Specificity, Selectivity, Accuracy, and Precision: A Comprehensive Guide to Analytical Method Validation in Pharmaceutical Development
This article provides a thorough examination of the core validation parameters—specificity, selectivity, accuracy, and precision—in analytical method development for pharmaceutical research and drug development.
Specificity, Selectivity, Accuracy, and Precision: A Comprehensive Guide to Analytical Method Validation in Pharmaceutical Development
Abstract
This article provides a thorough examination of the core validation parameters—specificity, selectivity, accuracy, and precision—in analytical method development for pharmaceutical research and drug development. Tailored for researchers, scientists, and industry professionals, it explores the foundational definitions, methodological applications, and troubleshooting strategies as per ICH Q2(R2), USP, and other global guidelines. The content bridges theoretical concepts with practical case studies, addresses phase-appropriate validation from early discovery to commercialization, and discusses emerging trends such as Analytical Quality by Design (AQbD) and green chemistry to equip the audience with the knowledge to ensure regulatory compliance, data integrity, and robust analytical performance.
Core Principles: Demystifying Specificity, Selectivity, Accuracy, and Precision in Analytical Method Validation
In the rigorous world of research and drug development, the integrity of data is paramount. Conclusions and decisions are only as sound as the methods used to gather and analyze information. Within this context, a clear understanding of key validation parameters—specificity, selectivity, accuracy, and precision—forms the bedrock of trustworthy science. These concepts are the pillars that support the entire structure of research validity, ensuring that findings are not only statistically significant but also meaningful and reflective of reality.
Confusion often arises between the terms specificity and selectivity, as well as between accuracy and precision. While sometimes used interchangeably in casual conversation, they hold distinct and critical meanings in a scientific setting. This guide provides a detailed, objective comparison of these fundamental parameters. By defining their roles, illustrating their differences with experimental data, and placing them within the broader framework of method validation, we aim to equip researchers, scientists, and drug development professionals with the knowledge to critically evaluate and improve their analytical techniques.
Specificity vs. Selectivity: Discriminating Power in Analysis
The terms specificity and selectivity both relate to an analytical method's ability to distinguish the analyte of interest from other components in the sample. However, a nuanced difference exists, and understanding it is crucial for proper method validation.
Conceptual Definitions
Specificity is the absolute ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradants, or matrix components. It is often considered a binary parameter—a method is either specific or it is not. Specificity is the preferred term in guidelines like those from the International Council for Harmonisation (ICH) [1]. A specific method can unambiguously measure the analyte even when other substances are present.
Selectivity, on the other hand, refers to the extent to which a method can determine a particular analyte in a mixture without interference from other analytes or compounds in that mixture. It is a measure of the degree of this discrimination. As one source notes, "selectivity is a parameter that can be graded whereas specificity is absolute" [2]. A highly selective method can quantify multiple analytes simultaneously while reliably distinguishing each one.
Experimental Protocols and Evaluation
Establishing specificity/selectivity is a fundamental step in bioanalytical method validation. The general protocol involves analyzing samples that contain potential interferents and comparing the results to a control.
Detailed Methodology:
- Prepare Samples: Analyze a blank biological matrix (e.g., plasma, urine) to ensure no endogenous components interfere with the analyte's signal. Then, analyze the matrix spiked with the analyte at a relevant concentration (e.g., the Lower Limit of Quantification, LLOQ).
- Introduce Interferents: Spike the matrix with known impurities, degradants, metabolites, or co-administered drugs at their expected maximum concentrations.
- Chromatographic Analysis: For methods like HPLC or LC-MS, inject the prepared samples and evaluate the resulting chromatograms. The critical parameters to assess are:
- Resolution: The peaks for the analyte and potential interferents should be baseline resolved.
- Peak Purity: Using a diode array detector (DAD) or mass spectrometry (MS), confirm that the analyte peak is homogeneous and not co-eluting with another substance [1].
- Data Interpretation: The method is considered specific if the analyte response is unaffected by the presence of interferents and each analyte of interest is resolved from all others.
Comparative Data and Scenarios
The following table summarizes the core differences and applications of specificity and selectivity.
Table 1: Specificity and Selectivity at a Glance
| Parameter | Core Question | Analogy | Primary Application in Drug Development |
|---|---|---|---|
| Specificity | Can the method measure only the analyte, with no interference? | A key that opens only one lock. | Stability-indicating methods; quantifying a single active drug in the presence of its degradants [1]. |
| Selectivity | To what extent can the method distinguish between multiple analytes? | a sieve with perfectly sized holes that separates different grains. | Bioanalysis in clinical pharmacology; simultaneously quantifying a drug and its major metabolites in patient plasma [1]. |
Accuracy vs. Precision: Cornerstones of Measurement Truth and Reproducibility
Accuracy and precision are foundational concepts in evaluating the quality of measurements. They describe different aspects of measurement performance, and a reliable method must demonstrate both.
Conceptual Definitions
- Accuracy refers to the closeness of agreement between a measured value and a true or accepted reference value. It answers the question, "Is my result correct?" [3]. Accuracy is about correctness and freedom from bias.
- Precision refers to the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. It answers the question, "Can I get the same result repeatedly?" [1] [3]. Precision is about reproducibility and consistency, regardless of whether the results are accurate.
Experimental Protocols and Evaluation
The validation of accuracy and precision in bioanalytical methods is typically conducted together through a study of repeatability (intra-day precision) and intermediate precision (inter-day precision, often involving different analysts or equipment).
Detailed Methodology for Accuracy and Precision Assessment:
- Sample Preparation: Prepare a minimum of five replicates per concentration level. The concentrations should cover the linear range of the method, typically including at least three levels: one near the LLOQ, one in the mid-range, and one near the upper limit of quantification (ULOQ) [1].
- Analysis: Analyze all samples using the validated method.
- Calculation:
- Accuracy: For each concentration level, calculate the mean measured value. Accuracy is expressed as the percentage recovery of the known added amount or as the relative bias. % Accuracy = (Mean Measured Concentration / Nominal Concentration) × 100%
- Precision: Calculate the standard deviation (SD) and relative standard deviation (RSD) for the replicates at each concentration level. The RSD, also known as the coefficient of variation (CV), is the primary metric for precision. % RSD = (Standard Deviation / Mean) × 100%
Comparative Data and the Bullseye Analogy
The classic bullseye analogy effectively illustrates the relationship between accuracy and precision.
Table 2: Interpreting Accuracy and Precision Combinations
| Scenario | Accuracy | Precision | Interpretation & Implication |
|---|---|---|---|
| High Accuracy, High Precision | High | High | The ideal scenario. Results are both correct and consistent. The method is robust and reliable for decision-making. |
| High Accuracy, Low Precision | High | Low | The average of the results is correct, but individual measurements are scattered. The method has high bias but is not reliable for single measurements. |
| Low Accuracy, High Precision | Low | High | Results are consistently wrong in the same direction. This indicates a systematic error (bias) that may be correctable through calibration. |
| Low Accuracy, Low Precision | Low | Low | The worst scenario. Results are inconsistent and incorrect. The method is unreliable and requires re-development. |
In a research context, accuracy is paramount when the actual value is critical, such as in determining the dosage of a drug based on its concentration in a formulation. Precision is more critical when consistency is the primary goal, such as in manufacturing quality control to ensure every product unit is identical [3].
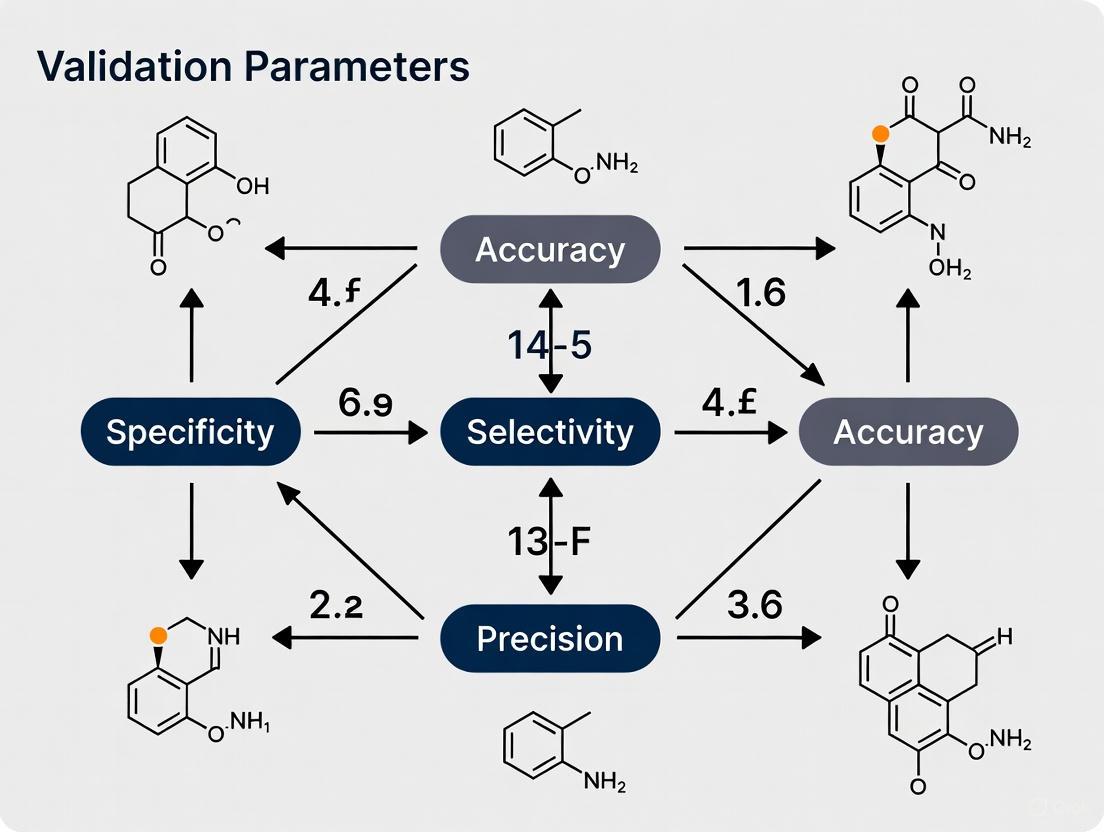
The Interconnected Framework: A Visual Synthesis
The relationships between the four pillars and their role in method validation can be visualized as a cohesive workflow. The following diagram maps the logical pathway from establishing the fundamental discriminatory power of a method to ensuring its quantitative reliability.
Diagram 1: The pillars of analytical method validation.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for conducting validation experiments for the parameters discussed in this guide.
Table 3: Essential Research Reagents and Materials for Method Validation
| Reagent/Material | Function in Validation | Application Example |
|---|---|---|
| Certified Reference Standard | Provides the true/accepted value against which accuracy is measured. Must be of high and documented purity. | Used to prepare known concentration solutions for accuracy and linearity studies [1]. |
| Blank Biological Matrix | Used to assess specificity by confirming the absence of interfering signals from endogenous components. | Control human plasma or urine in bioanalytical method development [1]. |
| Spiked Matrix Samples | Samples with known concentrations of analyte(s) and potential interferents, used to validate specificity, selectivity, accuracy, and precision. | Plasma samples spiked with a drug candidate and its known metabolites to establish selectivity [1]. |
| Chromatographic Columns | The stationary phase for separation; critical for achieving the resolution needed for specificity and selectivity. | A C18 column used in HPLC to separate a drug from its degradants in a stability-indicating method. |
| Mass Spectrometer (MS) | A detection system that provides high selectivity and specificity by identifying analytes based on their mass-to-charge ratio. | LC-MS is used in bioanalysis to specifically quantify a drug in complex biological samples like blood [1]. |
For researchers and drug development professionals, navigating the regulatory requirements for analytical procedure validation is fundamental to ensuring drug quality, safety, and efficacy. The landscape is primarily shaped by three key sets of guidelines: the International Council for Harmonisation (ICH) Q2(R2) guideline, the United States Pharmacopeia (USP) General Chapter <1225>, and the directives from the European Medicines Agency (EMA). While aligned in their overall goal, these guidelines exhibit critical differences in their structure, terminology, and emphasis, which can impact strategic regulatory planning. A solid understanding of the validation parameters—including specificity, selectivity, accuracy, and precision—across these frameworks is not merely a regulatory exercise but a cornerstone of robust analytical science. The recent adoption of the new ICH Q2(R2) guideline in 2023 marks a significant evolution, moving the industry from a static validation model toward a more dynamic, lifecycle approach inspired by Analytical Quality by Design (AQbD) principles [4] [5].
Comparative Analysis of ICH, USP, and EMA Guidelines
The following table provides a detailed, side-by-side comparison of the core validation parameters as defined by the ICH, USP, and EMA guidelines, highlighting the nuances in their definitions and requirements.
Table 1: Comparison of Core Validation Parameters Across ICH Q2(R2), USP, and EMA
| Validation Parameter | ICH Q2(R2) | USP General Chapter <1225> | EMA / EU GMP Annex 15 |
|---|---|---|---|
| Accuracy | Closeness of agreement between a test result and the accepted reference value [4]. | Closeness of test results obtained by that method to the true value [6]. | Expects demonstration of accuracy, typically through spike/recovery experiments, aligning with ICH principles [7]. |
| Precision | Expressed as repeatability, intermediate precision, and reproducibility. Assessed with a minimum of 9 determinations over 3 levels [6] [4]. | Degree of agreement among individual test results from repeated measurements. Expresses as standard deviation or relative standard deviation [6]. | Requires precision to be demonstrated, with a strong emphasis on the use of statistical process control and trend analysis in ongoing verification [8] [7]. |
| Specificity/Selectivity | Ability to assess unequivocally the analyte in the presence of components that may be expected to be present [6]. ICH prefers "specificity" [6]. | USP notes that other international authorities prefer "selectivity," reserving "specificity" for procedures that are completely selective [6]. | Requires specific procedures to demonstrate specificity, particularly for stability-indicating methods [7]. |
| Detection Limit (DL) | The lowest amount of analyte in a sample that can be detected, but not necessarily quantitated [6]. | Defined similarly to ICH. For instrumental methods, a signal-to-noise ratio of 2:1 or 3:1 is common [6]. | Expects the DL to be established for impurities, aligning with ICH Q2(R2) [7]. |
| Quantitation Limit (QL) | The lowest amount of analyte in a sample that can be quantitatively determined with suitable precision and accuracy [6]. | Defined similarly to ICH. A typical signal-to-noise ratio is 10:1 [6]. | Expects the QL to be established, consistent with ICH requirements [7]. |
| Linearity & Range | Linearity is replaced by "Reportable Range" and "Working Range" in Q2(R2), which includes suitability of the calibration model and verification of the lower range limit [4]. | Linearity: Ability to obtain test results proportional to analyte concentration. Range: Interval between upper and lower levels of analyte that has been demonstrated to be determined with precision, accuracy, and linearity [6]. | Requires demonstration of linearity and defines a suitable range for the procedure, consistent with the ICH foundation [7]. |
| Robustness | A new section in Q2(R2) provides more detailed guidance on robustness study design, recommending structured approaches like Design of Experiments (DoE) [4] [5]. | Measures capacity to remain unaffected by small, deliberate variations in method parameters [6]. | Strongly encourages robustness testing during method development, often as part of an AQbD approach, to ensure method reliability [7]. |
| Key Differentiators | - Lifecycle approach linked with ICH Q14 [5].- Covers modern analytical techniques (e.g., NIR, MS) [4].- Introduces "Analytical Procedure Lifecycle" [4]. | - Legally recognized standard in the US (FD&C Act) [6].- Distinguishes between validation, verification, and transfer [9].- User verification required for compendial methods [6]. | - Mandates a Validation Master Plan (VMP) [8] [7].- Integrated with EU GMP, particularly Annex 15 [8].- Emphasizes ongoing process verification (OPV) post-approval [8]. |
Key Strategic Implications of the Differences
The differences outlined in Table 1 have direct implications for regulatory strategy. The EMA's requirement for a Validation Master Plan creates a structured, top-down framework for all validation activities, which is more formal than the FDA's expectations [8]. Furthermore, the EMA's concept of Ongoing Process Verification (OPV) is integrated into the product quality review, emphasizing continuous monitoring rather than a one-time validation event [8]. With the advent of ICH Q2(R2), a major shift is the move from a static "validate once" approach to an Analytical Procedure Lifecycle model. This new paradigm, developed in parallel with ICH Q14, formalizes AQbD concepts such as the Analytical Target Profile (ATP) and Method Operable Design Region (MODR), enabling more flexible and robust method management post-approval [4] [5].
Experimental Protocols for Key Validation Parameters
To ensure robust and defensible method validation, standardized experimental protocols are essential. The following sections detail the general methodologies for establishing key validation parameters, synthesized from the ICH, USP, and EMA guidelines.
Protocol for Accuracy
The protocol for accuracy varies based on the sample type [6].
For Drug Substances:
- Sample Preparation: Analyze a minimum of 9 determinations over a minimum of 3 concentration levels (e.g., 80%, 100%, 120% of target concentration). Use a known purity reference standard.
- Comparison: Compare the measured value against the accepted true value of the reference standard.
- Calculation: Calculate accuracy as the percentage of recovery. Report the mean recovery and confidence intervals (e.g., %RSD) across all levels.
For Drug Products (Formulated):
- Sample Preparation: Use a placebo matrix (all components except the analyte). Spike with known quantities of the analyte across the specified range (3 levels, 3 replicates each).
- Analysis: Carry the spiked samples through the complete analytical procedure.
- Calculation: Calculate the percentage recovery of the known, added amount. The results demonstrate the ability of the method to accurately measure the analyte in the presence of the sample matrix.
Protocol for Precision
Precision should be investigated at multiple levels [6].
Repeatability:
- Sample Preparation: Use a homogeneous sample of drug substance or product (e.g., 100% test concentration).
- Analysis: Perform a minimum of 6 independent assays of the same sample. These must be complete, independent sample preparations taken through the entire analytical procedure.
- Calculation: Calculate the standard deviation (SD) or relative standard deviation (RSD) of the 6 results.
Intermediate Precision:
- Experimental Design: Vary conditions within the same laboratory, such as different analysts, different days, and different equipment.
- Analysis: Perform the assay under each of the varied conditions.
- Calculation: Evaluate the SD or RSD of the results from all conditions to establish the method's robustness to within-laboratory variations.
Protocol for Specificity/Selectivity
Specificity must be demonstrated for identification tests, purity tests, and assays [6].
- For an Impurity or Assay Method:
- Sample Preparation:
- A: Analyte alone (e.g., drug substance reference standard).
- B: Placebo or sample matrix.
- C: Sample spiked with potential impurities, degradation products (generated via stress studies: light, heat, humidity, acid/base hydrolysis, oxidation), or excipients.
- Analysis: Analyze all samples (A, B, C) using the proposed analytical procedure.
- Evaluation: For chromatography, demonstrate that the analyte peak is free from interference and that all critical peaks (e.g., impurities) are resolved. Peak purity tests using techniques like diode array detection (DAD) or mass spectrometry (MS) are highly recommended to prove the analyte peak is attributable to a single component [6].
- Sample Preparation:
Visualizing the Analytical Procedure Lifecycle
The revised ICH Q2(R2) and ICH Q14 guidelines introduce a fundamental shift from a one-time validation event to an integrated lifecycle management approach for analytical procedures. The following diagram illustrates this continuous process.
Diagram 1: Analytical Procedure Lifecycle per ICH Q14/Q2(R2)
This lifecycle model underscores that knowledge gained during routine use of the method, through ongoing monitoring and data trending, feeds back into the development and validation stages, enabling continuous improvement and facilitating managed post-approval changes within the established MODR [5].
The Scientist's Toolkit: Essential Reagent Solutions
The execution of validation studies requires specific high-quality materials. The table below details key reagent solutions and their critical functions in ensuring reliable analytical results.
Table 2: Essential Research Reagent Solutions for Validation Studies
| Reagent / Material | Function in Validation |
|---|---|
| Reference Standards | Certified materials with known purity and identity; used as the primary benchmark for quantifying the analyte and establishing method accuracy and linearity [6]. |
| System Suitability Solutions | Prepared mixtures used to verify that the chromatographic or analytical system is performing adequately at the time of testing, ensuring data integrity for parameters like precision and specificity [6]. |
| Placebo/Blank Matrix | Contains all components of the sample except the analyte; critical for demonstrating specificity/selectivity by proving the absence of interference from the sample matrix [6]. |
| Impurity/Degradation Standards | Isolated impurities or forced-degradation products; used to spike samples to confirm the method's ability to detect and quantify impurities, a key aspect of specificity [6]. |
| Buffers & Mobile Phases | High-purity solvents and salts prepared to exact specifications; their consistency is vital for maintaining robust separation and detector response, directly impacting precision, accuracy, and robustness [6]. |
The regulatory landscape for analytical validation parameters is a complex but coherent tapestry woven from the ICH, USP, and EMA guidelines. While the core parameters of specificity, accuracy, and precision are universally required, the strategic approach to demonstrating them is evolving. The USP provides a foundational, legally-recognized standard in the US, the EMA enforces a structured, plan-driven framework integrated with GMP, and the new ICH Q2(R2) ushers in a modern, lifecycle-oriented era. For drug development professionals, success lies in understanding the nuanced differences between these guidelines and implementing a holistic, science- and risk-based validation strategy. Embracing the Analytical Procedure Lifecycle model, with its emphasis on ATP, MODR, and continuous improvement, is no longer just a best practice but is becoming the expected standard for ensuring analytical methods remain fit-for-purpose throughout a product's life.
The Critical Role of Validated Methods in Drug Safety, Efficacy, and Quality Control
In the pharmaceutical industry, the validation of analytical methods is not merely a regulatory hurdle but a fundamental scientific requirement that forms the bedrock of drug safety, efficacy, and quality control. Method validation is a systematic process of performing numerous tests designed to verify that an analytical test system is suitable for its intended purpose and capable of providing useful and valid analytical data [10]. This process establishes evidence that provides a high degree of assurance that a specific process, method, or system will consistently produce results meeting predetermined acceptance criteria [11].
