Optimizing Nebulizer Gas Flow Rates for Enhanced Pharmaceutical Aerosol Delivery: A Comprehensive Guide for Researchers
This article provides a systematic review of the critical role of nebulizing gas flow rate in the efficacy of pharmaceutical aerosol delivery.
Optimizing Nebulizer Gas Flow Rates for Enhanced Pharmaceutical Aerosol Delivery: A Comprehensive Guide for Researchers
Abstract
This article provides a systematic review of the critical role of nebulizing gas flow rate in the efficacy of pharmaceutical aerosol delivery. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles governing flow rate's impact on aerosol characteristics, including droplet size distribution and respirable dose. The content delves into methodological approaches for application across different patient interfaces and ventilation systems, addresses key challenges and optimization strategies through advanced component design and synchronization techniques, and evaluates validation methods and comparative performance of nebulizer technologies. By synthesizing current research and in vitro findings, this resource offers a scientific framework for optimizing flow parameters to maximize lung deposition and therapeutic outcomes in both invasive and non-invasive ventilation scenarios.
The Science of Flow Rate: How Gas Flow Governs Aerosol Generation and Characteristics
Fundamental Principles of Nebulizer Gas Flow and Aerosolization
Nebulizer gas flow is the fundamental force driving the conversion of liquid pharmaceutical solutions into inhalable aerosols. Medical air-compression nebulizers, the most widely used type, operate on Bernoulli's theorem and the Venturi effect [1] [2]. As compressed gas passes through a progressively narrowing nozzle, its velocity increases dramatically, creating a negative pressure zone that draws aqueous medicine into the airflow, atomizing it into fine droplets [1]. This process of primary atomization is followed by secondary atomization where finer droplets are selected through baffle systems that intercept larger droplets, allowing them to return to the nebulization chamber for recirculation while smaller particles are made available for patient inhalation [1].
The efficiency of this aerosolization process directly determines therapeutic outcomes by influencing where drugs deposit within the respiratory tract. Understanding and optimizing gas flow parameters enables researchers and clinicians to target specific pulmonary regions, from the upper airways to the deep alveolar space, maximizing local drug concentration while minimizing systemic side effects [3].
Core Principles of Aerosolization
Physics of Gas-Driven Aerosol Generation
The aerosolization process in jet nebulizers involves complex fluid dynamics where gas flow characteristics determine the initial liquid breakup. When high-pressure gas passes through the nozzle, the dramatic velocity increase creates shear forces that tear the liquid solution into filaments and eventually droplets [1]. The kinetic energy transferred from the gas to the liquid must overcome both the liquid's surface tension and viscous forces to achieve successful atomization.
The size distribution of generated aerosols follows predictable patterns based on the energy input from the gas flow. Higher gas velocities generally produce smaller droplets, though this relationship is moderated by other factors including liquid properties and nebulizer chamber geometry. The median droplet size represents a dynamic equilibrium between primary atomization at the nozzle and secondary selection processes at the baffles [1].
Aerosol Deposition Mechanisms in the Respiratory Tract
Once generated, aerosol particles deposit in different respiratory regions based on their size and the patient's breathing pattern:
- Inertial Impaction: Predominates in the first 10 airway generations where high velocity and turbulence cause larger particles (>5-10 μm) to impact airway surfaces, making this mechanism ideal for targeting upper airways and large bronchi [3].
- Gravitational Sedimentation: Becomes significant in smaller airways (generations 5-16) where air velocity decreases, allowing medium-sized particles (1-5 μm) to settle by gravity, suitable for bronchiolar targeting [3].
- Diffusion (Brownian Motion): Dominates at the alveolar level where minimal air velocity exists, enabling submicron particles to deposit through random molecular motion, essential for alveolar delivery [3].
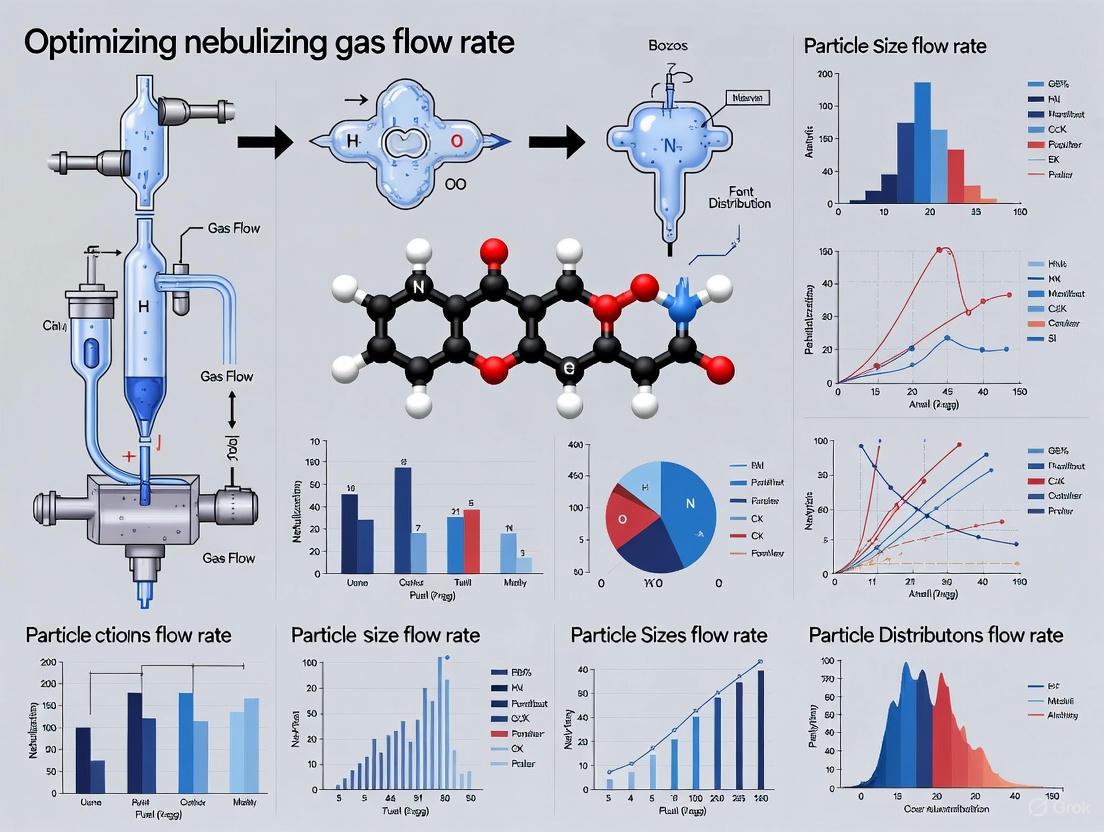
The following diagram illustrates the fundamental workflow of nebulizer gas flow and aerosol deposition:
Diagram 1: Nebulizer gas flow and aerosol deposition workflow.
Critical Factors Influencing Aerosolization Efficiency
Gas Flow Parameters
The supply gas pressure and resulting flow characteristics are primary determinants of nebulizer performance:
- Supply Gas Pressure: Directly influences critical output metrics. Increasing from 50 to 150 kPa can reduce Dv90 (diameter below which 90% of droplets fall) by up to 29.5% in nebulizers with 0.8 mm orifice diameters, creating finer aerosols [2].
- Gas Flow Rate: Varies with pressure and nozzle design. Studies document flow rates from 2.48 to 16.02 L/min for supply gas and 14.28 to 41.38 L/min for jet gas across different operational parameters [2].
- Nozzle Orifice Diameter: Affects the fundamental fluid dynamics. Smaller orifices (0.4 mm) produce higher velocity jets at the same pressure but may exhibit anomalous droplet size increases at higher pressures, while larger orifices (0.6-0.8 mm) demonstrate more consistent refinement of droplet size with increasing pressure [2].
Nebulizer Design Elements
The physical design of nebulizer components significantly moderates gas flow effects:
- Baffle Design: Strategic placement and geometry dramatically affect droplet size distribution. Studies show rounded, conical, flat, and concave baffle shapes effectively reduce sizes of atomized droplets, with mass medium aerodynamic diameter (MMAD) approximately 1.5 times higher in nebulizers without baffles [1].
- Cavity Dimensions: The resonant cavity (Hartmann whistle) between nozzle and baffle, characterized by width (W), depth (D), and insertion distance (S), influences particle size distribution through standing wave patterns and secondary atomization effects [1].
- Liquid Flow Path: Diameter of the liquid feed channel affects liquid flow rate, which combines with gas-liquid pressure differential to determine the final aerosol output concentration [1].
Formulation Characteristics
The physical and chemical properties of the nebulized solution interact with gas flow parameters:
- Solution Osmolarity: Significantly affects droplet size distribution at the nebulizer outlet. Various diluents (0.9% NaCl, 0.45% NaCl, deionized water) produce measurably different MMAD values, with hypertonic saline (3%) demonstrating improved clinical outcomes in some applications [1].
- Surface Tension and Viscosity: Higher values generally increase droplet size by resisting atomization, requiring optimization of gas flow parameters to achieve target aerosol distributions [1] [2].
Quantitative Data on Gas Flow Effects
Gas Pressure and Flow Rate Relationships
Table 1: Effect of supply gas pressure on nebulizer performance parameters [2].
| Supply Gas Pressure (kPa) | Supply Gas Flow Rate (L/min) | Jet Gas Flow Rate (L/min) | Atomizing Rate (mL/min) | Dv90 (μm) |
|---|---|---|---|---|
| 50 | 2.48 - 4.15 | 14.28 - 18.45 | 0.12 - 0.21 | 7.09 - 9.87 |
| 100 | 5.82 - 9.64 | 22.56 - 28.94 | 0.24 - 0.39 | 6.45 - 8.91 |
| 150 | 9.33 - 16.02 | 31.85 - 41.38 | 0.38 - 0.62 | 5.67 - 8.47 |
Nozzle Design Impact on Output
Table 2: Performance characteristics across different nozzle orifice diameters at 100 kPa [2].
| Nozzle Orifice Diameter (mm) | Gas Flow Rate (L/min) | Dv90 (μm) | Effective Output Dose (mg/L) | *Spray Concentration (Light Blocking %) * |
|---|---|---|---|---|
| 0.4 | 5.82 | 8.91 | 12.4 - 15.8 | 28.5 - 36.1 |
| 0.6 | 7.73 | 7.26 | 13.1 - 16.2 | 32.8 - 40.5 |
| 0.8 | 9.64 | 6.45 | 12.9 - 16.5 | 35.2 - 44.9 |
Respiratory Deposition by Particle Size
Table 3: Relationship between aerosol particle size and respiratory deposition patterns [1] [3].
| Particle Size (μm) | Primary Deposition Region | Deposition Mechanism | Therapeutic Applications |
|---|---|---|---|
| >10 | Upper Respiratory Tract (Nasopharyngeal) | Inertial Impaction | Upper Airway Conditions |
| 5-10 | Lower Respiratory Tract (Bronchial) | Inertial Impaction & Sedimentation | Asthma, COPD, Bronchitis |
| 1-5 | Alveolar Region | Gravitational Sedimentation | Pneumonia, Systemic Delivery |
| <1 | Alveolar Region | Diffusion (Brownian Motion) | Severe Pneumonia, Pulmonary Infections |
Experimental Protocols for Gas Flow Optimization
Protocol: Characterizing Droplet Size Distribution
Objective: To measure the droplet size distribution of a nebulizer under controlled gas flow parameters.
Materials:
- Laser Particle Size Analyzer (LPSA)
- Calibrated air compressor (0-150 kPa range)
- Precision gas flow meter (e.g., SIARGO-MF5700)
- Electronic balance (0.1 mg resolution, e.g., LICHEN-FA324TC)
- Test nebulizer unit
- Controlled environment chamber (20±2°C, 50±5% RH)
Methodology:
- Connect the nebulizer to the air compressor through the gas flow meter.
- Fill the nebulizer with 5 mL of standardized test solution (0.9% saline or formulation mimic).
- Set the supply gas pressure to the initial test condition (e.g., 50 kPa).
- Allow the system to stabilize for 30 seconds after initiation.
- Position the LPSA sampling inlet 10 cm from the nebulizer mouthpiece at a 45° angle.
- Record droplet size distribution (Dv10, Dv50, Dv90) over a 60-second sampling period.
- Simultaneously record gas flow rate and collect output for atomizing rate determination.
- Repeat measurements across pressure range (50, 100, 150 kPa) with fresh solution.
- Perform triplicate measurements for each condition.
Data Analysis:
- Calculate MMAD (Mass Median Aerodynamic Diameter) and GSD (Geometric Standard Deviation)
- Determine fine particle fraction (FPF) as percentage of particles <5μm
- Plot relationship between gas pressure and key size parameters
- Calculate emitted dose (ED) and effective output dose (EOD)
Protocol: Evaluating Baffle Design Modifications
Objective: To quantify the impact of baffle geometry on aerosol output under standardized gas flow conditions.
Materials:
- 3D printing system (SLA recommended for precision)
- CAD models of baffle variants (varying W, D, S dimensions)
- Cascade impactor (e.g., Marple 290 or Next Generation Impactor)
- Constant pressure gas supply (8 L/min recommended)
- Analytical balance (0.01 mg resolution)
Methodology:
- Fabricate baffle variants using 3D printing with medical-grade resin.
- Assemble nebulizer cups with each baffle configuration.
- Load with 5 mL of standardized formulation containing tracer compound.
- Operate at fixed gas flow rate (8 L/min) for exactly 2 minutes.
- Collect aerosol using cascade impactor with appropriate flow rate.
- Wash each stage with known volume of appropriate solvent.
- Analyze tracer concentration per stage using validated analytical method.
- Calculate stage-specific deposited mass and cumulative distribution.
- Determine MMAD and FPF for each baffle configuration.
Data Analysis:
- Compare MMAD values across baffle designs using ANOVA
- Optimize baffle dimensions for target particle size range (1-5μm)
- Correlate specific geometric parameters with aerosol performance
The Scientist's Toolkit: Essential Research Materials
Table 4: Essential reagents and materials for nebulization research.
| Item | Function/Application | Research Considerations |
|---|---|---|
| Laser Particle Size Analyzer | Measures droplet size distribution in real-time | Calibrate with standard particles; consider refractive index of test solutions |
| Cascade Impactor | Aerodynamic size separation by inertial impaction | Use with appropriate flow rate; stage coating prevents particle bounce |
| Precision Air Compressor | Delivers consistent gas pressure and flow | Requires regular calibration; pulsation damping may be necessary |
| Hot-Wire Anemometer (e.g., HTI-HT9829) | Measures jet gas velocity at nozzle outlet | Position carefully to avoid flow disturbance; account for turbulence |
| Electronic Balance (0.1 mg resolution) | Determines atomizing rate by mass loss | Environmental factors (vibration, drafts) affect precision |
| 3D Printing System (SLA) | Fabricates custom nebulizer components | Medical-grade biocompatible resins required for drug contact surfaces |
| Test Solutions (0.9% saline, hypertonic saline) | Standardized formulation for performance comparison | Osmolarity and viscosity affect atomization; match physiological properties |
| Fluorescent Tracers (e.g., fluorescein) | Quantifies deposition patterns in experimental models | Validate stability during nebulization; check for surface adsorption |
Advanced Research Applications
Personalized Aerosol Delivery
The recognition that fixed aerosol output parameters may not suit all patients has driven research into personalized nebulization systems. Gas flow control enables adaptation to patient-specific factors including age, disease state, and respiratory pattern [2]. Pediatric patients particularly benefit from modified aerosol characteristics due to their smaller airway dimensions and different breathing patterns compared to adults.
Advanced research explores real-time gas flow modulation synchronized with patient inspiration to maximize lung deposition while minimizing drug waste. This approach, combined with vibrating mesh nebulizer technology, demonstrates particularly efficient alveolar distribution in both healthy and injured lungs [4].
Disease-Specific Optimization
Pathological changes in airway anatomy significantly alter aerosol deposition patterns. Diseases such as COPD and asthma cause airway remodeling and mucous retention that create a proximal shift in deposition [3]. Regional lung diseases further complicate delivery through heterogeneous ventilation, with studies demonstrating lower deposition in atelectatic or poorly ventilated areas [3].
Gas flow optimization must account for these pathological factors. Research shows that despite decreased deposition in severely injured lung regions, nebulized antibiotics still achieve higher lung tissue concentrations than intravenous administration in experimental pneumonia models [3]. This confirms the clinical value of optimized nebulization even in challenging disease states.
Impact of Flow Rate on Droplet Size Distribution and MMAD
In pharmaceutical aerosol inhalation therapy, the efficiency of drug delivery to the respiratory tract is predominantly governed by the droplet size distribution of the generated aerosol [1]. The Mass Median Aerodynamic Diameter (MMAD) is a critical parameter that determines the deposition site of medication within the pulmonary system [1]. Optimal drug delivery requires precise control over droplet size, which is significantly influenced by the nebulizing gas flow rate [2]. This application note systematically examines the impact of gas flow rate on droplet characteristics and provides detailed protocols for researchers and drug development professionals to optimize nebulization parameters for enhanced therapeutic outcomes.
Theoretical Background and Key Principles
Aerosol inhalation therapy serves as an effective method for treating respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD) by delivering medication directly to the affected organs [1]. The targeted deposition of these aerosols is intrinsically linked to droplet size:
- Large particles (>10 μm): Primarily deposit in the upper respiratory tract (nasopharyngeal region)
- Medium-sized particles (5–10 μm): Deposit in the lower respiratory tract (bronchial region)
- Small particles (1–5 μm): Reach the alveolar region with high efficiency [1]
Air-compression nebulizers, which operate based on Bernoulli's theorem and the Venturi effect, utilize high-speed gas flow to atomize liquid medications into fine droplets [2]. In these systems, the supply gas pressure and flow rate are primary controllable parameters that directly influence atomization characteristics, including droplet size distribution, atomization rate, and spray concentration [2].
Quantitative Analysis: Flow Rate Impact on Droplet Characteristics
Effect of Supply Gas Pressure on Flow Rate and Droplet Size
Table 1: Impact of supply gas pressure on gas flow rates and droplet size distribution [2]
| Supply Gas Pressure (kPa) | Supply Gas Flow Rate (L/min) | Jet Gas Flow Rate (L/min) | Dv90 (μm) for 0.6 mm Nozzle | Dv90 (μm) for 0.8 mm Nozzle |
|---|---|---|---|---|
| 50 | 2.48 - 6.42* | 14.28 - 23.01* | 6.85 | 8.91 |
| 100 | 5.87 - 11.34* | 24.15 - 32.67* | 5.47 | 7.12 |
| 150 | 8.91 - 16.02* | 32.67 - 41.38* | 4.78 | 6.28 |
*Range represents variation across different nozzle orifice diameters (0.4-0.8 mm)
MMAD Variation with Nebulizer Operating Parameters
Table 2: MMAD variations across different nebulizer designs and operating conditions [1] [5]
| Nebulizer Type / Condition | MMAD (μm) | Operating Parameters | Notes |
|---|---|---|---|
| Commercial Brand 1 | 9.8 - 14.8 | Standard compressor | Baseline performance |
| Commercial Brand 4 | 0.93 - 3.5 | Standard compressor | Optimal baseline performance |
| With Baffles | ~4.0 - 6.0 | Standard compressor | Estimated from 1.5x reduction |
| Without Baffles | ~6.0 - 9.0 | Standard compressor | Estimated increase |
| ACI at 28.3 L/min | Lower MMAD | Standard testing | Industry standard flow rate |
| ACI at 18 L/min | Higher MMAD | Simulated patient use | More representative of actual patient conditions [5] |
Effective Output Dose (EOD) Considerations
The Effective Output Dose (EOD) represents the mass of drug contained in each liter of air jetted by the nebulizer, providing a crucial metric for estimating the dose inhaled by patients with each inspiration [2]. Research demonstrates that EOD increases with elevated supply gas pressure but shows no significant correlation with nozzle orifice diameter [2].
Figure 1: Relationship between nebulizer operating parameters and droplet characteristics. Increased gas flow rate, achieved through higher supply pressure or smaller nozzle diameter, enhances atomization efficiency and reduces MMAD.
Experimental Protocols
Protocol 1: Measuring Droplet Size Distribution Using Cascade Impaction
Principle: Cascade impactors separate aerosolized droplets by size through a series of stages with progressively smaller cut-off diameters, allowing for determination of MMAD and geometric standard deviation (GSD) [1] [5].
Materials:
- Andersen Cascade Impactor (ACI) or Marple 290 cascade impactor
- Air-compression nebulizer system
- Electronic balance (accuracy ±0.1 mg)
- Calibrated flow meter
- Vacuum pump with flow control
- Environmental control chamber (for humidity/temperature regulation)
Procedure:
- Equipment Setup: Assemble the cascade impactor according to manufacturer specifications. Connect the vacuum pump and adjust to the desired flow rate (e.g., 28.3 L/min for standard testing or 18 L/min for patient-representative conditions) [5].
- Flow Rate Calibration: Use a calibrated flow meter to verify and adjust the operating flow rate through the impactor. Record environmental conditions (temperature, relative humidity).
- Nebulizer Preparation: Fill the nebulizer with a known volume (typically 2-5 mL) of the drug formulation. Weigh the nebulizer assembly to determine initial mass.
- Aerosol Collection: Activate the nebulizer and simultaneously start aerosol collection through the impactor. Ensure a tight seal between the nebulizer outlet and impactor inlet.
- Sample Collection: Run the nebulizer until either the solution is depleted or a specific collection time has elapsed (typically 2-5 minutes).
- Mass Determination: Carefully disassemble the impactor and quantify the drug mass on each stage using appropriate analytical methods (HPLC, UV-Vis spectroscopy, or gravimetric analysis).
- Data Analysis: Plot the cumulative percentage of drug mass against the aerodynamic cut-off diameter for each stage. Determine MMAD as the diameter where the curve crosses 50% cumulative mass.
Critical Considerations:
- Conduct experiments at controlled relative humidity levels, as ambient humidity can significantly affect droplet size measurements [5].
- For patient-representative data, consider using 18 L/min impactor flow rate rather than the standard 28.3 L/min [5].
- Perform replicate measurements (n≥3) to ensure statistical significance.
Protocol 2: Investigating Supply Gas Pressure Effects on Atomization
Principle: Systematic variation of supply gas pressure while measuring resultant gas flow rates, atomization rate, and droplet size distribution [2].
Materials:
- Customizable air-compression nebulizer with interchangeable nozzles
- Regulated air compressor (0-200 kPa)
- Precision gas flow meter
- Laser Particle Size Analyzer (LPSA)
- Electronic balance (accuracy ±0.1 mg)
- Temperature and humidity sensors
Procedure:
- Nozzle Selection: Install nebulizer nozzle with specific orifice diameter (e.g., 0.4 mm, 0.6 mm, 0.8 mm).
