when supported by proper risk assessment [22].
Diagram 1: Method Validation Lifecycle with Risk Assessment
Experimental Protocols for Method Validation
Comparison of Methods Experiment
The comparison of methods experiment is critical for assessing the systematic errors that occur with real patient specimens, estimating inaccuracy or systematic error between a new method and a comparative method [24]. This experimental protocol directly addresses the risk of method inaccuracy impacting patient safety.
Experimental Design:
- Specimen Requirements: A minimum of 40 different patient specimens should be tested by the two methods, selected to cover the entire working range and represent the spectrum of diseases expected in routine application [24]. Specimen quality and range coverage are more critical than quantity alone.
- Time Period: The experiment should include several different analytical runs on different days (minimum of 5 days recommended) to minimize systematic errors that might occur in a single run [24].
- Measurement Approach: Common practice is to analyze each specimen singly by both methods, though duplicate measurements provide advantages for identifying sample mix-ups, transposition errors, and other mistakes [24].
- Comparative Method Selection: When possible, a reference method should be chosen whose correctness is well-documented. With routine methods, large differences may require additional experiments to identify which method is inaccurate [24].
Data Analysis Protocol:
- Graphical Analysis: Create difference plots (test minus comparative results versus comparative result) or comparison plots (test result versus comparative result) to visually inspect data patterns and identify discrepant results [24].
- Statistical Calculations: For data covering a wide analytical range, use linear regression statistics (slope, y-intercept, standard deviation of points about the line) to estimate systematic error at medical decision concentrations [24].
- Bias Calculation: For narrow analytical ranges, calculate the average difference between results (bias) using paired t-test calculations [24].
Validation of Screening Methods
For qualitative screening methods, validation focuses on different performance metrics related to classification accuracy, with specific experimental protocols to address risks of false positives and false negatives [25].
Experimental Design:
- Sample Set: A validation set of reference samples with a minimum of 20 samples for each class recommended to ensure representativeness [25].
- Contingency Analysis: Results are displayed in a contingency table comparing method results against reference values, calculating sensitivity, specificity, and predictive values [25].
- Applicability Indicators: Proposed indicators including error index, saving index, penalty index, and loss index to evaluate real-world performance in specific scenarios [25].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagent Solutions for Method Validation
| Reagent/ Material | Technical Function | Validation Application | Risk Mitigation Role |
|---|---|---|---|
| Reference Standards | Provides known concentration for accuracy determination [26] | Calibration curve construction, accuracy assessment | Ensures traceability and prevents systematic bias |
| Placebo Formulations | Blank matrix without active ingredient | Specificity testing, interference checking [22] | Confirms method selectively measures analyte |
| System Suitability Solutions | Verifies instrument performance before analysis | Precision validation, system verification [22] | Prevents instrument-related failures during validation |
| Stability Samples | Evaluates analyte durability under various conditions | Forced degradation studies, robustness assessment [22] | Identifies method vulnerabilities to environmental factors |
| Quality Control Materials | Monitors ongoing method performance | Precision studies, intermediate precision validation [22] | Detects method drift and analyst-to-analyst variability |
Quantitative Impact: Validation as Risk Reduction
The business case for method validation is substantiated by quantitative outcomes demonstrating risk reduction across multiple dimensions. Organizations implementing risk-based validation typically reduce unnecessary testing by 30-45% while maintaining or improving quality outcomes [23]. Case studies document specific financial impacts, with one medical center reporting savings of $2.3 million after implementing risk-based protocols that prioritized critical parameters while eliminating redundant tests [23].
Diagram 2: Validation Investment and Return Relationship
Analytical method validation represents far more than a regulatory requirement—it is a fundamental business strategy that systematically reduces risk while ensuring patient safety. By implementing modern, risk-based validation approaches aligned with ICH Q2(R2) and Q14 guidelines, organizations achieve dual objectives: substantial operational efficiencies quantified at 30-45% reduction in unnecessary testing, and robust patient protection through reliable analytical data. The validation lifecycle model, anchored by the Analytical Target Profile and continuous monitoring, provides a framework for maintaining method reliability throughout a product's commercial life. As pharmaceutical manufacturing evolves toward more complex modalities and global supply chains, the business case for rigorous method validation grows increasingly compelling, ultimately delivering value through protected patient health and sustainable business operations.
Core Validation Parameters and Practical Implementation Strategies
Within the framework of analytical method validation research, establishing the accuracy of an assay is paramount. Accuracy, defined as the closeness of agreement between a measured value and a true reference value, is quantitatively assessed through spike-and-recovery experiments [27]. This guide details the role of these experiments in validating immunoassays such as ELISA, providing in-depth technical protocols, data interpretation guidelines, and troubleshooting strategies essential for researchers, scientists, and drug development professionals. The core postulate is that a well-validated method must demonstrate that the sample matrix does not interfere with the accurate detection and quantification of the analyte, thereby ensuring the reliability of data used in critical decision-making processes [28] [29].
Core Principles and Definitions
The Purpose of Spike-and-Recovery Assessment
The fundamental purpose of a spike-and-recovery experiment is to determine whether the detection of an analyte is affected by differences between the matrix used for the standard curve and the biological sample matrix [27]. In an ideal assay, the response for a given amount of analyte would be identical whether it is in the standard diluent or the sample matrix. However, components within a complex biological sample (e.g., serum, plasma, urine, or cell culture supernatant) can alter the assay response, leading to either an overestimation or underestimation of the true analyte concentration [29]. This experiment involves adding ("spiking") a known quantity of the pure analyte into the natural sample matrix and then measuring the amount recovered by the assay [27] [28].
Relationship with Other Validation Parameters
Spike-and-recovery is intrinsically linked to other parameters in method validation:
- Dilutional Linearity: Determines if a sample spiked with analyte above the upper limit of detection can be reliably quantified after serial dilution within the assay's standard curve range [28]. It confirms assay flexibility and accuracy across dilutions.
- Parallelism: Assesses whether samples with high endogenous levels of the analyte provide the same degree of detection as the standard curve analyte after dilution, indicating comparable immunoreactivity [28].
Poor performance in any of these areas indicates potential matrix interference, which can stem from factors like pH, salt concentrations, detergents, or background proteins that affect antibody-binding affinity [28].
Experimental Methodology
Detailed Experimental Protocol
A robust spike-and-recovery experiment follows a structured protocol. The workflow below outlines the key stages from sample preparation to final calculation.
Step-by-Step Procedure:
- Sample Preparation: For each type of sample matrix to be validated, prepare a "neat" (undiluted) sample and/or a sample diluted in the chosen sample diluent to its Minimum Required Dilution (MRD) [29].
- Spiking: Spike a known amount of the pure standard analyte into the sample matrix. It is recommended to use 3-4 concentration levels covering the analytical range of the assay, ensuring the lowest is at least 2 times the Limit of Quantitation (LOQ) [29].
- Example: Spike 100 µL of a 100 ng/mL standard into 400 µL of the neat sample. This results in a 1:5 dilution and a final theoretical spike concentration of 20 ng/mL [29].
- Control Preparation: In parallel, prepare a control by spiking the same known amount of analyte into the standard diluent used for the standard curve. Also, prepare a "zero-spike" control for the sample matrix (sample + diluent without analyte) to account for any endogenous levels of the analyte [27] [29].
- Assay Execution: Run the complete ELISA procedure for all spiked samples, controls, and the standard curve.
- Calculation:
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials required for performing a spike-and-recovery experiment.
| Item | Function & Importance |
|---|---|
| Purified Analyte Standard | A known quantity of the pure protein or analyte is used to spike the sample. This serves as the reference "true value" for calculating recovery [27] [29]. |
| Appropriate Sample Matrix | The actual biological sample (e.g., serum, urine, cell culture supernatant) being validated. Its unique composition is the source of potential interference [27]. |
| Standard Diluent | The buffer used to prepare the standard curve. Optimizing its composition to match the sample matrix (e.g., by adding a carrier protein like BSA) can mitigate recovery issues [27]. |
| Sample Diluent | The buffer used to dilute the sample. It may differ from the standard diluent and is optimized to reduce matrix effects while maintaining analyte detectability [27]. |
| Validated ELISA Kit/Reagents | Includes the pre-coated plate, detection antibodies, and enzyme conjugate. The assay must be robust and characterized (LOD, LOQ, dynamic range) before spike-recovery assessment [29]. |
Data Interpretation and Acceptance Criteria
Interpreting Spike-and-Recovery Results
The calculated percentage recovery indicates the degree of matrix interference. According to ICH, FDA, and EMA guidelines on analytical procedure validation, recovery values within 75% to 125% of the spiked concentration are generally considered acceptable [29]. Recovery outside this range indicates significant interference.
- Under-Recovery (<75%): Suggests components in the sample matrix are inhibiting antibody binding or the analyte is being sequestered, leading to an underestimation of the true concentration [29].
- Over-Recovery (>125%): May indicate non-specific binding of matrix components to assay reagents or interaction of the drug substance with antibodies, causing an overestimation [29].
Representative Data Tables
The following tables illustrate how spike-and-recovery and linearity-of-dilution data are typically structured and analyzed.
Table 1: Example ELISA Spike-and-Recovery Data for Recombinant Human IL-1 beta in Human Urine Samples (n=9)
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| ... | ... | ... | ... | ... |
| Mean Recovery (± S.D.) | NA | 86.3% ± 9.9% | 85.8% ± 6.7% | 84.6% ± 3.5% |
Data adapted from a representative experiment [27].
Table 2: Summary of Linearity-of-Dilution Results for a Human IL-1 beta Sample
| Sample | Dilution Factor (DF) | Observed (pg/mL) × DF | Expected (Neat Value) | Recovery % |
|---|---|---|---|---|
| ConA-stimulated Cell Culture Supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 |
Data adapted from a representative experiment. Note that recoveries outside the 80-120% range indicate poor linearity at higher dilutions [27].
Troubleshooting and Assay Optimization
Correcting Poor Spike-and-Recovery Results
When recovery falls outside the acceptable range, the following optimization strategies can be employed, as visualized in the troubleshooting pathway below.
Specific corrective actions include:
- Alter the Sample Matrix: If a neat biological sample produces poor recovery, diluting it (e.g., 1:1) in the standard diluent or a logical sample diluent often corrects the issue [27]. Other adjustments include modifying the pH to match the standard diluent or adding a carrier protein like BSA to stabilize the analyte [27].
- Alter the Standard Diluent: The composition of the standard diluent can be modified to more closely resemble the sample matrix. For instance, if analyzing culture supernatants, using culture medium as the standard diluent may improve recovery. However, this may compromise the assay's signal-to-noise ratio, requiring a balance to be struck [27].
Spike-and-recovery analysis is not merely an academic exercise; it is a critical component of qualifying an immunoassay for use in regulated environments. It provides essential validation of assay accuracy, confirming that the method reliably measures the true analyte concentration in the presence of a complex sample matrix. As per regulatory guidelines, this experiment must be performed for each unique sample type evaluated and repeated if the manufacturing process changes [29]. When integrated with other validation parameters such as precision, sensitivity, and dilutional linearity, spike-and-recovery studies form the bedrock of a fit-for-purpose analytical method, ensuring the generation of reliable and defensible data for research and drug development.
Analytical method validation is a critical process in regulated laboratories, providing documented evidence that a method is fit for its intended purpose and ensuring the reliability of data during normal use [2]. This process is fundamental to pharmaceutical development, manufacturing, and quality control, as it supports product quality, patient safety, and regulatory compliance. Within this framework, the validation of analytical performance characteristics follows established guidelines from regulatory bodies such as the International Conference on Harmonisation (ICH) and the U.S. Food and Drug Administration (FDA) [2].
Precision is a core validation parameter and refers to the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [2]. It is essential for confirming that an analytical method can generate consistent and reliable results. Precision is typically investigated at three levels: repeatability, intermediate precision, and reproducibility. Understanding and accurately measuring these three levels provides a complete picture of a method's variability, from short-term operations within a single laboratory to long-term use across multiple sites. This whitepaper provides an in-depth technical guide on the definitions, experimental methodologies, and data interpretation for these three fundamental components of precision.
Defining the Components of Precision
The precision of an analytical method is not a single measurement but a hierarchy of consistency checks. Each level introduces more variables, providing a comprehensive understanding of the method's robustness.
Repeatability: Also known as intra-assay precision, repeatability expresses the closeness of results obtained under identical conditions over a short period of time [30] [31]. This represents the smallest possible variation a method can achieve, as it is assessed using the same measurement procedure, same operators, same measuring system, same operating conditions, and same location [30]. In practice, this is typically performed within a single day or a single analytical run [30] [2].
Intermediate Precision: This level of precision is obtained within a single laboratory over a longer period (e.g., several months) and accounts for additional, realistic variations in day-to-day laboratory operations [30]. Intermediate precision evaluates the impact of factors such as different analysts, different instruments, different calibrants, different batches of reagents, and different days [30] [2]. While these factors may be constant within a single day and behave systematically in the short term, they act as random variables over a longer timeframe. Consequently, the standard deviation for intermediate precision is expected to be larger than that for repeatability [30].
Reproducibility: Reproducibility expresses the precision between measurement results obtained in different laboratories [30] [31]. It is assessed through collaborative inter-laboratory studies and demonstrates that a method can be successfully transferred and executed in different environments, with different equipment and personnel [30] [2]. Reproducibility is critical for method standardization and for methods developed in R&D that will be used in multiple quality control laboratories [30].
The relationship between these three levels can be visualized as a hierarchy of variability, which the following diagram illustrates.
Experimental Protocols for Measuring Precision
A rigorous, statistically sound experimental design is paramount for accurately quantifying the different levels of precision. The following sections detail the standard methodologies for evaluating repeatability, intermediate precision, and reproducibility.
Protocol for Repeatability (Intra-Assay Precision)
Repeatability is the foundational level of precision and is typically the first to be assessed.
- Purpose: To determine the inherent variability of an analytical method when all controllable factors are kept constant [31].
- Experimental Design:
- Analyze a minimum of nine determinations across a minimum of three concentration levels covering the specified range of the procedure (e.g., 80%, 100%, and 120% of the target concentration, with three replicates each) [2].
- Alternatively, for an assay of the drug product, a minimum of six determinations at 100% of the test concentration may be sufficient [2].
- All measurements must be performed by the same analyst, using the same instrument, same batch of reagents, and within a short time frame (e.g., one day or one analytical run) [30] [31].
- Data Analysis:
- Calculate the mean, standard deviation (SD), and relative standard deviation (%RSD), also known as the coefficient of variation, for the results at each concentration level and for the overall data set [2].
- The %RSD is calculated as: (Standard Deviation / Mean) × 100.
- Acceptance Criteria: The calculated %RSD should be within pre-defined limits, which are based on the intended use of the method and industry standards. A lower %RSD indicates higher repeatability.
Protocol for Intermediate Precision
Intermediate precision builds upon repeatability by introducing realistic laboratory variations.
- Purpose: To quantify the method's robustness to normal, within-laboratory variations that occur over an extended period [30].
- Experimental Design:
- The study should incorporate deliberate changes in factors such as:
- An experimental design (e.g., a factorial design) can be employed to efficiently evaluate the effect of these individual variables [32] [2].
- A typical approach involves two analysts independently preparing and analyzing replicate sample preparations (e.g., six at 100% concentration), each using their own standards, solutions, and a different HPLC system [2].
- Data Analysis:
- Calculate the mean, SD, and %RSD for the combined data set from all the varied conditions.
- The results from different analysts can be compared using statistical tests, such as a Student's t-test, to determine if there is a statistically significant difference in the mean values obtained by each analyst [2].
- Acceptance Criteria: The overall %RSD for the intermediate precision study should meet pre-defined criteria and will generally be larger than the %RSD observed for repeatability. The difference between the means obtained by different analysts should also be within acceptable limits.
Protocol for Reproducibility
Reproducibility is the most stringent level of precision testing and is typically conducted during method transfer or collaborative studies.
- Purpose: To demonstrate that the method yields consistent results when deployed across multiple, independent laboratories [30] [2].
- Experimental Design:
- A collaborative study is conducted involving a minimum of two or more laboratories.
- Each laboratory follows the same, written analytical procedure.
- Each lab analyzes the same set of homogeneous samples (typically a minimum of ten parts, with two to three repeat measurements per part)[ccitation:8].
- The participating laboratories use their own analysts, equipment, and reagent batches.
- Data Analysis:
- The data from all laboratories are combined and analyzed using statistical methods, such as Analysis of Variance (ANOVA), to separate and quantify the different sources of variation (e.g., within-lab variation and between-lab variation).
- The overall mean, SD, and %RSD are calculated for the collaborative study [2].
- Acceptance Criteria: The %RSD from the reproducibility study should be within an acceptable, pre-defined range. Successful demonstration of reproducibility indicates that the method is robust and suitable for use in multiple locations.
The following workflow diagram maps the key steps involved in designing and executing a comprehensive precision study, from planning to final analysis.
Data Presentation and Acceptance Criteria
Clear presentation of data and adherence to pre-defined acceptance criteria are essential for demonstrating the precision of an analytical method. The following table summarizes the key characteristics and typical acceptance criteria for the three levels of precision. It is important to note that specific acceptance criteria must be defined based on the method's intended use and relevant regulatory guidelines.
Table 1: Summary of Precision Measurements and Typical Acceptance Criteria
| Precision Level | Experimental Conditions | Key Sources of Variation | Typical Acceptance Criteria* (%RSD) | Statistical Outputs |
|---|---|---|---|---|
| Repeatability | Same analyst, instrument, and day [30] [31] | Sample preparation, instrument noise [31] | Varies by analyte concentration; often ≤ 1% for assay [2] | Mean, Standard Deviation (SD), %RSD [2] |
| Intermediate Precision | Different analysts, instruments, and days within one lab [30] [2] | Analyst technique, instrument performance, reagent lots [30] | Slightly higher than repeatability but within pre-set limits [2] | Overall Mean, SD, %RSD; Student's t-test for analyst comparison [2] |
| Reproducibility | Different laboratories [30] [2] | Laboratory environment, equipment calibration, training [30] | Defined by collaborative study; higher than intermediate precision [2] | Overall Mean, SD, %RSD from collaborative study; ANOVA [2] |
Note: Specific acceptance criteria are established during method development based on the analyte and application, and are defined prior to the validation study.
Gauge Repeatability and Reproducibility (GR&R) Studies
In industrial settings, a Gauge Repeatability and Reproducibility (GR&R) study is a systematic statistical method used to evaluate a measurement system [31]. It partitions the total measurement variation into components attributable to:
- Repeatability: Variation from the measurement device itself.
- Reproducibility: Variation arising from different operators.
- Part-to-Part: The actual variation between the parts or samples being measured.
A typical GR&R study involves multiple operators (e.g., two or three) measuring the same set of parts (e.g., ten parts) multiple times (e.g., two or three repetitions) each [31]. The results are interpreted as follows:
- %GR&R < 10%: The measurement system is considered acceptable.
- 10% < %GR&R < 30%: The measurement system may be acceptable based on the application and associated cost of misclassification.
- %GR&R > 30%: The measurement system is considered unacceptable and requires improvement [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
The execution of a robust precision study requires high-quality, consistent materials and reagents. The following table details essential items and their functions in the context of chromatographic method validation.
Table 2: Key Research Reagent Solutions and Materials for Precision Studies
| Item | Function in Precision Studies |
|---|---|
| Reference Standard | A well-characterized, high-purity substance used to prepare solutions of known concentration for evaluating accuracy, linearity, and precision. Its stability is critical [32]. |
| High-Purity Reagents & Solvents | Used for mobile phase and sample preparation. Consistent quality and lot-to-lot reproducibility are vital for minimizing baseline noise and variability in retention times [32]. |
| Chromatographic Column | The stationary phase used for separation. Using columns from different lots or manufacturers is a key factor in intermediate precision testing [30] [32]. |
| Calibrants | Solutions used to calibrate the instrument. Different batches of calibrants can be a source of variation and should be included in intermediate precision studies [30]. |
| System Suitability Standards | A reference preparation used to verify that the chromatographic system is adequate for the intended analysis before the precision study is run. Parameters like plate count and tailing factor are checked [2]. |
Precision, encompassing repeatability, intermediate precision, and reproducibility, is a cornerstone of analytical method validation. A structured approach to measuring these three tiers of variability provides a comprehensive understanding of a method's performance, from its best-case scenario under ideal conditions to its real-world applicability across different laboratories. By employing rigorous experimental designs, such as those outlined in this guide, and utilizing high-quality reagents, scientists and drug development professionals can generate reliable, high-integrity data. This not only ensures regulatory compliance but also underpins product quality and patient safety throughout the drug development lifecycle. A well-validated, precise method is an indispensable tool for making critical decisions in pharmaceutical research and development.
Analytical method validation is a critical process in pharmaceutical development and other regulated industries, ensuring that analytical procedures are accurate, precise, and reliable for their intended purpose [33]. Within this framework, specificity and selectivity are fundamental validation parameters that establish a method's ability to accurately measure the analyte of interest without interference from other components [34]. These parameters underpin the entire validity of analytical results, ensuring that what is being measured is indeed the target substance, which is crucial for making informed decisions about drug safety, efficacy, and quality. As the industry evolves with novel modalities and advanced technologies, the principles of specificity and selectivity remain the bedrock of reliable analytics, directly supporting Quality-by-Design (QbD) and robust lifecycle management of analytical procedures [35].
Defining Specificity and Selectivity
While often used interchangeably, specificity and selectivity have distinct technical definitions in analytical chemistry. According to the ICH Q2(R1) guideline, specificity is "the ability to assess unequivocally the analyte in the presence of components which may be expected to be present" in the sample matrix, such as impurities, degradation products, or excipients [34]. It focuses on demonstrating that the method can accurately identify and quantify the target analyte despite these potential interferents.
Selectivity, while not explicitly defined in ICH Q2(R1), is addressed in other guidelines like the European bioanalytical method validation guideline and is considered by IUPAC to be the preferred term in analytical chemistry [34]. It describes the ability of the method to differentiate and quantify multiple analytes within a mixture, requiring the identification of all relevant components rather than just the primary analyte of interest [34] [33].
A helpful analogy is to consider a bunch of keys: specificity requires identifying only the one key that opens a particular lock, while selectivity requires identifying all keys in the bunch [34]. The table below summarizes the key differences between these two parameters.
Table 1: Comparative Analysis of Specificity and Selectivity
| Feature | Specificity | Selectivity |
|---|---|---|
| Definition | Ability to assess the analyte unequivocally in the presence of potential interferents [34] | Ability to differentiate and quantify multiple analytes in a mixture [34] [33] |
| Scope | Focuses on one primary analyte [34] | Encompasses multiple analytes or components [34] |
| Regulatory Mention | Explicitly defined in ICH Q2(R1) [34] | Not explicitly mentioned in ICH Q2(R1), but used in other guidelines [34] |
| Analogy | Finding the one correct key in a bunch that opens a specific lock [34] | Identifying all keys in the bunch [34] |
| Key Question | Is the method free from interference for the target analyte? | Can the method distinguish and measure all relevant analytes? |
For chromatographic techniques, specificity/selectivity is typically demonstrated by showing that the chromatographic peaks are well-resolved, particularly for "critical separations" where the resolution of the two closest-eluting components is crucial [34].
Experimental Protocols for Demonstration
Establishing Specificity
Demonstrating specificity involves experiments designed to show that the method is unaffected by the presence of other components likely to be present in the sample. Two primary approaches are used [34]:
- Analysis of the analyte spiked into a mixture of structurally similar compounds: This positive approach confirms the method can detect the target amid potential interferents.
- Analysis of a mixture of structurally similar molecules without the analyte: This negative approach, often referred to as checking for "matrix interference," verifies that the sample matrix itself does not produce a signal that could be mistaken for the analyte or that it does not cause enhancing or quenching effects [34].
A critical application of specificity testing is in forced degradation studies (also known as stress testing). Samples of the drug substance or product are subjected to various stress conditions (e.g., heat, light, acid, base, oxidation), and the method's ability to separate the main analyte from its degradation products is evaluated [34]. This proves that the method is stability-indicating.
Establishing Selectivity
The methodology for selectivity involves challenging the analytical method with samples containing all target analytes and potential interferents to confirm that each component can be distinguished and measured accurately [33]. The experimental protocol should be designed to identify and resolve all expected components in the mixture. For chromatographic methods, this is demonstrated by a clear baseline resolution between the peaks of interest [34]. The experimental workflow for determining both parameters is outlined in the diagram below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimental execution for specificity and selectivity requires carefully selected reagents and materials. The following table details key components of the research toolkit.
