From Prescriptive Checklists to Lifecycle Management: The Evolution of Analytical Method Validation Protocols
This article traces the transformative journey of analytical method validation from its origins in prescriptive checklists to the modern, science- and risk-based lifecycle approach.
From Prescriptive Checklists to Lifecycle Management: The Evolution of Analytical Method Validation Protocols
Abstract
This article traces the transformative journey of analytical method validation from its origins in prescriptive checklists to the modern, science- and risk-based lifecycle approach. Tailored for researchers, scientists, and drug development professionals, it explores the foundational regulatory principles, details contemporary methodological applications, addresses common troubleshooting and optimization challenges, and examines rigorous validation and comparative strategies. By synthesizing historical context with current trends like AQbD, AI, and real-time monitoring, the article provides a comprehensive resource for navigating the past, present, and future of ensuring data quality and regulatory compliance in pharmaceutical analysis.
The Roots of Reliability: Tracing the Origins and Regulatory Foundations of Method Validation
Before the establishment of global standards, analytical method validation existed as a fragmented landscape of in-house practices and company-specific standards. Pharmaceutical manufacturers operated with individualized approaches to demonstrating method suitability, creating a patchwork of technical requirements that complicated collaboration, technology transfer, and regulatory oversight. The absence of harmonized guidelines meant that methods developed in one organization often required significant rework when transferred to another facility, impeding efficiency and potentially compromising product quality consistency across regions. This case study explores the historical journey from these disparate internal standards to the coordinated global harmonization efforts that define modern pharmaceutical analysis, tracing the critical events, technological advancements, and regulatory developments that propelled this transformation.
The Early Drivers: Tragedy and Regulatory Response
The transition from in-house standards to formalized validation requirements was catalyzed by tragic events and subsequent regulatory interventions. A pivotal case was the 1971 Devonport incident, where contaminated intravenous solutions led to patient fatalities, highlighting critical gaps in sterilization process controls [1]. This tragedy refocused the entire pharmaceutical industry on the fundamental importance of manufacturing process safety and reliability, creating the imperative for more rigorous validation approaches [1].
The regulatory response emerged through key publications and requirements:
- The first UK "Orange Guide" (1971) established early Good Manufacturing Practice standards [1]
- US GMPs (21 CFR Parts 210 and 211) formalized validation requirements in 1978, with validation becoming a central term in 1983 [1]
- The 1983 FDA guide to inspection of computerized systems marked early recognition of automated system validation needs [1]
A landmark legal case, United States v. Barr Laboratories, Inc. (1993), definitively established that process validation was not merely guidance but a requirement under GMP regulations, settling industry disputes and reinforcing regulatory authority [1].
Evolution of Key Validation Parameters and Protocols
Foundational Analytical Performance Characteristics
Early validation practices focused on establishing core parameters that guaranteed method reliability, many of which remain fundamental to modern protocols. These parameters evolved from internal company requirements to standardized characteristics recognized across the industry [2].
Table 1: Core Analytical Performance Characteristics in Early Validation Practices
| Parameter | Technical Definition | Early Experimental Protocol |
|---|---|---|
| Accuracy | Closeness of agreement between accepted reference value and value found | Drug substance: comparison to standard reference material; Drug product: analysis of synthetic mixtures spiked with known quantities; Minimum 9 determinations over 3 concentration levels [2] |
| Precision | Closeness of agreement between individual test results from repeated analyses | Repeatability: Same conditions, short time interval, 9 determinations over specified range; Intermediate precision: Different days, analysts, equipment; Reproducibility: Between laboratories [2] |
| Specificity | Ability to measure analyte accurately in presence of expected components | Resolution of closely eluted compounds; Peak purity tests via photodiode-array or mass spectrometry; Spiking with impurities/excipients [2] |
| Linearity & Range | Ability to obtain results proportional to analyte concentration | Minimum of 5 concentration levels covering specified range; Documentation of calibration curve equation, coefficient of determination (r²), and residuals [2] |
| LOD/LOQ | Lowest concentration detectable (LOD) and quantifiable (LOQ) | Signal-to-noise ratios (3:1 for LOD, 10:1 for LOQ); Calculation via LOD/LOQ = K(SD/S) where K=3 for LOD, 10 for LOQ [2] |
| Robustness | Capacity to remain unaffected by small, deliberate variations | Deliberate variations in method parameters (pH, mobile phase composition, columns); Typically evaluated during method development [3] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Early validation practices relied on fundamental analytical tools and reagents that formed the backbone of method development and verification protocols.
Table 2: Essential Research Reagent Solutions in Early Analytical Validation
| Tool/Reagent | Function in Validation | Application Context |
|---|---|---|
| Reference Standards | Establish accuracy and calibration curves | USP reference materials; Qualified impurity standards; System suitability verification [2] |
| Chromatographic Materials | Separation mechanism for specificity assessment | HPLC/UHPLC columns; Various stationary phases; Mobile phase buffers and modifiers [4] [2] |
| Detection Systems | Specificity and peak purity verification | Photodiode-array detectors; Mass spectrometry systems; Orthogonal detection confirmation [2] |
| Sample Preparation Reagents | Extraction, dilution, and derivative formation | Protein precipitation agents; Derivatization reagents; Extraction solvents and solid-phase materials [5] |
| 2-Benzyl-3-hydroxypropyl acetate | 2-Benzyl-3-hydroxypropyl acetate, CAS:90107-01-0, MF:C12H16O3, MW:208.25 g/mol | Chemical Reagent |
| 3-((4-Bromophenyl)sulfonyl)azetidine | 3-((4-Bromophenyl)sulfonyl)azetidine|CAS 1706448-67-0 | 3-((4-Bromophenyl)sulfonyl)azetidine (CAS 1706448-67-0) is a versatile azetidine building block for drug discovery and research. For Research Use Only. Not for human or veterinary use. |
The Path to Global Harmonization
International Conference on Harmonisation (ICH) Initiatives
The formation of the International Conference on Harmonisation (ICH) marked a turning point in creating unified global validation standards. Between 2005 and 2009, ICH produced a series of quality guidelines that fundamentally reshaped pharmaceutical validation [1]:
- ICH Q8 Pharmaceutical Development (2005) introduced Quality by Design (QbD) principles [1]
- ICH Q9 Quality Risk Management (2005) formalized risk-based approaches [1]
- ICH Q10 Pharmaceutical Quality System (2008) established comprehensive quality systems [1]
These guidelines emphasized science-based approaches and risk management, moving beyond prescriptive requirements to more flexible, knowledge-driven methodologies [1]. The harmonization of terminology and requirements through ICH Q2 (Validation of Analytical Procedures) created a common language and technical framework that transcended regional regulatory differences [5] [3].
Industry Collaboration and Standards Development
Parallel to regulatory developments, industry professionals established collaborative frameworks to address emerging challenges:
- GAMP (Good Automated Manufacturing Practice) Community of Practice formed in response to FDA concerns about computer system validation [1]
- ASTM E2500 (2007) introduced risk-based approaches to qualification of manufacturing systems [1]
- USP general chapters (<1224>, <1225>, <1226>) provided standardized approaches for method transfer, validation, and verification [3]
These initiatives represented a shift from isolated company standards to collaborative knowledge sharing and consensus-based best practices across the industry [1].
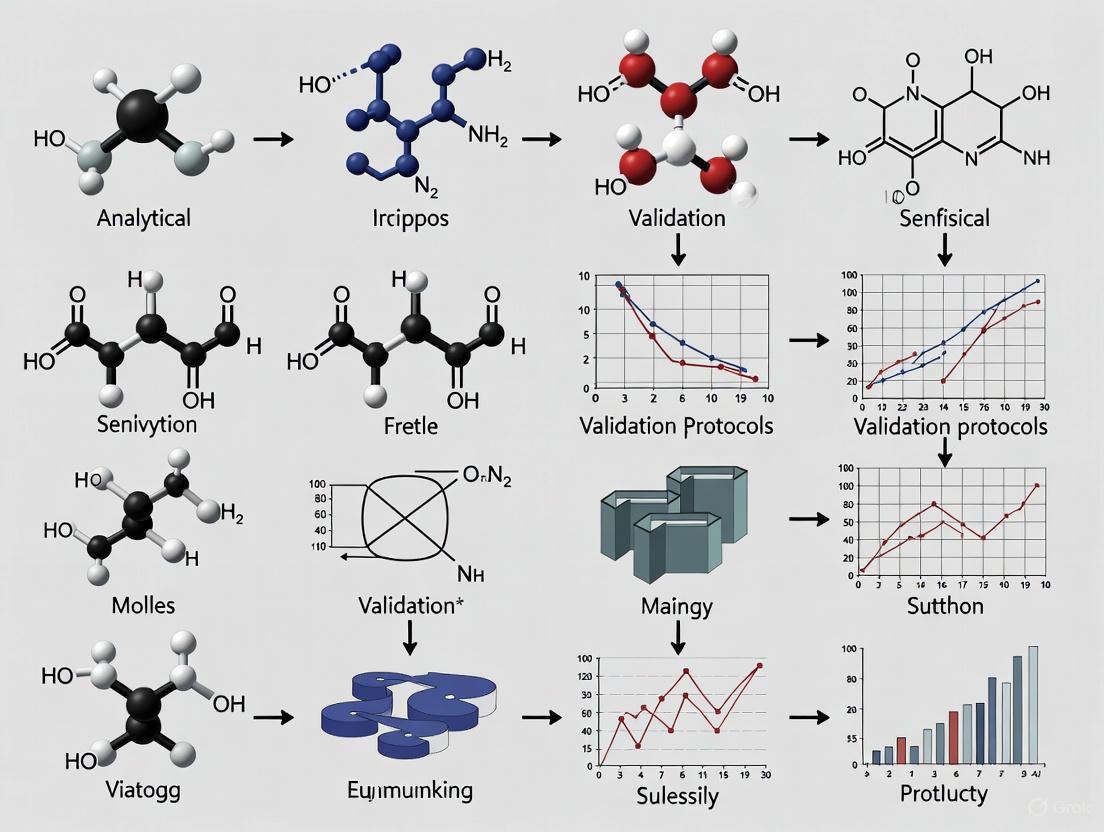
Method Validation Evolution Pathway
The transition from early practices to harmonized approaches follows a clear evolutionary pathway, visualized below:
Comparative Analysis: Early Practices vs. Harmonized Approaches
The transformation from in-house standards to globally harmonized approaches represents fundamental shifts in philosophy, methodology, and technical requirements.
Table 3: Evolution from Early Practices to Harmonized Approaches
| Aspect | Early Practices (Pre-Harmonization) | Harmonized Framework (Post-ICH) |
|---|---|---|
| Standardization | Company-specific protocols; In-house standards | Globally harmonized guidelines (ICH Q2); Unified terminology |
| Regulatory Alignment | Variable interpretations; Regional differences | Consistent expectations across FDA, EMA, and other agencies |
| Methodology | Fixed validation batches; Limited statistical basis | Risk-based approaches; Lifecycle management; Design of Experiments |
| Documentation | Varied formats and rigor | Standardized validation protocols and summary reports |
| Technology Transfer | Difficult, requiring significant revalidation | Streamlined via formal transfer protocols (USP <1224>) |
| Focus | Primarily on compliance and documentation | Science-based, patient-focused, with quality risk management |
The journey from fragmented in-house standards to global harmonization has fundamentally transformed pharmaceutical analytical method validation. While early practices were characterized by inconsistency and variable rigor, they established the foundational technical parameters that remain relevant today. The harmonization movement, driven by tragic quality failures, regulatory response, and industry collaboration, has created a more robust, science-based framework that prioritizes patient safety and product quality.
The legacy of early validation practices endures in the continued emphasis on method reliability, analytical accuracy, and technical rigor, even as the framework has evolved toward lifecycle management, risk-based approaches, and global standardization. This historical progression demonstrates how quality systems mature through the integration of technical knowledge, regulatory experience, and collaborative improvement—a process that continues today with emerging trends in real-time release testing, advanced analytics, and continuous process verification [4]. Understanding this evolution provides valuable context for contemporary validation challenges and opportunities for further advancement in pharmaceutical quality assurance.
Prior to the establishment of the International Council for Harmonisation (ICH), the global pharmaceutical industry faced a complex and fragmented regulatory environment. Requirements for drug development and registration diverged significantly across regions, leading to redundant testing, unnecessary animal studies, and substantial delays in making new medicines available to patients [6]. This lack of harmonization resulted in inefficient use of resources and complicated international trade in pharmaceuticals. The European Union had begun its own harmonization efforts in the 1980s, but a broader international initiative was clearly needed [7]. It was against this backdrop that regulatory authorities and industry representatives from Europe, Japan, and the United States came together to create ICH in April 1990, with the inaugural meeting held in Brussels [7] [6]. The fundamental mission of this new council was to promote public health through the development of harmonized technical guidelines and requirements for pharmaceutical product registration, thereby achieving greater efficiency while maintaining rigorous safeguards for quality, safety, and efficacy [7].
The ICH framework organized its work into four primary categories: Quality (Q series), Safety (S series), Efficacy (E series), and Multidisciplinary (M series) guidelines [7]. The Quality guidelines, particularly those addressing analytical procedure validation, would become some of the most impactful and enduring standards developed by the organization. The inception of ICH marked the beginning of a new era of international cooperation in pharmaceutical regulation, creating a structured process for building consensus among regulators and industry experts that would ultimately produce the gold standard for analytical method validation: the ICH Q2(R1) guideline.
The Genesis of ICH Q2(R1): Forging a Unified Standard
The development of ICH Q2(R1), titled "Validation of Analytical Procedures: Text and Methodology," represented a significant achievement in international regulatory harmonization. This guideline did not emerge in a vacuum; it was the culmination of a deliberate, multi-step consensus-building process characteristic of ICH's approach [7]. The journey to a harmonized guideline began with the identification of a need for consistent standards in analytical method validation, followed by the creation of a concept paper and business plan outlining the objectives for harmonization. An Expert Working Group (EWG) comprising regulatory and industry scientists from the founding ICH regions was then formed to develop the technical content [7].
The initial version of the quality guideline on analytical validation, ICH Q2A, was approved in 1993 (ICH Q2A, 1994). It defined key validation parameters such as specificity, accuracy, precision, detection limit, quantitation limit, linearity, and range [8]. This was subsequently complemented by ICH Q2B, which provided further guidance on methodology. In a pivotal move to streamline and consolidate these standards, the ICH unified Q2A and Q2B into a single comprehensive guideline—Q2(R1)—in November 2005 [8]. This revision provided a more cohesive and detailed framework, establishing consistent definitions and validation methodologies that could be applied across the pharmaceutical industry for both chemical and biological products [9]. The guideline was specifically designed for analytical procedures used in the release and stability testing of commercial drug substances and products, providing a common language and set of expectations for regulators and manufacturers alike [10].
Table 1: The Stepwise Development of ICH Q2(R1)
| Step | Document | Approval Date | Key Achievement |
|---|---|---|---|
| Step 1 | ICH Q2A | 1993 | Defined core validation parameters for analytical procedures. |
| Step 2 | ICH Q2B | 1996 | Provided further methodological details on validation. |
| Unification | ICH Q2(R1) | November 2005 | Consolidated Q2A and Q2B into a single, definitive guideline. |
Core Principles and Validation Parameters of ICH Q2(R1)
ICH Q2(R1) established a foundational framework for validating analytical procedures by defining a set of core performance characteristics that must be demonstrated to prove a method is suitable for its intended purpose [8]. The guideline provides clear definitions and methodological approaches for each parameter, ensuring that the term "validation" carries a consistent meaning across international borders. These parameters are not applied uniformly to all methods; rather, the specific validation requirements depend on the type of analytical procedure (e.g., identification, testing for impurities, assay). The following core principles form the bedrock of the Q2(R1) standard [2]:
- Specificity: The ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components. This is typically demonstrated by resolving the analyte from closely eluting compounds in chromatographic methods, often supported by peak purity assessment using techniques like photodiode-array (PDA) or mass spectrometry (MS) detection [2].
- Accuracy: The closeness of agreement between a test result and the true value or an accepted reference value. For drug substances, accuracy is established by application of the analytical procedure to an analyte of known purity or by comparison to a well-characterized method. For drug products, it is demonstrated by spiking known amounts of the analyte into the sample matrix (placebo) and determining recovery [2].
- Precision: Expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions. Precision is investigated at three levels: repeatability (intra-assay precision under the same operating conditions), intermediate precision (variation within a laboratory on different days, with different analysts, or different equipment), and reproducibility (precision between different laboratories) [2].
- Detection Limit (LOD) and Quantitation Limit (LOQ): The LOD is the lowest amount of analyte in a sample that can be detected, but not necessarily quantitated, under the stated experimental conditions. The LOQ is the lowest amount of analyte that can be quantitatively determined with suitable precision and accuracy. ICH Q2(R1) acknowledges that these can be determined based on visual evaluation, signal-to-noise ratio (typically 3:1 for LOD and 10:1 for LOQ), or a calculation based on the standard deviation of the response and the slope of the calibration curve [2].
- Linearity: The ability of the method to obtain test results that are directly proportional to the concentration of the analyte in the sample within a given range. It is typically established by evaluating a minimum of five concentrations and is reported along with the correlation coefficient, y-intercept, and slope of the regression line [2].
- Range: The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the analytical procedure has a suitable level of precision, accuracy, and linearity. The guideline specifies minimum ranges relative to the intended application of the method (e.g., for assay of a drug substance, the range is typically 80-120% of the test concentration) [2].
- Robustness: A measure of the analytical procedure's capacity to remain unaffected by small, deliberate variations in procedural parameters (such as pH, mobile phase composition, temperature, or flow rate in HPLC) and provides an indication of its reliability during normal usage. While ICH Q2(R1) does not mandate a specific methodology for robustness, it is expected to be studied during method development [2].
Table 2: ICH Q2(R1) Validation Parameters and Methodological Requirements
| Validation Parameter | Key Definition | Typical Experimental Methodology |
|---|---|---|
| Specificity | Ability to measure analyte unequivocally in the presence of potential interferents. | Chromatographic resolution; Peak purity via PDA or MS. |
| Accuracy | Closeness of agreement between test result and true value. | Spike/recovery experiments; Comparison to a reference method. |
| Precision | Closeness of agreement between a series of measurements. | Minimum 9 determinations over 3 concentration levels (repeatability). |
| Linearity | Ability to obtain results proportional to analyte concentration. | Minimum of 5 concentration levels. |
| Range | Interval between upper and lower analyte concentrations with suitable precision, accuracy, and linearity. | Defined based on the intended application of the method (e.g., 80-120% for assay). |
| LOD/LOQ | Lowest concentration that can be detected/quantitated. | Signal-to-noise (3:1 & 10:1) or statistical calculation (e.g., LOD=3.3σ/S). |
| Robustness | Capacity to remain unaffected by small, deliberate procedural variations. | Experimental design testing variations in key method parameters. |
Experimental Protocols: Implementing the Q2(R1) Framework
The successful implementation of ICH Q2(R1) requires carefully designed experimental protocols to generate the necessary data to demonstrate each validation characteristic. The following sections detail the standard methodologies employed by scientists to validate an analytical procedure, such as a High-Performance Liquid Chromatography (HPLC) method for a drug substance or product.
Protocol for Accuracy and Precision
Objective: To demonstrate that the method yields results that are both correct (accurate) and reproducible (precise). Materials: Drug substance standard, placebo matrix (for drug product), appropriate solvents and reagents, volumetric glassware, and HPLC system. Procedure:
- For a drug product, prepare a placebo mixture excluding the active ingredient.
- Prepare a minimum of nine samples over a minimum of three concentration levels (e.g., 80%, 100%, 120% of the target concentration), with three replicates at each level. For repeatability, six replicates at 100% of the test concentration may also be acceptable [2].
- Analyze each sample according to the proposed method.
- For Accuracy: Calculate the percent recovery of the known, added amount for each sample. The mean recovery should be within predefined acceptance criteria (e.g., 98-102%).
- For Precision (Repeatability): Calculate the relative standard deviation (RSD%) of the results for the replicates at each concentration level. The RSD should meet predefined criteria, which are often tighter for the 100% level.
- For Intermediate Precision: Have a second analyst repeat the entire procedure on a different day, using a different HPLC system and freshly prepared standards and reagents. Compare the results from both analysts statistically (e.g., using a Student's t-test) to ensure no significant difference exists [2].
Protocol for Specificity
Objective: To prove the method can distinguish and quantify the analyte in the presence of other components. Materials: Drug substance standard, known impurities/degradation products (if available), placebo matrix, forced degradation samples (e.g., exposed to heat, light, acid, base, oxidation). Procedure:
- Inject a blank (solvent) and the placebo preparation to demonstrate no interference at the retention time of the analyte.
- Inject the analyte standard to document its retention time and peak characteristics.
- Inject samples containing the analyte spiked with all available impurities and degradation products.
- Demonstrate that the analyte peak is baseline-resolved from all other peaks, with a resolution factor (Rs) typically greater than 1.5 [2].
- Use peak purity assessment tools (e.g., PDA or MS) to confirm that the analyte peak is homogeneous and not co-eluting with any interferent.
Protocol for Linearity and Range
Objective: To establish that the method provides a proportional response to analyte concentration and to define the working range. Materials: Drug substance standard, volumetric glassware. Procedure:
- Prepare a minimum of five standard solutions spanning the claimed range of the procedure (e.g., 50%, 80%, 100%, 120%, 150% for an impurity method).
- Analyze each standard solution in triplicate.
- Plot the mean response against the concentration.
- Perform linear regression analysis on the data. Report the correlation coefficient (r), coefficient of determination (r²), y-intercept, and slope of the regression line.
- The range is validated by demonstrating that the method meets the acceptance criteria for accuracy, precision, and linearity across the entire interval.
Diagram: ICH Q2(R1) Analytical Method Validation Workflow. This diagram outlines the typical sequence for validating an analytical procedure, beginning with specificity assessment and progressing through the core validation parameters.
The Scientist's Toolkit: Essential Reagents and Materials
The experimental protocols mandated by ICH Q2(R1) rely on a set of essential research reagents and materials to ensure the validity and reliability of the data generated. The following table details these key items and their critical functions within the validation framework.
Table 3: Essential Research Reagent Solutions and Materials for ICH Q2(R1) Validation
| Tool/Reagent | Function in Validation |
|---|---|
| Characterized Reference Standard | Serves as the benchmark for identity, purity, and potency; essential for preparing calibration standards for linearity, accuracy, and precision studies. |
| Placebo Matrix | For drug product methods, this mixture of excipients without the active ingredient is crucial for demonstrating specificity and for conducting spike/recovery experiments to prove accuracy. |
| Known Impurities and Degradation Products | Used in specificity experiments to demonstrate resolution from the main analyte and to validate impurity methods. When unavailable, forced degradation studies become more critical. |
| High-Purity Solvents and Reagents | Essential for preparing mobile phases, standard and sample solutions; ensures no interference, maintains system performance, and guarantees the reliability of the validation data. |
| Forced Degradation Samples | Samples of the drug substance or product stressed under various conditions (heat, light, acid, base, oxidation) are used to demonstrate the stability-inducing capability and specificity of the method. |
| Volumetric Glassware/Calibrated Balances | Foundational for ensuring the accuracy of all solution preparations, dilutions, and weighings, which directly impacts the reliability of all validation parameters. |
| 1-Azido-3-fluoro-5-methylbenzene | 1-Azido-3-fluoro-5-methylbenzene, CAS:1511741-94-8, MF:C7H6FN3, MW:151.14 g/mol |
| 1-(Chloromethyl)-2,6-dimethylnaphthalene | 1-(Chloromethyl)-2,6-dimethylnaphthalene, CAS:107517-28-2, MF:C13H13Cl, MW:204.69 g/mol |
The introduction of ICH Q2(R1) marked a paradigm shift in pharmaceutical analysis, establishing a unified, science-based standard for demonstrating the reliability of analytical methods. By harmonizing the definitions and methodologies for key validation parameters, it provided a common technical language that facilitated global drug development and registration [6]. This guideline became the undisputed international gold standard, ensuring that data generated in one part of the world could be trusted by regulators in another, thereby eliminating unnecessary repetition of studies and accelerating the availability of medicines to patients. The robustness and clarity of the Q2(R1) framework have ensured its longevity, remaining the cornerstone of analytical quality control for nearly two decades after its unification in 2005.
The legacy of ICH Q2(R1) extends beyond its direct application. It laid the essential foundation upon which subsequent guidelines, such as the recently adopted ICH Q2(R2) and ICH Q14 on Analytical Procedure Development, are built [9]. These new guidelines introduce a more modern, lifecycle approach to method development and validation, incorporating Quality by Design (QbD) principles and enhanced risk management. However, they do not replace the core parameters established by Q2(R1); rather, they augment and contextualize them within a more comprehensive framework [9]. Therefore, a thorough understanding of ICH Q2(R1) remains indispensable for any scientist or regulator involved in pharmaceutical development. It represents a critical chapter in the history of analytical method validation, one that instilled global harmony and continues to underpin the quality, safety, and efficacy of medicines worldwide.
In the history of analytical science, the establishment of formal validation protocols marks the transition from art to science, providing a standardized framework for ensuring that analytical methods consistently produce reliable, trustworthy data. Analytical method validation is the process of providing documented evidence that a test procedure does what it is intended to do, establishing through laboratory studies that the method's performance characteristics meet the requirements for its intended analytical application [2]. In regulated environments, this process is not merely good science—it is a fundamental regulatory requirement for all drug substance and drug product analytical procedures [11].
The evolution of validation guidelines, driven by agencies like the FDA and the International Conference on Harmonisation (ICH) since the late 1980s, has created a harmonized understanding of the core pillars that underpin method validity [2] [12]. These pillars—including accuracy, precision, specificity, and others—form an interlocking system of checks that collectively demonstrate a method's suitability. This guide explores these fundamental parameters in detail, providing researchers and drug development professionals with both the theoretical foundation and practical methodologies needed for rigorous method validation.
Historical Context of Validation Guidelines
The formalization of analytical method validation began in earnest in the late 1980s when regulatory bodies started issuing comprehensive guidelines. A pivotal moment came in 1987, when the FDA designated the specifications in the United States Pharmacopeia (USP) as legally recognized for determining compliance with the Federal Food, Drug, and Cosmetic Act [2]. This established a benchmark for method quality and consistency.
Subsequent decades saw significant efforts to harmonize requirements internationally. The landmark 1990 publication by Shah et al., "Analytical methods validation: bioavailability, bioequivalence and pharmacokinetic studies," laid important groundwork for bioanalytical method validation [13]. The FDA's 1999 draft guidance and its final 2001 "Guidance for Industry: Bioanalytical Method Validation" further refined these concepts, solidifying the core parameters discussed in this document [13]. The ICH Q2(R1) guideline, harmonizing requirements across the United States, Europe, and Japan, has become the contemporary international standard, defining the essential performance characteristics that constitute a validated analytical method [2].
The Fundamental Validation Parameters
Specificity
Definition and Importance: Specificity is the ability of a method to measure accurately and specifically the analyte of interest in the presence of other components that may be expected to be present in the sample matrix [2]. It ensures that a peak's response is due to a single component, accounting for potential interference from excipients, impurities, or degradation products [14] [2]. This parameter is typically tested first, as it confirms the method is detecting the correct target.
Experimental Protocol: For chromatographic methods, specificity is demonstrated by the resolution of the two most closely eluted compounds, usually the major component and a closely-eluting impurity [2]. If impurities are available, specificity is shown by spiking the sample with these materials and demonstrating that the assay is unaffected. When impurities are unavailable, results are compared to a second well-characterized procedure [2]. Modern practice recommends using peak-purity tests based on photodiode-array (PDA) detection or mass spectrometry (MS) to demonstrate specificity by comparing results to a known reference material [2].
Accuracy
Definition and Importance: Accuracy expresses the closeness of agreement between the value found and either a conventional true value or an accepted reference value [14] [2]. It is a measure of an analytical method's exactness, sometimes termed "trueness," and is established across the method's specified range.
Experimental Protocol: Accuracy is measured as the percent of analyte recovered by the assay [2]. For drug substances, accuracy is determined by comparing results to the analysis of a standard reference material or a second, well-characterized method. For drug products, accuracy is evaluated by analyzing synthetic mixtures spiked with known quantities of components [2]. Guidelines recommend collecting data from a minimum of nine determinations over at least three concentration levels covering the specified range (three concentrations, three replicates each) [2]. Data should be reported as percent recovery of the known, added amount, or as the difference between the mean and true value with confidence intervals.
Precision
Definition and Importance: Precision expresses the closeness of agreement among individual test results from repeated analyses of a homogeneous sample [2]. It is commonly evaluated at three levels: repeatability, intermediate precision, and reproducibility.
Experimental Protocol:
- Repeatability (intra-assay precision): Assesses results over a short time interval under identical conditions. Guidelines suggest a minimum of nine determinations covering the specified range (three levels/concentrations, three repetitions each) or a minimum of six determinations at 100% of the test concentration [2]. Results are typically reported as % RSD (Relative Standard Deviation).
- Intermediate precision: Evaluates within-laboratory variations from random events such as different days, analysts, or equipment. An experimental design should be used to monitor effects of individual variables, typically involving two analysts preparing and analyzing replicate sample preparations using different HPLC systems [2]. The %-difference in mean values is statistically tested (e.g., Student's t-test).
- Reproducibility: Represents collaborative studies between different laboratories, requiring comparison of standard deviation, relative standard deviation, and confidence intervals [2].
Table 1: Precision Measurements and Their Specifications
| Precision Type | Conditions | Minimum Testing Requirements | Reporting Metrics |
|---|---|---|---|
| Repeatability | Same analyst, same day, identical conditions | 9 determinations across 3 concentration levels or 6 determinations at 100% test concentration | % RSD |
| Intermediate Precision | Different days, different analysts, different equipment | Two analysts preparing and analyzing replicates independently | %-difference in means, statistical testing |
| Reproducibility | Different laboratories | Collaborative studies between laboratories | Standard deviation, % RSD, confidence intervals |
Sensitivity (Limit of Detection and Limit of Quantitation)
Definition and Importance: Sensitivity encompasses both the Limit of Detection (LOD) and Limit of Quantitation (LOQ). The LOD is the lowest concentration of an analyte that can be detected but not necessarily quantitated, while the LOQ is the lowest concentration that can be quantitated with acceptable precision and accuracy [2].
Experimental Protocol: The most common approach uses signal-to-noise ratios (S/N)—typically 3:1 for LOD and 10:1 for LOQ [2]. An alternative calculation-based method uses the formula: LOD/LOQ = K(SD/S), where K is a constant (3 for LOD, 10 for LOQ), SD is the standard deviation of response, and S is the slope of the calibration curve [2]. Regardless of the determination method, an appropriate number of samples must be analyzed at the calculated limit to fully validate method performance at that level.
Linearity and Range
Definition and Importance: Linearity is the ability of a method to provide test results directly proportional to analyte concentration within a given range [14]. The range is the interval between upper and lower analyte concentrations that have been demonstrated to be determined with acceptable precision, accuracy, and linearity using the method as written [2].
