Defining Validation Parameters for Comparative Method Selection: A Strategic Guide for Researchers
This article provides a comprehensive framework for researchers and drug development professionals on establishing validation parameters to guide the selection of comparative methods.
Defining Validation Parameters for Comparative Method Selection: A Strategic Guide for Researchers
Abstract
This article provides a comprehensive framework for researchers and drug development professionals on establishing validation parameters to guide the selection of comparative methods. It covers foundational principles of method comparison, detailed experimental methodologies, strategies for troubleshooting common issues, and the final validation process against regulatory standards. The guidance synthesizes current best practices to ensure that selected methods yield accurate, precise, and legally defensible data, thereby supporting robust scientific decision-making and regulatory compliance.
Core Principles and Definitions for Robust Method Comparison
In the context of analytical method validation and comparative method selection, understanding and quantifying error is fundamental to ensuring data reliability and scientific integrity. Systematic error, also known as bias, refers to a consistent, repeatable error that leads to measurements deviating from the true value in a predictable direction [1] [2]. Unlike random errors which cause scatter around the true value, systematic errors displace all measurements in the same direction, thus affecting the accuracy of a method—defined as the closeness of agreement between a measured value and its true value [3] [4]. The distinction between these concepts is crucial for researchers, particularly in drug development where methodological biases can significantly impact trial outcomes and regulatory decisions.
Systematic errors arise from identifiable factors such as faulty instrument calibration, improper analytical technique, or imperfect method specificity [3] [4]. These errors cannot be reduced by simply repeating measurements, unlike random errors which average out with sufficient replication. When comparing analytical methods, researchers must therefore prioritize the identification, quantification, and control of systematic errors to make valid comparisons about relative performance. The presence of unaddressed systematic error compromises method validation and can lead to incorrect conclusions about a method's suitability for its intended purpose.
Foundational Concepts: Accuracy, Precision, and Error Classification
Differentiating Accuracy and Precision
In analytical sciences, accuracy and precision represent distinct methodological attributes. Accuracy, as defined, refers to closeness to the true value, while precision describes the closeness of agreement between independent measurements obtained under specified conditions—essentially the reproducibility of the measurement [1] [2]. A method can be precise (yielding consistent, repeatable results) yet inaccurate due to systematic error, or accurate on average but imprecise due to substantial random error [3].
This relationship is visually represented in the diagram below, which illustrates the four possible combinations of these properties:
Classification of Measurement Errors
Measurement errors are broadly classified into three categories:
Systematic Errors: Consistent, reproducible inaccuracies due to factors that bias results in one direction. These include:
Random Errors: Unpredictable fluctuations caused by uncontrollable environmental or instrumental variables. These affect precision but not necessarily accuracy, as they may average out with sufficient replication [1] [3].
Gross Errors: Human mistakes such as incorrect recording, calculation errors, or procedural oversights [4].
Comparative Assessment of Systematic Error Evaluation Methods
The assessment of systematic error employs distinct methodological approaches, each with specific applications, advantages, and limitations. The selection of an appropriate assessment strategy depends on factors including the analytical context, availability of reference materials, and required rigor.
Table 1: Comparison of Methodologies for Assessing Systematic Error and Inaccuracy
| Methodology | Principle | Application Context | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Percent Error Calculation [1] | Calculates the absolute difference between experimental and theoretical values as a percentage of the theoretical value. | Method verification against known standards. | Simple to calculate and interpret; provides immediate measure of deviation. | Requires knowledge of the true value; single measurement may not represent overall method bias. |
| Reference Material/Standard Method Comparison [1] [2] | Compares results from the test method to those from an established reference method or certified reference material. | Method validation and calibration. | Directly assesses accuracy against an accepted reference; foundational to method validation. | Availability and cost of appropriate reference materials; assumes reference method is truly accurate. |
| Statistical Error Quantification (e.g., M-TDC) [5] | Employs specialized algorithms and circuitry (e.g., Magnitude-to-Time-to-Digital Converters) to quantify specific systematic error components like offset and gain. | High-precision instrumentation and engineering applications. | Quantifies individual error sources (offset, gain, phase imbalance); enables targeted compensation. | Requires technical expertise and specialized data processing; can be equipment-intensive. |
| Method of Known Additions (Spike Recovery) | Measures the method's ability to recover a known quantity of analyte added to a sample. | Evaluating method accuracy in complex matrices. | Assesses accuracy in the presence of the sample matrix; helps identify matrix effects. | Does not assess extraction efficiency from native sample; preparation intensive. |
Experimental Protocols for Systematic Error Assessment
Protocol 1: Assessment via Percent Error and Standard Method Comparison
This fundamental protocol is widely used in analytical chemistry and pharmaceutical sciences for initial method validation [1].
Workflow Overview:
Materials and Reagents:
- Certified Reference Material (CRM) or analyte standard of known purity
- Appropriate solvents and reagents for sample preparation
- Test instrument/methodology under evaluation
- Reference instrument/methodology (if performing comparison)
Procedural Steps:
Sample Preparation: Prepare a series of solutions containing the analyte at concentrations spanning the method's dynamic range, using the Certified Reference Material.
Analysis: Analyze each solution using both the test method and the reference method (if applicable). For a simple percent error calculation, only the test method is used, and results are compared to the known, prepared concentration [1].
Calculation: For each measurement, calculate the percent error using the formula:
Data Analysis: For a method comparison, use statistical tests (e.g., paired t-test, Bland-Altman analysis) to determine if a statistically significant systematic bias exists between the test method and the reference method.
Protocol 2: Quantification of Specific Systematic Error Components in Instrumentation
This advanced protocol, derived from engineering research, demonstrates the precise quantification of specific systematic error components (offset, gain, phase imbalance) in sinusoidal encoders using Magnitude-to-Time-to-Digital Converters (M-TDCs) [5].
Workflow Overview:
Materials and Reagents:
- Device Under Test (e.g., sinusoidal encoder)
- M-TDC circuit (comprising comparators, integrators, and a microcontroller unit)
- Precision signal generator
- Data acquisition system
Procedural Steps:
Signal Application: Apply a known, controlled input (e.g., a precise angular displacement to an encoder) [5].
Signal Acquisition: Acquire the corresponding output signals. For a sinusoidal encoder, this would be the voltage pairs (Vsin, Vcos) [5].
Digitization: Process the analog output signals through the M-TDC circuit, which converts signal magnitudes into time intervals for high-resolution digitization without requiring a conventional analog-to-digital converter (ADC) [5].
Error Parameter Calculation: Apply the quantification algorithm (e.g., Method I or II from the cited research) to the digitized data to solve for the specific systematic error parameters [5]:
- α, β: DC offset errors in the sine and cosine channels, respectively.
- τ: Amplitude mismatch between channels.
- ψ: Phase imbalance between channels.
Compensation: Use the calculated error parameters in a compensation function within the measurement algorithm to correct subsequent readings, thereby enhancing accuracy [5].
Case Studies in Research and Development
Case Study: Systematic Error Considerations in Alzheimer's Drug Development
The Alzheimer's disease (AD) drug development pipeline for 2025 includes 138 drugs across 182 clinical trials [6]. The high-profile failure of many past AD trials has been partly attributed to methodological systematic errors, including:
- Measurement Errors in Patient Stratification: Inaccurate diagnosis or imperfect biomarker-based patient selection led to enrolling heterogeneous populations, obscuring true treatment effects [6].
- Bias in Clinical Endpoints: The use of cognitive and functional scales susceptible to rater bias and placebo effects introduced systematic measurement error [6].
The contemporary response, as seen in the 2025 pipeline, is a concerted effort to mitigate these errors. This includes the incorporation of biomarkers as primary outcomes in 27% of active trials, which provides more objective, quantitative, and less biased measures of biological effect compared to purely clinical scales [6]. This shift exemplifies how recognizing and controlling for systematic error directly influences trial design and the likelihood of success in drug development.
Case Study: Technological Mitigation of Systematic Errors in Medication Safety
In pharmacy practice, technological advancements are increasingly deployed to control systematic human errors. For example:
- Electronic Health Records (EHRs) and Clinical Decision Support (CDS) Systems reduce systematic errors related to information gaps and flawed clinical reasoning by providing centralized patient data and evidence-based alerts [7].
- Barcode Medication Administration (BCMA) systematically prevents errors in patient identification and drug selection, a known source of consistent bias in the medication administration process [7].
These technologies function as systemic checks against historically persistent systematic errors, thereby enhancing overall accuracy in patient care and contributing to a estimated annual global cost savings by reducing medication errors [7].
Research Reagent Solutions for Error Assessment
The following table details key materials and tools essential for experiments designed to assess systematic error and inaccuracy.
Table 2: Essential Research Reagents and Tools for Systematic Error Assessment
| Item | Specification/Example | Primary Function in Error Assessment |
|---|---|---|
| Certified Reference Materials (CRMs) | NIST-traceable standards of known purity and concentration. | Serves as the benchmark "true value" for calculating percent error and assessing method accuracy [1]. |
| Signal Acquisition Hardware | Data acquisition cards (e.g., National Instruments USB-6211), high-resolution ADCs [5]. | Precisely captures analog output from devices under test for subsequent digital analysis of error. |
| Direct Interface Circuits | Custom Magnitude-to-Time-to-Digital Converters (M-TDCs) built with comparators and integrators [5]. | Enables high-resolution quantification of specific systematic error parameters (offset, gain) in instrumentation. |
| Statistical Analysis Software | R, Python (SciPy), MATLAB, GraphPad Prism. | Performs statistical comparisons (t-tests, regression) between methods to identify and quantify systematic bias. |
| Reference Methodologies | Pharmacopeial methods (e.g., USP), published standard analytical procedures. | Provides an accepted reference point against which the accuracy of a new or comparative method is evaluated [1] [2]. |
The rigorous assessment of systematic error and inaccuracy is a non-negotiable component of robust analytical and clinical research. As demonstrated, a variety of established and emerging methodologies—from fundamental percent error calculations to sophisticated computational quantification—are available to researchers for this purpose. The selection of an appropriate assessment strategy must be guided by the specific context of the method being validated and the consequences of inaccuracy. The ongoing integration of advanced technologies, including AI and automated error-compensation circuits, promises further enhancements in our ability to identify and control for systematic biases. For the drug development professional, a deep understanding of these principles is critical for designing valid clinical trials, interpreting complex biomarker data, and ultimately bringing effective, safe therapies to market. A method's precision is meaningless without demonstrable accuracy, and accuracy cannot be confirmed without a deliberate and thorough assessment of systematic error.
Table of Contents
- Introduction
- Core Definitions and Conceptual Framework
- Experimental Protocols for Quantification
- Quantitative Assessment and Data Analysis
- Research Reagent Solutions and Essential Materials
- Conclusion
In scientific research and drug development, reliable data is the foundation upon which all conclusions and decisions are built. The trustworthiness of this data hinges on the quality of the measurement systems used to generate it. Understanding and distinguishing between key validation parameters—accuracy, precision, bias, and repeatability—is therefore not merely academic; it is a critical prerequisite for robust comparative method selection and meaningful research outcomes [8]. A measurement system with poor accuracy can lead to incorrect conclusions about a drug's efficacy, while one with poor precision can obscure real biological signals with excessive noise [9]. This guide provides a detailed, objective comparison of these fundamental performance characteristics, complete with experimental protocols and quantitative assessment criteria, to empower researchers in validating their analytical methods.
Core Definitions and Conceptual Framework
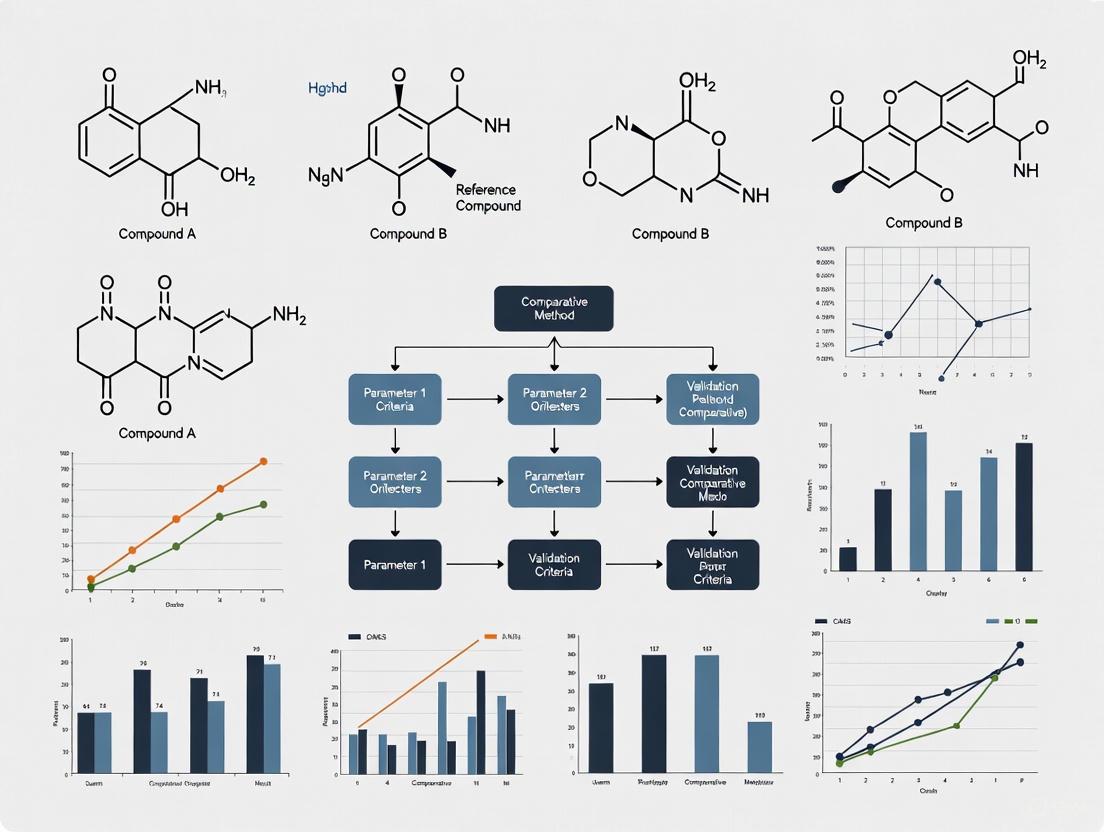
At its core, the quality of a measurement system is evaluated through two principal aspects: its accuracy (closeness to the true value) and its precision (the scatter of repeated measurements) [10]. The following diagram illustrates the logical relationships between these key terms and their components.
Diagram 1: Relationship of key measurement system concepts.
The definitions in the table below provide a clear, standardized foundation for understanding these distinct concepts, which are often conflated.
Table 1: Core Definitions of Key Measurement System Parameters
| Term | Definition | Synonyms / Related Terms | Answers the Question |
|---|---|---|---|
| Accuracy | The closeness of agreement between a measured value and the true or accepted reference value [10]. | Trueness (ISO) [10] | Is my measurement, on average, correct? |
| Precision | The closeness of agreement between independent measurements of the same quantity under specified conditions [10]. | Reliability, Variability [11] | How much scatter is in my measurements? |
| Bias | The systematic, directed difference between the average of measured values and the reference value [12] [9]. | Systematic Error, Accuracy (in part) | Does my method consistently over- or under-estimate the true value? |
| Repeatability | Precision under a set of conditions that includes the same measurement procedure, same operators, same measuring system, same operating conditions, and same location over a short period of time [12] [11]. | Intra-assay Precision, Test-Retest Reliability | When I measure the same sample multiple times in the same session, how consistent are the results? |
| Reproducibility | Precision under conditions where different operators, measuring systems, laboratories, or time periods are involved [12] [11]. | Inter-lab Precision | Can someone else, or a different instrument, replicate my results? |
It is crucial to recognize that accuracy and precision are independent. A method can be precise but inaccurate (biased), or accurate on average but imprecise [13]. The ideal system is both accurate and precise. The following conceptual diagram illustrates the four possible combinations of these properties.
Diagram 2: Pathways from poor to ideal measurement performance.
Experimental Protocols for Quantification
Moving from concept to practice requires standardized experiments to quantify these parameters. The following protocols are widely adopted across industries, including pharmaceutical development.
Gage Repeatability and Reproducibility (Gage R&R) Study
This experimental design is the gold standard for quantifying the precision of a measurement system by partitioning variation into its repeatability and reproducibility components [12] [9].
Table 2: Experimental Protocol for a Gage R&R Study
| Protocol Step | Detailed Description | Rationale |
|---|---|---|
| 1. Study Design | Select 2-3 appraisers (operators), 5-20 parts that represent the entire expected process or biological range, and plan for 2-3 repeated measurements per part by each appraiser [9]. | Using too few parts or operators will overestimate the measurement system's capability. Parts must encompass the full range to avoid underestimating error. |
| 2. Blinding & Randomization | Assign a random number to each part to conceal its identity. A third party should record data. Appraisers measure parts in a random order for all trials [9]. | Prevents operator bias from knowing previous results or part identity, ensuring that measured variation is genuine. |
| 3. Measurement Execution | Each appraiser measures all parts once in the randomized order. This process is repeated for the required number of trials, with parts being re-presented in a new random order each time [9]. | Replication under controlled but blinded conditions allows for the isolation of random measurement error (repeatability). |
| 4. Data Analysis | Data is analyzed using Analysis of Variance (ANOVA) to decompose the total variation into components: part-to-part variation, repeatability, and reproducibility [9]. | ANOVA provides a statistically rigorous method to quantify the different sources of variation within the measurement system. |
Bias and Linearity Study
This protocol assesses the accuracy of a measurement system across its operating range.
Table 3: Experimental Protocol for a Bias and Linearity Study
| Protocol Step | Detailed Description | Rationale |
|---|---|---|
| 1. Master Sample Selection | Select 5-10 parts or standards that cover the operating range of the measurement device (e.g., low, mid, and high values). The "true" reference value for each part must be known through a more accurate, traceable method [12] [9]. | Assessing bias at multiple points is necessary to determine if the bias is consistent (acceptable) or changes with the magnitude of measurement (linearity issue). |
| 2. Repeated Measurement | Measure each master part multiple times (e.g., 10-20 repetitions) in a randomized order [12]. | Averaging multiple measurements provides a stable estimate of the observed value for each part, reducing the influence of random noise on the bias calculation. |
| 3. Data Analysis | For each part, calculate bias as (Observed Average - Reference Value). Perform a linear regression analysis with bias as the response (Y) and the reference value as the predictor (X) [12]. | The regression analysis quantifies the linearity of the bias. A significant slope indicates that the bias changes as a function of the size of the measurand, which must be corrected for. |
Quantitative Assessment and Data Analysis
Once data is collected from the aforementioned experiments, it is analyzed against established criteria to determine the acceptability of the measurement system.
Assessing Precision: Gage R&R Acceptance Criteria
The results of a Gage R&R study are typically expressed as a percentage of contribution to the total observed variation. The automotive industry action group (AIAG) guidelines are commonly referenced for decision-making [9].
Table 4: Gage R&R Acceptance Criteria (AIAG Guidelines)
| % Gage R&R of Total Variation | Decision | Interpretation |
|---|---|---|
| ≤ 10% | Acceptable | The measurement system is considered capable. Variation is dominated by actual part-to-part differences. |
| > 10% to ≤ 30% | Marginal | The system may be acceptable for some applications based on cost, nature of the measurement, etc. Requires expert review. |
| > 30% | Unacceptable | The measurement system has excessive variation and is not suitable for data-based decision-making. Improvement is required [9]. |
Assessing Accuracy: Bias and Linearity Metrics
The output from a bias and linearity study provides specific metrics to quantify accuracy, as demonstrated in a recent study validating quantitative MRCP-derived metrics [14].