- System Calibration: Calibrate gas flow meter and pressure regulator. Verify accuracy with reference instruments.
- Parameter Setting: Set the supply gas pressure to the initial test condition (e.g., 50 kPa).
- Flow Rate Measurement: Record the supply gas flow rate and jet gas flow rate using the calibrated flow meter and hot-wire anemometer, respectively.
- Atomization Rate Determination: Measure the mass of nebulized solution over a fixed time period (typically 1-2 minutes) using an electronic balance.
- Droplet Size Analysis: Direct the aerosol output to the LPSA for real-time droplet size distribution measurement.
- Iterative Testing: Repeat steps 3-6 across a range of supply gas pressures (e.g., 50, 100, 150 kPa).
- EOD Calculation: Calculate Effective Output Dose using the formula: EOD = (Drug concentration × Atomization rate) / Jet gas flow rate.
Critical Considerations:
- Maintain consistent environmental conditions (temperature, humidity) throughout testing.
- Allow system stabilization at each new pressure setting before recording measurements.
- Test multiple nozzle diameters to understand interaction effects between orifice size and gas flow rate.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential materials and equipment for nebulization optimization research
| Item | Function/Application | Specification Notes |
|---|---|---|
| Cascade Impactor | Separates aerosol droplets by size for MMAD determination | Andersen or Marple-type; adjustable flow rate capability (e.g., 18-28.3 L/min) [5] |
| Laser Particle Size Analyzer | Real-time droplet size distribution measurement | Benchtop models with appropriate sizing range (0.1-1000 μm) |
| Benchtop NMR Spectrometer | Non-destructive droplet size distribution in emulsions | MQR time-domain NMR with pulsed-field gradient capability [6] |
| Precision Air Compressor | Controlled gas supply for nebulization | Adjustable pressure (0-200 kPa), stable output [2] |
| Flow Meters | Accurate measurement of gas flow rates | Calibrated for relevant range (e.g., 2-50 L/min) [2] |
| Hot-Wire Anemometer | Jet gas flow velocity measurement | HTI-HT9829 or equivalent [2] |
| Computational Fluid Dynamics Software | Simulation of droplet drying parameters and atomization performance | Capable of multiphase flow modeling with evaporation [7] |
| 3D Printing System | Rapid prototyping of nebulizer components | SLA or similar for high-resolution baffle designs [1] |
Advanced Research Applications
Computational Fluid Dynamics (CFD) in Process Optimization
Computational Fluid Dynamics provides powerful capabilities for simulating the complex multiphase flow and drying kinetics in nebulization systems [7]. CFD implementations can capture:
- Droplet trajectory and residence time distributions within the drying chamber
- Local temperature and relative humidity profiles affecting droplet evaporation
- Drying parameters (κavg, κmax) correlated with final particle characteristics
- Surface enrichment of specific constituents during droplet drying
CFD-guided optimization has demonstrated improved lung delivery efficiency exceeding 60% of the loaded dose in dry powder inhaler formulations [7].
Innovative Measurement Techniques
Time-domain NMR spectroscopy offers a non-destructive alternative for droplet size distribution measurement in emulsions, based on the phenomenon of restricted diffusion [6]. This method:
- Requires minimal sample preparation and avoids structure distortion
- Eliminates the need for hazardous solvents or contrast agents
- Provides excellent repeatability for quality control applications
- Allows further analysis of the same sample by other techniques
The nebulizing gas flow rate serves as a critical process parameter that directly controls droplet size distribution and MMAD in pharmaceutical aerosol products. Through systematic investigation using the protocols outlined in this application note, researchers can optimize flow rate conditions to target specific regions of the respiratory tract. The integration of advanced analytical methods, including cascade impaction, laser diffraction, and computational modeling, provides comprehensive characterization capabilities for developing next-generation nebulized therapies with enhanced pulmonary delivery efficiency.
Correlation Between Flow Rate and Respirable Dose Efficiency
The optimization of nebulizing gas flow rate is a critical parameter in pharmaceutical research and development for inhaled therapeutics. The respirable dose, defined as the fraction of the delivered drug mass residing in particles small enough to reach the lower respiratory tract (typically <5 µm in aerodynamic diameter), is directly influenced by the flow dynamics during aerosol generation [8]. For jet nebulizers, the gas flow rate is a primary determinant of aerosol output rate and particle size distribution, which in turn governs the respirable drug delivery rate (RDDR)—a key efficacy parameter for nebulizer systems [9]. This application note details the correlation between flow rate and respirable dose efficiency, providing standardized protocols for in vitro assessment to support robust pharmaceutical development.
Impact of Flow Rate and Breathing Pattern on Delivered Dose
Table 1: The Influence of Breathing Pattern and Nebulizer Type on Drug Delivery
| Parameter | Impact on Delivered Dose/Respirable Delivered Dose (RDD) | Magnitude of Effect | Citation |
|---|---|---|---|
| Inhalation:Exhalation (I:E) Ratio | Progressive reduction in Delivered Dose (DD) and RDD with increasing exhalation time. | RDD at I:E 1:4 was as little as 40% of the dose at I:E 1:1 for non-breath-activated nebulizers. | [8] |
| Nebulizer Type (General Performance) | Significant variance in delivered dose between different brands. | >4-fold difference in RDD observed between non-breath-activated nebulizers. | [8] |
| Breath-Activated Nebulizers | DD and RDD are largely independent of I:E ratio. | <20% change in RDD between I:E ratios of 1:1 and 1:4 for breath-activated jet nebulizers. | [8] |
| Nebulizer Type (RDDR Comparison) | The Respirable Drug Delivery Rate (RDDR) varies significantly between jet nebulizer systems. | The system with the highest RDDR displayed a value approximately three-fold higher than the system with the lowest RDDR. | [9] |
| High-Flow Nasal Cannula (HFNC) Flow Rate | In a "quiet" breathing pattern, the inhaled dose decreases with increasing gas flow rates. | The percentage of the loaded dose reaching the lung model can be very small, but is optimized at lower flows (e.g., 30 L/min) and with specific nebulizer placement. | [10] |
Table 2: Delivered Dose Efficiency Across Different Breathing Patterns (from BioMedical Engineering OnLine, 2021)
| Breathing Pattern | Tidal Volume (mL) | Respiration Rate (BPM) | I:E Ratio | Typical Delivered Dose Efficiency (Relative to ISO Standard) |
|---|---|---|---|---|
| ISO 27427:2013 | 500 | 15 | 1:1 | Baseline (Highest) |
| Normal Adult | 500 | 15 | 1:2 | Significant reduction |
| Asthma Adult | 290 | 25 | 1:2.5 | Further reduction |
| COPD | 494 | 20 | 1:4 | Lowest |
Experimental Protocols
Protocol 1: Assessment of Nebulizer Efficiency Using a Breathing Simulator
This protocol is designed to quantify the delivered dose and calculate the Respirable Drug Delivery Rate (RDDR) under simulated physiological conditions [9] [11] [12].
Materials and Equipment
- Nebulizer system(s) under test
- Breathing simulator (e.g., PARI COMPAS) capable of generating defined tidal volumes, frequencies, and I:E ratios
- Adult airway model (e.g., VTA-M, RDDonline)
- Next Generation Impactor (NGI) or equivalent particle sizing instrument
- High-Performance Liquid Chromatography (HPLC) system with UV detector
- Analytical balance
- Drug solution (e.g., 0.1% w/v salbutamol sulfate or a solution of your target pharmaceutical)
Procedure
- System Preparation: Fill the nebulizer with a precise volume (e.g., 2 mL) of the drug solution. Weigh the entire assembly to determine the initial mass.
- Breathing Simulation Setup: Program the breathing simulator to the desired pattern. The ISO 27427:2013 standard pattern is a common baseline: 500 mL tidal volume, 15 breaths per minute, and a 1:1 I:E ratio [8] [9].
- Aerosol Collection for Delivered Dose (DD): Connect the nebulizer to the breathing simulator and an appropriate filter placed after the airway model to capture the aerosol that would be inhaled. Activate the nebulizer and run the simulator until nebulization is complete (sputtering for jet nebulizers or no visible aerosol for mesh devices) [11] [12].
- Particle Size Analysis: Determine the aerosol's particle size distribution using the NGI at a defined flow rate (e.g., 15 L/min). This allows for the calculation of the Respirable Fraction (RF), which is the fraction of particles <5 µm [9].
- Data Analysis:
- Emitted Dose (ED): Determine gravimetrically or via drug assay of the nebulizer before and after treatment.
- Delivered Dose (DD): Quantify the amount of drug collected on the inhalation filter using HPLC.
- Respirable Delivered Dose (RDD): Calculate as RDD = DD × RF.
- Respirable Drug Delivery Rate (RDDR): Calculate as RDDR = (Aerosol Output Rate) × RF. The aerosol output rate is the emitted dose divided by the nebulization time [9].
Protocol 2: Optimizing Flow Rate for Nebulization within a High-Flow Nasal Cannula (HFNC) Circuit
This protocol defines the methodology for evaluating and optimizing aerosol delivery integrated with HFNC therapy, a complex clinical scenario where flow rate is a dominant variable [13] [10].
Materials and Equipment
- HFNC system (e.g., Airvo2)
- Vibrating Mesh Nebulizer (VMN) (e.g., Aerogen Solo)
- Adult or child airway model
- Heated humidifier chamber
- Drug solution (e.g., 2.5 mg albuterol)
- Collection filter apparatus
Procedure
- Circuit Setup: Place the VMN immediately upstream of the humidifier chamber. This position has been shown to be one of the most efficient for drug delivery [10].
- HFNC and Breathing Parameters: Set the HFNC to a specific gas flow rate (e.g., 30 L/min, 37 °C, 100% relative humidity). Program the breathing simulator to an appropriate pattern (e.g., "quiet" or "distressed" breathing).
- Nebulization: Add the drug solution to the nebulizer and initiate the HFNC flow. Start nebulization after the circuit is stabilized.
- Sample Collection: Collect the aerosol that passes through the airway model onto a filter.
- Variation of Flow Rate: Repeat the experiment at different HFNC flow rates (e.g., 10 L/min, 30 L/min, 50 L/min) while keeping all other parameters constant.
- Data Analysis: Quantify the drug on the filter for each condition. The results will demonstrate an inverse relationship between HFNC flow rate and inhaled dose under quiet breathing conditions, allowing for the identification of an optimal flow rate that balances therapy and delivery efficiency [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials for Nebulizer Efficiency and Flow Rate Studies
| Item | Function/Description | Example Models/Details |
|---|---|---|
| Breathing Simulator | Reproduces human breathing patterns (tidal volume, rate, I:E ratio) for in vitro testing. | PARI COMPAS; Custom systems with linear actuators and air cylinders. |
| Anatomical Airway Model | Mimics the geometry of the human upper airway, providing realistic deposition data. | VTA-M (Adult); 3D-printed pediatric models. |
| Cascade Impactor | Measures the aerodynamic particle size distribution (APSD) of aerosols. | Next Generation Impactor (NGI). |
| Laser Diffraction Analyzer | Provides real-time particle size analysis of the aerosol plume. | Malvern Spraytec. |
| Vibrating Mesh Nebulizer (VMN) | Aerosol generator known for high delivery efficiency and low residual volume; essential for HFNC studies. | Aerogen Solo, NE-SM1 NEPLUS. |
| Breath-Enhanced Jet Nebulizer | A type of jet nebulizer with a design that increases aerosol output during patient inhalation. | PARI LC SPRINT (used with PARI BOY compressor). |
| Analytical Quantification System | Precisely measures the amount of drug collected in filters or deposited in impactor stages. | HPLC with UV detection. |
Workflow for Nebulizer Efficiency Testing
The following diagram illustrates the logical workflow and decision points in a comprehensive nebulizer efficiency study.
Diagram 1: Experimental Workflow for Nebulizer Efficiency Assessment. This workflow integrates the selection of critical parameters (nebulizer, breathing pattern) with standardized experimental and analytical steps to determine key performance metrics like Delivered Dose (DD) and Respirable Drug Delivery Rate (RDDR).
The gas flow rate is a fundamental parameter that exhibits a strong and complex correlation with respirable dose efficiency. Key findings confirm that:
- Standardized testing using a single breathing pattern is insufficient to predict performance across the range of patterns seen in patients with respiratory diseases [8] [11].
- The Respirable Drug Delivery Rate (RDDR) serves as a superior, clinically relevant parameter for comparing nebulizer systems, as it integrates both aerosol output rate and respirable fraction [9].
- In integrated systems like HFNC, lower flow rates (e.g., 30 L/min) and strategic nebulizer placement (upstream of the humidifier) are critical for maximizing drug delivery [13] [10].
The experimental protocols outlined herein provide a framework for pharmaceutical researchers to systematically optimize nebulizing gas flow rates, ensuring the development of efficient and therapeutically effective inhaled products.
Understanding Depositional Losses in Delivery Circuits
In pharmaceutical aerosol research, depositional losses refer to the portion of a drug that is lost within the delivery circuit before it reaches the intended respiratory target. These losses significantly reduce delivery efficiency and therapeutic efficacy, particularly in nebulizer systems used for inhaled medications. For researchers optimizing nebulizing gas flow rates, understanding and minimizing these losses is paramount to developing effective drug delivery systems. Depositional mechanisms are influenced by multiple factors including particle characteristics, airway geometry, and breathing patterns [14]. This application note examines the primary mechanisms of depositional losses, provides quantitative data on key influencing factors, details standardized measurement protocols, and offers evidence-based strategies for circuit optimization.
Mechanisms of Depositional Losses
Therapeutic aerosol deposition in delivery circuits and respiratory systems occurs through several physical mechanisms, each dominant under different conditions.
Inertial Impaction: This mechanism predominates for larger particles (>0.5 μm) and in regions with high airflow velocity or directional changes, such as in the oropharyngeal region and at circuit bends. Particles cannot follow the abrupt changes in airflow streamlines and impact surfaces. In nebulizer circuits, impaction is significant at connection points, valves, and the proximal endotracheal tube [14] [15].
Sedimentation: This process results from gravitational settling and is primarily responsible for deposition in the smaller airways and alveolar region where airflow velocities are low. Its effect is most pronounced for particles in the 1-5 μm size range during breath-holding pauses [14].
Diffusion (Brownian Motion): For very small particles (<0.2 μm) and nanoparticles, random molecular motion causes deposition by diffusion, which becomes particularly important in the deep lung regions [14] [16].
Electrostatic Attraction: Pharmaceutical aerosols may carry electrostatic charges from generation processes, especially in DPIs and pMDIs. These charges can induce attractive image forces with circuit walls, enhancing deposition regardless of other particle characteristics [14].
Interception: This occurs when a particle following an airstream comes close enough to a surface for its edge to make contact. This mechanism is particularly relevant for fibrous or elongated particles [14].
Quantitative Factors Influencing Depositional Losses
Impact of Nebulizer Positioning in Ventilator Circuits
The position of the nebulizer within the delivery circuit dramatically affects lung deposition efficiency. The table below summarizes preclinical scintigraphy data comparing different nebulizer positions under humidified and dry conditions [15].
Table 1: Respiratory Tract Deposition Fraction Based on Nebulizer Position
| Nebulizer Position | Humidified Conditions | Dry Conditions |
|---|---|---|
| Next to ventilator | - | 18% (±4%) |
| Right before humidifier | 25% (±3%) | - |
| 15 cm to Y-piece | 57% (±8%) | - |
| Right after Y-piece (proximal) | 43% (±11%) | 53% (±4%) |
Effect of Supply Gas Parameters on Aerosol Characteristics
Gas flow rate and pressure significantly influence aerosol characteristics and subsequent deposition patterns. Higher supply gas pressures generally increase the effective output dose (EOD), defined as the mass of drug contained in each liter of air jetted by the nebulizer [2].
Table 2: Effect of Supply Gas Pressure on Nebulizer Performance
| Supply Gas Pressure (kPa) | Nozzle Orifice Diameter (mm) | Droplet Size (Dv90, μm) | Atomizing Rate Trend | EOD Trend |
|---|---|---|---|---|
| 50-150 | 0.4 | 7.09 to 8.47 (increase) | Increase | Increase |
| 50-150 | 0.6 | Decrease | Increase | Increase |
| 50-150 | 0.8 | 29.5% decrease | Increase | Increase |
Particle Size and Regional Deposition
Particle size fundamentally determines deposition patterns through the respiratory tract. The following table summarizes typical deposition fractions based on aerodynamic diameter during mouth breathing [14].
Table 3: Regional Deposition Fractions by Particle Size (Mouth Breathing)
| Aerodynamic Diameter (μm) | Oral Deposition | Tracheobronchial Deposition | Pulmonary Deposition |
|---|---|---|---|
| 1 | Low | Moderate | High |
| 3 | Moderate | High | Moderate |
| 5 | High | Moderate | Low |
| >10 | Very High | Very Low | Negligible |
Experimental Protocols for Quantifying Depositional Losses
Scintigraphic Deposition Measurement
Purpose: To quantitatively measure regional aerosol deposition in respiratory tracts and delivery circuits using radiolabeled tracers.
Materials:
- Gamma camera (SPECT/CT system)
- 99mTechnetium-labeled diethylene-triamine-penta-acetic acid (99mTc-DTPA)
- Vibrating mesh nebulizer (e.g., Aerogen Solo)
- Mechanical ventilator system
- Ex vivo respiratory tract model or anatomical replica
- Data acquisition and analysis software
Procedure:
- Prepare the radiolabeled tracer by adding 100 MBq of 99mTc-DTPA to the nebulizer medication chamber (3 mL total volume).
- Record the initial radioactive dose using scintigraphic images (180-s anterior/posterior acquisitions).
- Assemble the delivery circuit with the nebulizer positioned at the test location.
- Initiate mechanical ventilation with standardized parameters (tidal volume: 540 mL, respiratory rate: 20/min, inspiratory flow: 35 L/min).
- Begin nebulization and continue for a standardized duration (minimum 15 minutes).
- After nebulization completion, acquire scintigraphic images of each circuit component and respiratory region.
- Quantify deposition fractions by measuring radioactivity in each region relative to the initial nominal dose.
- Calculate losses in individual circuit components (nebulizer, tubing, connectors, valves) by summing the residual radioactivity [15].
Characterization of Aerosol Generation Parameters
Purpose: To measure the effect of supply gas parameters on nebulizer output characteristics.
Materials:
- Medical air-compression nebulizer with variable nozzle designs
- Air compressor with pressure regulation (0-150 kPa capacity)
- Laser Particle Size Analyzer (e.g., Malvern Spraytec)
- Gas flow meter (e.g., SIARGO-MF5700)
- Electronic balance (e.g., LICHEN-FA324TC)
- Hot-wire anemometer (e.g., HTI-HT9829)
Procedure:
- Connect the nebulizer to the pressure-regulated air supply.
- Place the nebulizer outlet in line with the laser particle size analyzer measurement zone.
- For each pressure setting (e.g., 50, 100, 150 kPa):
- Measure the supply gas flow rate using the gas flow meter
- Record the atomizing rate by weighing the nebulizer before and after a timed operation
- Measure droplet size distribution using the laser particle analyzer
- Calculate the Effective Output Dose (EOD): EOD = (Drug concentration × Atomizing rate) / Gas flow rate
- Repeat measurements for different nozzle orifice diameters (0.4, 0.6, 0.8 mm)
- Analyze correlations between supply pressure, droplet size distribution, and output metrics [2].
Single-Breath Nanoparticle Deposition Measurement
Purpose: To measure respiratory tract deposition of nanoparticles in a single breath with controlled breathing parameters.
Materials:
- Electrospray aerosol generator (e.g., TSI 3480)
- Differential Mobility Analyzer (e.g., TSI 3071)
- Condensation Particle Counter (e.g., TSI 3760)
- Computer-controlled four-way valve system
- Breathing flow meter with data acquisition (100 Hz resolution)
Procedure:
- Generate monodisperse nanoparticles (e.g., 22, 50, 75, 100 nm) using the electrospray generator and DMA.
- Direct the aerosol to a reservoir with continuous refreshment and dilution to 2000-6000 particles/cm³.
- Instruct the subject to breathe particle-free air for 30 seconds, then exhale to residual volume.
- At the start of inhalation, switch the valve to the aerosol reservoir.
- After complete inhalation to total lung capacity, initiate a programmed breath-holding period (3-20 s).
- During exhalation, collect a 300 mL sample from the predetermined volumetric lung depth.
- Measure particle concentration in both inhaled and exhaled samples using the CPC.
- Calculate particle recovery (deposition fraction): R = 1 - (Cexhaled / Cinhaled) with correction for instrument losses [16].
Research Reagent Solutions and Materials
Table 4: Essential Research Materials for Deposition Studies
| Material/Equipment | Function | Example Models/Types |
|---|---|---|
| Vibrating Mesh Nebulizer | Generates therapeutic aerosol with high efficiency | Aerogen Solo |
| Condensation Particle Counter | Detects and counts nanoparticle concentrations | TSI 3760, TSI 3010 |
| Differential Mobility Analyzer | Classifies particles by electrical mobility to generate monodisperse aerosols | TSI 3071 |
| Laser Particle Size Analyzer | Measures droplet size distribution in real-time | Malvern Spraytec |
| Electrospray Aerosol Generator | Produces monodisperse nanoparticles from solution | TSI 3480 |
| 99mTechnetium-DTPA | Radiolabeled tracer for scintigraphic deposition imaging | Technescan DTPA |
| Scanning Mobility Particle Sizer | Characterizes aerosol size distribution | Custom SMPS systems |
| Gamma Camera System | Quantifies regional deposition through radiation detection | SPECT/CT systems |
Optimization Strategies and Circuit Design
Based on current evidence, the following strategies minimize depositional losses:
Nebulizer Positioning: Place the nebulizer 15 cm proximal to the Y-piece adapter in ventilator circuits to maximize lung deposition (57% vs 18% when placed next to the ventilator) [15].
Gas Humidification: Maintain gas humidification during nebulization, as it improves overall deposition efficiency compared to dry gas conditions while preventing potential tissue damage from dry aerosol delivery [15].
Pressure and Nozzle Optimization: Select appropriate nozzle orifice diameter (0.6-0.8 mm) and moderate supply pressures (100-150 kPa) to balance droplet size reduction and gas consumption [2] [17].
Flow Rate Considerations: Higher gas flow rates generally produce smaller droplets but increase turbulent losses. The gas-liquid ratio is the primary factor affecting aerosol size when baffle width is constant [17].