The critical importance of validated methods extends across the entire drug development and manufacturing continuum. From raw material testing to finished product release, validated methods ensure that medications are free from contamination and impurities, protecting patients from adverse effects while guaranteeing that drugs deliver their optimal therapeutic benefits [12]. Within the context of global regulatory frameworks, method validation provides the necessary documentation to demonstrate compliance with standards set by agencies including the U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) [13].
As the pharmaceutical landscape evolves toward more complex molecules and innovative therapies, the role of validated methods becomes increasingly crucial. This article examines the core parameters of method validation, explores their application in ensuring drug safety and efficacy, and highlights emerging trends that are reshaping quality control practices for 2025 and beyond.
Core Parameters of Analytical Method Validation
Essential Validation Characteristics and Their Significance
Analytical method validation involves testing multiple attributes to demonstrate that a method can provide reliable and valid data when used routinely [10]. These parameters are systematically evaluated to establish that analytical methods are fit for their intended purpose in pharmaceutical analysis.
Table 1: Core Parameters for Analytical Method Validation
| Parameter | Definition | Methodological Approach | Acceptance Criteria |
|---|---|---|---|
| Specificity/Selectivity | Ability to measure analyte accurately in presence of potential interferences | Analyze chromatographic blanks; check for interference in expected analyte retention time window | No interference peaks at analyte retention time [10] |
| Accuracy | Degree of agreement between test results and true value | Spike sample matrix with known analyte concentrations; calculate % recovery | Varies by matrix; detailed in study plan [10] |
| Precision | Degree of agreement among individual test results from multiple samplings | Inject series of standards/samples; calculate %RSD from mean and standard deviation | Often based on Horwitz equation (e.g., 1.9% RSDr for 10% analyte) [10] |
| Linearity | Ability to obtain results proportional to analyte concentration | Inject minimum 5 concentrations (50-150% of expected range); plot concentration vs. response | Correlation coefficient (r) with specified minimum [10] |
| Range | Interval between upper and lower analyte levels demonstrated with precision, accuracy, and linearity | Confirm using concentrations from linearity testing | Established based on linearity results [10] |
| LOD/LOQ | Lowest concentrations detectable (LOD) and quantifiable (LOQ) | Calculate from linear regression (LOD=3.3σ/S, LOQ=10σ/S) or signal-to-noise (3:1 for LOD, 10:1 for LOQ) | Expressed in μg/mL or ppm; specific to method [10] |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters | Vary parameters (pH, temperature, mobile phase composition); measure impact on results | Consistent performance under varied conditions [13] |
The mathematical foundation for several validation parameters relies on statistical analysis. For precision evaluation, the Horwitz equation provides an empirical relationship between the among-laboratory relative standard deviation (RSD) and concentration (C): RSDR = 2(1-0.5logC) [10]. For estimation of repeatability (RSDr), this is modified to RSDr = 0.67 × 2(1-0.5logC). This equation has been proven to be largely independent of analyte, matrix, and method of evaluation across a wide concentration range [10].
Experimental Protocols for Key Validation Parameters
Protocol for Linearity Determination:
- Prepare a series of standard solutions at a minimum of five different concentrations covering 50-150% of the expected working range.
- Inject each solution in duplicate or triplicate using the specified chromatographic conditions.
- Record the instrument response (peak area) for each concentration.
- Plot concentration versus response and calculate the regression line using the equation y = a + bx.
- Calculate the correlation coefficient (r) to confirm linearity [10].
Protocol for Accuracy Evaluation:
- Prepare samples of the matrix of interest spiked with known concentrations of analyte standard.
- Analyze the samples using the method being validated.
- Calculate the percentage recovery for each concentration using the formula: % Recovery = (Measured Concentration / Theoretical Concentration) × 100.
- Compare results against predetermined acceptance criteria specified in the study plan [10].
Protocol for LOD/LOQ Determination from Linear Regression:
- Prepare a series of standard solutions at various concentrations covering the working range.
- Analyze each solution minimally twice and record instrument responses.
- Calculate the linear regression equation y = a + bx.
- Calculate the standard deviation of the residuals (σ).
- Calculate LOD as (3.3σ)/S and LOQ as (10σ)/S, where S is the slope of the calibration curve [10].
Analytical Method Validation in Pharmaceutical Quality Control
Integration into Pharmaceutical Quality Systems
Validated analytical methods form the technical foundation of robust pharmaceutical quality control systems, ensuring that every drug batch consistently meets predefined standards of identity, strength, purity, and quality [13]. The quality control process in the pharmaceutical industry follows a systematic, multi-stage approach that spans from raw materials to final product release.
Raw Material Testing: All primary raw materials including active pharmaceutical ingredients (APIs), excipients, and packaging components are tested for identity, purity, and safety using sophisticated instrumental techniques such as chromatography (HPLC, UPLC) and spectroscopy (MS) [12]. This initial testing prevents contaminants from entering the production process and ensures consistency and reliability in downstream development [13].
In-Process Quality Control (IPQC): During manufacturing, critical process parameters including temperature, pH, and mixing speed are continuously monitored to detect deviations early [13]. These controls maintain batch consistency and minimize the risk of reprocessing. The implementation of Process Analytical Technology (PAT) enables real-time monitoring of Critical Quality Attributes (CQAs) and Critical Process Parameters (CPPs), allowing immediate adjustments during production rather than relying solely on end-product testing [12].
Finished Product Testing: Before release, every drug batch undergoes rigorous testing to verify it meets specifications for identity, strength, purity, and performance [13]. Common assessments include content uniformity, dissolution profiles, sterility, and impurity profiling using advanced methods like UPLC-MS/MS and elemental analysis [13]. Validated methods are essential for regulatory submissions and are required for all critical quality attributes tested during this stage.
Stability Testing: This examines how a drug's quality evolves under various environmental conditions throughout its shelf life [13]. Long-term and accelerated studies conducted under ICH guidelines require robust analytical follow-up with controlled storage, time-point analysis, and biomarker tracking to ensure ongoing safety and efficacy [13].
Quality Risk Management and Regulatory Alignment
Quality risk management in pharmaceuticals represents a proactive approach to identifying, assessing, and mitigating risks throughout manufacturing and quality control processes [13]. It is an integral part of a modern pharmaceutical quality system and is emphasized in ICH Q9 and Q10 guidelines, encompassing three key aspects:
- Risk assessment: Systematically evaluating potential sources of variability or failure in processes, equipment, and materials
- Risk control: Implementing measures to minimize or eliminate identified risks
- Risk review: Continuously monitoring and updating risk assessments as new information or technologies become available [13]
The Quality by Design (QbD) approach, outlined in ICH Q8, advocates for a science- and risk-based framework that emphasizes understanding the product and process from the earliest development stages [13]. This includes defining Critical Quality Attributes (CQAs), establishing critical process parameters, and developing validated analytical methods using UPLC-MS/MS, ICP-MS, and other advanced tools [13].
Table 2: Quality Control Stages and Corresponding Validated Methods
| QC Stage | Primary Quality Focus | Common Analytical Methods | Validation Parameters Emphasized |
|---|---|---|---|
| Raw Material Testing | Identity, purity, safety | HPLC, UPLC, MS, Spectroscopy | Specificity, Accuracy, LOD/LOQ [13] [12] |
| In-Process Control | Batch consistency, process parameters | PAT, Real-time sensors, pH, temperature monitoring | Precision, Robustness [12] |
| Finished Product Testing | Identity, strength, purity, performance | UPLC-MS/MS, Dissolution testing, Sterility testing, Elemental analysis | Accuracy, Precision, Specificity, Linearity [13] |
| Stability Testing | Shelf-life determination, degradation profiles | HPLC, MS, Forced degradation studies | Specificity, Accuracy, Precision [13] |
Drug Safety and Efficacy Assessment in Clinical Trials
Clinical Trial Methodology for Safety and Efficacy Evaluation
The assessment of drug safety and efficacy progresses through rigorously designed clinical trials that serve as the ultimate validation of a drug's therapeutic value. Clinical research in humans to evaluate the safety and efficacy of new drugs involves trials conducted in sequential phases [14]:
Phase 1 trials primarily evaluate safety and dosage in humans, typically involving 20-100 healthy volunteers. The goal is to determine the dose at which toxicity first appears and establish initial safety profiles [14].
Phase 2 trials assess efficacy in treating the target disease and further evaluate side effects. These studies involve several hundred people with the target disease and aim to determine optimal dose-response relationships while continuing safety assessment [14].
Phase 3 trials constitute large-scale studies (often hundreds to thousands of people) in more heterogeneous populations with the target disease. These studies compare the drug with existing treatments, placebos, or both to verify efficacy and detect adverse effects that may not have been apparent in earlier, smaller trials. Phase 3 trials provide the majority of safety data used for regulatory approval [14].
Phase 4 (postmarketing surveillance) occurs after FDA approval and includes formal research studies along with ongoing reporting of adverse effects. Phase 4 trials can detect uncommon or slowly developing adverse effects that are unlikely to be identified in smaller, shorter-term premarketing studies [14].
Methodological Challenges in Safety Assessment
Randomized controlled trials (RCTs), while considered the gold standard for establishing efficacy, face significant methodological challenges in comprehensively evaluating drug safety [15]:
Limited Statistical Power: Premarketing clinical trials are typically statistically underpowered to detect specific harms, either due to recruitment of low-risk populations or low intensity of event ascertainment [15]. The lack of statistical significance should not be interpreted as proof of clinical safety in an underpowered clinical trial. For example, the development program for varenicline largely excluded patients with psychiatric comorbidity and cardiovascular disease despite the high prevalence of these conditions among smokers [15].
Inadequate Ascertainment and Classification of Adverse Events: Inconsistencies in adverse effects reporting create substantial challenges. Adverse events are typically recorded as secondary outcomes in trials and are often not prespecified [15]. Misclassification is possible, particularly when outcomes are collected through spontaneous reports from trial participants rather than systematic monitoring.
Limited Generalizability: Clinical trial participants are often carefully selected, potentially excluding high-risk populations or those with comorbidities [15]. This lack of generalizability means that safety data may not extrapolate well to wider populations who may be taking different doses or formulations in real-world settings.
The Therapeutic Index (TI) has emerged as a key indicator illustrating the delicate balance between efficacy and safety, typically considered as the ratio of the highest non-toxic drug exposure to the exposure producing the desired efficacy [16]. Drugs with narrow TI (NTI drugs, TI ≤3) pose particular challenges, as tiny variations in dosage may result in therapeutic failure or serious adverse drug reactions [16]. Research has revealed that the targets of NTI drugs tend to be highly centralized and connected in human protein-protein interaction networks, with a greater number of similarity proteins and affiliated signaling pathways compared to targets of drugs with sufficient TI [16].
Diagram 1: Drug Efficacy-Safety Balance Assessment. This workflow illustrates the parallel evaluation of safety and efficacy throughout clinical development phases, culminating in the determination of the Therapeutic Index.
Emerging Trends and Future Directions
Innovative Approaches in Pharmaceutical Validation
As we approach 2025, pharmaceutical validation is undergoing a significant transformation, with companies leveraging innovative technologies and methodologies to ensure product quality and safety while improving efficiency [17]. Several key trends are shaping the future landscape:
Continuous Process Verification (CPV) represents an evolution from traditional validation approaches by focusing on ongoing monitoring and control of manufacturing processes throughout the product lifecycle [17]. Instead of relying solely on the traditional three-stage process validation framework, CPV emphasizes real-time data collection and analysis to continuously verify that processes remain in a state of control. Benefits include reduced downtime through early identification of potential issues, real-time quality control enabling immediate process adjustments, enhanced regulatory compliance, and reduced waste through more efficient production processes [17].
Data Integrity has become increasingly crucial as regulations become more stringent. Standards like ALCOA+ (Attributable, Legible, Contemporaneous, Original, and Accurate) have become critical to ensure all data is correctly managed and traceable [17]. Maintaining data integrity enhances trust with regulatory bodies and customers, reduces compliance issues through strong data management, and provides the foundation for accurate quality assessment [17].
Digital Transformation involves integrating advanced digital tools and automation to streamline processes, reduce manual errors, and improve efficiency [17]. This includes the implementation of digital twins, robotics, and Internet of Things (IoT) devices. Benefits include improved accuracy through minimized human error, efficiency gains from automated validation processes, and enhanced adaptability to respond faster to market demands and regulatory changes [17].
Real-Time Data Integration combines data from multiple sources into a single system, enabling pharmaceutical manufacturers to monitor production continuously and respond quickly to changes [17]. By integrating data across departments, companies gain comprehensive, up-to-date insights that inform immediate decision-making and adjustments during production, enhancing both quality and efficiency [17].
Advanced Predictive Models and Regulatory Science
The Advanced Research Projects Agency for Health (ARPA-H) has launched the Computational ADME-Tox and Physiology Analysis for Safer Therapeutics (CATALYST) program, which aims to create human physiology-based computer models to accurately predict safety and efficacy profiles for Investigational New Drug (IND) candidates [18]. This initiative addresses the fact that over 90% of drug candidates never reach the commercial market, with approximately half of these failures due to efficacy issues and a quarter resulting from safety issues occurring during clinical trials that were not predicted before first-in-human studies [18].
CATALYST seeks to lessen the use of insufficiently predictive preclinical animal studies with more accurate, faster, and cost-effective in silico drug development tools grounded in human physiology [18]. These technologies could significantly reduce the failure rate of drug candidates, ensure that medicines reaching clinical trials have confident safety profiles, and better protect trial participants. The program aims to reach clinical trial readiness based on validated, in silico safety data and help meet the targets of the U.S. Food and Drug Administration's Modernization Act [18].
Table 3: Emerging Trends in Pharmaceutical Validation for 2025
| Trend | Core Principle | Technological Enablers | Impact on Validation |
|---|---|---|---|
| Continuous Process Verification | Ongoing monitoring throughout product lifecycle | PAT, Real-time sensors, Data analytics | Shifts validation from periodic to continuous [17] |
| Advanced Data Integrity | ALCOA+ principles for complete data traceability | Blockchain, Electronic lab notebooks, Audit trails | Enhances data reliability and regulatory confidence [17] [12] |
| Digital Transformation | Integration of digital tools and automation | IoT, Robotics, Digital twins, AI | Reduces human error and improves efficiency [17] |
| Predictive Modeling | In silico prediction of safety and efficacy | AI, Machine learning, Physiological modeling | Potentially reduces preclinical animal studies [18] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Modern pharmaceutical validation relies on a suite of sophisticated reagent solutions and analytical technologies that enable precise characterization of drug products throughout development and manufacturing.
Table 4: Essential Research Reagent Solutions for Pharmaceutical Validation
| Reagent Solution | Primary Function | Application Context | Key Characteristics |
|---|---|---|---|
| Chromatographic Reference Standards | Quantification and identification of analytes | HPLC, UPLC method development and validation | High purity, well-characterized, traceable to reference materials [13] |
| Mass Spectrometry Reagents | Enable ionization and detection in MS systems | UPLC-MS/MS impurity profiling, biomarker quantification | High purity, volatility compatible with MS systems, stable isotope labeling [13] |
| Process Analytical Technology (PAT) | Real-time monitoring of critical process parameters | In-process control during manufacturing | Non-destructive, real-time capability, robust in manufacturing environment [12] |
| Stability Testing Materials | Accelerated and long-term stability assessment | Forced degradation studies, shelf-life determination | Controlled storage conditions, ICH guideline compliance [13] |
| Quality Control Reference Materials | System suitability testing and method verification | Finished product testing, quality attribute verification | Documented traceability, appropriate expiration dating [13] [12] |
Diagram 2: Pharmaceutical Validation Technology Ecosystem. This diagram illustrates the interconnected analytical technologies and data systems that support validation activities across the pharmaceutical product lifecycle.
The critical role of validated methods in ensuring drug safety, efficacy, and quality control remains unquestionable in modern pharmaceutical development and manufacturing. As the industry continues to evolve, with increasing molecule complexity and regulatory expectations, the fundamental principles of method validation provide the necessary scientific foundation for reliable analytical data.
The comprehensive validation of analytical methods—encompassing specificity, accuracy, precision, linearity, and robustness—serves as an essential requirement for establishing the reliability of pharmaceutical testing methodologies [10]. When properly implemented within a quality risk management framework aligned with ICH guidelines, validated methods ensure that medications consistently meet predefined quality standards while protecting patient safety [13].
Looking toward the future, emerging trends including continuous process verification, digital transformation, and predictive modeling are poised to transform validation practices from discrete, documentation-heavy exercises to integrated, science-based processes that provide real-time quality assurance [17]. Initiatives such as the ARPA-H CATALYST program represent promising advances toward more predictive safety and efficacy assessment, potentially reducing the high failure rate of drug candidates in clinical development [18].
For researchers, scientists, and drug development professionals, maintaining expertise in both fundamental validation principles and emerging methodologies will be essential for navigating the evolving landscape of pharmaceutical quality. The ongoing harmonization of regulatory standards and adoption of innovative technologies will continue to shape validation practices, but the ultimate goal remains unchanged: to ensure that every pharmaceutical product reaching patients is safe, effective, and of consistently high quality.
In the pharmaceutical industry, the lifecycle of an analytical method is a continuous process that ensures reliable data generation from initial development through routine commercial use. A well-managed lifecycle is fundamental to decision-making in drug development, impacting everything from early-stage API synthesis to quality control of final marketed products [19] [20]. The modern approach to this lifecycle, often termed Analytical Procedure Lifecycle Management (APLM), moves beyond a simple linear path to an integrated framework emphasizing robustness, predictability, and continuous verification [21] [22]. This guide explores the stages of the analytical method lifecycle, compares it with alternative approaches, and provides a detailed examination of the experimental protocols and validation parameters that ensure data integrity throughout a method's operational life.
The Three-Stage Analytical Method Lifecycle
Regulatory and industry best practices have formalized the analytical method lifecycle into three defined stages, which align with process validation concepts for more efficient and reliable development [20] [21].
Stage 1: Method Design and Development
This initial stage transforms defined requirements into a working analytical procedure. The process begins with establishing an Analytical Target Profile (ATP), a prospective outline that specifies the method's performance requirements and its intended purpose [20] [21]. The ATP defines what the method needs to achieve, such as specific sensitivity (LOD, LOQ), precision, and accuracy levels, before any development work begins [19]. Method selection is then driven by marrying the "method requirement," "analyte properties," and "technique capability" to ensure final robustness [19]. For instance, Supercritical Fluid Chromatography (SFC) may be selected over Reverse-Phase Liquid Chromatography (RPLC) for chiral separations, water-sensitive analytes, or compounds with extreme hydrophobicity [19]. Development activities employ risk assessment tools and statistical experimental design (e.g., Design of Experiments) to understand method performance characteristics and establish a controlled, robust method [20].
Stage 2: Method Performance Qualification
This stage, traditionally known as validation, provides experimental confirmation that the developed analytical procedure consistently meets the criteria outlined in the ATP [20]. It confirms that the method delivers reproducible data suitable for its intended use, whether for quality control (QC), stability testing, or supporting pharmacokinetic studies [10] [1]. The activities in this phase are comprehensive, as detailed in the experimental protocols section below, and include testing for parameters such as accuracy, precision, specificity, and linearity [10] [23]. The finalization of the Analytical Control Strategy (ACS) also occurs here, defining the ongoing criteria for acceptable performance of the method during its routine use [20].
Stage 3: Continued Method Performance Verification
The lifecycle does not end with qualification. This ongoing stage provides assurance that the analytical procedure remains in a state of control during its routine use in a quality control laboratory [20] [21]. It involves continuous monitoring of system suitability and performance quality control data against pre-defined acceptance criteria [21]. Any deviations or trends are assessed through a structured change control process. This stage also encompasses any required method transfers between laboratories or sites, which must be documented and verified to ensure the method performs consistently in new environments [24] [1]. Ultimately, this phase ensures the method's reliability over many years of a product's commercial life [19].
The following diagram illustrates the interconnected nature of these three stages and their key components, including the essential feedback loops for continuous improvement.
Core Validation Parameters: The Pillars of Method Reliability
The qualification of an analytical method (Stage 2) rests on the demonstration of specific validation parameters. These parameters are the pillars that ensure the method is fit for its purpose and will generate reliable results throughout its lifecycle [10] [23].
Table 1: Key Analytical Method Validation Parameters and Their Definitions
| Validation Parameter | Definition and Purpose | Typical Acceptance Criteria |
|---|---|---|
| Accuracy | The degree of agreement between test results and the true value. Measures the exactness of the method [10]. | Recovery of 98–102% for drug substance, 98–102% for drug product (per ICH) [1]. |
| Precision | The degree of agreement among individual test results from multiple samplings. Measures reproducibility [10]. | RSD ≤ 2% for assay of drug substance, ≤ 3% for finished product [10] [1]. |
| Specificity/Selectivity | The ability to assess unequivocally the analyte in the presence of components that may be expected to be present (e.g., impurities, matrix) [10] [1]. | No interference observed from blank, placebo, or known impurities at the retention time of the analyte. |
| Linearity | The ability of the method to obtain test results proportional to the concentration of the analyte [10] [23]. | Correlation coefficient (r) > 0.998 [10] [1]. |
| Range | The interval between the upper and lower levels of analyte that have been demonstrated to be determined with precision, accuracy, and linearity [10]. | Typically 80-120% of the test concentration for assay [1]. |
| Limit of Detection (LOD) | The lowest concentration of an analyte that can be detected, but not necessarily quantified. Signal-to-noise ratio is typically 3:1 [10]. | Visual or statistical determination of a concentration with an S/N of 3:1. |
| Limit of Quantitation (LOQ) | The lowest concentration of an analyte that can be quantified with acceptable precision and accuracy. Signal-to-noise ratio is typically 10:1 [10]. | Visual or statistical determination of a concentration with an S/N of 10:1 and precision of ≤ 5% RSD. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., temperature, flow rate) [23] [22]. | The method meets system suitability criteria despite deliberate parameter fluctuations. |
Comparative Analysis: SFC vs. RPLC in Method Lifecycle Implementation
The choice of analytical technique fundamentally impacts the method's lifecycle trajectory. While Reversed-Phase Liquid Chromatography (RPLC) is the most widely employed technique, Supercritical Fluid Chromatography (SFC) offers distinct advantages for specific applications, affecting development time, robustness, and sustainability [19].