Table 5: Quantitative Metrics for Accuracy and Bias Assessment
| Metric | Calculation / Result | Interpretation and Context | ||
|---|---|---|---|---|
| Average Bias | 0.1253 | The overall average difference between measured values and the reference across all samples. A one-sample t-test can determine if this bias is statistically significant (p-value < 0.05) [12]. | ||
| % Linearity | (% Linearity = | Slope | × 100%) | The percentage by which the observed process variation is inflated due to the gage's linearity issue. A smaller value indicates better performance [12]. |
| Absolute Bias (Phantom Study) | 0.0 - 0.2 mm | In a phantom study simulating strictures and dilatations, the absolute bias was sub-millimeter, demonstrating high accuracy. The 95% limits of agreement were within ± 1.0 mm [14]. | ||
| Reproducibility Coefficient (RC) | Ranged from 3.3 to 51.7 for various duct metrics | The RC represents the smallest difference that can be detected with 95% confidence. Lower RCs indicate better reproducibility and greater sensitivity to detecting true change [14]. |
Research Reagent Solutions and Essential Materials
The following table details key materials and solutions required for executing the validation experiments described in this guide, with examples from both general metrology and specific biomedical research.
Table 6: Essential Materials for Measurement System Validation Studies
| Item / Solution | Function in Validation | Example from Literature |
|---|---|---|
| Traceable Reference Standards | Serves as the "ground truth" with a known value for bias assessment and calibration. Crucial for establishing accuracy. | Calibration weights, standard reference materials (SRMs) from national institutes [9]. |
| Stable Master Samples | A representative sample from the process, used for stability assessment over time via control charts. | A part measured to determine its reference value, used for ongoing stability monitoring [9]. |
| 3D-Printed Anatomical Phantoms | Provides a known ground-truth model with realistic geometry to assess measurement accuracy in imaging studies. | A phantom with tubes of sinusoidally-varying diameters used to validate MRCP+ software for biliary tree imaging [14]. |
| Gage R&R Study Kits | A prepared set of parts that represent the entire process spread, used for conducting the Gage R&R study. | 10-20 parts selected from production to cover the full range of process variation [9]. |
| Statistical Software with ANOVA | Performs the complex variance component analysis required for Gage R&R and linear regression for bias studies. | Software tools that automate Gage R&R calculations and produce associated control charts and graphs [9]. |
| Validated Biomarker Assays | A measurement tool with established performance characteristics used as a comparator in method selection research. | IceCube, Nedap Smart Tag, and CowManager sensors were identified as meeting validity criteria (≥85% precision, no bias) in a review of wearable sensors for dairy cattle [15]. |
A rigorous approach to method selection and validation is indispensable for generating reliable scientific data. As demonstrated, the parameters of accuracy, precision, bias, and repeatability are distinct yet interconnected concepts that must be evaluated through structured experimental protocols like Gage R&R and bias studies. The quantitative criteria derived from these studies provide an objective basis for accepting or rejecting a measurement system for its intended use. In the context of drug development and biomarker research, where decisions have significant clinical and financial implications, overlooking this foundational step can lead to failed trials and irreproducible results [8] [9]. Therefore, integrating these validation practices is not a mere technicality but a cornerstone of responsible and effective research.
In the discipline of laboratory medicine, there is consensus that routine measurement procedures claiming the same measurand should give equivalent results within clinically meaningful limits [16]. The comparison of methods experiment is a critical procedure performed to estimate this inaccuracy or systematic error [17]. The fundamental question in such studies is one of substitution: Can one measure a given analyte with either the test method or the comparative method and obtain equivalent results? [18] The selection of an appropriate comparative method—either a reference method or a routine method—forms the foundational decision that impacts all subsequent validation data and conclusions. This guide objectively compares these two approaches to equip researchers and drug development professionals with the evidence needed to make informed decisions within method validation frameworks.
Comparative Analysis: Reference Methods vs. Routine Methods
The analytical method used for comparison must be carefully selected because the interpretation of the experimental results depends on the assumptions that can be made about the correctness of the comparative method's results [17]. The core distinction lies in the documented evidence of accuracy and the resulting attribution of measurement differences.
Table 1: Core Characteristics of Reference and Routine Comparative Methods
| Characteristic | Reference Method | Routine Method |
|---|---|---|
| Fundamental Definition | A high-quality method whose results are known to be correct through comparison with definitive methods and/or traceable standards [17]. | An established method in routine clinical use, whose correctness may not be fully documented [17]. |
| Metrological Traceability | Sits high in the traceability chain; key to establishing metrological traceability of routine methods to higher standards (e.g., SI units) [16]. | Typically lower in the traceability chain; often calibrated using reference methods or materials. |
| Attribution of Error | Any observed differences are assigned to the test (candidate) method [17]. | Observed differences must be carefully interpreted; it may not be clear which method is the source of error [17]. |
| Quality Specifications | Must fulfill "genuine" requirements (e.g., direct calibration with primary reference materials, high specificity) and defined analytical performance specifications [19] [16]. | Performance specifications are typically based on clinical requirements (e.g., biological variation) or manufacturer's claims. |
| Operational Laboratories | Must be performed by laboratories complying with ISO 17025 and ISO 15195, often requiring accreditation and participation in specific round-robin trials [16]. | Operated in routine clinical laboratories following standard good laboratory practices. |
| Ideal Use Case | For unequivocally establishing the trueness (systematic error) of a new candidate method [17]. | For verifying that a new method provides equivalent results to the method currently in use in the laboratory [18]. |
Experimental Protocols for Method Comparison Studies
Regardless of the chosen comparative method, the experimental design must be rigorous to yield reliable estimates of systematic error. The following protocol outlines the key steps, highlighting considerations specific to the choice of comparative method.
The diagram below outlines the core workflow for designing and executing a method-comparison study.
Detailed Methodological Considerations
Specimen Selection and Number: A minimum of 40 different patient specimens should be tested by the two methods [17]. These specimens should be carefully selected to cover the entire working range of the method and represent the spectrum of diseases expected in its routine application. Twenty well-selected specimens covering a wide concentration range often provide better information than one hundred randomly selected specimens [17]. For a more robust assessment, especially when investigating method specificity, 100 to 200 specimens are recommended [17].
Measurement Protocol: The experiment should include several different analytical runs over a minimum of 5 days to minimize systematic errors that might occur in a single run [17]. A common practice is to analyze each specimen singly by the test and comparative methods. However, performing duplicate measurements—ideally on different samples analyzed in different runs or at least in different order—provides a valuable check for sample mix-ups, transposition errors, and other mistakes [17]. Specimens should generally be analyzed within two hours of each other by the two methods to avoid differences due to specimen instability [17].
Data Analysis Procedures: The analysis involves both graphical and statistical techniques. The data should be graphed as soon as possible during collection to identify discrepant results that need re-analysis while specimens are still available [17].
- Graphical Analysis: For methods expected to show one-to-one agreement, a difference plot (test result minus comparative result versus the comparative result) is ideal for visualizing constant and proportional errors [17]. For methods not expected to agree one-to-one, a comparison plot (test result versus comparative result) is more appropriate [17].
- Statistical Analysis: For data covering a wide analytical range, linear regression statistics (slope, y-intercept, standard error of the estimate, sy/x) are preferred. These allow for the estimation of systematic error (SE) at critical medical decision concentrations (Xc) using the formula: Yc = a + bXc, and then SE = Yc - Xc [17]. The correlation coefficient (r) is more useful for assessing whether the data range is wide enough for reliable regression (r ≥ 0.99) than for judging method acceptability [17]. For a narrower analytical range, calculating the average difference (bias) via a paired t-test is usually best [17]. The Bland-Altman plot (difference between methods vs. average of the two methods) is a highly recommended technique for assessing agreement, as it visually presents the bias (mean difference) and the limits of agreement (bias ± 1.96 standard deviation of the differences) [18].
Essential Reagents and Materials for Method Validation Studies
The table below details key reagents and materials required for conducting a robust method-comparison study.
Table 2: Research Reagent Solutions and Essential Materials for Method Comparison
| Item | Function / Purpose | Critical Considerations |
|---|---|---|
| Patient Specimens | To provide a matrix-matched, real-world sample for comparing the test and comparative methods. | Should cover the entire analytical range and include pathological states [17]. Stability must be ensured [17]. |
| Primary Reference Material | Used with a reference method for direct calibration, establishing metrological traceability [16]. | For reference methods, this is a genuine requirement; purity and commutability are critical [19] [16]. |
| Processed Calibrators | To calibrate both the test and routine comparative methods before the experiment. | Values should be traceable to a higher-order reference. Lot-to-lot variation should be monitored [20]. |
| Quality Control Materials | To monitor the stability and performance of both methods during the data collection period. | Should include at least two levels (normal and pathological); used to verify precision [17]. |
| Reagent Lots | The specific chemical reactants required for the analytical measurement. | New reagent lots for the test method should be documented; comparison of reagent lots is a common study goal [20]. |
The choice between a reference method and a routine method as the comparator hinges on the fundamental goal of the validation study. Selecting a reference method is the definitive approach for establishing the trueness of a new candidate method and anchoring its results within an internationally recognized traceability chain [17] [16]. This is the ideal choice for the initial validation of a novel method or when claiming metrological traceability. In contrast, comparing a new method to an established routine method answers a more practical clinical question: will the new method yield results that are equivalent to the one currently in use, thereby avoiding disruptive changes to clinical decision thresholds? [18] This pragmatic approach is common when replacing an old analyzer or verifying a new reagent lot. By understanding the distinct applications, strengths, and limitations of each approach—and by implementing a rigorous experimental protocol—researchers can generate defensible data to support confident decisions in the drug development and clinical testing pipeline.
In the highly regulated world of pharmaceutical development, the selection and validation of an analytical method are not merely procedural steps; they are critical strategic decisions that directly impact a product's safety, efficacy, and time-to-market. The principle that the method's performance must be rigorously linked to its intended use is foundational to this process. A method designed for stability-indicating purposes, for instance, demands a different scope of validation than one used for in-process testing. This guide provides a structured, comparative framework for selecting and validating analytical methods, underpinned by experimental protocols and data presentation tailored for drug development professionals. By objectively comparing validation approaches, this article aims to equip scientists with the tools to define a method's scope with precision and scientific rigor, ensuring compliance with evolving regulatory standards like the forthcoming ICH Q2(R2) and Q14 [21].
### The Foundation: Validation Parameters & Their Intended Use
The validation parameters required for an analytical method are directly dictated by its application. A one-size-fits-all approach is neither efficient nor compliant. The following table summarizes how the intended use of a method determines the necessary validation experiments, framing them within the broader validation lifecycle [21].
Table 1: Linking Method Performance to Intended Use: A Validation Parameter Guide
| Validation Parameter | Stability-Indicating Method | Potency Assay (Release Testing) | Impurity Identification | In-Process Control (IPC) |
|---|---|---|---|---|
| Specificity/Selectivity | Mandatory (Must demonstrate separation from degradation products) | Mandatory (Must demonstrate separation from known impurities) | Mandatory (Primary parameter; e.g., via HRMS) | Conditionally Required (Depends on process stream complexity) |
| Accuracy | Mandatory (Across the range, including degraded samples) | Mandatory (For the active ingredient) | Not Typically Applicable | Recommended (For the measured attribute) |
| Precision (Repeatability) | Mandatory | Mandatory | Mandatory (System suitability) | Sufficient for process decision |
| Intermediate Precision/Ruggedness | Mandatory | Mandatory | Recommended | Often not required |
| Linearity & Range | Mandatory (Wide range to cover degradation) | Mandatory (Established around specification) | Mandatory (For semi-quantitative estimation) | Sufficient range for process variation |
| Detection Limit (LOD) | Conditionally Required (For low-level impurities) | Not Typically Required | Mandatory | Not Typically Required |
| Quantitation Limit (LOQ) | Mandatory (For specified impurities) | Not Typically Required | Mandatory (For reporting thresholds) | Not Typically Required |
| Robustness | Highly Recommended | Mandatory | Highly Recommended | Conditionally Required |
This risk-based approach to validation, as outlined in ICH Q14, ensures that resources are allocated efficiently while fully supporting the method's claim. For example, a stability-indicating method requires rigorous demonstration of specificity towards degradation products, while an IPC method may prioritize speed and robustness over the ability to detect trace impurities [21].
### Comparative Experimental Design: A Case Study on HPLC Method Development
To illustrate the practical application of these principles, consider the development of a High-Performance Liquid Chromatography (HPLC) method for a new small molecule drug substance. The method must serve two distinct purposes: as a potency assay for release and a related substances method for stability studies. The experimental protocols below are designed to compare different methodological approaches objectively.
### Experimental Protocol 1: Specificity Forced Degradation Study
Objective: To demonstrate the method's ability to accurately measure the analyte in the presence of components that may be expected to be present, such as impurities, forced degradation products, and excipients [21].
Sample Preparation:
- Acid Degradation: Treat the drug substance with 0.1M HCl at 60°C for 1 hour. Neutralize.
- Base Degradation: Treat the drug substance with 0.1M NaOH at 60°C for 1 hour. Neutralize.
- Oxidative Degradation: Treat the drug substance with 3% H₂O₂ at room temperature for 1 hour.
- Thermal Degradation: Expose the solid drug substance to 70°C for 1 week.
- Photolytic Degradation: Expose the solid drug substance to UV and visible light as per ICH Q1B.
- Control: Prepare a untreated standard solution.
Chromatographic Conditions:
- Column: C18, 150 mm x 4.6 mm, 3.5 µm
- Mobile Phase A: 0.1% Formic acid in water
- Mobile Phase B: 0.1% Formic acid in acetonitrile
- Gradient: 5% B to 95% B over 25 minutes
- Flow Rate: 1.0 mL/min
- Detection: UV Diode Array Detector (DAD), 210-400 nm
- Injection Volume: 10 µL
Data Analysis: Chromatograms of stressed samples are compared to the control. The method is deemed specific if the analyte peak is pure (as confirmed by DAD peak purity assessment) and baseline separated from all degradation peaks.
### Experimental Protocol 2: Precision & Accuracy Study for Potency
Objective: To determine the closeness of agreement between a series of measurements and the true value (accuracy) and the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions (precision) [21].
Sample Preparation:
- Prepare a stock solution of the drug substance reference standard.
- Prepare nine sample preparations at three concentration levels (80%, 100%, and 120% of the target assay concentration) in triplicate, spiked into a placebo mixture.
Chromatographic Conditions: Use the isocratic mode derived from the specificity study for the main peak assay.
Data Analysis:
- Accuracy: Calculate the percent recovery for each prepared concentration. The mean recovery should be between 98.0% and 102.0%.
- Precision (Repeatability): Calculate the relative standard deviation (RSD) of the nine measurements. The RSD should be ≤ 2.0%.
### Comparative Data Presentation: Objective Performance Evaluation
The quantitative data generated from the experimental protocols should be summarized into clearly structured tables for objective comparison. This practice is crucial for communicating complex datasets efficiently [22] [23].
Table 2: Specificity Profile of Candidate HPLC Methods Under Forced Degradation
| Degradation Condition | Method A (Proposed Gradient) | Method B (Legacy Isocratic) |
|---|---|---|
| Acid Degradation | Peak Purity Pass; Resolution from main peak: 4.5 | Peak Purity Fail; Co-elution observed |
| Base Degradation | Peak Purity Pass; Resolution from main peak: 3.8 | Peak Purity Pass; Resolution from main peak: 1.2 |
| Oxidative Degradation | Two degradation products resolved (Rs > 2.0) | Three degradation products, one co-elutes with main peak |
| Main Peak Purity (All conditions) | Pass | Fail (Acid & Oxidative) |
Table 3: Precision and Accuracy Data for Potency Assay (n=9)
| Spiked Level (%) | Method A (Proposed) | Method B (Legacy) |
|---|---|---|
| 80% - Mean Recovery (%) | 99.5 | 101.2 |
| 100% - Mean Recovery (%) | 100.1 | 102.5 |
| 120% - Mean Recovery (%) | 99.8 | 103.1 |
| Repeatability (%RSD) | 0.7 | 1.8 |
| Conclusion | Meets acceptance criteria | Fails accuracy at upper levels |
The data clearly demonstrates that Method A is superior for its intended use as a stability-indicating potency assay, while Method B lacks the necessary specificity and accuracy.
### Visualizing the Method Selection Workflow
A logical, structured workflow is essential for robust method selection. The following diagram outlines the critical decision points, from defining the Analytical Target Profile (ATP) to the final method validation, ensuring the scope is always linked to the intended use [21].
### The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of robust analytical methods relies on high-quality materials and instrumentation. The following table details key resources essential for the development and validation of chromatographic methods as discussed in this guide [21].
Table 4: Essential Research Reagent Solutions for HPLC Method Development & Validation
| Item / Reagent | Function / Role in Experimentation |
|---|---|
| High-Purity Reference Standards | Serves as the benchmark for identifying the analyte peak and for quantifying accuracy, linearity, and potency. |
| Chromatography Columns (C18, C8, etc.) | The stationary phase responsible for the separation of the analyte from impurities and degradation products; critical for specificity. |
| Mass Spectrometry-Grade Solvents | Ensure low UV background and minimal ion suppression for sensitive and reproducible detection, especially in LC-MS/MS. |
| Forced Degradation Reagents (e.g., HCl, NaOH, H₂O₂) | Used in stress studies to intentionally generate degradation products and prove the stability-indicating power of the method. |
| Validated Spreadsheet Software / CDS | For statistical calculation of validation parameters (mean, RSD, regression analysis) with built-in data integrity controls (ALCOA+). |
| Diode Array Detector (DAD) | Enables the collection of spectral data across a wavelength range, which is crucial for confirming peak purity in specificity studies. |
| pH Buffers & Mobile Phase Additives | Modify the mobile phase to control ionization, retention, and peak shape, directly impacting method robustness and selectivity. |
Defining the scope of an analytical method is a deliberate, science-driven process that inextricably links performance characteristics to the method's intended use. As demonstrated through comparative experimental data and structured workflows, a one-size-fits-all validation strategy is untenable. A stability-indicating method demands a broader, more rigorous scope—particularly in specificity—than an in-process control method. The trends outlined in ICH Q14 and the adoption of a formal Analytical Procedure Lifecycle approach reinforce this paradigm, moving the industry toward more robust and flexible methods. By adhering to these principles and utilizing a structured toolkit, scientists and drug development professionals can make objective, defensible decisions in comparative method selection, ultimately ensuring product quality and accelerating the delivery of safe and effective therapies to patients.
Designing and Executing a Method-Comparison Experiment
Within the rigorous framework of comparative method selection research, the validation of a new analytical method hinges on the demonstration of its accuracy and reliability against a established comparative method. The cornerstone of this validation process is a well-designed comparison of methods experiment, where the inherent properties of the patient specimens used--their selection, number, and stability--directly influence the credibility of the systematic error estimates obtained. Proper experimental design in this phase is critical for generating data that can robustly support claims about a method's performance, ensuring that subsequent decisions in drug development or clinical practice are based on solid evidence [17] [8]. This guide outlines the core principles and detailed protocols for designing this critical experiment, providing researchers with a structured approach to specimen management.