Table 2: Essential Research Reagents and Materials for Specificity and Selectivity Studies
| Item | Function & Application |
|---|---|
| Matrix Blank | The sample matrix without the analyte present. Used to assess background signal and confirm the absence of interfering components from the matrix itself [33]. |
| Spiked Solutions | Solutions with a known concentration of the target analyte(s) added. Used to calculate analyte recovery and confirm the method's accuracy and response in the presence of the sample matrix [33]. |
| Forced Degradation Samples | Samples subjected to stress conditions (e.g., acidic, basic, oxidative, thermal, photolytic). Critical for demonstrating the method's specificity by proving it can separate the analyte from its degradation products [34]. |
| Reference Standards | Highly characterized materials with known purity and identity. Used to confirm the identity of peaks in the chromatogram and to quantify analytes, ensuring the method is measuring the correct substance [33]. |
| System Suitability Test (SST) Solutions | Mixtures containing critical analytes to test the resolution and reproducibility of the chromatographic system before and during analysis. Ensures the system is performing adequately for the intended separation [33]. |
Regulatory Context and Future Trends
Specificity is a mandatory validation parameter required for all quality control methods in a GMP environment, including identification tests, impurity tests, and assays [34]. The regulatory landscape is defined by the ICH Q2(R1) guideline and is evolving with forthcoming updates (ICH Q2(R2) and ICH Q14) that emphasize a more integrated, lifecycle approach to analytical procedures [35]. These trends encourage a deeper scientific understanding of the method, which is intrinsically linked to robust demonstrations of specificity and selectivity.
Modern technological advancements are enhancing the ability to establish these parameters. The adoption of Multi-Attribute Methods (MAM) for biologics, which consolidate the measurement of multiple quality attributes into a single assay, relies heavily on high selectivity [35]. Furthermore, hyphenated techniques like LC-MS/MS provide unparalleled selectivity by combining chromatographic separation with mass-based detection [35]. The application of Artificial Intelligence (AI) and machine learning is also emerging to optimize method parameters and improve the interpretation of complex data, further strengthening the reliability of specificity and selectivity assessments [35].
Specificity and selectivity are foundational pillars of a validated analytical method. While specificity ensures that a method is unequivocally measuring the target analyte in a complex mixture, selectivity expands this capability to precisely distinguish and quantify multiple analytes. A scientifically rigorous demonstration of these parameters, through well-designed experiments such as forced degradation studies and resolution testing, is non-negotiable for ensuring drug product quality, safety, and efficacy. As the pharmaceutical industry advances with increasingly complex modalities and embraces modern paradigms like QbD and Real-Time Release Testing (RTRT), the principles of specificity and selectivity will continue to be paramount, underpinned by advanced technologies and a proactive, lifecycle-oriented regulatory framework.
In the rigorous framework of analytical method validation, which is a cornerstone of pharmaceutical research and drug development, linearity and range are two fundamental parameters that establish the quantitative capabilities of an analytical procedure. They are not isolated concepts but are intrinsically linked, working in tandem to define the boundaries within which an analytical method can produce results directly proportional to the concentration of the analyte.
For researchers, scientists, and drug development professionals, demonstrating linearity and defining a suitable range is imperative for regulatory submissions to bodies like the FDA and EMA, which adhere to ICH guidelines [36] [4]. These parameters are critical for ensuring that methods accurately measure the Active Pharmaceutical Ingredient (API), impurities, and other components throughout the drug lifecycle, thereby guaranteeing product quality, safety, and efficacy [36].
Core Concepts and Definitions
Linearity
Linearity is the ability of an analytical method to elicit test results that are directly, or by a well-defined mathematical transformation, proportional to the concentration of analyte in samples within a given range [4]. It is a measure of the method's ability to obtain a straight-line response when the results are plotted against the analyte concentration.
Range
The range of an analytical method is the interval between the upper and lower concentrations (including these concentrations) of an analyte for which it has been demonstrated that the analytical procedure has a suitable level of precision, accuracy, and linearity [37]. It defines the quantitative boundaries within which the method is considered valid.
The Interrelationship
The relationship between linearity and range is symbiotic. Linearity is experimentally demonstrated across a specified range. Conversely, the validated range is the interval over which acceptable linearity, as well as accuracy and precision, has been proven. The following workflow illustrates the typical process for establishing and validating these parameters:
Regulatory Expectations and Acceptance Criteria
Analytical method validation must comply with established international guidelines. The International Council for Harmonisation (ICH) guideline Q2(R1) is the primary global standard, with a revised version (ICH Q2(R2)) currently under finalization [4]. The U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) align with these ICH guidelines [36] [4].
Regulatory authorities require that the validation parameters, including linearity and range, are based on the method's intended use. The table below summarizes the typical acceptance criteria for linearity and the corresponding range requirements for different types of analytical tests [4]:
Table 1: Typical Acceptance Criteria for Linearity and Range Based on ICH Guidelines
| Test Type | Linearity Acceptance (Correlation Coefficient R²) | Typical Range Specification |
|---|---|---|
| Assay of API | Usually ≥ 0.999 | 80% to 120% of the target concentration |
| Impurity Testing (Quantitative) | Usually ≥ 0.999 | From reporting threshold to 120% of specification |
| Impurity Testing (Limit Test) | Not typically required | Specified level ± 20% |
| Content Uniformity | Usually ≥ 0.999 | 70% to 130% of the target concentration |
| Dissolution Testing | Usually ≥ 0.999 | 20% below to 20% above the expected range |
Experimental Protocol for Establishing Linearity and Range
Establishing linearity and range is a multi-step process that requires careful planning and execution. The following provides a detailed methodology.
Materials and Reagents
The following materials are essential for conducting linearity and range experiments [37]:
Table 2: Essential Research Reagent Solutions for Linearity and Range Experiments
| Item | Function & Importance |
|---|---|
| Certified Reference Standard | High-purity analyte used to prepare known concentrations; critical for accuracy. |
| Appropriate Solvent | To dissolve the reference standard and sample matrix; must be compatible with the method. |
| Mobile Phase Components | For chromatographic methods (HPLC/GC); precise composition is key for consistent response. |
| System Suitability Standards | Used to verify the analytical system's performance is adequate before the linearity study. |
Step-by-Step Procedure
Step 1: Define the Target Range Based on the method's purpose (e.g., assay, impurity testing), define the expected range of analyte concentrations. This will determine the concentrations for the linearity study [37].
Step 2: Prepare Standard Solutions Prepare a minimum of five to six concentration levels across the target range. For an assay method ranging from 80% to 120%, appropriate levels might be 80%, 90%, 100%, 110%, and 120% of the target concentration [4]. Prepare each level in replicate, typically in triplicate.
Step 3: Analyze Solutions Analyze the standard solutions using the optimized analytical procedure (e.g., HPLC, UV-Vis). The analysis should be performed in a randomized sequence to minimize the effect of instrumental drift [4].
Step 4: Data Collection Record the analytical response (e.g., peak area in HPLC, absorbance in UV-Vis) for each injection.
Step 5: Data Analysis and Calculation
- Plot the Data: Create a scatter plot with concentration on the x-axis and the analytical response on the y-axis.
- Linear Regression: Apply a least-squares linear regression to the data to calculate the best-fit line:
y = mx + c, wheremis the slope andcis the y-intercept. - Calculate Correlation Coefficient (R²): Determine the R² value, which indicates the proportion of the variance in the response that is predictable from the concentration.
- Evaluate Residuals: Examine the residuals (the difference between the observed response and the response predicted by the regression line). They should be randomly distributed.
Step 6: Assess Acceptance Criteria The method demonstrates acceptable linearity if the R² value meets the pre-defined criterion (e.g., ≥ 0.999 for an assay) and the residual plot shows no obvious pattern [4]. The range is considered validated if the linearity, accuracy, and precision are all acceptable across the entire span.
The logical decision process for evaluating the results of a linearity study is summarized below:
Troubleshooting and Common Challenges
Even with careful planning, issues can arise during linearity and range studies.
- Poor Correlation Coefficient (Low R²): This can be caused by an improperly calibrated instrument, an impure reference standard, or an incorrect detector setting. Re-evaluate the method conditions and standard quality [4].
- Non-Linear Response: If the data consistently deviates from a straight line, the analytical range may be too wide, or the detector may be saturated at higher concentrations. The range should be narrowed, or a non-linear regression model may be considered if scientifically justified.
- Significant Y-Intercept: A large positive or negative y-intercept may indicate interference in the method or an issue with the sample preparation procedure. The method's specificity should be investigated [4].
Within the comprehensive thesis of analytical method validation research, establishing linearity and a defined range is not merely a regulatory checkbox. It is a fundamental scientific exercise that defines the quantitative heart of an analytical procedure. By rigorously demonstrating that a method provides a proportional and reliable response across a specified interval, researchers and drug development professionals ensure the generation of meaningful data. This, in turn, underpins critical decisions regarding drug quality, stability, and safety, ultimately contributing to the successful development of safe and effective pharmaceutical products for patients.
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
In the comprehensive framework of analytical method validation research, establishing the lowest levels at which an analyte can be reliably detected and quantified is fundamental to ensuring data credibility. The Limit of Detection (LOD) and Limit of Quantitation (LOQ) are two critical performance characteristics that define the sensitivity and utility of an analytical procedure [38] [39]. These parameters ensure that methods are "fit for purpose," providing researchers and drug development professionals with confidence in results generated at low analyte concentrations [38]. Within clinical, pharmaceutical, and bioanalytical contexts, proper determination of LOD and LOQ is not merely a regulatory formality but a scientific necessity that underpins the reliability of experimental data and subsequent decision-making [40] [39].
The terminology surrounding detection and quantification capabilities has evolved, with the outdated terms of "analytical and functional sensitivity" now being superseded by the more precise definitions of LOD and LOQ [41]. Understanding these concepts allows scientists to fully characterize the analytical performance of laboratory tests, comprehend their capabilities and limitations, and establish the effective dynamic range of an assay [38]. This guide provides an in-depth examination of the theoretical foundations, calculation methodologies, and practical applications of LOD and LOQ within modern analytical science.
Fundamental Concepts and Definitions
Limit of Blank (LoB)
The Limit of Blank (LoB) represents the highest apparent analyte concentration expected to be found when replicates of a blank sample containing no analyte are tested [38] [42]. Conceptually, LoB describes the background noise of the analytical system and establishes the threshold above which a signal can be considered potentially meaningful. LoB is calculated statistically by measuring multiple replicates of a blank sample and applying the formula:
LoB = mean~blank~ + 1.645(SD~blank~) [38]
This calculation assumes a Gaussian distribution of the raw analytical signals from blank samples, with the LoB representing the value that 95% of blank measurements would not exceed (one-sided confidence interval) [38]. The remaining 5% of blank values may produce responses that could be misinterpreted as containing analyte, representing statistically a Type I error (false positive) [38].
Limit of Detection (LOD)
The Limit of Detection (LOD) is defined as the lowest analyte concentration that can be reliably distinguished from the LoB and at which detection is feasible [38] [42]. Unlike LoB, which deals specifically with blank samples, LOD requires testing samples containing low concentrations of analyte to empirically demonstrate detection capability. The CLSI EP17 guideline defines LOD using both the measured LoB and test replicates of a sample containing low analyte concentration:
LOD = LoB + 1.645(SD~low concentration sample~) [38]
At this concentration, approximately 95% of measurements will exceed the LoB, with no more than 5% of values falling below the LoB (representing Type II error or false negative) [38]. A traditional but less rigorous approach estimates LOD simply as the mean blank value plus 2-3 standard deviations, though this method has been criticized as it "defines only the ability to measure nothing" without proving that low analyte concentrations can be distinguished from blanks [38].
Limit of Quantitation (LOQ)
The Limit of Quantitation (LOQ) represents the lowest concentration at which the analyte can not only be reliably detected but also quantified with established precision and accuracy under specified experimental conditions [38] [41]. The LOQ may be equivalent to the LOD or exist at a much higher concentration, but it cannot be lower than the LOD [38]. LOQ is determined by meeting predefined goals for bias and imprecision, often defined as the concentration that yields a coefficient of variation (CV) of 20% or less, sometimes referred to as "functional sensitivity" [38] [42]. If analytical goals for total error are met at the LOD, then LOQ may equal LOD; if not, higher concentrations must be tested until the requirements for precision and bias are satisfied [38].
Table 1: Comparative Overview of LoB, LOD, and LOQ
| Parameter | Definition | Sample Type | Key Characteristics |
|---|---|---|---|
| LoB | Highest apparent analyte concentration expected when testing a blank sample [38] | Sample containing no analyte [38] | Describes background noise; 95% of blank values fall below this level [38] |
| LOD | Lowest analyte concentration reliably distinguished from LoB [38] | Sample with low concentration of analyte [38] | Detection is feasible but not necessarily with precise quantification [38] |
| LOQ | Lowest concentration where quantification meets predefined precision and accuracy goals [41] | Sample with concentration at or above LOD [38] | Both reliable detection and acceptable quantification are achieved [38] |
Methodological Approaches for Determination
Standard Deviation of the Blank and Signal-to-Noise Ratio
For methods exhibiting background noise, the standard deviation of blank measurements provides a foundation for determining detection and quantification limits. This approach typically employs the formulas:
LOD = mean~blank~ + 3.3 × SD~blank~ [43]
LOQ = mean~blank~ + 10 × SD~blank~ [43]
The multipliers 3.3 and 10 correspond to confidence levels of approximately 95% and 99.95%, respectively, for detecting and quantifying the analyte [43]. Similarly, the signal-to-noise ratio method directly compares the analytical signal from a low concentration sample to the background noise, typically requiring ratios of 3:1 for LOD and 10:1 for LOQ [41]. This approach is particularly common in chromatographic methods such as HPLC, where baseline noise is readily measurable [41] [44].
Calibration Curve Approach
The International Conference on Harmonisation (ICH) Q2(R1) guideline describes an approach utilizing the standard deviation of response and the slope of the calibration curve [44]. This method is particularly suitable for instrumental techniques without significant background noise and involves the calculations:
Where σ represents the standard deviation of the response and S is the slope of the calibration curve [44]. The standard deviation (σ) can be estimated as the standard error of the regression line or the residual standard deviation of the regression line obtained from samples containing the analyte in the range of the expected LOD/LOQ [41] [44]. The slope serves to convert the variation in the instrumental response back to the concentration domain [43].
Visual Evaluation and Empirical Approaches
For non-instrumental methods or those with subjective endpoints, visual evaluation provides a practical determination approach [41]. This method involves analyzing samples with known concentrations of analyte and establishing the minimum level at which the analyte can be reliably detected or quantified [41]. For detection limits, samples at various low concentrations are tested, with each result recorded simply as "detected" or "not detected" [43]. Logistic regression analysis of these binary outcomes across concentrations allows estimation of the LOD as the concentration with 99% probability of detection, and LOQ at 99.95% probability [43]. This approach is valuable for methods such as microbial inhibition assays or visual titration endpoints [41].
Table 2: Comparison of LOD and LOQ Determination Methods
| Method | Basis | Typical Applications | Advantages | Limitations |
|---|---|---|---|---|
| Standard Deviation of Blank [43] | Statistical distribution of blank measurements | Methods with measurable background noise | Simple calculations; Direct measurement of system noise | Does not confirm detection of actual analyte [38] |
| Signal-to-Noise Ratio [41] | Direct comparison of analyte signal to background | Chromatographic methods (HPLC) [41] | Intuitively understandable; Instrument-independent | Requires defined baseline noise; Subjective measurement |
| Calibration Curve [44] | Standard error of regression and slope | Quantitative instrumental methods | Statistically rigorous; Uses actual analyte response [44] | Requires samples at low concentrations; Dependent on curve quality |
| Visual Evaluation [41] | Binary detection at known concentrations | Non-instrumental methods, titration | Practical for qualitative methods; Empirical confirmation | Subjective; Requires multiple concentrations and replicates |
Experimental Protocols and Validation
Sample Preparation and Experimental Design
Robust determination of LOD and LOQ requires careful experimental design. For manufacturer-established parameters, testing approximately 60 replicates of both blank and low concentration samples is recommended, while for verification studies, 20 replicates typically suffice [38]. Samples should be prepared in a matrix commutable with actual patient or test specimens to ensure relevance [38]. The low concentration samples are typically prepared as dilutions of the lowest non-negative calibrator or by spiking the matrix with a known amount of analyte [38]. When designing experiments, factors including number of kit lots, operators, instruments, and days (to capture inter-assay variability) should be considered to ensure the determined limits reflect realistic performance under typical laboratory conditions [42].
Calculation and Verification Procedures
Following data collection, LOD and LOQ are calculated using the appropriate statistical methods for the chosen approach. For the calibration curve method, linear regression analysis provides both the slope (S) and standard error (σ), which are directly applied in the LOD and LOQ formulas [44]. However, these calculated values represent only estimates and must be experimentally verified [44]. Validation involves preparing and analyzing multiple replicates (typically n=6) at the estimated LOD and LOQ concentrations [44]. For LOD verification, the analyte should be detectable in approximately 95% of measurements [38]. For LOQ, the results must demonstrate acceptable precision and accuracy, typically with a CV ≤20% and bias within established acceptability limits [38] [42]. If these criteria are not met, the estimates must be adjusted and the verification repeated at appropriately modified concentrations.
Advanced Approaches: Uncertainty and Accuracy Profiles
Recent research has introduced more sophisticated graphical approaches for determining detection and quantification limits, particularly the uncertainty profile and accuracy profile methods [40]. These techniques utilize tolerance intervals and measurement uncertainty to provide a comprehensive assessment of method validity across concentrations [40]. The uncertainty profile combines uncertainty intervals with acceptability limits in a single graphical representation, where the intersection at low concentrations between acceptability limits and uncertainty intervals defines the LOQ [40]. Comparative studies have demonstrated that these graphical approaches provide more realistic assessments of quantification capabilities compared to classical statistical methods, which tend to underestimate LOD and LOQ values [40]. These advanced methods simultaneously examine method validity and estimate measurement uncertainty, offering a more holistic approach to method validation [40].
The following workflow diagram illustrates the logical relationship between different determination approaches and key decision points in establishing LOD and LOQ:
Diagram 1: LOD and LOQ Determination Workflow
Essential Research Reagent Solutions
Successful determination of LOD and LOQ requires appropriate materials and reagents tailored to the analytical method. The following table outlines key solutions and their functions in detection and quantification studies:
Table 3: Essential Research Reagents for LOD/LOQ Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Blank Matrix [38] | Mimics sample matrix without analyte; establishes baseline signal | Must be commutable with actual test specimens; defines LoB [38] |
| Low Concentration Calibrators [38] | Provides known low analyte concentrations for empirical testing | Prepared by diluting stock solutions or spiking matrix; defines LOD [38] |
| Internal Standards [40] | Corrects for analytical variability in complex matrices | Essential for bioanalytical methods (e.g., HPLC-MS); improves precision [40] |
| Quality Control Materials [44] | Verifies method performance during validation | Prepared at LOD and LOQ concentrations; used in verification studies [44] |
| Matrix Modifiers | Compensates for matrix effects in complex samples | Reduces interference in biological samples; improves accuracy |
Regulatory Context and Recent Advances
Guidelines and Compliance Requirements
Determination of LOD and LOQ is mandated by major regulatory guidelines globally, including the ICH Q2(R2) guideline for pharmaceutical analysis and CLSI EP17 for clinical laboratory methods [42] [39]. These guidelines provide frameworks for validation but allow flexibility in the specific methodological approaches [40]. Regulatory authorities emphasize that analytical methods must be "fit for purpose," with detection and quantification limits appropriate to the intended application [38] [39]. For pharmaceutical quality control, validated methods are required under regulations such as 21 CFR 211 for OTC drug products, with the FDA increasingly focusing on method validation during audits [39].
Emerging Trends and Research Directions
Current research in detection and quantification capabilities focuses on improving the statistical rigor and practical relevance of determination methods. Comparative studies have demonstrated that classical statistical approaches often yield underestimated LOD and LOQ values, while graphical methods such as uncertainty profiles provide more realistic assessments [40]. The uncertainty profile approach, based on tolerance intervals and measurement uncertainty, represents a significant advancement as it simultaneously validates the analytical procedure and estimates measurement uncertainty [40]. Future directions include improved integration of detection capability assessment with measurement uncertainty principles and the development of standardized approaches for emerging technologies such as digital PCR and single-molecule arrays [45] [42].
Proper determination of Limit of Detection and Limit of Quantitation is a fundamental requirement in analytical method validation, providing essential information about the sensitivity and low-end performance of analytical procedures. The multiple available approaches—including blank standard deviation, signal-to-noise ratio, calibration curve, and visual evaluation methods—each offer distinct advantages for different analytical contexts. Recent advances in graphical methods such as uncertainty profiles provide more realistic assessments of quantification capability compared to classical statistical approaches. Through appropriate experimental design, rigorous calculation, and thorough verification, researchers can establish reliable detection and quantification limits that ensure analytical methods are truly fit for their intended purpose in pharmaceutical development, clinical diagnostics, and bioanalytical research.
Within the comprehensive framework of analytical method validation research, the demonstration that an analytical procedure is fit-for-purpose is paramount [46]. This validation process involves assessing a defined set of performance characteristics to ensure the method consistently produces reliable results that can be trusted for decision-making [22] [46]. While characteristics like accuracy and precision confirm a method's performance under ideal conditions, this guide focuses on two parameters that evaluate its reliability under real-world, variable conditions: robustness and ruggedness.
These parameters test the method's resilience, ensuring that minor, inevitable fluctuations in procedure or environment do not compromise the integrity of the analytical results. For researchers and drug development professionals, understanding and assessing robustness and ruggedness is critical for developing reliable methods that successfully transfer from research and development to quality control laboratories and, ultimately, support regulatory submissions [47] [22].
Defining Robustness and Ruggedness
Although sometimes used interchangeably, a clear distinction exists between robustness and ruggedness based on the source of variation.
Robustness is defined as a measure of an analytical procedure's capacity to remain unaffected by small, but deliberate variations in method parameters and provides an indication of its reliability during normal usage [47] [48] [49]. It is an intra-laboratory study that focuses on internal factors specified within the method protocol, such as mobile phase pH or column temperature [50] [51].
Ruggedness refers to the degree of reproducibility of test results obtained by the analysis of the same samples under a variety of normal test conditions, such as different laboratories, analysts, or instruments [48] [49]. It assesses the method's performance against external, environmental factors that are not specified in the method procedure [50] [51].
The following table summarizes the key differences:
Table 1: Core Differences Between Robustness and Ruggedness
| Feature | Robustness Testing | Ruggedness Testing |
|---|---|---|
| Purpose | To evaluate performance under small, deliberate variations in method parameters [49]. | To evaluate reproducibility under real-world, environmental variations [49]. |
| Scope & Variations | Intra-laboratory; small, controlled changes to internal parameters (e.g., pH, flow rate) [49] [50]. | Inter-laboratory; broader factors (e.g., different analysts, instruments, days) [48] [49]. |
| Typical Timing | During method development or at the beginning of validation [47] [48]. | Later in validation, often before method transfer [49]. |
| Key Question | "How well does the method withstand minor tweaks to its defined parameters?" | "How well does the method perform in different settings or by different people?" |
The Regulatory and Harmonized Context
From a regulatory perspective, robustness is recognized by both the International Council for Harmonisation (ICH) and the U.S. Pharmacopeia (USP) [48]. The ICH guideline Q2(R2) on the validation of analytical procedures includes robustness as a key characteristic [22] [9]. While not strictly required, its evaluation is highly recommended as it directly informs system suitability tests (SSTs), which are mandatory to ensure the validity of the analytical procedure is maintained whenever used [47] [22].
The term "ruggedness" is used by the USP but is falling out of favor in the international harmonized guidelines. The ICH addresses the same concept under the validation parameters of intermediate precision (within-laboratory variations) and reproducibility (between-laboratory variations from collaborative studies) [48].
Designing a Robustness Study: Methodologies and Protocols
A robustness test is an experimental set-up to evaluate the effect of individual method parameters on the method's responses [47]. The following sections provide a detailed protocol for conducting such a study.
Step 1: Identification of Factors and Responses
The first step is to select the factors to investigate and the responses to measure.
- Selecting Factors: Factors are selected from the written analytical procedure. For a chromatographic method, this typically includes variables such as mobile phase pH, mobile phase composition, flow rate, column temperature, and different columns (lots/suppliers) [47] [50]. Both operational and environmental factors can be considered.
- Defining Responses: The responses are the measurable outputs that indicate the method's performance. These include quantitative results (e.g., assay content, impurity level) and system suitability parameters (e.g., resolution, tailing factor, capacity factor) [47].
Step 2: Defining Ranges and Experimental Design
Once factors are identified, the high and low levels for each factor must be set. These variations should be small but deliberate, slightly exceeding the variations expected during routine use (e.g., pH ± 0.1 units, flow rate ± 0.1 mL/min) [47] [49]. The selection of an experimental design is critical for efficiency.
A univariate approach (changing one factor at a time) is inefficient and fails to detect interactions between factors. Multivariate screening designs are the preferred methodology as they allow for the simultaneous study of multiple variables [48]. The choice of design depends on the number of factors.