Table 2: Lifecycle Comparison of SFC and RPLC for Pharmaceutical Analysis
| Lifecycle Aspect | Supercritical Fluid Chromatography (SFC) | Reversed-Phase Liquid Chromatography (RPLC) |
|---|---|---|
| Technique Selection Driver | Optimal for chiral separations, water-labile compounds, and analytes with low or high LogP [19]. | Default technique for many molecular classes; driven by analyst familiarity and instrument availability [19]. |
| Method Development | High-throughput screening with open-access systems can significantly decrease development time [19]. | Can be complex and time-consuming, especially for analytes requiring specialized stationary phases or ion-pairing reagents [19]. |
| Analysis Time & Solvent Use | Faster separations due to low viscosity and high diffusivity of supercritical CO₂. Uses predominantly "green" CO₂ with minor organic modifier [19]. | Often longer run times. Uses large volumes of organic solvents (e.g., acetonitrile, methanol), which have environmental and cost implications [19]. |
| Validation & Transfer Success | Modern instrumentation is reliable enough to meet strict validation requirements, with successful transfers to commercial QC labs [19]. | Well-established validation protocols; widely accepted by regulators. |
| Routine Performance in QC | Proven to be very reliable in a GMP environment. At one Pfizer site, over 110 individual release runs were completed without major issues [19]. | The industry standard with predictable performance, though methods can be prone to issues like column blockage for highly lipophilic analytes [19]. |
| Representative Application | Chiral purity of Ritlecitinib; Determination of stereoisomer content in Nirmatrelvir (Paxlovid) [19]. | The most widely used technique for quality control across many small-molecule drug classes. |
Supporting Experimental Data: A direct comparison within Pfizer demonstrated the lifecycle efficiency of SFC. For an oil-based injectable drug product, a risk assessment of a potential RPLC method highlighted risks of matrix accumulation, analyte precipitation, and intensive sample preparation. In contrast, an SFC method was developed in a single day, leveraging the solubility of the API and formulation oils in the CO₂-organic mobile phase. This SFC method achieved good separation of the oil matrix and the API with simpler sample preparation, whereas the RPLC approach was projected to require several weeks of development and troubleshooting [19].
Detailed Experimental Protocols for Key Validation Parameters
To ensure the reliability of data generated throughout the method's lifecycle, specific experimental protocols are followed during the Method Performance Qualification stage (Stage 2).
Protocol for Determining Accuracy
Accuracy is typically determined by analyzing a minimum of nine determinations over a minimum of three concentration levels covering the specified range (e.g., 80%, 100%, 120% of the target concentration) [10] [1].
- Procedure: The sample matrix is spiked with a known concentration of the analyte standard. Each concentration level is analyzed in triplicate.
- Calculation: The recovery (%) for each level is calculated using the formula: (Measured Concentration / Theoretical Concentration) × 100. The mean recovery across all levels is then reported [10].
- Acceptance Criteria: For assay of a drug substance or product, recovery is typically 98–102% [1].
Protocol for Determining Precision
Precision is validated at multiple levels: repeatability, intermediate precision, and reproducibility [10] [23].
- Repeatability: Six replicate injections of a single, homogeneous sample at 100% of the test concentration. The standard deviation (SD) and relative standard deviation (%RSD) of the results are calculated [10].
- Intermediate Precision: The same procedure is repeated on a different day, by a different analyst, or using a different instrument within the same laboratory. The results from both sets are combined to calculate the overall SD and %RSD.
- Calculation: %RSD = (Standard Deviation / Mean) × 100.
- Acceptance Criteria: The Horwitz equation can provide guidance, but for assay methods, an RSD of ≤ 2% is often expected [10].
Protocol for Determining Linearity and Range
Linearity demonstrates that the analytical procedure produces results directly proportional to analyte concentration.
- Procedure: A series of standard solutions at a minimum of five concentration levels (e.g., 50%, 75%, 100%, 125%, 150% of the target concentration) is prepared and analyzed [10] [1].
- Calculation: A linear regression curve is plotted (Peak Response vs. Concentration). The correlation coefficient (r), y-intercept, and slope of the regression line are calculated. The residual sum of squares is also evaluated [10].
- Acceptance Criteria: A correlation coefficient (r) of > 0.998 is generally expected for assay methods [1].
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of an analytical method throughout its lifecycle depends on a foundation of high-quality materials and reagents.
Table 3: Essential Research Reagent Solutions for Analytical Method Development and Validation
| Item | Function and Importance in the Lifecycle |
|---|---|
| Reference Standards | Highly characterized substance of known purity and identity; essential for method development, calibration, and quantification. The quality of the standard directly impacts the accuracy of the entire method [1]. |
| Chromatographic Columns | The stationary phase is critical for achieving the required selectivity and resolution. Different chemistries (C18, chiral, HILIC, etc.) are selected based on the analyte's properties defined in the ATP [19]. |
| HPLC/SFC Grade Solvents | High-purity mobile phase components are necessary to maintain system health and prevent baseline noise, ghost peaks, and method variability that can compromise data in routine use [19]. |
| Sample Preparation Solvents & Reagents | Solvents for extraction, dilution, or derivatization must be compatible with both the sample matrix and the analytical technique to ensure accurate analyte recovery and stability [19] [1]. |
| System Suitability Standards | A prepared mixture used to verify that the chromatographic system is adequate for the intended analysis. It is a critical checkpoint before every analytical run in routine QC (Stage 3) [21]. |
The journey of an analytical method from development to routine use is not a one-time event but a dynamic, managed lifecycle. Adopting the structured, three-stage framework of Procedure Design, Performance Qualification, and Continued Verification ensures methods are robust, reliable, and compliant with evolving regulatory standards like ICH Q14 and USP <1220> [20] [21]. This holistic view, supported by rigorous validation protocols and a clear Analytical Target Profile, minimizes the resource burden of downstream redevelopment and troubleshooting [19]. As the industry continues to advance, the integration of Quality by Design (QbD) principles and lifecycle management will be paramount for pharmaceutical developers and researchers to ensure the consistent delivery of high-quality, safe, and effective medicines to patients.
From Theory to Practice: Implementing and Applying Key Validation Parameters
Experimental Designs for Assessing Specificity and Selectivity in Complex Matrices
The analysis of target compounds in complex matrices such as biological fluids, environmental samples, and food products presents significant analytical challenges due to the presence of numerous interfering substances that can compromise method reliability. Within method validation, specificity and selectivity are critical parameters that determine an analytical procedure's ability to accurately measure the analyte amidst these potential interferents [10]. While often used interchangeably, a distinction can be made where specificity refers to the method's ability to assess the analyte unequivocally in the presence of expected components, whereas selectivity describes its ability to differentiate the analyte from other analytes in the mixture [25] [10]. This guide objectively compares contemporary experimental designs for evaluating these parameters, focusing on mass spectrometry-based techniques that have become the cornerstone for high-quality quantitative analysis in complex matrices [26] [27].
Fundamental Concepts and Validation Parameters
According to international validation guidelines, the selectivity of an analytical method is defined as its ability to measure accurately an analyte in the presence of interferences that may be expected to be present in the sample matrix [10]. This is typically checked by examining chromatographic blanks in the expected time window of the analyte peak to confirm the absence of co-eluting signals [10]. Method validation requires testing multiple attributes to ensure the procedure provides useful and valid data, with specificity/selectivity being foremost among other parameters including accuracy, precision, linearity, and limits of detection and quantification [10].
The fundamental challenge in analyzing complex matrices is the matrix effect (ME), defined as the combined effects of all sample components other than the analyte on the measurement [27]. In mass spectrometry, these effects occur when interference species alter ionization efficiency in the source when co-eluting with the target analyte, causing either ion suppression or enhancement [27]. The extent of ME is variable and unpredictable—the same analyte can show different MS responses in different matrices, and the same matrix can affect different analytes differently [27].
Comparative Experimental Designs and Methodologies
Multiple Reaction Monitoring (MRM) and MRM³
Traditional MRM (MRM²) on triple quadrupole mass spectrometers has become the technique of choice for highly sensitive and selective quantification in biological matrices [26]. This approach provides two stages of mass filtering: selection of a precursor ion in the first quadrupole (Q1) and selection of a characteristic product ion after fragmentation in the second quadrupole (Q2) [26]. While this typically provides sufficient selectivity, detection can still be impacted by high background or interferences from the matrix that share the same transition [26].
MRM³ quantification represents an advanced workflow available on QTRAP systems that adds a third dimension of selectivity [26]. In this approach, the analyte ion is first selected in Q1, fragmented in the Q2 collision cell, then a specific product ion is isolated and fragmented again in the linear ion trap (LIT), with second-generation product ions scanned out to the detector [26]. This additional fragmentation step provides superior selectivity by eliminating interferences that might co-elute and share identical precursor and first-generation product ions with the analyte.
Table 1: Comparison of MRM² and MRM³ Performance Characteristics
| Parameter | Traditional MRM (MRM²) | MRM³ Quantification |
|---|---|---|
| Selectivity Principle | Two stages of mass selection (Q1, Q3) | Three stages of mass selection (Q1, LIT isolation, LIT fragmentation) |
| Interference Removal | Effective for most applications | Complete removal of tough interferences with same MRM transition and retention time |
| Sensitivity Impact | High sensitivity for most analytes | Potential for up to 100x higher sensitivity in LIT mode with Linear Accelerator technology |
| Best Applications | Routine analysis of low-complexity samples | Complex matrices with high background, difficult separations, simplified sample preparation |
| Limitations | Susceptible to interferences with identical transitions | Requires specialized instrumentation (QTRAP systems), slightly slower cycle times |
Experimental Protocol for MRM³ Method Development
- System Configuration: Utilize a QTRAP system with hybrid triple quadrupole linear ion trap configuration.
- Initial MS/MS Optimization: Infuse pure analyte standard to determine optimal precursor ion and most abundant product ions using traditional MRM.
- Ion Trap Parameter Optimization: For the most abundant product ion from step 2, optimize trap collision energy and excitation time for generation of second-generation product ions.
- MRM³ Method Setup: Configure the method with:
- Q1 selection at unit resolution (0.7 Th FWHM)
- Q2 collision energy optimized for first fragmentation
- LIT isolation of selected product ion
- Application of single frequency/narrow band excitation for second fragmentation
- Mass scan of second-generation product ions
- Chromatographic Optimization: Employ appropriate LC separation to minimize matrix components entering the MS simultaneously with the analyte.
- Validation: Compare method performance against traditional MRM using spiked matrix samples to quantify improvement in selectivity and reduction of background interference.
The following workflow diagram illustrates the fundamental operational principles of MRM² versus MRM³:
High-Resolution Mass Spectrometry (HRMS) and Chromatographic Solutions
As an alternative to MRM³ approaches, high-resolution mass spectrometry provides another dimension of selectivity through accurate mass measurements [28]. When compounds have identical or very close m/z values, HRMS can resolve minimal mass differences that triple quadrupole instruments cannot distinguish [28]. This approach is particularly valuable for non-targeted analysis and when analyzing compounds with similar fragmentation patterns.
Chromatographic optimization remains a fundamental strategy for improving selectivity [29]. Recent advances include:
- Multidimensional chromatography: Comprehensive two-dimensional LC (LC×LC) for increased peak capacity
- Advanced stationary phases: Novel chemistries providing alternative separation mechanisms
- On-line enrichment methodologies: Solid-phase microextraction (SPME) and other concentration techniques that also clean up samples [29]
Table 2: Comparison of Selectivity-Enhancement Techniques for Complex Matrices
| Technique | Mechanism of Selectivity | Best for Analyzing | Complexity/Cost | Key Limitations |
|---|---|---|---|---|
| Traditional MRM | Two mass filtering stages | Most small molecules in moderate matrix | Moderate | Interferences with same transition |
| MRM³ | Three mass filtering stages | Small molecules, peptides, protein biomarkers | High | Requires specific instrumentation |
| High-Resolution MS | Accurate mass measurement | Non-targeted analysis, unknown compounds | High | Lower sensitivity than triple quad |
| Multidimensional LC | Orthogonal separation mechanisms | Highly complex samples (e.g., proteomics) | High | Method development complexity |
| Advanced SPME Fibers | Selective extraction/enrichment | Trace analysis in environmental/biological samples | Moderate | Fiber lifetime, carryover potential |
Experimental Protocols for Assessing Matrix Effects
Post-Column Infusion Method
The post-column infusion method, initially proposed by Bonfiglio et al., provides a qualitative assessment of matrix effects throughout the chromatographic run [27].
Protocol:
- Prepare a blank sample extract using the intended sample preparation procedure.
- Inject the blank extract onto the LC column while maintaining a constant mobile phase flow.
- Using a T-piece, introduce a constant flow of analyte standard post-column (after separation but before MS ionization).
- Monitor the analyte signal throughout the chromatographic run.
- Identify regions of ion suppression or enhancement as decreases or increases in the steady analyte signal.
Data Interpretation: Signal suppression appears as negative peaks (dips) in the chromatogram, indicating regions where matrix components co-elute and suppress ionization of the analyte. This method is particularly valuable during method development to identify optimal chromatographic conditions and retention times that minimize matrix effects [27].
Post-Extraction Spike Method
The post-extraction spike method, developed by Matuszewski et al., provides quantitative assessment of matrix effects [27].
Protocol:
- Prepare blank matrix samples from at least six different sources.
- Process these blanks through the entire sample preparation procedure.
- Spike the analyte at known concentrations into the processed blank extracts (post-extraction).
- Prepare equivalent concentration standards in pure solvent.
- Analyze both sets and compare the responses.
Calculation: Matrix Effect (ME) = (Peak area of post-spiked sample) / (Peak area of standard solution) × 100%
An ME of 100% indicates no matrix effect, <100% indicates suppression, and >100% indicates enhancement. This method is particularly valuable for evaluating lot-to-lot variability of matrix effects [27].
Slope Ratio Analysis
The slope ratio analysis method, a modification by Romero-Gonzáles and Sulyok, extends the post-extraction spike approach across a concentration range [27].
Protocol:
- Prepare matrix-matched calibration standards at multiple concentration levels using blank matrix from at least six different sources.
- Prepare solvent-based calibration standards at identical concentrations.
- Analyze both sets and construct calibration curves.
- Compare the slopes of the matrix-matched versus solvent-based calibration curves.
Calculation: Matrix Effect = (Slope of matrix-matched calibration) / (Slope of solvent calibration) × 100%
This approach provides a more comprehensive assessment of matrix effects across the analytical range rather than at a single concentration level [27].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Specificity/Selectivity Experiments
| Reagent/Material | Function in Experimental Design | Application Context |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Compensates for matrix effects and extraction variability; ideal for quantitative accuracy | Bioanalytical method development, pharmacokinetic studies |
| Molecularly Imprinted Polymers (MIPs) | Provides highly selective extraction; mimics antibody-antigen recognition | Selective extraction of target analytes from complex matrices |
| Phospholipid Removal Plates | Selectively removes phospholipids (major source of matrix effects in biological samples) | Plasma/serum analysis to reduce ionization suppression |
| Diversified Blank Matrices | Assess matrix effects across different sources; essential for method validation | All bioanalytical methods (use at least 6 different lots) |
| Hybrid Triple Quadrupole-LIT Systems | Enables MRM³ capability for ultimate selectivity in challenging applications | Metabolomics, biomarker verification, complex impurity detection |
| Appropriate Surrogate Matrices | Alternative to scarce or expensive biological matrices; demonstrates similar MS response | Analysis of endogenous compounds where true blank matrix unavailable |
The selection of an appropriate experimental design for assessing specificity and selectivity must be guided by the particular analytical challenge, matrix complexity, and required sensitivity. For most routine applications, traditional MRM provides an excellent balance of performance and practicality. When facing persistent interferences that compromise data quality, MRM³ offers a powerful solution with superior selectivity, though it requires specialized instrumentation. For comprehensive method validation, a combination of post-column infusion (for qualitative assessment of problematic chromatographic regions) and post-extraction spike methods (for quantitative determination of matrix effects) provides the most complete picture of method performance. The fundamental principle remains that early and thorough evaluation of specificity and selectivity during method development prevents analytical failures during routine application, ultimately generating the dependable data required for critical decision-making in pharmaceutical, clinical, and environmental applications.
Protocols for Determining Accuracy (through Spiking/Recovery) and Precision (Repeatability, Intermediate Precision)
In pharmaceutical analysis and bioanalytical research, validating a method is crucial to confirm that it is suitable for its intended purpose, ensuring the reliability and consistency of results [30]. Accuracy and precision are two fundamental validation parameters that measure different aspects of this reliability. Accuracy refers to the closeness of agreement between a measured value and a true or accepted reference value [31] [32]. It is often assessed through spike-and-recovery experiments, which determine if a sample matrix affects the detection of an analyte compared to a standard diluent [33] [34]. Precision, on the other hand, expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under specified conditions [35] [31]. It is typically subdivided into repeatability (short-term, same-operator precision) and intermediate precision (longer-term, within-laboratory variations) [35] [36]. This guide objectively compares the performance of different methodological approaches for assessing these critical parameters, providing detailed protocols and representative data to support robust analytical practices.
Determining Accuracy through Spike-and-Recovery Experiments
Core Principles and Purpose
The spike-and-recovery experiment is designed to validate the accuracy of an assay, such as an ELISA, by quantifying the potential matrix effects of a biological sample [33] [34]. The fundamental question it answers is whether the sample matrix (e.g., serum, urine, culture supernatant) yields the same recovery of a known analyte as the standard diluent used for the calibration curve. When an analyte is spiked into a natural sample matrix, components of that matrix can sometimes interfere with antibody-analyte binding, leading to either an enhanced or diminished signal compared to the pure standard. A successful spike-and-recovery test confirms that the matrix does not interfere, thereby justifying the use of the standard curve for calculating analyte concentrations in unknown samples [33].
Detailed Experimental Protocol
The following protocol, adapted from established methodologies, outlines the key steps for performing a spike-and-recovery assessment [33] [34]:
- Preparation of Spiked Samples: A known quantity of the purified analyte (the "spike") is added to the natural sample matrix. The concentration of the spike should be within the quantitative range of the assay.
- Preparation of Control: An identical quantity of the analyte is spiked into the standard diluent (the matrix used to prepare the standard curve). This serves as the control, representing 100% ideal recovery.
- Assay Execution: Both the spiked sample matrix and the spiked standard diluent are analyzed using the assay (e.g., ELISA), and their responses are measured.
- Data Calculation: The percentage recovery is calculated using the formula:
- % Recovery = (Observed Concentration in Spiked Sample / Observed Concentration in Spiked Diluent) × 100%
- The observed concentration for the spiked sample matrix should ideally be corrected by subtracting the endogenous level of the analyte measured in an unspiked aliquot of the same sample [33].
Performance Data and Acceptance Criteria
The table below summarizes typical spike-and-recovery results for a recombinant human IL-1 beta ELISA in human urine samples, demonstrating the calculation of percent recovery [33].
Table 1: Representative ELISA Spike-and-Recovery Data for Recombinant Human IL-1 Beta in Human Urine
| Sample (n) | Spike Level | Expected Concentration (pg/mL) | Observed Concentration (Mean, pg/mL) | Recovery % |
|---|---|---|---|---|
| Diluent Control | Low (15 pg/mL) | 17.0 | 17.0 | 100.0 |
| Urine (9) | Low (15 pg/mL) | 17.0 | 14.7 | 86.3 |
| Diluent Control | Medium (40 pg/mL) | 44.1 | 44.1 | 100.0 |
| Urine (9) | Medium (40 pg/mL) | 44.1 | 37.8 | 85.8 |
| Diluent Control | High (80 pg/mL) | 81.6 | 81.6 | 100.0 |
| Urine (9) | High (80 pg/mL) | 81.6 | 69.0 | 84.6 |
The acceptance criteria for recovery are context-dependent but a common benchmark in immunoassays is a recovery of 80–120% [34]. Results outside this range indicate significant matrix interference. In the example above, the consistent ~85-86% recovery across spike levels suggests a constant matrix effect, which may be correctable by modifying the sample diluent [33]. The following workflow diagram summarizes the spike-and-recovery process and troubleshooting paths.
Determining Precision: Repeatability and Intermediate Precision
Core Principles and Definitions
Precision measures the random error or the scatter of results under specified conditions [37] [31]. It is hierarchically evaluated at different levels:
- Repeatability (also called intra-assay precision) expresses the precision under the same operating conditions over a short period of time (e.g., one day, one run) using the same instrument, operator, and reagents. It represents the smallest possible variation in results [35] [31].
- Intermediate Precision (also called within-laboratory precision) expresses the within-laboratory variation observed over an extended period (e.g., several months). It accounts for the effects of random events such as different analysts, different instruments, different reagent lots, different calibration cycles, and different days [35] [36]. Because it incorporates more sources of variability, the standard deviation of intermediate precision is always larger than that of repeatability [35].
Detailed Experimental Protocol and Statistical Analysis
A common approach to evaluate both repeatability and intermediate precision is a nested experimental design, such as the 20x2x2 design recommended by CLSI EP05A3 [37]. This involves:
- 20 test days
- 2 runs per day
- 2 replicate measurements per run
- All performed on a single, homogeneous sample [37].
The data from this design are analyzed using a nested Analysis of Variance (ANOVA) to partition the total variance into components attributable to different factors (e.g., day-to-day, run-to-run, and within-run). The steps for a 20x2x2 design are as follows [37]:
- Data Collection: Perform the 20x2x2 experiment, resulting in 80 data points.
- Model Fitting: Fit a nested components-of-variance model (e.g.,
y ~ day/runin R), where "run" is nested within "day". - Variance Component Estimation: Calculate the variance components for each factor:
- Within-run variance (V~error~) = MS~error~ (This represents repeatability)
- Between-run variance (V~run~) = (MS~run~ - MS~error~) / n~rep~
- Between-day variance (V~day~) = (MS~day~ - MS~run~) / (n~run~ * n~rep~)
- Precision Calculation: Calculate the standard deviation (SD) and percent coefficient of variation (%CV) for each component.