Specimen Selection and Number: Protocols and Data
The foundation of a successful comparison study lies in the strategic selection and adequate number of patient specimens. These factors determine how well the experiment captures the method's performance across its intended operating range and in the presence of real-world sample variations.
Experimental Protocol for Specimen Selection and Procurement
Objective: To acquire a set of patient specimens that accurately represent the entire working range of the method and the spectrum of diseases and conditions the method will encounter in routine use [17].
Methodology:
- Define the Analytical Range: Establish the low, high, and medically relevant decision levels for the analyte. Specimens should be selected to cover this entire range uniformly, rather than relying on randomly received samples.
- Identify Sample Sources: Procure leftover patient specimens from routine laboratory testing that fall within the desired concentration intervals.
- Ensure Sample Diversity: Deliberately include specimens from a diverse patient population, representing various pathophysiological conditions (e.g., different diseases, renal or hepatic impairment) that might be encountered in clinical practice. This helps test the method's specificity.
- Avoid Interference: If the new method uses a different chemical principle, be aware that individual sample matrices may cause interference. Specimens showing large discrepancies in initial testing should be investigated for potential interferences [17].
Quantitative Guidelines for Specimen Number
The appropriate number of specimens is a balance between statistical reliability and practical feasibility. The following table summarizes key recommendations:
Table 1: Recommendations for Number of Specimens in Comparison of Methods Experiment
| Factor | Minimum Recommendation | Enhanced Recommendation | Rationale |
|---|---|---|---|
| Total Specimens | 40 specimens [17] | 100 to 200 specimens [17] | A minimum of 40 provides a baseline for estimating systematic error. A larger number (100-200) is superior for assessing method specificity and identifying matrix-related interferences. |
| Data Distribution | Cover the entire working range [17] | Evenly distributed across the analytical measurement range | A wide range of concentrations is more critical than a large number of specimens clustered in a narrow range. It enables reliable linear regression analysis. |
| Analysis Schedule | Analyze specimens over a minimum of 5 days [17] | Extend over 20 days (2-5 specimens/day) [17] | Analysis across multiple days and analytical runs helps minimize systematic biases that could occur in a single run and provides more realistic precision estimates. |
Specimen Stability and Handling: Protocols and Data
Specimen stability is a critical variable that, if not controlled, can introduce pre-analytical error that is misattributed to the analytical method itself. A detailed protocol is essential to ensure observed differences are due to the methods being compared, and not specimen degradation.
Experimental Protocol for Specimen Stability and Handling
Objective: To ensure that all patient specimens remain stable throughout the testing process, thereby guaranteeing that results from both the test and comparative method reflect the true analyte concentration at the time of sampling.
Methodology:
- Define Stability Limits: Prior to the study, consult literature or perform preliminary tests to establish the stability of the analyte in the sample matrix (e.g., serum, plasma) under various storage conditions (room temperature, refrigerated, frozen).
- Synchronize Analysis: Analyze each patient specimen by the test method and the comparative method within two hours of each other [17]. This minimizes time-dependent degradation as a source of error.
- Standardize Handling: Define and systematize specimen handling procedures prior to study initiation. This includes:
- Centrifugation: Time and speed for serum/plasma separation.
- Aliquoting: Use of preservatives if necessary.
- Storage: Conditions (e.g., refrigeration at 4°C, freezing at -20°C or -70°C) for specimens not analyzed immediately.
- Freeze-Thaw Cycles: Limit the number of freeze-thaw cycles, as this can degrade many analytes.
- Document Procedures: Document all handling and storage steps meticulously to ensure consistency and for future reference.
Stability Considerations for Common Analytes
Table 2: Specimen Stability and Handling Considerations for Common Analytes
| Analyte Category | Stability Considerations | Recommended Handling Protocol |
|---|---|---|
| General Chemistry | Many stable for hours at room temp, days refrigerated. | Analyze within 2 hours or separate serum/plasma and refrigerate if analysis is delayed. |
| Labile Analytes (e.g., Ammonia, Lactate) | Highly unstable at room temperature. | Place samples on ice immediately after collection and analyze within 30 minutes. |
| Proteins & Enzymes | Generally stable for longer periods. | Refrigerate for short-term storage; freeze at -20°C or lower for long-term preservation. |
Workflow and Data Analysis
The following diagram illustrates the complete end-to-end workflow for the comparison of methods experiment, integrating the principles of specimen selection, stability, and subsequent data analysis.
Comparison of Methods Experimental Workflow
Data Analysis Protocol
Objective: To graphically and statistically analyze the paired data to identify outliers, understand the relationship between methods, and estimate the systematic error of the test method [17].
Methodology:
- Graphical Inspection:
- Difference Plot: Plot the difference between the test and comparative method results (test - comparative) on the y-axis against the comparative method result on the x-axis. This helps visualize constant and proportional errors and identify outliers [17].
- Comparison Plot: Plot the test method result (y-axis) against the comparative method result (x-axis). Draw a visual line of best fit. This is useful for methods not expected to show 1:1 agreement.
- Action: Identify and reanalyze any discrepant results while specimens are still available.
- Statistical Calculations:
- For Wide Analytical Ranges: Use linear regression (least squares) to calculate the slope (b) and y-intercept (a) of the regression line (Y = a + bX). The systematic error (SE) at a critical medical decision concentration (Xc) is calculated as: SE = Yc - Xc, where Yc = a + bXc [17].
- For Narrow Analytical Ranges: Calculate the average difference (bias) between the two methods using a paired t-test. The standard deviation of the differences describes the distribution of these differences [17].
- Correlation Coefficient (r): Use primarily to assess if the data range is wide enough for reliable regression analysis (r ≥ 0.99 is desirable) [17].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and solutions essential for conducting a robust comparison of methods experiment.
Table 3: Essential Research Reagents and Materials for Method Comparison Studies
| Item | Function / Description |
|---|---|
| Well-Characterized Patient Pool | Leftover, de-identified patient specimens covering the analytical measurement range. Serves as the primary resource for assessing method performance with real-world matrices. |
| Reference Method or Material | A high-quality method with documented correctness or Standard Reference Material (SRM) traceable to a definitive method. Used as the comparator to assign error to the test method [17]. |
| Quality Control (QC) Materials | Stable control materials at multiple levels (e.g., normal, abnormal). Used to monitor the precision and stability of both the test and comparative methods throughout the study period. |
| Calibrators | Materials of known concentration used to calibrate both analytical instruments. Ensures both methods are standardized against the same traceable basis before specimen analysis. |
| Specialized Collection Tubes | Tubes containing appropriate preservatives (e.g., fluoride/oxalate for glucose) or stabilizers (e.g., protease inhibitors) for labile analytes. Maintains analyte integrity from collection to analysis [17]. |
In the scientific method, the integrity of experimental data is paramount. For researchers, scientists, and drug development professionals, decisions regarding data collection strategies are foundational to robust comparative method selection and validation. A critical aspect of this planning involves determining the appropriate number of technical replicates—single, duplicate, or triplicate measurements—and constructing a realistic timeframe for the data collection process. This guide objectively compares these measurement approaches, providing supporting experimental data and contextualizing them within the broader framework of validation parameters for research. The choice between these strategies represents a fundamental trade-off between statistical power, resource efficiency, and error management, all of which directly impact the validity and reliability of research outcomes.
Understanding Replicates: Biological vs. Technical
Experimental science vitally relies on replicate measurements and their statistical analysis. However, not all replicates are created equal, and understanding their distinction is crucial for proper experimental design [24].
- Biological Replicates are distinct samples from different biological specimens (e.g., blood samples from various individual patients, or multiple mice in a study). They are essential for controlling for natural biological variability and form the bedrock of sound statistical analysis that allows for generalization to a population [25] [24].
- Technical Replicates are repetitions of the technical, experimental procedure using the same biological sample (e.g., running the same test multiple times with the same sample). They primarily serve to determine and control for the variability introduced by the method itself, such as pipetting inaccuracies or instrument noise [25].
A common and critical error in scientific research is misusing technical replicates to draw biological inferences. As demonstrated in a bone marrow colony experiment, using ten replicate plates from a single mouse pair (technical replicates) to calculate statistical significance (P < 0.0001) creates a false impression of robustness. In reality, since all replicates came from the same biological source, the experiment only represents a single biological comparison (n=1) and cannot support generalized conclusions about the mouse genotypes [24]. Technical replicates monitor experimental performance, but cannot provide evidence for the reproducibility of the main biological result [24].
Table 1: Comparison of Replicate Types
| Feature | Biological Replicates | Technical Replicates |
|---|---|---|
| Definition | Measurements from distinct biological sources | Repeated measurements from the same biological sample |
| Primary Purpose | Account for natural biological variability; allow generalization | Assess and control methodological variability |
| What they test | The hypothesis across a population | The precision of the assay itself |
| Statistical Power | Increase n for statistical inference |
Do not increase n for biological inference |
| Example | Using cells from 10 different human donors | Measuring the same sample solution 3 times in the same assay |
Comparative Analysis: Single, Duplicate, and Triplicate Measurements
The number of technical replicates per sample is a key decision point, balancing data quality with practical constraints like cost, time, and sample availability.
Single Measurements
Single measurements, using one well or test per sample, maximize throughput and resource efficiency [25].
- Pros: Allows for the maximum number of samples to be measured with a given assay. Ideal for high-throughput applications where testing a large sample volume is the priority, such as in quality control of biological manufacturing [25].
- Cons: The most significant drawback is the inability to identify outliers or erroneous data points. Faulty measurements will go unnoticed, potentially compromising the entire dataset [25].
- Ideal Use Cases:
- Qualitative or semi-quantitative analyses where results are positive/negative [25].
- Time-course experiments where samples from the same source are measured at intervals, allowing outliers to be identified relative to other time points [25].
- Studies where cohorts are large enough that individual errors do not compromise group mean analysis [25].
Duplicate Measurements
Duplicate measurements are widely considered the "sweet spot" for many applications, including ELISA, offering a practical compromise between error management and throughput [25].
- Pros: Enables a level of error compensation by calculating a mean of two values. Crucially, it allows for the detection of measurement deviations by calculating variability (%CV or standard deviation) between the two replicates [25].
- Cons: While duplicates can identify high variability, they cannot reliably correct for it. If the %CV exceeds a predefined threshold (commonly 15-20%), the sample should be disregarded and remeasured, as there is no systematic way to identify which of the two measurements is faulty [25].
- Ideal Use Cases: The recommended approach for the vast majority of quantitative assays where a balance of accuracy and efficiency is required [25].
Triplicate Measurements
Triplicate measurements provide the highest level of precision and error control at the cost of significantly reduced throughput and higher reagent use [25].
- Pros: The mean from triplicates is significantly more likely to represent the true value. Most importantly, triplicates allow for both error identification and correction. Outliers can be identified against the mean and excluded, allowing the sample to be quantified based on the remaining two measurements [25].
- Cons: Reduces throughput capacity by a third and uses more resources per sample [25].
- Ideal Use Cases: Indicated when data precision is paramount, or when working with rare or valuable samples where remeasurement may not be an option [25].
Table 2: Comparison of Single, Duplicate, and Triplicate Measurement Strategies
| Feature | Single Measurement | Duplicate Measurements | Triplicate Measurements |
|---|---|---|---|
| Throughput | Highest | Moderate | Lowest |
| Resource Efficiency | Highest | Moderate | Lowest |
| Error Detection | No | Yes | Yes |
| Error Correction | No | No | Yes (via outlier exclusion) |
| Best For | Qualitative screening, high-throughput | Most quantitative assays, ideal balance | Maximum precision, critical quantification |
| Data Analysis | Group means (large cohorts only) | Mean of two; exclude sample if %CV high | Mean of two or three; exclude outliers systematically |
Experimental Protocols and Data Presentation
Example Protocol: Bone Marrow Colony Assay
The following methodology, adapted from a study on the protein Biddelonin (BDL), illustrates the proper use of replicates [24].
- Objective: To test the hypothesis that BDL is required for a full response of bone marrow colony-forming cells to the cytokine HH-CSF.
- Materials:
- Wild-type (WT) and homozygous Bdl gene-deleted mice.
- Recombinant HH-CSF cytokine.
- Soft agar growth medium, 35 x 10 mm Petri dishes.
- Hemocytometer or flow cytometer for cell counting.
- Dissecting microscope.
- Method:
- Prepare bone marrow cell suspensions from a WT mouse and a Bdl−/− mouse (littermates).
- Adjust cell suspensions to a concentration of 1 × 10^5 cells per milliliter.
- Add 1 ml aliquots of the cell suspension to ten Petri dishes per condition.
- Add 10 µl of either saline (control) or HH-CSF to the respective plates, creating four sets:
- Set 1: WT cells + saline
- Set 2: Bdl−/− cells + saline
- Set 3: WT cells + HH-CSF
- Set 4: Bdl−/− cells + HH-CSF
- Incubate plates for one week.
- Count the number of colonies (>50 cells) per plate using a dissecting microscope.
- Data Analysis: The ten plates per condition are technical replicates. They provide a robust mean value for the response of that single biological replicate (one mouse of each genotype). To draw a biologically valid conclusion, the entire experiment must be repeated multiple times using different mice (biological replicates) [24].
Table 3: Sample Data from Bone Marrow Colony Assay (Colonies per Plate) [24]
| Plate Number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Mean | SD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WT + Saline | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0.2 | 0.42 |
| Bdl−/− + Saline | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0.3 | 0.67 |
| WT + HH-CSF | 61 | 59 | 55 | 64 | 57 | 69 | 63 | 51 | 61 | 61 | 60.1 | 4.73 |
| Bdl−/− + HH-CSF | 48 | 34 | 50 | 59 | 37 | 46 | 44 | 39 | 51 | 47 | 45.5 | 7.47 |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Materials and Their Functions in Cell-Based Assays
| Item | Function in Experiment |
|---|---|
| Biological Model (e.g., Mice) | Provides the biological system to test the hypothesis; using multiple animals is the source of biological replicates. |
| Cytokines/Growth Factors (e.g., HH-CSF) | The active molecule being tested to elicit a specific cellular response. |
| Cell Culture Medium (e.g., Soft Agar) | Provides the necessary nutrients and environment for cells to grow and proliferate. |
| Cell Counting Device (e.g., Hemocytometer) | Ensures accurate and consistent cell numbers are plated across all experiments, a key step in technical precision. |
| Imaging/Analysis Instrument (e.g., Microscope) | Used to quantify the experimental endpoint (e.g., colony count) in an objective and measurable way. |
Crafting a Realistic Data Collection Timeline
A well-planned timeline is a roadmap to successful research execution, ensuring feasibility and maintaining the quality and integrity of the study [26]. Key factors to consider include:
- Assessing the Study's Scope: Evaluate the extent of data collection. Consider the methods used (surveys, interviews, experimental methods), availability of resources (equipment, lab space), and the number of biological and technical replicates required. Always factor in time for unforeseen delays [26].
- Preparation is Key: This phase involves fine-tuning methods, conducting pilot tests to refine questions and approaches, and ensuring proficiency with equipment. Data storage and management plans should also be established during this time [26].
- Flexibility and Adaptation: Research is inherently unpredictable. A successful timeline is well-planned yet adaptable, allowing for adjustments in response to challenges while maintaining open communication with supervisors or team members [26].
To create an effective timeline, researchers should:
- Create a Work Breakdown Structure (WBS) by breaking the project into smaller, manageable tasks.
- Identify dependencies between tasks to sequence them correctly.
- Establish clear milestones to track progress.
- Use project management tools to visualize and enforce the timeline [26].
Visual Workflows and Decision Diagrams
The following diagram outlines the logical decision process for selecting a measurement strategy, incorporating both technical and biological replicate considerations.
Diagram 1: Decision workflow for selecting measurement approaches and ensuring robust design.
In comparative method selection research, graphical data analysis serves as the critical first step for assessing method agreement and identifying potential biases. Difference plots and scatter diagrams provide visual means to evaluate whether two analytical methods could be used interchangeably without affecting patient results or scientific conclusions [27]. These tools are indispensable in method validation, allowing researchers to detect patterns, trends, and outliers that might not be apparent through statistical analysis alone [28] [27].
The quality of method comparison studies determines the validity of conclusions, making proper experimental design and graphical presentation essential components of analytical research [27]. This guide examines the complementary roles of scatter diagrams and difference plots within a comprehensive method validation framework, providing researchers with practical protocols for implementation and interpretation.
Comparative Analysis of Primary Graphical Methods
Table 1: Core Characteristics of Scatter Plots and Difference Plots
| Characteristic | Scatter Plot | Difference Plot |
|---|---|---|
| Primary Function | Visualizes relationship between two methods across measurement range [29] | Displays agreement between methods by plotting differences against a reference [27] |
| Axes Configuration | Test method (y-axis) vs. reference/comparison method (x-axis) [29] | Differences between methods (y-axis) vs. average values or reference method (x-axis) [27] |
| Bias Detection | Identifies constant and proportional bias through visual pattern assessment [29] | Directly visualizes magnitude and pattern of differences across measurement range [17] |
| Ideal Relationship | Data points fall along identity line (y = x) [29] | Differences scatter randomly around zero line with no systematic pattern [27] |
| Data Variability Assessment | Shows whether variability is constant (constant SD) or value-dependent (constant CV) [29] | Reveals whether spread of differences remains consistent across measurement range [17] |
| Outlier Identification | Visual detection of points deviating from overall relationship pattern [27] | Direct visualization of differences exceeding expected agreement limits [28] |
Experimental Protocols for Method Comparison Studies
Specimen Selection and Handling
A properly designed method comparison experiment requires careful specimen selection and handling protocols. Researchers should select a minimum of 40 patient specimens, though 100 specimens are preferable to identify unexpected errors due to interferences or sample matrix effects [17] [27]. Specimens must be carefully selected to cover the entire clinically meaningful measurement range rather than relying on random selection [17] [27].
Temporal factors significantly impact results validity. Specimens should be analyzed within 2 hours of each other by test and comparative methods to prevent degradation, unless specific preservatives or handling methods extend stability [17]. The experiment should span multiple days (minimum of 5) and include multiple analytical runs to mimic real-world conditions and minimize systematic errors from a single run [17] [27].
Measurement Procedures
For measurement protocols, duplicate measurements are recommended for both current and new methods to minimize random variation effects [17] [27]. If duplicates are performed, the mean of two measurements should be used for plotting; with three or more measurements, the median is preferred [27]. Sample sequence should be randomized to avoid carry-over effects, and all samples should ideally be analyzed on the day of collection [27].
When differences between methods are observed, researchers should implement a protocol for immediate graphical inspection during data collection to identify discrepant results while specimens remain available for reanalysis [17]. This proactive approach confirms whether observed differences represent true methodological variance or procedural errors.
Statistical Analysis Following Graphical Inspection
While graphical methods provide initial assessment, statistical calculations quantify systematic errors. For data spanning a wide analytical range, linear regression statistics are preferred, providing slope (b), y-intercept (a), and standard deviation of points about the line (sy/x) [17]. The systematic error (SE) at critical decision concentrations is calculated as: Yc = a + bXc, then SE = Yc - X_c [17].
For narrow analytical ranges, researchers should calculate the average difference (bias) between methods along with the standard deviation of differences [17]. Correlation analysis alone is inadequate for method comparison as it measures association rather than agreement, and similarly, t-tests often fail to detect clinically relevant differences [27].