Table 2: Common Experimental Designs for Robustness Testing
| Design Type | Description | Best Use Case |
|---|---|---|
| Full Factorial | Examines all possible combinations of all factors at their high and low levels. For k factors, this requires 2k runs [48]. | A small number of factors (e.g., ≤4). Provides full information on main effects and interactions. |
| Fractional Factorial | A carefully selected subset (a fraction) of the full factorial combinations. Significantly reduces the number of runs [47] [48]. | A larger number of factors (e.g., 5-8). Efficient, but some interactions may be confounded with main effects. |
| Plackett-Burman | A highly efficient screening design where the number of runs is a multiple of 4 (e.g., 12 runs for up to 11 factors). Only main effects are calculated [47] [48]. | Screening a large number of factors to quickly identify the most influential ones. Ideal for robustness testing. |
The workflow for planning and executing a robustness study, from defining its purpose to drawing conclusions, is summarized in the following diagram:
Step 3: Execution, Data Analysis, and Interpretation
Experiments should be performed in a random sequence to avoid systematic bias from instrument drift or other time-related factors [47]. Using aliquots from the same homogeneous sample and standard preparations is crucial for accurate comparison.
Calculation of Effects: For each factor, the effect is calculated as the difference between the average response when the factor is at its high level and the average response when it is at its low level [47]. The formula is:
Effect (Eₓ) = [ΣY(+)/N] - [ΣY(-)/N]where ΣY(+) is the sum of responses at the high level, ΣY(-) is the sum of responses at the low level, and N is the number of experiments at each level [47].Interpretation: The calculated effects are then interpreted. Effects can be analyzed graphically (e.g., using normal probability plots) or statistically (e.g., using t-tests or by comparing the effect to a critical value) [47]. A factor with a statistically significant effect is considered influential. The practical relevance of this effect must be assessed—does it meaningfully impact the quantitative result or critical system suitability parameters?
The Scientist's Toolkit: Essential Reagents and Materials
Robustness testing requires careful preparation and the use of specific, well-characterized materials. The following table lists key items and their functions in the context of a chromatographic robustness study.
Table 3: Key Research Reagent Solutions and Materials for Robustness Testing
| Item | Function in Robustness Testing |
|---|---|
| Reference Standard | A highly purified and characterized substance used to prepare the known concentration samples for accuracy and linearity assessments. Serves as the benchmark for all measurements [52]. |
| Mobile Phase Buffers | Solutions of specific pH and composition. Different batches or slight variations in preparation are used to test the method's sensitivity to mobile phase conditions [50]. |
| Chromatographic Columns | Columns from different manufacturing lots or different suppliers are used to evaluate the method's performance against this critical and highly variable component [48] [50]. |
| Spiked Sample Solutions | Samples prepared by adding a known amount of analyte to the sample matrix. Used to assess accuracy and detectivity under varied method conditions [52]. |
| System Suitability Test (SST) Solutions | A specific mixture containing the analyte and its critical separations (e.g., impurities) used to verify that the chromatographic system is adequate for the analysis before or during the robustness test [47]. |
Establishing a Control Strategy: From Robustness to System Suitability
The ultimate goal of a robustness test is not just to identify sensitive factors, but to use this knowledge to establish a control strategy that ensures the method's reliability. The most direct consequence of a robustness evaluation is the establishment of evidence-based System Suitability Test (SST) limits [47] [22].
For example, if a robustness test reveals that resolution between two critical peaks is highly sensitive to mobile phase pH, the validation scientist can use the data from the robustness test to set a scientifically justified minimum resolution limit in the SST. This ensures that whenever the method is used, the system is verified to be capable of providing valid results, even with minor, expected variations in the mobile phase pH [47]. This transforms the robustness study from an academic exercise into a practical tool for ensuring daily method reliability.
Within the critical pathway of analytical method validation, robustness and ruggedness testing are not mere regulatory checkboxes. They are fundamental studies that bridge the gap between idealized method performance and reliable, real-world application. By proactively challenging a method with expected variations—both internal (robustness) and external (ruggedness)—researchers and drug development professionals can build a foundation of confidence. This confidence ensures that analytical methods are not only scientifically sound but also practically viable, transferable, and capable of producing unwavering data integrity throughout the product lifecycle.
System Suitability Testing (SST) serves as the critical bridge between analytical method validation and routine quality control, providing daily verification that a fully validated analytical method performs as intended at the time of analysis. Within the broader thesis of analytical method validation research, SST represents the operational component that ensures the ongoing reliability of analytical data in pharmaceutical development and manufacturing. While analytical method validation provides the foundational evidence that a method is suitable for its intended purpose, and Analytical Instrument Qualification (AIQ) verifies that instruments are operating properly, SST specifically confirms that the validated method is performing correctly on the qualified instrument system on any given day [53] [54]. This distinction is crucial for researchers and drug development professionals who must maintain data integrity and regulatory compliance throughout a method's lifecycle.
Regulatory authorities emphasize that SST is a mandatory, method-specific requirement, not an optional practice. The United States Pharmacopoeia (USP) and European Pharmacopoeia (Ph. Eur.) contain specific chapters mandating SST performance, particularly for chromatographic methods [53]. Furthermore, FDA warning letters have been issued for failures to properly implement and execute SST protocols, underscoring their importance in the regulatory landscape [53]. When an SST fails, the entire analytical run must be discarded, highlighting its gatekeeper function for data quality [53].
Core Principles and Regulatory Foundation
Defining System Suitability Testing
System Suitability Testing comprises a set of verification procedures performed either immediately before or concurrently with analytical sample runs to demonstrate that the complete analytical system—including instrument, reagents, columns, and the analytical method—is functioning adequately for its intended purpose on that specific day [53]. As defined in USP chapter <1058>, SST serves to "verify that the system will perform in accordance with the criteria set forth in the procedure" and that "the system's performance is acceptable at the time of the test" [53]. This real-time performance verification distinguishes SST from periodic instrument qualification and initial method validation, creating a three-tiered quality assurance framework essential for reliable analytical results in pharmaceutical research and development.
Distinction from Related Quality Processes
A critical understanding for researchers is differentiating SST from other quality processes, particularly Analytical Instrument Qualification (AIQ). While both ensure result quality, they serve distinct purposes [53]:
Analytical Instrument Qualification (AIQ) verifies that an instrument operates according to manufacturer specifications across defined operating ranges. It is instrument-focused, performed initially and at regular intervals, and is not method-specific [53] [54].
System Suitability Testing (SST) verifies that a specific analytical method performs as validated when applied to a qualified instrument. It is method-specific, performed with each analytical run, and confirms fitness for purpose at the time of analysis [53].
Regulatory authorities explicitly state that SST does not replace AIQ, nor does AIQ eliminate the need for SST [53]. Both are essential components of a comprehensive quality system in pharmaceutical analysis.
Critical SST Parameters and Acceptance Criteria
Fundamental Chromatographic Parameters
For chromatographic methods, which represent a significant portion of analytical techniques in pharmaceutical development, specific SST parameters have been established with defined acceptance criteria. These parameters collectively assess the quality of separation, detection, and quantification.
Table 1: Key SST Parameters for Chromatographic Methods
| Parameter | Description | Typical Acceptance Criteria | Scientific Purpose |
|---|---|---|---|
| Precision/Injection Repeatability | Measure of system performance via replicate injections | RSD ≤2.0% for 5 replicates (USP); stricter limits for Ph. Eur. based on specification limits [53] | Demonstrates system stability under defined conditions |
| Resolution (Rs) | Degree of separation between two adjacent peaks | Sufficient to baseline separate compounds of interest; typically >1.5 [53] | Ensures accurate quantitation of individual components |
| Tailing Factor (Tf) | Measure of peak symmetry | Typically ≤2.0 [53] | Confirms proper column condition and absence of secondary interactions |
| Capacity Factor (k') | Measure of compound retention relative to void volume | Appropriate to ensure peaks elute away from void volume [53] | Verifies appropriate retention and separation from solvent front |
| Signal-to-Noise Ratio (S/N) | Measure of detection sensitivity | Typically >10 for quantitation [53] | Confirms adequate sensitivity for accurate measurement |
| Relative Retention (r) | Retention time relative to reference standard | Within specified range [53] | aids in peak identification in impurity methods |
The establishment of appropriate acceptance criteria must balance scientific rigor with practical achievable performance. Regulatory guidelines provide framework requirements, but specific criteria should be established during method validation based on the method's intended purpose [53].
SST Parameters for Non-Chromatographic Methods
While chromatographic SST parameters are well-documented, system suitability concepts apply across analytical techniques used in pharmaceutical research:
- Microbiological assays: Employ positive and negative controls to verify assay conditions, such as testing E. coli strains for antibiotic resistance with plasmid-free negative controls and viable strain verification [53]
- Electrophoretic techniques (e.g., SDS-PAGE): Use molecular weight markers with clear band separation and reference standards at known positions [53]
- Photometric assays: Require multiple measurements of reference standards with defined limits for standard deviation (e.g., ±5% of nominal value) [53]
- Immunoassays (e.g., ELISA): Verify that standard curve points fall within manufacturer specifications [53]
These diverse applications demonstrate that SST principles can be adapted to virtually any analytical technique, with the core requirement being verification of acceptable performance at the time of analysis.
Establishment of System Suitability Protocols
Method Development and Validation Linkage
SST criteria should be established during the method validation phase, as validation data provides the scientific foundation for defining appropriate system suitability parameters and acceptance criteria [53]. The validation process characterizes method performance under varied conditions, establishing the boundaries within which the method provides reliable results. These boundaries then inform the SST parameters that will monitor whether the method remains within its validated operational space during routine use.
Researchers should consider several practical aspects when establishing SST protocols:
- Standard Preparation: When possible, both sample and reference standard should be dissolved in mobile phase or similar organic solvent composition [53]
- Concentration Matching: The concentration of sample and reference standard should be comparable to ensure relevant performance assessment [53]
- Filtration Considerations: When filtration is employed, potential analyte adsorption to filters must be considered, particularly at lower concentrations [53]
- Reference Standards: FDA recommends using high-purity primary or secondary reference standards qualified against former standards, not originating from the same batch as test samples [53]
These practical considerations ensure that SST protocols are not only scientifically sound but also practically executable in routine laboratory operations.
Implementation Framework
The following workflow diagram illustrates the strategic position of SST within the overall analytical quality system:
This framework positions SST as the critical decision point before sample analysis, ensuring that only data from properly performing methods is reported.
Experimental Protocols for SST
Chromatographic System Suitability Testing
A robust SST protocol for HPLC/UV-Vis methods, adapted from regulatory guidelines and industry practice, involves these key steps:
Materials and Reagents:
- Reference standard of known purity and identity
- Appropriate chromatographic solvents (HPLC grade)
- Mobile phase prepared as per validated method
- System suitability standard solution at defined concentration
Experimental Procedure:
- Prepare the system suitability standard solution according to the validated method
- Stabilize the chromatographic system with mobile phase until a stable baseline is achieved
- Inject the system suitability standard solution in replicate (typically 5-6 injections)
- Process the data to calculate key parameters: retention time, peak area, theoretical plates, tailing factor, and resolution (if multiple components)
- Compare calculated parameters against pre-defined acceptance criteria
- Document all results and comparison to acceptance criteria
Acceptance Criteria Verification:
- Precision: Calculate %RSD of peak areas from replicate injections; must not exceed 2.0%
- Tailing factor: Calculate for main peak; must not exceed 2.0
- Theoretical plates: Calculate for main peak; must meet minimum specified count
- Resolution (for multi-component standards): Calculate between critical pairs; must meet minimum specified value
This protocol provides a standardized approach to verify chromatographic system performance before sample analysis.
Generalized SST Protocol for Untargeted Analysis
For untargeted metabolomics and similar comprehensive analysis approaches, system suitability checks follow a slightly different paradigm:
System Suitability Sample Preparation:
- Prepare a solution containing 5-10 authentic chemical standards dissolved in appropriate diluent
- Select standards to distribute across the analytical range (retention time and m/z)
- Include both early-eluting and late-eluting compounds to assess full chromatographic performance
Acceptance Criteria Assessment:
- m/z error: ≤5 ppm compared to theoretical mass
- Retention time error: <2% compared to defined retention time
- Peak area: Within predefined acceptable range ±10%
- Peak shape: Symmetrical with no evidence of peak splitting [55]
This approach, while more flexible than traditional chromatographic SST, still provides measurable metrics to qualify instrument fitness for unbiased analysis.
Essential Research Reagent Solutions
The implementation of effective SST requires specific reagent solutions tailored to verify method performance. These solutions serve as benchmarks for system verification.
Table 2: Key Research Reagent Solutions for System Suitability
| Reagent Solution | Composition & Preparation | Function in SST | Quality Requirements |
|---|---|---|---|
| System Suitability Standard | Reference standard at defined concentration in appropriate solvent | Verify chromatographic performance, precision, and sensitivity | High-purity primary or secondary standard; qualified against former reference standard [53] |
| Blank Solution | Mobile phase or sample solvent without analyte | Assess system contamination and background interference | Prepared identical to samples but excluding analyte |
| Resolution Mixture | Multiple components with known separation challenges | Verify separation capability for critical peak pairs | Contains specifically selected compounds that challenge method selectivity |
| Carryover Check Solution | High concentration standard above ULOQ | Evaluate system carryover between injections | Typically 2-3 times upper limit of quantification |
| Reference Standard Solution | Authentic chemical standard of known concentration | Verify detection sensitivity and retention time stability | Must not originate from same batch as test samples [53] |
These reagent solutions form the toolkit that enables researchers to comprehensively evaluate analytical system performance before committing valuable samples to analysis.
Data Assessment and Compliance Documentation
Systematic Data Evaluation
The evaluation of SST data must follow a structured approach to ensure consistent application of acceptance criteria and appropriate decision-making. The following diagram illustrates the decision process for SST implementation:
This structured approach ensures consistent response to SST results and appropriate documentation of all outcomes, supporting data integrity principles.
Regulatory Documentation Requirements
Comprehensive documentation is essential for demonstrating SST compliance during regulatory inspections. Key documentation requirements include:
- Written Procedures: Detailed, approved instructions for SST execution and evaluation [53]
- Complete Records: Raw data and processed results for all SST parameters [53]
- Review Protocols: Evidence of qualified personnel review of SST data [53]
- Deviation Documentation: Complete records of any SST failures and subsequent investigations [53]
- Corrective Action Reports: Documentation of actions taken to address SST failures [53]
Regulatory authorities explicitly expect written instructions to be complied with and, in terms of data integrity, completeness of the records and their review [53]. This documentation provides the evidence trail demonstrating that SST was properly executed and the analytical system was verified as suitable before sample analysis.
System Suitability Testing represents the operational culmination of the analytical method validation framework, providing the essential ongoing verification that validated methods continue to perform as intended in regulated pharmaceutical research. By implementing robust SST protocols with scientifically justified acceptance criteria, researchers and drug development professionals ensure the reliability of analytical data supporting drug development and manufacturing. The integration of SST within the broader quality system—complementing AIQ and method validation—creates a comprehensive approach to data quality that meets regulatory expectations and scientific standards. As analytical technologies evolve, the fundamental principles of SST remain constant: verification of fitness for purpose at the point of use, ensuring that every analytical result generated stands on a foundation of demonstrated system performance.
Overcoming Common Validation Challenges and Implementing Best Practices
Analytical method validation is the documented process of proving that a laboratory procedure consistently produces reliable, accurate, and reproducible results for its intended purpose [56]. It serves as a fundamental pillar of pharmaceutical quality assurance, safeguarding product integrity and patient safety by ensuring the identity, potency, quality, and purity of drug substances and products [56] [57]. Within the broader research thesis on analytical method validation, this whitepaper addresses two critical failure points that persistently undermine data reliability and regulatory success: incomplete validation protocols and improper statistical practices. These pitfalls, though common, carry significant consequences, including regulatory rejection, costly delays, and compromised product safety [56] [58]. A "validated" method is not inherently "valid" if its foundational protocol and statistical analysis are flawed [59]. This guide provides researchers and drug development professionals with detailed methodologies to identify, avoid, and rectify these critical errors.
The Peril of Incomplete Protocols
An incomplete or poorly defined validation protocol is a primary source of failure. It creates ambiguity during execution, leads to unacceptable data variability, and raises red flags during regulatory audits [56]. The core issue often lies in a lack of thorough planning and a failure to define all necessary elements before experimentation begins.
Essential Components of a Complete Protocol
A robust validation protocol must be a comprehensive document that leaves no room for interpretation. The following table outlines the critical components that must be explicitly defined.
Table 1: Essential Components of a Complete Analytical Method Validation Protocol
| Protocol Component | Description and Key Considerations |
|---|---|
| Objective and Scope | Clearly state the method's intended use (e.g., raw material release, in-process control, final product testing) and the specific analyte [58]. |
| Roles & Responsibilities | Define the responsibilities of each team member, the sponsor, and any contract organizations to ensure accountability [56]. |
| Acceptance Criteria | Pre-establish scientifically justified and logical acceptance limits for every validation parameter (e.g., precision expressed as %RSD) [59]. |
| Detailed Experimental Procedure | Provide a step-by-step methodology that is robust enough to be replicated by different scientists. This includes sample preparation, instrumentation conditions, and data processing steps. |
| Sample Plan & Matrix | Specify the number of replicates, concentration levels, and the relevant sample matrices (e.g., placebo, stressed samples) to be tested. Failing to test across all relevant matrices is a common oversight [56]. |
| Definition of Parameters | Explicitly list all validation parameters (specificity, accuracy, precision, etc.) and the experiments required to demonstrate them. |
| Data Documentation | Mandate the reporting of all data, including out-of-specification (OOS) results, to ensure transparency and avoid regulatory citations [57]. |
Experimental Protocol: Assessing Method Specificity
Specificity is the ability of a method to unequivocally assess the analyte in the presence of other components. The following is a detailed experimental methodology to establish specificity.
- Objective: To demonstrate that the analytical method can accurately measure the target analyte without interference from impurities, degradants, or the sample matrix.
- Materials:
- Analyte Standard: High-purity reference standard of the target compound.
- Placebo/Blank Matrix: The sample matrix without the active analyte.
- Stressed Samples: Samples of the drug product or substance that have been subjected to stress conditions (e.g., heat, light, acid/base hydrolysis, oxidation) to generate potential degradants.
- Known Impurities: Authentic samples of known process-related impurities.
- Procedure:
- Inject the placebo/blank matrix and confirm the absence of interfering peaks at the retention time of the analyte and impurities.
- Inject the analyte standard to establish its retention time and response.
- Inject the placebo/blank matrix spiked with known impurities to confirm separation from the analyte and from each other.
- Inject the stressed samples and demonstrate that the analyte peak is pure and free from co-eluting degradants using a orthogonal technique like Diode Array Detector (DAD) or Mass Spectrometry (MS). The peak purity index should be within accepted limits.
- Quantify the analyte in the stressed sample and demonstrate that the amount found correlates with the expected loss due to degradation.
- Acceptance Criteria: The method is considered specific if there is no interference from the placebo at the analyte retention time, all critical peaks are baseline resolved (resolution >1.5), and the peak purity test passes.
The workflow for establishing method specificity is a systematic process, as illustrated below.
The Risk of Statistical Missteps
Improper application of statistical methods is a pervasive and often hidden risk. It can distort conclusions, mask method weaknesses, and reduce the statistical power needed to make confident decisions [56]. A method may appear to function until it encounters real-world variability, at which point its statistical flaws become critical.
Foundational Statistical Principles for Validation
Robust statistical analysis in method validation rests on several key principles, which are frequently misapplied.
- Insufficient Sample Size: Using too few data points increases statistical uncertainty. Regulatory bodies expect robust sample sizes for each validation parameter to generate reliable estimates of mean and variance [56]. A general guideline is a minimum of six replicates for accuracy and precision at each concentration level.
- Incorrect Statistical Tools: Selecting the wrong statistical test for the dataset type and validation objective is common. For instance, using a student's t-test for comparing more than two means, or failing to use analysis of variance (ANOVA) for intermediate precision studies involving multiple factors [56].
- Ignoring Assay Bias and Response Factors: All analytical procedures, especially biological assays, have an inherent degree of bias [59]. Failing to characterize this bias, particularly for methods that determine relative percentages of analytes (e.g., purity vs. impurities), leads to inaccurate reporting. Response factors for different analytes must be established and integrated into calculations [59].
- Misinterpreting Linearity and Range: A high correlation coefficient (r) alone does not demonstrate linearity. Statistical analysis must include an assessment of the residual plot to detect non-random patterns, and the y-intercept should not be significantly different from zero [58].
Experimental Protocol: Determining Linearity and Range
The following protocol provides a statistically sound methodology for establishing the linearity of an analytical procedure and its applicable range.
- Objective: To demonstrate that the analytical method produces results that are directly proportional to the concentration of the analyte within a specified range.
- Materials:
- Stock Solution: A standard solution of the analyte at a concentration near the top of the expected range.
- Diluent: An appropriate solvent that is compatible with the sample and the analytical system.
- Procedure:
- Prepare a minimum of five concentration levels across the claimed range (e.g., 50%, 75%, 100%, 125%, 150% of the target concentration) [58].
- Inject each concentration level in duplicate or triplicate.
- Record the analytical response (e.g., peak area) for each injection.
- Plot the mean response against the concentration.
- Perform a linear regression analysis on the data to calculate the slope, y-intercept, and correlation coefficient (r).
- Critically, analyze the residual plot (the difference between the observed value and the value predicted by the regression line vs. concentration). A random scatter of residuals around zero confirms linearity.
- Statistical Analysis and Acceptance Criteria:
- Correlation Coefficient (r): Typically, r ≥ 0.998 is expected for chromatographic methods.
- Y-Intercept: Should not be statistically significantly different from zero (e.g., p-value > 0.05 in a t-test).
- Residuals: Should be randomly distributed around zero with no obvious pattern.
- Range: The range is validated if all the above criteria are met across the entire span of concentrations tested.
The logical flow for statistical analysis of linearity data ensures all critical aspects are evaluated.
The following table consolidates the typical validation parameters, their statistical definitions, and common acceptance criteria for a chromatographic assay, providing a clear reference for protocol design.
Table 2: Key Analytical Validation Parameters, Definitions, and Acceptance Criteria
| Validation Parameter | Statistical Definition / Methodology | Typical Acceptance Criteria (e.g., Assay) |
|---|---|---|
| Accuracy | The closeness of agreement between a test result and the accepted reference value. Measured by % recovery of a spiked analyte. | Mean recovery between 98.0% and 102.0% |
| Precision (Repeatability) | The closeness of agreement between a series of measurements under the same conditions. Expressed as % Relative Standard Deviation (%RSD). | %RSD ≤ 2.0% for a minimum of 6 replicates |
| Intermediate Precision | The agreement between measurements under varied conditions (different days, analysts, equipment). Assessed via ANOVA. | Overall %RSD ≤ 2.0% with no significant difference between the varied conditions (p > 0.05) |
| Linearity | The ability to obtain results directly proportional to analyte concentration. Assessed via linear regression and residual analysis. | Correlation coefficient (r) ≥ 0.998; residuals random |
| Range | The interval between the upper and lower concentrations with demonstrated linearity, accuracy, and precision. | From 80% to 120% of the test concentration |
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of any validation study is contingent on the quality and consistency of the materials used. The following table details key reagent solutions and their critical functions in ensuring data integrity.
Table 3: Essential Research Reagents and Materials for Method Validation
| Reagent / Material | Function in Validation | Critical Considerations |
|---|---|---|
| Reference Standard | Serves as the benchmark for identifying the analyte and quantifying its amount. | Must be of known purity and identity. A two-tiered approach linking new working standards to a primary reference standard is recommended [60]. |
| System Suitability Solutions | Verifies that the chromatographic system is performing adequately at the time of the test. | Typically a mixture of the analyte and key impurities at a specific concentration to check parameters like resolution, tailing factor, and theoretical plates. |
| Stressed Samples | Samples intentionally degraded to demonstrate the method's ability to separate the analyte from its degradants (Specificity). | Generated under controlled stress conditions (heat, light, acid/base, oxidation). The degradation should be ~5-20% to be meaningful [57]. |
| Placebo/Blank Matrix | The formulation or biological matrix without the active ingredient. Used to prove the absence of interference. | Must be representative of the final product composition. |
| Critical Reagents | Antibodies, enzymes, or other biological components used in specific assays (e.g., ELISA). | Stability and lot-to-lot consistency are paramount. Expiration times must be established through stability studies [59]. |
Navigating the complexities of analytical method validation requires a vigilant, scientifically rigorous approach that proactively addresses the twin pitfalls of incomplete protocols and statistical missteps. As detailed in this guide, success hinges on developing exhaustive protocols that pre-define every critical element and on applying robust statistical principles to uncover the true performance of a method. Adherence to these practices, framed within a holistic understanding of the method's intended use and lifecycle, transforms validation from a regulatory checkbox into a definitive demonstration of quality and reliability. For researchers and drug development professionals, mastering these elements is not merely about compliance—it is about building a foundation of trustworthy data that ensures patient safety and accelerates the delivery of effective medicines to the market.
