Good Laboratory Practice (GLP) for Analytical Chemists: A Practical Guide to Compliance, Methods, and Data Integrity
This article provides a comprehensive guide to Good Laboratory Practice (GLP) specifically for analytical and bioanalytical chemists involved in drug development.
Good Laboratory Practice (GLP) for Analytical Chemists: A Practical Guide to Compliance, Methods, and Data Integrity
Abstract
This article provides a comprehensive guide to Good Laboratory Practice (GLP) specifically for analytical and bioanalytical chemists involved in drug development. It covers the foundational principles of GLP as a quality system for nonclinical safety studies, detailing the roles of chemists in method development, sample analysis, and data management. The content explores practical applications, including techniques like HPLC and LC-MS, addresses common troubleshooting challenges in peptide analysis and data silos, and outlines the rigorous requirements for method validation and compliance with FDA (21 CFR Part 58) and OECD standards. Aimed at researchers, scientists, and drug development professionals, this guide synthesizes regulatory expectations with practical laboratory strategies to ensure data quality, integrity, and regulatory acceptance.
Understanding GLP: The Quality Framework for Nonclinical Laboratory Studies
Good Laboratory Practice (GLP) is a quality system framework governing the organizational processes and conditions under which nonclinical laboratory studies are planned, performed, monitored, recorded, reported, and archived [1]. Established to ensure the quality and integrity of safety test data, GLP provides regulatory agencies with reliable, reproducible, and auditable evidence to support the approval of pharmaceuticals, agrochemicals, and other products [2] [3].
For analytical chemists, GLP is distinct from, yet complementary to, other quality systems. While Good Manufacturing Practice (GMP) ensures quality in production and Good Clinical Practice (GCP) governs human clinical trials, GLP specifically focuses on preclinical safety testing [4] [1]. Its fundamental purpose is not to assess the scientific merit of a study hypothesis but to verify that the process of data collection and handling is rigorous, consistent, and fully traceable [2]. In essence, GLP is “less about what you found and more about proving how you found it – cleanly, consistently, and under independent QA oversight” [2].
Historical Context and Regulatory Genesis
The formalization of GLP regulations was a direct response to widespread data integrity failures discovered in commercial testing laboratories during the 1970s [2] [5]. Prior to GLP, nonclinical safety studies were often plagued by insufficient quality control, leading to questions about the validity of data used to evaluate product safety.
The pivotal event that catalyzed regulatory action was the Industrial Bio-Test (IBT) Laboratories scandal [2] [3] [5]. IBT, a major contract research organization, was found to have fabricated and falsified safety data for numerous chemical manufacturers and the U.S. government. Investigations revealed that thousands of toxicology studies were scientifically unreliable, compromising the safety assessments of hundreds of products, from drugs to household items [5]. This breach of public trust prompted U.S. Congressional hearings and led the Food and Drug Administration (FDA) to draft the first GLP regulations [5].
The FDA issued the final rule for 21 CFR Part 58 (Good Laboratory Practice for Nonclinical Laboratory Studies) in 1978, with the regulations becoming effective in 1979 [2] [3]. The Environmental Protection Agency (EPA) followed with its own GLP rules under FIFRA and TSCA in 1983 [2] [5]. This U.S. regulatory framework has since become part of a global standard, harmonized through the Organization for Economic Co-operation and Development (OECD), which adopted GLP principles in 1992 to enable mutual acceptance of data among member countries [2] [3].
Scope and Applicability of GLP
Understanding the boundaries of GLP is critical for effective implementation. GLP applies specifically to nonclinical laboratory studies that support applications for research or marketing permits for products regulated by the FDA and other agencies [2] [6].
Table: Studies Requiring and Exempt from GLP Compliance
| GLP Compliance REQUIRED | GLP Compliance NOT REQUIRED |
|---|---|
| Standard repeated-dose toxicity studies [3] | Basic exploratory research [2] |
| Genotoxicity and carcinogenicity studies [4] [3] | Chemical method development [2] [1] |
| Safety pharmacology studies [3] | Analytical method validation trials [2] [1] |
| Reproductive and developmental toxicity studies [4] | Clinical trials on humans (governed by GCP) [2] [4] |
| Toxicokinetic (TK) and pharmacokinetic (PK) studies [4] | Organoleptic evaluations of food [1] |
| Studies to support IND, NDA, or marketing applications [2] [3] | Early-stage exploratory studies (e.g., preliminary ADME) [3] |
For analytical chemists, key applicable activities include characterizing the test article (drug substance), determining the stability of the test article and its mixtures, and analyzing specimens (e.g., blood, plasma, tissues) from test systems [4] [1].
Core Principles and Regulatory Framework
The 10 Principles of GLP
The OECD and FDA GLP regulations are built upon a set of foundational principles that create a managerial quality control system [4] [1].
Table: The 10 Principles of Good Laboratory Practice
| Principle Number | Principle Area | Core Requirement |
|---|---|---|
| 1 | Test Facility Organization & Personnel | Defined structure, sufficient staff, clear responsibilities [1] |
| 2 | Quality Assurance Programme | Independent QAU monitoring study conduct [1] |
| 3 | Facilities | Adequate size, construction, and separation to prevent interference [1] |
| 4 | Apparatus, Material & Reagents | Appropriately designed, calibrated, and maintained [1] |
| 5 | Test Systems | Proper characterization, housing, and care [1] |
| 6 | Test & Reference Items | Proper characterization, handling, and storage [2] [1] |
| 7 | Standard Operating Procedures (SOPs) | Written procedures for all study aspects [1] |
| 8 | Performance of the Study | Written protocol, raw data generated per GLP [1] |
| 9 | Reporting of Study Results | Comprehensive final report reconstructing study [1] |
| 10 | Storage & Retention of Records | Secure archiving of raw data, reports, and specimens [1] |
Key Requirements of 21 CFR Part 58
The U.S. FDA's 21 CFR Part 58 provides the detailed regulatory framework for GLP compliance, structured into multiple subparts [2] [7].
Table: Key Requirements of 21 CFR Part 58 Subparts
| Subpart | Focus Area | Specific Mandates |
|---|---|---|
| Subpart A | General Provisions | Defines scope, applicability, and definitions [2] |
| Subpart B | Organization & Personnel | Study Director responsibility; independent QAU [2] [7] |
| Subpart C | Facilities | Adequate lab, animal care, and article handling areas [2] [7] |
| Subpart D | Equipment | Appropriate design, maintenance, and calibration [2] [7] |
| Subpart E | Testing Facility Operations | Requires SOPs for all operations [2] |
| Subpart F | Test & Control Articles | Characterization, handling, and storage of test items [2] [7] |
| Subpart G | Protocol & Conduct | Written protocol; adherence to protocol during conduct [2] [7] |
| Subpart J | Records & Reports | Final report; raw data storage and retention [2] [7] |
GLP Organizational Structure and Data Flow
Critical Roles and Responsibilities
A clearly defined organizational structure with assigned responsibilities is a cornerstone of GLP.
The Study Director
The Study Director serves as the single point of control for the entire study and bears ultimate responsibility for its technical and GLP compliance [2] [7]. Key responsibilities include approving the study protocol, ensuring adherence to the protocol and SOPs, confirming accurate data collection, and preparing and approving the final study report, which includes a GLP compliance statement [2] [1].
The Quality Assurance Unit (QAU)
The QAU functions as the independent internal monitor, entirely separate from the personnel conducting the study [2] [3]. Its mandate is to "assure management that all facilities, equipment, personnel, methods, practices, records, and controls are in conformance with the regulations" [3]. The QAU achieves this through activities such as auditing final reports against raw data, conducting facility inspections, and reporting findings directly to management [2] [3].
Analytical Chemist Roles
Analytical chemists play two vital roles in GLP studies [4]:
Analytical Chemist (Test Article Characterization): Responsible for developing and using validated methods to determine the identity, strength, purity, composition, and stability of the test article (drug substance) and its formulations [4]. This ensures the test item is properly defined for the entire study duration.
Bioanalytical Chemist (Specimen Analysis): Analyzes biological samples (blood, plasma, urine, tissues) collected from test systems after administration of the test article [4]. These analyses, conducted according to validated methods (e.g., ICH M10), generate toxicokinetic and pharmacokinetic data critical for safety assessment [4].
Essential GLP Methodologies and Documentation
The Study Protocol
Every GLP study must be conducted according to a pre-approved, written protocol that acts as the study's master blueprint [2] [1]. The protocol must detail objectives, test system, study design, methods, materials, and schedules, ensuring all personnel understand the plan before initiation [1].
Standard Operating Procedures (SOPs)
SOPs are documented procedures for routine operations, from instrument use and animal care to data handling [2] [8]. They are the foundation for consistency and quality control, minimizing variability and errors. Any deviation from an SOP must be authorized by the Study Director and documented [1].
Data Integrity and Good Documentation Practice (GDocP)
Data integrity under GLP is often described by the ALCOA+ principles [4]:
- Attributable (who created the data)
- Legible (readable)
- Contemporaneous (recorded at the time of the activity)
- Original (the first recording)
- Accurate (error-free)
- Plus Complete, Consistent, Enduring, and Available [4]
All raw data, including chromatograms, notebook entries, and instrument printouts, must be preserved to allow for full reconstruction of the study [9].
The Final Report and Archiving
The Final Report, prepared and signed by the Study Director, provides a complete account of the study [2] [1]. It must describe any deviations from the protocol, present and interpret results, and include the QAU's audit statement. Upon completion, all raw data, documentation, and specimens are archived. Retention periods are mandated by regulation; for example, data supporting an FDA application must be kept for at least five years after submission [2] [1].
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Reagents and Materials for GLP-Compliant Analysis
| Item | GLP-Specific Function & Importance |
|---|---|
| Test Article (Drug Substance) | The item under investigation; requires full characterization (identity, purity, stability) per §58.105 to define what is being tested [2] [4]. |
| Control Article (Reference Item) | Provides a baseline for comparison; must be appropriately characterized and handled to ensure validity of the study results [1]. |
| Certified Reference Standards | For instrument calibration and method validation; their traceability and purity are critical for data accuracy [9]. |
| Reagents & Solutions | Must be labeled with identity, titer, expiration date, and storage conditions per §58.83 to ensure reliability of analytical procedures [2]. |
| Biological Matrices | Blood, plasma, urine from test systems; stability of the analyte in these matrices must be established to assure result integrity [4]. |
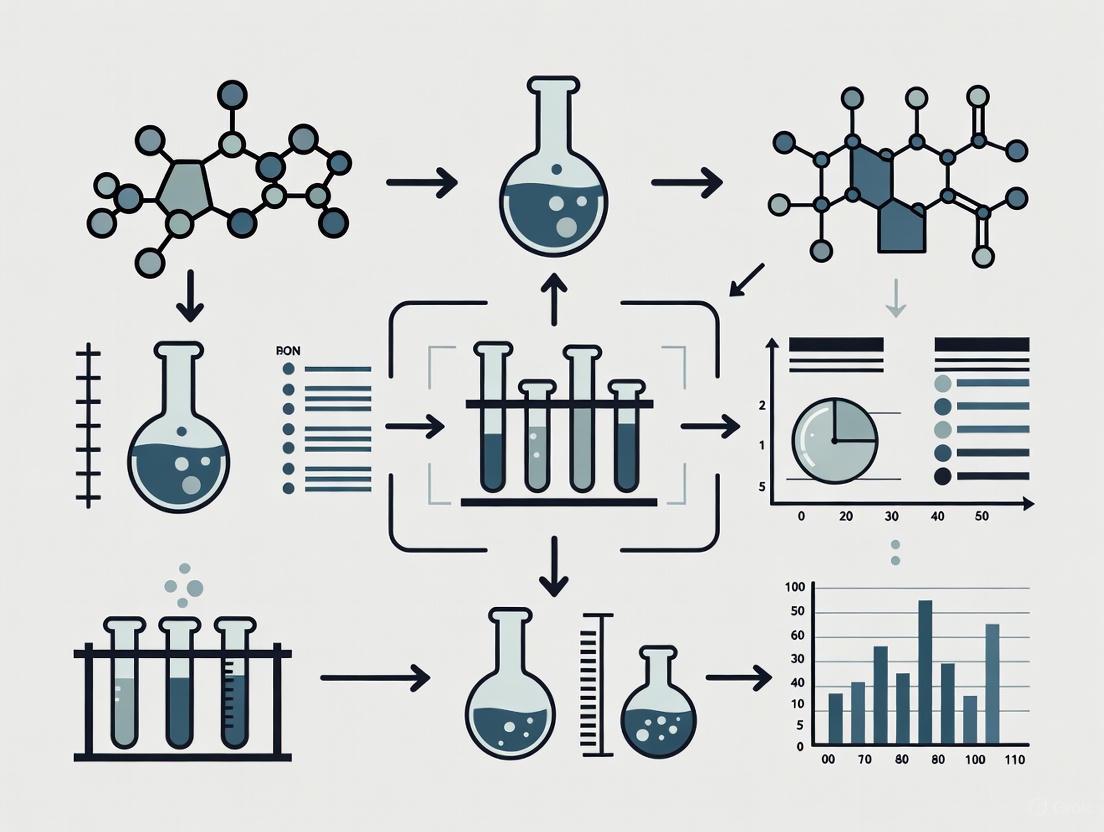
GLP-Compliant Experimental Workflow
The following diagram illustrates the core workflow of a GLP study, from initiation to archiving, highlighting the critical review points by the Study Director and QAU.
GLP Study Workflow Overview
Good Laboratory Practice provides an indispensable framework for generating reliable, defensible nonclinical safety data. For analytical chemists and drug development professionals, a thorough understanding of GLP's history, regulatory scope, and core principles—from the pivotal role of the Study Director and independent QAU to the rigorous demands of data integrity—is not merely a regulatory obligation. It is a fundamental component of scientific excellence, ensuring that the safety data underpinning new medicines can be trusted by regulators, the scientific community, and ultimately, the patients who will use them.
Good Laboratory Practice (GLP) is a quality system covering the organizational processes and conditions under which non-clinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and archived [10]. Originally developed in response to cases of laboratory fraud and misconduct in the 1970s, GLP regulations were enacted to ensure the quality, reliability, and integrity of safety test data submitted to regulatory authorities [4] [2]. Unlike methods that assess scientific validity, GLP focuses on process quality control, ensuring that data from nonclinical studies are accurate, reproducible, and auditable. For analytical chemists and drug development professionals, understanding GLP is essential for generating regulatory-submission-ready data that protects public health by providing trustworthy evidence of product safety [2].
Scope and Application of GLP Regulations
Types of Studies and Products Covered
GLP principles apply to non-clinical safety testing of various regulated products. The core requirement is that these principles govern "non-clinical" testing of items examined under laboratory conditions or in the environment, excluding studies using human subjects [10].
Table 1: Product Categories and Study Types Under GLP Regulations
| Product Categories Covered | Examples of GLP Study Types |
|---|---|
| Pharmaceutical products [10] | Physical-chemical testing [10] |
| Pesticide products [10] | Toxicity studies (acute, chronic) [10] [4] |
| Cosmetic products [10] | Mutagenicity studies [10] |
| Veterinary drugs [10] | Environmental toxicity studies [10] |
| Food and feed additives [10] | Studies on behavior in water, soil, and air [10] |
| Industrial chemicals [10] | Bioaccumulation studies [10] |
| Medical devices (in some jurisdictions) [10] | Analytical and clinical chemistry testing [10] |
For drug development, GLP compliance is mandatory for pivotal nonclinical safety studies conducted before first-in-human clinical trials. These typically include pharmacology/drug disposition and toxicology (safety) evaluations, which investigate the pharmacological effects, mechanisms of action, and toxicological profiles of investigational products [4]. Specifically, toxicokinetic (TK) studies determine drug concentration at exaggerated levels to understand toxicity, while pharmacokinetic (PK) studies determine bioavailability and absorption, distribution, metabolism, and excretion (ADME) characteristics [4].
Key Regulatory Frameworks and Their Jurisdictions
Three major GLP frameworks form the cornerstone of global regulatory compliance, with significant alignment between them.
Table 2: Comparison of Major GLP Regulatory Frameworks
| Framework | Jurisdiction & Authority | Key Document References | Notable Characteristics |
|---|---|---|---|
| 21 CFR Part 58 | United States (FDA) [11] | 21 CFR Part 58 [11] | Legally binding US regulation; applies to products under FDA purview [4] |
| OECD Principles of GLP | OECD Member Countries (38+) [10] [4] | OECD Series on Principles of GLP [10] | Facilitates international data acceptance via Mutual Acceptance of Data (MAD) system [2] |
| EPA GLP Regulations | United States (Environmental Protection Agency) [4] | 40 CFR 160 (FIFRA), 40 CFR 792 (TSCA) [4] | Regulates chemicals, pesticides, and other environmental agents [4] |
The OECD Principles of GLP serve as a global benchmark, with member countries establishing national GLP Compliance Monitoring Programmes (CMPs) responsible for monitoring GLP compliance through test facility inspections and study audits [10]. A facility found compliant is recognized as a GLP compliant test facility, and its data is accepted across OECD member countries [10]. The FDA similarly conducts careful inspections of facilities performing nonclinical laboratory studies to determine compliance with 21 CFR Part 58 [6].
Core Principles and Regulatory Requirements
Organizational Structure and Personnel Responsibilities
Effective implementation of GLP requires a clear organizational structure with defined roles and responsibilities. The following diagram illustrates the key personnel and their relationships in a GLP-compliant facility.
Key responsibilities for each role include:
- Test Facility Management: Provides adequate resources, appoints the Study Director, and establishes a Quality Assurance Unit (QAU) independent of study conduct [10] [2].
- Study Director: Serves as the single point of control with ultimate responsibility for the overall conduct of the study and final report [10]. This includes ensuring compliance with the protocol and GLP principles.
- Quality Assurance Unit (QAU): Monitors GLP compliance through audits of processes, raw data, and reports, maintaining independent oversight without being directly involved in study conduct [4] [2].
- Study Personnel: Must possess the education, training, and experience required to perform their assigned functions and comply with all GLP regulations relevant to their activities [2].
Facilities, Equipment, and Testing Operations
GLP regulations specify requirements for the physical environment and equipment to ensure study integrity:
- Facility Design: Laboratories must have adequate size, construction, and separation to prevent cross-contamination and mix-ups [11] [2]. This includes designated areas for test system handling, test article storage, and laboratory operations.
- Equipment Standards: All equipment used in generation, measurement, or assessment of data must be of appropriate design and adequate capacity, properly maintained and calibrated according to written Standard Operating Procedures (SOPs) [11] [2].
- Animal Care: Facilities housing animal test systems must have proper environmental controls (lighting, temperature, humidity) and sanitation processes to ensure animal well-being and prevent disease that could confound study results [11].
- Reagents and Solutions: All laboratory reagents and solutions must be properly labeled with identity, concentration, storage requirements, and expiration date to ensure their compositional integrity throughout the study [11].
Test and Control Articles Characterization
GLP mandates rigorous characterization and handling of test and control articles:
- Characterization Requirements: Each test and control article must be appropriately characterized to determine its identity, strength, purity, composition, and stability [11] [2]. Analytical chemists develop methods to establish these characteristics.
- Stability Determination: The stability of the test and control articles must be determined to assign appropriate storage conditions and ensure the concentration does not change significantly during the study [4].
- Handling Procedures: Procedures must ensure proper receipt, identification, labeling, storage, sampling, and distribution of test and control articles to prevent mix-ups, contamination, or degradation [11].
- Mixtures with Carriers: For articles mixed with carriers (e.g., vehicle solutions, feed), studies must determine the homogeneity, concentration, and stability of the mixture to ensure consistent dosing throughout the administration period [11].
Protocols and Study Conduct
Each nonclinical laboratory study requires a written, approved protocol that clearly defines the study's objectives and all methods for its conduct [11]. The protocol must include:
- Identification Information: Descriptive title, statement of purpose, test and control article identification, and sponsor/facility information.
- Experimental Design: Detailed study design including methods for controlling bias, number of test system units, and application of test articles including dosage levels and frequency.
- Data Collection: Type and frequency of tests, measurements, and observations to be made, along with statistical methods for data analysis.
- Study Amendments: Any changes to the protocol must be documented as formal amendments signed by the Study Director, maintaining the study's audit trail [11].
Records, Reports, and Archiving
Documentation and data integrity form the foundation of GLP compliance:
- Final Study Report: For each study, a comprehensive final report must include all protocol information, statistical methods, test article characterization, raw data storage information, and study results and conclusions signed by the Study Director [11].
- Data Integrity (ALCOA+): Good Documentation Practice (GDocP) follows the ALCOA+ principles: Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available [4]. All data must be recorded directly, promptly, and legibly in ink.
- Record Retention: All raw data, documentation, protocols, final reports, and specimens (except those subject to degradation) must be retained in archives for specified periods, typically several years after study completion [11] [2].
- Electronic Records: Computerized systems used in GLP studies must be validated, maintained, and controlled to ensure data integrity and compliance with electronic records requirements [10].
GLP Implementation for Analytical Chemists
Key Methodologies and Experimental Protocols
Analytical chemists play crucial roles in GLP-compliant studies through two primary functions: test article characterization and bioanalytical testing of samples from test systems.
Table 3: Analytical Chemistry Functions in GLP Studies
| Analytical Function | Key Responsibilities | Common Techniques & Methods |
|---|---|---|
| Test Article Characterization | Determine identity, strength, purity, composition, stability of test substances and formulations [4] | HPLC-UV, GC, MS, dissolution testing, physicochemical characterization [4] |
| Bioanalytical Testing | Analyze drug/metabolite concentrations in biological matrices from test systems; support TK/PK studies [4] | LC-MS/MS, ELISA, immunogenicity assays [4] |
| Dose Formulation Analysis | Confirm homogeneity and stability of test article in carrier vehicles; verify concentration during administration [4] | HPLC, UV-Vis spectroscopy [4] |
Test Article Characterization Protocol
Objective: To determine the identity, strength, purity, composition, and stability of test and control articles under GLP compliance [4] [2].
Methodology:
- Reference Standard Qualification: Establish qualified reference standards for comparison using orthogonal analytical techniques (e.g., HPLC, NMR, MS) to confirm identity and purity.
- Test Article Analysis: Perform phase-appropriate method validation for GLP studies, recognizing limited degradation data in early development [4].
- Stability Monitoring: Establish stability-indicating methods to assign appropriate storage conditions and ensure concentration remains within established ranges throughout the study [4].
- Documentation: Record all procedures, results, and instrument calibration data contemporaneously following ALCOA+ principles in electronic laboratory notebooks (ELNs) [4].
Bioanalytical Method Validation Protocol
Objective: To validate bioanalytical methods for quantitative measurement of drugs and their metabolites in biological matrices per ICH M10 guidelines [4].
Methodology:
- Precision and Accuracy: Determine intra-day and inter-day variability using quality control samples at multiple concentrations across multiple runs.
- Selectivity and Specificity: Verify ability to measure analyte unequivocally in presence of other components, evaluating potential interference from matrix components, metabolites, or co-administered medications [4].
- Stability Assessments: Evaluate analyte stability under various conditions: bench-top, frozen, freeze-thaw cycles, and processed sample stability [4].
- Matrix Effect Evaluation: For LC-MS methods, assess ion suppression/enhancement using samples from multiple sources, especially for rare disease populations with potentially different matrix compositions [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for GLP-Compliant Analysis
| Reagent/Material | Function & Application in GLP Studies | Quality & Documentation Requirements |
|---|---|---|
| Certified Reference Standards | Quantification and identity confirmation of test articles; method calibration [4] | Certificate of Analysis (CoA) documenting source, purity, and characterization data [4] |
| LC-MS Grade Solvents | Mobile phase preparation for HPLC and LC-MS analyses to minimize background interference | Must be properly labeled with receipt date, expiration date, and storage conditions [11] |
| Biological Matrix Samples | Method development and validation using appropriate matrices (plasma, serum, tissue) [4] | Documented source, collection method, and storage conditions; screening for inherent abnormalities [4] |
| Quality Control Materials | Intra-study monitoring of method performance accuracy, precision [4] | Prepared at low, medium, and high concentrations from independent weighings; stability documentation [4] |
Global Harmonization and Compliance Monitoring
International Convergence and Mutual Acceptance
The OECD Principles of GLP represent the cornerstone of international harmonization, enabling the Mutual Acceptance of Data (MAD) system where studies conducted in accordance with OECD GLP Principles in one member country must be accepted by other member countries [10] [2]. This framework eliminates redundant testing, reduces administrative burdens, and conserves resources while maintaining high-quality safety standards. The OECD Working Party on GLP maintains and updates guidance through Consensus and Advisory Documents that address specific technical aspects of GLP implementation, such as application to field studies, multi-site studies, in vitro studies, and computerised systems [10].
Compliance Monitoring and Inspection Procedures
National GLP Compliance Monitoring Programmes (CMPs) verify GLP compliance through regular inspections of test facilities and audits of GLP studies [10]. The inspection process typically involves:
- Facility Inspections: Comprehensive evaluation of organizational structure, facilities, equipment, procedures, and personnel qualifications to assess overall GLP compliance [10] [6].
- Study Audits: Examination of ongoing or completed studies to verify adherence to protocols, SOPs, and proper documentation practices [10].
- Corrective Actions: Facilities must address any deficiencies identified during inspections to maintain their GLP compliant status [10].
- Data Integrity Verification: Specific focus on computerized system validation, electronic records management, and data traceability in accordance with OECD GLP Advisory Document No. 17 on Computerised Systems [10].
The framework established by 21 CFR Part 58, OECD Principles of GLP, and related regulations provides a comprehensive quality system for ensuring the reliability and integrity of nonclinical safety data. For analytical chemists and drug development professionals, understanding these regulations is not merely a compliance exercise but a fundamental aspect of generating scientifically sound, regulatory-ready data. The continued global harmonization of GLP standards through organizations like OECD facilitates international acceptance of safety data, ultimately contributing to more efficient development of safe products worldwide. As regulatory science evolves, GLP principles continue to adapt to new technologies and testing paradigms while maintaining their core mission: ensuring that safety decisions are based on trustworthy, verifiable, and high-quality laboratory data.
Good Laboratory Practice (GLP) constitutes a pivotal quality system governing the organizational processes and conditions under which nonclinical laboratory studies are planned, performed, monitored, recorded, reported, and archived [4]. Enacted in 1978 and codified in Title 21 of the Code of Federal Regulations Part 58 (21 CFR Part 58), GLP regulations were established primarily to ensure the quality, reliability, and integrity of safety test data submitted to regulatory agencies like the U.S. Food and Drug Administration (FDA) and the Environmental Protection Agency (EPA) [4] [2]. These regulations apply specifically to nonclinical safety studies that support research or marketing permits for products including human and animal drugs, biologics, medical devices, and food additives [4] [2]. For analytical chemists, understanding GLP is fundamental, as their work in characterizing test articles and analyzing biological specimens forms the bedrock of credible nonclinical safety assessment.
The principal objective of GLP is to assure regulatory authorities that the safety data presented are a truthful and accurate representation of the study findings, thereby enabling valid risk assessments [2]. This is achieved through a framework emphasizing process standardization, meticulous documentation, and independent quality oversight. It is crucial to recognize that GLP is a quality system concerned with the process of data collection and documentation; it does not judge the scientific validity of a study's hypothesis but ensures that whatever was done can be accurately reconstructed and verified [2]. This distinction is paramount for analytical chemists, for whom data integrity is non-negotiable.
Within the drug development lifecycle, GLP governs the pivotal nonclinical safety studies conducted before first-in-human clinical trials [4]. These typically include pharmacology/drug disposition studies, which investigate a drug's pharmacological effects and its absorption, distribution, metabolism, and excretion (ADME), and toxicology studies, which monitor toxic effects in vitro and in vivo [4]. Pharmacokinetic (PK) and toxicokinetic (TK) studies are central to this phase, determining the concentration of a drug candidate in animals over time to establish safety margins and human equivalent doses [4]. The principles of GLP, while mandated for these nonclinical studies, are often adopted and combined with Good Clinical Practice (GCP) for clinical bioanalytical testing, a hybrid standard known as Good Clinical Laboratory Practice (GCLP) [4].
Regulatory Framework and Key Principles
The GLP regulatory landscape is multifaceted, involving both national and international authorities. In the United States, the FDA's GLP regulations are detailed in 21 CFR Part 58, while the EPA promulgates its own GLP standards under 40 CFR 160 (FIFRA) and 40 CFR 792 (TSCA) for pesticides and industrial chemicals, respectively [4] [12]. Internationally, the Organization for Economic Cooperation and Development (OECD) has established harmonized GLP principles that have been adopted by its 38 member countries, facilitating the mutual acceptance of data (MAD) across national borders [4] [2]. The European Union operates under Directives 2004/9/EC and 2004/10/EC, which align with OECD principles and require member states to designate GLP inspection authorities [7].
A foundational element of this framework is the definition of key roles and responsibilities within a testing facility, as outlined in the table below.
Table 1: Key Personnel Roles and Responsibilities under GLP
| Role | Primary Responsibility | Key Duties |
|---|---|---|
| Study Director | Single point of control and ultimate responsibility for the overall conduct of the study and its final report [1] [7]. | Approves the study protocol and any amendments; ensures GLP compliance; interprets, analyzes, and documents results; approves the final report [1]. |
| Quality Assurance Unit (QAU) | An independent entity that monitors GLP compliance [2] [7]. | Conducts in-study inspections; audits final reports for accuracy and compliance; reports findings directly to management and the Study Director [1] [2]. |
| Testing Facility Management | Provides overall organization and resources [1]. | Appoints the Study Director and QAU; ensures adequate personnel, facilities, and equipment are available [1]. |
| Analytical Chemist | Executes laboratory analyses related to test article characterization and bioanalysis [4]. | Develops and validates analytical methods; performs analysis; documents all activities in compliance with GDocP principles [4]. |
The core principles of GLP can be distilled into ten key areas, as defined by the OECD and other regulatory bodies. These principles provide the structural backbone for any GLP-compliant study [4] [1]:
- Test Facility Organization and Personnel: A clear organizational structure with defined responsibilities and appropriately qualified personnel.
- Quality Assurance Programme: An independent QAU responsible for monitoring GLP compliance.
- Facilities: Adequate, well-separated facilities to prevent cross-contamination and interference.
- Apparatus, Material, and Reagents: Properly designed, calibrated, and maintained equipment.
- Test Systems: Proper characterization, housing, and care of test systems (e.g., animals, cells).
- Test and Reference Items: Thorough characterization, handling, and storage to ensure stability and prevent mix-ups.
- Standard Operating Procedures (SOPs): Documented procedures for all routine operations.
- Performance of the Study: A written, approved study protocol and adherence to it during conduct.
- Reporting of Study Results: A final report that accurately and completely describes the study and its results.
- Storage and Retention of Records and Materials: Secure archiving of all raw data, documentation, specimens, and reports for defined retention periods [1].
For the analytical chemist, Good Documentation Practice (GDocP) is a pervasive and critical requirement. Often described by the acronym ALCOA+, data and records must be Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available [4]. This means all laboratory activities, from weighing materials to integrating chromatographic peaks, must be recorded in real-time, using electronic laboratory notebooks (ELNs) and other systems that ensure full traceability and data integrity.
The Analytical Chemist in Test Article Characterization
A primary responsibility of the analytical chemist in a GLP environment is the comprehensive characterization of the test and control articles. As mandated by 21 CFR 58.105, this involves determining the identity, strength, purity, composition, and stability of the articles to appropriately define them for the study [4] [2]. The data generated is essential for confirming that the test system is exposed to the correct, consistent material throughout the study, which is fundamental to interpreting toxicological outcomes.