Research Reagent Solutions for Method Comparison
Table 2: Essential Materials for Method Comparison Studies
| Research Reagent/Material | Function in Experiment |
|---|---|
| Reference Method Materials | Provides benchmark with documented correctness through comparative studies with definitive methods or traceable reference materials [17] |
| Patient Specimens (n=40-100) | Serves as test matrix covering clinical measurement range and disease spectrum; must represent actual testing conditions [17] [27] |
| Preservation Reagents | Maintains specimen stability during 2-hour analysis window; may include serum separators, anticoagulants, or stabilizers [17] |
| Quality Control Materials | Verifies proper performance of both test and comparative methods throughout study duration [17] |
| Statistical Software | Facilitates regression analysis, difference calculations, and graphical generation; options include R, Python, SPSS, SAS, or specialized tools [30] |
Workflow Visualization for Graphical Analysis
Graphical Analysis Workflow
Advanced Applications and Interpretation Guidelines
Specialized Difference Plot Applications
Beyond basic difference visualization, specialized applications enhance methodological assessment. The Bland-Altman plot specifically graphs differences between test and comparative method against their average values, incorporating bias lines and confidence intervals to assess agreement limits [31]. When distribution normality is questionable, researchers should supplement difference plots with histograms and box plots of differences to validate statistical assumptions [31].
For methods with differing specificities, difference plots can incorporate statistical assessment of the standard deviation of differences to evaluate aberrant-sample bias potentially indicating matrix effects [28]. These advanced applications transform difference plots from simple visual tools to quantitative assessment instruments.
Visual Interpretation Criteria
Systematic interpretation protocols ensure consistent graphical analysis. For scatter plots, researchers should assess whether points form a constant-width band (indicating constant standard deviation) or a band narrowing at small values (suggesting constant coefficient of variation) [29]. Data crossing the identity line suggests concentration-dependent bias requiring further investigation [31].
Difference plot interpretation focuses on random scatter around zero without systematic patterns [27]. The presence of trends (e.g., differences increasing with concentration magnitude) indicates proportional bias, while consistent offset above or below zero suggests constant bias [17]. Outliers should be investigated for potential methodological interferences or specimen-specific issues [27].
Difference plots and scatter diagrams provide complementary visual approaches for initial method comparison assessment. When implemented according to standardized experimental protocols with appropriate specimen selection and statistical validation, these graphical tools form the foundation of rigorous method validation frameworks. Their continued relevance in pharmaceutical research and clinical science stems from their unique ability to transform complex methodological relationships into intuitively accessible visual information, guiding researchers toward appropriate statistical testing and ultimately supporting robust comparative method selection decisions.
In the field of analytical science and drug development, the selection and validation of analytical methods is a critical process that ensures the reliability, accuracy, and precision of measurement data. Statistical calculations form the backbone of this comparative method selection, providing the objective framework needed to make informed decisions about method suitability. Within the context of validation parameters for comparative method selection research, three statistical methodologies emerge as fundamental: linear regression, bias estimation, and correlation analysis. These tools collectively enable researchers to quantify the relationship between methods, estimate systematic errors, and evaluate the strength of agreement, forming a comprehensive statistical toolkit for method comparison studies [17] [18] [32].
The importance of these statistical calculations extends beyond mere analytical convenience; they represent a rigorous approach to demonstrating that a new method performs equivalently to an established one, or that parallel methods can be used interchangeably in clinical or pharmaceutical settings. As regulatory authorities increasingly emphasize data-driven decision making in drug development, the proper application and interpretation of these statistical tools becomes paramount for successful method validation and adoption [33] [34] [32]. This guide provides a comprehensive comparison of these fundamental statistical approaches, supported by experimental data and detailed protocols to assist researchers in selecting appropriate validation strategies.
Comparative Analysis of Linear Regression Approaches
Linear regression serves as a fundamental statistical tool in method comparison studies, primarily used to model the relationship between measurements obtained from two different methods. When comparing a test method with a comparative method, regression analysis helps characterize both constant and proportional differences between the methods [17].
Ordinary Least Squares (OLS) Regression
The OLS approach estimates the regression coefficients by minimizing the sum of squared vertical distances between observed data points and the fitted regression line. For a method comparison study, the model takes the form Y = a + bX, where Y represents results from the test method, X represents results from the comparative method, a is the y-intercept (indicating constant difference), and b is the slope (indicating proportional difference) [17] [35]. The OLS estimator is calculated as β̂OLS = (X'X)⁻¹X'y, where X is the matrix of predictor variables and y is the vector of responses [35].
Despite its widespread use, OLS regression performs optimally only when specific assumptions are met: no multicollinearity among predictors, no influential outliers, constant error variance, and correct model specification [35]. Violations of these assumptions, particularly multicollinearity or the presence of outliers, can lead to unstable coefficient estimates with inflated variances, compromising the reliability of method comparison conclusions [35].
Advanced Regression Techniques for Challenging Data Conditions
Ridge Regression: To address multicollinearity issues, ridge regression introduces a bias parameter k to the diagonal elements of the X'X matrix, resulting in the estimator β̂k = (X'X + kI)⁻¹X'y [35]. This approach stabilizes coefficient estimates at the cost of introducing slight bias, often yielding superior performance in mean squared error (MSE) compared to OLS when multicollinearity is present [35].
Robust Ridge M-Estimators: For datasets affected by both multicollinearity and outliers, Two-Parameter Robust Ridge M-Estimators (TPRRM) integrate dual shrinkage with robust M-estimation [35]. Simulation studies demonstrate that TPRRM consistently achieves the lowest MSE, particularly in heavy-tailed and outlier-prone scenarios commonly encountered in real-world analytical data [35].
Table 1: Comparison of Linear Regression Methods in Method Comparison Studies
| Method | Key Formula | Optimal Use Cases | Performance Metrics |
|---|---|---|---|
| Ordinary Least Squares (OLS) | β̂ = (X'X)⁻¹X'y | No multicollinearity, normal errors, no outliers | Unbiased but vulnerable to multicollinearity |
| Ridge Regression | β̂k = (X'X + kI)⁻¹X'y | Multicollinearity present | Biased but reduced variance, improved MSE |
| Two-Parameter Robust Ridge (TPRRM) | β̂q,k = q̑(X'X + kI)⁻¹X'y | Multicollinearity with outliers | Lowest MSE in heavy-tailed distributions |
Bias Estimation Methodologies
Bias estimation represents a fundamental component of method comparison studies, providing a measure of the systematic difference between measurement methods. Proper quantification of bias is essential for determining whether two methods can be considered equivalent for their intended purpose [18] [32].
Experimental Design for Bias Assessment
A well-designed comparison of methods experiment requires careful planning to ensure reliable bias estimation. A minimum of 40 patient specimens is recommended, carefully selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application [17]. The specimens should be analyzed within a short time frame (typically within two hours of each other) to prevent specimen degradation from affecting the observed differences [17]. To minimize the impact of run-to-run variation, the experiment should span several different analytical runs on different days, with a minimum of 5 days recommended [17].
The choice of comparative method significantly influences the interpretation of bias estimates. When possible, a reference method with documented correctness should be used, allowing any observed differences to be attributed to the test method [17]. When comparing two routine methods, large and medically unacceptable differences require additional investigation through recovery and interference experiments to identify which method is inaccurate [17].
Statistical Approaches to Bias Quantification
Mean Difference: For comparisons where the difference between methods is constant across the measuring range, the mean difference provides a straightforward estimate of bias [20]. This approach is particularly suitable when comparing parallel instruments or reagent lots using the same measurement principle [20]. The mean difference is calculated as the average of (test result - comparative result) across all samples [17] [20].
Bias as a Function of Concentration: When the difference between methods varies with concentration, simple mean difference fails to adequately characterize the systematic error. In such cases, linear regression analysis provides a more nuanced approach to estimating bias [17]. The systematic error (SE) at a given medical decision concentration (Xc) is determined by first calculating the corresponding Y-value (Yc) from the regression line (Yc = a + bXc), then computing SE = Yc - Xc [17]. This approach requires a sufficient number of data points spread throughout the measuring range to reliably fit the regression model [20].
Bland-Altman Analysis: The Bland-Altman plot has emerged as a preferred methodology for assessing agreement between methods [18]. This approach involves plotting the difference between methods against the average of the two measurements for each specimen. The overall mean difference represents the bias, while the standard deviation of the differences describes the random variation around this bias [18]. The limits of agreement, calculated as bias ± 1.96 standard deviations, provide an interval within which 95% of differences between the two methods are expected to fall [18].
Table 2: Bias Estimation Methods in Method Comparison Studies
| Method | Calculation | Interpretation | Data Requirements |
|---|---|---|---|
| Mean Difference | Σ(test - reference)/n | Constant systematic error | Wide concentration range recommended |
| Regression-Based Bias | SE = (a + bXc) - Xc | Concentration-dependent error | 40+ samples across measuring range |
| Bland-Altman Limits of Agreement | Bias ± 1.96SD | Expected range of differences | Paired measurements, normal differences |
Correlation Analysis in Method Comparison
While correlation analysis is frequently included in method comparison studies, its proper application and interpretation require careful consideration to avoid misleading conclusions about method agreement.
The Role and Misuse of Correlation Coefficients
The correlation coefficient (r) quantifies the strength of the linear relationship between two methods but does not directly measure agreement [17]. A high correlation coefficient does not necessarily indicate that two methods agree; it merely shows that as one method gives higher results, so does the other [17]. This distinction is crucial in method validation, where the focus should be on whether methods can be used interchangeably rather than whether they correlate.
The correlation coefficient is mainly useful for assessing whether the range of data is wide enough to provide good estimates of the slope and intercept in regression analysis [17]. When r is 0.99 or larger, simple linear regression calculations generally provide reliable estimates; when r is smaller than 0.99, additional data collection or more sophisticated regression approaches may be necessary [17].
Advanced Correlation Considerations
In method comparison studies, the correlation coefficient is influenced by both the true relationship between methods and the range of analyte concentrations in the study specimens [17]. A wide concentration range tends to produce higher correlation coefficients, potentially creating a misleading impression of agreement if the data range is artificially expanded. Conversely, a narrow concentration range around a clinically relevant decision point may yield a lower correlation coefficient even when methods show good agreement at that critical level.
Experimental Protocols for Method Comparison Studies
Sample Size and Selection Protocol
The quality of a method comparison study depends more on obtaining a wide range of test results than simply a large number of test results [17]. Specimens should be carefully selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application [17]. For initial comparisons, a minimum of 40 patient specimens is recommended, though 100-200 specimens may be necessary to thoroughly evaluate method specificity, particularly when the new method employs a different chemical reaction or measurement principle [17].
To implement this protocol:
- Identify critical medical decision concentrations for the analyte
- Collect specimens spanning from below the lowest to above the highest decision level
- Include pathological specimens that represent common interferences encountered in practice
- Ensure specimens are fresh and stable for the duration of testing
- Analyze specimens within two hours by both methods to minimize degradation effects [17]
Data Collection and Measurement Protocol
The reliability of method comparison data depends on proper measurement procedures. While common practice involves analyzing each specimen singly by both test and comparative methods, duplicate measurements provide significant advantages [17]. Ideally, duplicates should be different samples analyzed in different runs or at least in different order rather than back-to-back replicates on the same sample [17].
Implementation steps:
- Process test and comparative method analyses within close time proximity
- Randomize the order of analysis between methods to avoid sequence effects
- Include quality control materials to monitor method performance throughout the study
- Perform duplicate measurements where possible to identify sample mix-ups or transposition errors
- Immediately investigate any large differences between methods while specimens are still available [17]
Data Analysis Protocol
A systematic approach to data analysis begins with graphical exploration followed by appropriate statistical calculations [17] [18].
Graphical Analysis Steps:
- Create difference plots (test minus comparative versus comparative result) for methods expected to show one-to-one agreement
- Create comparison plots (test versus comparative) for methods not expected to show one-to-one agreement
- Visually inspect for outliers, systematic patterns, and relationship linearity
- Identify any specimens with large differences for repeat analysis [17]
Statistical Analysis Steps:
- Calculate appropriate statistics based on data range and relationship
- For wide analytical ranges, compute linear regression statistics (slope, intercept, standard error of estimate)
- For narrow analytical ranges, calculate mean difference (bias) and standard deviation of differences
- Estimate systematic error at critical medical decision concentrations
- Compute correlation coefficient primarily to assess data range adequacy [17]
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials for Method Comparison Studies
| Material/Resource | Function in Method Comparison | Key Considerations |
|---|---|---|
| Patient Specimens | Provide biological matrix for method comparison | Cover entire measuring range; include pathological states |
| Reference Materials | Establish traceability and accuracy assessment | Certified values with uncertainty documentation |
| Quality Control Materials | Monitor method performance during study | Multiple concentration levels covering clinical range |
| Statistical Software | Perform complex calculations and generate graphs | Capable of regression, Bland-Altman, and advanced analyses |
| Data Management System | Organize and track paired measurements | Maintain specimen integrity and result linkage |
Workflow and Statistical Relationships
The statistical calculations compared in this guide—linear regression, bias estimation, and correlation analysis—provide complementary approaches for comprehensive method comparison studies. Linear regression characterizes the functional relationship between methods, bias estimation quantifies systematic differences, and correlation analysis assesses the strength of the linear relationship. When applied appropriately within a well-designed experimental framework, these statistical tools enable researchers to make objective, data-driven decisions about method selection and validation. The experimental protocols and comparative data presented herein provide a practical foundation for designing, conducting, and interpreting method comparison studies that meet the rigorous standards required in pharmaceutical research and drug development.
Identifying and Resolving Common Comparison Pitfalls
Handling Outliers and Discrepant Results
In empirical research, particularly in fields requiring high-precision data such as drug development, the presence of outliers and discrepant results presents a significant analytical challenge. Outliers are data points that deviate markedly from other observations in a dataset, potentially due to variability in the measurement or experimental errors [36] [37]. Discrepant results extend this concept to findings from entire studies that conflict with the broader evidence base, such as clinical trials from different settings reporting inconsistent effect estimates [38]. Properly identifying and managing these anomalies is a critical validation parameter for selecting and trusting comparative analytical methods.
The core challenge lies in determining whether an outlier represents a meaningless measurement error that should be suppressed or a valuable, rare event that should be preserved. Similarly, discrepant study-level results may indicate bias or reveal genuine context-dependent effects. This guide provides an objective comparison of the primary techniques for handling such anomalies, complete with experimental data and protocols, to inform robust method selection in scientific research and development.
Core Concepts and Definitions
What Are Outliers and Discrepant Results?
- Outliers: An outlier is an observation that lies an abnormal distance from other values in a random sample from a population [36] [37]. In practice, these are data points that appear to be in contradiction with the rest of the dataset. They may arise from data entry errors, measurement instrument inaccuracies, natural extreme variation, or novel phenomena.
- Discrepant Results: This term refers to systematic inconsistencies in findings between different studies or experimental conditions. A prominent example is illustrated by a 2025 meta-analysis which found that Randomized Clinical Trials (RCTs) conducted in low- and middle-income countries (LMICs) often report larger treatment effects (a Ratio of Odds Ratios, ROR, of 1.73) compared to RCTs from high-income countries (HICs), particularly for patient-reported outcomes [38].
Impact on Data Analysis and Model Performance
The presence of outliers can severely skew the results of statistical analyses and machine learning models. They disproportionately influence measures of central tendency; for instance, the mean is highly sensitive to outliers, whereas the median is more robust [37]. In machine learning, models like Linear Regression and K-Means Clustering are highly susceptible to outliers, which can distort the learned relationships and cluster centroids [36]. Conversely, models such as Decision Trees and Isolation Forests are inherently more resilient [36]. Discrepant results at the study level can lead to false conclusions about a treatment's efficacy, potentially derailing drug development efforts if their source is not properly investigated [38].
Comparative Analysis of Outlier Handling Methods
This section provides an experimental comparison of the most common statistical techniques and machine learning algorithms for outlier detection and handling, evaluating them on key performance metrics relevant to research scientists.
Performance Comparison of Detection Techniques
The following table summarizes the core characteristics, performance, and optimal use cases for five major outlier detection methods, based on a benchmark experiment using a synthetic dataset of customer spending data [39].
Table 1: Comparative Performance of Outlier Detection Techniques
| Method | Underlying Principle | Key Advantage | Key Limitation | Best-Suited Data Type |
|---|---|---|---|---|
| Z-Score | Distance from mean in standard deviations | Simple and fast calculation [39] | Assumes normal distribution; fails on skewed data [39] | Normally distributed data |
| IQR | Data spread within the 25th-75th percentile range | Robust to non-normal data and outliers themselves [37] [39] | Uses a fixed 1.5xIQR threshold which may not be universally optimal [39] | Skewed distributions, non-parametric data |
| Local Outlier Factor (LOF) | Local density deviation of a point compared to its neighbors | Effective at identifying local outliers in clustered data [39] | Computationally intensive; sensitive to parameter choice (k-neighbors) [39] | Data with clusters of different densities |
| Isolation Forest | Random partitioning to isolate observations | Efficient on high-dimensional data; does not require a distance metric [36] [39] | Less interpretable; requires hyperparameter tuning [36] | High-dimensional datasets, large datasets |
| Mahalanobis Distance | Multivariate distance from the centroid, accounting for covariance | Considers the dataset's covariance structure [39] | Sensitive to outliers in the estimation of the covariance matrix itself [39] | Multivariate data with known covariance |
Performance Comparison of Handling Techniques
Once detected, outliers must be handled appropriately. The choice of strategy depends on the context and the suspected nature of the outliers.
Table 2: Comparative Analysis of Outlier Treatment Strategies
| Method | Description | Impact on Data | Risk | Ideal Scenario |
|---|---|---|---|---|
| Trimming/Removal | Complete removal of outlier points from the dataset [36] [37] | Reduces dataset size; can improve model performance if outliers are noise [36] | Loss of information, especially if outliers are meaningful [36] | Outliers are known to be measurement errors |
| Imputation | Replacing outliers with a central value like the median or mean [36] [37] | Preserves dataset size and overall structure | Can reduce natural variance and create artificial "spikes" at the imputed value [36] | Small datasets where removal would lead to significant data loss |
| Winsorization (Capping/Flooring) | Capping extreme values at a specified percentile (e.g., 90th/10th) [36] [37] | Limits extreme value influence without removing data points [36] | Can distort the underlying data distribution [36] | Data with known, logical boundaries (e.g., age, percentage) |
| Transformation | Applying mathematical functions (e.g., log, Box-Cox) to compress data range [36] | Reduces skewness and the relative impact of extreme values | Makes model interpretation more complex [36] | Highly skewed data (e.g., income, biological concentration data) |
Machine Learning Model Resilience
Certain machine learning models are inherently more robust to outliers, which can be a key factor in model selection.
Table 3: Native Resistance of Machine Learning Models to Outliers
| Model | Resilience Level | Reason for Resilience |
|---|---|---|
| Tree-Based Models (e.g., Decision Trees, Random Forests) [36] | High | Splits are based on data partitions and are not influenced by the absolute distance of a single point. |
| Support Vector Machines (SVM) | Medium-High | Can be made robust with appropriate kernel and cost parameter tuning to ignore points far from the decision boundary [36]. |
| K-Nearest Neighbors (KNN) | Medium | Predictions are based on local neighbors, diluting the effect of a single outlier, especially with weighted voting [36]. |
| Linear Models (e.g., Linear/Logistic Regression) [36] | Low | Model coefficients are optimized based on the sum of squared errors, which is heavily influenced by extreme values. |
| K-Means Clustering [36] | Low | Cluster centroids are calculated as the mean of all points in the cluster, which is pulled towards outliers. |
Experimental Protocols and Methodologies
To ensure the reproducibility of the comparisons made in this guide, this section details the experimental protocols for key outlier detection techniques and for investigating discrepant results.