Analytical method validation is the cornerstone of reliable chemical and bioanalytical data, providing documented evidence that a specific analytical procedure is suitable for its intended use. Within pharmaceutical development and clinical monitoring, techniques including High-Performance Liquid Chromatography (HPLC), Gas Chromatography (GC), Ultraviolet-Visible spectroscopy (UV-Vis), and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) each present unique advantages and specific risks. Validation parameters such as specificity, linearity, accuracy, precision, and sensitivity (LOD/LOQ) are universal, but the approaches to demonstrating them and the associated challenges are highly technology-dependent. This guide examines the method-specific risks and considerations for these key analytical platforms, providing a framework for robust method development and validation within a broader research context.
High-Performance Liquid Chromatography (HPLC)
Core Risks and Mitigation Strategies
HPLC is widely used for the quantification of non-volatile and thermally labile compounds. A primary risk is inadequate specificity, where analyte peaks co-elute with interfering matrix components. Another significant challenge is carryover, which can falsely elevate results, as was documented in a method for immunosuppressants where one analyte exhibited 28.0% carryover to the lowest calibration point [61]. Column degradation over time also poses a risk to method robustness, potentially altering retention times and peak efficiency.
- Mitigation Strategies: To address specificity, utilize photodiode array (DAD) detectors to confirm peak purity. For carryover, implement robust autosampler wash protocols and assess carryover as a standard part of method validation [61]. To protect the analytical column from matrix effects, especially in bioanalytical methods, employ effective sample clean-up procedures such as solid-phase extraction or protein precipitation.
Experimental Protocol: HPLC Analysis of Bakuchiol in Cosmetics
A validated HPLC-DAD method for quantifying bakuchiol in cosmetic serums illustrates a standard workflow [62].
Chromatographic Conditions:
- Column: Reverse-phase, endcapped C18.
- Mobile Phase: Isocratic elution with acetonitrile containing 1% formic acid.
- Detection: DAD at λ = 260 nm.
- Flow Rate: 1.0 mL/min (typical).
- Injection Volume: 10-20 µL.
Sample Preparation: Cosmetic serum samples are dissolved and diluted in a suitable solvent (e.g., ethanol or acetonitrile). For complex matrices like oil-in-water emulsions, an extraction step (e.g., vortexing, sonication, centrifugation) is necessary to ensure complete dissolution and recovery of the analyte [62].
Validation Data:
Table 1: Key Validation Parameters for the HPLC Analysis of Bakuchiol [62]
| Parameter | Result/Description |
|---|---|
| Analyte | Bakuchiol |
| Detection | DAD at 260 nm |
| Retention Time | ~31.8 minutes |
| Specificity | No interference from other cosmetic ingredients |
| Precision (Intraday RSD) | < 2.5% |
| LOD/LOQ Calculation | Based on calibration curve standard deviation and slope |
Gas Chromatography (GC)
Core Risks and Mitigation Strategies
GC is ideal for volatile and thermally stable analytes. A major risk is the need for derivatization for non-volatile compounds, such as fatty acids, which introduces extra steps, potential for error, and variable recovery [63]. Inlet and column activity can lead with active compounds, resulting in peak tailing or decomposition. Furthermore, GC methods are highly sensitive to instability in chromatographic conditions like carrier gas flow rate and oven temperature.
- Mitigation Strategies: To avoid derivatization, develop methods using specialized columns, such as the DB-FFAP (nitroterephthalic acid modified polyethylene glycol) column, which successfully enabled the direct analysis of oleic acid and related fatty acids [63]. Use deactivated liners and columns and employ derivatization-free protocols where possible to improve accuracy and robustness. For robustness validation, deliberately vary parameters like carrier gas flow rate and oven temperature to establish method tolerances [64].
Experimental Protocol: Derivatization-Free GC-FID for Fatty Acids
A validated GC-FID method for oleic acid USP-NF material demonstrates a direct analysis approach [63].
Chromatographic Conditions:
- Column: DB-FFAP capillary column (30 m × 0.32 mm i.d.).
- Detector: Flame Ionization Detector (FID).
- Oven Program: Gradient optimized to separate 15 fatty acids within 20 minutes.
- Carrier Gas: Helium or Hydrogen.
- Injection Mode: Split or splitless.
Sample Preparation: Oleic acid samples are dissolved in a suitable volatile solvent. The method eliminates the need for derivatization, simplifying preparation and reducing error sources [63].
Validation Data:
- Specificity: Baseline separation of 15 fatty acids was achieved.
- Robustness: The method was validated for small, deliberate changes in operational parameters.
Table 2: Key Validation Parameters for the GC-FID Analysis of Oleic Acid [63]
| Parameter | Result/Description |
|---|---|
| Analytes | Oleic acid and 14 related fatty acids |
| Detection | Flame Ionization Detector (FID) |
| Column | DB-FFAP (for polar compounds) |
| Key Innovation | Derivatization-free analysis |
| Total Run Time | 20 minutes |
| Validation | Specificity, linearity, precision, accuracy, sensitivity, robustness |
Ultraviolet-Visible Spectroscopy (UV-Vis)
Core Risks and Mitigation Strategies
UV-Vis spectroscopy is simple and cost-effective but suffers from low specificity as it cannot distinguish between compounds with similar chromophores. A significant risk is matrix interference, where other sample components absorb at the same wavelength, leading to inaccurate concentration readings. The technique is also highly dependent on sample clarity; turbid or colored samples can scatter light and cause significant errors.
- Mitigation Strategies: Ensure complete and reproducible sample dissolution. For complex matrices like emulsions, a thorough extraction is critical; one study on bakuchiol serums could not properly quantify analytes in oil-in-water emulsions due to incomplete dissolution [62]. Use standard addition methods to correct for matrix effects. Confirm the identity of the analyte through a full spectrum overlay with a reference standard rather than relying on a single wavelength.
Experimental Protocol: UV-Vis Analysis of Bakuchiol
The quantification of bakuchiol in cosmetic serums using UV-Vis highlights both the application and limitations of the technique [62].
Instrument Conditions:
- Wavelength: 262 nm (λmax for bakuchiol).
- Solvent: Ethanol.
- Pathlength: 1 cm.
Sample Preparation: Solid serum samples are dissolved in ethanol. For homogeneous oil solutions, direct dilution may be sufficient. For oil-in-water emulsions (Samples 5 & 6), bakuchiol could not be properly extracted or quantified due to incomplete dissolution, highlighting a major limitation for such matrices [62].
Validation Data:
- Specificity: Assessed by comparing the sample's UV spectrum shape to that of a pure bakuchiol standard. Sample 2 showed no presence of bakuchiol, demonstrating a lack of specificity in the product [62].
- Linearity: Established using a calibration curve of bakuchiol standard solutions.
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)
Core Risks and Mitigation Strategies
LC-MS/MS offers superior sensitivity and specificity but introduces unique risks. The matrix effect is a critical challenge, where co-eluting matrix components can suppress or enhance the analyte's ionization, leading to inaccurate results. Cross-talk between MRM channels can occur when analyzing multiple compounds simultaneously. The complexity of the instrumentation also increases the risk of instrument downtime and requires highly skilled operators.
- Mitigation Strategies: To compensate for matrix effects and variability, use stable isotope-labeled internal standards (SIL-IS). This was effectively applied in an LC-MS/MS method for LXT-101, where 127I-LXT-101 was used as the IS [65]. Employ efficient chromatographic separation to reduce matrix interference and optimize sample clean-up (e.g., protein precipitation, solid-phase extraction). Routinely monitor instrument performance with quality control samples.
Experimental Protocol: LC-MS/MS for Immunosuppressants in Microvolume Blood
A method for simultaneous quantification of multiple immunosuppressants in 2.8 µL of whole blood demonstrates a advanced bioanalytical application [61].
Chromatographic & Mass Spectrometric Conditions:
- Column: C18 column.
- Mobile Phase: Gradient of water and acetonitrile, both with modifiers like formic acid.
- Ionization: Electrospray Ionization (ESI) in both positive (for Tac, Eve, Sir, CycA) and negative (for MPA, MPAG) modes.
- Detection: Selected Reaction Monitoring (SRM).
Sample Preparation:
- Protein precipitation with acetonitrile.
- Addition of internal standards.
- Vortex-mixing and centrifugation.
- Evaporation of supernatant and reconstitution in mobile phase [61].
Validation Data:
Table 3: Key Validation Parameters for an LC-MS/MS Method for Immunosuppressants [61]
| Parameter | Result/Description |
|---|---|
| Analytes | Tacrolimus, Everolimus, Sirolimus, Cyclosporine A, Mycophenolic Acid (MPA) |
| Sample Volume | 2.8 µL whole blood |
| Linearity (R²) | > 0.990 for all analytes |
| Precision (RSD) | < 10% for all QCs |
| Accuracy | Within ±15% |
| Key Feature | Simultaneous quantification of drugs in different matrices (whole blood/plasma) |
Critical Validation Parameters Across Techniques
Approaches for Determining LOD and LOQ
The Limit of Detection (LOD) and Limit of Quantification (LOQ) are fundamental to establishing method sensitivity. However, a universal protocol is lacking, and different approaches can yield significantly different values [40]. The classical strategy, which uses signal-to-noise ratios (3:1 for LOD, 10:1 for LOQ) or statistical parameters from the calibration curve (LOD = 3.3σ/S, LOQ = 10σ/S), is common but can provide underestimated values [62] [40] [64]. Modern graphical strategies, such as the accuracy profile and uncertainty profile, are more reliable as they incorporate the method's total error and uncertainty over the concentration range, providing a more realistic assessment [40].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Analytical Method Development
| Item | Function | Example from Research |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (SIL-IS) | Compensates for analyte loss during preparation and matrix effects during ionization in LC-MS/MS. | 127I-LXT-101 used in LC-MS/MS method for LXT-101 [65]. |
| Specialized GC Columns | Enables separation of specific compound classes without derivatization, simplifying sample preparation. | DB-FFAP column for direct analysis of fatty acids [63]. |
| High-Purity Mobile Phase Modifiers | Improves chromatographic peak shape and enhances ionization efficiency in LC-MS. | Formic acid in mobile phase for HPLC analysis of bakuchiol and LC-MS/MS of LXT-101 [62] [65]. |
| Internal Standard for qNMR | Enables accurate quantification in NMR where a stable, non-interacting reference is needed. | Nicotinamide used for quantification of bakuchiol in cosmetic products [62]. |
Analytical Method Validation Workflow
The following diagram outlines the core workflow for developing and validating an analytical method, integrating key considerations for each major technique.
Technology Selection Logic
This decision tree provides a high-level guide for selecting the most appropriate analytical technology based on the properties of the analyte and the requirements of the analysis.
The selection of an analytical technique and its subsequent validation are inextricably linked to a clear understanding of technology-specific risks. HPLC risks carryover and specificity issues, GC often necessitates complex derivatization, UV-Vis is prone to matrix interference, and LC-MS/MS, while powerful, is vulnerable to matrix effects and requires significant expertise. A thorough, risk-based validation strategy that employs modern graphical tools for defining limits and carefully selected reagents and materials is fundamental to generating reliable, defensible data. This approach ensures that analytical methods are not only scientifically sound but also fit for their intended purpose in pharmaceutical development and clinical diagnostics, forming a critical component of any rigorous research program.
Quality by Design (QbD) and Analytical Target Profile (ATP) Implementation
The pharmaceutical industry is undergoing a significant transformation from traditional, empirical analytical method development to a systematic, science-based framework known as Quality by Design (QbD). This approach, when applied to analytical methods (Analytical QbD or AQbD), represents a fundamental shift from "testing quality in" to "building quality in" from the outset [66] [67]. Rooted in the International Council for Harmonisation (ICH) guidelines Q8-Q12, and more recently Q14 for analytical development, AQbD emphasizes deep process understanding and proactive risk management over reactive quality testing [68] [69] [70].
Central to this framework is the Analytical Target Profile (ATP), a predefined statement that outlines the intended purpose of the analytical method and the performance criteria it must meet throughout its lifecycle [67]. The ATP acts as the foundational blueprint, ensuring the method remains fit-for-purpose from development through routine use and eventual retirement. Within the broader context of analytical method validation research, AQbD moves beyond a one-time validation event toward a holistic lifecycle management approach, enhancing robustness, regulatory flexibility, and continuous improvement [69] [67]. This guide provides an in-depth technical exploration of the core principles, implementation workflows, and practical applications of QbD and ATP in modern pharmaceutical analysis.
Core Principles and Definitions
Analytical Target Profile (ATP)
The Analytical Target Profile (ATP) is a prospective summary of the quality and performance requirements for an analytical procedure. It defines the criteria for the data quality necessary to support the intended purpose of the method, serving as the cornerstone of the AQbD approach [71] [67].
- Purpose and Scope: The ATP clearly states what the method must measure, why it is being measured (e.g., for release testing, stability monitoring, or impurity profiling), and the required level of quality for the resulting data [67].
- Key Elements: A well-constructed ATP includes performance criteria such as accuracy, precision, specificity, linearity, range, and robustness. These criteria are defined with specific, measurable targets [67].
- Practical Example: For a High-Performance Liquid Chromatography (HPLC) method developed to measure the potency of an Active Pharmaceutical Ingredient (API) in a tablet, the ATP might state: "The method must accurately and precisely quantify the API within a range of 90–110% of the label claim with an accuracy of ±2% and a precision (relative standard deviation) of ≤2%" [67].
Critical Quality Attributes (CQAs) and Critical Method Parameters (CMPs)
From the ATP, the Critical Quality Attributes (CQAs) of the analytical method are derived. CQAs are the measurable indicators of method performance that must be controlled to ensure the method meets its ATP [71] [68].
- Examples of CQAs: In a chromatographic method, typical CQAs include resolution between critical peak pairs, retention time stability, peak tailing factor, and Limit of Quantitation (LOQ) for impurities [67].
- Linking CQAs to CMPs: Critical Method Parameters (CMPs) are the input variables (e.g., mobile phase pH, column temperature, flow rate) that have a direct impact on the CQAs. Identifying the relationship between CMPs and CQAs is essential for achieving a robust method [67]. The interplay between ATP, CQAs, and CMPs creates a controlled, well-understood analytical method [67].
The AQbD Workflow: A Systematic Process
The implementation of AQbD follows a structured, sequential workflow that transforms the theoretical ATP into a validated and operational analytical method. The following diagram illustrates this comprehensive lifecycle approach.
AQbD Implementation Workflow
AQbD Implementation Framework
Risk Assessment and Management
Risk assessment is the engine that drives efficient AQbD implementation. It provides a systematic way to identify and prioritize the many potential factors that could affect method performance, allowing resources to be focused on the most critical areas [71] [67].
- Tools and Techniques: Common risk assessment tools include Ishikawa (fishbone) diagrams, which help brainstorm potential sources of variability (e.g., instrument, method, material, environment), and Failure Mode and Effects Analysis (FMEA), which ranks risks based on their severity, occurrence, and detection to calculate a Risk Priority Number (RPN) [71] [67].
- Application: The output of risk assessment is a prioritized list of CMPs that require further investigation. This ensures that experimental resources are directed toward understanding and controlling the parameters that matter most, avoiding wasted effort on insignificant factors [67].
Design of Experiments (DoE) for Method Optimization
Unlike the traditional "One Factor at a Time" (OFAT) approach, which can miss critical parameter interactions, Design of Experiments (DoE) is a statistical methodology for simultaneously studying multiple CMPs and their interactive effects on CQAs [66] [71].
- DoE Methodology: DoE involves creating a structured set of experiments where multiple factors are varied in a predefined pattern. Common designs include full factorial, fractional factorial, Box-Behnken, and Central Composite Designs [71] [72].
- Data Analysis and Modeling: The results of the DoE trials are analyzed using statistical software to generate a mathematical model (often a polynomial equation) that describes the relationship between the CMPs and each CQA. This model is used to create contour plots and response surface models that visually depict this relationship [72].
Establishing the Method Operable Design Region (MODR)
A key output of the DoE and optimization process is the Method Operable Design Region (MODR). The MODR is the multidimensional combination and interaction of input variables (CMPs) for which the analytical method has been demonstrated to provide results of suitable quality, meeting the ATP [71] [67].
- Regulatory Flexibility: Operating within the MODR is not considered a change from the validated method. This provides significant operational flexibility, as minor adjustments to method parameters within the MODR do not require regulatory re-validation, simplifying method troubleshooting and transfer [67].
- Control Strategy: A control strategy is developed to ensure the method operates within the MODR during routine use. This includes procedural controls, system suitability tests, and analyst training [68] [67].
Experimental Protocols and Applications
Case Study: QbD-Driven HPLC Method for Antidepressant Analysis
A practical application of AQbD is illustrated in the development of a stability-indicating RP-HPLC method for the simultaneous estimation of Bupropion and Dextromethorphan (AXS-05) in a synthetic mixture [72].
1. Define ATP: The ATP was to develop a single, selective, and precise HPLC method for the simultaneous quantification of both drugs in a synthetic mixture that could also separate and detect degradation products generated under forced degradation studies [72].
2. Identify CQAs and CMPs:
- CQAs: Retention time, resolution between peaks, and peak tailing.
- CMPs: Initial risk assessment and literature review identified buffer pH, organic phase composition (% organic), and flow rate as potential high-risk CMPs [72].
3. Experimental Design (DoE):
- A three-factor experimental design was generated using Design Expert 10.0 software, resulting in 27 trial runs.
- The factors and their studied ranges were:
- pH: 2.5 - 4.5
- % Organic: 65% - 75%
- Flow Rate: 0.8 - 1.2 mL/min [72].
4. Data Analysis and Optimization:
- Multiple linear regression analysis and a quadratic model were used to analyze the data.
- The 2D contour and 3D response surface plots were generated from the model to visualize the effects of the CMPs on the CQAs.
- The optimal chromatographic conditions were determined by optimizing numerical functions and desirability, balancing all CQAs [72].
5. Validation: The optimized method was validated per ICH guidelines, confirming that it met all ATP criteria for accuracy, precision, linearity, LOD, LOQ, and robustness [72].
Essential Research Reagent Solutions
The following table details key materials and instruments used in AQbD-based HPLC method development, as exemplified in the case study and broader practice.
| Item | Function & Application in AQbD |
|---|---|
| HPLC System with PDA/UV Detector | Enables separation and detection of analytes. Essential for executing DoE trials and measuring CQAs (retention time, peak area, spectral purity) [72]. |
| C18 Reverse-Phase Column | The stationary phase for separation. A critical source of variability; different brands/lots with the same specification are often tested as a CMP to ensure robustness [72] [67]. |
| Buffer Salts & pH Adjusters (e.g., Potassium Phosphate) | Used to prepare mobile phase buffers. Buffer pH and strength are frequently identified as CMPs due to their significant impact on retention, resolution, and peak shape [72]. |
| Organic Solvents (Methanol, Acetonitrile, Ethanol) | Mobile phase components. Composition is a key CMP. Green AQbD encourages ethanol/water mixtures over acetonitrile for environmental sustainability [71]. |
| Design of Experiments (DoE) Software (e.g., Design Expert, MODDE) | Critical for designing efficient experiments, modeling data, identifying interactions between CMPs, and defining the MODR [72] [73]. |
| Chemical Reference Standards | High-purity analytes used to prepare standard solutions for method development and validation. Essential for establishing accuracy, linearity, and range [72]. |
The experimental design and optimization process for this case study can be visualized as follows.
DoE-Based Method Optimization
Regulatory Landscape and Current Practices
ICH Guidelines: Q2(R2) and Q14
The regulatory framework for analytical procedures has recently evolved with the adoption of two pivotal ICH guidelines:
- ICH Q2(R2): "Validation of Analytical Procedures" is the revised guideline that provides a framework for validation, now encompassing a broader range of analytical techniques, including multivariate and biological methods. It introduces more detailed statistical approaches, such as the use of confidence intervals for accuracy and precision and allows for combined accuracy and precision assessments [69].
- ICH Q14: "Analytical Procedure Development" explicitly outlines science- and risk-based approaches for method development and describes the concept of the Analytical Procedure Lifecycle. It harmonizes the principles of AQbD, encouraging the establishment of an MODR and a lifecycle management approach [69].
A recent industry survey on the implementation of these guidelines revealed both opportunities and challenges [69]:
- Opportunities: Greater regulatory flexibility, acceptance of platform analytical procedures for similar molecules, and the ability to leverage prior knowledge and development data to reduce non-value-added studies.
- Challenges: Concerns about setting meaningful acceptance criteria for confidence intervals, lack of internal expertise for new statistical approaches, and potential inconsistencies in regulatory acceptance across different global health authorities.
AQbD vs. Traditional Approach
The advantages of implementing AQbD over the traditional approach are substantial and directly address common pain points in analytical laboratories.
Table: Comparison of Traditional and AQbD Analytical Method Development Approaches
| Aspect | Traditional Approach (OFAT) | AQbD Approach |
|---|---|---|
| Philosophy | Reactive; quality tested at the end | Proactive; quality built into the design [67] |
| Development | "One Factor at a Time" (OFAT), empirical | Systematic, using Risk Assessment and DoE [66] [67] |
| Robustness | Limited understanding of parameter interactions | Deep understanding of CMPs and their interactions, defined MODR [66] [67] |
| Validation | One-time event to prove method works | Confirmation that method meets predefined ATP within the MODR [67] |
| Regulatory Flexibility | Rigid; changes often require revalidation | Flexible; movement within MODR does not require re-approval [67] |
| Out-of-Specification (OOS) | Higher risk due to limited robustness understanding | Reduced OOS results due to robust design and understanding of failure edges [66] [67] |
| Lifecycle Management | Often static, with limited continuous improvement | Dynamic, with ongoing monitoring and continuous improvement [69] [67] |
The implementation of Quality by Design (QbD) and the Analytical Target Profile (ATP) represents a maturation of analytical science, aligning it with modern, risk-based regulatory paradigms. This systematic framework moves the industry beyond the limitations of empirical, OFAT development toward a future where methods are inherently robust, well-understood, and adaptable. The synergy of a clearly defined ATP, rigorous Risk Assessment, systematic DoE, and a well-characterized MODR creates a foundation for reliable analytical procedures that minimize failures and support continuous improvement throughout the product lifecycle.
While the adoption of ICH Q2(R2) and Q14 presents challenges in statistical expertise and global regulatory alignment, the benefits are clear: enhanced method robustness, increased regulatory flexibility, and more efficient use of resources [69]. As the industry continues to advance, integrating AQbD with emerging trends like Green Analytical Chemistry (GAC) and Artificial Intelligence (AI) will further enhance the sustainability, predictive power, and efficiency of pharmaceutical analysis, ensuring that quality remains a cornerstone of drug development and manufacturing [71].
Design of Experiments (DoE) for Efficient Method Optimization
Within the broader context of analytical method validation research, the development of robust, accurate, and precise analytical methods is a critical pillar in the drug development lifecycle. These methods are essential for ensuring the identity, purity, potency, and stability of pharmaceutical products, directly impacting their safety and efficacy [37]. Analytical method development involves the selection and optimization of methods to measure specific attributes of a drug substance or product, ensuring they are sensitive, specific, and robust [37]. In this framework, Design of Experiments (DoE) emerges as a powerful systematic methodology that transcends the inefficiencies and limitations of the traditional One-Variable-at-a-Time (OVAT) approach. By strategically varying multiple input parameters simultaneously and analyzing their individual and interactive effects on critical method outputs, DoE enables scientists to build predictive models for method robustness and establish a scientifically sound method operable design region (MODR). This structured approach to method optimization provides a high level of assurance that the method will perform reliably throughout its lifecycle, forming a solid foundation for the subsequent formal method validation process, which demonstrates the method's suitability for its intended use [37].
Fundamental Principles of Design of Experiments
The transition from a OVAT approach to a DoE methodology represents a paradigm shift in optimization strategy. OVAT, which involves changing one factor while holding all others constant, is not only time-consuming and resource-intensive but, more critically, fails to detect interactions between factors. This flaw can lead to a suboptimal understanding of the method's behavior and a lack of robustness. In contrast, DoE is founded on several key principles that ensure a comprehensive and efficient path to an optimized method.
- Factors: These are the input variables or parameters that can be controlled and varied during the experiment. In analytical method development, factors can include chromatographic conditions such as mobile phase pH, column temperature, gradient time, and flow rate.
- Responses: These are the output variables or measured outcomes that define the method's performance. Typical responses in method development are critical quality attributes like resolution, peak asymmetry, tailing factor, and retention time.
- Experimental Design: This is the structured set of experiments that defines the specific combinations of factor levels to be tested. The design is selected to maximize the information gained from a minimal number of experimental runs.
- Analysis of Variance (ANOVA): ANOVA is a statistical technique used to analyze the differences among group means in a sample. In DoE, it is used to partition the total variability in the response data into attributable sources, determining which factors and interactions have a statistically significant effect.
- Interaction Effects: This is a core concept that OVAT misses. An interaction occurs when the effect of one factor on the response depends on the level of another factor. DoE is uniquely capable of detecting and quantifying these interactions.
The following diagram illustrates the logical workflow for implementing DoE, from planning to application.