- Repeatability (within-run) Precision: SD~repeatability~ = √V~error~ ; %CV~R~ = (SD~repeatability~ / Mean) × 100
- Intermediate Precision (within-lab): SD~intermediate~ = √(V~day~ + V~run~ + V~error~) ; %CV~WL~ = (SD~intermediate~ / Mean) × 100
Performance Data and Acceptance Criteria
The table below illustrates hypothetical results from a precision study for a drug substance content determination, showing how different factors contribute to overall variability.
Table 2: Example Precision Study Results for a Drug Substance Assay
| Precision Level | Experimental Conditions | Mean (mg) | Standard Deviation (SD) | % Relative Standard Deviation (%RSD) |
|---|---|---|---|---|
| Repeatability | Single analyst, same day, same instrument (n=6) | 1.46 | 0.019 | 1.29% |
| Intermediate Precision | Two analysts, different instruments (n=12) | 1.40 | 0.057 | 4.09% |
The data show that while an analyst can be highly precise on their own equipment (low %RSD for repeatability), the inclusion of another analyst and a different instrument introduces more variability, reflected in the higher %RSD for intermediate precision [36]. Acceptance criteria for precision are method-specific, but a common requirement is that the %RSD should not be greater than 2.0% for assay values in pharmaceutical quality control [30]. The following diagram visualizes the hierarchical relationship and experimental design of precision parameters.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of accuracy and precision studies requires specific reagents and materials. The following table details key research reagent solutions and their functions in these validation experiments.
Table 3: Essential Research Reagent Solutions for Accuracy and Precision Studies
| Item | Function in Validation | Example Application |
|---|---|---|
| Purified Analyte/Standard | Serves as the known reference material for preparing calibration curves and spiking solutions. | Recombinant human IL-1 beta protein used for spiking in recovery experiments [33]. |
| Appropriate Biological Matrix | The sample environment (e.g., serum, plasma, urine) from the species of interest, used to assess matrix effects. | Human urine samples used to test for interference in an ELISA [33]. |
| Standard Diluent | The buffer or solution used to prepare the standard curve; its composition is optimized for the assay. | Phosphate-buffered saline (PBS) with 1% BSA used to dilute the recombinant protein standard [33]. |
| Sample Diluent | The buffer or solution used to dilute the biological sample. It may differ from the standard diluent to improve recovery. | PBS without additional protein used as a diluent for serum samples to mitigate matrix effects [33] [34]. |
| Reference Material (for Trueness) | A certified material with a known concentration of analyte, used to assess the bias (trueness) of the method. | Used in accuracy studies to compare the mean of a large number of test results to the accepted reference value [31]. |
| Homogeneous Sample Pool | A single, well-mixed sample used for precision studies to ensure that all variability measured is from the method, not the sample. | A large volume of drug substance solution or pooled serum used in a 20-day precision study [37] [36]. |
In the highly regulated world of pharmaceutical development, a phase-appropriate approach to analytical method validation has emerged as a widely accepted and adopted strategy to support clinical development of biologics and cell and gene therapies (CGT) [38]. This tailored framework aligns validation rigor with clinical development stages, balancing resource efficiency with regulatory compliance throughout the drug development lifecycle. As programs advance from preclinical research to commercial marketing applications, the extent of method validation escalates progressively from initial "fit-for-purpose" assessments to fully validated methods meeting stringent FDA/EMA/ICH guidelines [39].
The fundamental principle underpinning this approach recognizes that different clinical phases carry distinct requirements and risks [40]. Early development focuses on safety assessment and requires methods sufficient to support initial decision-making, while later stages demand robust, reproducible methods capable of confirming efficacy and supporting market approval [39]. This strategic framework enables sponsors to allocate resources efficiently while maintaining scientific rigor appropriate to each development phase, ultimately providing a faster and more efficient route to product development that complies with regulatory standards [38].
Phase-Appropriate Validation Across Clinical Development Stages
Preclinical to Phase 1: Fit-for-Purpose Methods
During early development stages, analytical methods require demonstration that they are appropriately controlled and provide reliable results for making decisions [38] [39]. The focus is on establishing methods with sufficient accuracy, reproducibility, and biological relevance to support early safety and pharmacokinetic studies [39]. According to regulatory guidance, validation of analytical procedures is usually not required for original investigational new drug submissions for Phase 1 studies; however, it should be demonstrated that test methods are appropriately controlled [38].
For early development, method development activities are performed to establish methods to address potential critical quality attributes (pCQAs) before initiating first-in-human studies [38]. At this stage, it is not unusual to have a majority (if not all) of quality attributes considered as pCQAs [38]. The analytical target profile (ATP) is defined during this period as a prospective, technology-independent description of the desired performance of an analytical procedure [38].
Table: Preclinical to Phase 1 Validation Focus
| Development Element | Preclinical to Phase 1 Requirements |
|---|---|
| Assay Stage | Stage 1 - Fit for Purpose [39] |
| Primary Focus | Screening/exploratory studies; early safety and dosing [39] |
| Key Parameters | Accuracy, reproducibility, biological relevance [39] |
| Regulatory Documentation | Method summaries and available qualification data in clinical trials application [38] |
| Typical Experiments | 2-6 experiments to meet Fit-for-Purpose standards [39] |
Phase 2 Clinical Studies: Method Qualification
As development advances into Phase 2 clinical studies, the validation focus shifts to method qualification with intermediate precision, accuracy, specificity, linearity, and range [39]. These enhanced capabilities support dose optimization, safety assessment, and process development activities [39]. The goal at this stage is to qualify assays through evaluating and refining critical performance parameters that will ultimately support successful assay validation [39].
During Phase 2, CQAs are refined as new methods are developed and additional process/product knowledge is gained [38]. Method qualification activities demonstrate that methods are fit for the intended purpose and perform in line with the ATP [38]. This typically involves a minimum of three replicate experiments following the finalized assay protocol to establish preliminary acceptance criteria and assay performance metrics [39]. For more robust qualification, two analysts typically conduct at least three independent runs, each using three assay plates to enable statistical analysis [39].
Table: Phase 2 Qualification Parameters and Standards
| Performance Parameter | Phase 2 Qualification Standards |
|---|---|
| Specificity/Interference | Drug matrix/excipients don't interfere with assay signal; negative controls show no activity [39] |
| Accuracy | EC50 values for Reference Standard and Test Sample agree within 20% [39] |
| Precision (Replicates) | %CV for replicates within 20% [39] |
| Precision (Curve Fit) | Goodness-of-fit to 4-parameter curve >95% [39] |
| Intermediate Precision | Relative Potency variation across experiments has CV <30% [39] |
| Parallelism | Dose-response curves of Reference Standard and Test Sample are parallel [39] |
| Experimental Requirements | 3-8 experiments to meet Qualified Assay Standards [39] |
Phase 3 to Commercialization: Full Method Validation
Prior to Biologics License Application (BLA) or New Drug Application (NDA) submission, assays must be fully validated to demonstrate statistical reproducibility, robustness, and minimal variability across different analysts, facilities, equipment, and time [39]. These validated methods support confirmatory efficacy and safety studies, lot release, stability testing, and post-market requirements [39].
GMP compliance becomes essential at this stage, with assays performed under Good Manufacturing Practice conditions with complete documentation and oversight from Quality Control and Quality Assurance teams [39]. The validation process typically requires 6-12 experiments to meet GMP validated assay standards [39]. The International Council for Harmonisation (ICH) guidelines, particularly ICH Q2(R2), provide clear direction on validation requirements for these late stages [40].
The validated assay must perform consistently, demonstrating it is robust, accurate, specific, and precise, supporting analysis of both activity (e.g., potency) and long-term stability of test samples [39]. A detailed Standard Operating Procedure (SOP) is essential at this stage, enabling any qualified operator to execute the method reliably [39].
Experimental Protocols and Validation Parameters
Core Validation Parameters and Methodologies
Throughout all development phases, specific validation parameters are assessed with appropriate rigor based on phase requirements. The ICH Q2(R2) guideline outlines essential validation characteristics including specificity, accuracy, precision, linearity, range, LOD, LOQ, and robustness [10].
Specificity and Selectivity: The ability to measure accurately an analyte in the presence of interferences that may be expected to be present in the sample matrix [10]. This is checked by examining chromatographic blanks in the expected time window of the analyte peak [10].
Precision: The degree of agreement among individual test results when the procedure is applied repeatedly to multiple samplings [10]. Precision is measured by injecting a series of standards or analyzing series of samples from multiple samplings from a homogeneous lot [10]. From the measured standard deviation and mean values, precision as relative standard deviation (% RSD) is calculated [10]. The Horwitz equation provides guidance for acceptable percent of relative standard deviation results for precision [10].
Accuracy: The degree of agreement of test results generated by the method to the true value [10]. Accuracy is measured by spiking the sample matrix of interest with a known concentration of analyte standard and analyzing the sample using the "method being validated" [10]. The procedure and calculation for accuracy (as % recovery) varies based on matrix type [10].
Linearity and Range: The ability to elicit test results that are directly proportional to the concentration of analytes within a given range [10]. Linearity is determined by injecting a series of standards at a minimum of five different concentrations in the range of 50-150% of the expected working range [10]. The range is the interval between the upper and lower levels that have been demonstrated to be determined with precision, accuracy and linearity using the set method [10].
LOD and LOQ: The limit of detection (LOD) represents the lowest concentration at which the instrument can detect but not quantify (signal-to-noise ratio 1:3), while the limit of quantitation (LOQ) is the lowest concentration at which the instrument can detect and quantify (signal-to-noise ratio 1:10) [10]. These can be determined through linear regression analysis of serial dilutions [10].
Method Bridging and Transfer
When new/revised methods with improved robustness, sensitivity, accuracy, or operational simplicity are developed to support clinical lot release and stability, replacing existing methods requires a bridging study [38]. Based on the ICH Q14 guideline on analytical procedure development, the design and extent of studies needed to support the change include an appropriate bridging strategy to establish the numerical relation between the reportable values of each method and its impact on product specification [38].
The selected bridging strategy should be risk-based and depend on product development stage, ongoing studies, the number and retention of historical batches, and other factors [38]. At a minimum, bridging studies should be anchored to a historical, well-established, and qualified or validated method [38].
Visualization of Phase-Appropriate Validation Workflow
Regulatory Landscape and Compliance Framework
Key Regulatory Guidelines
The phase-appropriate approach operates within a comprehensive regulatory framework defined by multiple guidelines from international authorities. The International Council for Harmonisation (ICH) provides fundamental guidance through ICH Q2(R2) on validation of analytical procedures and ICH Q14 on analytical procedure development [38]. The U.S. Food and Drug Administration (FDA) offers specific guidance documents including Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products, and Potency Tests for Cellular and Gene Therapy Products [38].
The European Medicines Agency (EMA) has similar requirements but includes higher expectations for safety tests [38]. According to regulatory expectations, more information is expected for product safety-related assays early in clinical development, while for other assays, there should be sufficient information on suitability based on their intended use in the manufacturing process [38].
Analytical Method Lifecycle Management
The life cycle of analytical methods is closely aligned to the product life cycle [38]. Key steps include developing biological products against the target product profile (TPP), which informs the desired attributes of the therapeutic product [38]. During preclinical development, product quality risk assessments help inform potential product CQAs that inform the phase-appropriate analytical assay validation strategy [38].
As products move into pivotal trial phases and process performance qualification lots, method validation studies ensure analytical data is fit for purpose and robust enough to meet performance criteria defined in the ATP [38]. For products with accelerated approval pathways, CMC development timelines may be reduced to support early pivotal trials, with additional agency interactions sought to agree on development plans aligned with approval timelines [38].
The Researcher's Toolkit: Essential Reagents and Materials
Table: Essential Research Reagents and Materials for Validation Studies
| Reagent/Material | Function/Purpose | Phase Application |
|---|---|---|
| Reference Standards (RS) | Benchmark for accuracy, precision, and system suitability testing [39] | All phases |
| Master Cell Bank | Consistent, characterized cell source for cell-based assays [39] | Phase 2 onwards |
| Analytical Standards | Calibrate instruments, establish linearity and range [10] | All phases |
| System Suitability Solutions | Verify chromatographic system performance before sample analysis [10] | All phases |
| Quality Control Samples | Monitor assay performance over time [39] | Phase 2 onwards |
| Extractable/Leachable Standards | Identify filter-related substances in drug product [41] | Commercial phase |
Implementing a phase-appropriate validation approach provides pharmaceutical companies with a structured methodology to navigate drug development complexity while reducing risks, enhancing efficiency, and ensuring patient safety throughout the drug development lifecycle [40]. This tailored framework enables accelerated timelines, better resource allocation, and adherence to regulatory standards [40].
The successful execution of this strategy requires ongoing assessment of critical quality attributes, which are typically generated at the preclinical stage, formally reviewed at each development phase, and finalized before commercialization [38]. As emphasized in ICH Q8(R2) and ICH Q11, a cascade of interacting elements defines this process: creating a target product profile for the drug being developed, defining a quality target product profile based on the TPP, and establishing CQAs using a risk-based assessment [38].
For researchers and drug development professionals, understanding and implementing this phased approach is essential for efficient resource allocation and regulatory success. By tailoring validation activities to specific development phases, sponsors can focus resources where they provide greatest value while maintaining compliance with regulatory standards and ensuring product safety and efficacy throughout the development lifecycle.
The choice of an analytical method is pivotal in drug development and quality control, balancing factors such as sensitivity, selectivity, cost, and environmental impact. This guide provides an objective comparison between Ultra-Fast Liquid Chromatography with Diode Array Detection (UFLC-DAD) and UV-Visible Spectrophotometry for the determination of active pharmaceutical ingredients (APIs). Framed within the broader context of analytical method validation, this comparison focuses on core validation parameters—specificity, selectivity, accuracy, and precision—using supporting experimental data from the literature. The aim is to offer researchers, scientists, and drug development professionals a clear, data-driven foundation for selecting the most appropriate technique for their specific analytical needs.
Experimental Protocols & Methodologies
To ensure a fair comparison, this analysis draws upon experimental protocols where both techniques were applied to similar analytical problems, primarily the determination of single or multiple APIs in pharmaceutical formulations.
Spectrophotometric Method Protocols
UV-Visible spectrophotometry is a well-established technique that measures the absorption of light by an analyte in solution. The following protocols highlight common approaches for single and multi-component analysis.
Single Component Analysis (Paracetamol Assay): A simple and direct method was developed for the assay of paracetamol in tablets [42]. The protocol involves dissolving the sample in a mixture of methanol and water, which acts as the diluent. The absorbance of the resulting solution is then measured at the wavelength of maximum absorption (λmax) for paracetamol. Quantification is achieved using a single-point standardization, where the concentration of the test sample is calculated by comparing its absorbance to that of a standard solution of known concentration [42].
Multi-Component Analysis (Double Divisor Ratio Spectra Derivative - DDRD): For the simultaneous determination of a ternary mixture containing analgin, caffeine, and ergotamine, more advanced spectrophotometric methods are required. The Double Divisor Ratio Spectra Derivative (DDRD) method was employed. This technique allowed for the determination of ergotamine at 355 nm and caffeine at 268 nm by utilizing the third and first derivative of the ratio spectra, respectively, to resolve the overlapping signals [43].
Chromatographic (UFLC-DAD) Method Protocols
Chromatography separates the components of a mixture before detection, which significantly enhances selectivity. The following protocol is representative of a validated UFLC-DAD method.
- HPLC-DAD for Ternary Mixture Analysis: An Inertsil-C8 column was used for the separation of analgin, caffeine, and ergotamine [43]. The method employed a gradient elution with a mobile phase composed of acetonitrile and ammonium format buffer (pH 4.2). The DAD detector was set to monitor analgin and caffeine at 280 nm and 254 nm, respectively. Due to its inherent fluorescence, ergotamine was detected using a fluorometric detector set at an excitation of 310 nm and an emission of 360 nm. This combination of separation and selective detection allows for the precise quantification of all three compounds in a single run [43].
Comparative Data on Validation Parameters
The reliability of an analytical method is formally assessed through a validation process that evaluates key performance parameters. The table below summarizes a comparative analysis of Spectrophotometry and UFLC-DAD based on validation data from the cited studies.
Table 1: Comparison of Key Validation Parameters for Spectrophotometry and UFLC-DAD
| Validation Parameter | Spectrophotometric Methods | UFLC-DAD Methods |
|---|---|---|
| Specificity/Selectivity | Lower; susceptible to interference from other absorbing compounds in multi-component mixtures [42] [44]. | High; achieves baseline separation of analytes from each other and from excipients or degradation products [43] [44]. |
| Accuracy (Recovery %) | Generally good; reported recoveries for paracetamol and in ternary mixtures were within acceptable limits (e.g., 96-100%) [42] [43]. | Excellent; recovery rates typically very high and close to 100% (e.g., 98-101%) [45] [43]. |
| Precision (% RSD) | Precise; RSD values for paracetamol and components in a ternary mixture were low, demonstrating good repeatability [42] [43]. | Highly precise; RSD values are consistently very low (e.g., ≤ 1% for retention time), indicating superior reproducibility [46] [43]. |
| Linearity Range | Wider for major components (e.g., 10-70 μg/mL for ergotamine) [43]. Confirmed via correlation coefficient (R²) [42]. | Broad and demonstrated over specified ranges (e.g., 50-400 μg/mL for analgin) [43]. Confirmed through tests for homoscedasticity and lack-of-fit [47]. |
| Limit of Detection (LOD) | Higher (less sensitive); suitable for major component assay but may not detect trace impurities [42]. | Lower (more sensitive); capable of detecting analytes at trace levels (e.g., ng/L in UHPLC-MS/MS, ng/mL in HPLC) [44] [43]. |
| Analysis Time | Fast; minimal sample preparation and direct measurement [42]. | Longer; includes time for column equilibration and separation [43]. |
| Cost & Sustainability | Lower operational cost; uses simpler instruments and greener solvents (e.g., water, methanol) [43] [42]. | Higher operational cost; requires expensive instruments, columns, and higher purity solvents [43] [44]. |
Visualizing Method Selection and Validation
The following diagrams illustrate the logical workflow for method selection and the foundational relationship between key validation parameters.
Diagram 1: A logical pathway to guide the selection of an analytical method based on key project requirements.
Diagram 2: The relationship between accuracy and its two core components: trueness and precision.
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of both spectrophotometric and chromatographic methods relies on a set of essential reagents and materials. The following table details key items and their functions in analytical development.
Table 2: Key Research Reagent Solutions for Method Development and Validation
| Item | Function in Analysis | Application Context |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides an accepted reference value with stated uncertainty to assess method accuracy and trueness [48]. | Used in both methods as a highest-level standard for calibration and accuracy studies. |
| Chromatography Columns (e.g., C8, C18) | The stationary phase for separating mixture components based on chemical interactions with the analytes [43] [49]. | Core component of UFLC-DAD systems; the choice of column chemistry is critical for method selectivity. |
| Mobile Phase Buffers (e.g., Ammonium Formate) | Controls the pH of the mobile phase to ensure consistent ionization of analytes, thereby improving peak shape and separation reproducibility [43]. | Essential for robust and reliable UFLC-DAD methods, especially for ionizable compounds. |
| UV-Transparent Solvents (e.g., Methanol, Water) | Serves as a diluent to prepare sample and standard solutions without absorbing significant UV light in the wavelength range of interest [42] [43]. | Critical for spectrophotometry and for preparing samples in UFLC-DAD. |
| Solid-Phase Extraction (SPE) Cartridges | Pre-concentrates target analytes and removes interfering matrix components from complex samples like biological fluids or environmental water [44]. | Used in sample preparation for UFLC-DAD to enhance sensitivity and protect the analytical column. |
Both UV-Visible Spectrophotometry and UFLC-DAD are powerful analytical techniques with distinct advantages. The choice between them is not a matter of which is universally better, but which is fit-for-purpose.
- Spectrophotometry is a robust, cost-effective, and rapid choice for the quantitative analysis of single APIs or simple mixtures in quality control settings, where high sensitivity and complete separation are not critical.
- UFLC-DAD is the unequivocal choice for complex analyses, including multi-component formulations, impurity profiling, and trace analysis, where its superior selectivity, sensitivity, and specificity are indispensable.
This comparative guide demonstrates that the decision must be grounded in the specific analytical requirements and validated through a structured assessment of performance parameters, ensuring data quality and regulatory compliance in drug development.
Solving Common Challenges and Enhancing Method Robustness
In the scientific and pharmaceutical communities, the validity of analytical data is paramount. The concepts of accuracy and precision, along with the related ISO-defined parameter of trueness, form the cornerstone of reliable measurement systems in drug development and research [50]. These performance characteristics are not synonymous; they describe different aspects of measurement quality and are influenced by distinct types of experimental error. Accuracy refers to the closeness of agreement between a single test result and the true or accepted reference value, while precision describes the closeness of agreement between independent test results obtained under stipulated conditions [31]. Trueness, a term introduced by the ISO, specifically expresses the closeness of agreement between the average value from a large series of results and the accepted reference value [50]. Understanding the relationship between these concepts—where accuracy is influenced by both random and systematic errors, and precision is influenced only by random errors—is the first critical step in identifying and mitigating measurement error [51].
Conceptual Framework: Accuracy, Precision, and Trueness
Definitions and Interrelationships
The relationship between accuracy, precision, and trueness, along with their underlying error types, can be visualized as a cohesive system. The following diagram illustrates how these concepts and their quantitative expressions interrelate.
This framework shows that accuracy encompasses both trueness (the inverse of systematic error) and precision (the inverse of random error) [52]. A method's accuracy, therefore, depends on minimizing both types of error. In a practical sense, a highly precise method yields reproducible results, but without trueness, those results are consistently wrong. Conversely, a method with good trueness has an average close to the true value, but with poor precision, individual measurements are unreliable. High-quality methods demonstrate both high trueness and high precision, leading to superior accuracy [50].