Experimental Protocol: Guidelines specify a minimum of five concentration levels to determine range and linearity [2]. The range should be expressed in the same units as test results. Data reporting should include the equation for the calibration curve line, the coefficient of determination (r²), residuals, and the curve itself.
Table 2: Minimum Recommended Ranges for Analytical Methods
| Method Type | Minimum Recommended Range |
|---|---|
| Assay | 80-120% of target concentration |
| Impurity Testing | From reporting level to 120% of specification |
| Content Uniformity | 70-130% of target concentration |
| Dissolution Testing | ±20% over specified range |
Robustness
Definition and Importance: Robustness measures a method's capacity to remain unaffected by small, deliberate variations in method parameters, providing an indication of reliability during normal usage [14] [2]. This parameter evaluates how resistant the method is to typical operational fluctuations.
Experimental Protocol: Robustness is tested by deliberately varying method parameters around specified values and assessing the impact on method performance [14] [2]. For chromatographic methods, this might include variations in pH, mobile phase composition, columns, temperature, or flow rate. In a Quality by Design (QbD) approach, key parameters are varied during method development to identify and address potential issues early.
The Validation Workflow Relationship
The fundamental validation parameters are interconnected through a logical workflow. The following diagram illustrates their relationships and the typical sequence of evaluation:
Essential Research Reagent Solutions and Materials
Successful method validation requires specific high-quality materials and reagents. The following table outlines key solutions and their functions in validation experiments:
Table 3: Essential Research Reagent Solutions for Method Validation
| Reagent/Material | Function in Validation |
|---|---|
| Standard Reference Materials | Provides accepted reference values for accuracy determination and method calibration [2] |
| Chromatographic Columns | Stationary phases for separation; critical for testing specificity and robustness [2] |
| Mobile Phase Components | Liquid phase for chromatographic separation; composition affects specificity and robustness [2] |
| Matrix Blanks | Sample matrix without target analyte; essential for specificity testing to confirm no interference [14] |
| Impurity Standards | Isolated impurities for specificity testing; demonstrate method can distinguish analyte from impurities [2] |
| System Suitability Standards | Reference mixtures to verify chromatographic system performance before validation testing [12] |
The fundamental validation parameters—specificity, accuracy, precision, sensitivity, linearity, range, and robustness—represent the essential pillars supporting reliable analytical methods. These parameters form an interconnected framework that collectively demonstrates a method's suitability for its intended purpose. As the pharmaceutical industry evolves, with emerging trends like continuous process verification and digital transformation gaining prominence, these core principles remain the foundation of quality and compliance [15].
Understanding these parameters, their experimental determination, and their interrelationships enables researchers to develop robust methods that generate reliable data, support regulatory submissions, and ultimately ensure product quality and patient safety. While validation approaches may be phased appropriately across drug development stages, the fundamental pillars remain constant, providing the scientific rigor necessary for confident decision-making throughout the product lifecycle [11].
The Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in the European Union establish and enforce the regulatory frameworks that guarantee the safety, efficacy, and quality of pharmaceutical products [16]. While sharing this common mission, their distinct approaches have profoundly influenced global industry practices, particularly in the realm of analytical method validation and quality assurance. The foundational FDA Current Good Manufacturing Practice (CGMP) regulations stipulate minimum requirements for the methods, facilities, and controls used in manufacturing, processing, and packing of a drug product, ensuring it is safe for use and possesses the ingredients and strength it claims to have [17]. The historical trajectory of analytical method validation protocols reveals a significant evolution: a shift from a compliance-driven, quality-by-testing paradigm to a modern, proactive framework centered on Quality by Design (QbD) and risk-based approaches across the entire product life cycle [18]. This whitepaper examines how the adoption and implementation of FDA and EMA guidelines have shaped and continue to transform industry standards and experimental protocols.
Historical Evolution of Validation Guidelines
The concept of validation within the pharmaceutical industry has undergone a fundamental transformation over the past several decades, driven largely by regulatory initiatives.
The Paradigm Shift to Quality by Design
The initial validation principles, as outlined in the FDA's 1987 guidance on general principles of process validation, focused on a traditional "fixed-point" approach where validation activities were typically concentrated in the late stages of product development, just before commercial filing [18]. A significant quality paradigm shift began in the early 2000s, moving toward building quality into the product and process design. As defined by the FDA, Quality by Design (QbD) is "a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management" [18]. Regulatory agencies actively encouraged this shift through various initiatives, including the FDA's 2004 report "Pharmaceutical cGMPs for the 21st Century – A Risk Based Approach" and the subsequent development of the ICH Q8, Q9, and Q10 guidelines, which outlined the scientific and risk-based foundations for pharmaceutical development and quality systems [18].
The Analytical Procedure Life Cycle
The validation of analytical procedures has mirrored this broader evolution. The traditional, checklist approach to method validation is being superseded by the Analytical Procedure Life Cycle (APLC) model, an enhanced approach driven by Analytical Quality by Design (AQbD) principles [18]. This holistic model, reflected in modern guidelines like USP General Chapter <1220> and the new ICH Q14 and Q2(R2) guidelines, provides connectivity between all stages of an analytical procedure's life—from initial design and development to continuous performance monitoring [18]. The major driver for this life cycle approach is to ensure the "fitness for use" of the reportable value, which forms the basis for critical decisions regarding a product's quality and compliance [18]. This represents a fundamental change in philosophy, from merely satisfying regulatory requirements to achieving a deep scientific understanding of the analytical procedure itself.
The following timeline illustrates the key milestones in this regulatory and conceptual evolution:
Comparative Analysis of FDA and EMA Regulatory Frameworks
Understanding the distinct organizational structures and philosophical approaches of the FDA and EMA is crucial for navigating their respective guidelines and their impact on industry practices.
Organizational Structure and Governance
The FDA operates as a centralized federal authority within the U.S. Department of Health and Human Services. Its Center for Drug Evaluation and Research (CDER) possesses direct decision-making power to approve, reject, or request additional information for new drug applications (NDAs) and Biologics License Applications (BLAs) [16]. This centralized model enables relatively swift decision-making, with review teams composed of full-time FDA employees, and results in immediate nationwide market access upon approval [16].
In contrast, the EMA functions as a coordinating body within a network of national competent authorities across EU Member States. For the centralized procedure, the Committee for Medicinal Products for Human Use (CHMP) conducts the scientific evaluation, but the legal authority to grant marketing authorization resides with the European Commission [16]. This network model incorporates broader scientific perspectives from across Europe but requires more complex coordination, reflecting diverse healthcare systems and medical traditions [16].
Key Differences in Regulatory Approaches
The structural differences between the two agencies lead to variations in their regulatory approaches, which are summarized in the table below.
Table 1: Key Regulatory Differences Between FDA and EMA
| Aspect | U.S. FDA | European Medicines Agency (EMA) |
|---|---|---|
| Organizational Structure | Centralized federal authority [16] | Coordinating network of national agencies [16] |
| Primary Application Types | New Drug Application (NDA), Biologics License Application (BLA) [16] | Centralized, Decentralized, and National Procedures [16] |
| Expedited Programs | Fast Track, Breakthrough Therapy, Accelerated Approval, Priority Review [16] | Accelerated Assessment, Conditional Approval [16] |
| Pediatric Requirements | Pediatric Research Equity Act (PREA) - studies often post-approval [16] | Pediatric Investigation Plan (PIP) - agreed before pivotal adult studies [16] |
| Risk Management | Risk Evaluation and Mitigation Strategy (REMS) when necessary [16] | Risk Management Plan (RMP) required for all new applications [16] |
| Clinical Trial Comparator | More accepting of placebo-controlled trials [16] | Generally expects comparison against relevant existing treatments [16] |
These differences necessitate strategic planning by drug developers aiming for both the U.S. and EU markets. For instance, a clinical trial designed to meet EMA's expectations for an active comparator may be more complex and costly than a placebo-controlled trial that might be acceptable to the FDA [16].
Impact on Industry Practices and Standards
The divergent and convergent paths of FDA and EMA guidelines have directly shaped how pharmaceutical companies operate, from clinical development to quality control.
Clinical Trial Design and Conduct
The recent finalization of ICH E6(R3) Good Clinical Practice in 2025 marks a significant evolution, introducing flexible, risk-based approaches and embracing innovations in trial design, conduct, and technology [19] [20]. This update, adopted by both the FDA and EU member states, encourages the use of a broader range of modern trial designs and data sources while maintaining a focus on participant protection and data reliability [19]. Furthermore, disease-specific guidelines continue to evolve. A 2025 comparative analysis of FDA and EMA guidelines for ulcerative colitis (UC) trials highlighted the FDA's 2022 emphasis on balanced participant representation and the use of full colonoscopy for endoscopic assessment, posing new implementation challenges for sponsors [21].
Chemistry, Manufacturing, and Controls (CMC)
The area of CMC has seen both significant regulatory convergence and notable ongoing differences. The EMA's 2025 guideline on clinical-stage Advanced Therapy Medicinal Products (ATMPs) serves as a primary reference, consolidating over 40 previous documents [22]. From a CMC perspective, the guideline's structure aligns well with the Common Technical Document (CTD) format, indicating substantial convergence between FDA and EMA expectations for organizing CMC information [22]. However, critical differences remain, particularly for cell-based therapies. These include divergent requirements for allogeneic donor eligibility determination, where the FDA is more prescriptive, and varying expectations for GMP compliance, with the EU mandating self-inspections and the FDA employing a phased, attestation-based approach verified later via pre-license inspection [22].
The Modern Analytical Toolkit: Research Reagent Solutions
The implementation of modern, QbD-driven validation protocols requires a suite of specialized reagents and materials. The following table details key components of the researcher's toolkit for robust analytical method development and validation.
Table 2: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Function in Validation Protocols |
|---|---|
| System Suitability Standards | Verifies chromatographic system performance prior to and during analysis to ensure data validity [18]. |
| Reference Standards (Primary & Secondary) | Serves as the definitive benchmark for quantifying the analyte of interest and establishing method accuracy [13]. |
| Stability-Indicating Metrics | Used in forced degradation studies to demonstrate the method's specificity in detecting analyte degradation [18]. |
| Critical Reagent Kits (e.g., for ELISA) | Provides key components for ligand-binding assays; requires rigorous characterization and stability testing [13]. |
| Matrix Components (e.g., serum, plasma) | Essential for validating bioanalytical methods to assess and control for matrix effects and ensure selectivity [13]. |
| Benzo[c]isothiazole-5-carbaldehyde | Benzo[c]isothiazole-5-carbaldehyde |
| 2-Amino-6-isopropylpyrimidin-4-ol | 2-Amino-6-isopropylpyrimidin-4-ol, CAS:73576-32-6, MF:C7H11N3O, MW:153.18 g/mol |
Detailed Experimental Protocols for Method Validation
Adherence to regulatory guidelines requires the execution of standardized, well-documented experimental protocols. The following sections outline core methodologies for validating analytical procedures under the modern life cycle framework.
Protocol for Bioanalytical Method Validation
This protocol is based on FDA and consensus guidelines for validating ligand-binding assays (e.g., ELISA) used in pharmacokinetic studies [13].
- Objective: To establish and document that the bioanalytical method is suitable for the reliable quantification of the analyte in a specific biological matrix.
- Materials:
- Reference Standard: Analyte of known purity and identity.
- Quality Control (QC) Samples: Prepared in the same biological matrix as study samples at low, medium, and high concentrations.
- Critical Reagents: Including antibodies, conjugates, and substrates. Full characterization data (source, lot, concentration) must be documented.
- Methodology:
- Selectivity and Specificity: Assess interference from at least 6 individual sources of the matrix. Cross-reactivity with structurally similar compounds should be evaluated.
- Accuracy and Precision: Perform a minimum of 5 runs per concentration level (LLOQ, Low, Mid, High QC) with 5 replicates per run. Accuracy should be within ±20% (±25% for LLOQ) of the nominal value, and precision should not exceed 20% CV (25% for LLOQ).
- Calibration Curve: Generate using a minimum of 6 non-zero concentrations. The curve model (e.g., 4- or 5-parameter logistic) must be justified and consistently used.
- Stability: Conduct experiments to evaluate analyte stability in the matrix under conditions of storage, freeze-thaw cycles, and benchtop temperatures.
Protocol for Analytical Procedure Life Cycle (APLC) Implementation
This protocol describes the enhanced approach for pharmaceutical analysis as per ICH Q2(R2) and USP <1220> [18].
- Stage 1: Procedure Design
- Define an Analytical Target Profile (ATP): A prospective description of the required quality of the reportable value and the level of uncertainty that is fit for purpose.
- Example ATP: "The procedure must be able to quantify impurity X in the drug substance with a target uncertainty of ±0.05% at a specification level of 0.5%."
- Risk Assessment: Use tools (e.g., Fishbone diagram, FMEA) to identify and rank potential method variables (instrument, analyst, reagent) that could impact the ATP.
- Stage 2: Procedure Performance Qualification
- This stage aligns with the traditional validation study but is guided by the ATP.
- Experiments are designed to confirm that the procedure performs as intended, testing parameters such as accuracy, precision, specificity, and range.
- The establishment of an Analytical Control Strategy is critical, defining the level of control for each critical method parameter.
- Stage 3: Ongoing Procedure Performance Verification
- System Suitability Tests (SST): Defined based on the ATP to ensure the procedure is functioning correctly at the time of use.
- Continuous Monitoring: Reportable values and associated QC data are tracked over time to verify the procedure remains in a state of control.
- Knowledge Management: All data and decisions from the procedure's life cycle are documented, facilitating any future changes or improvements.
The workflow for this life cycle approach is systematic and iterative, as shown below:
Case Studies in Regulatory Adoption
Advanced Therapy Medicinal Products (ATMPs)
The regulation of ATMPs (cell and gene therapies) provides a clear case study of both convergence and divergence. The EMA's 2025 clinical-stage ATMP guideline is a multidisciplinary document that consolidates quality, non-clinical, and clinical requirements [22]. An analysis of its CMC section reveals significant convergence with FDA expectations, as it is structured around the CTD format, providing a common roadmap for sponsors [22]. However, practical differences persist. For example, the FDA maintains more prescriptive requirements for allogeneic donor eligibility determination, including specific tests and laboratory qualifications, whereas the EMA guideline references broader EU and member state legal requirements [22]. This divergence can create additional complexity and cost for developers pursuing global markets.
Expedited Review Pathways
Both agencies have established programs to accelerate the development and review of drugs for serious conditions, but their structures differ, shaping sponsor strategy. The FDA offers multiple, overlapping expedited programs (Fast Track, Breakthrough Therapy, Accelerated Approval, Priority Review) that can be used in combination to provide intensive FDA guidance and faster approval based on surrogate endpoints [16]. The EMA's main expedited mechanism is Accelerated Assessment, which shortens the review timeline but has more stringent eligibility criteria [16]. A 2025 development is the FDA's pilot of a Commissioner's National Priority Voucher (CNPV) program, which suggests that drug pricing, an area traditionally outside the FDA's remit, could informally influence regulatory prioritization, representing a significant potential shift in regulatory policy [23].
The landscape of pharmaceutical regulation and analytical validation is dynamic. The guidelines issued by the FDA and EMA have been instrumental in shaping industry practices, driving a global shift toward more scientific, risk-based, and life cycle-oriented approaches. The ongoing adoption of ICH E6(R3) for clinical trials and the finalization of ICH Q14 and Q2(R2) for analytical procedures will further embed these principles, promoting greater international harmonization [19] [20] [18]. Future developments will likely focus on the integration of advanced technologies and data analytics, continued efforts toward global regulatory convergence for complex products like ATMPs [22], and adapting regulatory frameworks to accommodate innovations such as continuous manufacturing [18]. For researchers and drug development professionals, a deep and nuanced understanding of both the similarities and differences between FDA and EMA guidelines remains not just a regulatory necessity, but a strategic imperative for efficient global drug development.
The evolution of analytical method validation is characterized by a significant "Prescriptive Era," a period dominated by standardized, checklist-based protocols. These early approaches provided the foundational framework for ensuring data quality, safety, and efficacy in drug development and other scientific fields by offering a structured means of compliance with growing regulatory requirements. Framed within the history of analytical method validation protocols, this era represents a critical transition from informal, idiosyncratic practices to a more systematic and defensible approach to quality assurance. For researchers, scientists, and drug development professionals, understanding the strengths and limitations of these early checklist methodologies is not merely an academic exercise; it provides essential context for contemporary validation practices and informs the development of next-generation protocols [24] [25]. This whitepaper delves into the core principles of these prescriptive approaches, evaluates their enduring strengths and inherent limitations, and details the experimental protocols that characterized this formative period in pharmaceutical sciences.
Historical Context and Defining the "Prescriptive Era"
The "Prescriptive Era" in analytical method validation emerged as a direct response to the increasing complexity of pharmaceutical analysis and the need for international regulatory harmonization. Prior to this period, method validation was often an informal process, varying significantly between laboratories and lacking standardized criteria. The impetus for change was the necessity to prove that an analytical method was acceptable for its intended use, ensuring that measurements of a drug's potency, bioavailability, and stability were accurate, specific, and reliable [24] [25].
The formalization of this era was largely driven by the establishment of guidelines from international regulatory bodies. The International Conference on Harmonisation (ICH) played a pivotal role with the issuance of two landmark guidelines: Q2A, "Text on Validation of Analytical Procedures" (1994) and Q2B, "Validation of Analytical Procedure: Methodology" (1996). These documents, alongside standards from the United States Pharmacopeia (USP) and the U.S. Food and Drug Administration (FDA), codified a specific set of performance parameters that required validation [24] [25]. This created a paradigm where compliance was demonstrated by systematically "checking off" a pre-defined list of validation characteristics, hence the term "checklist approach." The primary objective was to ensure that methods for analyzing drug substances and products were thoroughly characterized, providing a unified standard for industry and regulators across the United States, the European Union, and Japan [25].
Core Principles of Early Checklist Approaches
The checklist approach was fundamentally rooted in a series of core principles that emphasized standardization, comprehensiveness, and demonstrable compliance.
- Standardization and Harmonization: The primary principle was the replacement of variable, lab-specific practices with a uniform set of criteria. The ICH Q2 guidelines provided a common language and a unified set of requirements for validation, which was crucial for multinational drug development and registration [25].
- Parameter-Centric Validation: The approach decomposed the abstract concept of "method quality" into a list of discrete, measurable performance characteristics. The validation process became an exercise in empirically testing each of these parameters against pre-defined acceptance criteria [26].
- Documentation and Audit Trail: A key principle was the creation of a documented evidence trail. Validation activities were conducted according to a pre-approved validation protocol, and results were meticulously documented in a validation report, providing objective evidence for regulatory scrutiny [25].
- Fitness for Purpose: Despite its prescriptive nature, the underlying principle was to demonstrate that the method was suitable for its intended use. The specific validation parameters required varied depending on the type of analytical procedure (e.g., identification tests, impurity tests, assays) [25].
Table 1: Key Validation Parameters as Defined by ICH Q2 and Other Regulatory Guidelines
| Validation Parameter | Definition | Primary Regulatory Source |
|---|---|---|
| Accuracy | The closeness of agreement between a measured value and a true value. | ICH, USP, FDA [25] |
| Precision | The closeness of agreement between a series of measurements. Includes repeatability and intermediate precision. | ICH, USP, FDA [25] |
| Specificity | The ability to assess the analyte unequivocally in the presence of other components. | ICH, USP [25] |
| Linearity | The ability to obtain test results proportional to the concentration of the analyte. | ICH, USP, FDA [25] |
| Range | The interval between the upper and lower concentrations of analyte for which suitability has been demonstrated. | ICH, USP, FDA [25] |
| Detection Limit (LOD) | The lowest amount of analyte that can be detected, but not necessarily quantified. | ICH, USP [25] |
| Quantitation Limit (LOQ) | The lowest amount of analyte that can be quantitatively determined. | ICH, USP [25] |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters. | ICH, USP [25] |
Strengths of the Checklist Paradigm
The prescriptive, checklist-based approach brought about transformative strengths that addressed critical needs in pharmaceutical analysis and regulation.
Foundation for Regulatory Compliance and Harmonization
The ICH Q2 guidelines provided a clear, internationally accepted roadmap for meeting regulatory expectations. This harmonization simplified the drug approval process across different regions, reduced redundant testing, and provided a definitive standard for audits and inspections. For scientists, it eliminated guesswork regarding what was required for method validation, ensuring that development efforts were aligned with global regulatory requirements from the outset [24] [25].
Enhanced Consistency and Data Quality
By mandating a standard set of experiments, the checklist approach ensured a consistent and comprehensive evaluation of analytical methods. This systematic process significantly reduced the risk of overlooking critical performance characteristics, thereby improving the overall quality and reliability of analytical data. It provided a structured framework that was particularly valuable for less experienced analysts, ensuring thoroughness regardless of an individual's level of expertise [27] [28].
Improved Communication and Efficiency
The establishment of standardized terminology and parameters fostered clear and unambiguous communication between laboratories, sponsors, and regulatory agencies. Furthermore, the use of a predefined checklist streamlined the validation process itself, making audit preparation more efficient and facilitating the delegation of specific tasks within a team [28].
Table 2: Quantitative Strengths of Checklist-Based Validation Approaches
| Strength | Quantitative or Qualitative Impact | Evidence from Broader Applications |
|---|---|---|
| Consistency & Completeness | Ensures common and known risks/parameters are not overlooked [27]. | In risk management, checklist analysis provides a "comprehensive starting point" and ensures completeness [27]. |
| Efficiency & Speed | Accelerates audit preparation and the questioning process [28]. | Checklists are noted for their ability to speed up processes and are an "efficient use of time and resources" [27] [28]. |
| Structured Guidance | Supports less experienced team members by providing a clear roadmap [27]. | Checklist analysis "helps less experienced team members identify risks" and "support auditor knowledge" [27] [28]. |
| Facilitation of Delegation | Allows a lead auditor to unambiguously delegate sections of an audit [28]. | Checklists provide clear accountability, enabling effective delegation within a team [28]. |
Limitations and Critical Weaknesses
Despite its foundational strengths, the rigid application of the checklist paradigm revealed several significant limitations that prompted the evolution of validation science.
The "Tick-Box" Mentality and Suppression of Scientific Judgment
A primary criticism was the tendency for the process to devolve into a mechanical "tick-box" exercise. This mentality could lead to a superficial review where the mere completion of a test was prioritized over a deep, scientific understanding of the method's behavior and limitations. Auditors and analysts relying solely on checklists could miss subtle but critical issues not explicitly listed, as the rigid structure discouraged professional curiosity and critical thinking beyond the set questions [29] [28].
Inherent Lack of Flexibility
Checklists, by their nature, are often generic to allow for wide application. This can render them unsuitable for novel or highly complex methodologies that do not fit the standard mold. They lack the flexibility to adapt to unique project-specific risks, emerging technologies, or non-routine scenarios, potentially stifling innovation and failing to address the most relevant questions for a given method's specific context [27] [28].
Failure to Address Broader Implications
The early checklist approach was predominantly focused on the technical performance of the method itself. It often failed to adequately consider the broader consequences of the assessment, a key source of validity evidence in modern frameworks [30]. This includes the impact of the method's results on downstream decisions, patient safety, and the potential for unintended negative effects, such as unnecessary re-testing or incorrect batch release decisions based on a technically "valid" but practically flawed method [30].
Risk of Becoming Outdated
Checklists require continuous maintenance to remain relevant. As new scientific knowledge, technologies, and types of therapeutics (e.g., biologics, cell therapies) emerge, a static checklist can quickly become obsolete. Without regular updating based on lessons learned, they may perpetuate the evaluation of irrelevant parameters while missing new, important risks [27].
Diagram: Checklist Approach Strengths and Limitations - This workflow illustrates the parallel paths of strengths (red) and limitations (blue) that result from applying a prescriptive checklist to analytical method validation, leading to a mixed outcome.
Detailed Experimental Protocols of the Prescriptive Era
The validation process during the Prescriptive Era was characterized by a series of standardized, well-defined experimental protocols designed to measure each parameter on the checklist.
Protocol for Accuracy
- Objective: To demonstrate the closeness of agreement between the measured value and the value accepted as a true value.
- Methodology: This was typically determined by analyzing samples spiked with known quantities of the analyte (drug substance) into a placebo or a synthetic mixture of excipients. The study was performed at a minimum of three concentration levels (e.g., 80%, 100%, 120% of the target concentration), with multiple replicates (e.g., n=3) at each level.
- Data Analysis: The recovery of the analyte at each level was calculated as:
(Measured Concentration / Spiked Concentration) * 100%. The mean recovery across all levels, along with the relative standard deviation, was then reported and evaluated against pre-defined acceptance criteria (e.g., mean recovery of 98-102% with RSD ≤ 2%) [25].
Protocol for Precision
- Objective: To evaluate the degree of scatter in a series of measurements under prescribed conditions.
- Methodology: Precision was investigated at multiple levels:
- Repeatability: Multiple injections (n=6) of a homogeneous sample at 100% of the test concentration by a single analyst using the same equipment on the same day.
- Intermediate Precision: The same repeatability experiment performed by different analysts, on different days, or using different instruments within the same laboratory.
- Data Analysis: The standard deviation or relative standard deviation (RSD) of the results was calculated. Acceptance criteria were set, for example, as RSD ≤ 1.0% for an assay [25].
Protocol for Linearity and Range
- Objective: To demonstrate that the analytical procedure produces results directly proportional to analyte concentration.
- Methodology: A series of standard solutions were prepared across a specified range (e.g., 50-150% of the target concentration). A minimum of five concentration levels were analyzed.
- Data Analysis: The instrument response (e.g., peak area) was plotted against concentration. The data was subjected to linear regression analysis to calculate the correlation coefficient (r), y-intercept, slope, and residual sum of squares. Acceptance criteria typically required a correlation coefficient (r) ≥ 0.999 [25].
Protocol for Specificity
- Objective: To prove that the measured response is due solely to the analyte of interest.
- Methodology: For chromatographic methods, this involved challenging the method by analyzing blank samples (placebo), samples spiked with potential interferents (degradation products, synthetic impurities, excipients), and stressed samples (e.g., exposed to heat, light, acid, base, oxidation).
- Data Analysis: Chromatograms were examined for peak purity (e.g., using diode array or mass spectrometry detection) and resolution. The method was considered specific if the analyte peak was pure and baseline-separated from all other peaks, and the blank showed no interference [25].
Table 3: The Scientist's Toolkit: Essential Reagents and Materials for Validation Experiments
| Item | Function in Validation |
|---|---|
| Drug Substance (Active Pharmaceutical Ingredient) | Serves as the primary analyte for which the method is being validated. Used to prepare standard and sample solutions for accuracy, linearity, and precision studies. |
| Placebo (Excipient Mixture) | The formulation matrix without the active ingredient. Used in specificity and accuracy experiments to demonstrate the absence of interference and to simulate the real sample. |
| Certified Reference Standards | Highly characterized materials with known purity and identity. Used to calibrate instruments and prepare standard solutions for generating the calibration curve in linearity studies. |
| Forced Degradation Samples | Samples of the drug substance or product intentionally degraded under stress conditions (heat, light, acid, base, oxidation). Used to demonstrate the method's stability-indicating properties and specificity. |
| Chromatographic Solvents & Reagents | High-purity mobile phase components, buffers, and diluents. Their quality and consistency are critical for achieving robust and reproducible chromatographic performance. |
The Prescriptive Era, with its steadfast reliance on checklist approaches, laid the indispensable groundwork for modern analytical method validation. It successfully instilled discipline, harmonized global standards, and provided a clear, auditable framework for proving method suitability. The strengths of this era—regulatory clarity, consistency, and improved data quality—are undeniable and continue to underpin current good manufacturing practices. However, the limitations of this paradigm, particularly its inflexibility, potential to stifle scientific judgment, and narrow focus on technical parameters over broader implications, ultimately drove the evolution toward more holistic, risk-based validation frameworks. For today's drug development professional, appreciating this historical context is crucial. It underscores that while checklists remain powerful tools for ensuring comprehensiveness, they are most effective when used to support, rather than replace, expert scientific reasoning and a deep, process-oriented understanding of the analytical method. The legacy of the Prescriptive Era is not a set of obsolete rules, but a foundation upon which more dynamic and intelligent validation practices have been built.
Modern Methodologies: Implementing Phase-Appropriate and QbD-Driven Validation
The development of analytical method validation protocols represents a significant evolution in pharmaceutical sciences, shifting from rigid, one-size-fits-all approaches to flexible, risk-based strategies. The fit-for-purpose principle has emerged as a cornerstone in this historical development, recognizing that the level of analytical validation should be commensurate with the stage of drug development and the specific decision-making needs at each phase [31]. This paradigm acknowledges that early research requires different evidence than late-stage regulatory submissions, thereby optimizing resource allocation while maintaining scientific rigor.
This approach has become particularly crucial in modern drug development, especially for complex modalities like cell and gene therapies, where well-defined platform methods may not yet exist and critical quality attributes may not be fully characterized initially [32]. The phase-appropriate validation framework allows developers to generate meaningful data throughout the drug development lifecycle while progressively building the analytical evidence package required for regulatory approvals.
Conceptual Foundation of Fit-for-Purpose Validation
Core Principles and Definitions
The International Organisation for Standardisation defines method validation as "the confirmation by examination and the provision of objective evidence that the particular requirements for a specific intended use are fulfilled" [31]. This definition inherently contains the essence of the fit-for-purpose approach—the notion that validation must be tied to "specific intended use" rather than abstract perfection.
Fundamentally, fit-for-purpose assay validation progresses through two parallel tracks that eventually converge: one experimental and one operational. The experimental track establishes the method's purpose and defines acceptance criteria, while the operational track characterizes assay performance through systematic experimentation [31]. The critical evaluation occurs when technical performance is measured against pre-defined purpose—if the assay meets these expectations, it is deemed fit for that specific purpose.
The Validation Spectrum: From Exploratory to Compliant
The position of a biomarker or analytical method along the spectrum between research tool and clinical endpoint dictates the stringency of experimental proof required for method validation [31]. This spectrum encompasses:
- Exploratory assays for early discovery and candidate screening
- Fit-for-purpose assays for preclinical and early clinical phases
- Qualified assays for mid-stage clinical development
- Fully validated assays for late-stage clinical trials and commercialization [33] [34]
This framework acknowledges that method flexibility is advantageous during early development when processes and products are still being characterized, while method standardization becomes crucial during later stages when regulatory compliance and product consistency are paramount [34].
Phase-Appropriate Implementation Framework
Preclinical to Phase 1: Fit-for-Purpose Assays
During early drug development, the primary goal is generating reliable data for internal decision-making regarding candidate selection and initial safety assessment. Fit-for-purpose assays at this stage require demonstration of accuracy, reproducibility, and biological relevance sufficient to support early safety and pharmacokinetic studies [33]. These assays function as "prototypes" – developed efficiently to generate meaningful data but not yet meeting all regulatory requirements for later development stages [34].