Core Responsibilities and Methodologies
The analytical chemist's role in test article characterization encompasses several critical activities:
- Method Development and Validation: Developing phase-appropriate analytical methods, typically using High-Performance Liquid Chromatography with UV detection (HPLC-UV) for small molecules, to assess key characteristics of the test article [4]. These methods must be validated to demonstrate they are suitable for their intended purpose, even at this early stage of development.
- Stability Assessment: Establishing the stability of the test article and its formulations (dosing solutions) under storage and use conditions is mandatory. This ensures the concentration and integrity of the article do not change significantly from the start to the end of the study, thereby validating the doses administered to the test system [4].
- Characterization of Formulations: For toxicology studies, the test article is often administered in a simple carrier or formulation. The chemist must analyze these mixtures to confirm homogeneity and concentration, ensuring uniform exposure across all test subjects [4].
The workflow for test article characterization is a meticulous, multi-stage process that ensures data integrity from sample receipt to final reporting, as illustrated below.
Essential Research Reagent Solutions
The work of characterization relies on a suite of specific reagents and materials, each serving a critical function in ensuring accurate and reliable results.
Table 2: Key Research Reagents and Materials for Test Article Characterization
| Reagent/Material | Function | GLP Compliance Consideration |
|---|---|---|
| Certified Reference Standards | Serves as the benchmark for determining identity, purity, and strength of the test article via comparison. | Must be fully characterized, with certificates of analysis (CoA) and stored according to specified conditions [4]. |
| HPLC-Grade Solvents | Used for mobile phases, sample dilution, and dissolution to ensure minimal interference and high signal-to-noise ratios. | Must be tracked for lot number and expiry; prepared and labeled in accordance with SOPs (§58.83) [2]. |
| Characterized Test & Control Articles | The substances being studied (test article) and compared against (control article). | Requirement for complete characterization (§58.105) including stability; chain of custody must be maintained [4] [1]. |
The Bioanalytical Chemist in Nonclinical Study Support
While the analytical chemist focuses on the test article itself, the bioanalytical chemist is responsible for measuring the concentration of the drug and its metabolites in biological matrices collected from the test system. This data is the cornerstone of PK and TK studies, which aim to demonstrate the drug's bioavailability, its fate in a living organism, and its relationship to observed toxicity [4]. This role is governed by 21 CFR 58.120 and 58.130, and the methods employed must be validated in accordance with international guidelines like the ICH M10 guideline on bioanalytical method validation [4].
Analytical Techniques and Method Validation
Bioanalytical chemists employ a range of sophisticated techniques tailored to the type of drug molecule being analyzed.
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS): This is the workhorse for the quantitative analysis of small molecule drugs and some peptides in biological fluids [4] [13]. It offers high selectivity, specificity, and a wide linear dynamic range (typically 3-4 orders of magnitude) [13].
- Ligand Binding Assays (LBA): Techniques like Enzyme-Linked Immunosorbent Assay (ELISA) and electrochemiluminescence (e.g., on MSD platforms) are typically used for large molecule drugs, such as therapeutic proteins and antibodies [4] [13]. LBAs can offer very high sensitivity (down to pg/mL) but may have a narrower quantitative range and be more susceptible to matrix effects [13].
For a method to be deemed GLP-compliant, it must undergo a rigorous validation process. Core validation parameters include precision, accuracy, selectivity, and specificity [4]. Additional experiments characterize the assay's performance, including the stability of the analyte in the biological matrix (e.g., at room temperature, frozen, and through freeze-thaw cycles) and the potential for interference from co-administered medications or the biological matrix itself [4].
A particularly complex area for the bioanalytical chemist is the analysis of modern biologic drugs, such as GLP-1 analogs (e.g., semaglutide, liraglutide). These molecules present unique challenges, including complex sample preparation to isolate the analyte from the biological matrix and their tendency to adsorb to surfaces within the LC-MS/MS system due to structural modifications like added lipid chains [13].
Specialized Area: Immunogenicity Testing
For biologic drugs, bioanalytical support extends beyond PK analysis to include immunogenicity testing [4] [13]. Immunogenicity is the tendency of a biologic drug to elicit an unwanted immune response, which can impact the drug's efficacy and safety [4]. Testing is a multi-tiered process typically involving:
- Screening Assays: To identify samples that contain anti-drug antibodies (ADAs).
- Confirmatory Assays: To verify that the immune response is specific to the drug.
- Neutralizing Antibody (NAb) Assays: To determine if the ADAs can block the biological activity of the drug.
These assays often use sophisticated LBA platforms like electrochemiluminescence or cell-based assays for NAb detection [4] [13]. The complexity of these analyses demands careful method development, particularly for smaller biologic drugs where labeling efficiency for assays can be low [13].
The following diagram outlines the integrated workflow for supporting a nonclinical study, from sample collection to data reporting.
Emerging Trends and Future Directions
The field of GLP-compliant analysis is not static; it is being reshaped by technological advancements that promise to enhance efficiency, data quality, and analytical capabilities.
- Laboratory Automation: Automated systems, particularly for sample preparation (e.g., pipetting robots), are becoming integral to handling large sample volumes from nonclinical studies [14]. These systems improve reproducibility, reduce human error, and free up skilled chemists for more complex tasks [14]. The trend is moving towards end-to-end automated workflows that integrate sample registration, preparation, analysis, and data evaluation.
- Digitalization and Data Integrity: The increasing digitalization of the laboratory, through Laboratory Information Management Systems (LIMS) and ELNs, ensures consistent data capture and facilitates compliance with GDocP and 21 CFR Part 11 (electronic records) [14]. The Internet of Things (IoT) allows for real-time monitoring of instrument conditions and sample storage environments, further safeguarding data integrity [14].
- Artificial Intelligence (AI): AI and machine learning are beginning to be applied to optimize laboratory processes, adjust method parameters in real-time, and assist in data review, potentially leading to faster and more precise analyses [14].
- Advanced Analytical Platforms: The ongoing evolution of LC-MS/MS and LBA platforms continues to push the boundaries of sensitivity and throughput. For complex molecules like GLP-1 analogs, the use of multiple analytical platforms (LC-MS/MS and LBA) is often necessary to overcome specific challenges like adsorption and to provide complementary data sets for regulatory submissions [13].
The role of the analytical and bioanalytical chemist is indispensable within the GLP framework. From the initial characterization of the test article to the complex quantification of drug levels in biological matrices, their work generates the foundational data upon which critical safety decisions are made. Adherence to the rigorous principles of GLP—through qualified personnel, validated methods, calibrated equipment, meticulous documentation, and independent quality assurance—is what transforms routine laboratory analysis into reliable, auditable, and defensible evidence for regulatory review. As drug modalities become more complex and technologies continue to advance, the chemist's expertise in adapting and applying these principles will remain a cornerstone of ethical and successful drug development.
For researchers, scientists, and drug development professionals, Good Laboratory Practice (GLP) constitutes a foundational quality system that ensures the integrity and reliability of nonclinical safety data. GLP is not merely a set of technical procedures but a comprehensive managerial quality control system covering the organizational processes and conditions under which non-clinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and archived [10]. For analytical chemists, particularly those supporting drug development, adherence to GLP principles is mandatory for pivotal nonclinical studies submitted to regulatory authorities like the FDA and EPA to support applications for research or marketing permits [15] [16]. This whitepaper delves into the four core pillars of GLP—Organization, Personnel, the Study Director, and the Quality Assurance Unit (QAU)—framing them within the specific context of the analytical laboratory's critical role in the drug development pipeline.
The Five Fundamental Points of GLP
The GLP framework rests on five interdependent fundamental points that together guarantee data quality and regulatory acceptance. These principles are:
- Organization and Personnel: The foundation of GLP, requiring a clear organizational structure with qualified, trained staff who understand their responsibilities [17] [18].
- Facilities and Equipment: Laboratories must maintain controlled, fit-for-purpose environments and properly calibrated, validated, and maintained instruments [17].
- Standard Operating Procedures (SOPs): Every critical task must be governed by written, approved procedures to ensure consistency and reproducibility of all operations [17] [16].
- Study Documentation and Reporting (Raw Data & Final Report): All raw data must be recorded promptly, accurately, and traceably, with final reports accurately reflecting the raw data [17].
- Quality Assurance (QA) Unit: An independent monitoring system must be in place to verify that all aspects of the study comply with GLP principles [17] [16].
These components form a cohesive system designed to produce studies that are scientifically sound, auditable, and defensible, providing regulatory agencies with confidence in the submitted data.
Detailed Analysis of Core GLP Pillars
Organization and Personnel
The GLP principles mandate a well-defined organizational structure with clear lines of authority and responsibility. Sufficient personnel with appropriate qualifications are essential for the timely and proper conduct of a study [19] [18].
Key Responsibilities: Test Facility Management holds the ultimate responsibility for the entire organization's compliance with GLP. Their extensive duties, as outlined by OECD, FDA, and EPA, are summarized in the table below [19] [18].
Table 1: Key Responsibilities of Test Facility Management
| Responsibility Area | Specific Requirement |
|---|---|
| Resources & Personnel | Ensure sufficient qualified personnel, facilities, equipment, and materials are available [18]. Maintain records of qualifications, training, and job descriptions [19]. |
| Study Oversight | Designate and replace (if necessary) a Study Director before a study is initiated [18]. For multi-site studies, designate a Principal Investigator as needed [19]. |
| Quality System | Ensure the establishment of a Quality Assurance Programme and approve all original and revised SOPs [19] [18]. |
| Facility Operations | Ensure test and reference items are appropriately characterized and that facility supplies meet requirements [18]. Maintain a master schedule of all studies [19]. |
Personnel Requirements: All individuals engaged in a study must possess the education, training, and experience necessary to perform their assigned functions [18]. Key requirements for study personnel include:
- Access and Compliance: Personnel must have access to the study plan and relevant SOPs and are responsible for complying with their instructions [18].
- Data Integrity: All personnel are responsible for recording raw data promptly, accurately, and in compliance with GLP principles, bearing direct responsibility for the quality of the data they generate [19] [18].
- Health Precautions: Personnel must take necessary personal sanitation and health precautions to avoid contaminating test systems and articles. They must report any medical condition that could adversely affect the study's integrity [18].
The Study Director: The Single Point of Control
The Study Director is the central pillar of any GLP study, serving as the "single point of study control" [20]. According to 21 CFR Part 58, this individual must be "a scientist or other professional of appropriate education, training, and experience" who assumes overall responsibility for the technical conduct of the study, as well as for the interpretation, analysis, documentation, and reporting of results [20].
Table 2: Core Responsibilities of the Study Director
| Responsibility | Description |
|---|---|
| Protocol Approval & Adherence | Approve the study protocol and any amendments, and ensure they are followed [20]. |
| Data Integrity | Ensure all experimental data, including observations of unanticipated responses, are accurately recorded and verified [20]. |
| Issue Management | Document unforeseen circumstances affecting the study, and implement and document corrective action [20]. |
| GLP Compliance | Assure that all applicable GLP regulations are followed throughout the study [20]. |
| Archiving | Ensure all raw data, documentation, protocols, specimens, and final reports are transferred to the archives upon study completion [20]. |
The Study Director acts as the primary communicator, liaising between management, the QAU, and study personnel. In multi-site studies, the Study Director may delegate specific supervisory duties for a defined phase of the study to a Principal Investigator, who then acts on the Study Director's behalf while ensuring their phase is conducted per the protocol, SOPs, and GLP [19].
The Quality Assurance Unit: The Independent Guarantor of Quality
The Quality Assurance Unit (QAU) is an independent entity within the test facility that provides assurance to management that the facilities, equipment, personnel, methods, practices, records, and controls are in compliance with GLP regulations [16]. The QAU is critical for maintaining objective oversight as its personnel must not be involved in the conduct of the study they are assuring [19].
The following diagram illustrates the logical relationships and workflow between the core personnel in a GLP-compliant study, highlighting the QAU's independent oversight role.
Diagram 1: GLP Personnel Relationships & Workflow (Width: 760px)
QAU Activities and Audits: The QAU's mandate is fulfilled through a systematic process of audits and inspections, which include [21]:
- Facility Audits: Assessing if the facility is fit for purpose and has the necessary supporting documentation.
- Process and Study-Based Inspections: Observing personnel in the laboratory to ensure they follow procedures and work in compliance with GLP.
- Study Plan and Final Report Audits: Reviewing the protocol and the final report to ensure the report accurately reflects the raw data and contains all required elements.
- Audit of Computerized Systems: Reviewing validation documentation and ongoing maintenance of systems used to generate or manipulate study data.
After each inspection, the QAU must promptly report findings in writing to management and the Study Director. Ultimately, the QAU prepares and signs a statement included in the final report, specifying the inspection dates and types and confirming that the report accurately reflects the raw data [19] [16].
GLP in Practice: An Analytical Chemist's Perspective
For analytical and bioanalytical chemists, GLP implementation translates into specific, rigorous practices tailored to their functions.
Key Methodologies and Experimental Protocols
1. Test Article Characterization and Stability Monitoring: The analytical chemist is responsible for developing and validating methods to characterize the test article (drug substance or formulation) to determine its identity, strength, purity, composition, and other defining characteristics [15].
- Detailed Methodology:
- Method Development & Validation: Develop phase-appropriate analytical methods, often using High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) for small molecules. The equipment must have proper qualification documentation [15].
- Stability Assessment: Conduct stability studies on the test and control articles (e.g., drug substance and dosing solution) under specified storage conditions. This involves testing samples over time to establish that the concentration and properties of the test article do not change significantly from manufacture through the study's end [15].
- Homogeneity Testing: For formulations, ensure the test article is homogeneously mixed or suspended.
2. Bioanalytical Method Validation and Sample Analysis: The bioanalytical chemist is responsible for analyzing biological specimens (blood, plasma, urine, tissues) collected from test systems after administration of the test article, supporting pharmacokinetic (PK) and toxicokinetic (TK) studies [15].
- Detailed Methodology:
- Method Validation per ICH M10: Validate bioanalytical methods in accordance with international guidelines. Core validation parameters include [15]:
- Precision and Accuracy: Evaluate across multiple validation runs.
- Selectivity and Specificity: Demonstrate the method can unequivocally assess the analyte in the presence of other components like metabolites or endogenous substances. Selectivity must be evaluated in relevant populations.
- Stability: Determine analyte stability in the biological matrix under various conditions (room temperature, frozen, freeze-thaw cycles).
- Sample Analysis: Use techniques like LC-MS/MS for small molecules or ELISA for large molecules to measure drug and metabolite concentrations. The process must adhere to a strict chain of custody for all specimens [15].
- Method Validation per ICH M10: Validate bioanalytical methods in accordance with international guidelines. Core validation parameters include [15]:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents essential for an analytical chemist conducting GLP-compliant studies.
Table 3: Essential Research Reagent Solutions for GLP-Compliant Analysis
| Item / Reagent | Function in GLP Studies |
|---|---|
| Certified Reference Standards | To calibrate instruments and verify method accuracy for test article characterization. Essential for generating definitive data on identity, strength, and purity [15]. |
| Chromatography Columns & Supplies | For HPLC and LC-MS systems to separate and resolve the analyte of interest from complex matrices (e.g., formulated drug product or biological samples) [15]. |
| Mass Spectrometry-Grade Solvents & Reagents | To ensure minimal interference and background noise during highly sensitive bioanalytical assays (e.g., PK/TK analysis), preventing inaccurate concentration measurements [15]. |
| Characterized Biological Matrices | (e.g., control plasma, serum). Used as the blank matrix for preparing calibration standards and quality control samples during bioanalytical method validation and sample analysis [15]. |
| Stable Isotope-Labeled Internal Standards | Used in LC-MS/MS bioanalysis to correct for variability in sample preparation and ionization efficiency, significantly improving data accuracy and precision [15]. |
| Quality Control (QC) Samples | Prepared at low, mid, and high concentrations from a separate weighing of the reference standard. Their analysis throughout a sample run validates the assay's performance and the integrity of the reported unknown sample concentrations [15]. |
Data Integrity and Documentation: The ALCOA+ Principle
Adherence to Good Documentation Practice (GDocP) is non-negotiable. For the analytical chemist, this means all data must be recorded in accordance with the ALCOA+ principle, which dictates that data must be [15]:
- Attributable (who recorded it and when),
- Legible,
- Contemporaneous (recorded at the time of the activity),
- Original (or a certified copy),
- Accurate. Furthermore, data should be Complete, Consistent, Enduring, and Available [15]. This is typically achieved using controlled laboratory notebooks, either electronic or paper-based, and a robust Chromatography Data System (CDS). All raw data, including electronic data and notebooks, must be archived at the study's close [20] [15].
The GLP principles are enforced by various regulatory bodies worldwide, each with its own specific regulations. The following table provides a comparative overview of key personnel requirements across major authorities.
Table 4: Regulatory Comparison of Key GLP Personnel Requirements
| Topic | FDA (21 CFR 58) | EPA (40 CFR 160/792) | OECD |
|---|---|---|---|
| Personnel Training & Experience | Education, training, experience to perform assigned functions [18]. | Education, training, experience to perform assigned functions [18]. | Personnel must be knowledgeable in applicable GLP principles [18]. |
| Summary of Training & Job Descriptions | Facility must maintain current summary for each individual [18]. | Facility must maintain current summary for each individual [18]. | Management must maintain a record of qualifications and job description [18]. |
| Designate a Study Director | Management must designate a study director before study initiation [18]. | Management must designate a study director before study initiation [18]. | Management must designate a Study Director with appropriate qualifications [18]. |
| Establish a QAU | Management must assure there is a QAU [18]. | Management must assure there is a QAU [18]. | Management must ensure a Quality Assurance Programme with designated personnel [18]. |
For analytical chemists and drug development professionals, the core GLP principles of Organization, Personnel, Study Director, and the QAU are not abstract regulations but practical necessities. They form an integrated framework that ensures the generation of high-quality, reliable, and defensible nonclinical safety data. The Study Director's role as the single point of control is paramount, providing unified scientific and managerial leadership. Simultaneously, the QAU's independent oversight and the foundational support of a well-structured organization with qualified personnel create a system of checks and balances. Mastering these principles is essential for successfully navigating the regulatory landscape and ultimately contributing to the development of safe and effective pharmaceuticals and other regulated products.
This whitepaper examines the ALCOA+ framework as a cornerstone of Data Integrity and Good Documentation Practice (GDocP) within Good Laboratory Practice (GLP) environments. Aimed at analytical chemists and drug development professionals, it provides a comprehensive technical guide for implementing these principles in analytical research, method validation, and data management. The guidelines detailed herein ensure regulatory compliance, data reliability, and scientific integrity throughout the research lifecycle.
In analytical chemistry and pharmaceutical research, data integrity forms the foundation of credible scientific results and regulatory submissions. Good Documentation Practice (GDocP) comprises the systematic approaches for creating, maintaining, and archiving records to ensure this integrity. For analytical chemists working under GLP standards, the primary objective is to generate data that is complete, consistent, and accurate from the point of acquisition through to final reporting and long-term retention [22] [23].
The U.S. Food and Drug Administration (FDA) and other international regulatory bodies mandate that all GxP data adhere to a robust framework to ensure its trustworthiness [24] [25]. The ALCOA+ principles provide this structured framework, offering a clear set of criteria that are equally applicable to paper, electronic, and hybrid records [26]. Adherence to these principles is not merely a regulatory formality but a fundamental component of a successful quality culture, ultimately protecting patient safety and product efficacy [22] [27].
The ALCOA+ Framework: Core Principles and Definitions
The ALCOA framework was first articulated by the FDA in the 1990s and has since evolved into ALCOA+ to address the complexities of modern data systems [28] [24]. The following table summarizes the core and expanded principles.
Table 1: The Core and Expanded Principles of the ALCOA+ Framework
| Principle | Acronym | Definition & Requirements |
|---|---|---|
| Attributable | A | Data must be linked to the person or system that created it. Requires recording who performed an action, what system was used, and when it occurred [22] [26] [29]. |
| Legible | L | Data must be readable and permanent, both immediately and for the entire retention period. This applies to handwriting and electronic formats, ensuring understanding over time [22] [26] [27]. |
| Contemporaneous | C | Data must be recorded at the time the activity is performed. Real-time documentation is critical to prevent errors of memory or retrospective recording [22] [29] [30]. |
| Original | O | The first or source record of data must be preserved. This includes the first capture in a notebook, electronic record, or a certified copy thereof [22] [26] [28]. |
| Accurate | A | Data must be error-free, truthful, and reflect actual observations. Any amendments must be documented without obscuring the original entry [22] [26] [29]. |
| Complete | + | All data must be present, including original entries, repeat analyses, and metadata. No data should be omitted or deleted from the dataset [22] [26] [25]. |
| Consistent | + | The data sequence should be chronologically logical. Timestamps must be consistent and follow the expected sequence of workflows [22] [26] [27]. |
| Enduring | + | Data must be recorded on durable, authorized media designed for long-term retention, surviving the required retention period (often decades) [22] [26] [25]. |
| Available | + | Data must be readily accessible for review, audit, or inspection over its entire lifetime, with proper indexing and searchability [22] [26] [27]. |
The "+" in ALCOA+: Traceability
Many modern interpretations, including ALCOA++, add a tenth principle: Traceable [28]. This emphasizes the need for a clear, documented journey for each datum, from its origin through all transformations, analyses, and reporting. A robust audit trail that captures the "who, what, when, and why" of all data changes is essential for meeting this principle and reconstructing the research process during an audit [28].
ALCOA+ in the Analytical Laboratory Workflow
For the analytical chemist, ALCOA+ principles are applied throughout the entire data lifecycle. The following diagram illustrates how these principles integrate into a typical analytical workflow.
Diagram 1: Application of ALCOA+ principles in an analytical workflow.
Experimental Protocols and Methodologies
The following detailed methodologies for common analytical procedures demonstrate the practical application of GDocP.
Protocol for HPLC Method Validation with ALCOA+
- Objective: To validate a new High-Performance Liquid Chromatography (HPLC) method for assay of an active pharmaceutical ingredient (API) in accordance with ALCOA+.
- Materials: HPLC system with validated software, reference standard, samples, and appropriate solvents.
- Procedure:
- System Suitability: Prior to analysis, perform system suitability tests (e.g., injection repeatability, theoretical plate count). The original chromatograms and accurate results must be saved directly to the network drive, not a local computer.
- Sample Analysis: Inject calibration standards and samples in sequence defined by the protocol. The contemporaneous timestamp for each injection is automatically recorded by the HPLC software's audit trail.
- Data Integration: Process chromatographic data using predefined, validated methods. Any manual integration must be attributable (logged with user ID) and accurate (justified with a reason documented in the audit trail, without obscuring the original integration).
- Calculation & Reporting: Generate the final report. The process must be complete, including all raw data, processed data, audit trail entries, and metadata. The final report must be an original record or a certified copy.
Protocol for Sample Weighting and Preparation
- Objective: To accurately weigh a sample for standard solution preparation.
- Materials: Certified analytical balance (calibrated), weighing vessels, and sample.
- Procedure:
- Tare: Place the weighing vessel on the balance and tare. Ensure the balance is connected to a printer or data capture system.
- Weighing: Add the sample to the vessel. Record the weight directly onto the controlled worksheet or via the balance's direct data output. The record must be legible and original.
- Documentation: The analyst must sign and date the entry immediately (contemporaneous). If an error is made, a single line is drawn through the mistake, the correction is written alongside, and the correction is initialed and dated (accurate, with original data preserved).
The Scientist's Toolkit: Essential Reagents and Materials
The following table details critical reagents and materials for GDocP-compliant analytical work, along with their functions and links to ALCOA+.
Table 2: Essential Research Reagent Solutions and Materials for GDocP
| Item | Function & Relevance to ALCOA+ |
|---|---|
| Controlled Laboratory Notebooks | Bound, pre-paginated notebooks with tamper-evident features provide an original, enduring medium for recording attributable data [31]. |
| Permanent Ink Pens | Use of indelible black ink ensures records are legible and permanent, preventing degradation or alteration over time [31]. |
| Certified Reference Standards | Materials with certified purity and traceability are essential for generating accurate and reliable calibration data [29]. |
| Calibrated Volumetric Glassware & Balances | Equipment regularly calibrated against traceable standards is fundamental for accurate measurement and data integrity [29] [25]. |
| Validated Chromatography Data System (CDS) | A validated CDS enforces contemporaneous data capture, maintains complete audit trails, and ensures data is consistent and available [22] [25]. |
| Secure Electronic Archives | Validated long-term storage systems ensure data remains enduring, available, and complete throughout its required retention period [26] [25]. |
Regulatory Foundation and Consequences
The ALCOA+ principles are embedded within the regulations of major international regulatory bodies, including the FDA (21 CFR Parts 11, 210, 211), EMA (Annex 11), and WHO (TRS 996) [22] [24]. Regulatory agencies conduct inspections with a focus on data integrity, and failures can lead to severe consequences, including warning letters, rejection of regulatory submissions, and consent decrees [28] [27]. Analysis indicates that a significant majority of FDA warning letters cite data integrity violations, highlighting its status as a top enforcement priority [28].
Implementing a Culture of Data Integrity
Technical controls are insufficient without a strong organizational culture of quality. The diagram below outlines the feedback loop for maintaining data integrity.
Diagram 2: The organizational lifecycle for sustaining data integrity.
Effective implementation requires:
- Management Responsibility: Leadership must allocate sufficient resources and establish a zero-tolerance policy for data manipulation [22].
- Procedures and Systems: Implement validated electronic systems with audit trails and controlled procedures for paper-based records [22] [31].
- Training: Conduct regular, role-specific training on GDocP and ALCOA+ principles to ensure all personnel are competent [22] [30].
- Audits and Monitoring: Perform routine data integrity audits and reviews of audit trails as part of a risk-based monitoring strategy [22] [28].
- Corrective and Preventive Action (CAPA): Address any identified gaps or deviations with robust CAPA processes to drive continuous improvement [22] [31].
For the analytical chemist, the ALCOA+ principles are not abstract regulatory concepts but practical, daily requirements for ensuring the integrity of every data point generated. By rigorously applying these principles through Good Documentation Practices, researchers and drug development professionals build a foundation of trust in their data. This commitment to data integrity is fundamental to meeting regulatory obligations, making sound scientific decisions, and, ultimately, ensuring the safety and efficacy of pharmaceutical products for patients.
Implementing GLP in the Laboratory: Analytical Techniques and Standard Procedures
Within the framework of Good Laboratory Practice (GLP), the rigorous characterization of a test article is a foundational prerequisite for any nonclinical laboratory study intended to support regulatory submissions for products such as human and animal drugs, biologics, and medical devices [4] [32]. GLP is a quality system that governs the organizational processes and conditions under which these pivotal nonclinical safety studies are planned, performed, monitored, recorded, reported, and archived [4]. The primary goal is to assure the quality and integrity of the safety data filed with regulatory agencies like the U.S. FDA and the EPA, thereby protecting public health [2] [32].
Test article characterization provides the critical baseline data that defines the material being evaluated in safety and toxicology studies. According to 21 CFR Part 58, characterization must include, at a minimum, the determination of the test article's identity, strength, purity, and composition, along with any other characteristics that appropriately define the substance [33] [32]. Failure to adequately characterize the test and control articles according to GLP standards will result in a compliance exception in the final study report, potentially jeopardizing the regulatory acceptance of the entire study [33]. For the analytical chemist, this process involves developing and validating phase-appropriate methods to generate reliable, auditable data that forms the cornerstone of credible safety assessment [4].
Regulatory Framework and Core Principles
Key Regulations and Standards
Test article characterization is mandated under specific sections of GLP regulations. In the United States, the FDA's 21 CFR Part 58 is the central regulation, which applies to nonclinical laboratory studies supporting applications for research or marketing permits for FDA-regulated products [2] [32]. Similarly, the Environmental Protection Agency (EPA) has established GLP standards under the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA) and the Toxic Substances Control Act (TSCA) for products under its purview [4] [34]. Internationally, the Organization for Economic Cooperation and Development (OECD) Principles of GLP have been adopted by member countries, creating a system of Mutual Acceptance of Data (MAD) that allows studies conducted in accordance with OECD guidelines to be accepted across international borders [2] [35].
While these regulations are broadly similar, key operational differences exist that laboratories must consider. For instance, the EPA typically requires a longer minimum record retention period and a specific Statement of Compliance in the final study report compared to FDA requirements [34].
The Role of the Analytical Chemist in GLP Compliance
Analytical chemists serve as the technical backbone of GLP-compliant test article characterization [34]. Their primary responsibilities encompass two main domains:
- Characterizing the Test Article: The analytical chemist develops methods to determine the identity, strength, purity, composition, and stability of the test article (drug substance) and its formulation (dosing solution) to ensure the material is suitable for the duration of the study [4]. This often involves techniques like High-Performance Liquid Chromatography (HPLC) for small molecules [4].
- Bioanalytical Support: For studies requiring it, bioanalytical chemists develop and validate methods to measure the concentration of the drug and its metabolites in biological matrices (e.g., blood, plasma, tissues) collected from test systems, in accordance with guidelines like ICH M10 [4].
A cornerstone of the chemist's role is adherence to Good Documentation Practice. The "ALCOA+" principle—ensuring data is Attributable, Legible, Contemporaneous, Original, and Accurate, plus Complete, Consistent, Enduring, and Available—is rigorously applied [4]. This means all activities, from sample weighing to data analysis, are contemporaneously recorded in an electronic laboratory notebook, with all raw data and documentation retained and archived as per standard operating procedures [4].
The Five Essential Parameters of Characterization
GLP characterization of a test article is built upon five essential points, which collectively ensure the material is fully defined and its quality is maintained throughout a nonclinical study [33].
Table 1: The Five Essential Parameters of GLP Test Article Characterization
| Parameter | Definition | Purpose in GLP Studies |
|---|---|---|
| Identity | Confirmation of the test article's fundamental chemical or biological structure. | Verifies that the correct substance is being studied. |
| Strength | The concentration of the active moiety, or the potency of a biological substance. | Ensures the test system is exposed to the correct and consistent dose. |
| Purity | The quantity of the desired substance relative to impurities, including related substances, residual solvents, and contaminants. | Assesses potential safety impacts from impurities. |
| Composition | For mixtures, the quantitative profile of all major components; for pure substances, confirmation of the stated composition. | Ensures batch-to-batch consistency and defines the material administered. |
| Stability | The capacity of a test article to remain within specified limits of identity, strength, and purity over time under defined storage conditions. | Assigns appropriate storage conditions and validates that article quality persists through study end. |
Identity and Composition
Establishing the identity of a test article is the first and most fundamental step. It confirms that the substance being administered in the study is indeed the intended compound. For chemical entities, this involves using techniques that provide structural information, such as Fourier-Transform Infrared Spectroscopy (FTIR), which identifies functional groups and molecular structure, and Mass Spectrometry (MS), which provides precise molecular weight and fragmentation patterns [33]. Ultraviolet-Visible Spectroscopy (UV-Vis) can also be used to confirm identity based on characteristic absorption spectra [33].
For test articles that are mixtures or formulations, determining composition is critical. This involves quantifying the active ingredient(s) and all major excipients or carriers to ensure the formulation is consistent and accurately represents the material intended for toxicological assessment.
Strength, Purity, and Stability
The strength (or potency) of a test article is typically determined using quantitative analytical techniques. High-Performance Liquid Chromatography is a workhorse method for this purpose, often coupled with various detectors like UV (HPLC-UV) for quantification [4] [33]. For more complex analyses or trace-level quantification, Liquid Chromatography-Mass Spectrometry is employed [33].
Purity analysis is closely linked to strength and is designed to detect and quantify impurities that could confound safety results. This involves using separation techniques capable of resolving the main active component from its impurities. HPLC with various detection methods and Gas Chromatography with detectors are commonly used [33]. The purity profile must be established for each batch of the test article used in the study.