Circuit Geometry: Minimize directional changes, constrictions, and unnecessary connections in delivery circuits to reduce inertial impaction losses.
Visualization of Experimental Workflows
Experimental Workflow for Single-Breath Deposition Measurement [16]
Deposition Mechanisms and Their Dominant Regions [14]
Depositional losses in delivery circuits represent a significant challenge in pharmaceutical aerosol research, substantially impacting drug delivery efficiency and therapeutic outcomes. Through systematic characterization of deposition mechanisms, precise measurement using standardized protocols, and implementation of optimization strategies focused on nebulizer positioning and gas flow parameters, researchers can significantly enhance aerosol delivery efficiency. The methodologies outlined in this application note provide a framework for evidence-based optimization of nebulizing gas flow rates and circuit configurations, ultimately contributing to the development of more efficient pharmaceutical aerosol delivery systems.
Applied Flow Rate Strategies for Different Delivery Systems and Patient Populations
Optimizing Flow Rates for Jet vs. Mesh Nebulizers
Nebulizers are critical devices in respiratory medicine, converting liquid medications into aerosols for inhalation. The efficiency of this drug delivery is profoundly influenced by the nebulizing gas flow rate, a key parameter that controls aerosol characteristics and deposition patterns in the lungs. For jet nebulizers (JNs), which operate on compressed gas, the flow rate is a primary, direct input. In contrast, vibrating mesh nebulizers (VMNs) use a vibrating piezoelectric element to push liquid through a mesh, and their "flow rate" often relates to the patient's inspiratory flow or the carrier gas flow in a circuit. This document provides application notes and experimental protocols for researchers and drug development professionals aiming to optimize these parameters for pharmaceutical aerosols.
Performance Data and Comparative Analysis
Quantitative Comparison of Nebulizer Technologies
The fundamental operational differences between JNs and VMNs lead to distinct performance profiles. The following table synthesizes key quantitative findings from recent research.
Table 1: Comparative Performance Metrics of Jet and Mesh Nebulizers
| Performance Parameter | Jet Nebulizer (JN) | Vibrating Mesh Nebulizer (VMN) | Citation & Context |
|---|---|---|---|
| Typical Delivered Dose (% of nominal dose) | 2.46% - 8.20% (Varies with breathing pattern) | 6.75% - 18.49% (Varies with breathing pattern) | In vitro model simulating spontaneous breathing [18]. |
| Relative Delivery Efficiency | Baseline | 2 to 3-fold higher than JN across all tested breathing patterns (normal, obstructive, restrictive) [18]. | In vitro model simulating spontaneous breathing [18]. |
| Improvement in Pulmonary Function (FEV1) | Significant improvement post-treatment | Significantly greater improvement post-treatment compared to JN [19]. | Clinical trial on pediatric asthma attacks [19]. |
| Improvement in Small Airway Function (FEF~25-75~) | Significant improvement post-treatment | Significantly greater improvement post-treatment compared to JN [19]. | Clinical trial on pediatric asthma attacks [19]. |
| Droplet Size Influence | Primarily determined by baffle design and gas pressure. | Smaller, more consistent particles; size can be tailored via mesh pore size [19] [20]. | Clinical and technical reviews [19] [20]. |
| Residual Drug Volume | Higher, leading to more waste [19]. | Lower, leading to higher inhaled dose [19]. | Clinical trial [19]. |
| Key Operational Parameter | Supply Gas Pressure/Flow Rate [2]. | Mesh pore size, vibration frequency, and formulation properties [21]. | Engineering and clinical studies [21] [2]. |
| Impact of Breathing Patterns | Delivery significantly reduced in obstructive/restrictive patterns vs. normal (e.g., ~65% reduction in severe obstruction) [18]. | Delivery significantly reduced in obstructive/restrictive patterns vs. normal, but absolute doses remain higher than JN [18]. | In vitro study [18]. |
Table 2: Impact of Jet Nebulizer Supply Gas Pressure on Atomization Characteristics
| Atomization Characteristic | Relationship with Increasing Supply Gas Pressure | Notes and Mechanisms |
|---|---|---|
| Supply Gas Flow Rate | Increases [2]. | Linear relationship with pressure. |
| Jet Gas Flow Velocity | Increases [2]. | Higher pressure generates higher velocity at the orifice. |
| Atomizing Rate | Increases [2]. | Higher gas velocity shears liquid more efficiently. |
| Droplet Size (D~v90~) | Decreases for orifice diameters ≥ 0.6 mm; may increase for smaller orifices (0.4 mm) at high pressure [2]. | Higher shear forces produce finer droplets. Anomalous increase in smaller orifices may be due to flow regime changes. |
| Droplet Size Uniformity | Improves (distribution narrows) [2]. | More stable and consistent atomization. |
| Spray Concentration | Increases [2]. | More liquid is aerosolized per unit volume of gas. |
| Effective Output Dose (EOD) | Increases [2]. | Represents the mass of drug per liter of air, indicating a higher effective dose per inspiration. |
Key Insights from Data
- VMN Superiority in Delivered Dose: Under identical conditions, VMNs consistently deliver a higher percentage of the nominal drug dose to the lungs, regardless of pathological breathing patterns [18]. This is attributed to their lower residual volume and ability to generate optimal droplet sizes without the need for a high-velocity gas stream [19].
- Criticality of JN Gas Pressure: For jet nebulizers, supply gas pressure is the master variable controlling nearly all atomization characteristics. Optimizing this parameter is essential for balancing droplet size (for deep lung penetration) and output rate (for treatment time) [2].
- Breathing Pattern is a Major Confounder: The patient's breathing pattern (normal, obstructive, restrictive) can cause a greater than 2.5-fold variation in delivered dose, irrespective of nebulizer type [18]. This underscores the need for in vitro testing under realistic breathing profiles.
Experimental Protocols
Protocol 1: Clinical Efficacy Comparison of JN vs. VMN
This protocol is based on a double-blind, randomized comparative clinical trial evaluating nebulizers in a pediatric asthma population [19].
1. Objective: To compare the efficacy of jet and mesh nebulizers in improving pulmonary function and vital signs in pediatric patients experiencing acute asthma exacerbations.
2. Materials:
- Nebulizers: Compressor nebulizer (CN) representing JN technology, and a vibrating mesh nebulizer (VMN).
- Drug: Short-acting β₂ agonist (e.g., Salbutamol solution).
- Equipment: Spirometer (for FEV1, FVC, FEF~25-75~), pulse oximeter, timer.
- Subjects: Patient cohort meeting inclusion criteria (e.g., aged 7-15, presenting with acute asthma attack).
3. Methodology:
- Study Design: Prospective, parallel, double-blind, randomized controlled trial.
- Randomization & Blinding: Patients are randomly assigned to JN or VMN groups. Treatments are administered by a third party to ensure blinding of both patients and outcome assessors.
- Intervention: All patients receive a standardized dose of Salbutamol via the assigned nebulizer.
- Data Collection:
- Baseline: Record demographic data, medical history, pre-treatment pulmonary function tests (FEV1, FVC, FEF~25-75~), and vital signs (respiratory rate, heart rate, SpO2).
- Post-treatment: Repeat pulmonary function tests and vital sign measurements immediately after the nebulization treatment is complete.
- Outcome Measures:
- Primary: Absolute and percent change in FEV1.
- Secondary: Changes in FEF~25-75~, FVC, respiratory rate, and heart rate.
- Statistical Analysis: Compare within-group and between-group changes using appropriate statistical tests (e.g., paired t-tests, ANOVA). A p-value < 0.05 is considered significant.
The workflow for this clinical evaluation is outlined below.
Protocol 2: In-Vitro Optimization of JN Gas Flow Rate
This protocol is derived from studies investigating the effect of operational parameters on nebulizer atomization characteristics [18] [2].
1. Objective: To determine the optimal supply gas pressure/flow rate for a jet nebulizer by characterizing its effect on droplet size distribution, atomizing rate, and effective output dose.
2. Materials:
- Test Nebulizer: Jet nebulizer(s) under investigation.
- Gas Supply: Compressed air or oxygen source with a precision pressure regulator and flow meter.
- Drug Simulant: 0.9% w/v Sodium Chloride (NaCl) solution or specific drug formulation.
- Equipment: Laser Particle Size Analyzer (LPSA), electronic balance (0.1 mg precision), filter setup, timer, hot-wire anemometer.
3. Methodology:
- Experimental Setup: Connect the gas supply to the nebulizer. Place the nebulizer cup on the balance and fill it with a fixed volume of the test solution (e.g., 2.5 mL or 5 mL).
- Variable Manipulation: Set the gas supply pressure to a series of predefined values (e.g., 50, 100, 150 kPa). For each pressure setting, record the corresponding gas flow rate (L/min).
- Data Collection at Each Pressure/Flow Setting:
- Atomizing Rate: Weigh the nebulizer before and after a fixed period of operation (e.g., 2 minutes). Calculate the mass loss per unit time (mg/min).
- Droplet Size Distribution: Direct the aerosol plume into the LPSA measurement zone. Record the volumetric median diameter (D~v50~) and the D~v90~ (diameter below which 90% of the droplet volume resides).
- Effective Output Dose (EOD): Collect the aerosol on an absolute filter for a known duration and volume of gas. Elute the drug and quantify it (e.g., via UV spectroscopy). Calculate EOD as (Mass of drug collected) / (Total gas volume used) (e.g., µg/L) [2].
- Data Analysis: Plot atomizing rate, D~v90~, and EOD against the supply gas pressure/flow rate. The "optimal" range is typically where a high EOD and atomizing rate coincide with a target D~v90~ of 1-5 µm for lower respiratory deposition.
The logical relationship between the controlled parameter and the measured outcomes is depicted below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Equipment for Nebulizer Flow Rate Research
| Item | Function/Application | Example/Citation |
|---|---|---|
| Laser Particle Size Analyzer (LPSA) | Measures the size distribution of aerosolized droplets in real-time, a critical quality attribute. | [2] |
| Electronic Balance (High Precision) | Used in gravimetric analysis to determine nebulizer output and atomizing rate by measuring mass loss over time. | [22] [2] |
| Bubble Absorption Tube / Absolute Filter | Captures the aerosol plume for chemical quantification, enabling calculation of delivered dose or EOD. | [21] [2] |
| Breathing Simulator | Simulates realistic human breathing patterns (tidal volume, waveform, rate) for in vitro deposition studies. | QuickLung Breather; used to model normal, obstructive, and restrictive patterns [18]. |
| UV-Vis Spectrophotometer | Quantifies the amount of drug collected on a filter by measuring the absorbance of an eluted sample. | Used to determine albuterol concentration in deposition studies [18]. |
| Sodium Chloride (0.9% w/v) | A common isotonic solution used as a drug simulant for foundational atomization performance testing. | [21] [2] |
| Compressed Gas Source & Regulator | Provides a controllable and stable supply of compressed air or oxygen for operating jet nebulizers. | Requires a precision pressure regulator and flow meter [2]. |
| Anatomical Airway Model | A physical replica (e.g., mouth-throat model) of the human airways used to study regional aerosol deposition. | Idealized MT (mouth-throat) model [21]. |
Flow Rate Considerations for Non-Invasive Ventilation (NIV) and High-Flow Nasal Cannula (HFNC)
Non-invasive respiratory support is a cornerstone in the management of acute respiratory failure, with Non-Invasive Ventilation (NIV) and High-Flow Nasal Cannula (HFNC) representing two primary modalities [23]. For researchers in pharmaceutical development, understanding the technical parameters of these devices is crucial, particularly when designing studies for aerosolized drug delivery. The flow rate setting is a critical operational parameter that directly influences the physiological effects of respiratory support, patient comfort, and the efficacy of concomitant nebulized therapies [2] [24]. This document provides a detailed examination of flow rate considerations for NIV and HFNC, framing them within the context of optimizing pharmaceutical research and nebulized drug delivery.
Physiological and Technical Fundamentals of Gas Flow
Distinct Mechanisms of Action
NIV and HFNC operate on distinct principles, which dictates their respective flow rate parameters and clinical applications. NIV, which includes Continuous Positive Airway Pressure (CPAP) and Bilevel Positive Airway Pressure (BiPAP), provides pressurized gas delivery through an interface, creating positive pressure throughout the respiratory cycle [23]. The key settings are the applied pressures (e.g., Inspiratory Positive Airway Pressure - IPAP, Expiratory Positive Airway Pressure - EPAP). The resulting flow is variable and depends on both ventilator settings and patient effort.
In contrast, HFNC delivers a constant, high flow of heated and humidified gas through nasal cannulas. Its physiological effects include: [23]
- Provision of Low-Level PEEP: HFNC generates positive airway pressure (typically 1-4 cmH₂O), which is flow-dependent and increases with higher set flow rates [23].
- Anatomical Dead Space Washout: High flows facilitate continuous flushing of carbon dioxide from the upper airways, improving alveolar ventilation [23].
- Enhanced Patient Comfort: The heating and humidification of gases allow for high flow rates to be well-tolerated for prolonged periods [23].
Interface and Gas Conditioning
The interface is a critical component differentiating these modalities. NIV is typically administered via facemasks, oro-nasal masks, or helmets, which can create a sealed system necessary for higher pressure delivery but may cause discomfort, claustrophobia, or skin damage [23] [25]. HFNC uses dedicated, often larger-bore, nasal cannulas, which are generally better tolerated and allow for talking, eating, and drinking [23] [26]. The heated and humidified gas in HFNC is essential for patient tolerance at high flows and for maintaining airway mucosa integrity [23]. For pharmaceutical research, the interface and gas conditioning directly impact drug delivery efficiency and patient compliance during experimental protocols.
Flow Rate Parameters and Clinical Outcomes
HFNC Flow Rate Titration and Evidence
HFNC flow rates are actively titrated based on clinical goals. The following table summarizes standard flow rate ranges and their rationales, particularly relevant for designing drug delivery studies.
Table 1: HFNC Flow Rate Titration and Clinical Evidence
| Clinical Scenario | Recommended Flow Rate | Physiological Rationale & Research Considerations | Key Evidence |
|---|---|---|---|
| General AHRF / Post-Extubation | 40-60 L/min [23] [27] | Higher flows (e.g., 60 L/min) maximize PEEP effect and oxygenation in hypoxemic states. Sufficient flow must meet or exceed patient's peak inspiratory flow. | A 2025 RCT (n=169) found no significant difference in reintubation between 40 vs. 60 L/min post-extubation, but 40 L/min group required more escalation (27.9% vs 9.6%) [27]. |
| Hypercapnic Respiratory Failure (e.g., AECOPD) | 30-40 L/min [23] | Lower flows may be sufficient for CO₂ clearance. Higher flows do not consistently offer additional benefits in reducing inspiratory workload in hypercapnia [23]. | A 2025 meta-analysis of AECOPD patients showed no mortality/intubation difference vs NIV, but a trend toward higher treatment failure with HFNC [25]. |
| Patient Tolerance & Comfort | Titrate from 30-50 L/min, adjust temperature [23] | Patient comfort is crucial for adherence. Discomfort can arise from high flow or excessive humidification. Starting at a lower temperature (31°C) may improve initial comfort [23]. | HFNC consistently demonstrates significantly better patient tolerance and lower treatment intolerance compared to NIV interfaces [25] [26]. |
NIV Pressure Settings and resultant Flow
NIV is titrated using pressure settings rather than a direct flow parameter. The resultant flow is variable. The following table outlines standard pressure settings for different clinical conditions, which is vital for understanding the environment in which nebulized drugs are delivered.
Table 2: NIV Mode and Pressure Setting Guidelines
| Clinical Indication | Recommended NIV Mode & Initial Settings | Physiological Rationale | Research Implications |
|---|---|---|---|
| Acute Hypercapnic Respiratory Failure (e.g., AECOPD) | BiPAP (PS/PEEP) via facemask [23] [28] | Pressure Support (PS) unloads respiratory muscles and aids CO₂ clearance. PEEP counteracts intrinsic PEEP (auto-PEEP). | The strong evidence base for NIV in AECOPD makes it a common model for studying hypercapnia rescue therapies. |
| Cardiogenic Pulmonary Edema | CPAP or BiPAP [23] [28] | Positive pressure reduces left ventricular preload and afterload, improving cardiac output. | A stable hemodynamic profile is important for pharmacokinetic studies. |
| de novo Acute Hypoxemic Respiratory Failure | HFNC is often first-line. CPAP may be considered [23] [29] | CPAP increases end-expiratory lung volume and reduces intrapulmonary shunt, improving oxygenation. | High driver pressures and intense inspiratory effort in these patients may increase the risk of patient-self-inflicted lung injury (P-SILI) [23]. |
Comparative Physiological Effects
A 2025 randomized crossover physiological study in high-risk extubation patients directly compared the effects of NIV and HFNO [30]. The study demonstrated that:
- Inspiratory Efforts: Were significantly lower with NIV (simplified esophageal pressure–time product (sPTPes) of 196 cm H₂O·s/min) compared to HFNO (220 cm H₂O·s/min) [30].
- Tidal Volumes: Were larger with NIV (8.4 mL/kg PBW) compared to HFNO (6.9 mL/kg PBW) [30].
These findings suggest that NIV provides more substantial ventilatory support by reducing work of breathing and increasing tidal volume, which may influence drug distribution within the respiratory tract.
Experimental Protocols for Respiratory Support Research
Protocol 1: Comparing HFNC Flow Rates on Extubation Outcomes
This protocol is adapted from a 2025 RCT investigating 40 L/min vs. 60 L/min flow rates [27].
1. Objective: To determine if a higher HFNC flow rate (60 L/min) reduces the rate of reintubation or rescue NIV use within 48 hours after planned extubation, compared to a standard flow rate (40 L/min).
2. Study Population:
- Inclusion Criteria: Adult patients (≥18 years) intubated for >24 hours undergoing planned extubation.
- Exclusion Criteria: Pre-existing tracheostomy, do-not-reintubate order, or immediate need for reintubation post-extubation.
3. Randomization & Blinding:
- Open-label, parallel-group randomized controlled trial.
- Computer-generated randomization sequence.
4. Intervention Groups:
- Experimental Group (60 L/min): HFNC flow rate set at 60 L/min immediately post-extubation. Temperature set to 37°C, FiO₂ titrated to SpO₂ ≥ 92%.
- Control Group (40 L/min): HFNC flow rate set at 40 L/min. Temperature and FiO₂ management identical to the experimental group.
- The assigned flow rate is maintained for 24 hours.
5. Primary Outcome:
- Composite of reintubation or use of rescue NIV within 48 hours post-extubation.
6. Key Secondary Outcomes:
- Escalation of respiratory support (e.g., use of NIV or up-titration of HFNC settings).
- 28-day mortality.
- Patient comfort measured using a visual analogue scale (VAS).
7. Statistical Analysis:
- Intention-to-treat analysis.
- Primary outcome compared using Chi-square test, reporting risk difference with 95% confidence interval.
Protocol 2: Physiological Comparison of NIV vs. HFNC
This protocol is based on a 2025 physiological crossover study [30].
1. Objective: To compare the physiological effects of prophylactic NIV and HFNC on inspiratory efforts and tidal volumes in patients at high-risk of extubation failure.
2. Study Design: Prospective, randomized, crossover physiological study.
3. Study Population:
- Inclusion Criteria: Intubated patients >24 hours, high-risk of extubation failure (age >65 or underlying cardiac/respiratory disease), successful spontaneous breathing trial.
- Exclusion Criteria: Contraindication to nasogastric tube or NIV, do-not-reintubate order.
4. Intervention & Measurements:
- Instrumentation: Prior to extubation, insert an esophageal balloon catheter to measure esophageal pressure (Pes). Place an Electrical Impedance Tomography (EIT) belt.
- Randomized Crossover Sequence: After extubation, patients receive in random order:
- NIV Period (20 min): Delivered via facemask in PSV mode. PEEP ≥5 cmH₂O, PS titrated to expired Vt 6-8 mL/kg PBW.
- HFNC Period (20 min): Flow set to at least 40 L/min. Each period is followed by a washout period on standard oxygen.
- Data Collection: During the last 5 minutes of each 20-minute period, record:
- Airway flow, esophageal pressure (Pes), and EIT signals.
- Calculate primary outcome: simplified Pes-time-product per minute (sPTPes).
- Calculate secondary outcomes: Tidal volume (from EIT), transpulmonary pressure swings, dynamic compliance.
5. Statistical Analysis:
- Use Wilcoxon signed-rank test for paired comparisons of sPTPes and tidal volumes between NIV and HFNC periods.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for Respiratory Support Research
| Item | Function/Application in Research |
|---|---|
| High-Flow Nasal Cannula Device (e.g., Airvo2, Optiflow) | Delivers heated and humidified gas at precise flow rates (up to 60 L/min). Essential for studying HFNC-specific interventions [26]. |
| ICU/Transport Ventilator with NIV Mode (e.g., Carescape R860, Astral 150) | Provides pressure-controlled ventilation (CPAP, BiPAP) via non-invasive interfaces. Necessary for NIV protocol implementation [30] [26]. |
| Esophageal Balloon Catheter System | The gold standard for directly measuring inspiratory effort and work of breathing via esophageal pressure (Pes) monitoring [30]. |
| Electrical Impedance Tomography (EIT) | Non-invasive, real-time imaging modality for assessing regional lung ventilation and tidal volume distribution [23] [30]. |
| Vibrating Mesh Nebulizer (VMN) | Advanced nebulizer technology that can be integrated into HFNC or NIV circuits for efficient aerosolized drug delivery without interrupting therapy [26]. |
| Transcutaneous CO₂/SpO₂ Monitor | Provides non-invasive, continuous monitoring of gas exchange, crucial for assessing response to therapy [30]. |
Decision Pathways and Experimental Workflows
Flow Rate Selection and Escalation Pathway
Diagram 1: Clinical Decision Pathway for Initial Device and Flow Selection
Experimental Protocol for Physiological Comparison
Diagram 2: Crossover Study Workflow for Physiological Comparison
Flow rate is a fundamental parameter in non-invasive respiratory support, with significant implications for physiological effect and clinical outcome. HFNC flow rates between 40-60 L/min are recommended for hypoxemic respiratory failure, while hypercapnic failure often requires the pressure support afforded by NIV. For the pharmaceutical researcher, these settings create distinct environments for aerosol delivery and drug deposition. The structured protocols and decision pathways provided herein offer a framework for rigorous investigation into optimizing respiratory support parameters, with direct relevance to the development and testing of inhaled therapeutics. Future research should continue to integrate precise physiological measurements with clinical outcomes to further refine these application notes.