Detailed Protocol for IQR-Based Outlier Detection
The Interquartile Range (IQR) method is a robust, non-parametric technique for identifying outliers [37] [39].
Experimental Workflow:
The following diagram illustrates the logical sequence of steps in the IQR method workflow.
Step-by-Step Procedure:
- Data Preparation: Begin with a one-dimensional array of numerical data. Ensure the data is complete, with any missing values addressed beforehand.
- Sorting: Sort the data in ascending order to facilitate the calculation of percentiles [37].
- Quartile Calculation: Calculate the first quartile (Q1), which is the 25th percentile, and the third quartile (Q3), the 75th percentile. This can be done using a function like
numpy.percentile[39]. - IQR Calculation: Compute the Interquartile Range (IQR) as IQR = Q3 - Q1. This represents the middle 50% of the data [37] [39].
- Boundary Definition: Establish the lower and upper bounds for "normal" data points:
- Lower Bound = Q1 - 1.5 * IQR
- Upper Bound = Q3 + 1.5 * IQR
- Outlier Identification: Iterate through the dataset and flag any data point that falls below the lower bound or above the upper bound. These flagged points are considered outliers [37] [39].
Detailed Protocol for Z-Score-Based Outlier Detection
The Z-score method is parametric and best suited for data that is approximately normally distributed [37] [39].
Step-by-Step Procedure:
- Parameter Calculation: For your dataset, calculate the population mean (μ) and standard deviation (σ).
- Z-Score Computation: For each data point (Xi) in the dataset, compute its Z-score using the formula: Z = (Xi - μ) / σ. The Z-score indicates how many standard deviations the point is from the mean [39].
- Threshold Application: Define a Z-score threshold, commonly set at an absolute value of 3. Any data point with |Z-score| > 3 is classified as an outlier, as it lies beyond three standard deviations from the mean, an event that is highly improbable under a normal distribution [37] [39].
Methodology for Analyzing Discrepant Clinical Trial Results
The investigation of discrepant results between RCTs from LMICs and HICs provides a template for handling study-level discrepancies [38].
Experimental Workflow:
The following diagram outlines the systematic process for identifying and analyzing the source of discrepant results between study groups.
Step-by-Step Procedure:
- Study Identification: Systematically identify relevant studies for analysis. The referenced study used meta-analyses from leading general medical journals and the Cochrane Database (2018-2023) [38].
- Grouping and Inclusion: Within each meta-analysis, classify RCTs into exposed (sponsored by and enrolling in LMICs) and control (sponsored by and enrolling in HICs) groups. The use of a negative control helps isolate the effect of interest [38].
- Data Transformation: Transform all reported effect estimates into a common metric, such as Odds Ratios (ORs), to ensure comparability [38].
- Comparative Metric Calculation: For each meta-analysis, calculate a Ratio of Odds Ratios (ROR) by comparing the combined OR from LMIC trials to the combined OR from HIC trials. An ROR > 1 indicates a larger effect size in LMICs [38].
- Pooling and Subgroup Analysis: Pool the RORs across all included meta-analyses to get an overall estimate. Conduct pre-specified subgroup analyses, for instance, by type of outcome (patient-reported, investigator-assessed, hard outcomes like mortality) and by the risk of bias of the included trials [38].
The Scientist's Toolkit: Key Reagents and Computational Solutions
This section details essential research reagents and computational tools critical for implementing the methodologies discussed in this guide, particularly in a pharmaceutical development context.
Table 4: Essential Research Reagent Solutions for Experimental Validation
| Item/Category | Function/Description | Example Use-Case in Validation |
|---|---|---|
| Certified Reference Materials (CRMs) | Highly characterized materials with certified property values, used for calibration and method validation. | Establishing measurement accuracy and traceability when developing a new bioanalytical assay (e.g., HPLC). |
| Quality Control (QC) Samples | Samples with known, stable analyte concentrations (low, medium, high) prepared in the same matrix as study samples. | Monitoring assay performance and stability during a run; identifying systematic drift or outliers. |
| Stable Isotope-Labeled Internal Standards | Analytically identical versions of the target molecule labeled with heavy isotopes (e.g., Deuterium, C-13). | Correcting for analyte loss during sample preparation and mitigating matrix effects in mass spectrometry. |
| Robust Statistical Software/Libraries | Programming libraries (e.g., Scikit-learn in Python) that implement robust statistical and ML algorithms. |
Employing Isolation Forest or LOF for high-dimensional outlier detection in -omics data (genomics, proteomics). |
The handling of outliers and discrepant results is not a one-size-fits-all process but a critical component of method validation. The experimental data and protocols presented in this guide demonstrate that the choice of technique must be guided by the nature of the data and the research question. For outliers, robust methods like IQR and model-based approaches like Isolation Forest offer significant advantages over parametric methods like Z-score for real-world, non-normal data. For discrepant results at the study level, a systematic investigative approach, as shown in the clinical trial example, is essential to determine whether discrepancies stem from bias or genuine effect modification. For researchers in drug development, integrating these rigorous assessment protocols into the method selection framework is paramount for generating reliable, reproducible, and actionable scientific evidence.
In analytical science and drug development, method comparison studies are essential for determining whether a new measurement procedure can satisfactorily replace an established one. A fundamental challenge arises when the difference between methods is not consistent across the measurement range—a phenomenon known as non-constant bias. Unlike fixed systematic error that remains constant regardless of concentration, non-constant bias manifests as differences between methods that increase or decrease as the analyte concentration changes [18] [40]. This specific form of bias can be proportional (where the difference scales with concentration) or follow more complex relationships that traditional statistical approaches often fail to detect [27].
Understanding and identifying non-constant bias is critical for researchers and scientists because it directly impacts methodological commutability. When bias varies with concentration, the acceptability of a new method may differ across the clinically relevant range, potentially leading to misinterpretation of results at specific decision thresholds [40] [17]. This guide examines detection methodologies, statistical approaches, and interpretation frameworks for addressing non-constant bias, providing drug development professionals with practical tools for rigorous method validation.
Experimental Design for Detecting Non-Constant Bias
Fundamental Design Considerations
Proper experimental design is prerequisite for reliable detection of non-constant bias. Key considerations include:
Sample Selection and Range: A minimum of 40 patient specimens is recommended, carefully selected to cover the entire clinically meaningful measurement range [17] [27]. The specimens should represent the spectrum of diseases and conditions expected in routine application. For assessing specificity similarities between methods, larger numbers (100-200 specimens) may be necessary [17].
Measurement Protocol: Analyze specimens within 2 hours of each other by both methods to minimize stability effects [17]. Perform measurements over multiple days (at least 5) and multiple runs to mimic real-world conditions and minimize the impact of run-specific artifacts [27]. Duplicate measurements are preferred to identify outliers and transcription errors [17].
Method Comparison Approach: The established method should ideally be a reference method with documented correctness, though routine methods may serve as comparators with appropriate interpretation caveats [17]. When comparing two routine methods, additional experiments (recovery, interference) may be needed to identify which method contributes observed biases [17].
Experimental Workflow
The following diagram illustrates the comprehensive experimental workflow for detecting non-constant bias:
Experimental Workflow for Non-Constant Bias Detection
Statistical Analysis Approaches
Inadequate Methods for Bias Detection
Common statistical approaches often fail to adequately detect or quantify non-constant bias:
Correlation Analysis: Correlation coefficient (r) measures the strength of linear relationship between methods but cannot detect proportional or constant bias [27]. Perfect correlation (r=1.00) can exist even when methods demonstrate substantial, clinically unacceptable differences [27].
t-Tests: Both paired and unpaired t-tests primarily assess differences in mean values and may miss concentration-dependent trends [27]. With small sample sizes, t-tests may fail to detect clinically meaningful differences, while with large samples, they may flag statistically significant but clinically irrelevant differences [27].
Recommended Statistical Techniques
| Method | Application | Bias Detection Capability | Requirements | Limitations |
|---|---|---|---|---|
| Bland-Altman Difference Plots [18] [27] | Visual assessment of agreement across concentration range | Constant and proportional bias | Paired measurements across analytical range | Subjective interpretation; may need log transformation for proportional bias [40] |
| Linear Regression [17] [41] | Quantification of constant and proportional error | Slope indicates proportional bias; intercept indicates constant bias | Wide concentration range; r > 0.99 for reliable estimates [17] | Assumes error only in y-direction; limited with narrow range [40] [41] |
| Deming Regression [40] [27] | Error in both methods | More accurate slope and intercept estimates with measurement error in both axes | Estimate of error ratio (λ); specialized software [40] [41] | Requires knowledge of analytical errors; more complex calculation [40] |
| Passing-Bablok Regression [40] [27] | Non-parametric approach; robust against outliers | No distributional assumptions; handles heteroscedastic data | Sufficient data points for reliable estimates | Computationally intensive; limited with small sample sizes [40] |
Implementing Difference Plots with Bias Statistics
The Bland-Altman difference plot is a fundamental tool for visualizing non-constant bias [18]. This approach plots the difference between methods (test method minus reference method) against the average of the two methods [18] [27]. The plot includes:
- Bias Line: The mean difference between all paired measurements [18]
- Limits of Agreement: Bias ± 1.96 standard deviations of the differences [18]
- Pattern Analysis: Visual inspection for concentration-dependent trends
When differences increase or decrease with concentration, the plot may reveal proportional bias, necessitating log transformation or ratio-based analysis [40]. The following diagram illustrates the decision process for interpreting difference plots:
Decision Process for Interpreting Difference Plots
Advanced Regression Techniques for Bias Quantification
When non-constant bias is suspected, advanced regression techniques provide more accurate quantification:
Deming Regression: Accounts for measurement error in both methods, requiring an estimate of the ratio of variances (λ) between the methods [40] [41]. This approach provides more reliable estimates of slope and intercept when both methods have comparable measurement errors [41].
Passing-Bablok Regression: A non-parametric method based on the median of all possible pairwise slopes [40] [27]. This approach is robust against outliers and does not require assumptions about error distributions, making it suitable for data with heteroscedasticity or non-normal error distributions [40].
The systematic error (SE) at medically important decision concentrations (Xc) can be calculated from regression parameters:
For linear regression: Yc = a + bXc, then SE = Yc - Xc [17]
This allows estimation of bias at critical decision levels, which is essential for assessing clinical impact [17].
Establishing Acceptance Criteria for Non-Constant Bias
Defining Clinically Acceptable Bias
Determining whether detected non-constant bias is clinically significant requires pre-defined acceptance criteria based on:
Biological Variation Models: Bias should ideally not exceed 0.25 times the within-subject biological variation for "desirable" performance, which limits the proportion of results outside reference intervals to less than 5.8% [40].
Clinical Outcome Considerations: For analytes with specific clinical decision thresholds (e.g., glucose for diabetes diagnosis), bias at these critical concentrations is more important than average bias across the range [40].
State-of-the-Art Performance: When biological variation data or outcome studies are unavailable, current best performance of established methods may serve as benchmarks [27].
Communicating Findings and Implications
When non-constant bias exceeds acceptable limits:
Method Interchangeability: Methods should not be used interchangeably without establishing concentration-specific correction factors or limitations [27]
Reference Interval Updates: Reference intervals may require revision if method differences are clinically significant [40]
Clinical Notification: Healthcare providers should be informed of method differences, particularly at critical decision thresholds [40]
Essential Research Reagent Solutions
The following reagents and materials are essential for conducting robust method comparison studies:
| Reagent/Material | Function in Method Comparison | Specification Guidelines |
|---|---|---|
| Patient-Derived Specimens [17] [27] | Primary test material for comparison studies | 40-100 specimens minimum; cover entire clinical range; various disease states |
| Reference Materials [40] | Trueness verification for both methods | Certified reference materials; CDC/NIST sources; appropriate matrix composition |
| Quality Control Materials [17] | Monitoring analytical performance during study | Multiple concentration levels; stable for study duration |
| Preservation Reagents [17] | Maintaining specimen stability | Appropriate for analyte (e.g., fluoride/oxalate for glucose, heparin for electrolytes) |
| Calibrators [17] | Ensuring proper method calibration | Traceable to reference materials; method-specific formulations |
Detecting and addressing non-constant bias requires careful experimental design, appropriate statistical analysis, and clinically relevant interpretation. Difference plots with bias statistics provide intuitive visualization, while advanced regression techniques like Deming and Passing-Bablok regression offer robust quantification of proportional and constant bias components. By implementing these protocols and establishing clinically driven acceptance criteria, researchers and drug development professionals can make informed decisions about method comparability, ensuring measurement reliability across the analytical range and maintaining data integrity in pharmaceutical research and patient care.
In the rigorous world of scientific research and drug development, the correlation coefficient, denoted as r, is often the first statistical measure consulted to understand relationships between variables. This value, ranging from -1 to +1, quantifies the strength and direction of a linear relationship. However, relying solely on this single number provides an incomplete picture and can lead to flawed interpretations and decisions. For researchers and scientists engaged in comparative method selection, a deeper statistical analysis is imperative. This guide outlines the critical parameters necessary to move beyond r and achieve a robust, validated interpretation of statistical output, ensuring that conclusions are both scientifically sound and reliable for critical applications such as drug development pipelines.
The Limitations of the Correlation Coefficient (r)
The correlation coefficient, while useful, has significant limitations that researchers must acknowledge. Its primary function is to measure the strength and direction of a linear relationship between two variables. Consequently, it may not properly detect or represent curvilinear relationships and can be significantly skewed by outliers in the data [42]. Furthermore, a correlation coefficient only provides insight into bivariate relationships and cannot account for the influence of additional, potentially confounding, variables.
Most critically, the value of r itself does not indicate whether an observed relationship is statistically reliable or likely due to random chance. A correlation coefficient, no matter how strong, is merely a point estimate derived from a sample of data. Interpreting it without additional context is a common pitfall that can undermine the validity of research findings, particularly when comparing the performance of analytical methods or assessing new biomarkers in clinical trials [6].
Essential Parameters for Robust Interpretation
To fully interpret a correlation analysis, several key parameters must be examined alongside the correlation coefficient. The following table summarizes these essential components.
Table 1: Key Statistical Parameters for Interpreting Correlation
| Parameter | Description | Interpretation Question |
|---|---|---|
| Sample Size (N) | The number of paired observations used to calculate r. | Is the analysis powered by a sufficient amount of data? |
| p-value | The probability that the observed correlation is due to chance, assuming no true relationship exists in the population. | Is the observed correlation statistically significant? |
| Confidence Interval (CI) | A range of plausible values for the population correlation coefficient (ρ). | What is the potential range of the true correlation in the broader population? |
| Coefficient of Determination (R²) | The proportion of variance in one variable that is explained by the other. | What is the practical strength and predictive utility of the relationship? |
| Scatterplot | A visual representation of the data points for the two variables. | Is the relationship linear? Are there outliers or a heteroscedastic pattern? |
The p-Value and Sample Size (N)
The p-value helps determine the statistical significance of the correlation. It tests the null hypothesis that the population correlation coefficient (ρ) is zero [43]. A low p-value (typically < 0.05) provides evidence to reject this null hypothesis, suggesting that the correlation is unlikely to be a fluke of the specific sample collected [42]. However, it is crucial to understand that a statistically significant correlation does not necessarily imply a strong relationship. With a very large sample size (N), even a very weak correlation can produce a highly significant p-value [44] [45]. Therefore, the p-value and sample size must always be considered together.
Confidence Intervals
A confidence interval (CI) provides a more informative alternative to a single p-value. It offers a range of values that is likely to contain the true population correlation coefficient (ρ) with a certain level of confidence (e.g., 95%). A wide CI indicates uncertainty about the true strength of the relationship, while a narrow CI suggests a more precise estimate. If a 95% CI includes zero, it is equivalent to a p-value greater than 0.05, indicating the correlation is not statistically significant.
The Coefficient of Determination (R²)
The square of the correlation coefficient, known as the coefficient of determination (R²), is a highly practical metric. It represents the proportion of variance in one variable that can be explained or accounted for by the other variable. For instance, a correlation of r = 0.60, which might be considered a "moderate" relationship, yields an R² of 0.36. This means only 36% of the variance in one variable is explained by the other, leaving 64% unexplained by this relationship [42]. This metric is vital for assessing the predictive utility of a correlation.
Experimental Protocol for Correlation Analysis
A standardized protocol is essential for conducting and reporting a rigorous correlation analysis, especially in a regulated environment like drug development.
Table 2: Experimental Protocol for Correlation Analysis
| Step | Action | Rationale & Best Practices |
|---|---|---|
| 1. Study Design | Define the research question, variables, and data collection method. | Ensure data integrity and relevance. Pre-register analysis plans to reduce bias. |
| 2. Data Collection | Gather paired measurements for the two variables. | Record data meticulously. Check for and document any potential sources of measurement error. |
| 3. Assumption Checking | Create a scatterplot and assess for linearity, outliers, and homoscedasticity. | Verify that a linear model is appropriate. Non-linear relationships require different analytical approaches. |
| 4. Coefficient Selection | Choose the appropriate type of correlation coefficient. | Use Pearson's r for normally distributed continuous data. Use Spearman's rho or Kendall's Tau for non-normal data, ordinal data, or data with many tied ranks [44]. |
| 5. Statistical Output | Calculate r, N, and the p-value. | Use reliable statistical software (e.g., SPSS, JMP) that provides these outputs clearly [45] [42]. |
| 6. Advanced Metrics | Calculate the 95% CI for r and compute R². | These metrics provide crucial context for the strength and precision of the observed relationship. |
| 7. Interpretation & Reporting | Synthesize all parameters to form a conclusion. | Report r, N, and the p-value together. Discuss the results in the context of the CI and R², and with reference to the scatterplot. |
The following workflow diagram visualizes the key decision points in this analytical process.
Guidelines for Interpreting Strength and Significance
Interpreting the strength of a correlation coefficient is not universally standardized, and conventions can vary by field. The table below synthesizes common interpretations from different scientific disciplines to provide a general framework [44].
Table 3: Interpreting the Strength of a Correlation Coefficient
| Value of | r | Chan et al. (Medicine) | Dancey & Reidy (Psychology) | Quinnipiac University (Politics) | |
|---|---|---|---|---|---|
| 0.9 - 1.0 | Very Strong | Strong | Very Strong | ||
| 0.7 - 0.9 | Moderate to Very Strong | Strong | Very Strong | ||
| 0.5 - 0.7 | Moderate | Moderate | Strong | ||
| 0.3 - 0.5 | Fair | Weak to Moderate | Moderate to Strong | ||
| 0.2 - 0.3 | Poor | Weak | Weak | ||
| 0.0 - 0.2 | Poor to None | Weak | Negligible to Weak |
It is critical to remember that these labels are subjective. When reporting, researchers should explicitly state the value of r, the p-value, and the sample size, and avoid over-relying on verbal labels [44]. A finding of "r = 0.5, p < 0.001, N=200" provides a much clearer picture of a moderate but highly significant correlation than the label "moderate correlation" alone.