Stability assessment is an ongoing process that monitors the test article under its storage conditions and in the dosing formulation (if applicable) throughout the study. This ensures that the concentration of the test article does not change outside established acceptance criteria from the time of manufacture until the last administration to the test system [4]. Stability-indicating methods, which can accurately measure the active ingredient in the presence of its degradation products, are essential for this purpose.
Table 2: Key Analytical Techniques for Test Article Characterization
| Technique | Acronym | Primary Application in Characterization |
|---|---|---|
| High-Performance Liquid Chromatography | HPLC | Quantification of strength, purity, and impurity profiling. |
| Gas Chromatography | GC | Analysis of volatile substances and residual solvents. |
| Mass Spectrometry | MS | Structural elucidation, identity confirmation, and trace analysis. |
| Fourier-Transform Infrared Spectroscopy | FTIR | Functional group analysis and identity confirmation. |
| Ultraviolet-Visible Spectroscopy | UV-Vis | Identity confirmation and quantification. |
| Inductively Coupled Plasma Mass Spectrometry | ICP-MS | Elemental analysis and trace metal impurity testing. |
| Ion Chromatography | IC | Analysis of ionic compounds and counterions. |
| Nuclear Magnetic Resonance | NMR | Definitive structural elucidation and identity confirmation (often outsourced). |
Experimental Workflows and Protocols
Generalized Workflow for Test Article Characterization
The following diagram illustrates the logical flow and key decision points in a GLP-compliant test article characterization process.
Detailed Methodologies for Key Experiments
Identity Confirmation via FTIR and MS
Objective: To unequivocally confirm the molecular structure and identity of the test article.
- FTIR Protocol: A small quantity (1-2 mg) of the test article is mixed with dried potassium bromide and compressed into a pellet using a hydraulic press. The pellet is placed in the FTIR spectrometer, and a spectrum is acquired over a wavenumber range of 4000-400 cm⁻¹. The resulting spectrum is compared to a reference standard spectrum of the expected compound. Key functional group absorptions must match the reference for identity confirmation [33].
- Mass Spectrometry Protocol: The test article is dissolved in a suitable solvent and introduced into the mass spectrometer via direct infusion or LC-MS. The instrument is operated in positive or negative ion mode to generate molecular ions. The mass spectrum is analyzed for the molecular ion peak to confirm the expected molecular weight. Tandem mass spectrometry can be used to fragment the molecular ion, providing a characteristic fragmentation pattern that serves as a unique fingerprint for the compound [33].
Determination of Strength and Purity by HPLC-UV
Objective: To accurately quantify the amount of active ingredient and related impurities in the test article batch.
- Protocol:
- Standard Solution Preparation: Precisely weigh a reference standard of known purity and dissolve it in the mobile phase to create a series of standard solutions covering the expected concentration range of the sample.
- Sample Solution Preparation: Precisely weigh the test article and dissolve it in the mobile phase to achieve a concentration within the linear range of the calibration curve.
- Chromatographic Conditions: Utilize a validated HPLC method. A common setup includes a C18 reversed-phase column, a mobile phase consisting of a mixture of aqueous buffer and an organic solvent, a flow rate of 1.0 mL/min, and UV detection at a wavelength specific to the analyte.
- Analysis: Inject the standard and sample solutions. The strength is calculated by comparing the peak area of the active ingredient in the sample to the calibration curve. Purity is assessed by integrating all peaks in the chromatogram and calculating the percentage of the main peak relative to the total peak area, or by reporting individual impurities against the main peak [4] [33].
Stability Monitoring in Dosing Formulation
Objective: To ensure the test article remains stable in its administered form throughout the study duration.
- Protocol:
- Sample Preparation: Prepare the dosing formulation at the target concentration(s) used in the study.
- Storage Conditions: Store the formulation in containers representative of those used in the study under defined conditions.
- Time Points: Test the formulation at time zero and at predetermined intervals that cover the period from preparation to the last administration.
- Analysis: At each time point, analyze the formulation using a stability-indicating method to quantify the concentration of the active ingredient and monitor the formation of degradation products. The acceptance criteria are typically set at ±5-10% of the initial concentration [4].
The Scientist's Toolkit: Essential Reagents and Materials
Successful characterization relies on a suite of high-quality reagents and materials. The following table details key items essential for the experiments described.
Table 3: Essential Research Reagent Solutions and Materials for Test Article Characterization
| Item | Function |
|---|---|
| HPLC-Grade Solvents | High-purity solvents for mobile phase preparation and sample dissolution to prevent interference and baseline noise. |
| Reference Standards | Substances of known identity and purity used for instrument calibration and method validation. |
| Potassium Bromide | Used for preparing pellets for FTIR spectroscopic analysis. |
| Volatile Buffers | Buffers compatible with mass spectrometry for maintaining pH and ion-pairing without fouling the ion source. |
| Certified Reference Materials | For calibrating and verifying the performance of instruments. |
| Stable Isotope-Labeled Analytes | Serve as internal standards in mass spectrometry to correct for matrix effects and recovery losses. |
| Titrants | Standardized solutions for determining concentration via titration. |
In the rigorously regulated environment of nonclinical safety assessment, comprehensive test article characterization is not merely a procedural step but a fundamental scientific and quality imperative. By systematically determining the identity, strength, purity, composition, and stability of a test article, analytical chemists provide the definitive evidence that the material under investigation is consistent, well-defined, and suitable for its intended use in GLP studies. The data generated through this process, underpinned by techniques such as HPLC, MS, and FTIR, and governed by the principles of GDocP and quality assurance, forms the bedrock of reliable safety data. This, in turn, supports robust regulatory submissions and ultimately contributes to the protection of public health by ensuring that decisions on the safety of new products are based on trustworthy and reproducible science.
Stability monitoring is a foundational element of Good Laboratory Practice (GLP), serving as a critical quality system that ensures the reliability and integrity of nonclinical safety studies. For analytical chemists, establishing and maintaining the stability of test and control articles—including drug substances and their formulations—provides the definitive proof that these materials did not change in composition or concentration in a way that would confound study results [15]. This process is mandated by regulations such as 21 CFR Part 58, which requires characterization of test articles to determine their identity, strength, purity, composition, and stability, thereby ensuring that the articles remain within established specifications from the date of manufacture through the study's conclusion [15] [2]. Effective stability monitoring directly supports regulatory submissions for investigational new drugs (INDs) and other applications by demonstrating that the safety data generated accurately reflect the properties of the material being tested [15].
Regulatory Framework and Governing Principles
Core GLP Regulations
The foundation of stability monitoring lies in the Good Laboratory Practice regulations, specifically 21 CFR Part 58. These regulations provide the legal framework for conducting nonclinical laboratory studies intended to support applications for FDA-regulated products [2]. Under Subpart F (§§58.105-58.113), the regulations explicitly address the handling of test and control articles, requiring proper characterization and stability determination to ensure the integrity of these critical materials throughout a study [2]. The fundamental goal is to assure the quality and integrity of the safety data filed in support of regulatory applications [2].
Beyond the United States, the OECD Principles of GLP have been adopted by 38 member countries, creating a globally harmonized system that allows for the mutual acceptance of data [15]. This international framework is particularly important for organizations conducting studies across multiple jurisdictions or submitting data to regulatory authorities in different countries.
The Role of the Analytical Chemist
Within this regulated environment, the analytical chemist assumes two primary responsibilities related to stability monitoring. First, they must develop and validate methods to characterize test articles (drug substances and early-phase drug product formulations) to determine identity, strength, purity, composition, and other defining characteristics [15]. Second, they must establish the stability of these test and control articles to assign appropriate storage conditions and verify that concentration remains within established ranges throughout the study duration [15]. This requires phase-appropriate method validation, where the extent of validation reflects the stage of drug development, with the understanding that complete degradation pathways may not be fully characterized during early nonclinical studies [15].
Designing a Stability Monitoring Program
Determining Stability Testing Requirements
A scientifically rigorous stability monitoring program begins with a clear definition of testing requirements based on the study objectives and material properties. The program must establish stability under specific storage conditions that mirror the actual handling of the test article throughout the nonclinical study. This includes not only long-term storage stability but also stability in the dosing formulation under the conditions of use [15].
For GLP studies, stability must be demonstrated for the test article (drug substance) itself, as well as for the formulated article (dosing solution/suspension) when applicable [15]. The testing should cover the entire duration from manufacture through the last analytical measurement, including any holding periods between manufacturing and testing. Furthermore, the stability of the test article in the biological matrix may be required for bioanalytical methods supporting toxicokinetic studies [15].
Key Experimental Protocols
Forced Degradation Studies
Forced degradation studies, also known as stress testing, provide critical data on the intrinsic stability of a molecule and help validate the stability-indicating methods.
Objective: To identify potential degradation products, understand degradation pathways, and validate the specificity of analytical methods.
Methodology:
- Acidic and Basic Conditions: Expose the test article to 0.1N HCl and 0.1N NaOH at room temperature and elevated temperatures (e.g., 40-60°C) for varying time periods (e.g., 1-4 weeks).
- Oxidative Stress: Treat with hydrogen peroxide (e.g., 0.1-3%) at room temperature for up to 1 week.
- Thermal Stress: Subject solid and solution state samples to elevated temperatures (e.g., 40-80°C) for defined periods.
- Photostability: Expose to controlled UV and visible light conditions per ICH Q1B guidelines.
- Analysis: Monitor degradation progress using the validated stability-indicating method, typically HPLC-UV, with characterization of major degradation products.
Long-Term and Accelerated Stability Studies
These studies establish recommended storage conditions and retest dates for test articles.
Objective: To determine the shelf life of the test article under defined storage conditions and establish expiration dates.
Methodology:
- Storage Conditions: Utilize controlled stability chambers that monitor and document temperature (±2-3°C) and relative humidity (±5% RH).
- Study Durations: Long-term studies typically run for 12-24 months at recommended storage temperature (e.g., 5°C ± 3°C, 25°C ± 2°C); accelerated studies run for 6 months at elevated temperatures (e.g., 40°C ± 2°C).
- Testing Intervals: Sample at time zero, 3, 6, 9, 12, 18, and 24 months for long-term; 0, 1, 2, 3, and 6 months for accelerated.
- Test Parameters: Include appearance, identity, assay/potency, impurities, and any other critical quality attributes.
The workflow for establishing a comprehensive stability monitoring program follows a systematic progression from initial method development through ongoing monitoring, as illustrated below:
Stability Monitoring Program Workflow
Quantitative Data Management and Analysis
Data Quality Assurance
Quality assurance begins with proper data management practices throughout the stability testing process. Implementation of Good Documentation Practice (GDocP) principles is essential, following the ALCOA+ framework: Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available [15]. All raw data and corresponding GLP documentation must be retained and archived according to standard operating procedures (SOPs) [15].
Data cleaning procedures must be implemented to ensure data quality prior to analysis. This includes checking for duplications, identifying and addressing missing data according to predefined thresholds, and detecting anomalies that deviate from expected patterns [36]. For stability data, this involves verification that all test results fall within the validated range of the analytical method and that control samples meet acceptance criteria.
Statistical Analysis of Stability Data
Statistical analysis of stability data follows a rigorous process to establish reliable expiration dating and storage conditions. The analysis typically proceeds through descriptive statistics to understand data distribution, followed by inferential statistics to make predictions about long-term stability.
Descriptive Analysis: Initial analysis should include measures of central tendency (mean, median) and dispersion (standard deviation, range) for stability results at each time point. Assessment of normality distribution is essential for selecting appropriate statistical tests, using measures such as skewness and kurtosis (with values of ±2 indicating normality) or formal tests like Kolmogorov-Smirnov or Shapiro-Wilk [36].
Inferential Analysis: Stability data are typically analyzed using regression analysis to estimate the rate of degradation and establish shelf life. For quantitative measurements like potency, a 95% confidence limit for the regression line is calculated, and the expiration date is determined as the time at which the lower confidence limit intersects the lower acceptance criterion [36].
The following table summarizes the key statistical methods employed in stability data analysis:
Table 1: Statistical Methods for Stability Data Analysis
| Analysis Type | Statistical Method | Application in Stability Monitoring | Key Outputs |
|---|---|---|---|
| Descriptive | Mean, Standard Deviation | Characterize central tendency and variability at each time point | Baseline understanding of data distribution |
| Descriptive | Skewness and Kurtosis | Assess normality of data distribution | Determines appropriateness of parametric tests |
| Inferential | Regression Analysis | Model degradation over time | Rate of degradation, prediction of shelf life |
| Inferential | Confidence Interval Estimation | Establish expiration dating with statistical confidence | 95% confidence limits for acceptance criteria intersection |
| Inferential | Analysis of Variance (ANOVA) | Compare stability across different batches or conditions | Detection of significant differences between groups |
For accelerated stability studies, the Arrhenius equation is commonly employed to predict shelf life under normal storage conditions based on degradation rates observed at elevated temperatures. This relationship allows for extrapolation of long-term stability from short-term accelerated data.
Documentation and Reporting Requirements
Stability Study Protocol and Report
A comprehensive stability study protocol must be written and approved before study initiation. This protocol should include:
- Detailed study objectives and justification
- Test article information (batch numbers, characterization data)
- Specific storage conditions to be evaluated
- Testing time points and total study duration
- Analytical methods to be used, referencing validation reports
- Acceptance criteria for all tested parameters
- Statistical analysis methods for dating period determination
The final stability study report must provide a complete account of the study conduct and results, including:
- Executive summary with conclusions and recommended storage conditions
- Detailed results for all tested parameters at each time point
- Statistical analysis and expiration date justification
- Deviations from protocol and their impact assessment
- Representative chromatograms or analytical outputs
- Conclusions regarding test article stability
Change Control and Ongoing Monitoring
Stability monitoring is not a one-time activity but requires ongoing surveillance throughout the product's lifecycle. A robust change control process must be established to assess the impact of any changes in manufacturing process, formulation, or packaging on product stability. When significant changes occur, additional stability studies should be initiated to confirm that the established storage conditions and expiration dating remain valid.
For studies of extended duration, periodic testing against established specifications ensures continued compliance. Any observed trends should be documented and investigated, with predetermined action limits triggering appropriate responses, which may include quarantine of materials, notification to regulatory authorities, or implementation of corrective actions.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful stability monitoring requires carefully selected materials and equipment that meet GLP standards. The following table details essential research reagent solutions and their functions in stability studies:
Table 2: Essential Research Reagents and Materials for Stability Monitoring
| Reagent/Material | Function in Stability Monitoring | GLP Compliance Considerations |
|---|---|---|
| Reference Standards | Serve as certified materials for method qualification and system suitability testing | Must be characterized and stored according to certificate of analysis; requires documentation of source, purity, and storage conditions |
| HPLC/UPLC Grade Solvents | Used as mobile phase components in chromatographic separations | Must meet manufacturer specifications; require expiration dating and proper storage to maintain purity |
| Chemical Reagents for Sample Preparation | Include buffers, acids, bases, and derivatization agents for sample treatment | Require preparation records with lot numbers and expiration dates; solutions must be labeled with identity, concentration, and preparer's initials |
| Authentic Degradation Standards | Used to identify and quantify specific degradation products in forced degradation studies | Should be synthesized and fully characterized when available; documentation should include structure confirmation and purity assessment |
| Calibrated Volumetric Glassware | Ensures accurate solution preparation for standards and samples | Must undergo regular calibration per established schedule; records must document calibration status and maintenance |
| Quality Control Samples | Used to monitor analytical method performance throughout the study | Should include system suitability samples and quality control samples at multiple concentrations; acceptance criteria must be predefined |
All equipment used in stability testing must have proper qualification documentation, including Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ) [15]. Regular calibration and maintenance according to established SOPs are essential to ensure data integrity and reliability.
The relationships between these essential components and the overall stability monitoring process are visualized below, showing how each element contributes to the comprehensive assessment of test article stability:
Stability Assessment Components
Stability monitoring represents a critical commitment to data quality and integrity within the GLP framework. Through systematic planning, execution, and documentation of stability studies, analytical chemists provide the essential evidence that test and control articles maintain their critical characteristics throughout nonclinical safety assessments. This rigorous approach to assigning storage conditions and ensuring article integrity directly supports the reliability of safety data submitted to regulatory authorities, ultimately contributing to the protection of public health by ensuring that decisions about product safety are based on trustworthy scientific evidence.
Bioanalytical methodologies form the cornerstone of modern drug development, providing critical data on the pharmacokinetics, pharmacodynamics, and immunogenicity of therapeutic compounds. For analytical chemists operating within Good Laboratory Practice (GLP) frameworks, these methods must yield reliable, reproducible, and accurate results to support regulatory submissions. GLP constitutes a quality system covering the organizational processes and conditions under which non-clinical laboratory studies are planned, performed, monitored, recorded, reported, and archived [4]. This framework ensures the integrity and reliability of safety test data submitted to regulatory bodies like the FDA and EPA [37].
The bioanalytical landscape for biological samples is predominantly served by three sophisticated methodological approaches: Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS), Enzyme-Linked Immunosorbent Assay (ELISA), and specialized immunogenicity testing platforms. LC-MS/MS offers exceptional sensitivity and specificity for quantifying small molecules and increasingly for large biologics, while ELISA provides a robust platform for detecting and quantifying proteins and biomarkers. Immunogenicity testing addresses the critical need to understand immune responses to biotherapeutics, particularly for monoclonal antibodies and antibody-drug conjugates (ADCs) [38]. The selection of an appropriate methodology is guided by the analyte's chemical properties, required sensitivity, the biological matrix, and the intended use of the data within the drug development pipeline.
Core Principles of Good Laboratory Practice (GLP)
GLP Framework and Relevance to Bioanalysis
Good Laboratory Practice (GLP) is a regulatory requirement designed to ensure the quality, reliability, and integrity of non-clinical safety studies conducted during drug development [4]. The core objective is to provide a standardized framework that minimizes variability and ensures that submitted data accurately reflects the experimental results. For bioanalytical chemists, GLP compliance is mandatory for pivotal nonclinical safety studies supporting applications for research or marketing permits [37] [1].
A fundamental GLP requirement is the establishment of a Quality Assurance Unit (QAU) that operates independently from the research team. The QAU is responsible for auditing studies, ensuring documentation accuracy, and verifying that all procedures comply with established protocols and Standard Operating Procedures (SOPs) [37]. Another critical role is the Study Director, who bears ultimate responsibility for the technical conduct of the study, as well as for the interpretation, analysis, documentation, and reporting of results [1]. This structured organization, with clear delineation of responsibilities, is essential for maintaining data integrity.
Essential GLP Requirements for Bioanalytical Laboratories
GLP principles encompass all aspects of laboratory operations. Key requirements include:
- Personnel Training and Qualifications: Staff must possess appropriate education, training, and experience. Regular competency assessments and training updates are essential to maintain high standards [37] [1].
- Facilities and Equipment: Laboratories must provide separation of activities to prevent interference or contamination. All equipment, including LC-MS instruments and plate readers, must be subjected to rigorous validation, calibration, and maintenance schedules, with comprehensive documentation of these activities [37] [4] [1].
- Standard Operating Procedures (SOPs): Well-documented, regularly reviewed SOPs are required for all critical processes, from sample handling and data recording to testing protocols and instrument operation [37]. These ensure consistency and minimize variability.
- Documentation and Archiving: Adherence to Good Documentation Practice (GDocP), often summarized by the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available), is mandatory [4]. Records and raw data must be retained for specified periods, typically ranging from 2 to 10 years depending on the regulatory application [1].
The following diagram illustrates the core organizational structure and workflow mandated under GLP:
GLP Organizational Structure and Data Flow
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) is a powerful analytical technique renowned for its high selectivity, sensitivity, and specificity in detecting and quantifying low levels of target analytes in complex biological matrices like plasma, serum, and tissue homogenates [39]. The technique couples the superior separation capabilities of liquid chromatography with the exceptional detection and identification power of a tandem mass spectrometer. This makes it indispensable in drug development for supporting pharmacokinetic (PK) and toxicokinetic (TK) studies, where precise measurement of drug and metabolite concentrations over time is critical [4] [40].
A significant advancement in the bioanalysis of large molecules, such as monoclonal antibodies, is the development of immunocapture LC-MS (IC-LC-MS). This hybrid approach uses an initial immunoaffinity step (e.g., with anti-human Fc antibodies) to selectively extract the target biologic from the matrix, followed by enzymatic digestion (e.g., with trypsin) and LC-MS/MS analysis of a signature surrogate peptide [40]. This method combines the specificity of ligand-binding assays with the precision and dynamic range of MS, reducing reliance on hard-to-produce critical reagents like anti-idiotypic antibodies, especially in early development [40].
Method Validation Parameters for LC-MS/MS
For an LC-MS/MS method to be considered reliable and GLP-compliant, it must undergo a rigorous validation process as per regulatory guidelines like ICH M10 [41]. The following table summarizes the eight essential validation characteristics and their significance.
Table 1: Essential Validation Parameters for LC-MS/MS Methods [39]
| Validation Parameter | Definition and Purpose | Typical Acceptance Criteria |
|---|---|---|
| Accuracy | The closeness of agreement between the measured value and the true value of the analyte. Assessed by comparing measured concentrations of quality control (QC) samples to their known concentrations. | Within ±15% of the nominal value (±20% at LLOQ). |
| Precision | The degree of scatter between multiple measurements of the same sample under stipulated conditions. Includes within-run (repeatability) and between-run (intermediate precision) precision. | Coefficient of variation (CV) ≤15% (≤20% at LLOQ). |
| Specificity | The ability to unequivocally assess the analyte in the presence of other components, such as metabolites, endogenous compounds, or concomitant medications. | No significant interference at the retention time of the analyte. |
| Quantification Limit (LLOQ) | The lowest concentration of the analyte that can be reliably and accurately measured with acceptable precision and accuracy. Determined by a predefined signal-to-noise ratio. | Accuracy and Precision within ±20%. |
| Linearity | The ability of the method to elicit results that are directly proportional to analyte concentration across a defined range. | Correlation coefficient (r) typically ≥0.99. |
| Recovery | The efficiency of the sample preparation and extraction process, measured by comparing the analyte response from extracted samples to unextracted standards. | Should be consistent and reproducible, not necessarily 100%. |
| Matrix Effect | The impact of co-eluting matrix components on the ionization efficiency of the analyte. Evaluated by comparing the response of analyte in post-extraction spiked matrix to neat solutions. | Precision (CV) of the internal standard-normalized matrix factor should be ≤15%. |
| Stability | The integrity of the analyte under specific conditions (e.g., benchtop, frozen, freeze-thaw cycles) over time, ensuring concentration does not change significantly. | Analyte should be stable within ±15% of the nominal concentration. |
The workflow for a generic immunocapture LC-MS/MS method for monoclonal antibodies is depicted below:
Immunocapture LC-MS Workflow for mAb Bioanalysis
Experimental Protocol: Generic Immunocapture LC-MS for mAb PK
Principle: This protocol outlines a generic method for quantifying human IgG-based therapeutics in non-clinical serum/plasma using commercial anti-human Fc capture and LC-MS/MS detection of a conserved surrogate peptide [40].
Materials:
- Biological Samples: Serum or plasma from study subjects.
- Capture Reagent: Biotinylated goat anti-human Fc antibody.
- Solid Support: Streptavidin-coated magnetic beads.
- Digestion Enzyme: Sequencing-grade trypsin.
- Internal Standard: Stable isotope-labeled (SIL) surrogate peptide.
- LC-MS/MS System: UHPLC coupled to a triple quadrupole mass spectrometer.
Procedure:
- Sample Preparation: Dilute samples and QCs appropriately with a suitable buffer (e.g., PBS).
- Immunocapture: Incubate samples with the biotinylated anti-human Fc reagent. Add streptavidin magnetic beads and incubate with mixing to capture the mAb-bead complex.
- Bead Washing: Use a magnetic rack to separate beads from the matrix. Wash multiple times with a buffer to remove non-specifically bound proteins.
- Denaturation and Reduction: Denature the captured mAb using a buffer (e.g., with RapiGest) and reduce disulfide bonds with a reagent like dithiothreitol (DTT).
- Alkylation: Alkylate the reduced cysteine residues with iodoacetamide.
- Digestion: Add trypsin and incubate to digest the mAb into peptides. The reaction is quenched with acid.
- LC-MS/MS Analysis: Inject the supernatant containing the surrogate peptide (e.g., VVSVLTVLHQDWLNGK) onto the LC-MS/MS. Quantitation is performed using Multiple Reaction Monitoring (MRM) by comparing the peak area ratio of the analyte peptide to the SIL internal standard against a calibration curve [40].
Enzyme-Linked Immunosorbent Assay (ELISA)
The Enzyme-Linked Immunosorbent Assay (ELISA) is a cornerstone ligand-binding assay (LBA) extensively used for measuring low-abundance proteins and biomarkers in biological fluids [42]. Its principle relies on the specific binding between an antigen and an antibody, with the detection achieved via an enzyme-conjugated antibody that produces a measurable colorimetric, chemiluminescent, or fluorescent signal. ELISA is particularly valuable for analytes where high sensitivity is required and for which suitable antibodies are available, such as in the measurement of Alzheimer's disease biomarkers like Aβ42, T-tau, and P-tau in cerebrospinal fluid [42].
Different ELISA formats cater to various analytical needs. The sandwich ELISA is common for complex antigens, using a capture and detection antibody for high specificity. Competitive ELISA is often employed for small molecules with a single epitope, where the analyte in the sample competes with a labeled analyte for a limited number of antibody binding sites. The performance of any ELISA is fundamentally governed by the affinity and specificity of the antibodies used, which directly impacts the assay's sensitivity and its potential for cross-reactivity [43].
Method Validation Parameters for ELISA
Similar to LC-MS/MS, ELISA methods require comprehensive validation to ensure data quality. The parameters, while conceptually similar, have specific considerations for immunoassays.
Table 2: Key Validation Parameters for ELISA Methods [42]
| Validation Parameter | Definition and Purpose | Key Considerations |
|---|---|---|
| Precision | The closeness of agreement between independent test results. Includes repeatability (within-run), intermediate precision (between-run), and reproducibility (between labs). | Imprecision is quantified as the coefficient of variation (CV). Factors like technician, day, and reagent lot should be varied for intermediate precision [42]. |
| Trueness / Accuracy | The closeness of agreement between the average value from a large series of results and an accepted reference value. Often assessed through recovery of spiked analyte. | Recovery should be within acceptable limits, demonstrating minimal systematic error [42]. |
| Selectivity / Specificity | The ability of the method to measure the analyte accurately in the presence of interfering components that may be expected in the sample matrix. | Assessed by testing common interferents like hemolyzed, lipemic, or icteric samples, and structurally similar molecules [42] [43]. |
| Limits of Quantification (LOQ) | The highest and lowest concentrations of analyte measurable with acceptable precision and accuracy. The Lower LOQ (LLOQ) is critically important. | LLOQ should have a precision (CV) ≤20% and accuracy within ±20% of nominal. Determined by analyzing diluted samples [42]. |
| Dilutional Linearity | Demonstrates that a sample with a concentration above the ULOQ can be reliably diluted into the assay's working range. | Back-calculated concentration of diluted samples should meet precision and accuracy criteria [42]. |
| Parallelism | Assesses the agreement between the dilution-response curve of the calibrator (in a substitute matrix) and the dilution-response curve of the endogenous analyte in the study matrix. | Crucial for validating assays for endogenous biomarkers to confirm matrix compatibility [41]. |
| Robustness | The capacity of the method to remain unaffected by small, deliberate variations in method parameters (e.g., incubation time, temperature). | Investigated during method development to establish acceptable tolerances in the SOP [42]. |
| Sample Stability | The stability of the analyte in the matrix under specific conditions (e.g., freeze-thaw, long-term frozen, benchtop). | Ensures analyte integrity is maintained from sample collection until analysis [42]. |
Strategies for Optimizing ELISA Sensitivity and Specificity
Sensitivity and specificity are paramount for a robust ELISA. Key strategies include:
- High-Affinity Antibodies: Using antibodies that bind strongly to the antigen significantly improves sensitivity and reproducibility [43].
- Signal Amplification: Employing enzymes with high turnover rates (e.g., HRP), or signal boosting methods like nanomaterials and enhanced chemiluminescence can lower detection limits. However, these must be optimized to avoid increasing background noise [43].
- Advanced Formats: Techniques like microfluidic ELISA for analyte preconcentration and digital immunoassays using beads and flow cytometry detection can achieve ultrasensitive detection [43].
- Minimizing Interference: Careful antibody selection and validation, including assessing cross-reactivity against related proteins, are essential for high specificity. Optimizing buffer composition, blocking agents, and wash stringency can also reduce non-specific binding [43].
Immunogenicity Testing
Fundamentals and Risk Assessment
Immunogenicity is the undesirable development of an adaptive immune response to a biotherapeutic drug [38]. The primary concern is the formation of Anti-Drug Antibodies (ADAs), which can impact both drug safety and efficacy. Consequences range from no clinical effect to altered pharmacokinetics (increased or decreased clearance), loss of efficacy (neutralization), and severe hypersensitivity or anaphylactic reactions [44]. Therefore, immunogenicity risk assessment is a critical component of the development of most biologic therapeutics, including monoclonal antibodies, antibody-drug conjugates (ADCs), and advanced therapy medicinal products (ATMPs) [38] [44].
The risk assessment is a two-part process evaluating: 1) the probability of the drug eliciting an immune response (based on factors like drug structure, patient population, and route of administration), and 2) the potential severity of the consequences if an immune response is induced [38]. For example, patients who are immunocompromised (e.g., oncology patients) typically show a lower incidence of immunogenicity compared to immunocompetent patients (e.g., with autoimmune diseases) [38]. This assessment directly informs the required testing strategy and bioanalytical method design.
Bioanalytical Strategy and Assay Platforms
The immunogenicity testing strategy is a multi-tiered approach designed to be highly sensitive for detection while providing characterization of the immune response.
- Screening Assay: The first tier is a sensitive immunoassay, typically a bridging ELISA or electrochemiluminescence (ECL)-based assay, designed to detect all ADAs in patient samples. The assay is designed to maximize sensitivity and minimize false negatives.
- Confirmation Assay: Samples that test positive in the screening assay are subsequently analyzed in a competitive inhibition assay using an excess of the free drug. This step confirms that the signal is specific to the drug.
- Neutralizing Antibody (NAb) Assay: This assay determines whether the confirmed ADAs can interfere with the drug's biological function. Cell-based assays are the gold standard, though competitive ligand-binding assays may be used in some cases [44].
For complex modalities like Antibody-Drug Conjugates (ADCs), immunogenicity assessment carries additional complexity. ADAs can develop not only against the protein component but also against the linker, the cytotoxic payload, or new epitopes created by the conjugation process (haptenic groups) [38]. Therefore, ADA characterization for ADCs often includes domain specificity testing (epitope mapping) to understand the target of the immune response, which has implications for clinical consequences [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key reagents and materials essential for conducting the bioanalytical methodologies described in this guide.