The experimental focus at this stage involves limited verification, typically requiring 2-6 experiments to establish that methods provide reliable results for making go/no-go decisions [33]. Common applications include early-stage drug discovery screening, exploratory biomarker studies, preclinical PK/PD investigations, and proof-of-concept research [34]. According to regulatory guidelines, validation of analytical procedures is usually not required for original investigational new drug submissions for Phase 1 studies; however, sponsors must demonstrate that test methods are appropriately controlled using scientifically sound principles [32].
Phase 2 Clinical Studies: Qualified Assays
As drug development advances to Phase 2 clinical studies, the analytical requirements intensify. The focus shifts to demonstrating repeatable and robust dose-dependent responses while ensuring acceptable intermediate precision and accuracy across multiple runs [33]. This qualification stage typically requires 3-8 experiments to evaluate and refine critical performance attributes including robustness, accuracy, precision, linearity, range, specificity, and stability [33].
Table 1: Qualification Stage Assay Performance Criteria
| Performance Parameter | Preliminary Acceptance Criteria | Purpose |
|---|---|---|
| Specificity/Interference | Drug matrix/excipients don't interfere with assay signal | Ensures measurement specificity |
| Accuracy | EC50 values for Reference Standard and Test Sample agree within 20% | Measures closeness to true value |
| Precision (Replicates) | %CV for replicates within 20% | Evaluates repeatability |
| Precision (Curve Fit) | Goodness-of-fit to 4-parameter curve >95% | Assesses model appropriateness |
| Intermediate Precision | Relative Potency variation across experiments CV <30% | Measures run-to-run variability |
| Parallelism | 4-parameter logistical dose-response curves of Reference Standard and Test Sample are parallel | Ensures similar biological activity |
| Stability | Acceptable stability after 1 and 3 freeze/thaw cycles | Determines sample handling requirements |
At this stage, developers typically establish preliminary acceptance criteria and assay performance metrics through a minimum of three replicate experiments following the finalized assay protocol [33]. For more robust qualification, two analysts typically conduct at least three independent runs, each using three assay plates, enabling statistical analysis of relative potency and percent coefficient of variation (%CV) [33].
Phase 3 to Commercialization: Validated Assays
Prior to Biologics License Application (BLA) or New Drug Application (NDA) submission, assays must undergo full validation to demonstrate statistical reproducibility, robustness, and minimal variability across different analysts, facilities, equipment, and time [33]. This most rigorous stage requires 6-12 experiments performed under Good Manufacturing Practice (GMP) conditions with complete documentation and oversight from Quality Control and Quality Assurance units [33].
The validation process must align with regulatory guidance from FDA, EMA, and ICH, particularly ICH Q2(R2) on validation of analytical procedures [32]. Fully validated assays require detailed Standard Operating Procedures (SOPs) enabling any qualified operator to execute the method reliably, accompanied by comprehensive multi-page workbooks documenting all essential details including equipment, reagents, methods, and raw data [33].
Experimental Protocols for Method Validation
Biomarker Assay Classification and Validation Parameters
The American Association of Pharmaceutical Scientists (AAPS) and US Clinical Ligand Society have established five general classes of biomarker assays, each with distinct validation requirements [31]:
- Definitive quantitative assays using fully characterized reference standards representative of the biomarker
- Relative quantitative assays using reference standards not fully representative of the biomarker
- Quasi-quantitative assays without calibration standards but with continuous response
- Qualitative ordinal assays relying on discrete scoring scales
- Qualitative nominal assays for yes/no situations [31]
Table 2: Recommended Performance Parameters by Biomarker Assay Category
| Performance Characteristic | Definitive Quantitative | Relative Quantitative | Quasi-quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy | + | |||
| Trueness (bias) | + | + | ||
| Precision | + | + | + | |
| Reproducibility | + | |||
| Sensitivity | + | + | + | + |
| LLOQ | LLOQ | LLOQ | ||
| Specificity | + | + | + | + |
| Dilution Linearity | + | + | ||
| Parallelism | + | + | ||
| Assay Range | + | + | + |
For definitive quantitative methods, recognized performance standards have been established, where repeat analyses of pre-study validation samples are expected to vary by <15%, except at the lower limit of quantitation (LLOQ) where 20% is acceptable [31]. For biomarker method validation specifically, more flexibility is allowed with 25% being the default value (30% at the LLOQ) for precision and accuracy during pre-study validation [31].
Accuracy Profile Methodology
The Societe Francaise des Sciences et Techniques Pharmaceutiques (SFSTP) has developed a robust approach for fit-for-purpose validation of quantitative methods based on an accuracy profile that accounts for total error (bias and intermediate precision) with pre-set acceptance limits defined by the user [31]. This method produces a plot based on the β-expectation tolerance interval that displays the confidence interval (e.g., 95%) for future measurements, allowing researchers to visually check what percentage of future values will likely fall within pre-defined acceptance limits [31].
To construct an accuracy profile, SFSTP recommends running 3-5 different concentrations of calibration standards and 3 different concentrations of validation samples (representing high, medium, and low points on the calibration curve) in triplicate on 3 separate days [31]. Additional performance parameters including sensitivity, dynamic range, LLOQ, and upper limit of quantitation (ULOQ) can be derived from the accuracy profile [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Method Validation
| Reagent/Material | Function | Phase-Appropriate Considerations |
|---|---|---|
| Reference Standards | Serves as benchmark for quantitative measurements | Early phase: may use partially characterized materials; Late phase: requires fully characterized, GMP-produced standards |
| Master Cell Bank | Provides consistent biological material for cell-based assays | Early phase: research cell banks; Late phase: GMP-produced Master Cell Banks with complete QC/QA documentation |
| Critical Reagents | Antibodies, detection reagents, enzymes essential for assay performance | Early phase: research-grade acceptable; Late phase: requires strict quality control, characterization, and change control |
| Assay Controls | Quality control samples for monitoring assay performance | Qualified controls for early phases; validated controls with established acceptance criteria for late phases |
| Matrix Materials | Biological matrices (plasma, serum, tissue) for assessing specificity | Should mimic study samples; requires characterization of potential interfering substances |
| 2-Isopropoxy-N-(3-isopropoxybenzyl)aniline | 2-Isopropoxy-N-(3-isopropoxybenzyl)aniline, CAS:1040683-86-0, MF:C19H25NO2, MW:299.4 g/mol | Chemical Reagent |
| 3-Methoxy-N-(4-propoxybenzyl)aniline | 3-Methoxy-N-(4-propoxybenzyl)aniline, CAS:1036543-63-1, MF:C17H21NO2, MW:271.35 g/mol | Chemical Reagent |
Method Transfer and Bridging Studies
Analytical Method Transfer Protocols
When moving methods between laboratories, analytical method transfer qualifies a receiving laboratory to use an analytical procedure that originated in another facility [35]. The transfer process involves comparative testing where a predetermined number of samples are analyzed in both receiving and sending units, with acceptance criteria typically based on reproducibility validation criteria [35].
Successful method transfers require thorough documentation including a transfer protocol specifying objectives, responsibilities, experimental design, and acceptance criteria, followed by a comprehensive transfer report documenting results, deviations, and conclusions regarding transfer success [35]. The European Union GMP guideline requires that original validation of test methods be reviewed to ensure compliance with current ICH/VICH requirements, with a gap analysis performed to identify any supplementary validation needed before technical transfer [35].
Analytical Method Bridging Strategies
When new or revised methods with improved robustness, sensitivity, or accuracy are developed to support clinical lot release and stability, replacing existing methods requires a bridging study [32]. These studies establish the numerical relationship between reportable values of each method and determine the impact on product specifications [32].
Based on ICH Q14 guideline on analytical procedure development, the design and extent of bridging studies should be risk-based and consider the product development stage, ongoing studies, and availability of historical batches [32]. At minimum, bridging studies should be anchored to a historical, well-established, and qualified or validated method, typically following new method qualification and/or validation activities [32].
Regulatory Landscape and Compliance Considerations
The regulatory framework for phase-appropriate validation encompasses multiple guidelines from various authorities:
- FDA Guidance: Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy INDs; Potency Tests for Cellular and Gene Therapy Products; Analytical Procedures and Methods Validation for Drugs & Biologics [32]
- EMA Guidance: Requirements for quality documentation concerning biological investigational medicinal products in clinical trials; Guidelines on good manufacturing practice specific for advanced therapies [32]
- ICH Guidelines: ICH Q2(R2) on Validation of Analytical Procedures; ICH Q14 on Analytical Procedure Development [32]
According to U.S. FDA CMC guidance for investigational gene therapies, validation of analytical procedures is generally not required for original IND submissions for Phase 1 studies; however, sponsors must demonstrate that test methods are appropriately controlled using scientifically sound principles [32]. The FDA recommends using compendial methods when appropriate and qualifying safety-related tests before initiating clinical trials [32].
The European Medicines Agency maintains similar though often more stringent requirements, particularly for safety tests, with higher expectations for safety test validation early in clinical development [32]. For other assays, sufficient information on suitability based on intended use in the manufacturing process is expected.
Visualizing the Method Validation Lifecycle
Method Validation Lifecycle Progression
Stages of Fit-for-Purpose Biomarker Assay Validation
The historical development of fit-for-purpose validation principles represents a significant maturation in pharmaceutical analytical sciences, balancing scientific rigor with practical resource management throughout the drug development lifecycle. This phase-appropriate approach enables efficient advancement of promising therapies while progressively building the comprehensive analytical evidence required for regulatory approvals.
The ongoing evolution of validation protocols continues to be shaped by emerging therapeutic modalities, technological advancements, and regulatory experience. The fundamental principle remains constant: analytical methods must be suited to their decision-making purpose at each development stage, with rigor increasing as programs advance toward commercialization. This framework ensures that patient safety and product quality remain paramount while facilitating efficient therapeutic development.
The pharmaceutical industry has witnessed a significant transformation in quality assurance, evolving from traditional quality-by-testing (QbT) approaches to a more systematic Quality by Design (QbD) framework. This paradigm shift represents a fundamental change in how quality is perceived and built into pharmaceutical products and processes. Analytical Quality by Design (AQbD) extends these principles to analytical method development, creating a structured framework that emphasizes proactive quality assurance over reactive testing [36] [37].
The historical context of analytical method validation reveals a progression from fixed, compliance-driven approaches to more flexible, science-based methodologies. Traditional methods often relied on one-factor-at-a-time (OFAT) experimentation and fixed operational conditions, which provided limited understanding of parameter interactions and method robustness [36] [38]. The QbD concept, initially introduced by Juran in the 1980s and later adopted by regulatory agencies including the US FDA and ICH, emphasizes that "quality should be designed into a product, and most quality issues stem from how a product was initially designed" [36] [39]. This philosophical foundation has since been applied to analytical method development through AQbD, which the ICH defines as "a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management" [36].
Theoretical Framework and Historical Evolution of AQbD
Historical Development of Quality Concepts
The conceptual foundation of QbD began as early as 1924 with Shewhart's introduction of quality control through statistical control charts [36]. Juran later laid the groundwork for QbD in 1985, emphasizing that quality must be designed into products during early development stages [36]. The International Council for Harmonisation (ICH) formalized these concepts through quality guidelines (Q8-Q12), providing a standardized approach to pharmaceutical development [36].
The extension of QbD principles to analytical methods began gaining momentum in the 2010s, with regulatory agencies encouraging systematic robustness studies starting with risk assessment and multivariate experiments [36]. This evolution represents a significant departure from traditional method validation approaches, which focused primarily on satisfying regulatory requirements rather than deeply understanding and controlling sources of variability [37].
The Regulatory Landscape and Standardization
Regulatory bodies worldwide have increasingly embraced AQbD principles. The U.S. Food and Drug Administration (FDA) encouraged AQbD implementation in 2015 by advising systematic robustness studies starting with risk assessment and multivariate experiments [36]. The ICH Q14 guideline on Analytical Procedure Development and the ICH Q2(R2) guideline on validation of analytical procedures further formalize the AQbD approach [37].
In 2022, the United States Pharmacopeia (USP) general chapter <1220> entitled "Analytical Procedure Life Cycle" provided a comprehensive framework for ensuring analytical procedure suitability throughout its entire life cycle [36] [40]. This regulatory evolution underscores the importance of integrating systematic tools into contemporary quality endeavors and represents a significant milestone in the history of analytical method validation protocols.
Core Principles of the AQbD Framework
Systematic Approach to Analytical Method Development
The AQbD methodology follows a structured, systematic approach that encompasses the entire analytical procedure lifecycle. This framework consists of five defined stages that ensure method robustness and reliability [36]:
- Stage 1: Analytical Target Profile (ATP) - Defining predefined objectives
- Stage 2: Risk Assessment - Identifying critical method parameters
- Stage 3: Design of Experiments (DoE) - Systematic method optimization
- Stage 4: Method Operable Design Region (MODR) - Establishing controllable ranges
- Stage 5: Control Strategy - Implementing ongoing monitoring
This systematic approach contrasts sharply with traditional method development, which often followed a trial-and-error process without comprehensive understanding of parameter interactions [38].
Comparative Analysis: Traditional vs. AQbD Approach
Table 1: Comparison between Traditional and AQbD Approach to Analytical Method Development
| Aspect | Traditional Approach | AQbD Approach |
|---|---|---|
| Philosophy | Quality by testing (QbT) | Quality by design |
| Method Development | Trial-and-error or OFAT | Systematic, based on DoE |
| Primary Focus | Compliance with regulatory requirements | Scientific understanding and risk management |
| Parameter Interactions | Often unknown | Systematically evaluated |
| Robustness | Limited understanding | Comprehensively demonstrated |
| Regulatory Flexibility | Limited; fixed method conditions | Enhanced within MODR |
| Lifecycle Management | Reactive changes | Continuous improvement |
Key Terminology and Definitions
Table 2: Essential AQbD Terminology and Definitions
| Term | Definition | Significance |
|---|---|---|
| Analytical Target Profile (ATP) | A prospective description of the desired performance of an analytical procedure | Defines the required quality of reportable values [40] |
| Critical Quality Attributes (CQAs) | Physical, chemical, biological properties within appropriate limits for desired product quality | Ensures method meets intended purpose [38] |
| Method Operable Design Region (MODR) | Multidimensional combination of analytical factors where method performance meets ATP criteria | Provides regulatory flexibility [40] |
| Critical Method Parameters (CMPs) | Input variables that affect method CQAs | Focus of method optimization [38] |
| Design of Experiments (DoE) | Structured approach for understanding parameter effects and interactions | Enables efficient method optimization [36] |
Implementation of AQbD: A Step-by-Step Methodology
Defining the Analytical Target Profile (ATP)
The foundation of AQbD implementation begins with establishing a clear Analytical Target Profile. The ATP serves as a prospective description of the desired analytical procedure performance, defining the quality requirements for reportable values [40]. The ATP should clearly specify:
- The target analyte(s) and required selectivity
- Appropriate measurement techniques (HPLC, UPLC, GC, etc.)
- Required validation parameters (precision, accuracy, specificity)
- The intended purpose and context of use
For medicinal plant analysis, where multiple components must be analyzed in complex biological materials, the ATP becomes particularly crucial as it must address the challenges of analyzing multiple phytochemicals with varying chemical properties [40].
Risk Assessment and Identification of CQAs
Risk assessment represents the second critical phase in AQbD implementation. This systematic process identifies and evaluates potential risks to method performance using various tools:
- Ishikawa (fishbone) diagrams for categorizing risk factors
- Failure Mode and Effects Analysis (FMEA) for risk prioritization
- Risk Estimation Matrix (REM) for visualizing risk levels
These tools help categorize risk factors into high-risk, noise, and experimental categories, enabling focused optimization efforts on the most critical parameters [38]. The risk assessment evaluates analyst approach, instrument setup, assessment variables, material features, preparations, and ambient circumstances to comprehensively understand potential sources of variability [38].
Design of Experiments (DoE) and Method Optimization
DoE represents a fundamental component of AQbD, replacing the traditional OFAT approach. DoE employs statistical principles to efficiently understand the relationship between Critical Method Parameters and Critical Quality Attributes [36]. The experimental process typically involves:
- Screening designs to identify significant factors
- Response surface methodology to model relationships
- Multivariate analysis to optimize multiple responses simultaneously
Common experimental designs include Box-Behnken, Central Composite, and Full Factorial designs, selected based on the specific optimization needs [38]. The DoE approach enables researchers to develop mathematical models that describe the relationship between input factors and output responses, facilitating the identification of optimal method conditions.
Establishing the Method Operable Design Region (MODR)
The MODR represents the multidimensional combination and interaction of input variables that have been demonstrated to provide assurance of quality [40]. Unlike traditional methods with fixed operating conditions, the MODR provides a operational flexibility where method parameters can be adjusted without requiring revalidation, as long as they remain within the defined region [41].
The MODR is typically represented through overlay contour plots that visually display the region where all CQA requirements are simultaneously met [38]. This graphical representation enables analysts to understand the boundaries of operational flexibility and make science-based decisions about method adjustments.
Control Strategy and Lifecycle Management
The final implementation stage involves developing a control strategy to ensure the method remains in a state of control throughout its lifecycle. This strategy includes:
- System suitability tests to verify method performance
- Control charts for ongoing performance monitoring
- Procedures for managing changes within the MODR
The control strategy is not a one-time activity but evolves throughout the method lifecycle based on accumulated knowledge and data [38]. The Analytical Procedure Lifecycle approach, as described in USP <1220>, emphasizes continuous monitoring and improvement, ensuring the method remains fit-for-purpose throughout its operational life [37].
Experimental Protocols and Applications
Chromatographic Method Development Using AQbD
Chromatographic techniques, particularly reversed-phase liquid chromatography, have extensively applied AQbD principles. The development process typically involves identifying CMAs such as peak retention, resolution, and tailing factor, which are critically influenced by CMPs including mobile phase composition, pH, column temperature, and gradient profile [36].
A representative experimental protocol for HPLC method development includes:
- ATP Definition: Specify required resolution, precision, and robustness
- Risk Assessment: Identify factors affecting separation quality
- DoE Implementation:
- Screening design to identify critical factors
- Response surface design to optimize conditions
- MODR Establishment: Define acceptable ranges for acetonitrile concentration, pH, and temperature
- Validation: Verify method performance across the MODR
This systematic approach has demonstrated significant advantages in pharmaceutical analysis, where robustness and reliability are paramount [36].
AQbD in Complex Matrices: Medicinal Plant Analysis
The application of AQbD to medicinal plant analysis presents unique challenges due to the complexity of chemical and biological properties in plant materials [40]. Unlike single compound analysis, medicinal plant analysis involves multiple components with varying chemical properties, requiring specialized approaches:
- Definition of multiple analytical targets for phytochemical markers
- Consideration of plant raw material diversity
- Development of control strategies addressing complex sample matrices
Despite these challenges, AQbD offers significant advantages for natural product analysis by providing systematic approaches to manage complexity and ensure reliable results [40].
Industrial Case Study: QbD in Drug Product Development
An industrial case study demonstrating QbD implementation for a generic two-API oral solid dosage form illustrates the practical application of these principles [39]. The development process involved:
- QTPP Definition: Summary of desirable quality characteristics
- CQA Identification: Using criticality assessment based on risk to patient
- Process Design: Selection of manufacturing process based on product knowledge
- Control Strategy: Implementation of monitoring and control measures
This case study demonstrated that systematic QbD application could expedite time to market, assure process assertiveness, and reduce risk of defects after product launch [39].
Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for AQbD Implementation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Chromatographic Columns | Stationary phase for separation | Critical reagent; batch-to-batch variability must be assessed [41] |
| Reference Standards | Method calibration and qualification | Purity and stability directly impact method accuracy [42] |
| Mobile Phase Components | Liquid phase for chromatographic separation | Quality and consistency essential for reproducible retention [36] |
| Sample Preparation Reagents | Extraction, purification, derivation | Impact method selectivity and sensitivity [40] |
| System Suitability Standards | Verify chromatographic system performance | Critical for ensuring method validity [37] |
AQbD Workflow Visualization
Benefits and Regulatory Implications
Advantages of AQbD Implementation
The systematic implementation of AQbD offers numerous advantages over traditional approaches:
- Enhanced Method Robustness: By systematically evaluating parameter effects and interactions, AQbD develops methods that withstand normal operational variations [38]
- Reduced OOS/OOT Results: The comprehensive understanding of method operation within the MODR minimizes unexpected failures [38]
- Regulatory Flexibility: Changes within the established MODR do not require regulatory submission, facilitating continuous improvement [41]
- Knowledge Management: AQbD generates comprehensive scientific understanding that supports method lifecycle management [36]
Regulatory Flexibility and Established Conditions
A significant advantage of AQbD is the regulatory flexibility it affords. The concept of Established Conditions recognizes that changes within the MODR do not constitute regulatory changes, reducing the burden of post-approval submissions [41]. This approach aligns with the ICH Q12 guideline on technical and regulatory considerations for pharmaceutical product lifecycle management [41].
The regulatory flexibility is particularly valuable in analytical method transfer and method updates, where adjustments within the MODR can be implemented without extensive regulatory documentation, provided they are supported by the development data [41].
Analytical Quality by Design represents a fundamental shift in how analytical methods are developed, validated, and managed throughout their lifecycle. By incorporating systematic, science-based approaches with quality risk management, AQbD moves beyond traditional compliance-driven methodologies to build quality directly into analytical procedures [36] [37].
The historical evolution of analytical method validation protocols reveals a clear trajectory toward more flexible, knowledge-based approaches that prioritize scientific understanding over rigid compliance. The adoption of AQbD principles continues to grow, with regulatory agencies increasingly recognizing its value in ensuring robust, reliable analytical methods [37].
Future developments in AQbD will likely focus on digitalization and the application of advanced data analytics to further enhance method understanding and control [41]. As the pharmaceutical industry embraces Pharma 4.0 concepts, the integration of AQbD with digital workflows will enable more efficient method development and enhanced lifecycle management [37]. The continued harmonization of regulatory expectations through ICH Q14 and Q2(R2) will further solidify AQbD as the standard approach for analytical method development in the pharmaceutical industry [37].
The landscape of analytical method validation has undergone a significant paradigm shift, moving from a prescriptive, checklist-based approach to a systematic, lifecycle-oriented model centered on the Analytical Target Profile (ATP). This technical guide explores the ATP as a foundational element in modern analytical science, framing it within the historical evolution of validation protocols. The ATP prospectively defines the criteria for a successful analytical method, ensuring it remains fit-for-purpose throughout its lifecycle. We detail the core components of an ATP, provide methodologies for its development and implementation, and visualize the integrated workflow connecting product development to analytical control. This whitepaper serves as a comprehensive resource for researchers and drug development professionals navigating the harmonized framework of ICH Q14 and Q2(R2).
The history of analytical method validation reveals a continual striving for greater scientific rigor, consistency, and regulatory harmonization. For decades, validation was often treated as a one-time event conducted at the end of method development, focused on verifying a fixed set of performance characteristics against pre-defined acceptance criteria [43]. This "check-the-box" approach, while structured, lacked the flexibility and scientific depth required for modern pharmaceutical development, particularly with the increasing complexity of biologics and advanced therapies [44].
The turn of the century saw a pivotal change with the introduction of Quality by Design (QbD) principles for pharmaceutical development through ICH Q8(R2). QbD emphasized building quality into the product from the beginning, using a science and risk-based approach. This created a logical need for an analogous concept for analytical procedures [45]. This need was fulfilled with the formal introduction of the Analytical Target Profile (ATP) in the ICH Q14 guideline [46]. The ATP represents a maturation of analytical science, shifting the focus from merely validating a method's performance at a single point in time to designing and controlling a method to be fit-for-purpose over its entire lifecycle [47].
The Analytical Target Profile: A Foundational Concept
Definition and Core Principles
The Analytical Target Profile (ATP) is a prospective summary of the quality characteristics of an analytical procedure [46]. It defines what the method needs to achieve—the "success criteria"—rather than prescribing how to achieve it. In essence, the ATP outlines the required quality of the reportable result to ensure it is suitable for its intended purpose in making correct quality decisions [45].
The ATP is directly analogous to the Quality Target Product Profile (QTPP) defined in ICH Q8 for drug products. Where the QTPP summarizes the quality characteristics of the drug product, the ATP summarizes the requirements for the measurement of those characteristics [46]. The core principle is that the ATP drives the entire analytical procedure lifecycle, from development and validation to routine use and post-approval changes [45].
Key Components of an ATP
A well-constructed ATP is a comprehensive document that links the analytical procedure to the product's Critical Quality Attributes (CQAs). The table below outlines the essential components of a typical ATP.
Table 1: Core Components of an Analytical Target Profile (ATP)
| ATP Component | Description | Example |
|---|---|---|
| Intended Purpose | A clear description of what the analytical procedure is meant to measure. | "Quantitation of the active ingredient in a drug product tablet." |
| Technology Selection | The chosen analytical technique with a rationale for its selection. | "Reversed-Phase HPLC with UV detection, selected for its robustness, resolving power, and compatibility with the analyte." |
| Link to CQAs | A summary of how the method provides reliable results for a specific CQA. | "The method must reliably quantify impurity levels to ensure product safety." |
| Performance Characteristics & Acceptance Criteria | The specific performance parameters and their required limits to ensure the reportable result is fit-for-purpose. | Accuracy, Precision, Specificity, Range (see Table 2 for details). |
| Reportable Range | The interval between the upper and lower concentrations (including appropriate accuracy and precision) of the analyte. | "From the reporting threshold of 0.05% to 120% of the specification limit." |
Regulatory Context: ICH Q14 and Q2(R2)
The ATP is a central pillar in the modernized regulatory framework established by ICH Q14: Analytical Procedure Development and the revised ICH Q2(R2): Validation of Analytical Procedures [47]. These complementary guidelines promote a more flexible, scientific approach.
- ICH Q14 provides a structured framework for development, introducing the concept of the ATP and outlining two approaches: a traditional (minimal) approach and a more systematic enhanced approach that leverages prior knowledge, risk assessment, and multivariate experiments [46].
- ICH Q2(R2) modernizes validation principles, expanding their application to newer analytical technologies and reinforcing the link between validation and the intended purpose of the method, as defined in the ATP [10] [44].
Together, these guidelines facilitate a lifecycle management model for analytical procedures, where the ATP serves as the fixed target against which any changes to the method are evaluated for their impact on performance [46] [47].
Implementing the ATP: From Theory to Practice
The ATP-Driven Method Lifecycle Workflow
The following diagram illustrates the integrated, ATP-driven workflow for analytical method lifecycle management, highlighting its connection to product development.
Diagram 1: ATP-Driven Analytical Method Lifecycle
Developing an ATP: A Step-by-Step Methodology
The creation of an ATP is a systematic process. The following steps provide a protocol for development teams.
- Define the Intended Purpose: Clearly state the goal of the measurement. This includes identifying the analyte (e.g., active ingredient, specific impurity) and the context of its use (e.g., release testing, stability monitoring) [46] [48]. The intended purpose is the cornerstone of the ATP.
- Identify the Link to CQAs: Formally document the specific CQA the method will measure and how a reliable measurement is critical to ensuring the product's safety, efficacy, or quality [46]. For example, a potency method is directly linked to the efficacy CQA.
- Establish the Reportable Range: Define the required range of concentrations over which the method must perform. This is driven by the specification limits for the attribute and the need to detect and quantify levels seen during stability and manufacturing [46].
- Define Performance Characteristics and Acceptance Criteria: This is the core of the ATP. For each relevant performance characteristic, set justified acceptance criteria based on the intended purpose and patient risk [45]. The criteria define the maximum allowable uncertainty in the reportable result.
Table 2: Defining Performance Characteristics in the ATP
| Performance Characteristic | Experimental Protocol for Validation [48] | Typical Acceptance Criteria Justification |
|---|---|---|
| Accuracy | Analyze a sample of known concentration (e.g., a reference standard or a placebo spiked with a known amount of analyte). Calculate the percentage recovery of the analyte. | Based on product requirements; e.g., 98-102% recovery for a drug substance assay [46]. |
| Precision | Repeatability: Inject multiple preparations of a homogeneous sample under the same conditions. Intermediate Precision: Have different analysts on different days using different instruments perform the analysis. Express as %RSD. | The required precision is based on the consequence of an incorrect decision; e.g., %RSD ≤ 2.0% for a potency assay to ensure correct dosage [44]. |
| Specificity | Demonstrate that the signal is due to the analyte alone. Inject blank matrices, placebo, and stressed samples (e.g., forced degradation) to show no interference at the retention time of the analyte. | The analyte peak should be pure and baseline-resolved from all other potential peaks (e.g., degradants, excipients) [48]. |
| Linearity & Range | Prepare and analyze a minimum of 5 concentrations spanning the defined range. Plot instrument response vs. concentration and evaluate using correlation coefficient (R²) and y-intercept. | A high degree of linearity (e.g., R² ≥ 0.999) is typically required for quantitative assays to ensure accuracy across the range [48]. |
The Scientist's Toolkit: Essential Reagents and Materials
The practical execution of an ATP-driven method development and validation relies on a set of core materials.
Table 3: Essential Research Reagent Solutions for Method Development & Validation
| Item | Function |
|---|---|
| Well-Characterized Reference Standard | Serves as the benchmark for quantifying the analyte and establishing accuracy. Its purity and identity must be unequivocally established. |
| Placebo/Blank Matrix | Used in specificity and accuracy experiments to demonstrate that the sample matrix does not interfere with the measurement of the analyte. |
| Forced Degradation Samples | Samples of the drug substance or product stressed under various conditions (e.g., heat, light, acid, base, oxidation). Critical for demonstrating specificity and the stability-indicating nature of a method. |
| System Suitability Standards | A reference preparation used to verify that the chromatographic or analytical system is performing adequately at the time of the test. Key parameters include resolution, tailing factor, and precision [44]. |
| High-Purity Solvents and Reagents | Essential for achieving robust and reproducible results, minimizing background noise, and ensuring the integrity of the analytical procedure. |
| 3-(Azepan-2-yl)-5-(thiophen-2-yl)isoxazole | 3-(Azepan-2-yl)-5-(thiophen-2-yl)isoxazole | Research Compound |
| Benzenamine, 2-[(hexyloxy)methyl]- | Benzenamine, 2-[(hexyloxy)methyl]-|CAS 80171-95-5 |
The Analytical Target Profile is more than a regulatory expectation; it is the cornerstone of a modern, scientific, and robust approach to analytical method design and lifecycle management. By prospectively defining the criteria for success, the ATP ensures that analytical methods are developed to be fit-for-purpose, generating reliable data that underpins critical quality decisions throughout a product's lifecycle. The adoption of the ATP, as guided by ICH Q14 and Q2(R2), empowers scientists to build quality and flexibility into their methods from the outset. This represents the culmination of decades of evolution in validation protocols, moving the pharmaceutical industry toward a more efficient, knowledge-driven, and patient-focused paradigm.
In the history of analytical method validation, the concept of robustness represents a critical evolution from simply proving a method works under ideal conditions to ensuring it remains reliable amidst the inevitable variations of real-world laboratories. Robustness, defined as a measure of a method's capacity to remain unaffected by small, deliberate variations in procedural parameters, is a cornerstone of reliable analytical science [2] [49]. Within the framework of Quality by Design (QbD), robustness is not an afterthought but an attribute built into methods from their inception [50] [51]. This systematic approach marks a significant departure from the traditional "One Factor At a Time" (OFAT) paradigm, which was inefficient and failed to capture interactions between variables [50] [52].