Pediatric and Infant-Specific Flow Rate Protocols
In the targeted delivery of inhaled pharmaceuticals to pediatric and infant populations, nebulizing gas flow rate stands as a critical parameter governing therapeutic efficacy. Optimization of this parameter is essential for overcoming the unique physiological and anatomical challenges presented by this patient demographic, including smaller airways, higher respiratory rates, and lower tidal volumes. The primary advantage of nebulized medication administration is that it treats the lung directly, avoiding systemic effects; however, lung deposition of the nebulized medication represents a relatively low fraction of the total dose, making efficient delivery paramount [31]. This document establishes application notes and experimental protocols for researchers and drug development professionals focused on enhancing drug delivery efficiency through precise flow rate control, with the goal of developing personalized atomization inhalation treatment plans tailored to pediatric patients [2].
Fundamental Principles of Pediatric Aerosol Delivery
Physiological Considerations by Age Group
Pediatric patients are not a homogenous group; their respiratory physiology evolves significantly from infancy through adolescence, directly impacting aerosol deposition patterns. Key physiological parameters influencing flow rate optimization are summarized in Table 1.
Table 1: Age-Based Physiological Parameters Relevant to Aerosol Delivery
| Age Group | Typical Tidal Volume (mL) | Typical Respiratory Rate (breaths/min) | Typical Inspiratory Flow (L/min) | Key Physiological Considerations |
|---|---|---|---|---|
| Preterm Neonates | 10-20 | 40-60 | 1.0-2.0 | Obligate nasal breathing, minimal breath-holding capacity, extremely small airways |
| Term Neonates (0-28 days) | 20-30 | 30-50 | 1.5-3.0 | Predominant nasal breathing, rapid respiratory rate, compliant chest wall |
| Infants (1-12 mos) | 30-50 | 25-40 | 2.5-4.5 | Transition to oral breathing, active respiratory patterns, developing coordination |
| Toddlers (1-3 yrs) | 50-100 | 20-35 | 3.5-6.0 | Variable cooperation, short attention span, ability to use mask interfaces |
| School-Age (6-11 yrs) | 100-250 | 16-25 | 6.0-12.0 | Ability to follow instructions, can typically use mouthpieces effectively |
| Adolescents (12-18 yrs) | 250-500 | 12-20 | 10.0-20.0 | Adult-like physiology, capable of complex inhalation maneuvers |
The selection of the correct nebulizer device is critical for successful administration in infants and children. Young children may not use a mouthpiece reliably; if the patient cannot hold a mouthpiece between the lips, a face mask should be used. Forcing the mask on a distressed patient will agitate them and may worsen respiratory distress [31].
Critical Atomization Characteristics
The efficiency of aerosol drug delivery is governed by several interdependent atomization characteristics that are directly influenced by the nebulizing gas flow rate:
- Droplet Size Distribution: The mass median aerodynamic diameter (MMAD) of aerosol droplets determines their deposition depth within the respiratory tract. Smaller droplets (1-5 µm) preferentially deposit in the alveolar region, while larger droplets (>5 µm) tend to deposit in the upper airways. For effective lower respiratory tract deposition, aerosols should have an MMAD of 1-5 µm [2].
- Atomizing Rate: The rate at which the drug solution is converted into aerosol, typically measured in mL/min. This parameter directly impacts treatment duration, which is a critical factor for pediatric patient compliance [2].
- Spray Concentration and Effective Output Dose (EOD): The EOD represents the mass of drug contained in each liter of air jetted by the nebulizer, providing a standardized metric to assess the effective dose inhaled by the patient with each inspiration [2].
- Nebulizer Output Flow Rate: The total flow of aerosol generated by the nebulizer, which must be compatible with the patient's inspiratory flow patterns to minimize drug loss during exhalation.
Quantitative Flow Rate and Atomization Data
Experimental Data on Flow Rate Parameters
Recent investigations have systematically quantified the relationship between supply gas pressure, resultant flow rates, and atomization characteristics in medical air-compression nebulizers. These relationships are fundamental to protocol development.
Table 2: Experimentally Measured Flow Parameters vs. Supply Pressure and Nozzle Diameter
| Supply Gas Pressure (kPa) | Nozzle Orifice Diameter (mm) | Supply Gas Flow Rate (L/min) | Jet Gas Flow Rate (L/min) | Resultant Droplet Size Dv90 (µm) |
|---|---|---|---|---|
| 50 | 0.4 | 2.48 | 14.28 | 7.09 |
| 50 | 0.6 | 5.85 | 22.15 | 8.92 |
| 50 | 0.8 | 8.41 | 29.64 | 9.33 |
| 100 | 0.4 | 6.95 | 25.31 | 7.65 |
| 100 | 0.6 | 10.24 | 31.08 | 7.21 |
| 100 | 0.8 | 12.88 | 35.42 | 7.54 |
| 150 | 0.4 | 11.02 | 33.74 | 8.47 |
| 150 | 0.6 | 13.56 | 37.15 | 6.58 |
| 150 | 0.8 | 16.02 | 41.38 | 6.58 |
Key findings from this data indicate that supply gas pressure significantly influences the atomization characteristics of air-compression nebulizers. With increasing supply gas pressure and nozzle orifice diameter, both the supply gas flow rate and jet gas flow rate increase substantially. The relationship between pressure and droplet size is complex, with the nebulizer with 0.8 mm orifice diameter showing a 29.5% decrease in Dv90 when pressure increased from 50 to 150 kPa, indicating a clear advantage in reducing the proportion of large droplets at higher pressures [2].
Research Reagent Solutions and Essential Materials
Table 3: Key Research Materials for Pediatric Flow Rate Studies
| Item | Function/Application in Research |
|---|---|
| Medical Air-Compression Nebulizers | Core device for aerosol generation; available with various nozzle orifice diameters (e.g., 0.4, 0.6, 0.8 mm) to study differential atomization [2] |
| Laser Particle Size Analyzer (LPSA) | Critical for measuring droplet size distribution (Dv10, Dv50, Dv90) to evaluate aerosol respirability [2] |
| Electronic Balance (e.g., LICHEN-FA324TC) | Precision measurement of atomizing rate by monitoring mass loss over time during nebulization [2] |
| Gas Flow Meter (e.g., SIARGO-MF5700) | Direct measurement of supply gas flow rate under various pressure conditions [2] |
| Hot-Wire Anemometer (e.g., HTI-HT9829) | Characterization of jet gas flow velocity at the nozzle outlet [2] |
| Age-Appropriated Airway Models | Anatomically accurate physical or computational models of pediatric airways for deposition studies |
| Simulated Lung Fluid | Physiologically relevant fluid media for in vitro dissolution and deposition testing |
| Pediatric Formulation Placebos | Drug-free formulations matching the physicochemical properties of active products for method development |
Experimental Protocols for Flow Rate Optimization
Protocol: Comprehensive Atomization Characterization
Objective: To systematically evaluate the influence of nebulizing gas flow rate on critical atomization characteristics using controlled laboratory methodology.
Materials Preparation:
- Medical air-compression nebulizer system with adjustable pressure regulator
- Laser Particle Size Analyzer (LPSA) calibrated for 0.1-100 µm range
- Precision electronic balance (0.1 mg sensitivity)
- Gas flow meter and hot-wire anemometer
- Data acquisition system for temporal recording
- Test formulation (appropriate placebo or active pharmaceutical ingredient)
Methodology:
- Setup Configuration: Assemble the experimental apparatus as shown in Figure 1, ensuring all instruments are calibrated and properly connected.
- Pressure-Flow Calibration: For each nebulizer nozzle diameter (0.4, 0.6, 0.8 mm), incrementally increase supply gas pressure from 50 to 150 kPa in 25 kPa increments. Record the corresponding supply gas flow rate and jet gas flow rate at each pressure setting.
- Droplet Size Analysis: Place the LPSA sampling inlet at a standardized distance (e.g., 2 cm) from the nebulizer outlet. For each pressure condition, collect droplet size distribution data (Dv10, Dv50, Dv90) over a minimum 30-second sampling period with triplicate measurements.
- Atomizing Rate Determination: Weigh the nebulizer unit with a standardized fill volume (e.g., 3 mL) of test formulation before and after a precisely timed 2-minute nebulization period. Calculate atomizing rate in mL/min.
- Spray Concentration Assessment: Utilizing the LPSA light-blocking rate data, calculate the spray concentration in particles/L of air. Derive the Effective Output Dose (EOD) for active formulations.
- Data Analysis: Plot relationships between supply gas pressure, flow rates, and atomization characteristics. Perform statistical analysis to identify significant differences between parameter combinations.
Protocol: Age-Specific Aerosol Delivery Efficiency
Objective: To evaluate nebulizer output efficiency matched to pediatric age-specific breathing patterns using realistic in vitro models.
Materials Preparation:
- Breathing simulator capable of reproducing age-specific tidal volumes, waveforms, and I:E ratios
- Anatomically accurate pediatric airway models (neonatal, infant, toddler, child)
- Nephelometer or chemical assay for quantifying deposited drug
- Nebulizer systems with adjustable flow rates
- Validated analytical method (e.g., HPLC-UV) for drug quantification
Methodology:
- Breathing Pattern Programming: Program the breathing simulator with age-appropriate parameters (Table 1) for target pediatric populations.
- Experimental Setup: Connect the appropriate airway model to the breathing simulator, placing a filter at the "tracheal" position to collect deposited aerosol.
- Nebulizer Operation: Operate the nebulizer at predetermined flow rates (e.g., 4, 6, 8 L/min for infants; 6, 8, 10 L/min for children) while the breathing simulator operates.
- Sample Collection: After a standardized number of breaths, carefully remove the deposition filter and any filters placed at the simulator "exhaust." Rinse the airway model with appropriate solvent to collect wall-deposited drug.
- Drug Quantification: Analyze all samples using the validated analytical method to determine total emitted dose, respirable dose, and regional deposition patterns.
- Efficiency Calculation: Calculate lung deposition efficiency as percentage of nominal dose. Correlate efficiency with flow rate and breathing parameters.
Clinical Application and Device Selection
Translating optimized flow parameters to clinical practice requires careful consideration of age-appropriate device selection. Clinical guidelines emphasize that pressurized metered-dose inhalers (pMDIs) with spacers represent the first-line option in most pediatric age groups, while nebulizers are reserved for specific clinical situations [32].
Table 4: Age-Based Device and Flow Rate Recommendations
| Age Group | Preferred Device | Alternative Devices | Recommended Flow Rate Range | Clinical Considerations |
|---|---|---|---|---|
| < 3 years | pMDI with spacer and mask | Nebulizer with mask | 4-6 L/min (if using nebulizer) | Ensure mask seal without forcing; involve family to calm patient [31] [32] |
| 3-4 years | pMDI with spacer (may transition to no mask) | Nebulizer for acute episodes | 5-7 L/min (if using nebulizer) | Monitor for tachycardia during treatment [31] [32] |
| 5-7 years | pMDI with spacer (no mask) | Dry powder device (possible) | 6-8 L/min (if using nebulizer) | Assess ability to use mouthpiece effectively [31] [32] |
| ≥ 8 years | pMDI with spacer or DPI | Nebulizer for severe exacerbations | 6-10 L/min (if using nebulizer) | Standard flow rates typically appropriate [31] |
For nebulizer treatments, the flow rate is typically set between 6 and 10 L/min as indicated on the device label. The correct flow rate ensures that a sufficient mist forms to indicate nebulization is occurring [31]. During treatment, patients should be monitored for tachycardia, which is a side effect of bronchodilators that can lead to hemodynamic instability in small infants and children [31].
Precise optimization of nebulizing gas flow rates represents a critical factor in enhancing the efficacy and safety of inhaled pharmaceutical delivery to pediatric populations. The protocols and data presented herein provide a systematic framework for researchers to establish evidence-based flow rate parameters that account for the complex interplay between device performance characteristics and pediatric physiological factors. Future research directions should focus on developing intelligent nebulization systems capable of real-time flow rate adjustment based on individual patient breathing patterns, ultimately advancing toward truly personalized pediatric aerosol medicine.
Synergizing Flow Rate with Inhalation Waveforms and Synchronization
The efficacy of nebulized pharmaceutical aerosols is not solely governed by the formulation but is profoundly influenced by the interplay of device operating parameters and patient-specific inhalation patterns. Optimizing nebulizing gas flow rate in synergy with inhalation waveforms and active synchronization represents a frontier in pulmonary drug delivery research, aiming to maximize lung deposition while minimizing extrapulmonary loss. This approach moves beyond static device operation to a dynamic, intelligent delivery system that adapts to the patient's breathing, ensuring the aerosol bolus is delivered during the most favorable phase of inspiration. This document outlines the core principles, quantitative relationships, and standardized experimental protocols for advancing research in this field, providing a framework for developing next-generation nebulization systems.
Core Principles and Key Data
The optimization of aerosol delivery hinges on controlling three interconnected elements: the nebulizer's operating flow rate, the patient's inhalation waveform, and the temporal synchronization of aerosol generation with inspiration.
The Critical Role of Nebulizing Gas Flow Rate
The gas flow rate is a primary determinant of aerosol generation, influencing key characteristics such as droplet size distribution, atomization rate, and effective output dose (EOD).
Table 1: Impact of Supply Gas Pressure on Nebulizer Performance (Air-Compression Nebulizers) [2]
| Supply Gas Pressure (kPa) | Nozzle Orifice Diameter (mm) | Sauter Mean Diameter (SMD, D32) (µm) | Atomizing Rate (mL/min) | Effective Output Dose (EOD) |
|---|---|---|---|---|
| 50 | 0.4 | 7.09 (Dv90) | Low | Low |
| 50 | 0.6 | Higher than at 0.8 mm | Medium | Medium |
| 50 | 0.8 | Lower than at 0.6 mm | Medium | Medium |
| 150 | 0.4 | 8.47 (Dv90) | Increased | Increased |
| 150 | 0.6 | Decreased | Increased | Increased |
| 150 | 0.8 | Decreased by 29.5% (Dv90) | High | High |
Data indicates that increasing supply gas pressure generally enhances the atomizing rate and EOD, which is the drug mass per liter of air inhaled by the patient [2]. The effect on droplet size is more complex and interacts with nozzle design; while smaller orifices can produce finer droplets at lower pressures, they may exhibit anomalous droplet growth at higher pressures. Conversely, larger orifices (e.g., 0.8 mm) show a significant reduction in large droplets (as measured by Dv90) at elevated pressures, promoting a more uniform and respirable aerosol cloud [2]. Furthermore, research on jet nebulizers demonstrates that increasing gas flow rates can linearly increase the portion of the spray mass in respirable droplets (e.g., ≤5 µm) [33].
Synchronization with Inhalation Waveforms
Continuous nebulization is highly inefficient, as a significant portion of the aerosol is generated during exhalation and is subsequently wasted. Inspiration-synchronized nebulization addresses this by generating aerosol only during the inspiratory phase.
Table 2: Synchronized vs. Continuous Nebulization in Mechanical Ventilation [34]
| Parameter | Ventilation Mode | VMNcont (Aerogen Solo) | VMNsyn (M-Neb flow+) | Comparison |
|---|---|---|---|---|
| Drug Deposition Rate | VC-CMV | Baseline | Comparable | No significant difference |
| PC-CMV | Baseline | 10.9% Lower | Significant reduction with synchronization | |
| Nebulization Time | VC-CMV | Baseline | 7.5x Longer | Dramatically prolonged |
| PC-CMV | Baseline | 4.2x Longer | Significantly prolonged | |
| Recommended Use | VC-CMV | - | Most Suitable | Optimal for prolonged inhalative administration |
An in vitro study comparing an inspiration-synchronized vibrating mesh nebulizer (VMNsyn) with a continuous VMN (VMNcont) found that synchronization achieved a similar deposition rate during volume-controlled ventilation while drastically extending nebulization time by a factor of 7.5 [34]. This makes it ideal for prolonged administration of drugs with short half-lives, such as iloprost. The deposition rate was slightly lower with synchronization in pressure-controlled mode, highlighting that the efficacy of synchronization can be affected by the ventilation waveform [34].
The Interplay with Inhalation Flow Rate
During high-flow nasal cannula (HFNC) therapy, the relationship between the set gas flow rate (GF) and the patient's inspiratory flow rate (IF) is critical. The GF:IF ratio determines aerosol delivery efficiency.
- GF:IF < 1: The inhaled dose is higher and more consistent. Placing the nebulizer (preferably a VMN) upstream of the humidifier is optimal for continuous nebulization [10] [35].
- GF:IF > 1: The inhaled dose decreases significantly due to aerosol dilution [10].
- Synchronization Advantage: When GF is set below 50% of the patient's IF, synchronized aerosol delivery can generate 30% more inhaled dose compared to continuous nebulization, regardless of the patient's breathing pattern (quiet or distressed) [10].
Experimental Protocols
Protocol 1: Quantifying Flow Rate Impact on Atomization
Objective: To characterize the effect of nebulizer gas flow rate on critical aerosol performance parameters.
Materials:
- Medical air-compression nebulizer unit
- Gas flow meter and pressure regulator
- Electronic balance (±0.0001 g)
- Laser particle size analyzer (LPSA)
- High-precision timer
- Model liquid (e.g., distilled water, saline, drug solution)
Methodology: [2]
- Setup: Connect the nebulizer to the gas source via the pressure regulator and flow meter.
- Gravimetric Analysis: Weigh the nebulizer cup empty (
w_empty). Fill with a known volume of model liquid and reweigh (w_filled). - Systematic Testing: For a range of supply gas pressures (e.g., 50, 100, 150 kPa):
a. Activate the nebulizer and start the timer.
b. Measure the gas flow rate using the flow meter.
c. Operate the nebulizer for a fixed duration (e.g., 1 minute), then weigh again (
w_end) to calculate the atomizing rate: (w_filled - w_end) / time. d. To measure droplet size distribution, direct the aerosol output into the laser beam of the LPSA. - Data Calculation: Calculate the Effective Output Dose (EOD) as the mass of drug delivered per liter of air jetted, derived from the atomizing rate and drug concentration.
Protocol 2: Evaluating Synchronization with Simulated Breathing
Objective: To compare the deposition efficiency and nebulization time of synchronized versus continuous aerosol delivery under simulated breathing conditions.
Materials:
- Breathing simulator or test lung
- Critical care ventilator or programmable breathing simulator
- Synchronized vibrating mesh nebulizer (VMNsyn) and continuous nebulizer (VMNcont)
- Absolute filter housing placed between the endotracheal tube and test lung
- Drug assay equipment (e.g., LC-MS/MS, UV-Vis spectrophotometer)
- High-precision scale
Methodology: [34]
- Circuit Setup: Assemble the ventilator circuit with the test lung. Place an absolute filter in-line between the endotracheal tube and the test lung, using a bypass with one-way valves to protect the filter during expiration.
- Nebulizer Positioning: Place the VMNsyn between the ETT and the Y-piece adapter. Place the VMNcont 15 cm upstream on the inspiratory limb.
- Ventilator Settings: Set the ventilator to both VC-CMV and PC-CMV modes with typical adult parameters (e.g., tidal volume 500 mL, frequency 15/min, PEEP 5 cm H₂O).
- Drug Nebulization: a. Fill the nebulizer chamber with a known mass of drug (e.g., iloprost in saline). b. For the VMNcont, run until sputtering (no aerosol produced). For the VMNsyn, ensure the synchronization feedback line is connected and run until sputtering. c. Record the total nebulization time.
- Sample Analysis: Carefully extract the drug from the absolute filter using a validated method (e.g., solvent extraction). Quantify the deposited drug mass (
m_filter) using analytical equipment.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function & Application |
|---|---|
| Vibrating Mesh Nebulizer (VMN) | Generates aerosol with a low residual volume and can be designed for continuous or inspiration-synchronized operation. |
| High-Flow Nasal Cannula (HFNC) System | Provides heated, humidified gas at high flows; a complex in vitro model for testing aerosol delivery under realistic clinical conditions. |
| Laser Particle Size Analyzer (LPSA) | Measures the droplet size distribution of the generated aerosol, a critical parameter for predicting lung deposition. |
| Breathing Simulator | Replicates human breathing patterns (e.g., quiet vs. distressed) to assess device performance under dynamic conditions. |
| Absolute Filter | Captures the aerosol dose delivered in an in vitro setup, allowing for quantitative analysis of deposition efficiency. |
| Computational Fluid Dynamics (CFD) Software | Enables in-silico modeling and visualization of fluid flow and aerosol deposition within devices and airways, guiding optimized design. |
Conceptual Workflow and Signaling Pathways
The following diagram illustrates the logical sequence and decision points for optimizing a nebulizer system through flow rate control and synchronization.
Optimization Workflow for Nebulizer Systems
This workflow outlines a systematic approach for researchers. It begins with defining the drug and target, followed by empirical characterization of the nebulizer's performance across a range of flow rates and simultaneous analysis of the intended patient's inhalation waveform. The core decision point involves determining the optimal Gas Flow-to-Inspiratory Flow (GF:IF) ratio, which guides the choice between implementing inspiration-synchronized or continuous delivery. System performance is then assessed against key metrics (Deposition, EOD, Nebulization Time), creating a feedback loop for further parameter refinement until an optimized system is achieved.
Overcoming Delivery Challenges: Advanced Flow Rate Optimization and Component Design
Identifying and Mitigating High Depositional Loss Zones
In the targeted delivery of pharmaceuticals via nebulization, depositional loss refers to the portion of an aerosolized drug that fails to reach the intended site of action within the respiratory tract. These losses occur in specific high-loss zones, critically reducing the therapeutic dose delivered to the patient and compromising treatment efficacy. For researchers and drug development professionals, understanding and mitigating these losses is paramount to optimizing drug formulations and delivery systems. This process is intrinsically linked to the optimization of nebulizing gas flow rates, a key operational parameter that directly influences fundamental aerosol characteristics such as droplet size distribution, velocity, and ultimately, deposition patterns within the complex geometry of the airways [2]. This application note provides a structured experimental framework to identify these critical zones and outlines effective protocols to mitigate losses, thereby enhancing the efficiency of pulmonary drug delivery.
Mechanisms and Impact of Depositional Loss
Depositional losses are governed by a combination of physical mechanisms and are significantly influenced by the nebulizer's operating parameters.
Primary Mechanisms of Aerosol Loss
- Impaction: This is the dominant mechanism for larger droplets and in areas with high airflow velocity and directional changes, such as the oropharynx and the first few bronchial branches. The inertia of the droplets prevents them from following the airstream path, causing them to impact and deposit on the mucosal surfaces. Higher gas flow rates can increase droplet momentum, exacerbating losses in these proximal zones [2] [10].
- Gravitational Settling (Sedimentation): This affects smaller droplets over time and is a primary deposition mechanism in the lower airways and alveoli, where airflow rates are low. While essential for therapeutic effect, excessive sedimentation in the delivery apparatus or central airways represents a loss.