Table 3: Essential Research Reagent Solutions for Bioanalysis
| Reagent / Material | Function and Role in Bioanalysis | Key Considerations |
|---|---|---|
| High-Affinity, Validated Antibodies | Critical for ELISA (capture/detection) and immunocapture LC-MS. Define assay specificity, sensitivity, and reliability. | Must be validated for specificity and lack of cross-reactivity. Affinity directly impacts LLOQ [43]. |
| Stable Isotope-Labeled (SIL) Internal Standards | Used in LC-MS/MS for precise quantitation. Compensates for variability in sample preparation and ionization efficiency. | Should be identical to the analyte in chemical behavior. Added to the sample at the earliest possible step [40]. |
| Certified Reference Standards | Provide the known, pure analyte for preparing calibration standards and QCs. Fundamental for establishing method accuracy and traceability. | Purity, stability, and concentration must be well-characterized and documented [42]. |
| Biotinylated Anti-Human Fc Antibody | The core capture reagent in generic IC-LC-MS methods for human IgG-based therapeutics. Enables extraction and purification of the drug from the matrix. | Commercially available, eliminating the need for program-specific critical reagents in early development [40]. |
| Streptavidin-Coated Magnetic Beads | Solid support for immobilizing the biotinylated capture antibody and the captured analyte. Facilitates efficient washing to remove matrix interferents. | Bead size and surface area can affect capture efficiency and reproducibility [40]. |
| Critical Cell Lines | Used in cell-based NAb assays to assess the functional impact of ADAs on the drug's biological activity. | Must be relevant to the drug's mechanism of action and exhibit a robust, measurable response. |
| Specialized Buffers and Matrix | Assay diluents, blocking buffers, and surrogate matrices. Optimize assay conditions, reduce non-specific binding, and serve as a background for calibrators. | Matrix selection is vital; should mimic the study sample as closely as possible to minimize matrix effects [42]. |
LC-MS/MS, ELISA, and immunogenicity testing represent a powerful triad of bioanalytical methodologies, each with distinct strengths and applications in the characterization of biological drugs. The choice of method is driven by the scientific question, the nature of the analyte, and the stage of drug development. LC-MS/MS offers unparalleled specificity and dynamic range for quantitative analysis, while ELISA provides a sensitive and high-throughput platform for protein biomarkers. Immunogenicity testing is a non-negotiable safety and efficacy assessment for biologic therapeutics.
Underpinning all these techniques is the rigorous framework of Good Laboratory Practice. From method validation according to ICH M10 guidelines [41] to the meticulous documentation practices enforced by the Quality Assurance Unit, GLP compliance ensures that the generated data is of the highest quality, integrity, and reliability. For analytical chemists and drug development professionals, a deep understanding of these methodologies, their validation parameters, and their place within the GLP quality system is fundamental to successfully navigating the complex pathway of bringing new therapeutics to market.
Liquid chromatography, particularly High-Performance Liquid Chromatography (HPLC) and Ultra-High-Performance Liquid Chromatography (UHPLC), serves as a cornerstone analytical technique in pharmaceutical research and development. For analytical chemists operating under Good Laboratory Practice (GLP) regulations, these techniques provide the reliability, precision, and accuracy required for generating defensible data for regulatory submissions. GLP is a quality system covering the organizational process and conditions under which non-clinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and retained [4]. Its principal goal is to ensure that safety study data are reliable, reproducible, and auditable, thereby protecting public health through trustworthy safety evidence [2]. Within this rigorous framework, HPLC and UHPLC applications for small molecules and peptides must adhere to strict protocols for method validation, equipment qualification, and documentation practices to maintain data integrity throughout the drug development pipeline.
The fundamental distinction between GLP and other quality systems lies in its application phase. GLP applies to the preclinical or nonclinical safety testing phase of drug development and focuses on shorter-term projects and standalone studies, often conducted in contract research organizations (CROs) [4]. This differs from Good Manufacturing Practice (cGMP), which applies to the late-stage drug manufacturing process of drug substances and products [4]. For analytical chemists supporting GLP studies, this means their work must comply with specific regulations outlined in 21 CFR Part 58, which requires standardized approaches to method development, equipment calibration, and data recording to ensure the quality and integrity of safety data that underlie FDA decisions [2].
Recent Innovations in HPLC/UHPLC Column Technology
The core of any chromatographic separation lies in the column technology, and recent innovations have significantly enhanced the analysis of both small molecules and peptides. The past year has witnessed substantial advancements in stationary phase design, particle technology, and hardware inertness, each contributing to improved separation efficiency, peak shape, and analytical sensitivity.
Advances in Stationary Phases for Small Molecules
For small molecule reversed-phase liquid chromatography (RPLC), which continues to represent the largest category of new column introductions, developments have centered around modern particle bonding and hardware technology [45]. These advances enhance peak shapes for challenging molecules, improve column efficiency, extend the usable pH range, and provide improved and alternative selectivity [45]. Notable recent introductions include specialized phases such as the Halo 90 Å PCS Phenyl-Hexyl from Advanced Materials Technology, which provides enhanced peak shape and loading capacity for basic compounds while offering alternative selectivity to C18 phases [45]. Similarly, the Halo 120 Å Elevate C18 column offers exceptional high pH- and high-temperature stability, handling a wide pH range (2–12) while excelling with basic compounds [45].
The trend toward utilizing superficially porous particles (also known as fused-core technology) continues due to their superior efficiency compared to fully porous particles. Restek's Raptor C8 LC Columns, built on superficially porous silica particles with 2.7 μm particle size and 90 Å pore size, offer faster analysis times with similar selectivity to C18 columns [45]. These columns are particularly suited for a wide range of compounds from acidic to slightly basic, making them valuable tools for method development in regulated laboratories.
Specialized Columns for Peptide Analysis
Peptide analysis presents unique challenges due to the molecular complexity and specific chemical properties of peptides. Recent column technologies have addressed these challenges through specialized stationary phases and surface chemistries. The Ascentis Express and BIOshell A160 Peptide PCS-C18 columns from Merck Life Sciences feature a superficially porous particle design with a positively charged surface, which enhances peak shapes and offers alternative selectivity for peptides and pharmaceuticals [45]. These columns provide high throughput, excellent peak symmetry, and particular suitability for peptide mapping applications [45].
Another significant innovation comes from Fortis Technologies with their Evosphere C18/AR RPLC column, which features monodisperse fully porous particles (MFPP) that offer higher efficiency compared to conventional products [45]. This column is particularly suited for the separation of oligonucleotides without the need for ion-pairing (IP) reagents, making it a valuable tool for chromatographers working with complex biomolecules [45]. The availability of different particle sizes (1.7 μm, 3μm, and 5 μm) with 100 Å pore sizes provides flexibility for various analytical and preparative applications.
Table 1: Recent HPLC/UHPLC Column Innovations for Small Molecules and Peptides
| Column Name | Manufacturer | Stationary Phase Characteristics | Key Applications | Special Features |
|---|---|---|---|---|
| Halo 90 Å PCS Phenyl-Hexyl | Advanced Materials Technology | Fused-core silica with phenyl-hexyl group | Small molecules, basic compounds | Enhanced peak shape, alternative selectivity to C18 |
| Halo 120 Å Elevate C18 | Advanced Materials Technology | Superficially porous hybrid particle | Small molecules, basic compounds | Wide pH range (2-12), high temperature stability |
| Evosphere C18/AR | Fortis Technologies | Monodisperse fully porous particles (C18/aromatic) | Oligonucleotides, peptides | No ion-pairing reagents needed, higher efficiency |
| Aurashell Biphenyl | Horizon Chromatography | Superficially porous silica with biphenyl group | Metabolomics, isomer separations | Multiple separation mechanisms (hydrophobic, π–π) |
| Ascentis Express/BIOshell A160 | Merck Life Sciences | Superficially porous with positively charged surface | Peptides, pharmaceuticals | Enhanced peak shapes, peptide mapping suitability |
| Raptor C8 | Restek | Superficially porous silica with C8 group | Small molecules (acidic to basic) | Faster analysis times, similar selectivity to C18 |
The Trend Toward Bioinert and Inert Hardware
A persistent trend in column technology involves the use of inert or "bioinert" hardware to prevent detrimental interactions between metal-sensitive analytes and stainless steel components [45]. This is particularly crucial for analyzing compounds containing phosphorous groups, metal-chelating functionalities, or biomolecules that can adsorb to metal surfaces, resulting in poor peak shape and reduced recovery. Advanced Materials Technology's Halo Inert series integrates passivated hardware to create a metal-free barrier between the sample and the stainless-steel components, significantly improving analyte recovery for phosphorylated compounds and metal-sensitive analytes [45].
Restek has expanded their inert offerings with multiple new products, including Raptor Inert HPLC Columns with superficially porous silica particles and various functional groups (HILIC-Si, FluoroPhenyl, Polar X), designed specifically to improve chromatographic response for metal-sensitive polar compounds [45]. Similarly, Fortis Technologies' Evosphere Max columns use inert hardware to enhance peptide recovery and sensitivity, providing improved performance for metal-chelating compounds [45]. For GLP-compliant laboratories, these inert solutions provide assurance that analytical methods will maintain accuracy and precision, especially for challenging analytes prone to metal interaction.
GLP Compliance in Chromatographic Analysis
Fundamental GLP Principles for Chromatographers
Good Laboratory Practice establishes a framework of quality standards that ensure the integrity and reliability of nonclinical safety studies submitted to regulatory agencies. For analytical chemists employing chromatographic techniques, GLP compliance requires adherence to specific practices throughout the analytical workflow. According to 21 CFR Part 58, GLP regulations apply to "nonclinical laboratory studies that support or are intended to support applications for research or marketing permits for products regulated by the FDA" [2]. This includes studies on food additives, color additives, drugs, devices, biologics, and more [2].
The ten principles of GLP, as defined by the OECD, provide the structural foundation for compliance [4]. These encompass test facility organization and personnel, quality assurance programs, facilities, apparatus and materials, test systems, test and reference items, standard operating procedures (SOPs), study performance, reporting of results, and storage and retention of records [1]. Within this structure, the analytical chemist bears specific responsibilities for characterizing test articles and supporting bioanalytical measurements.
Documentation and Data Integrity Requirements
Proper documentation practice represents a core element of GLP compliance for chromatographic analyses [4]. The acronym "ALCOA+" defines the standards for all GLP documentation: Attributable, Legible, Contemporaneous, Original, and Accurate, along with Complete, Consistent, Enduring, and Available [4]. For the chromatographer, this translates to comprehensive recording of all aspects of method development, validation, and sample analysis using electronic laboratory notebooks (ELNs) and chromatographic data systems (CDS).
Specific documentation requirements include detailed records of reagents, solvents, samples, balances, weights, pipettes, and equipment used to prepare and analyze test and control articles [4]. The analyst must also document technical procedures, data analysis techniques, CDS processing methods, and integration parameters [4]. Maintaining chain of custody documentation is essential for tracking the delivery, receipt, storage, preparation, analysis, and disposition of test and control articles throughout the study lifecycle [4].
Equipment Qualification and Calibration
GLP regulations mandate that "equipment used in the generation, measurement, or assessment of data shall be adequately tested, calibrated, and standardized" [2]. For HPLC/UHPLC systems, this requires establishing and executing equipment qualification protocols (IQ/OQ/PQ), regular preventive maintenance, and calibration of detectors, pumps, autosamplers, and column ovens according to documented schedules and SOPs [1]. All qualification, maintenance, and calibration activities must be thoroughly documented, with records readily available for review by the Quality Assurance Unit (QAU) and regulatory inspectors [1].
HPLC/UHPLC Methodologies for Small Molecules
Method Development Strategies
Developing robust HPLC/UHPLC methods for small molecules under GLP requires systematic approaches that consider both analytical performance and regulatory compliance. The process begins with understanding the physicochemical properties of the analyte, including polarity, ionization constants (pKa), solubility, and stability. Modern method development often employs quality by design (QbD) principles, identifying critical method parameters (CMPs) and critical quality attributes (CQAs) to establish a method operable design region (MODR) [45].
The selection of stationary phase represents the most significant decision in method development. While C18 columns remain the most popular choice for small molecules, alternative phases provide valuable selectivity options. Biphenyl columns, such as the Aurashell Biphenyl from Horizon Chromatography, offer multiple separation mechanisms including hydrophobic, π–π, dipole, and steric interactions, making them well-suited for metabolomics, polar/non-polar compound analysis, and isomer separations [45]. For basic compounds, charged surface hybrid (CSH) technology or columns with positive surface charge, such as the Ascentis Express series, can significantly improve peak symmetry and efficiency [45].
Quantitative Analysis and Method Validation
Under GLP regulations, analytical methods used to characterize test articles must be properly validated to determine identity, strength, purity, composition, and other characteristics that define the substance [4]. For small molecules, HPLC with UV detection remains the most commonly employed technique for testing small molecule test articles [4]. The validation parameters typically assessed include accuracy, precision, specificity, linearity, range, detection limit, quantification limit, and robustness.
The phase-appropriate method validation approach recognizes that validation requirements differ based on the development stage [4]. Early-phase GLP studies may employ validated methods with less extensive characterization than those used in later-stage development, acknowledging that there is often little data available on degradation products and pathways at early stages [4]. Nevertheless, all validation activities must be thoroughly documented, with acceptance criteria predefined in study protocols or SOPs.
Table 2: Essential GLP Documentation for HPLC/UHPLC Methods
| Document Type | Purpose | GLP Requirements |
|---|---|---|
| Study Protocol | Defines study objectives, methods, and design | Written protocol approved before study; any amendments documented [2] |
| Standard Operating Procedures (SOPs) | Detailed instructions for routine operations | SOPs for all laboratory operations; deviations authorized by study director [1] |
| Equipment Records | Documents qualification, calibration, maintenance | Equipment properly designed, maintained, calibrated per SOPs [2] |
| Test Article Characterization | Details identity, purity, composition, stability | Characterization of test and control articles; stability established [4] |
| Raw Data | Original observations and results | ALCOA+ principles; all raw data retained and archived [4] |
| Final Report | Comprehensive study results | Complete account of study conduct; GLP compliance statement [1] |
Stability-Indicating Methods
For GLP studies, stability-indicating methods are essential for determining the stability of test and control articles, such as drug substances and dosing solutions, to assign appropriate storage conditions and assure that concentration does not change outside established ranges throughout the study [4]. These methods must demonstrate specificity toward the analyte in the presence of degradation products and excipients, typically through forced degradation studies under various stress conditions (acid, base, oxidation, heat, light).
Modern columns with extended pH stability (pH 1-12) greatly facilitate stability-indicating method development by enabling the use of mobile phase pH as a key selectivity parameter. Columns such as the SunBridge C18 from ChromaNik Technologies, designed for pH conditions ranging from 1 to 12, offer a broader range of applications compared to conventional columns with limited pH stability [45]. The Halo 120 Å Elevate C18 similarly handles a wide pH range (2–12) and excels under aggressive high-pH conditions, making it highly suitable for diverse analyte types [45].
Advanced UHPLC Applications for Peptide Analysis
Peptide Separation Fundamentals
Peptide analysis presents unique challenges that demand advanced chromatographic solutions, including molecular complexity, structural diversity, and varying hydrophobicity. UHPLC has become the technique of choice for peptide separations due to its superior resolution, sensitivity, and throughput compared to conventional HPLC. The fundamental parameters for peptide separation include stationary phase selection, particle size, pore size, column dimensions, temperature, and mobile phase composition.
Stationary phases with wider pore sizes (typically 120-300 Å) are preferred for peptide separations to accommodate larger molecular dimensions and facilitate adequate pore penetration. The Halo 120 Å Elevate C18 column, for instance, is built for high pH- and high-temperature stability, providing improved peak shape, retention, and load tolerance for peptide applications [45]. Columns with charged surface technology, such as the Ascentis Express and BIOshell A160 Peptide PCS-C18, feature a superficially porous particle design with a positively charged surface that enhances peak shapes for peptides and offers alternative selectivity compared to other C18 phases [45].
High-Resolution Mass Spectrometry Detection
The combination of UHPLC with high-resolution mass spectrometry (HRMS) has revolutionized peptide analysis by enabling precise mass measurement, structural characterization, and identification in complex matrices. Hybrid quadrupole-Orbitrap mass spectrometers provide extremely high resolution, ideal sensitivity, increased mass accuracy, and rapid polarity switching capability, making them particularly suitable for peptide characterization [46].
For untargeted peptide analysis, data-dependent acquisition (DDA) methods offer the possibility to acquire real MS/MS spectra by selecting precursor ions from a full scan analysis for further fragmentation based on real-time evaluation of MS data [47]. Unlike data-independent acquisition (DIA), DDA provides cleaner spectra by establishing physical relationships between precursor ions and their fragments, significantly improving peptide annotation [47]. Proper optimization of DDA parameters is essential for successful peptide identification, including considerations for cycle time, mass windows, automatic gain control, and dynamic exclusion [47].
Methodologies for Complex Peptide Mixtures
Analysis of complex peptide mixtures, such as those generated from protein digests, requires optimized chromatographic conditions to achieve sufficient separation. Key methodological considerations include gradient optimization (typically shallow gradients for complex mixtures), mobile phase selection (acidic conditions for positive ion mode MS), and column temperature (elevated temperatures to improve efficiency and reduce backpressure).
The trend toward using smaller particles (sub-2μm) and longer columns has enabled unprecedented peak capacities for peptide separations. The Purospher STAR RP-18 endcapped capillary columns from Merck are designed specifically for applications in proteomics and lipidomics, providing high sensitivity, reduced sample volume, and lower solvent consumption while offering enhanced reproducibility for high-throughput and high-resolution analyses [45]. These advanced chromatography tools are particularly valuable for GLP-compliant laboratories where reproducibility and reliability are paramount.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful HPLC/UHPLC analyses under GLP require not only sophisticated instrumentation but also high-quality reagents and materials that meet strict quality standards. The following table summarizes essential items for chromatographic analyses of small molecules and peptides in regulated environments.
Table 3: Essential Research Reagent Solutions for HPLC/UHPLC Analyses
| Item Category | Specific Examples | Function & Importance | GLP Considerations |
|---|---|---|---|
| HPLC Columns | Halo C18, Ascentis Express C18, Raptor Biphenyl | Stationary phase for compound separation; primary determinant of selectivity | Certificate of analysis; documented characterization; stability data |
| Guard Columns | Raptor Inert Guard Cartridges, Force Inert Guard | Protect analytical column from particulates and contaminants | Documentation of installation date and usage; regular replacement |
| LC-MS Grade Solvents | Methanol, Acetonitrile, Water (LC-MS grade) | Mobile phase components; minimize background interference | Supplier qualification; certificate of analysis; expiration dating |
| Mobile Phase Additives | Formic Acid, Trifluoroacetic Acid (TFA), Ammonium Acetate | Modify retention and improve ionization | High-purity grades; documented preparation; stability evaluation |
| Reference Standards | USP/EP/BP Certified Reference Standards | Method development, calibration, and system suitability | Documented purity, storage conditions, and expiration dates |
| Quality Control Materials | In-house or commercial QC samples | Monitor method performance and system suitability | Stability data; predefined acceptance criteria |
| Vials and Inserts | Certified clean vials, low-volume inserts | Sample containment and introduction | Documentation of lot numbers; demonstrated inertness |
Integration with GLP Quality Systems
Roles and Responsibilities
GLP-compliant chromatographic operations require clearly defined roles and responsibilities within the organizational structure. The Study Director carries ultimate responsibility for the overall conduct of the study and its GLP compliance, including approval of the study plan and final report [1]. The Quality Assurance Unit (QAU) provides independent oversight, monitoring studies for GLP compliance and conducting in-study inspections of analytical chemists preparing test and control article samples to ensure correct procedures are followed [4]. The Analytical Chemist performs the hands-on work of method development, validation, and sample analysis while maintaining comprehensive documentation [4].
This separation of functions ensures proper checks and balances within the quality system. The QAU must be separate from or independent of the testing facility organization or management, reporting directly to facility management rather than to the study director [1]. This independence is crucial for objective assessment of study conduct and data integrity.
Protocol Development and Study Plan
The study plan or protocol serves as the master guidance document for GLP-compliant chromatographic analyses, outlining how the study should be performed and containing the general time schedule for the study and its various stages [1]. For analytical chemistry support, the protocol typically includes detailed methodology for sample preparation, chromatographic conditions, detection parameters, system suitability requirements, and acceptance criteria for results.
The protocol development process begins with the study director preparing the protocol and discussing its contents with personnel and other study staff [1]. After discussion, the study director approves the protocol with a dated signature [1]. The QAU then reviews the protocol for compliance with Good Laboratory Practice before study initiation [1]. Throughout this process, personnel must be instructed on their assigned duties and receive their own copies of the protocol [1].
Data Management and Archiving
GLP regulations mandate strict controls for data management, storage, and retention. All raw data, documentation, protocols, specimens, and final reports must be archived in a manner that prevents unauthorized access or modification [2]. The required retention period for archived records varies depending on the regulatory context but typically extends to at least 5 years after the date on which study results were submitted to the FDA for studies supporting an Investigational New Drug (IND) application [1].
Electronic chromatographic data systems must comply with 21 CFR Part 11 requirements for electronic records and electronic signatures, including audit trails, user access controls, and system validation [2]. The analytical chemist must document all data processing parameters, including integration events and any reprocessing of chromatographic data, to ensure complete reconstruction of the analytical process [4].
HPLC and UHPLC technologies continue to evolve, offering increasingly sophisticated solutions for the analysis of small molecules and peptides in GLP-regulated environments. The latest innovations in column chemistry, particularly superficially porous particles, charged surface hybrids, and inert hardware, provide enhanced separation efficiency, improved peak shapes, and reduced analyte interactions. When implemented within a robust GLP quality system that emphasizes documentation, equipment qualification, and standardized procedures, these chromatographic techniques generate the reliable, defensible data required for regulatory submissions. As pharmaceutical development advances toward more complex molecules and lower detection limits, the integration of UHPLC with high-resolution mass spectrometry will undoubtedly play an increasingly vital role in GLP-compliant laboratories, necessitating ongoing attention to method validation, data integrity, and quality assurance practices.
Developing and Adhering to Standard Operating Procedures (SOPs) for All Critical Operations
For analytical chemists and drug development professionals, Standard Operating Procedures (SOPs) are the foundational element of Good Laboratory Practice (GLP), ensuring the integrity and reliability of non-clinical safety data [48] [1]. These formalized sets of written instructions guide laboratory personnel in carrying out specific tasks, translating high-level regulatory standards into actionable, consistent, and reproducible laboratory operations [49]. In the context of GLP, which was established in the 1970s by bodies like the FDA and OECD in response to concerns over sloppy lab work and data integrity, SOPs are not merely suggestions but mandatory components of a quality system [48] [50]. They provide the detailed framework that ensures studies are planned, performed, monitored, recorded, reported, and archived in a manner that guarantees the quality and integrity of the test data submitted for regulatory approval [1] [37]. This guide details the development, implementation, and adherence to SOPs as a critical requirement for GLP compliance in analytical research.
Core Components of an Effective SOP
A well-constructed SOP is more than a simple checklist; it is a comprehensive document designed to eliminate ambiguity and ensure consistency. The following core components are essential for creating an effective SOP that meets regulatory scrutiny.
Structural Elements and Content
An SOP must be structured to provide complete clarity and guidance. The key structural elements are detailed in the table below.
Table: Essential Structural Components of a Laboratory SOP
| Component | Description | Purpose |
|---|---|---|
| Clear Title | A succinct title describing the SOP's purpose and application conditions [51]. | Allows for quick identification and correct selection of the procedure. |
| Document Control | Date of authorship, revision number, and date of revision [51]. | Ensures version control and that personnel use the most current procedure. |
| Author and Reviewer Information | Name of the author and reviewers, including signatures and dates where possible [51]. | Establishes accountability and confirms review and approval by qualified individuals. |
| Purpose Statement | A brief explanation of the SOP's objective [51]. | Clearly defines the goal and scope of the procedure for the user. |
| Scope and Applicability | Defines the specific conditions, known limitations, and interferents for the protocol's reliable use [51]. | Prevents misapplication of the procedure to unsuitable scenarios or materials. |
| Safety Notes and Precautions | Embedded hazards, required Personal Protective Equipment (PPE), and emergency protocols [49]. | Reinforces a culture of safety and ensures personnel are aware of risks at all times. |
| Step-by-Step Instructions | Unambiguous, sequential directions written in clear, concise language [49]. | Guides the user through the procedure without room for interpretation, ensuring consistency. |
Beyond these structural elements, the content must be meticulously detailed. The Introduction should provide relevant background information on the system, methods, and instruments used [51]. The Materials and Supplies section must list all reagents, including supplier names, to ensure reproducibility [51]. Furthermore, the Personnel Qualifications section should outline any required prior training or competencies needed to perform the procedure safely and effectively [51].
Detailed Methodologies and Protocols
The heart of the SOP is the "Actual Protocol" section, which provides the step-by-step instructions for accomplishing the procedure [51]. This section must be exhaustive and include:
- Sequential Actions: Break down the process into manageable, numbered steps. Each step should describe a single action.
- References to Equipment: Specify the analytical instruments, including manufacturer and model numbers, and detail any required equipment calibration steps [51] [49].
- Data Recording Instructions: Specify how and when to record data, including templates for observations and results [49].
- Examples of Calculations: If data analysis involves calculations, provide a worked example to ensure uniformity [51].
- Visual Aids: Incorporate diagrams, flowcharts, or reference images to enhance clarity and reduce the potential for error [49].
SOP Development, Implementation, and Adherence
A formalized process for the creation, rollout, and maintenance of SOPs is crucial for their effectiveness and for achieving GLP compliance.
The SOP Development Workflow
The creation of an SOP is a multi-stage process that involves drafting, testing, and formal review before final approval and implementation. The following workflow diagram visualizes this robust development lifecycle.
Implementation and Training for Adherence
Once developed and approved, the implementation phase is critical. SOPs must be stored in a centralized, accessible SOP library, whether in print binders or, more effectively, within a Laboratory Information Management System (LIMS) or Electronic Document Management System (EDMS) [49]. This ensures all personnel can reference the correct versions at any time.
Training is the cornerstone of adherence. The GLP-mandated Study Director is responsible for ensuring that personnel are instructed on their duties and have copies of the relevant SOPs [1]. Effective training strategies include:
- Transforming SOPs into Interactive Training: Using platforms like SafetyCulture to convert how-to guides into engaging, visual slides for training [1].
- Hands-On Sessions: Conducting practical, hands-on training sessions where personnel perform the procedure under guidance.
- Documenting Training Records: Meticulously recording all training sessions and participant competencies to demonstrate compliance during audits [52] [1].
Quality Assurance and Audit Preparedness
Adherence to SOPs is monitored by the independent Quality Assurance Unit (QAU), a cornerstone of GLP compliance [1] [37]. The QAU audits practices, ensures documentation accuracy, and upholds data management systems to maintain integrity [37]. All deviations from an approved SOP must be authorized by the Study Director and documented in the study's final report [1]. A robust QAU function, combined with comprehensive SOPs, ensures a laboratory is always prepared for regulatory inspections by agencies like the FDA and EPA, which can occur every two years [50].
The Scientist's Toolkit: Essential Research Reagent Solutions
The integrity of any analytical procedure defined in an SOP is dependent on the quality and consistency of the materials used. The following table outlines key reagent solutions and their critical functions in supporting GLP-compliant research.
Table: Essential Research Reagent Solutions for Analytical Chemistry
| Item | Function |
|---|---|
| Reference/Control Articles | A product that is not the test article, used to provide a baseline for comparison with the test article and to validate the analytical system [1]. |
| Characterized Test Articles | The product being studied; requires known identity, purity, composition, and stability to ensure the validity of the study [1] [37]. |
| Calibration Standards | Solutions of known concentration used to calibrate analytical instruments, ensuring the accuracy and traceability of measurements. |
| High-Purity Reagents | Solvents and chemicals of defined and documented purity to prevent contamination and interference that could compromise data integrity [49]. |
| Stable Reference Materials | Materials that are stable for the duration of the study, with properly documented receipt, expiry, and storage conditions [1] [37]. |
In the rigorously regulated environment of analytical chemistry and drug development, SOPs are the critical link between abstract GLP principles and the generation of reliable, auditable data. Their meticulous development, comprehensive implementation, and strict adherence form the bedrock of data integrity and regulatory compliance. By investing in a robust SOP system, supported by qualified personnel, a strong QAU, and quality materials, research facilities not only safeguard their data and ensure regulatory approval but also build a foundational culture of quality, safety, and scientific excellence.
Solving Common GLP Challenges: From Peptide Analysis to Data Management
Overcoming Analytical Hurdles in Peptide Analysis (e.g., GLP-1 Agonists)
The rise of glucagon-like peptide-1 receptor agonists (GLP-1RAs) represents a groundbreaking advancement in treating type 2 diabetes and obesity, with emerging potential in neurological, cardiovascular, and psychiatric disorders [53] [54]. These peptide-based therapeutics, typically composed of 25–50 amino acids, present unique analytical challenges that demand sophisticated separation and characterization strategies [53]. Unlike small molecule drugs, GLP-1 agonists exhibit complex structural features including strong hydrophilic and hydrophobic interactions, isomeric impurities, and post-translational modifications that complicate their analysis [55]. The structural complexity of these molecules is further enhanced by chemical modifications such as fatty acid conjugation and incorporation of non-natural amino acids to improve stability and pharmacokinetic properties [53].
Within the framework of Good Laboratory Practices (GLP), analytical chemists must overcome these hurdles to ensure the quality, reliability, and regulatory compliance of data supporting drug development [15]. GLP regulations mandate rigorous characterization of test articles to determine identity, strength, purity, composition, and stability characteristics that appropriately define the drug substance and product [15]. This technical guide examines the predominant analytical challenges in GLP-1 peptide analysis and provides detailed methodologies for developing robust, GLP-compliant analytical approaches that meet regulatory standards for preclinical and clinical studies.
Key Technical Challenges in GLP-1 Peptide Analysis
Chromatographic Separation Complexities
The chromatographic behavior of GLP-1 peptides differs fundamentally from small molecules, presenting significant separation challenges. In reversed-phase liquid chromatography (RPLC), small molecules are retained primarily by a partitioning mechanism between stationary and mobile phases. In contrast, peptides undergo a distinct adsorption-desorption process where only portions of the large molecule interact with the stationary phase via strong hydrophobic interactions [55]. This results in sharp elution peaks when the entire molecule desorbs at a specific organic solvent concentration, causing many peptide impurities to elute either immediately before or after the main active peptide peak [55].
Regulatory bodies including the FDA require identification and quantification of impurities at very low levels (0.5% for known impurities and 0.10% for unknown ones), creating significant sensitivity and selectivity challenges [55]. This is particularly difficult when impurities co-elute with the main peak or other matrix components. Method reproducibility is another major concern, as minor variations in mobile phase preparation, column batches, and system cleanliness can significantly impact retention times and peak areas, complicating both method validation and routine quality control [55].
Structural Characterization Limitations
High-resolution mass spectrometry (HRMS) methods face several key limitations when characterizing GLP-1 impurities. Isomeric and isobaric impurities with identical molecular formulas and masses but different structures are particularly problematic, as HRMS cannot distinguish these similar mass compounds alone [55]. For example, racemization (D-amino acid impurities) results in impurities with the same mass as the parent drug, making them extremely difficult to differentiate with mass spectrometry alone [55].
Ion suppression represents another significant challenge, as mobile phase additives used for peptide separation (such as trifluoroacetic acid) can significantly suppress ionization in the mass spectrometer, reducing signal intensity and compromising sensitivity [55]. When analyzing large peptides with tandem mass spectrometry (MS/MS), the fragmentation patterns can be highly complex and difficult to interpret, complicating the identification of minor modifications such as single amino acid substitutions or post-translational modifications [55]. Additionally, disulfide bridges in peptide impurities create analytical challenges, particularly since these impurities often exist at very low concentrations, making effective reduction of disulfide bonds difficult and limiting useful fragmentation patterns during HRMS/MS analysis [55].
Sample Preparation and Stability Concerns
Optimizing sample preparation for GLP-1 peptides is crucial to avoid loss, adsorption, or artifactual modifications before HPLC/LC-MS analysis. Diluent selection proves particularly challenging as peptide molecules can adsorb to glass or plastic consumables, leading to lower recovery rates, especially at the limit of quantitation (LOQ) levels [55]. The isoelectric point (pI) of the peptide and HPLC index must be considered during diluent selection, with pH optimization necessary to minimize ionic interactions [55]. At pH lower than pI, the molecule carries a net positive charge, while at pH greater than pI, there is an overall negative charge, both of which can affect analytical recovery and performance.