Design of Experiments (DoE) has emerged as the premier statistical tool for implementing this robust design efficiently. By investigating multiple factors simultaneously, DoE allows scientists to build a predictive model of the method's behavior, quantifying the effect of each parameter and its interactions with others [53] [50]. This guide provides an in-depth technical framework for utilizing DoE to embed robustness directly into analytical methods, ensuring they stand up to the rigors of routine use in research and regulated environments.
DoE in the Context of Method Validation
The Shift from OFAT to a Systematic DoE Approach
The pharmaceutical industry was a relative latecomer to adopting DoE, having long relied on OFAT studies for formulation development [51] [52]. The OFAT approach, which involves holding all variables constant except one, suffers from two fundamental flaws: extreme experimental inefficiency and a failure to capture interactions between critical process parameters (CPPs) or critical method variables [50]. In contrast, a DoE-based approach provides a structured and efficient framework for understanding a method holistically. It enables the development of a design space—a multidimensional combination of input variables demonstrated to provide assurance of quality [50]. Operating within this space offers operational flexibility, while moving outside of it is considered a change that requires regulatory notification [50].
The DoE Process: A Campaign for Knowledge
Implementing DoE is not a single experiment but a strategic campaign for knowledge acquisition. This process is typically broken into flexible, iterative stages [53]:
- Screening: The initial stage aims to differentiate the few vital factors from the trivial many. It uses the maximum and minimum ranges for each potential factor to quickly identify which have a significant effect on the method's output [53].
- Iteration and Refinement: This stage involves continuing to investigate which factors are important and within which ranges, honing in on the experimental region of interest [53].
- Optimization: This stage creates a high-quality predictive model to infer optimal conditions for the system. It requires a specific type of DoE design that investigates the vital factors in greater detail [53].
- Assessing Robustness: The final stage involves running experiments around your optimal conditions to determine the extent to which the system is sensitive to small changes in factor levels [53].
Designing a Robustness Study Using DoE
Pre-Experimental Planning: Defining the System
A successful robustness study begins with careful planning. Before any experiments are conducted, the following must be defined [53] [50]:
- Goal: The goal is not simply to "test robustness," but to ensure the method's key outputs (Critical Quality Attributes or CQAs) remain within acceptable limits when inputs are varied.
- Factors and Ranges: Identify the method parameters to be investigated (e.g., pH, temperature, flow rate, % organic solvent) and define realistic, slightly exaggerated "worst-case" ranges for each based on prior knowledge from the screening and optimization stages.
- Responses: Select the measurable CQAs that define method performance, such as assay results, impurity levels, resolution between critical pairs, and tailing factor.
Table 1: Example Factors and Ranges for an HPLC Robustness Study
| Factor | Low Level (-1) | High Level (+1) | Units |
|---|---|---|---|
| pH of Mobile Phase | 2.8 | 3.2 | pH |
| Column Temperature | 25 | 35 | °C |
| Flow Rate | 0.9 | 1.1 | mL/min |
| % Acetonitrile | 45 | 55 | % (v/v) |
Experimental Designs for Robustness Testing
For robustness studies, where the goal is to model local variability around a set point, specific DoE designs are most appropriate. These designs are highly efficient for estimating main effects and low-order interactions.
- Full Factorial Designs: A two-level full factorial design investigates all possible combinations of the factor levels. While it provides comprehensive data on all main effects and interactions, the number of runs grows exponentially with the number of factors (2^k for k factors). This is often the design of choice when the number of factors is small (e.g., 3-4) [51].
- Fractional Factorial Designs: When the number of factors is larger (e.g., 5 or more), a fractional factorial design is a practical alternative. It sacrifices the ability to estimate some higher-order interactions (which are often negligible) to significantly reduce the number of required experimental runs [51] [52].
- Plackett-Burman Designs: These are a specific type of highly fractional factorial design used primarily for screening a large number of factors when only the main effects are of interest. They are extremely efficient but assume interactions are negligible [51].
The workflow for designing and executing a robustness study is a systematic process, visualized below.
Diagram: Robustness Study Workflow
Data Analysis and Interpretation
Building and Interpreting the Model
Once the experimental data is collected, statistical analysis is used to build a mathematical model (often a multiple linear regression model) that describes the relationship between the varied factors and each response. The key outputs of this analysis include:
- Analysis of Variance (ANOVA): This statistical test determines which factors have a statistically significant effect on each response. A p-value (e.g., < 0.05) indicates a significant effect [54] [52].
- Regression Coefficients: These coefficients quantify the effect of each factor. A positive coefficient means the response increases as the factor moves from its low to high level, and vice versa.
- Response Surface Plots: These 3D or contour plots provide a visual representation of the model, showing how two factors and their interaction affect a response [54].
Table 2: Example Data Analysis from a Robustness Study on an Assay Method
| Factor | Effect on Assay Result | p-value | Statistically Significant? |
|---|---|---|---|
| pH | -0.15 | 0.45 | No |
| Temperature | 0.08 | 0.65 | No |
| Flow Rate | -1.25 | 0.01 | Yes |
| % Organic | 0.95 | 0.03 | Yes |
| pH * % Organic | -0.45 | 0.08 | No |
Defining the Robustness Window and Design Space
The ultimate goal of the analysis is to define the robustness window—the region within the tested ranges where the method consistently meets all acceptance criteria for its CQAs [53] [50]. This involves ensuring that for all responses (e.g., assay, purity, resolution), the predicted values across the operating ranges are within their predefined limits. This robustness window often forms a key part of the larger design space for the method [50]. The relationship between the broader knowledge space, the design space, and the final robust set point is a key outcome.
Diagram: From Knowledge Space to Robust Set Point
Advanced DoE Techniques and Regulatory Considerations
Advanced Optimality Criteria
For complex methods, advanced DoE criteria can enhance the robustness study. G-optimality is a powerful criterion that focuses on minimizing the maximum prediction variance across the entire design space [54]. A design with high G-efficiency ensures that no location within the experimental region has disproportionately high uncertainty about the predicted outcome, which is a key characteristic of a robust method. Algorithmic strategies for finding G-optimal designs include coordinate exchange algorithms, genetic algorithms, and particle swarm optimization [54].
Meeting Regulatory Expectations
Regulatory agencies strongly advocate for science-based and risk-based approaches, including the application of QbD principles to analytical methods [50] [49]. A well-executed DoE for robustness provides the documented evidence required for regulatory compliance.
- Quality by Design (QbD): DoE is the backbone for efficient implementation of QbD, building quality into the process or method from the beginning [50] [51].
- ICH Guidelines: ICH Q2(R1) provides guidance on validation methodology, and the principles of robustness align with this framework [2] [49]. Demonstrating robustness through DoE provides a higher level of assurance than traditional univariate approaches.
- Design Space and PARs: The output of a DoE study can be used to define the design space and Proven Acceptable Ranges (PARs) for method parameters, which may be included in regulatory submissions [50].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The execution of a robustness study requires careful preparation of specific materials to ensure accurate and reproducible results.
Table 3: Key Research Reagent Solutions for Robustness Studies
| Reagent/Solution | Function in the Study |
|---|---|
| System Suitability Standard | A standardized mixture used to verify the chromatographic system's performance is adequate before and during the robustness runs [49]. |
| Placebo Mixture | A mock sample containing all excipients/inactive components without the active analyte. Used to demonstrate specificity and absence of interference [49]. |
| Accuracy/Recovery Spikes | Samples spiked with known quantities of the analyte (and impurities, if available) into the placebo. Used to confirm the method's accuracy across the variable conditions [2] [49]. |
| Forced Degradation Sample | A stressed sample (e.g., via heat, light, acid/base) that generates degradation products. Used in specificity testing to ensure the method can separate the analyte from its degradants under all conditions [49]. |
| Retention Time Marker Solution | A solution containing the analyte and available impurities. Aids in peak tracking and identification despite retention time shifts caused by varying method parameters [49]. |
| 4-Fluoro-2-methyl-1H-indol-5-amine | 4-Fluoro-2-methyl-1H-indol-5-amine|CAS 398487-76-8 |
| Diethyl 2-(1-nitroethyl)succinate | Diethyl 2-(1-nitroethyl)succinate, CAS:4753-29-1, MF:C10H17NO6, MW:247.24 g/mol |
Utilizing Design of Experiments to demonstrate and optimize robustness represents a paradigm shift in analytical method validation. It moves the practice from a reactive, compliance-driven exercise to a proactive, knowledge-building endeavor. By systematically exploring the multidimensional parameter space, scientists can move beyond simply proving a method works at a single point, and instead define a robust region in which it is guaranteed to perform. This not only provides greater confidence in the reliability of analytical data but also offers operational flexibility and facilitates faster regulatory approval by building quality directly into the analytical procedure [50]. In an industry where the integrity of data is paramount, a DoE-led approach to robustness is not just an advanced technique—it is an essential component of modern, robust analytical science.
The history of analytical method validation in the biopharmaceutical industry reflects a continuous pursuit of efficiency, compliance, and scientific rigor. As biological products have grown more complex and manufacturing has become globalized, traditional approaches to method validation and transfer have undergone significant transformation. The industry has evolved from sequential, site-specific validation processes toward more integrated, parallelized strategies that can keep pace with accelerated development timelines, particularly for breakthrough therapies.
This evolution has been driven by several key industry trends: the rise of multi-product biologics facilities, increasing molecular diversity, stringent regulatory expectations, and the pressing need to expedite market entry for innovative treatments [55]. In response, two powerful strategies have emerged as cornerstones of modern analytical quality systems: platform validation and covalidation. These approaches represent a paradigm shift from repetitive, standalone validations to streamlined, risk-based models that maintain scientific rigor while significantly reducing time and resource investments across multiple sites.
Understanding Platform Validation Strategies
The Concept of Platform Validation
Platform validation, also referred to as generic validation, is a strategic approach where analytical methods are developed and validated for application across multiple similar biological products rather than for a single specific product [56]. This methodology is particularly powerful for manufacturers of monoclonal antibodies (MAbs) and other biologics with shared characteristics, as it leverages common analytical techniques across product portfolios.
The fundamental principle underlying platform validation is that once a method has been rigorously validated using selected representative materials, subsequent applications to similar products require only simplified verification rather than full revalidation [56]. This fit-for-purpose approach aligns with quality by design (QbD) principles, where method development goals and acceptance criteria are defined through an analytical target profile established early in development.
Implementation Framework
Successful implementation of platform validation requires systematic planning and execution. The process begins with careful selection of representative materials that adequately demonstrate method performance across anticipated product variations. For monoclonal antibody platforms, this typically involves choosing products with diverse structural characteristics and manufacturing process variations to challenge the method adequately.
The validation package generated then serves as a master validation for all future similar products. When a new product is introduced, manufacturers perform a targeted assessment to demonstrate the method's applicability to that specific product, rather than conducting a full validation [56]. This assessment typically focuses on product-specific attributes that may differ from the original validation materials.
Table 1: Platform Validation Application Examples for Monoclonal Antibodies
| Analytical Technique | Application | Platform Validation Approach | Subsequent Product Verification |
|---|---|---|---|
| Size-exclusion chromatography (SEC) | Aggregate and fragment quantification | Full validation with multiple stressed and unstressed MAb samples | Dilutional linearity and specificity with new product |
| Host cell protein assays | Process impurity testing | Validation with multiple representative processes | Comparison to platform standards and controls |
| Cell-based bioassays | Potency determination | Validation across multiple MAb modalities with different mechanisms | Parallelism assessment and relative potency demonstration |
| Peptide mapping | Identity and sequence confirmation | Validation with structural analogues | Comparison to expected map and pre-defined acceptance criteria |
Benefits and Challenges
The primary benefit of platform validation is substantial efficiency gain. By eliminating redundant validation activities for each new product, companies can accelerate investigational new drug (IND) submissions and reduce resource requirements during early product development [56]. This approach also promotes method standardization across product lines, facilitating easier technology transfers and more consistent data interpretation.
However, platform validation presents distinct challenges. The initial validation requires more comprehensive planning and execution to ensure the method is truly applicable across multiple products. There is also a risk of over-extending platform applicability to products with significant differences that require method modification. Successful implementation requires deep understanding of product similarities and critical method parameters to establish appropriate boundaries for platform application.
Covalidation: A Parallelized Approach to Multi-Site Qualification
Defining Covalidation
Covalidation represents a fundamental shift in the method transfer paradigm. The United States Pharmacopeia (USP) defines covalidation as an approach where "the transferring unit can involve the receiving unit in an interlaboratory covalidation, including them as a part of the validation team, and thereby obtaining data for the assessment of reproducibility" [57]. Unlike traditional sequential approaches where method validation precedes transfer, covalidation enables simultaneous method validation and receiving site qualification.
In this model, receiving laboratories participate as active members of the validation team rather than as passive recipients of fully validated methods [57]. This collaborative approach transforms method transfer from a verification exercise into an integrated knowledge-sharing opportunity, building receiving laboratory ownership and expertise from the outset.
Comparative Analysis of Transfer Approaches
Table 2: Analytical Method Transfer Approaches Comparison
| Transfer Approach | Definition | Best Suited For | Key Considerations |
|---|---|---|---|
| Covalidation | Simultaneous method validation and receiving site qualification | Accelerated timelines; breakthrough therapies; experienced receiving labs | Requires method robustness data; early receiving lab engagement |
| Comparative Testing | Both labs analyze same samples; results statistically compared | Established, validated methods; similar lab capabilities | Statistical analysis; sample homogeneity; detailed protocol [58] |
| Revalidation | Receiving lab performs full/partial revalidation | Significant differences in lab conditions/equipment; substantial method changes | Most rigorous, resource-intensive; full validation protocol needed [58] |
| Transfer Waiver | Transfer process formally waived based on justification | Highly experienced receiving lab; identical conditions; simple methods | Rare, high regulatory scrutiny; requires strong scientific justification [58] |
Covalidation Workflow and Implementation
The covalidation process requires meticulous planning and execution. The following diagram illustrates the key stages in a successful covalidation workflow:
The decision to employ covalidation should be guided by a risk-based assessment. Key decision points include satisfactory method robustness results from the transferring laboratory, receiving laboratory familiarity with the technique, absence of significant instrument or critical material differences between laboratories, and for commercial manufacturing sites, a timeline of less than 12 months between method validation and commercial manufacture [57].
Quantitative Benefits Demonstrated
A compelling case study from Bristol-Myers Squibb (BMS) demonstrates the significant efficiency gains achievable through covalidation. In a project involving the transfer of 50 release testing methods, covalidation reduced the time from method validation initiation to receiving site qualification from approximately 11 weeks to 8 weeks per method—a reduction of over 20% [57].
The resource utilization data further underscores the efficiency of this approach. The traditional comparative testing model required 13,330 total hours, while the covalidation model required only 10,760 hours—saving 2,570 hours while achieving the same qualification outcome [57]. These time savings are particularly valuable for breakthrough therapies with accelerated development pathways.
Integrated Implementation: Combining Platform and Covalidation Strategies
Strategic Integration Framework
The combination of platform and covalidation strategies creates a powerful synergy for multi-site biologics manufacturing. Platform validation establishes standardized, well-understood methods across product classes, while covalidation enables efficient multi-site qualification of these methods. This integrated approach is particularly valuable for global manufacturing networks and contract development and manufacturing organizations (CDMOs) that need to maintain consistency across facilities.
The integrated implementation begins with platform method development and validation, followed by strategic deployment to multiple sites using covalidation. This model enables "qualification by design," where future transfers are anticipated and facilitated through upfront planning and standardization.
Experimental Protocols and Methodologies
Platform Method Robustness Evaluation
Robustness testing is critical for both platform validation and covalidation success. A systematic approach to robustness evaluation during method development ensures adequate understanding and confidence in the method [57]. For HPLC method development, this typically involves examining multiple variants in a model-robust design, including:
- Binary organic modifier ratios
- Gradient slope variations
- Column temperature ranges
- pH variations of mobile phase
- Flow rate variations
Based on the identification of critical method parameters, method robustness ranges and performance-driven acceptance criteria are established. This comprehensive understanding enables confident application of the method across multiple products and sites.
Covalidation Experimental Protocol
A robust covalidation protocol should include several key elements. The receiving laboratory typically performs reproducibility testing as part of the interlaboratory validation [57]. The specific studies assigned to the receiving laboratory may include:
- Intermediate precision assessment
- Selectivity/specificity verification
- Quantitation limit/detection limit verification
- Robustness confirmation under local conditions
All data from both transferring and receiving laboratories are combined in a single validation package, demonstrating method suitability across sites. This comprehensive approach satisfies both validation and transfer requirements simultaneously.
Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Validation | Critical Considerations |
|---|---|---|
| Representative Biologic Samples | Platform validation foundation | Should cover product and process variability |
| Stressed/Degraded Samples | Specificity demonstration | Forced degradation under controlled conditions |
| Reference Standards | System suitability and calibration | Qualified, traceable, with documented stability |
| Critical Reagents | Method performance (e.g., antibodies, enzymes) | Rigorous qualification and stability testing |
| Spiking Materials | Accuracy/recovery studies (e.g., aggregates) | Representative of actual impurities; properly characterized |
Case Studies and Industry Applications
Biologics Manufacturer Implementation
Samsung Biologics has implemented a standardized validation framework across its growing manufacturing network to address challenges in maintaining validation consistency across multiple plants [55]. By establishing a common validation framework for its new Bio Campus II facilities, the company has enhanced consistency, streamlined validation execution, and ensured seamless product transfer between plants. This approach includes key elements such as paperless validation, comprehensive integration, and the implementation of a multiplant qualification strategy.
Multisite Multi-Analyzer Validation
LifeLabs Medical Laboratory Services provides another relevant case study in managing complex multi-site validations. The organization successfully validated three automated platforms across five sites, including 23 analyzers covering 45 assays from a single chemistry platform, and 28 analyzers covering 27 assays across two immunoassay platforms [59]. Their success factors included:
- A single comprehensive validation protocol for each platform
- Designated project managers with multi-site operational insights
- Staggered validation approach to optimize resources
- Automated data management systems to handle thousands of data points
- Visual validation progress tracking with color-coded status indicators
Risk Mitigation in Covalidation
A key lesson from industry implementation is the importance of robust risk mitigation strategies for covalidation. The primary risks include method unreadiness, knowledge retention challenges during extended gaps between validation and routine use, and receiving laboratory timeline constraints [57]. These risks can be mitigated through:
- Comprehensive method robustness assessment prior to covalidation
- Structured knowledge transfer and documentation
- Clear governance and communication protocols
- Early receiving laboratory engagement in method understanding
Regulatory Considerations and Compliance
Evolving Regulatory Landscape
Regulatory perspectives on method transfer continue to evolve. While definitive regulatory guidelines specifically for analytical method transfer are limited compared to method validation, several guidance documents provide frameworks for transfer activities [60]. Health Canada's Post-Notice of Compliance (NOC) Changes: Quality Document provides detailed information about types of changes, risk-based assessment approaches, and filing requirements [60].
The FDA has emphasized the importance of risk-based approaches that encourage manufacturers to take appropriate actions around validation activities based on risk [61]. Regulatory agencies generally expect transfer acceptance criteria to be supported by appropriate statistical analyses rather than relying solely on specification ranges [60].
Documentation Strategies
Streamlined documentation is a significant advantage of covalidation. Unlike comparative testing that requires separate transfer protocols and reports, covalidation incorporates procedures, materials, acceptance criteria, and results in validation protocols and reports, eliminating redundant documentation [57]. This integrated approach reduces administrative burden while maintaining regulatory compliance.
For platform validations, documentation should clearly establish the scientific rationale for platform applicability and the basis for subsequent product-specific verifications. This includes comprehensive development reports, robustness studies, and clearly defined boundaries for platform application.
Emerging Trends
The future of platform and covalidation strategies is closely tied to technological advancements in the biopharmaceutical industry. Several emerging trends are likely to shape future implementations:
- Increased Automation: The adoption of paperless validation solutions and digital workflows enhances consistency, reduces human error, and improves data integrity [55].
- Advanced Analytics: The incorporation of AI and machine learning for method performance monitoring and trend analysis.
- Standardized Data Formats: Implementation of consistent data structures across sites to facilitate comparison and transfer.
- Advanced Control Systems: Transition from programmable logic controllers (PLCs) to distributed control systems (DCS) for better process integration and data management [55].
Platform and covalidation strategies represent the evolution of analytical method validation from repetitive, site-specific activities to efficient, integrated approaches suited for modern global biologics manufacturing. The combination of these approaches enables organizations to maintain scientific rigor and regulatory compliance while significantly accelerating method deployment across multiple sites.
As the biopharmaceutical industry continues to evolve toward more complex molecules and accelerated development timelines, these streamlined strategies will become increasingly essential for maintaining competitiveness while ensuring product quality and patient safety. The successful implementation of platform and covalidation approaches requires cultural shifts toward collaboration, knowledge sharing, and cross-functional engagement, but the significant efficiency gains and quality improvements justify this transformation.
Navigating Challenges: Troubleshooting, Transfer, and Lifecycle Optimization
The history of analytical method validation is marked by efforts to standardize the proof of method reliability. Since the late 1980s, government and international agencies have worked to formalize expectations, with the FDA designating United States Pharmacopeia (USP) specifications as legally recognized in 1987 [2]. The International Conference on Harmonisation (ICH) Q2(R1) guideline, a cornerstone document, established a harmonized set of performance characteristics for validation, including the critical pillars of specificity, linearity, and accuracy—the latter being deeply intertwined with proper sample preparation [2]. This framework moved the industry from informal verification to a structured, documented process of proving a method is fit for its purpose.
The evolution continues with recent guidelines like ICH Q14, which advocates for an Analytical Procedure Lifecycle Management approach, emphasizing a deeper, more scientific understanding of method parameters and their controls from development through routine use [62]. This in-depth technical guide will explore common pitfalls associated with three foundational areas of method validation, providing detailed protocols and strategies to overcome them, framed within this historical and evolving regulatory context.
Specificity: Ensuring Unambiguous Measurement
Core Principle and Definition
Specificity is the ability of an analytical procedure to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradants, or matrix components [2] [63]. It ensures that a peak's response is due to a single component and is not the result of co-elution or interference. A lack of specificity can lead to inaccurate potency results or a failure to detect impurities, directly impacting assessments of product efficacy and patient safety [63].
Common Pitfalls and Investigative Protocols
A primary pitfall is relying solely on retention time comparison without confirming peak purity. This can miss co-eluting peaks with similar UV spectra. Another critical error is omitting forced degradation studies during development, which fails to demonstrate the method's "stability-indicating" capacity [63].
Experimental Protocol: Forced Degradation (Stress) Studies A comprehensive specificity study must include forced degradation to generate potential degradants and prove the method can separate the active ingredient from these products.
- Materials: Active Pharmaceutical Ingredient (API), placebo/excipients, finished product, relevant impurities (if available).
- Stress Conditions: Expose the sample to acid, base, oxidative, thermal, and photolytic conditions [63].
- Procedure:
- Acid/Base Stress: Treat sample with 0.1M HCl or 0.1M NaOH at room temperature for several hours. Neutralize prior to analysis.
- Oxidative Stress: Treat sample with 3% hydrogen peroxide at room temperature for several hours.
- Thermal Stress: Heat solid sample at 105°C for a defined period.
- Photolytic Stress: Expose sample to UV light (e.g., 1.2 million lux hours).
- Analysis: Inject stressed samples and analyze. The method is considered specific if there is baseline resolution between the analyte peak and all degradation peaks, and if peak purity tests confirm the homogeneity of the analyte peak [2].
Experimental Protocol: Peak Purity Assessment
- Procedure:
- Analyze a standard, a placebo, and a sample.
- Using a Photodiode Array (PDA) detector, collect spectra across the entire peak (apex, upslope, downslope).
- Use software to compare all spectra within the peak. A pure peak will have a high purity match factor.
- Interpretation: A drop in the purity threshold indicates a potential co-eluting impurity. For complex matrices, Mass Spectrometry (MS) detection provides unequivocal peak purity information and is the detection method of choice in many laboratories [2].
Advanced Techniques for Specificity
The following workflow outlines a strategic approach to specificity determination, incorporating modern techniques:
Linearity: Establishing Proportional Response
Core Principle and Definition
Linearity of an analytical procedure is its ability to elicit test results that are directly, or through a well-defined mathematical transformation, proportional to the concentration of analyte in samples within a given range [2] [63]. A critical distinction must be made between the linearity of results and the response function. The response function is the relationship between the analytical signal and the concentration of the standard. The linearity of results, which is the true requirement, refers to the proportionality between the calculated sample concentration and its true concentration [63]. A method with a non-linear response function can still produce linear results if the correct calibration model is applied.
Common Pitfalls and Investigative Protocols
A major pitfall is evaluating linearity using standard solutions alone, which fails to identify matrix effects that can cause non-linearity in real samples [63]. Other common errors include using too few concentration levels, failing to cover the entire specified range, and incorrectly using the coefficient of determination (r²) as the sole acceptance criterion, which can mask a lack of fit.
Experimental Protocol: Establishing Linearity of Results
- Materials: Authentic standard, placebo (for drug product), and appropriate solvent.
- Procedure:
- Prepare Spiked Samples: Create a minimum of 5 concentration levels across the specified range (e.g., 50%, 75%, 100%, 125%, 150% of target concentration). For drug products, these should be samples spiked into the placebo matrix [2] [63].
- Analyze: Analyze each level in triplicate. The analysis should be performed over different days to incorporate some variability.
- Calculate and Plot: For each spiked sample, calculate the recovered concentration. Plot the mean recovered concentration (y-axis) against the theoretical concentration (x-axis).
- Data Analysis:
- Perform linear regression on the data: ( y = mx + c )
- Key Parameters:
- Slope (m): Should be close to 1.
- Y-intercept (c): Should be close to zero and not statistically significant.
- Coefficient of determination (r²): Typically expected to be ≥ 0.99.
- Residuals Plot: Graphically analyze the residuals (difference between observed and predicted y-values) versus concentration. The residuals should be randomly scattered around zero, not following a pattern, which would indicate a poor fit of the linear model [63].
Table 1: Acceptance Criteria for Linearity Validation
| Parameter | Recommended Acceptance Criteria | Rationale |
|---|---|---|
| Number of Levels | Minimum of 5 [2] | Ensures adequate range characterization |
| Concentration Range | Typically 50-150% of test concentration (for assay) [2] | Covers expected sample concentrations |
| Slope (m) | Close to 1 (e.g., 0.98 - 1.02) | Indicates proportionality |
| Y-Intercept (c) | Not statistically significant from zero | Ensures no constant bias |
| Coefficient of Determination (r²) | ≥ 0.990 [63] | Measures strength of linear relationship |
| Residuals | Randomly distributed around zero | Confirms model appropriateness |
Sample Preparation: The Foundation of Accuracy
Core Principle and Connection to Accuracy
Sample preparation is the critical bridge between the sample and the analytical measurement. Inaccuracies introduced here propagate through the entire process and cannot be corrected later. It is intrinsically linked to the validation parameter of accuracy (trueness), which is defined as the closeness of agreement between the mean value obtained from a series of measurements and an accepted reference value [63]. Errors in sample preparation directly cause systematic error (bias), undermining the reliability of all results.
Common Pitfalls and Risk Mitigation
Pitfalls often arise from a poor understanding of the sample matrix. Failing to test across all relevant matrices can lead to unexpected interferences or recovery issues during real-world use [64]. Incomplete extraction of the analyte, inadequate homogenization, sample degradation during preparation, and ignoring adsorption effects to container surfaces are other common sources of error. Furthermore, ion suppression in LC-MS/MS methods, caused by co-eluting matrix components, is a significant but often overlooked risk that reduces sensitivity and distorts quantification [64].
Experimental Protocol: Determining Accuracy/Recovery This protocol is designed to uncover errors stemming from sample preparation.
- Materials: Authentic standard, placebo (excipient mixture), and finished product batch with known concentration.
- Procedure:
- Prepare Solutions: Prepare a minimum of 9 determinations over 3 concentration levels (e.g., 80%, 100%, 120%) covering the specified range [2] [63].
- Standard Solutions: Prepare in solvent.
- Spiked Placebo Solutions: Spike known amounts of analyte into the placebo matrix.
- Analyze: Analyze all samples using the validated method.
- Calculate Recovery: For each spiked sample, calculate the percentage recovery. ( \text{Recovery} = \frac{\text{Measured Concentration}}{\text{Theoretical Concentration}} \times 100\% )
- Prepare Solutions: Prepare a minimum of 9 determinations over 3 concentration levels (e.g., 80%, 100%, 120%) covering the specified range [2] [63].
- Data Analysis:
- Report the recovery at each level and the overall mean recovery.
- The mean recovery should be close to 100%, with acceptable precision (e.g., %RSD < 2% for the assay of a drug substance).
Table 2: Scientist's Toolkit for Sample Preparation
| Tool/Reagent | Function in Sample Preparation |
|---|---|
| Placebo (Excipient Mix) | Mimics the sample matrix without the analyte; essential for accuracy/recovery studies and specificity testing [63]. |
| Forced Degradation Solutions (e.g., 0.1M HCl/NaOH, 3% Hâ‚‚Oâ‚‚) | Used in specificity studies to generate degradation products and prove the method is stability-indicating [63]. |
| Appropriate Internal Standard (IS) | Compensates for variability in sample preparation and analysis; crucial for LC-MS/MS to correct for matrix effects [64]. |
| Matrix-Matched Calibrators | Calibration standards prepared in the same matrix as the sample; helps identify and correct for matrix effects [64]. |
The following diagram maps the sources of variability and their impact on the total error of the analytical procedure, with sample preparation being a major contributor:
Within the historical framework of analytical method validation, the parameters of specificity, linearity, and sample preparation (accuracy) remain perennial pillars. The evolution from a "check-box" compliance exercise toward a lifecycle approach, as championed by ICH Q14, demands a deeper scientific understanding of these parameters [62]. By recognizing the common pitfalls—such as inadequate peak purity assessment, overlooking matrix effects in linearity, and poor recovery studies—and implementing the detailed investigative protocols outlined, scientists can develop more robust and reliable methods. This rigorous approach ensures that analytical procedures not only meet regulatory requirements but also consistently deliver results that safeguard product quality and, ultimately, patient safety.
In the framework of analytical method validation, the accuracy of a method, often assessed through spiking recovery experiments, is a cornerstone of reliability. For Size-Exclusion Chromatography (SEC)—a technique whose history is rooted in the separation of macromolecules by their hydrodynamic volume—ensuring quantitative recovery is paramount for obtaining accurate molar mass averages and distributions [65]. A deviation from expected recovery, such as the 70% recovery observed in this case study, is not merely a numerical discrepancy; it signals a fundamental breakdown in the assumed separation mechanism, potentially leading to a severe mischaracterization of the polymeric sample.