- Evaporation and Hygroscopic Growth: The heated and humidified environment of the respiratory tract, particularly when using devices like a High-Flow Nasal Cannula (HFNC), can cause droplet size to change. Evaporation can reduce droplet size, potentially leading to exhalation losses, while hygroscopic growth can increase droplet size, shifting deposition to more proximal zones than intended [10].
Impact of Gas Flow Rate on Loss Zones
The nebulizing gas flow rate is a critical determinant of where and how these loss mechanisms manifest. As demonstrated in a 2025 study, increasing the supply gas pressure (and thus flow rate) in air-compression nebulizers leads to complex changes in atomization characteristics [2]:
- Increased Flow Rate: Generally produces a higher atomizing rate and spray volume.
- Variable Effect on Droplet Size: The effect on droplet size (
Dv90) depends on the nozzle orifice diameter. For smaller orifices (e.g., 0.4 mm), droplet size may anomalously increase with pressure, potentially increasing impaction losses. For larger orifices (e.g., 0.8 mm), droplet size can decrease significantly (e.g.,Dv90reduced by 29.5% when pressure increased from 50 to 150 kPa), promoting deeper lung penetration [2]. - Effective Output Dose (EOD): This metric, defined as the mass of drug per liter of air jetted, increases with supply gas pressure, suggesting a higher potential dose per inspiration, though a greater proportion may be lost in high-deposition zones if the droplet size is not optimized [2].
Table 1: Impact of Supply Gas Pressure on Key Atomization Characteristics [2]
| Parameter | Impact of Increasing Supply Gas Pressure | Correlation with Nozzle Orifice Diameter |
|---|---|---|
| Supply Gas Flow Rate | Increases (2.48 to 16.02 L/min) | Increases with diameter |
| Jet Gas Flow Rate | Increases (14.28 to 41.38 L/min) | Increases with diameter |
| Atomizing Rate | Progressive increase | Progressive increase with diameter |
| Droplet Size (Dv90) | Variable: increases for 0.4mm orifice; decreases for 0.6/0.8mm orifices | Decreases with larger orifices at high pressure |
| Effective Output Dose (EOD) | Increases | No significant correlation |
Experimental Characterization of Depositional Loss
A multi-faceted approach, combining in vitro and in silico methods, is required to fully characterize depositional loss zones.
Protocol: Droplet Size Distribution Analysis
Objective: To measure the droplet size distribution generated by a nebulizer under different gas flow rates, as this is the primary factor influencing deposition via impaction and sedimentation.
Materials:
- Laser Particle Size Analyzer (LPSA) [2]
- Air-compression nebulizer with adjustable supply gas pressure
- Gas flow meter (e.g., SIARGO-MF5700) [2]
- Electronic balance (e.g., LICHEN-FA324TC) for atomizing rate measurement [2]
- Model liquid (e.g., distilled water, saline, or drug formulation)
Method:
- Setup: Place the nebulizer, filled with a standard volume of model liquid, at a fixed distance and alignment from the LPSA laser beam.
- Parameter Sweep: Conduct a series of tests across a range of supply gas pressures (e.g., 50 kPa to 150 kPa) [2].
- Data Collection: For each pressure setting:
- Record the supply gas flow rate using the flow meter.
- Measure the atomizing rate by weighing the nebulizer before and after a fixed period of operation.
- Use the LPSA to record the droplet size distribution, specifically noting percentiles such as
Dv10,Dv50(median), andDv90[2].
- Analysis: Plot the relationship between gas flow rate and key droplet size metrics. A stable or decreasing
Dv90with increasing flow is often desirable to minimize proximal losses.
Protocol: In Vitro Airway Model Deposition
Objective: To visualize and quantify spatial deposition in a simulated respiratory tract.
Materials:
- Anatomical airway model (plastic or silicone)
- Nebulizer with characterized output
- Colored or fluorescent tracer (e.g., methylene blue, sodium fluorescein) added to the model liquid [36]
- High-efficiency imaging system (camera or scanner)
- Image analysis software
Method:
- Preparation: Add a known concentration of tracer to the nebulizer reservoir.
- Aerosol Collection: Direct the nebulizer output into the inlet of the anatomical model. Run the nebulizer for a standardized duration or until a specific volume is aerosolized.
- Deposition Capture: Dissect the airway model into segments representing different zones (oropharyngeal, bronchial, alveolar).
- Quantification: For each segment:
- If using a colored tracer, elute the deposited dye and measure its concentration spectrophotometrically.
- If using a fluorescent tracer, capture images under consistent UV light and quantify the fluorescence intensity per zone using image analysis software [36].
- Data Normalization: Express deposition in each zone as a percentage of the total recovered dose to identify the primary loss zones.
Protocol: In Silico Deposition Simulation
Objective: To predict deposition in patient-specific airways using computational fluid dynamics (CFD).
Method: This protocol is based on advanced deposition simulations, including two- and four-way coupling to account for particle-particle interactions, which are critical for simulating realistic dosage concentrations [37].
- Model Generation: Import a 3D reconstruction of the human airways from medical CT or MRI scans into CFD software.
- Mesh Generation: Create a computational mesh of the airway geometry.
- Physics Setup:
- Define the continuous phase (air) with appropriate inlet flow conditions simulating inhalation.
- Define the discrete phase (aerosol droplets) with properties (size distribution, density, velocity) matching your experimental characterization.
- Select an appropriate multiphase coupling model. Two-way coupling accounts for the effect of the fluid on the particles, while four-way coupling also includes particle-particle interactions (coagulation, collision) and is necessary for high-concentration aerosols [37].
- Simulation and Analysis: Run the simulation to track particle trajectories. Post-process the results to quantify regional deposition fractions and visualize spatial deposition patterns.
The following workflow diagram illustrates the integrated experimental and computational approach to characterizing depositional loss:
Diagram 1: Deposition Characterization Workflow
Mitigation Strategies and Protocols
Once high-loss zones are identified, targeted strategies can be implemented to mitigate them.
Optimizing Nebulizing Gas Flow Rate
Protocol: Determining Patient-Specific Flow Rate Rationale: A "one-size-fits-all" gas flow rate is suboptimal due to varying patient respiratory characteristics [2] [10].
Method:
- Characterize Nebulizer: First, establish the relationship between your nebulizer's gas flow rate and its output
Dv90using Protocol 3.1. - Define Target Deposition Zone: Select the desired droplet size profile based on the target lung region (e.g., smaller droplets <5 µm for alveolar region).
- Match to Inspiratory Flow: For patients using HFNC, set the nebulizing gas flow rate below the patient's inspiratory flow (IF). Studies show the aerosol delivery is higher when gas flow is set below the patient's IF, with a plateau effect at approximately 50% of IF [10]. This reduces the dilution of the aerosol bolus and subsequent exhalation loss.
- Clinical Titration: For sensitive populations, start with a lower flow rate and titrate upwards, monitoring for therapeutic effect and adverse events like airway irritation from high-velocity impactors.
Device and Formulation Adjustments
- Nebulizer Type and Placement: When integrating with HFNC, use a vibrating mesh nebulizer (VMN) and place it upstream from the humidifier chamber. This position has been identified as the most efficient for aerosol delivery, likely because it allows the aerosol to be carried by the fully humidified gas stream, minimizing evaporation and loss in the circuit [10].
- Synchronized Nebulization: Implement inspiration-synchronized nebulization. In-vitro data indicates that synchronized delivery can generate a 30% higher inhaled dose compared to continuous nebulization, as it avoids aerosol generation during the exhalation phase when 100% of the dose is lost [10].
- Formulation Engineering: Add excipients like mannitol, sorbitol, or trehalose to biological formulations (e.g., monoclonal antibodies). These excipients can stabilize the drug and may help prevent macrophage engulfment, a form of cellular-level "loss" in the deep lung [38].
Table 2: Mitigation Strategies for High Depositional Loss Zones
| Loss Zone / Mechanism | Mitigation Strategy | Experimental/Clinical Evidence |
|---|---|---|
| Proximal Airways (Impaction) | Optimize gas flow to reduce droplet size (Dv90); Use larger nozzle orifices at higher pressure [2]. |
Study showed 29.5% reduction in Dv90 for 0.8mm orifice when pressure increased from 50 to 150 kPa [2]. |
| Delivery Circuit (Evaporation/Impaction) | Use VMN placed upstream of humidifier in HFNC circuits [10]. | In-vitro study identified this position as most efficient for aerosol delivery [10]. |
| Exhalation Loss | Implement inspiration-synchronized nebulization [10]. | In-vitro data showed 30% higher inhaled dose with synchronized vs. continuous nebulization [10]. |
| Macrophage Clearance | Formulate with excipients like mannitol or trehalose [38]. | Excipients prevent aggregation and may reduce macrophage engulfment of biologics [38]. |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Brief Explanation |
|---|---|
| Laser Particle Size Analyzer (LPSA) | Measures the droplet size distribution (e.g., Dv10, Dv50, Dv90) of the generated aerosol, which is the fundamental property governing deposition [2]. |
| Anatomical Airway Model | A physical model of the human respiratory tract used for in-vitro testing to visualize and quantify spatial deposition patterns of aerosols. |
| Computational Fluid Dynamics (CFD) Software | Enables in-silico modeling of aerosol deposition in patient-specific airway geometries, allowing for simulation of complex physics like 4-way coupling [37]. |
| Vibrating Mesh Nebulizer (VMN) | A nebulizer technology known for high efficiency and minimal dead volume; recommended for integration with high-flow oxygen systems to reduce circuit losses [10]. |
| Stabilizing Excipients (e.g., Trehalose) | Protect biological drugs (e.g., mAbs) from denaturation and aggregation during the stress of nebulization, ensuring dosage accuracy and stability [38]. |
The following diagram summarizes the decision-making process for selecting the appropriate mitigation strategy based on the identified primary loss zone and mechanism:
Diagram 2: Mitigation Strategy Decision Map
Streamlined Component Design to Minimize Drug Loss
In pharmaceutical aerosol research, drug loss during nebulization represents a critical challenge, compromising therapeutic efficacy and economic viability. A primary strategy to mitigate this lies in the optimization of nebulizing gas flow rates and the implementation of streamlined component design. Inefficient traditional nebulizers can waste over 50% of the loaded drug dose [39], with only approximately 10% of the nominal dose typically deposited in the lungs [40]. This application note provides detailed protocols and data, framed within a broader thesis on gas flow rate optimization, to guide researchers in designing nebulizer systems that maximize drug delivery efficiency through minimized retention and depositional losses.
Background and Significance
Nebulizer function is governed by core fluid dynamics principles. Jet nebulizers operate on the Venturi effect, where compressed gas passing through a narrow orifice creates a region of low pressure, drawing liquid medication from a reservoir into the gas stream to be shattered into droplets [41] [39]. The resulting aerosol droplet size distribution is paramount, with droplets smaller than 5 µm being essential for reaching and depositing medication in the lower airways and alveoli [41].
Drug loss occurs through several mechanisms:
- Device Retention: Medication left in the nebulizer reservoir (dead volume) after treatment [39].
- Connection Losses: Deposition of aerosol on internal components, connectors, and valves due to impaction in turbulent flow regions [40].
- Environmental Release: Aerosol released into the environment during patient exhalation in continuously operating systems [39].
Streamlined component design addresses these losses by minimizing internal obstructions, using smooth flow paths, and optimizing geometries to reduce turbulent flow and impaction, thereby ensuring a greater proportion of the generated aerosol is available for inhalation [40].
Quantitative Data on Component Design and Performance
Table 1: Impact of Structural Modifications on Droplet Size Distribution
| Design Parameter | Baseline Performance (Sub-5 µm droplets) | Optimized Performance (Sub-5 µm droplets) | Experimental Conditions |
|---|---|---|---|
| Standard Crushing Baffle | 54.60% | - | Gas Flow Rate: 15 m/s [41] |
| Improved Symmetrical Crushing Baffle | - | 59.25% (+4.65%) | Gas Flow Rate: 15 m/s [41] |
| Gas Flow Rate | 59.25% (at ~15 m/s) | >59.25% (with further optimized flow) | Modified Baffle Structure [41] |
Table 2: Comparative Lung Delivery Efficiency of Nebulizer Technologies
| Nebulizer Technology | Typical Lung Delivery Efficiency | Key Factors Influencing Drug Loss |
|---|---|---|
| Traditional Jet Nebulizer | ~10% of loaded dose [39] | High dead volume, continuous operation, turbulent connections [40] [39] |
| Vibrating Mesh Nebulizer (Aerogen Ultra) | Up to 34% of loaded dose [40] | Reduced residual volume, more monodisperse aerosol [40] |
| Adaptive Aerosol Delivery (Halolite) | ~60% of emitted dose [39] | Breath-actuation eliminates exhaled loss [39] |
| Metered-Dose Liquid Inhaler (AERx, Respimat) | 30-75% of emitted dose [39] | Fine aerosol generation, low-velocity spray [39] |
Experimental Protocols
Protocol: Optimizing Gas Flow Rate and Baffle Geometry for Droplet Size
Objective: To systematically investigate the effects of nebulizing gas flow rate and crushing baffle geometry on the resulting aerosol droplet size distribution.
Materials & Reagents:
- Medical air-compression nebulizer (customizable test unit) [41]
- Compressed gas source with precise flow controller (0-30 m/s capability)
- Laser diffraction particle size analyzer (e.g., Malvern Spraytec) [41]
- Test solution: 0.9% saline or drug formulation (e.g., 0.5 mg/ml Albuterol sulfate)
- Finite Element Analysis software (e.g., ANSYS Fluent) [41]
Methodology:
- Computational Fluid Dynamics (CFD) Modeling:
- Create a 2D or 3D geometry of the nebulizer's internal flow path, focusing on the nozzle, liquid channel, and baffle region [41].
- Define boundary conditions: Inlet (gas flow rate), Outlet (pressure), and Walls (no-slip condition) [41].
- Simulate the multiphase flow (air and liquid) using a model such as the conservative level-set method to track the liquid atomization [41].
- Run a parametric study, varying the gas inlet velocity (e.g., 10, 15, 20, 25 m/s) and the geometrical parameters of the crushing baffle (e.g., stand-off distance, angle, surface curvature).
- Extract data on the simulated droplet size distribution (DSD) at the mist outlet for each parameter set.
- Experimental Validation:
- Manufacture prototypical crushing baffles based on the most promising CFD results, ensuring symmetrical structures [41].
- Assemble the nebulizer with the first prototype baffle. Fill the reservoir with a defined volume of test solution.
- Connect the nebulizer to the compressed gas source and set the flow rate to the first test condition.
- Activate the nebulizer and the laser diffraction analyzer. Measure the DSD of the emitted aerosol over a minimum of 3 separate runs.
- Record the volume percentage of droplets below 5 µm.
- Repeat the measurement for each gas flow rate and with each prototype baffle geometry.
- Statistically compare the experimental data with the CFD predictions to validate the model.
Data Analysis:
- Plot the proportion of sub-5 µm droplets against gas flow rate for each baffle design.
- Identify the flow rate that maximizes the fine droplet fraction for a given design.
- Use Analysis of Variance to determine the statistical significance of design and flow rate changes on the output.
Protocol: In-Vitro Assessment of Total Drug Delivery Efficiency
Objective: To quantify depositional losses within a nebulizer system and measure the delivered dose under simulated breathing conditions.
Materials & Reagents:
- Test nebulizer system (jet or mesh)
- A breathing simulator with programmable profiles (adult, pediatric)
- An absolute filter (to capture the "lung" dose)
- A validated inhalation test rig, including a realistic upper airway model
- HPLC system with validated assay for the drug product
- Test solution: Drug product at target concentration
Methodology:
- System Setup:
- Assemble the nebulizer system according to clinical use, including all connectors, tubing, and a patient interface (mouthpiece or mask).
- Place an absolute filter at the position of the "trachea" in the test rig, downstream of the upper airway model [40].
- Connect the output of the airway model to the breathing simulator.
- Dose Collection and Analysis:
- Pipette a precise volume and known concentration of the drug solution into the nebulizer reservoir.
- Activate the nebulizer and the breathing simulator simultaneously. Use a standard adult breathing pattern unless otherwise specified.
- Run the test until the nebulizer begins to sputter, indicating the end of nebulization.
- Carefully disassemble the entire system and recover the drug from each critical component:
- Nebulizer reservoir and internal surfaces (retained dose)
- Internal connectors, valves, and tubing (component loss)
- The interior of the upper airway model (extrathoracic loss)
- The absolute filter (lung dose)
- Rinse each component with an appropriate solvent and dilute to a known volume.
- Analyze all samples using HPLC to determine the drug mass in each fraction.
Data Analysis:
- Calculate the mass balance (sum of all recovered drug masses should be ~100% of initial load).
- Report the lung delivery efficiency as (Mass on Filter / Initial Loaded Dose) * 100%.
- Report the total system retention/loss as (Mass in Nebulizer & Connectors / Initial Loaded Dose) * 100%.
- Compare the performance of different component designs (e.g., standard vs. streamlined connectors) using these metrics.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for Nebulizer Performance Characterization
| Item | Function/Application |
|---|---|
| Laser Diffraction Particle Size Analyzer | Measures the aerodynamic droplet size distribution of the emitted aerosol, critical for predicting lung deposition [41]. |
| Computational Fluid Dynamics (CFD) Software | Uses finite element analysis to model internal flow fields, predict droplet formation, and optimize component geometry computationally before prototyping [40] [41]. |
| Breathing Simulator | Provides physiologically relevant inhalation profiles for in-vitro testing, allowing for the assessment of delivery efficiency under realistic conditions [40]. |
| Realistic Upper Airway Model | A physical replica of the human mouth-throat geometry, used in test rigs to measure extrathoracic depositional losses accurately [40]. |
| High-Performance Liquid Chromatography | Quantifies the precise mass of the active pharmaceutical ingredient recovered from different parts of the test system, enabling calculation of delivery efficiency [38]. |
| Vibrating Mesh Nebulizer (e.g., Aerogen) | A reference technology known for high efficiency; used for comparative studies against new jet nebulizer designs [40]. |
Workflow and Pathway Visualizations
<75 chars: Nebulizer Component Optimization Workflow
<75 chars: Primary Drug Loss Pathways in Nebulization
The Role of Flow Rate in Reducing Oro-Pharyngeal Deposition
Inhaled pharmacotherapy is a cornerstone for treating respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). The therapeutic effectiveness of inhaled medications is intrinsically linked to the quantity of drug deposited beyond the oropharyngeal region [42]. Oro-pharyngeal deposition represents a significant pharmacological loss, reducing lung availability and potentially causing localized side effects [14]. Multiple factors influence this deposition pattern, including particle aerodynamic properties, airway geometry, and breathing patterns [42]. Among controllable parameters, inhalation flow rate emerges as a critical variable that directly affects aerosol transport dynamics and deposition efficiency through inertial impaction mechanisms [43]. This application note examines the role of flow rate in reducing oropharyngeal deposition and provides structured experimental frameworks for optimizing nebulized drug delivery systems.
Mechanisms of Aerosol Deposition
Primary Deposition Mechanisms in the Respiratory Tract
Understanding deposition mechanisms is fundamental to optimizing flow parameters. The dominant mechanisms governing aerosol particle behavior in the respiratory tract include:
- Inertial Impaction: The primary deposition mechanism for particles >5μm in upper airways where airflow changes direction rapidly [14] [42]. Particles with sufficient momentum cannot follow airflow streamlines and impact airway walls, particularly in the oropharyngeal region with its 90° bend [43].
- Sedimentation: Dominates in smaller airways and alveolar regions where airflow velocity decreases, allowing gravitational settling [42].
- Diffusion: Significant for submicron particles (<0.5μm) due to Brownian motion [14].
- Interception: Relevant for fibrous particles that contact airway surfaces due to their elongated shape [42].
For most pharmaceutical aerosols with mass median aerodynamic diameters (MMAD) between 1-5μm, inertial impaction and sedimentation represent the dominant deposition mechanisms [42].
Flow Rate Influence on Deposition Mechanics
The relationship between flow rate and deposition efficiency follows fundamental fluid dynamics principles. Higher flow rates increase particle momentum, enhancing inertial impaction in the oropharyngeal region [43]. Computational studies demonstrate that at 30 L/min, particles >20μm deposit onto the oropharynx, while particles <12μm navigate the curved geometry to reach lower airways [43]. The Stokes number (Stk), representing the ratio of particle stopping distance to characteristic airway dimension, directly correlates with impaction deposition efficiency:
Stk = (ρp × dp² × U) / (18 × μ × D)
Where ρp is particle density, dp is particle diameter, U is characteristic velocity, μ is air viscosity, and D is airway diameter [43].
Table 1: Dominant Deposition Mechanisms by Airway Region
| Airway Region | Dominant Deposition Mechanism | Particle Size Most Affected | Flow Rate Dependence |
|---|---|---|---|
| Oropharyngeal | Inertial Impaction | >5μm | High positive correlation |
| Central Airways | Impaction & Sedimentation | 1-10μm | Moderate correlation |
| Small Airways & Alveoli | Sedimentation & Diffusion | 0.5-5μm & <0.5μm | Inverse correlation |
Quantitative Effects of Flow Rate on Deposition
Flow Rate and Particle Size Interrelationship
Experimental data reveal a complex interplay between flow rate, particle size, and regional deposition. Increasing flow rate produces higher shear forces, potentially reducing droplet size in nebulizers, but simultaneously increases inertial impaction of larger particles in the oropharynx [2] [44].
Table 2: Effect of Supply Gas Pressure on Nebulizer Output Characteristics
| Supply Gas Pressure (kPa) | Nozzle Orifice Diameter (mm) | Gas Flow Rate (L/min) | Droplet Size Dv90 (μm) | Atomizing Rate (mL/min) |
|---|---|---|---|---|
| 50 | 0.4 | 2.48-16.02 | 7.09 | Baseline |
| 100 | 0.4 | Increased | 7.68 | Increased |
| 150 | 0.4 | Increased | 8.47 | Increased |
| 50 | 0.8 | 2.48-16.02 | Larger baseline | Baseline |
| 100 | 0.8 | Increased | Reduced | Increased |
| 150 | 0.8 | Increased | 29.5% reduction | Increased |
Data adapted from [2] demonstrates that increasing supply gas pressure from 50 to 150 kPa in a nebulizer with 0.8 mm orifice diameter reduced Dv90 (diameter below which 90% of droplets exist) by 29.5%, potentially enhancing lower airway penetration [2].