Advanced Analytical Strategies and Orthogonal Methodologies
Two-Dimensional Liquid Chromatography (2D-LC)
Two-dimensional liquid chromatography (2D-LC) significantly enhances resolution and confidence in GLP-1 analysis, particularly for complex peptide formulations and impurity profiles [53]. This technique combines two different separation mechanisms in a single analysis, typically with reversed-phase chromatography in the first dimension and hydrophilic interaction liquid chromatography (HILIC) or ion-exchange in the second dimension [55]. This orthogonal separation approach resolves impurities that co-elute in traditional 1D LC, particularly those masked under the main peak or in complex impurity profiles [53].
The 2D-LC platform enables enhanced impurity detection by uncovering hidden or low-level impurities that would otherwise go undetected, crucial for ensuring safety and efficacy of GLP-1 drugs [53]. When coupled with mass spectrometry, 2D-LC facilitates detailed structural elucidation by isolating specific fractions (via multiple heart-cutting) for further analysis, helping identify degradation products, process-related impurities, or formulation-related artifacts [53]. This approach is particularly valuable in method development, validation, stability studies, comparability assessments, and investigations of batch-to-batch variability [53].
Advanced Mass Spectrometry Techniques
Innovative mass spectrometry approaches address the limitations of conventional HRMS for GLP-1 characterization. Electron transfer dissociation (ETD) provides superior fragmentation compared to standard collision-induced dissociation (CID), improving sequence coverage and facilitating precise localization of post-translational modifications [55]. This is particularly valuable for identifying complex isoforms and subtle structural modifications that conventional techniques might miss.
Hydrogen-deuterium exchange (HDX) mass spectrometry offers powerful biophysical characterization that provides information on higher-order structure beyond simple mass determination [55]. This technique monitors the exchange of labile hydrogen atoms on the peptide backbone with deuterium atoms from a deuterated solvent, with exchange rates dependent on the molecule's solvent accessibility and hydrogen-bonding patterns [55]. This provides crucial information about protein folding and structural integrity that complements standard mass analysis.
Hydrophilic Interaction Liquid Chromatography (HILIC)
HILIC operates on a fundamentally different separation principle compared to traditional reversed-phase HPLC, making it particularly valuable for orthogonal analysis of GLP-1 therapeutics [53]. The innovation of HILIC methods lies in their comprehensive analytical capability, allowing simultaneous analysis of both the active pharmaceutical ingredient (API) and formulation components such as phosphate ions and other excipients within a single method [53]. This enables detection of impurities not only from the drug substance but also those arising from the formulation process, which standard methods typically miss [53].
The use of bio-inert LC systems with passivated surfaces significantly improves peak shapes for sensitive analytes, particularly ions that tend to interact with stainless steel surfaces [53]. This enhancement in chromatographic performance demonstrates clear advantages for GLP-1 analysis. Additionally, incorporating dual detection using diode array detection (DAD) and evaporative light scattering detection (ELSD) provides complementary analysis where DAD detects compounds with chromophores while ELSD enables detection of non-chromophoric species such as certain ions and excipients that would otherwise go undetected [53].
Size-Exclusion Chromatography (SEC) for Aggregate Analysis
Size-exclusion chromatography plays a critical role in analyzing and quantifying aggregates in GLP-1 formulations, a key quality attribute. Parameters affecting resolution in SEC columns include particle size, column length, internal diameter, pore size, and injected sample volume [55]. Optimal resolution capable of measuring twofold molecular weight differences typically requires longer columns with smaller internal diameters, moderate flow rates, small particle sizes, and lower sample volumes [55]. Sample viscosity should match the mobile phase to maintain optimal separation conditions.
Buffer conditions compatible with peptide stability must be carefully selected, as extremes in pH and ionic strength or the presence of denaturing agents can cause conformational changes [55]. Sodium chloride at optimized concentrations helps avoid nonspecific ionic interactions with the matrix that can delay peak elution [55]. The product of interest should be collected in a suitable buffer maintaining adequate buffering capacity and constant pH throughout the analysis [55].
Table 1: Orthogonal Analytical Methods for GLP-1 Peptide Characterization
| Analytical Technique | Separation Mechanism | Primary Applications | Key Advantages |
|---|---|---|---|
| Reversed-Phase HPLC/UHPLC | Hydrophobicity | Routine impurity profiling, quality control | High efficiency, well-understood, robust |
| HILIC | Hydrophilicity/polarity | Orthogonal impurity separation, excipient analysis | Complementary selectivity to RPLC, detects non-chromophoric compounds |
| 2D-LC (RP-HILIC) | Orthogonal hydrophobic/hydrophilic | Complex impurity profiles, co-eluting peaks | Enhanced resolution, hidden impurity detection |
| Size-Exclusion Chromatography | Molecular size/hydrodynamic volume | Aggregate quantification, higher-order structure | Preserves native structure, identifies oligomers |
| Ion-Exchange Chromatography | Charge characteristics | Charge variant analysis, post-translational modifications | Separates isoforms, degradation products |
Experimental Protocols and Methodologies
LC-MS/MS Method Development for GLP-1 Agonists
The development of a sensitive LC-MS/MS assay for PF-06882961 (danuglipron), an oral small molecule agonist of the GLP-1 receptor, demonstrates a systematic approach to GLP-1 analysis [56]. This method employed statistical instrument parameter optimization using response surface methodology to enhance sensitivity and reliability [56]. The validated method successfully supported a proof-of-concept microdose pharmacokinetics preclinical study in monkeys, administering PF-06882961 (0.005 mg total, average dose = 0.0007 mg/kg) via intravenous bolus injection [56]. This approach demonstrated the feasibility of analyzing human microdose plasma samples for PF-06882961 by LC-MS/MS instead of accelerator mass spectrometry, reducing costs and eliminating synthesis and exposure to 14C labeled material [56].
For bioanalytical methods supporting GLP studies, validation must adhere to International Council for Harmonisation (ICH) M10 guidelines [15]. Core validation experiments include assessments of precision, accuracy, selectivity, and specificity [15]. Additional validation characterizes the assay and evaluates analyte stability in the biological matrix, with stability evaluated at room temperature, frozen, and after multiple freeze-thaw cycles over an appropriate concentration range [15]. Selectivity must be evaluated in relevant patient populations, presenting particular challenges for projects with rare disease indications [15].
Orthogonal Method Validation for Impurity Profiling
Regulatory requirements mandate proving impurity sameness using at least two orthogonal analytical methods based on fundamentally different principles [55]. A robust orthogonal strategy typically combines a primary method for routine impurity analysis using HPLC-UV/diode array detection (DAD) with reverse-phase chromatography stationary phases (C4, C8, and C18) for impurity separation, complemented by an orthogonal approach using HILIC chromatography or anion exchange/cation exchange stationary phases [55]. Coupling LC-HRMS generates a powerful dataset where an impurity's identity is confirmed by both chromatographic behavior and precise mass [55].
For comprehensive impurity profile comparison between active pharmaceutical ingredient (API) and drug product—particularly when API is outsourced—validated analytical methods must identify and quantify all impurities above specified thresholds [55]. Similar impurity analysis must be performed on the final drug product, including samples from forced degradation and long-term stability studies [55]. Any new analytical method for drug product analysis requires re-establishing the drug substance's impurity profile using the newly developed method or establishing method equivalency between drug substance and drug product analytical methods [55].
Table 2: GLP-1 Peptide Analysis Experimental Parameters and Conditions
| Parameter Category | Specific Conditions | Optimization Considerations | GLP Compliance Requirements |
|---|---|---|---|
| Chromatographic Separation | Column: C4, C8, C18 for RP; Specialized HILIC for orthogonal | Batch-to-batch column consistency, surface chemistry | Column qualification documentation, retention time reproducibility |
| Mobile Phase | TFA, formic acid, acetonitrile/water gradients | Ion suppression effects, pH control, buffer capacity | Documented preparation procedures, stability studies |
| Mass Spectrometry | HRMS resolution >25,000; ESI positive mode; CID/ETD fragmentation | Fragmentation energy, collision gas pressure, source temperatures | Mass accuracy calibration, sensitivity verification |
| Sample Preparation | Diluent pH adjustment relative to pI; low-adsorption surfaces | Recovery rates at LOQ, minimization of artifactual modifications | Chain of custody documentation, stability in matrix |
| System Suitability | Plate count, tailing factor, retention time stability | Injection precision, carryover assessment, baseline noise | Pre-run system checks, defined acceptance criteria |
Experimental Workflow for Comprehensive GLP-1 Characterization
The following diagram illustrates a integrated workflow for GLP-1 peptide analysis that incorporates orthogonal methodologies and meets GLP compliance requirements.
Diagram 1: Comprehensive GLP-1 Peptide Analysis Workflow. This integrated approach combines orthogonal separation techniques with advanced structural analysis to ensure comprehensive characterization and GLP compliance.
The Scientist's Toolkit: Essential Reagents and Materials
Successful GLP-1 peptide analysis requires carefully selected reagents, materials, and instrumentation that meet the specific challenges of peptide characterization while maintaining GLP compliance. The following toolkit outlines essential components for establishing robust analytical methods.
Table 3: Essential Research Reagent Solutions for GLP-1 Peptide Analysis
| Toolkit Component | Specific Examples/Properties | Function in Analysis | GLP Compliance Considerations |
|---|---|---|---|
| Chromatography Columns | C4, C8, C18 for RP-HPLC; Specialized HILIC; SEC with optimized pore size | Peptide separation, impurity resolution, aggregate analysis | Column qualification certificates, batch-to-batch reproducibility documentation |
| Mobile Phase Additives | Trifluoroacetic acid (TFA), formic acid, ammonium acetate/ bicarbonate | Modulation of retention, peak shape improvement, MS compatibility | Documented preparation procedures, established stability data |
| Mass Spectrometry Systems | HRMS (Q-TOF, Orbitrap) with advanced fragmentation (CID, HCD, ETD) | Molecular weight determination, sequence confirmation, impurity identification | System qualification, calibration records, performance verification |
| Bio-Inert LC Systems | Passivated surfaces (e.g., Agilent InfinityLab Bio LC) | Reduced analyte adsorption, improved peak shapes for sensitive peptides | Installation qualification (IQ), operational qualification (OQ), preventive maintenance records |
| Sample Preparation Materials | Low-adsorption tubes/plates, optimized diluents (pH adjusted) | Minimize peptide loss, prevent artifactual modifications, maintain stability | Chain of custody documentation, compatibility studies |
| Reference Standards | Highly characterized GLP-1 agonist reference materials | System suitability testing, method qualification, quantitative analysis | Certificate of analysis, storage conditions, stability documentation |
GLP Compliance in Peptide Analysis
Documentation and Quality Systems
Good Laboratory Practice regulations require comprehensive documentation practices to ensure data integrity and reliability. Good Documentation Practice (GDocP) represents a core element of GLP compliance, with pharmaceutical companies establishing their own GDocP standards aligned with industry principles [15]. The ALCOA+ framework guides documentation requirements: Attributable, Legible, Contemporaneous, Original, Accurate, along with Complete, Consistent, Enduring, and Available [15]. For analytical chemists, this necessitates using electronic lab notebooks to contemporaneously record all reagents, solvents, samples, equipment, and technical procedures used in sample preparation and analysis [15].
The chain of custody is essential to maintaining GLP study integrity, requiring comprehensive documentation of the delivery, receipt, storage, preparation, analysis, and disposition of test and control articles [15]. The study director or test facility manager typically enforces these regulatory aspects, with the quality assurance unit (QAU) potentially conducting in-study inspections of analytical chemists preparing test and control article samples to verify correct procedure adherence [15]. All raw data and corresponding GLP documentation must be retained and archived according to standard operating procedures (SOPs) [15].
Analytical Method Validation
For GLP studies, analytical chemists must develop methods to characterize test articles (drug substances and early-phase drug product formulations) to determine identity, strength, purity, composition, and other defining characteristics [15]. Test articles in GLP studies require characterization using GLP-compliant methods and procedures, with phase-appropriate method validation employed since limited data may be available on degradation products and pathways at early development stages [15]. Equipment used in GLP studies must have proper qualification documentation, with high performance liquid chromatography (HPLC) with ultraviolet (UV) detection commonly employed for testing small molecule test articles [15].
Stability of test and control articles (including drug substance and dosing solution when applicable) must be established to assign appropriate storage conditions and ensure the test article concentration remains within established ranges from manufacture through study completion [15]. For bioanalytical methods supporting clinical studies, additional testing includes immunogenicity assessment—the tendency of a drug candidate to elicit an immune response—which typically consists of screening, confirmatory, titration, and neutralization assays to fully identify and characterize immune responses [15].
The analytical characterization of GLP-1 receptor agonists demands sophisticated approaches that address their unique structural complexities while maintaining rigorous GLP standards. Through implementation of orthogonal methodologies, advanced mass spectrometry techniques, and comprehensive impurity profiling, analytical scientists can overcome the significant challenges presented by these therapeutic peptides. The framework presented in this guide provides a pathway to robust, reproducible, and regulatory-compliant analysis of GLP-1 agonists, supporting the continued development and quality assurance of these groundbreaking therapeutics. As the applications of GLP-1 agonists expand beyond metabolic disorders into neurological, cardiovascular, and psychiatric conditions, the analytical strategies outlined here will become increasingly vital to ensuring their safety, efficacy, and quality throughout the drug development lifecycle.
Addressing Co-elution and Low-Level Impurity Detection with 2D-LC-HRMS
In the pharmaceutical laboratory, the accurate separation, identification, and quantification of impurities in active pharmaceutical ingredients (APIs) and drug products is a fundamental requirement of Good Laboratory Practices (GLP). Conventional one-dimensional liquid chromatography (1D-LC) often encounters a critical limitation: co-elution, where multiple compounds exit the chromatography column simultaneously. This phenomenon is particularly problematic for peptide and oligonucleotide therapeutics, where impurities frequently share very similar structures with the main product [55] [57]. When co-elution occurs, it compromises the accuracy of impurity quantification and can obscure critical quality attributes, thereby violating the fundamental principles of data integrity and product understanding that underpin GLP.
The combination of two-dimensional liquid chromatography with high-resolution mass spectrometry (2D-LC-HRMS) represents a paradigm shift in addressing these analytical challenges. By subjecting sample components to two distinct separation mechanisms, 2D-LC dramatically increases the peak capacity (the number of distinct peaks that can be separated in a given time) of the analytical system [58] [59]. When this enhanced separation power is coupled with the accurate mass measurement and structural elucidation capabilities of HRMS, analysts gain a powerful tool for resolving co-elutions and characterizing low-level impurities down to the 0.10% level required by regulatory bodies like the FDA [55].
Fundamentals of 2D-LC Separation
Core Principles and Configurations
Two-dimensional liquid chromatography operates on the principle of subjecting the effluent from a first separation dimension ('D) to a second, independent separation mechanism ('D). The theoretical peak capacity of a 2D-LC system is approximately 60% of the product of the individual dimension peak capacities, representing a substantial increase over 1D-LC [60]. The effectiveness of this system hinges on the concept of orthogonality—the degree to which the two separation mechanisms are uncorrelated and based on different physicochemical properties of the analytes [58].
Two primary operational modes define the practice of 2D-LC, each with distinct advantages for impurity analysis:
- Comprehensive 2D-LC (LC×LC): The entire effluent from the 'D separation is transferred in consecutive fractions to the 'D column for further separation. This mode provides a complete two-dimensional separation of the entire sample, making it ideal for untargeted impurity profiling and discovery workflows [60] [59].
- Heart-Cutting 2D-LC (LC-LC) and Multiple Heart-Cutting (mLC-LC): In this targeted approach, one or a few specific regions of interest (e.g., a single peak suspected of containing co-elutions) from the 'D chromatogram are transferred to the 'D column. The multiple heart-cutting variant uses a series of sampling loops to store several 'D fractions for subsequent 'D analysis, which is exceptionally useful for method development in impurity analysis of APIs [60] [61].
Orthogonality in Separation Mechanisms
The selection of orthogonal separation phases is critical for success in 2D-LC. A common and robust approach for small molecule drugs is Reversed-Phase × Reversed-Phase (RP×RP) using different column chemistries (e.g., C18 in the first dimension and phenyl-hexyl in the second) and mobile phases (e.g., water-methanol gradient in 'D and water-acetonitrile gradient in 'D) [60]. For analytes with diverse physicochemical properties, such as highly polar pesticides, a HILIC × RP configuration can provide superior orthogonality [62]. Other orthogonal combinations include Ion Exchange Chromatography (IEX) × Reversed-Phase LC and Size-Exclusion Chromatography (SEC) × Reversed-Phase LC, the latter being particularly valuable for separating mAbs and ADCs based on size variants before desalting and MS analysis [63].
Table 1: Common Orthogonal Phase Combinations in 2D-LC for Impurity Analysis
| 'D Separation Mode | 'D Separation Mode | Primary Application Context | Key Advantage |
|---|---|---|---|
| Reversed-Phase (C18) | Reversed-Phase (Phenyl-Hexyl) | Small Molecule APIs, Taxanes [60] | High peak capacity in both dimensions; high robustness and MS compatibility |
| HILIC | Reversed-Phase (C18) | Multi-residue Pesticides [62] | Excellent for mixtures of analytes with wide polarity ranges |
| Strong Cation Exchange (SCX) | Reversed-Phase (C18) | Therapeutic Peptides/Proteins [60] | Separates based on charge before hydrophobicity |
| Size-Exclusion (SEC) | Reversed-Phase (C18) | mAbs, ADCs [63] | Resolves aggregates/fragments before desalting and MS analysis |
Tackling Low-Level Impurity Detection with HRMS
The Role of High-Resolution Mass Spectrometry
While 2D-LC solves the separation challenge, High-Resolution Mass Spectrometry (HRMS) provides the definitive identification power necessary for GLP-compliant impurity identification. Techniques such as Fourier Transform Ion Cyclotron Resonance Mass Spectrometry (FTICR-MS) provide the high mass accuracy and resolving power required to determine charge states from single m/z values and to model isotopic distributions for unambiguous confirmation of an impurity's elemental composition [57]. This is crucial for differentiating between isobaric and isomeric impurities that may co-elute even in a 2D system.
HRMS faces specific challenges in impurity analysis. Ion suppression from mobile phase additives (e.g., trifluoroacetic acid) or co-eluting matrix components can reduce signal intensity for low-level impurities [55]. Furthermore, for large biomolecules like peptides, complex fragmentation patterns in MS/MS can make data interpretation difficult [55]. Finally, HRMS alone cannot always distinguish between isomeric impurities, such as those resulting from racemization (D-amino acids) or different sites of modification, which have identical masses [55].
Advanced HRMS Techniques for Structural Elucidation
To overcome these limitations, advanced HRMS strategies are employed:
- Electron Transfer Dissociation (ETD): This fragmentation technique, as an alternative to traditional collision-induced dissociation (CID), provides more comprehensive peptide backbone coverage and facilitates the precise localization of post-translational modifications (PTMs) without the loss of labile side chains [55].
- Hydrogen-Deuterium Exchange MS (HDX-MS): This powerful biophysical technique probes the higher-order structure of a molecule by monitoring the exchange of labile hydrogen atoms on the peptide backbone with deuterium from a deuterated solvent. The rate and extent of this exchange provide information on solvent accessibility and hydrogen-bonding patterns, which can help characterize impurities that affect protein structure [55].
Practical 2D-LC-HRMS Methodologies and GLP Compliance
A Protocol for Impurity Profiling of Synthetic Peptides
The following detailed protocol for the impurity analysis of a synthetic peptide (e.g., a GLP-1 analog) using multiple heart-cutting 2D-LC-HRMS ensures adherence to GLP principles of reliability and traceability [55] [61].
First Dimension Separation Setup
- Column: 'D RP column (e.g., C18, 2.1 x 150 mm, 1.7 µm).
- Mobile Phase: A: 0.1% Formic Acid in Water; B: 0.1% Formic Acid in Acetonitrile.
- Gradient: A shallow gradient optimized for the specific peptide (e.g., 2-40% B over 60 minutes) to maximize resolution of impurities.
- Flow Rate: 0.1 - 0.2 mL/min.
- Detection: UV at 214 nm.
- Temperature: Maintained at a constant temperature (e.g., 40°C) to enhance reproducibility.
Heart-Cutting and Transfer
- Interface: A 2-position switching valve equipped with two or more storage loops (e.g., 40 µL volume).
- Method: Based on an initial scouting run, define the time windows for heart-cutting. Suspected co-elution regions and the main peak are cut. For a broad main peak, use a selective comprehensive (sLCxLC or HiRes) approach, taking multiple adjacent fractions across the entire peak to assess purity [61].
- Dynamic Peak Parking (DPP): To compensate for retention time fluctuations between runs—a critical factor for robustness and reproducibility—implement DPP. This technique uses a consistently eluting peak (e.g., a deamidation product) as an internal retention time standard (IRTS). All subsequent timed cutting events are dynamically adjusted "on-the-fly" based on the observed retention time shift of this IRTS, ensuring cuts are always taken at the correct position [61].
Second Dimension Separation and HRMS Detection
- Column: 'D RP column with orthogonal selectivity (e.g., Phenyl-Hexyl, 2.1 x 50 mm, 1.7 µm).
- Mobile Phase: MS-compatible buffers (e.g., 0.1% Formic Acid).
- Gradient: A fast, steep gradient (e.g., 5-95% B in 5 minutes) to rapidly separate the transferred heart-cut before the next transfer.
- Flow Rate: 0.4 - 0.8 mL/min.
- MS Parameters:
- Ionization: Electrospray Ionization (ESI) in positive mode.
- Mass Analyzer: Orbital trapping or Time-of-Flight (TOF) mass analyzer.
- Resolution: >50,000 FWHM.
- Mass Accuracy: < 3 ppm.
- Data Acquisition: Full-scan MS and data-dependent MS/MS (ddMS²) with both CID/HCD and ETD fragmentation triggered above a predefined threshold.
The following workflow diagram illustrates the heart-cutting process with dynamic peak parking:
Essential Research Reagent Solutions
The following table catalogues critical reagents and materials required for developing and executing a robust 2D-LC-HRMS method for impurity analysis, aligning with GLP requirements for material qualification.
Table 2: Key Research Reagent Solutions for 2D-LC-HRMS Impurity Analysis
| Reagent / Material | Function / Purpose | Technical Considerations for GLP |
|---|---|---|
| Orthogonal LC Columns | Provide the two distinct separation mechanisms. | Certificates of Analysis (CofA) for column lot-to-lot reproducibility are critical. Examples: 'D C18, 'D Phenyl-Hexyl [60]. |
| MS-Compatible Solvents & Additives | Form the mobile phase for optimal ionization. | High-purity solvents (LC-MS grade) and volatile additives (e.g., Formic Acid, Ammonium Formate) to prevent ion suppression and source contamination [55]. |
| IP-RP HPLC Buffers | Specific for oligonucleotide analysis. | Pre-mixed, qualified buffers (e.g., TEA/HFIP) ensure consistent retention and ionization for phosphorothioate oligonucleotides [57]. |
| Stable Isotope-Labeled Internal Standards | For absolute quantification and monitoring of analytical performance. | Corrects for recovery variations and matrix effects, improving data accuracy and precision. |
| System Suitability Test Mixtures | Verify instrument performance before sample analysis. | Must contain analytes and known impurities to confirm resolution, sensitivity, and retention time stability as per GLP [61]. |
Quantitative Data and Regulatory Considerations
Demonstrating Orthogonality for Impurity "Sameness"
Regulatory guidelines (e.g., FDA) require demonstrating impurity "sameness" using at least two orthogonal analytical methods [55]. A successful strategy involves coupling a primary quantitative method like HPLC-UV with an orthogonal separation (e.g., HILIC or IEX) coupled to HRMS. This generates a powerful dataset where an impurity's identity is confirmed by both its chromatographic behavior (retention time) in two different systems and its precise mass [55]. The quantitative data from comprehensive 2D-LC can be processed using advanced chemometrics to handle the complex, voluminous data, ensuring accurate quantification of resolved impurities [58].
Table 3: Quantitative Performance of 2D-LC-HRMS for Impurity Analysis
| Analytical Metric | 1D-LC-HRMS Performance | 2D-LC-HRMS Performance | Impact on GLP Compliance |
|---|---|---|---|
| Theoretical Peak Capacity | ~500 (in 1 hour) [60] | ~60% of ('D nc × 'D nc) (e.g., ~3000) [60] [58] | Drastically reduces co-elution, ensuring data integrity for purity assessments. |
| Impurity Detection Limit | Challenging at 0.10% due to ion suppression/co-elution [55] | Significantly improved via heart-cutting and reduced matrix interference [55] [62] | Enables reliable detection and identification of unknown impurities at the 0.10% threshold. |
| Confidence in Impurity ID | Reliant on MS alone; struggles with isomers [55] | High confidence from 2D retention indices + accurate mass + MS/MS [55] [57] | Provides definitive evidence for impurity identity, satisfying regulatory requirements. |
| Number of Impurities Detected (Oligonucleotides) | Limited with low-resolution MS [57] | ~60% more impurities identified with LC-FTMS [57] | Offers a more complete and accurate impurity profile for process understanding and control. |
GLP and Regulatory Alignment
Framing the 2D-LC-HRMS workflow within GLP ensures the generation of reliable, auditable data. Key considerations include:
- Method Validation: While the complexity of 2D-LC presents validation challenges, parameters such as specificity, accuracy, precision, and LOD/LOQ for target impurities must be established. The inherent orthogonality and peak capacity of 2D-LC directly support demonstrations of specificity [58].
- System Suitability and Robustness: Procedures like Dynamic Peak Parking (DPP) directly enhance method robustness by compensating for expected variations in chromatographic conditions, a critical aspect of ensuring data quality over the method's lifecycle [61].
- Data Integrity: The automated nature of on-line 2D-LC reduces manual intervention (e.g., compared to off-line fraction collection), minimizing errors and improving the traceability of the analytical process [63]. All data, including the 'D and 'D chromatograms and MS spectra, must be stored in a raw, unprocessed, and auditable format.
The integration of two-dimensional liquid chromatography with high-resolution mass spectrometry provides a formidable solution to the persistent challenges of co-elution and low-level impurity detection in pharmaceutical development. By leveraging orthogonal separation mechanisms to dramatically increase peak capacity and coupling this with the definitive identification power of HRMS, the 2D-LC-HRMS platform enables analytical scientists to achieve a depth of product understanding that is both technically superior and fully aligned with the rigorous principles of Good Laboratory Practices. As this technology continues to become more robust and user-friendly with commercial instrumentation and software, its adoption is poised to become a standard for characterizing complex therapeutics—from small molecules and peptides to oligonucleotides and biologics—ensuring the highest standards of product quality and patient safety.
Managing Heterogeneous Lab Environments and Isolated Data Silos
In modern drug development, analytical chemists and research scientists operate within increasingly complex laboratory environments. These environments are characterized by two interconnected challenges: heterogeneous systems and isolated data silos. Heterogeneity manifests in various forms, including diverse instrument types from multiple vendors, varying data formats, specialized software applications, and disparate operational protocols across departments. This technical diversity inevitably leads to the creation of data silos—collections of data held by one group that are not easily or fully accessible by other groups within the same organization [64].
Within the framework of Good Laboratory Practice (GLP), these challenges present significant regulatory and operational risks. GLP regulations provide a quality system covering the organizational processes and conditions under which nonclinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and retained [4]. The fundamental principles of GLP—including proper documentation, data integrity, and traceability—become exponentially more difficult to maintain when data is fragmented across disconnected systems. The regulated laboratory must therefore implement strategic approaches to manage heterogeneity and eliminate silos to ensure both regulatory compliance and operational excellence.
The Impact of Data Silos on Laboratory Operations and Data Integrity
Data silos undermine core GLP requirements in several significant ways, creating barriers to information sharing and collaboration across departments [64]. In the context of GLP-regulated studies, these barriers directly impact data quality, integrity, and ultimately, study validity.
Operational and Scientific Consequences
- Limited Data View: Silos prevent relevant data from being shared, limiting each department's analysis to its own narrow view [64]. For the analytical chemist supporting a toxicokinetic study, this may mean incomplete understanding of sample history or preparation methods, potentially compromising result interpretation.
- Threatened Data Integrity: When data is siloed, the same information is often stored in different databases, leading to inconsistencies between departmental data [64]. From a GLP perspective, this violates the fundamental principle of data accuracy and reliability [4].
- Resource Inefficiency: Storing the same information in different places wastes precious storage and requires redundant IT maintenance [64]. This is particularly problematic in GLP environments where data must be retained for specific periods [4].
- Impaired Collaboration: Data silos reinforce cultural separation between departments, making collaboration difficult [64]. In drug development, this can delay critical decisions as information flows sluggishly between analytical, bioanalytical, and toxicology teams.
Regulatory Compliance Implications
From a GLP perspective, the most significant risk of data silos lies in their potential to compromise data integrity and traceability. The GLP principle of Good Documentation Practice (GDocP) requires that all data be Attributable, Legible, Contemporaneous, Original, and Accurate (ALCOA+) [4]. Siloed data environments make it exceptionally difficult to maintain these standards across the entire data lifecycle. Furthermore, the GLP requirement for a Quality Assurance Unit (QAU) to conduct inspections becomes more complex when data is fragmented across multiple inaccessible systems [4].
Table 1: Impact of Data Silos on GLP Compliance Elements
| GLP Compliance Element | Impact of Data Silos | Potential Regulatory Risk |
|---|---|---|
| Good Documentation Practice (GDocP) | Inconsistent metadata across systems; difficulty maintaining data provenance | Data integrity deficiencies; regulatory citations |
| Quality Assurance Unit Inspections | QAU cannot access complete data trail for audit | Incomplete study audits; compliance failures |
| Study Director Responsibility | Difficulty overseeing all aspects of study | Failure to maintain overall control of study |
| Final Report Completeness | Risk of omitting relevant data from final report | Submission deficiencies; approval delays |
| Data Retention | Multiple storage systems with inconsistent retention policies | Inability to reconstruct studies during regulatory inspection |
Methodologies for Integrating Heterogeneous Laboratory Data
Effective management of heterogeneous lab environments requires systematic approaches to data integration. Multiple methodologies exist, each with distinct advantages for GLP-regulated environments.
Structured versus Unstructured Data Processing
Laboratory data exists in two primary forms, each requiring different handling approaches [65]:
Structured data are well-organized and precisely formatted, typically existing in relational database management system (RDBMS) format. In the analytical laboratory, this includes data from chromatography data systems (CDS) or laboratory information management systems (LIMS) that store information in tables with linked rows and columns.
Unstructured data include information in various forms that do not conform to common data models, such as instrument log files, image data, or textual observations. These are more difficult to analyze and are not easily retrievable using conventional database approaches.
For GLP compliance, structured data approaches are generally preferred for their inherent traceability and validation capabilities. However, modern laboratories must handle both types effectively. Conversion methods for transforming unstructured to structured data include [65]:
- Normalization: Reducing data expressed in different ways to a standardized format
- Categorization: Grouping objects according to certain properties using tags
- Syntactic Parsing: Analyzing sequences of formal elements to determine grammatical structure
- Content Analysis: Identifying key themes and concepts using statistical methods
Data Integration Techniques
Several data integration techniques have emerged as effective solutions for heterogeneous laboratory environments [65]:
- Manual Integration or Common User Interface: Provides users with access to all source systems through unified web interfaces
- Application-Based Integration: Specifically designed for a finite number of applications within the laboratory environment
- Middleware Data Integration: Transfers logic from applications to a new middleware layer
- Unified Data Access or Virtual Integration: Defines a set of views that give users access to a single view of all data
Table 2: Data Integration Techniques for GLP Environments
| Integration Technique | Best Suited Laboratory Scenarios | GLP Compliance Considerations |
|---|---|---|
| Cloud-Based ETL (Extract, Transform, Load) | Multi-site studies; high data volume environments | Ensure cloud provider meets GLP electronic record requirements; maintain audit trails |
| Laboratory Information Management System (LIMS) | Centralized sample management; regulated studies | Validate system per GLP requirements; ensure proper user access controls |
| Middleware Data Integration | Environments with legacy instruments and systems | Maintain data integrity during transformation; document all mapping procedures |
| Unified Data Access | Research environments requiring flexible data exploration | Implement procedures to ensure data views do not alter original records |
| API-Based Integration | Real-time data sharing between validated systems | Validate all interfaces; maintain complete transaction logs |
Experimental Protocols for Data Integration in GLP Environments
Implementing data integration in regulated laboratories requires carefully controlled protocols to maintain GLP compliance. The following methodologies provide structured approaches for integrating heterogeneous data sources while preserving data integrity.