The history of analytical method validation underscores the importance of this parameter. As bioanalytical method validation guidance has evolved, the consistency of a method's ability to recover an analyte from a biological matrix has been a key indicator of its robustness and fitness for purpose [66]. This case study situates a modern SEC troubleshooting problem within the broader historical context of validation protocols, demonstrating how foundational principles guide the resolution of contemporary analytical challenges.
Historical and Technical Background of SEC
A Brief History of SEC Development
The origins of SEC can be traced back to the 1950s. The technique was first recognized when researchers noted that neutral small molecules and oligomers eluted from columns based on decreasing molecular weight [67] [68]. The pivotal milestone occurred in 1959 when Porath and Flodin synthesized cross-linked dextran packings with different pore sizes and successfully demonstrated the size separation of peptides and oligosaccharides [65]. Pharmacia Corporation subsequently marketed this packing under the name Sephadex, cementing the technique, then known as Gel Filtration Chromatography (GFC), in biochemistry laboratories worldwide [67].
Shortly thereafter, the technique was adapted for synthetic polymers. In 1962, John Moore of Dow Chemical Company produced cross-linked polystyrene resins for determining the molecular weight distribution of polymers soluble in organic solvents, a technique termed Gel Permeation Chromatography (GPC) [67] [68]. The licensing of this technology to Waters Associates made GPC instrumentation and columns widely available. Although the terms GFC and GPC persisted, it is now understood they represent the same fundamental size-exclusion mechanism, collectively referred to as SEC [65].
Fundamental Principles of SEC
Separation in SEC is governed solely by the hydrodynamic size and shape of macromolecules relative to the size and shape of the pores of the column packing [65]. The core principle is an entropic partitioning process where larger analytes, too big to enter the pores, are excluded and elute first. Smaller analytes can penetrate the pore volume and experience a longer path through the column, resulting in later elution [65]. The entire polymer sample is designed to elute within a defined volume, between the total volume of the mobile phase in the column and the volume of the mobile phase outside the packing particles [67].
Table 1: Key Historical Milestones in SEC Development
| Year | Development | Key Researchers/Entities | Impact |
|---|---|---|---|
| 1953-1956 | Early observations of size-based separation | Wheaton & Bauman; Lathe & Ruthven [65] | Established foundational concept of separation by size |
| 1959 | Synthesis of cross-linked dextran packings (Sephadex) | Porath & Flodin (Pharmacia) [67] [65] | Birth of Gel Filtration Chromatography (GFC) for biomolecules |
| 1962 | Development of cross-linked polystyrene resins | John Moore (Dow Chemical) [67] [68] | Birth of Gel Permeation Chromatography (GPC) for synthetic polymers |
| 1970s | Introduction of smaller (10 µm) rigid particles (µ-Styragel) | Waters Associates [65] | Enabled higher pressure, faster, and more efficient analyses |
The Case: Investigating Low Spiking Recovery in SEC
Problem Presentation
A laboratory is validating an SEC method for the analysis of a proprietary monoclonal antibody fragment. The method uses a modern silica-based SEC column with an aqueous mobile phase (0.1 M sodium phosphate, 0.1 M sodium chloride, pH 6.8). As part of the validation, a spiking recovery experiment is performed. A known concentration of the analyte is spiked into the validation sample matrix, and the measured peak area is compared to that of a standard of the same concentration in pure mobile phase. The experiment returns a recovery of 70%, far below the typical acceptance criteria of 90-105% for bioanalytical methods [66]. This low recovery suggests a significant portion of the analyte is being lost or not detected, threatening the validity of all subsequent quantitative data.
Initial Diagnostic Workflow
A structured approach is essential to diagnose the root cause. The following workflow outlines the logical sequence for investigating low SEC recovery, from simple quick checks to more complex mechanistic studies.
Systematic Investigation of Root Causes
The recovery problem can be systematically investigated by examining several key areas of the SEC method. The following table outlines the most common causes, their diagnostic signatures, and the underlying mechanisms.
Table 2: Root Cause Analysis for Low SEC Spiking Recovery
| Root Cause Category | Specific Examples | Diagnostic Signatures | Mechanism of Loss |
|---|---|---|---|
| Non-Size Exclusion Interactions | Hydrophobic interactions with packing [65]; Ionic interactions with charged residues | Peak tailing, abnormal retention time (shift from expected), reduced recovery with low salt | Adsorption of analyte to the stationary phase, removing it from the separation stream |
| Sample Preparation Issues | Adsorption to filters or vial surfaces; Inaccurate dilution or pipetting | Recovery loss after specific preparation step; Inconsistent results between replicates | Physical loss of analyte due to binding to labware or human error |
| Column & Mobile Phase | Mobile phase pH/ionic strength promoting aggregation; Degraded or fouled column | High backpressure; Presence of high-mass "aggregate" peak early in chromatogram; Shifting baseline | Formation of insoluble or too-large aggregates that are excluded or trapped, or degradation of the analyte itself |
| Analyte Instability | Chemical degradation during processing or analysis; Enzyme activity | Appearance of new, unexpected peaks (degradants); Disappearance of main peak | Analyte is chemically altered or decomposed into species not quantified as the intact product |
Experimental Protocols for Diagnosis and Resolution
Protocol 1: Investigating Secondary Interactions
Objective: To confirm and mitigate non-size exclusion interactions (e.g., hydrophobic or ionic) between the analyte and the stationary phase.
Methodology:
- Analyze Peak Shape and Retention: Inject the standard and note any peak tailing or fronting. Compare the retention time to a known inert analyte to check for unexpected shifts caused by adsorption/desorption processes [65].
- Mobile Phase Modification Scouting:
- For suspected ionic interactions: Prepare mobile phases with increasing ionic strength (e.g., 0.1 M, 0.2 M, 0.3 M sodium chloride). A trend of increasing recovery with higher salt concentration confirms ionic interactions.
- For suspected hydrophobic interactions: Prepare mobile phases with small percentages of organic modifier (e.g., 1-5% acetonitrile or isopropanol). Caution: Only use modifiers compatible with the column's warranty and stability. An increase in recovery suggests hydrophobic interactions.
- Evaluate Alternative Columns: Test a different SEC column from another manufacturer. The surface chemistry of the base matrix and the bonding chemistry can differ significantly, potentially minimizing undesirable interactions.
Protocol 2: Assessing Sample Preparation Losses
Objective: To isolate and quantify analyte loss during the sample preparation process.
Methodology:
- Filter Adsorption Test:
- Prepare a standard solution at the target concentration.
- Split it into two aliquots. Analyze one aliquot directly.
- Pass the second aliquot through the specific filter membrane (e.g., PVDF, nylon, cellulose acetate) intended for use.
- Analyze the filtrate.
- Calculate the percentage recovery by comparing the peak areas of the filtered vs. unfiltered samples. A significant drop indicates filter adsorption.
- Vial Adsorption Test:
- Prepare a standard solution and place it in the intended autosampler vial.
- Analyze it immediately (T=0).
- Let the solution sit in the vial in the autosampler for the duration of a typical analytical run (e.g., 8-24 hours) and re-inject from the same vial.
- A decrease in peak area over time suggests surface adsorption to the vial.
Protocol 3: Testing for Analyte Aggregation
Objective: To determine if the analyte is forming high molecular weight aggregates that are excluded from the pore network or precipitate.
Methodology:
- Multi-Angle Light Scattering (MALS) Detection: If available, coupling the SEC system to a MALS detector provides an absolute measurement of molar mass. A significant mass signal at the void volume confirms the presence of large aggregates [65].
- Dynamic Light Scattering (DLS): Perform DLS on the sample solution before injection. An increase in the mean hydrodynamic radius or the presence of a large-size population is indicative of aggregation.
- Visual Inspection: Centrifuge the sample vial and visually inspect for any pellet or haziness, which would indicate precipitation.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for SEC Troubleshooting
| Item | Function & Application in Troubleshooting |
|---|---|
| High-Purity Salts (e.g., NaCl, KCl, NaPhosphate) | Used to adjust the ionic strength of the mobile phase to screen for and suppress ionic interactions between the analyte and column [67]. |
| Controlled-Pore Packing Materials (e.g., Silica, Polymeric Gels) | The stationary phase itself. Different base matrices (silica vs. polymer) and surface chemistries offer alternatives if one column type shows strong secondary interactions [67] [68]. |
| SEC Molecular Weight Standards | Narrow dispersity polymers (e.g., proteins, PEG) used to calibrate the column and assess performance. A shift in their expected retention can indicate column damage or secondary interactions [65]. |
| Inert Syringe Filters (e.g., low protein binding membranes) | Used during sample preparation to remove particulates. Testing different membrane materials (e.g., PVDF, PES) helps diagnose and resolve filter-mediated analyte loss. |
| 2-Amino-6-chlorobenzoyl chloride | 2-Amino-6-chlorobenzoyl Chloride|CAS 227328-16-7 |
| Fmoc-2-amino-6-fluorobenzoic acid | Fmoc-2-amino-6-fluorobenzoic acid, CAS:1185296-64-3, MF:C22H16FNO4, MW:377.4 g/mol |
Resolution and Broader Implications for Method Validation
In the presented case, the investigation revealed that the monoclonal antibody fragment was experiencing hydrophobic interactions with the stationary phase, a known pitfall where the separation is no longer purely based on size exclusion [65]. This was diagnosed via Protocol 1, where the addition of 3% isopropanol to the mobile phase improved recovery to 98%. Furthermore, Protocol 2 identified a minor additional loss (5%) due to adsorption to a specific nylon filter. Switching to a low-binding PVDF filter resolved this issue completely. The final validated method incorporated these two changes, ensuring accurate and reliable quantification.
This case underscores a critical lesson in the context of analytical method validation history: initial full validation must be rigorous and holistic [66]. Parameters like selectivity and accuracy are deeply interconnected. A method can appear linear and precise yet fail utterly in recovery due to an unaddressed matrix or interaction effect. The principles codified in guidance documents, such as the need for cross-validation when methods are altered, stem from precisely these kinds of observational learnings [66]. Troubleshooting a spiking recovery problem is not just about fixing a single method; it is an exercise in applying the cumulative, historical wisdom of analytical science to ensure data integrity in drug development and beyond.
The evolution of analytical method validation protocols represents a relentless pursuit of quality, traceability, and reproducibility in pharmaceutical sciences. Historically, method validation focused primarily on establishing performance characteristics within a single laboratory environment. Regulatory guidance documents such as ICH Q2(R1) and USP General Chapter 〈1225〉 provided a foundation for validating procedures for parameters like accuracy, precision, and specificity [64]. However, as drug development became increasingly globalized, with manufacturing, stability testing, and release activities distributed across multiple sites, the challenge of transferring methods while maintaining data integrity became paramount. This necessitated formalized processes for analytical method transfer (AMT) to ensure that methods remained robust and reproducible when transferred from a transferring laboratory (TL) to a receiving laboratory (RL) [69] [70].
The regulatory framework has progressively recognized this need, with documents like USP 〈1224〉 providing specific guidance on transfer strategies [69]. More recently, the adoption of ICH Q14 on Analytical Procedure Development and the integrated approach to knowledge management throughout the analytical procedure lifecycle signifies a shift towards a more systematic, risk-based framework. This modern paradigm emphasizes that validation is not a one-time event but requires continuous verification, especially when methods are deployed across different sites with varying equipment and personnel [62]. Understanding this historical progression is essential for appreciating the strategies and best practices required to overcome the persistent hurdle of cross-laboratory method consistency.
The Foundation: Principles of Analytical Method Transfer
At its core, analytical method transfer (AMT) is a documented process that demonstrates the receiving laboratory (RL) is capable of successfully performing the analytical procedure transferred from the transferring laboratory (TL), producing results that are comparable and reliable [69] [70]. Each transfer involves these two main parties: the TL, which is the source or origin of the method and possesses the foundational knowledge about its performance; and the RL, which must demonstrate the capability to replicate the method's performance [69] [70].
The success of a transfer is governed by several key principles. First, the method's robustness must be established in the transferring laboratory. A method that is not robust and resilient to minor, expected variations will inevitably face challenges when replicated in a different environment [71]. Second, a risk-based approach should be applied throughout the transfer process. This involves assessing factors such as the RL's prior experience with the methodology, the complexity of the method, and the specifications of the product [69]. Finally, clear and unambiguous documentation is critical. The language used in transfer protocols must allow for only a single interpretation to prevent subjective understanding from leading to deviations [71].
Method Transfer Strategies: A Comparative Analysis
The United States Pharmacopeia (USP) General Chapter 〈1224〉 outlines several standardized approaches for conducting an analytical method transfer. The choice of strategy depends on the specific context of the transfer, including the method's maturity, the receiving unit's familiarity with the technology, and regulatory considerations [69] [71].
The table below summarizes the primary transfer strategies as defined by USP 〈1224〉:
| Type of Strategy | Design | Typical Applications |
|---|---|---|
| Comparative Testing | The same set of samples (e.g., from a stability batch or manufactured lot) is tested by both the TL and the RL, and the results are statistically compared [69]. | LC/GC assay and related substances, and other methods like tests for water, residual solvents, and ions [69]. |
| Co-validation | The RL is included as a participant from the outset of the method validation process. The reproducibility data generated across the laboratories forms part of the validation evidence [69]. | Methods being transferred from a development unit to a quality control (QC) unit, where the RL is part of the validation team [69] [71]. |
| Revalidation | The RL performs a full or partial validation of the analytical method, independent of the original validation studies conducted by the TL [69]. | Microbiological testing, other critical threshold tests, or when the sending laboratory is not involved in the testing [69] [71]. |
| Transfer Waiver | A transfer without additional testing is justified based on scientific rationale. This is not a default option and requires strong justification [69]. | Can be considered for all method transfers but requires scientific justification since testing is not performed. Justification may include the RL's existing experience with identical methods on the same product [69]. |
Experimental Protocols for Successful Transfer
A successful transfer is not an ad-hoc activity but a meticulously planned and executed project. The following sections detail the key experimental and procedural components.
The Method Transfer Plan and Protocol
Before execution, a comprehensive analytical method transfer plan is crucial. This plan assesses time and resources and is particularly recommended when transferring two or more methods [69]. The plan should include objectives, scope, responsibilities, and the chosen transfer strategy [69].
This plan is operationalized through a detailed transfer protocol, approved by both the TL and RL. The protocol must include [69]:
- Purpose and Scope: Clearly defined objectives and boundaries of the transfer.
- Materials and Equipment: A detailed list of critical reagents, reference standards, and equipment, including any allowable equivalents.
- Experimental Design: A precise description of the testing to be performed, including the number of samples, replicates, and analytical runs.
- Acceptance Criteria: Pre-defined, justified criteria based on the method's validation data and current regulatory requirements.
The Comparison of Methods Experiment
A cornerstone of the "Comparative Testing" strategy is the comparison of methods experiment. Its purpose is to estimate the systematic error or inaccuracy between the test method at the RL and the comparative method at the TL [72].
Experimental Design Guidelines:
- Sample Number and Selection: A minimum of 40 different patient specimens is recommended. These specimens should cover the entire working range of the method and represent the expected sample matrix variability [72].
- Replication and Timing: Analyses should be performed over multiple days (minimum of 5 days) to capture inter-day variation. While single measurements are common, duplicate measurements can help identify outliers and transposition errors [72].
- Data Analysis: Data should be graphed immediately during collection to identify discrepant results. A difference plot (test result minus comparative result vs. comparative result) is ideal for visualizing constant and proportional systematic errors [72].
- Statistical Calculations: For data covering a wide analytical range, linear regression statistics (slope, y-intercept, standard deviation about the regression line) are preferred. The systematic error (SE) at a critical medical decision concentration (Xc) is calculated as:
Yc = a + bXc, thenSE = Yc - Xc[72].
The following diagram illustrates the key decision points and workflow in a typical analytical method transfer process.
Case Study: A 5-Year Comparability Verification
A 2022 study demonstrates a real-world application of ensuring consistency across multiple instruments (a form of internal transfer). Researchers maintained comparability of five clinical chemistry instruments from different manufacturers over five years using a protocol of weekly verification with pooled residual patient samples [73].
Methodology:
- Samples: Two pooled residual serum samples were used each week.
- Procedure: Twelve clinical chemistry analytes were measured on all five instruments weekly.
- Acceptance Criteria: The Royal College of Pathologists of Australasia (RCPA) total allowable performance goals were used.
- Corrective Action: If results from any instrument exceeded the allowable verification range versus the comparative instrument for 2-4 weeks, a simplified comparison using 10-20 samples was performed. The results were then converted using a linear regression equation (
Cconverted = (Cmeasured - a) / b) before being reported to clinicians [73].
Quantitative Results (2015-2019): The study collected 432 weekly verification results. The methodology successfully maintained comparability, as shown in the table below.
| Analyte Category | Percentage of Results\nRequiring Conversion | Outcome of Conversion Action |
|---|---|---|
| All Analytes | 58% | The inter-instrument CV for results after conversion action was "much lower" than for the original measured data, demonstrating improved harmonization [73]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of an analytical method transfer is contingent on the quality and consistency of the materials used. The following table details key reagents and materials that must be controlled.
| Item | Function & Importance in Transfer |
|---|---|
| Certified Reference Standards | Provides the known benchmark for instrument calibration and method accuracy. Inconsistency between standards used at TL and RL is a major source of transfer failure [69] [64]. |
| Critical Reagents | Specific reagents (e.g., buffers, derivatization agents) whose properties directly impact method performance (e.g., retention time, peak shape). Must be sourced from the same vendor or qualified for equivalence [69] [70]. |
| System Suitability Test (SST) Materials | A preparation used to verify that the chromatographic system (or other instrumentation) is capable of reproducing the required performance criteria before sample analysis. Essential for daily method verification [62]. |
| Stable Sample Pools | Well-characterized, homogeneous, and stable patient or product sample pools are crucial for comparative testing. They allow for a meaningful comparison of results between the TL and RL over time [73]. |
Navigating Common Pitfalls and Current Challenges
Despite well-defined protocols, several common pitfalls can derail an analytical method transfer. Awareness and proactive mitigation of these risks are essential.
- Undefined or Unjustified Acceptance Criteria: One of the most critical failures is setting acceptance criteria without a scientific basis rooted in the method's validation history. Mitigation: Use risk assessment to set criteria that are challenging yet achievable, reflecting the method's actual performance [70].
- Inadequate Documentation and Communication: Poorly written protocols open to interpretation, and ineffective communication between TL, RL, and sponsors lead to deviations. Mitigation: Ensure language is unambiguous and plan for regular communication meetings with all stakeholders [70] [71].
- Poor Coordination of Samples and Materials: Mismanagement in the logistics of shipping and qualifying samples, standards, and reagents can cause significant delays. Mitigation: Have a strict, well-defined plan for coordinating these materials well in advance of the transfer [70].
- Adoption of Modern Guidelines (ICH Q14): The industry is currently grappling with the implementation of ICH Q14, which introduces an enhanced approach to analytical procedure development and lifecycle management. Challenges include defining an Analytical Target Profile (ATP), establishing Method Operable Design Regions (MODR), and managing post-approval changes through Established Conditions (ECs) [62]. This represents a significant shift from the traditional, fixed-parameter approach to a more flexible, knowledge-based framework.
The following workflow outlines the key steps in the comparison of methods experiment, a critical component of many transfer protocols.
Overcoming the transfer hurdle to ensure method consistency across laboratories and sites remains a dynamic challenge in pharmaceutical development. The journey from historically focused, single-lab validation protocols to today's lifecycle-oriented frameworks like ICH Q14 underscores a growing recognition of complexity and the need for proactive, knowledge-driven science. Success hinges on a foundation of robust method development, strategic and well-documented transfer protocols, and rigorous comparative experimentation. Furthermore, the increasing globalization of the pharmaceutical supply chain necessitates continuous improvement in harmonization practices. By learning from historical precedents, adhering to structured protocols, and embracing modern, flexible regulatory frameworks, scientists can ensure that analytical methods consistently produce reliable data—a non-negotiable requirement for safeguarding product quality and, ultimately, patient safety.
The paradigm for analytical method validation has undergone a fundamental shift from a static, one-time event to a dynamic, holistic lifecycle approach. This transformation is embedded within the broader historical context of pharmaceutical quality systems, which have evolved from discrete compliance exercises toward integrated, knowledge-driven frameworks. The adoption of ICH Q14 on Analytical Procedure Development and the revised ICH Q2(R2) on Validation of Analytical Procedures represents the most significant modernization of analytical method guidelines in decades, moving beyond the prescriptive, "check-the-box" validation model established by earlier guidelines like ICH Q2(R1) [47] [74]. This whitepaper examines the core principles of lifecycle management under this new framework, focusing on the mechanisms for continuous verification and structured post-approval change management that ensure methods remain robust, reliable, and compliant throughout their operational lifetime.
The Modern Regulatory Framework: ICH Q14 and Q2(R2)
The simultaneous publication of ICH Q14 and ICH Q2(R2) provides a harmonized foundation for the scientific and technical approach to analytical procedure lifecycle management [74]. These guidelines, adopted in 2023, introduce a structured, science-based framework that encourages an enhanced approach to development and validation [62] [47].
- ICH Q14 (Analytical Procedure Development): This guideline outlines the principles for systematic, risk-based analytical procedure development. It introduces the Analytical Target Profile (ATP) as a foundational element and provides a structured approach for establishing an analytical control strategy and managing post-approval changes [74].
- ICH Q2(R2) (Validation of Analytical Procedures): This revised guideline expands the scope of its predecessor to include modern analytical technologies and emphasizes that validation is an activity within the broader method lifecycle, not an isolated event [47].
Together, these guidelines describe a holistic journey for an analytical method, from initial conception through development, validation, routine use, and eventual retirement, with continuous verification and managed change as critical sustaining activities [47].
Core Principle: The Analytical Procedure Lifecycle
The analytical procedure lifecycle is a continuous process comprised of three interconnected stages: procedure design and development, procedure performance qualification, and ongoing procedure performance verification [62]. This model ensures that methods are not only validated once but are actively managed to remain fit-for-purpose throughout their entire operational life.
The following diagram illustrates the key stages, control points, and feedback loops within the analytical procedure lifecycle.
Establishing Continuous Verification Through an Analytical Control Strategy
An effective Analytical Control Strategy is the cornerstone of continuous verification, ensuring ongoing method reliability by proactively identifying and controlling sources of variability [62]. This strategy transforms method maintenance from a reactive investigation of failures to a proactive system of quality assurance.
Key Components of an Analytical Control Strategy
- System Suitability Tests (SSTs) and Sample Suitability: These tests are executed with each analytical run to verify that the system is performing as expected. The control strategy defines the critical SST parameters and acceptance criteria, which are derived from the method's understanding gained during development [62].
- Established Conditions (ECs): As defined in ICH Q12 and applied to analytical procedures in ICH Q14, ECs are the legally binding, validated parameters and criteria necessary to assure analytical procedure performance [62]. They include:
- Performance characteristics and acceptance criteria.
- Procedure principles (e.g., the specific technology used).
- Set points or ranges for critical method parameters.
- Continuous Monitoring and Feedback Loops: Routine monitoring of method performance outputs, such as SST results and control chart data, is essential. This data is trended to quickly detect Out-of-Trend (OOT) performance, facilitating root cause analysis and preventing Out-of-Specification (OOS) results [62].
The Scientist's Toolkit: Essential Materials for Continuous Verification
Table 1: Key Research Reagent Solutions and Materials for Lifecycle Management
| Item | Function in Continuous Verification |
|---|---|
| Reference Standards | Qualified standards are critical for ensuring the accuracy and precision of the method during system suitability testing and ongoing quality control. |
| Critical Reagents | Well-characterized reagents (e.g., antibodies, enzymes, buffers) with established stability profiles and expiration dates are vital for maintaining method robustness [75]. |
| Automated Data Management Systems (LIMS) | Laboratory Information Management Systems are essential for trending SST results, managing OOT alerts, and maintaining audit-ready data trails for regulatory inspections [62] [76]. |
| Stability Study Materials | Samples, standards, and critical reagents are placed on stability studies to establish and verify expiration times, preventing degradation from impacting data quality [75]. |
Managing Post-Approval Changes with a Science- and Risk-Based Approach
A pivotal benefit of the enhanced approach under ICH Q14 is the regulatory flexibility it provides for managing post-approval changes [62]. By thoroughly understanding the method and its risk profile during development, organizations can implement a more efficient and science-driven change management process.
The Role of Established Conditions and Risk Categorization
The foundation for efficient change management lies in the proper definition and risk categorization of Established Conditions (ECs) during the initial submission [62]. Each EC is assessed for its potential impact on method performance and, consequently, product quality. This risk categorization directly dictates the regulatory pathway for any future changes.
- High-Impact ECs: Changes to these parameters (e.g., the fundamental analytical technique) carry a high risk and typically require prior approval from regulatory authorities.
- Low-Impact ECs: Changes within the predefined ranges of low-risk parameters, or changes to parameters with a demonstrated low impact, may only require notification to the authorities [62].
Mechanism: Post-Approval Change Management Protocols (PACMPs)
For changes with potential impact, ICH Q14 endorses the use of Post-Approval Change Management Protocols (PACMPs) [62]. A PACMP is a prospective, approved plan that outlines the studies and acceptance criteria required to justify a specific type of change. By submitting a PACMP with the original application or as a supplement, a company can pre-define the data needed to support a future change, thereby streamlining the implementation process once the data is collected.
The following workflow outlines the decision-making process for managing a proposed change to an analytical procedure, demonstrating the interaction between risk assessment and regulatory pathways.
Experimental Protocols for Lifecycle Management
The practical implementation of lifecycle management relies on specific experimental studies conducted during development and in support of changes.
Protocol for Defining the Method Operable Design Region (MODR)
- Objective: To identify the combination of critical method parameter ranges within which the method delivers consistent, reliable performance, ensuring robustness for routine use.
- Methodology: Utilize a structured Design of Experiments (DoE) [62]. DoE efficiently evaluates multiple parameters and their interactions simultaneously. A typical workflow involves:
- Risk Assessment: Use an Ishikawa diagram or FMEA to identify potentially critical method parameters [62].
- Screening Design: A fractional factorial or Plackett-Burman design to identify which parameters have a significant effect on critical method attributes (e.g., resolution, accuracy).
- Response Surface Methodology: A Central Composite Design or Box-Behnken design to model the relationship between the significant parameters and the method responses, allowing for the visualization and definition of the MODR.
- Data Analysis: Statistical analysis of the DoE data to build a model and identify the proven acceptable ranges (PAR) or the broader MODR for each critical parameter. This data directly supports the setting of Established Conditions [62].
Protocol for Continuous Verification via System Suitability and Trend Monitoring
- Objective: To provide ongoing, real-time assurance that the analytical procedure remains in a state of control during routine use.
- Methodology:
- Define SST Criteria: Establish scientifically justified system suitability test criteria (e.g., precision, resolution, tailing factor) based on development data and the ATP [62] [12].
- Execute and Record: Require that these SSTs are performed and recorded with every analytical run. The procedure is only used if the SST criteria are met [12].
- Data Trending: Utilize a LIMS or other data management system to collect all SST results and key performance data over time [62].
- Statistical Process Control (SPC): Apply control charts to the trended data to establish normal process variation and set alert and action limits. This allows for the detection of OOT results before they lead to an OOS failure [62].
Table 2: Key Validation Parameters and Their Role in the Method Lifecycle
| Validation Parameter | Traditional Role (One-Time Event) | Lifecycle Role (Continuous Verification) |
|---|---|---|
| Precision | Demonstrated during initial validation under controlled conditions. | Monitored continuously through system suitability test results and control charts of sample replicates. |
| Robustness | Evaluated by testing deliberate variations in method parameters. | The foundation of the MODR; changes within the MODR are managed via the control strategy without revalidation. |
| Specificity | Confirmed during validation against potential interferents. | Re-assessed when changes in the manufacturing process or formulation introduce new potential interferents. |
| Accuracy | Established during validation through spike/recovery experiments. | Verified periodically through the analysis of certified reference materials or proficiency testing samples. |
The modern framework for analytical procedure lifecycle management, as defined by ICH Q14 and Q2(R2), marks a significant evolution in pharmaceutical quality systems. By integrating continuous verification through a robust analytical control strategy and enabling science-based post-approval change management, this approach moves the industry beyond compliance toward a state of enhanced product understanding and operational excellence. For researchers and drug development professionals, adopting this lifecycle model is not merely a regulatory requirement but a strategic imperative. It builds a resilient system where methods are designed for reliability, monitored for consistency, and adapted with agility, ultimately ensuring the ongoing quality, safety, and efficacy of medicines for patients.
The history of analytical method validation is, at its core, a history of the pursuit of data integrity. As regulatory frameworks for pharmaceutical development have evolved, the focus has shifted from simply proving a method works to ensuring the entire data lifecycle is trustworthy, reliable, and defensible. Data integrity provides the foundation for credible analytical results, which in turn underpin the safety, efficacy, and quality of every drug product. In today's regulatory environment, the ALCOA+ framework has emerged as the global standard for achieving this integrity, translating broad principles into tangible, auditable attributes for data generated throughout a method's lifecycle—from development and validation to routine use in quality control [77] [78].
The consequences of data integrity failures are severe. Analyses of regulatory actions indicate that over half of the FDA Form 483 observations issued to clinical investigators involve data integrity violations [78]. These gaps—whether from human error, technical issues, or inadequate processes—compromise patient safety and can lead to warning letters, consent decrees, and the rejection of drug applications [77] [78]. This guide provides researchers and drug development professionals with a detailed roadmap for implementing ALCOA+ principles, offering practical methodologies to identify and remediate the compliance gaps that threaten analytical research.
The ALCOA+ Framework: From Foundational Principles to Practical Application
The ALCOA acronym, articulated by the FDA in the 1990s, has expanded to meet the complexities of modern, data-intensive laboratories. The “+†adds critical attributes that ensure data is not only created correctly but remains reliable over its entire lifecycle [78]. The following table summarizes the core and expanded ALCOA+ principles.
Table: The ALCOA+ Principles for Data Integrity
| Principle | Core/Expanded | Definition & Technical Requirements |
|---|---|---|
| Attributable | Core ALCOA | Uniquely links each data point to the individual or system that created or modified it. Requirements: Unique user IDs (no shared accounts), role-based access controls, and a validated audit trail that captures the user, date, and time [77] [79]. |
| Legible | Core ALCOA | Data must be permanently readable and reviewable in their original context. Requirements: Reversible encoding/compression; human-readable formats for long-term archiving; no obscured records [77]. |
| Contemporaneous | Core ALCOA | Recorded at the time of the activity or observation. Requirements: Automatically captured date/time stamps synchronized to an external standard (e.g., UTC/NTP); manual time zone conversions are non-compliant [77] [78]. |
| Original | Core ALCOA | The first capture of the data or a certified copy created under controlled procedures. Requirements: Preservation of dynamic source data (e.g., instrument waveforms); validated processes for creating certified copies; audit trails that preserve history without obscuring the original [77] [78]. |
| Accurate | Core ALCOA | Data must be correct and truthful, representing what actually occurred. Requirements: Faithful representation of events; validated calculations and transfers; calibrated and fit-for-purpose equipment; amendments that do not obscure the original record [77]. |
| Complete | ALCOA+ | All data, including repeat or failed analyses, metadata, and audit trails, must be present. Requirements: Configurations that prevent permanent deletion; audit trails that capture all changes; retention of all data needed to reconstruct the process [77] [78]. |
| Consistent | ALCOA+ | The data lifecycle is sequential and time-ordered, with no contradictions. Requirements: Chronologically consistent timestamps; standardized definitions and units across systems; controlled sequencing of activities [77]. |
| Enduring | ALCOA+ | Data remains intact and usable for the entire required retention period. Requirements: Suitable, stable storage formats (e.g., PDF/A); validated backups; disaster recovery plans; measures to prevent technology lock-in [77] [79]. |
| Available | ALCOA+ | Data can be retrieved in a timely manner for review, audit, or inspection over the retention period. Requirements: Searchable, indexed archives; tested retrieval pathways; clear labeling of storage locations [77] [78]. |
| Traceable | ALCOA++/C | A further enhancement ensuring a clear, end-to-end lineage for data. Requirements: An unbroken chain of documentation from source to report; audit trails that link all related records and changes [77]. |
The relationship between these principles forms a cohesive framework for managing data throughout the analytical method lifecycle, from data creation and processing to storage and retrieval.