The Bullseye Analogy for Conceptual Clarity
A classic method for visualizing these concepts is the bullseye or dartboard analogy, which correlates target patterns with different combinations of accuracy and precision [53]. The table below summarizes these scenarios.
Table 1: Interpretation of Bullseye Analogy for Accuracy and Precision
| Scenario | Accuracy | Precision | Interpretation |
|---|---|---|---|
| Group A: Darts far from bulls-eye and scattered | Low | Low | High systematic and random error; neither true nor precise. |
| Group B: Darts far from bulls-eye but clustered | Low | High | Low trueness (high systematic error/bias) but high precision (low random error). |
| Group C: Darts spaced around bulls-eye | High* | Low | High trueness (low systematic error) on average, but low precision (high random error). |
| Group D: Darts clustered on bulls-eye | High | High | Low systematic and random error; both true and precise. |
*The average position of the darts is at the bulls-eye, indicating trueness. However, the imprecision of individual measurements is a major limitation [53].
Quantitative Expression and Experimental Protocols
Quantifying Performance Characteristics
To move from concept to practice, specific statistical parameters are used to quantify trueness, precision, and accuracy. These quantitative expressions allow for objective comparison and validation of analytical methods [50] [52].
Table 2: Quantitative Expression of Performance Characteristics
| Performance Characteristic | What It Estimates | Typical Quantitative Expression | Key Statistical Parameter(s) | ||
|---|---|---|---|---|---|
| Trueness | Systematic Error | Bias | • Average value (( \bar{x} ))• Reference value (( x_{Ref} ))• Bias = ( | \bar{x} − x_{Ref} | ) or % Recovery |
| Precision | Random Error | Standard Deviation, Relative Standard Deviation (RSD) | • Standard Deviation (SD)• % Relative Standard Deviation (%RSD) = (SD / ( \bar{x} )) × 100% | ||
| Accuracy | Total Error | Measurement Uncertainty | • Combination of bias and standard deviation estimates, often forming a confidence interval. |
Core Experimental Protocol: Precision and Accuracy Study
A fundamental validation study involves a precision and accuracy (P&A) experiment, which can be designed to efficiently evaluate multiple parameters simultaneously [54]. The workflow for this integrated approach is detailed below.
Detailed Methodology:
- Sample Preparation: Prepare six independent samples from a homogeneous source at the target concentration (e.g., 100% of the expected value) [54].
- Analysis: Analyze these samples under conditions that reflect the method's intended use, incorporating expected variations (e.g., different analysts, days, or equipment) to estimate intermediate precision [54].
- Precision Calculation: Calculate the %RSD (Relative Standard Deviation) of the six results. This provides a direct measure of random error under normal operating conditions [54].
- Accuracy/Trueness Calculation: Calculate the difference (bias) between the average of the results and the accepted reference value. This can be expressed as an absolute difference or as a % recovery [54].
- Data Assessment: The bias and precision estimates are combined with pre-defined acceptance criteria to calculate the probability that a future measurement will pass specifications. A high probability (e.g., ≥0.95) indicates the method is fit for purpose [54].
Supporting Experimental Protocols
Specificity Study
Specificity is the ability to assess the analyte unequivocally in the presence of potential interferents [54]. It is a special case of accuracy testing.
- For Separation Techniques (e.g., HPLC): Inject samples spiked with potential interferents and measure the resolution between the analyte peak and the closest eluting interference. A resolution of NLT (Not Less Than) 1.5 is typically considered acceptable [54].
- For Non-Chromatographic Techniques: Prepare samples spiked with known interferents and measure the resulting error. The error caused by all interferences combined must not exceed the allowable bias established in the core P&A study [54].
Range Study
The range is validated by demonstrating that the method provides acceptable precision and trueness across the entire claimed operating interval [54].
- Protocol: Perform the Precision and Accuracy study at multiple concentrations across the intended range (e.g., 50%, 80%, 100%, 120%, and 150% for assay methods, or 50%-150% for impurities) [54].
- Assessment: The recovery value ( [Mean]/[Known] × 100% ) at each concentration level should meet the acceptance criteria (e.g., probability NLT 0.95) [54].
Detectability Study
This study replaces traditional Limit of Detection (LOD) validation with a more practical assessment of a method's ability to reliably distinguish a signal from background at the specified limit [54].
- Protocol:
- Measure a standard solution of the impurity at the specified limit concentration.
- Measure a sample solution spiked with the impurity at the limit.
- Measure a standard solution spiked with the impurity at a concentration of (100% - %RSD), where the RSD can be estimated using models like the Horwitz equation.
- Assessment: The response for the spiked sample (Step 2) must be distinguishable from the unspiked sample and should match the response of the standard at the limit (Step 1). The solution at the lower concentration (Step 3) must demonstrate a measurably smaller response [54].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental for executing the validation protocols described and for ensuring the overall quality of analytical measurements.
Table 3: Key Reagents and Materials for Analytical Validation
| Item | Critical Function in Validation |
|---|---|
| Certified Reference Materials (CRMs) | Provides an traceable, accepted reference value essential for quantifying bias and establishing trueness. The uncertainty of the CRM must be factored into the overall measurement uncertainty [50] [52]. |
| High-Purity Analytical Standards | Used to prepare calibration curves and fortified samples for accuracy/recovery, specificity, and range studies. Their purity directly impacts the accuracy of the calculated results. |
| Chromatographically Pure Solvents & Mobile Phases | Essential for maintaining a stable baseline in separation techniques, which is critical for achieving the precision and detectability required for low-level impurity testing. |
| Well-Characterized Interference Stocks | Used in specificity studies to challenge the method's ability to distinguish the analyte from similar compounds, thereby verifying that the method's response is due to the analyte alone. |
Mitigation Strategies for Measurement Errors
Effective error mitigation requires targeted strategies based on the type of error identified.
Mitigating Systematic Errors (Improving Trueness)
Systematic errors produce consistent, repeatable deviations from the true value and are reflected in a method's bias [50] [51].
- Calibration: Regularly calibrate instruments against traceable standards and validate calibration curves across the intended range [3].
- Blank Analysis: Use method blanks to identify and correct for constant background interference or contamination contributing to bias.
- Standard Addition: Employ the method of standard addition to compensate for matrix effects that can cause proportional systematic error.
- Independent Method Comparison: Analyze samples using a fundamentally different, well-validated analytical technique to identify method-specific biases [55].
Mitigating Random Errors (Improving Precision)
Random errors cause unpredictable fluctuations in results and are quantified by the standard deviation or RSD [50] [51].
- Standardized Operating Procedures (SOPs): Develop and adhere to detailed SOPs to minimize operator-induced variability and ensure consistency across different analysts and time periods [3].
- Environmental Control: Stabilize environmental conditions (e.g., temperature, humidity) that can contribute to instrumental drift or sample variation.
- Instrument Maintenance: Implement a rigorous and preventive maintenance schedule for analytical instruments to ensure they operate at peak performance and stability.
- Adequate Replication: Perform a sufficient number of replicate measurements (e.g., n=6 in the P&A study) to obtain a reliable estimate of the random error and improve the reliability of the mean value [54].
A rigorous approach to identifying and mitigating measurement error is non-negotiable in research and drug development. By understanding the distinct natures of accuracy, precision, and trueness, and by implementing structured experimental protocols like the combined Precision and Accuracy study, scientists can quantitatively assess method performance. The strategic mitigation of systematic error through calibration and specificity studies, coupled with the control of random error via standardized procedures and replication, leads to robust, reliable, and valid analytical methods. This foundational work ensures that the data generated is truly fit for its intended purpose, ultimately supporting the development of safe and effective medicines.
Strategies for Resolving Interferences and Improving Specificity/Selectivity
In the highly regulated pharmaceutical industry, selectivity and specificity are foundational validation parameters that directly impact the accuracy, reliability, and overall validity of analytical results [56] [57]. Selectivity refers to the ability of an analytical method to distinguish between the analyte of interest and other components present in the sample matrix, while specificity ensures the method can accurately measure the analyte without interference from impurities, degradants, or the sample matrix itself [56] [57]. For researchers and drug development professionals, mastering strategies to resolve interferences is not merely a regulatory hurdle but a critical component of ensuring product safety and efficacy. This guide provides a comparative analysis of modern techniques and technologies designed to enhance method selectivity, supported by experimental data and practical workflows.
Core Principles and Advanced Techniques
Fundamentals of Selectivity
The principle of selectivity is rooted in exploiting unique chemical or physical properties of the analyte, such as molecular structure, charge, size, and reactivity [56]. The level of selectivity achieved has a profound impact on analytical quality, reducing the risk of false positives or negatives, which is particularly critical in pharmaceuticals, clinical diagnostics, and environmental monitoring [56].
Advanced Techniques for Selectivity Enhancement
To enhance selectivity, analysts employ advanced techniques that improve specificity, increase sensitivity, and reduce sample preparation complexity.
- Nanomaterials and Molecularly Imprinted Polymers (MIPs): These are powerful tools for enhancing selectivity. Nanomaterials can be engineered to have specific properties for selective interaction with target analytes. MIPs are synthetic polymers designed with specific binding sites complementary to the analyte, functioning like a lock and key mechanism. They are particularly effective in solid-phase extraction (SPE) for selectively capturing analytes from complex matrices [56].
- Advanced Chromatographic Techniques: Chromatography remains a cornerstone, with techniques like HPLC, GC, and supercritical fluid chromatography (SFC) offering enhanced separation capabilities. The development of new stationary phases and the use of multidimensional chromatography have further expanded the toolkit for achieving high selectivity [56].
- Selective Detection Methods: The choice of detection method is crucial. Techniques such as mass spectrometry (MS), especially when coupled with chromatography (e.g., LC-MS/MS), offer high selectivity by monitoring specific mass transitions. Other methods include electrochemical detection (for analytes undergoing redox reactions), fluorescence detection (exploiting fluorescent properties), and chemiluminescence detection [56].
Comparative Performance Data
The following tables summarize experimental data and performance characteristics of various selectivity enhancement strategies.
Table 1: Performance Comparison of Selectivity Enhancement Algorithms in Chromatography-Mass Spectrometry
This table summarizes findings from a 155-day study correcting for instrumental drift in chromatography-mass spectrometry data using pooled quality control (QC) samples. The study normalized 178 target substances using three algorithms [58].
| Algorithm | Correction Model Stability | Key Performance Characteristics | Best Suited For |
|---|---|---|---|
| Random Forest (RF) | Most stable | Provided the most stable correction model for long-term, highly variable data. Confirmed by PCA and standard deviation analysis [58]. | Long-term data with large fluctuations [58]. |
| Support Vector Regression (SVR) | Less stable, tends to over-fit | Showed less stable correction outcomes. For data with large variation, SVR tends to over-fit and over-correct [58]. | Datasets with low to moderate variability [58]. |
| Spline Interpolation (SC) | Less stable | Showed less stable correction outcomes compared to Random Forest [58]. | --- |
Table 2: Comparative Analysis of Selectivity Enhancement Techniques
This table provides a broader comparison of common techniques used in analytical chemistry to improve method selectivity [56] [57].
| Technique | Principle of Selectivity | Typical Applications | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Molecularly Imprinted Polymers (MIPs) | Selective binding via synthetic, complementary cavities [56]. | Sample clean-up (SPE), biosensors [56]. | High specificity, reusable, stable in harsh conditions [56]. | Complex polymer development, potential for non-specific binding [56]. |
| LC-MS/MS (Hyphenated Technique) | Physical separation via chromatography + mass/charge filtering via MS [56]. | Metabolite identification, multi-residue analysis [56]. | Exceptional specificity and sensitivity, can handle complex mixtures [56]. | High instrument cost, requires specialized operational skills [56]. |
| Immunoassays | Selective antibody-antigen binding (chemical selectivity) [56]. | Clinical diagnostics, therapeutic drug monitoring [56]. | High throughput, excellent sensitivity for specific analytes [56]. | Cross-reactivity with similar compounds can compromise specificity [56]. |
Experimental Protocols and Workflows
Protocol: Method Validation for Specificity and Selectivity (per ICH Guidelines)
For the assay of a drug substance or product, ICH guidelines require the demonstration of specificity, accuracy, precision, linearity, and range [57].
- Forced Degradation Studies: To demonstrate specificity, the method should be challenged with samples of the analyte that have been subjected to stress conditions (e.g., acid, base, oxidation, thermal, and photolytic degradation). The method's ability to separate and accurately quantify the analyte in the presence of its degradants is assessed [57].
- Analysis of Placebo and Matrix Blanks: The method is run using a placebo (excipients without API) and the sample matrix to confirm the absence of interfering peaks at the retention time of the analyte [57].
- Spiked Recovery Experiments: To demonstrate accuracy and the absence of matrix effects, the sample matrix is spiked with a known quantity of the analyte. The measured value is compared to the accepted true value, and the percentage recovery is calculated. A recovery of 98-102% is typically considered acceptable [57].
Protocol: Correcting Instrumental Drift with Quality Control Samples
A rigorous protocol for correcting long-term instrumental drift in chromatography-mass spectrometry, validated over 155 days, involves the following steps [58]:
- Establish a QC Data Set: Perform repeated tests (e.g., 20 times) on a set of pooled quality control (QC) samples over an extended period (e.g., 155 days) to establish a robust data set for modeling instrumental drift [58].
- Algorithm Application: Apply correction algorithms (e.g., Random Forest, Support Vector Regression, Spline Interpolation) to perform normalization on the target substances in the test samples. The QC sample data serves as the reference for these models [58].
- Handling Non-QC Components: For chemical components present in test samples but absent in the QC samples, normalization can still be achieved by either:
- Using an adjacent chromatography peak for correction.
- Applying the average correction coefficients derived from all QC data [58].
- Performance Verification: Use principal component analysis (PCA) and standard deviation analysis to confirm satisfactory correction performance. The Random Forest algorithm has been shown to provide the most stable correction model for long-term, highly variable data [58].
Visualized Workflows and Strategies
MIP-SPE Sample Preparation Workflow
This diagram illustrates the workflow for using Molecularly Imprinted Solid-Phase Extraction (MIP-SPE) to selectively isolate an analyte from a complex sample matrix, a key strategy for improving selectivity during sample preparation [56].
Strategic Path for Enhancing Method Selectivity
This decision-making flowchart guides scientists in selecting the most appropriate strategy to resolve interferences and improve method selectivity based on the nature of the analytical challenge [56] [57].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Selective Analysis
This table details essential materials and reagents used in developing and executing selective analytical methods.
| Item / Reagent | Function in Enhancing Selectivity/Specificity |
|---|---|
| Molecularly Imprinted Polymers (MIPs) | Synthetic antibodies; used in solid-phase extraction (SPE) cartridges to selectively bind and isolate target analytes from complex matrices, reducing interference [56]. |
| Chromatography Stationary Phases | The solid support in a chromatography column; different chemistries (C18, phenyl, HILIC, etc.) provide unique separation selectivities based on analyte properties like hydrophobicity or polarity [56]. |
| Quality Control (QC) Samples | A pooled sample used to monitor and correct for instrumental performance and data drift over time, ensuring consistency and reliability of analytical results [58]. |
| Internal Standards | A known compound, often deuterated or structurally similar, added to the sample to correct for variability in sample preparation and instrument response [57]. |
| Derivatization Reagents | Chemicals that react with specific functional groups of the analyte to produce a derivative with more favorable properties for selective detection (e.g., fluorescence) or separation [56]. |
Resolving interferences in pharmaceutical analysis requires a strategic approach that leverages both foundational principles and modern technological solutions. The comparative data presented in this guide demonstrates that while techniques like LC-MS/MS offer exceptional inherent specificity and MIPs provide powerful sample clean-up, the choice of algorithm for data correction, such as Random Forest, is critical for maintaining accuracy in long-term studies. Adherence to ICH validation protocols remains the universal standard for proving method robustness. By integrating these advanced techniques—from sample preparation with MIP-SPE to selective detection and sophisticated data normalization—scientists can develop methods with the high specificity and selectivity required to ensure drug quality and patient safety.
Leveraging Analytical Quality by Design (AQbD) for Proactive Method Development
In the pharmaceutical industry, the reliability of analytical data is paramount, directly influencing decisions about product quality, safety, and efficacy. The conventional approach to analytical method development, often described as a one-factor-at-a-time (OFAT) or quality-by-testing (QbT) methodology, is increasingly being superseded by a more systematic and proactive framework: Analytical Quality by Design (AQbD) [59] [60]. Rooted in the Quality by Design (QbD) principles outlined in ICH Q8, AQbD is "a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management" [59] [61]. Unlike the traditional paradigm, which fixes method parameters and relies on final quality assurance through testing, AQbD builds quality into the analytical method from the outset [62] [60]. This enhanced approach transforms method development from a discrete, static activity into an integrated, dynamic lifecycle management process, leading to more robust, reliable, and regulatory-flexible analytical procedures [59] [61] [63].
AQbD vs. Traditional Approach: A Comparative Analysis
The core distinction between AQbD and the traditional approach lies in their fundamental philosophy and execution. The following table provides a structured comparison of these two paradigms.
Table 1: Objective Comparison between Traditional Analytical Method Development and AQbD
| Aspect | Traditional Approach (QbT) | AQbD Approach |
|---|---|---|
| Philosophy | Reactive; quality ensured by testing the final method [60]. | Proactive; quality built into the development process [59] [60]. |
| Development Process | Often trial-and-error or OFAT, which can be time-consuming and lack reproducibility [59] [60]. | Systematic, structured, and science-based using risk assessment and Design of Experiments (DoE) [59] [63]. |
| Primary Focus | Fixed method parameters with strict adherence to set conditions [59]. | Understanding the relationship between Critical Method Parameters (CMPs) and Critical Quality Attributes (CQAs) [59] [60]. |
| Output | A single, fixed set of operational conditions [59]. | A Method Operable Design Region (MODR), a multidimensional region where method performance criteria are met [59] [64] [63]. |
| Regulatory Flexibility | Low; any change requires regulatory notification or prior approval [61]. | High; movement within the predefined MODR offers regulatory flexibility without needing revalidation [59] [63]. |
| Robustness & Control | Method robustness may not be fully understood, leading to higher risk of Out-of-Specification (OOS) results [63]. | Enhanced method robustness and understanding, minimizing OOS and Out-of-Trend (OOT) results [59] [63] [60]. |
| Lifecycle Management | Lifecycle management is less structured [61]. | Integrated lifecycle management with continuous monitoring and improvement, as outlined in USP <1220> [59] [61]. |
The Systematic AQbD Workflow: From Definition to Control
The implementation of AQbD follows a structured workflow that ensures a deep understanding of the analytical method and its performance boundaries. This process is cyclical, supporting continual improvement throughout the method's lifecycle.
Figure 1: The AQbD Workflow. This diagram illustrates the systematic, lifecycle-based approach for developing analytical methods under AQbD principles.
Defining the Analytical Target Profile (ATP) and Critical Quality Attributes (CQAs)
The first step in AQbD is to define the Analytical Target Profile (ATP), a prospective description of the analytical procedure's desired performance requirements [59] [61]. The ATP outlines the purpose of the method and defines the required quality of the reportable value, linking it to the decision risk for the product's Critical Quality Attributes (CQAs) [61]. It specifies performance criteria such as accuracy, precision, specificity, and range [61]. From the ATP, Critical Method Attributes (CMAs), which are performance characteristics like resolution or tailing factor, are identified [59] [60].
Risk Assessment and Initial Screening
A risk assessment is conducted to identify method parameters that may significantly impact the CMAs. Tools like Ishikawa (fishbone) diagrams and Failure Mode and Effects Analysis (FMEA) are used to prioritize factors for experimental evaluation [59] [60]. Parameters with the highest risk are selected as Critical Method Parameters (CMPs) [59]. Initial screening designs, such as Plackett-Burman design, are then employed to narrow down the list of CMPs that have a substantial effect on the method's performance [64].
Optimization and Defining the Method Operable Design Region (MODR)
The optimized CMPs are further investigated using Response Surface Methodology (RSM) based designs like Central Composite Design (CCD) or Box-Behnken Design [64] [65] [60]. These DoE studies model the relationship between the CMPs and the responses (CMAs) mathematically. The Method Operable Design Region (MODR) is established from this model as the multidimensional combination of CMPs where the method meets the ATP criteria [59] [63]. Operating within the MODR provides flexibility and ensures robustness, as the method will perform as intended even with minor, deliberate adjustments of parameters within this space [59] [61].
Control Strategy and Lifecycle Management
A control strategy is developed, which is a planned set of controls derived from current product and process understanding that ensures analytical procedure performance [59] [60]. Finally, the method enters the lifecycle management stage, where it is continuously monitored to verify its ongoing fitness for purpose, in alignment with regulatory guidelines like ICH Q14 and USP <1220> [59] [61].
Experimental Protocol: Implementing AQbD for an RP-HPLC Method
To illustrate the practical application of AQbD, the following is a detailed protocol for developing a Reverse-Phase High-Performance Liquid Chromatography (RP-HPLC) method for the simultaneous determination of two antihypertensive drugs, Perindopril Erbumine (PERI) and Moxonidine Hydrochloride (MOXO), in a synthetic mixture [65].
Phase 1: Define ATP and CQAs
- ATP Definition: The objective is to develop a precise, accurate, and robust RP-HPLC method for the simultaneous quantification of PERI (25–125 µg/mL) and MOXO (1–5 µg/mL) in a synthetic mixture. The method must demonstrate specificity, linearity (r² > 0.999), accuracy (98–102%), and precision (RSD < 2%) [65].
- CQAs Identification: The critical quality attributes for the chromatographic method are identified as Resolution between the two peaks, Retention Time, Theoretical Plates (column efficiency), and Tailing Factor [65] [60].
Phase 2: Risk Assessment and Screening
- Risk Assessment: An Ishikawa diagram is used to identify potential CMPs affecting the CQAs. Factors include mobile phase composition (type and ratio), pH of the aqueous phase, flow rate, column temperature, and detection wavelength [65] [60].