Protocol: Implementation of a Centralized Data Repository
Objective: To create a single, GLP-compliant repository for all study data that ensures data accessibility, integrity, and traceability.
Materials and Equipment:
- Validated server infrastructure (cloud or on-premises)
- Data warehouse or data lake software
- Network infrastructure with appropriate security controls
- Backup and disaster recovery systems
Procedure:
- System Qualification: Qualify the repository infrastructure following GLP equipment validation protocols [4].
- Data Mapping: Document all data sources, formats, and metadata requirements using a standardized taxonomy.
- ETL Process Development: Implement automated Extract, Transform, Load processes for each data source:
- Extract: Establish secure connections to source systems
- Transform: Convert data to standardized formats while preserving original values
- Load: Transfer transformed data to the central repository
- Metadata Application: Apply consistent metadata tags to all data elements, ensuring alignment with GLP study identifiers.
- Access Control Implementation: Establish role-based access controls that reflect organizational responsibilities and GLP requirements.
- Audit Trail Configuration: Enable comprehensive audit trails that capture all data interactions, modifications, and accesses.
- System Validation: Execute protocol testing to verify data integrity throughout the integration process.
Quality Control: The Quality Assurance Unit must verify that the implementation maintains data integrity and meets all GLP requirements for electronic records [4].
Protocol: Integration of Heterogeneous Instrument Data
Objective: To standardize data outputs from diverse laboratory instruments for consolidated analysis and reporting while maintaining GLP compliance.
Materials and Equipment:
- Source instruments with data export capabilities
- Data transformation software or scripts
- Validated conversion algorithms
- Standardized data templates
Procedure:
- Instrument Inventory: Catalog all instruments, their data formats, and export capabilities.
- Standardized Format Definition: Establish a laboratory-wide standard data format based on industry standards (e.g., AnIML, Allotrope).
- Transformation Development: Create and validate data transformation routines for each instrument type:
- Develop parsing algorithms for instrument-specific data formats
- Map instrument-specific metadata to standardized terminology
- Preserve raw data files in original format as required by GLP
- Validation Testing: Execute comparative testing to verify transformed data matches original instrument outputs.
- Integration Implementation: Deploy transformation routines within the laboratory workflow.
- Documentation: Complete comprehensive documentation including transformation algorithms, validation results, and operating procedures.
Quality Control: The analytical chemist must verify that data transformations preserve numerical accuracy and contextual metadata through statistical comparison of original and transformed data.
Visualization of Data Integration Workflows
Effective management of heterogeneous laboratory data requires well-defined workflows that maintain GLP compliance throughout the data lifecycle. The following diagrams illustrate key processes for integrating disparate data sources into a unified, compliant environment.
GLP Data Integration Workflow
Data Integrity Verification Process
The Scientist's Toolkit: Essential Solutions for Heterogeneous Data Management
Successful management of heterogeneous laboratory environments requires both technical solutions and methodological approaches. The following tools and systems form a comprehensive toolkit for analytical chemists operating in GLP-regulated environments.
Table 3: Research Reagent Solutions for Data Integration
| Tool Category | Specific Solutions | Function in Managing Heterogeneity |
|---|---|---|
| Laboratory Information Management Systems (LIMS) | Clarity LIMS, Thermo Fisher LIMS | Track samples, manage associated data, automate workflows, and integrate instruments [66] [67] |
| Data Integration Platforms | Cloud-based ETL Tools, Talend Data Fabric | Extract, transform and load data from disparate sources into a unified format [64] |
| Electronic Laboratory Notebooks (ELN) | GLP-compliant ELN systems | Provide structured environment for recording experimental data with full audit trails [4] |
| Data Standardization Tools | AnIML, Allotrope Framework | Convert instrument-specific data into standardized formats for comparison and analysis |
| Quality Management Systems | Electronic QAU tools | Enable Quality Assurance Units to monitor studies and conduct inspections across integrated data systems [4] |
| Cloud Data Repositories | Validated cloud data warehouses | Centralize storage of study data with appropriate access controls and backup [64] |
Managing heterogeneous lab environments and eliminating data silos represents both a technical challenge and a regulatory imperative for analytical chemists working under GLP standards. The integration methodologies, experimental protocols, and toolkits presented in this whitepaper provide a framework for transforming fragmented data ecosystems into unified, compliant environments. By implementing these strategies, drug development professionals can enhance data integrity, improve operational efficiency, and maintain rigorous compliance with GLP regulations while accelerating the development of new therapeutics.
The essential conclusion for researchers and scientists is that effective data management must be viewed not as an administrative burden, but as a fundamental scientific and quality requirement. In an era of increasingly complex laboratory technologies and data sources, the principles outlined here provide a path toward robust, reproducible, and compliant research practices that form the foundation of reliable drug development.
Optimizing Sample Preparation to Avoid Adsorption, Loss, and Artefactual Modifications
In Good Laboratory Practice (GLP) for analytical chemistry, sample preparation is not merely a preliminary step but a pivotal stage that determines the success or failure of an entire analysis. For researchers and drug development professionals working with sensitive biomolecules, particularly peptides like GLP-1 receptor agonists, ineffective sample preparation can lead to substantial analyte loss, inaccurate measurements, and ultimately, false scientific conclusions [68]. The unpredictable nature of peptide binding to surfaces necessitates systematic optimization of experimental containers and protocols to ensure data reliability and regulatory compliance [68]. This technical guide provides a comprehensive framework for optimizing sample preparation workflows to mitigate adsorption, prevent artefactual modifications, and ensure the integrity of analytical results within GLP environments.
Fundamental Challenges in Sample Preparation
Mechanisms of Adsorption and Loss
Peptides and proteins, being inherently amphiphatic in nature, readily absorb to most surfaces encountered during laboratory analysis [68]. This absorptive behavior stems from:
- Hydrophobic and Hydrophilic Interactions: Peptides possess mixed polarity, leading to both hydrophobic and electrostatic interactions with container surfaces [69].
- Ionic Interactions: Depending on their net charge and the pH of the solution, peptides can undergo strong ionic interactions with container walls [55].
- Surface Compatibility Issues: The amphiphilic characteristics of peptides like GLP-1 analogs complicate their behavior in analytical systems, increasing susceptibility to adsorption [69].
The extent of adsorption varies significantly based on a peptide's physicochemical properties, including net ionic charge (ranging from -4 to +6), size (8 to 154 amino acids), end groups, and post-translational modifications such as acylation and sulfation [68].
Consequences of Inadequate Preparation
Inadequate sample preparation manifests in several critical analytical deficiencies:
- Inaccurate Quantification: Substantial loss of peptides to container surfaces leads to underestimation of actual concentration levels [68].
- Impaired Sensitivity: Adsorption phenomena particularly affect detection capabilities at the limit of quantitation (LOQ), compromising method sensitivity [55].
- Reduced Reproducibility: Inconsistent recovery rates introduce variability that undermines method robustness and reliability [55] [69].
- Instrumental Fouling: Transfer of inadequately prepared samples to LC-MS systems can lead to contamination of the interface and other components, increasing downtime and maintenance costs [70].
Material Selection and Container Optimization
Comparative Surface Recovery Profiles
Choosing the appropriate experimental container is fundamental to avoiding unpredictable peptide loss. Research demonstrates significant differences in peptide binding capacities across various surfaces [68]. The recovery rates of radiolabeled peptides from different container materials under standardized conditions reveal crucial patterns for material selection.
Table 1: Percentage Recovery of 125I-Labeled Peptides from Different Surfaces After 48 Hours
| Peptide | Borosilicate Glass | Flint Glass | Polypropylene | Polystyrene |
|---|---|---|---|---|
| Ghrelin | 45% | 51% | 89% | 92% |
| GLP-1 | 62% | 58% | 94% | 90% |
| Insulin | 68% | 65% | 91% | 88% |
| Leptin | 59% | 62% | 93% | 90% |
| CCK-8S | 71% | 68% | 95% | 92% |
| PYY | 66% | 63% | 92% | 89% |
Data adapted from recovery experiments conducted with radiolabeled peptides [68].
Practical Guidelines for Container Selection
Based on comprehensive recovery studies, the following guidelines emerge for container selection:
- Polypropylene Surfaces: Generally provide superior recovery for most peptides due to lower binding affinity [68].
- Borosilicate Glass: Demonstrates variable recovery, performing adequately for some peptides but showing significant loss for others [68].
- Siliconization Treatment: Applying siliconizing fluid to glass surfaces decreases binding to some extent but does not equal the performance of optimal plastic surfaces [68].
- Specialized Applications: For procedures requiring ultrahigh centrifugation, polyallomer or polycarbonate tubes are necessary and should be evaluated for peptide compatibility [68].
The evidence clearly indicates that no single surface is optimal for all peptides, emphasizing the necessity of empirical determination of the best container for each specific peptide [68].
Diluent and Buffer Optimization Strategies
Key Parameters for Diluent Selection
Diluent selection profoundly influences recovery, adsorption, and stability during sample preparation. Critical parameters to consider include:
- Isoelectric Point (pI) Considerations: The pH of the buffer must be optimized relative to the peptide's isoelectric point to minimize ionic interactions. At pH lower than pI, the molecule contains a net positive charge, while at pH greater than pI, there is an overall negative charge [55].
- HPLC Index Compatibility: The diluent must be compatible with subsequent chromatographic separation to avoid peak distortion or shifting [55].
- Additive Selection: Mobile phase additives such as trifluoroacetic acid (TFA) can significantly suppress ionization in mass spectrometry, requiring careful optimization [55].
Effective Additives for Improving Recovery
Table 2: Common Additives for Minimizing Peptide Adsorption and Loss
| Additive | Concentration Range | Mechanism of Action | Applications |
|---|---|---|---|
| Bovine Serum Albumin (BSA) | 0.1-1% | Competes for binding sites on container surfaces | Radioimmunoassays, general peptide handling |
| Fmoc-arginine | 100-300 µM | Amphiphatic structure blocks hydrophobic and ionic interactions | Peptide purification, mass spectrometry |
| Ion-Pairing Reagents (TFA) | 0.05-0.1% | Modifies peptide interaction with surfaces and stationary phases | LC-MS analysis, particularly for hydrophobic peptides |
| Organic Solvents | 1-10% | Reduces hydrophobic interactions by altering solvation | Sample dilution prior to chromatographic analysis |
| High Salt Concentrations | 50-200 mM | Disrupts electrostatic interactions with surfaces | Extraction from complex matrices |
Optimized Diluent Formulations
For GLP-1 peptides and similar analogs, specific diluent formulations have demonstrated efficacy:
- Acidic Diluents: For peptides with basic characteristics, diluents containing 0.1% acetic acid have shown improved recovery and stability during storage [68].
- BSA-Containing Buffers: Addition of 1% BSA to assay buffers significantly improves recovery from various surfaces, making it particularly valuable for radioimmunoassays and ELISA procedures [68].
- Combination Approaches: Using specialized containers with optimized diluents provides the most robust protection against adsorption. For instance, combining polypropylene tubes with BSA-containing buffers typically yields recovery rates exceeding 89% for most peptides [68].
Experimental Protocols for Method Optimization
Protocol 1: Container Compatibility Assessment
Purpose: To determine the optimal container material for a specific peptide to minimize adsorption losses.
Materials:
- Peptide of interest (standard solution)
- Radiolabeled or fluorescently-labeled analog (for detection)
- Test containers (borosilicate glass, flint glass, polypropylene, polystyrene)
- Appropriate assay buffer
- Siliconizing agent (optional)
- Gamma counter or fluorescence plate reader
Procedure:
- Prepare a standardized solution of the peptide in assay buffer at a concentration relevant to experimental conditions.
- Aliquot identical volumes into each test container type (n=5 per group).
- Incubate at relevant temperature (typically 4°C or room temperature) for 24-48 hours.
- Transfer solutions to fresh, low-binding containers and quantify remaining peptide.
- Compare recovery rates across container types using statistical analysis (ANOVA with post-hoc testing).
- For problematic peptides, repeat assessment with siliconized containers or with BSA (1%) added to the buffer.
Validation: The optimal container demonstrates >85% recovery with low variability (CV <5%) [68].
Protocol 2: Diluent Optimization Procedure
Purpose: To identify the diluent composition that maximizes recovery and stability for a specific peptide.
Materials:
- Peptide standard
- Candidate buffers (varying pH, ionic strength, additives)
- Optimized container material (from Protocol 1)
- Analytical instrumentation for quantification (HPLC-UV, LC-MS)
Procedure:
- Prepare peptide solutions in each candidate diluent at standardized concentration.
- Aliquot into optimized containers and incubate under relevant conditions.
- Measure initial concentration and at predetermined time points (1, 4, 24 hours).
- Assess not only recovery but also formation of degradation products or aggregates.
- Evaluate compatibility with analytical endpoints (chromatography, mass spectrometry).
- Select the diluent that provides optimal recovery while maintaining analytical compatibility.
Key Considerations:
- pH should be at least 1 unit away from peptide pI to minimize ionic interactions [55]
- Additives should not interfere with subsequent analysis
- Conditions should mimic final experimental setup as closely as possible
Workflow Integration and GLP Compliance
Comprehensive Sample Preparation Workflow
The sample preparation process must be structured as a coordinated sequence of optimized steps, as visualized in the following workflow:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Optimized Sample Preparation
| Item | Function | Application Notes |
|---|---|---|
| Polypropylene Tubes | Primary container with low binding properties | Superior recovery for most peptides compared to glass or polystyrene |
| Bovine Serum Albumin (BSA) | Blocking agent that competes for binding sites | Use at 0.1-1% in buffers; avoid in MS sample preparation |
| Fmoc-arginine | Amphiphatic blocking reagent | Effective at 100-300 µM; compatible with mass spectrometry |
| Siliconizing Fluid | Surface treatment to reduce adsorption | Applied to glass surfaces; less effective than optimal plastic |
| Low-Binding Tips and Tubes | Specialized surfaces to minimize loss | Essential for low-concentration samples near LOQ |
| Acetic Acid Solutions | Acidic diluent for basic peptides | 0.1% solution improves stability and recovery |
| Ion-Pairing Reagents | Modulate peptide-surface interactions | TFA (0.05-0.1%) common but may suppress MS ionization |
GLP Documentation Requirements
In regulated environments, sample preparation protocols must be thoroughly documented to ensure reproducibility and compliance:
- Standard Operating Procedures (SOPs): Detailed, step-by-step protocols for sample handling, including specific container specifications and diluent formulations [70].
- Method Validation Data: Recovery studies demonstrating optimization of sample preparation conditions for each analyte [55].
- Stability Records: Documentation of sample stability under prepared conditions, including time-to-analysis windows [69].
- Quality Control Metrics: Regular monitoring of recovery rates as part of method performance verification [70].
Optimizing sample preparation to avoid adsorption, loss, and artefactual modifications represents a critical investment in data quality and reliability. Through systematic evaluation of container materials, strategic formulation of diluents, and implementation of targeted additives, researchers can significantly improve recovery and reproducibility in peptide analysis. The methodologies outlined in this guide provide a framework for developing robust, GLP-compliant sample preparation workflows that maintain analyte integrity from collection to analysis. In an era of increasingly complex therapeutics like GLP-1 receptor agonists, such rigorous attention to sample preparation fundamentals is not merely advantageous—it is essential for generating meaningful, actionable analytical data in drug development research.
Strategies for Ensuring Robustness and Reproducibility in Chromatographic Methods
Within the framework of Good Laboratory Practice (GLP), the reliability of analytical data is paramount. For chromatographic methods, this reliability rests on two foundational concepts: robustness and reproducibility. These characteristics are not merely academic exercises but are critical for ensuring that methods transfer successfully between laboratories, produce consistent results over time, and generate data that regulatory authorities can trust for making safety assessments on products ranging from human drugs to agrochemicals [15] [10]. GLP is a quality system covering the organizational processes and conditions under which non-clinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and retained [10]. For analytical chemists supporting these studies, demonstrating method robustness and reproducibility is a fundamental part of regulatory compliance.
Although sometimes used interchangeably, robustness and reproducibility refer to distinct and measurable characteristics. The robustness of an analytical procedure is a measure of its capacity to remain unaffected by small, deliberate variations in method parameters listed in the procedure itself [71] [72]. It is an indicator of the method's reliability during normal use. In contrast, reproducibility (often called between-lab reproducibility) expresses the precision between measurement results obtained in different laboratories [73]. It is a measure of a method's transferability. A related, often conflated term is ruggedness, which the USP defines as the degree of reproducibility of results under a variety of normal operating conditions, such as different analysts, instruments, or reagent lots [71]. In modern terminology, this is largely addressed under intermediate precision—the precision obtained within a single laboratory over a longer period, accounting for different analysts, equipment, and reagent batches [71] [73].
Defining the Key Concepts
Robustness vs. Reproducibility: A Critical Distinction
A clear understanding of the differences between robustness and reproducibility is essential for proper method validation and implementation. The table below summarizes their core distinctions.
Table 1: Distinguishing Between Robustness and Reproducibility
| Aspect | Robustness | Reproducibility |
|---|---|---|
| Definition | Measure of method capacity to remain unaffected by small, deliberate variations in procedural parameters [71]. | Precision between measurement results obtained at different laboratories [73]. |
| Scope of Variation | Internal to the method; parameters specified in the procedure (e.g., mobile phase pH, temperature, flow rate) [71]. | External to the method; conditions normal to laboratory operation (e.g., different labs, analysts, instruments) [71]. |
| Primary Focus | Method's inherent reliability and suitability for its intended use. | Method's transferability between different testing sites. |
| When Assessed | Typically during later stages of method development or early in validation [71]. | During method transfer or collaborative studies involving multiple laboratories. |
| Regulatory Context | Addressed in both USP and ICH guidelines, though not always listed as a primary validation characteristic [71]. | Addressed under reproducibility (between-lab) and intermediate precision (within-lab) in ICH Q2(R1) [71] [72]. |
The GLP Framework for Analytical Data
Good Laboratory Practice provides the overarching quality system for non-clinical safety studies. Compliance with GLP ensures the reliability and integrity of studies and the accuracy of the data submitted to regulatory authorities [15]. For analytical chemists, this translates to specific responsibilities:
- Characterization of Test Articles: Analytical chemists develop methods to determine the identity, strength, purity, composition, and stability of drug substances and formulations used in GLP studies [15].
- Bioanalysis: Bioanalytical chemists analyze specimens (e.g., blood, plasma, tissues) from test systems to support pharmacokinetic (PK) and toxicokinetic (TK) studies, using validated methods per guidelines like ICH M10 [15].
- Documentation and Data Integrity: Adherence to good documentation practice (GDocP) principles, often encapsulated by "ALCOA+" (Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, Available), is a core element of GLP compliance [15]. All raw data and documentation must be retained and archived.
The following diagram illustrates how robustness and reproducibility testing fits within the broader method development and validation lifecycle in a GLP environment.
Strategic Approaches to Method Robustness
Key Parameters for Robustness Testing
A robustness study involves the intentional variation of method parameters to see if the method results are affected [71]. The specific parameters chosen depend on the chromatographic mode, but some are nearly universal. For instance, in reversed-phase liquid chromatography (LC), critical parameters often include mobile phase composition, pH, temperature, and flow rate [71]. For the analysis of complex molecules like monoclonal antibodies, parameters such as column temperature and acidic modifier concentration (e.g., TFA) are particularly critical, as they can significantly impact selectivity and recovery [74].
Table 2: Typical Parameters and Ranges for Robustness Testing in LC
| Parameter | Typical Variation | Impact on Method Performance |
|---|---|---|
| Mobile Phase pH | ± 0.1 - 0.2 units | Can dramatically affect retention time, selectivity, and peak shape of ionizable compounds. |
| Column Temperature | ± 2 - 5 °C | Affects retention, efficiency, and backpressure; critical for biomolecule separations [74]. |
| Flow Rate | ± 5 - 10% | Directly impacts retention time, pressure, and possibly resolution. |
| Organic Modifier Concentration | ± 2 - 5% relative | Alters solvent strength, affecting retention times and resolution. |
| Gradient Slope/Time | ± 5 - 10% | Impacts the resolution of all peaks in the chromatogram [74]. |
| Buffer Concentration | ± 5 - 10% | Can affect retention and peak shape for ionizable analytes. |
| Wavelength | ± 2 - 5 nm (if applicable) | May affect detection sensitivity and linearity. |
| Different Column Batches | Batches from different lots | Checks for consistency of stationary phase properties [74]. |
Experimental Designs for Robustness Studies
The traditional "one-variable-at-a-time" approach to robustness testing is inefficient and can miss important interactions between parameters. Multivariate experimental designs, which vary multiple parameters simultaneously, are far more effective and informative [71]. The choice of design depends on the number of factors to be investigated.
- Full Factorial Designs: This design involves studying all possible combinations of factors at their high and low levels. For k factors, this requires 2k runs. While comprehensive, this becomes impractical for more than five factors (e.g., 5 factors = 32 runs) [71].
- Fractional Factorial Designs: These are a carefully chosen subset (a fraction) of the full factorial combinations. They are highly efficient for screening a larger number of factors (e.g., 9 factors can be screened in as few as 32 runs) but come with a trade-off: some effects are "aliased" or confounded with interactions between other factors. Proper design selection, guided by chromatographic knowledge, is key to interpreting the results [71].
- Plackett-Burman Designs: These are very efficient screening designs, useful in multiples of four runs, and are ideal when the goal is to identify which of many factors have significant main effects on the method, rather than to quantify each effect precisely [71].
The strategy for a robustness test can be systematically divided into six steps: select factors and their levels, define a proper experimental design, run the experiments, analyze the results statistically, interpret the effects, and finally, recommend possible improvements or define system suitability criteria [75].
Ensuring Reproducibility and Intermediate Precision
While robustness deals with internal method parameters, reproducibility and its within-lab counterpart, intermediate precision, deal with external factors. As defined in the ICH guidelines, this involves deliberate changes in the operational environment [71] [72].
- Repeatability expresses the precision under the same operating conditions over a short interval of time (intra-assay precision) [73]. It is assessed by analyzing a minimum of nine determinations covering the specified range (e.g., three concentrations, three replicates each) [72].
- Intermediate Precision assesses the within-laboratory variation due to random events, such as different days, different analysts, or different equipment [72] [73]. An experimental design is used so that the effects of these individual variables can be monitored. Results from different analysts using different instruments and preparing their own standards are compared, typically using statistical tests like a Student's t-test [72].
- Reproducibility represents the highest level of precision testing, referring to collaborative studies conducted between different laboratories. This is critical for methods that will be standardized and used across multiple sites, such as in collaborative studies for method standardization [73].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and solutions essential for developing, validating, and implementing robust and reproducible chromatographic methods.
Table 3: Essential Research Reagents and Materials for Robust Chromatography
| Item | Function / Relevance |
|---|---|
| High-Purity Buffers & Solvents | To ensure consistent mobile phase preparation, minimize baseline noise, and prevent system contamination or column degradation. |
| Characterized Test Articles | Drug substances and products of known identity, strength, and purity are required for GLP studies to prepare accurate calibration standards and spikes for recovery studies [15]. |
| Trifluoroacetic Acid (TFA) | A common ion-pairing agent and acidic modifier in reversed-phase LC of proteins and peptides; concentration must be tightly controlled as small variations (e.g., 0.09% vs. 0.11%) can significantly impact retention and recovery [74]. |
| SPP/UHPLC Columns | Columns packed with superficially porous particles (SPP) offer high efficiency and improved mass transfer, beneficial for both small molecules and large biomolecules [45]. |
| "Inert" or "Biocompatible" Columns | Columns with passivated or metal-free hardware are crucial for analyzing metal-sensitive compounds (e.g., phosphorylated molecules, certain pharmaceuticals) to prevent adsorption and poor peak shape [45]. |
| Mass Spectrometry-Compatible Buffers | Volatile buffers (e.g., ammonium formate, ammonium acetate) are essential when coupling LC with MS detection to avoid ion source contamination and signal suppression. |
| System Suitability Standards | A well-characterized mixture of analytes used to verify that the entire chromatographic system is performing adequately before sample analysis begins. |
In the regulated environment of drug development, ensuring the robustness and reproducibility of chromatographic methods is not optional—it is a fundamental requirement of GLP. A strategic approach, which involves clearly distinguishing between these concepts, employing efficient multivariate experimental designs for robustness testing, and rigorously assessing intermediate precision, is crucial for success. By investing in this upfront diligence during method development and validation, analytical scientists can create reliable methods that transfer seamlessly between laboratories, stand up to the rigors of routine use, and generate the high-quality, defensible data that underpin critical product safety decisions.
Ensuring Data Credibility: Method Validation, Compliance, and Quality Assurance
The Imperative of Analytical Method Validation under GLP
Analytical method validation is a critical, non-negotiable component of Good Laboratory Practice (GLP) that serves as the definitive proof of an analytical procedure's suitability for its intended purpose [76]. Within the GLP framework, which governs nonclinical safety studies, the integrity, reliability, and accuracy of all generated data are paramount [2] [4]. Method validation provides the foundational evidence that the analytical methods used to characterize test articles and analyze biological samples meet stringent standards for quality, ensuring that safety assessments submitted to regulatory bodies are trustworthy [4] [34]. This guide details the regulatory requirements, core parameters, and experimental protocols essential for demonstrating that analytical methods are fit-for-purpose under GLP, thereby upholding the integrity of the entire drug development process.
The GLP Framework
Good Laboratory Practice (GLP) is a quality system covering the organizational process and conditions under which nonclinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and archived [2] [4]. Codified in the US by the FDA under 21 CFR Part 58, GLP regulations were established in response to cases of laboratory fraud and misconduct to ensure the quality and integrity of safety data submitted to regulatory agencies [2]. The principal goal of GLP is not to assess the scientific validity of a hypothesis, but rather to ensure that the data collected are reliable, reproducible, and auditable [2]. In essence, GLP focuses on proving how data were collected—cleanly, consistently, and under independent quality assurance oversight [2].
GLP mandates several key components to achieve this goal, including:
- A written study protocol approved before study initiation [2].
- A Study Director with overall responsibility for the study [2].
- An independent Quality Assurance Unit (QAU) responsible for monitoring GLP compliance [2].
- Detailed Standard Operating Procedures (SOPs) for all laboratory operations [2] [8].
- Comprehensive documentation and archiving of all raw data and reports [2] [8].
The Centrality of Analytical Method Validation
For the analytical chemist, method validation is the practical application of GLP principles to the specific procedures that generate critical data. A validated method provides assurance that the results it produces are accurate, precise, and reproducible, which is non-negotiable for studies supporting regulatory submissions like Investigational New Drug (IND) applications [4] [76].
Under GLP, analytical chemists play two primary roles [4]:
- Characterizing the Test Article: Determining the identity, strength, purity, composition, and stability of the drug substance or formulation (21 CFR Part 58.105) [4].
- Bioanalytical Testing: Analyzing biological samples (blood, plasma, urine, tissues) collected from test systems after administration of the test article to determine pharmacokinetic (PK) and toxicokinetic (TK) profiles (21 CFR Part 58.120, 58.130) [4].
In both roles, the methods employed must be validated to demonstrate they are suitable for their intended use, forming the bedrock of credible safety assessments [77] [76].
Regulatory Foundations and Guidelines
Navigating the regulatory landscape is essential for successful method validation. The requirements are harmonized across major international guidelines.
Table 1: Key Regulatory Guidelines for Analytical Method Validation
| Guideline Issuing Body | Guideline Name/Number | Focus and Scope |
|---|---|---|
| International Council for Harmonisation (ICH) | ICH Q2(R2): Validation of Analytical Procedures [78] | The global gold standard for validating analytical procedures; outlines core validation parameters and a science- and risk-based approach. |
| International Council for Harmonisation (ICH) | ICH Q14: Analytical Procedure Development [78] | Provides a framework for systematic, risk-based analytical procedure development, introducing the Analytical Target Profile (ATP). |
| U.S. Food and Drug Administration (FDA) | 21 CFR Part 58 (GLP Regulations) [2] [4] | Legally mandates the standards for conducting nonclinical laboratory studies, including the need for reliable and validated methods. |
| U.S. Food and Drug Administration (FDA) | Bioanalytical Method Validation [4] [77] | Provides specific recommendations for validating methods used for the quantitative determination of drugs and their metabolites in biological matrices. |
| Organisation for Economic Co-operation and Development (OECD) | OECD Principles of GLP [2] [4] | Internationally recognized GLP principles under which data are mutually accepted by member countries, ensuring the quality and integrity of nonclinical safety studies. |
A significant modern evolution in the regulatory mindset is the shift from validation as a one-time event to a lifecycle management approach, as emphasized in the simultaneous issuance of ICH Q2(R2) and ICH Q14 [78]. This new paradigm encourages a more scientific, flexible, and proactive approach to ensuring method quality throughout its entire use.
Core Validation Parameters and Experimental Protocols
The validation process involves experimentally testing a series of performance characteristics to confirm the method is fit-for-purpose. The following parameters, as defined in ICH Q2(R2), form the core of any validation study [78] [77].
Table 2: Core Analytical Method Validation Parameters and Protocols
| Validation Parameter | Experimental Protocol & Methodology | Acceptance Criteria (Example) |
|---|---|---|
| Accuracy | Protocol: Analyze a minimum of 3 replicates at 3 different concentration levels (e.g., 80%, 100%, 120% of target) covering the specified range. Spiked samples with known quantities of analyte are used. Calculation: (Mean Measured Concentration / Theoretical Concentration) x 100 [78] [77]. | Recovery should be within 98-102% for drug substance assays. |
| Precision | 1. Repeatability: Analyze 6 replicates at 100% of the test concentration by the same analyst on the same day. 2. Intermediate Precision: Perform the analysis on different days, with different analysts, or using different instruments. Calculation: Relative Standard Deviation (RSD) of the results [78] [77]. | RSD ≤ 1.0% for repeatability; RSD ≤ 2.0% for intermediate precision (for drug substance assay). |
| Specificity | Protocol: Chromatographic Methods: Inject blank matrix, placebo, standard, and sample to demonstrate baseline separation of the analyte from any potential interferents (impurities, degradation products, matrix components). Forced degradation studies (acid/base, oxidative, thermal stress) are often used [77]. | The method should be able to unequivocally assess the analyte in the presence of components that may be expected to be present. No interference at the retention time of the analyte. |
| Linearity | Protocol: Prepare a series of standard solutions (e.g., 5-8 concentrations) across the defined range. Plot the instrument response (e.g., peak area) versus concentration. Calculation: Perform linear regression analysis to obtain the correlation coefficient (r), slope, and y-intercept [78] [77]. | Correlation coefficient (r) ≥ 0.998. |
| Range | The interval between the upper and lower concentration levels for which linearity, accuracy, and precision have been demonstrated [78]. | Typically established from the linearity study, e.g., 80-120% of the test concentration for an assay. |
| Limit of Detection (LOD) & Quantitation (LOQ) | LOD: Signal-to-Noise ratio of 3:1, or based on the standard deviation of the response and the slope. LOQ: Signal-to-Noise ratio of 10:1, or based on the standard deviation of the response and the slope. LOQ must also be demonstrated with acceptable accuracy and precision [78] [77]. | LOD: Typically 1/3rd of the LOQ. LOQ: Accuracy and Precision should be within ±20% (for trace analysis). |
| Robustness | Protocol: Deliberately introduce small, deliberate variations in method parameters (e.g., mobile phase pH ±0.2 units, flow rate ±10%, column temperature ±5°C). Evaluate the impact on system suitability criteria (e.g., resolution, tailing factor) [78] [77]. | The method should remain unaffected by small variations, meeting all system suitability requirements. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Analytical Method Validation
| Item | Function in Validation |
|---|---|
| Certified Reference Standard | Provides a substance of known purity and identity to prepare calibration standards, serving as the benchmark for all quantitative measurements. |
| High-Purity Solvents & Reagents | Ensure the mobile phase and sample solutions are free from interferents that could affect baseline noise, retention times, or detector response. |
| Blank Biological Matrix | Essential for bioanalytical validation; used to prepare calibration standards and quality control samples to assess specificity, matrix effects, and accuracy. |
| Stable Isotope-Labeled Internal Standard | Used in LC-MS/MS bioanalysis to correct for variability in sample preparation, injection, and ionization efficiency, improving accuracy and precision. |
| Characterized Impurities and Degradation Products | Used to challenge the method's specificity, ensuring it can separate and quantify the analyte of interest from potential impurities. |
The Method Validation Workflow under GLP
The journey from method development to a fully validated status under GLP is a structured process that integrates rigorous scientific testing with comprehensive documentation and quality assurance. The following diagram illustrates the key stages and their relationships.