Identifying Compliance Gaps: A Proactive Methodology
Despite understanding ALCOA+, many laboratories struggle with implementation. A reactive approach—waiting for an audit finding—is high-risk. Instead, organizations should proactively identify and remediate gaps using Data Process Mapping [80] [81]. This technique moves beyond generic checklists to provide a visual understanding of how data flows through an analytical process, pinpointing exactly where vulnerabilities exist.
Experimental Protocol: Data Process Mapping for a Chromatographic Analysis
The following methodology, adapted from regulatory guidance, is a practical way to identify data integrity gaps in analytical methods [80].
- Objective: To visually map the end-to-end process of a chromatographic analysis, from sample preparation to the final reportable result, in order to identify and risk-assess vulnerabilities in data and records.
- Materials & Personnel:
- Facilitator: One person to lead the session.
- Subject Matter Experts (2-3): Analysts and laboratory managers who know the process intimately.
- Tools: Whiteboard/large sheet, Post-it notes, pencils, and an eraser. (Software like Visio should only be used for the final documentation.)
- Step-by-Step Procedure:
- Define Process Boundaries: Clearly mark the start (e.g., sample receipt) and end (e.g., result approval and reporting) of the process.
- Map Process Steps: The SMEs write each activity of the process on a Post-it note and place them in sequence on the whiteboard. The facilitator should challenge and refine the flow through 2-3 iterations until it accurately reflects the real-world process.
- Document Data & Records: For each activity, document all data inputs, outputs, processing steps, verification checks, and storage locations (e.g., paper logbook, standalone CDS, network drive, Excel spreadsheet).
- Identify Vulnerabilities: For each step, the team must ask critical questions [80]:
- Criticality: How critical is this data to product quality decisions?
- Storage & Vulnerability: Where is the data stored? Is it vulnerable to loss, alteration, or obscuring?
- Access Control: Who can access the data? Are access controls adequate and is there segregation of duties?
- Audit Trail: Are changes to electronic data captured in a secure, understandable audit trail?
- Attribution & Verification: Is responsibility for each step clear? How is data accuracy verified?
- Risk Assessment and Remediation: Each identified vulnerability must be risk-assessed based on its criticality and probability. Remediation plans should be developed, ranging from quick fixes (e.g., implementing a logbook procedure) to long-term solutions (e.g., replacing a non-compliant standalone system with a networked, validated CDS) [80].
Diagram: A simplified data process map for a chromatographic analysis, highlighting common high-risk gaps such as reliance on paper as raw data and uncontrolled spreadsheets.
The Scientist's Toolkit: Essential Research Reagent Solutions
Upholding ALCOA+ requires a combination of technological solutions and methodological rigor. The following tools are essential for constructing a compliant research environment.
Table: Essential Research Reagent Solutions for Data Integrity
| Tool / Solution | Primary Function in Upholding ALCOA+ | Key Features & Compliance Rationale |
|---|---|---|
| Validated Chromatography Data System (CDS) | Centralized data acquisition and processing for chromatographic methods. | Features: Configurable audit trails, electronic signatures, role-based access, and data encryption. Rationale: Ensures data is Attributable, Original, and Complete by preventing deletion and capturing all changes [80]. |
| Electronic Lab Notebook (ELN) | Digital management of experimental procedures and observations. | Features: Template-driven protocols, time-stamped entries, and integration with instruments. Rationale: Enforces Contemporaneous and Legible recording, replacing error-prone paper notebooks [77]. |
| Laboratory Information Management System (LIMS) | Manages sample lifecycle, associated data, and workflows. | Features: Sample tracking, workflow enforcement, and result management. Rationale: Promotes Consistency and Availability by standardizing processes and providing structured data retrieval [80]. |
| Statistical Analysis Software (e.g., SAS, R) | Performs statistical computing and advanced data validation checks. | Features: Scripted analyses, reproducible results, and environment for automated validation. Rationale: Supports Accuracy and Traceability by providing a reproducible audit trail of data transformations and calculations [82]. |
| Electronic Data Capture (EDC) System | Captures clinical trial data directly from sites in real-time. | Features: Built-in edit checks (range, format, logic), direct data entry, and audit trails. Rationale: Ensures Accurate and Complete data at the point of collection, minimizing transcription errors [82]. |
Detailed Experimental Protocols for Key Compliance Activities
Protocol: Risk-Based Audit Trail Review for a CDS or LIMS
Regulators expect proactive, ongoing review of audit trails focused on critical data, not just a retrospective check before an inspection [77].
- Objective: To routinely monitor the audit trails of a critical computerized system (e.g., CDS, LIMS) for anomalous activities that may indicate data integrity issues.
- Scope & Frequency: The review should focus on critical data related to product quality (e.g., sample results, integration parameters, method changes). A triage-level review should be performed weekly, with a deep-dive review monthly, as per a risk-based schedule [79].
- Procedure:
- Define Review Scope: Identify the key data segments and time period for the review.
- Execute Query: Use the system's audit trail review tool to generate a report filtered for critical activities (e.g., deletions, reprocessing, manual integrations, changes to results or methods).
- Analyze for Anomalies: Investigate the generated report for the following patterns [79]:
- Unplanned changes to methods or records without documented justification.
- Failed login attempts or repeated account lockouts.
- Time stamp anomalies suggesting clock drift or manipulation.
- Bulk edits or mass updates that lack a corresponding batch record.
- Admin overrides or privilege escalations without a documented business need.
- Document and Act: Document the scope, findings, and any resulting corrective and preventive actions (CAPA). Trends should be analyzed and discussed monthly [79].
Protocol: Implementing Targeted Source Data Verification (tSDV) in Clinical Trials
This technique aligns with Risk-Based Quality Management (RBQM) principles to focus validation efforts on the most critical clinical data.
- Objective: To verify the accuracy and reliability of high-impact clinical data points by comparing them against original source documents, thereby optimizing resource allocation.
- Procedure:
- Identify Critical Data Points: Based on the trial's RBQM plan, identify key variables pivotal to outcomes and safety (e.g., primary efficacy endpoints, adverse events, key inclusion/exclusion criteria) [82].
- Develop a Targeted SDV Plan: Specify the exact data points and source documents requiring verification. This plan should be documented and followed by clinical monitors.
- Execute Verification: The monitor compares the data entered in the Case Report Form (CRF)—typically in an EDC system—against the original source document (e.g., hospital medical record).
- Manage Queries: Any discrepancies are flagged as queries within the EDC system for the site to resolve. All queries and their resolutions are tracked to ensure Accuracy and Completeness [82].
Upholding ALCOA+ principles and overcoming compliance gaps is not a one-time project but an ongoing commitment woven into the fabric of analytical science. It requires a holistic strategy that integrates robust technological controls, clear process methodologies like data process mapping, and, most importantly, a strong quality culture [79] [83]. This culture is built by leadership that champions data integrity, provides scenario-based training, and rewards transparency and early error reporting [79].
By adopting the proactive protocols and tools outlined in this guide, researchers and drug development professionals can move beyond a state of inspection readiness to one of inherent control. This not only satisfies regulatory expectations but also produces the highest quality data—the undeniable foundation for safe, effective, and innovative medicines.
Contemporary Standards and Comparative Analysis: ICH Q2(R2) and the Path Forward
The International Council for Harmonisation (ICH) has ushered in a new era for pharmaceutical analytical science with the simultaneous introduction of ICH Q2(R2) on the validation of analytical procedures and ICH Q14 on analytical procedure development. This revised framework represents a fundamental shift from a discrete, checklist-based approach to an integrated, lifecycle management philosophy for analytical procedures. The development of these guidelines was a coordinated effort, with ICH Q2(R2) providing a general framework for validation principles and ICH Q14 offering harmonized guidance on scientific approaches for development [84]. Together, they create a cohesive system that encourages science-based and risk-based decision-making, aiming to enhance the robustness of analytical methods and facilitate more efficient post-approval change management [84] [85].
The impetus for this modernization stems from the need to accommodate advancing analytical technologies and to align with broader quality paradigms established in other ICH guidelines. The original ICH Q2(R1) guideline, established in 2005, required revision to include more recent applications of analytical procedures, such as the use of spectroscopic or spectrometry data (e.g., NIR, Raman, NMR, MS) which often require multivariate statistical analyses [86]. This revision directly addresses the evolution in analytical technology that has occurred since the previous guideline was implemented, creating a framework that is fit-for-purpose for both traditional and modern analytical techniques.
Historical Context: The Trajectory of Analytical Validation
The journey toward the current harmonized position began over three decades ago. The initial ICH Q2A guideline on validation of analytical procedures was approved in 1994, focusing on definitions and terminology [86]. This was followed by ICH Q2B in 1996, which concentrated on methodology [86]. These two documents were merged in 2005 to create ICH Q2(R1), which stood as the primary standard for nearly two decades until the recent comprehensive revision [86].
Throughout this period, the philosophy surrounding analytical method validation progressively evolved. Initially, method validation was primarily devoted to establishing a common vocabulary specific to chemical measurement [43]. The focus then shifted toward defining detailed validation procedures for methods, which was particularly challenging as analysts simultaneously confronted rapid technological changes in analytical instrumentation and data processing capabilities [43]. The emergence of Measurement Uncertainty (MU) and Total Analytical Error (TAE) concepts further refined expectations, moving the field toward a greater consideration of end-user requirements, who are ultimately concerned with the quality of the result rather than merely the quality of the method [43].
Table: Historical Evolution of ICH Q2 Guidelines
| Date | Guideline Code | Key Development |
|---|---|---|
| October 1994 | Q2A | Initial approval focusing on definitions and terminology |
| November 1996 | Q2B | Approval focusing on methodology |
| November 2005 | Q2(R1) | Merging of Q2A and Q2B into a single document |
| November 2023 | Q2(R2) | Comprehensive revision to include modern analytical techniques and align with Q14 |
Core Principles of the Modernized Framework
The Lifecycle Approach to Analytical Procedures
A cornerstone of the modernized framework is the application of a lifecycle approach to analytical procedures, mirroring the lifecycle concepts applied to pharmaceutical products. ICH Q14 formally defines this lifecycle, which encompasses three key stages: Procedure Design, Procedure Performance Qualification (PPQ), and Continued Procedure Performance Verification (CPV) [87]. This systematic approach ensures that analytical procedures remain fit-for-purpose throughout their entire operational lifespan, from initial development through routine use and eventual retirement or modification.
The Procedure Design stage involves structured development activities to create a robust method. The PPQ stage demonstrates that the procedure, as designed, performs reliably for its intended purpose in its operational environment—this aligns with the traditional validation study but with greater emphasis on leveraging knowledge from development. The CPV stage involves ongoing monitoring to ensure the procedure continues to perform as expected during routine use, enabling proactive management rather than reactive responses [87]. This lifecycle management is further supported by appropriate change management processes, ensuring that any modifications to analytical procedures are scientifically justified and properly documented [87].
The Analytical Target Profile (ATP)
A pivotal concept introduced in ICH Q14 is the Analytical Target Profile (ATP), which serves as the foundation for analytical procedure development [87]. The ATP is a predefined objective that specifies the requirements for the analytical procedure—essentially, what the procedure needs to achieve, rather than how it should be achieved. It defines the intended purpose of the procedure by specifying the attribute(s) to be measured, the required performance characteristics, and the corresponding acceptance criteria for these characteristics over the reportable range [87].
The ATP acts as a guiding document throughout the analytical procedure lifecycle. During development, it informs technology selection and optimization strategies. During validation, it provides the acceptance criteria for demonstrating the procedure is fit-for-purpose. During routine use, it serves as a reference for method performance monitoring and any future improvements [87]. By defining what constitutes success at the outset, the ATP facilitates science-based and risk-based decision-making and provides a clear basis for justifying the control strategy.
Knowledge Management and Risk Assessment
The modernized framework explicitly emphasizes the importance of knowledge management throughout the analytical procedure lifecycle. This involves systematically gathering and applying knowledge from both internal sources (such as a company's prior experience with similar methods) and external sources (including scientific publications and established scientific principles) [87]. This accumulated knowledge provides the scientific foundation for making informed decisions during development, validation, and lifecycle management.
Complementing knowledge management, the framework encourages the application of formal quality risk management principles, consistent with ICH Q9, to minimize the risk of analytical procedure performance issues [87]. Risk assessment tools are used to identify and prioritize method variables that may affect performance, directing resources toward understanding and controlling the most critical factors. This risk-based approach ensures that development and validation activities are focused appropriately, enhancing efficiency while maintaining rigorous quality standards.
Key Changes in ICH Q2(R2): From Linearity to Reportable Range
The revised ICH Q2(R2) guideline introduces several significant changes that reflect the evolution in analytical science and align with the principles outlined in ICH Q14. One of the most notable conceptual shifts is the move from the traditional "Linearity" characteristic to "Working Range" and "Reportable Range" [86]. This change acknowledges that not all analytical procedures, particularly those based on biological systems or multivariate models, demonstrate a linear response. The reportable range represents the interval between the upper and lower levels of analyte that have been demonstrated to be determined with suitable precision and accuracy, while the working range refers to the specific range within which the procedure operates as described by the calibration model [86].
Other important updates in ICH Q2(R2) include greater flexibility in leveraging development data for validation purposes. The guideline explicitly states that suitable data derived from development studies (as described in ICH Q14) can be used as part of validation data, reducing unnecessary duplication of studies [86]. Additionally, when an established platform analytical procedure is used for a new purpose, reduced validation testing is permitted when scientifically justified [86]. This represents a more efficient, pragmatic approach to validation that recognizes when extensive re-validation may not be necessary.
Table: Comparison of Key Validation Terminology Between ICH Q2(R1) and Q2(R2)
| ICH Q2(R1) Terminology | ICH Q2(R2) Terminology | Key Changes |
|---|---|---|
| Linearity | Working Range and Reportable Range | Accommodates non-linear analytical procedures and biological assays |
| Discrete Validation | Lifecycle Approach with Development Data Integration | Suitable data from development (per Q14) can be used in validation |
| Full Revalidation Often Required | Reduced Validation for Platform Procedures | Permits reduced testing for established platform methods with scientific justification |
| - | Enhanced Consideration of Multivariate Methods | Explicitly includes validation principles for spectroscopic and multivariate analyses |
Analytical Procedure Lifecycle Flow
Analytical Procedure Development Under ICH Q14
Minimal vs. Enhanced Approaches
ICH Q14 outlines two complementary approaches to analytical procedure development: the minimal approach and the enhanced approach [87]. The minimal approach represents a traditional, direct development path that emphasizes establishing a simple, robust, and well-defined analytical procedure suitable for its intended purpose without excessive optimization. This approach still requires demonstrating method suitability through evaluation of parameters such as specificity, linearity, accuracy, precision, and detection limits, but it typically involves less extensive systematic optimization studies [87].
In contrast, the enhanced approach represents a more systematic methodology that employs statistical tools and Design of Experiments (DoE) principles to optimize and understand the method's critical parameters more comprehensively [87]. This approach aligns with Quality by Design (QbD) principles, involving a thorough risk assessment to identify and prioritize method variables that affect performance, followed by structured experimental designs to establish a method operable design region [87]. The enhanced approach considers the entire lifecycle of the analytical method from the outset, facilitating continuous monitoring and improvement.
Robustness Evaluation and Parameter Ranges
A critical aspect of analytical procedure development under ICH Q14 is the formal evaluation of robustness and establishment of parameter ranges [87]. Robustness evaluation assesses the procedure's ability to remain unaffected by small, deliberate variations in method parameters, demonstrating reliability during normal usage. ICH Q14 recommends that robustness be tested through deliberate variations of analytical procedure parameters, with prior knowledge and risk assessment informing the selection of which parameters to investigate [87].
Parameter ranges can be established through either univariate experiments (testing one factor at a time) or multivariate experiments (which can identify interactions between parameters) [87]. The guideline notes that categorical variables, such as different instruments or columns, can also be considered part of the experimental design. Once established, these parameter ranges typically become part of the analytical procedure's control strategy and are usually subject to regulatory approval [87].
Analytical Procedure Control Strategy
ICH Q14 emphasizes establishing an analytical procedure control strategy to ensure the procedure is performed consistently and reliably during routine use [87]. This strategy includes defined analytical procedure parameters to control, along with appropriate system suitability tests (SST) to verify the system's performance at the time of analysis. In some cases, sample suitability assessments may also be necessary to ensure the procedure is appropriate for specific sample types [87].
Consistent with ICH Q12 principles, applicants may define Established Conditions (ECs) for an analytical procedure [87]. These are the legally binding elements that must be maintained within the approved state to ensure product quality. For analytical procedures, ECs may focus on performance criteria, analytical principles, and parameter ranges rather than fixed operational parameters, providing greater flexibility for continuous improvement within the approved design space [87].
Implementation Strategies and Industry Impact
Practical Implementation Roadmap
Successful implementation of the modernized ICH Q2(R2) and Q14 framework requires a systematic approach. Companies should begin with an assessment of current analytical procedures, methods, and validation processes to identify gaps and areas where the new principles can be applied [87]. For each analytical procedure, defining an Analytical Target Profile (ATP) is a critical first step, as this establishes the foundation for all subsequent development and validation activities [87].
Organizations should then adopt QbD principles for method development, including risk assessment, design of experiments, and identification of critical method attributes [87]. Method validation should be planned and executed according to ICH Q2(R2), leveraging knowledge and data from the development phase to the greatest extent possible. Finally, implementing a Continued Procedure Performance Verification (CPV) plan ensures ongoing monitoring of analytical procedure performance throughout its operational life, enabling proactive management and continuous improvement [87].
Impact on Regulatory Submissions and Post-Approval Changes
The modernized framework is intended to improve regulatory communication between industry and regulators and facilitate more efficient, science-based approval processes [86]. A significant benefit is the potential for more flexible post-approval change management of analytical procedures when changes are scientifically justified [84]. By providing a more structured approach to understanding analytical procedures, the framework enables better risk assessment of proposed changes, potentially leading to more predictable regulatory outcomes and reduced reporting categories for lower-risk changes [87].
When transferring methods between laboratories or sites, the new guidelines recommend conducting a risk assessment to determine the extent of revalidation required, rather than automatically requiring full revalidation [87]. For cross-validation situations where two or more bioanalytical methods are used to generate data within the same study, a comparison approach is recommended to establish interlaboratory reliability [66].
Table: Essential Research Reagents and Solutions for Analytical Procedure Development
| Reagent/Solution | Function/Purpose | Key Considerations |
|---|---|---|
| Reference Standards | To ensure accuracy and reliability of analytical measurements | Proper characterization and qualification are essential; may include primary and working standards |
| System Suitability Test Solutions | To verify chromatographic system performance at time of use | Typically prepared from reference standards; should test critical parameters (e.g., resolution, precision) |
| Forced Degradation Samples | To establish specificity and stability-indicating capabilities | Includes samples treated under various stress conditions (heat, light, acid, base, oxidation) |
| Placebo/Blank Matrix | To demonstrate absence of interference from non-active components | Should represent all formulation components except active ingredient(s) |
| Quality Control (QC) Samples | To monitor method performance during validation and routine use | Prepared at multiple concentrations covering the reportable range |
The simultaneous implementation of ICH Q2(R2) and ICH Q14 represents a transformative shift in the pharmaceutical industry's approach to analytical procedures. By integrating development and validation into a cohesive lifecycle management system, the framework promotes deeper scientific understanding, more robust procedures, and more efficient regulatory processes. The emphasis on Analytical Target Profiles, risk-based approaches, and knowledge management aligns analytical science with modern pharmaceutical quality systems, facilitating continuous improvement and innovation.
As the industry adopts this modernized framework, benefits are expected to include enhanced method development, improved method validation, greater resource efficiency, and strengthened data integrity [87]. Most importantly, by ensuring that analytical procedures are consistently fit-for-purpose throughout their lifecycle, these guidelines ultimately contribute to the reliable assessment of drug product quality, supporting the availability of safe and effective medicines to patients worldwide. The adoption of these guidelines marks not an endpoint, but rather the beginning of a new chapter in analytical science—one characterized by greater scientific rigor, regulatory flexibility, and a commitment to quality that spans the entire product lifecycle.
The pharmaceutical industry is undergoing a fundamental transformation in how it conceptualizes and implements validation. This shift moves the discipline from a static, document-centric activity to a dynamic, data-driven lifecycle process [88]. The traditional validation model, often characterized as a one-time "compliance theater," is being challenged by enhanced approaches that embed quality throughout the entire product lifecycle [89]. This evolution is driven by the convergence of regulatory guidance, such as the FDA's 2011 Process Validation guidance and the ICH Q2(R2) and Q14 framework, and the advent of Industry 4.0 technologies [88] [90]. This paper provides a comparative analysis of these two paradigms, examining their core principles, methodologies, and impacts on efficiency and compliance within the context of modern drug development. The transition represents more than a technical update; it is a strategic imperative for organizations aiming to thrive in an increasingly complex regulatory and technological landscape, fostering a culture of continuous improvement and proactive quality assurance [88].
Historical Context and the Drivers for Change
The Traditional Validation Framework
For decades, pharmaceutical validation was dominated by a traditional framework rooted in the 1987 FDA process validation guide. This approach treated validation as a discrete event, primarily focused on generating documented evidence that a process could reproducibly yield a product meeting its predetermined specifications [90]. The core activity often involved executing three consecutive validation batches, which became an unwritten "industry norm" [90]. This model was inherently reactive, with compliance verification typically occurring after processes were finalized, often leading to bottlenecks, delays, and increased costs if issues were identified [88]. The mindset was to "lock down the process," with the emphasis on qualification documentation rather than a deep understanding of the underlying process science and variability [90].
The Impetus for an Enhanced Approach
The limitations of the traditional model became increasingly apparent, prompting a fundamental rethinking. Key drivers for change include:
- Regulatory Evolution: The 2011 FDA Guidance for Industry: Process Validation: General Principles and Practices marked a pivotal turn, introducing a formal lifecycle model integrating process design, qualification, and verification [90]. This was further reinforced by ICH guidelines Q8 (Pharmaceutical Development), Q9 (Quality Risk Management), and Q10 (Pharmaceutical Quality System), which together emphasize building quality in through scientific understanding and risk management [90].
- Technological Advancement: The rise of Pharma 4.0 has enabled enhanced validation. Technologies such as Artificial Intelligence (AI), the Internet of Things (IoT), and cloud computing facilitate real-time data analytics and continuous monitoring, which are foundational to the lifecycle approach [88].
- Operational Efficiency Demands: The traditional model's inefficiencies, including its time-consuming, document-heavy nature, became a significant barrier to innovation and speed-to-market. Industry leaders recognized that validation could be a value-added activity rather than just a cost [90].
Core Principles and Methodologies
Traditional Validation Approach
The traditional approach is characterized by its static and sequential nature. Its principles include:
- Document-Centricity: The primary artifacts are paper or static electronic documents (e.g., PDFs), with manual version control and change management [88] [91].
- Fixed Point Verification: Validation is essentially a one-time activity conducted during process qualification, with the infamous "three validation batches" serving as the primary evidence of validation [90].
- Reactive Compliance: The system is designed to prove compliance at specific points, often leading to a "firefighting" culture when deviations occur [91].
Enhanced Lifecycle Validation Approach
In stark contrast, the enhanced approach, as outlined in modern regulatory guidance, is built on the principle of continuous assurance [89]. The core principles include:
- Lifecycle Management: Validation is viewed as a continuous process encompassing all stages from initial process design through commercial manufacturing. ICH Q14 and USP <1220> formalize this as the "Analytical Procedure Lifecycle" [89].
- Risk-Based Approach: Efforts and resources are focused on critical aspects that impact product quality, using formal risk assessment tools [90].
- Data-Centricity: The model shifts from documents to structured data objects. This enables real-time traceability, automated compliance, and sophisticated analysis [91].
- Proactive and Adaptive Control: The goal is to build systems that are "always-ready" for audits through continuous monitoring and self-correcting workflows, fostering a culture of continuous improvement [91].
The following workflow diagram illustrates the fundamental differences in the stages and feedback mechanisms between the two validation approaches.
Comparative Analysis: Key Dimensions
The differences between the traditional and enhanced lifecycle approaches manifest across several critical dimensions, from their core philosophy to their operational execution and technological needs.
Table 1: Comprehensive Comparison of Validation Approaches
| Dimension | Traditional Validation | Enhanced Lifecycle Validation |
|---|---|---|
| Core Philosophy | Static, one-time event to prove compliance [89] | Dynamic, continuous process to ensure ongoing control [89] |
| Compliance Focus | Reactive (post-process verification) [88] | Proactive (real-time monitoring & adaptation) [88] [15] |
| Primary Documentation | Paper-based or static PDFs (Document-Centric) [91] | Structured data objects (Data-Centric) [91] |
| Data Utilization | Limited, for retrospective reporting | Real-time analytics for predictive decision-making [15] |
| Role of Technology | Manual processes, limited automation | Integrated digital tools, AI/ML, IoT, automation [88] [92] |
| Validation Scope | Fixed process parameters | Defined design space with understanding of parameter interactions [90] |
| Change Management | Rigid, often avoided due to revalidation burden [90] | Agile, facilitated by risk-based approaches and continuous data [92] |
| Resource Emphasis | Extensive manual documentation effort | Investment in digital infrastructure and skilled data analysts [88] |
| Cost Profile | High long-term costs due to deviations and rework [88] | Higher initial investment, lower long-term cost of quality [88] |
Quantitative Benefits and Industry Adoption
The adoption of enhanced lifecycle approaches and digital tools is yielding measurable benefits, driving a sector-wide transformation.
Table 2: Quantitative Benefits and 2025 Adoption Metrics of Enhanced Validation
| Metric | 2025 Status & Impact |
|---|---|
| Digital Validation Tool Adoption | 58% of organizations now use these tools, a 28% increase from 2024 [93]. 93% of firms either use or plan to adopt them [93]. |
| Reported ROI | 63% of early adopters meet or exceed ROI expectations [93]. |
| Efficiency Gains | Digital tools can achieve 50% faster cycle times and reduced deviations [93]. |
| AI Adoption | 57% of professionals believe AI/ML will become integral to validation [92]. |
| Primary Challenge | Audit readiness has overtaken compliance burden as the industry's top challenge [93]. |
Implementation and Operationalization
The Enhanced Validation Lifecycle in Practice
The enhanced lifecycle approach, as defined by modern regulatory guidance, is operationalized through three interconnected stages:
- Stage 1: Process Design: This stage focuses on building a robust understanding of the process. Using risk assessment tools like FMEA and experimental designs like DOE, developers identify Critical Quality Attributes (CQAs) and the Critical Process Parameters (CPPs) that affect them. The goal is to establish a predictive model and a control strategy that ensures quality is built in from the outset [90] [94].
- Stage 2: Process Qualification: This stage confirms that the process design, when implemented in the commercial manufacturing facility, is capable of reproducible commercial manufacturing. It involves both equipment qualification (IQ/OQ/PQ) and process performance qualification (PPQ). Unlike the traditional three-batch approach, the scope and number of batches in a PPQ are determined by statistical rationale and process understanding gained in Stage 1 [90] [95].
- Stage 3: Continued Process Verification (CPV): This is the most dynamic stage, ensuring the process remains in a state of control throughout its commercial life. CPV involves continuous monitoring of CPPs and CQAs using Statistical Process Control (SPC) tools. Data from manufacturing is continuously collected and analyzed to detect trends, identify process drift, and trigger corrective actions before they lead to a deviation [15] [95].
The Scientist's Toolkit: Essential Components for Lifecycle Validation
Implementing a successful lifecycle validation strategy requires a suite of methodological, technological, and regulatory tools.
Table 3: Essential Research and Validation Tools
| Tool Category | Specific Tool/Technology | Function & Role in Lifecycle Validation |
|---|---|---|
| Risk Management | FMEA (Failure Mode and Effects Analysis) | Systematically identifies potential process failures and prioritizes risks to product quality [94]. |
| Experimental Design | DOE (Design of Experiments) | Efficiently explores the relationship between multiple process parameters and quality attributes to define a design space [94]. |
| Statistical Analysis | SPC (Statistical Process Control) Charts | Monitors process performance in real-time (Stage 3 CPV) to detect trends and signals of process variation [95] [94]. |
| Process Monitoring | PAT (Process Analytical Technology) | Enables real-time, in-line monitoring of critical quality attributes during manufacturing for immediate control [90]. |
| Data Management | LIMS (Laboratory Information Management System) | Centralizes and manages analytical data, ensuring data integrity and supporting trend analysis [95]. |
| Digital Execution | Digital Validation Platforms | Replaces paper protocols with automated, data-centric systems for executing studies, managing deviations, and ensuring audit readiness [93] [92]. |
| Knowledge Management | Analytical Target Profile (ATP) | A predefined objective that specifies the required quality of reportable analytical results, guiding method development and validation [89]. |
Conceptual Framework for a Data-Centric Validation Platform
A key enabler of the enhanced lifecycle approach is the transition from document-centric to data-centric systems. The following diagram outlines the architecture of a unified data layer that supports this modern paradigm.
Challenges and Future Directions
Implementation Hurdles
Despite its clear advantages, the transition to an enhanced lifecycle model presents significant challenges:
- Cultural and Organizational Resistance: Shifting from a familiar, document-centric mindset to a dynamic, data-driven one requires effective change management. Resistance from staff accustomed to traditional methods is a major hurdle [88].
- Initial Investment and Resource Constraints: Transitioning requires substantial upfront investment in new technologies (digital platforms, PAT tools) and training for personnel [88]. This is compounded by workload increases and lean teams, with 39% of companies reporting fewer than three dedicated validation staff [93].
- Technical and Knowledge Gaps: Implementing concepts like combined accuracy-precision evaluation and managing a unified data layer require sophisticated statistical and data science expertise that may not be present in traditional analytical laboratories [89].
Emerging Trends and the Future Landscape
The evolution of validation is continuing, shaped by several key trends:
- Artificial Intelligence and Machine Learning: AI and ML are poised to transform validation through predictive modeling, automated protocol generation, and enhanced risk assessment, though adoption is still in early stages [92].