Application in Drug Development and Research
In the high-stakes field of drug development, moving beyond the simple correlation coefficient is not just best practice—it is essential for making valid decisions. For example, in the 2025 Alzheimer's disease drug development pipeline, biomarkers play a crucial role in determining trial eligibility and serving as outcomes [6]. When a new biomarker is correlated with a clinical endpoint, researchers must assess not just the strength (r) but the precision (CI) and statistical significance (p-value) of that relationship to validate the biomarker's utility.
Furthermore, with the rise of AI in drug discovery, where machine learning models inform target prediction and compound prioritization, understanding the nuances of statistical relationships is key to building reliable predictive frameworks [46] [47]. A model might show a strong correlation (r) in training data, but without examining significance and potential confounding factors, its translational predictivity could be low.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key software and statistical tools that are essential for conducting thorough correlation analyses.
Table 4: Essential Tools for Statistical Correlation Analysis
| Tool / Reagent | Type | Primary Function in Correlation Analysis |
|---|---|---|
| SPSS | Statistical Software Suite | Provides comprehensive correlation output, including Pearson's r, Sig. (2-tailed) p-value, and sample size N for pairwise or listwise analyses [45]. |
| JMP | Statistical Discovery Software | Guides users through the correlation analysis process, from creating scatterplots to calculating the r and p-values, with an emphasis on visual data exploration [42]. |
| Graphing Software (e.g., Sigma, Excel) | Data Visualization Tool | Creates scatterplots to visually assess the linearity and nature of the relationship between two variables before calculating r [48]. |
| ColorBrewer | Accessibility Tool | Assists in choosing color palettes for scatterplots and other data visualizations that are colorblind-safe and meet WCAG contrast guidelines, ensuring accessibility for all audiences [49] [50]. |
Optimizing for Specificity and Robustness Against Matrix Effects
Matrix effects represent a critical challenge in bioanalytical chemistry, particularly in liquid chromatography-tandem mass spectrometry (LC-MS/MS), where they can severely impact assay specificity, robustness, and data reliability. These effects cause ion suppression or enhancement, leading to inaccurate quantification of target analytes [51]. For researchers and drug development professionals, selecting analytical methods with minimal matrix interference is paramount for generating valid, reproducible results. This guide provides a systematic comparison of current methodologies for evaluating and mitigating matrix effects, supported by experimental data and standardized protocols aligned with regulatory requirements.
The persistence of matrix effects across diverse sample types necessitates method-specific optimization strategies. In environmental analysis, PFAS (per- and polyfluoroalkyl substances) quantification in sludge demonstrates how complex matrices require enhanced extraction approaches to overcome analytical challenges [52]. Similarly, in pharmaceutical and clinical settings, the accuracy of glucosylceramide quantification in cerebrospinal fluid depends critically on comprehensive matrix effect assessment [51]. Understanding these method-specific parameters enables scientists to select optimal approaches for their particular analytical challenges.
Comparative Analysis of Matrix Effect Evaluation Methods
Standardized Protocols from Regulatory Guidelines
International guidelines provide varying approaches for matrix effect assessment, with differences in methodological requirements and acceptance criteria. The table below summarizes key recommendations from major regulatory bodies:
Table 1: Comparison of Matrix Effect Evaluation in International Guidelines
| Guideline | Matrix Lots Required | Concentration Levels | Evaluation Protocol | Key Assessment Parameters | Acceptance Criteria |
|---|---|---|---|---|---|
| EMA (2011) | 6 | 2 | Post-extraction spiked matrix vs neat solvent | Absolute and relative matrix effects; IS-normalized matrix factor | CV <15% for MF |
| ICH M10 (2022) | 6 | 2 (3 replicates) | Evaluation of matrix effect precision and accuracy | Matrix effect in relevant patient populations | Accuracy <15%; Precision <15% |
| CLSI C62A (2022) | 5 | 7 | Post-extraction spiked matrix vs neat solvent | Absolute %ME; CV of peak areas; IS-norm %ME | CV <15% for peak areas |
| CLSI C50A (2007) | 5 | Not specified | Pre- and post-extraction spiked matrix and neat solvent | Absolute matrix effect; extraction recovery; process efficiency | Refers to Matuszewski et al. |
The integrated approach recommended by CLSI C50A provides the most comprehensive assessment by evaluating matrix effects, recovery, and process efficiency within a single experiment [51]. This methodology offers a more complete understanding of the factors influencing method performance compared to approaches focusing solely on matrix effects.
Experimental Data from Method Application Studies
Practical applications of these protocols demonstrate their effectiveness across different sample matrices:
Table 2: Experimental Data from Matrix Effect Optimization Studies
| Study Focus | Sample Matrix | Optimized Parameters | Performance Improvement | Key Quantitative Findings |
|---|---|---|---|---|
| PFAS Analysis [52] | Sewage sludge | Liquid-solid ratio (30 mL/g); Methanol ammonia hydroxide (99.5:0.5, v/v); Oscillation time (60 min, 300 rpm); pH = 3 before SPE | Significant improvement in method precision and correctness | Recovery ratios: 85.2%-112.8% (L/S-20); 88.3%-116.3% (L/S-30); ME minimization: 72.5%-117.3% |
| Glucosylceramide Analysis [51] | Human cerebrospinal fluid | Three complementary approaches in single experiment; Pre- and post-extraction spiking | Comprehensive understanding of factors influencing method performance | Addressed limited sample volume and endogenous analytes; Systematic evaluation protocol provided |
| General LC-MS/MS [53] | Various bioanalytical matrices | Chromato-graphic performance optimization | Essential for method assessment, optimization and transfer | Matrix effects strongly suppress ionization efficiency and reduce sensitivity |
The sludge study demonstrated that optimized extraction conditions significantly improved recovery ratios, particularly for long-chain PFAS (C ≥ 8) which have stronger hydrophobicity and affinity to sludge flocs [52]. The higher liquid-solid ratio (30 mL/g) proved crucial for effective separation of these challenging analytes.
Detailed Methodologies for Matrix Effect Assessment
Integrated Experimental Protocol for Comprehensive Evaluation
The integrated approach based on Matuszewski et al. involves preparing three sample sets from different matrix lots to assess matrix effects, recovery, and process efficiency simultaneously [51]:
- Set 1 (Neat Solution): Prepared by spiking standard and internal standard solutions in mobile phase B to establish baseline response without matrix interference
- Set 2 (Post-extraction Spiked): Blank matrix taken through extraction procedure then spiked with standards to evaluate matrix effects
- Set 3 (Pre-extraction Spiked): Standards added to matrix before extraction to assess recovery and process efficiency
This protocol requires at least five different matrix lots evaluated at two concentration levels (low and high QC levels) with a fixed internal standard concentration [51]. Corresponding blank samples for each set and matrix lot should be prepared to subtract endogenous baseline signals.
PFAS Extraction Optimization Protocol for Complex Matrices
The enhanced full-process method for PFAS analysis in sludge involves a rigorously validated extraction workflow [52]:
- Liquid-Solid Ratio Optimization: Test ratios of 10, 20, and 30 mL/g TS to determine optimal extraction efficiency
- Extraction Solvent Selection: Compare alkaline methanol, acetonitrile, and methanol-ammonia hydroxide (99.5:0.5, v/v)
- Extraction Conditions: Optimize oscillation time (30-90 minutes) and speed (200-400 rpm)
- pH Adjustment: Adjust to pH = 3 before solid-phase extraction (SPE)
- Clarification Procedure: Implement effective cleanup to remove interfering compounds
This method was systematically compared with three previously reported extraction methods: ASTM D2216, HJ 1334-2023, and EPA method 1633A [52]. The optimized approach demonstrated superior performance across 48 different PFAS compounds in diverse sludge samples.
Visualization of Method Evaluation Workflow
Diagram 1: Matrix Effect Assessment Workflow
This workflow illustrates the integrated approach for assessing matrix effects, recovery, and process efficiency within a single experimental design, facilitating comprehensive method validation [51].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Matrix Effect Minimization
| Reagent/Category | Specific Examples | Function in Method Optimization |
|---|---|---|
| Extraction Solvents | Methanol-ammonia hydroxide (99.5:0.5, v/v); Acetonitrile; Alkaline methanol | Weaken hydrophobic/electrostatic interactions between analytes and matrix; Improve elution efficiency [52] |
| Internal Standards | Isotopically labeled analogs (e.g., GluCer C22:0-d4); 13C2-PFDoA for PFAS analysis | Compensate for variability introduced by matrix and recovery fraction; Improve data quality [51] [52] |
| SPE Sorbents | C18, WAX, MAX cartridges; Mixed-mode polymers | Remove interfering compounds; Reduce co-elution of matrix components; Customize selectivity [52] |
| LC-MS Mobile Phase | Ammonium formate; Formic acid; LC-MS grade methanol, acetonitrile, isopropanol | Enhance chromatographic separation; Improve ionization efficiency; Reduce source contamination [51] |
| Calibration Standards | Native PFAS standards (48 compounds); GluCer isoforms (C16:0, C18:0, C24:1) | Establish quantification reference; Monitor method performance over time; Ensure accuracy [52] [51] |
The selection of appropriate research reagents is critical for developing robust methods resistant to matrix effects. Methanol-ammonia hydroxide mixtures have demonstrated particular effectiveness for PFAS extraction from complex sludge matrices by effectively weakening the electrostatic and hydrophobic interactions that impede separation efficiency [52]. Similarly, isotopically labeled internal standards are essential for compensating variability in recovery and matrix effects, with their effectiveness documented across multiple studies [52] [51].
Optimizing for specificity and robustness against matrix effects requires a systematic approach integrating multiple evaluation strategies. The comparative data presented demonstrates that methods incorporating comprehensive assessment of matrix effects, recovery, and process efficiency within a single experimental design provide superior reliability for quantitative analysis. Environmental and bioanalytical applications consistently show that method performance depends critically on parameter optimization, including extraction conditions, solvent selection, and internal standard implementation.
Researchers should prioritize methodologies aligned with regulatory guidelines while recognizing that matrix-specific optimization remains essential. The protocols and experimental data presented herein provide a foundation for selecting and validating methods that ensure specificity and robustness across diverse analytical challenges in drug development and environmental monitoring.
Final Validation and Regulatory Alignment for Method Acceptance
Assessing Method Acceptability Against Medical Decision Levels
Method acceptability is a cornerstone of analytical validation in pharmaceutical development and clinical science. It reflects the extent to which a new measurement procedure (test method) demonstrates sufficient agreement with an established comparative method to be considered interchangeable without affecting clinical decision-making [27] [54]. Establishing method acceptability requires rigorous experimental design and statistical analysis to determine whether the observed differences between methods (bias) fall within predefined performance specifications at critical medical decision concentrations [17].
This systematic overreliance on correlation coefficients represents a fundamental misunderstanding of method comparison statistics. A perfect correlation can exist alongside clinically unacceptable bias, rendering such analyses misleading for acceptability determinations [27]. This guide establishes robust frameworks for designing, executing, and interpreting method comparison studies to objectively assess acceptability against medically relevant criteria.
Theoretical Framework of Method Acceptability
The theoretical framework for method acceptability extends beyond simple statistical measures to encompass multiple validity dimensions. Acceptability is a multi-faceted construct reflecting whether users consider a method appropriate based on anticipated or experienced responses [54]. In method comparison, this translates to several component constructs:
- Analytical Validity: The closeness of agreement between measured values of the test and comparative methods [55]
- Perceived Effectiveness: The belief that the method will achieve its intended purpose in a real-world context [54]
- Practical Burden: The perceived amount of effort required to implement and maintain the method [54]
- Ethicality: The extent to which the method fits with ethical standards and values [54]
This multi-construct nature necessitates a comprehensive assessment strategy that integrates quantitative performance metrics with practical implementation considerations.
Experimental Design for Method Comparison Studies
Core Design Principles
A well-designed method comparison experiment is fundamental to obtaining reliable acceptability assessments. Key design considerations include:
Sample Size and Selection: A minimum of 40 patient specimens is recommended, with 100-200 preferred to identify matrix-specific interferences [17] [27]. Specimens should cover the entire clinically meaningful measurement range and represent the spectrum of diseases expected in routine application. Specimen quality and concentration range are more critical than sheer quantity [17].
Timeframe and Replication: The experiment should span several different analytical runs across a minimum of 5 days, with 20 days ideal for robust assessment [17]. Duplicate measurements are strongly recommended to identify sample mix-ups, transposition errors, and other mistakes that could compromise results [17].
Specimen Handling and Stability: Specimens should generally be analyzed within two hours of each other by both methods unless stability data supports longer intervals [17]. Handling procedures must be carefully standardized to ensure observed differences reflect analytical performance rather than preanalytical variables.
Comparative Method Selection
The choice of comparative method fundamentally influences acceptability interpretation. When possible, a reference method with documented correctness through definitive method comparison or traceable reference materials should be selected [17]. With routine methods as comparators, observed differences require careful interpretation, and additional experiments may be needed to identify which method produces inaccurate results [17].
Table 1: Key Experimental Design Parameters for Method Comparison Studies
| Design Parameter | Minimum Recommendation | Optimal Recommendation | Rationale |
|---|---|---|---|
| Sample Size | 40 specimens | 100-200 specimens | Identifies matrix effects and interferences [17] [27] |
| Experimental Duration | 5 days | 20 days | Captures long-term performance variation [17] |
| Replication | Single measurements | Duplicate measurements | Detects procedural errors; improves precision [17] |
| Concentration Range | Clinically reportable range | Entire clinically meaningful range | Enables assessment across decision levels [17] |
| Sample Type | Patient specimens | Diverse disease states | Evaluates specificity in intended population [17] |
Statistical Approaches for Assessing Acceptability
Graphical Analysis Methods
Visual data inspection represents the foundational step in method comparison analysis, enabling identification of patterns, outliers, and potential error types.
Difference Plots: Visualize the difference between test and comparative method results (y-axis) against the comparative method values (x-axis) [17]. These plots effectively show systematic error patterns and highlight outliers requiring investigation.
Scatter Plots: Display test method results (y-axis) against comparative method results (x-axis) across the measurement range [27]. These help visualize the analytical range, linearity of response, and general relationship between methods.
Bland-Altman Plots: Graph differences between methods against the average of both methods, highlighting proportional bias and agreement limits [27].
Diagram 1: Statistical Analysis Workflow for Method Comparison Studies. This workflow illustrates the sequential process for analyzing method comparison data, beginning with visual assessment and progressing to statistical evaluation against clinical acceptability criteria.
Quantitative Statistical Methods
Statistical calculations provide numerical estimates of systematic error at medically important decision concentrations:
Linear Regression Analysis: For data covering a wide analytical range, linear regression calculates slope (proportional error), y-intercept (constant error), and standard deviation about the regression line (sy/x) [17]. The systematic error (SE) at a medical decision concentration (Xc) is calculated as:
- Yc = a + bXc
- SE = Yc - Xc [17]
Bias Analysis: For narrow analytical ranges, the average difference between methods (bias) with standard deviation of differences provides appropriate systematic error estimation [17] [27]. This approach is typically used with paired t-test calculations.
Correlation Analysis Limitations: The correlation coefficient (r) primarily assesses whether data range is sufficient for reliable regression estimates rather than method acceptability [17] [27]. Correlation values of 0.99 or greater generally indicate adequate range for linear regression.
Table 2: Statistical Methods for Assessing Systematic Error in Method Comparison
| Statistical Method | Application Context | Outputs | Interpretation |
|---|---|---|---|
| Linear Regression | Wide analytical range(e.g., cholesterol, glucose) | Slope (b)Y-intercept (a)Standard error of estimate (s_y/x) | Slope ≠ 1: Proportional errorIntercept ≠ 0: Constant error [17] |
| Bias Analysis(Paired t-test) | Narrow analytical range(e.g., sodium, calcium) | Mean difference (bias)Standard deviation of differences | Statistical vs. clinical significancemust be distinguished [17] [27] |
| Difference Plot Analysis | All comparison studies | Visual error patternsOutlier identification | Detects concentration-dependentbias and anomalies [17] [27] |
Establishing Performance Specifications for Acceptability
Determining whether observed method differences are medically significant requires establishing acceptability criteria before conducting the comparison experiment. The Milano hierarchy provides a framework for setting evidence-based performance specifications:
- Clinical Outcomes: Direct or indirect evidence linking analytical performance to clinical outcomes [27]
- Biological Variation: Based on components of biological variation of the measurand [27]
- State-of-the-Art: Current capabilities of best-performing laboratories or methods [27]
These specifications define the allowable total error (TE_a) at critical medical decision concentrations, creating objective benchmarks for acceptability determinations. The systematic error observed in method comparison studies should be compared against these established criteria to make evidence-based decisions about method interchangeability.
Implementation Considerations and Research Reagents
Essential Research Reagent Solutions
Successful method comparison studies require carefully characterized materials and reagents:
- Certified Reference Materials: Provide metrological traceability and calibration verification for both test and comparative methods [17] [56]
- Quality Control Materials: Include at least three concentration levels (low, medium, high) spanning the reportable range to monitor assay performance [17]
- Patient Specimen Panels: Carefully selected to represent clinically relevant subpopulations and potential interfering substances [17]
- Stability Testing Reagents: Assess sample integrity under various storage conditions and time intervals [17]
Practical Implementation Framework
Translating comparison results into practical implementation decisions requires systematic evaluation:
- Risk Assessment: Evaluate potential clinical impact of observed biases at critical decision points
- Method Alignment: Determine whether constant or proportional errors can be corrected through calibration adjustment
- Process Integration: Assess workflow compatibility, including sample throughput, hands-on time, and required operator skill
- Verification Monitoring: Establish ongoing quality monitoring protocols to ensure maintained performance
Assessing method acceptability against medical decision levels requires a multifaceted approach integrating rigorous experimental design, appropriate statistical analysis, and clinically relevant performance specifications. By moving beyond correlation coefficients to focus on systematic error estimation at critical decision concentrations, researchers can make evidence-based determinations about method interchangeability. The frameworks presented in this guide provide pharmaceutical developers and clinical researchers with validated protocols for demonstrating method acceptability within comprehensive validation parameters, ultimately supporting the implementation of reliable measurement procedures that safeguard patient care and drug development integrity.
In pharmaceutical research and drug development, the reliability of analytical data is paramount. Analytical method validation provides documented evidence that a laboratory test consistently produces results that are fit for their intended purpose, supporting the identity, strength, quality, purity, and potency of drug substances and products [57]. This process is not a single event but a rigorous, structured exercise that confirms the performance characteristics of an analytical method meet the requirements of its specific application [58]. For researchers and scientists, understanding and correctly applying key validation parameters is a critical competency that ensures regulatory compliance and the generation of scientifically sound data.
The International Council for Harmonisation (ICH) guideline Q2(R2) serves as the primary global standard for validating analytical procedures [57] [59]. This guideline, along with others from regulatory bodies like the FDA, outlines the fundamental parameters that constitute a thorough validation. Among these, Accuracy, Precision, Specificity, Limit of Detection (LOD), Limit of Quantitation (LOQ), and Linearity form the essential core set that establishes the foundation for a method's capability [60] [61]. These parameters collectively answer crucial questions about a method: Does it measure the correct value? Are the results consistent? Does it only respond to the target analyte? How little can it detect and quantify? And is the response proportional to the amount of analyte?
Detailed Analysis of Key Validation Parameters
Accuracy
Accuracy refers to the closeness of agreement between a measured value and a value accepted as either a conventional true value or an accepted reference value [60] [61]. It is typically expressed as the percentage of recovery of a known, added amount of analyte [58]. In practice, accuracy demonstrates that a method is free from significant systematic error and provides results that are "correct" on average.