Detailed Workflow Stages
Define the Analytical Target Profile (ATP): Before any laboratory work begins, the intended purpose of the method and its required performance criteria must be prospectively defined [78]. The ATP is a foundational element of ICH Q14 and answers the question: "What do we need this method to do?" It specifies the analyte, the concentration range, and the required levels of accuracy and precision.
Method Development: A systematic approach is used to create a method capable of meeting the ATP. This involves selecting the technique (e.g., HPLC, LC-MS), optimizing conditions (column, mobile phase, detection), and conducting preliminary experiments to understand the method's behavior [78] [76]. Knowledge gained here informs the robustness testing in the validation protocol.
Create the Validation Protocol: A detailed, written protocol is essential [76]. It must be approved before validation begins and should specify:
- The validation parameters to be tested (from Table 2).
- The exact experimental design and methodology for each parameter.
- Pre-defined acceptance criteria for each test.
- Responsibilities of personnel involved.
Execute Protocol and Document Data: The laboratory work is performed precisely as outlined in the protocol. Good Documentation Practice (GDocP) is critical here. All raw data, including chromatograms, sample weights, and calculations, must be recorded contemporaneously, legibly, and indelibly, adhering to ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) [4]. The chain of custody for all test articles and samples must be meticulously maintained [4] [34].
QAU Audit and Independent Review: The independent Quality Assurance Unit (QAU) audits the conduct of the validation study. They inspect the raw data, records, and facilities to ensure compliance with the protocol, SOPs, and GLP regulations [2] [8]. The QAU does not approve the science but verifies that the processes were followed. They issue a statement attesting to GLP compliance for the final report.
Finalize and Archive the Validation Report: A final report is generated, summarizing the objectives, methods, results, and conclusion on the method's validity. All data, the report, and the QAU statement are archived for the legally mandated period (minimum of 5 years for FDA, 10 years for EPA) to ensure long-term traceability [2] [34].
Analytical method validation is not merely a regulatory hurdle but a scientific and ethical imperative within the GLP framework. It is the definitive process that transforms a laboratory procedure from a theoretical technique into a trusted tool for decision-making. For analytical chemists and drug development professionals, a rigorous, well-documented validation provides the confidence that safety data are accurate and reliable, ultimately protecting public health and ensuring the efficacy of new therapeutics. By embracing the modern, lifecycle approach outlined in ICH Q2(R2) and Q14, and by embedding GLP principles—meticulous documentation, independent QA, and robust protocols—into every step of validation, laboratories can uphold the highest standards of data integrity and scientific excellence.
For analytical chemists and drug development professionals, ensuring the reliability of generated data is not just a scientific endeavor but a regulatory imperative. Within the framework of Good Laboratory Practice (GLP), analytical method validation provides the documented evidence that a testing procedure is fit for its intended purpose [79]. GLP is a quality system regulating the organizational processes and conditions under which nonclinical laboratory studies are planned, performed, monitored, recorded, reported, and archived [15] [2]. Its principal goal is to assure the quality and integrity of safety test data submitted to regulatory authorities [2].
This foundation makes the validation of analytical methods a cornerstone of compliance. As codified in the ICH Q2(R2) guideline, validation demonstrates that methods are suitable for providing data to support the identity, strength, quality, and purity of drug substances and products [80] [81]. Among the key parameters, accuracy, precision, selectivity, and linearity form the essential pillars for proving that a method produces results that are correct, consistent, specific, and proportional across the intended range [79] [82]. This guide provides an in-depth technical examination of these four critical parameters, framing them within the rigorous demands of GLP to help researchers build robust, defensible, and reliable analytical methods.
Core Principles of Good Laboratory Practice (GLP)
Good Laboratory Practice (GLP) is a regulatory requirement that ensures the quality, reliability, and integrity of nonclinical safety studies conducted during drug development [15]. According to 21 CFR Part 58, GLP applies to nonclinical laboratory studies that support applications for research or marketing permits for products regulated by the FDA [2]. The core objective is to ensure that study data are accurate, reproducible, and auditable, thereby forming a trustworthy foundation for regulatory decisions on product safety [2].
For the analytical chemist, several GLP elements are of paramount importance. The Study Director carries ultimate responsibility for the technical conduct of the study, while an independent Quality Assurance Unit (QAU) audits critical phases to ensure GLP compliance [15] [1]. All equipment must be appropriately designed, calibrated, and maintained, and every aspect of the study must be conducted according to pre-defined Standard Operating Procedures (SOPs) and a detailed study protocol [1]. A critical practice is Good Documentation Practice (GDocP), often described by the acronym "ALCOA+"—requiring data to be Attributable, Legible, Contemporaneous, Original, and Accurate, as well as Complete, Consistent, Enduring, and Available [15]. This framework of controlled procedures and comprehensive documentation provides the context in which analytical method validation occurs, ensuring that all generated data is of the highest integrity.
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of validation protocols under GLP requires the use of well-characterized materials and reagents. The following table details key items essential for experiments validating accuracy, precision, selectivity, and linearity.
| Item | Function in Validation |
|---|---|
| Reference Standards | Highly purified substances of known identity and concentration used as benchmarks to prepare calibration curves and spiked samples for accuracy, precision, and linearity studies [83]. |
| Test and Control Articles | The drug substance or product being studied (test article) and the placebo or comparator (control article). Under GLP, these must be thoroughly characterized for identity, purity, composition, and stability [15] [2]. |
| Blank Matrix | The biological or sample material (e.g., plasma, a cream base) without the analyte. It is used to prepare calibration standards and quality control samples to assess selectivity and the absence of interference [79] [83]. |
| Chemical Reagents & Solvents | High-purity reagents, buffers, and solvents are required for sample preparation, mobile phases, and other solutions. Their quality must be specified in SOPs to ensure consistent method performance and robustness [1]. |
| System Suitability Test Solutions | Mixtures containing the analyte and key interferents used to verify that the analytical system (e.g., HPLC) is performing adequately at the start of each run, checking parameters like resolution and precision [84]. |
Detailed Examination of Key Validation Parameters
Accuracy
Definition and Regulatory Context Accuracy is defined as the closeness of agreement between a test result and an accepted reference value, or true value [79] [82]. It measures the exactness of an analytical method and is typically expressed as percent recovery [82]. Under ICH guidelines, demonstrating accuracy proves that a method measures what it is intended to measure without significant bias [80] [81].
Experimental Protocol for Assessment The accuracy of a method should be established across its specified range, typically using a minimum of nine determinations over a minimum of three concentration levels (e.g., low, medium, and high) [79] [80]. The following procedure is standard:
- Preparation of Spiked Samples: Known quantities of the reference standard are introduced (spiked) into a blank matrix to create samples of known concentration (e.g., 80%, 100%, and 120% of the target concentration) [79].
- Analysis and Calculation: The spiked samples are analyzed using the method under validation. The measured concentration for each sample is compared to the theoretical (spiked) concentration.
- Recovery Calculation: Percent recovery is calculated for each sample using the formula: Recovery (%) = (Measured Concentration / Theoretical Concentration) × 100 [82].
- Data Interpretation: The mean recovery across all replicates and concentration levels is reported. Acceptance criteria depend on the sample type and range but are often set at 98–102% recovery for drug substance assays and with tighter or wider ranges as justified [82].
Quantitative Acceptance Criteria
| Application | Typical Acceptance Criteria for Accuracy (% Recovery) |
|---|---|
| Drug Substance Assay | 98 - 102% [81] |
| Drug Product Assay | 98 - 102% |
| Impurity Quantitation | Varies with level; e.g., ±10-20% of the true value |
Precision
Definition and Regulatory Context Precision expresses the degree of scatter between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [79] [81]. It is a measure of the method's repeatability and reproducibility, often expressed as the variance, standard deviation, or coefficient of variation (%RSD) of a series of measurements [79] [82]. A highly precise method will produce tightly grouped results, though it is critical to note that high precision does not guarantee high accuracy [79].
Experimental Protocol for Assessment Precision is evaluated at three tiers: repeatability, intermediate precision, and reproducibility [82] [80].
- Repeatability (Intra-assay Precision): This assesses precision under the same operating conditions over a short interval. It is determined by analyzing a minimum of six replicates of a homogeneous sample at 100% of the test concentration [79] [81]. The %RSD is calculated from the results.
- Intermediate Precision: This evaluates the impact of random, intra-laboratory variations, such as different analysts, different days, or different equipment. The experimental design should incorporate these variables, and the combined %RSD from all results is calculated [80].
- Reproducibility (Ruggedness): This represents the precision between laboratories, as assessed during method transfer or collaborative studies [79] [82].
Quantitative Acceptance Criteria
| Precision Level | Typical Acceptance Criteria (%RSD) |
|---|---|
| Repeatability | Not more than 1-2% for assay of drug substance/product [82] [81] |
| Intermediate Precision | The method is acceptable if the variability between the results from different conditions meets the pre-defined criteria, often comparable to repeatability. |
Selectivity (Specificity)
Definition and Regulatory Context While often used interchangeably, selectivity and specificity have a nuanced distinction. Specificity is the unequivocal assessment of the analyte in the presence of other components that are expected to be present, such as impurities, degradants, or matrix components [79] [82]. Selectivity is the ability of the method to measure the analyte accurately in the presence of these interferences [79]. In practice, "selectivity" is more frequently used, as analytical techniques are seldom specific to only one analyte [79].
Experimental Protocol for Assessment The method's ability to discriminate is tested by analyzing samples with potential interferents and comparing the results to a control.
- Blank Matrix Analysis: The blank matrix (e.g., placebo, biological fluid) is analyzed to demonstrate the absence of interfering signals at the retention time of the analyte [79] [80].
- Analysis of Spiked/Stressed Samples: The analyte is spiked into the blank matrix in the presence of all potential interferents (e.g., impurities, degradants, metabolites). For stability-indicating methods, this includes analyzing samples that have been forcibly degraded (e.g., via heat, light, acid/base) to produce degradants [82].
- Resolution Assessment: In chromatographic methods, the resolution between the analyte peak and the closest eluting potential interferent peak is calculated. A resolution greater than 1.5 or 2.0 is typically required [82].
Visualizing the Selectivity Assessment Workflow The following diagram illustrates the logical process for experimentally proving method selectivity.
Linearity and Range
Definition and Regulatory Context Linearity is the ability of an analytical procedure to produce test results that are directly proportional to the concentration of the analyte in the sample within a given range [79] [85]. The range of the method is the interval between the upper and lower concentrations of analyte for which it has been demonstrated that the procedure has a suitable level of precision, accuracy, and linearity [79] [81].
Experimental Protocol for Assessment A linearity study involves preparing and analyzing a series of standard solutions at a minimum of five to six concentration levels spanning the intended range (e.g., 80% to 120% of the target concentration for an assay) [79] [83] [80].
- Preparation of Standards: Standard solutions are prepared by serial dilution from a stock solution or by separate weighings.
- Analysis and Plotting: The responses (e.g., peak area) of the standards are plotted against their theoretical concentrations.
- Statistical Analysis: A linear regression model is applied to the data. The correlation coefficient (r), y-intercept, slope, and residual sum of squares are calculated [79] [82]. The correlation coefficient (r) should be ≥ 0.99 [79] [80]. The y-intercept should be statistically indistinguishable from zero, and the residuals should be randomly scattered.
Quantitative Acceptance Criteria
| Parameter | Typical Acceptance Criteria |
|---|---|
| Correlation Coefficient (r) | ≥ 0.99 [79] [80] |
| Y-Intercept | Should be not significantly different from zero (statistically) |
| Residuals | Random scatter around zero |
The rigorous validation of accuracy, precision, selectivity, and linearity is not an academic exercise but a fundamental requirement for generating reliable data within a GLP-compliant environment. These parameters are deeply interconnected; a method must be selective to be accurate, and its linearity and precision define the quantitative range over which it can be accurately applied [79] [82]. For researchers and drug development professionals, a thorough understanding and application of these validation principles, as codified in ICH and FDA guidelines, ensures that analytical methods are fit-for-purpose [80] [81]. This, in turn, guarantees the integrity of the safety and efficacy data that underpin regulatory submissions and, ultimately, protect public health. By adhering to this disciplined approach, analytical chemists uphold the highest standards of scientific rigor and quality, forming the bedrock of trustworthy nonclinical and clinical research.
Meeting FDA Requirements with Orthogonal Methods for Impurity Profiling
For analytical chemists and drug development professionals, ensuring data integrity and regulatory compliance is a fundamental aspect of Good Laboratory Practice (GLP). A core component of this is impurity profiling, a critical activity where the use of orthogonal analytical methods is not just a best practice but often a regulatory expectation. Regulatory bodies like the FDA require the identification and quantification of impurities at very low levels—0.5% for known impurities and 0.10% for unknown ones [55]. Achieving this level of sensitivity and selectivity is exceptionally difficult when impurities co-elute with the main peak or other matrix components.
Orthogonal methods, which employ distinct separation mechanisms or detection principles, provide a robust solution. This approach compensates for the weaknesses of one technique with the strengths of another, delivering a comprehensive and defensible impurity profile. For peptides like GLP-1 receptor agonists, this is particularly crucial. Their complex nature, with strong hydrophilic and hydrophobic interactions, makes separation a significant technical challenge [55]. This guide details the strategic implementation of orthogonal methods to meet FDA requirements within a GLP framework.
Regulatory Framework and GLP Foundations
Good Laboratory Practice (GLP) and Data Integrity
GLP is a quality system governing the organizational processes and conditions under which nonclinical laboratory studies are planned, performed, monitored, recorded, reported, and archived [4]. Its primary goal is to ensure the quality, reliability, and integrity of study data, which is paramount for regulatory submissions.
A core element of GLP compliance is Good Documentation Practice (GDocP), often described by the ALCOA+ principles: data must be Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available [4]. For the analytical chemist, this means contemporaneously recording all aspects of method development, validation, and sample analysis in an Electronic Laboratory Notebook (ELN). Furthermore, all raw data and corresponding documentation must be retained and archived as per standard operating procedures (SOPs) [4] [8].
FDA Requirements for Impurity Profiling
The FDA's requirement for proving impurity sameness is clear: it must be demonstrated using at least two orthogonal analytical methods [55]. This is especially critical for complex drug substances like synthetic peptides.
For generic peptide products, such as GLP-1 receptor agonists, the FDA mandates that the impurity profile of the generic product must be comparable to the Reference Listed Drug (RLD). The presence of new impurities is strictly controlled:
- New impurities ≥ 0.5% are not acceptable.
- New impurities between 0.10% and 0.5% that are absent or present at lower levels in the RLD require a justification demonstrating that the impurity does not impact the product's safety, efficacy, or immunogenicity potential.
- All impurities ≥ 0.10% must be identified and characterized [86].
Meeting these stringent demands requires a well-designed analytical strategy rooted in orthogonal principles.
The Scientific Basis for Orthogonal Methodologies
The Challenge of Peptide Impurity Profiling
The behavior of peptides in chromatographic systems differs fundamentally from that of small molecules. Small molecules are typically retained via a partitioning mechanism. In contrast, due to their large size, only a portion of a peptide interacts with the stationary phase. This interaction is a strong hydrophobic adsorption, resulting in a single adsorption/desorption process that yields sharp peaks but also causes most peptide impurities to elute either immediately before or after the main active peptide peak [55]. This makes baseline separation and accurate quantification particularly challenging.
The Principle of Orthogonality
Orthogonality in analytical chemistry refers to the use of techniques that operate on fundamentally different physical or chemical principles to measure the same analyte. The goal is that if an impurity is separated, detected, or characterized by one method, a second, orthogonal method will confirm its identity and quantity without sharing the same potential for interference or masking. This two-pronged approach significantly reduces the uncertainty in impurity identification and provides regulatory agencies with a higher degree of confidence in the results.
Designing an Orthogonal Method Strategy
The most effective strategy for meeting the FDA's requirement for impurity sameness is to leverage techniques that rely on fundamentally different principles [55]. A one-size-fits-all approach is rarely sufficient; the optimal combination depends on the specific drug substance and its known or potential impurities.
Selection of Primary and Orthogonal Methods
A robust orthogonal strategy for peptide impurity profiling often involves the following combinations:
Table 1: Orthogonal Method Combinations for Peptide Impurity Profiling
| Analysis Goal | Primary Method | Orthogonal Method | Rationale for Orthogonality |
|---|---|---|---|
| Related Substances | Reversed-Phase (RP)-HPLC/UHPLC-UV/DAD (C4, C8, C18 stationary phases) [55] | Hydrophilic Interaction Liquid Chromatography (HILIC) [55] | Separation Mechanism: RP-HPLC separates based on hydrophobicity, while HILIC separates based on hydrophilicity. This is highly effective for resolving co-eluting polar and non-polar impurities. |
| Impurity Identity Confirmation | LC-UV | LC-High Resolution Mass Spectrometry (HRMS) [55] | Detection Principle: UV detection provides retention time and spectral data; HRMS provides exact mass and fragmentation data for definitive structural identification. |
| Aggregate Analysis | Size-Exclusion Chromatography (SEC) [55] | Analytical Ultracentrifugation (AUC) or Field-Flow Fractionation (FFF) | Separation Principle: SEC separates by hydrodynamic volume in an aqueous buffer. AUC separates by sedimentation velocity under centrifugal force, and FFF separates by diffusion coefficient in a cross-flow field. |
| Charge Variants | Cation Exchange Chromatography (CEX) | Capillary Zone Electrophoresis (CZE) | Separation Principle: CEX separates based on electrostatic interactions with a charged stationary phase. CZE separates based on charge-to-size ratio in a free solution under an electric field. |
Advanced and Emerging Orthogonal Techniques
For particularly challenging impurities, more advanced orthogonal techniques are emerging:
- Two-Dimensional Liquid Chromatography (2D-LC-HRMS): This technique combines two different separation mechanisms (e.g., RP in the first dimension and HILIC in the second) in a single automated analysis. It provides superior resolving power, allowing for the separation of very similar impurities that are impossible to resolve with a single column [55].
- Advanced Fragmentation Techniques: Beyond standard Collision-Induced Dissociation (CID), methods like Electron Transfer Dissociation (ETD) provide different and often more informative fragmentation patterns. This is particularly useful for localizing post-translational modifications and identifying complex isoforms [55].
- Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS): This biophysical technique provides information on the higher-order structure (secondary and tertiary) of a molecule by monitoring the exchange of labile hydrogen atoms with deuterium. It is a powerful orthogonal method for confirming conformational changes or structural differences in impurities that are not detectable by standard chromatographic methods [55].
Experimental Protocols and Workflows
Workflow for Comprehensive Impurity Profiling
The following diagram illustrates the integrated workflow for implementing orthogonal methods in impurity profiling, from sample preparation to regulatory submission.
Detailed Methodologies
Sample Preparation Protocol
Proper sample preparation is critical to avoid loss, adsorption, or artefactual modifications of GLP-1 peptides before analysis.
- Diluent Selection: The diluent pH must be optimized relative to the peptide's isoelectric point (pI). At a pH lower than the pI, the molecule carries a net positive charge; at a pH higher, it carries a net negative charge. The pH should be optimized to minimize ionic interactions with glass or plastic consumables [55].
- Procedure:
- Determine pI: Calculate or reference the isoelectric point of the target peptide.
- Prepare Diluent: Prepare a buffer with a pH at least 1.0 unit above or below the pI to ensure the peptide is fully charged and soluble. Common buffers include ammonium acetate or formate.
- Reconstitution: Gently dissolve the peptide in the selected diluent. Avoid vigorous shaking or vortexing to prevent aggregation or shearing.
- Storage: Keep samples at a controlled, cool temperature and analyze promptly to prevent degradation.
Protocol for SEC Aggregate Analysis
Size-exclusion chromatography is key for quantifying aggregates, a critical quality attribute.
- Key Parameters: Resolution is governed by particle size, column length, pore size, and injected sample volume. Use a long column with smaller internal diameter, moderate flow rate, small particle size, and low injection volume for optimal resolution [55].
- Mobile Phase: Use a buffer compatible with peptide stability (e.g., phosphate or citrate buffer). Include sodium chloride at an optimized concentration (e.g., 100-150 mM) to minimize non-specific ionic interactions with the column matrix [55].
- Procedure:
- Equilibration: Equilibrate the SEC column with at least 1.5 column volumes of mobile phase.
- Standard Calibration: Inject a set of molecular weight standards to calibrate the column.
- Sample Analysis: Inject the peptide sample. Ensure the sample matrix is exchanged into the running buffer or that the injection volume is small enough to avoid viscosity effects.
- Data Analysis: Integrate the monomer and aggregate peaks. Calculate the percentage of aggregates based on peak area.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Orthogonal Impurity Profiling
| Item | Function & Importance | Technical Considerations |
|---|---|---|
| Chromatography Columns (C4, C8, C18, HILIC, SEC, Ion Exchange) | The primary tool for separation. Different stationary phases are the foundation of orthogonality. | Select pore size appropriate for peptide molecular weight. C18 for short peptides, C8 or C4 for larger peptides/proteins to prevent irreversible binding [55]. |
| Mass Spectrometry Grade Solvents & Additives | Used in mobile phase preparation for LC-MS. Critical for minimizing ion suppression and background noise. | Use high-purity solvents (e.g., LC-MS grade). Replace ion-pairing agents like TFA with MS-compatible alternatives (e.g., formic acid) to improve sensitivity [55]. |
| Stable Isotope-Labeled Internal Standards | Used in bioanalytical methods to correct for matrix effects and recovery losses, improving accuracy and precision. | Essential for quantitative bioanalysis of peptides in biological matrices (e.g., plasma) for pharmacokinetic/toxicokinetic studies [4]. |
| Reference Standards & Controls | Well-characterized material used to calibrate instruments and validate methods. Crucial for data comparability. | Describe creation, qualification, and stability in regulatory submissions [87]. |
| Validated Cell Lines & Reagents (for Bioactivity/ Potency Assays) | Used in cell-based assays to measure the biological activity of the drug product, an essential orthogonal measure of quality. | Must be properly characterized and controlled. Their quality directly impacts the reliability of potency data, a key CMC requirement [87]. |
In the highly regulated environment of pharmaceutical development, a proactive and strategic approach to impurity profiling is non-negotiable. For analytical chemists operating under GLP, the implementation of a well-considered orthogonal method strategy is the most robust path to generating reliable, high-quality data that unequivocally demonstrates product understanding and control. By leveraging fundamentally different separation and detection mechanisms, as outlined in this guide, scientists can confidently identify and characterize impurities to the stringent levels required by the FDA. This not only ensures compliance and facilitates smoother regulatory reviews but also fundamentally reinforces the commitment to product quality and patient safety.
In the tightly regulated pharmaceutical industry, Good Laboratory Practice (GLP) and Current Good Manufacturing Practice (cGMP) represent two foundational quality systems that govern different stages of a product's lifecycle. For the analytical chemist, understanding the distinction between these frameworks is not merely academic; it is critical to ensuring regulatory compliance, data integrity, and the successful transition of a compound from the research bench to the patient. GLP governs the nonclinical safety studies that form the bedrock of evidence for an investigational product's initial safety profile [2] [4]. In contrast, cGMP (often used interchangeably with GMP) provides the framework for the manufacturing processes that ensure every batch of a marketed drug product is safe, pure, and effective [88] [89]. This guide will delve into the technical specifics of both systems, highlighting their distinct requirements, documentation standards, and practical implications for scientists and drug development professionals.
The genesis of these regulations underscores their importance. GLP regulations emerged in the late 1970s following congressional investigations that uncovered widespread fraud and misconduct in industrial toxicology laboratories, most notably the Industrial Bio-Test Laboratories scandal [2] [37]. This prompted the FDA to formalize quality standards for nonclinical lab studies to ensure data reliability and integrity [2]. Meanwhile, cGMP regulations evolved to prevent contamination, mix-ups, and errors in the manufacturing process, thereby protecting consumers from adulterated drugs [89].
The following table provides a high-level comparison of the core attributes of GLP and cGMP, illustrating their distinct focuses and applications.
Table 1: Core Comparison of GLP and cGMP
| Attribute | Good Laboratory Practice (GLP) | Current Good Manufacturing Practice (cGMP) |
|---|---|---|
| Primary Focus | Data integrity and reliability of nonclinical safety studies [2] [90] | Consistent production quality and safety of marketed products [88] [89] |
| Governing FDA Regulations | 21 CFR Part 58 [2] | 21 CFR Parts 210 & 211 [88] |
| Application Phase | Preclinical research and development [4] [90] | Commercial manufacturing and quality control [91] [90] |
| Key Personnel | Study Director (single point of control) [2] [37] | Quality Control Unit [92] |
| Quality Oversight | Independent Quality Assurance Unit (QAU) [2] | Quality Control Unit and Quality Assurance [92] [9] |
| Core Objective | Ensure study data is accurate, reproducible, and auditable for regulatory submission [2] | Ensure products are consistently produced and controlled to quality standards [89] |
Detailed Breakdown of Good Laboratory Practice (GLP)
Scope, Application, and Key Principles
GLP is a quality system covering the organizational process and conditions under which nonclinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and archived [2] [4]. Its principal goal is to promote the quality and validity of test data used for determining the safety of products regulated by the FDA and other authorities [2]. This includes pharmaceuticals, food additives, color additives, medical devices, and biocides [4].
GLP applies specifically to nonclinical laboratory studies intended to support applications for research or marketing permits. These typically include:
- Toxicology studies: Acute, subchronic, and chronic toxicity; carcinogenicity; reproductive and developmental toxicity [4].
- Safety Pharmacology studies: Assessing potential undesirable pharmacodynamic effects [4].
- Toxicokinetic (TK) and Pharmacokinetic (PK) studies: To determine the systemic exposure of the test article and its relationship to toxicity findings [4].
It is critical to note that GLP does not cover basic exploratory research or clinical trials in humans. The focus is squarely on studies that generate safety data for regulatory review [2].
Core Requirements and Organizational Structure
The structure of a GLP-compliant facility is built on several key pillars defined in 21 CFR Part 58 [2].
- Organization and Personnel: Management has the responsibility to ensure adequate resources, qualified personnel, and a defined Study Director for each study. The Study Director serves as the single point of control and ultimate responsibility for the overall conduct of the study and its final report [2] [37]. All personnel must have the education, training, and experience to perform their assigned functions.
- Quality Assurance Unit (QAU): A defining feature of GLP is the requirement for an independent QAU. This unit is separate from the personnel engaged in the direction and conduct of the study. The QAU is responsible for monitoring each study to assure management that the facilities, equipment, personnel, methods, practices, records, and controls are in conformance with GLP regulations [2] [37]. The QAU conducts audits of critical phases of studies and reviews the final study report to assure it accurately reflects the raw data.
- Facilities and Equipment: Laboratories must have adequate facility size, design, and separation to prevent mix-ups and contamination. This includes separate areas for receipt and storage of test articles, mixing of test and control articles, animal care, and specimen and data storage. Equipment must be appropriately designed, inspected, cleaned, maintained, and calibrated according to SOPs [2] [9].
- Testing Facility Operations: A fundamental requirement is the use of Standard Operating Procedures (SOPs) for all aspects of laboratory operations. SOPs provide detailed, written instructions to ensure the consistency and reproducibility of routine activities, from instrument use and animal care to data processing and record-keeping [2] [37].
- Test and Control Articles: GLP mandates the proper characterization of the test article (the substance being evaluated) and control articles. This includes establishing and documenting their identity, strength, purity, composition, and stability [2] [4]. Procedures must be in place to ensure the proper handling, storage, and mixing of these articles to avoid contamination or mix-ups.
- Protocol and Study Conduct: Every study must be conducted according to a pre-approved, detailed written protocol. The protocol defines the study's objectives and all methods for its conduct. Any changes to the protocol must be authorized as a formal amendment. The Study Director must ensure the study is conducted in full compliance with the protocol [2].
- Records and Reports: GLP places a heavy emphasis on data integrity and traceability, often summarized by the ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, and Available) [4]. All raw data, documentation, protocols, and final reports must be retained in archives for specified periods, typically for at least 5 years after the application's approval or for 2 years after the application is withdrawn [2] [90].
Detailed Breakdown of Current Good Manufacturing Practice (cGMP)
Scope, Application, and Key Principles
cGMP regulations provide for systems that assure proper design, monitoring, and control of manufacturing processes and facilities [89]. The core mission of cGMP is to ensure that every batch of a drug product—whether for clinical trials or commercial market—meets the quality standards for its intended use, possessing the required identity, strength, quality, and purity [91] [89]. The "C" in cGMP stands for "current," requiring manufacturers to employ up-to-date technologies and systems to comply with regulations [89].
cGMPs are comprehensive, governing all aspects of production, including:
- Raw materials and supplier qualification
- Manufacturing processes and process validation
- Packaging and labeling controls
- Laboratory controls and testing of in-process and finished products
- Holding and distribution [91]
Unlike GLP, which is study-based, cGMP is a continuous, ongoing system applied throughout the product's commercial lifecycle.
Core Requirements and the "Five P's"
The cGMP framework can be effectively understood through its fundamental elements, often called the "Five P's" [91].
- People: All personnel must have the education, training, and experience to perform their assigned functions. Training in cGMP and specific SOPs is mandatory, and a strong quality culture is essential. A key organizational element is the Quality Control (QC) Unit, which holds the responsibility and authority to approve or reject all components, drug products, and procedures [92] [91].
- Processes: Manufacturing processes must be well-defined, validated, and controlled to ensure consistency from batch to batch. This includes establishing a state of control and demonstrating that the process, when operated within specified parameters, will consistently yield a product meeting its pre-determined quality attributes [91].
- Procedures: Written SOPs are the bedrock of cGMP compliance. They provide step-by-step instructions for all significant operations, ensuring consistency and compliance with validated processes. Deviations from procedures must be documented and investigated [91].
- Premises: Facilities must be designed, constructed, and maintained to facilitate proper cleaning, maintenance, and operations. They must prevent contamination, mix-ups, and errors. This includes controls for air handling, water systems, and segregation of different operations [91].
- Products: All products, including raw materials and finished dosage forms, must have established specifications and testing procedures. A Certificate of Analysis (CoA) is generated for each batch, demonstrating it meets all release criteria. Products must be stored, labeled, and distributed under controlled conditions to maintain quality [91].