Key DoE Designs and Selection Criteria
Selecting the correct experimental design is paramount to the success of a DoE study. The choice depends on the goals of the study, the number of factors to be investigated, and the need for model complexity. Screening designs are used in the early stages to identify the few critical factors from a long list of potential variables. In contrast, optimization designs are employed to model the response surfaces in detail and locate the true optimum. The table below summarizes the primary DoE designs used in analytical method development.
Table 1: Common DoE Designs for Method Development and Optimization
| Design Type | Primary Objective | Typical Use Case | Key Characteristics | Number of Experiments (for k factors) |
|---|---|---|---|---|
| Full Factorial | Screening, Modeling | Identifying all main effects and interactions for a small number (2-4) of factors. | Tests all possible combinations of factor levels. Provides full information on all effects. | ( 2^k ) to ( 3^k ) |
| Fractional Factorial | Screening | Identifying vital few main effects from many (5+) factors; assumes some interactions are negligible. | A carefully selected fraction of a full factorial design. Reduces experimental burden. | ( 2^{k-p} ) |
| Plackett-Burman | Screening | Very efficient screening of a large number (up to 11 with 12 runs) of factors. | A special, highly fractional design for main effects only. | N (multiple of 4) |
| Central Composite (CCD) | Optimization | Building a precise quadratic response surface model for 2-5 critical factors. | Combines factorial, axial, and center points to fit a second-order model. | ( 2^k + 2k + C_p ) |
| Box-Behnken | Optimization | Building a quadratic model without a factorial corner points; useful when extremes are impractical. | A spherical design with all points lying on a sphere of radius √2. | ( 2k(k-1) + C_p ) |
Note: ( k ) = number of factors, ( C_p ) = number of center points.
Experimental Protocols for DoE in HPLC Method Optimization
To illustrate the practical application of DoE, consider the development of a reversed-phase High-Performance Liquid Chromatography (HPLC) method for the separation of a multi-component pharmaceutical formulation. The protocol below outlines a detailed, step-by-step methodology.
Protocol: DoE for HPLC Method Development
1. Define Objective and CQAs:
- Objective: Develop a robust, stability-indicating HPLC method for the simultaneous quantification of Active Pharmaceutical Ingredient (API) and its three potential degradation products.
- Critical Quality Attributes (CQAs): The key responses are Resolution (Rs) between critical peak pairs (minimum > 2.0), Analysis Time (t) (maximizing throughput, target < 15 minutes), and Peak Tailing Factor (Tf) (maintaining symmetry, target < 1.5).
2. Identify Critical Method Parameters (Factors):
- Through risk assessment and prior knowledge, select three continuous factors for optimization:
- Factor A: pH of aqueous mobile phase (e.g., 3.0 - 5.0).
- Factor B: Gradient Time (tG) from low to high organic solvent concentration (e.g., 10 - 20 minutes).
- Factor C: Column Temperature (T) (e.g., 30 - 50 °C).
3. Select and Execute Experimental Design:
- A Central Composite Design (CCD) is ideal for this 3-factor scenario as it efficiently fits a quadratic model, allowing for the identification of potential curvature in the response surface.
- The CCD will require a total of ( 2^3 = 8 ) factorial points, ( 2*3 = 6 ) axial points, and 4-6 center point replicates, totaling 18-20 experimental runs. The center points are crucial for estimating pure error and testing model lack-of-fit.
- Prepare mobile phases and test samples according to the randomized run order provided by the DoE software to minimize bias.
4. Data Collection and Model Building:
- Execute all HPLC runs as per the randomized design matrix, recording the responses (Rs, t, Tf) for each chromatogram.
- Input the data into a statistical software package (e.g., JMP, Design-Expert, Minitab).
- Perform Multiple Linear Regression (MLR) to build a mathematical model for each response. The general form of a quadratic model for three factors is: ( Y = β0 + β1A + β2B + β3C + β{12}AB + β{13}AC + β{23}BC + β{11}A^2 + β{22}B^2 + β{33}C^2 )
- Use Analysis of Variance (ANOVA) to assess the significance and adequacy of each model. Look for a high F-value and a low p-value (< 0.05) for the model, a non-significant lack-of-fit test (p > 0.05), and a high coefficient of determination (R²).
5. Optimization and MODR Establishment:
- Utilize the software's numerical and graphical optimization tools (e.g., desirability functions, overlay plots) to find a region in the factor space that simultaneously satisfies all the CQAs.
- The Method Operable Design Region (MODR) is defined as the multidimensional combination and interaction of input variables (e.g., pH, tG, T) that have been demonstrated to provide assurance of method performance. An example of a resulting MODR is visualized in the following response surface plot.
6. Verification and Robustness Testing:
- Select one set of optimum conditions within the MODR (e.g., pH 4.2, tG 14 min, T 40°C) and perform a minimum of three verification runs to confirm that the predicted responses align with the observed values.
- A robustness test, using a small-scale DoE (e.g., a Plackett-Burman or fractional factorial) around the set point, can formally demonstrate the method's resilience to small, deliberate variations in method parameters, a key component of the subsequent validation [37].
The Scientist's Toolkit: Essential Reagents and Instrumentation
The successful execution of a DoE-based method development and validation study relies on a suite of high-quality materials and sophisticated instrumentation. The following table details the key research reagent solutions and equipment essential for this field.
Table 2: Essential Research Reagents and Instrumentation for Analytical Method Development
| Item / Category | Function & Importance in Method Development | Specific Examples |
|---|---|---|
| Reference Standards | Highly characterized substances used to calibrate instruments and validate methods. They are the benchmark for identity, potency, and purity assessments. | Certified Reference Materials (CRMs), USP/EP reference standards, drug substance and impurity standards. |
| Chromatographic Columns | The heart of the separation. Different column chemistries (C18, C8, phenyl, HILIC) are selected based on the analyte's properties to achieve optimal resolution. | Waters Acquity UPLC BEH C18, Phenomenex Luna C18(2), Agilent Zorbax Eclipse Plus C8. |
| HPLC/UPLC Grade Solvents & Reagents | High-purity mobile phase components are critical to minimize baseline noise, ghost peaks, and system contamination, ensuring accurate and reproducible results. | LC-MS grade water, acetonitrile, and methanol; high-purity buffers (e.g., ammonium formate, phosphate salts) and additives (e.g., trifluoroacetic acid). |
| State-of-the-Art Instrumentation | Provides the platform for precise and accurate analysis. Advanced systems offer superior detection, sensitivity, and data integrity for regulated environments. | HPLC/UPLC (Waters, Agilent), LC-MS/MS & HRMS (Sciex, Thermo Fisher) for identification and quantification, GC-MS for volatiles, NMR (Bruker) for structural elucidation [37]. |
| System Suitability Test (SST) Kits | Pre-made mixtures of analytes used to verify that the total chromatographic system is adequate for the intended analysis before sample runs begin. | Mixtures specified in pharmacopoeias (USP, Ph. Eur.) containing compounds to test parameters like plate count, tailing, and resolution. |
Integration with the Analytical Method Validation lifecycle
The ultimate output of a DoE-led optimization is a well-characterized and robust analytical method, poised for formal validation. The principles of DoE are deeply intertwined with the validation lifecycle, which is conducted per regulatory guidance from bodies like the FDA, EMA, and ICH [37]. The method validation process systematically demonstrates that the method is suitable for its intended purpose, evaluating performance characteristics including accuracy, precision, specificity, linearity, range, limit of detection (LOD), limit of quantification (LOQ), ruggedness, and robustness [37]. The robustness testing, in particular, is a direct application of small-scale DoE principles to verify the method's reliability against minor operational and environmental changes. A successfully validated method ensures that drugs are manufactured to the highest quality standards, safe and effective for patient use [37].
Analytical method validation research provides the foundational data that demonstrates a therapeutic product is safe, pure, potent, and consistent. Within the context of a broader thesis on analytical method validation research, this guide addresses the critical frameworks and methodologies required to characterize complex drug modalities. The biopharmaceutical landscape is undergoing a profound shift, with new modalities now accounting for an estimated $197 billion, representing 60% of the total pharma projected pipeline value as of 2025 [74]. This growth is driven by modalities including monoclonal antibodies (mAbs), antibody-drug conjugates (ADCs), bispecific antibodies (BsAbs), cell therapies, gene therapies, and nucleic acid-based therapies [74]. This expansion necessitates parallel advancements in analytical strategies to meet rising complexity and regulatory expectations, moving beyond traditional small-molecule approaches to address the unique challenges of characterizing large biomolecules, viral vectors, and genetically modified cells [75] [35].
The Evolving Landscape of Novel Modalities
The accelerating pipeline of novel modalities presents a diverse set of analytical challenges. Each modality possesses a unique and complex critical quality attribute (CQA) profile that must be thoroughly understood and controlled.
- Antibodies and Proteins: This category, including mAbs, ADCs, and BsAbs, continues to demonstrate robust growth. The clinical pipeline for mAbs remains the largest among new modalities, expanding 7% in 2025, with growth extending into neurology, rare diseases, and cardiovascular areas [74]. ADCs have seen a 40% growth in expected pipeline value over the past year, driven by new approvals [74]. The key analytical challenges for these molecules include assessing post-translational modifications, aggregation, drug-to-antibody ratio (for ADCs), and potency.
- Cell and Gene Therapies: This category shows mixed progress. While CAR-T cell therapies continue their rapid pipeline growth, other emerging cell therapies like TCR-T, TIL, and CAR-NK face challenges related to high manufacturing costs and limited adoption [74]. Gene therapy growth has stagnated somewhat due to safety concerns and regulatory scrutiny, highlighting the intensified need for robust analytical methods to characterize vector integrity, purity, and potency [75] [74].
- Nucleic Acids: Modalities such as antisense oligonucleotides (DNA/RNA) and RNAi are on a steady upward path, with projected revenue for DNA/RNA therapies up 65% year-over-year [74]. In contrast, mRNA pipeline value is declining as the pandemic wanes [74]. These therapies require methods to confirm sequence integrity, modification patterns, and purity from process-related impurities.
Table 1: Key Modalities and Associated Analytical Challenges
| Modality Category | Representative Modalities | Primary Analytical Challenges | Key CQAs |
|---|---|---|---|
| Antibodies & Proteins | mAbs, ADCs, BsAbs, Recombinant Proteins (e.g., GLP-1) | Aggregation, Charge Variants, Post-Translational Modifications, Drug-to-Antibody Ratio (DAR), Potency | Purity, Size Variants, Potency, Aggregation, Fragmentation |
| Cell Therapies | CAR-T, TCR-T, TIL, Stem Cell Therapies | Viability, Phenotype, Potency, Purity (e.g., residual vector), Transgene Expression, Cytokine Secretion | Cell Viability, Identity, Potency, Purity (microbial, vector), Vector Copy Number |
| Gene Therapies | AAV, Lentiviral Vectors, CRISPR-based platforms | Full/Empty Capsid Ratio, Genome Integrity (e.g., truncated sequences), Potency, Purity (host cell DNA/Protein) | Titer, Full/Empty Capsid Ratio, Potency, Purity, Genome Integrity |
| Nucleic Acids | ASO, RNAi, mRNA | Sequence Verification, Modification Pattern, Purity (related substances), Impurities (e.g., dsRNA) | Sequence Identity, Purity, Potency, Impurity Profile |
Regulatory Framework and Lifecycle Approach
The regulatory climate for analytical methods is evolving towards a more integrated, science-based, and lifecycle-oriented approach. Regulatory bodies enforce rigorous standards per guidelines such as ICH Q2(R1) and the forthcoming ICH Q2(R2) and Q14, which emphasize precision, robustness, and data integrity [35]. A central theme in modern validation is the Quality-by-Design (QbD) framework. QbD leverages risk-based design to develop methods aligned with a product's CQAs, using tools like Method Operational Design Ranges (MODRs) to ensure robustness across operational conditions as outlined in ICH Q8 and Q9 [35]. This represents a shift from a one-time validation event to a lifecycle management strategy, as inspired by ICH Q12, which spans method design, routine use, and continuous improvement [35]. Furthermore, the ALCOA+ framework (Attributable, Legible, Contemporaneous, Original, Accurate) is critical for data governance, requiring electronic systems with robust audit trails to ensure transparency and regulatory confidence [35].
Table 2: Core Analytical Validation Parameters and Considerations for Complex Modalities
| Validation Parameter | Traditional Small Molecule Focus | Enhanced Considerations for Complex Modalities |
|---|---|---|
| Accuracy/Recovery | Spiked recovery of analyte in matrix | Demonstrating accuracy for potency assays (e.g., cell-based bioassays); assessing impact of complex sample matrix (e.g., host cell proteins). |
| Precision | Repeatability and intermediate precision of assay | Accounting for inherent biological variability in cell-based assays; ensuring robustness across multiple product lots and operators. |
| Specificity | Discrimination from impurities and degradants | Ability to measure the active pharmaceutical ingredient (API) in the presence of related variants, product-related impurities, and process-related impurities (HCP, DNA). |
| Linearity & Range | Proportionality of response over a range | Defining the range to encompass all potential sample concentrations, from highly purified drug substance to in-process samples and potentially diluted clinical samples. |
| Robustness | Deliberate variations in method parameters | Using Design of Experiments (DoE) to systematically evaluate multiple parameters and their interactions for a robust method [35]. |
| Solution Stability | Short-term and long-term stability | Evaluating stability of the analyte in the specific biological matrix (e.g., serum, lysate) under storage and handling conditions. |
Advanced Analytical Technologies and Workflows
Addressing the complexity of novel modalities requires a toolbox of advanced orthogonal technologies. The industry is integrating sophisticated tools into GMP-ready, QC-compatible workflows to ensure product consistency, safety, and regulatory compliance [75].
- Separation and Mass Spectrometry-Based Techniques: Ultra-high-performance liquid chromatography (UHPLC) and high-resolution mass spectrometry (HRMS) provide unmatched sensitivity and throughput for characterizing complex molecules, including sequence variants, post-translational modifications, and impurity profiling [35]. Multi-attribute methods (MAM) using LC-MS platforms are increasingly adopted to monitor multiple CQAs simultaneously in biologics, streamlining analysis and reducing analytical redundancy [35].
- Techniques for Biophysical Characterization: For gene therapies, critical techniques for assessing viral vector quality include analytical ultracentrifugation (AUC) and mass photometry for determining full/empty capsid ratios [75]. These methods are vital for ensuring product potency and consistency.
- Bioassays and Potency Assays: Developing relevant, validated potency assays is a central challenge. These often involve cell-based systems that measure the biological activity of the drug product, which is a direct indicator of its efficacy. The trend is towards validating these assays for high-throughput and incorporation into real-time release testing (RTRT) paradigms where justified [35].
- Automation and Digital Transformation: Laboratory automation platforms and robotics are being deployed to eliminate human error and boost efficiency in method development and execution [35]. Furthermore, Artificial Intelligence (AI) and machine learning are being leveraged to optimize method parameters, predict equipment maintenance, and refine data interpretation, enhancing overall method reliability [35].
Orthogonal Methods for CQA Confirmation
Detailed Experimental Protocols
This section provides detailed methodologies for key analytical experiments critical for characterizing complex modalities.
Protocol for Full/Empty Capsid Ratio Determination Using AUC
Objective: To separate and quantify the relative proportions of full (genome-containing) and empty (non-genome-containing) capsids in an adeno-associated virus (AAV) sample using Analytical Ultracentrifugation (AUC). This ratio is a critical quality attribute for gene therapy products, directly impacting potency [75].
Principle: AUC separates particles based on their sedimentation velocity under a high centrifugal force. Full and empty capsids have different buoyant densities due to the presence or absence of the DNA genome, allowing for their separation and quantification.
Table 3: Research Reagent Solutions for AUC Capsid Ratio Analysis
| Item | Function / Description |
|---|---|
| AAV Sample | The gene therapy product intermediate or drug substance, properly stored and diluted. |
| Reference Buffer | Matches the formulation buffer of the sample (e.g., PBS with surfactants). Essential for the blank measurement and sample dilution. |
| Optical Cells & Centerpieces | Holds the sample and reference buffer during centrifugation. Requires meticulous cleaning and assembly. |
| Interference or Absorbance Optics | System for detecting the sedimenting boundaries of particles; absorbance at 260 nm is often used to detect DNA-containing capsids. |
Methodology:
- Sample Preparation: Dilute the AAV sample in the reference buffer to an appropriate absorbance within the linear range of the detector (typically ~0.5-1.0 AU). Ensure the sample and buffer are clarified by centrifugation to remove any aggregates or particulates.
- Cell Assembly: Load the reference buffer and the diluted sample into a double-sector centerpiece, which is then sealed with windows and assembled into an optical cell. Proper assembly is critical to prevent leakage.
- Instrument Setup: Place the assembled cell into the rotor. Program the centrifuge method:
- Temperature: 20°C (standard, but must be controlled).
- Rotor Speed: Typically 10,000 - 30,000 rpm, optimized for the specific AAV serotype to achieve clear separation.
- Data Collection: Use absorbance (260 nm) and/or interference optics. Collect scans at regular time intervals (e.g., every 2-3 minutes).
- Data Analysis: Use software (e.g., SEDFIT) to model the sedimentation data. The analysis will resolve the data into discrete sedimenting species.
- Identify the peaks corresponding to empty capsids (~60 Svedberg units for AAV8) and full capsids (~80-120 Svedberg units, depending on genome size and serotype).
- Integrate the area under each peak to calculate the relative percentage of full and empty capsids.
Protocol for Cell-Based Potency Assay (Using a Reporter Gene System)
Objective: To determine the biological activity (potency) of a gene therapy vector or a biologics product that activates a specific signaling pathway, by measuring the expression of a reporter gene.
Principle: A cell line is engineered to express a reporter gene (e.g., Luciferase, GFP) under the control of a pathway-specific response element. Successful transduction and transgene expression by the product lead to reporter protein production, which is quantified luminescently or fluorescently.
Table 4: Research Reagent Solutions for Cell-Based Potency Assay
| Item | Function / Description |
|---|---|
| Reporter Cell Line | Stably transfected cells with a pathway-specific response element driving a reporter gene (e.g., Luciferase). |
| Cell Culture Media | Standard growth medium (e.g., DMEM+10% FBS) for cell maintenance and assay execution. |
| Assay Plates | White-walled, clear-bottom 96-well plates for cell seeding and luminescence measurement. |
| Positive Control | A reference standard of the drug product with assigned potency (100% activity). |
| Luciferase Assay Reagent | Commercial kit providing cell lysis and luciferin substrate for luminescence detection. |
| Dilution Buffer | Appropriate buffer (e.g., PBS with formulation excipients) for serial dilution of test samples and standard. |
Methodology:
- Cell Seeding: Harvest reporter cells in the log phase of growth and seed them into a 96-well assay plate at a density that will reach 70-90% confluency at the time of assay readout.
- Dosing: After 24 hours, prepare a serial dilution of the test sample and the reference standard. Remove the culture medium from the cells and add the diluted samples to the wells. Include a negative control (dilution buffer only) and a blank (wells without cells).
- Incubation: Incubate the plates for a predetermined time (e.g., 24-48 hours) under standard cell culture conditions (37°C, 5% CO₂) to allow for transduction and gene expression.
- Signal Detection: Remove the dosing medium. Following the manufacturer's instructions, add the luciferase assay reagent to lyse the cells and initiate the luminescent reaction.
- Data Analysis: Measure the luminescence signal on a plate reader. Plot the relative luminescence units (RLU) against the log of the sample concentration for both the test sample and the reference standard. Use a parallel line analysis or 4-parameter logistic (4PL) curve fitting model to calculate the relative potency of the test sample compared to the reference standard.
Cell-Based Potency Assay Workflow
Effectively managing the complex matrices of biologics, gene therapies, and other novel modalities is a cornerstone of modern drug development. As the industry continues its pivot towards these sophisticated therapeutics, the role of analytical method validation research becomes increasingly critical. Success hinges on adopting a holistic, lifecycle-oriented approach that integrates QbD principles, leverages advanced orthogonal technologies like HRMS and AUC, and implements robust, fit-for-purpose bioassays. The future of analytical development will be shaped by trends such as Real-Time Release Testing (RTRT), the application of AI for data analysis and method optimization, and the creation of digital twins for in-silico validation [35]. By investing in these advanced analytical frameworks and fostering a culture of innovation and compliance, developers can navigate the intricate analytical landscape, ensure product quality, and ultimately bring safe and effective novel therapies to patients faster.
Within the framework of analytical method validation research, the generation of audit-ready documentation is not merely an administrative task; it is a fundamental pillar of quality and regulatory compliance. For researchers, scientists, and drug development professionals, the validation protocol and its subsequent report serve as the definitive record of a method's capability, reliability, and fitness for its intended purpose. These documents provide objective evidence to regulatory agencies, such as the FDA and EMA, that the analytical method consistently produces results meeting predefined acceptance criteria, thereby ensuring the safety, efficacy, and quality of pharmaceutical products. This guide details the core components and methodologies for constructing comprehensive validation protocols and reports that withstand rigorous regulatory scrutiny.
Core Components of a Validation Protocol
A robust validation protocol is a prospective plan that precisely defines the activities, acceptance criteria, and experimental design for the validation process. It acts as the blueprint for all subsequent work. The protocol must be approved prior to the initiation of any validation experiments.
- 1.0 Objective: Clearly and concisely state the purpose of the validation study, specifying the method and the analyte(s) of interest.
- 2.0 Scope: Define the boundaries of the validation, including the specific instrumentation, software, and locations (e.g., laboratory, production floor) where the method is intended for use [76].
- 3.0 Responsibilities: Outline the roles and responsibilities of all personnel involved, including the quality unit, laboratory analysts, and project management.
- 4.0 Experimental Design and Methodology: This is the core of the protocol. It must provide a detailed, step-by-step description of all experiments to be performed. The design should incorporate Quality by Design (QbD) principles, using tools like Design of Experiments (DoE) to understand method robustness thoroughly [77]. A comprehensive design covers the following key validation parameters:
- Accuracy: The protocol must detail how closeness of the measured value to the true value will be determined, typically through spike-and-recovery experiments using a placebo, or by comparison to a reference method.
- Precision: The methodology for evaluating repeatability (intra-assay) and intermediate precision (inter-assay, inter-analyst, inter-day) must be explicitly described, including the number of preparations and injections.
- Specificity: The experimental procedure must demonstrate the method's ability to unequivocally assess the analyte in the presence of potential interferents like excipients, impurities, or degradation products.
- Linearity and Range: The protocol must specify the concentration levels (typically 5-8) that will be prepared and analyzed to establish the method's linear response and the specific range over which it will be demonstrated.
- Detection Limit (LOD) and Quantitation Limit (LOQ): The specific methodology (e.g., signal-to-noise ratio, standard deviation of the response) for determining these limits must be defined.
- Robustness: The plan should indicate the deliberate, small variations in method parameters (e.g., pH, temperature, flow rate) that will be tested to evaluate the method's reliability.
- 5.0 Acceptance Criteria: Predefine scientifically justified and numerically specific acceptance criteria for every experiment described in section 4.0. These criteria must be based on regulatory guidance and product-specific requirements.
- 6.0 Deviations and Corrective Actions: Define the process for documenting, investigating, and approving any deviations from the approved protocol.
- 7.0 Data Integrity: State adherence to ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) and relevant regulations like 21 CFR Part 11 for electronic records [77].
- 8.0 Report Preparation: Specify the format and content requirements for the final validation report, which will summarize all data, outcomes, and the final conclusion.
The Validation Lifecycle: From Plan to Report
The following workflow visualizes the end-to-end process of analytical method validation, from initial planning to the final audit-ready documentation.
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of an analytical method is contingent upon the quality and consistency of the materials used in its execution. The following table details key reagents and their critical functions within a typical validation study.
Table 1: Essential Research Reagents and Materials for Analytical Method Validation
| Item | Function in Validation |
|---|---|
| Reference Standard | A highly characterized substance of known purity and identity used as the benchmark for quantifying the analyte and establishing method accuracy and linearity. |
| Chemical Reagents & Solvents | High-purity grades (e.g., HPLC, ACS) are used to prepare mobile phases, solutions, and samples. Their quality is critical for achieving baseline stability, specific retention times, and preventing interference. |
| Placebo/Blank Matrix | The formulation or biological matrix without the active analyte. It is essential for demonstrating method specificity, determining background interference, and performing accuracy (spike-and-recovery) studies. |
| System Suitability Standards | A prepared standard used to verify that the chromatographic or analytical system is performing adequately at the start of, and throughout, the validation run as per predefined criteria (e.g., precision, resolution, tailing factor). |
| Stressed Samples (Forced Degradation) | Samples of the drug substance or product that have been subjected to stress conditions (e.g., heat, light, acid, base, oxidation) to generate degradants and demonstrate the method's stability-indicating properties (specificity). |
A critical component of the validation report is the clear and structured presentation of experimental data against predefined acceptance criteria. The following table provides a template for summarizing key parameters.