- Screening Design: A two-level full factorial design is employed to screen the most influential parameters. The analysis identifies the % of organic modifier, pH of the buffer, and flow rate as the CMPs with the most significant impact on resolution and retention time [65].
Phase 3: Optimization via DoE and MODR Establishment
- Experimental Design: A Central Composite Design (CCD) is used for optimization. The three CMPs are varied at different levels, and the chromatographic responses (CQAs) are recorded for each experimental run [65].
- MODR Establishment: The data from the CCD is used to build mathematical models and create contour plots. The MODR is defined as the region where resolution is greater than 2.0, the tailing factor is less than 1.5, and the runtime is minimized. A working point within the MODR is selected: Mobile Phase: Methanol:Acetonitrile:Phosphate Buffer (34:30:36 v/v/v) at pH 3.5, Flow Rate: 1.0 mL/min, and Column Temperature: 40°C [65].
Phase 4: Control Strategy and Validation
- Control Strategy: The selected working point and the MODR boundaries are documented. The control strategy specifies the acceptable ranges for the CMPs (e.g., pH ± 0.1 units, flow rate ± 0.05 mL/min) to ensure method performance [65].
- Method Validation: The method is validated according to ICH Q2(R1) guidelines at the chosen working point, confirming it meets all ATP requirements for specificity, linearity, accuracy, precision, and robustness [65].
Table 2: Summary of Validation Results for the AQbD-based RP-HPLC Method [65]
| Validation Parameter | Result for Perindopril Erbumine | Result for Moxonidine HCl |
|---|---|---|
| Linearity Range | 25 - 125 µg/mL | 1 - 5 µg/mL |
| Correlation Coefficient (r²) | 0.9996 | 0.9993 |
| Accuracy (% Recovery) | 99.5 - 100.5% | 99.2 - 100.8% |
| Precision (% RSD) | < 1.0% | < 1.5% |
| Specificity | No interference from excipients | No interference from excipients |
The Scientist's Toolkit: Essential Reagents and Solutions
The following table lists key materials and reagents commonly used in AQbD-driven chromatographic method development, along with their critical functions.
Table 3: Key Research Reagent Solutions for AQbD-based Chromatographic Methods
| Reagent / Material | Function in Analytical Development |
|---|---|
| High-Purity Solvents (e.g., Acetonitrile, Methanol) | Used as components of the mobile phase to elute analytes from the column. Purity is critical for baseline stability and detection sensitivity [65]. |
| Buffer Salts (e.g., Potassium Dihydrogen Phosphate, Ammonium Acetate) | Used to prepare the aqueous phase of the mobile phase. They control pH, which is often a Critical Method Parameter (CMP) impacting ionization, retention, and selectivity [64] [65]. |
| pH Adjusters (e.g., Ortho-Phosphoric Acid, Formic Acid) | Used to modify the pH of the aqueous buffer to the exact value required for optimal separation, as defined by the MODR [65]. |
| Stationary Phases (e.g., C18, C8 columns) | The heart of the chromatographic separation. The choice of column chemistry (e.g., ethylene-bridged hybrid C18) is a key variable screened during method development [64] [65]. |
| Standard Reference Compounds | Highly purified samples of the analyte(s) of interest. They are essential for identifying retention times, establishing calibration curves, and determining method accuracy and specificity [65]. |
Analytical Quality by Design represents a fundamental shift from a reactive, fixed-point method development process to a proactive, holistic, and knowledge-driven framework. By systematically defining objectives through the ATP, employing risk assessment and DoE to understand parameter impacts, and establishing a flexible MODR, AQbD delivers highly robust and reliable analytical methods [59] [63] [60]. This approach not only minimizes the occurrence of OOS and OOT results but also provides a scientific basis for regulatory flexibility, allowing for continuous improvement throughout the method's lifecycle without compromising data quality [61] [63]. As the pharmaceutical industry continues to evolve, the adoption of AQbD is poised to become the standard for developing analytical procedures that are fit-for-purpose, resilient, and capable of supporting the development of high-quality medicines.
The Role of Automation, AI, and Machine Learning in Optimization
The integration of artificial intelligence (AI) and machine learning (ML) is fundamentally reshaping optimization processes in pharmaceutical research and development. This transformation is most evident in the enhanced specificity, selectivity, and accuracy of experimental designs and outcomes. By leveraging predictive modeling and automated data analysis, these technologies are accelerating the path from discovery to clinical application while rigorously validating each step against traditional benchmarks.
Quantitative Impact of AI on Drug Development
AI and automation are delivering measurable gains across the drug development lifecycle, from initial discovery to clinical trials. The following data summarizes the statistical impact of AI adoption on key efficiency and success metrics.
Table 1: Statistical Impact of AI on Drug Discovery and Development
| Metric | Impact of AI | Traditional Benchmark | Data Source/Timeframe |
|---|---|---|---|
| Preclinical R&D Cost Reduction | 25% - 50% reduction [66] | N/A | AllAboutAI Analysis 2025 [66] |
| Development Timeline Acceleration | Up to 60% faster [66] | 10-15 years [66] | AllAboutAI Analysis 2025 [66] |
| Hit-to-Lead Conversion Rates | 1% - 40% (10-400x improvement) [66] | 0.01% - 0.14% [66] | AllAboutAI Analysis 2025 [66] |
| Phase I Clinical Trial Success Rate | 80% - 90% [66] | 40% - 65% [66] | AllAboutAI Analysis 2025 [66] |
| Probability of Clinical Success | Significant increase [67] | ~10% [67] | Industry Analysis [67] |
| Clinical Trial Patient Recruitment | Significant speed-up via AI-powered screening of EHRs [67] | Manual, time-consuming process [67] | Industry Analysis [67] |
Table 2: Predictive Accuracy of Advanced AI Models in Preclinical Stages
| Model Application | Reported Accuracy | Outperformance Versus |
|---|---|---|
| Toxicity Prediction | 75% - 90% [66] | Traditional methods [66] |
| Efficacy Forecasting | 60% - 80% [66] | Traditional methods [66] |
| Target Identification | High precision in sifting through biological data [67] | Manual trial and error [67] |
Experimental Protocols and Methodologies
The quantitative benefits of AI are realized through specific, reproducible experimental protocols designed to validate its predictive power against established methods.
Protocol for AI-Enhanced Virtual Screening and Hit Identification
This protocol outlines the use of AI for the high-throughput identification of lead compounds, optimizing for specificity and selectivity.
- Objective: To rapidly screen millions of compound structures in silico to identify high-probability hits for a defined biological target, thereby accelerating the discovery phase and reducing reliance on random, high-throughput physical screening [66] [67].
- Methodology:
- Data Curation and Featurization: Compile a diverse, high-quality dataset of molecular structures and their associated biological activity data from public and proprietary databases. Convert chemical structures into numerical feature vectors that encode molecular properties [67].
- Model Training and Validation: Train machine learning models (e.g., Random Forest, Deep Neural Networks) on the curated dataset to learn the complex relationships between chemical structures and biological activity. Model performance is validated using standard techniques like k-fold cross-validation to ensure accuracy and prevent overfitting [66].
- Virtual Screening Campaign: Apply the trained model to screen ultra-large virtual compound libraries (containing millions to billions of molecules). The model predicts and ranks compounds based on their probability of being active against the target and having desirable drug-like properties [66] [67].
- Experimental Validation: Synthesize or procure the top-ranking compounds identified by the AI model for experimental validation in in vitro assays. This step confirms the model's predictions and provides a critical feedback loop for model refinement [66].
- Validation Parameters:
- Specificity/Selectivity: Assessed by testing hits against related off-targets to confirm selective binding.
- Accuracy: Quantified by the model's hit rate (percentage of AI-predicted compounds that show confirmed activity in lab assays), which has been shown to reach 1-40%, far exceeding the 0.01-0.14% rate of traditional screening [66].
- Precision: Evaluated through the reproducibility of the model's predictions across different batches of virtual compounds.
Protocol for AI-Generated Digital Twins in Clinical Trial Optimization
This methodology employs AI to create virtual control patients, enhancing the precision and efficiency of Phase II and III clinical trials [68].
- Objective: To reduce the size of control arms in clinical trials by generating AI-simulated "digital twins" of real patients, which provide predicted disease progression trajectories for comparison with treated patients [68].
- Methodology:
- Real-World Data (RWD) Aggregation: Collect comprehensive, de-identified patient data from electronic health records (EHRs), including medical history, biomarkers, and disease progression metrics [68] [67].
- Predictive Model Development: Train generative AI models on the aggregated RWD to learn the statistical relationships between patient baseline characteristics and their subsequent disease outcomes. These models simulate how a patient's condition would likely evolve without experimental intervention [68].
- Twin Generation and Randomization: For each real patient enrolled in the trial, the AI generates a digital twin with a similar baseline profile. These twins are used to form a synthetic control arm [68].
- Outcome Comparison and Analysis: The clinical outcomes (e.g., change in a disease biomarker) of the treated patients are statistically compared against the predicted outcomes of their digital twins. A significant difference in favor of the treated group indicates drug efficacy [68].
- Validation Parameters:
- Accuracy: The predictive accuracy of the digital twin model is validated by checking its forecasts against held-out historical patient data before trial application.
- Statistical Rigor: The methodology is designed with regulatory input to strictly control the Type I error rate (false positives), ensuring that the trial's integrity is maintained and the risk of approving an ineffective drug is not increased [68].
- Precision: The model's ability to precisely match individual patient baselines is critical for a valid comparison.
AI Clinical Trial Optimization Flow
Signaling Pathways and Workflow Visualization
The integration of AI into the drug discovery pipeline creates an iterative, data-driven workflow that enhances decision-making at each stage.
AI-Driven Drug Discovery Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The implementation of advanced AI protocols relies on a suite of specialized computational and data resources.
Table 3: Key Reagents and Tools for AI-Driven Research
| Tool/Reagent | Function | Application in Protocol |
|---|---|---|
| AlphaFold & ProteinMPNN | Predicts protein 3D structures and designs novel protein/peptide sequences [69]. | Used in molecular design for generating novel drug candidates (e.g., peptides) with high target binding affinity [69]. |
| AI-Driven Digital Twin Generator | Creates AI models that simulate individual patient disease progression [68]. | Core to the clinical trial optimization protocol for generating synthetic control arms [68]. |
| Electronic Health Record (EHR) Databases | Large-scale, de-identified repositories of real-world patient clinical data [67]. | Provides the foundational data for training digital twin models and for AI-powered patient recruitment [68] [67]. |
| Molecular Docking & QSAR Software | Computational tools for simulating drug-target interactions and predicting biological activity [67]. | Forms the basis of many virtual screening workflows for evaluating compound libraries in silico [67]. |
| Curated Compound Libraries | Extensive virtual databases of synthesizable molecular structures [66] [67]. | Serves as the search space for AI-driven virtual screening campaigns to identify initial hits [66] [67]. |
Ensuring Compliance and Comparing Analytical Techniques Across Frameworks
Validation is a cornerstone of pharmaceutical development and manufacturing, ensuring that products consistently meet predefined standards of quality, safety, and efficacy. This guide provides a comparative analysis of validation requirements under four major regulatory frameworks: the International Council for Harmonisation (ICH), the United States Pharmacopeia (USP), the Chinese Pharmacopoeia (ChP), and Brazil's National Health Surveillance Agency (ANVISA). Understanding the nuances in their approaches—ranging from ICH's internationally harmonized, science-based principles to ANVISA's highly detailed and prescriptive documentation rules—is crucial for researchers and drug development professionals designing global development and regulatory submission strategies [70] [71]. This analysis is framed within the context of validation parameters—specificity, selectivity, accuracy, and precision—providing a structured comparison of experimental protocols and regulatory expectations.
The ICH, USP, ChP, and ANVISA represent a spectrum of regulatory philosophies, from international harmonization to national specificity.
- ICH: The International Council for Harmonisation brings together regulatory authorities and the pharmaceutical industry from the US, EU, Japan, and other regions to create globally harmonized technical guidelines. Its guidelines are science-based, risk-oriented, and flexible, promoting innovation while ensuring quality, safety, and efficacy. They serve as a foundation for many national regulations and are intended to eliminate duplication in development and registration processes [70] [71].
- USP: The United States Pharmacopeia is an independent, non-governmental organization that sets publicly available compendial standards for medicines, food ingredients, and dietary supplements. Its standards, published in the USP-NF (United States Pharmacopeia–National Formulary), are legally enforceable in the United States under the Federal Food, Drug, and Cosmetic Act. USP standards provide specific testing methods and acceptance criteria that manufacturers must meet to demonstrate product quality [72] [73].
- ChP: The Chinese Pharmacopoeia is the official pharmacopoeia of the People's Republic of China, issued by the Chinese Pharmacopoeia Commission. It sets mandatory standards for drug quality within China. The ChP has an established history of collaboration with the USP to harmonize standards and improve global medicine quality, reflecting China's growing integration into the global pharmaceutical landscape [74].
- ANVISA: Brazil's National Health Surveillance Agency is the national regulatory authority responsible for regulating pharmaceuticals and other health products. ANVISA's guidelines are compliance-driven, documentation-intensive, and aligned with Brazilian Good Manufacturing Practices (GMP). They are often highly detailed, with specific numerical acceptance criteria and stringent documentation formats, reflecting a prescriptive regulatory approach [71] [75].
Table 1: Core Characteristics of the Regulatory Frameworks
| Framework | Nature & Legal Status | Primary Focus & Approach | Geographic Reach |
|---|---|---|---|
| ICH | International harmonized guidelines; adopted into regional/national law | Science and risk-based; flexible; promotes robust development and lifecycle management | Global (US, EU, Japan, and many other countries) [71] |
| USP | Official compendium; standards are enforceable by law in the US [72] | Public quality standards; specific test methods and acceptance criteria | Primarily US, but used in over 140 countries [72] |
| ChP | Official pharmacopoeia; mandatory standards in China | National quality standards; increasingly harmonizing with international norms [74] | Primarily China |
| ANVISA | National regulatory authority; guidelines are legally binding in Brazil | Compliance-driven and prescriptive; detailed requirements and documentation [71] | Brazil |
Comparative Analysis of Key Validation Parameters
This section delves into the specific requirements for critical validation parameters, highlighting where the frameworks align and diverge. This is essential for designing defensible validation protocols.
Analytical Method Validation
Analytical method validation demonstrates that a testing procedure is suitable for its intended purpose. The following table compares requirements for key parameters.
Table 2: Comparison of Analytical Method Validation Parameters
| Validation Parameter | ICH Q2(R2) | USP General Chapters | ANVISA RDC 166/2017 | ChP (Aligned with ICH/WHO) |
|---|---|---|---|---|
| Linearity | At least 5 concentration levels (e.g., 80-120%); replicates not strictly required but recommended [71] | Follows ICH principles; visual plot and correlation coefficient required [71] | At least 5 levels (often 50-150%); minimum of 3 replicates per level; requires ANOVA and residual analysis [71] | Aligned with ICH and WHO principles [76] |
| Precision | At least 3 concentrations with triplicate measurements [71] | Validation required per ICH; system suitability tests are critical for daily operation [73] | 5 concentration levels (including LLOQ); stringent criteria for intermediate precision; ANOVA often required [71] | Aligned with ICH and WHO principles [76] |
| Specificity/Separation | General principles provided; forced degradation studies recommended [71] | Method-specific requirements in monographs; system suitability is a key focus [73] | Forced degradation studies are mandatory; specific conditions required (e.g., oxidation with metal ions like Cu(II) and Fe(III)); target degradation of ~10% to confirm method sensitivity [71] | Requires demonstration of specificity, in line with ICH [76] |
| Robustness & Ruggedness | Robustness should be evaluated; ruggedness is considered optional [71] | Implied through system suitability and verified methods | Both robustness and ruggedness must be demonstrated explicitly [71] | Requires robustness testing [76] |
Cleaning Validation
Cleaning validation ensures that equipment is free from residues, cleaning agents, and contaminants to prevent cross-contamination.
- ICH Framework: ICH guidelines (Q7, Q8, Q9, Q10) promote a risk-based, science-driven lifecycle approach [70]. Key requirements include:
- Acceptance Criteria: Residue limits must be scientifically justified based on health-based exposure limits (HBELs), maximum daily dose, and product toxicity [70].
- Risk Management (ICH Q9): Use of tools like FMEA to identify high-risk equipment and tailor sampling procedures accordingly [70].
- Process Design (ICH Q8): Cleaning parameters are established within a validated design space, and Quality by Design (QbD) principles are encouraged [70].
- USP: While not creating cleaning validation guidelines per se, USP provides analytical methods and standards (e.g., for residual solvents in USP <467>) used to verify cleaning effectiveness [73].
- ANVISA: Follows a prescriptive approach, with detailed documentation requirements for cleaning procedures and validation protocols, consistent with its overall regulatory style [75].
Stability Testing
Stability testing provides evidence of how a drug's quality varies over time under environmental factors.
- ICH: The ICH Q1 series is the global benchmark. A newly revised, unified ICH Q1 Step 2 Draft Guideline (2025) consolidates previous documents (Q1A-F, Q5C) and expands scope to include advanced therapies (ATMPs like gene and cell therapies), conjugated products, and drug-device combinations [77]. It emphasizes reduced testing designs (bracketing, matrixing) and stability modeling for shelf-life prediction [77].
- USP and ChP: Both pharmacopoeias incorporate stability testing requirements that are largely aligned with ICH principles. ChP collaborates with USP on standard-setting and harmonization [74].
- ANVISA: Requires stability studies for registration in Brazil. While it acknowledges ICH guidelines, it may have specific national requirements for study conditions and data presentation.
Experimental Protocols and Workflows
This section outlines generalized experimental workflows for key validation activities, integrating requirements from the different frameworks.
Protocol for a Forced Degradation Study
Forced degradation studies stress a drug product to establish the stability-indicating properties of analytical methods.
- Objective: To demonstrate method specificity by showing separation of degradation peaks from the active ingredient and to understand the drug's intrinsic stability [71] [77].
- Sample Preparation: Prepare a solution of the drug substance or a suspension of the drug product at a known concentration.
- Stress Conditions:
- Acid and Base Hydrolysis: Treat samples with 0.1N HCl and 0.1N NaOH at room temperature and elevated temperatures (e.g., 60°C) for several hours to days [71].
- Oxidative Stress: Treat samples with hydrogen peroxide (e.g., 0.3%). ANVISA specifically requires additional oxidative stress using metal ions like copper (II) and iron (III) [71].
- Thermal Stress: Expose solid drug substance and product to dry heat (e.g., 70°C) [77].
- Photostability: Expose samples to UV and visible light per ICH Q1B conditions [77].
- Analysis: Analyze stressed samples and unstressed controls using the developed method (e.g., HPLC-UV). The method should be able to detect and resolve degradation products.
- Acceptance Criteria: ANVISA recommends targeting ~10% degradation to confirm method sensitivity, though lower levels can be justified for highly stable molecules [71]. ICH is less prescriptive, focusing on the ability to detect and separate degradants.
Workflow for Analytical Method Validation
The following diagram illustrates a logical workflow for developing and validating an analytical method intended for global regulatory submissions, incorporating key requirements from ICH, USP, and ANVISA.
Diagram 1: Analytical Method Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials essential for conducting validation studies, along with their critical functions as referenced across the regulatory frameworks.
Table 3: Essential Reagents and Materials for Validation Studies
| Item | Function & Application in Validation | Regulatory Context |
|---|---|---|
| USP/ChP/EP Reference Standards | Physical reference materials with certified purity and properties; used to calibrate instruments, qualify methods, and identify substances during testing [72] [78]. | Mandatory for testing against USP, ChP, or European Pharmacopoeia (EP) monographs. Required for identity, assay, and impurity tests [72] [73]. |
| Certified Reference Materials (CRMs) | High-purity materials from National Metrology Institutes (e.g., NIST) with certified property values; used for ultimate traceability and method validation beyond pharmacopeial applications [78]. | Used for instrument qualification, method validation, and establishing metrological traceability. |
| Validated Cell Lines & Biological Reagents | Essential for bioassays (e.g., potency, immunogenicity) for biological products and biosimilars. Characterized cell banks and reagents ensure assay reproducibility [76]. | Critical for demonstrating comparability for biosimilars per WHO, EMA, and USFDA guidelines [76]. |
| Pharmacopeial Buffers & Media | Specified buffers and culture media are required for dissolution testing, microbial enumeration, and sterility testing per compendial methods [73]. | Required for tests described in USP, ChP, and other pharmacopoeias (e.g., USP <61>, <71>) [73]. |
| Residual Solvents & Elemental Impurity Standards | Standard solutions of Class 1-3 solvents and elemental impurities; used to validate and perform testing for impurities as per USP <467> and USP <232>/<233> [73]. | Necessary to control toxic impurities as mandated by pharmacopeial standards [73]. |
The comparative analysis reveals a spectrum of regulatory stringency and specificity. The ICH guidelines provide a flexible, science-based framework for building a robust validation strategy. USP and ChP provide the detailed, enforceable quality standards and test methods that form the basis of daily quality control. ANVISA stands out for its highly prescriptive and documentation-intensive approach, particularly for analytical method validation.
For global drug development, a successful strategy involves designing studies that meet the most stringent requirements from the outset—often those of ANVISA for method validation and ICH for stability and cleaning validation. This "highest common denominator" approach ensures that data packages are robust, defensible, and adaptable for submissions across multiple regions, ultimately accelerating patient access to safe and effective medicines worldwide.
In the pharmaceutical, biotechnology, and contract research sectors, the integrity and consistency of analytical data are paramount. Analytical method transfer is a documented process that qualifies a receiving laboratory (RU) to use an analytical test procedure that originated in a transferring laboratory (TU). Its primary goal is to demonstrate that the RU can perform the method with equivalent accuracy, precision, and reliability as the TU, producing comparable results for quality control testing [79]. This process is not merely a logistical exercise but a scientific and regulatory imperative, ensuring that product quality and patient safety are maintained regardless of where the testing occurs [80] [79].