GLP vs. cGMP: A Detailed Comparison for the Laboratory
Side-by-Side Comparison of Key Elements
For the analytical chemist, the practical differences between working under GLP and cGMP are profound. The following table provides a detailed, technical comparison of their requirements in a laboratory context.
Table 2: Detailed Laboratory Comparison of GLP and cGMP
| Element | Good Laboratory Practice (GLP) | Current Good Manufacturing Practice (cGMP) |
|---|---|---|
| Primary Goal | Ensure integrity and reconstructability of study data [2] | Ensure batch quality, safety, and efficacy of a marketed product [89] |
| Application in Lab | Nonclinical safety and efficacy studies (e.g., TK, toxicology) [4] [93] | Quality control and release testing of raw materials, in-process, and finished products [91] [93] |
| Quality Oversight | Independent Quality Assurance Unit (QAU) auditing studies [2] | Quality Control (QC) Unit with release authority; broader Quality Assurance (QA) [92] |
| Leadership Role | Study Director has overall responsibility for a single study [2] [92] | No single "Study Director"; responsibility is shared across functions (e.g., Production, QC) [92] |
| Documentation Focus | Study-based raw data and final report for regulatory submission; proving how data was generated [2] [4] | Batch records, CoAs, and SOPs; proving consistent production to specification [91] |
| Test Article/Product | Characterization required (identity, purity, stability), but may not be fully finalized [4] | Rigorous specifications and validated methods for all materials and finished products [91] |
| Method Validation | Phase-appropriate validation for bioanalytical methods (e.g., per ICH M10) [4] | Full validation per ICH Q2(R1) for release methods; verified for compendial methods [91] |
The Analytical Chemist's Role in GLP and cGMP
The responsibilities of an analytical chemist differ significantly between the two frameworks.
Under GLP, the chemist is typically involved in two main areas [4]:
- Test Article Characterization: Developing and using methods to determine the identity, strength, purity, and stability of the test article (drug substance) and its formulations used in animal studies.
- Bioanalysis: Analyzing biological samples (blood, plasma, tissues) from test systems to determine the concentration of the drug and its metabolites for TK and PK assessments. This requires rigorous method validation per guidelines like ICH M10 and strict adherence to a pre-defined analytical plan [4].
Under cGMP, the analytical chemist's role shifts to quality control [91]:
- Performing release testing of raw materials, intermediates, and finished drug products against established specifications.
- Validating and transferring analytical methods for commercial use.
- Investigating out-of-specification (OOS) results, a critical and highly regulated activity.
- Ensuring all laboratory controls and documentation comply with cGMP to support the batch's release to the market.
Practical Implementation and Workflow
The Product Lifecycle Journey from GLP to cGMP
The following diagram illustrates how GLP and cGMP sequentially govern different stages of the drug development and manufacturing lifecycle.
Essential Research Reagents and Materials
The following table details key reagents and materials used in GLP-regulated studies, underscoring the importance of rigorous characterization and documentation.
Table 3: Key Research Reagent Solutions in GLP Studies
| Reagent/Material | Function in GLP Studies | GLP-Specific Requirements |
|---|---|---|
| Test Article | The investigational substance whose safety is being evaluated [4]. | Must be characterized for identity, purity, stability, and composition. Documentation of handling, storage, and formulation is critical [2] [4]. |
| Control Article | Provides a baseline for comparison with the test article (e.g., vehicle or placebo) [2]. | Must be appropriately characterized and documented to ensure it does not interfere with the study results [2]. |
| Dose Formulation | The mixture of the test/control article with a vehicle to facilitate administration to the test system [4]. | Must be analyzed for concentration, homogeneity, and stability over the duration of its use to ensure accurate dosing [4]. |
| Reference Standards | Qualified standards used to calibrate equipment and validate analytical methods [4]. | Must be traceable, properly stored, and characterized. Their use and preparation must be documented per SOPs [9]. |
| Biological Matrices | Samples derived from test systems (e.g., plasma, serum, tissue) for bioanalysis [4]. | Chain of custody, storage conditions, and stability in the matrix must be meticulously documented and maintained [4]. |
For the analytical chemist engaged in drug development, a clear and operational understanding of both GLP and cGMP is indispensable. While both are quality systems enforcing rigorous documentation and control, their purposes, applications, and specific requirements are distinct. GLP is the framework for generating trustworthy nonclinical safety data, focusing on the reconstructability and integrity of entire studies. cGMP is the framework for ensuring consistent product quality, focusing on controlling every aspect of the manufacturing process. Navigating the transition of a compound from the GLP-regulated preclinical environment to the cGMP-regulated clinical and commercial environment is a critical step in the journey of bringing safe and effective medicines to patients. Mastery of these distinct "good practices" empowers scientists to not only maintain compliance but also to uphold the highest standards of scientific rigor and product quality.
Good Laboratory Practice (GLP) is a quality system covering the organizational process and conditions under which non-clinical health and environmental safety studies are planned, performed, monitored, recorded, reported, and archived [2]. Established by the FDA in 1978 and adopted globally through OECD principles, GLP provides a framework for ensuring the quality, integrity, and traceability of data produced in non-clinical research laboratories [2] [94]. Unlike Good Manufacturing Practice (GMP) which governs production, GLP specifically applies to preclinical laboratory studies that support applications for research or marketing permits for FDA- and EPA-regulated products, including pharmaceuticals, pesticides, and industrial chemicals [2] [12] [95].
The Quality Assurance Unit (QAU) serves as the independent oversight body within this framework, functioning as the guardian of data integrity and compliance. The QAU's fundamental purpose is to provide assurance to test facility management and regulatory authorities that studies are conducted in accordance with GLP principles [95]. This independent unit performs regular inspections and audits to verify that facilities, equipment, personnel, methods, practices, records, and controls comply with the rigorous standards required for regulatory acceptance [2] [95]. By maintaining this objective oversight, the QAU ensures that safety study data are reliable, reproducible, and auditable, thereby protecting public health through trustworthy safety evidence [2].
Foundational GLP Principles and Regulatory Framework
Core Components of GLP Compliance
The GLP framework rests on several interconnected pillars that collectively ensure study quality and integrity. These components create a comprehensive system of checks and balances throughout the research lifecycle.
Table 1: Key Components of Good Laboratory Practice (GLP)
| Component | Description | Regulatory Reference |
|---|---|---|
| Organization & Personnel | Defined test facility management, qualified personnel, Study Director with overall responsibility for each study | 21 CFR 58.29-35 [2] |
| Quality Assurance Unit (QAU) | Independent unit responsible for monitoring GLP compliance through audits of SOPs, raw data, protocols, and reports | 21 CFR 58.35 [2] [95] |
| Facilities | Adequate laboratory facilities with separated areas for animal housing, test operations, and specimen storage to prevent cross-contamination | 21 CFR 58.41-51 [2] |
| Equipment | Appropriately designed equipment that is properly maintained and calibrated according to SOPs | 21 CFR 58.61-63 [2] |
| Testing Facility Operations | Written Standard Operating Procedures (SOPs) for all laboratory operations | 21 CFR 58.81-90 [2] |
| Test & Control Articles | Proper characterization, handling, and storage of test and control articles to ensure identity, strength, and purity | 21 CFR 58.105-113 [2] |
| Protocol & Conduct | Written study protocol approved before study initiation with documented amendments | 21 CFR 58.120-130 [2] |
| Records & Reports | Final study reports with complete raw data documentation; proper archiving for reconstruction | 21 CFR 58.185-195 [2] |
The Study Director and QAU Partnership
A critical relationship in the GLP framework exists between the Study Director and the QAU. The Study Director serves as the single point of control with ultimate responsibility for the technical conduct of the study, interpretation and analysis of data, and reporting of results [95]. Meanwhile, the QAU operates independently to verify that the study complies with GLP principles without assuming direct responsibility for the study's scientific conduct [95]. This partnership creates an effective system of checks and balances where scientific oversight and quality oversight work in tandem to ensure both scientific validity and regulatory compliance.
The QAU maintains written records of each inspection and provides periodic status reports to both management and the Study Director [95]. This regular communication ensures that any compliance issues identified during audits are promptly addressed by the responsible parties. The QAU also reviews the final study report to verify that it accurately reflects the raw data and methods described in the protocol [95]. This collaborative yet independent relationship forms the backbone of effective quality assurance in GLP environments.
The Audit Trail: Concept and Implementation
Defining the Audit Trail in GLP Context
Within GLP frameworks, an audit trail comprises a secure, computer-generated, and time-stamped record that allows for the reconstruction of the course of events relating to the creation, modification, or deletion of an electronic record [2]. It provides a chronological sequence of documentation that enables independent verification of who did what, when, and why throughout the research process. The audit trail serves as the evidentiary backbone of a GLP-compliant study, creating a transparent path from raw data generation through final analysis and reporting.
The fundamental purpose of the audit trail is to ensure data integrity and reconstructability. According to GLP principles, storage and archiving of all records and reports must be done in a manner that minimizes deterioration and allows for orderly storage and expedient retrieval [95]. A properly maintained audit trail enables regulatory agencies to trace the complete history of a study, verifying that all activities were performed according to the approved protocol and standard operating procedures. This comprehensive documentation is essential for regulatory acceptance, as it demonstrates that the study data is trustworthy and has not been improperly altered or influenced.
Essential Elements of a Compliant Audit Trail
Effective audit trails in GLP environments share several critical characteristics that ensure their utility for reconstruction and verification:
- Completeness: The audit trail must document all critical data and procedural steps, including instrument-generated data, manual observations, calculations, and any modifications to existing records [2].
- Chronological Integrity: Each entry must include a secure timestamp that cannot be altered, establishing an unambiguous sequence of events [2].
- Attributability: Every action must be clearly linked to the individual who performed it, typically through secure electronic signatures or manual initials [2].
- Accuracy: The documented information must precisely reflect what occurred during the study conduct without ambiguity [2].
- Persistence: Audit trails must be maintained throughout the study lifecycle and retained according to regulatory requirements, typically for many years after study completion [95].
These elements collectively ensure that the audit trail fulfills its fundamental purpose of providing a verifiable, step-by-step account of the entire research process that can be independently reconstructed if necessary.
Preparing for QAU Inspections and Regulatory Audits
Pre-Audit Preparation Protocol
Systematic preparation is essential for successful QAU inspections and regulatory audits. The following methodology outlines a comprehensive approach to audit readiness that should be implemented continuously throughout the study lifecycle.
Table 2: Audit Preparation Timeline and Activities
| Timeline | Preparation Activity | Responsible Personnel |
|---|---|---|
| Ongoing | Maintain complete and organized raw data, equipment records, and training documentation | All Study Personnel |
| 90 Days Pre-Audit | Conduct internal quality check of critical study components; review SOP compliance | Study Director, QAU |
| 60 Days Pre-Audit | Perform mock audit focusing on high-risk areas identified in previous inspections | QAU, Study Director |
| 30 Days Pre-Audit | Complete comprehensive document review; verify all protocol amendments properly documented | Study Director |
| 2 Weeks Pre-Audit | Resolve all outstanding deficiencies identified during mock audits | Study Personnel |
| 1 Week Pre-Audit | Prepare presentation of study overview; organize documentation for efficient retrieval | Study Director |
The preparatory phase should include a thorough review of Standard Operating Procedure (SOP) compliance across all study activities. SOPs provide clear instructions for laboratory operations, ensuring consistency and reliability in data collection and reporting [94]. Each SOP should detail procedures for equipment usage, sample handling, data recording, and safety measures, which helps minimize errors and variability in results [94]. Verification that all personnel have completed required training on relevant SOPs is a critical preparatory step that is frequently scrutinized during regulatory inspections.
Common Compliance Deficiencies and Remediation Strategies
Understanding frequent areas of non-compliance enables proactive remediation before formal audits. Common GLP deficiencies include:
- Incomplete Documentation: Missing raw data, unsigned or undated entries, and incomplete calibration records represent frequent findings. Remediation requires implementing systematic document control processes and regular reviews by supervisory staff [94].
- Inadequate SOP Development and Training: SOPs that are outdated, insufficiently detailed, or not properly followed by personnel. Regular SOP reviews and comprehensive training programs address this deficiency [94].
- Poor Audit Trail Management: Incomplete reconstruction documentation, inadequate change control records, and insufficient description of reasons for modifications. Electronic systems with automated audit trails can mitigate these issues [2].
- Equipment Calibration Deficiencies: Lack of documented calibration, use of expired standards, or inadequate maintenance records. Implementing a robust metrology program with scheduled calibrations and strict documentation requirements addresses this concern [2] [96].
- Sample Management Issues: Inadequate characterization, improper storage conditions, or incomplete chain-of-custody documentation for test articles. Clear protocols for receipt, storage, and usage of all materials are essential [2].
Proactive identification and remediation of these common deficiencies significantly enhances audit readiness and demonstrates a commitment to quality that regulatory inspectors recognize and appreciate.
The Inspection Process: Protocols and Procedures
QAU Inspection Workflow
The QAU inspection process follows a systematic workflow designed to comprehensively evaluate GLP compliance across all study components. The diagram below illustrates this inspection workflow, highlighting key decision points and documentation requirements.
Regulatory Agency Inspection Protocols
Regulatory inspections conducted by agencies such as the FDA and EPA follow established protocols to verify GLP compliance. The EPA's Good Laboratory Practice Standards (GLPS) compliance monitoring program, for example, ensures the quality and integrity of test data submitted to the Agency in support of pesticide product registration under FIFRA and TSCA [12]. EPA inspectors conduct examinations to "monitor compliance with the regulations" and to assure that studies "were done with integrity, are of good quality and valid" [12].
During regulatory inspections, auditors typically focus on several key areas:
- Study-Based Audit: Comprehensive review of a single study from protocol development through final reporting, examining raw data, personnel records, equipment logs, and QAU reports.
- Facility-Based Audit: Evaluation of overall facility compliance, including organization, personnel training, equipment maintenance, SOP management, and QAU operation.
- Process-Based Audit: Focus on specific laboratory processes or techniques across multiple studies to verify consistency and compliance.
Inspectors collect physical samples and documentary evidence during these evaluations, with particular attention to data authenticity and traceability [12]. The inspection process is designed not merely as a compliance exercise, but as a means to verify that the fundamental principles of data quality and integrity have been maintained throughout the research process.
Post-Inspection Actions and Continuous Improvement
Responding to Inspection Findings
The period immediately following an inspection is critical for addressing identified deficiencies and implementing sustainable improvements. Upon receipt of the final inspection report, the testing facility should implement a structured response protocol:
- Formal Response Development: Prepare a comprehensive written response to each observation within the designated timeframe (typically 30 days). Each response should acknowledge the finding, identify the root cause, and describe specific corrective actions.
- Corrective and Preventive Action (CAPA) Implementation: Execute the proposed corrective actions, ensuring they adequately address both the specific deficiency and any underlying systemic issues. Documentation of all corrective actions is essential for verification.
- Effectiveness Verification: The QAU should verify the effectiveness of implemented corrections through follow-up audits, ensuring that the deficiencies have been genuinely remediated and are unlikely to recur.
This structured approach demonstrates to regulatory authorities a genuine commitment to compliance and continuous quality improvement. A prompt, thorough, and well-documented response to inspection findings can significantly influence regulatory perceptions and outcomes.
Continuous Quality Improvement Methodology
Beyond addressing specific audit findings, successful GLP facilities implement ongoing quality improvement processes. This proactive approach includes:
- Trend Analysis: Regular review of audit findings, deviations, and non-conformances to identify recurring issues or systemic weaknesses.
- SOP Optimization: Continuous refinement of Standard Operating Procedures based on technological advancements, regulatory updates, and practical experience [94].
- Training Enhancement: Evolving training programs to address identified knowledge gaps and incorporate lessons learned from audits and inspections.
- Metric Monitoring: Establishing and tracking quality metrics related to data integrity, protocol compliance, and audit outcomes to measure improvement over time.
Measurement assurance is essential in ensuring that laboratory results are both valid and reliable, forming a critical component of continuous improvement efforts [94]. This involves using several strategies, including the establishment of reference materials, quality control procedures, and equipment calibration to ensure data generated during studies is traceable and adheres to recognized standards [94].
Essential Research Reagents and Solutions for GLP Compliance
Proper management of research reagents and solutions is fundamental to GLP compliance and data integrity. The following table outlines critical materials and their quality assurance requirements in GLP environments.
Table 3: Essential Research Reagent Solutions and Quality Assurance Requirements
| Reagent/Solution | GLP Function | Quality Assurance Requirements |
|---|---|---|
| Test and Control Articles | Substances being evaluated for safety and efficacy | Characterization of identity, purity, strength, stability; proper receipt, storage, and labeling [2] |
| Reference Standards | Calibration and verification of analytical methods | Certified purity and traceability; proper storage conditions; documentation of preparation and usage |
| Biologically Active Reagents | Cell-based assays, enzyme reactions, immunoassays | Documentation of source, lot number, and expiration; verification of activity; proper storage conditions [96] |
| Calibration Solutions | Equipment performance verification | Traceability to reference standards; documentation of preparation; stability assessments [96] |
| Mobile Phases and Buffers | Chromatographic separations and analytical procedures | Documented preparation following SOPs; verification of pH and composition; established stability periods [94] |
| Cleaning and Decontamination Solutions | Equipment maintenance and contamination prevention | Standardized concentrations; documented preparation; verification of efficacy [96] |
Reagents must be correctly labeled with information about their shelf life, the date they were opened, standard safety information, and hazard symbols [96]. Any testing items that have exceeded their shelf life must be disposed of, unless the shelf life has been formally extended based on documented analytical testing [96]. This extension requires exact documentation and can only be mandated by the testing manager, demonstrating the strict controls governing reagent use in GLP environments.
Successful navigation of QAU inspections and regulatory audits requires meticulous preparation, comprehensive understanding of GLP principles, and unwavering commitment to data integrity throughout the research lifecycle. The audit trail serves as the foundational element that enables study reconstruction and verification, making its proper maintenance a critical success factor. By implementing robust quality systems, maintaining complete and accurate documentation, and fostering a culture of quality, research facilities can not only pass regulatory scrutiny but also generate data of the highest integrity and reliability. The practices outlined in this technical guide provide a roadmap for analytical chemists and drug development professionals to achieve excellence in GLP compliance, ultimately contributing to the advancement of public health through trustworthy scientific research.
Conclusion
For analytical chemists, adherence to Good Laboratory Practice is not merely a regulatory hurdle but a fundamental component of generating reliable, high-quality data that forms the bedrock of drug safety assessment. Mastering the foundational principles, applying robust methodological techniques, proactively troubleshooting analytical challenges, and rigorously validating methods are all critical for regulatory success. As the field evolves with increasingly complex therapeutics like peptides and biologics, the role of the chemist will continue to expand, demanding a deeper integration of advanced analytical strategies with core GLP quality systems. The future of GLP will likely involve greater data standardization to combat laboratory heterogeneity and a continued emphasis on sound science underpinned by unassailable data integrity, ultimately ensuring that safe and effective medicines reach patients.
References
- 1. A Guide to Good Laboratory Practice (GLP) [https://safetyculture.com/topics/good-laboratory-practice-glp]
- 2. 21 CFR Part 58: A Guide to Good Laboratory Practice (GLP) [https://intuitionlabs.ai/articles/21-cfr-part-58-glp-guide]
- 3. What is GLP & Why Is Good Laboratory Practice Important? [https://www.allucent.com/resources/blog/what-are-good-laboratory-practices-glp-nonclinical-studies]
- 4. Good Laboratory Practice (GLP): An Overview for the ... [https://www.chromatographyonline.com/view/good-laboratory-practice-glp-an-overview-for-the-analytical-chemist]
- 5. The History of Good Laboratory Practices (GLP) [https://gxp-storage.com/history-of-glp/]
- 6. Nonclinical Laboratories Inspected under Good ... [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-references/nonclinical-laboratories-inspected-under-good-laboratory-practices]
- 7. Regulatory requirements for GLP labs [https://www.pharmko.com/blog/regulatory-requirements-for-glp-labs]
- 8. 10 Examples of Good Laboratory Practice (GLP) [https://www.materials.zone/blog/examples-of-good-laboratory-practice-glp]
- 9. Good laboratory practice - FDA GLP regulations for ... [https://www.gmpsop.com/good-laboratory-practice-glp-regulations-by-fda/]
- 10. Good Laboratory Practice and Compliance Monitoring [https://www.oecd.org/en/topics/sub-issues/testing-of-chemicals/good-laboratory-practice-and-compliance-monitoring.html]
- 11. 21 CFR Part 58 -- Good Laboratory Practice for Nonclinical ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-58?toc=1]
- 12. Good Laboratory Practices Standards Compliance ... [https://www.epa.gov/compliance/good-laboratory-practices-standards-compliance-monitoring-program]
- 13. Bioanalysis of GLP-1 Antagonist Drugs [https://labtesting.wuxiapptec.com/2025/01/02/bioanalysis-of-glp-1-antagonist-drugs-by-multiple-analytical-platforms/]
- 14. HPLC 2025 Preview: The Present and Future of ... [https://www.chromatographyonline.com/view/hplc-2025-preview-the-present-and-future-of-automation-in-analytical-laboratories]
- 15. Good Laboratory Practice: An Overview for the Analytical ... [https://www.chromatographyonline.com/view/good-laboratory-practice-overview-analytical-chemist]
- 16. Good Laboratory Practices (GLPs) – Quality Assurance [https://research.uga.edu/quality-assurance/glps/]
- 17. What are 5 fundamental points of GLP? [https://www.generi-biotech.com/faq/what-are-5-fundamental-points-of-glp/]
- 18. Organization & Personnel [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/fda-bioresearch-monitoring-information/organization-personnel]
- 19. ROLE AND RESPONSIBILITIES OF DIFFERENT ... [https://www.slideshare.net/slideshow/role-and-responsibilities-of-different-personnel-of-glp-studies-pptx-0b67/269831176]
- 20. 21 CFR 58.33 -- Study director. [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-58/subpart-B/section-58.33]
- 21. Good Laboratory Practice - Quality Assurance - RQA [https://qa.therqa.com/goodlaboratorypractice.html]
- 22. ALCOA, ALCOA+ and ALCOA++ Principles | Ensuring Data ... [https://www.pharmaguideline.com/2018/12/alcoa-to-alcoa-plus-for-data-integrity.html]
- 23. Data Quality and Integrity [https://www.utmb.edu/orncs/regulatory-ops/data-quality-and-integrity]
- 24. Why ALCOA Principles Matter for Data Integrity in Life ... [https://www.cognidox.com/blog/data-integrity-alcoa-principles]
- 25. Alcoa Validation Data | NNIT [https://www.nnit.com/insights/articles/alcoa-validation-data]
- 26. ALCOA+ - what does it mean? [https://www.gmp-compliance.org/gmp-news/alcoa-what-does-it-mean]
- 27. ALCOA Principles: A Guide to Data Integrity for Life Sciences… [https://tulip.co/blog/alcoa-principles-a-guide-to-data-integrity/]
- 28. The ALCOA++ Principles for Data Integrity in Clinical Trials [https://www.quanticate.com/blog/alcoa-principles]
- 29. What are the ALCOA Principles in Life Sciences ... [https://www.scilife.io/glossary/alcoa]
- 30. Good Documentation Practice in the GLP [https://www.biopharmaservices.com/blog/phase-1-understanding-good-documentation-practice-gdp-and-its-role-in-good-laboratory-practice-glp/]
- 31. Good Documentation Practices (GDocP) | GMP Basics [https://www.pharmout.net/good-documentation-practices-gdocp-gmp/]
- 32. 21 CFR Part 58 -- Good Laboratory Practice for Nonclinical ... [https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-58]
- 33. GLP Characterization Studies [https://www.eag.com/app-note/glp-characterization-studies/]
- 34. Comparing GLP regulatory standards [https://www.pharmko.com/blog/comparing-glp-regulatory-standards]
- 35. Guidelines for the Testing of Chemicals [https://www.oecd.org/en/topics/sub-issues/testing-of-chemicals/test-guidelines.html]
- 36. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 37. Lab requirements for GLP compliance [https://www.pharmko.com/blog/lab-requirements-for-glp-compliance]
- 38. Immunogenicity of Antibody Drug Conjugates [https://pmc.ncbi.nlm.nih.gov/articles/PMC4287284/]
- 39. 8 Essential Characteristics of LC-MS/MS Method Validation [https://www.resolian.com/bioanalytics/8-essential-characteristics-of-lc-ms-ms-method-validation/]
- 40. Immunocapture LC–MS Methods for Pharmacokinetics of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11845110/]
- 41. ICH M10 Bioanalytical Method Validation Guideline-1 year ... [https://link.springer.com/article/10.1208/s12248-024-00974-y]
- 42. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 43. ELISA Sensitivity and Specificity [https://www.mybiosource.com/learn/elisa-sensitivity-and-specificity/]
- 44. Immunogenicity Assay [https://www.bioagilytix.com/solutions/bioanalytical-laboratory-services/immunogenicity-assay/]
- 45. Innovations in Liquid Chromatography: 2025 HPLC ... [https://www.chromatographyonline.com/view/innovations-in-liquid-chromatography-2025-hplc-column-and-accessories-review]
- 46. Rapid screening of 70 colorants in dyeable foods by using ... [https://www.sciencedirect.com/science/article/abs/pii/S030881462100649X]
- 47. Eight key rules for successful data‐dependent acquisition in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10078780/]
- 48. Understanding Good Laboratory Practice (GLP) Guidelines [https://www.cfpie.com/understanding-good-laboratory-practice-glp-guidelines]
- 49. What Makes a Good Laboratory Standard Operating ... [https://www.msesupplies.com/blogs/news/what-makes-a-good-laboratory-standard-operating-procedure-sop?srsltid=AfmBOoqZ-iJBaerjypWV1xlcOm5is_LsRj9tn_DBq7Q-WxibD_AMCWzY]
- 50. FDA guidelines for GLP products [https://www.pharmko.com/blog/fda-guidelines-for-glp-products]
- 51. Standard Operating Protocols (SOPs) - WebGURU [https://webguru.sites.northeastern.edu/standard-operating-protocols-sops-2/]
- 52. GLP Certification and Compliance Guide for Biotech Labs ... [https://www.scispot.com/blog/glp-certification-and-compliance-guide-for-biotech-lab]
- 53. HPLC 2025 Update: The Rise of GLP-1 Therapeutics [https://www.chromatographyonline.com/view/the-rise-of-glp-1-therapeutics]
- 54. An analysis on the role of glucagon-like peptide-1 receptor ... [https://www.nature.com/articles/s44220-025-00390-x]
- 55. Analytical Challenges and Emerging Strategies for GLP-1 ... [https://www.chromatographyonline.com/view/analytical-challenges-and-emerging-strategies-for-glp-1-analysis]
- 56. Development of a sensitive LC-MS/MS assay to support ... [https://pubmed.ncbi.nlm.nih.gov/39088035/]
- 57. DETECTING LOW-LEVEL SYNTHESIS IMPURITIES IN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3146765/]
- 58. Advanced applications of two-dimensional liquid ... [https://www.sciencedirect.com/science/article/abs/pii/S0021967325000111]
- 59. Two-Dimensional High-Performance Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10343842/]
- 60. On-Line Two-Dimensional Liquid Chromatography (2D-LC ... [https://www.chromatographyonline.com/view/line-two-dimensional-liquid-chromatography-2d-lc-analysis-pharmaceuticals]
- 61. Dealing with Wandering First-Dimension Peaks in 2D-LC ... [https://www.chromatographyonline.com/view/dealing-with-wandering-first-dimension-peaks-in-2d-lc-separations]
- 62. Simultaneous analysis of highly polar and multi-residue ... [https://pubmed.ncbi.nlm.nih.gov/37454518/]
- 63. 2D-LC–MS for the Analysis of Monoclonal Antibodies and ... [https://www.quality-assistance.com/news/2d-lc-ms-analysis-monoclonal-antibodies-and-antibody-drug-conjugates-regulated-environment]
- 64. Data Silos, Why They're a Problem, & How to Fix It [https://www.talend.com/resources/what-are-data-silos/]
- 65. Data Integration from Heterogeneous Control Levels for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9786177/]
- 66. Laboratory Information Management Systems (LIMS) [https://www.thermofisher.com/us/en/home/digital-solutions/lab-informatics/lab-information-management-systems-lims.html]
- 67. Laboratory Information Management Systems (LIMS) [https://www.illumina.com/informatics/infrastructure-pipeline-setup/lims.html]
- 68. The importance of using the optimal plastic and glassware in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3290000/]
- 69. Advanced Analytical Challenges of GLP-1 Receptor Agonists [https://www.sepscience.com/the-peptide-complexity-problem-advanced-analytical-challenges-of-glp-1-receptor-agonists-12172]
- 70. The Importance of Sample Preparation in Quantitative ... [https://www.chromatographyonline.com/view/the-importance-of-sample-preparation-in-quantitative-bioanalytical-liquid-chromatography-mass-spectrometry]
- 71. Method Validation and Robustness [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 72. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 73. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 74. Method Robustness and Reproducibility for Monoclonal ... [https://www.chromatographyonline.com/view/method-robustness-and-reproducibility-for-monoclonal-antibody-purity-analysis]
- 75. Strategy for ruggedness tests in chromatographic method ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267099001130]
- 76. Best Practices For Successful Method Validation [https://lgmpharma.com/blog/best-practices-for-successful-method-validation/]
- 77. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 78. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 79. Introduction to Analytical Method Validation [https://lab-training.com/introduction-to-analytical-method-validation/]
- 80. Analytical Method Validation: A Recipe for Accurate Results [https://certified-laboratories.com/blog/analytical-method-validation-a-recipe-for-accurate-results/]
- 81. Analytical Method Validation in Pharmaceutical Quality ... [https://ndgcs.com/analytical-method-validation-in-pharmaceutical-quality-assurance/]
- 82. Key Parameters for Analytical Method Validation [https://altabrisagroup.com/analytical-method-validation-parameters/]
- 83. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 84. What are the differences and key steps in Analytical ... [https://resources.eirgenix.com/blog/method_dev_qual_validation]
- 85. Understanding the Four Types of Analytical Method ... [https://www.oxford-analytical.co.uk/understanding-the-four-types-of-analytical-method-validation/]
- 86. FDA Requirements for Generic GLP-1 Peptide Injections [https://eliquent.com/resource/fda-requirements-for-the-approval-of-glp-1-generic-peptide-injections/]
- 87. FDA IND CMC Requirements for Biologics: A 2025 ... [https://scxcmc.com/fda-ind-cmc-requirements-for-biologics/]
- 88. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 89. Facts About the Current Good Manufacturing Practice ... [https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp]
- 90. Good Laboratory Practices vs. Good Manufacturing Practices [https://www.eurofinsus.com/food-testing/resources/good-laboratory-practices-vs-good-manufacturing-practices-whats-the-difference/]
- 91. Current Good Manufacturing Practice (cGMP): An Overview ... [https://www.chromatographyonline.com/view/current-good-manufacturing-practice-cgmp-an-overview-for-the-analytical-chemist]
- 92. GLP and GMP: Understanding the differences [https://www.linkedin.com/pulse/glp-gmp-understanding-differences-amila-j-halahakoon-eajvf]
- 93. GMP vs. GLP in Laboratory Testing & Validation [https://www.thefdagroup.com/blog/gmp-vs.-glp-in-lab-testing-validation]
- 94. Quality assurance for GLP supplies [https://www.pharmko.com/blog/quality-assurance-for-glp-supplies]
- 95. Good Laboratory Practices (GLPs) - UF Research [https://research.ufl.edu/compliance/good-laboratory-practices.html]
- 96. "Good Laboratory Practice" (GLP): Your checklist - Binder World [https://www.binder-world.com/int-en/insights/glp-checklist-co2-incubator]