Deposition Fractions Across Flow Rates
Computational and experimental studies quantify deposition fractions across different flow rates:
- At 30 L/min, particles >16μm primarily deposit in the oropharynx [43]
- Increasing flow rate from sedentary (15 L/min) to activity conditions (60 L/min) significantly increases oropharyngeal deposition for particles >2.5μm [44]
- For particles <1.0μm, deposition fraction increases with flow rate but remains significantly lower than larger particles [44]
The following diagram illustrates the relationship between flow rate, particle size, and deposition patterns in the human respiratory tract:
Experimental Protocols for Flow Rate Optimization
Protocol 1: Nebulizer Output Characterization at Varied Flow Rates
Objective: To quantify nebulizer output characteristics (droplet size distribution, atomization rate, and output dose) across a range of supply gas pressures/flow rates.
Materials and Equipment:
- Medical air-compression nebulizer with adjustable supply gas pressure
- Gas flow meter (e.g., SIARGO-MF5700)
- Laser particle size analyzer (LPSA)
- Electronic balance (e.g., LICHEN-FA324TC)
- Hot-wire anemometer (e.g., HTI-HT9829)
- Model drug solution (e.g., 0.9% saline or drug formulation)
- Timer/stopwatch
Procedure:
- Connect the nebulizer to the adjustable pressure air supply.
- Install the gas flow meter between the pressure source and nebulizer.
- Add a fixed volume (e.g., 5 mL) of model drug solution to the nebulizer reservoir.
- Set the initial supply gas pressure to 50 kPa.
- Activate the system and simultaneously start the timer.
- Record the gas flow rate using the flow meter.
- Measure the jet gas flow rate at the nebulizer outlet using the hot-wire anemometer.
- Collect droplet size distribution data using the LPSA at a distance of 5 cm from the spray outlet.
- After 1 minute of operation, record the remaining solution mass using the electronic balance.
- Repeat steps 4-9 at increasing pressure intervals (e.g., 75, 100, 125, 150 kPa).
- Calculate atomization rate (mL/min) from mass difference.
- Compute Effective Output Dose (EOD) as the mass of drug per liter of air jetted.
Data Analysis:
- Plot droplet size parameters (Dv50, Dv90) versus supply gas pressure
- Correlate atomization rate with gas flow rate
- Identify optimal pressure settings that minimize large droplet fraction (>5μm)
Protocol 2: In Vitro Deposition Assessment Using Anatomical Airway Models
Objective: To quantify regional aerosol deposition patterns across different flow rates using realistic upper airway models.
Materials and Equipment:
- Realistic mouth-throat airway model (idealized or patient-specific)
- Breathing simulator capable of programmed flow profiles
- Nebulizer or inhaler device with test formulation
- Next-generation impactor (NGI) or similar particle sizing instrument
- Fluorescent tracer or radiolabeled compound for quantification
- Spectrofluorometer or gamma counter for analysis
Procedure:
- Prepare test formulation with appropriate tracer (e.g., sodium fluorescein 0.1%).
- Connect the airway model to the breathing simulator.
- Program the simulator to generate specific constant flow rates (e.g., 15, 30, 45, 60 L/min).
- For each flow rate, activate the nebulizer/inhaler and draw aerosol through the airway model for a fixed duration.
- Collect particles passing through the airway model using the NGI.
- Disassemble the airway model and wash each anatomical section separately.
- Quantify deposited tracer in each airway section using appropriate analytical methods.
- Repeat experiments across multiple flow rates (n≥3 for each condition).
Data Analysis:
- Calculate deposition fraction in each anatomical region
- Determine the fine particle fraction (<5μm) reaching the lower airways
- Establish flow rate - deposition efficiency correlations for different particle sizes
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Essential Materials for Flow Rate-Deposition Studies
| Category | Specific Items | Function/Application | Example Models/Types |
|---|---|---|---|
| Flow Measurement | Gas Flow Meter | Measures supply gas flow rate to nebulizer | SIARGO-MF5700 |
| Hot-Wire Anemometer | Measures jet gas flow rate at nebulizer outlet | HTI-HT9829 | |
| Breathing Simulator | Generates controlled, reproducible inhalation profiles | Programmable mechanical simulators | |
| Particle Characterization | Laser Particle Size Analyzer | Measures droplet size distribution in real-time | Spraytec, Malvern series |
| Cascade Impactor | Aerodynamic particle size distribution under different flow conditions | Next Generation Impactor (NGI) | |
| Aerosol Generation | Adjustable Pressure Nebulizer | Generates aerosol with controlled characteristics | Medical air-compression nebulizers with pressure control 0-150 kPa |
| Deposition Assessment | Anatomical Airway Models | Realistic oro-pharyngeal geometry for in vitro testing | Idealized USP throat, patient-specific 3D models |
| Analytical Detection Systems | Quantification of deposited mass in different regions | Spectrofluorometer, gamma counter, HPLC | |
| Data Acquisition | High-Speed Camera | Visualization of spray formation and development | iPhone 14Pro or specialized high-speed systems |
| Electronic Balance | Precise measurement of solution mass change during atomization | LICHEN-FA324TC |
Computational Approaches for Deposition Prediction
Rapid Deposition Analysis (RDA) Framework
Recent advances enable rapid prediction of aerosol deposition using dimensionless analysis derived from computational fluid dynamics (CFD) results [45]. This approach utilizes 34 dimensionless quantities encoding airway features, device characteristics, drug formulation properties, and inhalation profiles to predict total, regional, and lobar deposition [45].
The RDA method demonstrates high agreement with CFD training data (intraclass correlation coefficient = 0.92) and differs from in vivo data by only 1.3% in average lobar deposition [45]. This approach significantly reduces computational time compared to full CFD simulations while maintaining accuracy for personalized drug delivery optimization.
CFD-DEM Simulation Considerations
For detailed particle trajectory analysis, coupled Computational Fluid Dynamics-Discrete Element Method (CFD-DEM) simulations provide insights into flow patterns and particle residence times [46]. Key considerations include:
- Inlet velocity profile: Realistic mouth inlet profiles enhance deposition prediction accuracy, particularly on the tongue [44]
- Flow splitting: Measured air flow splitting must be imposed in simulations for physiological accuracy [46]
- Secondary flows: Vortex structures persist to the 7th generation, growing in intensity rather than attenuating [46]
- Turbulence modeling: Air turbulence survives to the 7th generation of human airways [46]
The following workflow diagram illustrates the computational approach for predicting flow rate effects on deposition:
Optimizing inhalation flow rate presents a critical opportunity to reduce oropharyngeal deposition and enhance therapeutic efficiency. The relationship between flow rate and deposition is complex, involving competing effects on particle size, inertial forces, and respiratory tract penetration. Based on current evidence:
- For local lung targeting: Moderate flow rates (20-30 L/min) typically balance adequate lung penetration while minimizing oropharyngeal loss [43]
- For systemic delivery: Lower flow rates (15-20 L/min) may enhance peripheral deposition through reduced impaction [42]
- Nebulizer optimization: Adjusting supply gas pressure and nozzle orifice diameter enables tuning of output characteristics for specific clinical requirements [2]
Implementation of these principles requires individualized consideration of the specific drug-device combination, patient population, and target lung region. The experimental protocols and computational approaches outlined provide robust methodologies for systematic optimization of flow parameters in pharmaceutical development.
Adapting Flow Parameters for Viscous Formulations and High-Dose Therapies
The optimization of nebulizing gas flow rates represents a critical frontier in the pharmaceutical development of inhalation therapies. Effective aerosol delivery depends on the precise interplay between a formulation's physical properties, particularly its viscosity, and the operational parameters of the delivery device. For high-dose therapies requiring viscous formulations—often necessary to accommodate high-concentration biologics and large molecules—this interplay becomes even more crucial. Traditional nebulizer designs and fixed operational parameters frequently prove inadequate for these advanced formulations, potentially compromising therapeutic efficacy through suboptimal droplet size distributions, inefficient delivery rates, and poor lung deposition. This application note synthesizes recent research findings to provide structured protocols for optimizing gas flow parameters, specifically addressing the challenges posed by high-viscosity formulations and high-dose therapies within the broader context of pharmaceutical nebulization research.
The Impact of Gas Flow Parameters on Atomization Characteristics
Fundamental Relationships Between Pressure and Flow
In medical air-compression nebulizers, the supply gas pressure serves as the primary controllable variable governing the atomization process. Unlike industrial systems that allow independent control of multiple flow parameters, medical nebulizers exhibit coupled effects where gas flow velocity, gas flow rate, and liquid flow rate are all influenced by the supply gas pressure and the nebulizer's nozzle orifice diameter [2]. This coupling makes understanding the pressure-flow relationship fundamental to optimization.
Research demonstrates that increasing supply gas pressure significantly increases both the supply gas flow rate and the jet gas flow rate. Experimental data with nebulizers of varying orifice diameters (0.4 mm, 0.6 mm, and 0.8 mm) showed that as supply gas pressure increased, the nebulizer's supply gas flow rate increased from 2.48 to 16.02 L/min, while the jet gas flow rate increased from 14.28 to 41.38 L/min [2]. This substantial increase in flow energy directly impacts the resulting aerosol characteristics.
Effects on Critical Atomization Metrics
The atomization characteristics critical to therapeutic efficacy—including droplet size distribution, atomizing rate, and spray concentration—show direct, quantifiable dependencies on gas flow parameters.
Table 1: Effect of Supply Gas Pressure on Nebulizer Performance Characteristics
| Performance Parameter | Effect of Increasing Gas Pressure | Magnitude of Change | Influence of Orifice Diameter |
|---|---|---|---|
| Droplet Size (Dv90) | Varies by orifice diameter | 0.4 mm: Increase (7.09 to 8.47 μm)0.6/0.8 mm: Decrease0.8 mm: 29.5% decrease at 150 kPa | Significant interaction |
| Atomizing Rate | Progressive increase | Correlated with pressure increase | Increases with larger diameters |
| Spray Concentration | Progressive increase | Correlated with pressure increase | Minor correlation |
| Effective Output Dose (EOD) | Increases | Correlated with pressure increase | No significant correlation |
| Spray Penetration | Increases | Correlated with pressure increase | Increases with larger diameters |
The relationship between orifice diameter and pressure reveals particularly important design considerations. While increasing pressure generally improves atomization efficiency, the effect on droplet size depends on the nozzle geometry. With a 0.4 mm orifice diameter, increasing pressure actually produced an anomalous increase in droplet size (Dv90 grew from 7.09 to 8.47 μm). In contrast, nebulizers with 0.6 and 0.8 mm orifice diameters exhibited decreased droplet size with increasing pressure, resulting in a more uniform droplet size distribution [2]. The 0.8 mm orifice diameter nebulizer showed a clear advantage in reducing the proportion of large droplets, with Dv90 decreasing by 29.5% when pressure increased from 50 to 150 kPa [2].
The Effective Output Dose (EOD), defined as the mass of drug contained in each liter of air jetted by the nebulizer, provides a crucial metric for estimating the dose inhaled by a patient with each inspiration. EOD increases with higher supply gas pressure but shows no significant correlation with orifice diameter, indicating that pressure control offers a more direct pathway to dosing control than nozzle geometry alone [2].
Protocol for Optimizing Nebulizer Parameters for Viscous Formulations
Experimental Setup and Equipment Specification
Objective: To systematically characterize and optimize gas flow parameters for the efficient nebulization of high-viscosity formulations.
Materials and Equipment:
- Medical Air-Compression Nebulizer: Configured with interchangeable nozzle orifice diameters (recommended: 0.4 mm, 0.6 mm, 0.8 mm)
- Gas Supply System: Air compressor capable of precise pressure control (0-150 kPa minimum) with accurate pressure regulation and monitoring
- Flow Measurement Instruments: - Gas flow meter (e.g., SIARGO-MF5700) for supply gas flow rate - Hot-wire anemometer (e.g., HTI-HT9829) for jet gas flow rate
- Droplet Characterization System: Laser Particle Size Analyzer (LPSA) for measuring droplet size distribution
- Output Measurement: Analytical balance (e.g., LICHEN-FA324TC, ±0.1 mg) for atomizing rate determination
- Data Acquisition: Camera system (e.g., iPhone 14Pro or equivalent) for spray pattern documentation and penetration analysis
- Formulations: Placebo formulations with viscosity modifiers (e.g., hyaluronic acid) to achieve target viscosity ranges (1-20 cP)
Step-by-Step Experimental Procedure
System Calibration
- Calibrate all measurement instruments according to manufacturer specifications
- Verify pressure regulator accuracy using a reference standard
- Confirm nozzle orifice diameters using appropriate metrology equipment
Baseline Characterization
- Install the smallest orifice diameter nozzle (0.4 mm) in the nebulizer assembly
- Load the reservoir with a low-viscosity placebo formulation (1 cP)
- Set the supply gas pressure to the lowest test point (50 kPa)
- Allow the system to stabilize for 30 seconds after pressure application
Flow Rate Measurement
- Record the supply gas flow rate using the gas flow meter
- Measure jet gas flow rate using the hot-wire anemometer positioned at the nozzle exit
- Perform triplicate measurements at each pressure setting
Atomization Performance Assessment
- Collect nebulized output for exactly 60 seconds onto the analytical balance
- Record mass deposited to determine atomizing rate (mg/min)
- Initiate droplet size analysis using the LPSA, ensuring proper alignment with the spray plume
- Capture spray images for subsequent penetration distance analysis
Parameter Progression
- Incrementally increase supply gas pressure to the next test point (e.g., 75, 100, 125, 150 kPa)
- Repeat steps 3-4 at each pressure level
- Replace with higher viscosity formulations (10 cP, 20 cP) and repeat the entire protocol
- Change nozzle orifice diameter and repeat the complete experimental sequence
Data Compilation
- Calculate mean values and standard deviations for all measured parameters
- Compute Effective Output Dose (EOD) using the formula: EOD = (Atomizing Rate × Drug Concentration) / Jet Gas Flow Rate
- Correlate operating parameters with performance metrics
Table 2: Key Parameter Combinations for Targeted Outcomes
| Therapeutic Objective | Recommended Orifice Diameter | Optimal Pressure Range | Expected Dv90 (μm) | Clinical Application |
|---|---|---|---|---|
| Deep Lung Delivery | 0.6-0.8 mm | 100-150 kPa | 2-5 μm | Targeted alveolar delivery |
| Bronchial Deposition | 0.4-0.6 mm | 75-125 kPa | 5-10 μm | Asthma, COPD therapies |
| High-Dose Delivery | 0.8 mm | 125-150 kPa | 1-3 μm (with reduced proportion of large droplets) | High-potency medications |
| Viscous Formulations | 0.8 mm | 125-150 kPa | 3-5 μm | Biologics, monoclonal antibodies |
Data Analysis and Interpretation
The following diagram illustrates the complex relationships between operational parameters, atomization mechanisms, and final aerosol characteristics, providing a conceptual framework for data interpretation:
High-Dose Therapy Considerations
Clinical Evidence for Dosing Strategies
The optimization of gas flow parameters becomes particularly critical when administering high-dose therapies, where conventional dosing regimens may prove insufficient. Clinical studies have investigated various dosing strategies for acute conditions, comparing different dosage levels and administration patterns:
Comparative Dose Studies: A double-blind randomized trial comparing 2.5 mg versus 7.5 mg nebulized albuterol for acute asthma treatment found no statistically significant difference in spirometric outcomes between the groups, suggesting that lower doses may be sufficient for moderate cases [47].
Continuous vs. Intermittent Administration: Research on severe acute asthma in adults demonstrated that continuous administration of albuterol (7.5 mg over one hour) produced similar improvement in FEV1 as the standard intermittent dosing (three 2.5 mg treatments over 60-90 minutes) [48]. This approach, enabled by optimized flow parameters, maintains consistent drug delivery while potentially improving patient compliance.
Integration with Viscosity Considerations
High-dose therapies frequently necessitate higher concentration formulations, which often exhibit increased viscosity due to elevated protein-protein interactions [49]. This creates a complex optimization challenge where gas flow parameters must be adjusted to accommodate both the dosing requirements and the physical properties of the formulation:
Viscosity-Pressure Relationship: Higher viscosity formulations typically require increased gas pressure to achieve optimal atomization. The enhanced shear forces generated at higher flow rates help overcome the internal resistance of viscous solutions, preventing the formation of improperly atomized large droplets.
EOD Considerations: For high-dose therapies, maximizing the Effective Output Dose becomes paramount. Research indicates that EOD increases with supply gas pressure but shows no significant correlation with orifice diameter [2], suggesting that pressure modulation offers the most direct control over delivered dose.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Materials for Nebulization Optimization Studies
| Item | Specification | Research Function | Application Notes |
|---|---|---|---|
| Interchangeable Nozzles | Orifice diameters: 0.4, 0.6, 0.8 mm | Systematic investigation of geometry effects | Enables diameter-performance correlation |
| Precision Gas Pressure Regulator | Range: 0-150 kPa, Accuracy: ±1% | Controlled manipulation of primary independent variable | Essential for dose-response studies |
| Hyaluronic Acid Solutions | Viscosity range: 1-20 cP | Formulation viscosity modulation without drug activity | Placebo model for biologic viscosities |
| Laser Particle Size Analyzer | Measurement range: 0.1-1000 μm | Critical droplet size distribution characterization | Determines respirable fraction |
| Hot-Wire Anemometer | Range: 0-50 m/s, Response time: <0.5s | Jet gas velocity quantification | Correlates energy input with atomization |
| Electronic Microbalance | Resolution: 0.1 mg, Capacity: 300g | Atomizing rate determination | Calculates output and efficiency |
The optimization of nebulizing gas flow parameters for viscous formulations and high-dose therapies requires a systematic approach that acknowledges the complex interplay between device operational settings, formulation physical properties, and therapeutic objectives. The experimental protocols outlined herein provide a validated methodology for characterizing these relationships and identifying optimal parameter combinations for specific clinical applications. The demonstrated impact of supply gas pressure and nozzle geometry on critical performance metrics—particularly droplet size distribution, atomizing rate, and Effective Output Dose—underscores the importance of tailored parameter selection rather than one-size-fits-all approaches. As pharmaceutical pipelines continue to incorporate increasingly complex biologics and high-potency compounds, these optimization strategies will prove essential for developing efficient, patient-centric inhalation therapies that maximize therapeutic benefit while minimizing treatment burden.
Validating Efficacy: In Vitro and CFD Methods for Flow Rate Analysis and Technology Comparison
In Vitro Experimental Setups for Aerosol Delivery Efficiency Measurement
Within pharmaceutical research, the optimization of nebulizing gas flow rate is a critical parameter for ensuring efficient aerosol delivery to the target pulmonary structures. In vitro experimental models provide a controlled, reproducible, and ethically advantageous platform for quantifying aerosol performance before progressing to complex and costly clinical trials. These setups are indispensable for screening formulation variables, characterizing device performance, and establishing key cause-effect relationships, such as the influence of gas flow rate on the inhaled dose [50] [51]. This document outlines standardized application notes and protocols for establishing these essential in vitro methodologies, providing a framework for generating robust, high-quality data for drug development.
Key Experimental Setups and Their Applications
Researchers can select from several established in vitro models, each offering unique advantages for specific aspects of aerosol delivery assessment. The choice of model depends on the research question, whether it relates to device performance, aerosol behaviour in simulated airways, or drug transport across biological membranes.
The following table summarizes the primary in vitro setups used in the field.
Table 1: Overview of Primary In Vitro Aerosol Delivery Experimental Models
| Experimental Model | Key Measurable Outputs | Primary Applications | Key Advantages |
|---|---|---|---|
| Air-Liquid Interface (ALI) Exposure Systems [52] | Cytotoxicity, Genotoxicity, Immunomodulation, Transcriptomic changes | Hazard ranking of aerosols (e.g., cigarette smoke, pharmaceuticals), efficacy assessment of inhaled drugs. | Direct exposure of lung cells to native aerosols; high-throughput capability (e.g., 96-well platforms). |
| Real-Time In Vitro Assessment with Scintigraphy [53] | Inhaled Mass (IM), Delivered Dose, Mass Balance, Deposition in circuit components. | Optimization of nebulizer function and placement during mechanical ventilation; analysis of circuit parameters. | Provides minute-by-minute delivery data; identifies sites of high depositional loss; uses surrogate radiolabels (e.g., 99mTc). |
| Computational Fluid Dynamics (CFD) [35] | Aerosol Deposition Fraction, Penetration Fraction, Particle trajectories in airway models. | Guided optimization of delivery parameters (e.g., waveform, synchronization); device design. | Provides high-resolution spatial data without physical prototypes; models complex physiology. |
| Evidence-Based Design-of-Experiments (DoE) [54] | Optimized values for factors like polymer MW, LA/GA ratio, polymer/drug ratio. | Systematically optimizing drug delivery system formulation parameters using historical data. | Reduces experimental burden by leveraging published data; establishes quantitative factor interactions. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of in vitro aerosol studies requires a suite of specialized materials and reagents. The following toolkit details essential components for setting up and conducting these experiments.
Table 2: Essential Research Reagents and Materials for In Vitro Aerosol Studies
| Item Name | Function/Application | Specific Examples / Notes |
|---|---|---|
| Vibrating Mesh Nebulizer (VMN) [50] | Generating aerosol with high efficiency and minimal residual volume. Often identified as the most efficient type for use in circuits like HFNC. | Aeroneb Solo; Placed upstream of the humidifier in HFNC circuits for optimal delivery. |
| Jet Nebulizer (JN) [50] [51] | A common, cost-effective aerosol generator. Can be used with an external gas source, which may impact ventilator performance. | Often requires a driving gas flow of 5-10 L/min; used for both bolus and continuous infusion studies. |
| Gamma Camera & Scintillation Ratemeter [53] | Quantifying regional aerosol deposition and providing real-time measurement of aerosol delivery. | Used with a radiolabel surrogate (e.g., 99mTc-Pertechnetate in saline); allows for mass balance determination. |
| Test Lung / Ventilation Simulator [53] [51] | Simulating patient's respiratory mechanics (compliance, resistance) during mechanical ventilation. | Rubber test lungs (e.g., neoprene) are used with set tidal volumes, rates, and PEEP to mimic breathing. |
| Andersen Cascade Impactor (ACI) [35] | Characterizing the aerodynamic particle size distribution of the generated aerosol. | Determines Mass Median Aerodynamic Diameter (MMAD) and Geometric Standard Deviation (GSD). |
| Polymeric Drug Carriers (e.g., PLGA) [54] | Serving as a biodegradable controlled-release matrix for API in model drug delivery systems. | Variables include molecular weight (MW) and Lactic Acid to Glycolic Acid (LA:GA) ratio. |
| Surrogate Aerosol Solutions [53] | Acting as a non-biohazardous stand-in for active pharmaceutical ingredients (APIs) during setup optimization. | Technetium-99m (99mTc) in saline for scintigraphy; Albuterol sulfate/salbutamol for chemical assay. |
Detailed Experimental Protocols
Protocol 1: Real-Time In Vitro Aerosol Delivery Assessment During Mechanical Ventilation
This protocol, adapted from the work of [53], details a method for the real-time quantification of aerosol delivery during mechanical ventilation, which is critical for optimizing nebulizer function and circuit configuration.