Table 2: Example Summary of Validation Parameters and Acceptance Criteria
| Validation Parameter | Experimental Methodology Summary | Predefined Acceptance Criteria |
|---|---|---|
| Accuracy (Spike-and-Recovery) | Spike analyte at 3 concentration levels (e.g., 50%, 100%, 150%) into placebo matrix (n=3 per level). | Mean recovery between 98.0% - 102.0%; %RSD ≤ 2.0% per level. |
| Precision (Repeatability) | Analyze 6 independent preparations of analyte at 100% of test concentration. | %RSD of assay results ≤ 2.0%. |
| Linearity | Prepare and analyze standard solutions at 5-8 concentration levels across the specified range (e.g., 50-150%). | Correlation coefficient (r) ≥ 0.998. Residuals randomly distributed. |
| Specificity | Chromatographic analysis of blank (placebo), analyte, and samples spiked with known interferents/degradants. | No interference at the analyte retention time. Resolution from closest eluting peak > 2.0. |
| Robustness | Deliberate variations in a single parameter (e.g., flow rate ±0.1 mL/min, column temp ±2°C). | System suitability criteria are met in all varied conditions. |
Risk Management in Method Validation
Adopting a risk-based approach is a modern regulatory expectation. It ensures that validation efforts are focused on the most critical aspects of the method that impact product quality and patient safety.
Achieving documentation excellence does not conclude with the successful execution of a validation protocol. A state of audit-readiness is maintained through Continuous Process Validation (CPV), which uses real-time data to monitor the method's performance throughout its lifecycle [77]. Furthermore, the Validation Master Plan (VMP) must be reviewed and updated annually to reflect new products, processes, and regulatory changes [77]. By integrating these dynamic elements with meticulously prepared protocols and reports, organizations can create a robust, defensible, and enduring framework for analytical quality, fully prepared for the challenges of 2025 and beyond.
Advanced Lifecycle Management and Regulatory Strategy
Analytical method validation is a critical process in pharmaceutical development that confirms a test method produces reliable and reproducible data, thereby supporting consistent product quality, efficacy, and patient safety throughout the drug lifecycle [78]. It ensures that analytical methods accurately assess the identity, potency, and purity of pharmaceutical products, preventing batch-to-batch variability, regulatory rejection, and patient risk [78]. Until recently, the "minimal" or traditional approach to validation was the default for many organizations. However, the International Council for Harmonisation (ICH) Q14 guideline, entitled "Analytical Procedure Development," has officially introduced an alternative: the enhanced approach [79]. This modern framework provides a systematic way of generating knowledge as an analytical procedure evolves, marking a pivotal shift from rigid, document-centric validation to a dynamic, science-based, and lifecycle-oriented paradigm [79] [35].
This whitepaper frames this discussion within the broader context of analytical method validation research, which continuously seeks to improve the robustness, efficiency, and regulatory flexibility of the methods that underpin drug development. The audience of researchers, scientists, and drug development professionals will find that the enhanced approach is not merely a regulatory update but a strategic opportunity to deepen process understanding, facilitate continuous improvement, and accelerate market access for new therapies.
Core Principles: Traditional vs. Enhanced Approach
The Traditional (Minimal) Approach
The traditional approach, as the name implies, involves submitting a minimum amount of information acceptable to Regulatory Authorities [79]. It is characterized by its static nature, focusing on validating a fixed set of parameters—such as accuracy, precision, and specificity—at a single point in time [35]. This approach creates a rigid regulatory space that severely restricts a sponsor's ability to make analytical method updates during development and post-approval without prior regulatory submission and approval [79]. While simpler to implement and perceived as cost-effective, this rigidity can lead to inefficiencies, especially when unforeseen changes in equipment or materials necessitate method adjustments [80] [79].
The ICH Q14 Enhanced Approach
The enhanced approach, in contrast, is a holistic framework designed to build a comprehensive understanding of an analytical procedure throughout its entire lifecycle [79]. It emphasizes proactive and risk-based methodologies, shifting the focus from mere compliance to building scientific understanding [80]. The core objective is to establish a well-understood method with a defined Analytical Procedure Control Strategy, which allows for greater flexibility and more efficient management of post-approval changes [79].
The enhanced approach is built upon several key elements that differentiate it from the traditional method:
- Analytical Target Profile (ATP): A predefined objective that outlines the required quality of the analytical data, defining what the method is intended to measure [79].
- Risk Assessments: Systematic processes used to identify analytical procedure factors and operational steps with a potential impact on method performance [79].
- Proven Acceptable Ranges (PARs) and Method Operational Design Region (MODR): PARs define the range for a single parameter that delivers acceptable results, while an MODR defines the multi-dimensional space of method parameters that has been verified to produce results meeting the ATP [79]. Operating within an approved MODR allows for changes without the need for prior approval from regulatory authorities [79].
- Lifecycle Change Management Plan: A proactive strategy for managing future changes, which may include established conditions (ECs) and the use of Post-Approval Change Management Protocols [79].
The following diagram illustrates the systematic workflow and the key elements that contribute to building a robust Analytical Procedure Control Strategy within the enhanced approach.
Comparative Analysis: Minimal vs. Enhanced Approach
The choice between the minimal and enhanced approaches has significant implications for regulatory flexibility, cost, and operational efficiency throughout a product's lifecycle. The table below summarizes the key differences between the two paradigms.
Table 1: A Comparative Overview of the Traditional (Minimal) and Modern (Enhanced) Validation Approaches
| Factor | Traditional (Minimal) Approach | Modern (Enhanced) Approach |
|---|---|---|
| Core Philosophy | Reactive, document-focused [80] | Proactive, risk-based, and science-focused [80] [79] |
| Regulatory Flexibility | Rigid; changes often require prior approval [79] | Flexible; changes within MODR/PARs do not require prior approval [79] |
| Development Focus | Gathering minimum information for regulatory acceptance [79] | Systematic knowledge generation and understanding [79] |
| Data Utilization | Relies on historical data and periodic reviews [80] | Leverages real-time data and continuous monitoring for decision-making [80] [81] |
| Cost Profile | Lower initial investment, but higher potential for costly post-approval changes and delays [80] [79] | Higher initial investment in development, but lower long-term costs due to streamlined changes and reduced compliance risks [79] |
| Lifecycle Management | Static; revalidation often needed for changes [79] | Dynamic; continuous improvement is built-in, supporting easier method optimization [79] [35] |
The benefits of the enhanced approach are substantial. By establishing MODRs, sponsors can make changes within the approved parameter range without notifying regulators, significantly reducing the regulatory burden and accelerating implementation [79]. Furthermore, a well-established control strategy can reduce the need for full revalidation and allow for a more streamlined validation program by referencing existing development data [79]. This approach also encourages the use of prior knowledge to eliminate redundant studies, making it efficient and purposeful rather than merely expensive [79].
Experimental Protocols for the Enhanced Approach
Implementing the enhanced approach requires a structured methodology for experimentation and data analysis. The following protocols are central to building the knowledge base required for a robust analytical procedure.
Design of Experiments (DoE)
Objective: To systematically investigate the relationship between multiple Analytical Procedure Parameters (APPs) and the resulting performance, identifying critical parameters and their interactions.
Methodology:
- Define Scope and Objectives: Determine the goal, which is typically to identify the MODR or to establish PARs for critical method parameters [79] [35].
- Identify Factors and Responses: Select the independent variables (APPs, e.g., pH, temperature, gradient time) and the dependent variables (Critical Method Performance Characteristics, e.g., resolution, tailing factor, accuracy) based on a prior risk assessment [79].
- Select Experimental Design: Choose an appropriate statistical design, such as a Full Factorial, Fractional Factorial, or Central Composite Design, depending on the number of factors and the desired model resolution [35].
- Execute Experiments: Run the experiments in a randomized order to minimize the impact of uncontrolled variables.
- Analyze Data and Build Model: Use statistical software to perform analysis of variance (ANOVA) and generate a mathematical model (e.g., a response surface) that describes the relationship between the factors and responses [35].
- Verify the Model: Confirm the model's predictive power by running a set of verification experiments within the predicted MODR.
Establishing the Method Operational Design Region (MODR)
Objective: To define the multi-dimensional space of APPs that will consistently produce analytical results meeting the ATP criteria.
Methodology:
- Set Acceptance Limits: Define the acceptable ranges for the performance characteristics (responses) based on the ATP [79].
- Overlay Response Surfaces: Use the models from the DoE to identify the combination of factor settings where all response predictions simultaneously meet their acceptance criteria. This overlapping region is the MODR [79].
- Verify MODR Robustness: Conduct experimental testing at the edges (worst-case corners) of the MODR to confirm that method performance remains acceptable.
- Document and Justify: The MODR, its boundaries, and the supporting data are documented in the regulatory submission as part of the enhanced approach [79].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the enhanced approach relies on a foundation of robust tools and materials. The following table details key reagents, standards, and materials critical for developing and validating analytical methods, particularly in chromatographic analysis.
Table 2: Key Research Reagent Solutions for Analytical Method Development and Validation
| Item | Function / Explanation |
|---|---|
| System Suitability Standards | A mixture of analytes and related compounds used to verify that the chromatographic system is operating within specified parameters before and during analysis. |
| Pharmaceutical Reference Standards | Highly characterized materials of the drug substance and impurities with certified identity and purity. Essential for specificity, accuracy, and quantification. |
| Certified Mobile Phase Components | High-purity solvents, buffers, and additives (e.g., mass spectrometry grade) to ensure reproducibility, minimize background noise, and prevent system contamination. |
| Column Characterization Kits | A set of chemical probes used to characterize the properties (e.g., hydrophobicity, steric selectivity) of HPLC/UHPLC columns to ensure batch-to-batch consistency. |
| Stressed Samples (Forced Degradation) | Samples of the drug substance and product intentionally degraded under various conditions (e.g., heat, light, acid/base). Critical for demonstrating method specificity and stability-indicating properties. |
Implementing the Enhanced Approach: A Lifecycle Workflow
Adopting the ICH Q14 enhanced approach requires a shift in workflow from a linear process to a continuous, knowledge-driven cycle. The following diagram maps the key stages of the analytical procedure lifecycle, highlighting the iterative nature of monitoring and improvement that the enhanced approach enables.
This lifecycle management, inspired by ICH Q12 principles, ensures that the method remains fit-for-purpose [35]. As historical data is collected during the "Continuous Procedure Performance Verification" phase, it provides a feedback loop for continual improvement. This allows for method optimization based on performance trends, ensuring robustness and enabling more efficient regulatory handling of post-approval changes, potentially downgrading the reporting category of a change based on a justified lower risk [79].
The transition from traditional validation to the modern ICH Q14 enhanced approach represents a fundamental evolution in pharmaceutical analytical science. While the traditional minimal approach offers simplicity, its rigidity is ill-suited for the dynamic environment of modern drug development. In contrast, the enhanced approach, with its emphasis on proactive science, risk management, and systematic knowledge building, provides significant long-term advantages. These include unparalleled regulatory flexibility, reduced lifecycle costs, and a stronger foundation for ensuring consistent product quality.
For researchers, scientists, and drug development professionals, embracing the enhanced approach is not just about regulatory compliance; it is about building a more profound understanding of their analytical methods. This deeper knowledge empowers organizations to accelerate development, respond agilely to changes, and ultimately, deliver safe and effective medicines to patients more efficiently. As the industry advances with complex modalities and continuous manufacturing, the principles of ICH Q14 will undoubtedly become the cornerstone of robust and future-ready analytical practices.
For researchers, scientists, and drug development professionals, the lifecycle management of an analytical method is a critical, continuous process that begins long before its initial validation and extends throughout the commercial life of a pharmaceutical product. This process ensures that methods remain fit-for-purpose, providing reliable data to guarantee the identity, purity, potency, and stability of drug substances and products [37]. Framed within analytical method validation research, lifecycle management embodies a paradigm shift from a one-time validation event to a holistic approach that integrates method development, validation, and ongoing monitoring, aligning with the core thesis that data quality is inextricably linked to product quality and patient safety. This guide details the technical and regulatory framework for managing this journey, from initial development to post-approval change management.
The Lifecycle Stages: From Conception to Continuous Monitoring
The analytical method lifecycle can be systematically divided into three core stages, each with distinct activities and deliverables.
Stage 1: Analytical Method Development
The initial stage focuses on designing a method that is sensitive, specific, and robust for its intended purpose [37]. This involves a systematic approach to selecting and optimizing procedures to measure a specific critical quality attribute (CQA).
- Define Objectives: The process begins by defining the analytical method's objectives, including the specific attribute to be measured, the acceptance criteria, and the intended use of the method [37].
- Literature Review: A comprehensive literature review is conducted to identify existing methods and establish a baseline for development [37].
- Method Plan and Optimization: A detailed plan is developed, outlining the methodology, instrumentation, and experimental design. The method is then optimized by adjusting parameters such as sample preparation, mobile phase composition, column chemistry, and detector settings [37].
Stage 2: Analytical Method Validation
Method validation is the process of demonstrating, through laboratory studies, that the method meets its intended performance requirements for the analysis of the validated analyte [37]. The following table summarizes the key performance characteristics and their typical validation protocols.
Table 1: Core Components of Analytical Method Validation
| Validation Parameter | Experimental Protocol & Methodology | Objective & Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a minimum of 3 concentrations with 3 replicates each using a placebo spiked with known quantities of the analyte. Compare measured value to true value [37]. | Demonstrates the closeness of the test results to the true value. Typically requires recovery within 98-102%. |
| Precision | Perform repeatability (multiple measurements by same analyst on same day) and intermediate precision (different days, different analysts, different equipment) studies [37]. | Measures the degree of agreement among individual test results. %RSD of ≤2.0% is often acceptable for assay. |
| Specificity | Inject blank, placebo, and samples containing the analyte to demonstrate that the response is due to the analyte alone and not other components. Forced degradation studies may be used [37]. | Ensures the method can unequivocally assess the analyte in the presence of potential interferents. |
| Linearity & Range | Prepare a series of standard solutions (e.g., 5-8 concentrations) across the claimed range. Plot response vs. concentration and calculate the correlation coefficient [37]. | Demonstrates a directly proportional relationship between concentration and response. A correlation coefficient (r²) of ≥0.999 is often targeted. |
| Limit of Detection (LOD) & Quantification (LOQ) | LOD: Signal-to-Noise ratio of 3:1 or based on standard deviation of the response. LOQ: Signal-to-Noise ratio of 10:1 or based on standard deviation of the response, with demonstrated precision and accuracy [37]. | LOD is the lowest amount of analyte that can be detected. LOQ is the lowest amount that can be quantified with acceptable precision and accuracy. |
| Robustness | Deliberately introduce small, intentional variations in method parameters (e.g., pH, temperature, flow rate) and evaluate the impact on system suitability criteria [37]. | Measures the method's capacity to remain unaffected by small, deliberate variations in method parameters. |
Stage 3: Continuous Monitoring and Post-Approval Change Management
Once a method is validated and implemented, its performance must be continuously monitored during routine use. Furthermore, changes are inevitable, and a structured process is required for their management. The International Council for Harmonisation (ICH) Q12 guideline provides a framework for managing post-approval Chemistry, Manufacturing, and Controls (CMC) changes, making them more predictable and efficient [82].
- Established Conditions (ECs): ICH Q12 introduces the concept of Established Conditions, which are the legally binding elements that assure product quality. A change to an EC requires a regulatory submission [82].
- Post-Approval Change Management Protocol (PACMP): This is a proactive tool where a company can pre-plan the path for future changes. A PACMP, agreed upon with regulators, defines the supporting studies and the reporting category for a specified change, streamlining its implementation [82].
- Product Lifecycle Management (PLCM) Document: This document serves as a central repository for all ECs and their associated reporting categories, providing a clear roadmap for managing the product during its commercial life [82].
The following diagram illustrates the overarching workflow of the analytical method lifecycle, integrating the stages of development, validation, and continuous monitoring within the regulatory framework.
Diagram 1: Analytical Method Lifecycle Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and validation of robust analytical methods rely on a suite of critical reagents and instrumentation. The following table details key materials and their functions in this context.
Table 2: Key Research Reagent Solutions for Analytical Development & Validation
| Item / Reagent | Function & Role in Method Lifecycle |
|---|---|
| Reference Standards | Highly characterized substances used to confirm the identity, strength, quality, and purity of the drug substance/product. They are essential for method calibration, qualification, and validation [37]. |
| Chromatography Columns | The heart of separation techniques (HPLC, UPLC, GC). Different column chemistries (C18, HILIC, etc.) are selected and optimized to achieve the required resolution, peak shape, and specificity for the analyte [37]. |
| Mobile Phase Reagents | High-purity solvents and buffers used to elute the analyte from the chromatography column. Their composition, pH, and ionic strength are critical method parameters optimized for robustness and reproducibility [37]. |
| Mass Spectrometry (MS) Compatible Reagents | Volatile buffers and solvents (e.g., formic acid, ammonium acetate) specifically selected for methods using LC-MS, HRMS, or MS/MS detection to prevent ion suppression and instrument fouling [37]. |
| System Suitability Standards | A preparation of the analyte used to verify that the chromatographic system is adequate for the intended analysis. It is run before a batch of samples to ensure precision, resolution, and tailing factor meet predefined criteria. |
Managing Post-Approval Changes: A Protocol-Driven Workflow
When a change to an analytical method is proposed after approval, a structured process must be followed to evaluate its impact and determine the necessary regulatory actions. The ICH Q12 guideline categorizes changes based on their potential impact on product quality, which dictates the level of regulatory reporting [82]. The following diagram details this decision-making workflow.
Diagram 2: Post-Approval Change Management Protocol
The reporting categories for changes to Established Conditions are critical for regulatory strategy. The following table summarizes these categories as outlined in ICH Q12.
Table 3: Reporting Categories for Post-Approval Changes to Established Conditions (ECs) [82]
| Reporting Category | Regulatory Action & Timeline | Example Scenarios (Illustrative) |
|---|---|---|
| Prior Approval Supplement | Regulatory approval required before implementation. Review can take up to a year [82]. | Major change to the analytical procedure for a drug product's release test. |
| Changes Being Effected (CBE) | Regulatory notification (supplement) submitted, and change can be implemented 30 days after submission. | Moderate change, such as extending the analytical method's linear range following validation. |
| Changes Being Effected (CBE-0) | Regulatory notification (supplement) submitted, and change can be implemented immediately upon submission. | A change with minimal impact not requiring prior approval. |
| Annual Report | Change is documented and reported in the next annual report to the regulatory agency. | Minor change, like adjusting the needle wash sequence in an automated method. |
Effective lifecycle management of analytical methods, from development through continuous monitoring, is a foundational element of modern pharmaceutical quality systems. By adopting a structured, science-based approach that integrates robust development, rigorous validation, and a proactive, protocol-driven change management process, organizations can ensure ongoing regulatory compliance, enhance operational efficiency, and, most importantly, maintain the consistent quality, safety, and efficacy of pharmaceutical products for patients. The frameworks provided by regulatory guidelines like ICH Q12 empower manufacturers to manage post-approval changes predictably, transforming lifecycle management from a regulatory obligation into a strategic advantage.
Establishing Analytical Control Strategies and Method Operable Design Regions
The establishment of robust analytical control strategies and Method Operable Design Regions (MODR) represents a paradigm shift in pharmaceutical analysis, moving from a traditional, reactive approach to a systematic, proactive framework grounded in Analytical Quality by Design (AQbD) principles [83]. This modern approach, aligned with ICH Q14 guidelines, emphasizes deep scientific understanding and risk management throughout the entire analytical procedure lifecycle [84]. The lifecycle begins with predefined objectives, emphasizes procedure understanding and control, and supports continual improvement, ensuring that analytical methods remain fit-for-purpose from development through routine commercial use [84] [85]. This technical guide details the core components, experimental protocols, and implementation strategies for establishing scientifically sound control strategies and design regions within the broader context of analytical method validation research.
Regulatory and Conceptual Framework
ICH Q14: Minimal vs. Enhanced Approaches
The ICH Q14 guideline provides a scientific and risk-based framework for analytical procedure development, distinguishing between two fundamental approaches [84]:
The Minimal Approach: This traditional pathway requires identifying:
- Critical attributes of the drug substance/product to be tested.
- Appropriate analytical technology and instrumentation.
- Evaluation of performance characteristics (specificity, accuracy, robustness).
- A defined analytical procedure description and control strategy [84].
The Enhanced Approach: This represents a systematic, AQbD-aligned methodology that includes all elements of the minimal approach plus one or more of the following:
- Defining an Analytical Target Profile (ATP).
- Evaluating sample properties.
- Identifying critical procedure parameters via risk assessment.
- Investigating parameter ranges and interactions through uni- or multi-variate experiments.
- Establishing an analytical procedure control strategy.
- Creating a lifecycle change management plan with Established Conditions (ECs), Proven Acceptable Ranges (PARs), or MODR [84].
The enhanced approach is not a regulatory requirement but offers significant advantages in regulatory flexibility and facilitates better post-approval change management [84].
The Role of the Analytical Target Profile (ATP)
The Analytical Target Profile (ATP) forms the cornerstone of the AQbD paradigm. It is a predefined objective that outlines the quality requirements for an analytical method, including the intended purpose of the test, the attribute to be measured, and the required performance criteria [85]. The USP Validation and Verification Expert Panel defines the ATP as "the objective of the test and quality requirements, including the expected level of confidence, for the reportable result that allows the correct conclusion to be drawn regarding the attributes of the material that is being measured" [85]. Essentially, the ATP defines what the method needs to achieve, not how it should be done, making it method-independent and ensuring it is fit-for-purpose [85].
Figure 1: The Analytical QbD Workflow. This diagram outlines the systematic sequence from defining requirements to lifecycle management.
Core Components of an AQbD Framework
Analytical Target Profile (ATP) and Critical Quality Attributes (CQAs)
The process initiates with the Analytical Target Profile (ATP), which outlines the method's intended purpose, the measurement details, and the relevant performance criteria [83] [85]. For instance, the ATP for an impurity method would specify the analytes, required detection and quantification limits, and the necessary precision and accuracy. Following the ATP, Critical Quality Attributes (CQAs) are defined. These are the physical, chemical, biological, or microbiological properties or characteristics of the analytical method that must be controlled within appropriate limits to ensure the method meets the ATP [83]. Common analytical CMAs include specificity, accuracy, precision, and robustness.
Risk Assessment and Experimental Design
A systematic risk assessment is conducted to identify and prioritize Critical Method Parameters (CMPs)—the variable settings in the analytical procedure that can impact the CMAs [83]. Tools such as Fishbone (Ishikawa) diagrams and Failure Mode and Effects Analysis (FMEA) are employed to qualitatively and semi-quantitatively rank factors like mobile phase composition, column temperature, pH, and flow rate based on their potential impact on method performance [83].
Following risk assessment, Design of Experiments (DoE) is used to systematically investigate the relationship between CMPs and CMAs [83]. Unlike the traditional one-factor-at-a-time approach, DoE allows for the efficient exploration of interactions between multiple parameters. Common designs include Fractional Factorial designs for screening a large number of factors and Box-Behnken or Central Composite designs for response surface modeling and optimization [83] [72].
Design Space and Method Operable Design Region (MODR)
The knowledge gained from DoE studies is used to build a mathematical model and define the Design Space (DS). The DS is the multidimensional combination and interaction of CMPs that have been demonstrated to provide assurance of quality [83]. The Method Operable Design Region (MODR) is the region within the DS that produces the intended values for the CMAs, ensuring the method is robust and fit for its intended purpose [84] [83]. It represents the proven acceptable ranges for multiple variables within which the analytical procedure performs as expected without the need for any adjustment [84].
Table 1: Core Validation Parameters and Their Role in AQbD
| Validation Parameter | Traditional Role (ICH Q2) | Enhanced Role in AQbD |
|---|---|---|
| Specificity | Confirm method can distinguish analyte from impurities [78] | A foundational CMA; demonstrated across the MODR [83] |
| Accuracy & Precision | Measure closeness and variability of results [78] | Performance criteria defined in the ATP; verified throughout the MODR [83] [85] |
| Linearity & Range | Establish proportionality of response to concentration [78] | Used to define the MODR for the concentration axis [83] |
| Robustness | Often a late-stage study [78] | Integral to defining MODR boundaries via DoE; systematic assessment of CMPs [84] [83] |
Experimental Protocols for MODR Establishment
Protocol for Factor Screening and DoE
Objective: To identify Critical Method Parameters (CMPs) and model their effect on Critical Method Attributes (CMAs) for a novel RP-HPLC method for a synthetic mixture [72].
Materials & Reagents:
- Instrument: Agilent HPLC (Infinity 1200) with UV-VIS detector and Phenomenex ODS C18 column [72].
- Chemicals: Active ingredients, Methanol (HPLC grade), Potassium Phosphate Buffer (HPLC grade) [72].
- Software: Design Expert 10.0 for experimental design and data analysis [72].
Methodology:
- Define CMPs and CMAs: Based on prior knowledge and risk assessment, CMPs (e.g., buffer pH, organic phase %, flow rate) and CMAs (e.g., retention time, resolution, peak tailing) are selected [72].