Experimental Protocol for Assessing Accuracy: A standard protocol for determining accuracy involves analyzing a minimum of nine determinations over a minimum of three concentration levels covering the specified range of the method (for example, three concentrations and three replicates each) [61] [58]. This is typically done by:
- Spiking known quantities of a reference standard of the analyte into a blank matrix (e.g., placebo for a drug product or a synthetic biological fluid).
- Analyzing the spiked samples using the method under validation.
- Calculating the percent recovery for each sample by comparing the measured value to the theoretical (spiked) value.
- Reporting the overall mean recovery and confidence intervals (e.g., ± standard deviation) across all concentration levels [61].
The data should be reported as the percent recovery of the known, added amount. Acceptance criteria are method-specific but generally require mean recovery to be within 80-110% for the assay of a drug product, with tighter ranges often set for impurities [61].
Precision
Precision describes the closeness of agreement (degree of scatter) between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [60] [58]. It is a measure of the method's random error and is usually expressed as the relative standard deviation (%RSD) or coefficient of variation. Precision is investigated at three levels:
- Repeatability (Intra-assay Precision): Assesses precision under the same operating conditions over a short interval of time (e.g., same analyst, same instrument, same day). Guidelines suggest a minimum of six determinations at 100% of the test concentration or nine determinations covering the specified range (e.g., three concentrations with three replicates each) [58].
- Intermediate Precision: Evaluates the impact of within-laboratory variations, such as different days, different analysts, or different equipment. An experimental design where two analysts prepare and analyze replicate samples using different HPLC systems and different standards is typical. Results are compared using statistical tests (e.g., Student's t-test) [58].
- Reproducibility (Ruggedness): Represents the precision between laboratories, as in collaborative studies. This is assessed when transferring a method to a new site [58].
Specificity
Specificity is the ability to assess unequivocally the analyte of interest in the presence of other components that may be expected to be present in the sample matrix, such as impurities, degradants, or excipients [57] [60]. A specific method produces a response for only a single analyte, free from interference. The related term, selectivity, describes the method's capability to distinguish and quantify multiple analytes within a complex mixture [61].
Experimental Protocol for Assessing Specificity: Specificity is demonstrated by challenging the method with samples containing potential interferents and verifying that the method still accurately identifies and quantifies the target compound. Key experiments include:
- Analysis of blank matrix: A sample of the blank matrix (e.g., placebo, biological fluid) should yield no response at the retention time of the analyte.
- Forced degradation studies: The active ingredient is stressed under various conditions (e.g., acid/base hydrolysis, oxidation, thermal degradation, photolysis) to generate degradants. The method must be able to separate the analyte peak from all degradation peaks [61].
- Spiking with interferents: The sample is spiked with known impurities or other components expected to be present. The method's ability to resolve the analyte peak from interferents is quantified using resolution and peak purity tests [58].
- Peak purity verification: Modern techniques like Photodiode-Array (PDA) detection or Mass Spectrometry (MS) are used to confirm that a chromatographic peak is attributable to a single component by comparing spectra across the peak [58].
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
The Limit of Detection (LOD) is the lowest concentration of an analyte in a sample that can be detected, but not necessarily quantified, under the stated experimental conditions. The Limit of Quantitation (LOQ) is the lowest concentration that can be quantitatively determined with acceptable precision and accuracy [58].
Experimental Protocols for Determining LOD and LOQ:
- Signal-to-Noise Ratio (S/N): This common approach, particularly for chromatographic methods, sets the LOD at a concentration that yields a S/N ratio of 3:1, and the LOQ at a S/N of 10:1 [61] [58].
- Standard Deviation of the Response and Slope: The LOD and LOQ can be calculated based on the standard deviation of the response (σ) and the slope (S) of the calibration curve: LOD = 3.3σ/S and LOQ = 10σ/S. The standard deviation can be determined from the regression line itself or from the analysis of blank samples [58].
It is critical to note that after the LOD/LOQ is calculated, an appropriate number of samples at that concentration must be analyzed to experimentally confirm the method's performance meets the definitions [58].
Linearity
Linearity of an analytical procedure is its ability (within a given range) to obtain test results that are directly proportional to the concentration (amount) of analyte in the sample [60]. The range of the method is the interval between the upper and lower concentrations of analyte for which it has been demonstrated that the linearity, precision, and accuracy are acceptable [60] [58].
Experimental Protocol for Assessing Linearity: Linearity is established by preparing and analyzing a series of standard solutions at a minimum of five concentration levels spanning the intended range of the method [58] [59]. For example, a range of 50% to 150% of the target concentration might be used for an assay. The data is then subjected to linear regression analysis, which provides:
- The correlation coefficient (r) or coefficient of determination (r²)
- The y-intercept
- The slope of the regression line
- The residual sum of squares
A visual examination of the plotted calibration curve and a review of the residuals plot are also performed to detect any potential deviations from linearity [61]. Acceptance criteria often include an r² value of not less than 0.99 for assay methods.
Table 1: Summary of Key Validation Parameters and Experimental Protocols
| Parameter | Definition | Typical Experimental Protocol | Common Acceptance Criteria |
|---|---|---|---|
| Accuracy [61] [58] | Closeness of results to the true value. | Analyze a minimum of 9 samples over 3 concentration levels. Report % recovery. | Mean recovery of 80-110% for assay. |
| Precision [58] | Closeness of agreement between individual test results. | Repeatability: 6-9 replicates. Intermediate Precision: 2 analysts, different days/instruments. | %RSD < 2% for assay repeatability. |
| Specificity [60] [58] | Ability to measure analyte unequivocally amid interference. | Analyze blank, stress samples (forced degradation), and samples spiked with impurities. | No interference from blank; resolution > 1.5 between peaks; peak purity confirmed. |
| LOD [58] | Lowest detectable concentration. | Determine via Signal-to-Noise (3:1) or calculation (LOD=3.3σ/S). | Signal-to-Noise ratio ≥ 3:1. |
| LOQ [58] | Lowest quantifiable concentration with precision & accuracy. | Determine via Signal-to-Noise (10:1) or calculation (LOQ=10σ/S). Verify with precision/accuracy at LOQ. | Signal-to-Noise ratio ≥ 10:1; Precision (%RSD) and Accuracy at LOQ meet pre-set criteria. |
| Linearity [58] [59] | Proportionality of response to analyte concentration. | Analyze minimum of 5 concentrations across the range. Perform linear regression. | Correlation coefficient (r) ≥ 0.99 (or r² ≥ 0.98). |
Experimental Protocols and Research Toolkit
Generalized Workflow for a Validation Study
A robust validation study follows a structured plan to ensure all parameters are assessed systematically and documented thoroughly.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of validation protocols relies on a set of high-quality materials and reagents. The following table details key items essential for experiments like the accuracy and linearity assessments described previously.
Table 2: Essential Research Reagents and Materials for Validation Studies
| Item | Function / Purpose | Key Considerations |
|---|---|---|
| Certified Reference Standard [62] | Serves as the benchmark for the analyte with known identity and purity. Used to prepare calibration standards and spiked samples for accuracy. | High purity and well-characterized identity are critical. Must be traceable to a recognized standard. |
| Blank Matrix | The sample material without the analyte. Used to prepare calibration standards and assess specificity by detecting potential interference. | Should be representative of the actual test samples (e.g., placebo for drug product, biological fluid for biomarkers). |
| Chromatographic Columns | The stationary phase for separation in HPLC/UPLC. Critical for achieving specificity (resolution) and robustness. | Different columns (C18, C8, etc.) may be screened during development. A specific column type is defined in the final method. |
| High-Purity Solvents & Reagents | Used to prepare mobile phases, standard solutions, and sample solutions. | Purity is essential to minimize background noise (affecting LOD/LOQ) and avoid introducing interfering peaks (affecting specificity). |
| System Suitability Standards [63] | A reference preparation used to confirm that the chromatographic system is performing adequately before and during the analysis. | Typically a mixture of the analyte and/or known impurities. Used to verify parameters like resolution, tailing factor, and repeatability. |
Comparative Data and Regulatory Context
Validation requirements can differ based on the type of method and its intended use. The concept of "fit-for-purpose" is increasingly important, especially in emerging fields like biomarker analysis, where a direct application of ICH M10 (for pharmacokinetic assays) may not be appropriate due to challenges like the lack of a reference standard identical to the endogenous analyte [62]. The following table provides a comparative overview of typical acceptance criteria for different analytical applications, based on ICH Q2(R2) and related guidelines [57] [58].
Table 3: Comparison of Typical Validation Requirements by Application
| Parameter | Assay (Drug Substance/Product) | Impurity Test (Quantitative) | Impurity Test (Limit Test) |
|---|---|---|---|
| Accuracy | Mean Recovery 98-102% | Mean Recovery 90-107%* | - |
| Precision (%RSD) | NMT 2.0% (Repeatability) | Dependent on level (e.g., < 5% RSD for 1% impurity) | - |
| Specificity | Required. No interference. | Required. Resolution from analyte and other impurities. | Required. Able to detect impurity in presence of analyte. |
| LOD | - | - | Required. Must be below reporting threshold. |
| LOQ | - | Required. Must be at or below reporting threshold. | - |
| Linearity (r²) | Typically > 0.999 | Typically > 0.99 | - |
| Range | 80-120% of test conc. | From reporting level to 120% of specification. | At or near specification level. |
Note: NMT = Not More Than; *Wider range may be acceptable for low-level impurities. Criteria are examples and should be justified based on the method's intended use.
The six parameters of Accuracy, Precision, Specificity, LOD, LOQ, and Linearity form the foundational pillars of analytical method validation. A deep understanding of their definitions, the experimental protocols required to evaluate them, and the appropriate acceptance criteria is non-negotiable for researchers and drug development professionals. This rigorous process, guided by ICH and other regulatory frameworks, transforms an analytical procedure from a mere technical operation into a validated, reliable tool. It provides the documented evidence necessary to ensure that the data generated is trustworthy, ultimately supporting the development and manufacture of safe and effective pharmaceutical products. As the field evolves with new analytical technologies, the fundamental principles of these validation parameters remain the constant bedrock of quality and scientific integrity.
For pharmaceutical companies and drug development professionals, achieving global market access requires simultaneous navigation of multiple regulatory frameworks. The United States Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the International Council for Harmonisation (ICH) represent the cornerstone of pharmaceutical regulation across major markets [64]. While these bodies share the ultimate goal of protecting public health by ensuring that medicines are safe, effective, and of high quality, their regulatory philosophies, processes, and technical requirements differ in significant ways [64] [65]. Understanding these differences is not merely an administrative exercise but a strategic imperative that directly impacts development timelines, costs, and ultimate market access success [64].
This guide provides an objective comparison of the FDA, EMA, and ICH requirements, structured within the context of validation parameters for comparative method selection research. By presenting key differences in organizational structure, approval pathways, scientific standards, and risk management, this analysis equips researchers and drug development professionals with the evidence-based data needed to design robust global development strategies.
Organizational Structures and Legal Frameworks
The most fundamental differences between the FDA and EMA arise from their distinct legal foundations and institutional architectures, which in turn shape all subsequent regulatory processes.
FDA: A Centralized Federal Authority
The FDA operates as a federal agency within the U.S. Department of Health and Human Services, functioning as a centralized regulatory authority with direct decision-making power [64]. Its jurisdiction extends beyond human drugs to include biologics, medical devices, tobacco products, cosmetics, and most foods [65]. For medicinal products, the Center for Drug Evaluation and Research (CDER) evaluates New Drug Applications (NDAs) for small molecules, while the Center for Biologics Evaluation and Research (CBER) handles Biologics License Applications (BLAs) for most biological products [64] [65]. The FDA's model enables relatively swift decision-making, as review teams consist of FDA employees who maintain consistent internal communication [64]. Once the FDA approves a drug, it is immediately authorized for marketing throughout the entire United States [64].
EMA: A Coordinated Network Model
In contrast, the EMA operates as a coordinating body rather than a direct decision-making authority [64]. Based in Amsterdam, it coordinates the scientific evaluation of medicines through a network of National Competent Authorities (NCAs) across EU Member States [64] [66]. For the centralized procedure, the Committee for Medicinal Products for Human Use (CHMP) conducts scientific evaluations through rapporteurs appointed from national agencies [64]. The CHMP issues scientific opinions, which are then forwarded to the European Commission, which holds the legal authority to grant the actual marketing authorization [64] [65]. This decentralized model means that assessments involve experts from multiple countries, potentially bringing broader scientific perspectives but requiring more complex coordination [64].
Table 1: Fundamental Structural Differences Between FDA and EMA
| Parameter | FDA (U.S.) | EMA (EU) |
|---|---|---|
| Legal Authority | Direct approval authority [64] | Provides scientific opinion; European Commission grants authorization [64] [65] |
| Geographic Scope | Single country (nationwide authorization) [64] | 27 EU Member States plus EEA-EFTA countries [65] |
| Regulatory Scope | Drugs, biologics, medical devices, food, cosmetics, tobacco [65] | Human and veterinary medicines only [65] |
| Primary Review Bodies | CDER (drugs), CBER (biologics) [65] | CHMP (Committee for Medicinal Products for Human Use) [64] |
| Inspection Approach | Centralized conduct by federal staff [66] | Decentralized, conducted by National Competent Authorities [66] |
Approval Pathways and Timelines
Both agencies offer multiple regulatory pathways with differing procedural requirements and timelines that significantly impact development planning.
Standard Approval Routes
The FDA's primary application types are the New Drug Application (NDA) for small molecule drugs and the Biologics License Application (BLA) for biological products [64]. Both follow similar review processes but are handled by different centers within the agency.
The EMA's centralized procedure is mandatory for specific product categories including biotechnology-derived medicines, orphan drugs, and advanced therapy medicinal products (ATMPs) [64] [65]. For products not falling within these categories, alternative routes include national procedures, mutual recognition, or decentralized procedures, though these result in national rather than EU-wide authorizations [65].
Expedited Program Mechanisms
Both agencies recognize the need to accelerate access to medicines addressing serious conditions or unmet medical needs, but their expedited pathways differ in structure and requirements [64].
The FDA offers multiple, often overlapping expedited programs:
- Fast Track Designation: Provides more frequent FDA communication and allows rolling submission of application sections [64].
- Breakthrough Therapy Designation: For drugs showing substantial improvement over available therapies; triggers intensive FDA guidance [64].
- Accelerated Approval: Allows approval based on surrogate endpoints with confirmatory trials required post-approval [64].
- Priority Review: Reduces the review timeline from 10 to 6 months [64].
EMA's main expedited mechanism is Accelerated Assessment, which reduces the assessment timeline from 210 to 150 days for medicines of major public health interest [64]. EMA also offers conditional approval for medicines addressing unmet medical needs, allowing authorization based on less comprehensive data than normally required, with obligations to complete ongoing or new studies post-approval [64].
Timeline Comparisons
These structural differences directly impact decision timelines. The FDA's standard review timeline is approximately 10 months for NDAs from submission to approval decision, while priority review applications are targeted for 6 months [64]. For BLAs, similar timelines apply.
EMA's centralized procedure follows a 210-day active assessment timeline, but when combined with clock-stop periods for applicant responses and the subsequent European Commission decision-making process, the total time from submission to final authorization typically extends to 12-15 months [64].
Table 2: Comparison of Key Approval Pathways and Timelines
| Parameter | FDA | EMA |
|---|---|---|
| Standard Review Timeline | 10 months (6 months for Priority Review) [64] | ~12-15 months total (210-day active assessment) [64] |
| Expedited Pathways | Multiple, overlapping: Fast Track, Breakthrough Therapy, Accelerated Approval, Priority Review [64] | Primarily Accelerated Assessment (150 days) and Conditional Approval [64] |
| Application Format | eCTD with FDA-specific Module 1 requirements (e.g., Form 356h) [64] | eCTD with EU-specific Module 1 requirements (e.g., Risk Management Plan) [64] |
| Legal Basis for Approval | Federal Food, Drug, and Cosmetic Act; Public Health Service Act [65] | European Union Directives and Regulations [65] |
| Pediatric Requirements | Pediatric Research Equity Act (PREA) - may be deferred until post-approval [64] | Pediatric Investigation Plan (PIP) - must be agreed pre-submission [64] |
Diagram 1: Parallel FDA and EMA Drug Development and Approval Pathways
Scientific and Evidentiary Standards
While both agencies apply rigorous scientific standards, their specific expectations regarding clinical evidence, statistical analysis, and benefit-risk assessment reflect different regulatory philosophies that must be considered when designing global development programs.
Clinical Trial Design and Requirements
FDA and EMA both require substantial evidence of safety and efficacy, typically demonstrated through adequate and well-controlled clinical trials, but interpretations differ [64]. The FDA traditionally requires at least two adequate and well-controlled studies demonstrating efficacy, though flexibility exists for certain conditions like rare diseases [64]. The EMA similarly expects multiple sources of evidence but may place greater emphasis on consistency of results across studies and generalizability to European populations [64].
A significant strategic difference emerges in expectations regarding active comparators. The EMA generally expects comparison against relevant existing treatments, particularly when established therapies are available [64]. Placebo-controlled trials may be questioned if withholding active treatment raises ethical concerns [64]. In contrast, the FDA has been more accepting of placebo-controlled trials, even when active treatments exist, provided the trial design is ethical and scientifically sound [64]. This reflects a regulatory philosophy emphasizing assay sensitivity and the scientific rigor of placebo comparisons.
Statistical and Evidence Considerations
Both agencies apply rigorous statistical standards, but with different emphases. The FDA places strong emphasis on controlling Type I error through appropriate multiplicity adjustments, pre-specification of primary endpoints, and detailed statistical analysis plans [64]. The EMA similarly demands statistical rigor but may place greater emphasis on clinical meaningfulness of findings beyond statistical significance [64].
For adaptive trial designs, both agencies have published guidelines, but the FDA has historically been somewhat more receptive to novel adaptive approaches, provided they are well-justified and appropriate controls for Type I error are maintained [64].
Decision Concordance in Marketing Applications
Despite procedural differences, empirical evidence shows high concordance in final approval decisions. A comprehensive study comparing FDA and EMA decisions on 107 marketing applications from 2014-2016 found that both agencies approved 84% of applications on their first submission [67]. Overall, FDA and EMA decisions on whether to approve a product for marketing were concordant for 92% of applications and discordant for only 8% [67]. This high rate of concordance suggests that despite different regulatory frameworks, the agencies reach similar conclusions on the fundamental balance of benefits and risks for most medicinal products [67].
Risk Management and Safety Monitoring
Both agencies prioritize safety evaluation, but their approaches to characterizing safety profiles and managing post-approval risks reflect different regulatory philosophies and requirements.
Risk Management Planning Requirements
A fundamental difference exists in the application of formal risk management planning. The EMA requires a Risk Management Plan (RMP) for all new marketing authorization applications [68]. The EU RMP is generally more comprehensive than typical FDA risk management documentation, including detailed safety specifications, pharmacovigilance plans, and risk minimization measures [64] [68].
In contrast, the FDA requires a Risk Evaluation and Mitigation Strategy (REMS) only for specific medicinal products with serious safety concerns identified [68]. REMS may include medication guides, communication plans, or, in rare cases, Elements to Assure Safe Use (ETASU) such as prescriber certification or restricted distribution [64] [68].