A poorly executed transfer can lead to significant issues, including delayed product releases, costly retesting, regulatory non-compliance, and ultimately, a loss of confidence in data [79]. For researchers and drug development professionals, understanding the nuances of different transfer protocols is essential for maintaining operational excellence and ensuring the continuous quality of pharmaceutical products. This guide objectively compares the performance of various method transfer approaches, providing the experimental frameworks and data needed to select the optimal protocol for your specific context.
Comparative Analysis of Method Transfer Protocols
Selecting the appropriate transfer approach depends on factors such as the method's complexity, its regulatory status, the experience of the receiving lab, and the level of risk involved [79]. The following table compares the four primary protocols as defined by regulatory guidance from USP 〈1224〉 and ICH [80] [79] [81].
Table 1: Performance Comparison of Analytical Method Transfer Protocols
| Transfer Protocol | Experimental Design & Workflow | Key Performance Metrics & Acceptance Criteria | Typical Use Cases & Limitations |
|---|---|---|---|
| Comparative Testing [80] [79] | Both TU and RU analyze a predetermined number of identical samples (e.g., 3 batches in triplicate by two analysts). Results are statistically compared for equivalence [80]. | Accuracy/Precision: Difference in mean assay < 2.0%. Impurities: Difference < 25.0% or RSD < 5.0% [80]. Jointly established acceptance criteria must be met [82]. | Best for: Well-established, validated methods between labs with similar capabilities. Limitations: Requires careful sample homogeneity and robust statistical analysis [79]. |
| Co-validation [80] [79] | The analytical method is validated simultaneously by both TU and RU as part of a joint team, establishing reproducibility from the outset [80]. | Follows standard validation acceptance criteria per ICH Q2(R1) (accuracy, precision, specificity, etc.) [79] [81]. Data assessment is based on a pre-approved protocol [80]. | Best for: New methods or methods developed specifically for multi-site use. Limitations: Resource-intensive; requires close collaboration and harmonized protocols [79]. |
| Revalidation [80] [79] [81] | The RU performs a full or partial revalidation of the method, addressing parameters most likely to be affected by the transfer (e.g., precision, robustness) [80]. | Uses standard validation criteria + additional AMT acceptance criteria. A full validation protocol and report are required [79]. | Best for: Transfer to a lab with significantly different equipment, personnel, or environmental conditions. Limitations: Most rigorous and resource-intensive approach [79]. |
| Transfer Waiver [80] [79] [82] | No formal testing is performed. Eligibility is based on documented justification and risk assessment [80] [83]. | Requires robust scientific justification and documentation for regulatory review [79]. | Best for: Highly experienced RU; identical conditions; simple, robust methods; or personnel moving from TU to RU [80] [79]. Limitations: Rarely used; high regulatory scrutiny [79]. |
Experimental Data and Performance Insights
- Comparative Testing Efficiency: This is the most common transfer method and, when designed properly, provides a high level of confidence with manageable resource investment. Its success hinges on a pre-approved protocol with predetermined, statistically sound acceptance criteria [80] [79].
- Co-validation for Complex Methods: While resource-intensive, co-validation builds method robustness and reproducibility data directly into the method's lifecycle. This can prevent future transfer issues and is ideal for critical methods intended for long-term, multi-site use [79].
- Revalidation as a Comprehensive Solution: Revalidation is the most thorough but also the slowest and most expensive protocol. It is the only option when the receiving laboratory's environment is substantially different, as it essentially treats the method as new to the site [79].
- Waiver for Low-Risk Scenarios: A waiver can save significant time and resources, but it demands irrefutable justification. Common scenarios include the transfer of an unchanged pharmacopoeial method (which only requires verification) or when the receiving unit already has extensive experience with a highly similar method [80] [81] [82].
Experimental Protocol Design and Workflow
A successful method transfer is a structured, protocol-driven activity. The following workflow outlines the critical stages, from initial planning to final closure, ensuring regulatory compliance and reliable results.
Detailed Methodologies for Key Experiments
The core of any transfer protocol is the experimental design. Below are detailed methodologies for testing the critical performance parameters as cited in comparative studies.
Table 2: Key Research Reagent Solutions and Materials
| Item Category | Specific Examples | Critical Function in Transfer |
|---|---|---|
| Reference Standards [79] [81] [82] | Certified Reference Materials (CRMs), API working standards | Serves as the benchmark for accuracy and system suitability; ensures traceability and validity of all quantitative results. |
| Test & Validation Samples [80] [82] | Homogeneous batches of API/drug product, spiked placebo samples, forced degradation samples | Used for precision, accuracy, and specificity studies. Must be representative and stable for the duration of the transfer. |
| Critical Chromatographic Reagents [82] [84] | HPLC-grade solvents, qualified HPLC/GC columns, mobile phase additives | Directly impact method performance (retention time, peak shape, resolution). Must be equivalent between TU and RU. |
| Placebo/Matrix Blanks [84] | Drug product formulation without the Active Pharmaceutical Ingredient (API) | Essential for demonstrating specificity and proving that excipients do not interfere with the quantitation of the analyte. |
Assay and Impurity Precision and Accuracy
This experiment is fundamental to demonstrating that the RU can execute the method with the same reliability as the TU.
- Sample Preparation: For a drug product, a placebo is spiked with the API and known impurities at multiple concentration levels. A typical design involves a minimum of nine determinations over three concentration levels (e.g., 50%, 100%, 150% of target for assay; from the reporting threshold to 120% of specification for impurities) [84].
- Experimental Execution: Each preparation is analyzed, and the recovered amount is calculated against a reference standard. The results are evaluated for accuracy (% recovery) and precision (% relative standard deviation, %RSD) [10] [84].
- Acceptance Criteria: For assay, recovery is often 98.0-102.0% with an RSD of ≤2.0%. For impurities, a sliding scale is common, allowing for higher variability at lower levels (e.g., ±25.0% at the reporting threshold) [80] [84].
Specificity and System Suitability
This experiment proves the method can unequivocally quantify the analyte in the presence of other components.
- Sample Preparation: Analyze a blank (diluent), a placebo (if applicable), a standard, a sample spiked with known impurities and degradants (a "cocktail" solution), and an actual test sample [84].
- Experimental Execution: The chromatograms are compared to ensure the analytic peak is pure and baseline-resolved from all other peaks. Peak purity is often assessed using a Photo-Diode Array (PDA) or Mass Spectrometry (MS) detector [84].
- Acceptance Criteria: The blank and placebo must show no interference at the retention times of the analyte and impurities. Resolution between critical peak pairs should be greater than a specified limit (e.g., 1.5 or 2.0) [84].
Critical Success Factors and Regulatory Alignment
The Scientist's Toolkit for a Smooth Transfer
Beyond the protocol, several factors are paramount to success. Comprehensive planning and a robust, pre-approved protocol are the cornerstones, defining scope, responsibilities, and acceptance criteria to prevent misunderstandings [79]. Robust communication and collaboration between TU and RU, through dedicated teams and regular meetings, ensures knowledge transfer and rapid issue resolution [79] [83]. Finally, a risk-based approach should be applied throughout, identifying potential challenges like equipment differences or analyst experience and developing mitigation strategies early in the process [79].
Alignment with Validation Parameters
Method transfer directly builds upon the foundation of method validation. The parameters challenged during transfer—primarily precision, accuracy, and specificity—are a subset of the full validation parameters outlined in ICH Q2(R1) [81] [10] [85]. The transfer exercise confirms that these key characteristics remain consistent when the method's environment changes, effectively demonstrating the reproducibility of the method, a higher-order form of precision [81] [10]. A method must be properly validated before transfer, as the transfer process itself qualifies the laboratory, not the method [82].
The principles of green analytical chemistry (GAC) have become increasingly integrated into the framework of analytical method validation, representing a critical expansion beyond traditional parameters of specificity, selectivity, accuracy, and precision. Greenness assessment evaluates the environmental, health, and safety impacts of analytical procedures, ensuring they are not only scientifically valid but also environmentally benign and sustainable. Within validation protocols, this assessment has emerged as a complementary dimension that researchers and drug development professionals must consider to align with evolving regulatory expectations and corporate sustainability goals. The complexity of quantifying greenness has necessitated dedicated metric tools that can systematically evaluate multiple aspects of analytical methodologies, transforming subjective environmental considerations into objective, comparable data.
The AGREE (Analytical GREEnness) metric approach represents a significant advancement in this field, providing a comprehensive, flexible, and straightforward assessment methodology that generates easily interpretable results. Unlike traditional validation parameters that focus exclusively on technical performance, AGREE and similar tools enable scientists to benchmark the environmental footprint of their methods, creating opportunities for optimization that benefit both operational efficiency and ecological impact. This comparative guide examines the leading greenness assessment tools, with particular emphasis on the AGREE framework, to equip researchers with the knowledge needed to implement these assessments within their validation workflows effectively.
The AGREE Metric System
The AGREE metric system embodies a holistic approach to greenness assessment, incorporating the 12 principles of green analytical chemistry into a unified scoring framework. This tool transforms each principle into a normalized score on a 0-1 scale, subsequently calculating a comprehensive final score based on all criteria. The output is an intuitive pictogram that displays both the overall score and performance across each individual criterion, with darker green shading indicating superior environmental performance. The software supporting this metric is open-source and freely available, making it accessible to researchers across institutional settings [86] [87].
A key innovation of the AGREE system is its flexibility; users can assign different weights to each of the 12 principles based on their specific analytical needs and priorities. This weighting capability allows method developers to emphasize certain aspects of greenness most relevant to their applications while maintaining a comprehensive assessment structure. The 12 principles encompassed within AGREE include: the application of direct analytical techniques to avoid sample treatment; minimization of sample requirements; reduction of energy consumption; use of safer materials; implementation of miniaturization and automation; waste reduction and management; elimination of derivatization; enhancement of operator safety; integration of energy-efficient procedures; and utilization of renewable sources [87].
Complementary Assessment Tools
While AGREE represents a comprehensive recent advancement, several other tools have contributed to the evolution of greenness assessment in analytical chemistry:
NEMI (National Environmental Methods Index): This earlier metric system employs a simple pictogram divided into four quadrants, each representing different environmental criteria. While user-friendly, its binary assessment approach (pass/fail for each category) offers less granularity than more recent tools [87].
Analytical Eco-Scale: This semi-quantitative assessment tool assigns penalty points to analytical procedures based on their environmental impact, with higher penalty scores indicating poorer greenness performance. The final score is calculated by subtracting total penalty points from an ideal baseline of 100, providing an accessible measure for comparative assessment [87].
GAPI (Green Analytical Procedure Index): This tool utilizes a multi-criteria assessment approach visualized through a colored pictogram, evaluating environmental impact across the entire analytical procedure from sample collection to final determination [86].
Table 1: Comparison of Major Greenness Assessment Tools
| Tool Name | Assessment Approach | Scoring System | Key Principles | Output Format | Complexity |
|---|---|---|---|---|---|
| AGREE | Comprehensive 12-principle framework | 0-1 scale (1 = greener) | All 12 GAC principles | Pictogram with overall score and segment performance | Moderate |
| NEMI | Four-criteria binary assessment | Pass/Fail per quadrant | Toxicity, waste, hazardous chemicals, corrosiveness | Simple pictogram with filled/unfilled quadrants | Low |
| Analytical Eco-Scale | Penalty point system | 100 - penalty points = final score | Reagents, waste, energy, hazards | Numerical score with qualitative assessment | Low to Moderate |
| GAPI | Multi-stage procedural assessment | Color-coded evaluation | Sample collection, preparation, detection, etc. | Colored pictogram with process stages | Moderate |
Experimental Protocols for Greenness Assessment
AGREE Implementation Protocol
Implementing the AGREE assessment requires a systematic approach to ensure accurate and reproducible results. The following protocol outlines the standardized methodology for applying this tool to analytical procedures:
Software Acquisition and Installation
- Download the open-source AGREE software from the official repository at https://mostwiedzy.pl/AGREE [86].
- Install the software following the provided documentation, ensuring all dependencies are correctly configured.
- Verify successful installation by running the provided test cases.
Data Collection and Input
- Compile comprehensive data on the analytical method to be assessed, including:
- Sample preparation requirements (amount, treatment steps)
- Reagent consumption (types, quantities, toxicity data)
- Energy requirements (instrumentation, duration)
- Waste generation (volume, disposal requirements)
- Operator safety considerations
- Launch the AGREE software and select the appropriate assessment template.
- Input collected data into the corresponding fields within the software interface, ensuring accurate unit conversions and classifications.
Assessment Configuration
- Assign weighting factors to each of the 12 principles based on methodological priorities and regulatory requirements. Default weightings assign equal importance to all principles.
- Review principle-specific parameters and adjust scoring thresholds if necessary for specialized applications.
- Validate input data through the software's consistency checks to identify potential errors or omissions.
Execution and Interpretation
- Execute the assessment algorithm to generate the AGREE pictogram and numerical score.
- Interpret results by examining:
- The overall score (center of pictogram, 0-1 scale)
- Segment-specific performance (colored segments 1-12)
- Comparative performance against benchmark methods
- Generate assessment reports for documentation and regulatory submissions.
- Utilize results to identify opportunities for methodological improvements targeting lower-performing segments.
Comparative Assessment Protocol
To objectively benchmark multiple analytical methods or compare alternatives, the following experimental protocol ensures consistent evaluation:
Method Selection and Characterization
- Identify the analytical methods to be compared, ensuring they address similar analytical challenges (e.g., HPLC vs. UPLC for pharmaceutical compounds).
- Document complete methodological parameters for each approach, including:
- Instrumental configuration and specifications
- Chromatographic conditions (column dimensions, mobile phase composition, flow rate)
- Sample preparation workflow (steps, reagents, consumables)
- Runtime and throughput capabilities
- Establish performance benchmarks for each method using traditional validation parameters (specificity, accuracy, precision, LOD, LOQ) to ensure technical comparability [88] [89].
Parallel Greenness Assessment
- Apply the AGREE assessment protocol to each method independently, maintaining consistent weighting factors across all evaluations.
- Supplement with additional greenness tools (NEMI, Eco-Scale) to provide multidimensional assessment.
- Document all scores and pictorial outputs for comparative analysis.
Cost-Effectiveness Integration
- Calculate direct costs for each method, including:
- Reagent and consumable expenses per analysis
- Instrument capital and maintenance costs
- Energy consumption based on local utility rates
- Waste disposal costs
- Factor in operational considerations:
- Analysis throughput (samples per hour)
- Personnel time requirements
- Method development and validation investments
- Normalize costs to a standard unit (e.g., cost per sample) for direct comparison.
Data Synthesis and Decision Matrix
- Compile all greenness scores and cost data into a comprehensive comparison table.
- Apply weighting factors to different criteria based on organizational priorities (e.g., environmental compliance vs. cost containment).
- Generate visual comparisons highlighting trade-offs and advantages across the assessed methods.
- Document limitations and assumptions for transparent reporting.
Visualization of Assessment Workflows
AGREE Assessment Process
Comprehensive Method Benchmarking
Comparative Data Analysis
Greenness Tool Performance Comparison
Table 2: Technical Comparison of Greenness Assessment Tools
| Feature | AGREE | NEMI | Analytical Eco-Scale | GAPI |
|---|---|---|---|---|
| Number of Evaluation Criteria | 12 principles | 4 categories | 6 main categories | 5 process stages |
| Scoring Resolution | Continuous (0-1) | Binary (pass/fail) | Numerical (0-100) | Semi-quantitative (color codes) |
| Weighting Flexibility | Yes, user-defined | No | Limited | No |
| Software Dependence | Required for calculation | Not required | Not required | Not required |
| Visual Output Quality | High (detailed pictogram) | Medium (simple pictogram) | Low (numerical score) | High (colored diagram) |
| Learning Curve | Moderate | Low | Low | Moderate |
| Regulatory Acceptance | Growing | Established | Established | Growing |
| Application Scope | Comprehensive | Basic screening | Intermediate | Comprehensive |
Method Comparison Case Study
To illustrate the practical application of greenness assessment tools, the following case study compares three chromatographic methods for pharmaceutical analysis:
Table 3: Greenness and Cost Comparison of Chromatographic Methods
| Parameter | Traditional HPLC | UPLC | Green HPLC |
|---|---|---|---|
| AGREE Overall Score | 0.45 | 0.58 | 0.72 |
| NEMI Quadrants | 2/4 | 3/4 | 4/4 |
| Eco-Scale Score | 48 | 62 | 78 |
| Solvent Consumption (mL/sample) | 15.2 | 5.8 | 8.3 |
| Energy Consumption (kWh/sample) | 1.8 | 1.2 | 1.5 |
| Hazardous Reagents | 3 (acetonitrile, phosphoric acid, TFA) | 2 (acetonitrile, formic acid) | 1 (ethanol) |
| Waste Generation (mL/sample) | 14.8 | 5.5 | 7.9 |
| Analysis Time (min) | 25 | 8 | 18 |
| Cost per Analysis (USD) | $4.85 | $3.92 | $3.45 |
| Specificity | Meets requirements | Meets requirements | Meets requirements |
| Accuracy (% Recovery) | 98.5% | 99.2% | 98.8% |
| Precision (%RSD) | 1.8% | 1.5% | 1.6% |
| LOQ (ng/mL) | 12.5 | 8.2 | 10.3 |
The data demonstrates the complex relationship between greenness, cost, and analytical performance. While UPLC offers advantages in analysis speed and solvent reduction, the Green HPLC method achieves superior overall greenness scores through careful solvent selection and waste minimization, while maintaining acceptable analytical performance at the lowest operational cost.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Reagents and Materials for Green Analytical Chemistry
| Item | Function | Green Alternatives | Considerations |
|---|---|---|---|
| Acetonitrile (HPLC grade) | Common reversed-phase mobile phase component | Ethanol, methanol, acetone | Higher toxicity, requires specialized waste disposal |
| Methanol | Mobile phase component, extraction solvent | Ethanol, isopropanol | Toxic, but less than acetonitrile |
| n-Hexane | Extraction solvent for non-polar compounds | Cyclopentyl methyl ether, heptane | Highly flammable, neurotoxic |
| Chloroform | Lipid extraction, solvent | Ethyl acetate, methyl tert-butyl ether | Carcinogenic, environmental persistence |
| Trifluoroacetic acid | Ion-pairing reagent for separations | Formic acid, phosphoric acid | Highly corrosive, environmental impacts |
| Derivatization reagents | Analyte modification for detection | Direct analysis methods | Additional steps, reagent use, waste generation |
| Solid-phase extraction cartridges | Sample clean-up and concentration | Miniaturized SPE, µ-SPE | Reduced solvent consumption |
| Traditional HPLC columns (250mm) | Chromatographic separation | UHPLC columns (50-100mm) | Reduced solvent consumption, faster analysis |
The integration of greenness assessment tools like AGREE into analytical method validation represents a significant advancement in sustainable scientific practice. These tools provide researchers and drug development professionals with standardized approaches to quantify and benchmark the environmental performance of their methodologies, creating opportunities for improvement that align with broader sustainability goals. The comparative data presented in this guide demonstrates that greenness optimization frequently correlates with improved cost-effectiveness and maintained analytical performance, challenging the historical perception of environmental considerations as merely regulatory burdens.
As validation parameters continue to evolve beyond traditional metrics of specificity, selectivity, accuracy, and precision, greenness assessment establishes itself as a complementary dimension of methodological quality. The structured implementation of tools like AGREE, following the experimental protocols outlined in this guide, enables systematic evaluation and comparison of analytical approaches. This empowers scientists to make informed decisions that balance analytical performance, environmental impact, and operational efficiency—the essential trifecta of modern analytical chemistry in pharmaceutical development and beyond.
In the rigorous landscape of drug development and clinical diagnostics, biomarkers are indispensable tools for decision-making. Their credibility, however, rests on two distinct but interconnected processes: analytical validation and clinical qualification. These terms are often used interchangeably, but they address fundamentally different questions. Analytical validation asks, "Does the assay measure the biomarker accurately and reliably?" while clinical qualification asks, "Does the biomarker measurement meaningfully predict or reflect a biological or clinical outcome?" [90] [91]. The failure to navigate this distinction is a significant roadblock to the clinical implementation of otherwise promising biomarkers [91]. This guide provides a structured comparison of these two processes, underpinned by experimental data and clear frameworks, to equip researchers and scientists with the knowledge to robustly advance their biomarker pipelines.
Part 1: Core Conceptual Frameworks and Definitions
The Fundamental Distinction
At its core, the difference lies in what is being validated: the assay itself versus the biological or clinical interpretation of the result.
- Analytical Validation is the process of assessing an assay's performance characteristics. It confirms that the test method is capable of generating reproducible and accurate data about the biomarker's quantity or presence. It is primarily a test of the measurement technology [90] [92].
- Clinical Qualification is the evidentiary process of linking a biomarker with biological processes and clinical endpoints. It establishes the relationship between the biomarker measurement and the physiological, toxicological, or clinical state it is intended to indicate [90].
The following diagram illustrates the sequential yet distinct pathways of assay validation and clinical qualification, highlighting how they converge to support a biomarker's context of use.
The Role of "Context of Use" and "Fit-for-Purpose"
A critical concept in modern biomarker development is "Context of Use" (COU). The COU is a precise description of how the biomarker will be used in drug development and regulatory decision-making [92]. For instance, HER2 can be used as a predictive biomarker to select patients for a clinical trial or as a pharmacodynamic biomarker to confirm drug mechanism.
The COU directly dictates the extent of validation and qualification required, guided by a "Fit-for-Purpose" (FFP) strategy [92] [93]. An exploratory biomarker used internally for early research decisions may require only a base level of analytical validation. In contrast, a biomarker used as a primary endpoint in a pivotal Phase III trial, with data intended for product labeling, will require the most stringent levels of both analytical validation and clinical qualification [92].
Part 2: A Detailed Comparison of Validation Parameters
The following table provides a head-to-head comparison of the key parameters for analytical validation versus clinical qualification, illustrating their different objectives and assessment methods.