1. Experimental Setup and Apparatus Assembly:
- Connect a mechanical ventilator to a breath-enhanced jet nebulizer (e.g., i-AIRE).
- Connect the nebulizer outlet to the inlet of a heated humidifier chamber (e.g., Fisher & Paykel MR850) set to 37°C.
- Attach the humidifier outlet to a standard dual-limb heated wire ventilator circuit, terminating in a patient-Y connector.
- Connect a closed-system suction device and an endotracheal tube (ETT, e.g., 7.5-mm ID) to the Y-connector.
- Attach a pair of 1-L test lungs to the ETT via an Inhaled Mass (IM) filter (e.g., Pari) to collect the delivered aerosol.
- Connect the expiratory limb of the circuit to an expiratory aerosol filter.
- Orient a shielded gamma ratemeter (e.g., Ludlum Model 2200) towards the IM filter for real-time counting.
- Calibrate the ratemeter against a gamma camera (e.g., General Electric Maxi Camera) to convert counts to quantitative activity units (µCi).
2. Aerosol Generation and Data Acquisition:
- For bolus delivery, inject a known volume (e.g., 3 or 6 mL) and activity (~1200-1500 µCi) of 99mTc-pertechnetate in saline into the nebulizer. Measure the residual activity in the syringe to determine the precise nominal dose.
- For continuous infusion, fill a syringe pump with a 99mTc-saline solution and connect it to the nebulizer's medication port.
- Start the ventilator with the following typical settings: Constant flow pattern, Rate = 20 bpm, Tidal Volume = 650 mL, PEEP = 5 cm H2O.
- Initiate nebulization with medical air at 3.5 L/min and 50 psig.
- Trigger the ratemeter to record counts on the IM filter at pre-set intervals (e.g., every 2 minutes).
3. Data Analysis and Mass Balance:
- At experiment conclusion, measure the radioactivity on the IM filter, EXP filter, nebulizer residual, and all circuit components using the gamma camera.
- Calculate the Inhaled Mass (%) as: (Activity on IM Filter / Initial Nebulizer Charge) × 100.
- Perform a mass balance to account for 100% of the initial radioactivity, identifying major sites of depositional loss.
Protocol 2: Aerosol Delivery Optimization via High-Throughput Air-Liquid Interface (ALI) Exposure
This protocol, based on the HTES described by [52], is designed for the high-throughput comparative assessment of aerosols, such as for hazard ranking or drug efficacy screening.
1. Cell Culture and ALI Preparation:
- Culture relevant lung epithelial cells (e.g., A549 alveolar cells) according to standard protocols.
- Seed cells onto 96-well HTS insert microplates designed for ALI exposure.
- Allow cells to differentiate and form confluent monolayers at the Air-Liquid Interface for the required duration prior to exposure.
2. Aerosol Generation and System Configuration:
- Connect a high-throughput exposure system (HTES, e.g., VITROCELL 96) to an aerosol generator (e.g., VITROCELL Smoking Machine VC 1 for tobacco products or a nebulizer for pharmaceuticals).
- The HTES should be configured to provide multiple, precise aerosol concentration levels (e.g., 11 dilution stages plus a vehicle control) with several technical replicates per level.
- Ensure the system maintains continuous-flow ALI conditions with integrated temperature regulation and real-time monitoring of flow and humidity to preserve cell homeostasis.
3. Aerosol Exposure and Biological Endpoint Analysis:
- Transfer the 96-well insert plate to the HTES exposure module.
- Expose cells to the generated aerosol for a predetermined duration, with the vehicle control column receiving only humidified, clean air.
- Post-exposure, collect the apical and basolateral compartments for analysis.
- Assess biological endpoints using a predictive assay panel, which may include:
- Cytotoxicity (e.g., MTT, LDH release).
- Genotoxicity (e.g., high-content in-situ γ-H2AX analysis).
- Immunomodulation (e.g., cytokine profiling via ELISA).
- Generate dose-response curves for each endpoint to determine points of departure (PoDs) for efficient aerosol prioritization.
The in vitro protocols detailed herein provide a robust foundation for the precise measurement and optimization of aerosol delivery efficiency. The integration of real-time scintigraphic methods and high-throughput ALI systems enables researchers to deconstruct complex delivery challenges into manageable, quantitative parameters. By systematically applying these models, particularly in investigating critical variables like nebulizing gas flow rate, scientists can significantly accelerate the development of inhaled pharmaceuticals, ensuring that optimized formulations and devices progress to clinical stages with a higher probability of therapeutic success.
Computational Fluid Dynamics (CFD) for Flow Field and Particle Deposition Analysis
Computational Fluid Dynamics (CFD) has emerged as a transformative tool in pharmaceutical development, enabling researchers to simulate and analyze the complex interplay between fluid flow and aerosolized particles. Within the context of optimizing nebulizing gas flow rates, CFD provides a critical bridge between device engineering and clinical efficacy, allowing for the precise evaluation of how operational parameters influence drug delivery to the respiratory tract. By creating virtual prototypes, CFD simulations offer insights that are often difficult or expensive to obtain experimentally, facilitating the design of nebulizers that maximize lung deposition while minimizing drug waste [55]. This protocol details the application of CFD for analyzing airflow and particle deposition, with a specific focus on parameter optimization for pharmaceutical aerosols.
The therapeutic efficacy of inhaled medications is profoundly influenced by the aerodynamic particle size distribution and the dynamics of the flow field generated by the delivery device. Air-compression nebulizers, which operate based on Bernoulli’s theorem and the Venturi effect, use a high-speed gas jet to tear the drug solution into fine droplets [2]. The supply gas pressure, a key controllable parameter, directly determines the gas flow rate and velocity, which in turn affect critical atomization characteristics such as droplet size distribution, atomization rate, and spray concentration [2]. Optimizing this parameter is therefore essential for developing efficient and personalized inhalation therapies.
Key Applications and Case Studies
CFD analysis enables a systematic investigation of the factors governing aerosol generation and deposition. The following case studies illustrate its application in optimizing pharmaceutical drug delivery.
Table 1: CFD Applications in Nebulizer Optimization and Aerosol Deposition
| Study Focus | Key CFD Findings | Impact on Performance |
|---|---|---|
| Supply Gas Pressure & Nozzle Design [2] | Increasing supply pressure reduces droplet size (Dv90 decreased by 29.5% at 0.8 mm orifice), but can cause anomalous size increase in smaller orifices (0.4 mm). | Higher pressure and larger orifice diameter increase the effective output dose (EOD) and atomizing rate, enabling more efficient drug delivery. |
| Baffle Geometry Optimization [56] | Conical baffle designs (0.25 mm protrusion) demonstrated superior pressure distribution and airflow streamlines compared to flat or arc-shaped baffles. | Enhanced baffle design improves nebulizer spray output efficiency, leading to greater medication output with minimal breath force. |
| Patient-Specific Deposition Analysis [45] | A rapid data-driven model based on 34 dimensionless quantities was developed from over 3,400 CFD simulations on patient-specific airways. | Enables prediction of lobar aerosol deposition with high accuracy (ICC: 0.92), facilitating personalized treatment plans without time-consuming CFD. |
| Upper Airway Fluid Dynamics [57] | Secondary flow structures (vortices) persist up to the 7th generation of airways, and airflow splitting at bifurcations is not uniform. | Accurate modeling of these phenomena is crucial for predicting local deposition patterns in the tracheobronchial tree. |
Experimental and Computational Protocols
This section provides detailed methodologies for conducting CFD analysis of nebulizer flow fields and particle deposition.
Protocol for Analyzing Nebulizer Atomization Characteristics
This protocol outlines the steps for evaluating the impact of operating parameters, such as gas flow rate, on nebulizer performance [2].
1. Problem Definition and Objective Setting:
- Define the key atomization characteristics to be investigated: droplet size distribution (e.g., Dv90, Sauter Mean Diameter), atomizing rate (mass of liquid aerosolized per unit time), spray concentration, and effective output dose (EOD).
- Identify the independent variables: supply gas pressure (e.g., 50-150 kPa) and nozzle orifice diameter (e.g., 0.4 mm, 0.6 mm, 0.8 mm).
2. Computational Model Setup:
- Geometry Creation: Develop a 3D computer-aided design (CAD) model of the nebulizer, including the internal flow channels, nozzle orifice, and baffle. The geometry can be simplified by removing minor features like door frames to accelerate simulation without sacrificing critical accuracy [58].
- Meshing (Grid Generation): Discretize the computational domain into a volume mesh of small, interrelated cells. Use inflation layers near solid boundaries (walls, baffles) to resolve high-velocity gradients. Perform a mesh sensitivity analysis to ensure results are independent of cell size [57] [56].
- Boundary Conditions:
- Inlet: Set as a pressure inlet (specifying supply gas pressure) or a mass flow inlet.
- Outlet: Set as a pressure outlet (typically atmospheric pressure).
- Walls: Apply a no-slip boundary condition.
3. Numerical Simulation:
- Solver Settings: Use a pressure-based solver. For steady-state simulations of the internal flow field, select a Reynolds-Averaged Navier-Stokes (RANS) approach. The SST k-ω model is often suitable for modeling turbulence in such internal flows [57].
- Material Properties: Define the working fluids (e.g., air as the gas phase, water or a drug solution as the liquid phase).
- Solution: Run the simulation until key parameters (e.g., residuals, mass flow rate at outlets) converge.
4. Data Analysis and Validation:
- Extract results including internal pressure distribution, gas flow velocity, and streamline patterns to visualize airflow [56].
- Validate CFD predictions against experimental data. Critical experiments include:
Protocol for Simulating Aerosol Deposition in Human Airways
This protocol describes a workflow for predicting where inhaled pharmaceutical aerosols deposit in a patient-specific airway model [57] [45].
1. Airway Geometry Reconstruction:
- Obtain high-resolution computed tomography (CT) scans of the patient's thorax at both total lung capacity (TLC) and functional residual capacity (FRC).
- Use a semi-automatic algorithm to segment and reconstruct 3D models of the airways and lung lobes. Smooth the geometry with a volume compensation algorithm [45].
2. Computational Mesh Generation:
- Generate a computational mesh of the segmented airway geometry. For complex geometries like the tracheobronchial tree, an unstructured hexahedral-dominant mesh is often used [57].
- Refine the mesh at bifurcations and near walls to capture secondary flows and boundary effects. A mesh with ~8 million elements may be necessary for sufficient accuracy in upper airways [57].
3. Airflow Modeling and Boundary Conditions:
- Governing Equations: Solve the Navier-Stokes equations using a finite volume method (FVM).
- Turbulence Modeling: For tidal breathing or deep inhalation (e.g., from a DPI), use a RANS model such as SST k-ω with low-Reynolds wall functions [57].
- Boundary Conditions (Mixed-Driven Approach):
- Inlet (Mouth): Impose a realistic velocity profile corresponding to the patient's inhalation profile or device output.
- Outlets (Lobar Bronchi): Impose the experimentally measured or physiologically derived flow splitting ratios across the different lung lobes to ensure realistic ventilation [57].
4. Particle Transport and Deposition:
- Particle Injection: Introduce particles at the mouth/inlet. For nebulizers, particles can be released with zero initial velocity. For MDIs, assign an initial velocity and spray cone angle [45].
- Particle Tracking: Use a Discrete Element Method (DEM) or a Lagrangian particle-tracking model. Account for forces including drag, pressure gradient, and gravity [57].
- Deposition Mechanisms: The model will inherently capture major deposition mechanisms: inertial impaction (in oropharynx and bifurcations), sedimentation (in small airways and alveoli), and diffusion (for nanoparticles <0.2 μm) [14].
5. Data Analysis and Model Validation:
- Quantify total, regional (extrathoracic, central, distal, peripheral), and lobar deposition fractions [45].
- Validate the CFD model against in vivo data from imaging techniques like Single-Photon Emission Computed Tomography (SPECT)/CT using radiolabeled compounds [45].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Software for CFD Analysis of Aerosol Delivery
| Item | Function/Description | Application Note |
|---|---|---|
| CAD Software (e.g., SolidWorks) | Creates 3D digital models of nebulizer components and internal flow channels. | Essential for designing and modifying nebulizer geometry, including baffles and nozzles, for simulation [56]. |
| CFD Software (e.g., ANSYS Fluent, OpenFOAM) | Solves the fundamental equations of fluid flow and particle transport numerically. | OpenFOAM is open-source; ANSYS Fluent is commercial. Both can model internal flow and Lagrangian particle tracking [57] [45]. |
| Patient-Specific Airway Models | 3D geometries reconstructed from medical CT or MRI scans. | Provides anatomical realism for predicting deposition in specific patient populations (e.g., asthmatics, COPD) [45]. |
| Laser Particle Size Analyzer (LPSA) | Measures the size distribution of aerosol droplets produced by a nebulizer. | Critical for validating the accuracy of CFD predictions of droplet size (e.g., Dv90) [2]. |
| Design of Experiments (DoE) Software | Provides a statistical framework for efficiently optimizing multiple CFD input parameters. | Used to systematically evaluate the effect of factors like gas pressure, gas temperature, and flow rate on spray output [59]. |
| Hot-Wire Anemometer & Gas Flow Meter | Measures gas flow velocity and volumetric flow rate. | Used for experimental validation of simulated gas flow rates from the nebulizer [2]. |
The integration of CFD into the development and optimization of nebulized pharmaceutical products provides a powerful, in-silico platform for advancing targeted drug delivery. By applying the protocols outlined herein, researchers can systematically dissect the relationship between nebulizing gas flow rates and critical performance metrics, from initial atomization to final lung deposition. The ability to simulate these processes in patient-specific geometries paves the way for truly personalized inhalation therapy, ensuring that medications are delivered efficiently to the intended site of action. As computational power and modeling techniques continue to evolve, CFD is poised to play an even greater role in reducing development costs and accelerating the creation of more effective inhaled therapeutics.
Aerosol delivery devices are critical in the administration of pharmaceuticals for respiratory diseases. This application note provides a detailed comparative analysis of Jet Nebulizers, Vibrating Mesh Nebulizers (VMNs), and Pressurized Metered-Dose Inhalers (pMDIs), with a specific focus on the impact of nebulizing gas flow rate on aerodynamic performance. Within the context of optimizing pharmaceutical research, we present standardized experimental protocols for in vitro evaluation, data on key performance parameters, and advanced visualization of operational mechanisms. The findings underscore the critical relationship between device engineering, aerosol flow dynamics, and resultant deposition efficiency, providing a scientific foundation for device selection and formulation development.
Inhalation therapy represents a cornerstone of treatment for respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and infectious diseases. The efficacy of an inhaled drug is not solely dependent on its pharmacological activity but is profoundly influenced by the delivery device's performance. The device must generate an aerosol with an aerodynamic particle size distribution suitable for reaching the target region of the lungs, typically the 1-5 μm range for alveolar deposition [60].
The optimization of nebulizing gas flow rates is a critical parameter in pharmaceutical research and development. It directly influences key aerosol characteristics, including the Mass Median Aerodynamic Diameter (MMAD), Fine Particle Fraction (FPF), and ultimately, the lung deposition fraction. This application note details the comparative performance of the three primary nebulizer types—Jet, Vibrating Mesh, and pMDIs—framed within the essential research context of flow rate optimization. It is intended to equip researchers and drug development professionals with the methodologies and data necessary to make informed decisions in inhaler formulation and device testing.
Operational Mechanisms
- Jet Nebulizers: Operate on the Bernoulli principle, using a pressurized gas stream passing through a venturi to draw liquid medication from a reservoir and shear it into droplets [61]. They are categorized into standard, breath-enhanced, and breath-actuated types.
- Vibrating Mesh Nebulizers (VMNs): Utilize a piezoelectric element to vibrate a mesh with micron-sized holes, pumping the liquid formulation through the apertures to generate a low-velocity aerosol [61] [60]. They are classified as either Active (vibration powered by the element) or Passive (vibration driven by a horn).
- Pressurized Metered-Dose Inhalers (pMDIs): Deliver a precise dose of drug suspended or dissolved in a propellant via a pressurized canister. Actuation releases a high-speed plume containing the drug. Optimal use requires precise patient coordination between actuation and inhalation.
Comparative Performance Data
The following table summarizes the key characteristics and performance metrics of each device type, based on current literature.
Table 1: Comprehensive Comparison of Aerosol Delivery Devices
| Parameter | Jet Nebulizer | Vibrating Mesh Nebulizer (VMN) | Pressurized Metered-Dose Inhaler (pMDI) |
|---|---|---|---|
| Mechanism of Action | Bernoulli/Venturi Effect [61] | Piezoelectric Micropumping [61] [60] | Pressurized Propellant [62] |
| Typical Droplet Size (MMAD) | >5 μm [61] | <5 μm [61] [60] | Formulation-dependent |
| Fine Particle Fraction (FPF) | Lower & flow-dependent [63] | Higher (e.g., 77.4-80.6% <5μm) [60] | Varies by device/resistance [62] |
| Typical Residual Volume | High [61] | Minimal [61] | Very Low (in canister) |
| Nebulization Time | Longer | Shorter [61] | Instantaneous |
| Flow Rate Sensitivity | High (MMAD increases at lower flow) [63] | Lower (passive systems can be affected) | High (requires sufficient PIF for deaggregation) [62] |
| Portability | Low (requires gas source) | High [61] | High |
| Ease of Use/Cleaning | Difficult to clean [61] | Cleaning can be difficult [61] | Easy (no cleaning) |
| Cost | Cheap [61] | More expensive [61] | Inexpensive |
| Key Advantages | Effective for drugs not in pMDIs/DPIs [61] | Silent, portable, high efficiency, minimal drug loss [61] [64] | Portable, multi-dose, rapid delivery |
| Key Disadvantages | Inefficient, needs compressed gas, difficult to clean [61] | Clogging with viscous/crystallizing drugs, cost [61] | Requires coordination, oropharyngeal deposition |
Impact of Nebulizing Gas Flow Rate
The flow rate is a critical variable in aerodynamic performance assessment. Research indicates that for jet nebulizers, operating an Andersen Cascade Impactor (ACI) at the standard 28.3 L/min versus a more physiologically relevant 18 L/min resulted in a significant increase in MMAD and geometric standard deviation (GSD) [63]. This demonstrates that evaluating at higher flow rates may overestimate the lung dose a patient would receive, as the additional air mixed with the drug affects its size distribution before inhalation.
For VMNs, optimization extends to the inlet structure. A 2023 study showed that a multiple-orifice air inlet structure significantly improved delivery efficiency to 20% deposition fraction at 15 L/min in a mouth-throat model, compared to simpler inlet designs, by directing airflow to the center and reducing droplet-wall collisions [21]. For pMDIs and DPIs, the inspiratory flow rate generated by the patient is the critical factor. Studies on DPIs show that devices like the Diskus and NEXThaler deliver a more consistent dose and FPF across a range of flow rates (30-90 L/min), whereas devices like the Turbohaler are more sensitive to low flow rates, showing a decrease in emitted dose and FPF [62].
Experimental Protocols for In-Vitro Testing
This section provides detailed methodologies for the key in-vitro experiments cited in this field, enabling researchers to replicate and build upon established practices.
Protocol: Aerodynamic Particle Size Distribution (APSD) via Cascade Impaction
Objective: To determine the APSD, specifically the MMAD and FPF, of aerosols generated by nebulizers and pMDIs, and to investigate the influence of flow rate.
Key Reagent Solutions & Equipment:
- Next Generation Impactor (NGI) or Andersen Cascade Impactor (ACI): The primary apparatus for segregating particles by aerodynamic diameter [63] [62].
- HPLC System with UV/PDA Detector: For sensitive and specific quantification of drug mass deposited on each impactor stage [62].
- Vacuum Pump & Flow Controller: To generate and precisely regulate the air flow through the impactor (e.g., 15, 28.3, 60, 90 L/min) [63] [62].
- Dose Unit Sampling Apparatus (DUSA): For delivered dose uniformity testing [62].
Methodology:
- Apparatus Setup: Assemble the impactor and connect it to the vacuum pump with a calibrated flow controller. Ensure all seals are airtight.
- Flow Rate Selection: Define the test flow rates based on the device and research question. For jet nebulizers, include both pharmacopeial (e.g., 28.3 L/min) and patient-representative (e.g., 15-18 L/min) flows [63]. For DPIs, test across a range (e.g., 30, 60, 90 L/min) [62].
- Actuation/Dosing: For each test run, introduce a single dose into the system.
- Nebulizers: Place the device before the throat inlet and run until sputtering (dryness) [21].
- pMDIs/DPIs: Actuate the device into a USP/Ph.Eur. induction port (throat model) attached to the impactor inlet.
- Sample Collection: Disassemble the impactor and carefully wash the drug from the induction port, each impactor stage, and the final filter/micro-orifice collector into separate volumetric flasks.
- Quantification: Analyze each solution using a validated HPLC-UV method to determine the drug mass per stage [62].
- Data Analysis: Calculate the cumulative percentage of drug deposition. Plot the data on log-probability paper or use software to determine the MMAD and GSD. The FPF is calculated as the percentage of the total emitted dose with an aerodynamic diameter below a specific cutoff (e.g., 5 μm or 1 μm) [60].
Protocol: Deposition Fraction Analysis in Anatomical Airway Models
Objective: To quantify the regional deposition (oropharyngeal vs. lung) of aerosols using realistic airway replicas.
Key Reagent Solutions & Equipment:
- 3D-Printed Anatomical Airway Model: Idealized or patient-specific replicas of the mouth, throat, and upper airways [65] [21].
- Bubble Absorption Tubes & Membrane Filters (pore size 0.1 μm): To capture the aerosol that passes through the airway model ("lung dose") [21].
- High-Speed Imaging/Schlieren Setup: To visualize spray kinematics and droplet breakup dynamics [66].
- Sar-Gel or Chemical Assay: For visualizing and quantifying deposition on the airway model surface itself [21].
Methodology:
- Model Preparation: Fabricate a realistic airway model (e.g., adult MT, infant, or NHP model) using 3D printing [65] [21].
- Experimental Setup: Connect the inhaler device to the model's inlet. Connect the model's outlet to a series of traps (bubble tube, prefilter, membrane filter) to collect the non-deposited aerosol. A flow meter and vacuum pump control the inhalation flow rate [21].