- Remote and Virtual Validation: The rise of remote regulatory assessments (RRAs) is accelerating the adoption of remote and virtual validation tools, including augmented reality (AR) and digital collaboration platforms [92].
- Continuous Validation: The industry is moving towards a model of "continuous validation," where validation is seamlessly integrated throughout the product lifecycle, allowing for real-time updates in response to process or regulatory changes [92].
- Advanced Statistics and the "Reportable Result": The revised USP <1225> introduces a sharper focus on the "reportable result," forcing a more holistic view of method performance and encouraging the use of statistical intervals that combine accuracy and precision for a more scientifically rigorous assessment [89].
The comparative analysis reveals that the enhanced lifecycle approach to validation represents a fundamental and necessary evolution from the traditional model. The transition from a static, document-centric exercise to a dynamic, data-driven lifecycle management system is crucial for modern pharmaceutical development and manufacturing. While the traditional approach provided a simple and established framework, its reactive and inefficient nature is ill-suited to the demands of today's complex regulatory and competitive environment [88].
The enhanced lifecycle paradigm, enabled by digital transformation and aligned with modern regulatory guidance, offers significant advantages: it enhances operational efficiency, fosters a proactive culture of quality, and provides a deeper, more scientific understanding of processes [88] [90]. This ultimately leads to more robust manufacturing processes, improved product quality, and greater patient safety. Although the implementation journey requires navigating challenges related to cost, change management, and skill development, the long-term benefits—including a reduced cost of quality and sustained regulatory compliance—make it a strategic imperative. For researchers, scientists, and drug development professionals, mastering and implementing these enhanced validation approaches is no longer optional but essential for driving innovation and achieving excellence in the pharmaceutical industry.
The pharmaceutical industry is undergoing a transformative shift, driven by an unprecedented wave of innovative therapeutic modalities and advanced instrumentation. As of 2025, new modalities—including monoclonal antibodies (mAbs), antibody-drug conjugates (ADCs), bispecific antibodies (BsAbs), cell and gene therapies, and nucleic acid-based treatments—now account for $197 billion, representing 60% of the total pharmaceutical pipeline value, a significant increase from 57% in 2024 [96]. This rapid evolution demands a parallel transformation in analytical method validation protocols to ensure these complex therapies meet rigorous safety, efficacy, and quality standards.
The framework for analytical method validation is itself evolving from a traditional, compliance-driven checklist approach to a holistic, lifecycle risk-based paradigm rooted in Analytical Quality by Design (AQbD) principles [18]. This shift, embodied in new and updated regulatory guidelines such as ICH Q14 on analytical procedure development and ICH Q2(R2) on validation, emphasizes deep scientific understanding, risk management, and continuous verification over the entire lifespan of an analytical procedure [4] [18]. Simultaneously, technological breakthroughs in instrumentation—from high-resolution mass spectrometry (HRMS) and nuclear magnetic resonance (NMR) to artificial intelligence (AI)-driven analytics and Process Analytical Technologies (PAT)—are creating new possibilities and challenges for characterization and quality control [4]. This technical guide explores the strategies, methodologies, and practical protocols for successfully validating methods in this dynamic environment, ensuring that innovation in therapeutics is matched by excellence in analytical science.
The Modern Regulatory and Quality Framework
The regulatory landscape for analytical method validation is increasingly defined by a lifecycle approach and the formal integration of Quality by Design (QbD) principles. This represents a significant paradigm shift from the traditional "fixed-point" validation model, which focused primarily on verifying performance at a single point in time, towards a holistic system that ensures a method remains fit-for-purpose throughout its entire use [18].
Key Regulatory Guidelines and Standards
The following guidelines form the cornerstone of the modern validation framework:
- ICH Q2(R2): Validation of Analytical Procedures: This revised guideline provides an updated framework for method validation, placing greater emphasis on a science- and risk-based approach that aligns with the product lifecycle [4] [18].
- ICH Q14: Analytical Procedure Development: A companion to Q2(R2), this new guideline explicitly outlines a systematic approach for analytical procedure development, encouraging the use of AQbD principles, risk assessment, and enhanced control strategies [4] [18].
- USP General Chapter <1220>: Analytical Procedure Life Cycle: This chapter formalizes the lifecycle concept, structuring it into three stages: Procedure Design, Procedure Performance Qualification, and Ongoing Procedure Performance Verification (OPPV). It underscores the importance of establishing an Analytical Target Profile (ATP) as the foundational document defining the method's required performance [18].
- USP General Chapter <1058>: Analytical Instrument and System Qualification (AISQ): The updated draft version introduces a modernized, integrated lifecycle model for ensuring instrument fitness for purpose, mirroring the APLC approach. It emphasizes a three-phase process: Specification and Selection, Installation, Qualification, and Validation, and Ongoing Performance Verification (OPV) [97].
Analytical Quality by Design (AQbD) in Practice
AQbD is the practical application of QbD principles to analytical methods. Its implementation ensures that quality is built into the method from the outset, rather than merely tested at the end.
- Analytical Target Profile (ATP): The ATP is a predefined quantitative summary of the required quality of the reportable result. It specifies the performance requirements the method must meet throughout its lifecycle (e.g., precision, accuracy, range) based on its intended use [18].
- Risk Assessment and Control Strategy: AQbD employs systematic risk assessment tools (e.g., Ishikawa diagrams, FMEA) to identify and prioritize variables that can impact method performance. This knowledge is then used to establish a control strategy, which may include Method Operational Design Ranges (MODRs) for key parameters, ensuring robustness under normal operational variation [4].
- Design of Experiments (DoE): DoE is a critical statistical tool within AQbD. It uses structured experiments to efficiently model the relationship between method input parameters (e.g., pH, temperature, mobile phase composition) and output responses (e.g., resolution, peak asymmetry). This model is used to define the method's design space, providing a scientific basis for establishing the MODR [4].
Table 1: Core Principles of the Modern Analytical Procedure Lifecycle (APLC)
| Lifecycle Stage | Core Objective | Key Activities & Deliverables |
|---|---|---|
| Stage 1: Procedure Design | To design a method that is fit for its intended purpose based on sound science. | - Define the Analytical Target Profile (ATP).- Conduct risk assessment to identify Critical Method Parameters (CMPs).- Use DoE to optimize parameters and establish a Method Operational Design Range (MODR). |
| Stage 2: Procedure Performance Qualification | To verify that the method, as designed, performs as intended in the actual environment of use. | - Execute the validation protocol (specificity, accuracy, precision, etc.) as per ICH Q2(R2).- Document evidence that the method meets the ATP criteria. |
| Stage 3: Ongoing Procedure Performance Verification | To ensure the method remains in a state of control throughout its operational life. | - Continuous monitoring of system suitability and control charting.- Manage changes through a formal change control process.- Periodically review method performance against the ATP. |
Validation Challenges Posed by Novel Modalities
The rise of complex biologics and advanced therapies introduces unique analytical challenges that strain the capabilities of conventional methods. These modalities are often larger, more heterogeneous, and function through complex mechanisms, necessitating a new generation of analytical techniques and validation strategies.
Specific Challenges by Modality
- Cell and Gene Therapies: These products present immense challenges related to their biological complexity and living nature. For CAR-T therapies, critical quality attributes (CQAs) include potency, transduction efficiency, phenotypic characterization, and cytokine secretion profile. Gene therapies require methods to assess vector titer, identity, purity, and genomic integrity. The validation of bioassays (e.g., qPCR, flow cytometry, potency assays) is particularly challenging due to their inherent higher variability [96] [4]. Recent safety incidents, such as the temporary pause of a gene therapy shipment in 2025 due to safety concerns, highlight the critical need for robust, validated analytical methods for these potent products [96].
- Nucleic Acid Therapies (DNA, RNA, RNAi): This category, one of the fastest-growing with a 65% year-over-year increase in projected revenue, includes antisense oligonucleotides and RNAi therapies [96]. Key challenges include characterizing and quantifying the full-length product versus related shorter fragments (degradation products), and accurately measuring drug substance and drug product purity. Techniques like LC-MS/MS and capillary electrophoresis are essential, and their validation must account for the unique chemical properties of these molecules [4].
- Complex Biologics (mAbs, ADCs, BsAbs): While more established, these modalities continue to push analytical boundaries. Antibody-Drug Conjugates (ADCs) require validation of methods to determine drug-to-antibody ratio (DAR), distribution of conjugated species, and the presence of unconjugated payload and linker. Bispecific Antibodies (BsAbs) necessitate assays to confirm correct assembly and functionality of both binding arms [96]. The industry is increasingly adopting Multi-Attribute Methods (MAM) using LC-MS, which can monitor multiple CQAs (e.g., oxidation, deamidation, glycosylation) simultaneously in a single assay, fundamentally changing the validation paradigm [4].
Table 2: Analytical Techniques and Validation Considerations for Novel Modalities
| Therapeutic Modality | Common Analytical Techniques | Key Validation Considerations Beyond Standard Parameters |
|---|---|---|
| Cell Therapies (e.g., CAR-T) | Flow Cytometry, qPCR, Potency Bioassays, Viability Assays | - High inter-assay variability requires wider precision acceptance criteria.- Demonstrating assay specificity in a complex biological matrix.- Ensuring sample stability is representative of the live product. |
| Gene Therapies (e.g., AAV Vectors) | ddPCR/qPCR (titer), CE/SEC (purity & empty/full capsid), TCID50 (potency), NGS (identity) | - Validation of reference standards for absolute quantification.- Specificity for the transgene in the presence of host cell DNA.- Accuracy and linearity for a wide range of concentrations. |
| Antibody-Drug Conjugates (ADCs) | HIC-HPLC (DAR), LC-MS (peptide mapping), HRMS (intact mass) | - Demonstrating robustness for methods separating multiple DAR species.- Validation of forced degradation studies to show stability-indicating power.- Specificity for quantifying unconjugated payload and linker. |
| Oligonucleotides | IP-RP-UHPLC, LC-MS/MS, CE | - Specificity for resolving the product from related impurities (n-X sequences).- Accuracy in the presence of a complex mixture of failure sequences.- Demonstration of column longevity due to harsh mobile phases. |
Advanced Instrumentation and Qualification Strategies
The technological backbone of modern analytical laboratories is evolving rapidly, enabling the characterization of novel modalities but also demanding more sophisticated instrument qualification approaches.
Emerging Analytical Technologies
- Next-Generation Instrumentation: Techniques like High-Resolution Mass Spectrometry (HRMS) and multi-dimensional Ultra-High-Performance Liquid Chromatography (UHPLC) provide the sensitivity, resolution, and throughput required to deconvolute the complexity of new modalities. These instruments are central to implementing MAM and for detailed characterization of biosimilars and novel entities [4].
- Hyphenated Techniques: The combination of separation techniques with powerful detectors, such as LC-MS/MS and GC-MS, has become routine for quantifying drugs and metabolites in complex matrices. The validation of these integrated systems must consider the performance of both the separation and detection components as a unified whole [4].
- Process Analytical Technology (PAT) and Real-Time Release Testing (RTRT): A major trend for 2025 is the shift towards RTRT, which uses in-line, on-line, or at-line PAT (e.g., in-line spectroscopy) to monitor CQAs during manufacturing. This allows for the release of products based on process data rather than end-product testing, significantly reducing cycle times. Validating PAT methods requires a focus on their accuracy, precision, and robustness in a non-laboratory, industrial environment [4].
- Automation and AI: Laboratory automation and robotics are being deployed to eliminate human error and increase throughput. Furthermore, Artificial Intelligence (AI) and machine learning algorithms are being used to optimize method parameters, predict equipment maintenance needs, and assist in interpreting complex, multi-dimensional data from techniques like HRMS [4].
Enhanced Instrument Qualification: USP <1058> Update
The qualification of these advanced systems is guided by the enhanced framework outlined in the draft update to USP <1058>, now titled "Analytical Instrument and System Qualification (AISQ)" [97].
The updated chapter introduces a three-phase integrated lifecycle model that aligns with the APLC and modern process validation guidance:
- Phase 1: Specification and Selection: This begins with a comprehensive User Requirements Specification (URS) that defines the instrument's intended use, including operating parameters and acceptance criteria traceable to national or international standards. A risk-based assessment is conducted to determine the appropriate qualification level [97].
- Phase 2: Installation, Qualification, and Validation: This phase involves installation, commissioning, and executing qualification protocols (IQ/OQ/PQ). For complex Group C systems (e.g., a computerized LC-MS system), this includes integrated testing and software validation to ensure all components work together to meet the URS [97].
- Phase 3: Ongoing Performance Verification (OPV): This critical phase ensures the instrument continues to be "fit for intended use" throughout its operational life. It includes periodic testing, calibration, maintenance, change control, and a review of performance data against the baseline established in the URS [97].
Diagram 1: USP <1058> Instrument Qualification Lifecycle
Experimental Protocols for Advanced Method Validation
This section provides detailed methodologies for key experiments commonly required when validating methods for novel modalities.
Protocol: Validation of a UHPLC-UV Method for Oligonucleotide Purity
This protocol outlines the key experiments for validating a method to separate and quantify a synthetic oligonucleotide from its related impurities (e.g., n-1, n-2 sequences).
- 1. Objective: To validate a UHPLC-UV method for the determination of purity and related substances of a therapeutic oligonucleotide according to ICH Q2(R2) principles.
- 2. Experimental Procedure:
- Apparatus: UHPLC system with UV detector, thermostatted column compartment, and auto-sampler. Column: C18, 2.1 x 100 mm, 1.7 µm.
- Mobile Phase: A) 100 mM Hexafluoroisopropanol (HFIP), 16.3 mM Triethylamine (TEA) in water; B) Methanol.
- Gradient: 5% B to 25% B over 25 minutes.
- Detection: UV at 260 nm.
- 3. Validation Parameters & Acceptance Criteria:
Table 3: Validation Protocol for an Oligonucleotide Purity Method
| Validation Parameter | Experimental Design | Acceptance Criteria |
|---|---|---|
| Specificity | Inject blank, placebo, standard, and stressed samples (heat, acid, base, oxidative conditions). | Baseline separation (Rs > 2.0) between the main peak and all critical impurity peaks. The method must be stability-indicating. |
| Linearity & Range | Prepare and analyze a minimum of 5 concentrations from 50% to 150% of the target assay concentration (e.g., 0.5-1.5 mg/mL). | Correlation coefficient (r) > 0.998. %y-intercept of the line ≤ 2.0%. |
| Accuracy (Spike Recovery) | Spike known quantities of impurity standards (n-1, n-2) into the drug substance at 50%, 100%, and 150% of the specification level. Analyze in triplicate. | Mean recovery for each impurity: 90-110%. |
| Precision (Repeatability) | Prepare and analyze six independent sample preparations at 100% concentration by a single analyst on the same day. | %RSD of the main peak area and purity result ≤ 2.0%. |
| Intermediate Precision | A second analyst repeats the repeatability study on a different day using a different UHPLC system and column lot. | The overall %RSD (combining both studies) for the main peak area and purity result ≤ 3.0%. No statistically significant difference (e.g., p > 0.05 by t-test) between the two sets of results. |
| Robustness | Deliberately vary key parameters (e.g., column temp. ±2°C, flow rate ±0.05 mL/min, gradient slope ±5%) using a Design of Experiments (DoE) approach. | The method meets system suitability criteria in all experimental conditions. No significant impact on CQAs (resolution, retention time). |
Protocol: Validation of a Cell-Based Potency Bioassay
This protocol describes the validation of a bioassay to measure the biological activity of a novel biologic, such as a CAR-T cell product or a cytokine.
- 1. Objective: To validate a cell-based reporter gene assay for determining the potency of a biologic drug, ensuring the method is suitable for lot release and stability studies.
- 2. Experimental Procedure:
- Cell Line: Engineered cell line expressing the relevant receptor and a luciferase reporter gene under the control of the signaling pathway activated by the drug.
- Assay Protocol: Seed cells in 96-well plates. On the following day, add a dilution series of the reference standard and test samples. Incubate for a predetermined time (e.g., 6 hours). Lyse cells and add luciferase substrate. Measure luminescence.
- Data Analysis: Fit the dose-response data (luminescence vs. log[concentration]) to a 4-parameter logistic (4PL) curve. Calculate the relative potency of the test sample compared to the reference standard.
- 3. Validation Parameters & Acceptance Criteria:
- Accuracy/Relative Potency: Report the mean relative potency of known potency samples (e.g., 80%, 100%, 120%). Acceptance: 80-120% of the known value.
- Precision (Repeatability & Intermediate Precision): %RSD of relative potencies from multiple runs should be ≤ 20% for a cell-based assay.
- Linearity & Range: Demonstrate that the assay provides a linear (or 4PL) response over a suitable range (e.g., 50-150% of the expected potency).
- Specificity: Show that the response is specific to the drug's mechanism by using relevant negative controls (e.g., a receptor-blocking antibody should inhibit the signal).
- System Suitability: Each run must include a standard curve that meets pre-defined criteria (e.g., R² > 0.95, EC50 within a specified range, maximum signal-to-background ratio > 10).
The Scientist's Toolkit: Essential Research Reagent Solutions
Successfully developing and validating methods for novel modalities requires a suite of specialized reagents, standards, and materials.
Table 4: Essential Research Reagent Solutions for Method Validation
| Tool / Reagent | Function / Application | Key Considerations for Validation |
|---|---|---|
| Well-Characterized Reference Standard | Serves as the primary benchmark for quantifying the analyte, determining potency, and qualifying impurities. | Must be thoroughly characterized for identity, purity, and strength. Stability under storage conditions must be established. |
| Impurity and Isoform Standards | Used to identify and quantify specific product-related impurities (e.g., aggregates, fragments, oxidized species, charge variants). | Requires independent confirmation of identity and purity. Used to demonstrate specificity and establish reporting/deletion thresholds. |
| Stable, Qualified Cell Lines | Essential for bioassays (potency, neutralizing antibody assays). Must consistently respond to the drug product. | Requires banking under cGMP-like conditions and extensive characterization (e.g., identity, purity, stability, passage number limits). |
| Critical Reagents (e.g., Antibodies, Enzymes, Ligands) | Used in ligand-binding assays (ELISA, SPR) and as detection reagents in various formats. | Must be qualified for specificity, affinity, and lot-to-lot consistency. A robust critical reagent management program is mandatory. |
| Synthetic Oligonucleotide Standards | Used for quantitative PCR assays for gene therapy vector titer and cell therapy transgene copy number. | Requires precise sequence confirmation and accurate concentration determination via UV-Vis with a calculated molar extinction coefficient. |
| Matrix Samples | The biological fluid (e.g., plasma, serum) in which the analyte is measured for pharmacokinetic studies. | For ligand-binding assays, demonstration of selectivity in samples from at least 10 individual donors is required to assess matrix effects. |
The successful navigation of the modern pharmaceutical landscape, characterized by its reliance on novel modalities and advanced instrumentation, is intrinsically linked to the adoption of next-generation analytical validation strategies. The industry-wide shift towards a lifecycle management approach, as championed by ICH Q14, Q2(R2), and USP <1220>, provides the necessary framework to ensure analytical methods are not only validated at a single point but remain scientifically sound, robust, and fit-for-purpose throughout the product's life. This requires a deep commitment to AQbD principles, a proactive stance on continuous verification, and a mastery of the sophisticated technologies that enable the characterization of these complex molecules.
As therapeutic innovation continues to accelerate—with cell and gene therapies, oligonucleotides, and multi-specific antibodies taking center stage—the role of the analytical scientist has never been more critical. By embracing the integrated strategies of enhanced regulatory science, risk-based qualification of advanced instruments, and robust experimental validation protocols, the industry can build the necessary foundation of quality and control. This foundation is paramount to fulfilling the promise of these groundbreaking therapies, ensuring they are not only innovative but also safe, efficacious, and reliably available to patients worldwide.
The paradigm of pharmaceutical quality assurance is undergoing a fundamental transformation, shifting from traditional discrete testing approaches toward integrated, data-driven monitoring systems. This evolution within analytical method validation protocols is characterized by the adoption of Continuous Process Verification (CPV) and Real-Time Release Testing (RTRT), which together represent a significant departure from historical quality control methodologies. Where traditional quality assurance relied heavily on end-product testing and retrospective statistical process control, modern frameworks emphasize continuous monitoring, process understanding, and proactive quality control throughout the manufacturing lifecycle [15] [98]. This shift is embedded within regulatory guidance from the FDA and EMA that advocates for a science- and risk-based approach to pharmaceutical manufacturing [99] [100].
The integration of CPV and RTRT represents more than a technical enhancement; it constitutes a philosophical realignment toward Quality by Design (QbD) principles that emphasize building quality into products rather than merely testing for it post-production [98]. This transformation has been facilitated by advancements in Process Analytical Technology (PAT) tools, sophisticated data analytics, and digital integration capabilities that enable unprecedented levels of process transparency and control [15] [98]. Within this context, this technical guide examines the implementation frameworks, methodological requirements, and practical applications of CPV and RTRT as foundational elements of modern pharmaceutical quality systems.
Theoretical Foundations: CPV and RTRT in the Validation Lifecycle
Continuous Process Verification (CPV)
CPV represents the third stage of the FDA's process validation lifecycle model, defined as "ongoing monitoring and evaluation of process performance indicators to ensure the process remains in a state of control during routine production" [99]. Unlike traditional validation approaches that primarily verified process consistency during initial qualification runs, CPV establishes a continuous feedback loop that monitors both Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs) throughout the commercial manufacturing lifecycle [15].
The operational methodology of CPV is characterized by two pillars: (1) ongoing monitoring through continuous collection and statistical analysis of process data, and (2) adaptive control through adjustments informed by risk-based insights [99]. This approach enables manufacturers to detect process deviations in real-time, understand their impact on product quality, and implement corrective actions before product quality is compromised. The implementation of CPV requires a foundation of process understanding developed during Stage 1 (Process Design) and statistical baselines established during Stage 2 (Process Qualification) of the validation lifecycle [99].
Real-Time Release Testing (RTRT)
RTRT is defined as "the ability to evaluate and ensure the quality of in-process and/or final product based on process data, which typically includes a valid combination of measured material attributes and process controls" [101] [100]. This approach allows for the parametric release of pharmaceutical products without requiring extensive end-product testing, provided that the manufacturing process demonstrates consistent control and the RTRT methodology has been adequately validated [100].
Regulatorily, RTRT requires pre-authorization by competent authorities and must be supported by substantial comparative data through parallel testing of production batches during method validation [100]. The European Medicines Agency emphasizes that even with RTRT authorization, manufacturers must establish formal product specifications, and each batch must demonstrate compliance with these specifications "if tested" [100]. RTRT typically comprises a combination of process controls utilizing PAT instruments, with common technologies including NIR spectroscopy and Raman spectroscopy for material characterization and quality attribute measurement [100].
Interrelationship Between CPV and RTRT
CPV and RTRT function as complementary elements within an advanced pharmaceutical quality system. While CPV provides the monitoring framework that ensures process control throughout the product lifecycle, RTRT serves as the release mechanism that leverages this process understanding to justify parametric release decisions [98]. The successful implementation of RTRT typically depends on the foundation established by a robust CPV system that provides continuous verification of process performance and product quality.
The integration of these approaches represents a maturation of quality systems beyond traditional quality-by-testing (QbT) methodologies toward modern quality-by-design (QbD) and real-time quality control paradigms [98]. This evolution enables manufacturers to respond more effectively to process variations, reduce production cycle times, and allocate quality assurance resources more efficiently through risk-based approaches.
Implementation Framework: Methodologies and Protocols
CPV Methodology and Tool Selection
The implementation of an effective CPV program requires a structured methodology aligned with regulatory expectations and scientific rigor. The FDA's process validation lifecycle model provides a framework for CPV activities, with tool selection guided by data suitability assessments and risk-based prioritization [99].
Data Suitability Assessments
Data suitability forms the foundation of effective CPV programs, ensuring monitoring tools align with statistical and analytical realities. Three core assessments are critical:
- Distribution Analysis: Determines whether process data follows normal distribution patterns using statistical tests (Shapiro-Wilk, Anderson-Darling) and visual tools (Q-Q plots, histograms). Parameters with data clustered near detection limits often exhibit non-normal distributions, requiring non-parametric monitoring methods [99].
- Process Capability Evaluation: Quantifies a parameter's ability to meet specifications relative to natural variability using indices (Cp, Cpk). High capability indices (>2) indicate minimal variability, potentially rendering traditional control charts ineffective and necessitating alternative monitoring approaches [99].
- Analytical Performance Considerations: Addresses parameters operating near analytical limits of detection (LOD) or quantification (LOQ), where measurement variability may overshadow true process signals. Implementation requires decoupling analytical variability through dedicated method monitoring programs [99].
Risk-Based Tool Selection
The ICH Q9 Quality Risk Management framework provides a structured methodology for aligning CPV tools with parameter criticality. Implementation follows a systematic process:
- Assess Parameter Criticality: Categorize parameters based on impact on CQAs as Critical, Key, or Non-Critical [99].
- Select Tools Using ICU Framework: Evaluate parameters based on Importance, Complexity, and Uncertainty to determine appropriate monitoring tools [99].
- Document and Justify Selection: Provide scientific rationale for tool selection aligned with regulatory expectations for risk-based decisions [99].
Table 1: CPV Tool Selection Based on Parameter Risk Profile
| Risk Category | Impact on Product Quality | Recommended CPV Tools | Statistical Methods |
|---|---|---|---|
| Critical | Direct impact on safety/efficacy | FMEA, Statistical Process Control, Adaptive Control Charts | Tolerance intervals, Multivariate analysis, Trend analysis |
| Key | Influential but not directly impacting safety/efficacy | Control charts, Risk ranking matrices, Batch-wise trending | Process capability analysis, Normal probability plots |
| Non-Critical | No measurable quality impact | Checklists, Simplified monitoring, Limit-based alerts | Basic statistics, Run charts |
RTRT Implementation and Validation
RTRT implementation requires a systematic approach encompassing method development, validation, and regulatory submission. The methodology typically involves several distinct phases:
PAT Implementation Framework
Process Analytical Technology provides the technological foundation for RTRT through integrated analytical tools that monitor Critical Quality Attributes during processing. PAT implementation follows a structured approach:
- Tool Selection: Identification of appropriate analytical technologies (NIR, Raman, etc.) based on the specific quality attributes being monitored and process constraints [98].
- Method Development: Establishment of correlation models between PAT measurements and reference analytical methods, including determination of measurement ranges and accuracy requirements [98].
- Control Strategy Integration: Incorporation of PAT data into process control systems to enable real-time adjustments and release decisions [98].
The implementation of PAT enables RTRT by providing the real-time data necessary to assess product quality without traditional end-product testing. PAT applications span pharmaceutical unit operations including blending, granulation, tableting, and coating, with monitoring of Intermediate Quality Attributes (IQAs) to ensure consistent finished product quality [98].
RTRT Validation Protocol
RTRT validation follows a comprehensive protocol to demonstrate method suitability for its intended purpose:
- Comparative Testing: Generation of substantial data through parallel testing of production batches comparing RTRT results with traditional compendial methods [100].
- Method Accuracy Demonstration: Statistical comparison establishing equivalence between RTRT and reference methods across the product specification range.
- Robustness Testing: Evaluation of method performance under varied process conditions to ensure reliability during routine manufacturing.
- System Suitability: Definition and validation of ongoing monitoring criteria to ensure continued method performance throughout its lifecycle.
Upon successful validation, RTRT results are reported on the Certificate of Analysis as "complies if tested" with an explanatory footnote indicating "Controlled by approved Real Time Release Testing" [100].
Material Tracking in Continuous Manufacturing
For continuous manufacturing processes, Material Tracking (MT) models represent a critical enabler for both CPV and RTRT implementation. These mathematical models, typically built on Residence Time Distribution (RTD) principles, allow manufacturers to predict material movement through integrated production systems [102].
MT Model Development and Validation
MT model development follows a structured methodology:
- RTD Characterization: Determination of how long material parcels remain within unit operations through tracer studies, step-change testing, or in silico modeling [102].
- Model Integration: Combination of individual unit operation RTDs into a comprehensive system model that tracks material through the entire manufacturing process [102].
- Validation Protocol: Demonstration of model accuracy across the commercial operating range using statistically sound approaches commensurate with the model's impact on quality decisions [102].
Under ICH Q13, MT models typically qualify as medium-impact models because they inform GxP decisions including material diversion and batch definition [102]. Validation must therefore provide high assurance that model predictions support reliable quality decisions.
Visualization of Workflows and Relationships
CPV Implementation Workflow
The following diagram illustrates the systematic workflow for implementing Continuous Process Verification within the FDA's process validation lifecycle:
CPV Implementation Workflow
RTRT Integration Pathway
The following diagram illustrates the integration pathway for Real-Time Release Testing within a pharmaceutical quality system:
RTRT Integration Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of CPV and RTRT requires specific technological tools and analytical solutions. The following table details essential research reagents and materials critical for establishing robust monitoring and release testing programs.
Table 2: Essential Research Reagent Solutions for CPV and RTRT Implementation
| Tool Category | Specific Technologies | Function in CPV/RTRT | Application Examples |
|---|---|---|---|
| PAT Analytical Tools | NIR Spectroscopy, Raman Spectroscopy, Chemical Imaging | Real-time monitoring of critical quality attributes during processing | Blend uniformity analysis, granulation endpoint determination, coating thickness measurement [98] |
| Reference Standards | Qualified impurity standards, System suitability standards | Method validation and verification for PAT and RTRT methods | Comparative testing during RTRT validation, daily system suitability testing [100] |
| Tracer Materials | UV-absorbing compounds, Colored dyes, API at altered concentration | Residence Time Distribution studies for material tracking model development | Characterization of blender performance, system integration studies for continuous manufacturing [102] |
| Data Analytics Platforms | Multivariate analysis software, Statistical process control systems | Data analysis, trend detection, and statistical monitoring | Multivariate chart development, real-time statistical process control, trend analysis for CPV [15] [99] |
| Method Validation Materials | Accuracy standards, Precision samples, Linearity solutions | Performance characterization of analytical methods | Determination of LOD/LOQ, accuracy and precision validation, range establishment [11] |
Comparative Analysis: Quantitative Data Representation
The implementation of CPV and RTRT generates substantial quantitative data that demonstrates their impact on pharmaceutical manufacturing quality and efficiency. The following tables summarize key comparative metrics and monitoring parameters.