Table 1: Comparative Framework: Analytical Validation vs. Clinical Qualification
| Parameter | Analytical Validation (The Assay) | Clinical Qualification (The Biomarker) |
|---|---|---|
| Primary Objective | To demonstrate the assay's reliability, reproducibility, and accuracy in measuring the biomarker [91]. | To establish the biomarker's relationship with a biological process or clinical endpoint [90] [91]. |
| Key Questions | Does the test work in the lab? Is it precise? Is it sensitive? | What does the result mean for the patient? Does it predict outcome or response? |
| Accuracy | Relative Accuracy: Assessed via parallelism studies and repeated measures of endogenous samples, as reference standards are often recombinant proteins that differ from the endogenous analyte [94]. | Clinical Accuracy: Evaluated by how well the biomarker classifies patients into correct clinical categories (e.g., disease vs. healthy, responder vs. non-responder). |
| Precision | Measures the assay's reproducibility (repeatability and intermediate precision) in generating the same result for a given sample [91]. | Refers to the consistency of the biomarker's predictive value across different patient populations and independent studies [90]. |
| Specificity | Confirms the assay detects only the intended biomarker, not interfering substances. Demonstrated through parallelism of calibrator and endogenous analyte [94]. | Establishes that changes in the biomarker are specifically linked to the defined biological process or intervention, and not to unrelated processes. |
| Sensitivity | The lowest concentration of the biomarker that can be reliably distinguished from zero (LLOQ) [94]. | The biomarker's ability to detect a clinically meaningful change or difference in patient status (e.g., early disease detection). |
| Scope of Evidence | Confined to the performance of the analytical method in a controlled setting. | Requires broad clinical evidence from multiple studies, often involving large, diverse patient cohorts and longitudinal data [90] [91]. |
Part 3: Experimental Protocols and Supporting Data
Experimental Protocol for a Key Analytical Validation Test: Parallelism
A cornerstone of biomarker assay validation is the parallelism experiment, which addresses the fundamental challenge that recombinant calibrants may not behave identically to the endogenous biomarker in a patient sample [94].
Objective: To demonstrate that the dilution-response curve of the endogenous biomarker in a study sample is parallel to the calibration curve of the recombinant standard. This confirms the assay recognizes both forms similarly and that relative quantification is valid [94].
Methodology:
- Sample Selection: Select several individual study samples containing the endogenous biomarker at medium to high levels.
- Sample Dilution: Create a series of dilutions for each sample (e.g., 1:2, 1:4, 1:8) using the appropriate assay matrix.
- Calibrator Curve: Run a standard calibrator curve using the recombinant protein.
- Assay Run: Analyze all diluted study samples and the calibrator curve in the same assay run.
- Data Analysis: Plot the measured concentration (or response) against the dilution factor for both the study samples and the calibrator. The curves should be parallel. A lack of parallelism indicates potential assay interference or differences between the recombinant standard and the endogenous biomarker, invalidating the calibration [94].
Quantitative Data from a Cross-Platform Comparison Study
Robust analytical validation often involves comparing different technology platforms. A large-scale community study comparing DNA methylation assays provides exemplary quantitative data on key validation parameters across different methods [95].
Table 2: Performance Comparison of DNA Methylation Assay Technologies [95]
| Assay Technology | Accuracy (vs. Reference) | Precision (CV%) | Sensitivity (Input DNA) | Key Strengths |
|---|---|---|---|---|
| Amplicon Bisulfite Sequencing | High | Low | <10 ng | High multiplexing capability, single-CpG resolution |
| Bisulfite Pyrosequencing | High | Low | ~10 ng | Excellent quantitative accuracy, established workflow |
| EpiTyper | Moderate | Moderate | ~20 ng | Provides haplotypic information |
| MethyLight | Moderate | Low | <10 ng | High sensitivity, suitable for low-input samples |
| MS-HRM | Moderate | Moderate | <10 ng | Low cost, simple workflow |
Experimental Context: This data was generated from a study where 18 laboratories received 32 standardized reference DNA samples to analyze using their chosen methylation assay for 27 predefined genomic regions. The performance was benchmarked for its utility in biomarker development and clinical diagnostics [95].
Part 4: The Scientist's Toolkit: Key Research Reagent Solutions
The reliability of biomarker data is directly dependent on the quality of reagents used. The following table details essential materials and their critical functions in assay development.
Table 3: Essential Research Reagents for Biomarker Assay Development
| Reagent / Material | Function and Importance in Validation |
|---|---|
| Recombinant Reference Standard | Serves as the calibrator for the assay. Critical for defining the analytical range, but its potential structural differences from the endogenous biomarker make parallelism testing essential [92] [94]. |
| Characterized Biobanked Samples | Well-defined biological samples (e.g., serum, tissue) from healthy and diseased donors. Used as quality controls (QCs) and for assessing precision, selectivity, and stability of the endogenous analyte [94]. |
| High-Affinity Capture and Detection Antibodies | The core of ligand-binding assays (LBA). Specificity and affinity directly determine the assay's sensitivity, dynamic range, and freedom from matrix interference [96]. |
| Standardized Matrix (e.g., Charcoal-Stripped Serum) | Used in preparing calibrators and QCs for biomarkers with high endogenous levels. A surrogate matrix aims to mimic the study sample matrix while providing a "blank" background [93]. |
| Reference Materials for Harmonization | Materials like standardized beads or control samples used to harmonize signal intensities across different instruments or laboratories, ensuring data comparability [97]. |
Part 5: Navigating Current Challenges and Regulatory Landscapes
Despite established frameworks, significant challenges persist. A major issue is reproducibility, often stemming from a lack of standardized protocols and insufficient analytical validation, creating a roadblock to clinical implementation [91]. Furthermore, validating biomarkers across diverse populations is critical, as genetic and environmental factors can affect biomarker performance, and generalizing from a non-diverse population can perpetuate health disparities [91].
The regulatory landscape is evolving. The U.S. Food and Drug Administration (FDA) emphasizes a Fit-for-Purpose strategy for biomarker bioanalysis [92] [93]. However, recent guidance directs developers to ICH M10, a guideline that explicitly excludes biomarkers, creating confusion within the bioanalytical community [93]. This underscores the necessity of early and clear communication with regulatory agencies about the biomarker's Context of Use.
The following diagram maps the journey of a biomarker from discovery to application, highlighting the key challenges and regulatory checkpoints at each stage.
The path from a discovered biomarker to a clinically qualified tool is complex and demanding. Success hinges on a rigorous and deliberate strategy that treats analytical validation and clinical qualification as separate but interconnected evidentiary processes. By adopting a Fit-for-Purpose approach, grounded in a clearly defined Context of Use, researchers can allocate resources efficiently, meet regulatory expectations, and ultimately deliver robust, reliable biomarkers that accelerate drug development and improve patient care.
Conclusion
The rigorous validation of specificity, selectivity, accuracy, and precision is not a mere regulatory formality but a fundamental requirement for generating reliable data that underpins drug development and ensures patient safety. A phase-appropriate strategy, guided by ICH and other regulatory frameworks, allows for efficient resource allocation while building method robustness as a product advances. The future of analytical method validation is being shaped by trends such as AQbD for enhanced robustness, AI/ML for optimization, and green chemistry principles for sustainability. Continued global harmonization of guidelines and the adoption of these innovative approaches will be crucial for accelerating the development of vital medicines and bringing them to patients faster without compromising on quality.
References
- 1. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 2. Selectivity or specificity? Validation of analytical methods from the perspective of an analytical chemist in the pharmaceutical industry - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/0731708595016791]
- 3. What's the Difference Between Accuracy and Precision ? [ 2025 ]... [https://asana.com/resources/accuracy-vs-precision]
- 4. ( ICH ) Validation of Analytical Procedures: An... | QbD Group Q 2 R 2 [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 5. AQbD & the new era of ICH 14 + Q ( Q ) | QbDVision 2 R 2 [https://www.qbdvision.com/aqbd-ich-q14-q2r2-guidelines-cmc/]
- 6. <1225> VALIDATION OF COMPENDIAL METHODS [http://www.uspbpep.com/usp29/v29240/usp29nf24s0_c1225.html]
- 7. Navigating EMA Validation Requirements: A Step-by-Step Guide [https://altabrisagroup.com/ema-validation-requirements/]
- 8. EMA vs FDA Expectations on Process Validation | Pharmaguideline [https://www.pharmaguideline.com/2025/07/ema-vs-fda-expectations-on-process-validation.html]
- 9. Validation, Verification, and Transfer of Analytical Procedures (On-Demand) [https://www.usp.org/events-training/course/validation-verification-and-transfer-analytical-procedures-demand]
- 10. Validation of Analytical Methods | IntechOpen [https://www.intechopen.com/chapters/57909]
- 11. The Importance of Method in Pharmaceutical Analysis Validation [https://www.linkedin.com/pulse/importance-method-validation-pharmaceutical-bj3of]
- 12. Pharmaceutical Quality : Control Playbook 2025 [https://www.pharmanow.live/pharma-manufacturing/quality-control-in-pharmaceutical-manufacturing]
- 13. Pharma Quality in Control Development and... | AMSbiopharma Drug [https://amsbiopharma.com/pharma-quality-control-strategies/]
- 14. Evaluating Drug Efficacy and Safety - Clinical Pharmacology - Merck Manual Professional Edition [https://www.merckmanuals.com/professional/clinical-pharmacology/concepts-in-pharmacotherapy/evaluating-drug-efficacy-and-safety]
- 15. Drug safety assessment in clinical trials: methodological challenges and opportunities | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-13-138]
- 16. Determining the Balance Between Drug Efficacy and Safety by the Network and Biological System Profile of Its Therapeutic Target - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6220079/]
- 17. Leading Pharmaceutical Validation Trends for 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 18. ARPA-H launches program to develop predictive drug safety and efficacy models | ARPA-H [https://arpa-h.gov/news-and-events/arpa-h-launches-program-develop-predictive-drug-safety-and-efficacy-models]
- 19. of SFC Analytical from Method ... Lifecycle Methods Development [https://www.chromatographyonline.com/view/analytical-method-lifecyle-of-sfc-methods-from-development-use-to-routine-qc-implementation-supporting-small-molecule-r-d-and-commercialization]
- 20. A Better Lifecycle for Analytical ? | Technology Networks Methods [https://www.technologynetworks.com/informatics/blog/a-better-life-for-analytical-methods-319591]
- 21. Understanding the Lifecycle Approach for Analytical Procedures | LCGC International [https://www.chromatographyonline.com/view/understanding-lifecycle-approach-analytical-procedures]
- 22. management of Life cycle analytical methods [https://pubmed.ncbi.nlm.nih.gov/28666555/]
- 23. Key aspects of analytical method validation and linearity evaluation - PubMed [https://pubmed.ncbi.nlm.nih.gov/18929516/]
- 24. Method Development and Validation – FCAD Group [https://www.fcad.com/features/method-development-and-validation/]
- 25. Measuring specificity in multi-substrate/product systems as a simple... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4924809/]
- 26. MRM3 quantitation for highest selectivity in complex matrices [https://sciex.com/tech-notes/technology/mrm3-quantitation-for-highest-selectivity-in-complex-matrices]
- 27. Compensate for or Minimize Matrix Effects? Strategies for Overcoming Matrix Effects in Liquid Chromatography-Mass Spectrometry Technique: A Tutorial Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 28. 2.2. Selectivity : detector-side (MS) selectivity – Validation of liquid... [https://sisu.ut.ee/lcms_method_validation/22-detector-side-ms-selectivity/]
- 29. RECENT HPLC STRATEGIES TO IMPROVE SENSITIVITY... | Scilit [https://www.scilit.com/publications/900065e0aff7dbfc79327bbcbb6d7f81]
- 30. Analytical Method Validation Protocol for... | Pharmaguideline [https://www.pharmaguideline.com/2013/10/analytical-method-validation-protocol-for-pharmaceuticals.html]
- 31. Accuracy and precision - Wikipedia [https://en.wikipedia.org/wiki/Accuracy_and_precision]
- 32. Accuracy and Precision - UCalgary Chemistry Textbook [https://chem-textbook.ucalgary.ca/version2/review-of-background-topics/measurements-and-data/uncertainty-accuracy-and-precision/accuracy-and-precision/]
- 33. and Spike and Linearity of... | Thermo Fisher Scientific - US Recovery [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 34. Dilutional Linearity, Parallelism, Spike -and- Recovery in ELISA... - Enzo [https://www.enzo.com/note/dilutional-linearity-parallelism-spike-and-recovery-in-elisa-how-to-qc-your-results/]
- 35. 4.1. Repeatability , intermediate and reproducibility... precision [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 36. Intermediate precision [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/intermediate-precision]
- 37. Evaluation | KeepNotes blog Intermediate Precision [https://bioinfo-scrounger.com/archives/precision-evaluation/]
- 38. A Phase - Appropriate For Assay Approach In Cell Gene... Validation [https://www.cellandgene.com/doc/a-phase-appropriate-approach-for-assay-validation-in-cell-gene-therapies-0001]
- 39. Selecting Bioanalytical Assays for FDA... - Marin Biologic Laboratories [https://www.marinbio.com/company/selecting-bioanalytical-assays-fda-clinical-trials-commercialization/]
- 40. Method Phase in Drug Development Appropriate Validation [https://vicihealthsciences.com/phase-appropriate-method-validation/]
- 41. Filter Phase For... | Agno Pharmaceuticals Appropriate Validation [https://agnopharma.com/blog/phase-appropriate-filter-validation-for-sterile-drug-product-manufacturing/]
- 42. Uv-visible spectrophotometric development and method ... validation [https://ijpsr.com/bft-article/uv-visible-spectrophotometric-method-development-and-validation-of-assay-of-paracetamol-tablet-formulation/?view=fulltext]
- 43. HPLC- Validated and DAD for... Spectrophotometric Methods [https://pubmed.ncbi.nlm.nih.gov/36326356/]
- 44. Development and validation of a green/blue UHPLC-MS/MS method for trace pharmaceutical monitoring | Scientific Reports [https://www.nature.com/articles/s41598-025-15614-4]
- 45. HPLC-DAD and UV-spectrophotometry for the determination of lychnopholide in nanocapsule dosage form: validation and application to release kinetic study - PubMed [https://pubmed.ncbi.nlm.nih.gov/23247030/]
- 46. Validation of Chromatographic Methods of Analysis - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0099542805320090]
- 47. Experimental and statistical protocol for the effective validation of chromatographic analytical methods - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7248235/]
- 48. Assessment of Accuracy in Chromatographic Analysis | LCGC International [https://www.chromatographyonline.com/view/assessment-accuracy-chromatographic-analysis]
- 49. Ultrafast Liquid Chromatography - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/ultrafast-liquid-chromatography]
- 50. Trueness, accuracy and precision [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/trueness-accuracy-precision]
- 51. Accuracy and precision [https://web.chem.ox.ac.uk/teaching/Physics%20for%20CHemists/Errors/Precision.html]
- 52. 7 Precision , trueness, accuracy – Estimation of measurement... [https://sisu.ut.ee/measurement/7-precision-trueness-accuracy/]
- 53. Practices of Science: Precision vs. Accuracy [https://manoa.hawaii.edu/exploringourfluidearth/physical/world-ocean/map-distortion/practices-science-precision-vs-accuracy]
- 54. Usp chemical medicines & excipients - evolution of validation practices [https://www.slideshare.net/slideshow/usp-chemical-medicines-excipients-evolution-of-validation-practices/27721116]
- 55. 3.4: Selecting an Analytical Method - Chemistry LibreTexts [https://chem.libretexts.org/Bookshelves/Analytical_Chemistry/Analytical_Chemistry_2.1_(Harvey)/03:__The_Vocabulary_of_Analytical_Chemistry/3.04:_Selecting_an_Analytical_Method]
- 56. The Power of Selectivity : A Deep Dive [https://www.numberanalytics.com/blog/the-power-of-selectivity-in-analytical-chemistry]
- 57. Analytical Method Validation : Ensuring Quality and Consistency in... [https://www.webofpharma.com/2025/11/analytical-method-validation-ensuring.html]
- 58. Correction of Chromatography-Mass Spectrometry Long-term Instrumental Drift using Quality Control Samples over 155 days | Sciety [https://sciety.org/articles/activity/10.21203/rs.3.rs-7401283/v1]
- 59. Analytical Quality by Design (AQbD) Approach to the Development of Analytical Procedures for Medicinal Plants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9653622/]
- 60. AQbD-novel strategy for analytical methods | Future Journal of Pharmaceutical Sciences | Full Text [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 61. Analytical Quality by Design, Life Cycle Management, and Method Control | The AAPS Journal [https://link.springer.com/article/10.1208/s12248-022-00685-2]
- 62. Development of quality-by-design analytical methods - PubMed [https://pubmed.ncbi.nlm.nih.gov/21280050/]
- 63. Analytical quality by design: a tool for regulatory flexibility and robust analytics - PubMed [https://pubmed.ncbi.nlm.nih.gov/25722723/]
- 64. Enhancing Pharmaceutical Analysis with Analytical ... Quality by [https://pubmed.ncbi.nlm.nih.gov/40503695/]
- 65. Analytical quality by design ( AQbD ) methodology for concurrent... [https://link.springer.com/article/10.1007/s44371-024-00067-x]
- 66. in AI Statistics Drug : The $60 Billion Reality vs.... Development 2025 [https://www.allaboutai.com/resources/ai-statistics/drug-development/]
- 67. in Pharma and Biotech: Market Trends AI and Beyond 2025 [https://www.coherentsolutions.com/insights/artificial-intelligence-in-pharmaceuticals-and-biotechnology-current-trends-and-innovations]
- 68. How AI will reshape pharma in 2025 | Drug Target Review [https://www.drugtargetreview.com/article/154981/how-ai-will-reshape-pharma-by-2025/]
- 69. Material AI & Drug Discovery: AI Tech Report 2025 [https://brainxx.org/blog/material-ai-and-drug-discovery]
- 70. Cleaning Validation : A Practical ICH Guidelines Guide [https://www.leucine.io/cleaning-validation-blogs/cleaning-validation-ich-guidelines]
- 71. And ICH Method ANVISA Guidelines: Key... - PharmaGuru Validation [https://pharmaguru.co/ich-and-anvisa-method-validation-guidelines/]
- 72. qualitymatters. usp .org/what- usp - standard [https://qualitymatters.usp.org/what-usp-standard]
- 73. Requirements: Clear, Practical, Audit-Ready USP [https://pharmuni.com/2025/10/06/usp-requirements-clear-practical-audit-ready/]
- 74. USP and Chinese Pharmacopeia Extend Partnership to Improve Medicines Quality and Patient Safety | USP [https://www.usp.org/news/usp-and-chinese-pharmacopeia-extend-partnership-improve-medicines-quality-and-patient-safety]
- 75. Guidelines for the regulation of biologicals, biosimilars and radiopharmaceuticals in Brazil [https://gabionline.net/guidelines/guidelines-for-the-regulation-of-biologicals-biosimilars-and-radiopharmaceuticals-in-brazil]
- 76. Quality, Non-clinical and Clinical Considerations for Biosimilar Monoclonal Antibody Development: EU, WHO, USA, Canada, and BRICS-TM Regulatory Guidelines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6192287/]
- 77. All You Need to Know About the 2025 Q1 (Draft) ICH Guideline [https://www.linkedin.com/pulse/all-you-need-know-2025-ich-q1-draft-guideline-chandramouli-r-fmd1c]
- 78. Pharmacopeia & Metrological Institute Standards [https://www.sigmaaldrich.com/US/en/products/analytical-chemistry/reference-materials/pharmacopeia-and-metrological-institutes-standards]
- 79. Analytical Method Transfer: Best Practices and Guidelines | Lab Manager [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 80. Analytical method (module 01) | PPTX transfer [https://www.slideshare.net/slideshow/analytical-method-transfer-module-01/48996157]
- 81. Getting Analytical Method Validation, Verification & Transfer Right [https://www.complianceonline.com/resources/getting-the-analytical-method-validation-verification-and-transfer-right.html]
- 82. Analytical Method (USP 1224) Guideline - Pharma Beginners Transfer [https://pharmabeginers.com/analytical-method-transfer-usp1224-guideline/]
- 83. Analytical Method : step-by-step guide & best practices Transfer [https://www.qbdgroup.com/en/blog/analytical-method-transfer-steps]
- 84. Validation of Stability-Indicating HPLC Methods for Pharmaceuticals: Overview, Methodologies, and Case Studies | LCGC International [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 85. The Analytical Method Development and Validation: A Review | Journal of Drug Delivery and Therapeutics [https://jddtonline.info/index.php/jddt/article/view/2774]
- 86. -Analytical AGREE Metric Approach and Software GREEnness [https://pubmed.ncbi.nlm.nih.gov/32538619/]
- 87. —Analytical AGREE Metric Approach and... GREEnness [https://www.bohrium.com/paper-details/agree-analytical-greenness-metric-approach-and-software/812600291080798208-100657]
- 88. UPDATED REVIEW: VALIDATION AND METHOD... | PharmaTutor [https://www.pharmatutor.org/articles/updated-review-validation-method-validation-parameters]
- 89. HPLC Method Validation : Ensuring Accuracy and Regulatory... [https://www.mastelf.com/hplc-method-validation-ensuring-accuracy-and-regulatory-compliance/]
- 90. of Validation Methods for Analytical Employed in Drug... Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 91. Understanding biomarker , validation ... | TechTarget qualification [https://www.techtarget.com/pharmalifesciences/feature/Understanding-biomarker-validation-qualification-challenges]
- 92. of Analysis Bioanalysis Method Development and... Biomarker [https://www.linkedin.com/pulse/analysis-biomarker-bioanalysis-method-development-validation-]
- 93. FDA Guidance for Industry on Bioanalytical Method Validation (BMV) for Biomarkers [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 94. The Science of Biomarker : A Comprehensive... Assay Validation [https://www.linkedin.com/pulse/science-biomarker-assay-validation-comprehensive-qih5e]
- 95. Quantitative comparison of DNA methylation assays for biomarker ... [https://www.nature.com/articles/nbt.3605?error=cookies_not_supported]
- 96. processes of protein Validation in serum--a cross platform... biomarkers [https://pubmed.ncbi.nlm.nih.gov/23112739/]
- 97. Interlaboratory comparison of high-throughput protein biomarker ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0301418]