- Aerosol Administration: Generate the aerosol under the defined test conditions (specific to the device and flow rate).
- Deposition Quantification:
- Oropharyngeal Dose: Rinse the internal surface of the airway model and analyze the washings via HPLC.
- Lung Dose: Extract and analyze the drug collected in the bubble absorption tube and on the final membrane filter [21].
- Calculation: The Deposition Fraction (DF) in the airway model and the Lung Delivery Efficiency are calculated as a percentage of the total emitted dose or the loaded dose [65].
Visualizing Experimental Workflows and Performance Relationships
Experimental Workflow for Aerosol Performance Testing
The following diagram illustrates the logical workflow for a comprehensive in-vitro aerosol performance assessment, integrating the protocols described above.
Diagram 1: Aerosol Performance Testing Workflow.
Relationship Between Flow Rate and Aerosol Performance
This diagram conceptualizes the complex relationships between device type, operational flow rate, and key aerosol performance outcomes.
Diagram 2: Flow Rate Impact on Aerosol Performance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagent Solutions and Equipment for Aerosol Research
| Item | Function/Application | Example Usage & Notes |
|---|---|---|
| Next Generation Impactor (NGI) | Standardized apparatus for measuring Aerodynamic Particle Size Distribution (APSD) [62]. | Used with a calibrated flow rate to determine MMAD and FPF. Critical for comparing device performance. |
| High-Performance Liquid Chromatography (HPLC) | Quantitative analysis of drug mass deposited on impactor stages or in anatomical models [62]. | Provides specificity and sensitivity; requires method development for each drug compound. |
| 3D-Printed Anatomical Airway Models | Replicas of human or animal airways for realistic in-vitro deposition studies [65] [21]. | Allows for regional deposition analysis (oropharyngeal vs. tracheal vs. lung). Can be idealized or patient-specific. |
| Active Servo-Lung Simulator | Precisely simulates patient respiratory mechanics for testing under realistic breathing patterns [67]. | Essential for evaluating device performance in simulated COPD or asthma conditions during mechanical ventilation. |
| Sodium Chloride (NaCl) 0.9% Solution | Common placebo model formulation for aerosol performance testing [21]. | Serves as a standard, non-active test liquid for characterizing nebulizer output and deposition. |
| Vibrating Mesh Nebulizer Sources | The core component in VMNs and certain spray dryers for initial droplet formation [60]. | Pore size and vibration characteristics are key design parameters influencing initial droplet size and distribution. |
| Laser Diffraction Analyzer | Provides real-time, volume-based droplet size distribution of aerosols in flight [60]. | Useful for rapid characterization, though it does not measure aerodynamic diameter directly. |
Benchmarking Delivery Efficiency Across Commercial Devices and Interfaces
Inhalation therapy represents a critical modality for treating respiratory diseases, enabling targeted drug delivery directly to the site of action. For researchers and drug development professionals, the selection of optimal nebulizer systems and interfaces presents a significant challenge due to substantial performance variations among commercially available devices. These efficiency differences can profoundly impact therapeutic outcomes through underdosing or delayed symptom relief [9]. Within pharmaceutical research, benchmarking these systems provides essential data for optimizing nebulizing gas flow rates and other operational parameters to maximize respirable drug delivery.
The pressing need for standardized evaluation protocols has emerged from studies demonstrating wide variations in nebulizer drug delivery efficiency [9]. This application note synthesizes current benchmarking data and methodologies to support evidence-based device selection and optimization in both research and clinical settings.
Quantitative Benchmarking of Commercial Devices
Key Performance Metrics for Nebulizer Evaluation
Efficiency assessment of nebulizer systems requires measurement of multiple interdependent parameters that collectively predict clinical performance:
- Aerosol Output (AO): The total mass of drug emitted from the nebulizer, typically measured in microliters (μL) or milligrams (mg) of active pharmaceutical ingredient [9].
- Aerosol Output Rate (AOR): The rate of drug emission, expressed as mass per unit time (e.g., μL/min), indicating treatment duration [9].
- Respirable Fraction (RF): The percentage of aerosol particles with aerodynamic diameter smaller than 5 μm, representing the proportion capable of reaching the lower airways [9].
- Mass Median Aerodynamic Diameter (MMAD): The diameter at which 50% of aerosol particles by mass are larger and 50% are smaller, determining deposition patterns [9].
- Respirable Dose (RD): The total mass of drug in the respirable fraction, calculated as RD = RF × AO [9].
- Respirable Drug Delivery Rate (RDDR): The rate of respirable drug delivery, calculated as RDDR = RF × AOR, representing the most clinically relevant efficiency parameter [9].
Comparative Performance of Jet Nebulizer Systems
Recent evaluation of 15 commercially available jet nebulizer systems according to EN ISO 27427 standards revealed significant efficiency variations, with RDDR values differing approximately three-fold between highest and lowest-performing devices [9].
Table 1: Performance Parameters of Select Commercial Jet Nebulizer Systems
| Device Model | Aerosol Output (μL) | Aerosol Output Rate (μL/min) | Respirable Dose (μL) | RDDR (μL/min) |
|---|---|---|---|---|
| PARI BOY Junior (yellow NA) | 450 | 142 | 363 | 115 |
| PARI COMPACT2 | 520 | 160 | 358 | 105 |
| MPV MicroDrop Family2 | 520 | 155 | 317 | 94 |
| PARI BOY Classic/Pro (blue NA) | 400 | 135 | 295 | 99 |
| Omron C28P/Omron X105 | 530 | 145 | 285 | 82 |
| aponorm Compact PLUS (max setting) | 190 | 75 | 114 | 45 |
Data adapted from Fischer (2023) [9]. Testing conditions: filled with 2 mL of 0.1% (w/v) salbutamol; measured with PARI COMPAS breath simulator (tidal volume 500 mL, 15 breaths/min, inhalation:exhalation ratio 50:50).
Historical data from a 1994 comparison of 17 jet nebulizers demonstrates that performance variability has long been a challenge in the field, with respirable particle delivery rate (RPDR) values ranging from 0.03 ml/min to 0.26 ml/min across devices [68]. The PARI LC JET (0.24 ml/min) and PARI-JET (0.26 ml/min) demonstrated significantly higher RPDR than most other models tested [68].
The Critical Impact of Gas Flow Parameters
The atomization characteristics of medical air-compression nebulizers are significantly influenced by supply gas pressure, which directly affects droplet size distribution, atomization rate, and overall delivery efficiency [2]. Recent research demonstrates that increasing supply gas pressure generally enhances the effective output dose (EOD) - the mass of drug contained in each liter of air jetted by the nebulizer - thereby improving the effective dose inhaled by patients with each inspiration [2].
Table 2: Impact of Nozzle Orifice Diameter and Supply Pressure on Atomization Characteristics
| Orifice Diameter (mm) | Supply Pressure (kPa) | Supply Gas Flow Rate (L/min) | Jet Gas Flow Rate (L/min) | Dv90 (μm) | EOD Trend |
|---|---|---|---|---|---|
| 0.4 | 50 | 2.48 | 14.28 | 7.09 | Increases with pressure |
| 0.4 | 150 | 6.85 | 25.42 | 8.47 | Increases with pressure |
| 0.6 | 50 | 6.95 | 22.15 | 9.84 | Increases with pressure |
| 0.6 | 150 | 16.02 | 41.38 | 7.12 | Increases with pressure |
| 0.8 | 50 | 8.84 | 19.64 | 12.45 | Increases with pressure |
| 0.8 | 150 | 15.12 | 34.28 | 8.78 | Increases with pressure |
Data adapted from recent research on supply gas pressure effects (2025) [2]. Dv90 represents the diameter below which 90% of the droplet volume exists.
Notably, nebulizers with larger orifice diameters (0.8 mm) demonstrated a 29.5% reduction in Dv90 when supply gas pressure increased from 50 to 150 kPa, indicating improved droplet size distribution with higher pressure [2]. This relationship between operational parameters and atomization characteristics provides critical guidance for optimizing nebulizer systems for specific patient populations and therapeutic applications.
Advanced Experimental Protocols for Efficiency Benchmarking
Standardized In Vitro Evaluation Protocol
Comprehensive benchmarking of nebulizer systems requires rigorous standardized methodology to generate comparable data across devices:
Equipment Setup
- Nebulizer systems to be tested
- PARI COMPAS breath simulator or equivalent
- Next Generation Impactor (NGI) or equivalent particle sizing instrument
- Validated HPLC system with UV detection for drug quantification
- Precision balance (accuracy ±0.1 mg)
- Environmental control chamber (maintain 23°C, 50% relative humidity)
Methodology
- Prepare test solution: 0.1% (w/v) salbutamol in sterile saline or appropriate drug formulation [9].
- Fill nebulizer with 2.0 mL test solution using precision pipette [9].
- Operate breath simulator with adult breathing pattern: tidal volume 500 mL, frequency 15 breaths/min, inhalation:exhalation ratio 1:1 [9].
- Collect aerosol output on appropriate filter for specified duration.
- Determine aerosol output (AO) by weighing nebulizer before and after operation or through chemical analysis [9].
- Measure particle size distribution using NGI at flow rate of 15 L/min [9].
- Calculate respirable fraction (RF) as percentage of particles <5 μm [9].
- Determine drug mass via validated HPLC-UV method [9].
- Calculate derived parameters (RD, RDDR) using standard formulas.
- Perform statistical analysis with significance level of p<0.05.
This protocol should be repeated with three individual systems of each nebulizer type, with duplicate measurements providing six readings per device type [9].
Advanced Platform for High-Efficiency Delivery Assessment
For research applications requiring maximal delivery efficiency, such as with expensive biologics or targeted therapies, the Heated Dryer System (HDS) platform represents a sophisticated experimental approach:
Figure 1: HDS Platform Configuration and Performance
HDS-HFNC Protocol for Combined Respiratory Support and Aerosol Delivery:
- Configure HDS with dual mesh nebulizers - one for humidity control (isotonic saline) and one for drug delivery [69].
- Set HFNC parameters to clinical flow rates (e.g., 30 L/min for adults) [69].
- Implement active synchronization to sense inhalation and coordinate drug aerosol delivery [69].
- Operate drug nebulizer during portion of inhalation cycle only [69].
- Characterize aerosol size distribution pre- and post-heating section (MMAD typically reduced from ~5.3μm to ~1.2μm) [69].
- Assess regional deposition using in vitro airway models with simulated breathing [69].
The HDS platform demonstrates how integrating multiple optimization strategies - active aerosol size change, synchronization with inhalation, streamlined connections, and improved interfaces - can achieve lung delivery efficiencies of 75-78% during HFNC therapy and >90% with oral inhalation [69].
Interface-Specific Evaluation Protocol
Device interfaces significantly impact delivery efficiency, particularly in pediatric populations. Standardized evaluation of interface performance should include:
Comparative Interface Protocol
- Select appropriate interfaces for target population (mouthpiece, facemask, nasal mask, pacifier mask, HFNC) [70].
- Prepare test system with realistic upper airway model appropriate for target population (adult, pediatric, infant) [70].
- Implement simulated breathing pattern appropriate for population (tidal volume, frequency, I:E ratio) [24].
- Measure deposited drug mass at different anatomical regions (upper airways, lower airways, gastrointestinal).
- Quantify losses in device, interface, and upper airways.
- Assess impact of leaks and breathing pattern variations.
Critical findings from interface studies include the superior efficiency of mouthpieces (where feasible), the importance of well-fitting anatomic facemasks with minimal dead space, and the significant losses associated with "blow-by" techniques (50-85% reduction compared to facemask) [70]. Recent innovations like the pacifier mask show promise for improving compliance and delivery in infant populations [70].
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Essential Research Reagents and Materials for Nebulizer Benchmarking
| Item | Function | Application Notes |
|---|---|---|
| Salbutamol sulfate (0.1% w/v) | Model drug for aerosol characterization | Standardized reference formulation; enables cross-study comparisons [9] |
| Synthetic surfactant (e.g., Poractant alfa) | Simulates pulmonary surfactant interaction | Assesses drug-surfactant interactions for biologic stability |
| Precision gas flow meter | Measures supply gas flow rates | Critical for parameter optimization; accuracy ±2% recommended [2] |
| Laser particle size analyzer | Determines droplet size distribution | Alternative to cascade impactors for rapid screening [2] |
| Breathing pattern simulator | Generates physiologically relevant waveforms | Enables standardized testing across devices [9] |
| Next Generation Impactor (NGI) | Aerodynamic particle size characterization | Gold standard for inhaler testing; use at 15 L/min [9] |
| HPLC-UV system | Drug quantification | Validated method required for precise deposition measurement [9] |
| Anatomic airway models | Simulates upper airway deposition | Should match target population (adult, pediatric, infant) [70] |
| Heated humidity delivery system | Mimics clinical respiratory support conditions | Essential for HFNC and NIV application testing [69] |
Benchmarking delivery efficiency across commercial devices and interfaces provides essential data for optimizing nebulized drug delivery in pharmaceutical research. Significant performance variations among devices underscore the importance of evidence-based selection, with the respirable drug delivery rate (RDDR) representing the most clinically relevant efficiency parameter. Optimization of nebulizing gas flow rates and pressure parameters presents a key opportunity for enhancing delivery efficiency, particularly when matched to specific patient populations and their interface requirements.
The experimental protocols outlined herein enable standardized, reproducible evaluation of nebulizer systems, from basic quality assessment to advanced high-efficiency platforms. By adopting these methodologies, researchers can generate comparable data to guide device selection and optimization, ultimately contributing to more effective inhaled therapies through targeted delivery efficiency benchmarking.
Conclusion
Optimizing nebulizer gas flow rate is a critical, multi-faceted determinant of successful pharmaceutical aerosol delivery. The evidence synthesized from foundational principles to advanced validation confirms that precise flow rate control directly enhances the respirable fraction, minimizes depositional losses, and maximizes lung dose. Key takeaways include the superior efficiency of mesh nebulizers at lower flow rates, the transformative potential of streamlined component design in NIV circuits, and the power of CFD-guided optimization. Future directions for biomedical research must focus on developing intelligent, flow-adaptive nebulizer systems, further refining synchronized delivery techniques for high-flow therapy, and establishing standardized, patient-specific flow protocols that account for disease state and breathing patterns. The continued integration of advanced simulation with robust in vitro validation will be paramount in developing the next generation of high-efficiency aerosol delivery systems for costly and critical therapeutics.
References
- 1. Optimizing the droplet size distribution of personal ... [https://www.sciencedirect.com/science/article/abs/pii/S1773224725010706]
- 2. The Effect of Supply Gas Pressure on the Atomization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12138825/]
- 3. Fundamentals of aerosol therapy in critical care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5054555/]
- 4. Alveolar distribution of nebulized solution in health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11503722/]
- 5. Influence of impactor operating flow rate on particle size ... [https://vivo.health.unm.edu/display/n1970094111]
- 6. Measurement of droplet size distribution in emulsions ... [https://nmr.oxinst.com/learning/view/article/measurement-of-droplet-size-distribution-in-emulsions-using-benchtop-nmr]
- 7. Computational Fluid Dynamics (CFD) Guided Spray Drying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8958016/]
- 8. Variability in delivered dose and respirable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5295794/]
- 9. Efficiency Assessment of 15 Nebuliser Systems by the ... [https://www.emjreviews.com/respiratory/symposium/efficiency-assessment-of-15-nebuliser-systems-by-the-respirable-drug-delivery-rate-a-comparable-quality-parameter/]
- 10. Aerosol delivery through high-flow nasal therapy [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1098427/full]
- 11. In vitro delivery efficiencies of nebulizers for different breathing ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-021-00895-3]
- 12. Evaluation of antibody drug delivery efficiency via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10691028/]
- 13. Nasal high-flow bronchodilator nebulization: a randomized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6301902/]
- 14. Mechanisms of Pharmaceutical Aerosol Deposition in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4037474/]
- 15. Impact of gas humidification and nebulizer position under ... [https://www.nature.com/articles/s41598-023-38281-9]
- 16. A new method for measuring lung deposition efficiency of ... [https://www.nature.com/articles/srep36147]
- 17. Flow-Field Characteristics and Spray ... [https://www.sciencedirect.com/science/article/pii/S100093452500135X]
- 18. Impact of normal, obstructive, and restrictive breathing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005052/]
- 19. Comparing mesh and compressor nebulizers in pulmonary ... [https://www.sciencedirect.com/science/article/abs/pii/S0954611125000289]
- 20. Different Types of Nebulizers | Which Is Right for You? [https://nebology.com/blogs/education/what-are-the-different-types-of-nebulizers?srsltid=AfmBOop1RvOGXQ1Gj3PcHkVZ2jBMhbd8I0NCUyz2Szvwyif2hqT-iAxY]
- 21. Optimization of Vibrating Mesh Nebulizer Air Inlet Structure ... [https://www.mdpi.com/2073-4433/14/10/1509]
- 22. Measuring nebulizer output. Aerosol production vs ... [https://pubmed.ncbi.nlm.nih.gov/9149595/]
- 23. A clinical guide to non-invasive respiratory support in acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625427/]
- 24. Influence of nebulizer pressure drop on breathing profiles ... [https://www.sciencedirect.com/science/article/pii/S0021850225000977]
- 25. Comparison of clinical outcomes between high-flow nasal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12379362/]
- 26. High-flow nasal cannula versus non-invasive ventilation for ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1582749/full]
- 27. Effect of Flow Rates of High-Flow Nasal Cannula on ... [https://www.sciencedirect.com/science/article/abs/pii/S0012369224057295]
- 28. Non-Invasive Ventilation: When, Where, How to Start, and ... [https://www.mdpi.com/2077-0383/14/14/5033]
- 29. Noninvasive ventilation in acute hypoxemic respiratory failure [https://www.sciencedirect.com/science/article/pii/S2667100X25000040]
- 30. Physiological comparison of noninvasive ventilation and high ... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-025-05366-y]
- 31. Medication Administration: Nebulized (Pediatric) CE [https://elsevier.health/en-US/preview/medication-administration-nebulized-ped]
- 32. Inhalation therapy: current and emerging devices in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602052/]
- 33. the effects of increased nebulizer flow rates and reservoirs [https://pubmed.ncbi.nlm.nih.gov/12396415/]
- 34. The Use of an Inspiration-Synchronized Vibrating Mesh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10458390/]
- 35. CFD Guided Optimization of Nose-to-Lung Aerosol ... [https://link.springer.com/article/10.1007/s11095-020-02923-8]
- 36. A novel nebulized drug delivery system based on an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921402/]
- 37. Deposition simulations of realistic dosages in patient ... [https://www.sciencedirect.com/science/article/pii/S0378517324012535]
- 38. Steps toward nebulization in-use studies to understand the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9770090/]
- 39. Pulmonary drug delivery. Part II: The role of inhalant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1884297/]
- 40. Devices for Improved Delivery of Nebulized Pharmaceutical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6781258/]
- 41. Enhancing the Proportion of Sub-5 μm Atomized Droplet ... [https://www.mdpi.com/2073-8994/17/1/6]
- 42. Deposition of Inhaled Particles in the Lungs [https://archbronconeumol.org/en-deposition-inhaled-particles-in-lungs-articulo-S1579212912000845]
- 43. Flow Patterns and Particle Residence Times in the Oral Cavity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9612176/]
- 44. Effects of inlet velocity profile, inhalation flowrate and ... [https://www.sciencedirect.com/science/article/pii/S0021929015006715]
- 45. Rapid deposition analysis of inhaled aerosols in human ... [https://www.nature.com/articles/s41598-024-75578-9]
- 46. A critical analysis of the CFD-DEM simulation ... [https://www.sciencedirect.com/science/article/pii/S0010482524000325]
- 47. High-dose versus low-dose nebulized albuterol in acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4098280/]
- 48. Asthma Continuous vs Intermittent Albuterol, at High and ... [https://www.sciencedirect.com/science/article/abs/pii/S0012369215463378]
- 49. IN THE THICK OF IT: ACCELERATING THE MIXING AND ... [https://www.ondrugdelivery.com/in-the-thick-of-it-accelerating-the-mixing-and-delivery-of-high-viscosity-injectables/]
- 50. Aerosol delivery through high-flow nasal therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC9889634/]
- 51. Aerosol delivery via invasive ventilation: a narrative review [https://pmc.ncbi.nlm.nih.gov/articles/PMC8105868/]
- 52. Next-generation high-throughput in vitro exposure system for ... [https://enveurope.springeropen.com/articles/10.1186/s12302-025-01258-8]
- 53. Real-Time In Vitro Assessment of Aerosol Delivery During ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8867090/]
- 54. A new evidence-based design-of-experiments approach ... [https://www.nature.com/articles/s41598-024-82496-3]
- 55. Design and validation of processing systems using CFD [https://forcetechnology.com/en/services/simulations-and-cfd/processing-system-simulations]
- 56. Increasing Nebulizer Spray Efficiency Using a Baffle with a ... [https://www.mdpi.com/2306-5354/12/7/680]
- 57. A Critical Analysis of the CFD-DEM Simulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11434992/]
- 58. CFD simulations validate pharma company's HVAC CapEx ... [https://www.crbgroup.com/projects/cfd-simulations-validate-hvac-capex-investment]
- 59. Underutilized Methods for Optimizing LC–MS Sensitivity [https://www.chromatographyonline.com/view/lcgc-blog-underutilized-methods-optimizing-lc-ms-sensitivity]
- 60. Effects of Different Mesh Nebulizer Sources on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10527815/]
- 61. Table 1 Comparison of different types of nebulizers [https://ccforum.biomedcentral.com/articles/10.1186/s13054-016-1448-5/tables/1]
- 62. Effect of Flow Rate on In Vitro Aerodynamic Performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4841907/]
- 63. Influence of impactor operating flow rate on particle size ... [https://pubmed.ncbi.nlm.nih.gov/17763140/]
- 64. Comparison of bronchodilator administration with vibrating ... [https://www.sciencedirect.com/science/article/pii/S0735675717309075]
- 65. Influence of mesh nebulizer characteristics on aerosol ... [https://www.sciencedirect.com/science/article/pii/S0928098723002361]
- 66. Fluids, Volume 10, Issue 11 (November 2025) – 28 articles [https://www.mdpi.com/2311-5521/10/11]
- 67. Effects of jet nebulization on ventilator performance with ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1004551/full]
- 68. A Comparison of Commercial Jet Nebulizers [https://www.sciencedirect.com/science/article/abs/pii/S0012369215444307]
- 69. In Vitro Evaluation of Nebulized Pharmaceutical Aerosol ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9994751/]
- 70. Drug delivery interfaces: A way to optimize inhalation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4978620/]