- Design Experiment: A three-factorial design (e.g., Box-Behnken) is selected using software, generating a set of experimental runs (e.g., 17-27) [72].
- Execute Experiments: Prepare standard solutions and perform all chromatographic runs as per the experimental design matrix.
- Data Analysis:
- Visualization: Construct 2D contour plots and 3D response surface plots to visualize the interaction effects of factors on the responses and identify the optimal region [72].
Protocol for MODR Visualization and Control Strategy
Objective: To define the MODR and establish the associated control strategy from the DoE data.
Methodology:
- Set Suitability Criteria: Define the acceptable limits for each CMA (e.g., Resolution > 2, retention time within a specific range) based on the ATP [84] [72].
- Generate MODR Graphically:
- Establish Control Strategy: The control strategy is built on the statistical knowledge from the MODR. This includes:
Figure 2: Process for Defining the MODR. This chart shows the data-driven process from experimental data to a defined operational region.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Reagents for AQbD Experiments
| Item | Function / Purpose | Example from Literature |
|---|---|---|
| HPLC/UPLC System with Diode Array Detector | High-resolution separation and quantification of analytes; essential for generating DoE data. | Agilent HPLC (Infinity 1200) with UV-VIS detector [72] |
| C18 Reverse Phase Chromatography Column | The stationary phase for analyte separation; a critical source of variability. | Phenomenex ODS C18 column (250 x 4.6 mm) [72] |
| HPLC Grade Solvents & Buffers | Mobile phase components; purity is critical for baseline stability and reproducible retention times. | Methanol, Potassium Phosphate Buffer [72] |
| pH Meter | Accurate preparation of buffer solutions, a CMP in most chromatographic methods. | Labman LMPH 10 pH meter [72] |
| DoE & Statistical Analysis Software | Designing experiments, modeling data, generating response surfaces, and defining the MODR. | Design Expert 10.0 [72] |
| Method Development & Management Software | Streamlining development, documenting decisions, modeling, and visualizing MODR (e.g., resolution maps). | AutoChrom [84] |
The analytical method and its MODR are not standalone elements; they are integral components of the broader pharmaceutical control strategy. A control strategy is a planned set of controls, derived from current product and process understanding, that ensures process performance and product quality [85]. These controls can include:
- Input Material Controls: Raw material and reagent specifications.
- Procedural Controls: The defined analytical procedure itself.
- In-Process Controls: Tests performed during manufacturing.
- Lot Release Tests: Such as drug substance and drug product specifications [85].
The specification limits for a CQA are directly linked to the capability of the analytical method. The method's measurement uncertainty must be sufficiently controlled to ensure the reportable result is reliable for making a pass/fail decision against the specification [85]. In an AQbD framework, specification limits should be based on safety, efficacy, and process understanding across the entire design space, rather than solely on historical batch data from a narrow operating range [85]. This ensures the analytical method, with its defined MODR, remains fit-for-purpose across the entire operational range of the manufacturing process.
Lifecycle Management and Regulatory Flexibility
A principal advantage of implementing an AQbD approach for analytical methods is enhanced lifecycle management. The deep understanding gained from defining the MODR allows for more predictable and manageable post-approval changes [84] [83]. Regulatory flexibility is increased because changes within the approved MODR are not considered as major variations, as the method's performance has already been proven across this region [84] [83]. This facilitates continuous improvement,
allowing for method adjustments and optimization without the need for extensive revalidation, provided the method remains within the MODR and continues to meet the ATP [83]. This proactive, science-based management of the analytical procedure lifecycle minimizes the occurrence of out-of-trend (OOT) and out-of-specification (OOS) results, ensuring ongoing product quality and regulatory compliance [84] [83].
The pharmaceutical product lifecycle extends far beyond initial regulatory approval. Post-approval changes are inevitable and necessary for continuous improvement, supply reliability, and compliance with evolving regulations. These changes can include modifications to manufacturing processes, batch sizes, analytical methods, and supply chains. However, implementing such changes requires a careful, systematic approach to risk assessment and regulatory compliance to ensure that product quality, safety, and efficacy remain unaffected. Within the broader context of analytical method validation research, understanding how to manage these changes is critical for maintaining product control throughout its commercial life. This guide provides a comprehensive technical framework for assessing risks and navigating global regulatory submission pathways for post-approval changes, with a particular focus on analytical procedures.
Regulatory Framework for Post-Approval Changes
Global Guidelines and Harmonization Efforts
The International Council for Harmonisation (ICH) has developed guidelines to provide a structured framework for managing post-approval changes. ICH Q12, "Technical and Regulatory Considerations for Pharmaceutical Product Lifecycle Management," is pivotal in this landscape. It introduces concepts designed to facilitate more predictable and efficient management of Chemistry, Manufacturing, and Controls (CMC) changes [86]. The guideline aims to harmonize the classification and reporting of post-approval changes across regions, though full implementation varies.
- Established Conditions (ECs): ICH Q12 defines ECs as the legally binding, critical elements of a product's manufacturing process and quality control strategy that require regulatory oversight if changed. A clear understanding of ECs helps manufacturers and regulators distinguish between changes that necessitate regulatory action and those that can be managed within the company's Pharmaceutical Quality System (PQS) [86] [87].
- Post-Approval Change Management Protocols (PACMPs): These are prospective, approved plans that outline the data and justification needed to support a future change. Using a PACMP can reduce the regulatory reporting category for a change, enabling faster implementation [86] [87].
- Product Lifecycle Management (PLCM) Document: This document contains the agreed-upon ECs and their reporting categories for a specific product, serving as a reference for managing post-approval changes [86].
Despite these harmonization efforts, significant challenges remain. The time required for global approval of a single change can take years due to differing regional requirements, forcing manufacturers to maintain parallel processes and inventory [86]. Furthermore, a recent analysis of commercial products found that over half of all changes were regulatory-relevant, and among those, 43% (approximately 38,700 variations) were related to analytical procedures, highlighting the significant burden associated with method changes [87].
Health Authority-Specific Requirements
While ICH provides a framework, individual health authorities have specific regulations and interpretations.
- U.S. Food and Drug Administration (FDA): The FDA has issued draft guidance on ICH Q12 implementation and has run a pilot program for Established Conditions [86]. The FDA also employs Risk Evaluation and Mitigation Strategies (REMS) for certain medications with serious safety concerns, which can impose specific requirements that interact with post-approval change processes [88].
- European Medicines Agency (EMA): The EU currently operates within its existing variations regulation and does not formally recognize the PLCM document, though it does acknowledge PACMPs [86].
- Other Regions: Japan's PMDA, China's NMPA, and Health Canada are at various stages of implementing ICH Q12 and Q14, each with unique regional nuances that must be considered for global submissions [86].
Table 1: Key Regulatory Guidelines for Post-Approval Changes
| Guideline / Concept | Issuing Body | Primary Focus | Key Tool |
|---|---|---|---|
| ICH Q12 | ICH | Pharmaceutical Product Lifecycle Management | Established Conditions (ECs), PACMPs |
| ICH Q14 | ICH | Analytical Procedure Development | Analytical Target Profile (ATP) |
| ICH Q2(R2) | ICH | Validation of Analytical Procedures | Validation Parameters (Accuracy, Precision, etc.) |
| REMS | FDA | Drug Safety for High-Risk Products | Medication Guides, Communication Plans |
Risk Assessment of Post-Approval Changes
A science- and risk-based assessment is the cornerstone of effective post-approval change management. The goal is to evaluate the potential impact of a proposed change on the product's Critical Quality Attributes (CQAs), which are physical, chemical, biological, or microbiological properties or characteristics that should be within an appropriate limit, range, or distribution to ensure the desired product quality.
Risk Assessment Methodology
The risk assessment process for a post-approval change, particularly for an analytical procedure, involves a systematic evaluation of several factors [87]:
- Complexity of the Test: Is the test a simple identity check or a complex potency assay for a biologic?
- Extent of the Modification: Is it a minor adjustment (e.g., mobile phase pH modification) or a major change (e.g., replacement of the analytical technology)?
- Relevance to Product Quality: How directly does the analytical procedure measure a CQA? A change to a dissolution test for a solid oral dosage form (a CQA) would be higher risk than a change to a residual solvent test method.
Based on this assessment, changes are classified as high-, medium-, or low-risk. This classification directly influences the depth of required validation data and the regulatory reporting pathway [87].
Applying Risk Assessment to Analytical Procedure Changes
The ICH Q14 guideline emphasizes a risk-based approach for managing analytical procedure changes. The diagram below illustrates the logical workflow for assessing and implementing a change.
Change Management Workflow for Analytical Procedures
This process ensures that the level of effort and regulatory scrutiny is commensurate with the potential risk to product quality. A key output of this risk assessment is the determination of whether the change can be managed within the PQS or requires regulatory notification or prior approval.
Analytical Method Validation in Change Management
When a post-approval change involves an analytical procedure, demonstrating that the modified method remains fit-for-purpose is paramount. This is achieved through method validation, the process of proving that an analytical method is suitable for its intended use [37].
Core Validation Parameters
According to ICH Q2(R2), validation of analytical procedures involves testing several performance characteristics [9] [37] [7]. The specific parameters tested depend on the type of analytical procedure (e.g., identification, impurity testing, assay).
Table 2: Analytical Method Validation Parameters and Definitions
| Validation Parameter | Definition | Role in Change Management |
|---|---|---|
| Accuracy | The closeness of agreement between a measured value and a true or accepted reference value. | Confirms the changed method recovers the true value without bias. |
| Precision | The closeness of agreement between a series of measurements. Includes repeatability and intermediate precision. | Ensures the changed method produces reproducible results. |
| Specificity | The ability to assess the analyte unequivocally in the presence of other components. | Demonstrates the changed method can distinguish the analyte from interferences. |
| Linearity | The ability of the method to obtain test results proportional to the concentration of the analyte. | Verifies the analytical range remains valid post-change. |
| Range | The interval between the upper and lower concentrations of analyte for which the method has suitable precision, accuracy, and linearity. | Confirms the operating range is unaffected. |
| Limit of Detection (LOD) | The lowest amount of analyte that can be detected, but not necessarily quantified. | Critical for impurity methods; ensures sensitivity is maintained. |
| Limit of Quantitation (LOQ) | The lowest amount of analyte that can be quantitatively determined. | Critical for impurity methods; ensures quantitation capability is maintained. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters. | Evaluates the method's reliability under normal operational variations. |
The Role of the Analytical Target Profile (ATP)
ICH Q14 introduces the Analytical Target Profile (ATP) as a central concept. The ATP is a predefined set of performance criteria that a method must achieve to be fit for its intended purpose [87]. When managing a method change, the ATP serves as the benchmark against which the modified method's validation data is compared. This shifts the focus from simply replicating the old method's parameters to demonstrating that the new method meets the same predefined quality criteria.
Bridging Studies
A critical component of analytical method changes is the bridging study. These studies are designed to directly compare the original (or currently approved) method and the modified method by testing the same set of representative samples [87]. The objective is to generate data demonstrating that the new method is equivalent or superior to the original method and that the change has no adverse impact on the ability to control product quality. The design of these studies—including the number of batches, sample types, and statistical approaches—should be justified based on the risk level of the change.
Experimental Protocols for Key Analytical Changes
This section provides detailed methodologies for common analytical procedure change scenarios, incorporating the principles of risk assessment and validation.
Protocol 1: Changing Chromatography Column Chemistry
Objective: To validate an analytical procedure after a change from a C18 (USP L1) column to another C18 column from a different vendor due to supply chain constraints.
Workflow:
- Risk Assessment: Classified as Low to Medium Risk. Justification: The column chemistry is similar, and the method is for assay with known impurity profiles that do not co-elute with the main peak.
- Experimental Design:
- System Suitability: Verify that the new column meets all system suitability criteria of the original method (theoretical plates, tailing factor, resolution from a known impurity).
- Comparative Analysis: Analyze a minimum of three batches of drug product (covering low, medium, and high potency, if available) using both the original and new columns.
- Validation Parameters: Focus on precision (repeatability with 6 injections of a single preparation) and accuracy (via spike recovery studies if applicable).
- Statistical Analysis: Perform a statistical comparison (e.g., student's t-test) of the assay results from both methods. The results should show no significant difference at a 95% confidence level.
- Regulatory Reporting: Based on the risk assessment and with prior regulatory agreement (e.g., via an EC), this change may be managed as a low-risk notification [87].
Protocol 2: Implementing a New Analytical Technology
Objective: To replace an HPLC-based assay with a UPLC-based method for improved efficiency and reduced solvent consumption.
Workflow:
- Risk Assessment: Classified as Medium Risk. Justification: The fundamental principle (reversed-phase chromatography) remains the same, but operating parameters and instrumentation change.
- Experimental Design:
- Method Optimization: Adjust parameters like flow rate, gradient profile, and injection volume to achieve optimal separation on the UPLC system.
- Full Validation: Since this is considered a new procedure, a full validation according to ICH Q2(R2) is required. This includes assessing accuracy, precision, specificity, linearity, and range [37] [7].
- Bridging Study: Conduct a comprehensive comparison using a statistically significant number of batches (e.g., 5-10) representing the entire product shelf-life. Generate a correlation plot and calculate R² to demonstrate equivalence.
- Robustness Testing: Evaluate the impact of small variations in column temperature, mobile phase pH, and flow rate on the UPLC method's performance.
- Regulatory Reporting: This change typically requires a prior-approval supplement unless a PACMP was approved in advance, which could lower the reporting category [87].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of post-approval change protocols relies on high-quality materials and reagents. The table below details key items used in the experiments described in this guide.
Table 3: Key Research Reagents and Materials for Analytical Change Management
| Item | Function / Application | Criticality in Change Management |
|---|---|---|
| Chemical Reference Standards | Highly characterized substances used to confirm identity, potency, and purity of the analyte. | Serves as the benchmark for all comparative (bridging) studies and validation experiments. |
| System Suitability Test Mixtures | A preparation containing the analyte and key known impurities or degradation products. | Verifies that the chromatographic system (pre- and post-change) is capable of providing data of acceptable quality. |
| Certified Chromatography Columns | Columns with documented performance characteristics from the vendor. | Ensures reproducibility and reliability of separation methods during method transfer and changes. |
| Mass Spectrometry-Grade Solvents | High-purity solvents for LC-MS and other sensitive techniques. | Minimizes background noise and interference, crucial for maintaining method specificity and LOD/LOQ. |
| Stable Isotope-Labeled Internal Standards | Used in bioanalytical and impurity methods to correct for analyte loss during sample preparation. | Essential for ensuring the accuracy and precision of quantitative methods, especially after a change. |
Regulatory Submission Strategies
Once the risk assessment and experimental work are complete, the data must be compiled and submitted to the relevant health authorities according to the appropriate pathway.
Submission Pathways and Data Requirements
The submission pathway is determined by the risk classification of the change.
- Prior-Approval Supplement: Required for high-risk changes that have a substantial potential to adversely affect product quality. Implementation of the change cannot occur until regulatory approval is received. Example: Changing the synthesis route of a drug substance [89].
- Changes Being Effected (CBE) Supplement: For moderate-risk changes, which can be further subdivided:
- CBE-30: The supplement is submitted, and the change can be implemented 30 days after the FDA receives it.
- CBE-0: The change can be implemented immediately upon supplement submission.
- Annual Report: For low-risk changes that have a minimal potential to impact product quality. These changes are documented in an annual report submitted to the FDA.
The data package for a submission should include a summary of the change, the risk assessment, a description of the studies conducted, the complete validation report, data from bridging studies, and a conclusion demonstrating that the modified method meets the ATP and poses no adverse impact to product quality.
Leveraging ICH Q12 Tools for Efficient Submissions
To streamline the submission and approval process, manufacturers should proactively utilize ICH Q12 tools.
- Utilize PACMPs: For a known future change, submitting a PACMP as part of the original marketing application can allow for a lower reporting category (e.g., annual reportable) when the change is eventually executed, significantly reducing the regulatory burden and time to implementation [86] [87].
- Reference the PLCM Document: For products with an approved PLCM document, the agreed-upon ECs and reporting categories provide a clear roadmap. A change that does not affect an EC can often be managed within the PQS without a regulatory submission [86].
The following diagram illustrates the interconnected nature of these tools and concepts in an efficient post-approval change management system.
Integrated Change Management System
Managing post-approval changes through robust risk assessment and strategic regulatory submissions is a complex but essential discipline in the pharmaceutical industry. The advent of ICH Q12 and Q14 provides a more harmonized, science-based framework that emphasizes proactive planning and risk-based decision-making. By deeply understanding and applying concepts like Established Conditions, Post-Approval Change Management Protocols, and the Analytical Target Profile, organizations can navigate the global regulatory landscape more efficiently. This ensures that necessary improvements can be implemented rapidly, maintaining a reliable supply of high-quality medicines to patients while upholding the strictest standards of regulatory compliance. As the regulatory environment continues to evolve, a commitment to continual improvement and early, strategic engagement with health authorities will be key to successful product lifecycle management.
Analytical method transfer is a critical, documented process that qualifies a receiving laboratory (RL) to perform a validated analytical method transferred from a sending laboratory (TL) [90]. This procedure is fundamental to the pharmaceutical industry and drug development, ensuring that analytical methods remain reproducible and robust when relocated to a different site, thereby guaranteeing the consistency and quality of products and stability data [91] [92]. The core objective is to demonstrate that the receiving laboratory can generate results equivalent to those from the original laboratory, thus upholding data integrity and compliance with regulatory standards [90].
Within the broader context of analytical method validation research, method transfer acts as a practical confirmation of a method's inter-laboratory precision, or reproducibility—a key validation parameter [91] [90]. It bridges the gap between initial method validation and routine application across different geographical and operational environments.
Foundational Concepts and Regulatory Framework
Key Definitions and Responsibilities
A successful transfer hinges on the clear definition of roles and responsibilities for both the sending and receiving laboratories [91] [90].
Transferring Laboratory (TL) Responsibilities: The TL, as the method originator, is responsible for providing the RL with a comprehensive transfer package. This includes the analytical procedure, method validation report, known method performance issues, sample chromatograms, and details on reference standards [91] [90]. Crucially, the TL must also facilitate training and maintain open communication with the RL to transfer tacit knowledge not captured in written documentation [91].
Receiving Laboratory (RL) Responsibilities: The RL must evaluate the received documentation, prepare and approve the transfer protocol and report, ensure personnel are trained, and execute the transfer study [90]. Furthermore, the RL is responsible for having the necessary qualified equipment and materials to perform the method [90].
Inter-Laboratory Comparisons and Proficiency Testing
Inter-laboratory comparisons (ILCs) are systematic exercises used to assess laboratory performance [93]. In regulated industries, these are often formalized as proficiency testing, which provides evidence of a laboratory's technical competence [93]. The statistical assessment often involves criteria like the normalized error (|Ei|), which should be ≤1 for a passing result, though more advanced probability-based criteria are also employed to ensure rigorous comparison [94].
Approaches to Method Transfer
The United States Pharmacopeia (USP) <1224> outlines several formal approaches for method transfer, each suited to different circumstances [92].
The following diagram illustrates the decision-making workflow for selecting the appropriate transfer strategy.
Comparative Testing
This is the most frequently used strategy [91] [90]. It involves both the TL and RL testing the same set of samples, typically from the same lot, and comparing the results against pre-defined acceptance criteria [91] [90]. This approach is ideal for methods that have already been validated.
Co-validation
In this model, the receiving laboratory participates in the method validation process, particularly the reproducibility study, while the method is still under development [91] [92]. This is suitable for transfers from a development site to a commercial site before validation is complete [91].
Revalidation or Partial Revalidation
This approach is necessary when the original sending laboratory is not available for comparison, or when the original validation did not meet current ICH requirements [91]. The RL performs a full or partial revalidation, focusing on parameters that might be affected by the transfer [91].
Transfer Waivers
In specific, justified cases, a formal method transfer can be waived. Common scenarios include the use of straightforward pharmacopoeial methods (which require verification, not transfer), or when the method is applied to a new product strength with only minor changes [91].
The Method Transfer Protocol: A Step-by-Step Workflow
A meticulously planned and executed workflow is fundamental to a successful analytical method transfer. The process is highly collaborative and document-intensive.
Step 1: Initiate Transfer and Share Knowledge
The process begins with the TL compiling and providing all relevant method knowledge to the RL [91] [90]. This includes the analytical procedure, validation reports, and any "tacit knowledge" or practical tips not found in the official documentation [91]. A kick-off meeting is highly recommended to introduce teams and discuss the method in detail [91].
Step 2: Develop and Approve the Transfer Protocol
The transfer protocol is the master document that governs the entire process. It is typically prepared by the RL or TL and must be approved by both laboratories, as well as the Quality Assurance (QA) unit [91] [90]. A robust protocol includes the elements shown in the table below.
Table: Essential Components of a Method Transfer Protocol
| Component | Description |
|---|---|
| Objective & Scope | Clearly defines the purpose and boundaries of the transfer [91]. |
| Responsibilities | Outlines the roles and tasks for TL, RL, and QA [91]. |
| Analytical Procedure | The exact method to be transferred [91]. |
| Experimental Design | Specifies the number of samples, replicates, and lots to be tested [91] [90]. |
| Acceptance Criteria | Pre-defined, statistically justified criteria for success for each test parameter [91]. |
| Deviations Management | Procedure for handling and documenting any deviations from the protocol [91]. |
Step 3: Training and Familiarization
If the method is complex, on-site training at the RL by TL experts may be necessary [91]. This familiarization period allows the RL to run the method as written and ensure they can meet its requirements before the formal study begins [90].
Step 4: Execute the Experimental Study
The RL (and TL, in a comparative transfer) performs the analytical testing as stipulated in the protocol. This involves testing a pre-determined number of samples, often with replication, to generate a robust data set for comparison [91] [90].
Step 5: Analyze Data and Prepare the Transfer Report
The collected data is statistically analyzed against the protocol's acceptance criteria [91]. A final transfer report is prepared, which includes all raw data, a comparison of results, and a conclusion on whether the transfer was successful [91] [90]. The report must also justify any deviations from the protocol [91].
Step 6: Close-Out and Implement Method
Upon successful completion, the method is formally released for routine use at the receiving laboratory. All records are archived according to data integrity policies [90].
Defining Acceptance Criteria and Statistical Evaluation
Setting scientifically sound and justified acceptance criteria is arguably the most critical element of the transfer protocol. These criteria are typically based on the method's validation data and its intended use [91].
Table: Typical Acceptance Criteria for Common Analytical Tests
| Test | Typical Acceptance Criteria |
|---|---|
| Identification | Positive (or negative) identification obtained at the receiving site [91]. |
| Assay | Absolute difference between the results from the two sites is not more than 2-3% [91]. |
| Related Substances | Criteria vary with impurity level. For low levels, recovery of 80-120% for spiked impurities may be used. For higher levels (e.g., >0.5%), absolute difference criteria are applied [91]. |
| Dissolution | Absolute difference in mean results is not more than 10% at time points with <85% dissolved, and not more than 5% at time points with >85% dissolved [91]. |
The statistical evaluation often involves calculating the relative standard deviation (RSD), confidence intervals, and the difference between the mean values obtained by each laboratory [91]. For complex methods, statistical equivalence tests may be employed [90].
Case Study: Inter-Laboratory Transfer of a Cell-Based Bioassay
A 2024 study on transferring a microneutralization (MN) assay for anti-AAV9 neutralizing antibodies provides a robust example of a successful, complex method transfer [95].
Experimental Protocol and Workflow
The method was transferred from a leading laboratory to two other research teams. The protocol involved:
- Sample Pre-treatment: Serum or plasma samples were heat-inactivated at 56°C for 30 minutes [95].
- Virus Neutralization: Serial two-fold dilutions of samples were incubated with a recombinant AAV9 vector for 1 hour at 37°C [95].
- Cell Culture Inoculation: The virus-antibody mixture was added to susceptible HEK293 cells and incubated for 48-72 hours [95].
- Signal Detection: Gaussian luciferase activity in the supernatant was measured as the readout for viral transduction [95].
- Data Analysis: The 50% inhibitory concentration (IC50) titer was calculated using four-parameter logistic (4PL) regression [95].
The following diagram details the experimental workflow.
Research Reagent Solutions and Key Materials
The successful transfer and execution of this complex bioassay relied on several critical reagents and materials.