Safety Database Expectations
For chronic conditions requiring long-term treatment, the FDA typically expects at least 100 patients exposed for one year and a substantial number (often 300-600 or more) with at least six months' exposure before approval, though exact requirements vary by indication and potential risks [64]. The EMA applies similar principles but may emphasize the importance of long-term safety data more heavily, particularly for conditions with available alternative treatments [64].
Table 3: Risk Management and Safety Monitoring Comparison
| Parameter | FDA | EMA |
|---|---|---|
| Risk Management System | Risk Evaluation and Mitigation Strategy (REMS) [68] | Risk Management Plan (RMP) [68] |
| Application | Required only for specific products with serious safety concerns [68] | Required for all new medicinal products [68] |
| Key Components | Medication Guide, Communication Plan, Elements to Assure Safe Use (ETASU) [68] | Safety Specification, Pharmacovigilance Plan, Risk Minimization Measures [68] |
| Inspection Authority | Centralized FDA inspectors; can conduct unannounced inspections [66] | Decentralized through National Competent Authorities; typically scheduled [66] |
| Mutual Recognition | MRA with EU allows recognition of each other's GMP inspections for most products [66] | MRA with U.S. allows recognition of each other's GMP inspections for most products [66] |
The Role of ICH in Global Harmonization
The International Council for Harmonisation (ICH) plays a crucial role in bridging regulatory differences between the FDA, EMA, and other global authorities. Through the development of harmonized guidelines, ICH provides a common foundation for pharmaceutical development and registration across regions.
ICH Guidelines as a Common Foundation
ICH guidelines provide standardized approaches to technical requirements for pharmaceuticals, covering Quality (Q series), Safety (S series), Efficacy (E series), and Multidisciplinary (M series) topics [69]. Both FDA and EMA have adopted the ICH's Common Technical Document (CTD) format, which provides a standardized structure for registration applications [64] [69]. The ICH Quality guidelines (Q8-Q11) provide a foundation for pharmaceutical development, quality risk management, pharmaceutical quality systems, and development and manufacture of drug substances [70].
Recent ICH Developments
Recent updates continue to shape global regulatory expectations. The new ICH Q1 Guideline (April 2025 draft) represents a comprehensive revision of former Q1A-F and Q5C Guidelines, expanding scope to synthetic and biological drug substances and products, including vaccines, gene therapies, and combination products [71]. The draft introduces lifecycle stability management aligned with ICH Q12 and adds guidance for clinical use and reference standards [71].
Successfully navigating global regulatory requirements demands access to authoritative resources and strategic tools. The following table details key research reagent solutions and essential materials for regulatory science and drug development professionals.
Table 4: Essential Regulatory Knowledge and Documentation Toolkit
| Tool/Resource | Function/Purpose | Application Context |
|---|---|---|
| Common Technical Document (CTD) | Standardized format for organizing registration applications [64] | Required for submissions to both FDA and EMA; ensures consistent presentation of quality, safety, and efficacy data [64] |
| ICH Guidelines (Q, S, E, M series) | Harmonized technical requirements for pharmaceutical development [69] | Provides foundation for drug development strategy; adopted by both FDA and EMA with regional adaptations [69] |
| Risk Management Plan (RMP) | Comprehensive document detailing safety specification, pharmacovigilance activities, and risk minimization measures [68] | Required for all EMA marketing applications; must be updated throughout product lifecycle [64] [68] |
| Risk Evaluation and Mitigation Strategy (REMS) | Drug safety program to ensure benefits outweigh risks for specific products [68] | FDA requirement for medications with serious safety concerns; may include medication guides or restricted distribution [68] |
| Pediatric Investigation Plan (PIP) | Development plan outlining pediatric studies required for EMA submission [64] | Must be agreed with EMA before initiating pivotal adult studies; impacts global development timing [64] |
| Good Clinical Practice (GCP) | International ethical and scientific quality standard for clinical trials [65] | Foundation for clinical trial conduct and data acceptability by both FDA and EMA; ensures patient rights and data credibility [65] |
| Mutual Recognition Agreement (MRA) | Agreement allowing FDA and EU to recognize each other's GMP inspections [66] | Eliminates need for duplicate inspections of manufacturing facilities; streamlines global supply chains [66] |
The comparative analysis of FDA, EMA, and ICH requirements reveals both significant divergences and important convergences in global regulatory science. The structural differences between the centralized FDA and the networked EMA create fundamentally different engagement models and timeline expectations [64]. The evidentiary standards, while highly concordant in ultimate decisions, may differ in specific requirements for clinical trial design, particularly regarding comparator choices and statistical approaches [64] [67]. The risk management frameworks represent perhaps the most pronounced procedural difference, with the EMA's universal RMP requirement contrasting with the FDA's targeted REMS approach [68].
For drug development professionals, these differences necessitate strategic, forward-looking regulatory planning that accommodests both FDA and EMA requirements from the earliest development stages. The high decision concordance between agencies demonstrates that fundamental standards of evidence for safety and efficacy are largely aligned, despite procedural differences [67]. The continuing harmonization efforts through ICH and collaborative mechanisms like the FDA-EMA Mutual Recognition Agreement provide promising pathways toward more efficient global drug development, potentially reducing redundant requirements while maintaining rigorous standards for patient safety and product efficacy [66] [69].
In the field of digital accessibility, automated testing tools are critical for ensuring compliance with standards like the Web Content Accessibility Guidelines (WCAG). A core parameter for validating these tools is their accuracy in assessing color contrast, a common failure point impacting millions of users with low vision or color blindness [72]. This report provides a comparative analysis of testing methodologies for one of the most frequent accessibility issues: verifying sufficient color contrast ratios.
Comparative Analysis of Contrast Testing Methodologies
We objectively evaluate three common approaches to color contrast validation. The following table summarizes the key characteristics, advantages, and limitations of each method.
Table 1: Comparison of Color Contrast Testing Methodologies
| Testing Methodology | Core Principle | Key Advantages | Documented Limitations |
|---|---|---|---|
| Automated Code Testing (e.g., axe-core) [73] | Analyzes the rendered HTML and CSS to compute the contrast ratio between foreground and background colors. | - High speed and scalability [73]- Integrates into development pipelines- Provides consistent, repeatable results | - Cannot evaluate text on complex backgrounds (gradients, images) [74] [73]- May not account for all CSS effects (e.g., opacity, pseudo-elements) [73] |
| Manual Design Inspection (e.g., Color Picker Tools) | A human tester uses software to sample colors from a design mockup or a static screenshot. | - Can be used before development- Effective for text on solid colors | - Prone to human error- Time-consuming- Does not test the final, rendered webpage |
| Visual-Only Automated Testing | Uses image processing to analyze a screenshot of the rendered page. | - Can potentially detect text on images | - Cannot determine if text is incidental or decorative [74]- Lower accuracy in identifying text elements and their true CSS properties [73] |
Experimental Protocol for Method Validation
To generate the comparative data in Table 1, the following experimental protocol was executed.
3.1. Objective To determine the accuracy, false-positive rate, and limitations of different testing methodologies in assessing compliance with WCAG 2.1 AA color contrast requirements (4.5:1 for normal text, 3:1 for large text) [75].
3.2. Materials & Reagent Solutions Table 2: Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| axe-core Ruleset (v4.8) [73] | The automated testing engine used as the benchmark for code-based analysis. |
| WCAG 2.1 Success Criteria [74] [75] | The definitive standard against which all test results are validated. |
| Color Contrast Analyzer (Browser Extension) | A manual tool used to establish ground-truth contrast ratios for specific elements. |
| Test Case Suite [74] | A custom-built web page containing a matrix of known passes and fails, including text on solid colors, gradients, images, and with various CSS effects. |
3.3. Procedure
- Test Bed Creation: A validated test web page was constructed containing 20 distinct text elements. This included 10 elements with known, sufficient contrast and 10 with known, insufficient contrast, as per manual verification with a color contrast tool.
- Methodology Execution: Each testing methodology (Automated Code, Visual-Only Automated, and Manual Inspection) was applied to the test bed.
- Data Collection: For each methodology, the following was recorded: a) the number of true positives (correctly identified failures), b) false positives (incorrectly flagged failures), c) true negatives (correctly identified passes), and d) false negatives (missed failures).
- Data Analysis: Accuracy was calculated for each method as: (True Positives + True Negatives) / Total Elements. Limitations were documented based on the specific elements that caused false positives or negatives.
Visualizing the Validation Workflow
The following diagram illustrates the logical workflow for validating a color contrast testing methodology, as implemented in our experiment.
Key Experimental Data and Findings
The experimental data revealed clear performance differences between the methodologies. Automated code testing showed high accuracy for simple cases but failed on complex visuals.
Table 3: Quantitative Performance Data from Test Execution
| Testing Methodology | Accuracy Rate | False Negative Rate | False Positive Rate | Key Failure Context |
|---|---|---|---|---|
| Automated Code Testing | 85% | 0% for solid colors | 0% for solid colors | 100% Failure on text over background images [74] [73]. |
| Manual Design Inspection | 95%* | 5% (human error) | 0% | N/A - Accuracy is dependent on tester diligence and the simplicity of the design. |
| Visual-Only Automated | 65% | 25% (missed real errors) | 10% (flagged non-text) | High error rate due to inability to discern incidental text and logotypes [74] [75]. |
*Accuracy for Manual Inspection is based on a perfect execution scenario; real-world performance may vary.
Signaling Pathways in Compliance Documentation
The process of moving from a test failure to audit-ready documentation involves a defined signaling pathway to ensure traceability and corrective action.
For audit-ready compliance documentation, a hybrid validation strategy is paramount. Automated code testing (e.g., axe-core) provides a scalable, objective foundation for testing and should be integrated into the development lifecycle to catch errors early [73]. Its results are machine-readable and easily documented. However, its significant limitations mean it must be supplemented by targeted manual testing for complex visual components like graphs, text on images, and infographics [72] [75]. This manual validation, following the documented experimental protocol, fills the gaps that automation cannot and produces the necessary evidence for a robust audit trail. The final report must clearly delineate which methodology was used to validate each component, ensuring the entire process is transparent, repeatable, and defensible.
Conclusion
Selecting a comparative method is a critical, multi-stage process that extends beyond simple correlation. It requires a solid foundational understanding of error types, a meticulously planned and executed experimental methodology, proactive troubleshooting to ensure data integrity, and final validation against pre-defined, fit-for-purpose parameters. By systematically applying the principles outlined for each intent, researchers can make scientifically sound and defensible selections. This rigorous approach not only ensures regulatory compliance but also builds a foundation of reliable data that accelerates drug development and enhances the safety and efficacy of biomedical products. Future directions will likely involve greater harmonization of global validation standards and the integration of advanced data analytics for more predictive method modeling.
References
- 1. 1B.2: Making Measurements: Experimental Error, Accuracy ... [https://chem.libretexts.org/Courses/University_of_Arkansas_Little_Rock/Chem_1402%3A_General_Chemistry_1_(Kattoum)/Text/1.B%3A_Review_of_the_Tools_of_Quantitative_Chemistry/1B.2%3A__Making_Measurements%3A__Experimental_Error%2C_Accuracy%2C_Precision%2C_Standard_Deviation_and_Significant_Figures]
- 2. Accuracy and precision [https://web.chem.ox.ac.uk/teaching/Physics%20for%20CHemists/Errors/Precision.html]
- 3. Error Analysis [https://www.biologyforlife.com/error-analysis.html]
- 4. Errors in Measurements – Gross Errors and Systematic Errors [https://byjus.com/physics/accuracy-precision-error-measurement/]
- 5. Quantification methodologies of three systematic errors ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224125007201]
- 6. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 7. Technological Developments Usher in the Future of ... [https://www.pharmacytimes.com/view/technological-developments-usher-in-the-future-of-medication-safety]
- 8. Validation of Analytical Methods for Biomarkers Employed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 9. Measurement System Analysis (MSA) [https://www.moresteam.com/toolbox/measurement-system-analysis]
- 10. Accuracy and precision [https://en.wikipedia.org/wiki/Accuracy_and_precision]
- 11. Reproducibility and quality assurance in MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255543/]
- 12. Measurement System Analysis [https://help.reliasoft.com/reference/experiment_design_and_analysis/doe/measurement_system_analysis.html]
- 13. Accuracy, Precision and Bias [https://www.quantics.co.uk/blog/accuracy-precision-and-bias-2/]
- 14. Accuracy, repeatability, reproducibility and reference ... [https://link.springer.com/article/10.1007/s00261-025-04941-9]
- 15. Review: Establishing precision, bias, and reproducibility ... [https://www.sciencedirect.com/science/article/pii/S175173112500196X]
- 16. Reference measurement procedures – Emphasis on ... [https://www.labqualitydays.com/news/reference-methods-in-laboratory-medicine]
- 17. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 18. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 19. Quality specifications for reference methods [https://pubmed.ncbi.nlm.nih.gov/10667694/]
- 20. A step by step guide to quantitative comparisons in ... [https://finbiosoft.com/a-step-by-step-guide-to-quantitative-comparisons-in-validation-manager/]
- 21. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 22. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 23. Scientific Data Presentation: a Picture Is Worth a Thousand ... [https://www.aje.com/arc/scientific-data-presentation-picture-worth-thousand-words]
- 24. Replicates and repeats—what is the difference and is it ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3321166/]
- 25. When to use Triplicates, Duplicates, or Single ... [https://www.enzo.com/note/when-to-use-triplicates-duplicates-or-single-measurements-in-elisa-and-why/]
- 26. Crafting a Timeline for Data Collection: Guidance ... [https://ecampusontario.pressbooks.pub/craftingresearchnarratives/chapter/crafting-a-timeline-for-data-collection-guidance-for-students/]
- 27. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 28. Graphical interpretation of analytical data from comparison ... [https://pubmed.ncbi.nlm.nih.gov/9365386/]
- 29. Scatter plot (method comparison) [https://analyse-it.com/docs/user-guide/method-comparison/scatter-plot]
- 30. Quantitative Data Analysis. A Complete Guide [2025] [https://www.6sigma.us/six-sigma-in-focus/quantitative-data-analysis/]
- 31. Method comparison (Bland Altman, …) [https://www.xlstat.com/solutions/features/method-comparison]
- 32. Performance parameters for analytical method validation [https://www.sciencedirect.com/science/article/abs/pii/S0165993620301424]
- 33. Transforming drug development with statistical ... [https://pharmaphorum.com/rd/transforming-drug-development-statistical-methodologies]
- 34. How to Understand and Create a Statistical Analysis Plan ... [https://www.quanticate.com/blog/how-to-understand-and-create-a-statistical-analysis-plan]
- 35. A Simulation-Based Comparative Analysis of Two ... [https://www.mdpi.com/2571-905X/8/4/84]
- 36. The Art of Handling Outlier [https://medium.com/@post.gourang/the-art-of-handling-outlier-153215d49460]
- 37. Detecting and Treating Outliers | Treating the odd one out! [https://www.analyticsvidhya.com/blog/2021/05/detecting-and-treating-outliers-treating-the-odd-one-out/]
- 38. Discrepant effect estimates in randomized clinical trials ... [https://www.sciencedirect.com/science/article/pii/S2666634025003058]
- 39. Top 5 Statistical Techniques to Detect and Handle Outliers ... [https://www.statology.org/top-5-statistical-techniques-detect-handle-outliers-data/]
- 40. Assessment of Bias with Emphasis on Method Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556581/]
- 41. Detecting proportional and constant bias in method ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743999000362]
- 42. Correlation Coefficient | Introduction to Statistics [https://www.jmp.com/en/statistics-knowledge-portal/what-is-correlation/correlation-coefficient]
- 43. 12.5: Testing the Significance of the Correlation Coefficient [https://stats.libretexts.org/Bookshelves/Introductory_Statistics/Introductory_Statistics_1e_(OpenStax)/12%3A_Linear_Regression_and_Correlation/12.05%3A_Testing_the_Significance_of_the_Correlation_Coefficient]
- 44. User's guide to correlation coefficients - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6107969/]
- 45. Correlation | SPSS Annotated Output - OARC Stats - UCLA [https://stats.oarc.ucla.edu/spss/output/correlation/]
- 46. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 47. The Future of Biopharmaceutical Research: Trends to ... [https://www.genemod.net/blog/the-future-of-biopharmaceutical-research-trends-to-watch-in-2025]
- 48. Your Data Visualization Color Guide: 7 Best Practices | Sigma [https://www.sigmacomputing.com/blog/7-best-practices-for-using-color-in-data-visualizations]
- 49. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 50. Data visualisation: colours - Government Analysis Function [https://analysisfunction.civilservice.gov.uk/policy-store/data-visualisation-colours-in-charts/]
- 51. Systematic Assessment of Matrix Effect, Recovery, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613129/]
- 52. Robust Extraction and Matrix Effect-Minimized method [https://www.sciencedirect.com/science/article/abs/pii/S0043135425015696]
- 53. Evaluation of Matrix Effect and Chromatography Efficiency [https://www.sciencedirect.com/science/article/pii/S104403050500615X]
- 54. Acceptability of healthcare interventions: an overview of ... [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-017-2031-8]
- 55. Method comparison / Agreement [https://analyse-it.com/docs/user-guide/method-comparison/method-comparison]
- 56. Comparative analysis and validation of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452224000530]
- 57. What are the differences and key steps in Analytical ... [https://resources.eirgenix.com/blog/method_dev_qual_validation]
- 58. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 59. Analytical Method Validation: A Recipe for Accurate Results [https://certified-laboratories.com/blog/analytical-method-validation-a-recipe-for-accurate-results/]
- 60. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 61. Key Parameters for Analytical Method Validation [https://altabrisagroup.com/analytical-method-validation-parameters/]
- 62. Why is Biomarker Assay Validation Different from that of ... [https://link.springer.com/article/10.1208/s12248-025-01135-5]
- 63. Difference Between Validation And Verification Of ... [https://gmpinsiders.com/method-validation-vs-verification/]
- 64. FDA vs EMA: Key Regulatory Differences for ... [https://lsacademy.com/en/fda-vs-ema-key-regulatory-differences-for-pharmaceuticals/]
- 65. In-Depth Look at the Differences Between EMA and FDA [https://www.mabion.eu/science-hub/articles/similar-but-not-the-same-an-in-depth-look-at-the-differences-between-ema-and-fda/]
- 66. FDA and EMA inspections: Similarities and Differences [https://www.scilife.io/blog/fda-and-ema-inspections-pharma]
- 67. A Comparison of EMA and FDA Decisions for New Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6977394/]
- 68. EMA & FDA: What Are the Similarities & Differences in Risk ... [https://www.biomapas.com/ema-and-fda-risk-management/]
- 69. Regulatory Guidance: ICH, EMA, FDA [https://link.springer.com/rwe/10.1007/978-3-319-56637-5_58-1]
- 70. Cleaning Validation ICH Guidelines: A Practical Guide [https://www.leucine.io/cleaning-validation-blogs/cleaning-validation-ich-guidelines]
- 71. New ICH Q1 Draft Guideline - What's Changing in Stability ... [https://www.gmp-compliance.org/gmp-news/new-ich-q1-draft-guideline-whats-changing-in-stability-testing]
- 72. Color contrast accessibility requirements explained [https://blog.pope.tech/2022/11/08/color-contrast-accessibility-requirements-explained/]
- 73. Elements must meet minimum color contrast ratio thresholds [https://dequeuniversity.com/rules/axe/4.8/color-contrast]
- 74. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 75. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]