Table 3: Impact Assessment of CPV and RTRT Implementation
| Performance Metric | Traditional Approach | CPV/RTRT Approach | Documented Improvement |
|---|---|---|---|
| Quality Control Timeline | Days to weeks (end-product testing) | Real-time (parametric release) | Reduction from 14-21 days to immediate release [15] |
| Process Deviation Detection | Retrospective (after completion) | Real-time (during processing) | 72% reduction in false positives through proper data suitability assessment [99] |
| Batch Rejection Rates | 2-5% (full batch rejection) | <0.5% (targeted diversion only) | Up to 90% reduction in material waste through targeted diversion [102] |
| Monitoring Frequency | Discrete sampling (1-5% of units) | Continuous monitoring (100% of process) | Comprehensive material tracking versus statistical sampling [98] |
| Data Utilization | Limited statistical analysis | Multivariate modeling and trend analysis | Enhanced process understanding through PAT data integration [98] |
Table 4: Critical Monitoring Parameters for Pharmaceutical Unit Operations
| Unit Operation | Critical Process Parameters | Intermediate Quality Attributes | PAT Monitoring Tools |
|---|---|---|---|
| Blending | Blending time, Blending speed, Order of input, Filling level | Drug content, Blending uniformity, Moisture content | NIR spectroscopy, Chemical imaging [98] |
| Granulation | Binder solvent amount, Binder solvent concentration, Granulation time | Granule-size distribution, Granule strength, Flowability, Density | Focused beam reflectance measurement, Raman spectroscopy [98] |
| Tableting | Compression force, Compression speed, Feed frame speed | Tablet hardness, Weight uniformity, Disintegration time | NIR spectroscopy, Laser diffraction [98] |
| Coating | Spray rate, Pan speed, Inlet temperature, Air flow | Coating thickness, Coating uniformity, Weight gain | Raman spectroscopy, Optical coherence tomography [98] |
The pharmaceutical industry's adoption of Continuous Process Verification and Real-Time Release Testing represents a fundamental evolution in quality assurance paradigms. These approaches transcend traditional quality-by-testing methodologies by establishing integrated, data-driven quality systems that emphasize process understanding, risk-based control, and continuous improvement. The implementation of CPV and RTRT, facilitated by advances in Process Analytical Technology and data analytics, enables manufacturers to achieve unprecedented levels of product quality assurance while improving operational efficiency.
The historical trajectory of analytical method validation protocols reveals a clear progression toward more scientifically rigorous, risk-based approaches that align with the ICH Q8, Q9, and Q10 guidelines. This evolution is characterized by the transition from discrete testing to continuous verification, from reactive quality control to proactive quality assurance, and from empirical operations to knowledge-driven manufacturing. As the industry continues to advance toward continuous manufacturing and digital transformation, CPV and RTRT will undoubtedly play increasingly central roles in pharmaceutical quality systems.
For researchers, scientists, and drug development professionals, understanding these trends is essential for navigating the future landscape of pharmaceutical manufacturing. The successful implementation of CPV and RTRT requires multidisciplinary expertise encompassing process engineering, analytical chemistry, statistics, and regulatory science. By embracing these advanced quality assurance methodologies, the pharmaceutical industry can enhance patient safety, improve manufacturing efficiency, and accelerate the availability of critical medicines to market.
The landscape of analytical method validation has undergone a profound transformation, evolving from manual, document-centric processes to dynamic, computational approaches. Traditional validation frameworks, established through initiatives like the Bioanalytical Method Validation guidance from the US Food and Drug Administration, initially provided standardized parameters for assessing method performance [13]. These foundational protocols ensured reliability in bioavailability, bioequivalence, and pharmacokinetic studies but were constrained by their static nature and extensive resource requirements.
The emergence of sophisticated computational technologies has initiated a paradigm shift toward more adaptive validation ecosystems. Artificial Intelligence (AI), Digital Twins, and Advanced Data Analytics now enable predictive validation models that continuously learn and adapt, moving beyond the one-time event mentality that characterized historical approaches [103]. This transformation is particularly evident in regulated industries like pharmaceuticals and life sciences, where modernization pressures demand validation processes that are both rigorous and responsive to rapid technological change.
This whitepaper examines how these technologies collectively future-proof validation methodologies, creating systems that are not merely compliant but inherently resilient, predictive, and self-optimizing.
The AI Revolution in Validation Paradigms
From Static Checklists to Intelligent Validation
AI technologies are redefining validation core principles by introducing dynamic learning capabilities that transcend traditional rule-based systems. Modern AI-driven validation incorporates active learning frameworks that create iterative feedback loops between computational prediction and experimental validation, substantially accelerating discovery cycles while improving model accuracy [104]. This approach tightly integrates data and computation to improve predictive models through continuous refinement, transforming validation from a linear process to an iterative, intelligent paradigm.
The implementation of explainable AI (XAI) has become critical for validation in regulated environments. Where traditional "black box" models created regulatory challenges, interpretable AI systems now provide transparent rationale for predictions, enabling researchers to understand the structural determinants of successful outcomes [104]. This transparency is particularly valuable in high-stakes applications such as drug design, where understanding why a model makes a specific prediction is as important as the prediction itself.
AI-Enhanced Data Validation Tools
Contemporary data validation tools leverage AI to provide unprecedented capabilities for ensuring data quality and reliability. These tools employ machine learning algorithms for automated error detection, pattern recognition, and data standardization at scale [105]. Key features of modern AI-powered validation platforms include:
- Real-time validation that prevents incorrect data entry at the source
- Automated duplicate detection and merging using fuzzy matching algorithms
- Predictive analytics that identify potential data quality issues before they impact operations
- Custom rule configuration that adapts to specific business requirements and evolving needs
These capabilities are essential for maintaining data integrity in complex research environments where decisions are increasingly data-driven [106]. The integration of AI has transformed data validation from a retrospective cleaning activity to a proactive quality preservation process.
Experimental Protocol: Active Learning for Compound Validation
Objective: To validate AI-predicted compound efficacy and safety using an active learning framework that iteratively improves prediction accuracy through targeted experimental validation.
Methodology:
- Initial Model Training: Train deep neural networks on public compound datasets (e.g., ChEMBL, PubChem) incorporating structural fingerprints, physicochemical properties, and known biological activities.
- Uncertainty Sampling: Deploy the model for virtual screening of compound libraries, selecting candidates for experimental validation based on both predicted efficacy and model uncertainty.
- Experimental Validation:
- Synthesize or procure top candidate compounds
- Conduct in vitro assays for target engagement and selectivity
- Perform cytotoxicity screening against human cell lines
- Model Refinement: Integrate experimental results into training data, retrain the model, and repeat the cycle for continuous improvement.
Key Measurements:
- Prediction accuracy improvement per iteration
- Reduction in false positive rates
- Structural diversity of selected compounds
- Experimental validation of AI-generated hypotheses
This protocol exemplifies the iterative validation paradigm that AI enables, where each cycle enhances the predictive capability while generating experimentally testable hypotheses [104].
Digital Twins: Virtual Validation and Computational Prototyping
Defining Digital Twins in Healthcare Applications
Digital Twins (DTs) represent one of the most transformative technologies for validation, creating dynamic virtual counterparts of physical entities. According to the National Academies of Sciences, Engineering, and Medicine (NASEM), a true digital twin must be personalized, dynamically updated, and have predictive capabilities to inform decision-making [107]. The healthcare sector has rapidly adopted this technology, though a recent scoping review revealed that only 12.08% of studies claiming to create human digital twins fully met the NASEM criteria, highlighting the rigorous standards for proper implementation [107].
The taxonomy of digital representations exists on a spectrum:
- Digital Models: Static virtual representations with no automatic data exchange
- Digital Shadows: One-way data flow from physical to virtual environment
- Digital Twins: Bidirectional, dynamic data exchange between physical and virtual systems
- Virtual Patient Cohorts: Generalized digital representations of patient populations for in-silico trials
True digital twins in healthcare enable unprecedented capabilities for validation, allowing researchers to simulate interventions, predict outcomes, and optimize parameters before physical implementation [108].
Validation Applications in Clinical Trials and Drug Development
Digital twins are revolutionizing validation in clinical research through multiple applications:
Enhanced Clinical Trial Design: Digital twins enable the creation of synthetic control arms that reduce the need for placebo groups while maintaining statistical rigor [108]. By generating virtual patients that mirror the distribution of relevant covariates in the actual population, researchers can improve trial generalizability while reducing sample size requirements. This approach addresses the critical limitation of traditional randomized controlled trials (RCTs), which often suffer from restrictive eligibility criteria that limit participant diversity and real-world applicability.
Predictive Safety Validation: DTs significantly enhance drug safety assessments by leveraging comprehensive patient data to predict adverse events and individual treatment responses [108]. These virtual models integrate genetic, physiological, and environmental factors to simulate how a patient might react to a specific therapy, allowing researchers to identify potential safety issues before they occur in actual patients. This predictive capability enables preemptive adjustments to treatment protocols, minimizing risks and improving overall patient safety.
Accelerated Drug Development: Throughout the drug development pipeline, digital twins provide validation at multiple stages:
- Early-stage discovery: Model disease mechanisms and identify therapeutic targets
- Preclinical testing: Simulate human responses, potentially reducing animal research
- Clinical trial simulation: Optimize trial parameters through virtual cohorts
- Post-market surveillance: Continuously monitor safety and efficacy with real-world data [108]
Experimental Protocol: Digital Twin Validation for Personalized Treatment
Objective: To create and validate a digital twin for predicting individual patient responses to a specific therapeutic intervention.
Methodology:
- Data Integration:
- Collect multi-omics data (genomics, proteomics, metabolomics)
- Acquire medical imaging (CT, MRI, PET)
- Gather clinical parameters and real-time sensor data
- Document social determinants of health
Model Construction:
- Develop mechanistic models based on physiological principles
- Implement empirical models trained on population data
- Create hybrid models combining both approaches
- Establish uncertainty quantification measures
Validation Framework:
- Perform verification to ensure correct model implementation
- Conduct validation to assess model accuracy against experimental data
- Implement uncertainty quantification to evaluate prediction reliability
- Compare predictions with actual patient outcomes
Clinical Decision Support:
- Simulate intervention options on the digital twin
- Predict outcomes for each potential intervention
- Recommend optimal therapeutic strategy
- Continuously update model with real-world patient data
Key Measurements:
- Prediction accuracy for clinical outcomes
- Model sensitivity and specificity
- Uncertainty quantification metrics
- Clinical utility and impact on decision-making
This rigorous validation protocol ensures that digital twins meet the NASEM standards while providing clinically actionable insights [107] [108].
Advanced Data Analytics: The Backbone of Modern Validation
Next-Generation Data Validation Frameworks
Advanced data analytics provides the foundational capabilities required for modern validation processes. Contemporary data validation tools offer sophisticated features that ensure data integrity throughout the research lifecycle:
Table 1: Key Features of Advanced Data Validation Tools
| Feature Category | Specific Capabilities | Validation Impact |
|---|---|---|
| Automated Error Detection | Pattern recognition, anomaly detection, outlier identification | Reduces manual review effort while improving error identification accuracy |
| Real-time Validation | Immediate data quality checks at point of entry | Prevents propagation of erroneous data throughout systems |
| Data Standardization | Format conversion, unit normalization, terminology mapping | Ensures consistency across diverse data sources for integrated analysis |
| Duplicate Management | Fuzzy matching, record linkage, merge/purge algorithms | Maintains data integrity by eliminating redundant entries |
| Custom Rule Configuration | Business-specific validation rules, adaptive criteria | Aligns validation with specific research requirements and evolving needs |
These capabilities are implemented in leading data validation platforms such as Astera, Informatica, and Talend, which provide the technical infrastructure for maintaining data quality in complex research environments [105] [106].
Statistical and Machine Learning Approaches
Advanced analytics incorporates sophisticated statistical and machine learning methods for validation:
Statistical Validation Techniques:
- Hypothesis testing for significance validation
- Probability distributions for modeling expected outcomes
- Regression analysis for relationship validation
- A/B testing for comparative assessment
Machine Learning Validation:
- Feature engineering for data optimization
- Model validation through train-test splits and cross-validation
- Performance tuning using precision, recall, and F1 scores
- Supervised and unsupervised learning applications for different data types [109]
These methodologies enable researchers to move beyond simple rule-based validation toward probabilistic, multi-dimensional assessment frameworks that better reflect the complexity of modern research data.
Integrated Workflows: Convergence of Technologies for Comprehensive Validation
Future-Proofing Through Technology Integration
The convergence of AI, digital twins, and advanced analytics creates a powerful ecosystem for validation that is inherently future-proof. This integration enables:
Continuous Validation Processes: Modern software validation in life sciences is shifting from episodic to continuous validation, with quality teams validating in step with software updates and business process changes [103]. This approach aligns with regulatory evolution, including the FDA's Computer Software Assurance (CSA) framework, which promotes risk-based validation focused on functionality that truly impacts product quality, patient safety, or data integrity.
Adaptive Validation Frameworks: The combination of these technologies enables validation systems that learn and adapt over time. AI algorithms improve through active learning, digital twins refine their predictions with new data, and analytics platforms incorporate emerging patterns into validation rules. This creates a virtuous cycle where validation becomes increasingly accurate and efficient.
Risk-Based Validation Prioritization: Exhaustive validation checklists are giving way to risk-based approaches that focus resources on areas with the greatest impact on compliance and patient safety [103]. This prioritization is enabled by AI-driven risk assessment and digital twin simulation capabilities that identify critical validation targets.
Implementation Framework
Successful implementation of future-proofed validation methodologies requires a structured approach:
- Assessment of Current Validation Maturity
- Identification of High-Impact Validation Opportunities
- Technology Selection and Integration
- Staged Implementation with Measured Outcomes
- Continuous Improvement Through Feedback Loops
This framework ensures that organizations can systematically enhance their validation processes while maintaining regulatory compliance and operational efficiency.
Comparative Analysis: Quantitative Assessment of Validation Technologies
Table 2: Performance Metrics of Advanced Validation Technologies
| Technology | Application Scope | Validation Efficiency Gain | Implementation Complexity | Regulatory Acceptance |
|---|---|---|---|---|
| AI & Machine Learning | Data validation, predictive modeling, pattern recognition | 40-60% reduction in manual validation effort [105] | High (requires specialized expertise) | Moderate (evolving standards for algorithm validation) |
| Digital Twins | Clinical trial optimization, personalized treatment prediction, safety assessment | 50-70% reduction in trial recruitment time [108] | Very High (multidisciplinary team required) | Emerging (12% meet full NASEM criteria [107]) |
| Advanced Data Analytics | Data quality assurance, statistical validation, trend analysis | 30-50% improvement in data quality metrics [106] | Moderate (tools increasingly user-friendly) | High (well-established statistical principles) |
| Integrated Platform Approach | End-to-end validation workflow automation | 60-80% improvement in validation cycle times [103] | High (integration challenges across systems) | Growing (CSA framework adoption [103]) |
Visualization of Next-Generation Validation Workflows
AI-Enhanced Validation Ecosystem
AI-Enhanced Validation Ecosystem: This diagram illustrates the iterative feedback loop between AI prediction, digital twin simulation, and experimental validation that characterizes modern validation approaches.
Digital Twin Validation Architecture
Digital Twin Validation Architecture: This architecture demonstrates the bidirectional data flow between physical and virtual systems, highlighting the critical role of Verification, Validation, and Uncertainty Quantification (VVUQ) in maintaining model fidelity.
The Researcher's Toolkit: Essential Solutions for Modern Validation
Table 3: Research Reagent Solutions for Advanced Validation
| Tool Category | Specific Solutions | Primary Function | Validation Application |
|---|---|---|---|
| Data Validation Platforms | Astera, Informatica, Talend | Automated data quality assessment, cleansing, and monitoring | Ensures data integrity throughout research lifecycle [106] |
| AI/ML Frameworks | Python, Scikit-learn, TensorFlow, PyTorch | Machine learning model development, training, and validation | Enables predictive modeling and pattern recognition for validation [109] |
| Digital Twin Platforms | Custom implementations (varies by institution) | Virtual patient modeling, simulation, and predictive analytics | Facilitates in-silico validation and clinical trial optimization [108] [107] |
| Statistical Analysis Tools | R, Python, SAS, Jupyter Notebooks | Statistical validation, hypothesis testing, probability analysis | Provides rigorous statistical foundation for validation decisions [109] |
| Workflow Automation | SIMCO AV, Custom automation scripts | Validation process automation, test execution, documentation | Accelerates validation cycles while ensuring consistency [103] |
The convergence of AI, digital twins, and advanced data analytics represents a fundamental transformation in validation methodologies. These technologies enable a shift from static, document-centric validation to dynamic, computational approaches that are predictive, adaptive, and evidence-based. The future of validation lies in integrated systems that continuously learn and improve, reducing time-to-insight while enhancing reliability and reproducibility.
For researchers, scientists, and drug development professionals, embracing these technologies is no longer optional but essential for maintaining competitiveness and scientific rigor. The organizations that successfully implement these future-proofed validation methods will lead in innovation, efficiency, and impact, ultimately accelerating the translation of research into real-world solutions.
Conclusion
The evolution of analytical method validation protocols marks a decisive shift from a static, prescriptive exercise to a dynamic, science-based lifecycle management system. This journey, driven by regulatory harmonization and technological innovation, emphasizes proactive quality building through AQbD, ATP, and risk-management. The key takeaways are the enduring importance of foundational parameters, the efficiency gains from phase-appropriate and platform strategies, and the critical need for robust troubleshooting and transfer protocols. Looking ahead, the integration of AI, real-time data, and continuous monitoring will further transform validation into an agile, predictive process. For biomedical research, these advancements promise to accelerate the development of complex therapies, enhance patient safety through more reliable data, and establish a more flexible and efficient global regulatory environment for the next generation of medicines.
References
- 1. The History & Future of Validation [https://ispe.org/pharmaceutical-engineering/march-april-2021/history-future-validation]
- 2. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 3. GLP and GMP Approaches to Method Validation [https://www.spectroscopyonline.com/view/glp-and-gmp-approaches-method-validation-going-same-way]
- 4. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 5. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 6. ICH - Instilling 'harmony' for 30 years, and never more ... [https://www.efpia.eu/news-events/the-efpia-view/blog-articles/ich-instilling-harmony-for-30-years-and-never-more-relevant-than-today/]
- 7. International Council for Harmonisation of Technical ... [https://en.wikipedia.org/wiki/International_Council_for_Harmonisation_of_Technical_Requirements_for_Pharmaceuticals_for_Human_Use]
- 8. ICH Q2(R1) Validation of Analytical Procedures [https://www.gmp-compliance.org/guidelines/gmp-guideline/ich-q2r1-validation-of-analytical-procedures-text-and-methodology]
- 9. Navigating the Biopharmaceutical Method Validation [https://synergbiopharma.com/navigating-the-evolution-from-ich-q2r1-to-ich-q2r2-and-implementation-of-ich-q14-in-biopharmaceutical-method-validation/]
- 10. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 11. Analytical Strategies from Early Development to Validation [https://www.registech.com/blog/analytical-strategies-from-early-development-to-validation-part-two/]
- 12. Analytical Method Validation: Back to Basics, Part I [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 13. The history of bioanalytical method validation and regulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2751303/]
- 14. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 15. Leading Pharmaceutical Validation Trends for 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 16. FDA vs EMA: Key Regulatory Differences for ... [https://lsacademy.com/en/fda-vs-ema-key-regulatory-differences-for-pharmaceuticals/]
- 17. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 18. Evolution of Analytical Procedure Validation Concepts: Part I [https://www.pharmtech.com/view/evolution-of-analytical-procedure-validation-concepts-part-i-analytical-procedure-life-cycle-and-compendial-approaches]
- 19. E6(R3) Good Clinical Practice (GCP) September 2025 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e6r3-good-clinical-practice-gcp]
- 20. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 21. Comparison of the FDA and EMA guidance on drug ... [https://pubmed.ncbi.nlm.nih.gov/40692351/]
- 22. EMA Guideline On Clinical-Stage ATMPs Comes Into Effect [https://www.cellandgene.com/doc/ema-guideline-on-clinical-stage-atmps-comes-into-effect-on-the-verge-of-convergence-0001]
- 23. Recent FDA Actions Pose Big Changes and Questions for ... [https://www.hklaw.com/en/insights/publications/2025/07/recent-fda-actions-pose-big-changes-and-questions-for-health]
- 24. A review on analytical method validation and its regulatory ... [https://jddtonline.info/index.php/jddt/article/view/2403]
- 25. Validation of Analytical Methods: A Review [https://www.gavinpublishers.com/article/view/validation-of-analytical-methods-a-review]
- 26. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 27. Checklist Analysis - Risk Identification Techniques [https://trustedinstitute.com/concept/pmi-rmp/risk-identification-techniques/checklist-analysis-risk-id/]
- 28. Strengths and weaknesses of the checklist approach to ... [https://www.quality.org/article/strengths-and-weaknesses-checklist-approach-auditing]
- 29. Critical Evaluation: Criteria Checklist Approach: CRAAP [https://libguides.bcu.ac.uk/critical-evaluation/checklist-approach]
- 30. Validation of educational assessments: a primer for simulation ... [https://advancesinsimulation.biomedcentral.com/articles/10.1186/s41077-016-0033-y]
- 31. Fit-for-purpose biomarker method validation for application in clinical trials of anticancer drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990602/]
- 32. A Phase-Appropriate Approach For Assay Validation In Cell & Gene Therapies [https://www.cellandgene.com/doc/a-phase-appropriate-approach-for-assay-validation-in-cell-gene-therapies-0001]
- 33. Selecting Bioanalytical Assays for FDA Approved Clinical Trials and Commercialization - Marin Biologic Laboratories [https://www.marinbio.com/company/selecting-bioanalytical-assays-fda-clinical-trials-commercialization/]
- 34. Fit-for-Purpose Assays vs. Validated Assays: What’s the Difference? - SoCal Biosciences [https://www.socalbiosci.com/fit-for-purpose-assays-vs-validated-assays-whats-the-difference/]
- 35. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 36. Recent applications of analytical quality-by-design ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743924001837]
- 37. Analytical Quality by Design and Analytical Procedure Life Cycle [https://qualitymatters.usp.org/paradigm-shift-drug-development-analytical-quality-design-and-analytical-procedure-life-cycle]
- 38. AQbD-novel strategy for analytical methods [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 39. An industrial case study: QbD to accelerate time-to-market of a ... [https://aapsopen.springeropen.com/articles/10.1186/s41120-021-00047-w]
- 40. Analytical Quality by Design (AQbD) Approach to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9653622/]
- 41. Established Conditions for Analytical Procedures and QbD [https://www.a3p.org/en/analytical-procedures-qbd/]
- 42. Verification of quantitative analytical methods in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8199534/]
- 43. From method validation to result assessment [https://www.sciencedirect.com/science/article/abs/pii/S0165993618300797]
- 44. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 45. Using the Analytical Target Profile to Drive ... [https://pubmed.ncbi.nlm.nih.gov/30624912/]
- 46. Applying ICH Q14 in Pharmaceuticals Part 1 [https://premier-research.com/perspectives/applying-ich-q14-in-pharmaceuticals-part-1-the-application-of-analytical-target-profile-in-analytical-method-development/]
- 47. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 48. Introduction to Analytical Method Development and ... [https://www.labmanager.com/introduction-to-analytical-method-development-and-validation-33922]
- 49. Validation of Stability-Indicating HPLC Methods for ... [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 50. Why DOE Is Essential in the (Bio)Pharma Industry [https://www.sartorius.com/en/knowledge/science-snippets/why-doe-is-essential-in-the-biopharma-industry-601720]
- 51. Design of experiments (DoE) in pharmaceutical development [https://pubmed.ncbi.nlm.nih.gov/28166428/]
- 52. Design of Experiments (DoE) in (bio)Pharmaceuticals [https://www.vennlifesciences.com/articles-and-research/design-of-experiments-doe-blog/]
- 53. Process: A Step-by-Step Guide to How It Works - Synthace DOE [https://www.synthace.com/blog/the-doe-process]
- 54. Advanced G-Optimal DOE Techniques [https://www.numberanalytics.com/blog/advanced-g-optimal-doe-techniques]
- 55. A Scalable Validation Model for Multiproduct Facilities [https://www.pharmasalmanac.com/articles/accelerating-biomanufacturing-facility-readiness-a-scalable-validation-model-for-multiproduct-facilities]
- 56. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 57. Covalidation Strategies to Accelerate Analytical Method ... [https://www.pharmtech.com/view/covalidation-strategies-accelerate-analytical-method-transfer-breakthrough-therapies]
- 58. Analytical Method Transfer: Best Practices and Guidelines [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 59. How to Keep Multisite Multi-Analyzer Validations on Track [https://myadlm.org/cln/articles/2020/janfeb/how-to-keep-multisite-multi-analyzer-validations-on-track]
- 60. Methods on the Move: Addressing Method Transfer ... [https://www.bioprocessintl.com/cmc-forums/methods-on-the-move-addressing-method-transfer-challenges-for-the-biopharmaceutical-industry]
- 61. Managing Cleaning Validation in Multi-Product Biologics ... [https://www.biopharminternational.com/view/managing-cleaning-validation-multi-product-biologics-facilities]
- 62. Challenges in Developing Analytical Procedures with the ... [https://www.pharmoutsourcing.com/Featured-Articles/621016-Challenges-in-Developing-Analytical-Procedures-with-the-New-ICH-Q14-Guideline/]
- 63. Some good validation practices for analytical procedures [https://www.a3p.org/en/bonnes-pratiques-validation/]
- 64. The Hidden Risks in Analytical Method Validation - [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 65. Size-Exclusion Chromatography: A Twenty-First Century ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9813945/]
- 66. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 67. The Early Development of Size Exclusion Chromatography [https://www.chromatographyonline.com/view/early-development-size-exclusion-chromatography-historical-perspective-0]
- 68. The Early Development of Size-Exclusion Chromatography [https://www.chromatographyonline.com/view/early-development-size-exclusion-chromatography-historical-perspective]
- 69. Transfer Of Analytical Methods Between Two Units And ... [https://orioledhub.com/transfer-of-analytical-methods-between-two-units-and-laboratories/]
- 70. Analytical Method Transfer: Common Pitfalls and How to ... [https://www.qbdgroup.com/en/blog/analytical-method-transfer-common-pitfalls-and-how-to-avoid-them]
- 71. Best Practices for Transferring Analytical Methods [https://www.jmolner.com/post/transferring-analytical-methods]
- 72. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 73. Periodic Comparability Verification and Within-Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8548239/]
- 74. ICH Guidance Q14 / Q2(R2) - Analytical Method ... [https://www.gmp-compliance.org/gmp-news/ich-guidance-q14-q2r2-analytical-method-development-method-validation-published-for-consultation]
- 75. Validating Analytical Methods for Biopharmaceuticals, Part 1 [https://www.biopharminternational.com/view/validating-analytical-methods-biopharmaceuticals-part-1-development-and-optimization]
- 76. AMV 2025 Updates: Enhancing Global Compliance and ... [https://www.linkedin.com/posts/rohit-yadav-76a123139_analyticalmethodvalidation-pharmaquality-activity-7392942502166585344-H3KH]
- 77. The ALCOA++ Principles for Data Integrity in Clinical Trials [https://www.quanticate.com/blog/alcoa-principles]
- 78. ALCOA Data-Integrity Principles: A Complete 2025 Guide [https://redica.com/data-integrity-and-alcoa/]
- 79. Data Integrity Guidelines: What You Must Do Now - [https://pharmuni.com/2025/10/17/data-integrity-guidelines-what-you-must-do-now/]
- 80. Data Integrity Focus, Part II: Using Data Process Mapping ... [https://www.chromatographyonline.com/view/data-integrity-focus-part-ii-using-data-process-mapping-identify-integrity-gaps]
- 81. Addressing Data Integrity Gaps: Does Your Lab Have a ... [https://chemetrix.co.za/addressing-data-integrity-gaps-does-your-lab-have-a-strategy/]
- 82. Data Validation in Clinical Data Management [https://www.quanticate.com/blog/data-validation-in-clinical-data-management]
- 83. Ensuring data integrity: Best practices and strategies in ... [https://www.sciencedirect.com/science/article/pii/S2949866X24001060]
- 84. Q14 Analytical Procedure Development March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q14-analytical-procedure-development]
- 85. ICH Q14 Analytical procedure development - Scientific guideline [https://www.ema.europa.eu/en/ich-q14-analytical-procedure-development-scientific-guideline]
- 86. ICH Q2(R2) Validation of Analytical Procedures [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 87. ICH Q14- Analytical Procedure Development [https://biotech.com/2024/06/26/ich-q14-analytical-procedure-development/]
- 88. Validation Strategy in Pharma 4.0: Comparing Modern and ... [https://www.avslifesciences.com/blog-post/validation-strategy-in-pharma-4-0-comparing-modern-and-traditional-methods]
- 89. USP Revised: Aligning Compendial Validation with ... [https://investigationsquality.com/2025/11/13/usp-1225-revised-aligning-compendial-validation-with-ich-q2r2-and-q14s-lifecycle-vision/]
- 90. The Lifecycle Change of Process Validation and Analytical ... [https://www.biopharminternational.com/view/lifecycle-change-process-validation-and-analytical-testing]
- 91. Navigating the Evolving Landscape of Validation in 2025 [https://investigationsquality.com/2025/06/12/navigating-the-evolving-landscape-of-validation-in-2025-trends-challenges-and-strategic-imperatives/]
- 92. The Future of Validation [https://kneat.com/article/2025-validation-trends/]
- 93. Validation in Transition: Why 2025 is the Turning Point for ... [https://ispe.org/pharmaceutical-engineering/ispeak/validation-transition-why-2025-turning-point-industry]
- 94. Process Validation in Six Sigma: A Complete Guide [https://www.6sigma.us/process-improvement/process-validation/]
- 95. Mastering Process Validation and Continued ... [https://www.labmanager.com/mastering-process-validation-and-continued-process-verification-in-pharma-labs-34127]
- 96. Emerging New Drug Modalities in 2025 [https://www.bcg.com/publications/2025/emerging-new-drug-modalities]
- 97. An Enhanced Approach to Analytical Instrument and ... [https://www.spectroscopyonline.com/view/an-enhanced-approach-to-analytical-instrument-and-system-qualification]
- 98. Process Analytical Technology Tools for Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8234957/]
- 99. ( Continuous ) Methodology and Tool... Process Verification CPV [https://investigationsquality.com/2025/03/30/continuous-process-verification-cpv-methodology-and-tool-selection-a-framework-guided-by-fda-process-validation/]
- 100. New EMA Guideline on Real Time Release Testing [https://www.gmp-compliance.org/gmp-news/new-ema-guideline-on-real-time-release-testing]
- 101. Real time release testing - Scientific guideline [https://www.ema.europa.eu/en/real-time-release-testing-scientific-guideline]
- 102. Material Tracking Models in Continuous Manufacturing [https://investigationsquality.com/2025/10/24/material-tracking-models-in-continuous-manufacturing-development-validation-and-lifecycle-management/]
- 103. The Future of Software Validation in Life Sciences: Trends ... [https://www.simco.com/blog/software-validation-trends/]
- 104. Next Decade’s AI -Based Drug Features Tight... Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880149/]
- 105. The Best 5 Data Validation Tools in 2025 [https://numerous.ai/blog/data-validation-tools]
- 106. Top 7 Data Validation Tools to Explore in 2025 [https://www.astera.com/type/blog/data-validation-tools/]
- 107. A scoping review of human digital twins in healthcare ... [https://www.nature.com/articles/s41746-025-01910-w]
- 108. Enhancing randomized clinical trials with digital twins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494699/]
- 109. Google Advanced Data Analytics Professional Certificate [https://www.coursera.org/professional-certificates/google-advanced-data-analytics]