Table: Essential Research Reagents for the Anti-AAV9 Microneutralization Assay
| Reagent/Material | Function in the Assay |
|---|---|
| rAAV9-EGFP-2A-Gluc Vector | Recombinant virus serving as the assay target; encodes Gaussian luciferase reporter for detection [95]. |
| HEK293-C340 Cell Line | Susceptible host cells for viral transduction; a qualified cell bank is essential for consistency [95]. |
| Gaussian Luciferase Substrate (Coelenterazine) | Enzyme substrate that produces a luminescent signal proportional to viral transduction [95]. |
| Mouse Neutralizing Monoclonal Antibody | System suitability control; used to monitor inter-assay precision and validate assay performance [95]. |
| Pooled Human Negative Serum | Matrix for preparing sample dilutions and controls, ensuring the assay is performed in a biologically relevant environment [95]. |
Outcomes and Performance Metrics
The transfer was deemed successful, demonstrating excellent reproducibility. The intra-laboratory variation (precision) for low positive controls was 7-35%, and the inter-laboratory variation was 23-46% for blinded human samples, which was within the pre-defined acceptance criteria (%GCV <50%) [95]. This highlights the power of a well-designed transfer study.
A successful analytical method transfer is a cornerstone of ensuring data reliability and product quality in a multi-laboratory environment. It is not merely an administrative task but a rigorous scientific exercise that confirms a method's reproducibility—a key validation parameter. The process demands meticulous planning, open communication, and robust documentation [91]. By adhering to structured protocols, employing scientifically justified acceptance criteria, and fostering collaboration between laboratories, organizations can ensure that analytical methods perform consistently and reliably, thereby supporting the integrity of the drug development process and the safety of medicinal products.
The landscape of analytical method validation is undergoing a fundamental transformation, driven by the convergence of artificial intelligence, real-time release testing (RTRT), and comprehensive digitalization. This evolution moves the field beyond traditional, discrete laboratory tests toward continuous, data-driven assurance of product quality. Within pharmaceutical development, this shift is enabling unprecedented levels of efficiency, precision, and agility. Analytical method validation now encompasses the verification of not only classical analytical procedures but also sophisticated AI algorithms and continuous monitoring systems that form the backbone of modern quality control strategies [96].
This transformation is particularly evident in the life sciences sector, where digitalization is streamlining operations from drug discovery to commercial manufacturing [97]. The integration of Artificial Intelligence and machine learning is substantially accelerating drug discovery processes, with AI-driven drug discovery alliances increasing dramatically from merely 10 in 2015 to over 105 by 2021 [97]. Furthermore, the adoption of advanced frameworks like Pharma 4.0, characterized by connectivity, automation, and real-time analytics, is creating agile and efficient production environments where RTRT becomes a feasible and valuable component of the quality system [97].
Table 1: Quantitative Impact of Digital Transformation in Pharma (2025 Outlook)
| Area | Key Technology | Projected Impact/Value |
|---|---|---|
| Drug Discovery | AI & Machine Learning | Adds $350–$410 billion in annual value to the pharma sector [97] |
| Functional Testing | AI-Powered Test Automation | 70% faster test creation, 85% reduction in maintenance costs [98] |
| Clinical Trials | Decentralized Clinical Trials (DCTs) & AI | Increased patient participation and diversity; significant timeline and cost reduction [97] |
| Manufacturing | IoT, Robotics, Advanced Analytics | Predictive maintenance reduces downtime and improves production consistency [97] |
The Role of AI and Machine Learning in Analytical Validation
Artificial Intelligence is redefining the capabilities and scope of analytical method validation. AI's primary value lies in its ability to learn from complex datasets, predict outcomes, and autonomously adapt to new information, thereby creating more robust and intelligent validation protocols.
Agentic AI and Autonomous Validation Systems
A leading trend is the move from AI-assisted to Agentic AI systems. These systems operate with significant autonomy, handling complex tasks that previously required constant human intervention. In the context of analytical method validation, an Agentic AI could manage the entire lifecycle of a method [99].
For example, it could autonomously:
- Prioritize validation activities based on risk assessment of new product or process changes.
- Dynamically execute a validation protocol across different instrument platforms and conditions.
- Analyze results in real-time, classifying any deviations based on severity and identifying root causes.
- Maintain the validated state by continuously learning from new data and triggering re-validation only when necessary [99].
This represents a shift toward continuous validation, a concept that aligns perfectly with the goals of real-time release testing.
AI for Enhanced Testing and Quality Control
AI's application extends to specific testing functions that support RTRT. Modern AI test automation tools demonstrate capabilities that are directly transferable to analytical method development and execution.
Table 2: AI Testing Capabilities with Applications to Analytical Method Validation
| AI Capability | Description | Application in Analytical Validation |
|---|---|---|
| Self-Healing Tests [100] [98] | AI automatically adapts test scripts when underlying systems or UIs change, reducing maintenance by up to 85% [98]. | An analytical method could automatically compensate for minor, predictable changes in detector performance or mobile phase composition, maintaining its validity without manual re-calibration. |
| Predictive Analytics [100] | Machine learning models analyze historical defect patterns and code commits to flag risks with high accuracy. | Predict potential method failures or out-of-specification (OOS) results by analyzing process analytical technology (PAT) data trends, enabling proactive intervention. |
| Visual Validation [100] [101] | Computer vision AI validates UI consistency across browsers and resolutions, ignoring benign changes. | Automatically compare chromatogram peaks or spectroscopic readouts against a baseline, intelligently distinguishing between significant anomalies and acceptable noise. |
| Intent-Driven Testing [98] | The system understands the user's goal (the "what") and autonomously generates the necessary steps to achieve it (the "how"). | A scientist could describe the desired analytical outcome, and the AI would design and optimize the experimental protocol to meet predefined acceptance criteria. |
Real-Time Release Testing: Methodology and Implementation
Real-Time Release Testing (RTRT) is a quality assurance framework where the quality of a product batch is assessed based on process data collected throughout manufacturing, rather than solely through laboratory testing on collected samples. This approach is a cornerstone of the FDA's Process Analytical Technology (PAT) initiative and is enabled by a suite of digital technologies.
Core Principles and Regulatory Basis
RTRT relies on the principle that quality should be built into the product, not tested into it. It involves:
- At-line, On-line, or In-line Measurements: Using PAT tools to measure critical quality attributes (CQAs) during the manufacturing process.
- Multivariate Data Analysis: Employing models to understand the complex relationships between process parameters and product CQAs.
- Process Control: Using the data and models in real-time to ensure the process remains within a state of control.
Regulatory bodies support this approach. The FDA and EMA have frameworks encouraging the use of continuous verification and real-time monitoring. The revised ICH E6(R3) Good Clinical Practice guideline, effective July 2025, further shifts trial oversight toward risk-based, decentralized models, which aligns with the philosophy of RTRT [102].
Enabling Technologies and Experimental Protocols
The implementation of RTRT is feasible only through the integration of several advanced technologies.
Table 3: Essential Research Reagent Solutions for RTRT and AI-Driven Development
| Item / Technology | Function in RTRT & AI Validation |
|---|---|
| Process Analytical Technology (PAT) Probes (e.g., NIR, Raman spectrometers) | Provide continuous, non-destructive measurement of CQAs (e.g., concentration, moisture content, polymorphic form) directly in the process stream. |
| Digital Twins [97] [103] | A virtual replica of the process used to simulate outcomes, test control strategies, and predict product quality without disrupting actual production. |
| AI/ML Modeling Platforms (e.g., TensorFlow, PyTorch in GxP systems) | Develop and validate predictive models that correlate process data (from PAT) with final product quality, forming the core algorithm for RTRT. |
| Structured Data Management Systems (e.g., SPOR [96]) | Ensure data is machine-readable and standardized, which is a prerequisite for training reliable AI models and for regulatory submission of data-rich dossiers. |
| IoT Sensors and Edge Computing [97] | Collect high-volume process data (temperature, pressure, flow rate) and perform initial data processing at the source for low-latency feedback control. |
Detailed Experimental Protocol: Validating an AI Model for RTRT
This protocol outlines the key steps for establishing and validating an AI-based predictive model as the primary method for releasing a product batch, in accordance with regulatory expectations for AI credibility [102].
Objective: To develop, train, and validate a machine learning model that predicts a Critical Quality Attribute (e.g., dissolution rate) based on real-time process data, for use in a Real-Time Release Testing strategy.
Materials:
- Historical manufacturing data (process parameters, PAT data) with corresponding lab results for the CQA.
- Data from at least 10-15 representative commercial-scale batches.
- GxP-compliant data analytics platform with ML capabilities.
- Validated PAT tools for continuous data input.
Methodology:
- Data Sourcing and Curation:
- Collect and consolidate data from all relevant unit operations (e.g., blending, granulation, compression).
- Perform data cleaning, handling missing values and outliers using statistically sound methods.
- Annotate data with relevant metadata (batch ID, time stamp, equipment ID).
Model Training and Tuning:
- Divide the dataset into a training set (~70-80%) and a test set (~20-30%). Use techniques like k-fold cross-validation on the training set to tune hyperparameters.
- Train multiple algorithm types (e.g., Multiple Linear Regression, Random Forest, Neural Networks) to identify the best performer.
- The model's output is the predicted CQA value.
Analytical Validation (AI Model Credibility): This is the core of the method validation and must demonstrate [102]:
- Accuracy: The mean prediction error versus the actual lab value should be within a pre-defined, justified acceptance criterion (e.g., ±5%).
- Precision (Repeatability): Assess the variability of predictions when the model is applied to multiple subsets of the test data.
- Specificity: Demonstrate that the model is sensitive to changes in process parameters that are known to affect the CQA.
- Range: Ensure the model is accurate across the entire design space of the manufacturing process.
Continuous Performance Monitoring:
- Establish a system to monitor the model's predictive performance during routine commercial production.
- Implement a trigger for model re-training or alerting if prediction errors drift outside of established control limits.
Diagram 1: AI Model Validation Workflow for RTRT
The Digital Transformation Ecosystem
The successful implementation of AI and RTRT does not occur in isolation; it is part of a broader digital transformation reshaping the entire pharmaceutical and life sciences industry.
Data Integration and Structured Authoring
The foundation of any digital quality system is structured data. Regulatory authorities are increasingly emphasizing data-centric submissions. The EMA's focus on implementing SPOR (Substance, Product, Organisation and Referential) master data services is a prime example of the push toward digital submissions with an emphasis on data rather than documents [96]. Combining structured data with AI-driven technologies like natural language processing (NLP) allows for the extraction of content from unstructured documents, facilitating a machine-readable information flow that is essential for automated quality systems [96].
Real-World Evidence (RWE) and Digital Health Technologies
There is a growing emphasis on using Real-World Evidence to bridge the gap between clinical effectiveness and commercial outcomes [96]. RWE provides insights from much larger and more diverse patient data sets than traditional clinical trials. The ICH M14 guideline, adopted in September 2025, sets a global standard for pharmacoepidemiological safety studies using real-world data, marking a pivotal shift toward harmonized expectations for evidence quality [102].
Furthermore, the rise of Digital Health Technologies, including wearables and health apps, provides access to continuous streams of real-world data. This influences not only drug development but also post-market surveillance, creating a feedback loop that can inform product quality and lifecycle management [96].
Diagram 2: The Integrated Digital Quality Ecosystem
Regulatory Landscape and Future Outlook
As digital tools and AI become integral to pharmaceutical development and quality control, global regulatory bodies are evolving their frameworks to ensure safety and efficacy while fostering innovation.
Evolving Regulatory Frameworks
Regulators are actively developing guidelines for the use of advanced technologies. Key developments include:
- AI Credibility Frameworks: The FDA released draft guidance in January 2025 proposing a risk-based credibility framework for AI models used in regulatory decision-making [102]. This provides a pathway for validating the AI components central to RTRT.
- Global Divergence and Modernization: While agencies like the FDA and EMA are modernizing with adaptive pathways and rolling reviews, regional divergence adds complexity. The EU's AI Act, fully applicable by August 2027, classifies healthcare AI as "high-risk," imposing stringent validation and traceability requirements [102]. This makes early engagement with regulators and strategic planning essential.
The convergence of AI, Real-Time Release Testing, and Digital Transformation represents the future of analytical method validation. This new paradigm shifts quality assurance from a discrete, end-of-process checkpoint to a continuous, predictive, and data-driven endeavor embedded throughout the product lifecycle. For researchers, scientists, and drug development professionals, mastering this integrated approach is no longer optional but a strategic imperative to accelerate development, enhance product quality, and ensure robust regulatory compliance in the digital age. The organizations that will lead are those that build agility into their strategies, integrate evidence generation across clinical and digital domains, and embed regulatory foresight directly into their innovation pipelines [102].
Conclusion
Analytical method validation has evolved from a one-time compliance exercise to a continuous, science-based lifecycle process. Mastering foundational parameters, implementing QbD principles, and adopting robust troubleshooting strategies are essential for developing methods that ensure product quality and patient safety. The integration of ICH Q2(R2) and Q14 guidelines provides a modern framework emphasizing proactive risk management and regulatory flexibility. As novel therapeutic modalities emerge, the strategic application of advanced technologies like AI, real-time monitoring, and digital twins will further transform validation practices, positioning analytical excellence as a cornerstone of pharmaceutical innovation and global market success.
References
- 1. Performance Characteristics Measured in Method Validation [https://www.chromatographyonline.com/view/performance-characteristics-measured-method-validation]
- 2. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 3. Verification of quantitative analytical methods in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8199534/]
- 4. Introduction to Analytical Method Development and ... [https://www.labmanager.com/introduction-to-analytical-method-development-and-validation-33922]
- 5. Pharmaceutical Validation Guide: Proper Implementation [https://dicksondata.com/pharmaceutical-validation-6-principles-for-effective-implementation?srsltid=AfmBOoq1V5lIysGb1opi_yDqkC_6AedlH9pfxsJ99q7zzo3M_jgB_Pa7]
- 6. ( ICH ) Validation of Analytical Procedures: An... | QbD Group Q 2 R 2 [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 7. Q2(R2) Validation of Analytical Procedures March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r2-validation-analytical-procedures]
- 8. FDA Releases Guidance on Analytical Procedures [https://www.biopharminternational.com/view/fda-releases-guidance-on-analytical-procedures]
- 9. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 10. Analytical Procedures and Methods Validation for Drugs ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/analytical-procedures-and-methods-validation-drugs-and-biologics]
- 11. specifications, analytical procedures and analytical validation [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/scientific-guidelines/quality-guidelines/quality-specifications-analytical-procedures-analytical-validation]
- 12. EMA publishes Document on the Validation of analytical ... [https://www.gmp-compliance.org/gmp-news/ema-publishes-document-on-the-validation-of-analytical-methods]
- 13. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 14. Frequently Asked Questions about Method Validation [https://www.ofnisystems.com/services/method-validation/frequently-asked-questions-about-method-validation/]
- 15. Impact of introducing a new biological matrix into ... [https://pubmed.ncbi.nlm.nih.gov/38693051/]
- 16. ANALYTICAL METHOD VALIDATION IN PHARMA [https://pharmadevils.com/analytical-method-validation/]
- 17. Method Validation - an overview [https://www.sciencedirect.com/topics/engineering/method-validation]
- 18. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 19. ISO/IEC 17025:2017 - General requirements for ... [https://www.iso.org/standard/66912.html]
- 20. Explaining ISO/IEC 17025 Competency Requirements [https://a2la.org/explaining-iso-iec-17025-competency-requirements/]
- 21. Analytical Method Validation: A Comprehensive Review of ... [http://www.seejph.com/index.php/seejph/article/view/6516]
- 22. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 23. What Is Method Validation Risk Assessment and Its ... [https://altabrisagroup.com/method-validation-risk-assessment/]
- 24. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 25. Validation requirements of screening analytical methods ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993619305345]
- 26. Comparative analysis and validation of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452224000530]
- 27. Spike and Recovery and Linearity of Dilution Assessment [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 28. Dilutional Linearity, Parallelism, Spike-and-Recovery in ... [https://www.enzo.com/note/dilutional-linearity-parallelism-spike-and-recovery-in-elisa-how-to-qc-your-results/]
- 29. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOor2hkstU8TXgcWupy9jwvTBPaKZVdxsnzbSE4qCt9RO5xkJUQ7d]
- 30. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 31. Repeatability: Test-Retest Reliability & Reproducibility [https://sixsigmadsi.com/glossary/repeatability/]
- 32. Design of Experiments for Analytical Method Development ... [https://www.biopharminternational.com/view/design-experiments-analytical-method-development-and-validation]
- 33. A Guide to Analytical Method Validation [https://scioninstruments.com/us/blog/a-guide-to-analytical-method-validation-2/]
- 34. What is the difference between specificity and selectivity? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/specificity-selectivity]
- 35. Trends In Pharmaceutical 2025 Development... Analytical Methods [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 36. An Introduction to Analytical Method Development and ... [https://www.sofpromed.com/an-introduction-to-analytical-method-development-and-validation-in-early-phase-clinical-trials]
- 37. A Step-by-Step Guide to Analytical Method Development ... [https://emerypharma.com/blog/a-step-by-step-guide-to-analytical-method-development-and-validation/]
- 38. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 39. Analytical Method Validation: A Recipe for Accurate Results [https://certified-laboratories.com/blog/analytical-method-validation-a-recipe-for-accurate-results/]
- 40. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 41. What is meant by the limit of detection and quantification (LOD ... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/limit-of-detection-quantifcation]
- 42. Approaches to Assay Characterization and Validation: Part 1 [https://www.quanterix.com/approaches-to-assay-characterization-and-validation-part-1-limit-of-detection-and-lower-limit-of-quantitation/]
- 43. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 44. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 45. Methods to determine limit of detection and ... [https://www.sciencedirect.com/science/article/pii/S2214753516300286]
- 46. The Fitness for Purpose of Analytical Methods (2025) [https://www.eurachem.org/index.php/publications/guides/mv]
- 47. Guidance for robustness/ruggedness tests in method ... [https://www.sciencedirect.com/science/article/abs/pii/S073170850000529X]
- 48. Method Validation and Robustness [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 49. Robustness and Ruggedness Testing in Analytical Chemistry [https://www.labmanager.com/robustness-and-ruggedness-testing-in-analytical-chemistry-34247]
- 50. Difference between robustness and ruggedness [https://ask.pharmaguideline.com/t/difference-between-robustness-and-ruggedness/7171]
- 51. 10. Ruggedness, robustness [https://sisu.ut.ee/lcms_method_validation/10-ruggedness-robustness/]
- 52. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 53. What are system suitability tests (SST) of analytical methods? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sst]
- 54. Analytical Method Validation: Back to Basics, Part I [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 55. Guidelines and considerations for the use of system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5960010/]
- 56. The Hidden Risks in Analytical Method Validation - [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 57. Best Practices For Successful Method Validation [https://lgmpharma.com/blog/best-practices-for-successful-method-validation/]
- 58. Top Mistakes in Analytical Method Validation and How to ... [https://www.pharmoutsourcing.com/Featured-Articles/350046-Top-Mistakes-in-Analytical-Method-Validation-and-How-to-Avoid-Them/]
- 59. Validating Analytical Methods for Biopharmaceuticals, Part 1 [https://www.biopharminternational.com/view/validating-analytical-methods-biopharmaceuticals-part-1-development-and-optimization]
- 60. Challenges in Analytical Method Development and ... [https://www.biopharminternational.com/view/challenges-analytical-method-development-and-validation]
- 61. Analytical Validation of an LC-MS/MS Method for ... [https://www.mdpi.com/1422-0067/26/13/6358]
- 62. Comparison of Quantification Using UV-Vis, NMR, and ... [https://www.mdpi.com/1422-0067/26/14/6638]
- 63. Development and validation of a GC–FID method ... [https://www.sciencedirect.com/science/article/pii/S2095177915000179]
- 64. Conducting GC Method Validation Using High Accuracy ... [https://www.environics.com/2024/08/23/gc-method-validation-high-accuracy-standards/]
- 65. Development and validation of an LC–MS/MS method ... [https://www.nature.com/articles/s41598-025-96764-3]
- 66. of Implementation (AQbD or QbD) in... Analytical Quality by Design [https://www.linkedin.com/pulse/implementation-analytical-quality-design-aqbd-qbd-method-hossain]
- 67. (AQbD) - Veeprho Analytical Quality by Design [https://veeprho.com/analytical-quality-by-design-aqbd/]
- 68. Aspects and Implementation of Pharmaceutical Quality ... by Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 69. Readiness for Implementation of ICH Q2(R2) and Q14 Industry... [https://ispe.org/pharmaceutical-engineering/september-october-2025/readiness-implementation-ich-q2r2-and-q14]
- 70. | GreyRigge Associates Quality by Design [https://www.greyrigge.com/quality-by-design]
- 71. Eco-Friendly AQbD-Driven HPLC: A Sustainable Approach to Method... [https://jyoungpharm.org/10.5530/jyp.20250087]
- 72. Novel analytical method development and validation of ... [https://fjps.springeropen.com/articles/10.1186/s43094-025-00877-5]
- 73. (QbD) Principles in Quality ... - Chemical CEO by Design Analytical [https://chemicalceo.com/analytical-techniques/quality-by-design-qbd-principles-in-analytical-method-development/]
- 74. Emerging New Drug Modalities in 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 75. Home | 7th Gene Therapy Analytical Development Summit 2025 [https://www.genetherapy-analytical-cmc.com/]
- 76. Validation Protocols | Pioneering Diagnostics - bioMerieux [https://www.biomerieux.com/us/en/our-offer/industry-products/validation-protocols.html]
- 77. How to be prepared for Pharmaceutical Validation in 2025 [https://www.gillsprocess.com/blog-1/2024/12/11/how-to-be-prepared-for-pharmaceutical-validation-in-2025]
- 78. How Analytical Method Validation Ensures Product Quality [https://www.pharmsky.com.au/how-analytical-method-validation-ensures-product-quality/]
- 79. Applying ICH Q14 in Pharmaceuticals Part 2: The Benefits ... [https://premier-research.com/perspectives/applying-ich-q14-in-pharmaceuticals-part-2-the-benefits-of-an-enhanced-approach-in-the-lifecycle-management-and-post-approval-changes-of-analytical-procedures/]
- 80. Validation Best Practices vs. Traditional Compliance [https://www.avslifesciences.com/blog-post/validation-best-practices-vs-traditional-compliance-a-guide-for-officers]
- 81. Leading Pharmaceutical Validation Trends for 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 82. Pharmaceutical Product Lifecycle Management & ICH Q12 ... [https://www.advarra.com/blog/pharmaceutical-product-lifecycle-management/]
- 83. AQbD-novel strategy for analytical methods [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 84. Implement ICH Q14 Guidelines More Easily with Method ... [https://www.acdlabs.com/blog/implement-ichq14-guidelines-more-easily-with-method-development-software/]
- 85. Analytical Methods and Control Strategies: The Forgotten ... [https://www.pharmoutsourcing.com/Featured-Articles/171114-Analytical-Methods-and-Control-Strategies-The-Forgotten-Interface/]
- 86. Streamlining Postapproval Submissions Using ICH Q12 & ... [https://ispe.org/pharmaceutical-engineering/september-october-2022/streamlining-postapproval-submissions-using-ich]
- 87. Streamlining Post-Approval Changes Industry Insights on ... [https://ispe.org/pharmaceutical-engineering/september-october-2025/streamlining-post-approval-changes-industry]
- 88. Risk Evaluation and Mitigation Strategies | REMS [https://www.fda.gov/drugs/drug-safety-and-availability/risk-evaluation-and-mitigation-strategies-rems]
- 89. Post-Approval Change Submissions [https://www.freyrsolutions.com/medicinal-products/post-approval-change-submissions]
- 90. Importance of acceptance criteria in analytical method ... [https://www.gmpsop.com/importance-of-acceptance-criteria-in-analytical-method-transfer/]
- 91. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 92. Best Practices for Transferring Analytical Methods [https://www.jmolner.com/post/transferring-analytical-methods]
- 93. Interlaboratory comparisons - The Joint Research Centre [https://joint-research-centre.ec.europa.eu/projects-and-activities/reference-and-measurement/interlaboratory-comparisons_en]
- 94. Evaluating Inter-Laboratory Comparison Data [https://www.nist.gov/publications/evaluating-inter-laboratory-comparison-data]
- 95. Methodological Validation and Inter-Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11512302/]
- 96. The digital pharmaceutical journey: 2025 and beyond [https://www.pharmalex.com/thought-leadership/blogs/the-digital-pharmaceutical-journey-2025-and-beyond/]
- 97. The Digital Transformation Landscape of Pharma in 2025 [https://blog.pulsehealth.tech/the-digital-transformation-landscape-of-pharma-in-2025/]
- 98. Real AI Test Automation Tools 2025 | How to Identify ... [https://www.virtuosoqa.com/post/real-ai-test-automation-2025]
- 99. 8 Automation Testing Trends for 2025 (Agentic AI) [https://testguild.com/automation-testing-trends/]
- 100. AI Testing Trends 2025: Boost ROI with Automated QA Tools [https://www.testriq.com/blog/post/ai-testing-trends-2025]
- 101. Top 12 AI Test Automation Tools for Smarter Software ... [https://www.startearly.ai/post/top-12-ai-test-automation-tools]
- 102. Regulatory strategy reimagined: Three trends accelerating ... [https://www.drugdiscoverytrends.com/regulatory-strategy-reimagined-three-trends-accelerating-drug-development/]
- 103. 2025 life sciences outlook | Deloitte Insights [https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-life-sciences-executive-outlook.html]